24f7ff8e83d3bc1665ec626a0d5c03bd.ppt
- Количество слайдов: 41
HOW I DO CMR SCANNING SAFELY Elisabeth Burman Research Sister Royal Brompton Hospital, London UK This presentation is posted for members of scmr as an educational guide – it represents the views and practices of the author, and not necessarily those of SCMR. 2011 update: some updates added to terminology, MR conditional devices, and contrast with renal failure. JMoon
Magnetic Resonance One of the safest imaging modalities but there are still safety issues Advantages • Non-invasive • No ionizing radiation • Repeat studies present no problem • Fewer ethical problems imaging volunteers Why are there safety issues? • Potential for accidents and even fatalities • Damage to equipment / cost
Safety issues centre around the 3 electromagnetic fields and issues indirectly related Static magnetic field biological effects mechanical effects Gradient Field induced currents (PNS) auditory damage RF Field RF power deposition Burns Other issues contrast agents critically ill patients/resuscitation monitoring quench claustrophobia
Static magnetic field Measured in Gauss or Tesla (10, 000 G equivalent to 1 T) 1. 5 T is 30, 000 x the strength of earth’s magnetic field
Static Magnetic Fields A superconducting magnet is always switched on! 1. Biological effects (potential risk) - exposure to static magnetic fields of up to 4 T are not thought to be harmful Biological effects relevant to clinical imaging - distorted ECG (magnetohydrodynamic effect) - consider prudency with pregnancy 2. Mechanical effects (very real risk) - translational or attractive forces on metallic objects when brought into the field
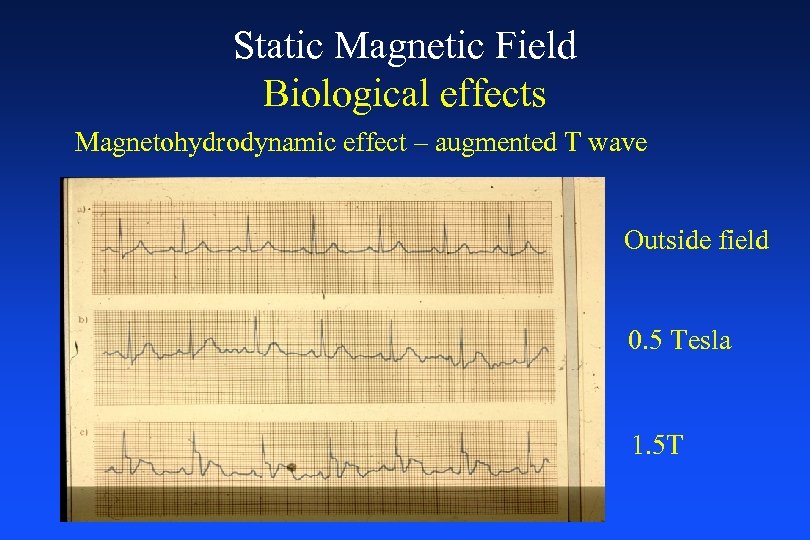
Static Magnetic Field Biological effects Magnetohydrodynamic effect – augmented T wave Outside field 0. 5 Tesla 1. 5 T
Magnetohydrodynamic effect seen as augmentation of T-wave • Caused by the effect of the static magnetic field on moving blood (systole) as a conducting fluid. • The gradient and RF fields also affect the configuration of the ECG • Morphological ECG changes are therefore difficult to detect and diagnose, but rhythm is usually recognised • Any concern regarding rhythm, remove patient from scanner and perform 12 lead ECG
