133e9fcf16fd8182397dc5c3abd77f20.ppt
- Количество слайдов: 48
How to increase the number of PD patients Olof Heimbürger, MD, Ph. D Ass Professor, Dept of Clinical Science, Intervention and Technology, Karolinska Institutet Senior Consultant, Dept of Renal Medicine, Karolinska University Hospital
Outline • Interventions to increase PD use • Unplanned start • Decision aids – Planned start – Unplanned start • How should the information be given • Shared decision making and patient empowerment • Why do our patients do not make the ”right” decision
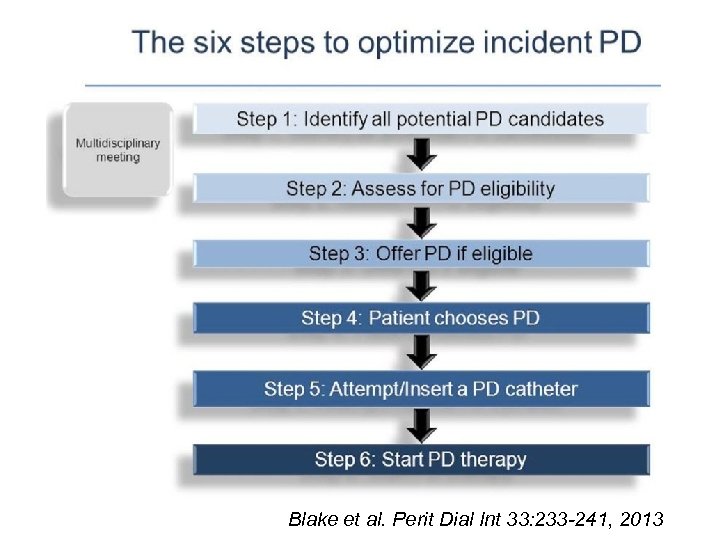
Blake et al. Perit Dial Int 33: 233 -241, 2013
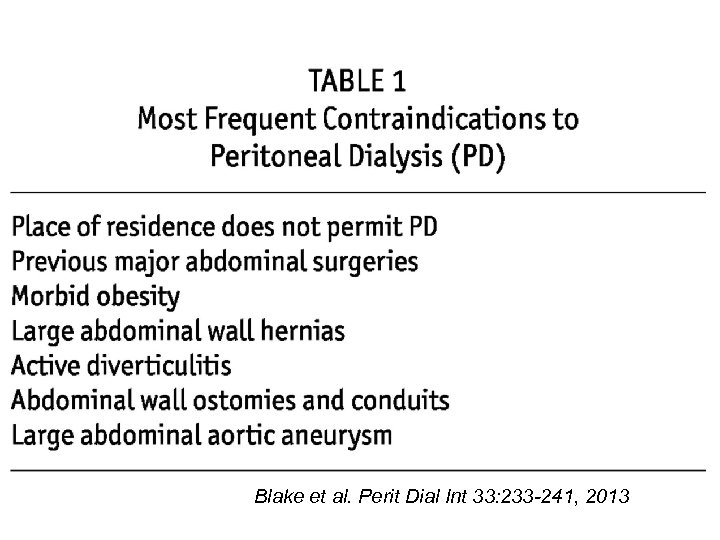
Blake et al. Perit Dial Int 33: 233 -241, 2013
• Systematic review • Screened 4063 papers, 339 full-text articles assessed • 52 included in the qualitative synthesis Mann BS et al. Perit Dial Int 37: 159 -164, 2017
Interventions to increase PD utlization • • • PD-first policy Unplanned start of PD Pre-dialysis education Assistance with delivery of PD Nephrologist placing PD-catheters Mann BS et al. Perit Dial Int 37: 159 -164, 2017
Interventions to increase PD utlization • • • PD-first policy Unplanned start of PD Pre-dialysis education Assistance with delivery of PD Nephrologist placing PD-catheters Mann BS et al. Perit Dial Int 37: 159 -164, 2017
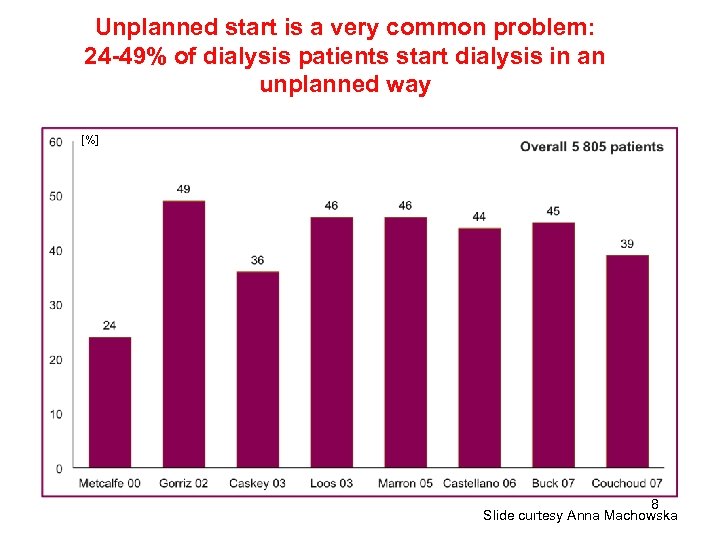
Unplanned start is a very common problem: 24 -49% of dialysis patients start dialysis in an unplanned way [%] 8 Slide curtesy Anna Machowska
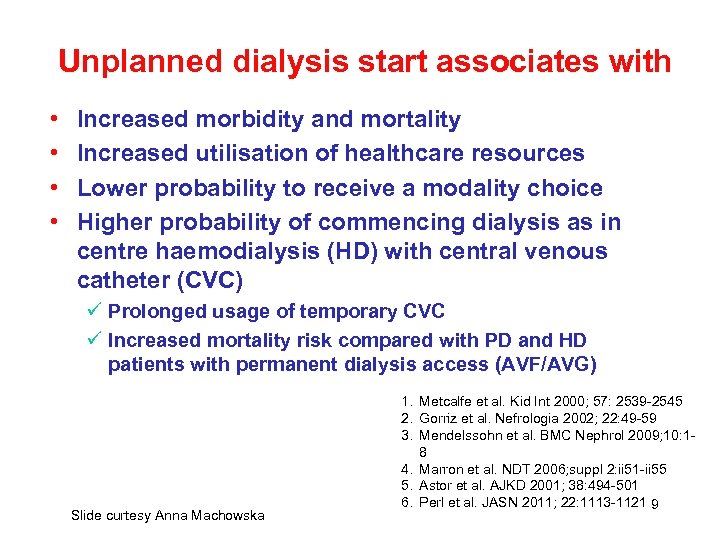
Unplanned dialysis start associates with • • Increased morbidity and mortality Increased utilisation of healthcare resources Lower probability to receive a modality choice Higher probability of commencing dialysis as in centre haemodialysis (HD) with central venous catheter (CVC) ü Prolonged usage of temporary CVC ü Increased mortality risk compared with PD and HD patients with permanent dialysis access (AVF/AVG) Slide curtesy Anna Machowska 1. Metcalfe et al. Kid Int 2000; 57: 2539 -2545 2. Gorriz et al. Nefrologia 2002; 22: 49 -59 3. Mendelssohn et al. BMC Nephrol 2009; 10: 18 4. Marron et al. NDT 2006; suppl 2: ii 51 -ii 55 5. Astor et al. AJKD 2001; 38: 494 -501 6. Perl et al. JASN 2011; 22: 1113 -1121 9
