274d5ef4686851c949495522c6cd12ba.ppt
- Количество слайдов: 79
 How to Successfully Influence Test Utilization & Improve Laboratory Efficiency Fred V. Plapp, Cynthia Essmyer, Anne Byrd & Marjorie Zucker Saint Luke’s Health System Kansas City
How to Successfully Influence Test Utilization & Improve Laboratory Efficiency Fred V. Plapp, Cynthia Essmyer, Anne Byrd & Marjorie Zucker Saint Luke’s Health System Kansas City
 Why Be Concerned About Excessive Testing? 1. Increased laboratory costs § Once operational efficiencies are maximized, reducing unnecessary testing is the only way to significantly reduce costs 2. Payer pressure § § Continued squeeze on reimbursement Required documentation of utilization
Why Be Concerned About Excessive Testing? 1. Increased laboratory costs § Once operational efficiencies are maximized, reducing unnecessary testing is the only way to significantly reduce costs 2. Payer pressure § § Continued squeeze on reimbursement Required documentation of utilization
 Why Be Concerned About Test Utilization? 3. Increased potential for direct & indirect harm n Increased number of false & weak positives n Follow-up increases cost, worry, discomfort, risk n Confirmatory tests n Specialist referrals n Invasive procedures n Unnecessary postponement of procedure n Attention diverted from primary problem
Why Be Concerned About Test Utilization? 3. Increased potential for direct & indirect harm n Increased number of false & weak positives n Follow-up increases cost, worry, discomfort, risk n Confirmatory tests n Specialist referrals n Invasive procedures n Unnecessary postponement of procedure n Attention diverted from primary problem
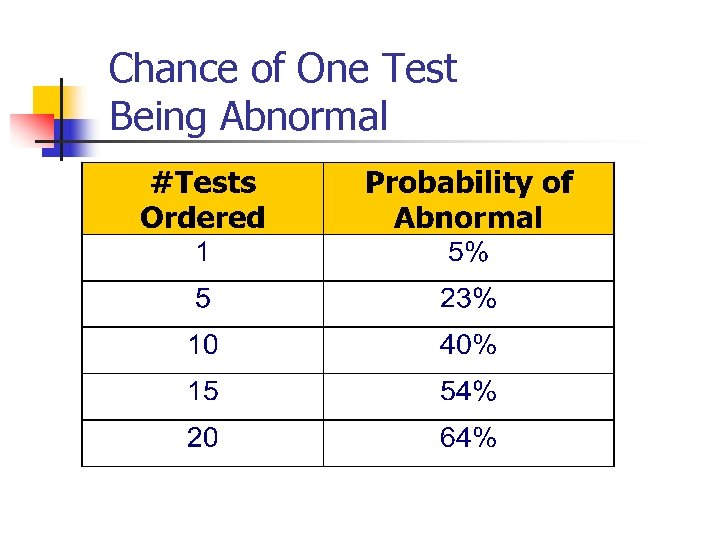 Chance of One Test Being Abnormal
Chance of One Test Being Abnormal
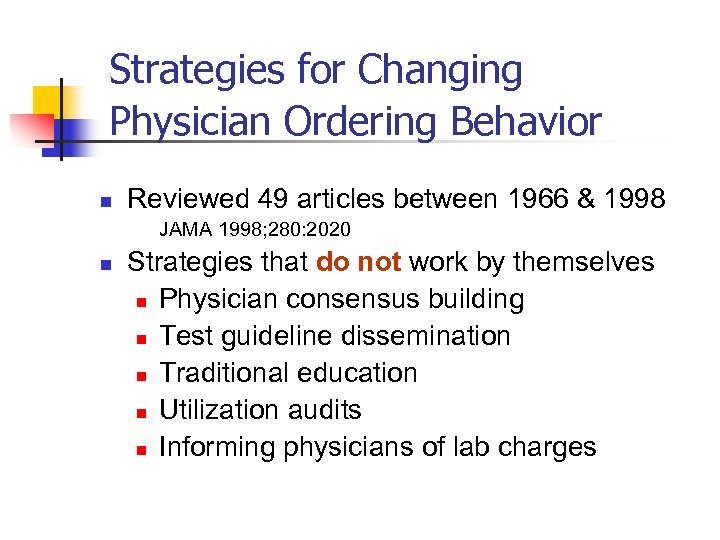 Strategies for Changing Physician Ordering Behavior n Reviewed 49 articles between 1966 & 1998 JAMA 1998; 280: 2020 n Strategies that do not work by themselves n Physician consensus building n Test guideline dissemination n Traditional education n Utilization audits n Informing physicians of lab charges
Strategies for Changing Physician Ordering Behavior n Reviewed 49 articles between 1966 & 1998 JAMA 1998; 280: 2020 n Strategies that do not work by themselves n Physician consensus building n Test guideline dissemination n Traditional education n Utilization audits n Informing physicians of lab charges
 Strategies for Changing Physician Ordering Behavior n Strategies that do work n n n Administrative interventions Environmental interventions Combinations with other strategies
Strategies for Changing Physician Ordering Behavior n Strategies that do work n n n Administrative interventions Environmental interventions Combinations with other strategies
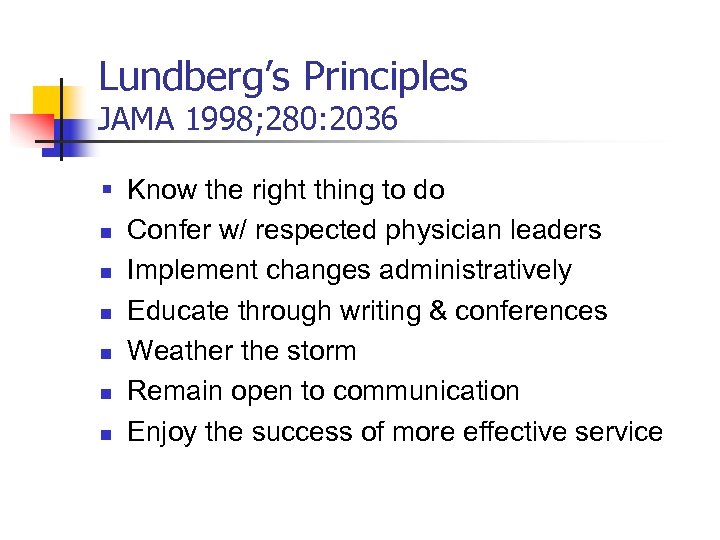 Lundberg’s Principles JAMA 1998; 280: 2036 § Know the right thing to do n Confer w/ respected physician leaders n Implement changes administratively n Educate through writing & conferences n Weather the storm n Remain open to communication n Enjoy the success of more effective service
Lundberg’s Principles JAMA 1998; 280: 2036 § Know the right thing to do n Confer w/ respected physician leaders n Implement changes administratively n Educate through writing & conferences n Weather the storm n Remain open to communication n Enjoy the success of more effective service
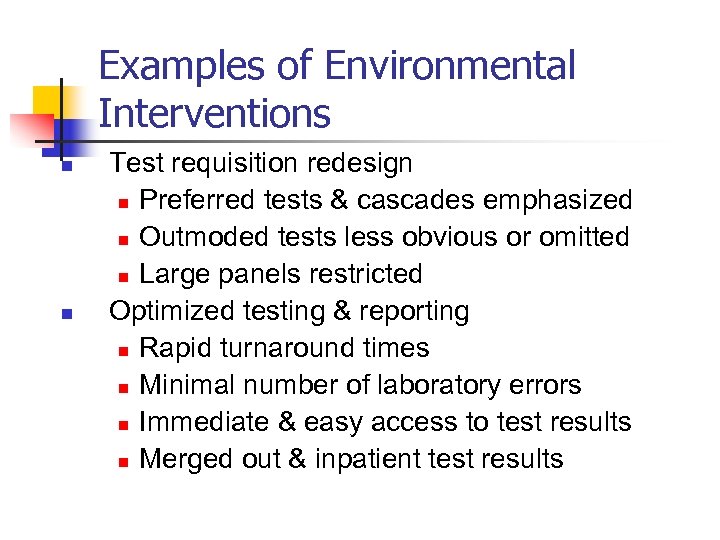 Examples of Environmental Interventions n n Test requisition redesign n Preferred tests & cascades emphasized n Outmoded tests less obvious or omitted n Large panels restricted Optimized testing & reporting n Rapid turnaround times n Minimal number of laboratory errors n Immediate & easy access to test results n Merged out & inpatient test results