Static Magnetic Field Pregnancy Patients • 1 st trimester – prudent to avoid CMR where possible • 2 nd and 3 rd trimester – decision made on a risk versus benefit determination. For example if it avoids the patient being subjected to x-rays. Health Care Workers • May enter MR scanning room regardless of trimester • Should not remain in the room when scanner is operational, avoiding exposure to gradient and radiofrequency fields
Static Magnetic Field Mechanical effects • Projectile or missile effect - the attractive forces exerted by the static magnetic field present the greatest potential for patient injury - objects will be pulled out of hands, pockets etc, and fly into magnet which has caused injury and death. • Effect on ferromagnetic implants - electro-mechanical eg pacemakers - biomedical eg valves, stents
What is typically ferromagnetic? EQUIPMENT • Oxygen cylinders • Wheelchairs • Trolleys • IV stands • Monitoring equipment • Ventilators PERSONAL ITEMS (leave outside) Keys, pens Bleeps Mobile phones Coins Stethoscopes Scissors It is easy to forget objects, particularly when responding to an emergency! Remember also – magnetic strips will be wiped (credit cards)
Warnings to minimise accidents? OUTSIDE THE SCANNER ROOM • Signage • Barrier cords to scanner room • Restricted access - swipe card / coded entry system INSIDE THE SCANNER ROOM (fringe field – 5 Gauss line) Older systems - passively shielded - extensive fringe field gave a warning Newer systems - actively shielded - small fringe field • greater hazard because there is no gradual warning • field strength increases hundreds of gauss in a few inches
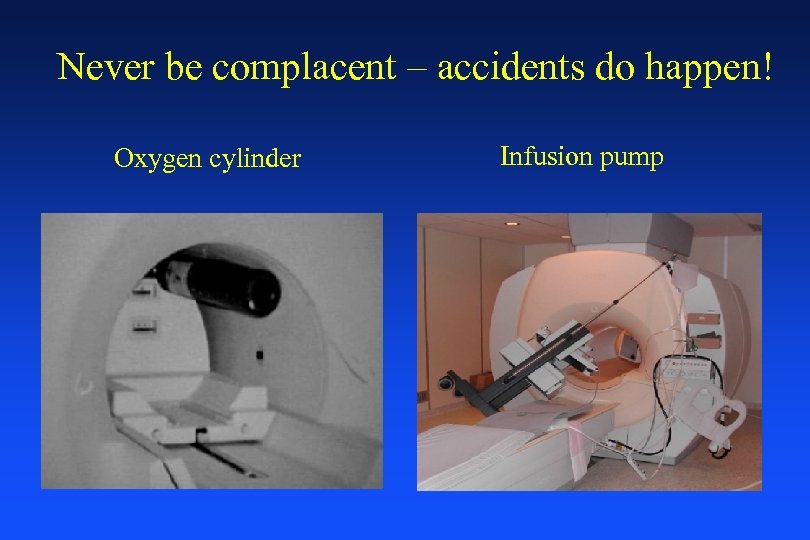
Never be complacent – accidents do happen! Oxygen cylinder Infusion pump
Floor buffer
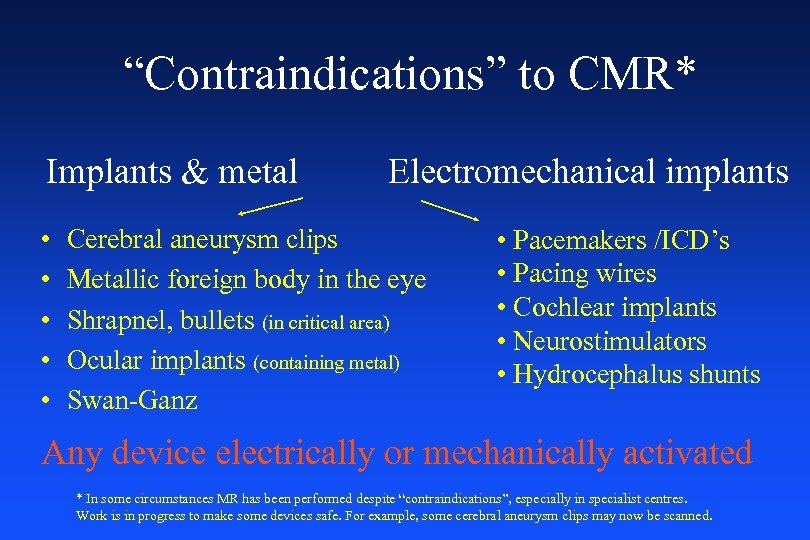
“Contraindications” to CMR* Implants & metal • • • Electromechanical implants Cerebral aneurysm clips Metallic foreign body in the eye Shrapnel, bullets (in critical area) Ocular implants (containing metal) Swan-Ganz • Pacemakers /ICD’s • Pacing wires • Cochlear implants • Neurostimulators • Hydrocephalus shunts Any device electrically or mechanically activated * In some circumstances MR has been performed despite “contraindications”, especially in specialist centres. Work is in progress to make some devices safe. For example, some cerebral aneurysm clips may now be scanned.
