73cd9602d7500b7be9c94c164a05c23d.ppt
- Количество слайдов: 41
Hypersensitivity (超敏反应) Qingqing Wang Institute of Immunology Zhejiang University School Of Medicine wqq@zju. edu. cn
o Hypersensitivity Some immune responses can give rise to an excessive or inappropriate reaction, resulting in significant tissue damage or even death. o The classification: type I~IV
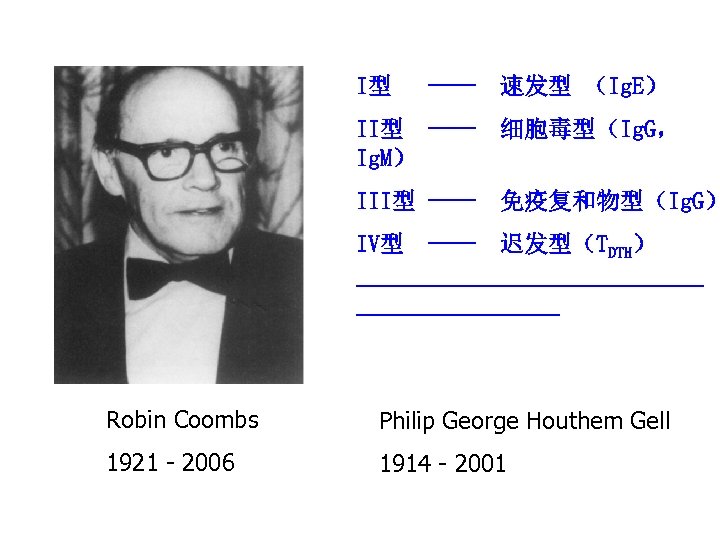
I型 ---- 速发型 (Ig. E) II型 ---- 细胞毒型(Ig. G, Ig. M) III型 ---- 免疫复和物型(Ig. G) IV型 ---- 迟发型(TDTH) ----------------------- Robin Coombs Philip George Houthem Gell 1921 - 2006 1914 - 2001
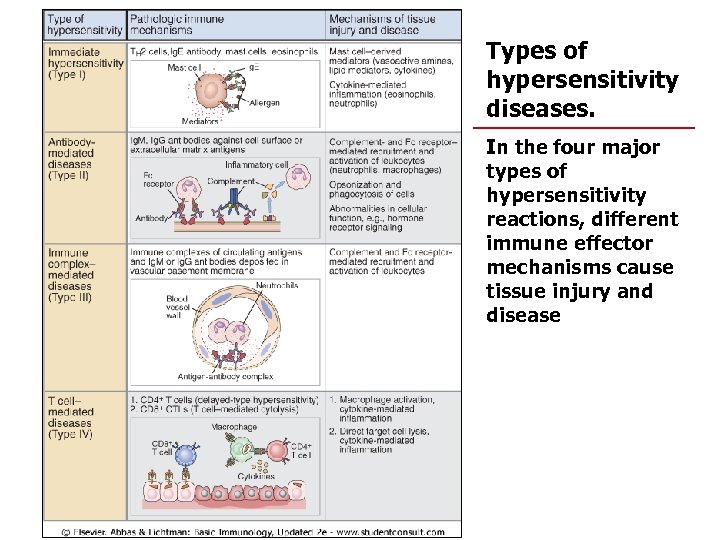
Types of hypersensitivity diseases. In the four major types of hypersensitivity reactions, different immune effector mechanisms cause tissue injury and disease
Type I hypersensitivity (immediate hypersensitivity)
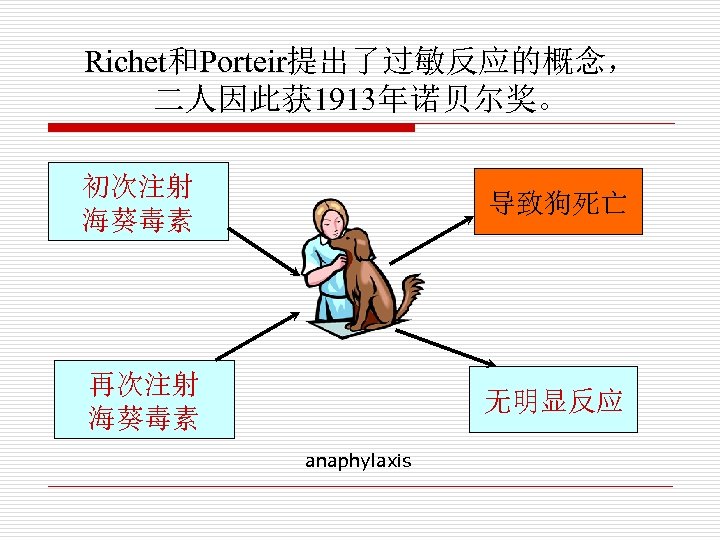
Richet和Porteir提出了过敏反应的概念, 二人因此获 1913年诺贝尔奖。 初次注射 海葵毒素 导致狗死亡 再次注射 海葵毒素 无明显反应 anaphylaxis
Type I hypersensitivity Carl Prausnitz-Giles 1876 -1963

1921 Prausnitz-Kustner test --- “reagin”
1966 Reagin = Ig. E Kimishige Ishizaka(1925 -)and Teruka Ishizaka
1. Characteristics of Type I hypersensitivity 1. Rapid: react and disappear quickly on re-exposure to Ag 2. Dysfunction: dysfunction rather than severe tissue and cell damage occurs 3. Strong hereditary tendency: obvious individual difference and genetic correlation
