hyperparathyroidism.pptx
- Количество слайдов: 37
Hyperparathyroidism Dr. E. Murat AKBAŞ Erzincan University
Hyperparathyroidism • Hyperparathyroidism is a disease characterized by excessive secretion of parathyroid hormone, an 84–amino acid polypeptide hormone. • The secretion of parathyroid hormone is regulated directly by the plasma concentration of ionized calcium.
Hyperparathyroidism • The main effects of parathyroid hormone are; – to increase the concentration of plasma calcium by increasing the release of calcium and phosphate from bone matrix, – increasing calcium reabsorption by the kidney, – and increasing renal production of 1, 25 -dihydroxyvitamin D-3 (calcitriol), which increases intestinal absorption of calcium. • Thus, overproduction of parathyroid hormone results in elevated levels of plasma calcium. • Parathyroid hormone also causes phosphaturia, thereby decreasing serum phosphate levels. • Hyperparathyroidism is usually subdivided into – primary, – secondary, – and tertiary hyperparathyroidism.
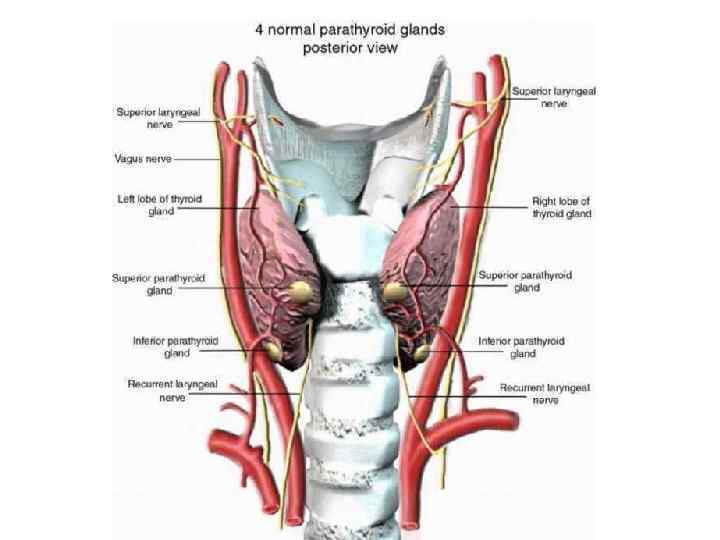
Anatomy and Embryology • Usually, 4 parathyroid glands are situated posterior to the thyroid gland. • The glands are identified based on their location as right or left and superior or inferior. • The inferior glands are derived from the third pharyngeal pouch. This structure is also the embryologic origin of the thymus. • Because of their embryologic association with the thymus, the inferior glands are often found adjacent to or within the thymus. • They are usually located near the inferior pole of the thyroid. • The superior glands are usually found just superior to the intersection of the inferior thyroid artery and the recurrent laryngeal nerve. • The superior glands are derived embryologically from the fourth pharyngeal pouch.
Primary Hyperparathyroidism
Primary Hyperparathyroidism • Primary hyperparathyroidism is the unregulated overproduction of parathyroid hormone (PTH) resulting in abnormal calcium homeostasis. • The prevalence has been reported to be approximately 21 cases per 100, 000 person-years. • The mean age at diagnosis has remained between 52 and 56 years, and women have consistently made up the majority of cases (with a female-tomale ratio of 3: 1).
Pathophysiology • In primary hyperparathyroidism due to adenomas, the normal feedback on parathyroid hormone production by extracellular calcium seems to be lost, resulting in a change in the set point. • However, this is not the case in primary hyperparathyroidism from parathyroid hyperplasia. • An increase in the cell numbers is probably the cause.
Etiology • In approximately 85% of cases, primary hyperparathyroidism is caused by a single adenoma. • In 15% of cases, multiple glands are involved (ie, either multiple adenomas or hyperplasia). • Rarely, primary hyperparathyroidism is caused by parathyroid carcinoma. • The etiology of adenomas or hyperplasia remains unknown in most cases.
Pathophysiology • The chronic excessive resorption of calcium from bone caused by excessive parathyroid hormone can result in osteopenia. • In severe cases, this may result in osteitis fibrosa cystica, which is characterized by – – subperiosteal resorption of the distal phalanges, tapering of the distal clavicles, salt-and-pepper appearance of the skull, and brown tumors of the long bones. • In addition, the chronically increased excretion of calcium in the urine can predispose to the formation of renal stones.
Clinical presentation The clinical syndrome of primary hyperparathyroidism can be easily remembered as "Bones, stones, abdominal groans, and psychic moans. " • Gastrointestinal • Skeletal manifestations; – Selective cortical bone loss manifestations; – – Bone and joint pain, Pseudogout, And chondrocalcinosis Osteitis fibrosa cystica • Renal manifestations; – – polyuria, kidney stones, hypercalciuria, and rarely nephrocalcinosis – – – Anorexia, constipation, Nausea, vomiting, Abdominal pain, Peptic ulcer disease, and Acute pancreatitis.