Examples of Environmental Interventions n n Test requisition redesign n Preferred tests & cascades emphasized n Outmoded tests less obvious or omitted n Large panels restricted Optimized testing & reporting n Rapid turnaround times n Minimal number of laboratory errors n Immediate & easy access to test results n Merged out & inpatient test results
 Examples of Administrative Interventions n Administrative policy changes n n Pathologist approval for special tests Pathologist approval of send out tests Test intervals, frequencies & reflex policy Financial feedback n n Review of CPT codes denied payment Decision support systems
Examples of Administrative Interventions n Administrative policy changes n n Pathologist approval for special tests Pathologist approval of send out tests Test intervals, frequencies & reflex policy Financial feedback n n Review of CPT codes denied payment Decision support systems
 Examples of Educational Interventions n Clinical Laboratory Letter n n Clinical pathways n n n Test recommendations & algorithms Practice guidelines w/ standardized testing Timely pathology consults Physician feedback n Test utilization by service or peer group
Examples of Educational Interventions n Clinical Laboratory Letter n n Clinical pathways n n n Test recommendations & algorithms Practice guidelines w/ standardized testing Timely pathology consults Physician feedback n Test utilization by service or peer group
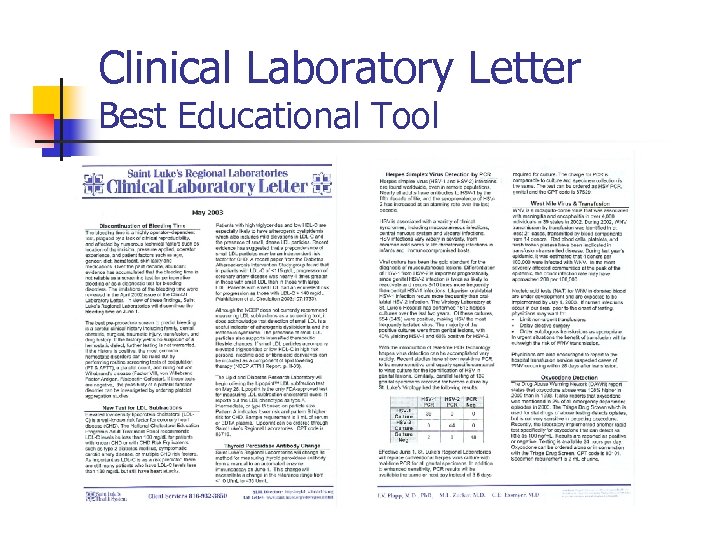 Clinical Laboratory Letter Best Educational Tool
Clinical Laboratory Letter Best Educational Tool
 Analyzing the Problem n High test volume & diverse test menu n n 2 million tests performed per year >300 different tests offered No single project would be effective Multi-pronged long term strategy was required
Analyzing the Problem n High test volume & diverse test menu n n 2 million tests performed per year >300 different tests offered No single project would be effective Multi-pronged long term strategy was required
 Arriving at a Solution n n Pathologists & staff continuously monitor testing trends within their areas of expertise Targeted tests with following characteristics: n High volume n Expensive n Difficult to perform n Questionable medical benefit n Unusual number of abnormal results
Arriving at a Solution n n Pathologists & staff continuously monitor testing trends within their areas of expertise Targeted tests with following characteristics: n High volume n Expensive n Difficult to perform n Questionable medical benefit n Unusual number of abnormal results
 Action Plan n Lab collaborated with: n n n Pathologists discussed proposals with: n n Hospital departments & patient care committees Nursing and medical staffs Key physicians Entire medical departments Hospital Performance Improvement committee Clinical Laboratory Letter n Published test utilization data & algorithms
Action Plan n Lab collaborated with: n n n Pathologists discussed proposals with: n n Hospital departments & patient care committees Nursing and medical staffs Key physicians Entire medical departments Hospital Performance Improvement committee Clinical Laboratory Letter n Published test utilization data & algorithms
 Types of Projects Undertaken n n n Excessive Tests Obsolete Tests Clinical Pathways Reference Ranges Wastage Turnaround Time n n n Algorithms & Reflex Testing Send Out Tests In-sourcing Tests Transfusion Error Rate
Types of Projects Undertaken n n n Excessive Tests Obsolete Tests Clinical Pathways Reference Ranges Wastage Turnaround Time n n n Algorithms & Reflex Testing Send Out Tests In-sourcing Tests Transfusion Error Rate
 Vancomycin Monitoring Example of Excess Testing n Clinical pharmacologists noted too many drug levels ordered in 1994 n n n Peak & trough levels ordered together Little scientific evidence supporting peak Lab & Pharmacy educated medical staff n n n Presented at medical staff meetings Published data in Clinical Laboratory Letter Deleted peak from computer order screens
