12c2e68bbcb5229fffaf32d2d77869c1.ppt
- Количество слайдов: 71
 Hypersensitivity Láng, Orsolya MD, Ph. D Dept. Genetics, Cell & Immunobiology, Semmelweis University Lecture ED 2015 www. dgci. sote. hu
Hypersensitivity Láng, Orsolya MD, Ph. D Dept. Genetics, Cell & Immunobiology, Semmelweis University Lecture ED 2015 www. dgci. sote. hu
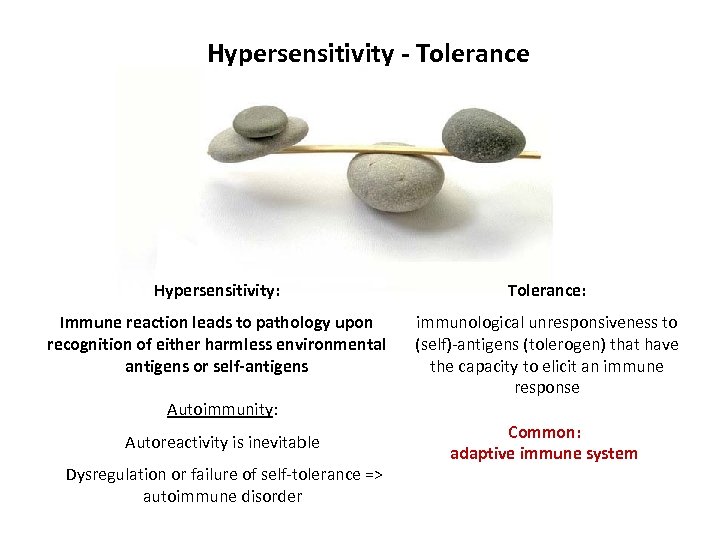 Hypersensitivity - Tolerance Hypersensitivity: Tolerance: Immune reaction leads to pathology upon recognition of either harmless environmental antigens or self-antigens immunological unresponsiveness to (self)-antigens (tolerogen) that have the capacity to elicit an immune response Autoimmunity: Autoreactivity is inevitable Dysregulation or failure of self-tolerance => autoimmune disorder Common: adaptive immune system
Hypersensitivity - Tolerance Hypersensitivity: Tolerance: Immune reaction leads to pathology upon recognition of either harmless environmental antigens or self-antigens immunological unresponsiveness to (self)-antigens (tolerogen) that have the capacity to elicit an immune response Autoimmunity: Autoreactivity is inevitable Dysregulation or failure of self-tolerance => autoimmune disorder Common: adaptive immune system
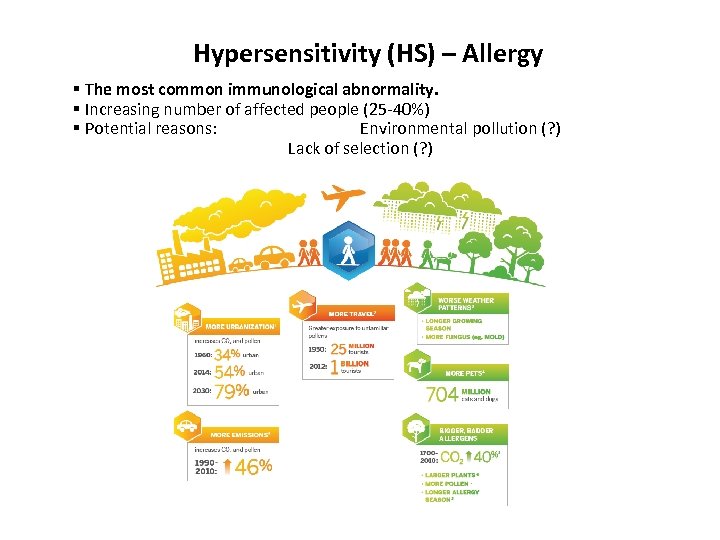 Hypersensitivity (HS) – Allergy § The most common immunological abnormality. § Increasing number of affected people (25 -40%) § Potential reasons: Environmental pollution (? ) Lack of selection (? )
Hypersensitivity (HS) – Allergy § The most common immunological abnormality. § Increasing number of affected people (25 -40%) § Potential reasons: Environmental pollution (? ) Lack of selection (? )
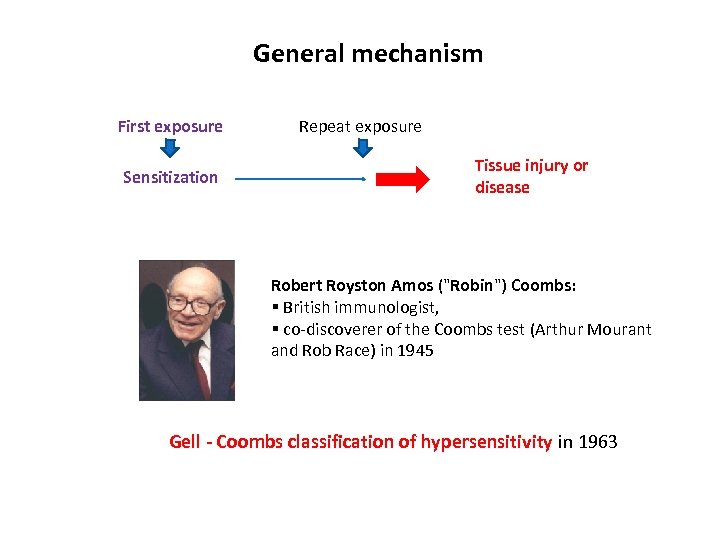 General mechanism First exposure Sensitization Repeat exposure Tissue injury or disease Robert Royston Amos ("Robin") Coombs: § British immunologist, § co-discoverer of the Coombs test (Arthur Mourant and Rob Race) in 1945 Gell - Coombs classification of hypersensitivity in 1963
General mechanism First exposure Sensitization Repeat exposure Tissue injury or disease Robert Royston Amos ("Robin") Coombs: § British immunologist, § co-discoverer of the Coombs test (Arthur Mourant and Rob Race) in 1945 Gell - Coombs classification of hypersensitivity in 1963
 Four classifications § § Type I (Immediate) hypersensitivity Type II (cytotoxic) hypersensitivity Type III (immune complex mediated) hypersensitivity Type IV (delayed) hypersensitivity
Four classifications § § Type I (Immediate) hypersensitivity Type II (cytotoxic) hypersensitivity Type III (immune complex mediated) hypersensitivity Type IV (delayed) hypersensitivity
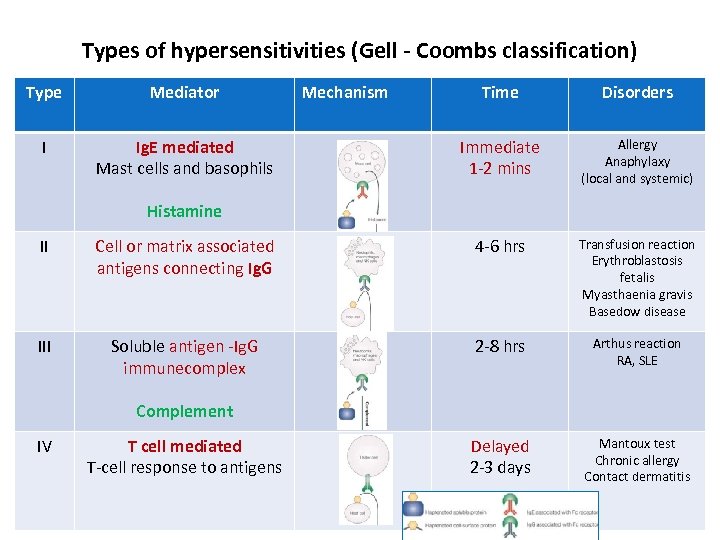 Types of hypersensitivities (Gell - Coombs classification) Type Mediator I Ig. E mediated Mast cells and basophils Mechanism Time Disorders Immediate 1 -2 mins Allergy Anaphylaxy (local and systemic) Histamine II Cell or matrix associated antigens connecting Ig. G 4 -6 hrs Transfusion reaction Erythroblastosis fetalis Myasthaenia gravis Basedow disease III Soluble antigen -Ig. G immunecomplex 2 -8 hrs Arthus reaction RA, SLE Delayed 2 -3 days Mantoux test Chronic allergy Contact dermatitis Complement IV T cell mediated T-cell response to antigens
Types of hypersensitivities (Gell - Coombs classification) Type Mediator I Ig. E mediated Mast cells and basophils Mechanism Time Disorders Immediate 1 -2 mins Allergy Anaphylaxy (local and systemic) Histamine II Cell or matrix associated antigens connecting Ig. G 4 -6 hrs Transfusion reaction Erythroblastosis fetalis Myasthaenia gravis Basedow disease III Soluble antigen -Ig. G immunecomplex 2 -8 hrs Arthus reaction RA, SLE Delayed 2 -3 days Mantoux test Chronic allergy Contact dermatitis Complement IV T cell mediated T-cell response to antigens
 Type I. hypersensitivity (HS) Immediate HS or Allergy , Atopy – inherited tendency to respond immunologically to inhaled or ingested allergens with increased Ig. E production
Type I. hypersensitivity (HS) Immediate HS or Allergy , Atopy – inherited tendency to respond immunologically to inhaled or ingested allergens with increased Ig. E production
