ce9765a732ee6a699fb12f36e7274425.ppt
- Количество слайдов: 33
 House Officer’s Guide To Renal Patients Staci Smith, DO
House Officer’s Guide To Renal Patients Staci Smith, DO
 Water Exchange • Sensible water loss – able to be measured • Insensible water loss – evaporatory water loss through skin and lungs – normally 10 cc/kg/day – depends on pt’s status • body surface area, temperature, humidity
Water Exchange • Sensible water loss – able to be measured • Insensible water loss – evaporatory water loss through skin and lungs – normally 10 cc/kg/day – depends on pt’s status • body surface area, temperature, humidity
 Water Exchange • Sensible losses – Urine 800 -1500 cc – Intestinal 0 -250 cc – Sweat 500 cc • Insensible losses – 600 -900 cc – Respiratory 400 cc
Water Exchange • Sensible losses – Urine 800 -1500 cc – Intestinal 0 -250 cc – Sweat 500 cc • Insensible losses – 600 -900 cc – Respiratory 400 cc
 Dialysis Patients • Some dialysis pts still make urine • Treat them as if the fluid you give will remain – gain 1 -4 kg in between dialysis sessions
Dialysis Patients • Some dialysis pts still make urine • Treat them as if the fluid you give will remain – gain 1 -4 kg in between dialysis sessions
 Dialysis Patients • Studies have suggested that each 250 cc increment in a daily urine volume is associated with a 36% reduction in mortality. • They also show a 56% risk reduction for death in patients with residual renal function.
Dialysis Patients • Studies have suggested that each 250 cc increment in a daily urine volume is associated with a 36% reduction in mortality. • They also show a 56% risk reduction for death in patients with residual renal function.
 Vascular Access • Three main types of access – arteriovenous fistula – arteriovenous graft – HD catheter • Never stick the fistula or graft • Avoid bp measurements, labs, IV’s in access arm
Vascular Access • Three main types of access – arteriovenous fistula – arteriovenous graft – HD catheter • Never stick the fistula or graft • Avoid bp measurements, labs, IV’s in access arm
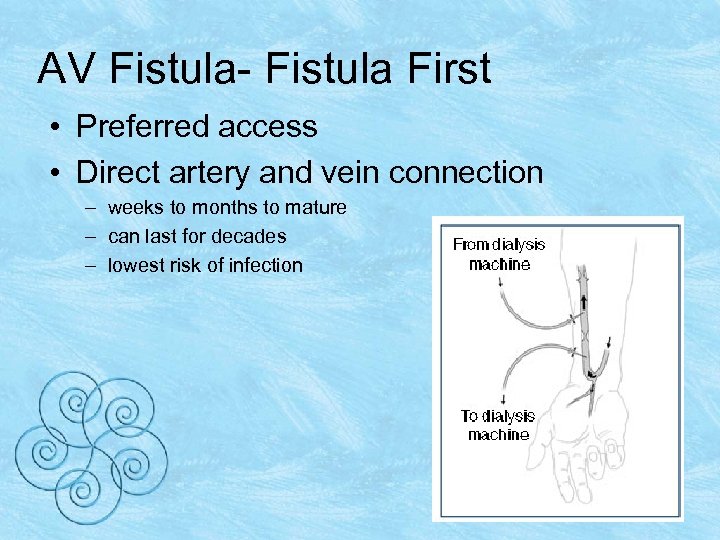 AV Fistula- Fistula First • Preferred access • Direct artery and vein connection – weeks to months to mature – can last for decades – lowest risk of infection
