57e9db008b8b5bae105ff5f631836f32.ppt
- Количество слайдов: 37
 Hypertension in Adults Paul D. Simmons, MD Faculty Physician St. Mary’s Family Medicine Residency Program Grand Junction, Colorado
Hypertension in Adults Paul D. Simmons, MD Faculty Physician St. Mary’s Family Medicine Residency Program Grand Junction, Colorado
 Key Points • 1. Properly measure BP in the office setting: • • Position pt with back supported. Arm supported and at level of heart. Bladder width ⅔ upper arm length. Bladder length 80% of arm circumference. Lower edge of cuff 2 cm above antecubital space. Inflate cuff to 20 mm. Hg > SBP. Lower pressure at 2 -4 mm. Hg/sec.
Key Points • 1. Properly measure BP in the office setting: • • Position pt with back supported. Arm supported and at level of heart. Bladder width ⅔ upper arm length. Bladder length 80% of arm circumference. Lower edge of cuff 2 cm above antecubital space. Inflate cuff to 20 mm. Hg > SBP. Lower pressure at 2 -4 mm. Hg/sec.
 Key Points • • 2. Current classification of hypertension: • • • Normal <120 / 80 Prehypertension 120 -139 / 80 -89 Stage I HTN 140 -159 / 90 -99 Stage II HTN >160 / > 100 Isolated systolic HTN >140 / <90 Two or more abnormal readings at two or more visits.
Key Points • • 2. Current classification of hypertension: • • • Normal <120 / 80 Prehypertension 120 -139 / 80 -89 Stage I HTN 140 -159 / 90 -99 Stage II HTN >160 / > 100 Isolated systolic HTN >140 / <90 Two or more abnormal readings at two or more visits.
 Key Points • 3. Initial Evaluation of HTN • Is it primary (essential) or secondary? • What testing to get, if any? • BMP, lipids, glucose, H&H, UA with micro and EKG.
Key Points • 3. Initial Evaluation of HTN • Is it primary (essential) or secondary? • What testing to get, if any? • BMP, lipids, glucose, H&H, UA with micro and EKG.
 Key Points • 4. Pharmacologic Tx of HTN • • Don’t forget lifestyle modification! Classes of medications: • • • diuretics: HCTZ, chlorthalidone, furosemide, etc. ACEI/ARB: lisinopril, benazepril, losartan, etc. aldosterone antagonists: spironolactone, eplerenone, amiloride. sympatholytics: clonidine, methyldopa, reserpine, etc. B-blockers: metoprolol, propranolol, carvedilol, etc. alpha-blockers: prazosin, doxazosin, terazosin. CCBs: nifedipine, verapamil, diltiazem, etc. direct vasodilators: hydralazine, minoxidil. renin inhibitors: aliskiren.
Key Points • 4. Pharmacologic Tx of HTN • • Don’t forget lifestyle modification! Classes of medications: • • • diuretics: HCTZ, chlorthalidone, furosemide, etc. ACEI/ARB: lisinopril, benazepril, losartan, etc. aldosterone antagonists: spironolactone, eplerenone, amiloride. sympatholytics: clonidine, methyldopa, reserpine, etc. B-blockers: metoprolol, propranolol, carvedilol, etc. alpha-blockers: prazosin, doxazosin, terazosin. CCBs: nifedipine, verapamil, diltiazem, etc. direct vasodilators: hydralazine, minoxidil. renin inhibitors: aliskiren.
 Our Case • • A 70 -year-old woman with a long-standing history of hypertension comes for follow-up. Her medications include atenolol (100 mg daily), hydrochlorothiazide(12. 5 mg daily), lisinopril (40 mg daily), and ibuprofen (400 mg twice daily for osteoarthritis). She does not smoke or drink alcohol. Her body-mass index is 32. Her systolic and diastolic blood pressures (measured three times while she was seated) range from 164 to 170 mm Hg and 92 to 96 mm Hg, respectively, and the pulse rate is 72 per minute. N Engl J Med 355; 4
Our Case • • A 70 -year-old woman with a long-standing history of hypertension comes for follow-up. Her medications include atenolol (100 mg daily), hydrochlorothiazide(12. 5 mg daily), lisinopril (40 mg daily), and ibuprofen (400 mg twice daily for osteoarthritis). She does not smoke or drink alcohol. Her body-mass index is 32. Her systolic and diastolic blood pressures (measured three times while she was seated) range from 164 to 170 mm Hg and 92 to 96 mm Hg, respectively, and the pulse rate is 72 per minute. N Engl J Med 355; 4
 Hypertension Defined • • According to JNC-7 guideline, released 2004: • • Normal BP: <120/80 Prehypertension: 120 -139 / 80 -89 Stage I HTN: 140 -159 / 90 -99 Stage 2 HTN: >160 / >100 (1 x = dx) Two or more readings on two or more occasions (home or office!).
Hypertension Defined • • According to JNC-7 guideline, released 2004: • • Normal BP: <120/80 Prehypertension: 120 -139 / 80 -89 Stage I HTN: 140 -159 / 90 -99 Stage 2 HTN: >160 / >100 (1 x = dx) Two or more readings on two or more occasions (home or office!).
 Pathogenesis • Increased sympathetic activity and enhanced B-adrenergic responsiveness. • Increased AT II activity and mineralocorticoid excess. • Genetic factors (~30%). • Reduced adult nephron mass (aging, infections, congenital).
Pathogenesis • Increased sympathetic activity and enhanced B-adrenergic responsiveness. • Increased AT II activity and mineralocorticoid excess. • Genetic factors (~30%). • Reduced adult nephron mass (aging, infections, congenital).
 Risk Factors • • Black race. Parental hypertension. Increased salt intake: necessary but not sufficient. Excess alcohol intake. Obesity (main determinant in HTN w age). Dyslipidemia (independently of obesity). High fructose corn syrup (>2. 5 soft drinks/day), independent of obesity and lipids. Hostile, impatient, “type A” personality (i. e. , physicians).
Risk Factors • • Black race. Parental hypertension. Increased salt intake: necessary but not sufficient. Excess alcohol intake. Obesity (main determinant in HTN w age). Dyslipidemia (independently of obesity). High fructose corn syrup (>2. 5 soft drinks/day), independent of obesity and lipids. Hostile, impatient, “type A” personality (i. e. , physicians).
