09f0cc3aff3239dfe5b16897323d1072.ppt
- Количество слайдов: 31
 Household Care Survey discussion on Data Analysis Jane Remme, Lucia Rost, Thalia Kidder December 2014
Household Care Survey discussion on Data Analysis Jane Remme, Lucia Rost, Thalia Kidder December 2014
 While you are waiting 1. Test your audio • Tools > Audio set up Wizard 2. Close down any other applications E. g. Skype 3. Don’t use Internet Explorer. Use Chrome or other browser to launch and join Blackboard Collaborate. 4. Participating in the webinar: • All questions and comments are welcome! • Type comments/questions in the chat box at any time, • To use microphone: signal, turn on, speak slowly, turn off. • The webinar will be recorded and available for others afterwards 5. Any problems? • Let us know via the chat box • Email mmichalopoulou@oxfam. org. uk Page 2
While you are waiting 1. Test your audio • Tools > Audio set up Wizard 2. Close down any other applications E. g. Skype 3. Don’t use Internet Explorer. Use Chrome or other browser to launch and join Blackboard Collaborate. 4. Participating in the webinar: • All questions and comments are welcome! • Type comments/questions in the chat box at any time, • To use microphone: signal, turn on, speak slowly, turn off. • The webinar will be recorded and available for others afterwards 5. Any problems? • Let us know via the chat box • Email mmichalopoulou@oxfam. org. uk Page 2
 Problems? If you are having trouble hearing or being heard: 1. Close other applications on your computer (improves speed!) 2. Change your connection speed Go to Edit menu -> Preferences->Session, and then select ISDN, wireless or other lower connection 3. Still having problems? Connect to session via phone • • Call: 0044 207 819 3600 Participants code: 14800312# Page 3
Problems? If you are having trouble hearing or being heard: 1. Close other applications on your computer (improves speed!) 2. Change your connection speed Go to Edit menu -> Preferences->Session, and then select ISDN, wireless or other lower connection 3. Still having problems? Connect to session via phone • • Call: 0044 207 819 3600 Participants code: 14800312# Page 3
 Your Questions: If you have specific questions now that you would like answered in this webinar – please type them in! Page 4
Your Questions: If you have specific questions now that you would like answered in this webinar – please type them in! Page 4
 Some of the WE-Care team from Oxfam House Thalia Kidder Jane Remme Lucia Rost Page 5
Some of the WE-Care team from Oxfam House Thalia Kidder Jane Remme Lucia Rost Page 5
 Objectives of today’s Webinar This webinar is designed as a discussion of options. We encourage your feedback We aim to: • Review the main research questions to be answered by data analysis of the first quantitative household survey • Propose a standard set of analyses in each project and offer a several standard tables to present the findings: 1. Household characteristics 2. Time use 3. Gender and age inequality 4. Norms and perceptions 5. Factors influencing heavy & unequal care • Outline more analyses to be done ‘centrally’ in Oxford • Discuss, comment, modify. . . Page 6
Objectives of today’s Webinar This webinar is designed as a discussion of options. We encourage your feedback We aim to: • Review the main research questions to be answered by data analysis of the first quantitative household survey • Propose a standard set of analyses in each project and offer a several standard tables to present the findings: 1. Household characteristics 2. Time use 3. Gender and age inequality 4. Norms and perceptions 5. Factors influencing heavy & unequal care • Outline more analyses to be done ‘centrally’ in Oxford • Discuss, comment, modify. . . Page 6