AV Fistula- Fistula First • Preferred access • Direct artery and vein connection – weeks to months to mature – can last for decades – lowest risk of infection
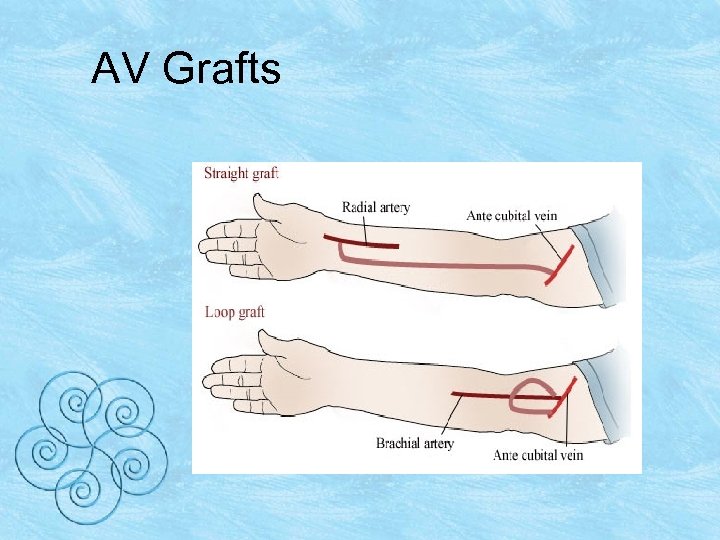 AV Grafts
AV Grafts
 Vascular Access • Check the access for a thrill and bruit • Hypotension leads to thrombosis of the AFV/AVG • Write hold orders for antihypertensives to avoid BP drops
Vascular Access • Check the access for a thrill and bruit • Hypotension leads to thrombosis of the AFV/AVG • Write hold orders for antihypertensives to avoid BP drops
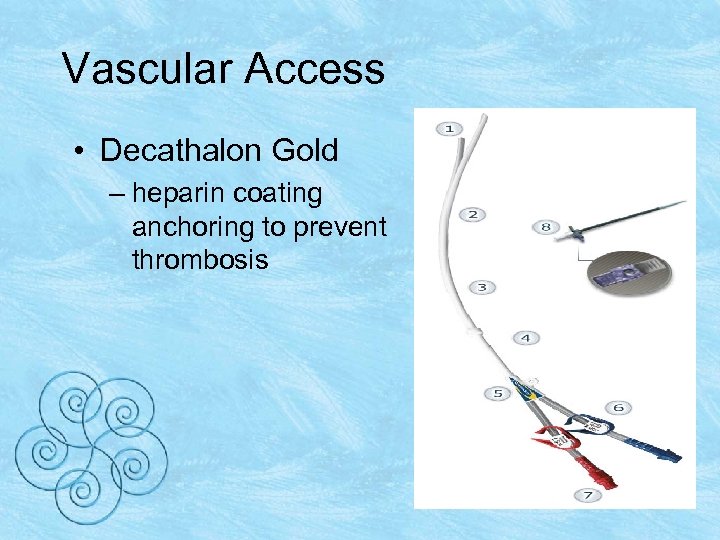 Vascular Access • Decathalon Gold – heparin coating anchoring to prevent thrombosis
Vascular Access • Decathalon Gold – heparin coating anchoring to prevent thrombosis
 Catheters • Usually patients have a tunneled catheter accessing the IJ vein • Try to avoid using the subclavian v – stenosis more frequently – complicating AFV/AVG on that side • Patients may have a catheter for access as they await maturation of the AFV/AVG – short term option
Catheters • Usually patients have a tunneled catheter accessing the IJ vein • Try to avoid using the subclavian v – stenosis more frequently – complicating AFV/AVG on that side • Patients may have a catheter for access as they await maturation of the AFV/AVG – short term option
 Catheters • catheter is heparinized with 1: 5000 solution – heparin flush is 1: 1000 • catheter is labeled with the amount of flush for each port • add 0. 1 cc to the labeled amount
Catheters • catheter is heparinized with 1: 5000 solution – heparin flush is 1: 1000 • catheter is labeled with the amount of flush for each port • add 0. 1 cc to the labeled amount
 Catheters • If the catheter must be used for IV support – draw off 10 cc of blood from the port – flush with saline – never advance the heparin into the patient. • Call Pt’s nephrologist before using the catheter • Obviously, in a code situation aspirate 10 cc’s and use the line!
Catheters • If the catheter must be used for IV support – draw off 10 cc of blood from the port – flush with saline – never advance the heparin into the patient. • Call Pt’s nephrologist before using the catheter • Obviously, in a code situation aspirate 10 cc’s and use the line!