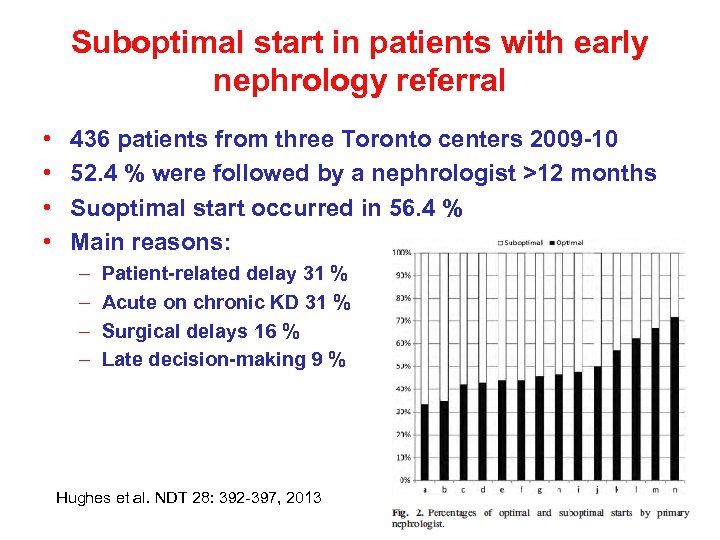
Suboptimal start in patients with early nephrology referral • • 436 patients from three Toronto centers 2009 -10 52. 4 % were followed by a nephrologist >12 months Suoptimal start occurred in 56. 4 % Main reasons: – – Patient-related delay 31 % Acute on chronic KD 31 % Surgical delays 16 % Late decision-making 9 % Hughes et al. NDT 28: 392 -397, 2013
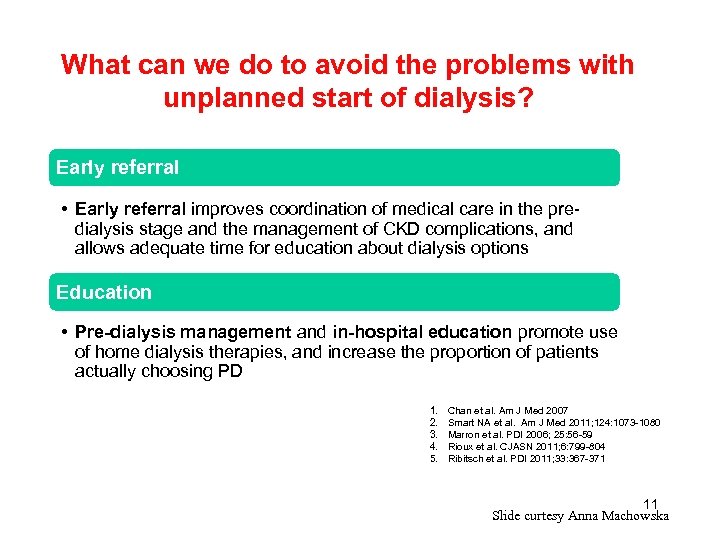
What can we do to avoid the problems with unplanned start of dialysis? Early referral • Early referral improves coordination of medical care in the predialysis stage and the management of CKD complications, and allows adequate time for education about dialysis options Education • Pre-dialysis management and in-hospital education promote use of home dialysis therapies, and increase the proportion of patients actually choosing PD 1. 2. 3. 4. 5. Chan et al. Am J Med 2007 Smart NA et al. Am J Med 2011; 124: 1073 -1080 Marron et al. PDI 2006; 25: 56 -59 Rioux et al. CJASN 2011; 6: 799 -804 Ribitsch et al. PDI 2011; 33: 367 -371 11 Slide curtesy Anna Machowska
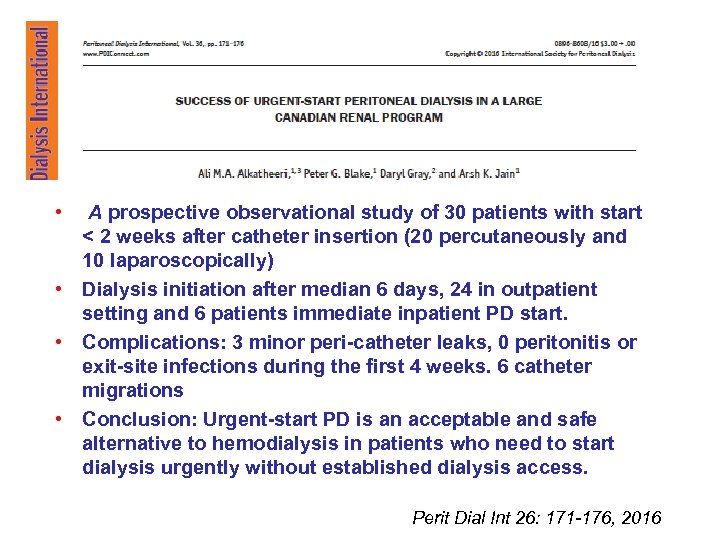
• A prospective observational study of 30 patients with start < 2 weeks after catheter insertion (20 percutaneously and 10 laparoscopically) • Dialysis initiation after median 6 days, 24 in outpatient setting and 6 patients immediate inpatient PD start. • Complications: 3 minor peri-catheter leaks, 0 peritonitis or exit-site infections during the first 4 weeks. 6 catheter migrations • Conclusion: Urgent-start PD is an acceptable and safe alternative to hemodialysis in patients who need to start dialysis urgently without established dialysis access. Perit Dial Int 26: 171 -176, 2016
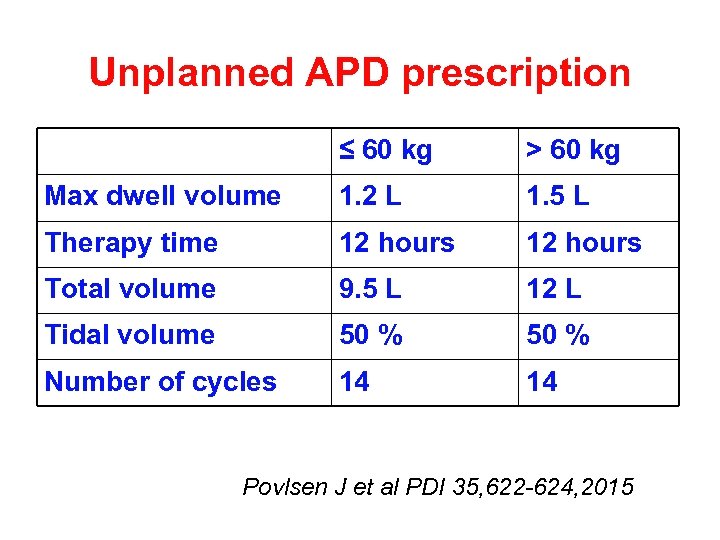
