17c4585e8fe9461111c48cfa4b670cdf.ppt
- Количество слайдов: 31
 HYPERSENSITIVITY 1
HYPERSENSITIVITY 1
 HYPERSENSITIVITY REACTIONS Over immune reaction refers to excessive, undesirable (damaging, discomfort-producing and sometimes fatal) reactions produced by the normal immune system. 2
HYPERSENSITIVITY REACTIONS Over immune reaction refers to excessive, undesirable (damaging, discomfort-producing and sometimes fatal) reactions produced by the normal immune system. 2
 Hypersensitivity reactions can be divided into four types: type I, type III and type IV, based on the mechanisms involved and time taken for the reaction. Frequently, a particular clinical condition (disease) may involve more than one type of reaction. 3
Hypersensitivity reactions can be divided into four types: type I, type III and type IV, based on the mechanisms involved and time taken for the reaction. Frequently, a particular clinical condition (disease) may involve more than one type of reaction. 3
 Musts for Hypersensitivity Contact with allergen Sensitizing/priming dose Shocking dose 4
Musts for Hypersensitivity Contact with allergen Sensitizing/priming dose Shocking dose 4
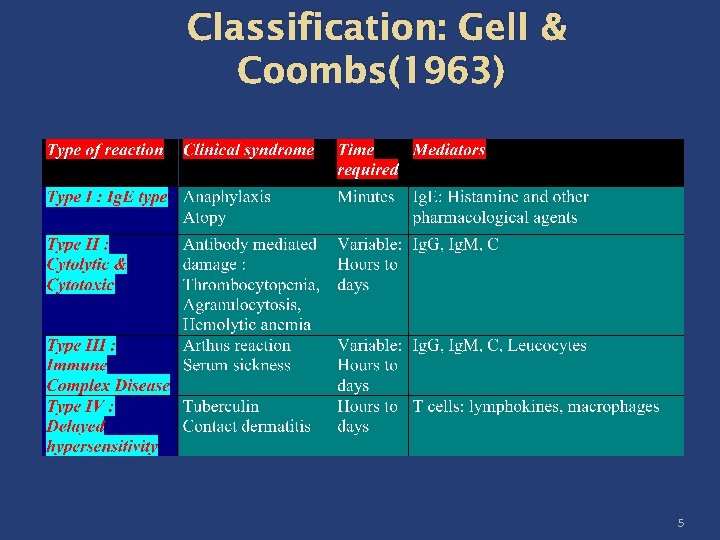 Classification: Gell & Coombs(1963) 5
Classification: Gell & Coombs(1963) 5
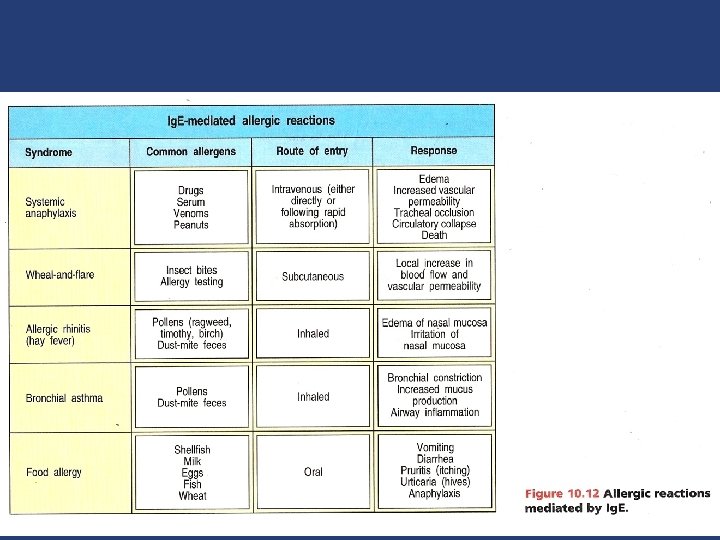
 TYPE I HYPERSENSITIVITY Type I hypersensitivity is also known as immediate or anaphylactic hypersensitivity. The reaction may involve skin (urticaria), eyes (conjunctivitis), nasopharynx (rhinorrhea, rhinitis), bronchopulmonary tissues (asthma) and gastrointestinal tract (gastroenteritis) 6
TYPE I HYPERSENSITIVITY Type I hypersensitivity is also known as immediate or anaphylactic hypersensitivity. The reaction may involve skin (urticaria), eyes (conjunctivitis), nasopharynx (rhinorrhea, rhinitis), bronchopulmonary tissues (asthma) and gastrointestinal tract (gastroenteritis) 6
 Requirements of type I hypersensitivity 1 -Reaginic antibodies: Ig. E mainly , Ig. G 4 uncommon. 2 -cells : The primary cellular component in this hypersensitivity is the mast cell or basophil, have Fc receptors for reaginic antibodies. The reaction is amplified and/or modified by platelets, neutrophils and eosinophils. 7