 Peritoneal Dialysis • Peritoneal dialysis uses the peritoneum – has many tiny holes and acts as a filter – allows waste products and fluid from the blood to pass through it – holes are too small to allow large molecules to pass through • blood and dialysate will never mix
Peritoneal Dialysis • Peritoneal dialysis uses the peritoneum – has many tiny holes and acts as a filter – allows waste products and fluid from the blood to pass through it – holes are too small to allow large molecules to pass through • blood and dialysate will never mix
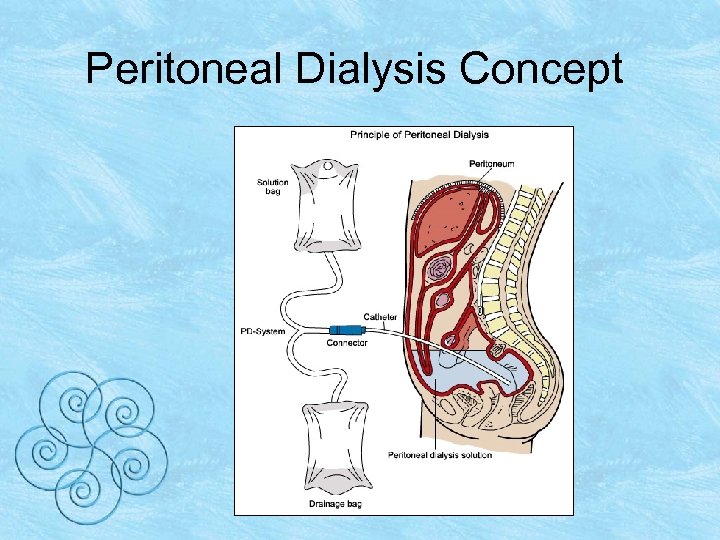 Peritoneal Dialysis Concept
Peritoneal Dialysis Concept
 Peritoneal Dialysis • Do not confuse a PD catheter for a PEG tube • Infusing feedings into a PD catheter can be fatal
Peritoneal Dialysis • Do not confuse a PD catheter for a PEG tube • Infusing feedings into a PD catheter can be fatal
 Pain Meds • HD patients usually require fewer narcotics than other patients • Typically, a patient will have an order for morphine 2 -4 mg q 2 -4 hours • Alternative choices – Dilaudid – Fentanyl
Pain Meds • HD patients usually require fewer narcotics than other patients • Typically, a patient will have an order for morphine 2 -4 mg q 2 -4 hours • Alternative choices – Dilaudid – Fentanyl
 Pain Meds • If the dose is inadequate, you can always give more. • Giving more narcotics is always easier than treating with a narcan drip and pressors • Avoid demerol if possible – its metabolite normeperidine can cause seizures if it accumulates
Pain Meds • If the dose is inadequate, you can always give more. • Giving more narcotics is always easier than treating with a narcan drip and pressors • Avoid demerol if possible – its metabolite normeperidine can cause seizures if it accumulates
 Pain Meds • If a patient has residual renal function, try to avoid NSAID’s • Remember that overdosing NSAIDS can lead to salicylate toxicity • Pts present with tinnitus, headache, nausea, and fever • HD patients have a narrow therapeutic range and develop salicylism with less drug
Pain Meds • If a patient has residual renal function, try to avoid NSAID’s • Remember that overdosing NSAIDS can lead to salicylate toxicity • Pts present with tinnitus, headache, nausea, and fever • HD patients have a narrow therapeutic range and develop salicylism with less drug
 Diabetics • As kidney function declines and ceases, insulin is not cleared as quickly. • The insulin and oral agent’s effects last longer – Sulfonylureas – Avoid Metformin once GFR is less than 40 ml/min
Diabetics • As kidney function declines and ceases, insulin is not cleared as quickly. • The insulin and oral agent’s effects last longer – Sulfonylureas – Avoid Metformin once GFR is less than 40 ml/min
 Diabetics • The patient’s response to insulin and oral agents is a marker of getting close to dialysis • Patients think their DM is doing great – needs less insulin to control blood sugars.
Diabetics • The patient’s response to insulin and oral agents is a marker of getting close to dialysis • Patients think their DM is doing great – needs less insulin to control blood sugars.