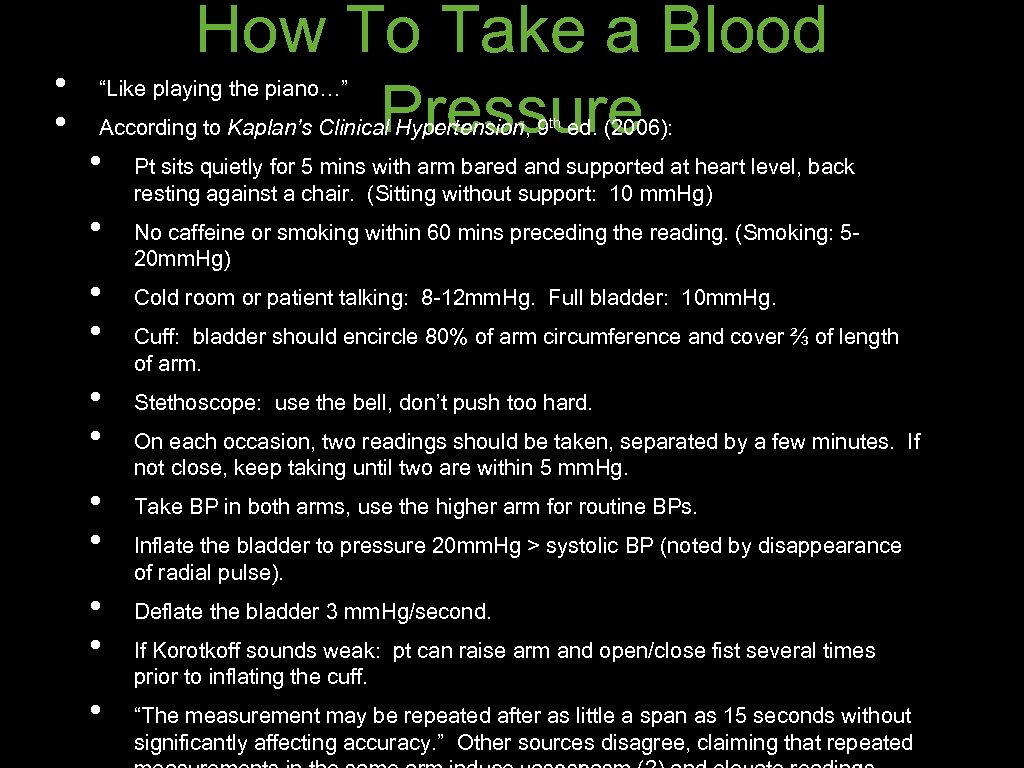 • • How To Take a Blood Pressure “Like playing the piano…” According to Kaplan’s Clinical Hypertension, 9 th ed. (2006): • • • Pt sits quietly for 5 mins with arm bared and supported at heart level, back resting against a chair. (Sitting without support: 10 mm. Hg) No caffeine or smoking within 60 mins preceding the reading. (Smoking: 520 mm. Hg) Cold room or patient talking: 8 -12 mm. Hg. Full bladder: 10 mm. Hg. Cuff: bladder should encircle 80% of arm circumference and cover ⅔ of length of arm. Stethoscope: use the bell, don’t push too hard. On each occasion, two readings should be taken, separated by a few minutes. If not close, keep taking until two are within 5 mm. Hg. Take BP in both arms, use the higher arm for routine BPs. Inflate the bladder to pressure 20 mm. Hg > systolic BP (noted by disappearance of radial pulse). Deflate the bladder 3 mm. Hg/second. If Korotkoff sounds weak: pt can raise arm and open/close fist several times prior to inflating the cuff. “The measurement may be repeated after as little a span as 15 seconds without significantly affecting accuracy. ” Other sources disagree, claiming that repeated
• • How To Take a Blood Pressure “Like playing the piano…” According to Kaplan’s Clinical Hypertension, 9 th ed. (2006): • • • Pt sits quietly for 5 mins with arm bared and supported at heart level, back resting against a chair. (Sitting without support: 10 mm. Hg) No caffeine or smoking within 60 mins preceding the reading. (Smoking: 520 mm. Hg) Cold room or patient talking: 8 -12 mm. Hg. Full bladder: 10 mm. Hg. Cuff: bladder should encircle 80% of arm circumference and cover ⅔ of length of arm. Stethoscope: use the bell, don’t push too hard. On each occasion, two readings should be taken, separated by a few minutes. If not close, keep taking until two are within 5 mm. Hg. Take BP in both arms, use the higher arm for routine BPs. Inflate the bladder to pressure 20 mm. Hg > systolic BP (noted by disappearance of radial pulse). Deflate the bladder 3 mm. Hg/second. If Korotkoff sounds weak: pt can raise arm and open/close fist several times prior to inflating the cuff. “The measurement may be repeated after as little a span as 15 seconds without significantly affecting accuracy. ” Other sources disagree, claiming that repeated
 Needless to say… this rarely happens.
Needless to say… this rarely happens.
 Sphygmomanometer s • Most accurate: mercury manometer with auscultatory method. • Aneroid: should be checked against Hg on occasion. • Automated oscillometric: readings typically lower, more error, and studies based on auscultatory method.
Sphygmomanometer s • Most accurate: mercury manometer with auscultatory method. • Aneroid: should be checked against Hg on occasion. • Automated oscillometric: readings typically lower, more error, and studies based on auscultatory method.
 Even with correct technique. . . • According to several large clinical trials and specialty clinic studies with drug titration protocols: • “. . . blood pressure goals may be difficult to achieve in as many as 40 percent of patients. ” N Engl J Med 355; 4
Even with correct technique. . . • According to several large clinical trials and specialty clinic studies with drug titration protocols: • “. . . blood pressure goals may be difficult to achieve in as many as 40 percent of patients. ” N Engl J Med 355; 4
 What About White • Coat Hypertension? Definition: elevated BPs at the office, normal BPs at home. • • • Prevalence 10 -20%, one study: up to ⅓ of patients! BP drops 10 -15 mm. Hg between 1 st and 3 rd visits in newly-diagnosed patients. Stable readings take 6 visits in some pts. It is not benign - we are NOT the most stressful thing in our patient’s life: • if it persists >3 visits, treat. If any evidence of end-organ damage (proteinuria, LVH), treat.