o o o Mediated by Ig. E antibodies Typical examples include polymorphisms of the promoter region for IL-4 and polymorphism of the gene for IL-5, either of which can directly influence the Ig. E production to allergens. ‘atopy’: An Ig. E-dependent allergy often arising from exposure to an unknown Ag.
II. Components involved in type I hypersensitivity o o Allergen is an antigen that gives rise to immediate hypersensitivity. protein or chemicals For example: pollen, house dust mite, animal hair, dander, some foods, foreign serum, drugs. Allergin is a specific Ig. E that gives rise to immediate hypersensitivity.
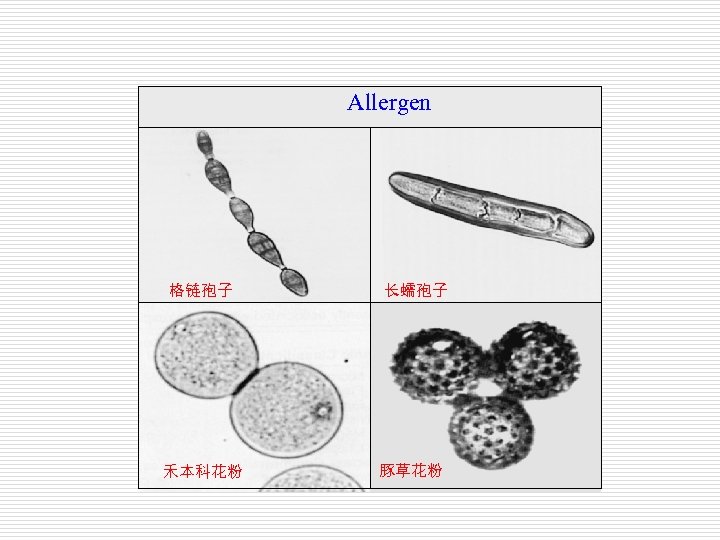
Allergen 格链孢子 禾本科花粉 长蠕孢子 豚草花粉
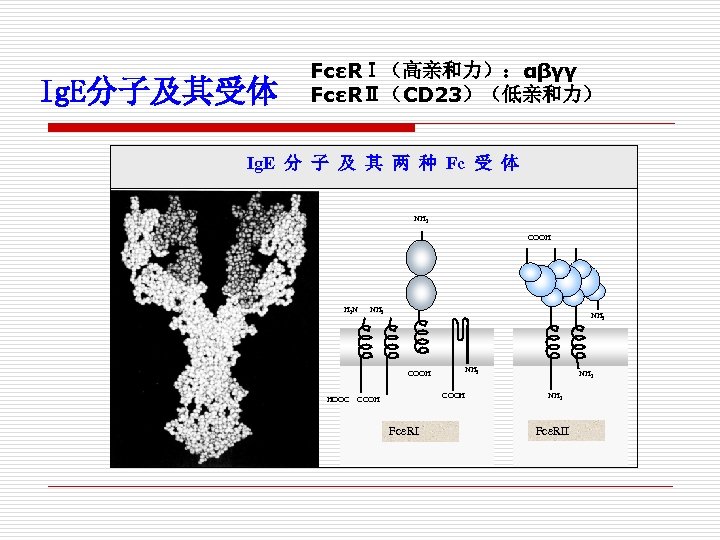
Ig. E分子及其受体 FcεRⅠ(高亲和力):αβγγ FcεRⅡ(CD 23)(低亲和力) Ig. E 分 子 及 其 两 种 Fc 受 体 NH 2 COOH H 2 N NH 2 COOH HOOC NH 2 COOH Fce. RI NH 2 Fce. RII
o o The majority of humans mount significant Ig. E response only as a defense against parasitic infections. After an individual has been exposed to a parasite, serum Ig. E levels increase and remain high until the parasite is successfully cleared from the body. Atopic individuals allow non-parasitic Ags to stimulate inappropriate Ig. E production, leading to type I hypersensitivity.