Requirements of type I hypersensitivity 1 -Reaginic antibodies: Ig. E mainly , Ig. G 4 uncommon. 2 -cells : The primary cellular component in this hypersensitivity is the mast cell or basophil, have Fc receptors for reaginic antibodies. The reaction is amplified and/or modified by platelets, neutrophils and eosinophils. 7
 3 -Allergens (antigens ): these allergens can be inhalants (house dust mites), Ingestants (egg, fish, cheese), Injectants (antibiotics), Cotactants (wool, feather). 8
3 -Allergens (antigens ): these allergens can be inhalants (house dust mites), Ingestants (egg, fish, cheese), Injectants (antibiotics), Cotactants (wool, feather). 8
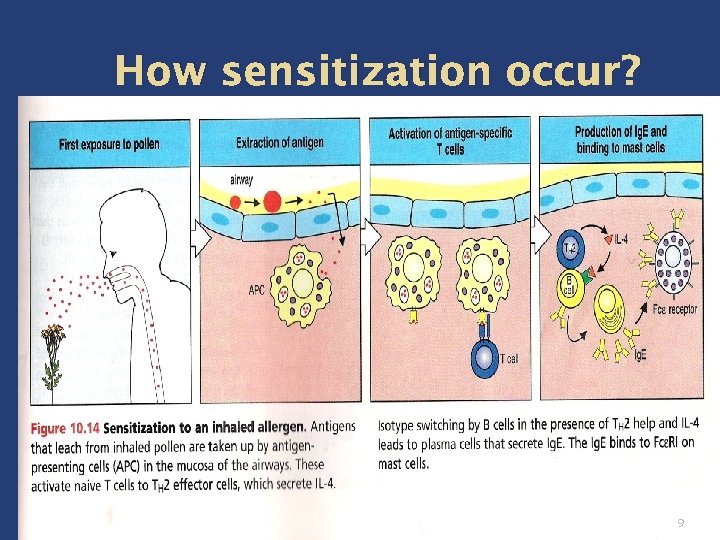 How sensitization occur? 9
How sensitization occur? 9
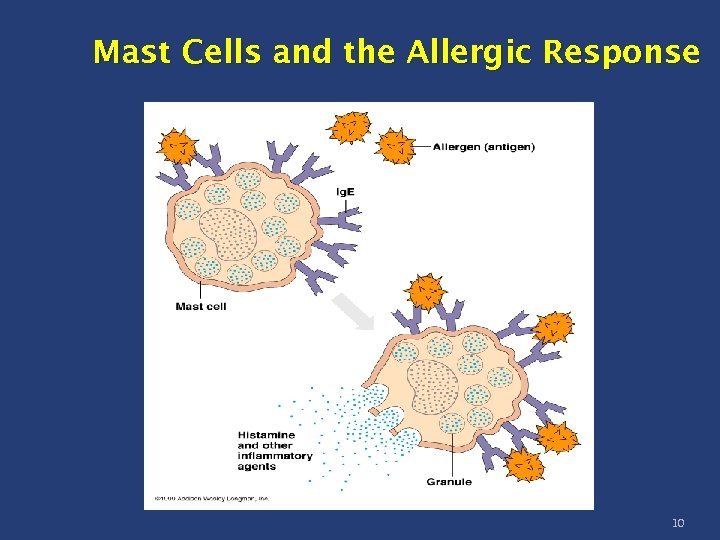 Mast Cells and the Allergic Response 10
Mast Cells and the Allergic Response 10
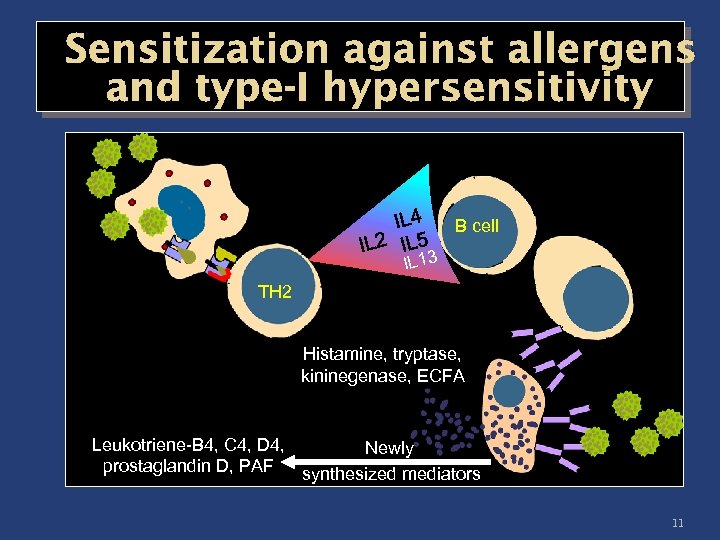 Sensitization against allergens and type-I hypersensitivity B cell IL 13 TH 2 Histamine, tryptase, kininegenase, ECFA Leukotriene-B 4, C 4, D 4, Newly prostaglandin D, PAF synthesized mediators 11
Sensitization against allergens and type-I hypersensitivity B cell IL 13 TH 2 Histamine, tryptase, kininegenase, ECFA Leukotriene-B 4, C 4, D 4, Newly prostaglandin D, PAF synthesized mediators 11
 Kher 12
Kher 12
 Type I Reactions ( Ig. E Mediated) Anaphylaxis – Classical immediate reaction Sensitization Most effective when Ag introduced parenterally May occur by any route exposure to Ag Minute quantities are enough Interval of 2 -3 wks needed between sensitizing & shocking dose Once sensitized it remains so for long time The shocking Ag must be similar to Sensitizing Ag 13
Type I Reactions ( Ig. E Mediated) Anaphylaxis – Classical immediate reaction Sensitization Most effective when Ag introduced parenterally May occur by any route exposure to Ag Minute quantities are enough Interval of 2 -3 wks needed between sensitizing & shocking dose Once sensitized it remains so for long time The shocking Ag must be similar to Sensitizing Ag 13