 Diabetics • What really happens is: • The patient is uremic and loses his appetite • He eats less • The insulin hangs around • Now the blood sugars look great and the patient needed a fistula last month
Diabetics • What really happens is: • The patient is uremic and loses his appetite • He eats less • The insulin hangs around • Now the blood sugars look great and the patient needed a fistula last month
 Hemostasis • Uremic plasma factors lead to abnormal platelet aggregation and adhesion • Dialysis removes these factors • Unfortunately, the dialysis membrane alters the platelet membrane receptors for v. WF and fibrinogen
Hemostasis • Uremic plasma factors lead to abnormal platelet aggregation and adhesion • Dialysis removes these factors • Unfortunately, the dialysis membrane alters the platelet membrane receptors for v. WF and fibrinogen
 Hemostasis • Manifestation of this platelet dysfunction can range from oozing at a venipuncture site to GI hemorrhage • If a patient is bleeding after a simple procedure, start with the simple treatments
Hemostasis • Manifestation of this platelet dysfunction can range from oozing at a venipuncture site to GI hemorrhage • If a patient is bleeding after a simple procedure, start with the simple treatments
 Hemostasis • DDAVP may be used if the bleeding cannot be controlled • Use 0. 3 mg/kg IV over about 20 minutes • DDAVP stimulates release of v. WF – increases GPIIb platelet adhesion factor expression
Hemostasis • DDAVP may be used if the bleeding cannot be controlled • Use 0. 3 mg/kg IV over about 20 minutes • DDAVP stimulates release of v. WF – increases GPIIb platelet adhesion factor expression
 Reminders • When you evaluate a patient keep in mind that HD patients are different • These patients need the same workup for the same complaints • Your differential will be the same • Your treatment may be modified
Reminders • When you evaluate a patient keep in mind that HD patients are different • These patients need the same workup for the same complaints • Your differential will be the same • Your treatment may be modified
 Causes of Outpatient Mortality • Cardiovascular events • GI bleed • Infection
Causes of Outpatient Mortality • Cardiovascular events • GI bleed • Infection
 Inpatient Mortality • Sepsis/Infection • Cardiovascular events • GI bleed
Inpatient Mortality • Sepsis/Infection • Cardiovascular events • GI bleed
 Cardiovascular Risk of Patients with CKD • Treat them as if they have already had their first MI. • Should be on B-Blocker, ASA, Statin, and ACE or ARB. • May need to stop the ACE/ARB as renal function declines • Think about restarting it once they are on dialysis. • Be careful about writing “no ACE/ARB or Contrast” in these pts.
Cardiovascular Risk of Patients with CKD • Treat them as if they have already had their first MI. • Should be on B-Blocker, ASA, Statin, and ACE or ARB. • May need to stop the ACE/ARB as renal function declines • Think about restarting it once they are on dialysis. • Be careful about writing “no ACE/ARB or Contrast” in these pts.
 Hypotenstion • • • Treat the HD patient with IV fluids 0. 9% saline, 250 cc bolus Albumin / Hespan Check for response You have treated the HD patients like the other patients • All you changed was the amount of fluid
Hypotenstion • • • Treat the HD patient with IV fluids 0. 9% saline, 250 cc bolus Albumin / Hespan Check for response You have treated the HD patients like the other patients • All you changed was the amount of fluid
 Meds to Consider • • • Demerol Morphine NSAID’s ACEI / ARBS Glucophage Antibiotics
Meds to Consider • • • Demerol Morphine NSAID’s ACEI / ARBS Glucophage Antibiotics
 Meds to Avoid/Think About • Contrast- IV contrast can be given in dialysis patients • Keep in mind that the osmotic effects of contrast can shift fluid into the intravascular space and cause pulmonary edema
Meds to Avoid/Think About • Contrast- IV contrast can be given in dialysis patients • Keep in mind that the osmotic effects of contrast can shift fluid into the intravascular space and cause pulmonary edema
 Bibliography • Johnson, Comprehensive Clinical Nephrology • Rose, Clinical Physiology of Acid. Base and Electrolyte Disorders • Renal and Urology News, Nov. /Dec. 2004 • http: //www. pharmacyrxworld. com/pro ductimages/ddavp. jpg
Bibliography • Johnson, Comprehensive Clinical Nephrology • Rose, Clinical Physiology of Acid. Base and Electrolyte Disorders • Renal and Urology News, Nov. /Dec. 2004 • http: //www. pharmacyrxworld. com/pro ductimages/ddavp. jpg