o Most allergic Ig. E response occur on mucous membrane surfaces in response to allergens that enter the body by either inhalation or ingestion.
• mast cells, basophils and eosinophils o o o Mast cells are found throughout connective tissue, particularly near blood and lymphatic vessels. Some tissues, including skin and mucous membrane surfaces of the respiratory and gastrointestinal tracts, contain high concentrations of mast cells. Basophils and eosinophils are granulocytes that circulate in the blood of most vertebrates.
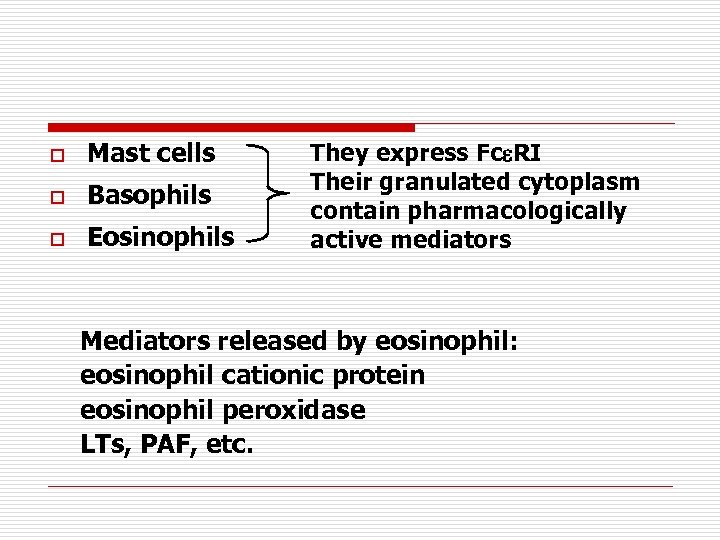
o Mast cells o Basophils o Eosinophils They express Fc RI Their granulated cytoplasm contain pharmacologically active mediators Mediators released by eosinophil: eosinophil cationic protein eosinophil peroxidase LTs, PAF, etc.