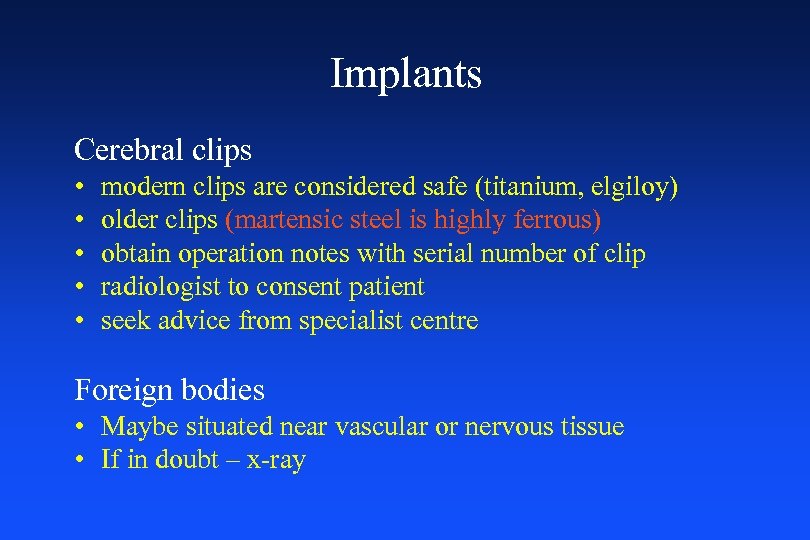
Implants Cerebral clips • • • modern clips are considered safe (titanium, elgiloy) older clips (martensic steel is highly ferrous) obtain operation notes with serial number of clip radiologist to consent patient seek advice from specialist centre Foreign bodies • Maybe situated near vascular or nervous tissue • If in doubt – x-ray
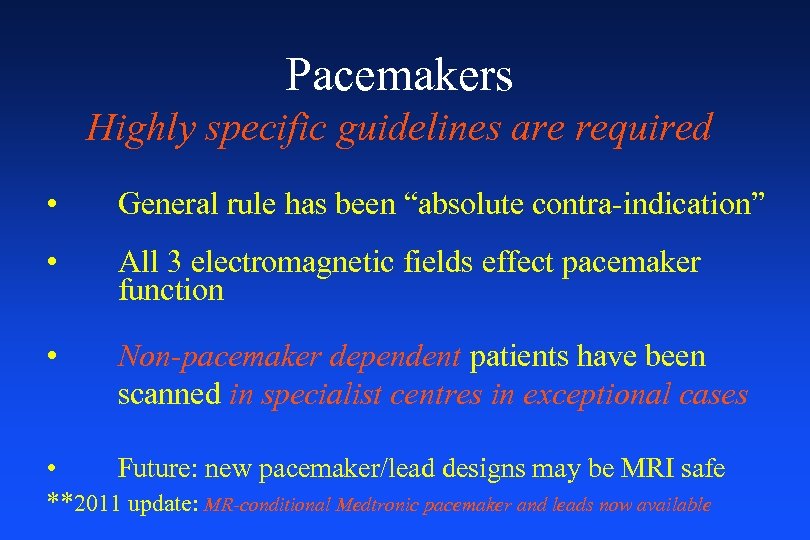
Pacemakers Highly specific guidelines are required • General rule has been “absolute contra-indication” • All 3 electromagnetic fields effect pacemaker function • Non-pacemaker dependent patients have been scanned in specialist centres in exceptional cases • Future: new pacemaker/lead designs may be MRI safe **2011 update: MR-conditional Medtronic pacemaker and leads now available
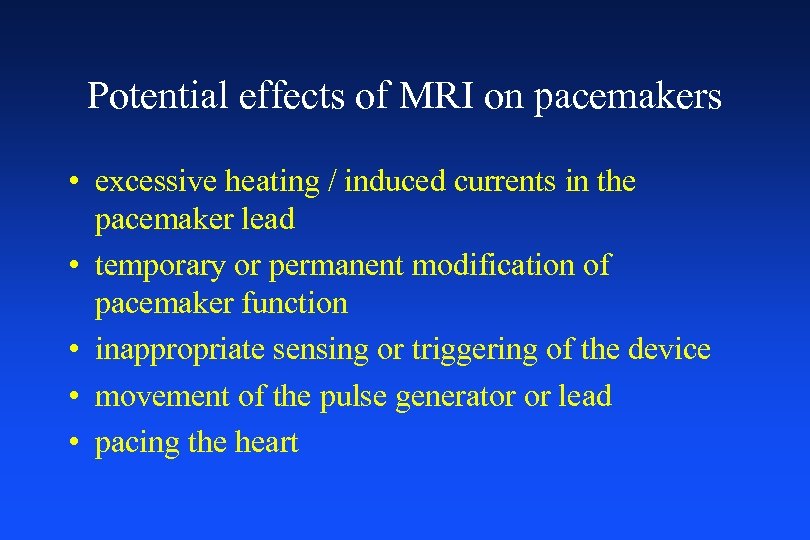
Potential effects of MRI on pacemakers • excessive heating / induced currents in the pacemaker lead • temporary or permanent modification of pacemaker function • inappropriate sensing or triggering of the device • movement of the pulse generator or lead • pacing the heart
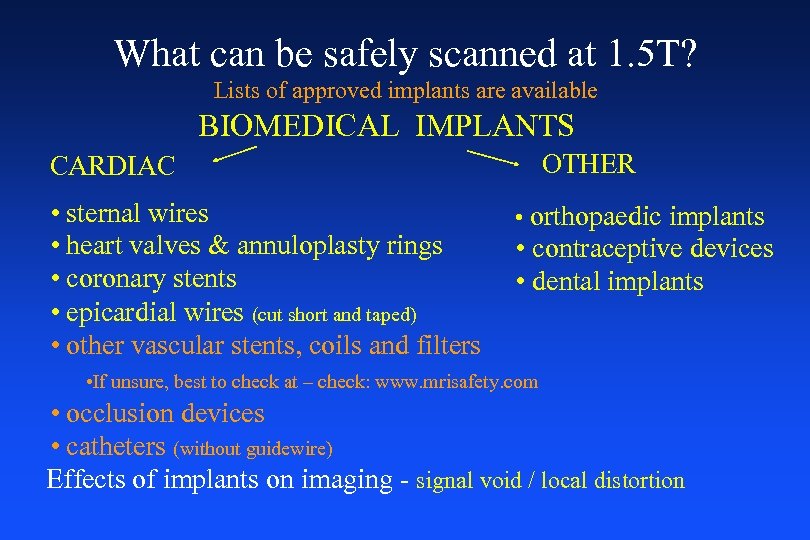
What can be safely scanned at 1. 5 T? Lists of approved implants are available BIOMEDICAL IMPLANTS OTHER CARDIAC • sternal wires • heart valves & annuloplasty rings • coronary stents • epicardial wires (cut short and taped) • other vascular stents, coils and filters • orthopaedic implants • contraceptive devices • dental implants • If unsure, best to check at – check: www. mrisafety. com • occlusion devices • catheters (without guidewire) Effects of implants on imaging - signal void / local distortion