 Mechanism of anaphylaxis Mediators of anaphylaxis – Primary mediators Preformed contents of Mast cells & Basophils Histamine, serotonin, eosinophils chemotactic factor of anaphylaxis (ECF-A), Neutrophil chemotactic factor (NCF), Heparin & various proteolytic enzymes Secondary mediators – Newly formed after stimulation by Mast cells, Basophils & other leucocytes Slow reacting substance of anaphylaxix (SRS- A), leukotriene , Prostaglandins & Platelet activating factors (PAF) 14
Mechanism of anaphylaxis Mediators of anaphylaxis – Primary mediators Preformed contents of Mast cells & Basophils Histamine, serotonin, eosinophils chemotactic factor of anaphylaxis (ECF-A), Neutrophil chemotactic factor (NCF), Heparin & various proteolytic enzymes Secondary mediators – Newly formed after stimulation by Mast cells, Basophils & other leucocytes Slow reacting substance of anaphylaxix (SRS- A), leukotriene , Prostaglandins & Platelet activating factors (PAF) 14
 Primary Mediators of Anaphylaxis Histamine – Most important vasoactive amine of Human anaphylaxis, formed from histidine found in granules. Released into skin, causes burning & itching. Causes vasodilatation & hyperemia by an axon reflex (Flare) and edema by increasing capillary permeability (Weal). Induces smooth muscle contraction of different tissues & organs. 15
Primary Mediators of Anaphylaxis Histamine – Most important vasoactive amine of Human anaphylaxis, formed from histidine found in granules. Released into skin, causes burning & itching. Causes vasodilatation & hyperemia by an axon reflex (Flare) and edema by increasing capillary permeability (Weal). Induces smooth muscle contraction of different tissues & organs. 15
 Primary Mediators of Anaphylaxis Serotonin (5 -HT) – Base derived by decarbolxylation of Tryptophan. Found in intestinal mucosa, brain & platelets. Causes smooth muscle contraction, ↑ Vascular permeability. 16
Primary Mediators of Anaphylaxis Serotonin (5 -HT) – Base derived by decarbolxylation of Tryptophan. Found in intestinal mucosa, brain & platelets. Causes smooth muscle contraction, ↑ Vascular permeability. 16