Vancomycin Monitoring Example of Excess Testing n Clinical pharmacologists noted too many drug levels ordered in 1994 n n n Peak & trough levels ordered together Little scientific evidence supporting peak Lab & Pharmacy educated medical staff n n n Presented at medical staff meetings Published data in Clinical Laboratory Letter Deleted peak from computer order screens
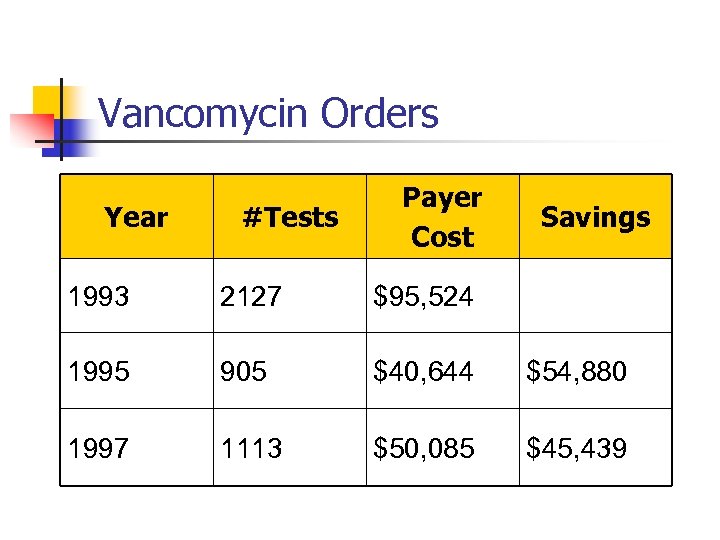 Vancomycin Orders Year #Tests Payer Cost Savings 1993 2127 $95, 524 1995 905 $40, 644 $54, 880 1997 1113 $50, 085 $45, 439
Vancomycin Orders Year #Tests Payer Cost Savings 1993 2127 $95, 524 1995 905 $40, 644 $54, 880 1997 1113 $50, 085 $45, 439
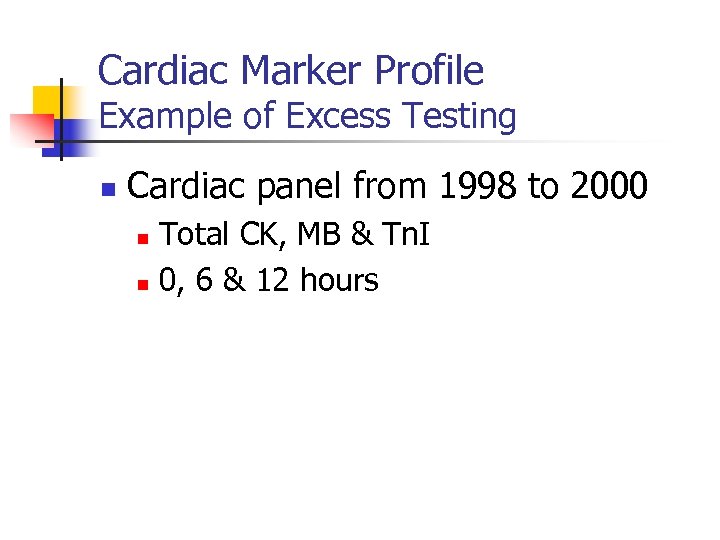 Cardiac Marker Profile Example of Excess Testing n Cardiac panel from 1998 to 2000 Total CK, MB & Tn. I n 0, 6 & 12 hours n
Cardiac Marker Profile Example of Excess Testing n Cardiac panel from 1998 to 2000 Total CK, MB & Tn. I n 0, 6 & 12 hours n
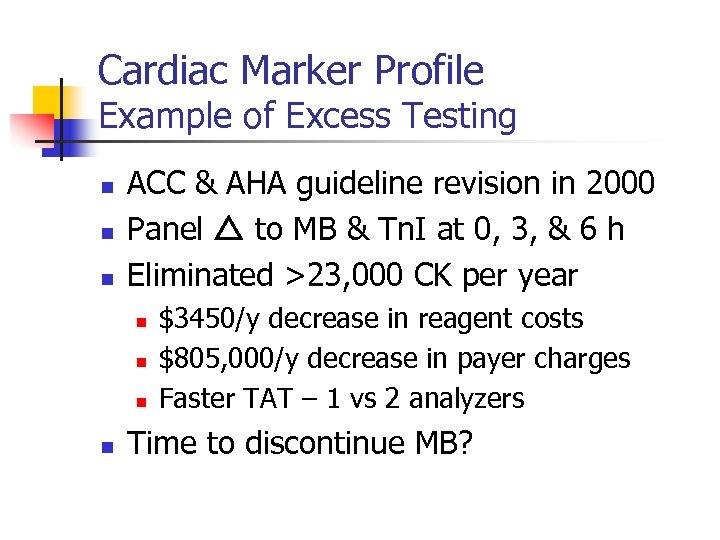 Cardiac Marker Profile Example of Excess Testing n n n ACC & AHA guideline revision in 2000 Panel to MB & Tn. I at 0, 3, & 6 h Eliminated >23, 000 CK per year n n $3450/y decrease in reagent costs $805, 000/y decrease in payer charges Faster TAT – 1 vs 2 analyzers Time to discontinue MB?
Cardiac Marker Profile Example of Excess Testing n n n ACC & AHA guideline revision in 2000 Panel to MB & Tn. I at 0, 3, & 6 h Eliminated >23, 000 CK per year n n $3450/y decrease in reagent costs $805, 000/y decrease in payer charges Faster TAT – 1 vs 2 analyzers Time to discontinue MB?
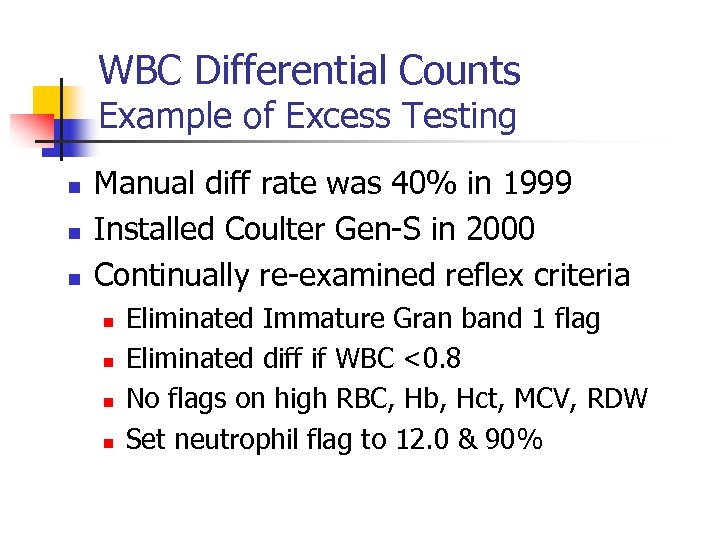 WBC Differential Counts Example of Excess Testing n n n Manual diff rate was 40% in 1999 Installed Coulter Gen-S in 2000 Continually re-examined reflex criteria n n Eliminated Immature Gran band 1 flag Eliminated diff if WBC <0. 8 No flags on high RBC, Hb, Hct, MCV, RDW Set neutrophil flag to 12. 0 & 90%
WBC Differential Counts Example of Excess Testing n n n Manual diff rate was 40% in 1999 Installed Coulter Gen-S in 2000 Continually re-examined reflex criteria n n Eliminated Immature Gran band 1 flag Eliminated diff if WBC <0. 8 No flags on high RBC, Hb, Hct, MCV, RDW Set neutrophil flag to 12. 0 & 90%
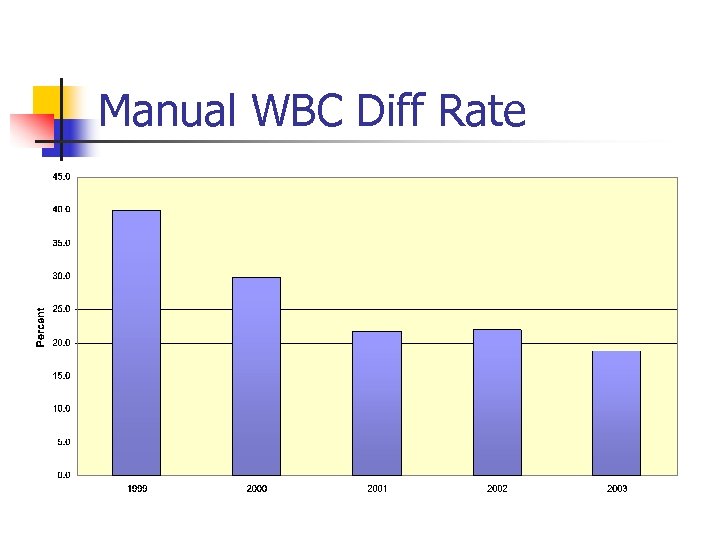 Manual WBC Diff Rate
Manual WBC Diff Rate
 WBC Differential Counts SLH Outcomes n n n Avoid 15, 000 manual diffs per year CAP average time = 11 minutes/slide Save 2750 hours of labor per year n n >1 FTE Expect rate to further in 2004 n n New analyzer Eliminate band counts
WBC Differential Counts SLH Outcomes n n n Avoid 15, 000 manual diffs per year CAP average time = 11 minutes/slide Save 2750 hours of labor per year n n >1 FTE Expect rate to further in 2004 n n New analyzer Eliminate band counts
 Rapid Bacterial Antigen Tests Example of an Obsolete Test n Introduced in 1980 s for Dx of bacterial meningitis n H flu n N meningitidis n E coli n S pneumo n GBS
Rapid Bacterial Antigen Tests Example of an Obsolete Test n Introduced in 1980 s for Dx of bacterial meningitis n H flu n N meningitidis n E coli n S pneumo n GBS
 Rapid Bacterial Antigen Tests Example of an Obsolete Test n Clinical utility questioned today n n n Not sensitive enough to rule out bacterial origin Not specific enough to direct antibiotic therapy Improved empiric antibiotic Rx available
Rapid Bacterial Antigen Tests Example of an Obsolete Test n Clinical utility questioned today n n n Not sensitive enough to rule out bacterial origin Not specific enough to direct antibiotic therapy Improved empiric antibiotic Rx available
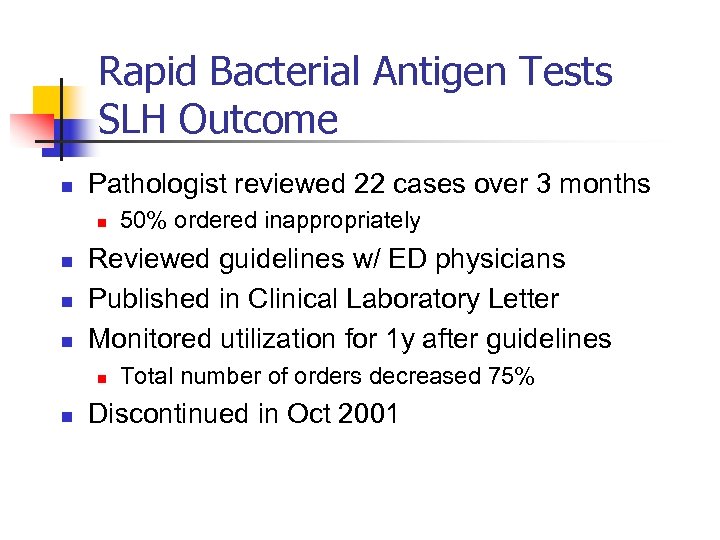 Rapid Bacterial Antigen Tests SLH Outcome n Pathologist reviewed 22 cases over 3 months n n Reviewed guidelines w/ ED physicians Published in Clinical Laboratory Letter Monitored utilization for 1 y after guidelines n n 50% ordered inappropriately Total number of orders decreased 75% Discontinued in Oct 2001