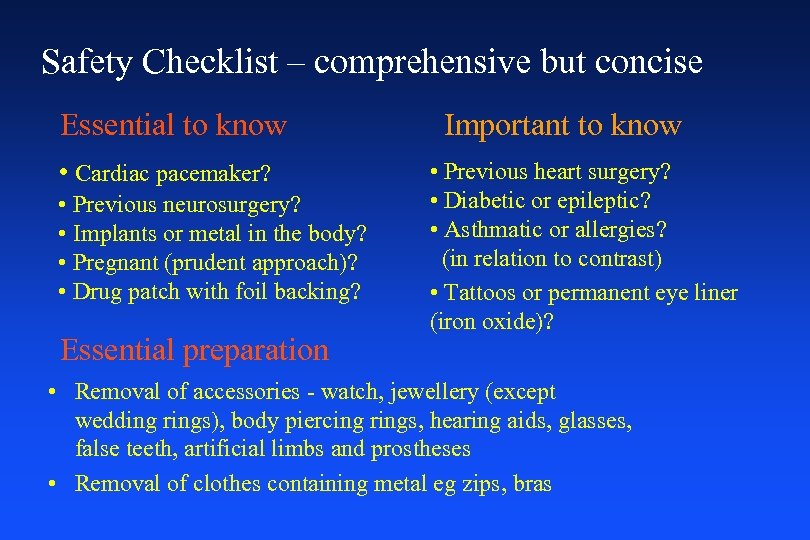
Safety Checklist – comprehensive but concise Essential to know • Cardiac pacemaker? • Previous neurosurgery? • Implants or metal in the body? • Pregnant (prudent approach)? • Drug patch with foil backing? Essential preparation Important to know • Previous heart surgery? • Diabetic or epileptic? • Asthmatic or allergies? (in relation to contrast) • Tattoos or permanent eye liner (iron oxide)? • Removal of accessories - watch, jewellery (except wedding rings), body piercing rings, hearing aids, glasses, false teeth, artificial limbs and prostheses • Removal of clothes containing metal eg zips, bras
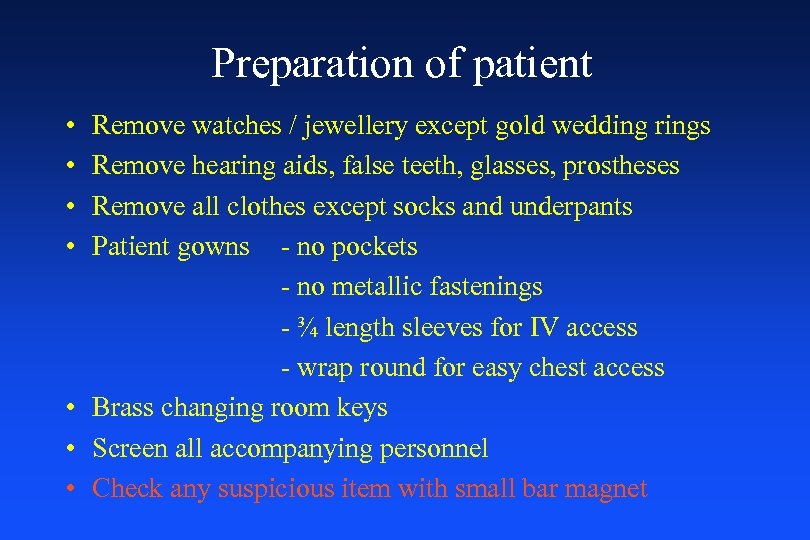
Preparation of patient • • Remove watches / jewellery except gold wedding rings Remove hearing aids, false teeth, glasses, prostheses Remove all clothes except socks and underpants Patient gowns - no pockets - no metallic fastenings - ¾ length sleeves for IV access - wrap round for easy chest access • Brass changing room keys • Screen all accompanying personnel • Check any suspicious item with small bar magnet
Gradient fields - Induced Currents Gradient fields induce an electric field and thus a current in the patient, potentially this can be of sufficient intensity in modern systems to produce a physiological response - peripheral nerve stimulation (PNS) - cardiac stimulation is not considered possible