 Primary Mediators of Anaphylaxis Chemotactic factors – ECF-A released from mast cell granules are strongly chemotactic for eosinophils. Accounts for high eosinophil counts in many hypersensitivity reactions. NCF – Attracts neutrophils Enzymatic mediatores such as proteases & hydrolases are also released from the mast cell granules. 17
Primary Mediators of Anaphylaxis Chemotactic factors – ECF-A released from mast cell granules are strongly chemotactic for eosinophils. Accounts for high eosinophil counts in many hypersensitivity reactions. NCF – Attracts neutrophils Enzymatic mediatores such as proteases & hydrolases are also released from the mast cell granules. 17
 Secondary mediators of anaphylaxis Prostaglandins & leukotrienes – Derived from Arachidonic acid formed from the disruption of mast cell membrane Lipoxygenase pathway - Leukotrienes Cycloxygenase pathway - Prostaglandins One of the family of Leukotrienes is SRS-A (slow reacting substance of anaphylaxis) Prostaglandins are bronchoconstrictors, affect secretions of mucus glands, platelet adhesion, permeability, dilatation of capillaries & pain threshold. 18
Secondary mediators of anaphylaxis Prostaglandins & leukotrienes – Derived from Arachidonic acid formed from the disruption of mast cell membrane Lipoxygenase pathway - Leukotrienes Cycloxygenase pathway - Prostaglandins One of the family of Leukotrienes is SRS-A (slow reacting substance of anaphylaxis) Prostaglandins are bronchoconstrictors, affect secretions of mucus glands, platelet adhesion, permeability, dilatation of capillaries & pain threshold. 18
 Secondary mediators of anaphylaxis Platelet activating factor – PAF Low mol wt lipid released from basophils Causes aggregation of platelets and release of their vasoactive amines 19
Secondary mediators of anaphylaxis Platelet activating factor – PAF Low mol wt lipid released from basophils Causes aggregation of platelets and release of their vasoactive amines 19
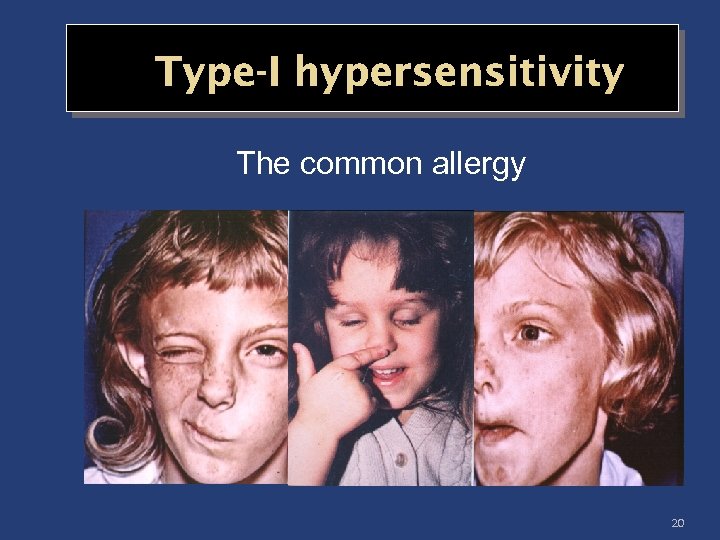 Type-I hypersensitivity The common allergy 20
Type-I hypersensitivity The common allergy 20