Rapid Bacterial Antigen Tests SLH Outcome n Pathologist reviewed 22 cases over 3 months n n Reviewed guidelines w/ ED physicians Published in Clinical Laboratory Letter Monitored utilization for 1 y after guidelines n n 50% ordered inappropriately Total number of orders decreased 75% Discontinued in Oct 2001
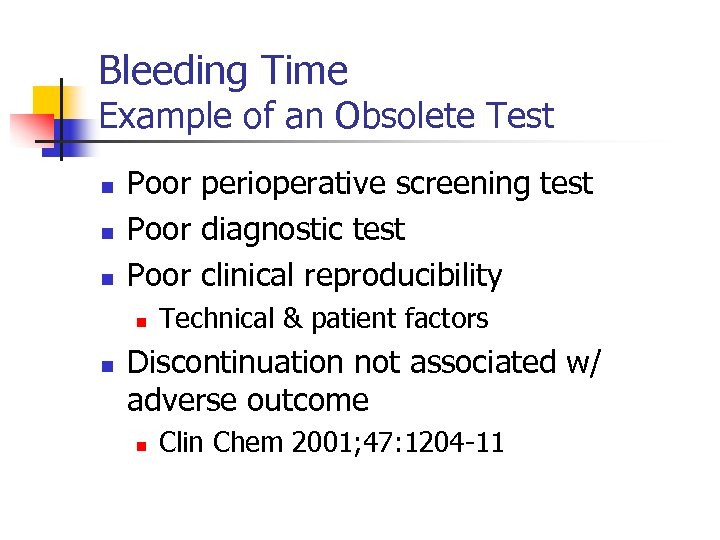 Bleeding Time Example of an Obsolete Test n n n Poor perioperative screening test Poor diagnostic test Poor clinical reproducibility n n Technical & patient factors Discontinuation not associated w/ adverse outcome n Clin Chem 2001; 47: 1204 -11
Bleeding Time Example of an Obsolete Test n n n Poor perioperative screening test Poor diagnostic test Poor clinical reproducibility n n Technical & patient factors Discontinuation not associated w/ adverse outcome n Clin Chem 2001; 47: 1204 -11
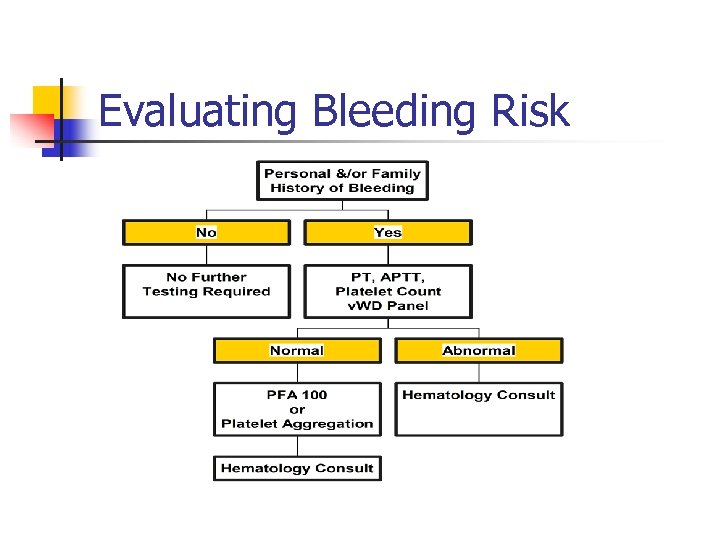 Evaluating Bleeding Risk
Evaluating Bleeding Risk
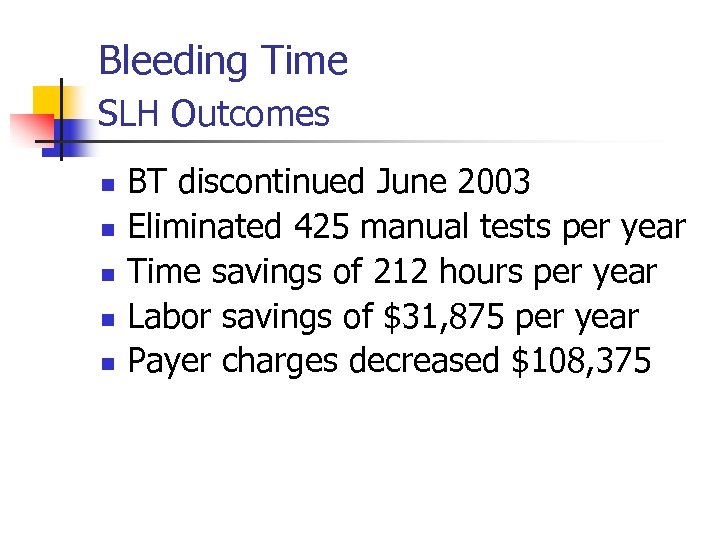 Bleeding Time SLH Outcomes n n n BT discontinued June 2003 Eliminated 425 manual tests per year Time savings of 212 hours per year Labor savings of $31, 875 per year Payer charges decreased $108, 375
Bleeding Time SLH Outcomes n n n BT discontinued June 2003 Eliminated 425 manual tests per year Time savings of 212 hours per year Labor savings of $31, 875 per year Payer charges decreased $108, 375
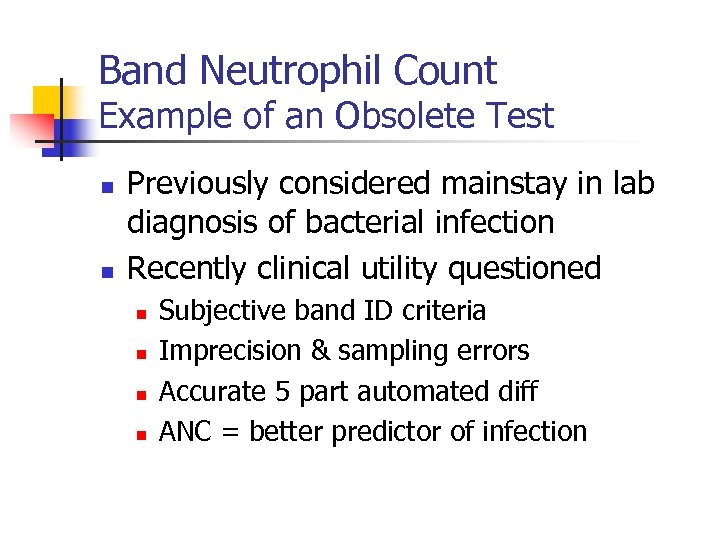 Band Neutrophil Count Example of an Obsolete Test n n Previously considered mainstay in lab diagnosis of bacterial infection Recently clinical utility questioned n n Subjective band ID criteria Imprecision & sampling errors Accurate 5 part automated diff ANC = better predictor of infection
Band Neutrophil Count Example of an Obsolete Test n n Previously considered mainstay in lab diagnosis of bacterial infection Recently clinical utility questioned n n Subjective band ID criteria Imprecision & sampling errors Accurate 5 part automated diff ANC = better predictor of infection
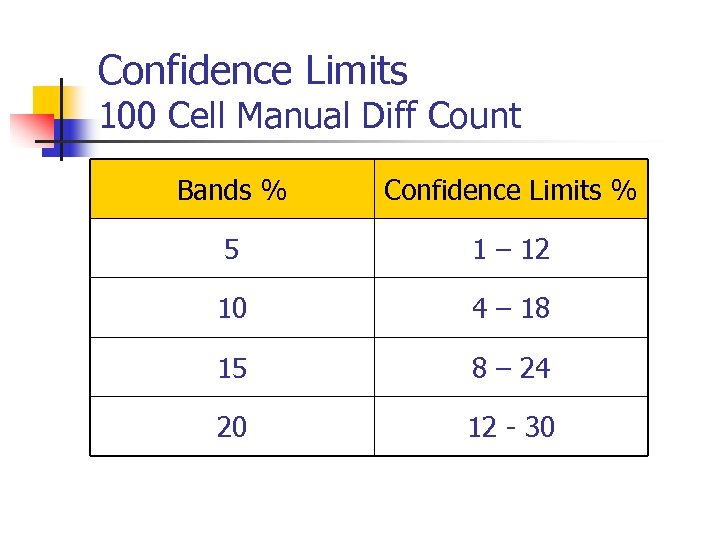 Confidence Limits 100 Cell Manual Diff Count Bands % Confidence Limits % 5 1 – 12 10 4 – 18 15 8 – 24 20 12 - 30
Confidence Limits 100 Cell Manual Diff Count Bands % Confidence Limits % 5 1 – 12 10 4 – 18 15 8 – 24 20 12 - 30
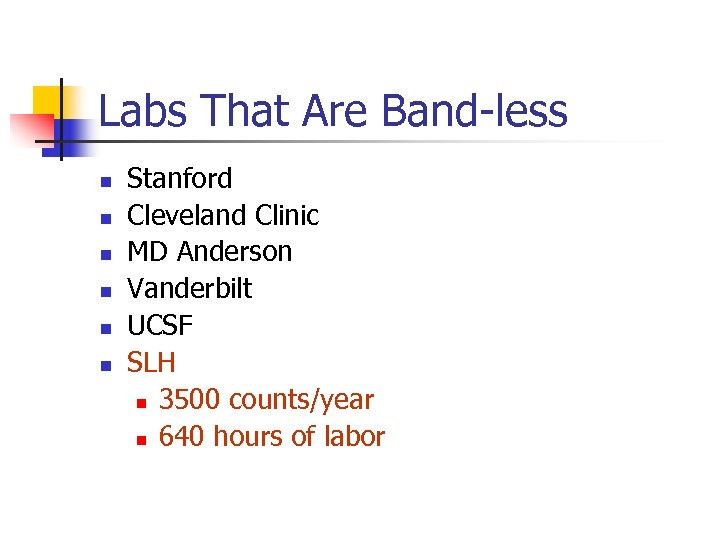 Labs That Are Band-less n n n Stanford Cleveland Clinic MD Anderson Vanderbilt UCSF SLH n 3500 counts/year n 640 hours of labor
Labs That Are Band-less n n n Stanford Cleveland Clinic MD Anderson Vanderbilt UCSF SLH n 3500 counts/year n 640 hours of labor
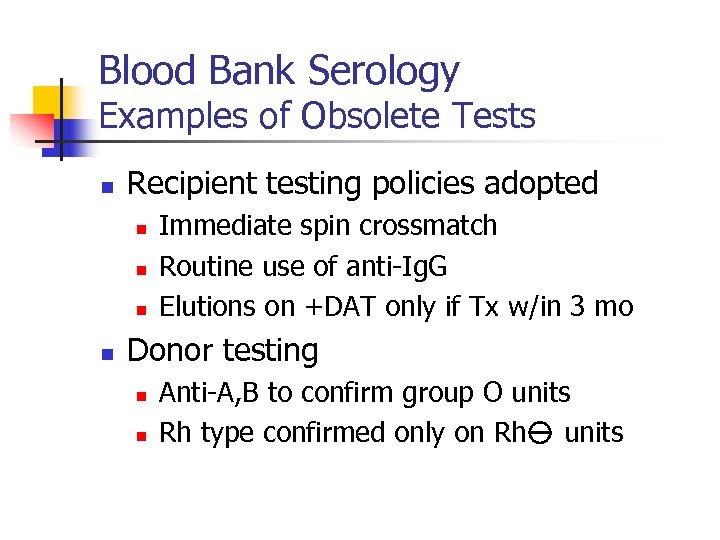 Blood Bank Serology Examples of Obsolete Tests n Recipient testing policies adopted n n Immediate spin crossmatch Routine use of anti-Ig. G Elutions on +DAT only if Tx w/in 3 mo Donor testing n n Anti-A, B to confirm group O units Rh type confirmed only on Rh units
Blood Bank Serology Examples of Obsolete Tests n Recipient testing policies adopted n n Immediate spin crossmatch Routine use of anti-Ig. G Elutions on +DAT only if Tx w/in 3 mo Donor testing n n Anti-A, B to confirm group O units Rh type confirmed only on Rh units
 Blood Bank Serology Examples of Obsolete Tests n Recipient tests eliminated n n n Anti-A, B testing on recipients Autocontrol Weak D testing including moms Reading Ab screen after immediate spin Antigen typing for insignificant Ab
Blood Bank Serology Examples of Obsolete Tests n Recipient tests eliminated n n n Anti-A, B testing on recipients Autocontrol Weak D testing including moms Reading Ab screen after immediate spin Antigen typing for insignificant Ab
 Blood Bank Serology Examples of Obsolete Tests n Cord blood test policies n n ABO & Rh typing only if mom is Group O or Rh negative No elution if DAT+
Blood Bank Serology Examples of Obsolete Tests n Cord blood test policies n n ABO & Rh typing only if mom is Group O or Rh negative No elution if DAT+
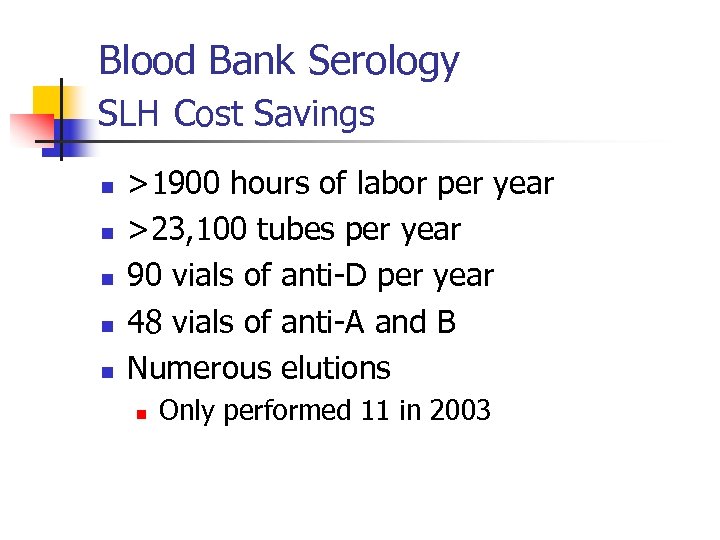 Blood Bank Serology SLH Cost Savings n n n >1900 hours of labor per year >23, 100 tubes per year 90 vials of anti-D per year 48 vials of anti-A and B Numerous elutions n Only performed 11 in 2003