Gradient fields – Auditory damage Hearing protection mandatory above 90 d. B time averaged for: • patients • staff remaining in the scanner room • relatives accompanying children or patients
Radiofrequency (RF) fields Thermogenic effects - health & safety concern Physiological tissue heating response • most of the transmitted RF power is transferred into heat within the patient’s tissue • all MR systems have safety thresholds to avoid dangerous levels • Patients with compromised thermoregularory systems are at greatest risk
Specific Absorption Rate (SAR) SAR is the RF power absorbed per unit mass of tissue (expressed in W/kg) • complex function of numerous variables • calculated by software from the average forward power passing into the RF transmitter coil and the body mass situated in the RF transmitting field Therefore an accurate patient weight is vital • SAR increases 9 fold from 0. 5 T to 1. 5 T
Radiofrequency (RF) fields Potential for burns • 1°, 2°, 3° burns have occurred in the past in patients undergoing MRI • This is a result of excessive heat developing in the devices or objects • ECG system is often the culprit • Interventional MRI poses greater risk
Prevention of burns • Electrodes - carbon fibre studs - placed close together • ECG leads - carbon fibre - fibre optic - high impedance - short as possible (plaited if necessary) • All conductive leads should be placed in a linear fashion coming out of bore of scanner • Avoid crossed limbs where possible
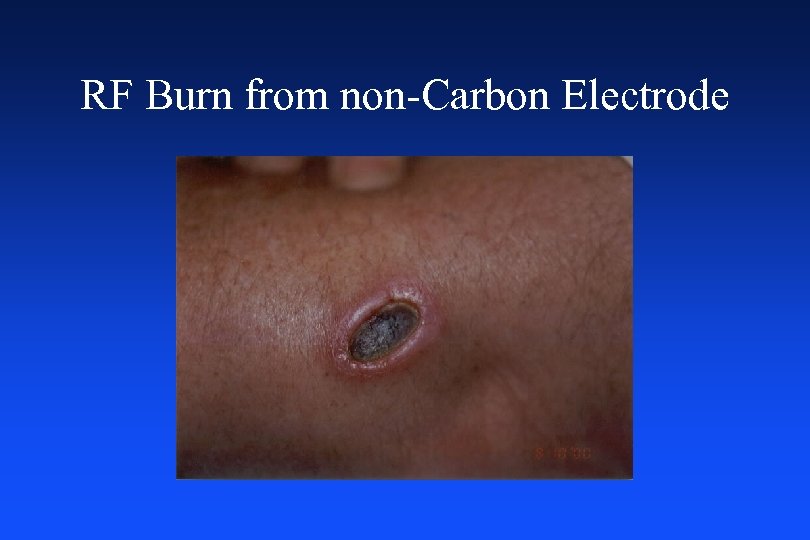
RF Burn from non-Carbon Electrode