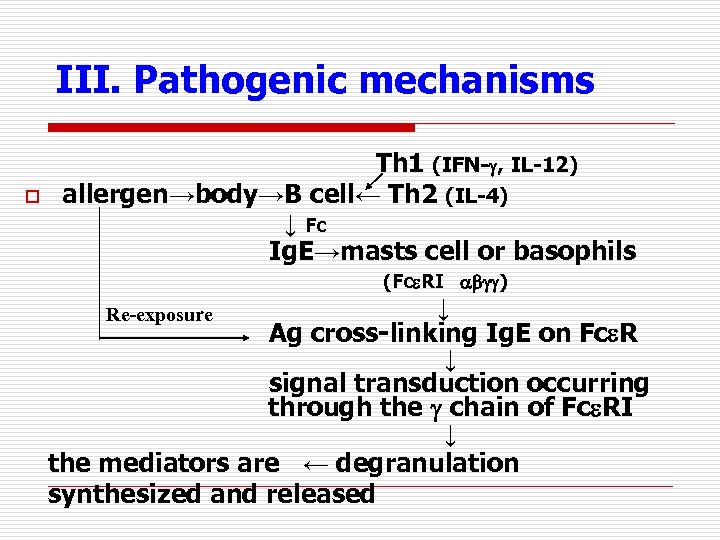
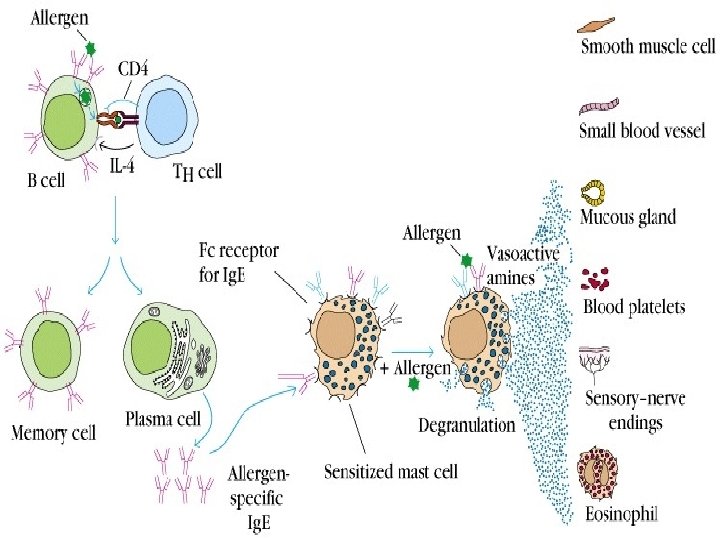
III. Pathogenic mechanisms o Th 1 (IFN- , IL-12) allergen→body→B cell← Th 2 (IL-4) ↓ Fc Ig. E→masts cell or basophils (Fc RI ) ↓ Ag cross-linking Ig. E on Fc R ↓ signal transduction occurring through the chain of Fc RI ↓ the mediators are ← degranulation synthesized and released Re-exposure
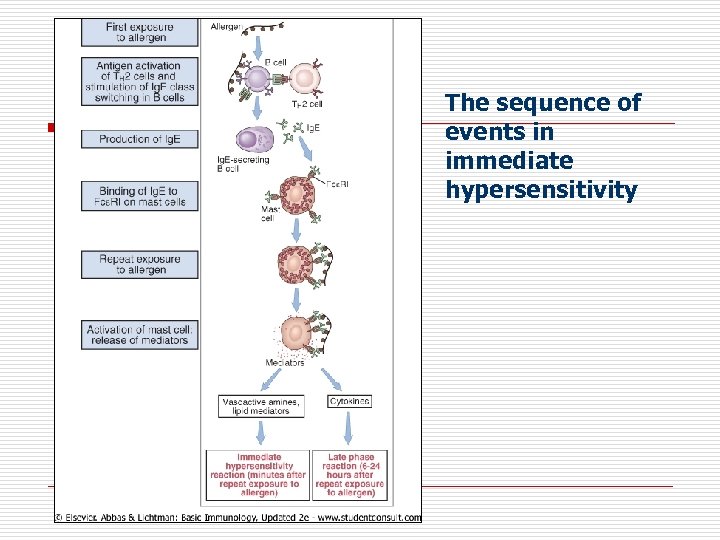
The sequence of events in immediate hypersensitivity
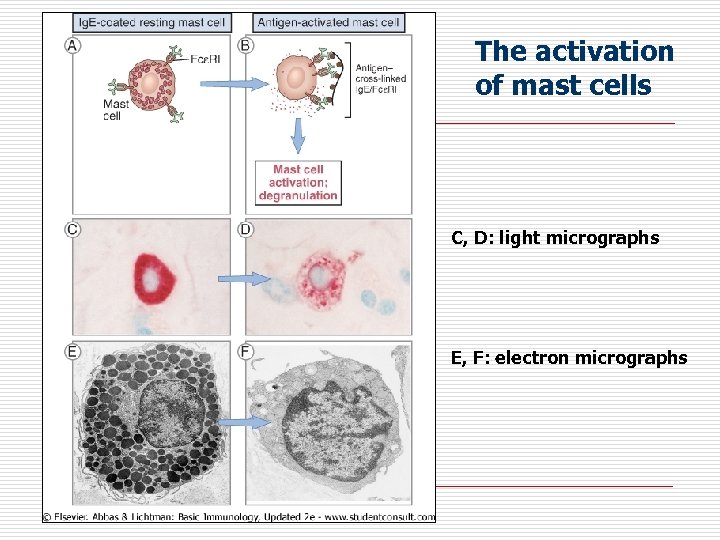
The activation of mast cells C, D: light micrographs E, F: electron micrographs
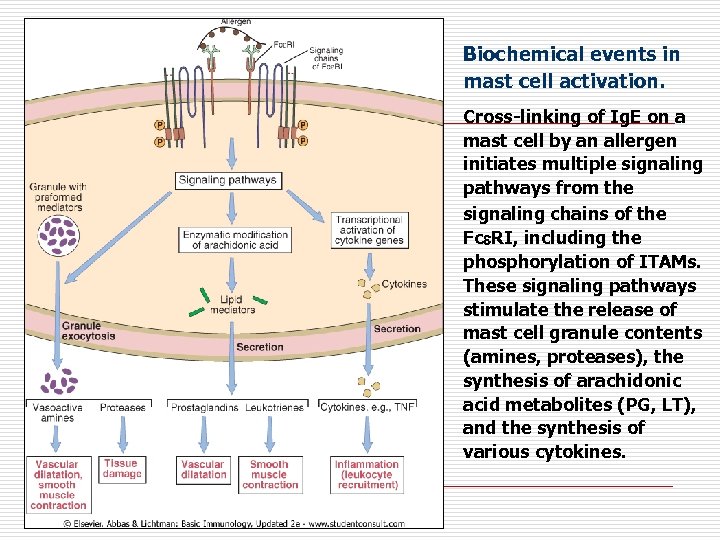