What About White • Coat Hypertension? Definition: elevated BPs at the office, normal BPs at home. • • • Prevalence 10 -20%, one study: up to ⅓ of patients! BP drops 10 -15 mm. Hg between 1 st and 3 rd visits in newly-diagnosed patients. Stable readings take 6 visits in some pts. It is not benign - we are NOT the most stressful thing in our patient’s life: • if it persists >3 visits, treat. If any evidence of end-organ damage (proteinuria, LVH), treat.
 Our Case (cont. ) • What physical exam findings should we look for?
Our Case (cont. ) • What physical exam findings should we look for?
 Our Case (cont. ) • Examination of her ocular fundi reveals arteriolar narrowing. The results of cardiovascular examination are normal. There are no abdominal bruits.
Our Case (cont. ) • Examination of her ocular fundi reveals arteriolar narrowing. The results of cardiovascular examination are normal. There are no abdominal bruits.
 • Initial Evaluation of HTN History and physical examination: • • • Cardiovascular risk factors, hyperthyroidism. Med review: steroids, OCPs, NSAIDs, decongestants, cyclosporine, others. Physical exam: laterally displaced or enlarged PMI, S 4, copper wire arteriopathy (2 disc diameters from disc), A-V nicking, flame hemorrhages, cotton-wool spots, papilledema, Osler’s sign in the elderly. Sadly: routine fundoscopy not supported by current evidence (BMJ 2005 Jul 9) Evidence of target-organ damage: CHF, angina, prior MI, stroke, CKD, PAD, retinopathy.
• Initial Evaluation of HTN History and physical examination: • • • Cardiovascular risk factors, hyperthyroidism. Med review: steroids, OCPs, NSAIDs, decongestants, cyclosporine, others. Physical exam: laterally displaced or enlarged PMI, S 4, copper wire arteriopathy (2 disc diameters from disc), A-V nicking, flame hemorrhages, cotton-wool spots, papilledema, Osler’s sign in the elderly. Sadly: routine fundoscopy not supported by current evidence (BMJ 2005 Jul 9) Evidence of target-organ damage: CHF, angina, prior MI, stroke, CKD, PAD, retinopathy.
 • • • Dietary/Lifestyle Modification Sodium restriction: • Cochrane 2003: short-term, may reduce BP (1 -5/0. 5 -2) in HTN pts, but no mortality, CV outcome improvement. Data poor quality, not consistent. DASH diet (high fiber, mod fat/prot, low sat fat/chol/sodium): BP -11/5. 5 mm. Hg and incidence of HTN. • • reduces lipid and homocysteine levels. reduced risk of CV mortality, MI, stroke (obs study). Other possible interventions: fiber, caffeine restriction, increased fruit/veggies, mod Et. OH intake, vit D, antioxidants, K/Mg, dark chocolate, garlic, Co. Q 10, omega-6 FA… Aerobic exercise: -4/2. 5 mm. Hg, dose dependent, reduces mainly DBP in elderly. Weight loss: 10# = -4/3 mm. Hg, proportional to wt loss, not wellmaintained.