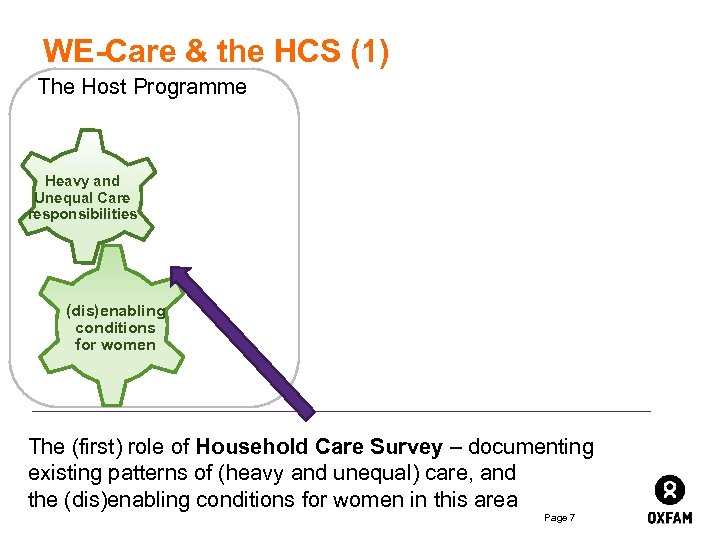 WE-Care & the HCS (1) The Host Programme Heavy and Unequal Care responsibilities (dis)enabling conditions for women The (first) role of Household Care Survey – documenting existing patterns of (heavy and unequal) care, and the (dis)enabling conditions for women in this area Page 7
WE-Care & the HCS (1) The Host Programme Heavy and Unequal Care responsibilities (dis)enabling conditions for women The (first) role of Household Care Survey – documenting existing patterns of (heavy and unequal) care, and the (dis)enabling conditions for women in this area Page 7
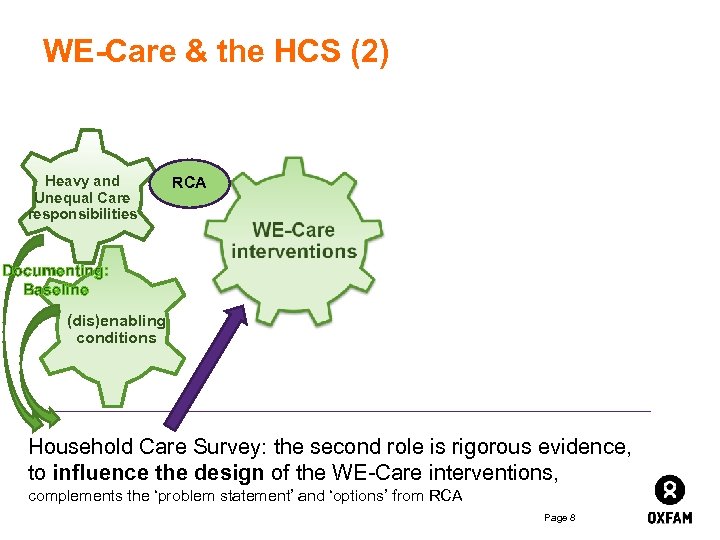 WE-Care & the HCS (2) Heavy and Unequal Care responsibilities RCA Documenting: Baseline (dis)enabling conditions Household Care Survey: the second role is rigorous evidence, to influence the design of the WE-Care interventions, complements the ‘problem statement’ and ‘options’ from RCA Page 8
WE-Care & the HCS (2) Heavy and Unequal Care responsibilities RCA Documenting: Baseline (dis)enabling conditions Household Care Survey: the second role is rigorous evidence, to influence the design of the WE-Care interventions, complements the ‘problem statement’ and ‘options’ from RCA Page 8
 How will change happen in care patterns? The 4 Rs • Recognition of care work • Reducing arduous and difficult care tasks/ hours of work • Redistributing care – in the household, and to the state (and employers) • Representation of carers in decision-making Page 9
How will change happen in care patterns? The 4 Rs • Recognition of care work • Reducing arduous and difficult care tasks/ hours of work • Redistributing care – in the household, and to the state (and employers) • Representation of carers in decision-making Page 9
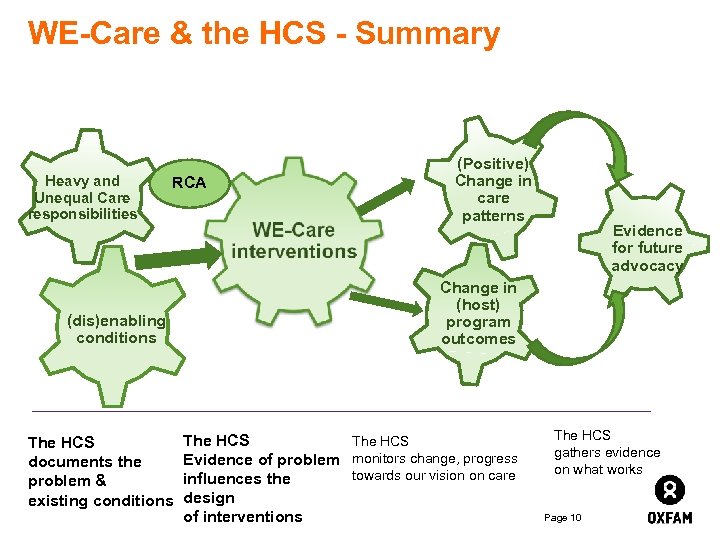 WE-Care & the HCS - Summary Heavy and Unequal Care responsibilities RCA (dis)enabling conditions The HCS documents the problem & existing conditions (Positive) Change in care patterns Evidence for future advocacy Change in (host) program outcomes The HCS Evidence of problem monitors change, progress towards our vision on care influences the design of interventions The HCS gathers evidence on what works Page 10
WE-Care & the HCS - Summary Heavy and Unequal Care responsibilities RCA (dis)enabling conditions The HCS documents the problem & existing conditions (Positive) Change in care patterns Evidence for future advocacy Change in (host) program outcomes The HCS Evidence of problem monitors change, progress towards our vision on care influences the design of interventions The HCS gathers evidence on what works Page 10
 What are indicators of positive (negative) change (1) • Number of total hours spent on care work for women/families • Positive: Reduced number of total hours spent on care tasks for women, girls, families • Negative: Increased number of total hours spent on care tasks for women, girls, families • Gender distribution of household care work • Positive: Increased % of care work done by men and boys • Negative: Increased % of care work done by girls, older/other women in households • Attitudes towards care and gender roles • Positive: Increased recognition and value given to care work / Men’s contribution to care work is promoted and valued • Negative: Increased VAW/GBV / Women who do less care work are criticised / Men who do more care work are criticised Page 11