Blood Bank Serology SLH Cost Savings n n n >1900 hours of labor per year >23, 100 tubes per year 90 vials of anti-D per year 48 vials of anti-A and B Numerous elutions n Only performed 11 in 2003
 Clinical Pathways Example of Practice Guidelines n n Nurses & physicians wrote guidelines Pathologists reviewed lab tests Suggestions returned to authors Test utilization monitored before & after
Clinical Pathways Example of Practice Guidelines n n Nurses & physicians wrote guidelines Pathologists reviewed lab tests Suggestions returned to authors Test utilization monitored before & after
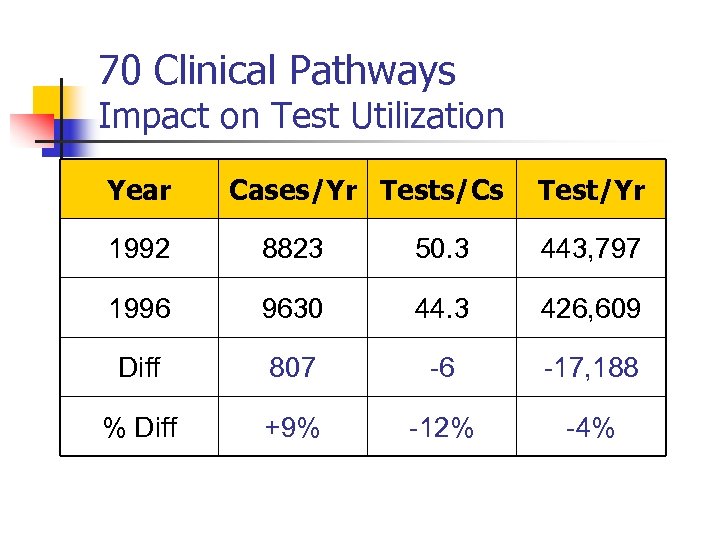 70 Clinical Pathways Impact on Test Utilization Year Cases/Yr Tests/Cs Test/Yr 1992 8823 50. 3 443, 797 1996 9630 44. 3 426, 609 Diff 807 -6 -17, 188 % Diff +9% -12% -4%
70 Clinical Pathways Impact on Test Utilization Year Cases/Yr Tests/Cs Test/Yr 1992 8823 50. 3 443, 797 1996 9630 44. 3 426, 609 Diff 807 -6 -17, 188 % Diff +9% -12% -4%
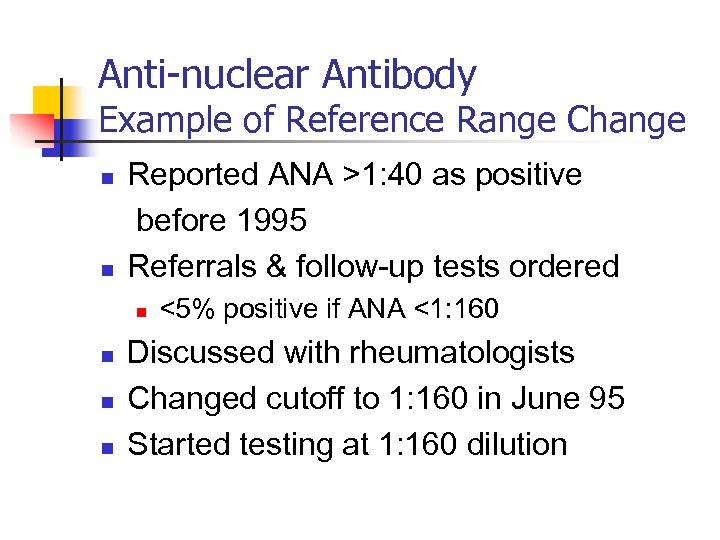 Anti-nuclear Antibody Example of Reference Range Change n n Reported ANA >1: 40 as positive before 1995 Referrals & follow-up tests ordered n n <5% positive if ANA <1: 160 Discussed with rheumatologists Changed cutoff to 1: 160 in June 95 Started testing at 1: 160 dilution
Anti-nuclear Antibody Example of Reference Range Change n n Reported ANA >1: 40 as positive before 1995 Referrals & follow-up tests ordered n n <5% positive if ANA <1: 160 Discussed with rheumatologists Changed cutoff to 1: 160 in June 95 Started testing at 1: 160 dilution
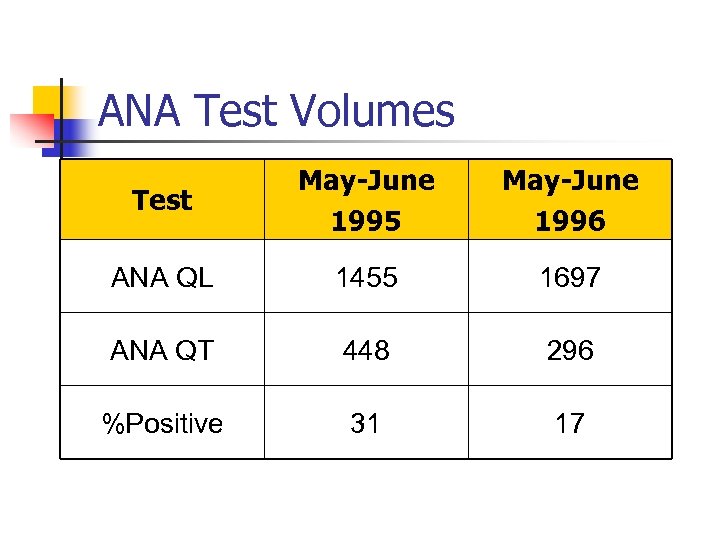 ANA Test Volumes Test May-June 1995 May-June 1996 ANA QL 1455 1697 ANA QT 448 296 %Positive 31 17
ANA Test Volumes Test May-June 1995 May-June 1996 ANA QL 1455 1697 ANA QT 448 296 %Positive 31 17
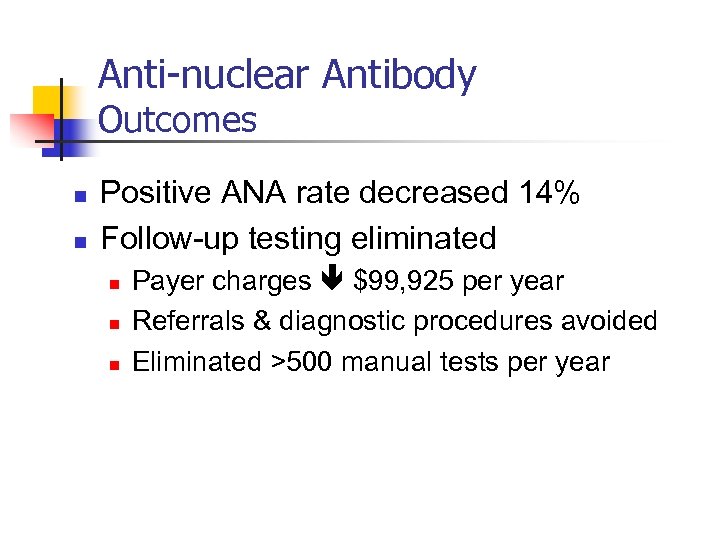 Anti-nuclear Antibody Outcomes n n Positive ANA rate decreased 14% Follow-up testing eliminated n n n Payer charges $99, 925 per year Referrals & diagnostic procedures avoided Eliminated >500 manual tests per year
Anti-nuclear Antibody Outcomes n n Positive ANA rate decreased 14% Follow-up testing eliminated n n n Payer charges $99, 925 per year Referrals & diagnostic procedures avoided Eliminated >500 manual tests per year
 Blood Culture Contamination Example of Decreased Wastage n Contamination w/ skin flora causes n n n Unnecessary antibiotic administration Additional cultures & other lab tests Increased length of stay Increased hospital cost of ~$5000/case ASM goal is contamination rate <3% n ED usually have higher rates
Blood Culture Contamination Example of Decreased Wastage n Contamination w/ skin flora causes n n n Unnecessary antibiotic administration Additional cultures & other lab tests Increased length of stay Increased hospital cost of ~$5000/case ASM goal is contamination rate <3% n ED usually have higher rates
 Blood Culture Contamination Procedure Change n Chlorhexidine blood culture prep n n One step application Decreased drying time ED trial in August 2002 Hospital-wide in May 2003
Blood Culture Contamination Procedure Change n Chlorhexidine blood culture prep n n One step application Decreased drying time ED trial in August 2002 Hospital-wide in May 2003
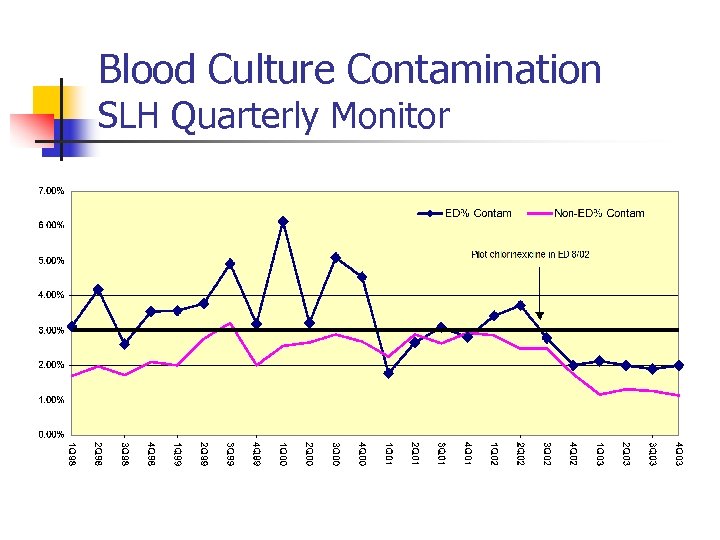 Blood Culture Contamination SLH Quarterly Monitor
Blood Culture Contamination SLH Quarterly Monitor
 Blood Culture Contamination SLH Savings n n n 9740 blood cultures per year Contaminants from 238 to 135 $515, 000 hospital cost savings per year
Blood Culture Contamination SLH Savings n n n 9740 blood cultures per year Contaminants from 238 to 135 $515, 000 hospital cost savings per year
 Specimen in Lab Policy Example of Decreased Wastage n n Worked with Blood Conservation Team to reduce iatrogenic blood loss SIL Policy implemented n n n Stored blood specimens for 2 weeks Publicized in Lab Letter & Nursing publications Avoided redrawing patients for add on tests