Clinical presentation • Neuromuscular and psychologic manifestations include; – – – proximal myopathy, weakness and easy fatigability, Depression, inability to concentrate, and memory problems • Cardiovascular manifestations; – – hypertension, bradycardia, shortened QT interval, and left ventricular hypertrophy. • Physical examination; – usually noncontributory – Examination may reveal muscle weakness and depression.
Diagnostic considerations • The causes of hypercalcemia that result in a concomitantly elevated parathyroid hormone level are few. • These include; – familial benign (hypocalciuric) hypercalcemia (FHH) – Lithium-induced hypercalcemia, – and tertiary hyperparathyroidism.
Laboratory studies • Total serum calcium and albumin levels or ionized calcium levels should be measured. • Testing of the intact parathyroid hormone level is the core of the diagnosis. • An elevated intact parathyroid hormone level with an elevated ionized serum calcium level is diagnostic of primary hyperparathyroidism. • A 24 -hour urine calcium measurement is necessary to rule out FHH. • Other laboratory findings in primary hyperparathyroidism include mild hyperchloremic acidosis, hypophosphatemia, and mild-to-moderate increase in urinary calcium excretion rate.
Imaging studies • Imaging studies are not used to make the diagnosis of primary hyperparathyroidism (which is based on laboratory data) or to make a decision about whether to pursue surgical therapy (which is based on clinical criteria). • Imaging studies are used to guide the surgeon once surgical therapy has been decided. – – Neck ultrasonography Nuclear medicine scanning with radiolabeled sestamibi Single-photon emission computed tomography (SPECT) scanning MRI • With either sestamibi scanning or ultrasonography, an abnormal parathyroid may be detected preoperatively in 70 -80% of cases.
Treatment • There is universal agreement that surgical treatment should be offered to all patients with symptomatic disease. • The indications of surgery for asymptomatic disease; – One mg/d. L above the upper limit of the reference range for serum calcium – Twenty-four-hour urinary calcium excretion greater than 400 mg – A 30% reduction in creatinine clearance – Bone mineral density T-score below -2. 5 at any site – Age younger than 50 years

Treatment • Some clinicians advocate surgical therapy in all patients with primary hyperparathyroidism, modified only for those patients who are not able to tolerate surgery. • They argue that the operation is generally well tolerated and such treatment prevents complications and may reverse symptoms that patients often do not realize they have (eg, fatigue, mild depression). • For monitoring of patients with asymptomatic hyperparathyroidism who do not undergo surgery, the following are recommended: – serum calcium and creatinine levels every 6 months and – annual bone mineral density (all 3 sites).
Complications and postoperative care • Calcium levels must be monitored postoperatively every 12 hours until stabilization. • The nadir of serum calcium usually occurs 24 -72 hours postoperatively. • Many patients become hypocalcemic, but few become symptomatic. • Hypocalcemia after parathyroid surgery may be due to hungry bone syndrome where calcium and phosphorus are rapidly deposited in the bone. • If hypoparathyroidism persists, oral supplementation with calcium and vitamin D is required.
Secondary Hyperparathyroidism
Secondary Hyperparathyroidism • Secondary hyperparathyroidism is the overproduction of parathyroid hormone secondary to a chronic abnormal stimulus for its production. • Typically, this is due to chronic renal failure or vitamin D deficiency.
Etiology • In chronic kidney disease, overproduction of parathyroid hormone occurs in response to; – hyperphosphatemia, – hypocalcemia, – and impaired 1, 25 -dihydroxyvitamin D production by the diseased kidneys. • Hyperphosphatemia appears to be particularly important; – it can directly stimulate parathyroid hormone synthesis and parathyroid hyperplasia – and indirectly promotes secondary hyperparathyroidism by decreasing free calcium level.
Pathophysiology • Chronic overproduction of parathyroid hormone in patients with renal failure contributes to the spectrum of bone disease observed in patients on dialysis (eg, osteitis fibrosa cystica and mixed uremic osteodystrophy). • Nonskeletal consequences include cardiovascular calcification, soft tissue calcification, endocrine disturbances, compromised immune system, neurobehavioral changes, and altered erythropoiesis.
Clinical presentation • Because virtually all patients with renal failure have hyperparathyroidism to some degree, the clinical presentation is often that of renal failure. • In patients with secondary hyperparathyroidism due to vitamin D deficiency, the symptoms are mainly due to the vitamin deficiency. • In advanced cases of secondary hyperparathyroidism, some patients may have bone pain.
Laboratory studies • Serum level of parathyroid hormone, calcium, phosphorus, and 25 - hydroxyvitamin D should be measured. • Patients with secondary hyperparathyroidism usually have a low-normal calcium and elevated parathyroid hormone. • The phosphate level may vary based on the etiology, trending towards high values in renal insufficiency and low values in vitamin D deficiency. • Vitamin D deficiency is defined by most experts as a 25 hydroxyvitamin D level of less than 20 ng per milliliter (50 nmol per liter). • A level of 21 -29 ng per milliliter can be considered to indicate relative insufficiency of vitamin D and a level of 30 ng per milliliter or greater can be considered to indicate sufficient vitamin D.