• • • Dietary/Lifestyle Modification Sodium restriction: • Cochrane 2003: short-term, may reduce BP (1 -5/0. 5 -2) in HTN pts, but no mortality, CV outcome improvement. Data poor quality, not consistent. DASH diet (high fiber, mod fat/prot, low sat fat/chol/sodium): BP -11/5. 5 mm. Hg and incidence of HTN. • • reduces lipid and homocysteine levels. reduced risk of CV mortality, MI, stroke (obs study). Other possible interventions: fiber, caffeine restriction, increased fruit/veggies, mod Et. OH intake, vit D, antioxidants, K/Mg, dark chocolate, garlic, Co. Q 10, omega-6 FA… Aerobic exercise: -4/2. 5 mm. Hg, dose dependent, reduces mainly DBP in elderly. Weight loss: 10# = -4/3 mm. Hg, proportional to wt loss, not wellmaintained.
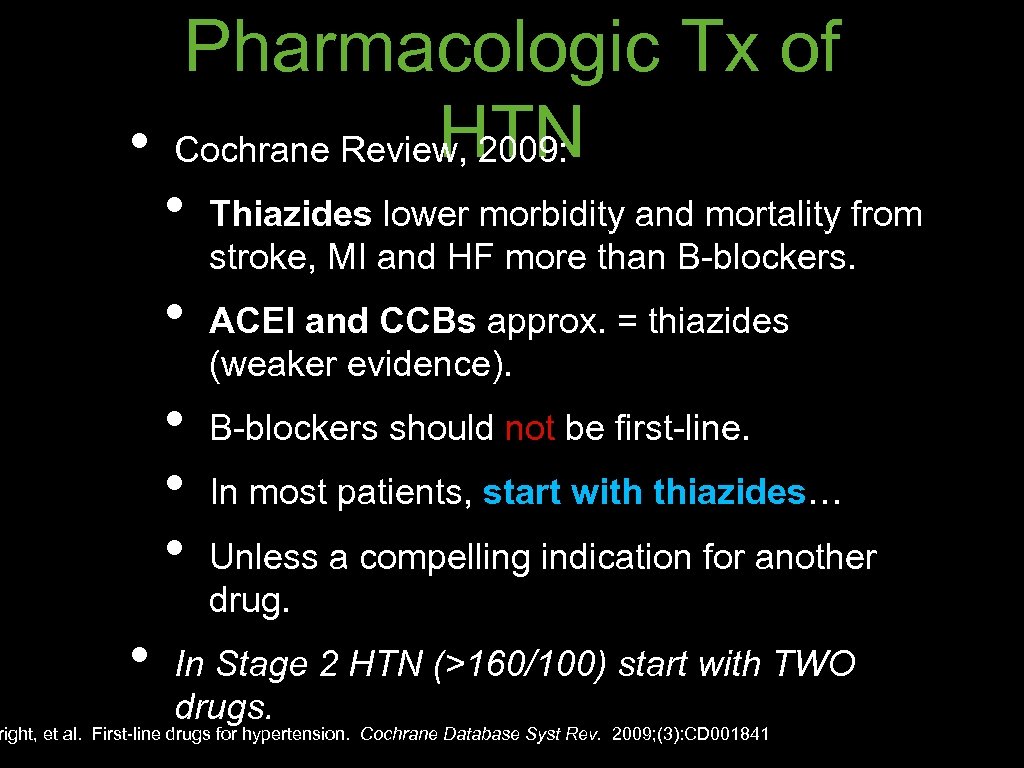 Pharmacologic Tx of HTN • Cochrane Review, 2009: • • • Thiazides lower morbidity and mortality from stroke, MI and HF more than B-blockers. ACEI and CCBs approx. = thiazides (weaker evidence). B-blockers should not be first-line. In most patients, start with thiazides… Unless a compelling indication for another drug. In Stage 2 HTN (>160/100) start with TWO drugs. right, et al. First-line drugs for hypertension. Cochrane Database Syst Rev. 2009; (3): CD 001841
Pharmacologic Tx of HTN • Cochrane Review, 2009: • • • Thiazides lower morbidity and mortality from stroke, MI and HF more than B-blockers. ACEI and CCBs approx. = thiazides (weaker evidence). B-blockers should not be first-line. In most patients, start with thiazides… Unless a compelling indication for another drug. In Stage 2 HTN (>160/100) start with TWO drugs. right, et al. First-line drugs for hypertension. Cochrane Database Syst Rev. 2009; (3): CD 001841
 “Compelling indications” Disease: Consider: Heart failure B-blocker, ACEI/ARB, aldo antag. Post-MI B-blocker, ACEI, aldo antag. CAD B-blocker, ACEI/ARB, CCB Diabetes B-blocker, ACEI/ARB, CCB CKD ACEI/ARB
“Compelling indications” Disease: Consider: Heart failure B-blocker, ACEI/ARB, aldo antag. Post-MI B-blocker, ACEI, aldo antag. CAD B-blocker, ACEI/ARB, CCB Diabetes B-blocker, ACEI/ARB, CCB CKD ACEI/ARB
 • • Our Case (cont. ) But our 70 year old woman is still uncontrolled on 3 meds (HCTZ, lisinopril and atenolol). What testing (if any) do you want to do?
• • Our Case (cont. ) But our 70 year old woman is still uncontrolled on 3 meds (HCTZ, lisinopril and atenolol). What testing (if any) do you want to do?
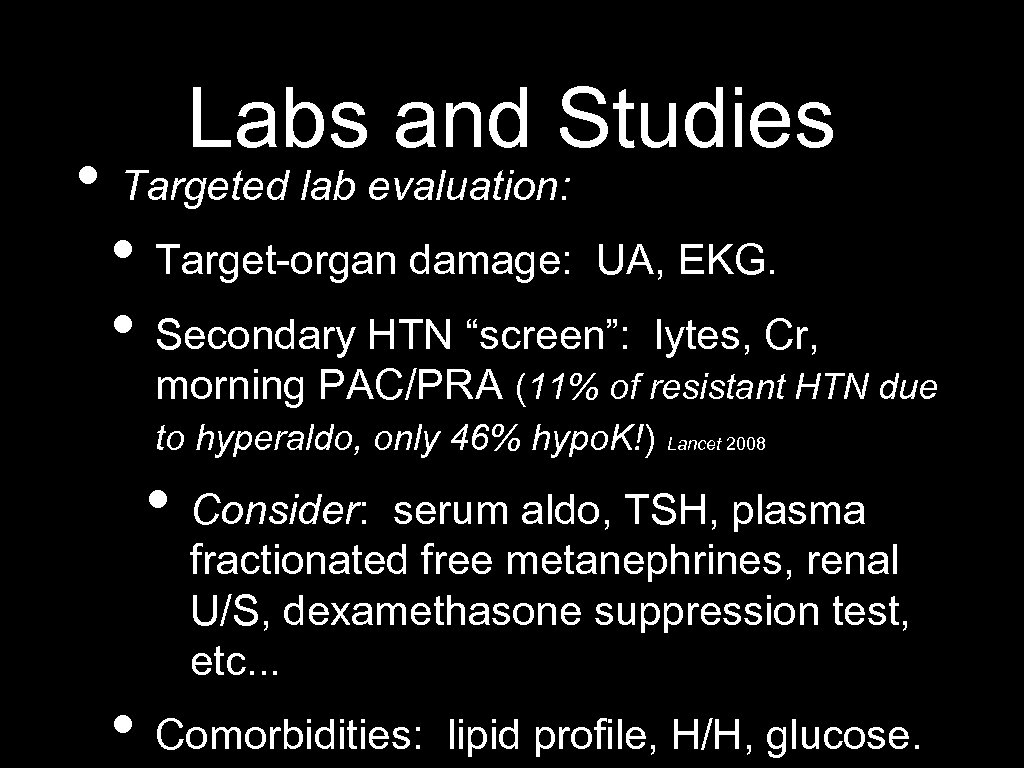 Labs and Studies • Targeted lab evaluation: • Target-organ damage: UA, EKG. • Secondary HTN “screen”: lytes, Cr, morning PAC/PRA (11% of resistant HTN due to hyperaldo, only 46% hypo. K!) Lancet 2008 • Consider: serum aldo, TSH, plasma fractionated free metanephrines, renal U/S, dexamethasone suppression test, etc. . . • Comorbidities: lipid profile, H/H, glucose.
Labs and Studies • Targeted lab evaluation: • Target-organ damage: UA, EKG. • Secondary HTN “screen”: lytes, Cr, morning PAC/PRA (11% of resistant HTN due to hyperaldo, only 46% hypo. K!) Lancet 2008 • Consider: serum aldo, TSH, plasma fractionated free metanephrines, renal U/S, dexamethasone suppression test, etc. . . • Comorbidities: lipid profile, H/H, glucose.
 Our Case (cont. ) • Serum potassium is 3. 8 m. Eq/L. • Serum creatinine level is 1. 2 mg/d. L • No microalbuminuria.
Our Case (cont. ) • Serum potassium is 3. 8 m. Eq/L. • Serum creatinine level is 1. 2 mg/d. L • No microalbuminuria.