Specimen in Lab Policy Example of Decreased Wastage n n Worked with Blood Conservation Team to reduce iatrogenic blood loss SIL Policy implemented n n n Stored blood specimens for 2 weeks Publicized in Lab Letter & Nursing publications Avoided redrawing patients for add on tests
 Specimen in Lab Policy SLH Outcomes n n 11, 244 requests for tests on SIL $51, 726 savings in labor & supplies Avoided 11, 244 venipunctures Conserved 71, 428 m. L of blood n Equivalent to 140 units of RBCs
Specimen in Lab Policy SLH Outcomes n n 11, 244 requests for tests on SIL $51, 726 savings in labor & supplies Avoided 11, 244 venipunctures Conserved 71, 428 m. L of blood n Equivalent to 140 units of RBCs
 CMV PCR Quantitation Example of Decreased Wastage n n Cobas Amplicor CMV QT - Oct 2001 Initially performed on M, W, F schedule n n Not enough specimens to use complete kit Unused reagents had to be discarded n n Wastage cost $5000 per month Flexible schedule introduced Jan 2003 n n Run whenever have 9 specimens Monitored wastage & TAT
CMV PCR Quantitation Example of Decreased Wastage n n Cobas Amplicor CMV QT - Oct 2001 Initially performed on M, W, F schedule n n Not enough specimens to use complete kit Unused reagents had to be discarded n n Wastage cost $5000 per month Flexible schedule introduced Jan 2003 n n Run whenever have 9 specimens Monitored wastage & TAT
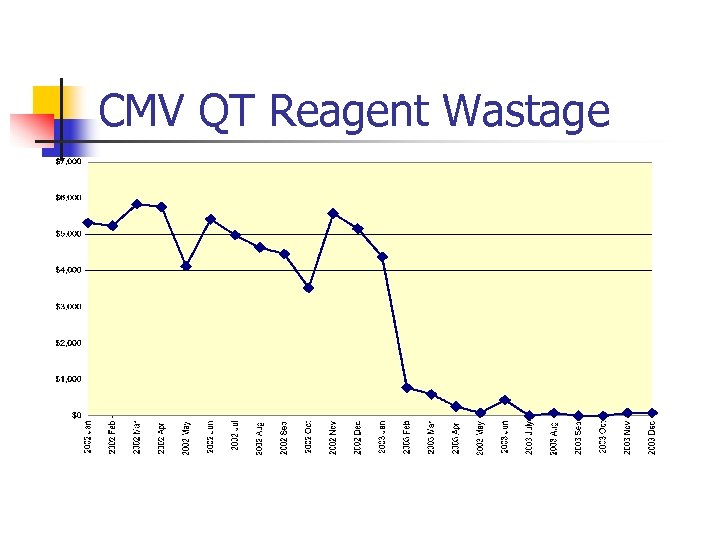 CMV QT Reagent Wastage
CMV QT Reagent Wastage
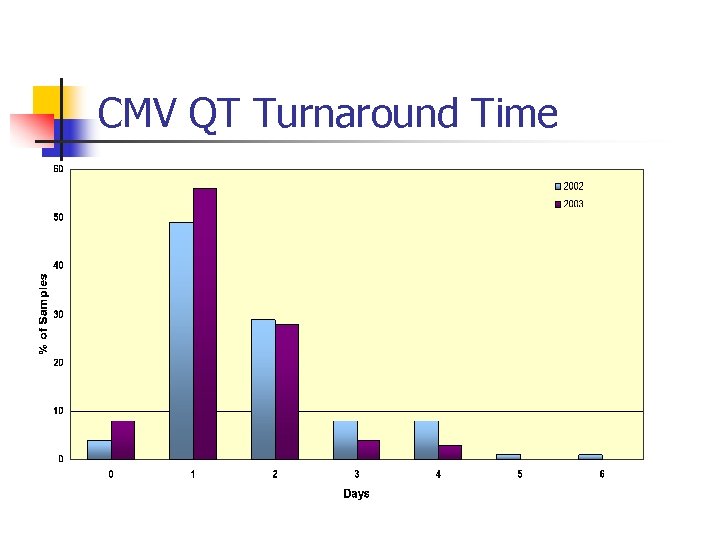 CMV QT Turnaround Time
CMV QT Turnaround Time
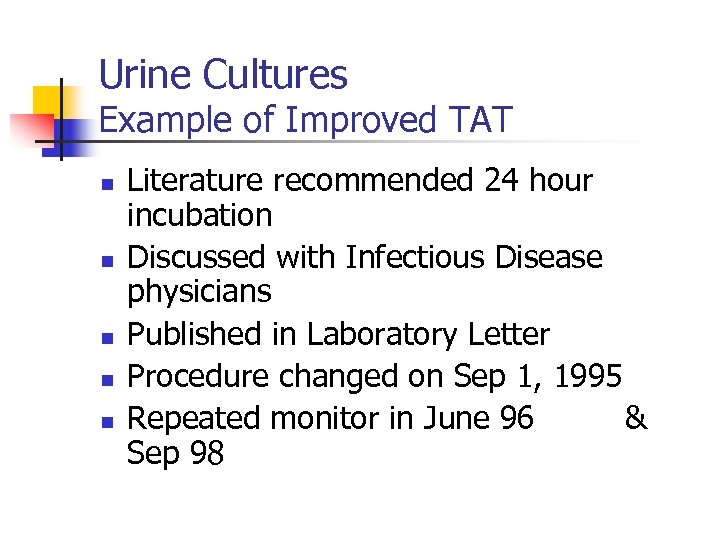 Urine Cultures Example of Improved TAT n n n Literature recommended 24 hour incubation Discussed with Infectious Disease physicians Published in Laboratory Letter Procedure changed on Sep 1, 1995 Repeated monitor in June 96 & Sep 98
Urine Cultures Example of Improved TAT n n n Literature recommended 24 hour incubation Discussed with Infectious Disease physicians Published in Laboratory Letter Procedure changed on Sep 1, 1995 Repeated monitor in June 96 & Sep 98
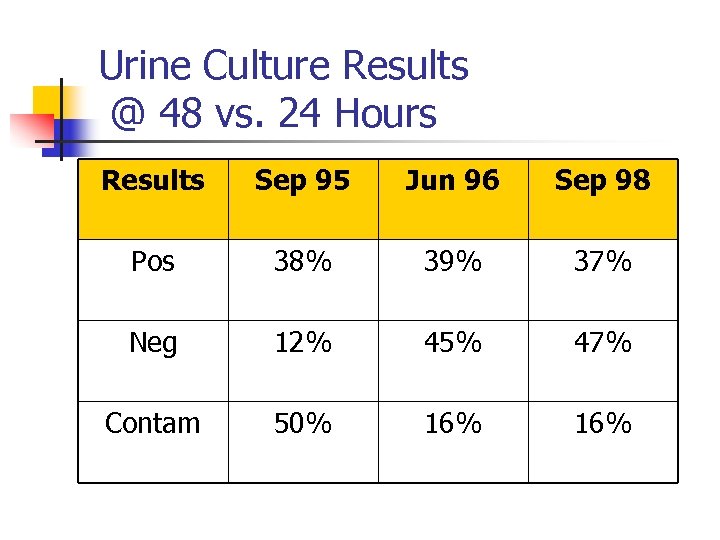 Urine Culture Results @ 48 vs. 24 Hours Results Sep 95 Jun 96 Sep 98 Pos 38% 39% 37% Neg 12% 45% 47% Contam 50% 16%
Urine Culture Results @ 48 vs. 24 Hours Results Sep 95 Jun 96 Sep 98 Pos 38% 39% 37% Neg 12% 45% 47% Contam 50% 16%
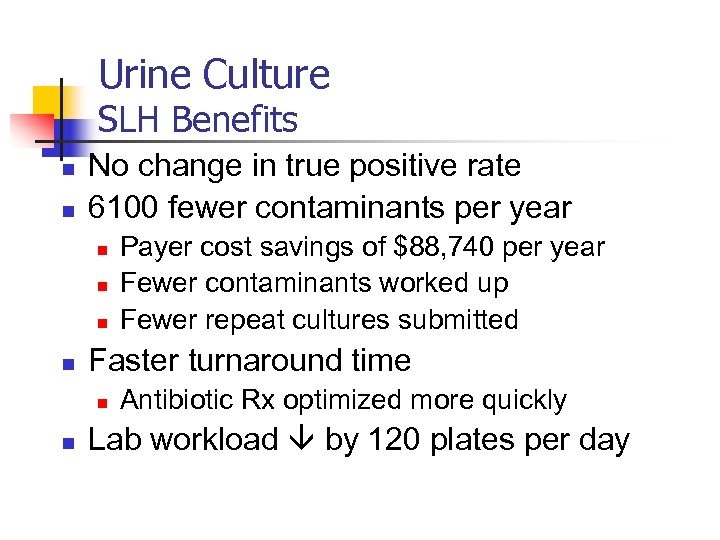 Urine Culture SLH Benefits n n No change in true positive rate 6100 fewer contaminants per year n n Faster turnaround time n n Payer cost savings of $88, 740 per year Fewer contaminants worked up Fewer repeat cultures submitted Antibiotic Rx optimized more quickly Lab workload by 120 plates per day
Urine Culture SLH Benefits n n No change in true positive rate 6100 fewer contaminants per year n n Faster turnaround time n n Payer cost savings of $88, 740 per year Fewer contaminants worked up Fewer repeat cultures submitted Antibiotic Rx optimized more quickly Lab workload by 120 plates per day
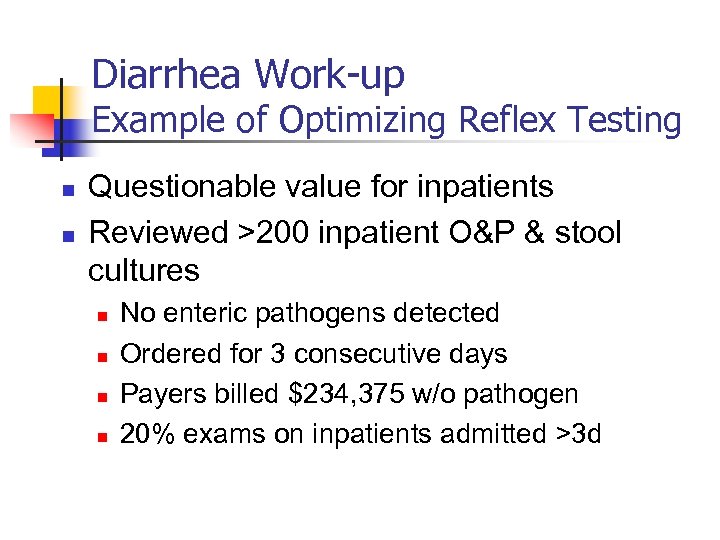 Diarrhea Work-up Example of Optimizing Reflex Testing n n Questionable value for inpatients Reviewed >200 inpatient O&P & stool cultures n n No enteric pathogens detected Ordered for 3 consecutive days Payers billed $234, 375 w/o pathogen 20% exams on inpatients admitted >3 d
Diarrhea Work-up Example of Optimizing Reflex Testing n n Questionable value for inpatients Reviewed >200 inpatient O&P & stool cultures n n No enteric pathogens detected Ordered for 3 consecutive days Payers billed $234, 375 w/o pathogen 20% exams on inpatients admitted >3 d
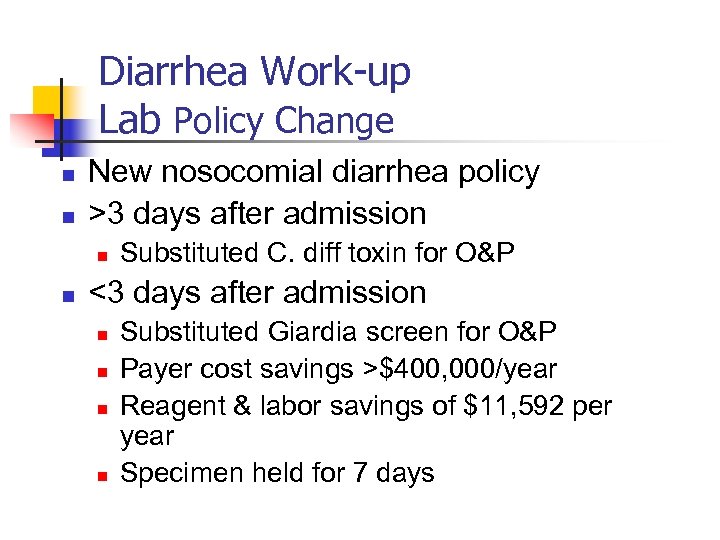 Diarrhea Work-up Lab Policy Change n n New nosocomial diarrhea policy >3 days after admission n n Substituted C. diff toxin for O&P <3 days after admission n n Substituted Giardia screen for O&P Payer cost savings >$400, 000/year Reagent & labor savings of $11, 592 per year Specimen held for 7 days