 Diagnosis of hypersensitivity I 1 -Tests that are done with patients (In vivo) Skin prick test Prick to prick test 2_tests that are done on blood (in vitro): Detection of total & specific Ig. E Serum eosinophil cataionic protein (poor indicator in chronic asthma). 21
Diagnosis of hypersensitivity I 1 -Tests that are done with patients (In vivo) Skin prick test Prick to prick test 2_tests that are done on blood (in vitro): Detection of total & specific Ig. E Serum eosinophil cataionic protein (poor indicator in chronic asthma). 21
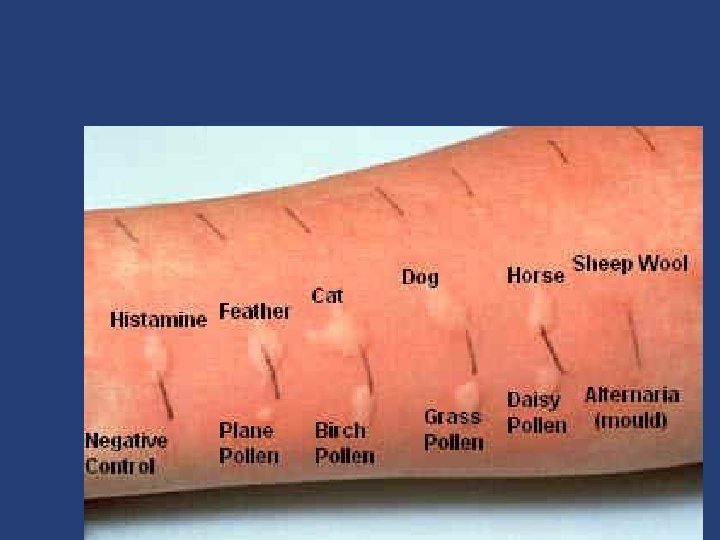
 Skin Prick or Scratch Allergy Testing We use standardized glycerinated extracts of the various allergen extracts such as house dust mite, cat and dog dander, tree, grass and pollen and fungal spores. There is also a negative control (saline) and positive control histamine (used as a quality control reference). 22
Skin Prick or Scratch Allergy Testing We use standardized glycerinated extracts of the various allergen extracts such as house dust mite, cat and dog dander, tree, grass and pollen and fungal spores. There is also a negative control (saline) and positive control histamine (used as a quality control reference). 22
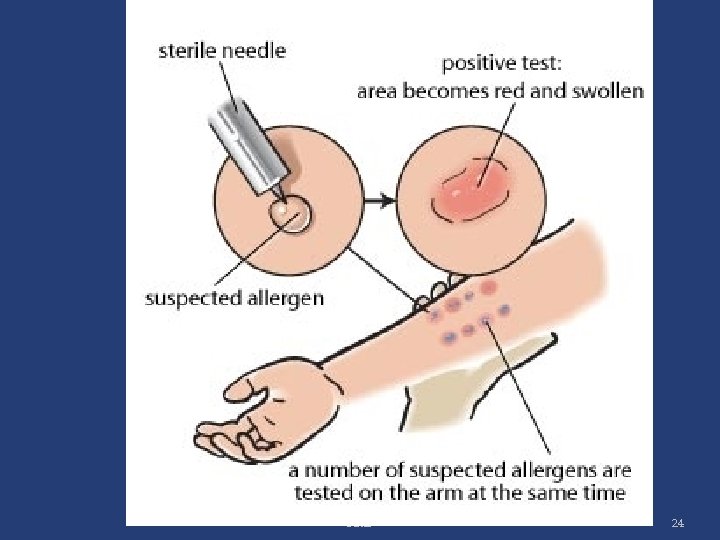
 A droplet of each extract is placed on the inner aspect of the forearm about 3 cm apart and we penetrate through the drop at 90 degrees to the skin using a specially modified lancet A positive result is a typically raised wheal and red flare reaction on the skin. The reactions are read after 15 to 20 minutes and a positive reaction should have at least 3 mm of raised wheal. 23
A droplet of each extract is placed on the inner aspect of the forearm about 3 cm apart and we penetrate through the drop at 90 degrees to the skin using a specially modified lancet A positive result is a typically raised wheal and red flare reaction on the skin. The reactions are read after 15 to 20 minutes and a positive reaction should have at least 3 mm of raised wheal. 23
 Kher 24
Kher 24
 Kher 25
Kher 25
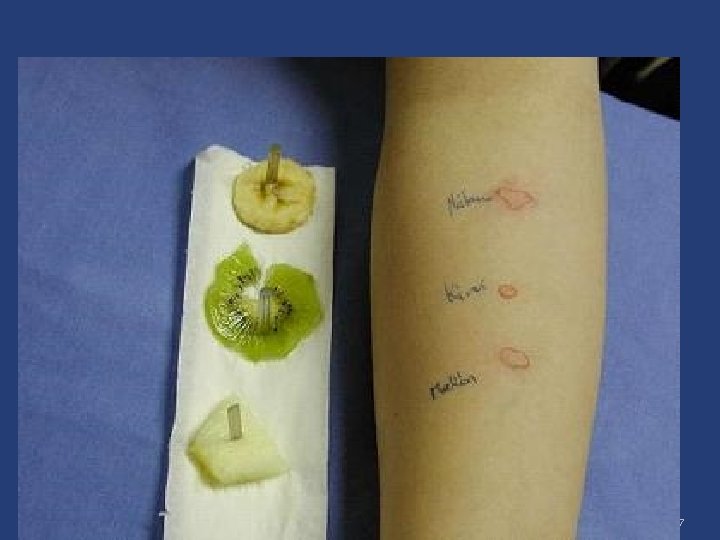