 Difficult-to-treat HTN • Differential Diagnosis: • White-coat HTN • Non-adherence to medical plan • Interfering substances • Obesity / metabolic syndrome • Secondary causes
Difficult-to-treat HTN • Differential Diagnosis: • White-coat HTN • Non-adherence to medical plan • Interfering substances • Obesity / metabolic syndrome • Secondary causes
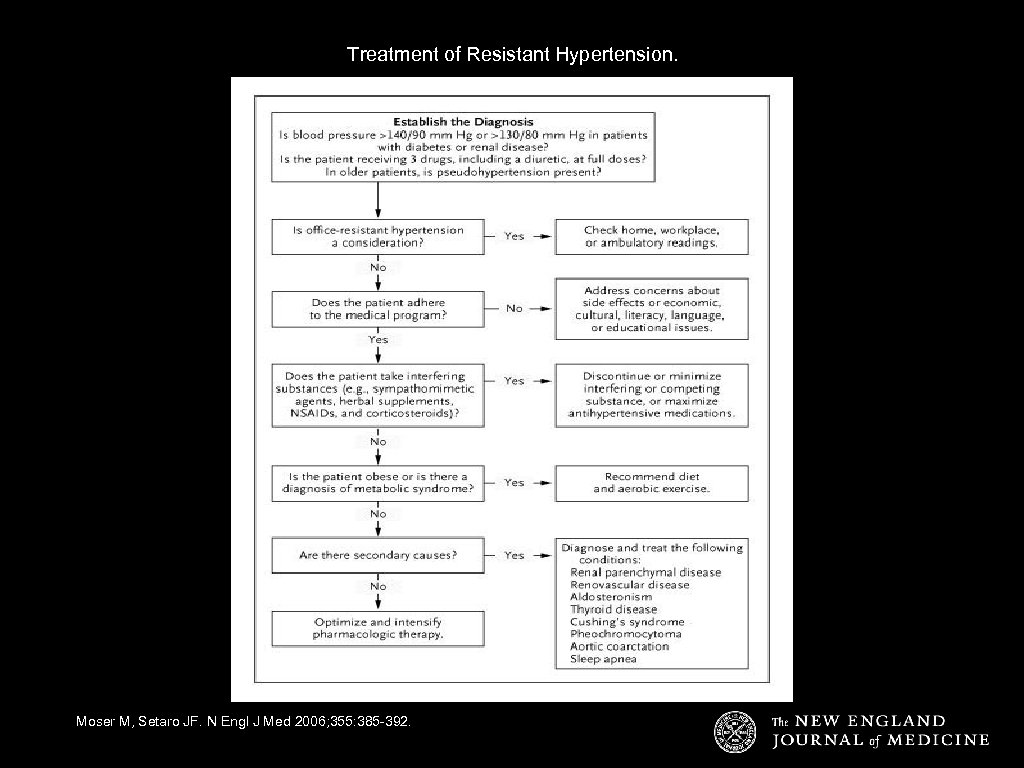 Treatment of Resistant Hypertension. Moser M, Setaro JF. N Engl J Med 2006; 355: 385 -392.
Treatment of Resistant Hypertension. Moser M, Setaro JF. N Engl J Med 2006; 355: 385 -392.
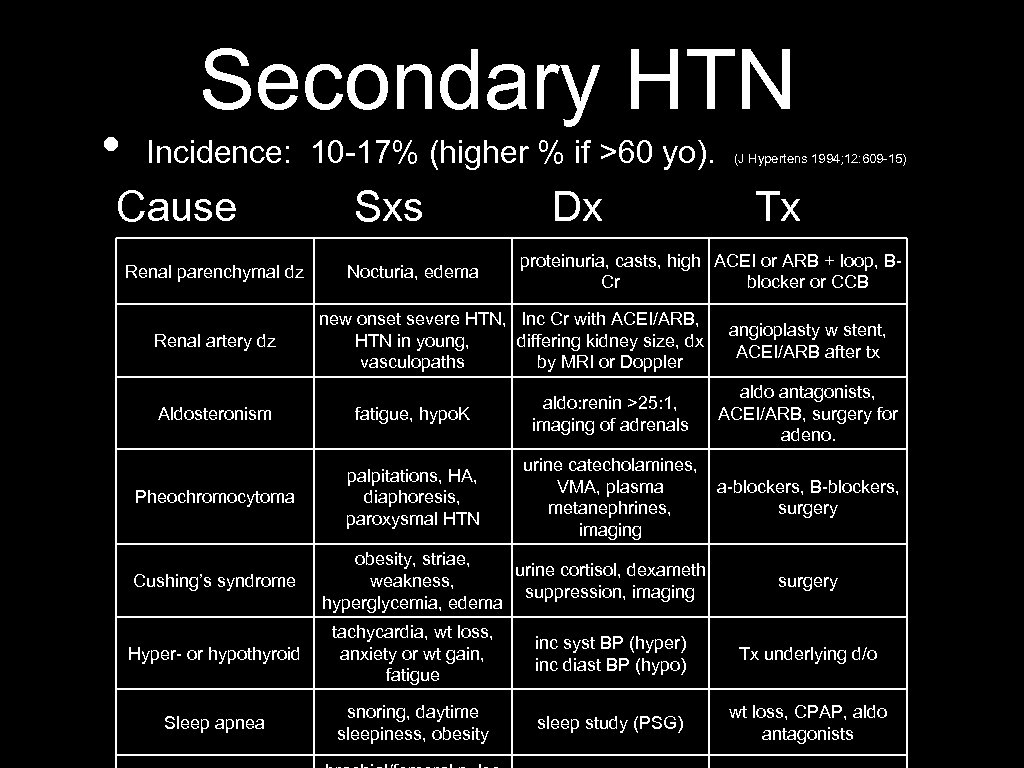 • Secondary HTN Incidence: 10 -17% (higher % if >60 yo). Cause Renal parenchymal dz Renal artery dz Sxs Nocturia, edema Dx Tx proteinuria, casts, high ACEI or ARB + loop, BCr blocker or CCB new onset severe HTN, Inc Cr with ACEI/ARB, HTN in young, differing kidney size, dx vasculopaths by MRI or Doppler Aldosteronism fatigue, hypo. K aldo: renin >25: 1, imaging of adrenals Pheochromocytoma palpitations, HA, diaphoresis, paroxysmal HTN urine catecholamines, VMA, plasma metanephrines, imaging Cushing’s syndrome (J Hypertens 1994; 12: 609 -15) obesity, striae, urine cortisol, dexameth weakness, suppression, imaging hyperglycemia, edema angioplasty w stent, ACEI/ARB after tx aldo antagonists, ACEI/ARB, surgery for adeno. a-blockers, B-blockers, surgery Hyper- or hypothyroid tachycardia, wt loss, anxiety or wt gain, fatigue inc syst BP (hyper) inc diast BP (hypo) Tx underlying d/o Sleep apnea snoring, daytime sleepiness, obesity sleep study (PSG) wt loss, CPAP, aldo antagonists