Unplanned APD prescription ≤ 60 kg > 60 kg Max dwell volume 1. 2 L 1. 5 L Therapy time 12 hours Total volume 9. 5 L 12 L Tidal volume 50 % Number of cycles 14 14 Povlsen J et al PDI 35, 622 -624, 2015
Decision aids Winterbottom et al PDI 36: 374 -381, 2016
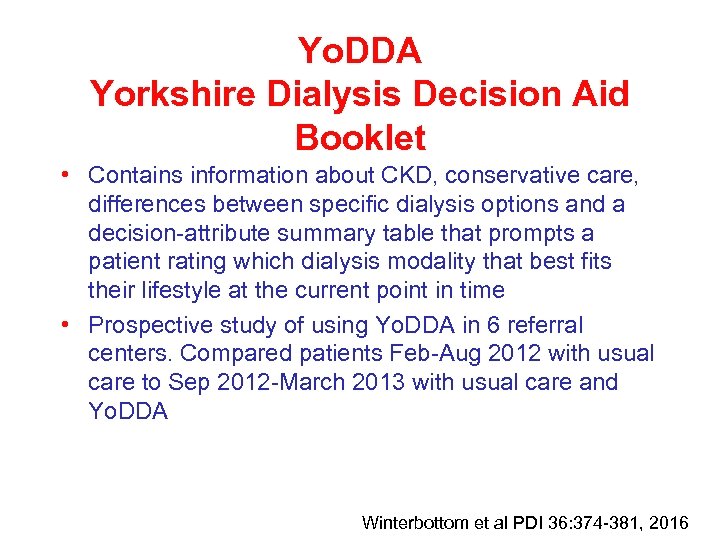
Yo. DDA Yorkshire Dialysis Decision Aid Booklet • Contains information about CKD, conservative care, differences between specific dialysis options and a decision-attribute summary table that prompts a patient rating which dialysis modality that best fits their lifestyle at the current point in time • Prospective study of using Yo. DDA in 6 referral centers. Compared patients Feb-Aug 2012 with usual care to Sep 2012 -March 2013 with usual care and Yo. DDA Winterbottom et al PDI 36: 374 -381, 2016
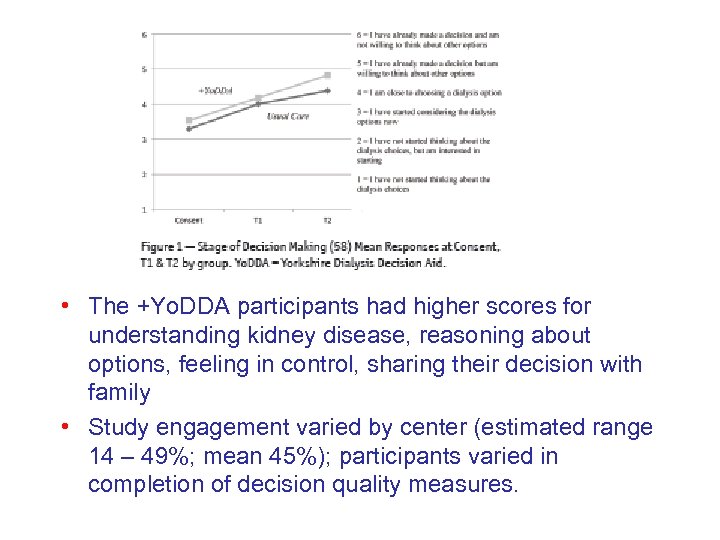
• The +Yo. DDA participants had higher scores for understanding kidney disease, reasoning about options, feeling in control, sharing their decision with family • Study engagement varied by center (estimated range 14 – 49%; mean 45%); participants varied in completion of decision quality measures.
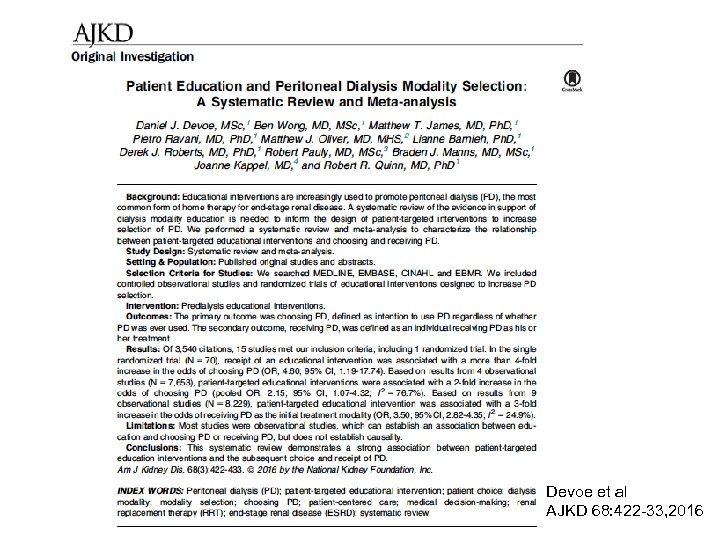
Devoe et al AJKD 68: 422 -33, 2016
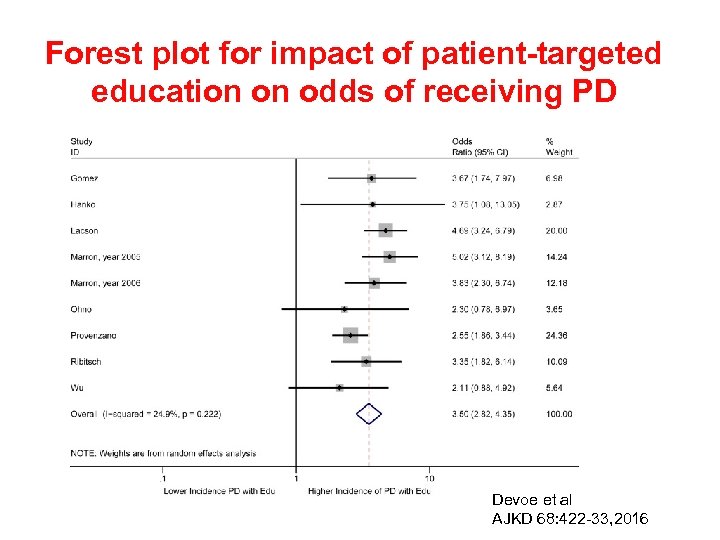
Forest plot for impact of patient-targeted education on odds of receiving PD Devoe et al AJKD 68: 422 -33, 2016

• A non-interventional, prospective, multi-center, observational study • 270 UPS patients from 26 centers in 6 European countries (Austria, Germany, Denmark, France, United Kingdom and Sweden) • Presented acutely, or were being followed by nephrologists but required urgent dialysis commencement by an acutely placed CVC or PD catheter Machowska A et al. BMC Nephrology (2017) 18: 18
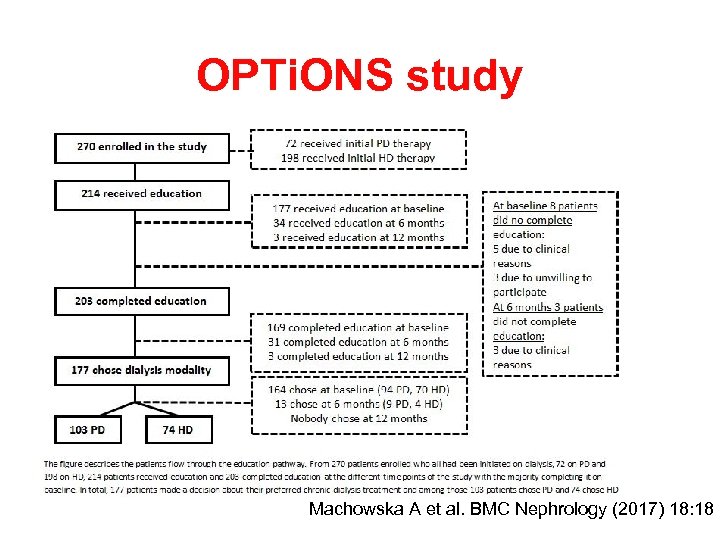
OPTi. ONS study Machowska A et al. BMC Nephrology (2017) 18: 18
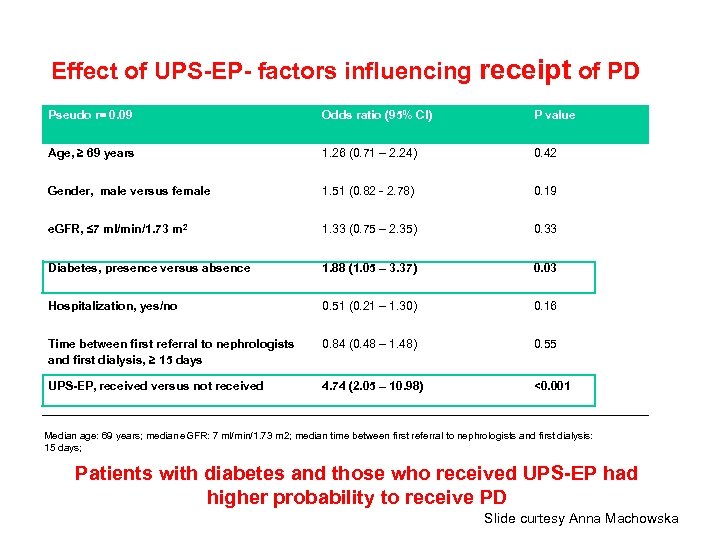