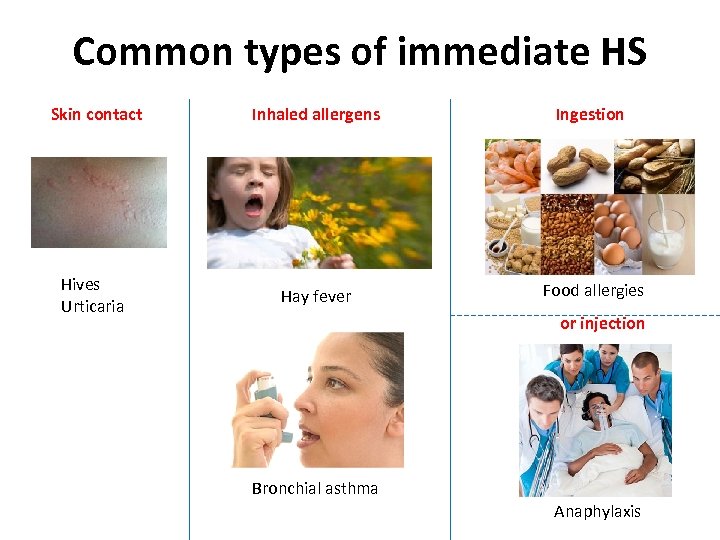 Common types of immediate HS Skin contact Inhaled allergens Ingestion Hives Urticaria Hay fever Food allergies or injection Bronchial asthma Anaphylaxis
Common types of immediate HS Skin contact Inhaled allergens Ingestion Hives Urticaria Hay fever Food allergies or injection Bronchial asthma Anaphylaxis
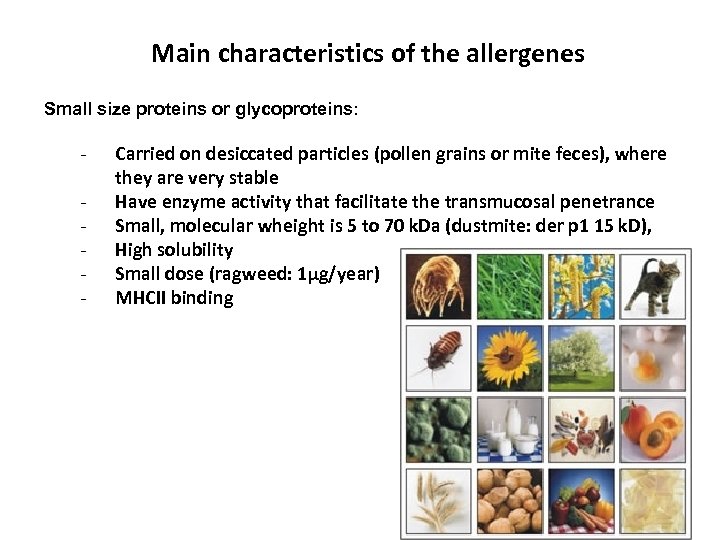 Main characteristics of the allergenes Small size proteins or glycoproteins: - Carried on desiccated particles (pollen grains or mite feces), where they are very stable Have enzyme activity that facilitate the transmucosal penetrance Small, molecular wheight is 5 to 70 k. Da (dustmite: der p 1 15 k. D), High solubility Small dose (ragweed: 1µg/year) MHCII binding
Main characteristics of the allergenes Small size proteins or glycoproteins: - Carried on desiccated particles (pollen grains or mite feces), where they are very stable Have enzyme activity that facilitate the transmucosal penetrance Small, molecular wheight is 5 to 70 k. Da (dustmite: der p 1 15 k. D), High solubility Small dose (ragweed: 1µg/year) MHCII binding
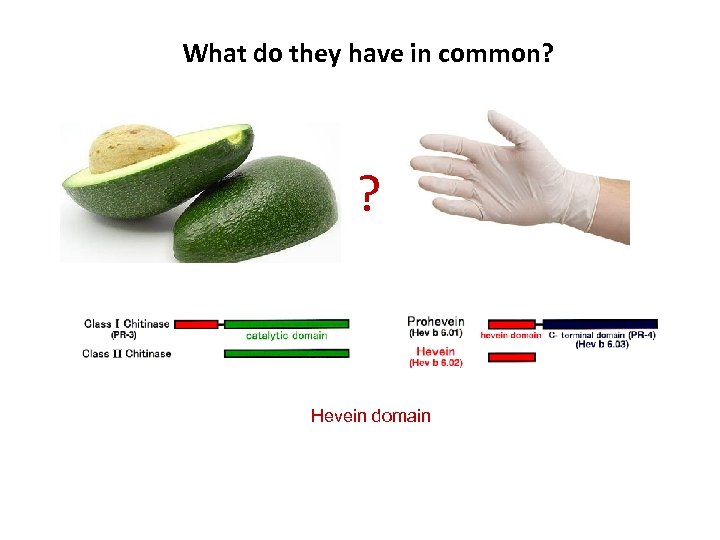 What do they have in common? ? Hevein domain
What do they have in common? ? Hevein domain
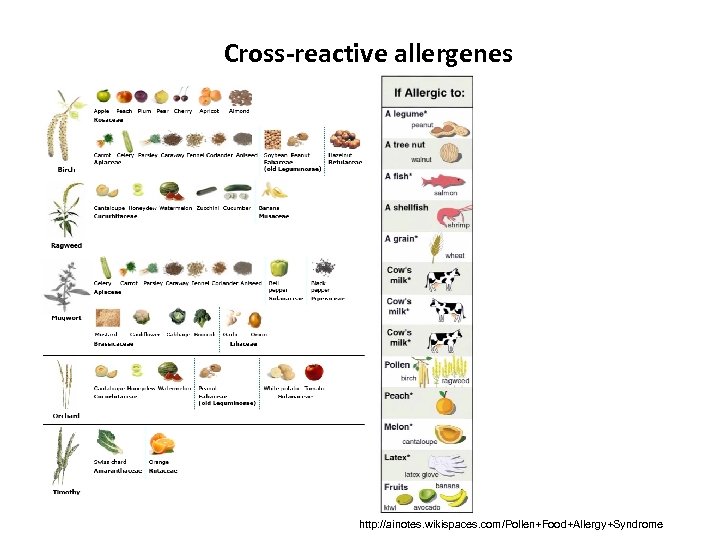 Cross-reactive allergenes http: //ainotes. wikispaces. com/Pollen+Food+Allergy+Syndrome
Cross-reactive allergenes http: //ainotes. wikispaces. com/Pollen+Food+Allergy+Syndrome
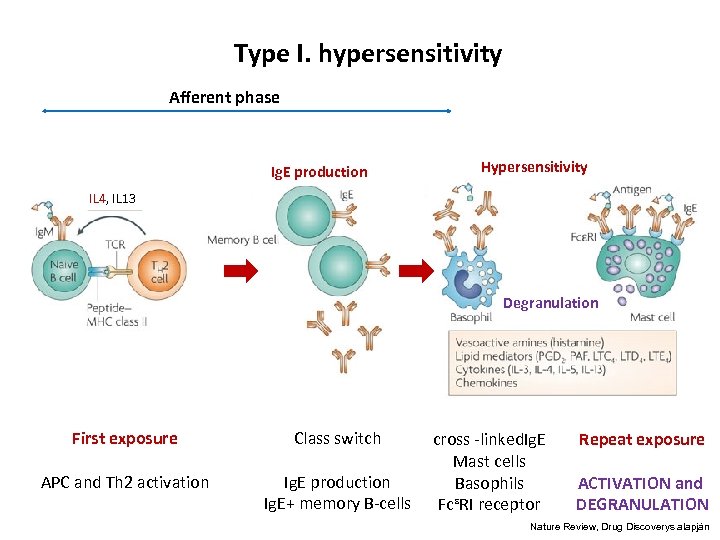 Type I. hypersensitivity Afferent phase Ig. E production Hypersensitivity IL 4, IL 13 Degranulation First exposure Class switch APC and Th 2 activation Ig. E production Ig. E+ memory B-cells cross -linked. Ig. E Mast cells Basophils FcᵋRI receptor Repeat exposure ACTIVATION and DEGRANULATION Nature Review, Drug Discoverys alapján
Type I. hypersensitivity Afferent phase Ig. E production Hypersensitivity IL 4, IL 13 Degranulation First exposure Class switch APC and Th 2 activation Ig. E production Ig. E+ memory B-cells cross -linked. Ig. E Mast cells Basophils FcᵋRI receptor Repeat exposure ACTIVATION and DEGRANULATION Nature Review, Drug Discoverys alapján
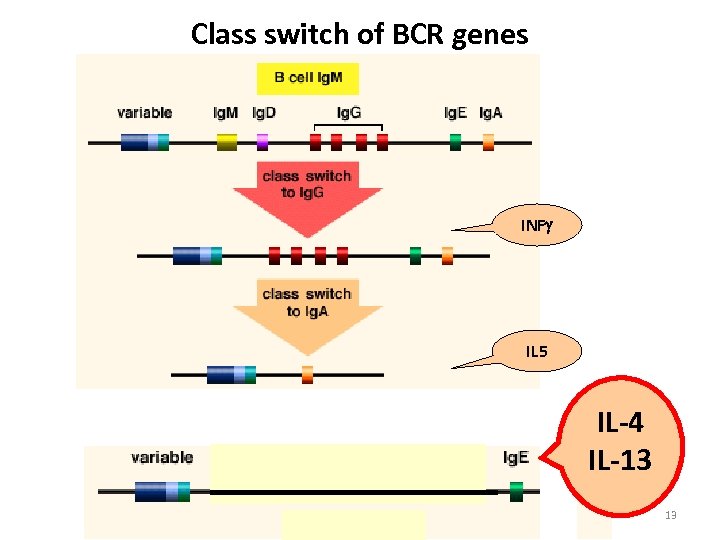 Class switch of BCR genes INF IL 5 IL-4 IL-13 13
Class switch of BCR genes INF IL 5 IL-4 IL-13 13
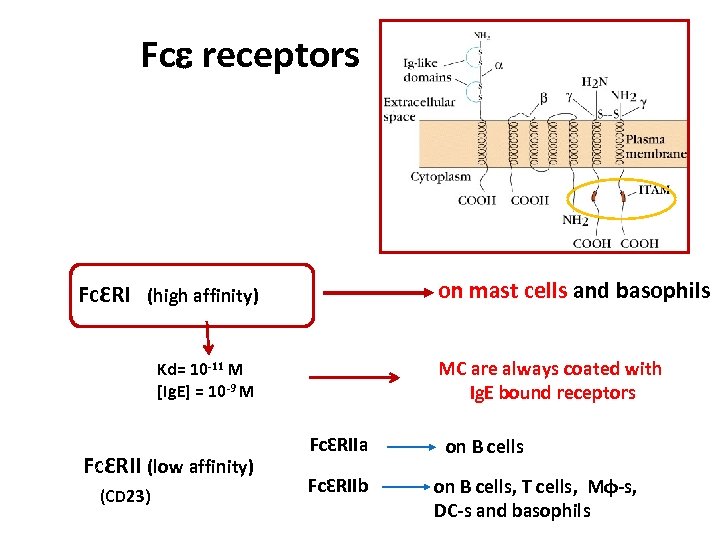 Fce receptors on mast cells and basophils FcƐRI (high affinity) MC are always coated with Ig. E bound receptors Kd= 10 -11 M [Ig. E] = 10 -9 M FcƐRII (low affinity) (CD 23) FcƐRIIa FcƐRIIb on B cells, T cells, Mφ-s, DC-s and basophils
Fce receptors on mast cells and basophils FcƐRI (high affinity) MC are always coated with Ig. E bound receptors Kd= 10 -11 M [Ig. E] = 10 -9 M FcƐRII (low affinity) (CD 23) FcƐRIIa FcƐRIIb on B cells, T cells, Mφ-s, DC-s and basophils
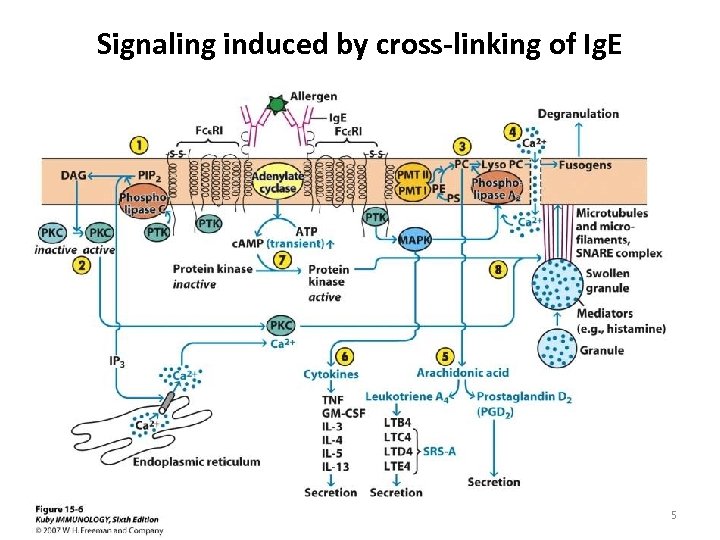 Signaling induced by cross-linking of Ig. E 15
Signaling induced by cross-linking of Ig. E 15
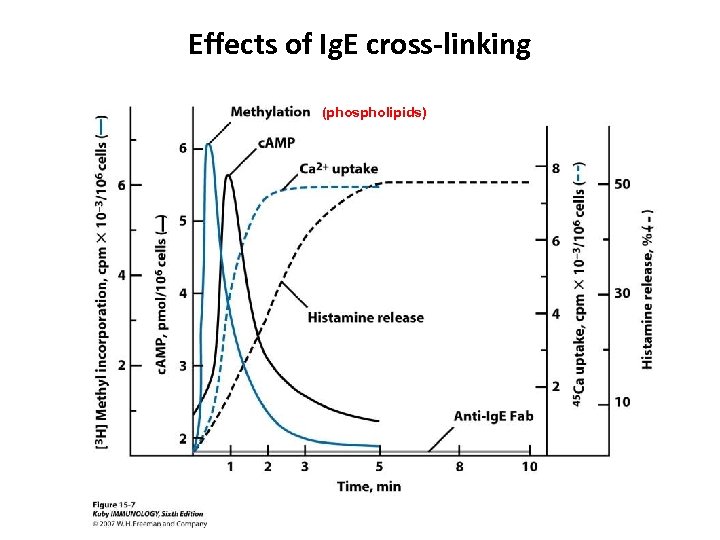 Effects of Ig. E cross-linking (phospholipids)
Effects of Ig. E cross-linking (phospholipids)
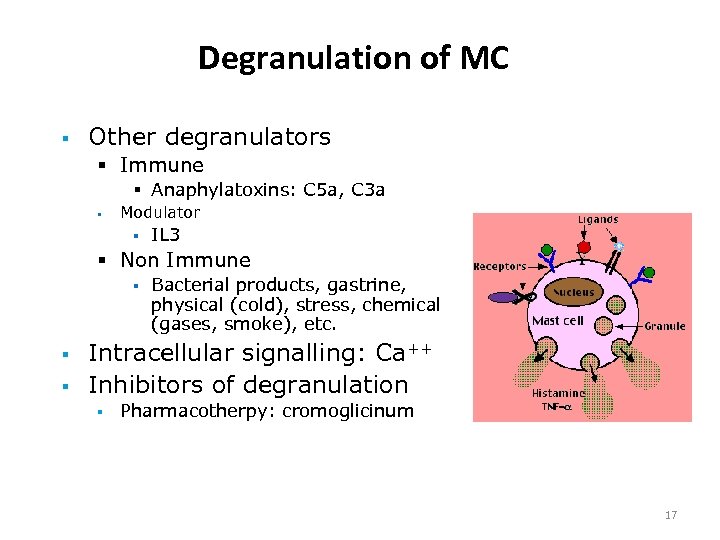 Degranulation of MC § Other degranulators § Immune § Anaphylatoxins: C 5 a, C 3 a § Modulator § IL 3 § Non Immune § § § Bacterial products, gastrine, physical (cold), stress, chemical (gases, smoke), etc. Intracellular signalling: Ca++ Inhibitors of degranulation § Pharmacotherpy: cromoglicinum 17
Degranulation of MC § Other degranulators § Immune § Anaphylatoxins: C 5 a, C 3 a § Modulator § IL 3 § Non Immune § § § Bacterial products, gastrine, physical (cold), stress, chemical (gases, smoke), etc. Intracellular signalling: Ca++ Inhibitors of degranulation § Pharmacotherpy: cromoglicinum 17