What are indicators of positive (negative) change (1) • Number of total hours spent on care work for women/families • Positive: Reduced number of total hours spent on care tasks for women, girls, families • Negative: Increased number of total hours spent on care tasks for women, girls, families • Gender distribution of household care work • Positive: Increased % of care work done by men and boys • Negative: Increased % of care work done by girls, older/other women in households • Attitudes towards care and gender roles • Positive: Increased recognition and value given to care work / Men’s contribution to care work is promoted and valued • Negative: Increased VAW/GBV / Women who do less care work are criticised / Men who do more care work are criticised Page 11
 What are indicators of positive (negative) change (2) • Investments in time- and labour-saving equipment • Positive: Increased purchased by families (men’s income) of care services (e. g. already ground flour) • Negative: Increase in poor nutrition and poor care (e. g. pot noodles, less nutritious meals) • Presence/access to state services • Positive: Increased access to and use of state infrastructure (e. g. closer clinics, water and energy) / Increased state and employer services (e. g. childcare, healthcare) • Negative: Reduction in access to and use of state infrastructure / Reduction in state and employer services GAPS IDENTIFIED in research model, so far: • Gender-based violence, criticism, abuse against women for doing less care work, or men doing more care work. • Influence of group membership Page 12
What are indicators of positive (negative) change (2) • Investments in time- and labour-saving equipment • Positive: Increased purchased by families (men’s income) of care services (e. g. already ground flour) • Negative: Increase in poor nutrition and poor care (e. g. pot noodles, less nutritious meals) • Presence/access to state services • Positive: Increased access to and use of state infrastructure (e. g. closer clinics, water and energy) / Increased state and employer services (e. g. childcare, healthcare) • Negative: Reduction in access to and use of state infrastructure / Reduction in state and employer services GAPS IDENTIFIED in research model, so far: • Gender-based violence, criticism, abuse against women for doing less care work, or men doing more care work. • Influence of group membership Page 12
 Your Questions: If you have questions or comments – please type them in! Page 13
Your Questions: If you have questions or comments – please type them in! Page 13
 Standard tables – prioritising certain analyses & findings
Standard tables – prioritising certain analyses & findings
 Main research questions: The baseline: • Who are the families/households being surveyed? • What is the demand for care? (current patterns of care work) • How heavy are work hours, how heavy is care work? • How unequal is care work? • What equipment, infrastructure, services are accessible? • What are the norms and perceptions about care work? The regressions to inform interventions: • What factors are correlated with heavy and unequal care work? Or with less-heavy and more-equal patterns? Page 15
Main research questions: The baseline: • Who are the families/households being surveyed? • What is the demand for care? (current patterns of care work) • How heavy are work hours, how heavy is care work? • How unequal is care work? • What equipment, infrastructure, services are accessible? • What are the norms and perceptions about care work? The regressions to inform interventions: • What factors are correlated with heavy and unequal care work? Or with less-heavy and more-equal patterns? Page 15