Effect of UPS-EP- factors influencing receipt of PD Pseudo r= 0. 09 Odds ratio (95% CI) P value Age, ≥ 69 years 1. 26 (0. 71 – 2. 24) 0. 42 Gender, male versus female 1. 51 (0. 82 - 2. 78) 0. 19 e. GFR, ≤ 7 ml/min/1. 73 m 2 1. 33 (0. 75 – 2. 35) 0. 33 Diabetes, presence versus absence 1. 88 (1. 05 – 3. 37) 0. 03 Hospitalization, yes/no 0. 51 (0. 21 – 1. 30) 0. 16 Time between first referral to nephrologists and first dialysis, ≥ 15 days 0. 84 (0. 48 – 1. 48) 0. 55 UPS-EP, received versus not received 4. 74 (2. 05 – 10. 98) <0. 001 Median age: 69 years; median e. GFR: 7 ml/min/1. 73 m 2; median time between first referral to nephrologists and first dialysis: 15 days; Patients with diabetes and those who received UPS-EP had higher probability to receive PD Slide curtesy Anna Machowska
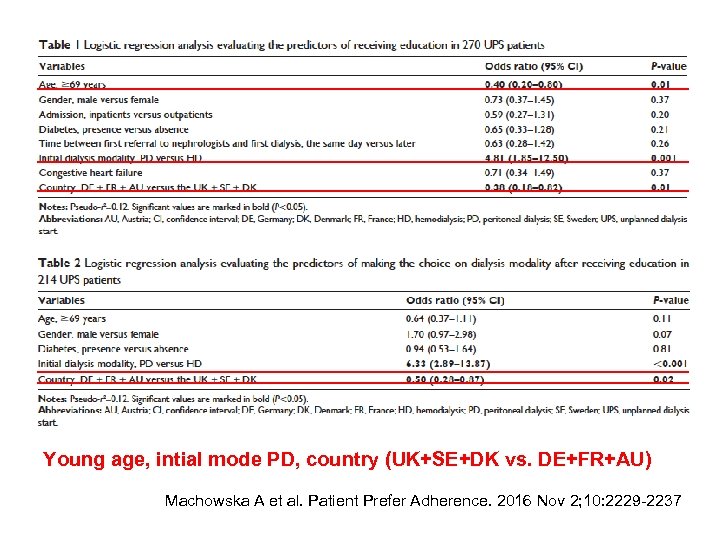
Young age, intial mode PD, country (UK+SE+DK vs. DE+FR+AU) Machowska A et al. Patient Prefer Adherence. 2016 Nov 2; 10: 2229 -2237
Lopez-Vargas et al AJKD 68: 353 -70, 2016
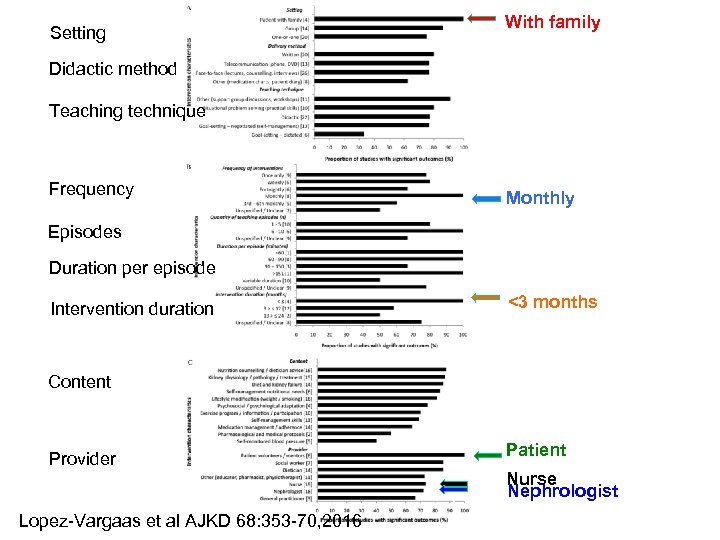
With family Setting Didactic method Teaching technique Frequency Monthly Episodes Duration per episode <3 months Intervention duration Content Provider Lopez-Vargaas et al AJKD 68: 353 -70, 2016 o f o Patient f Nurse Nephrologist
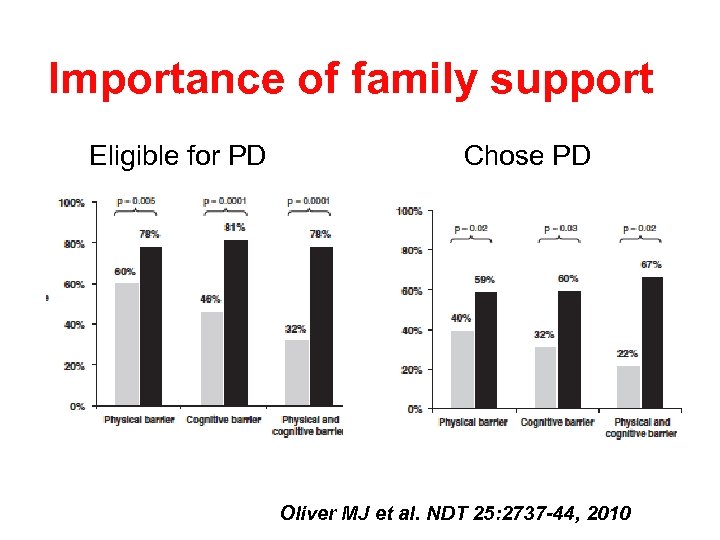
Importance of family support Eligible for PD Chose PD Oliver MJ et al. NDT 25: 2737 -44, 2010
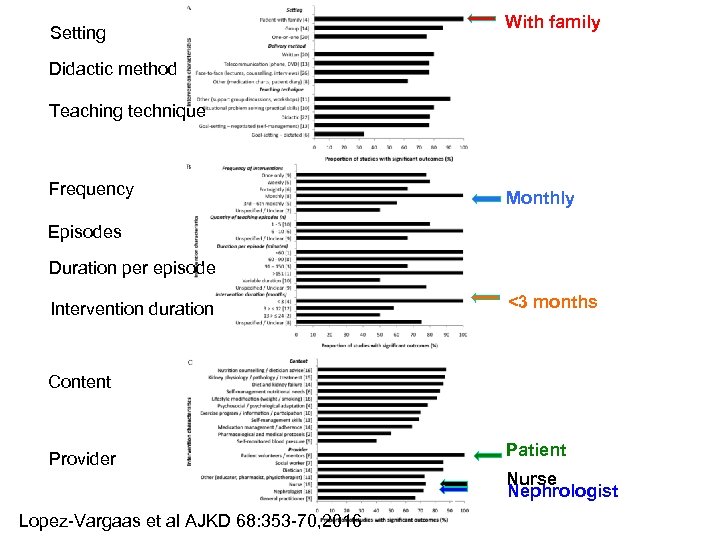
With family Setting Didactic method Teaching technique Frequency Monthly Episodes Duration per episode <3 months Intervention duration Content Provider Lopez-Vargaas et al AJKD 68: 353 -70, 2016 o f o Patient f Nurse Nephrologist
• 1694 participants viewed online information about HD and CCPD • Using actors, treatment information was varied by presenter (Doctor, Patient), order of presenter (Patient first, Doctor first) and mode of delivery (written, video), inclusion of a decision table and sex of the ‘patient’ and ‘Doctor’ • Participants were more likely to choose the dialysis modality presented by the patient rather than that presented by the doctor • There was no effect for mode of delivery (video versus written) or inclusion of a decision table • The authors recommend caution in using patients stories Winterbottom et al. NDT 27: 325 -31, 2012