Diarrhea Work-up Lab Policy Change n n New nosocomial diarrhea policy >3 days after admission n n Substituted C. diff toxin for O&P <3 days after admission n n Substituted Giardia screen for O&P Payer cost savings >$400, 000/year Reagent & labor savings of $11, 592 per year Specimen held for 7 days
 Diarrhea Algorithm
Diarrhea Algorithm
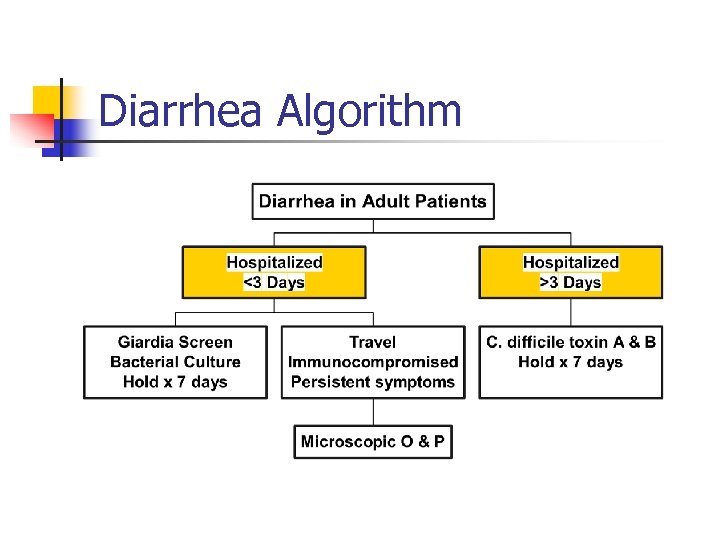
 1995 HCV Algorithm Example of Optimizing Reflex Testing
1995 HCV Algorithm Example of Optimizing Reflex Testing
 1995 HCV Algorithm Inefficiency Identified PCR if RIBA positive or indeterminate n n Most RIBA were Indeterminate 66% had RIBA & PCR performed Shared data with GI & ID physicians Changed algorithm in 1997
1995 HCV Algorithm Inefficiency Identified PCR if RIBA positive or indeterminate n n Most RIBA were Indeterminate 66% had RIBA & PCR performed Shared data with GI & ID physicians Changed algorithm in 1997
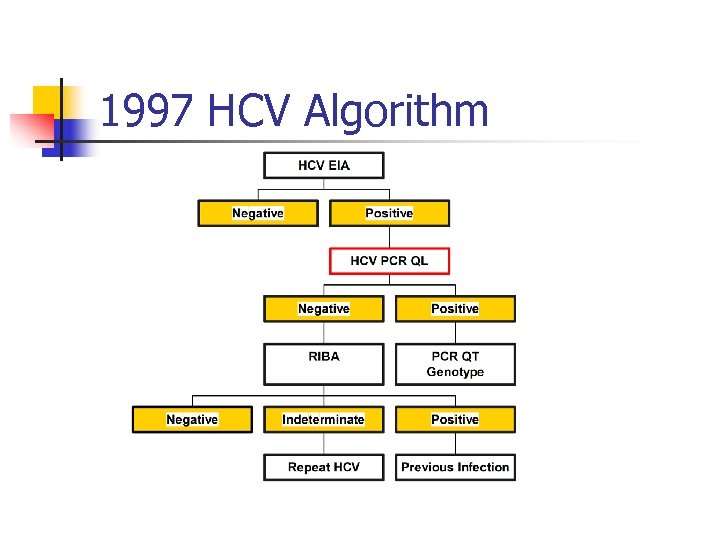 1997 HCV Algorithm
1997 HCV Algorithm
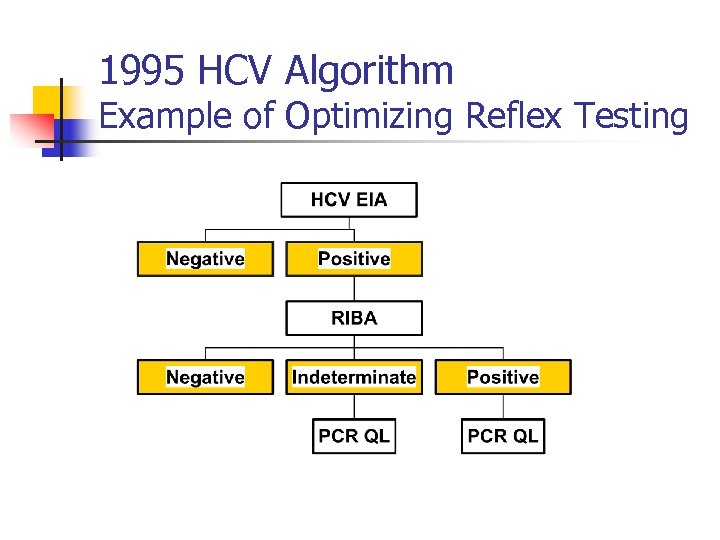
 1997 HCV Algorithm n Financial Impact n n PCR had better sensitivity & specificity n Fewer RIBA performed Based on 1997 test volumes n Payer charges decreased $63, 000 n Laboratory costs decreased $39, 000
1997 HCV Algorithm n Financial Impact n n PCR had better sensitivity & specificity n Fewer RIBA performed Based on 1997 test volumes n Payer charges decreased $63, 000 n Laboratory costs decreased $39, 000
 1997 HCV Algorithm Limitations n PCR QT had limited dynamic range n n n Not as sensitive as PCR QL 25% cases exceeded linearity Taq. Man RT PCR conversion n Much wider dynamic range n n Eliminated need for PCR QL Eliminated repeat testing n $23, 000 per year cost savings
1997 HCV Algorithm Limitations n PCR QT had limited dynamic range n n n Not as sensitive as PCR QL 25% cases exceeded linearity Taq. Man RT PCR conversion n Much wider dynamic range n n Eliminated need for PCR QL Eliminated repeat testing n $23, 000 per year cost savings
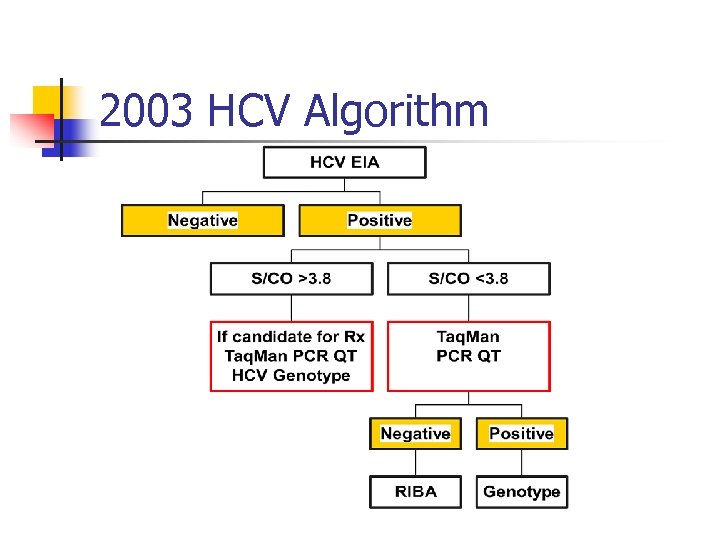 2003 HCV Algorithm
2003 HCV Algorithm
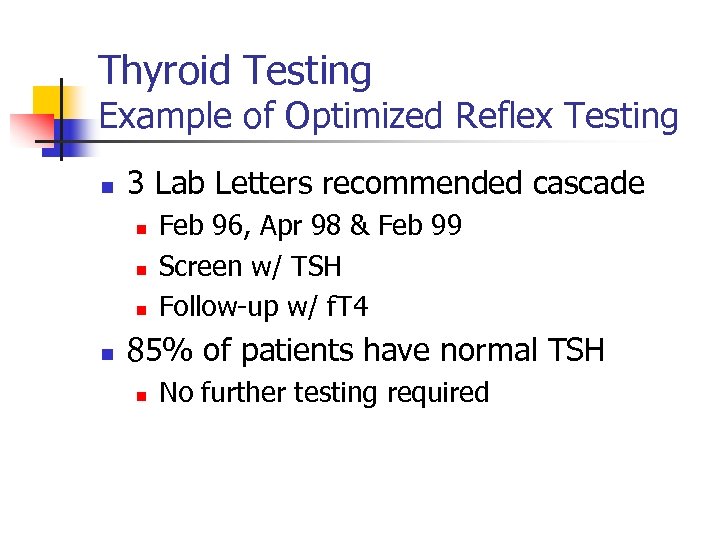 Thyroid Testing Example of Optimized Reflex Testing n 3 Lab Letters recommended cascade n n Feb 96, Apr 98 & Feb 99 Screen w/ TSH Follow-up w/ f. T 4 85% of patients have normal TSH n No further testing required
Thyroid Testing Example of Optimized Reflex Testing n 3 Lab Letters recommended cascade n n Feb 96, Apr 98 & Feb 99 Screen w/ TSH Follow-up w/ f. T 4 85% of patients have normal TSH n No further testing required
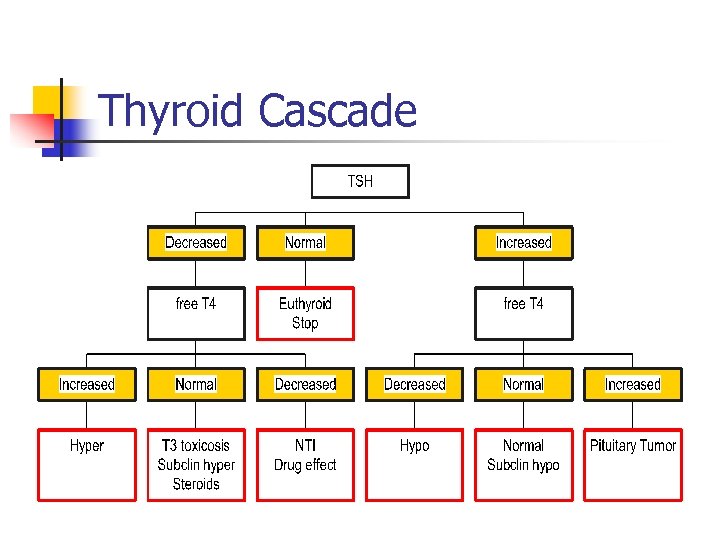 Thyroid Cascade
Thyroid Cascade
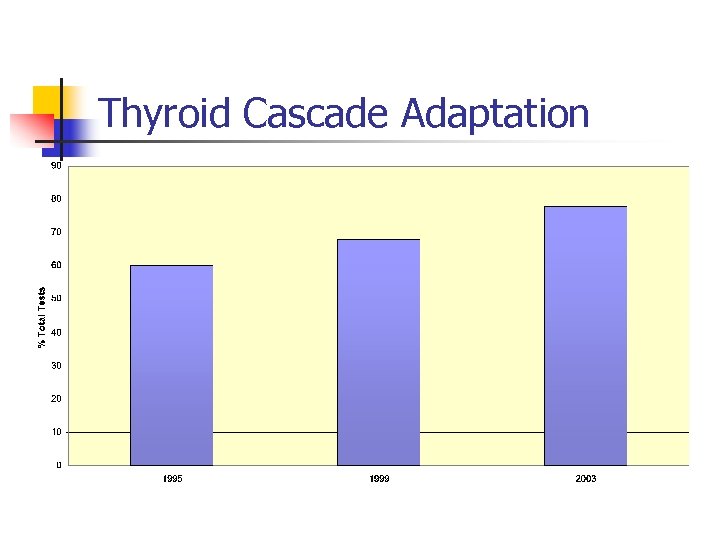 Thyroid Cascade Adaptation
Thyroid Cascade Adaptation
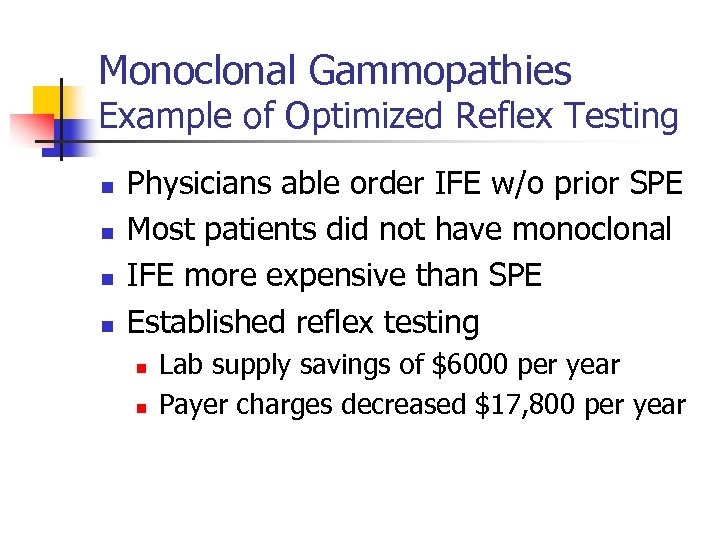 Monoclonal Gammopathies Example of Optimized Reflex Testing n n Physicians able order IFE w/o prior SPE Most patients did not have monoclonal IFE more expensive than SPE Established reflex testing n n Lab supply savings of $6000 per year Payer charges decreased $17, 800 per year
Monoclonal Gammopathies Example of Optimized Reflex Testing n n Physicians able order IFE w/o prior SPE Most patients did not have monoclonal IFE more expensive than SPE Established reflex testing n n Lab supply savings of $6000 per year Payer charges decreased $17, 800 per year
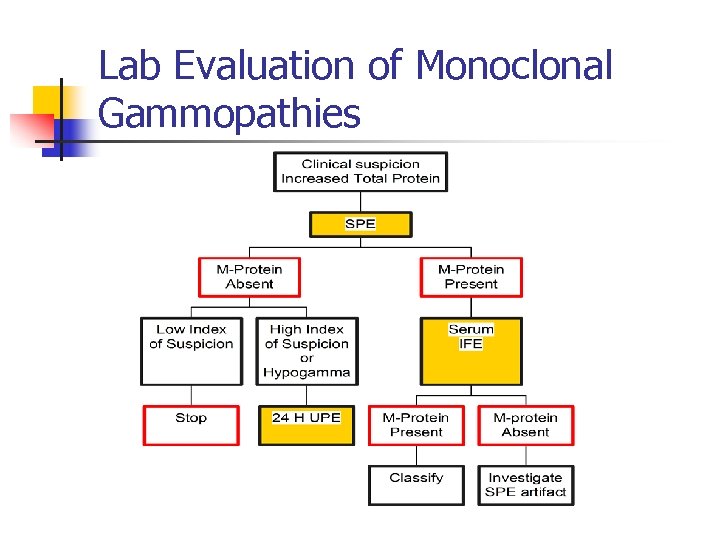 Lab Evaluation of Monoclonal Gammopathies
Lab Evaluation of Monoclonal Gammopathies
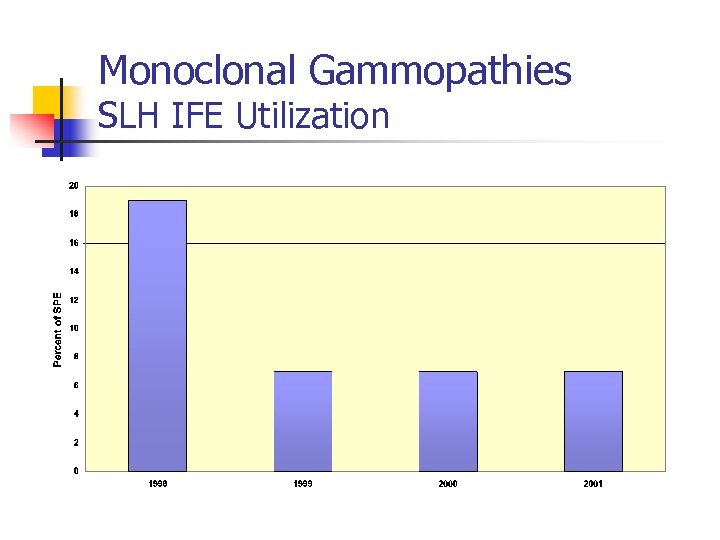 Monoclonal Gammopathies SLH IFE Utilization
Monoclonal Gammopathies SLH IFE Utilization
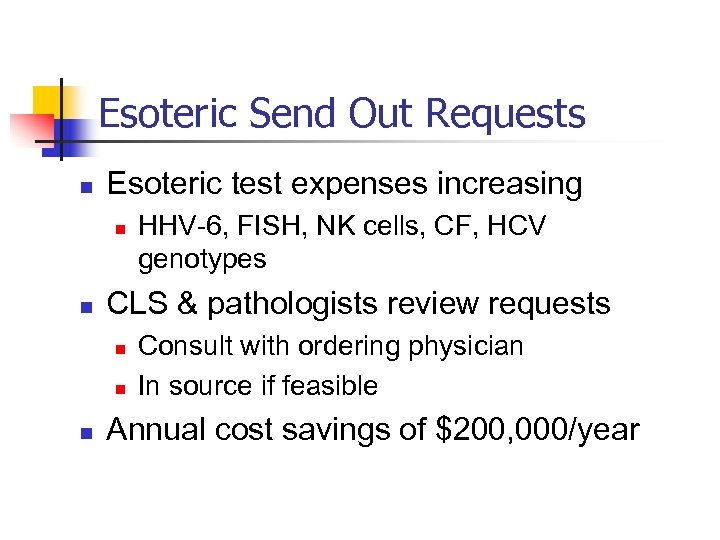 Esoteric Send Out Requests n Esoteric test expenses increasing n n CLS & pathologists review requests n n n HHV-6, FISH, NK cells, CF, HCV genotypes Consult with ordering physician In source if feasible Annual cost savings of $200, 000/year