Other Issues • Contrast agents • Critically ill patients / resuscitation • Monitoring and equipment related hazards • Quench of superconducting magnets • Claustrophobia
Contrast agents • all gadolinium chelates • overall patient tolerance high • incidence of adverse reactions very low Possible reactions: • headache, nausea and vomiting, pain if extravasation occurs • anaphylaxis 1: 100, 000 Contraindications • GFR<30 ms/minute • pregnancy (risk versus benefit ratio) • breast feeding mothers • infants < 2 years Caution • asthmatics, history of previous reactions
Critically ill patients AICU and High Dependency Patients • • Assess patient the day before Lengthen and prime IV lines on ward Replace electrodes - carbon studs Lengthen chest drains Check intubation circuits for metal Educate nursing staff in preparing patient Ensure status of patient has not changed since referral Screen all accompanying personnel
Sedated patients • Departmental ‘sedation protocol’ with anaesthetic approval • Nil by mouth for 6 hrs (food & milk) 2 hrs water • Medical examination • Informed consent • Tipping trolley, piped oxygen, full resuscitation equipment • Responsible adult to collect from department and remain with for 24 hours
Resuscitation • • Alert cardiac arrest team Call for help BLS only can be performed in scanner room Keep MR Compatible ‘tipping trolley’ adjacent to scanner • Patient must be moved to designated resuscitation area as quickly as possible • Appoint non-clinical person to prevent access to scanner room • Practice regular ‘cardiac arrest’ scenarios to identify potential problems