• Secondary HTN Incidence: 10 -17% (higher % if >60 yo). Cause Renal parenchymal dz Renal artery dz Sxs Nocturia, edema Dx Tx proteinuria, casts, high ACEI or ARB + loop, BCr blocker or CCB new onset severe HTN, Inc Cr with ACEI/ARB, HTN in young, differing kidney size, dx vasculopaths by MRI or Doppler Aldosteronism fatigue, hypo. K aldo: renin >25: 1, imaging of adrenals Pheochromocytoma palpitations, HA, diaphoresis, paroxysmal HTN urine catecholamines, VMA, plasma metanephrines, imaging Cushing’s syndrome (J Hypertens 1994; 12: 609 -15) obesity, striae, urine cortisol, dexameth weakness, suppression, imaging hyperglycemia, edema angioplasty w stent, ACEI/ARB after tx aldo antagonists, ACEI/ARB, surgery for adeno. a-blockers, B-blockers, surgery Hyper- or hypothyroid tachycardia, wt loss, anxiety or wt gain, fatigue inc syst BP (hyper) inc diast BP (hypo) Tx underlying d/o Sleep apnea snoring, daytime sleepiness, obesity sleep study (PSG) wt loss, CPAP, aldo antagonists
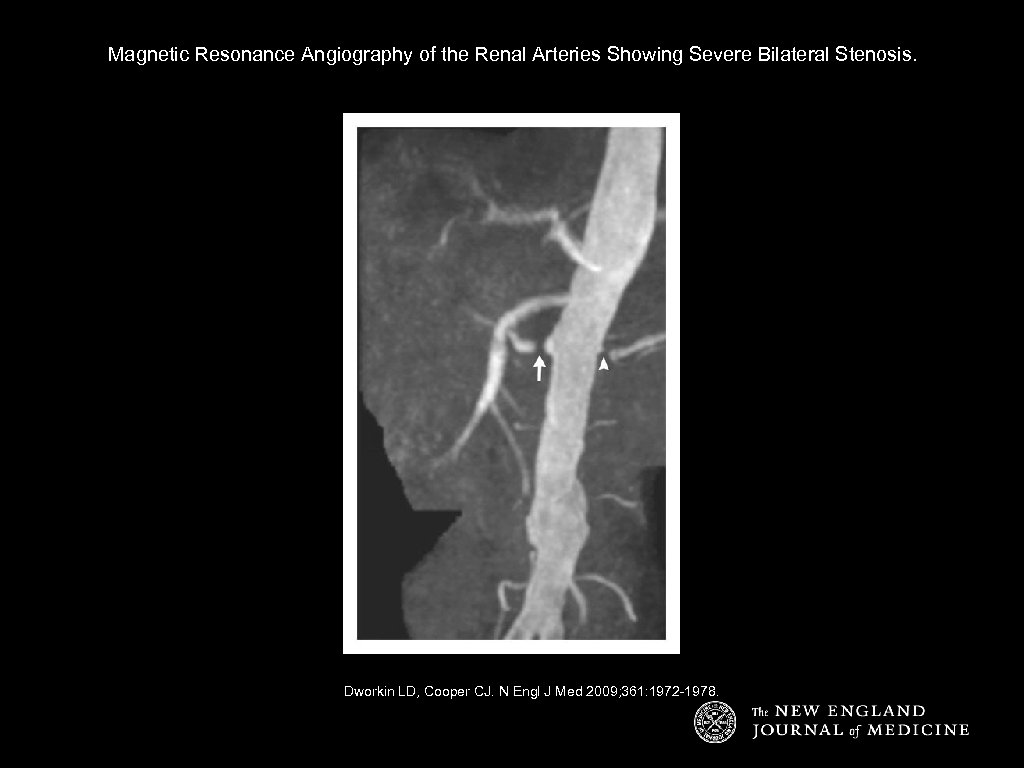 Magnetic Resonance Angiography of the Renal Arteries Showing Severe Bilateral Stenosis. Dworkin LD, Cooper CJ. N Engl J Med 2009; 361: 1972 -1978.
Magnetic Resonance Angiography of the Renal Arteries Showing Severe Bilateral Stenosis. Dworkin LD, Cooper CJ. N Engl J Med 2009; 361: 1972 -1978.