Biochemical events in mast cell activation. Cross-linking of Ig. E on a mast cell by an allergen initiates multiple signaling pathways from the signaling chains of the Fc RI, including the phosphorylation of ITAMs. These signaling pathways stimulate the release of mast cell granule contents (amines, proteases), the synthesis of arachidonic acid metabolites (PG, LT), and the synthesis of various cytokines.
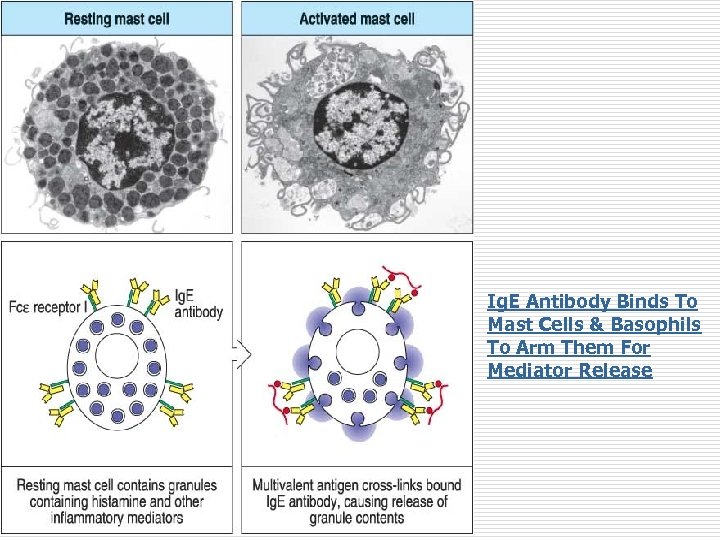
Ig. E Antibody Binds To Mast Cells & Basophils To Arm Them For Mediator Release
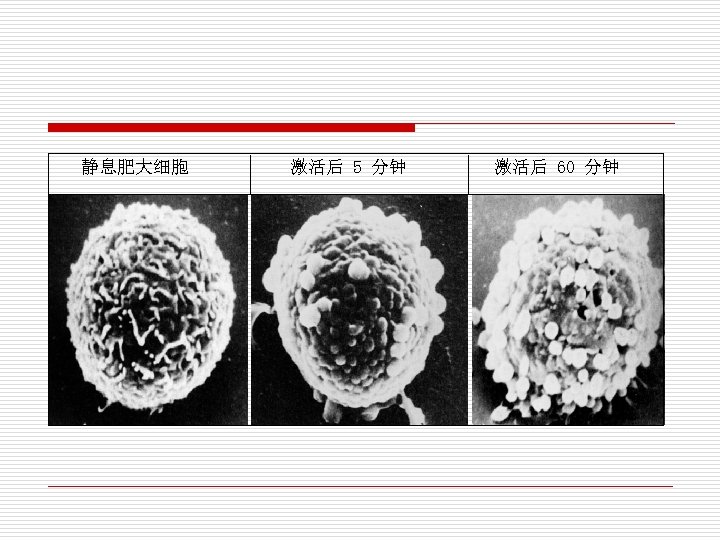
静息肥大细胞 激活后 5 分钟 激活后 60 分钟
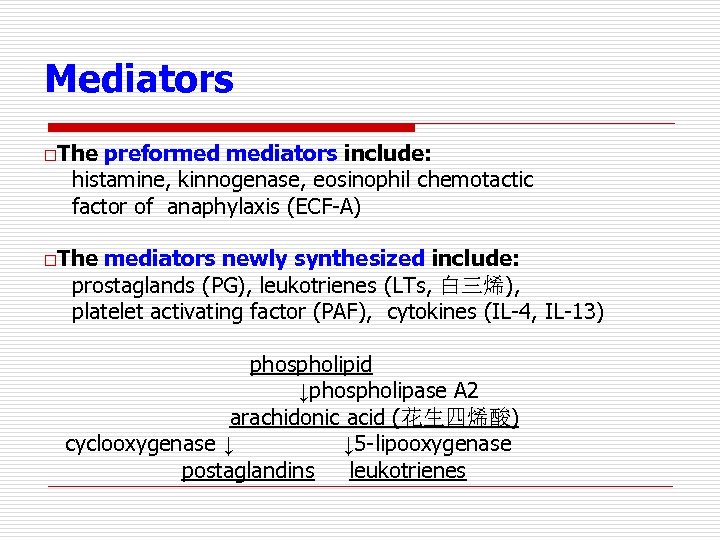
Mediators o. The preformed mediators include: histamine, kinnogenase, eosinophil chemotactic factor of anaphylaxis (ECF-A) o. The mediators newly synthesized include: prostaglands (PG), leukotrienes (LTs, 白三烯), platelet activating factor (PAF), cytokines (IL-4, IL-13) phospholipid ↓phospholipase A 2 arachidonic acid (花生四烯酸) cyclooxygenase ↓ ↓ 5 -lipooxygenase postaglandins leukotrienes
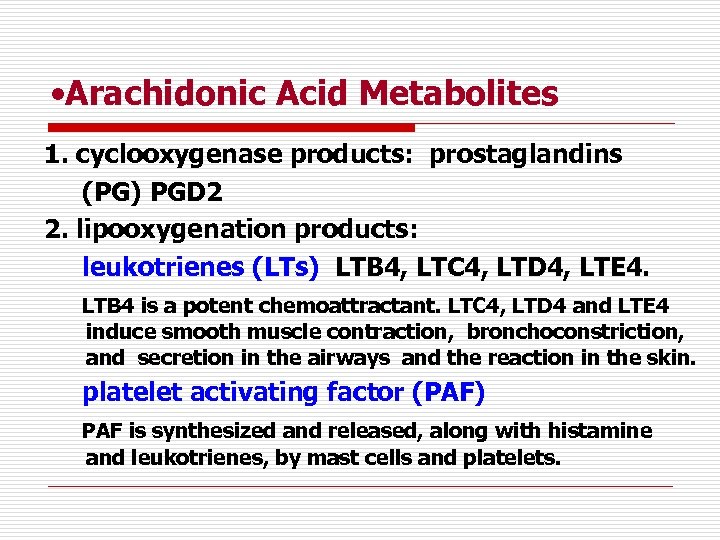
• Arachidonic Acid Metabolites 1. cyclooxygenase products: prostaglandins (PG) PGD 2 2. lipooxygenation products: leukotrienes (LTs) LTB 4, LTC 4, LTD 4, LTE 4. LTB 4 is a potent chemoattractant. LTC 4, LTD 4 and LTE 4 induce smooth muscle contraction, bronchoconstriction, and secretion in the airways and the reaction in the skin. platelet activating factor (PAF) PAF is synthesized and released, along with histamine and leukotrienes, by mast cells and platelets.