 Household characteristics(1 a) Family characteristics (101 -107 women) • Average number of household members • Average of male and female respondents • Three most common types of employment and percentages • Average level of education of respondents, male and female • Religion, and percentages of respondents (male and female) Households’ economic status (301 -308, 310 -313 women) • Percentage of household owning 4 -5 key assets (tbd locally) • Percentage of women with independent income • Percentage of women with independent savings • Assets used to determine wealth categories for households surveyed Page 16
Household characteristics(1 a) Family characteristics (101 -107 women) • Average number of household members • Average of male and female respondents • Three most common types of employment and percentages • Average level of education of respondents, male and female • Religion, and percentages of respondents (male and female) Households’ economic status (301 -308, 310 -313 women) • Percentage of household owning 4 -5 key assets (tbd locally) • Percentage of women with independent income • Percentage of women with independent savings • Assets used to determine wealth categories for households surveyed Page 16
 Household characteristics(1 b) Wealth categories: (301 -308 women) How much does household economic status explain differences in care patterns? 1. Local knowledge determines which assets are characteristic of households in each quintile (quartile? ); Ø Ø Food security surveys have asset-lists to identify households at risk of food insecurity Take list of assets in survey and put assets in relative wealth groups: top: motorcycle, house made of brick, television, over xx animals; next: house with zinc roof, yy animals; etc 2. Identify/label respondent-households by quintile/quartile 3. Regression analysis with wealth and hours, wealth and gender distribution of care responsibility Analysis also on hours of care work, and whether women report an independent income, independent savings, decision-making power over more than 50% of her own income. Page 17
Household characteristics(1 b) Wealth categories: (301 -308 women) How much does household economic status explain differences in care patterns? 1. Local knowledge determines which assets are characteristic of households in each quintile (quartile? ); Ø Ø Food security surveys have asset-lists to identify households at risk of food insecurity Take list of assets in survey and put assets in relative wealth groups: top: motorcycle, house made of brick, television, over xx animals; next: house with zinc roof, yy animals; etc 2. Identify/label respondent-households by quintile/quartile 3. Regression analysis with wealth and hours, wealth and gender distribution of care responsibility Analysis also on hours of care work, and whether women report an independent income, independent savings, decision-making power over more than 50% of her own income. Page 17
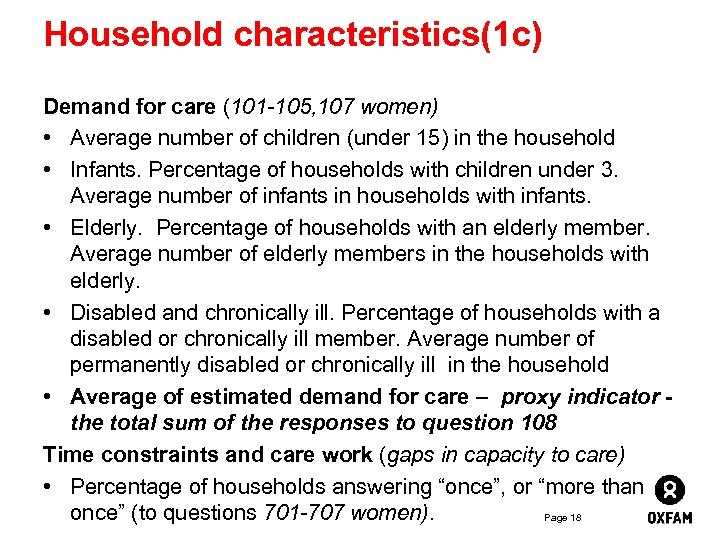 Household characteristics(1 c) Demand for care (101 -105, 107 women) • Average number of children (under 15) in the household • Infants. Percentage of households with children under 3. Average number of infants in households with infants. • Elderly. Percentage of households with an elderly member. Average number of elderly members in the households with elderly. • Disabled and chronically ill. Percentage of households with a disabled or chronically ill member. Average number of permanently disabled or chronically ill in the household • Average of estimated demand for care – proxy indicator the total sum of the responses to question 108 Time constraints and care work (gaps in capacity to care) • Percentage of households answering “once”, or “more than once” (to questions 701 -707 women). Page 18