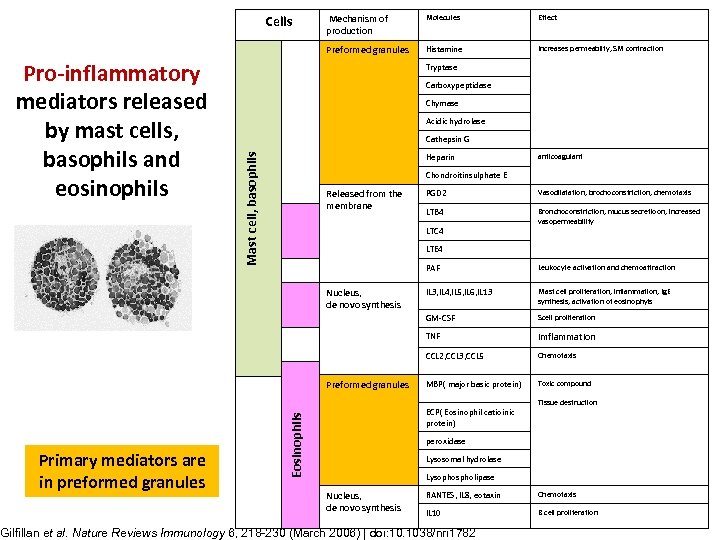 Cells Molecules Effect Preformed granules Histamine Increases permeabilty, SM contraction Tryptase Carboxypeptidase Chymase Acidic hydrolase Cathepsin G Mast cell, basophils Pro-inflammatory mediators released by mast cells, basophils and eosinophils Mechanism of production Heparin anticoagulant Chondroitinsulphate E Released from the membrane PGD 2 Vasodilatation, brochoconstriction, chemotaxis LTB 4 Bronchoconstriction, mucus secretioon, increased vasopermeability LTC 4 LTE 4 PAF Scell proliferation imflammation CCL 2, CCL 3, CCL 5 Chemotaxis MBP( major basic protein) Toxic compound ECP( Eosinophil catioinic protein) Eosinophils Primary mediators are in preformed granules Mast cell proliferation, inflammation, Ig. E synthesis, activation of eosinophyls TNF Preformed granules IL 3, IL 4, IL 5, IL 6, IL 13 GM-CSF Nucleus, de novo synthesis Leukocyte activation and chemoattraction Tissue destruction peroxidase Lysosomal hydrolase Lysophospholipase Nucleus, de novo synthesis RANTES, IL 8, eotaxin Chemotaxis IL 10 B cell proliferation Gilfillan et al. Nature Reviews Immunology 6, 218 -230 (March 2006) | doi: 10. 1038/nri 1782
Cells Molecules Effect Preformed granules Histamine Increases permeabilty, SM contraction Tryptase Carboxypeptidase Chymase Acidic hydrolase Cathepsin G Mast cell, basophils Pro-inflammatory mediators released by mast cells, basophils and eosinophils Mechanism of production Heparin anticoagulant Chondroitinsulphate E Released from the membrane PGD 2 Vasodilatation, brochoconstriction, chemotaxis LTB 4 Bronchoconstriction, mucus secretioon, increased vasopermeability LTC 4 LTE 4 PAF Scell proliferation imflammation CCL 2, CCL 3, CCL 5 Chemotaxis MBP( major basic protein) Toxic compound ECP( Eosinophil catioinic protein) Eosinophils Primary mediators are in preformed granules Mast cell proliferation, inflammation, Ig. E synthesis, activation of eosinophyls TNF Preformed granules IL 3, IL 4, IL 5, IL 6, IL 13 GM-CSF Nucleus, de novo synthesis Leukocyte activation and chemoattraction Tissue destruction peroxidase Lysosomal hydrolase Lysophospholipase Nucleus, de novo synthesis RANTES, IL 8, eotaxin Chemotaxis IL 10 B cell proliferation Gilfillan et al. Nature Reviews Immunology 6, 218 -230 (March 2006) | doi: 10. 1038/nri 1782
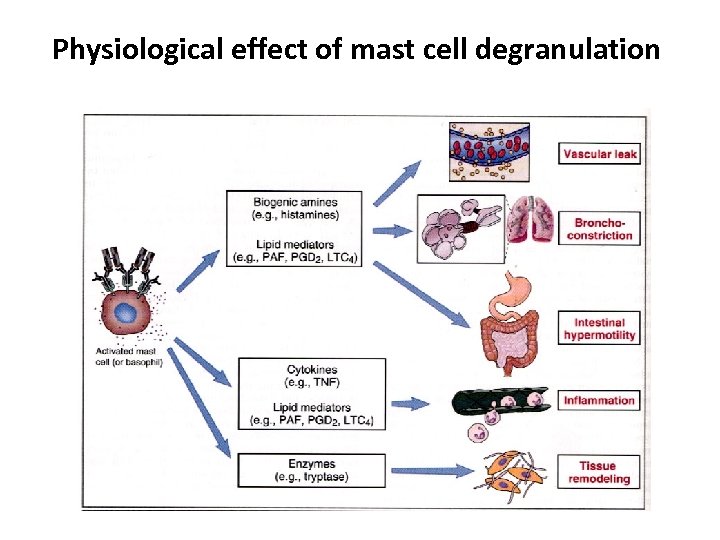 Physiological effect of mast cell degranulation
Physiological effect of mast cell degranulation
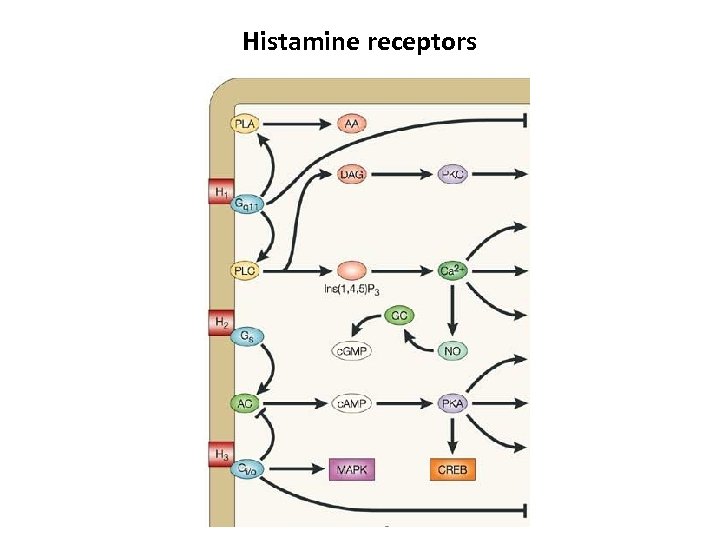 Histamine receptors
Histamine receptors
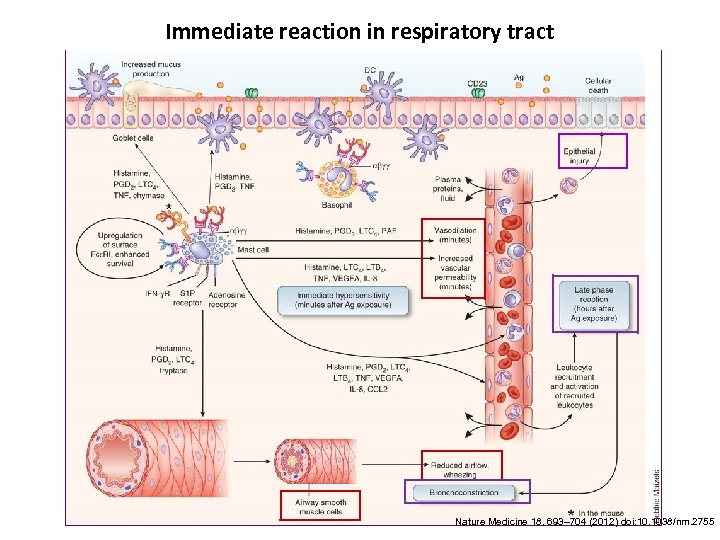
 Histamine is the key mediator and their receptors H 1: e. g GIT, bronchoconstriction ↑; vessel permeabilty↑ H 2: e. g. vasodilataion ↑; secretion of exocrine gland(e. g. gastric acid)↑; secretion (H 3: neural system) H 4: eosinophil chemotaxis
Histamine is the key mediator and their receptors H 1: e. g GIT, bronchoconstriction ↑; vessel permeabilty↑ H 2: e. g. vasodilataion ↑; secretion of exocrine gland(e. g. gastric acid)↑; secretion (H 3: neural system) H 4: eosinophil chemotaxis
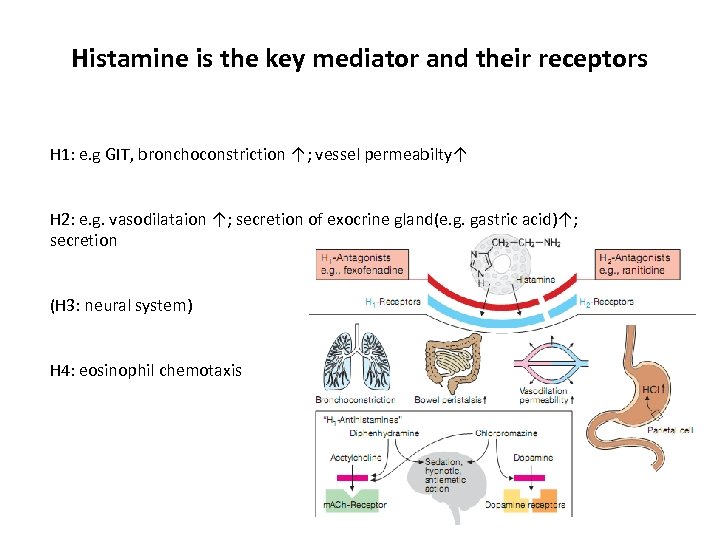
 Role of the Mast cells (MC) MC (Connective tissue) Intravenous , high dose capillaries Systemic anaphylaxis Subcutanous, low dose capillaries urticaria Mucosal MCs Inhalation, low dose SM in brochus Ingestion SM in intestin Hay fever, Food allergy: Bronchial asthma diarrhea, vomiting utricaria, anaphylaxis
Role of the Mast cells (MC) MC (Connective tissue) Intravenous , high dose capillaries Systemic anaphylaxis Subcutanous, low dose capillaries urticaria Mucosal MCs Inhalation, low dose SM in brochus Ingestion SM in intestin Hay fever, Food allergy: Bronchial asthma diarrhea, vomiting utricaria, anaphylaxis
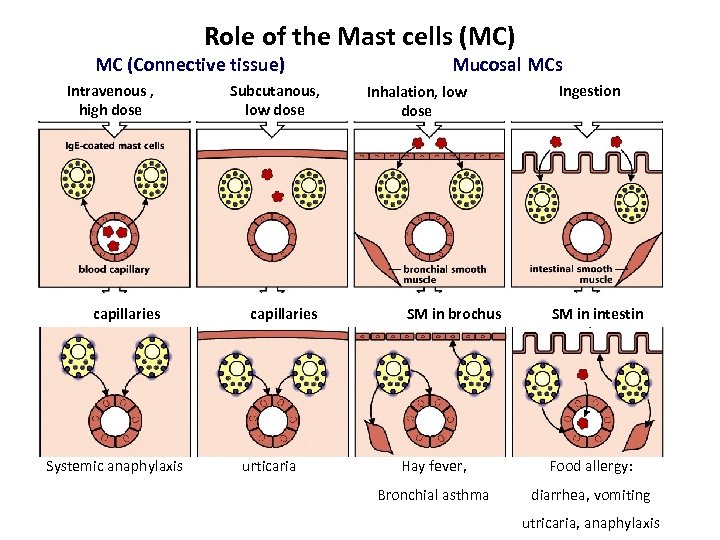
 Immediate reaction in respiratory tract Nature Medicine 18, 693– 704 (2012) doi: 10. 1038/nm. 2755
Immediate reaction in respiratory tract Nature Medicine 18, 693– 704 (2012) doi: 10. 1038/nm. 2755
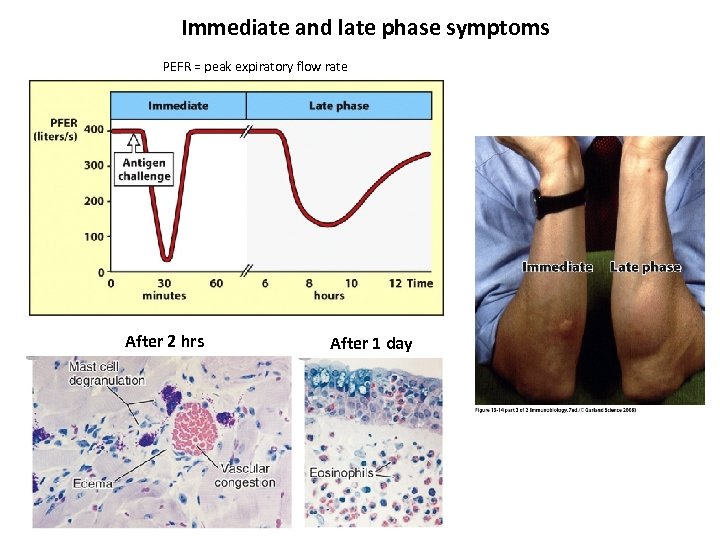 Immediate and late phase symptoms PEFR = peak expiratory flow rate After 2 hrs After 1 day
Immediate and late phase symptoms PEFR = peak expiratory flow rate After 2 hrs After 1 day
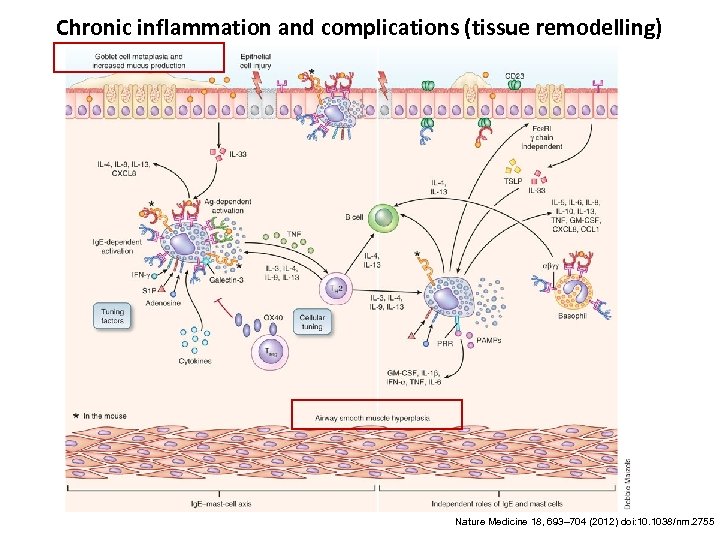 Chronic inflammation and complications (tissue remodelling) Nature Medicine 18, 693– 704 (2012) doi: 10. 1038/nm. 2755
Chronic inflammation and complications (tissue remodelling) Nature Medicine 18, 693– 704 (2012) doi: 10. 1038/nm. 2755
 Atopy § Atopy is the term for the genetic trait to have a predisposition for localized anaphylaxis. § Atopic individuals have higher levels of Ig. E and eosinophils.