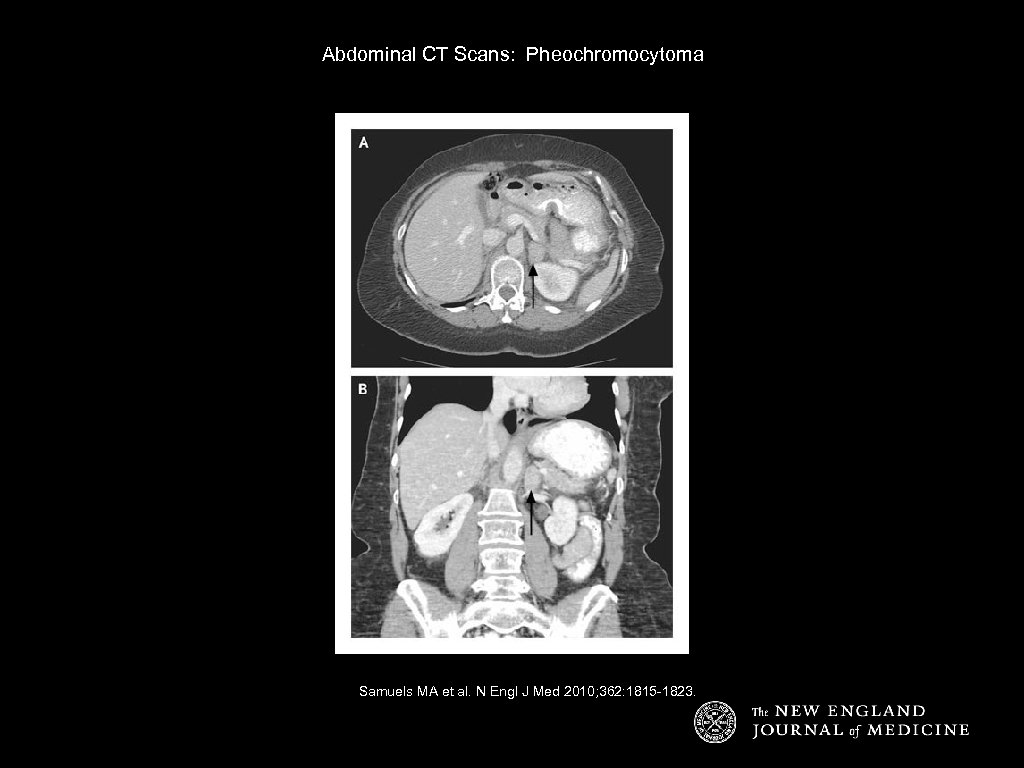 Abdominal CT Scans: Pheochromocytoma Samuels MA et al. N Engl J Med 2010; 362: 1815 -1823.
Abdominal CT Scans: Pheochromocytoma Samuels MA et al. N Engl J Med 2010; 362: 1815 -1823.
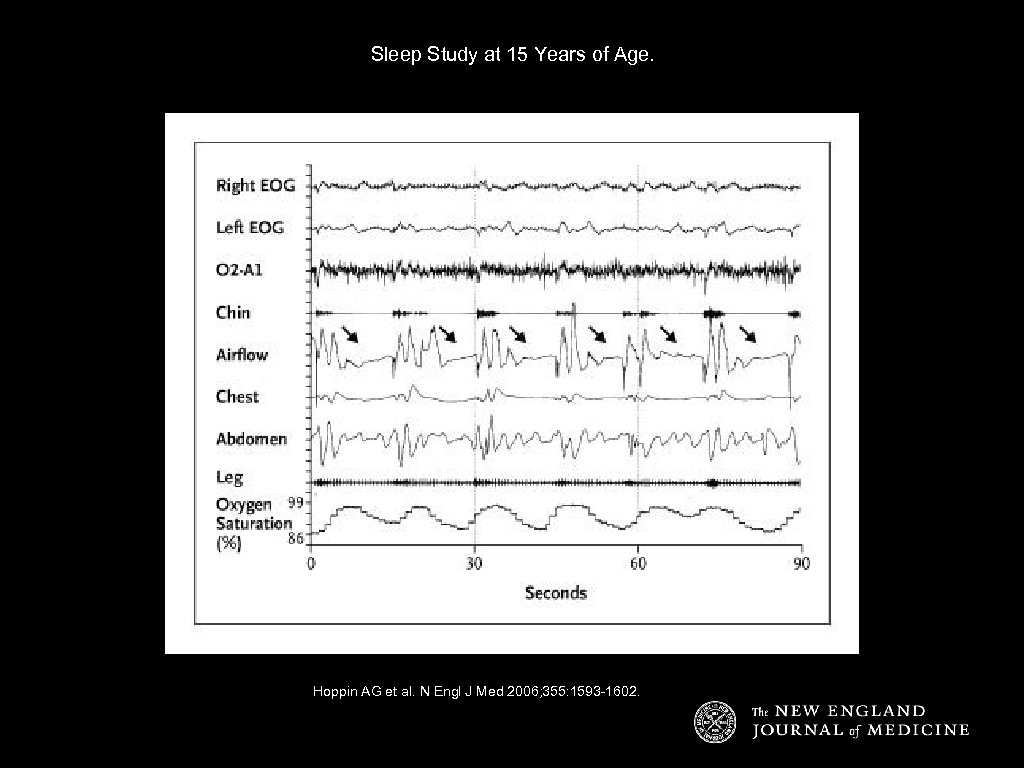 Sleep Study at 15 Years of Age. Hoppin AG et al. N Engl J Med 2006; 355: 1593 -1602.
Sleep Study at 15 Years of Age. Hoppin AG et al. N Engl J Med 2006; 355: 1593 -1602.
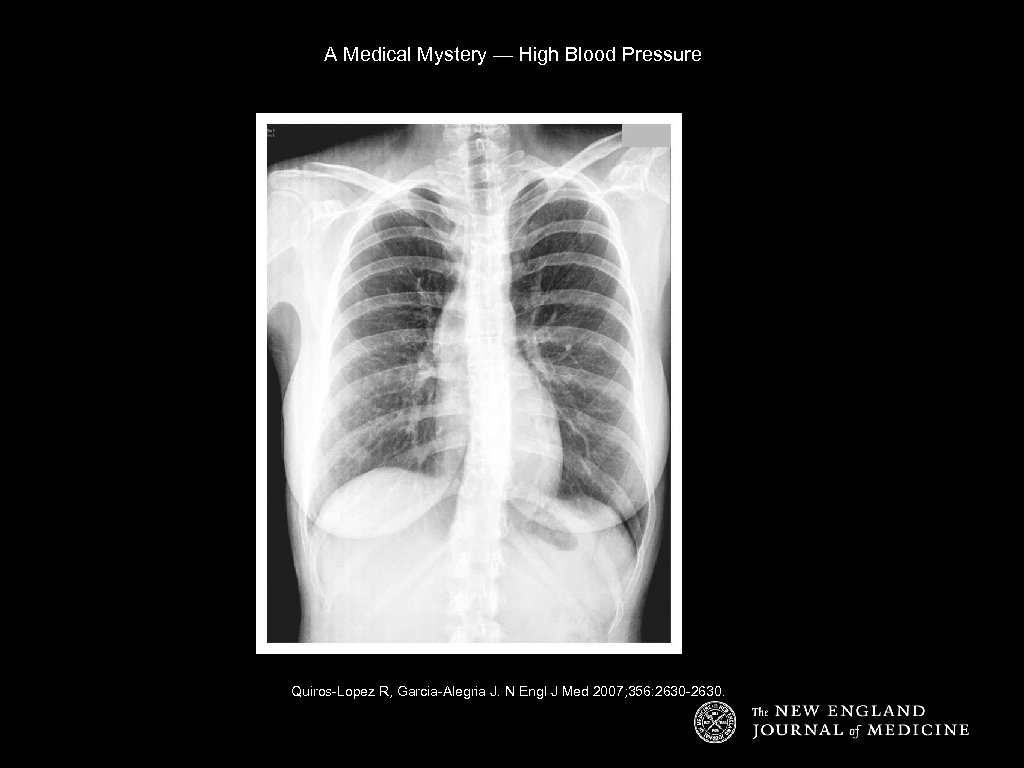 A Medical Mystery — High Blood Pressure Quiros-Lopez R, Garcia-Alegria J. N Engl J Med 2007; 356: 2630 -2630.