Household characteristics(1 c) Demand for care (101 -105, 107 women) • Average number of children (under 15) in the household • Infants. Percentage of households with children under 3. Average number of infants in households with infants. • Elderly. Percentage of households with an elderly member. Average number of elderly members in the households with elderly. • Disabled and chronically ill. Percentage of households with a disabled or chronically ill member. Average number of permanently disabled or chronically ill in the household • Average of estimated demand for care – proxy indicator the total sum of the responses to question 108 Time constraints and care work (gaps in capacity to care) • Percentage of households answering “once”, or “more than once” (to questions 701 -707 women). Page 18
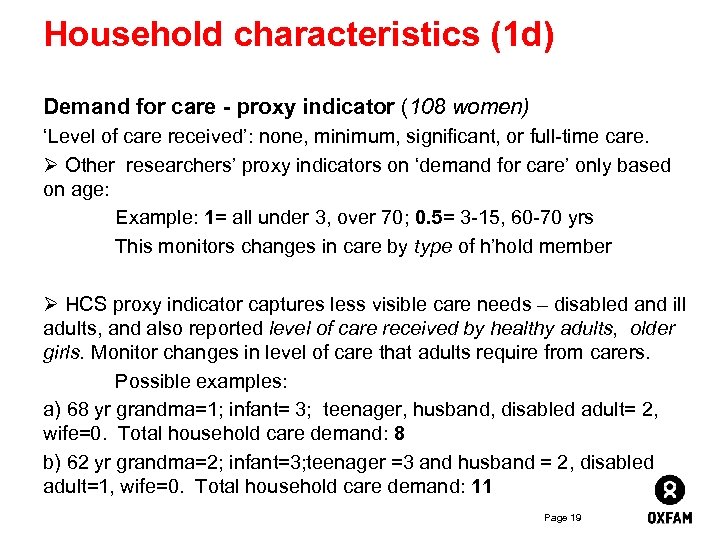 Household characteristics (1 d) Demand for care - proxy indicator (108 women) ‘Level of care received’: none, minimum, significant, or full-time care. Ø Other researchers’ proxy indicators on ‘demand for care’ only based on age: Example: 1= all under 3, over 70; 0. 5= 3 -15, 60 -70 yrs This monitors changes in care by type of h’hold member Ø HCS proxy indicator captures less visible care needs – disabled and ill adults, and also reported level of care received by healthy adults, older girls. Monitor changes in level of care that adults require from carers. Possible examples: a) 68 yr grandma=1; infant= 3; teenager, husband, disabled adult= 2, wife=0. Total household care demand: 8 b) 62 yr grandma=2; infant=3; teenager =3 and husband = 2, disabled adult=1, wife=0. Total household care demand: 11 Page 19
Household characteristics (1 d) Demand for care - proxy indicator (108 women) ‘Level of care received’: none, minimum, significant, or full-time care. Ø Other researchers’ proxy indicators on ‘demand for care’ only based on age: Example: 1= all under 3, over 70; 0. 5= 3 -15, 60 -70 yrs This monitors changes in care by type of h’hold member Ø HCS proxy indicator captures less visible care needs – disabled and ill adults, and also reported level of care received by healthy adults, older girls. Monitor changes in level of care that adults require from carers. Possible examples: a) 68 yr grandma=1; infant= 3; teenager, husband, disabled adult= 2, wife=0. Total household care demand: 8 b) 62 yr grandma=2; infant=3; teenager =3 and husband = 2, disabled adult=1, wife=0. Total household care demand: 11 Page 19
 Your Questions: If you have ideas, comments or questions now – please type them in! Page 20
Your Questions: If you have ideas, comments or questions now – please type them in! Page 20
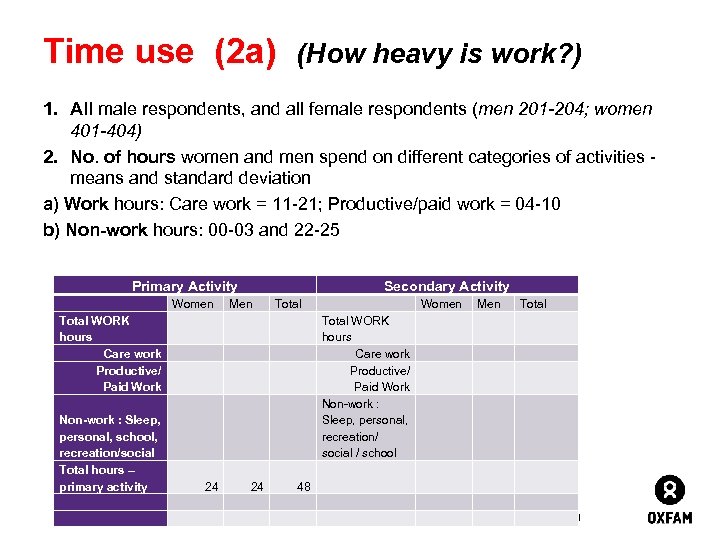 Time use (2 a) (How heavy is work? ) 1. All male respondents, and all female respondents (men 201 -204; women 401 -404) 2. No. of hours women and men spend on different categories of activities - means and standard deviation a) Work hours: Care work = 11 -21; Productive/paid work = 04 -10 b) Non-work hours: 00 -03 and 22 -25 Primary Activity Women Secondary Activity Men Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, school, recreation/social Total hours – primary activity 24 24 Total Women Men Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, recreation/ social / school 48 Page 21