Esoteric Send Out Requests n Esoteric test expenses increasing n n CLS & pathologists review requests n n n HHV-6, FISH, NK cells, CF, HCV genotypes Consult with ordering physician In source if feasible Annual cost savings of $200, 000/year
 Cystic Fibrosis Example of In-sourcing a Test n ACOG & ACMG recommendation n n March 2001 Offer screening to pregnant couples Sent to reference lab initially Roche CF Gold in November 2002 n $40, 000 cost savings in 2003
Cystic Fibrosis Example of In-sourcing a Test n ACOG & ACMG recommendation n n March 2001 Offer screening to pregnant couples Sent to reference lab initially Roche CF Gold in November 2002 n $40, 000 cost savings in 2003
 HCV Genotyping Example of In-sourcing a Test n n 6 HCV genotypes recognized Genotype determines therapy n n n Type 1 requires 48 months Types 2 & 3 require 24 months Interferon Rx very expensive
HCV Genotyping Example of In-sourcing a Test n n 6 HCV genotypes recognized Genotype determines therapy n n n Type 1 requires 48 months Types 2 & 3 require 24 months Interferon Rx very expensive
 HCV Genotyping SLH Savings n n n Sent to reference lab initially INNO-Li. Pa HCV II implemented in 2001 $55, 670 cost savings in 2002
HCV Genotyping SLH Savings n n n Sent to reference lab initially INNO-Li. Pa HCV II implemented in 2001 $55, 670 cost savings in 2002
 Open Heart Surgery Example of Transfusion Review n n OHS transfused ~one third of components Pathologist analyzed blood usage each year n n n Surgeon specific usage Reviewed with CTS team Evaluated risk factors, meds, practice variations Published transfusion guidelines & risks Presented to medical & house staff
Open Heart Surgery Example of Transfusion Review n n OHS transfused ~one third of components Pathologist analyzed blood usage each year n n n Surgeon specific usage Reviewed with CTS team Evaluated risk factors, meds, practice variations Published transfusion guidelines & risks Presented to medical & house staff
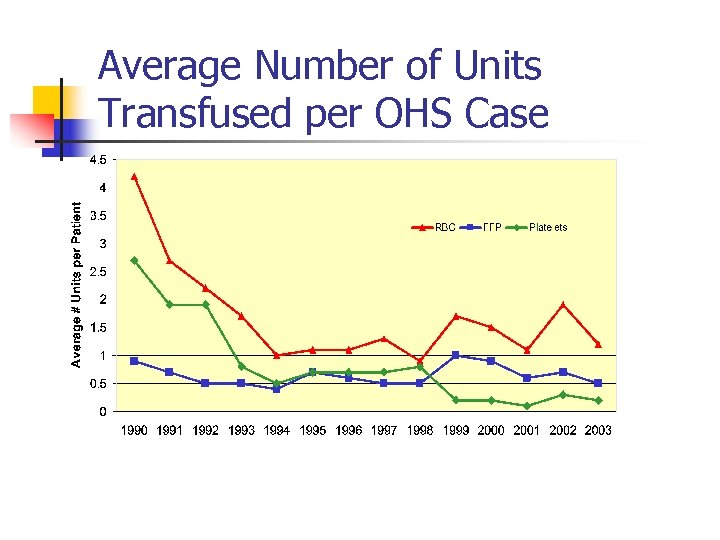 Average Number of Units Transfused per OHS Case
Average Number of Units Transfused per OHS Case
 Benefits of Decreased Transfusion n n 1000 OHS cases performed each year $600, 000 cost savings per year Transfusion reaction risks decreased Blood Bank workload decreased Nursing time for transfusion decreased
Benefits of Decreased Transfusion n n 1000 OHS cases performed each year $600, 000 cost savings per year Transfusion reaction risks decreased Blood Bank workload decreased Nursing time for transfusion decreased
 POC Blood Glucose Testing Patient Identification Errors n Manual Patient ID entry n n 12, 000 tests per month 9. 7% average error rate ~450 unidentified results per month PI project in December 2002 n n Accu-Chek Inform & RALS Plus Barcoded armbands
POC Blood Glucose Testing Patient Identification Errors n Manual Patient ID entry n n 12, 000 tests per month 9. 7% average error rate ~450 unidentified results per month PI project in December 2002 n n Accu-Chek Inform & RALS Plus Barcoded armbands
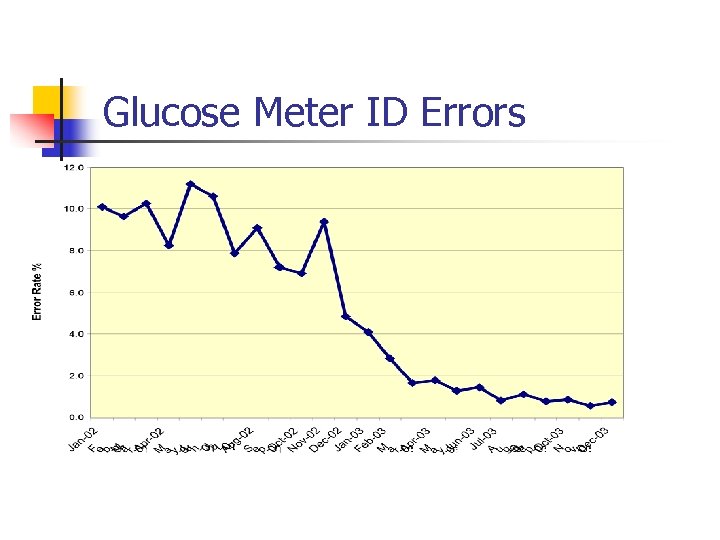 Glucose Meter ID Errors
Glucose Meter ID Errors
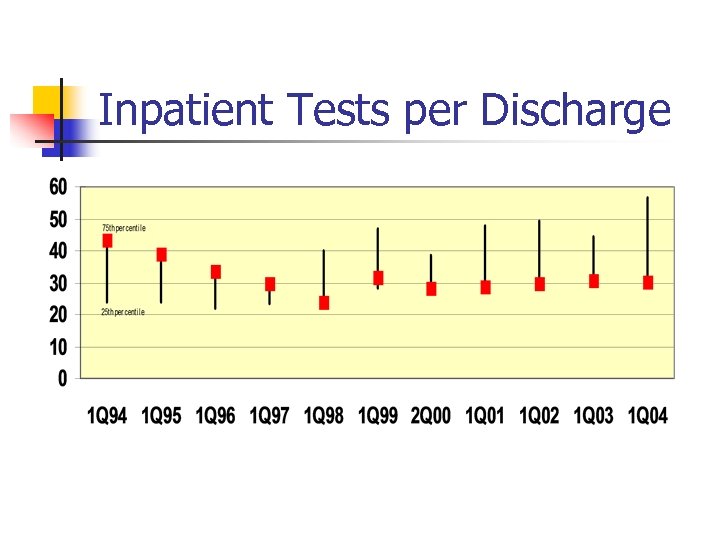 Inpatient Tests per Discharge
Inpatient Tests per Discharge
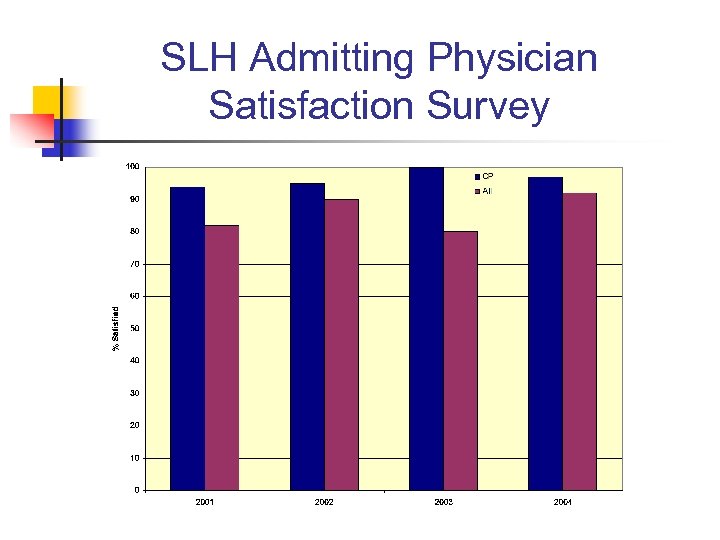 SLH Admitting Physician Satisfaction Survey
SLH Admitting Physician Satisfaction Survey
 Summary of the SLH Approach n n n Target problems that are solvable Collect & analyze data from your own lab Present the data to influential physicians n n Communicate changes to medical staff n n These experts are the lab’s best advocates Lab newsletter is a very effective educational tool Monitor impact of changes
Summary of the SLH Approach n n n Target problems that are solvable Collect & analyze data from your own lab Present the data to influential physicians n n Communicate changes to medical staff n n These experts are the lab’s best advocates Lab newsletter is a very effective educational tool Monitor impact of changes