Atopy § Atopy is the term for the genetic trait to have a predisposition for localized anaphylaxis. § Atopic individuals have higher levels of Ig. E and eosinophils.
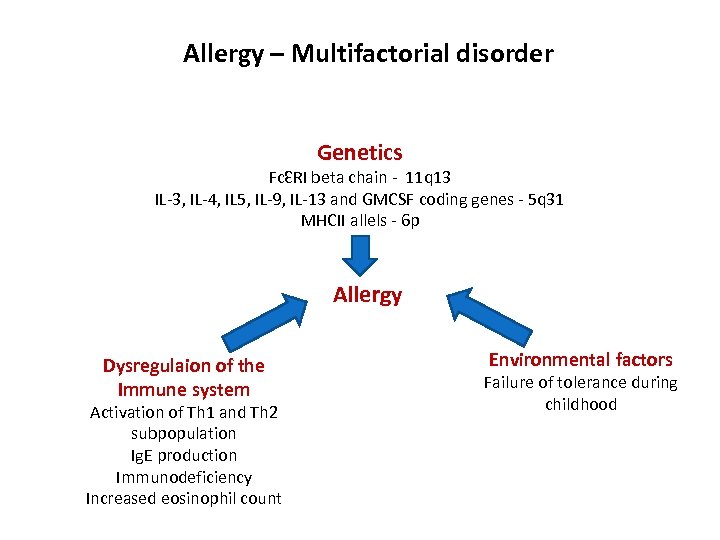 Allergy – Multifactorial disorder Genetics FcƐRI beta chain - 11 q 13 IL-3, IL-4, IL 5, IL-9, IL-13 and GMCSF coding genes - 5 q 31 MHCII allels - 6 p Allergy Dysregulaion of the Immune system Activation of Th 1 and Th 2 subpopulation Ig. E production Immunodeficiency Increased eosinophil count Environmental factors Failure of tolerance during childhood
Allergy – Multifactorial disorder Genetics FcƐRI beta chain - 11 q 13 IL-3, IL-4, IL 5, IL-9, IL-13 and GMCSF coding genes - 5 q 31 MHCII allels - 6 p Allergy Dysregulaion of the Immune system Activation of Th 1 and Th 2 subpopulation Ig. E production Immunodeficiency Increased eosinophil count Environmental factors Failure of tolerance during childhood
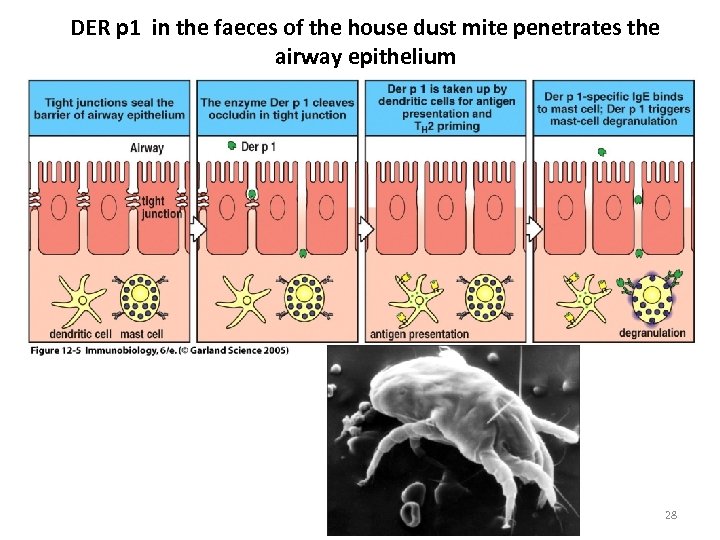 DER p 1 in the faeces of the house dust mite penetrates the airway epithelium 28
DER p 1 in the faeces of the house dust mite penetrates the airway epithelium 28
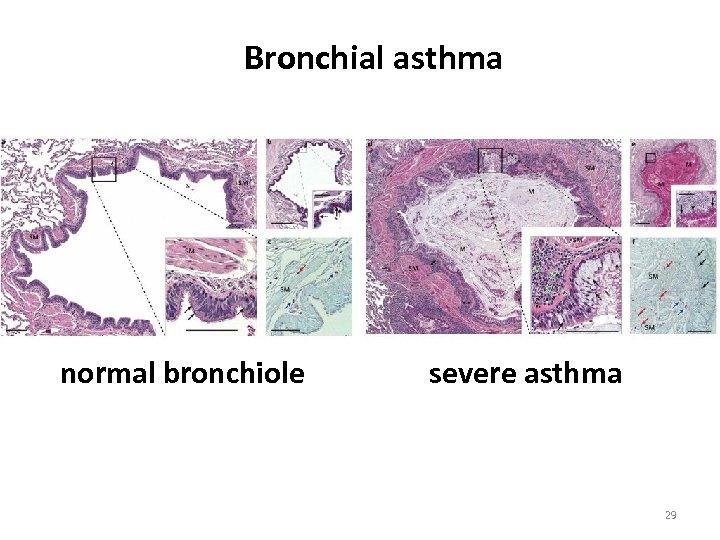 Bronchial asthma normal bronchiole severe asthma 29
Bronchial asthma normal bronchiole severe asthma 29
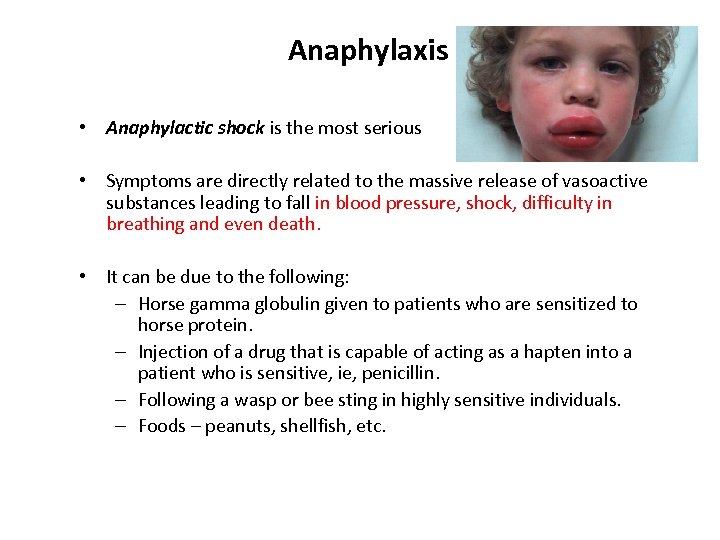 Anaphylaxis • Anaphylactic shock is the most serious • Symptoms are directly related to the massive release of vasoactive substances leading to fall in blood pressure, shock, difficulty in breathing and even death. • It can be due to the following: – Horse gamma globulin given to patients who are sensitized to horse protein. – Injection of a drug that is capable of acting as a hapten into a patient who is sensitive, ie, penicillin. – Following a wasp or bee sting in highly sensitive individuals. – Foods – peanuts, shellfish, etc.
Anaphylaxis • Anaphylactic shock is the most serious • Symptoms are directly related to the massive release of vasoactive substances leading to fall in blood pressure, shock, difficulty in breathing and even death. • It can be due to the following: – Horse gamma globulin given to patients who are sensitized to horse protein. – Injection of a drug that is capable of acting as a hapten into a patient who is sensitive, ie, penicillin. – Following a wasp or bee sting in highly sensitive individuals. – Foods – peanuts, shellfish, etc.
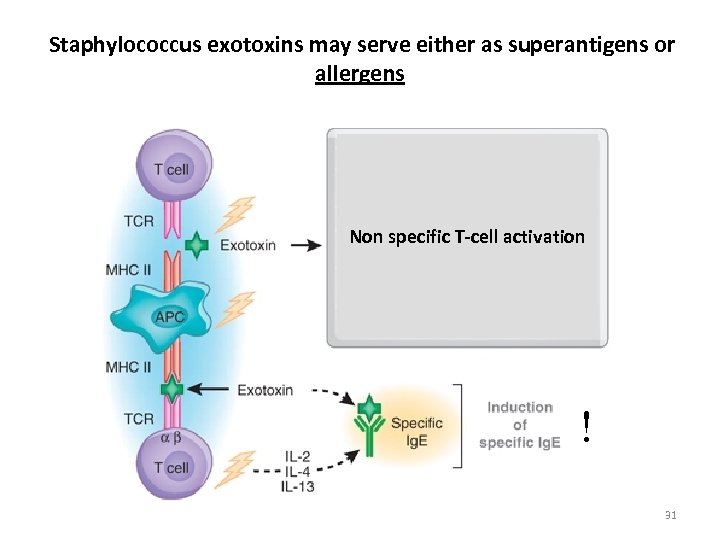 Staphylococcus exotoxins may serve either as superantigens or allergens Non specific T-cell activation ! 31
Staphylococcus exotoxins may serve either as superantigens or allergens Non specific T-cell activation ! 31
 Therapy – Avoidance of known allergens – Localized reactions use OTC antihistamines and decongestants. – Asthma uses combination – antihistamines, bronchodilators and corticosteroids. – Systemic use epinephrine – Hyposensitization – inject antigen to cause production of Ig. G which binds to antigen (allergen) before it reaches Ig. E coated cells. – Monocolonal anti-Ig. E – inject, binds to receptors on mast cells blocking them from the Ig. E.
Therapy – Avoidance of known allergens – Localized reactions use OTC antihistamines and decongestants. – Asthma uses combination – antihistamines, bronchodilators and corticosteroids. – Systemic use epinephrine – Hyposensitization – inject antigen to cause production of Ig. G which binds to antigen (allergen) before it reaches Ig. E coated cells. – Monocolonal anti-Ig. E – inject, binds to receptors on mast cells blocking them from the Ig. E.