Imaging studies • Imaging of the parathyroid glands is not indicated unless primary hyperparathyroidism is suggested. • Radiographic evaluation is limited to assessments of the bone disease.
Treatment • Unlike primary hyperparathyroidism, medical management is the mainstay of treatment for secondary hyperparathyroidism. • Correcting vitamin D deficiency can be achieved using 50, 000 -IU capsule of vitamin D 2/D-3 once a week for 8 weeks and repeating the course for another 8 weeks if needed to achieve vitamin D sufficiency.
Treatment • For patients with chronic kidney disease, it has been recommended to reduce parathyroid hormone levels to within a range that supports normal bone turnover and minimizes ectopic calcification. • Dietary phosphate restriction can be initiated if parathyroid hormone is elevated despite sufficient 25 -hydroxyvitamin D (>30 ng/m. L). • Phosphate binders can be used if hyperphosphatemia persists despite dietary phosphate restriction. These include; – calcium-based phosphate binders such as calcium carbonate or calcium acetate – and non-calcium-based phosphate binders such as sevelamer hydrochloride. • Calcium supplementation should be limited to less than 2 g/d. • Vitamin D and its analogs may be used, including calcitriol and analogs of calcitriol, including paricalcitol, doxercalciferol, maxacalcitol, and falecalcitriol. • non-calcium/non-Vitamin D analog ; Cinecalcet; reduce the need for parathyroidectomy for refractory hyperparathyroidism.
Treatment • Parathyroidectomy can be considered in patients with severe hyperparathyroidism (persistent serum levels of intact parathyroid hormone greater than 800 pg/m. L [88. 0 pmol/L]), associated with hypercalcemia and/or hyperphosphatemia that is refractory to medical therapy. • The procedure of choice is either total parathyroidectomy with autotransplantation or 3. 5 -gland parathyroidectomy.
Tertiary Hyperparathyroidism
Tertiary Hyperparathyroidism • Tertiary hyperparathyroidism is a state of excessive secretion of parathyroid hormone after longstanding secondary hyperparathyroidism and resulting in hypercalcemia. • The etiology is unknown but may be due to monoclonal expansion of parathyroid cells (nodule formation within hyperplastic glands). • A change may occur in the set point of the calcium-sensing mechanism to hypercalcemic levels. • Four-gland involvement occurs in most patients.
Tertiary Hyperparathyroidism • The hypertrophied parathyroid glands fail to return to normal and continue to oversecrete parathyroid hormone, despite serum calcium levels that are within the reference range or even elevated. • In these cases, the hypertrophied glands become autonomic and cause hypercalcemia, even after withdrawal of calcium and calcitriol therapy. • They also may become resistant to calcimimetic treatment. • This type of tertiary disease is particularly dangerous because the phosphate level is often elevated. • If the calcium value multiplied by the phosphate value yields a high product, diffuse calcinosis may occur.
Clinical presentation/Treatment • The clinical manifestations of tertiary hyperparathyroidism include persistent hyperparathyroidism after renal transplantation or new hypercalcemia in the setting of chronic secondary hyperparathyroidism. • Total parathyroidectomy with autotransplantation or subtotal parathyroidectomy is indicated.
Related Disorders
Related Disorders Familial benign (hypocalciuric) hypercalcemia • Familial benign (hypocalciuric hypercalcemia (FHH) is caused by a loss-of-function mutation of one allele of the gene for the calcium-sensing receptor (Ca. R). • It causes hypercalcemia, hypophosphatemia, and hypermagnesemia. • The parathyroid hormone level is usually within the reference range or is mildly elevated. • It can be distinguished from primary hyperparathyroidism by low 24 -hour urinary calcium excretion. • Persons with FHH are asymptomatic. • Parathyroidectomy is not indicated.
Related Disorders Hypercalcemia of malignancy • This disorder is usually caused by tumor release of a hormone called parathyroid hormone -related peptide. • Less commonly, hypercalcemia of malignancy is caused by local osteolytic lesions and, rarely, by overproduction of 1, 25 -dihydroxyvitamin D. • This disorder is the most common cause of hypercalcemia in hospitalized patients. • The hypercalcemia of malignancy results in a low or undetectable intact parathyroid hormone level. • Usually, it is easily distinguished from hyperparathyroidism. • Only a few cases of ectopic production of true parathyroid hormone are reported in the literature.
Related Disorders Calciphylaxis • Calciphylaxis, also known as uremic gangrene syndrome, is a rare disorder observed in patients with renal failure and secondary or tertiary hyperparathyroidism. • It is characterized by ischemic necrosis of the skin due to calcium phosphate crystal deposition and subsequent inflammation in small-to-medium–sized vessels. • The exact mechanism is unknown because the product of the calcium value multiplied by the phosphate value is often near the reference range. • The disease is often fatal. • In many cases, total parathyroidectomy appears to reverse the course of the disease.

hyperparathyroidism.pptx