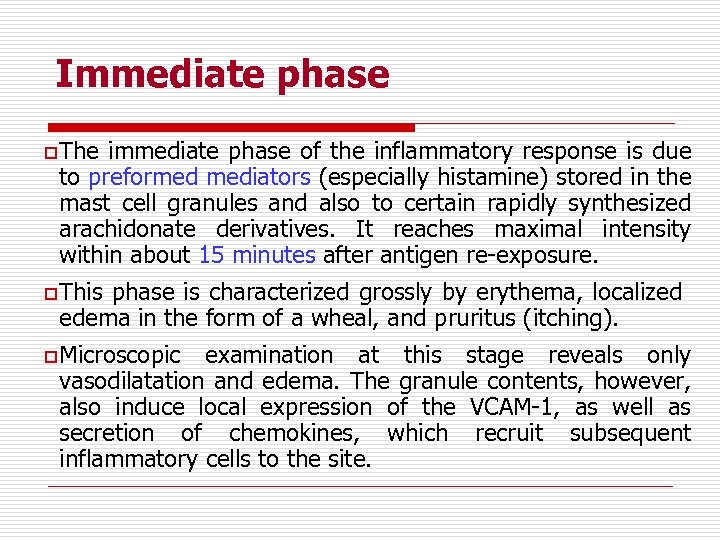
Immediate phase o The immediate phase of the inflammatory response is due to preformed mediators (especially histamine) stored in the mast cell granules and also to certain rapidly synthesized arachidonate derivatives. It reaches maximal intensity within about 15 minutes after antigen re-exposure. o This phase is characterized grossly by erythema, localized edema in the form of a wheal, and pruritus (itching). o Microscopic examination at this stage reveals only vasodilatation and edema. The granule contents, however, also induce local expression of the VCAM-1, as well as secretion of chemokines, which recruit subsequent inflammatory cells to the site.
Late phase o o o Manifestation of the late phase are due in part to presynthesized TNF- and in part to other mediators (principally PAF, LT, IL-4, etc. ) whose synthesis begins after the mast cell degranulates. The effects of these mediators become apparent about 6 hours after antigen contact and are marked by an infiltration of eosinophils and neutrophils. Clinical features of the late phase include erythema, induration, warmth, pruritus, and a burning sensation at the affected site. Fibrin deposition probably occurs transiently. TNF- not only functions in the short term as a leukocyte chemokine but also can stimulate local angiogenesis, fibroblast proliferation, and scar formation during prolonged hypersensitivity reactions.
IV. Type I hypersensitivityassociated diseases o The clinical manifestations of type I hypersensitivity can range from serious life-threatening conditions, such as systemic anaphylaxis and asthma, to hay fever (枯草热) and eczema(湿疹), which are merely annoying.
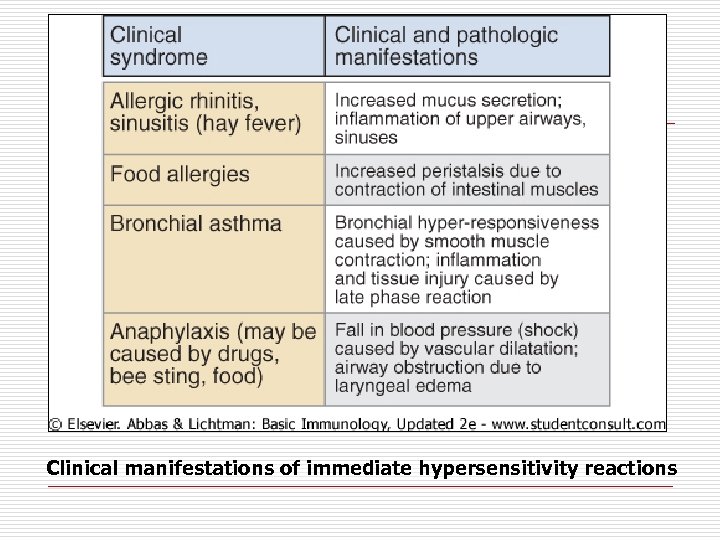
Clinical manifestations of immediate hypersensitivity reactions
1. Systemic anaphylaxis (shock) o o Systemic anaphylaxis is a shock-like and often fatal state whose onset occurs within minutes of a type I hypersensitivity reaction. If not treated quickly, these reactions can be fatal. Allergens: penicillin, antitoxin, etc.