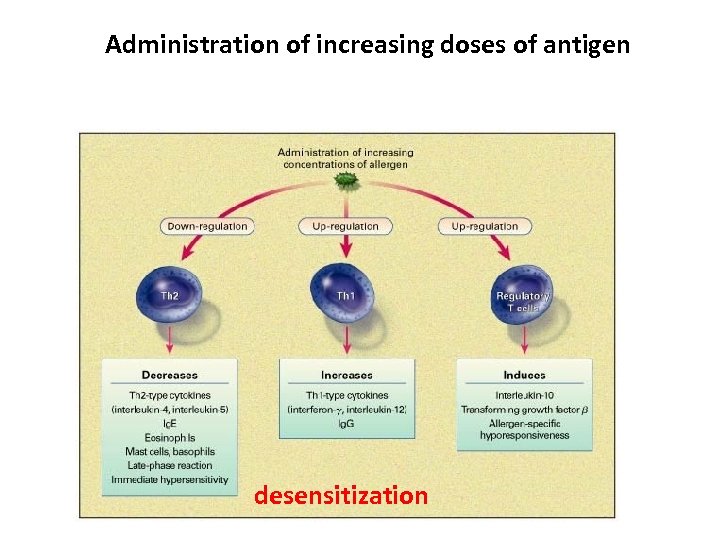 Administration of increasing doses of antigen desensitization
Administration of increasing doses of antigen desensitization
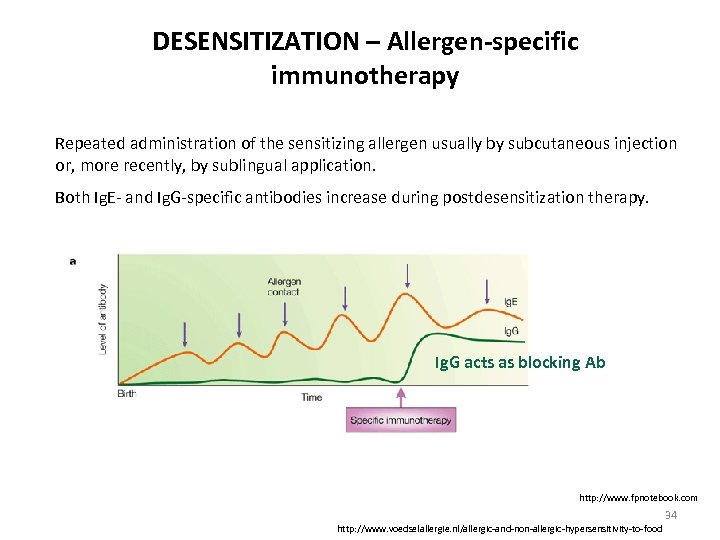 DESENSITIZATION – Allergen-specific immunotherapy Repeated administration of the sensitizing allergen usually by subcutaneous injection or, more recently, by sublingual application. Both Ig. E- and Ig. G-specific antibodies increase during postdesensitization therapy. Ig. G acts as blocking Ab http: //www. fpnotebook. com 34 http: //www. voedselallergie. nl/allergic-and-non-allergic-hypersensitivity-to-food
DESENSITIZATION – Allergen-specific immunotherapy Repeated administration of the sensitizing allergen usually by subcutaneous injection or, more recently, by sublingual application. Both Ig. E- and Ig. G-specific antibodies increase during postdesensitization therapy. Ig. G acts as blocking Ab http: //www. fpnotebook. com 34 http: //www. voedselallergie. nl/allergic-and-non-allergic-hypersensitivity-to-food
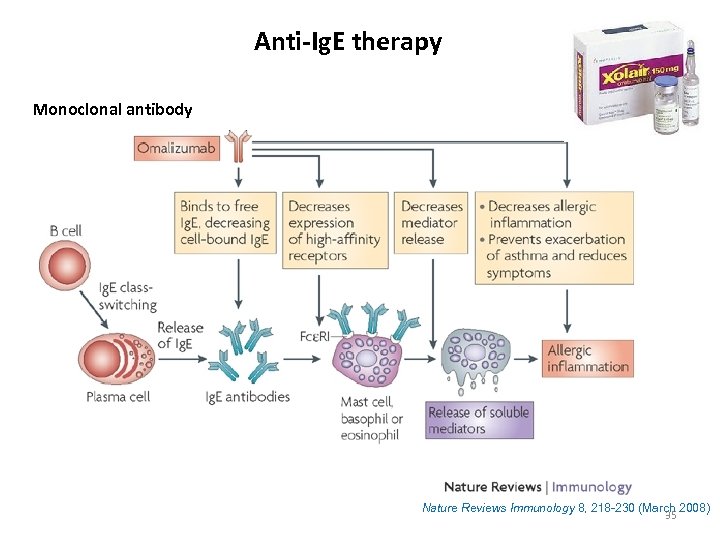 Anti-Ig. E therapy Monoclonal antibody Nature Reviews Immunology 8, 218 -230 (March 2008) 35
Anti-Ig. E therapy Monoclonal antibody Nature Reviews Immunology 8, 218 -230 (March 2008) 35
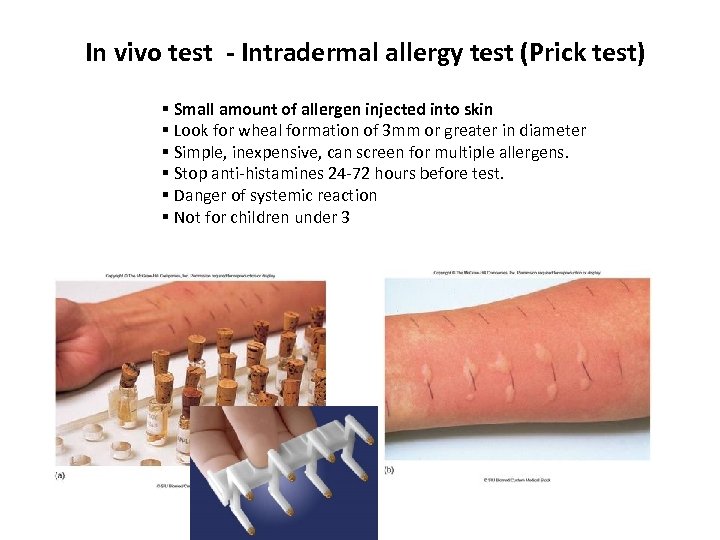 In vivo test - Intradermal allergy test (Prick test) § Small amount of allergen injected into skin § Look for wheal formation of 3 mm or greater in diameter § Simple, inexpensive, can screen for multiple allergens. § Stop anti-histamines 24 -72 hours before test. § Danger of systemic reaction § Not for children under 3
In vivo test - Intradermal allergy test (Prick test) § Small amount of allergen injected into skin § Look for wheal formation of 3 mm or greater in diameter § Simple, inexpensive, can screen for multiple allergens. § Stop anti-histamines 24 -72 hours before test. § Danger of systemic reaction § Not for children under 3
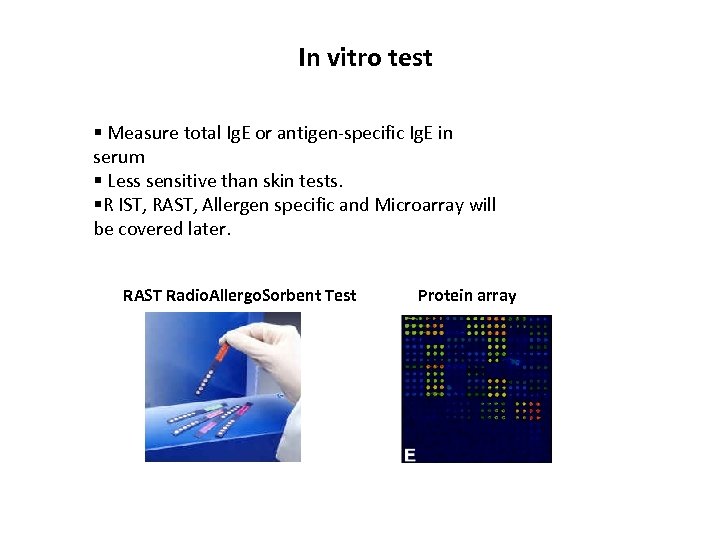 In vitro test § Measure total Ig. E or antigen-specific Ig. E in serum § Less sensitive than skin tests. §R IST, RAST, Allergen specific and Microarray will be covered later. RAST Radio. Allergo. Sorbent Test Protein array
In vitro test § Measure total Ig. E or antigen-specific Ig. E in serum § Less sensitive than skin tests. §R IST, RAST, Allergen specific and Microarray will be covered later. RAST Radio. Allergo. Sorbent Test Protein array
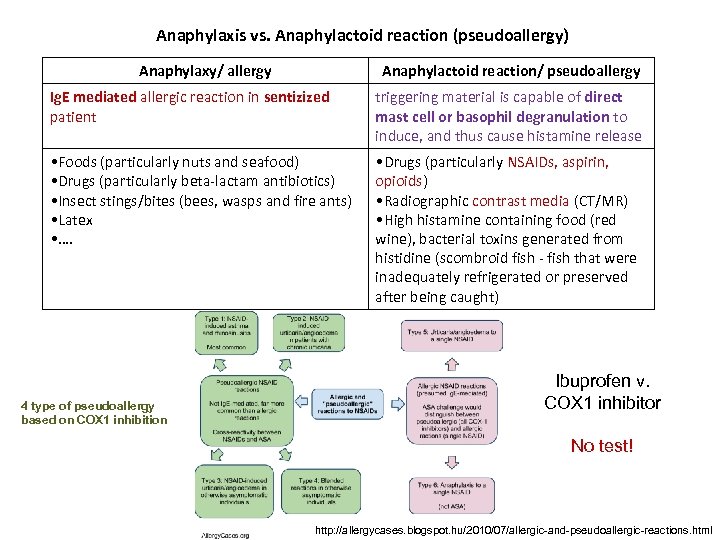 Anaphylaxis vs. Anaphylactoid reaction (pseudoallergy) Anaphylaxy/ allergy Anaphylactoid reaction/ pseudoallergy Ig. E mediated allergic reaction in sentizized patient triggering material is capable of direct mast cell or basophil degranulation to induce, and thus cause histamine release • Foods (particularly nuts and seafood) • Drugs (particularly beta-lactam antibiotics) • Insect stings/bites (bees, wasps and fire ants) • Latex • …. • Drugs (particularly NSAIDs, aspirin, opioids) • Radiographic contrast media (CT/MR) • High histamine containing food (red wine), bacterial toxins generated from histidine (scombroid fish - fish that were inadequately refrigerated or preserved after being caught) 4 type of pseudoallergy based on COX 1 inhibition Ibuprofen v. COX 1 inhibitor No test! http: //allergycases. blogspot. hu/2010/07/allergic-and-pseudoallergic-reactions. html
Anaphylaxis vs. Anaphylactoid reaction (pseudoallergy) Anaphylaxy/ allergy Anaphylactoid reaction/ pseudoallergy Ig. E mediated allergic reaction in sentizized patient triggering material is capable of direct mast cell or basophil degranulation to induce, and thus cause histamine release • Foods (particularly nuts and seafood) • Drugs (particularly beta-lactam antibiotics) • Insect stings/bites (bees, wasps and fire ants) • Latex • …. • Drugs (particularly NSAIDs, aspirin, opioids) • Radiographic contrast media (CT/MR) • High histamine containing food (red wine), bacterial toxins generated from histidine (scombroid fish - fish that were inadequately refrigerated or preserved after being caught) 4 type of pseudoallergy based on COX 1 inhibition Ibuprofen v. COX 1 inhibitor No test! http: //allergycases. blogspot. hu/2010/07/allergic-and-pseudoallergic-reactions. html