• 1694 participants viewed online information about HD and CCPD • Using actors, treatment information was varied by presenter (Doctor, Patient), order of presenter (Patient first, Doctor first) and mode of delivery (written, video), inclusion of a decision table and sex of the ‘patient’ and ‘Doctor’ • Participants were more likely to choose the dialysis modality presented by the patient rather than that presented by the doctor • There was no effect for mode of delivery (video versus written) or inclusion of a decision table • The authors recommend caution in using patients stories Winterbottom et al. NDT 27: 325 -31, 2012
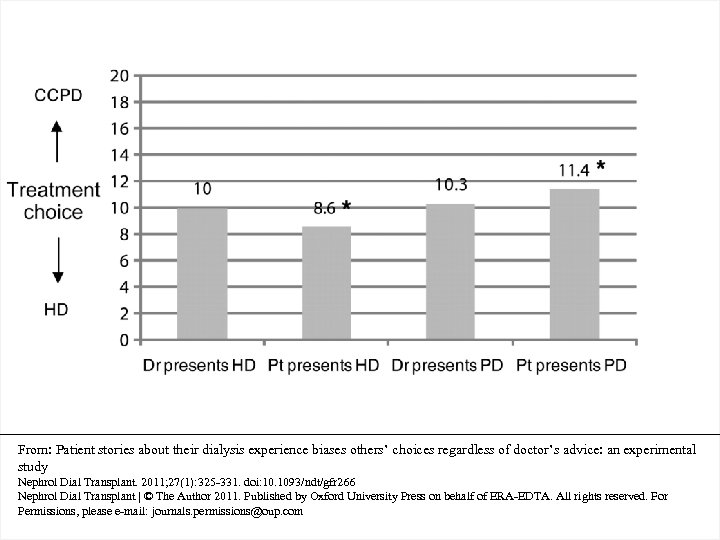
From: Patient stories about their dialysis experience biases others’ choices regardless of doctor’s advice: an experimental study Nephrol Dial Transplant. 2011; 27(1): 325 -331. doi: 10. 1093/ndt/gfr 266 Nephrol Dial Transplant | © The Author 2011. Published by Oxford University Press on behalf of ERA-EDTA. All rights reserved. For Permissions, please e-mail: journals. permissions@oup. com
• • • 535 prevalent ESRD patients and 30 new patients Higher decision making scores with lower age, lower comorbidity index score, higher executive brain function, belonging in the self-caring cohort and being unemployed In the prospectively studied cohort of predialysis patients: no change in decision-making preference scores after dialysis start CONCLUSION: ESRD patients prefer to receive information, but this does not always imply active involvement in decision-making By understanding modifiable and non-modifiable factors which affect patient preferences for involvement in healthcare decision-making, health professionals may acknowledge the need to accommodate individual patient preferences to the extent determined by the individual patient factors.