A Medical Mystery — High Blood Pressure Quiros-Lopez R, Garcia-Alegria J. N Engl J Med 2007; 356: 2630 -2630.
 • • Treatment of Resistant HTN Restrict Na+ intake. Adjust diuretic therapy based on pt’s renal function: • • If Cr <1. 5 - use a thiazide. If Cr >1. 5 - use a loop • use several times a day: intermittent natriuresis can cause reactive Na retention and worsen BP! Long-acting loop like torsemide is expensive. Use multiple classes: vasodilators (ACEI, DHP CCBs) + HR-lowering agents (Bblockers and non-DHP CCBs) + diuretics. “Last-ditch efforts” - consult a specialist while trying: • • • Combine alpha- and beta-blockers. Use dual CCBs (DHP and non-DHP). Combine ACEI and ARB (follow K and Cr closely!) Add centrally-acting agent (e. g. , clonidine). Add direct vasodilators (hydralazine or minoxidil).
• • Treatment of Resistant HTN Restrict Na+ intake. Adjust diuretic therapy based on pt’s renal function: • • If Cr <1. 5 - use a thiazide. If Cr >1. 5 - use a loop • use several times a day: intermittent natriuresis can cause reactive Na retention and worsen BP! Long-acting loop like torsemide is expensive. Use multiple classes: vasodilators (ACEI, DHP CCBs) + HR-lowering agents (Bblockers and non-DHP CCBs) + diuretics. “Last-ditch efforts” - consult a specialist while trying: • • • Combine alpha- and beta-blockers. Use dual CCBs (DHP and non-DHP). Combine ACEI and ARB (follow K and Cr closely!) Add centrally-acting agent (e. g. , clonidine). Add direct vasodilators (hydralazine or minoxidil).
 Our Case: The Plan • • 70 year old woman with resistant HTN, taking 3 drugs, with evidence of target-organ damage (retinopathy). Is she adherent? Discontinue ibuprofen. Encourage wt loss and Na restriction. Increase diuresis (and supplement K). Consider adding CCB. Consider screening for RAS (given her age).
Our Case: The Plan • • 70 year old woman with resistant HTN, taking 3 drugs, with evidence of target-organ damage (retinopathy). Is she adherent? Discontinue ibuprofen. Encourage wt loss and Na restriction. Increase diuresis (and supplement K). Consider adding CCB. Consider screening for RAS (given her age).
 Key Points • 1. Properly measure BP in the office setting: • • Position pt with back supported. Arm supported and at level of heart. Bladder width ⅔ upper arm length. Bladder length 80% of arm circumference. Lower edge of cuff 2 cm above antecubital space. Inflate cuff to 20 mm. Hg > SBP. Lower pressure at 2 -4 mm. Hg/sec.
Key Points • 1. Properly measure BP in the office setting: • • Position pt with back supported. Arm supported and at level of heart. Bladder width ⅔ upper arm length. Bladder length 80% of arm circumference. Lower edge of cuff 2 cm above antecubital space. Inflate cuff to 20 mm. Hg > SBP. Lower pressure at 2 -4 mm. Hg/sec.
 Key Points • • 2. Current classification of hypertension: • • • Normal <120 / 80 Prehypertension 120 -139 / 80 -89 Stage I HTN 140 -159 / 90 -99 Stage II HTN >160 / > 100 Isolated systolic HTN >140 / <90 Two or more abnormal readings at two or more visits.
Key Points • • 2. Current classification of hypertension: • • • Normal <120 / 80 Prehypertension 120 -139 / 80 -89 Stage I HTN 140 -159 / 90 -99 Stage II HTN >160 / > 100 Isolated systolic HTN >140 / <90 Two or more abnormal readings at two or more visits.
 Key Points • 3. Initial Evaluation of HTN • Is it primary or secondary? • What testing to get, if any? • BMP, lipids, glucose, H&H, UA with micro and EKG.
Key Points • 3. Initial Evaluation of HTN • Is it primary or secondary? • What testing to get, if any? • BMP, lipids, glucose, H&H, UA with micro and EKG.
 Key Points • 4. Pharmacologic Tx of HTN • • Don’t forget lifestyle modification! Classes of medications: • • • diuretics: HCTZ, chlorthalidone, furosemide, etc. ACEI/ARB: lisinopril, benazepril, losartan, etc. aldosterone antagonists: spironolactone, eplerenone, amiloride. sympatholytics: clonidine, methyldopa, reserpine, etc. B-blockers: metoprolol, propranolol, carvedilol, etc. alpha-blockers: prazosin, doxazosin, terazosin. CCBs: nifedipine, verapamil, diltiazem, etc. direct vasodilators: hydralazine, minoxidil. renin inhibitors: aliskiren.
Key Points • 4. Pharmacologic Tx of HTN • • Don’t forget lifestyle modification! Classes of medications: • • • diuretics: HCTZ, chlorthalidone, furosemide, etc. ACEI/ARB: lisinopril, benazepril, losartan, etc. aldosterone antagonists: spironolactone, eplerenone, amiloride. sympatholytics: clonidine, methyldopa, reserpine, etc. B-blockers: metoprolol, propranolol, carvedilol, etc. alpha-blockers: prazosin, doxazosin, terazosin. CCBs: nifedipine, verapamil, diltiazem, etc. direct vasodilators: hydralazine, minoxidil. renin inhibitors: aliskiren.
 Thanks for Listening!
Thanks for Listening!