 Type II. hypersensitivity (HS)
Type II. hypersensitivity (HS)
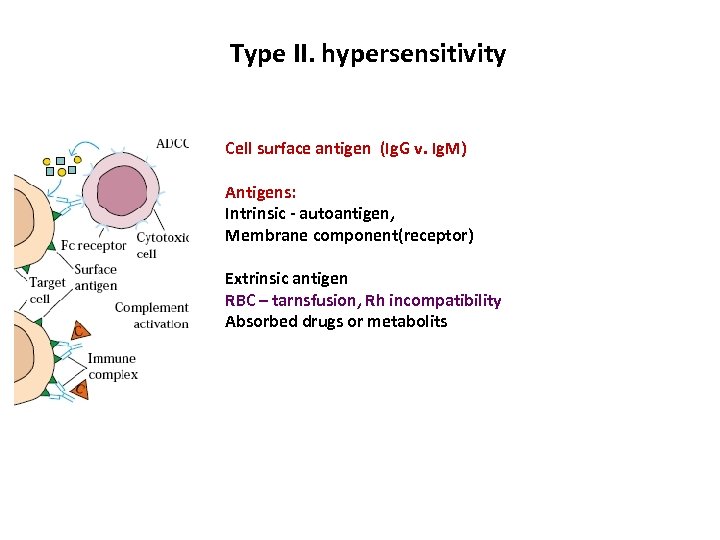 Type II. hypersensitivity Cell surface antigen (Ig. G v. Ig. M) Antigens: Intrinsic - autoantigen, Membrane component(receptor) Extrinsic antigen RBC – tarnsfusion, Rh incompatibility Absorbed drugs or metabolits
Type II. hypersensitivity Cell surface antigen (Ig. G v. Ig. M) Antigens: Intrinsic - autoantigen, Membrane component(receptor) Extrinsic antigen RBC – tarnsfusion, Rh incompatibility Absorbed drugs or metabolits
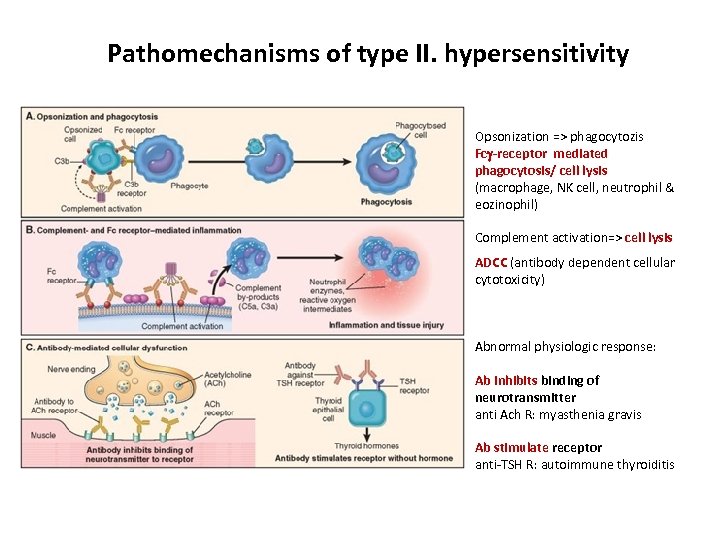 Pathomechanisms of type II. hypersensitivity Opsonization => phagocytozis Fc -receptor mediated phagocytosis/ cell lysis (macrophage, NK cell, neutrophil & eozinophil) Complement activation=> cell lysis ADCC (antibody dependent cellular cytotoxicity) Abnormal physiologic response: Ab inhibits binding of neurotransmitter anti Ach R: myasthenia gravis Ab stimulate receptor anti-TSH R: autoimmune thyroiditis
Pathomechanisms of type II. hypersensitivity Opsonization => phagocytozis Fc -receptor mediated phagocytosis/ cell lysis (macrophage, NK cell, neutrophil & eozinophil) Complement activation=> cell lysis ADCC (antibody dependent cellular cytotoxicity) Abnormal physiologic response: Ab inhibits binding of neurotransmitter anti Ach R: myasthenia gravis Ab stimulate receptor anti-TSH R: autoimmune thyroiditis
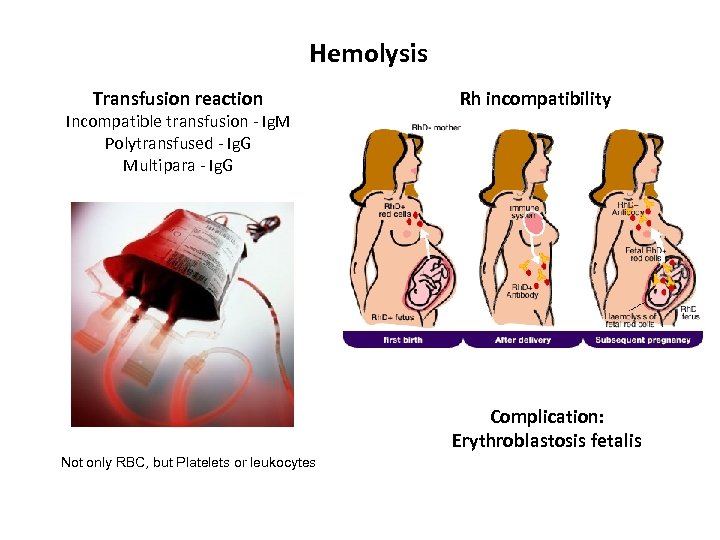 Hemolysis Transfusion reaction Incompatible transfusion - Ig. M Polytransfused - Ig. G Multipara - Ig. G Rh incompatibility Complication: Erythroblastosis fetalis Not only RBC, but Platelets or leukocytes
Hemolysis Transfusion reaction Incompatible transfusion - Ig. M Polytransfused - Ig. G Multipara - Ig. G Rh incompatibility Complication: Erythroblastosis fetalis Not only RBC, but Platelets or leukocytes
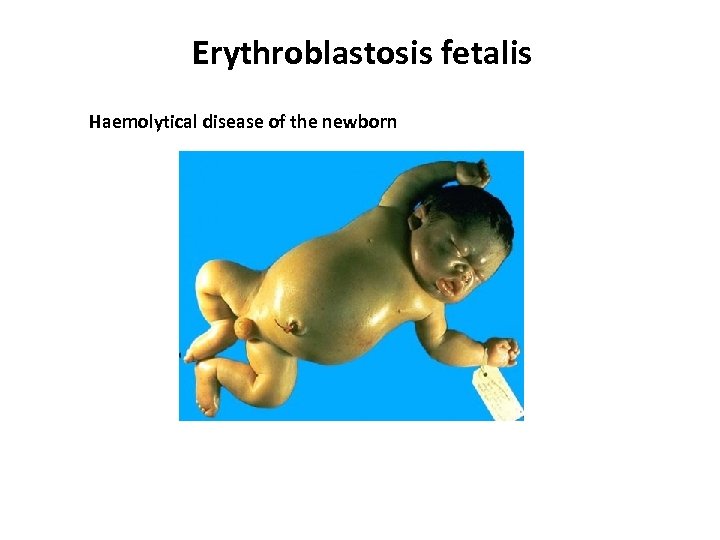 Erythroblastosis fetalis Haemolytical disease of the newborn
Erythroblastosis fetalis Haemolytical disease of the newborn
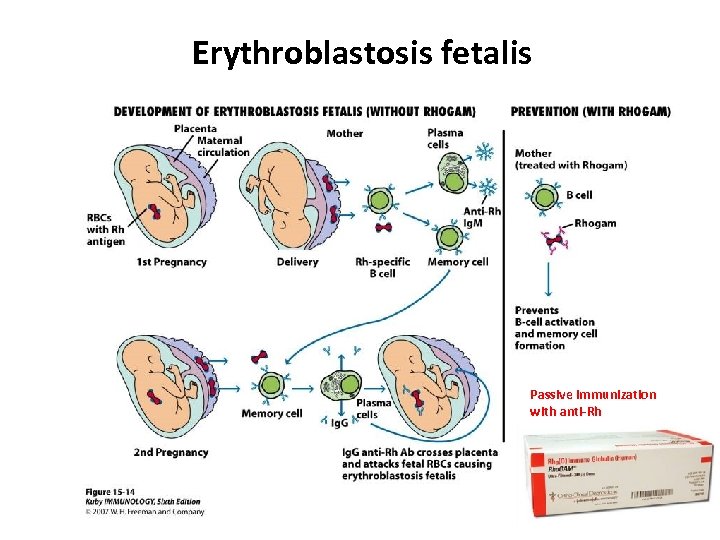 Erythroblastosis fetalis Passive immunization with anti-Rh
Erythroblastosis fetalis Passive immunization with anti-Rh
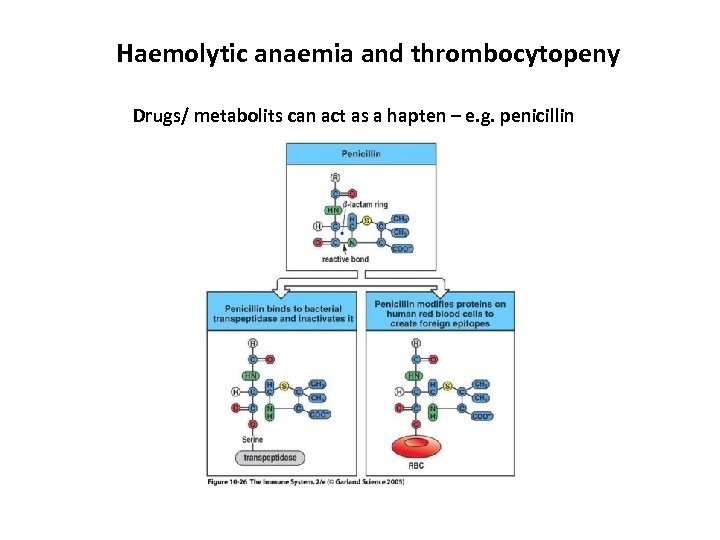 Haemolytic anaemia and thrombocytopeny Drugs/ metabolits can act as a hapten – e. g. penicillin
Haemolytic anaemia and thrombocytopeny Drugs/ metabolits can act as a hapten – e. g. penicillin
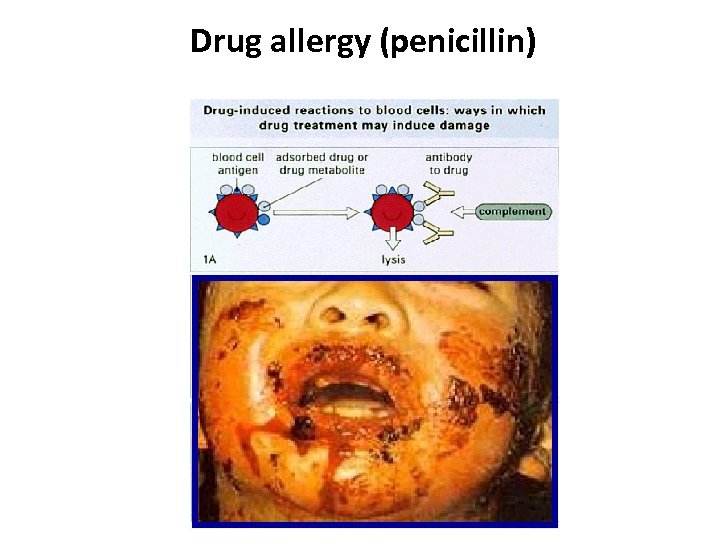 Drug allergy (penicillin)
Drug allergy (penicillin)
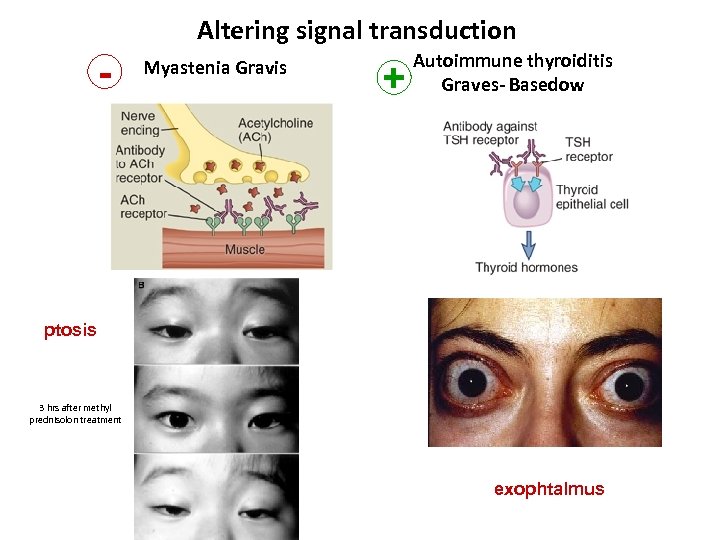 Altering signal transduction - Myastenia Gravis + Autoimmune thyroiditis Graves- Basedow ptosis 3 hrs after methyl prednisolon treatment exophtalmus
Altering signal transduction - Myastenia Gravis + Autoimmune thyroiditis Graves- Basedow ptosis 3 hrs after methyl prednisolon treatment exophtalmus
 Type III. HS Soluble antigen-antibody complex - IMMUNE COMPLEX disease
Type III. HS Soluble antigen-antibody complex - IMMUNE COMPLEX disease
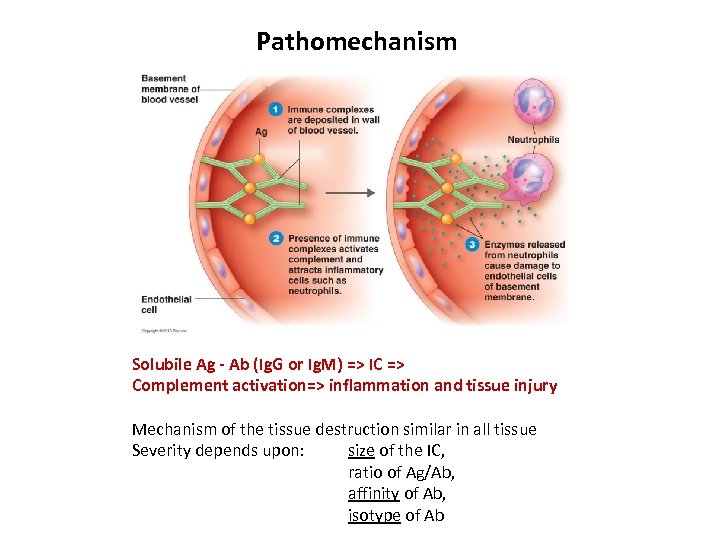 Pathomechanism Solubile Ag - Ab (Ig. G or Ig. M) => IC => Complement activation=> inflammation and tissue injury Mechanism of the tissue destruction similar in all tissue Severity depends upon: size of the IC, ratio of Ag/Ab, affinity of Ab, isotype of Ab
Pathomechanism Solubile Ag - Ab (Ig. G or Ig. M) => IC => Complement activation=> inflammation and tissue injury Mechanism of the tissue destruction similar in all tissue Severity depends upon: size of the IC, ratio of Ag/Ab, affinity of Ab, isotype of Ab
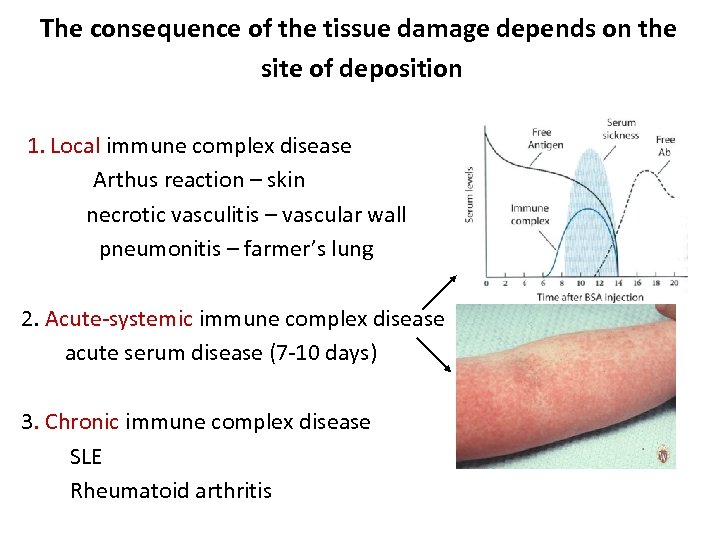 The consequence of the tissue damage depends on the site of deposition 1. Local immune complex disease Arthus reaction – skin necrotic vasculitis – vascular wall pneumonitis – farmer’s lung 2. Acute-systemic immune complex disease acute serum disease (7 -10 days) 3. Chronic immune complex disease SLE Rheumatoid arthritis
The consequence of the tissue damage depends on the site of deposition 1. Local immune complex disease Arthus reaction – skin necrotic vasculitis – vascular wall pneumonitis – farmer’s lung 2. Acute-systemic immune complex disease acute serum disease (7 -10 days) 3. Chronic immune complex disease SLE Rheumatoid arthritis