• • • 535 prevalent ESRD patients and 30 new patients Higher decision making scores with lower age, lower comorbidity index score, higher executive brain function, belonging in the self-caring cohort and being unemployed In the prospectively studied cohort of predialysis patients: no change in decision-making preference scores after dialysis start CONCLUSION: ESRD patients prefer to receive information, but this does not always imply active involvement in decision-making By understanding modifiable and non-modifiable factors which affect patient preferences for involvement in healthcare decision-making, health professionals may acknowledge the need to accommodate individual patient preferences to the extent determined by the individual patient factors.
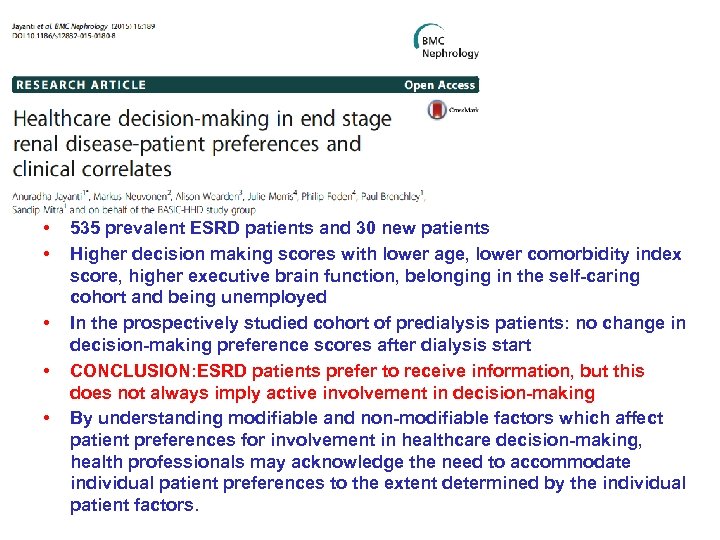
Muthalagapappan S et al. NDT 28: 2717 -22, 2013
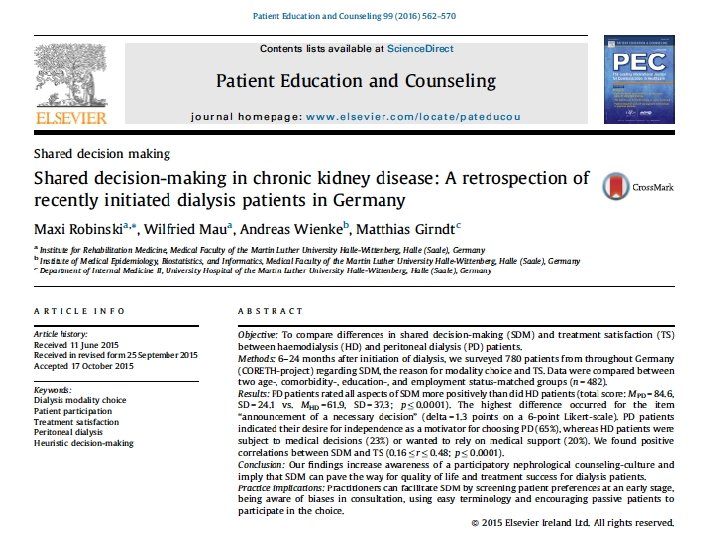
Robinski et al. Patient Educ Couns 99: 56270, 2016
• PD patients indicated their desire for independence as a motivator for choosing PD (65%), whereas HD patients were subject to medical decisions (23%) or wanted to rely on medical support (20%). • PD patients rated all aspects of shared decisionmaking more positively than HD patients. The authors found a positive correlation between shared decision-making and treatment satisfaction. Robinski et al. Patient Educ Couns 99: 562 -70, 2016
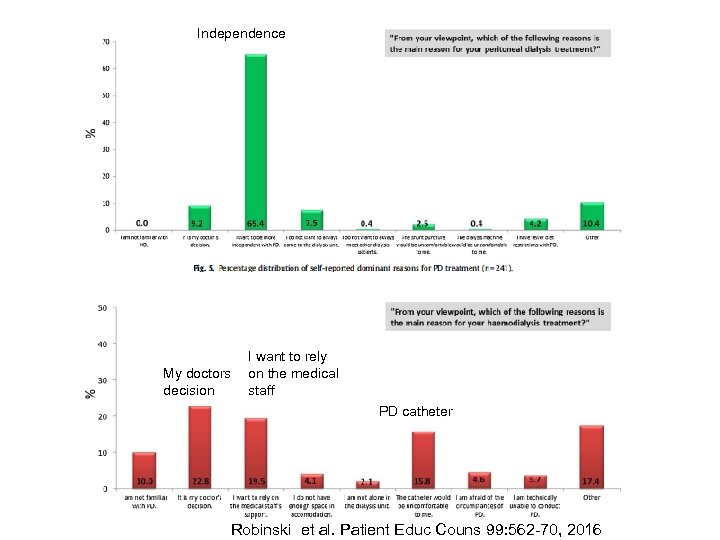
Independence My doctors decision I want to rely on the medical staff PD catheter Robinski et al. Patient Educ Couns 99: 562 -70, 2016
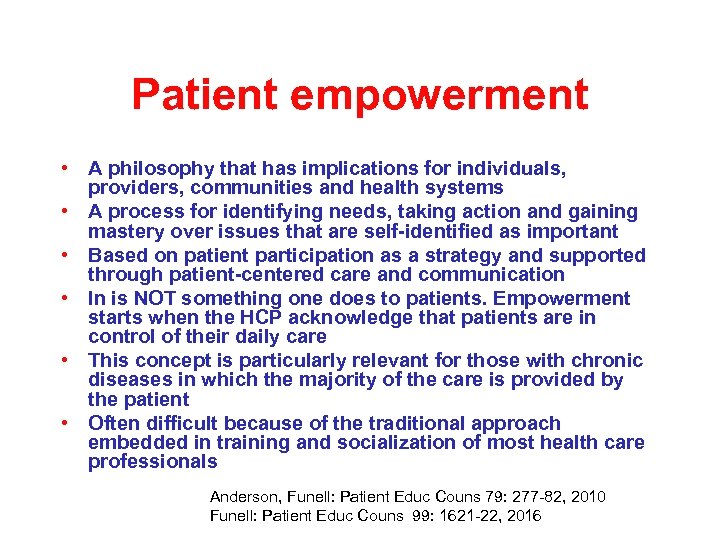
Patient empowerment • A philosophy that has implications for individuals, providers, communities and health systems • A process for identifying needs, taking action and gaining mastery over issues that are self-identified as important • Based on patient participation as a strategy and supported through patient-centered care and communication • In is NOT something one does to patients. Empowerment starts when the HCP acknowledge that patients are in control of their daily care • This concept is particularly relevant for those with chronic diseases in which the majority of the care is provided by the patient • Often difficult because of the traditional approach embedded in training and socialization of most health care professionals Anderson, Funell: Patient Educ Couns 79: 277 -82, 2010 Funell: Patient Educ Couns 99: 1621 -22, 2016