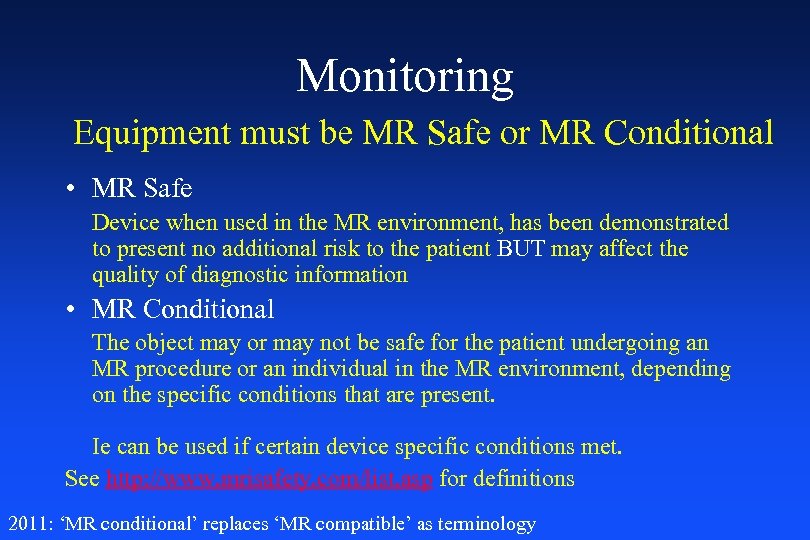
Monitoring Equipment must be MR Safe or MR Conditional • MR Safe Device when used in the MR environment, has been demonstrated to present no additional risk to the patient BUT may affect the quality of diagnostic information • MR Conditional The object may or may not be safe for the patient undergoing an MR procedure or an individual in the MR environment, depending on the specific conditions that are present. Ie can be used if certain device specific conditions met. See http: //www. mrisafety. com/list. asp for definitions 2011: ‘MR conditional’ replaces ‘MR compatible’ as terminology
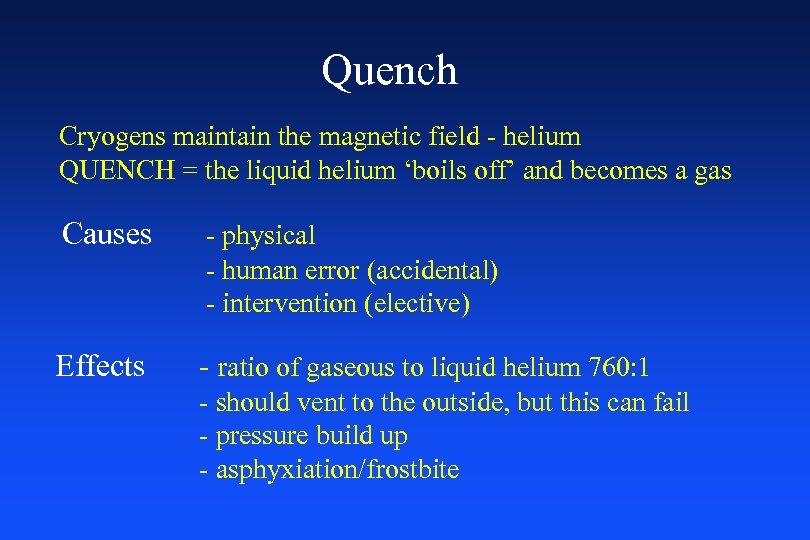
Quench Cryogens maintain the magnetic field - helium QUENCH = the liquid helium ‘boils off’ and becomes a gas Causes - physical - human error (accidental) - intervention (elective) Effects - ratio of gaseous to liquid helium 760: 1 - should vent to the outside, but this can fail - pressure build up - asphyxiation/frostbite
Elective Quenching The magnet should only be quenched in two situations: • If someone is trapped to the scanner by a ferromagnetic object and is injured and/or distressed (eg O 2 cylinder, piece of equipment) • If there is a fire in the immediate vicinity on order to reduce risk to the Fire Brigade
Action to be taken in the event of a Quench • • • Evacuate the room as quickly as possible Ensure the door is kept open during evacuation Close door after evacuation If trapped in room stay close to floor level Seek the advice of a senior physicist immediately Call scanner engineer