Time use (2 a) (How heavy is work? ) 1. All male respondents, and all female respondents (men 201 -204; women 401 -404) 2. No. of hours women and men spend on different categories of activities - means and standard deviation a) Work hours: Care work = 11 -21; Productive/paid work = 04 -10 b) Non-work hours: 00 -03 and 22 -25 Primary Activity Women Secondary Activity Men Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, school, recreation/social Total hours – primary activity 24 24 Total Women Men Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, recreation/ social / school 48 Page 21
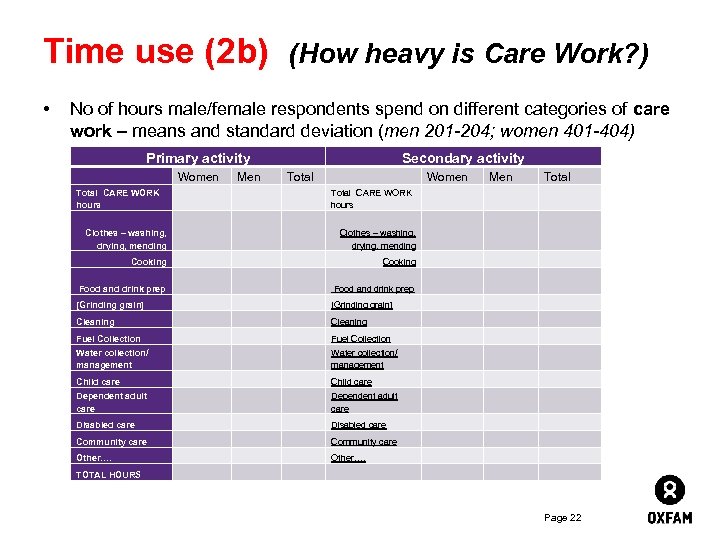 Time use (2 b) (How heavy is Care Work? ) • No of hours male/female respondents spend on different categories of care work – means and standard deviation (men 201 -204; women 401 -404) Secondary activity Primary activity Women Men Total CARE WORK hours Women Total CARE WORK hours Men Total Clothes – washing, drying, mending Cooking Food and drink prep [Grinding grain] Cleaning Fuel Collection Water collection/ management Child care Dependent adult care Disabled care Community care Other…. TOTAL HOURS Page 22
Time use (2 b) (How heavy is Care Work? ) • No of hours male/female respondents spend on different categories of care work – means and standard deviation (men 201 -204; women 401 -404) Secondary activity Primary activity Women Men Total CARE WORK hours Women Total CARE WORK hours Men Total Clothes – washing, drying, mending Cooking Food and drink prep [Grinding grain] Cleaning Fuel Collection Water collection/ management Child care Dependent adult care Disabled care Community care Other…. TOTAL HOURS Page 22
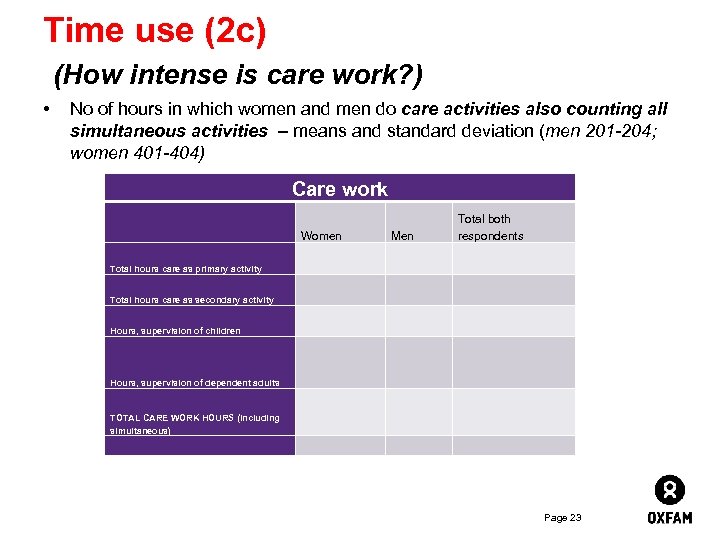 Time use (2 c) (How intense is care work? ) • No of hours in which women and men do care activities also counting all simultaneous activities – means and standard deviation (men 201 -204; women 401 -404) Care work Women Men Total both respondents Total hours care as primary activity Total hours care as secondary activity Hours, supervision of children Hours, supervision of dependent adults TOTAL CARE WORK HOURS (including simultaneous) Page 23
Time use (2 c) (How intense is care work? ) • No of hours in which women and men do care activities also counting all simultaneous activities – means and standard deviation (men 201 -204; women 401 -404) Care work Women Men Total both respondents Total hours care as primary activity Total hours care as secondary activity Hours, supervision of children Hours, supervision of dependent adults TOTAL CARE WORK HOURS (including simultaneous) Page 23
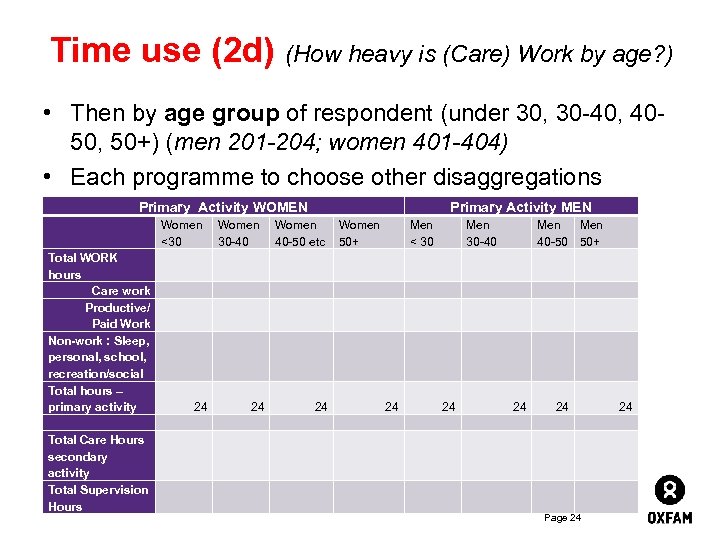 Time use (2 d) (How heavy is (Care) Work by age? ) • Then by age group of respondent (under 30, 30 -40, 4050, 50+) (men 201 -204; women 401 -404) • Each programme to choose other disaggregations Primary Activity WOMEN Women <30 Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, school, recreation/social Total hours – primary activity Total Care Hours secondary activity Total Supervision Hours Women 30 -40 Primary Activity MEN Women 40 -50 etc Women 50+ Men < 30 30 -40 Men 40 -50 50+ 24 24 24 Page 24
Time use (2 d) (How heavy is (Care) Work by age? ) • Then by age group of respondent (under 30, 30 -40, 4050, 50+) (men 201 -204; women 401 -404) • Each programme to choose other disaggregations Primary Activity WOMEN Women <30 Total WORK hours Care work Productive/ Paid Work Non-work : Sleep, personal, school, recreation/social Total hours – primary activity Total Care Hours secondary activity Total Supervision Hours Women 30 -40 Primary Activity MEN Women 40 -50 etc Women 50+ Men < 30 30 -40 Men 40 -50 50+ 24 24 24 Page 24
 Your Questions: An opportunity for more ideas, comments or questions – please type them in! Page 25
Your Questions: An opportunity for more ideas, comments or questions – please type them in! Page 25