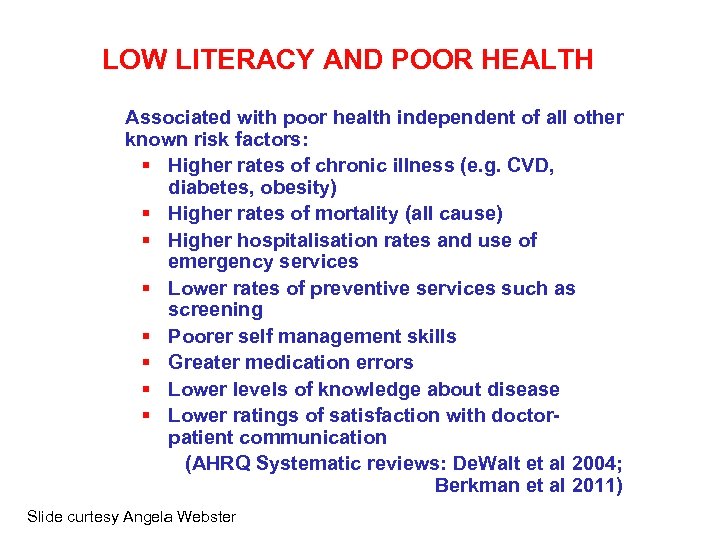
Why are our patients not making the right decision? • Poor information • Poor understanding – Cognitive function – Health literacy • Lack of trust – Patient doctor relationship – Poor continuity – Previous biased information • Fear of change • Other values, the decision may be right for the patients
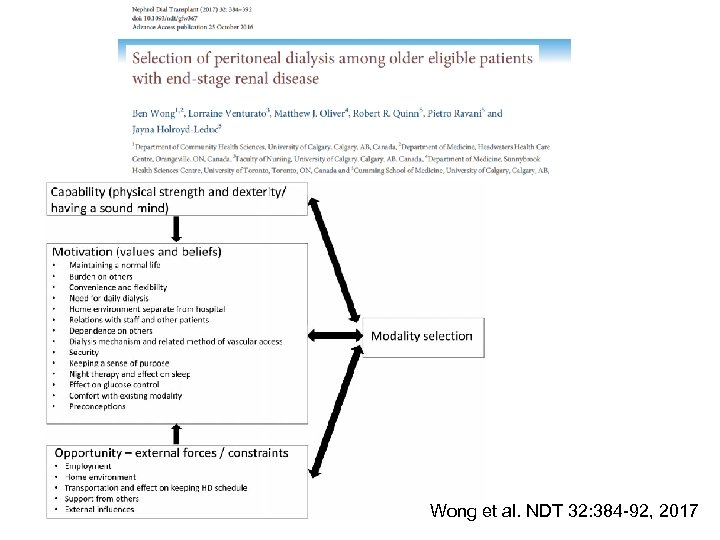
Wong et al. NDT 32: 384 -92, 2017
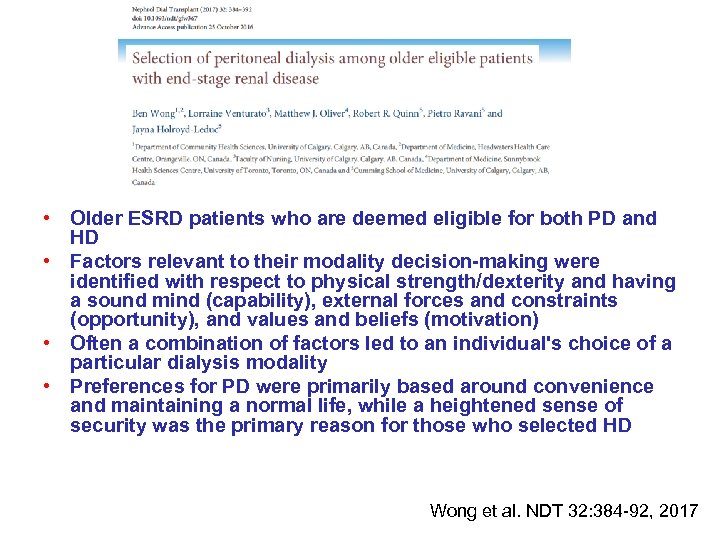
• Older ESRD patients who are deemed eligible for both PD and HD • Factors relevant to their modality decision-making were identified with respect to physical strength/dexterity and having a sound mind (capability), external forces and constraints (opportunity), and values and beliefs (motivation) • Often a combination of factors led to an individual's choice of a particular dialysis modality • Preferences for PD were primarily based around convenience and maintaining a normal life, while a heightened sense of security was the primary reason for those who selected HD Wong et al. NDT 32: 384 -92, 2017
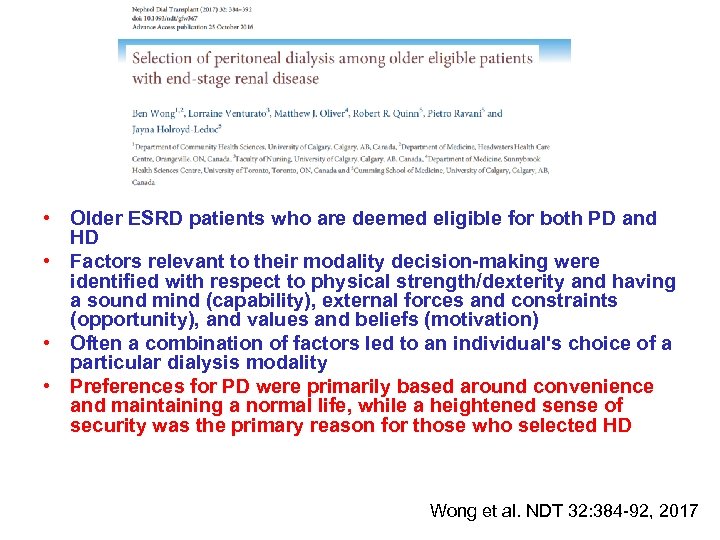
• Older ESRD patients who are deemed eligible for both PD and HD • Factors relevant to their modality decision-making were identified with respect to physical strength/dexterity and having a sound mind (capability), external forces and constraints (opportunity), and values and beliefs (motivation) • Often a combination of factors led to an individual's choice of a particular dialysis modality • Preferences for PD were primarily based around convenience and maintaining a normal life, while a heightened sense of security was the primary reason for those who selected HD Wong et al. NDT 32: 384 -92, 2017
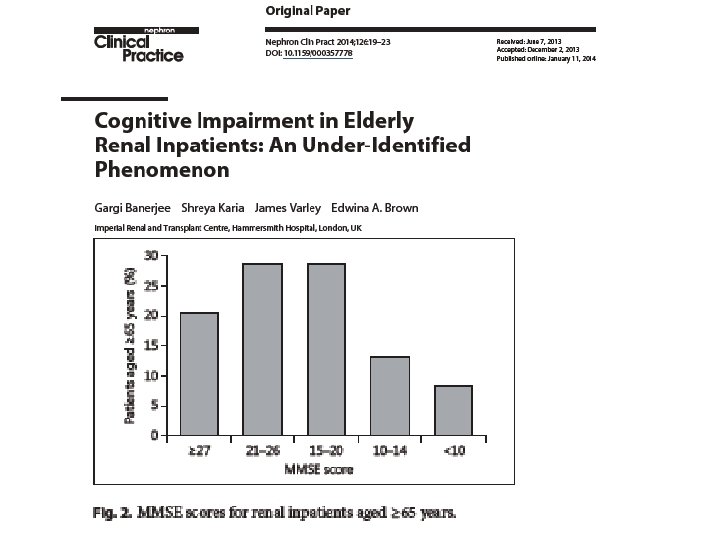