 Prick tests to are a type of Skin Prick tests used for food allergies and are performed using a drop of the fresh food extract. All oral antihistamine medication should be avoided for 2 – 3 days before hand, as these suppress skin reactivity. 26
Prick tests to are a type of Skin Prick tests used for food allergies and are performed using a drop of the fresh food extract. All oral antihistamine medication should be avoided for 2 – 3 days before hand, as these suppress skin reactivity. 26
 Kher 27
Kher 27
 Treatment Three distinct strategies are used to reduce the effects of allergic disease. The first strategy is that contact with allergens should be avoided. 28
Treatment Three distinct strategies are used to reduce the effects of allergic disease. The first strategy is that contact with allergens should be avoided. 28
 second strategy pharmacological Symptomatic treatment is achieved with antihistamines which block histamine receptors. Chromolyn sodium inhibits mast cell degranulation, probably, by inhibiting Ca++ influx 29
second strategy pharmacological Symptomatic treatment is achieved with antihistamines which block histamine receptors. Chromolyn sodium inhibits mast cell degranulation, probably, by inhibiting Ca++ influx 29
 Hyposensitization The third strategy is immunological (immunotherapy or desensitization) is successful in a number of allergies, particularly to insect venoms and, to some extent, pollens. 30
Hyposensitization The third strategy is immunological (immunotherapy or desensitization) is successful in a number of allergies, particularly to insect venoms and, to some extent, pollens. 30
 Patients are given a series of allergen injections in which the dose is initially very small and is gradually increased. This schedule of immunization can gradually convert a TH 2 cell response that produces Ig. E into TH 1 response that ceases to make Ig. E. 31
Patients are given a series of allergen injections in which the dose is initially very small and is gradually increased. This schedule of immunization can gradually convert a TH 2 cell response that produces Ig. E into TH 1 response that ceases to make Ig. E. 31