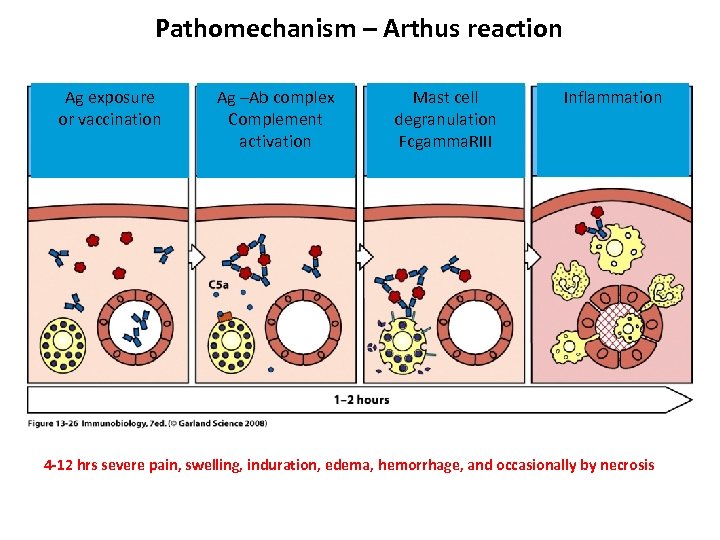 Pathomechanism – Arthus reaction Ag exposure or vaccination Ag –Ab complex Complement activation Mast cell degranulation Fcgamma. RIII Inflammation 4 -12 hrs severe pain, swelling, induration, edema, hemorrhage, and occasionally by necrosis
Pathomechanism – Arthus reaction Ag exposure or vaccination Ag –Ab complex Complement activation Mast cell degranulation Fcgamma. RIII Inflammation 4 -12 hrs severe pain, swelling, induration, edema, hemorrhage, and occasionally by necrosis
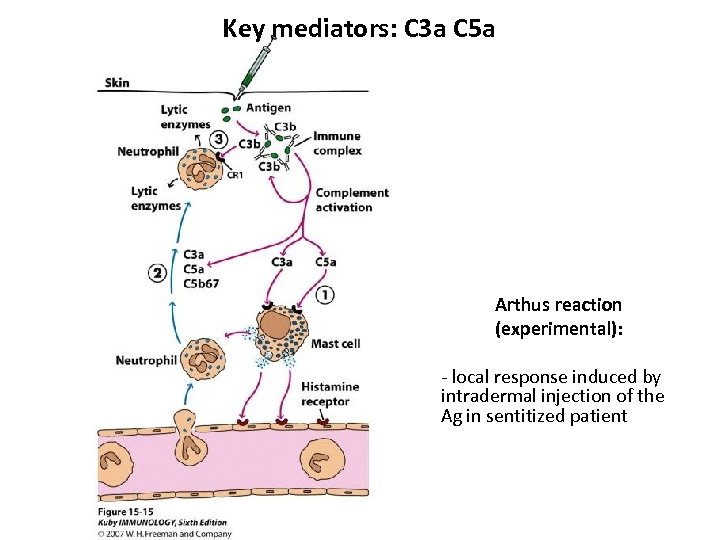 Key mediators: C 3 a C 5 a Arthus reaction (experimental): - local response induced by intradermal injection of the Ag in sentitized patient
Key mediators: C 3 a C 5 a Arthus reaction (experimental): - local response induced by intradermal injection of the Ag in sentitized patient
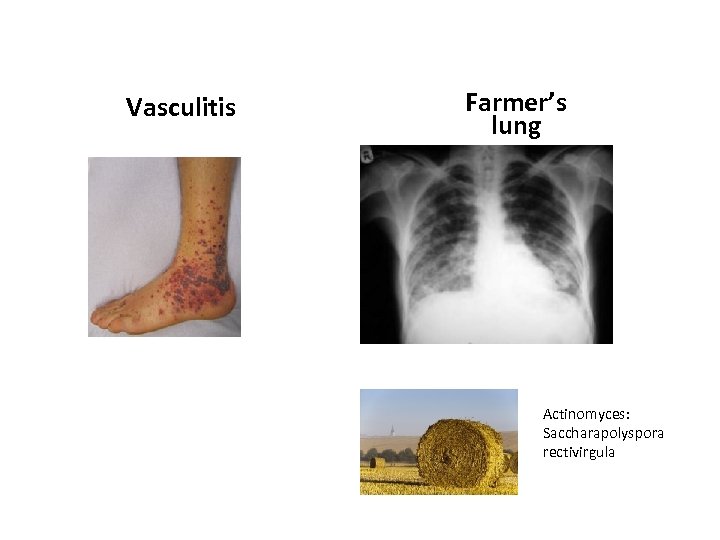 Vasculitis Farmer’s lung Actinomyces: Saccharapolyspora rectivirgula
Vasculitis Farmer’s lung Actinomyces: Saccharapolyspora rectivirgula
 Type IV. HS T cell mediated disease Delayed HS
Type IV. HS T cell mediated disease Delayed HS
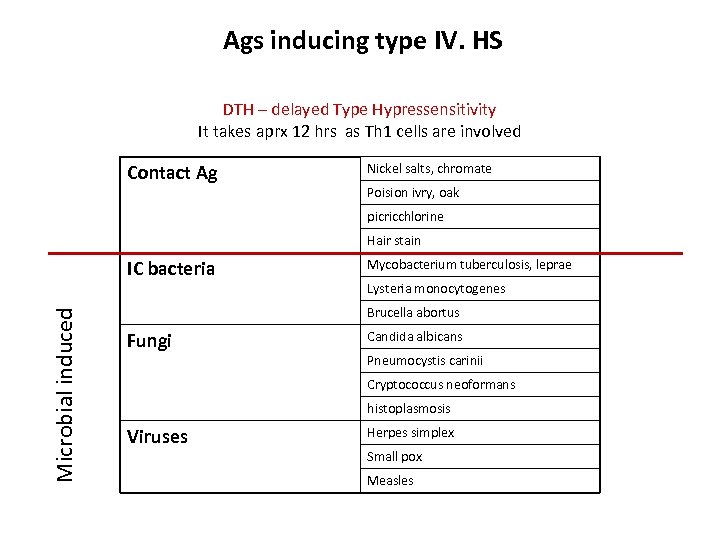 Ags inducing type IV. HS DTH – delayed Type Hypressensitivity It takes aprx 12 hrs as Th 1 cells are involved Contact Ag Nickel salts, chromate Poision ivry, oak picricchlorine Hair stain Microbial induced IC bacteria Mycobacterium tuberculosis, leprae Lysteria monocytogenes Brucella abortus Fungi Candida albicans Pneumocystis carinii Cryptococcus neoformans histoplasmosis Viruses Herpes simplex Small pox Measles
Ags inducing type IV. HS DTH – delayed Type Hypressensitivity It takes aprx 12 hrs as Th 1 cells are involved Contact Ag Nickel salts, chromate Poision ivry, oak picricchlorine Hair stain Microbial induced IC bacteria Mycobacterium tuberculosis, leprae Lysteria monocytogenes Brucella abortus Fungi Candida albicans Pneumocystis carinii Cryptococcus neoformans histoplasmosis Viruses Herpes simplex Small pox Measles
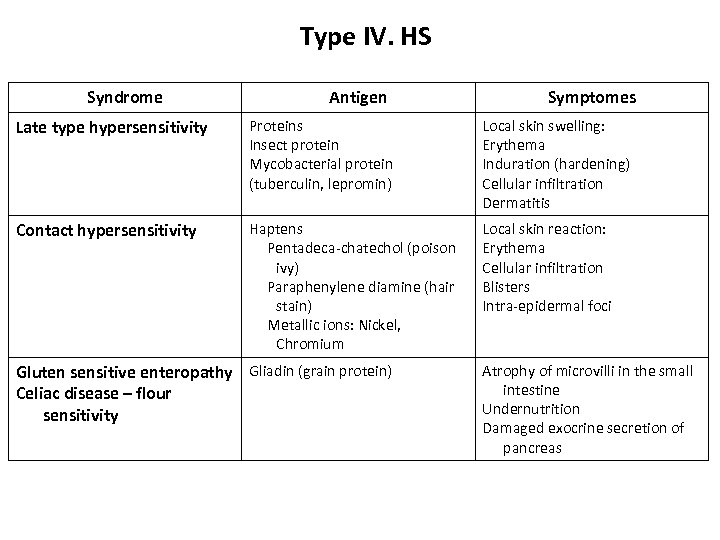 Type IV. HS Syndrome Antigen Symptomes Late type hypersensitivity Proteins Insect protein Mycobacterial protein (tuberculin, lepromin) Local skin swelling: Erythema Induration (hardening) Cellular infiltration Dermatitis Contact hypersensitivity Haptens Pentadeca-chatechol (poison ivy) Paraphenylene diamine (hair stain) Metallic ions: Nickel, Chromium Local skin reaction: Erythema Cellular infiltration Blisters Intra-epidermal foci Gluten sensitive enteropathy Gliadin (grain protein) Celiac disease – flour sensitivity Atrophy of microvilli in the small intestine Undernutrition Damaged exocrine secretion of pancreas
Type IV. HS Syndrome Antigen Symptomes Late type hypersensitivity Proteins Insect protein Mycobacterial protein (tuberculin, lepromin) Local skin swelling: Erythema Induration (hardening) Cellular infiltration Dermatitis Contact hypersensitivity Haptens Pentadeca-chatechol (poison ivy) Paraphenylene diamine (hair stain) Metallic ions: Nickel, Chromium Local skin reaction: Erythema Cellular infiltration Blisters Intra-epidermal foci Gluten sensitive enteropathy Gliadin (grain protein) Celiac disease – flour sensitivity Atrophy of microvilli in the small intestine Undernutrition Damaged exocrine secretion of pancreas
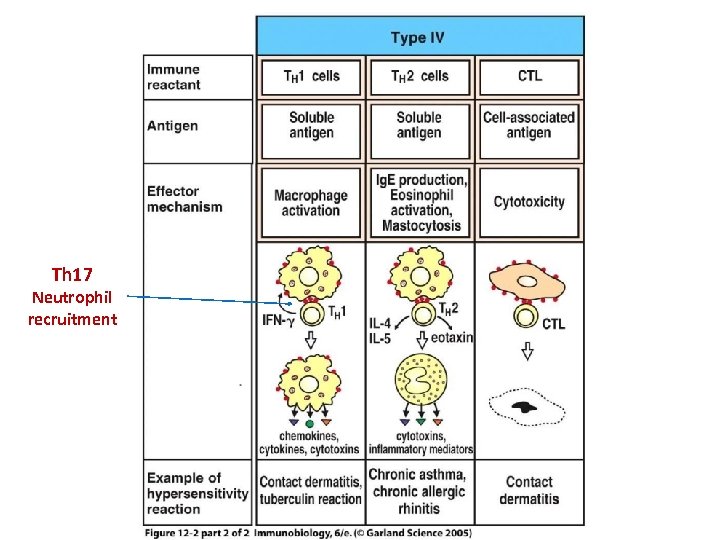 Th 17 Neutrophil recruitment
Th 17 Neutrophil recruitment
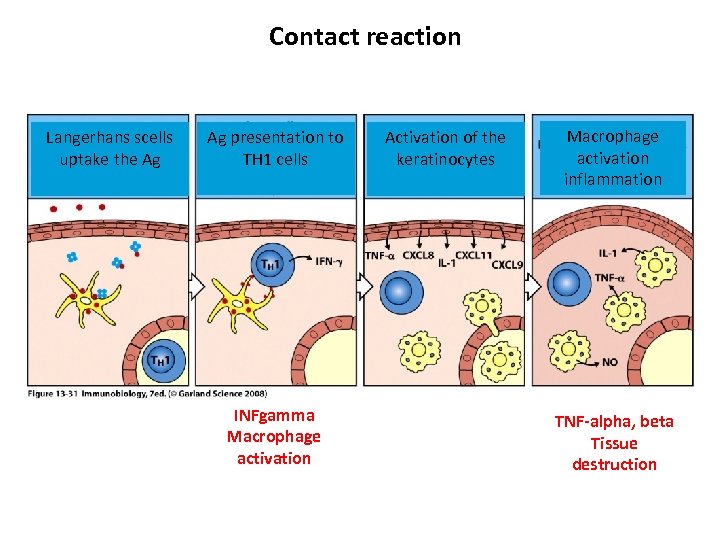 Contact reaction Langerhans scells uptake the Ag Ag presentation to TH 1 cells INFgamma Macrophage activation Activation of the keratinocytes Macrophage activation inflammation TNF-alpha, beta Tissue destruction
Contact reaction Langerhans scells uptake the Ag Ag presentation to TH 1 cells INFgamma Macrophage activation Activation of the keratinocytes Macrophage activation inflammation TNF-alpha, beta Tissue destruction
 A schematic view of the sensitization phase Tetsuya Honda (2013) 133, 303 -315. doi: 10. 1038/jid. 2012. 284
A schematic view of the sensitization phase Tetsuya Honda (2013) 133, 303 -315. doi: 10. 1038/jid. 2012. 284
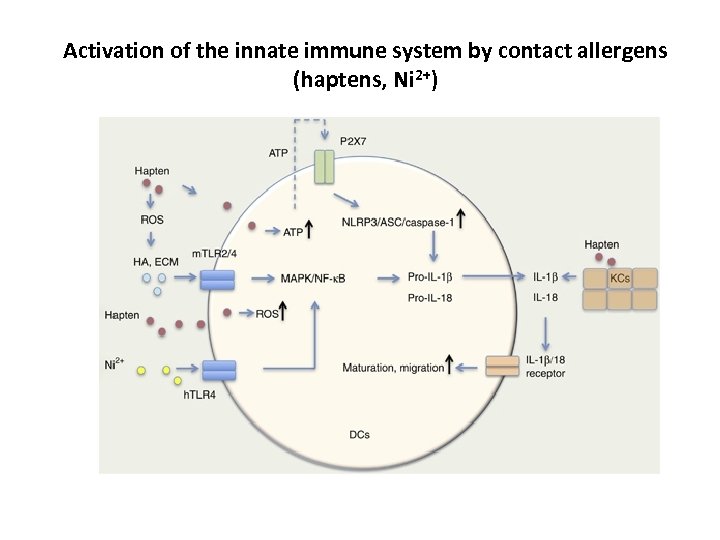 Activation of the innate immune system by contact allergens (haptens, Ni 2+)
Activation of the innate immune system by contact allergens (haptens, Ni 2+)