What is health literacy? Framework: Nutbeam’s Multilevel model of Health Literacy 2008 Critical HL Communicative/ interactive HL Functional HL Ability to analyse and act on information Advanced cognitive and social skills Reading, writing, numeracy, oral skills Slide curtesy Angela Webster
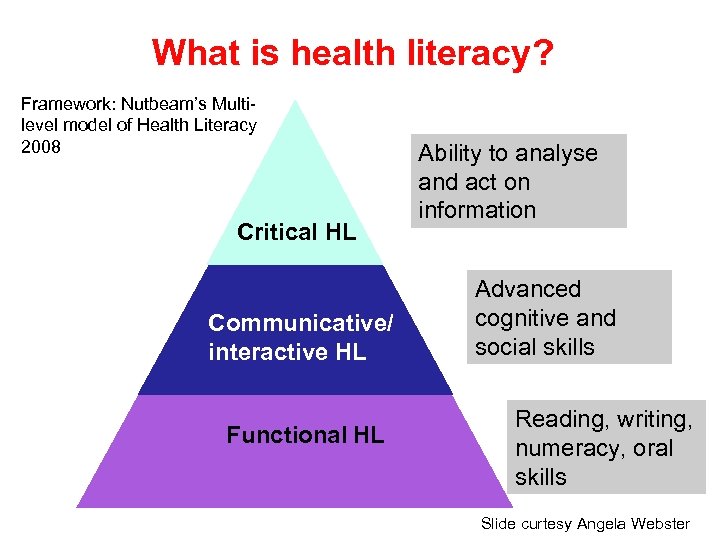
Functional literacy – the evidence Literacy and health literacy must be considered when engaging patients Trouble understandi ng bus timetable Slide curtesy Angela Webster Cannot understand weather map or summarise text Trouble interpreting pie chart, or extracting information from pamphlet. Minimum level for coping
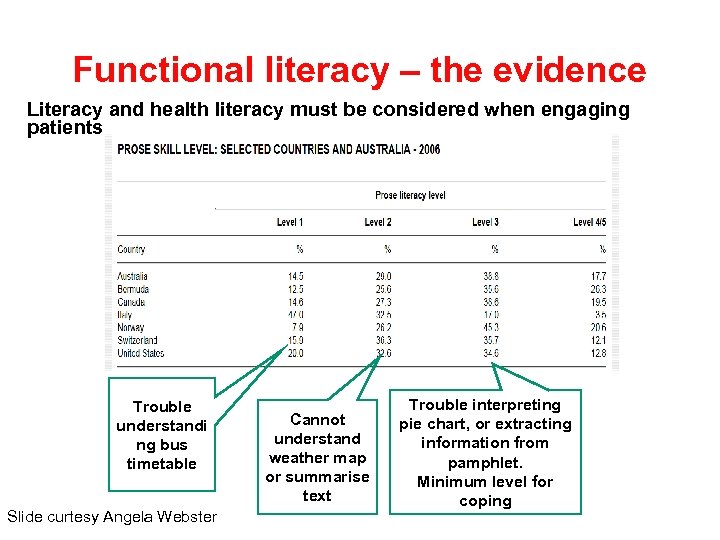
LOW LITERACY AND POOR HEALTH Associated with poor health independent of all other known risk factors: § Higher rates of chronic illness (e. g. CVD, diabetes, obesity) § Higher rates of mortality (all cause) § Higher hospitalisation rates and use of emergency services § Lower rates of preventive services such as screening § Poorer self management skills § Greater medication errors § Lower levels of knowledge about disease § Lower ratings of satisfaction with doctorpatient communication (AHRQ Systematic reviews: De. Walt et al 2004; Berkman et al 2011) Slide curtesy Angela Webster
What about health literacy for people with CKD? Prevalence of limited health literacy 21 - 25 % Lower likelihood of referral for transplant Higher mortality Slide curtesy Angela Webster
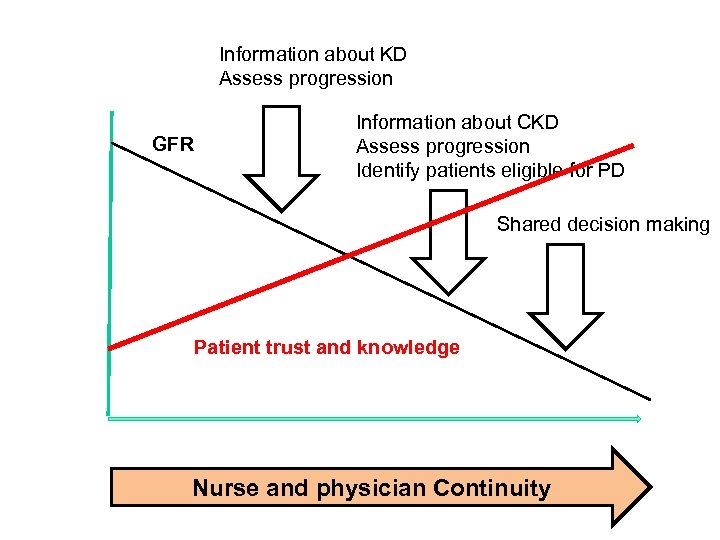
Information about KD Assess progression GFR Information about CKD Assess progression Identify patients eligible for PD Shared decision making Patient trust and knowledge Nurse and physician Continuity
Summary • Indentify all patients eligible for PD • Good logistics for catheter incersion are crucial • Education should be individualized, repeated and often together with family • Patient to patient involvement in education is good but some caution is needed • Decision aids are very usefull but consider health literacy • We need to listen and trust our patients and aim at shared decision making • We need to accept patients choices may be different form ours
133e9fcf16fd8182397dc5c3abd77f20.ppt