2. Localized anaphylaxis (atopy) o Allergic rhinitis(过敏性鼻炎) It is the most common atopic disorders. It results from the reaction of airborne allergens with sensitized mast cells in the conjunctivae and nasal mucosa to induce the release of pharmacologically active mediators from the mast cells. These mediators then cause localized vasodilation and increased capillary permeability. The symptoms include watery exudation of the conjunctivae, nasal mucosa, and upper respiratory tract, as well as sneezing and coughing.
l o o Bronchial asthma In some cases, airborne or blood-borne allergens, such as pollens, dust, fumes, insect products, or viral antigens, trigger an asthmatic attack. Asthma is triggered by degranulation of mast cells with release of mediators, but instead of occurring in nasal mucosa, the reaction develops in the lower respiratory tract. The resulting contraction of bronchial smooth muscles leads to bronchoconstriction.
• Anaphylaxis to foods o o Various foods can induce localized anaphylaxis in allergic individuals. Allergen crosslinking of Ig. E on mast cells along the upper and lower gastrointestinal tract can induce localized smooth muscle contraction and vasodilation. Vomiting and diarrhea are the most common symptoms of food allergies.

荨麻疹
• Atopic dermatitis(特应性皮炎,湿疹) o o Atopic dermatitis is an inflammatory disease of skin that is frequently associated with a family history of atopy. The disease is observed most frequently in young children, often developing during infancy. The reaction is characterized by infiltration of neutrophils, eosinophils, macrophages, lymphocytes, and basophils. The localized late-phase response also may be mediated by cytokines released from mast cells.
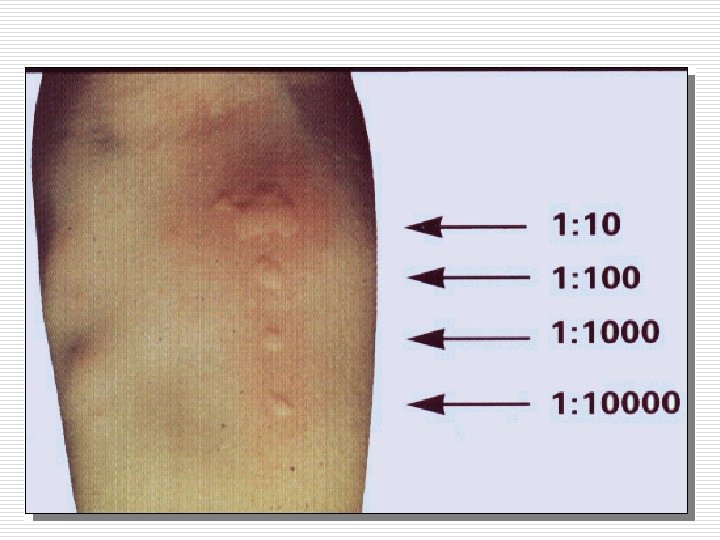
V. Immunoprophylaxis & immunotherapy 1. Skin test to identify allergen and avoid the offending allergen 2. Hyposensitization or desensitization with allergens 1) For antitoxin: stimulation with small dose of Ag provokes a minimal amount of mediators release, and the latter are rapidly resolved.
2) For specific allergens o o o Gradually increasing quantities of Ag are injected subcutaneously. This is a form of immunotherapy aimed at stimulating the production of Ig. G blocking antibody that binds the offending antigen and prevents its combining to Ig. E. The response to treatment includes an increase in Ig. G antibodies, a decrease in Ig. E antibodies in the serum.
Thanks for your attention! o o Thank you very much for your support and cooperation in my teaching If you have any question and suggestion, please feel free to contact me: wqq@zju. edu. cn
73cd9602d7500b7be9c94c164a05c23d.ppt