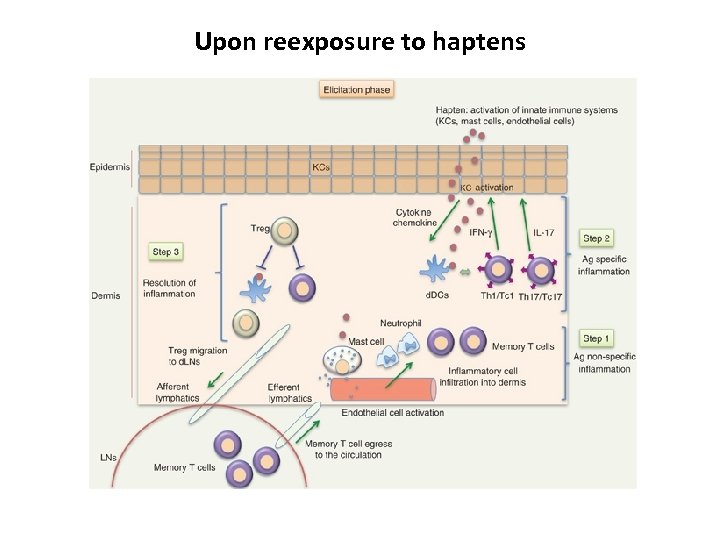 Upon reexposure to haptens
Upon reexposure to haptens
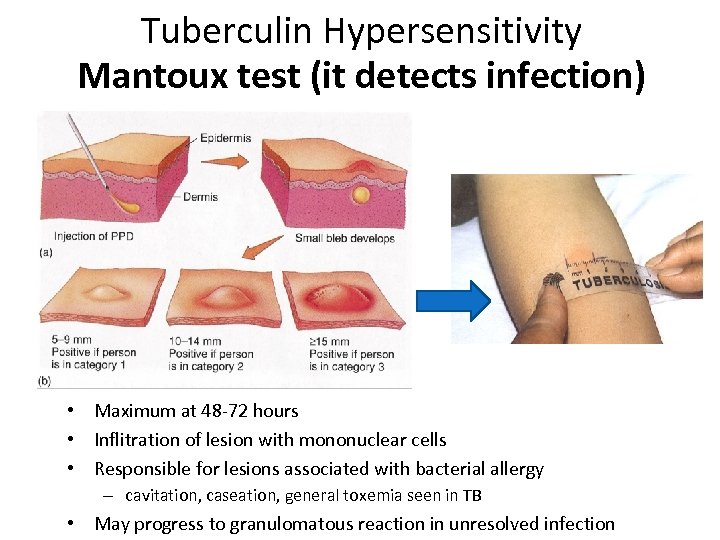 Tuberculin Hypersensitivity Mantoux test (it detects infection) • Maximum at 48 -72 hours • Inflitration of lesion with mononuclear cells • Responsible for lesions associated with bacterial allergy – cavitation, caseation, general toxemia seen in TB • May progress to granulomatous reaction in unresolved infection
Tuberculin Hypersensitivity Mantoux test (it detects infection) • Maximum at 48 -72 hours • Inflitration of lesion with mononuclear cells • Responsible for lesions associated with bacterial allergy – cavitation, caseation, general toxemia seen in TB • May progress to granulomatous reaction in unresolved infection
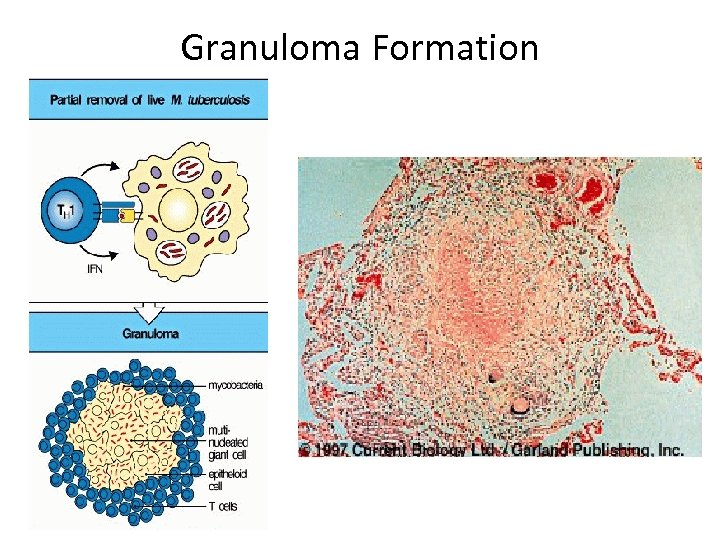 Granuloma Formation
Granuloma Formation
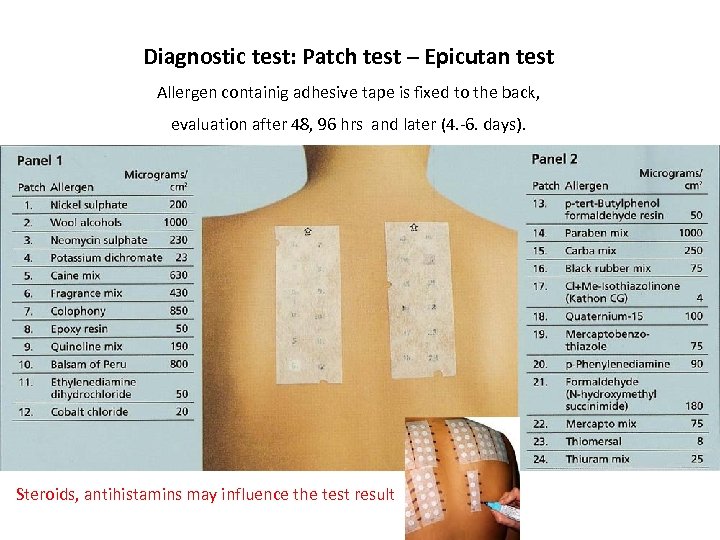 Diagnostic test: Patch test – Epicutan test Allergen containig adhesive tape is fixed to the back, evaluation after 48, 96 hrs and later (4. -6. days). Steroids, antihistamins may influence the test result
Diagnostic test: Patch test – Epicutan test Allergen containig adhesive tape is fixed to the back, evaluation after 48, 96 hrs and later (4. -6. days). Steroids, antihistamins may influence the test result
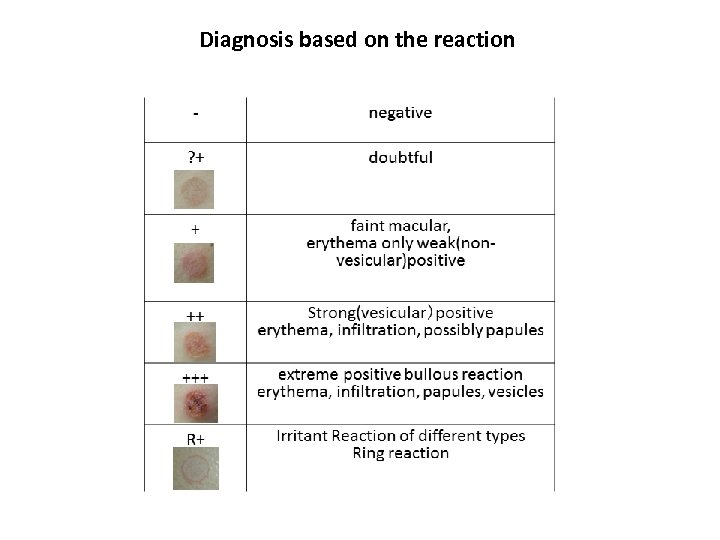 Diagnosis based on the reaction
Diagnosis based on the reaction
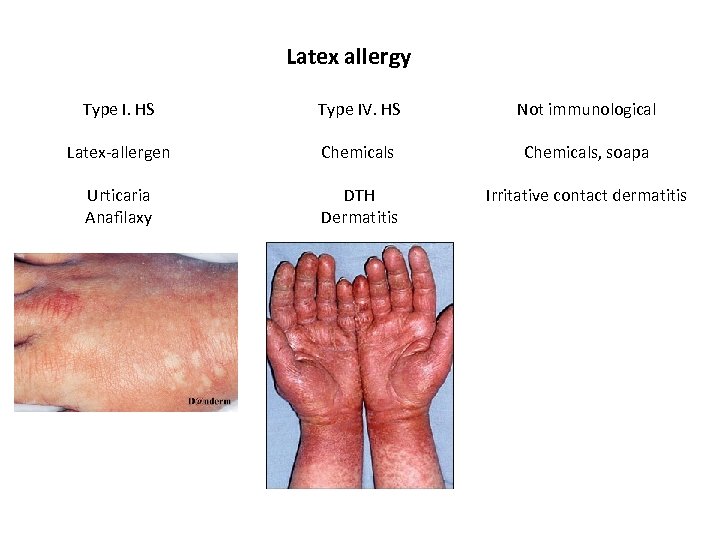 Latex allergy Type I. HS Type IV. HS Not immunological Latex-allergen Chemicals, soapa Urticaria Anafilaxy DTH Dermatitis Irritative contact dermatitis
Latex allergy Type I. HS Type IV. HS Not immunological Latex-allergen Chemicals, soapa Urticaria Anafilaxy DTH Dermatitis Irritative contact dermatitis
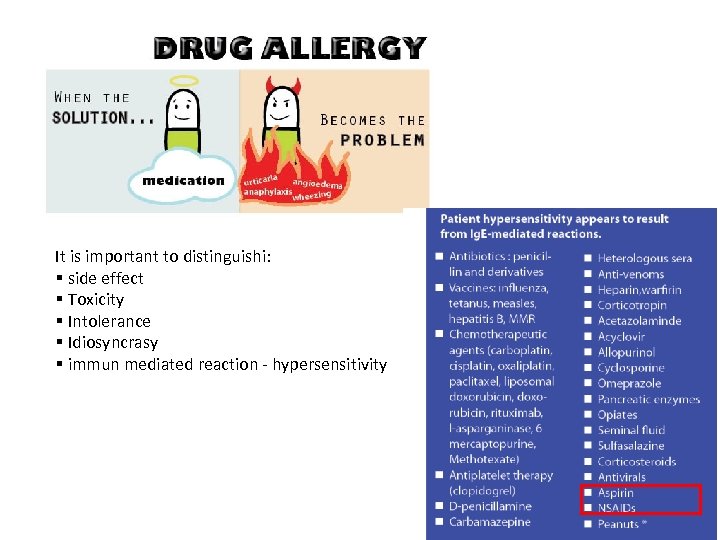 It is important to distinguishi: § side effect § Toxicity § Intolerance § Idiosyncrasy § immun mediated reaction - hypersensitivity
It is important to distinguishi: § side effect § Toxicity § Intolerance § Idiosyncrasy § immun mediated reaction - hypersensitivity
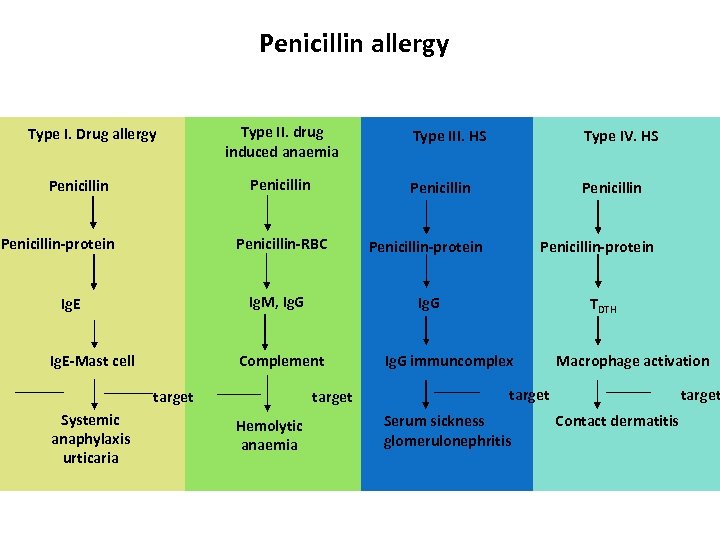 Penicillin allergy Type I. Drug allergy Type II. drug induced anaemia Penicillin-protein Penicillin-RBC Ig. M, Ig. G Ig. E target Systemic anaphylaxis urticaria target Hemolytic anaemia Penicillin-protein Ig. G Complement Ig. E-Mast cell Type IV. HS Penicillin Type III. HS TDTH Ig. G immuncomplex Macrophage activation target Serum sickness glomerulonephritis target Contact dermatitis
Penicillin allergy Type I. Drug allergy Type II. drug induced anaemia Penicillin-protein Penicillin-RBC Ig. M, Ig. G Ig. E target Systemic anaphylaxis urticaria target Hemolytic anaemia Penicillin-protein Ig. G Complement Ig. E-Mast cell Type IV. HS Penicillin Type III. HS TDTH Ig. G immuncomplex Macrophage activation target Serum sickness glomerulonephritis target Contact dermatitis
 Allegies in dentristry Chlorhexidine: including allergy (Type I HS ) and allergic contact dermatitis/stomatitis (Type IV HS) Flouride - Type I and VI. HS skin rashes, mouth lesions Metals- e. g. Ti : Type I and VI. HS stomatitis, facial erythema
Allegies in dentristry Chlorhexidine: including allergy (Type I HS ) and allergic contact dermatitis/stomatitis (Type IV HS) Flouride - Type I and VI. HS skin rashes, mouth lesions Metals- e. g. Ti : Type I and VI. HS stomatitis, facial erythema
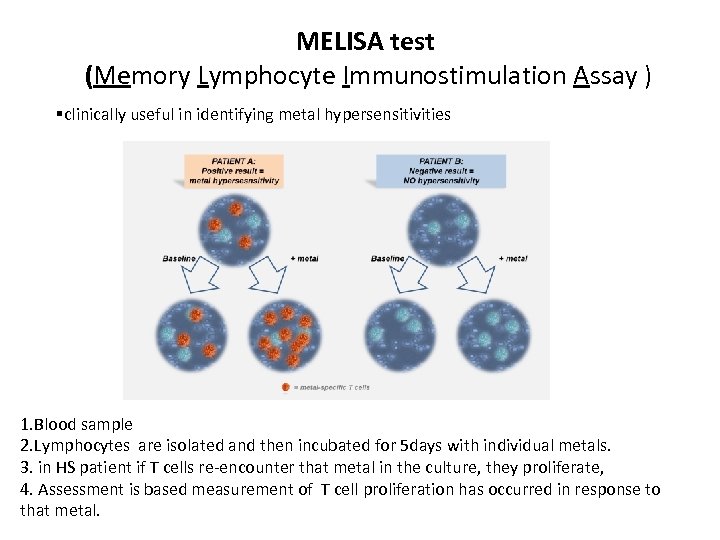 MELISA test (Memory Lymphocyte Immunostimulation Assay ) §clinically useful in identifying metal hypersensitivities 1. Blood sample 2. Lymphocytes are isolated and then incubated for 5 days with individual metals. 3. in HS patient if T cells re-encounter that metal in the culture, they proliferate, 4. Assessment is based measurement of T cell proliferation has occurred in response to that metal.
MELISA test (Memory Lymphocyte Immunostimulation Assay ) §clinically useful in identifying metal hypersensitivities 1. Blood sample 2. Lymphocytes are isolated and then incubated for 5 days with individual metals. 3. in HS patient if T cells re-encounter that metal in the culture, they proliferate, 4. Assessment is based measurement of T cell proliferation has occurred in response to that metal.