Claustrophobia Affects 5 -10% of patients Causes • restrictive dimensions of the interior of the magnet • duration of the examination • gradient coil induced noises • the ambient condition within the imaging bore
Factors to reduce anxiety • • • education and explanation trial visit to the department maintaining physical and verbal contact presence of a relative or friend use of a mirror, prism glasses good communication system alarm good light and ventilation music pleasant thoughts
Ensuring Safe Practice • Safety Checklist – comprehensive but concise • Restricted access to magnetic field area • MR Compatible equipment – monitors, wheelchairs, syringe pumps, stethoscopes • Awareness of medication common to patient area – contrast agents, stress agents • Staff Induction • Education and training of staff of all disciplines • Risk Assessments • Policies and Procedures – cardiac arrest, quench
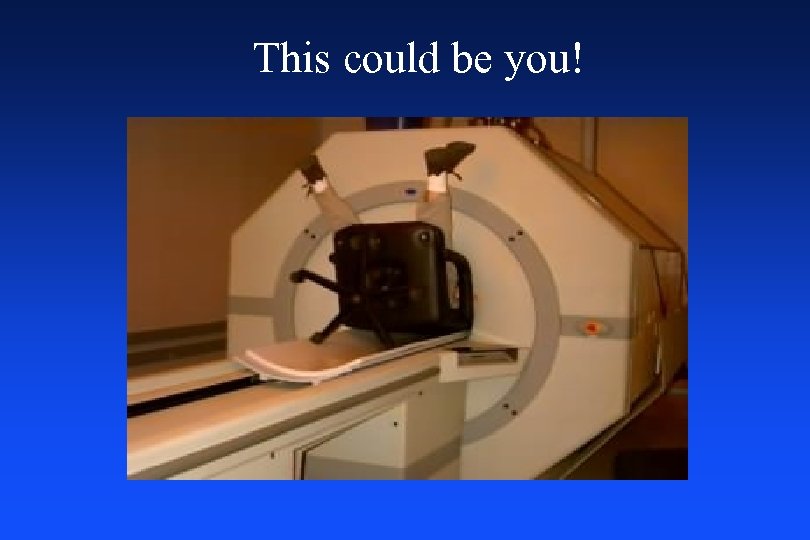
This could be you!
References • Shellock F. G. and Kanal E. (2001) - Magnetic Resonance Bioeffects, Safety, and Patient Management • Health Protection Agency (HPA) (was National Radiological Protection Board -NRPB) • International Electrical Committee (IEC) • Medical and Healthcare products Regulatory Agency (MRHA) (was Medical Devices Agency - MDA) • http: //www. mrisafety. com (Shellock and Kanal) • http: //www. imrser. org/ • http: //www. magneticresonancesafetytesting. com/
24f7ff8e83d3bc1665ec626a0d5c03bd.ppt