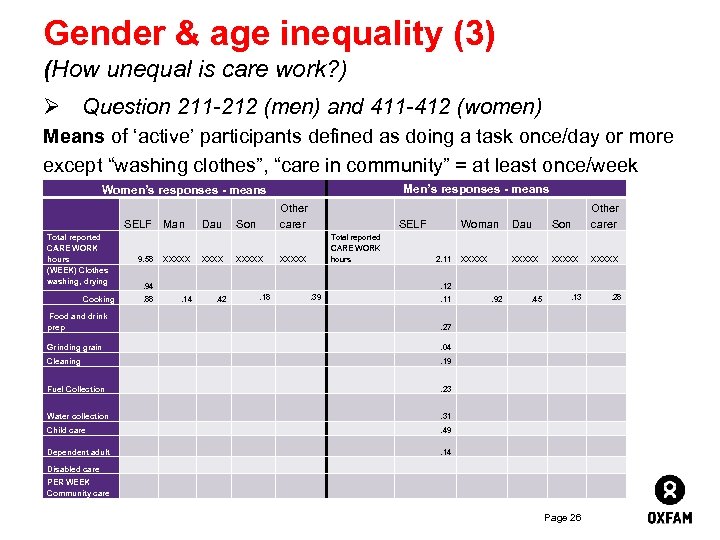 Gender & age inequality (3) (How unequal is care work? ) Ø Question 211 -212 (men) and 411 -412 (women) Means of ‘active’ participants defined as doing a task once/day or more except “washing clothes”, “care in community” = at least once/week Men’s responses - means Women’s responses - means SELF Total reported CARE WORK hours (WEEK) Clothes washing, drying Cooking 9. 58 Man XXXXX Dau XXXX Other carer XXXXX Son Total reported CARE WORK hours . 18 . 39 . 42 . 19 . 23 . 31 . 49 . 04 Dependent adult . 27 . 45 . 28 . 92 . 13 . 11 . 12 Water collection XXXXX PER WEEK Community care XXXXX Fuel Collection Disabled care XXXXX Child care XXXXX Other carer Son Grinding grain Cleaning 2. 11 Dau . 14 Food and drink prep Woman . 94. 88 SELF . 14 Page 26
Gender & age inequality (3) (How unequal is care work? ) Ø Question 211 -212 (men) and 411 -412 (women) Means of ‘active’ participants defined as doing a task once/day or more except “washing clothes”, “care in community” = at least once/week Men’s responses - means Women’s responses - means SELF Total reported CARE WORK hours (WEEK) Clothes washing, drying Cooking 9. 58 Man XXXXX Dau XXXX Other carer XXXXX Son Total reported CARE WORK hours . 18 . 39 . 42 . 19 . 23 . 31 . 49 . 04 Dependent adult . 27 . 45 . 28 . 92 . 13 . 11 . 12 Water collection XXXXX PER WEEK Community care XXXXX Fuel Collection Disabled care XXXXX Child care XXXXX Other carer Son Grinding grain Cleaning 2. 11 Dau . 14 Food and drink prep Woman . 94. 88 SELF . 14 Page 26
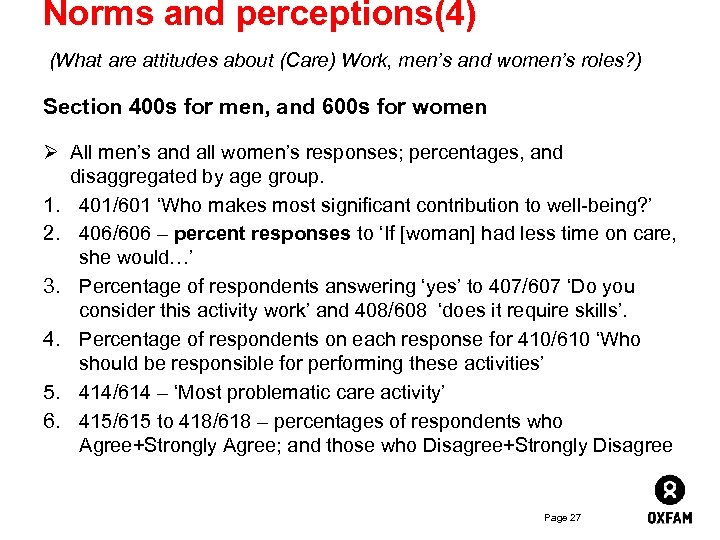 Norms and perceptions(4) (What are attitudes about (Care) Work, men’s and women’s roles? ) Section 400 s for men, and 600 s for women Ø All men’s and all women’s responses; percentages, and disaggregated by age group. 1. 401/601 ‘Who makes most significant contribution to well-being? ’ 2. 406/606 – percent responses to ‘If [woman] had less time on care, she would…’ 3. Percentage of respondents answering ‘yes’ to 407/607 ‘Do you consider this activity work’ and 408/608 ‘does it require skills’. 4. Percentage of respondents on each response for 410/610 ‘Who should be responsible for performing these activities’ 5. 414/614 – ‘Most problematic care activity’ 6. 415/615 to 418/618 – percentages of respondents who Agree+Strongly Agree; and those who Disagree+Strongly Disagree Page 27
Norms and perceptions(4) (What are attitudes about (Care) Work, men’s and women’s roles? ) Section 400 s for men, and 600 s for women Ø All men’s and all women’s responses; percentages, and disaggregated by age group. 1. 401/601 ‘Who makes most significant contribution to well-being? ’ 2. 406/606 – percent responses to ‘If [woman] had less time on care, she would…’ 3. Percentage of respondents answering ‘yes’ to 407/607 ‘Do you consider this activity work’ and 408/608 ‘does it require skills’. 4. Percentage of respondents on each response for 410/610 ‘Who should be responsible for performing these activities’ 5. 414/614 – ‘Most problematic care activity’ 6. 415/615 to 418/618 – percentages of respondents who Agree+Strongly Agree; and those who Disagree+Strongly Disagree Page 27
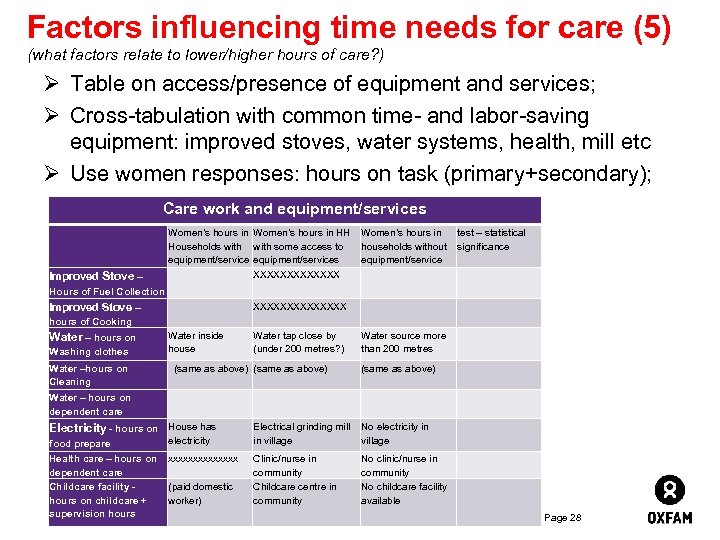 Factors influencing time needs for care (5) (what factors relate to lower/higher hours of care? ) Ø Table on access/presence of equipment and services; Ø Cross-tabulation with common time- and labor-saving equipment: improved stoves, water systems, health, mill etc Ø Use women responses: hours on task (primary+secondary); Care work and equipment/services Improved Stove – Women’s hours in HH Households with some access to equipment/services XXXXXXX Women’s hours in test – statistical households without significance equipment/service Hours of Fuel Collection XXXXXXX Improved Stove – Water tap close by (under 200 metres? ) Water source more than 200 metres hours of Cooking Water – hours on Washing clothes Water –hours on Cleaning Water inside house (same as above) Water – hours on dependent care Electricity - hours on House has food prepare (same as above) electricity Health care – hours on xxxxxxx dependent care Childcare facility - (paid domestic hours on childcare + worker) supervision hours Electrical grinding mill No electricity in in village Clinic/nurse in community Childcare centre in community No clinic/nurse in community No childcare facility available Page 28
Factors influencing time needs for care (5) (what factors relate to lower/higher hours of care? ) Ø Table on access/presence of equipment and services; Ø Cross-tabulation with common time- and labor-saving equipment: improved stoves, water systems, health, mill etc Ø Use women responses: hours on task (primary+secondary); Care work and equipment/services Improved Stove – Women’s hours in HH Households with some access to equipment/services XXXXXXX Women’s hours in test – statistical households without significance equipment/service Hours of Fuel Collection XXXXXXX Improved Stove – Water tap close by (under 200 metres? ) Water source more than 200 metres hours of Cooking Water – hours on Washing clothes Water –hours on Cleaning Water inside house (same as above) Water – hours on dependent care Electricity - hours on House has food prepare (same as above) electricity Health care – hours on xxxxxxx dependent care Childcare facility - (paid domestic hours on childcare + worker) supervision hours Electrical grinding mill No electricity in in village Clinic/nurse in community Childcare centre in community No clinic/nurse in community No childcare facility available Page 28
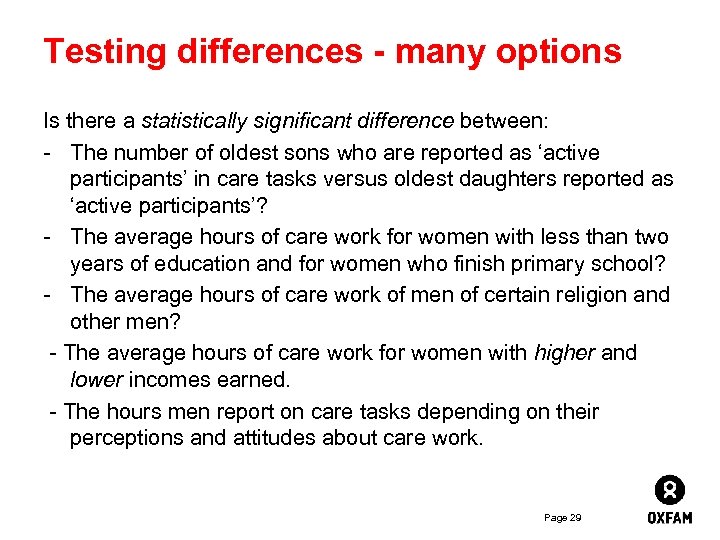 Testing differences - many options Is there a statistically significant difference between: - The number of oldest sons who are reported as ‘active participants’ in care tasks versus oldest daughters reported as ‘active participants’? - The average hours of care work for women with less than two years of education and for women who finish primary school? - The average hours of care work of men of certain religion and other men? - The average hours of care work for women with higher and lower incomes earned. - The hours men report on care tasks depending on their perceptions and attitudes about care work. Page 29
Testing differences - many options Is there a statistically significant difference between: - The number of oldest sons who are reported as ‘active participants’ in care tasks versus oldest daughters reported as ‘active participants’? - The average hours of care work for women with less than two years of education and for women who finish primary school? - The average hours of care work of men of certain religion and other men? - The average hours of care work for women with higher and lower incomes earned. - The hours men report on care tasks depending on their perceptions and attitudes about care work. Page 29
 Your Questions: PLEASE EMAILYOUR IDEAS for FURTHER DISCUSSION Page 30
Your Questions: PLEASE EMAILYOUR IDEAS for FURTHER DISCUSSION Page 30
 Be part of the discussion… http: //growsellthrive. org/group/we-careprogramme-team www. oxfam. org. uk/care Page 31
Be part of the discussion… http: //growsellthrive. org/group/we-careprogramme-team www. oxfam. org. uk/care Page 31


