ea0efef2afa39bed478baeb1e7808a26.ppt
- Количество слайдов: 73
 Hospital-Acquired Pneumonia (HAP) & Ventilator-Associated Pneumonia (VAP) Thursday 18 April 2013 Kamal Mergani, MD, FSCCM Internal Medicine & Critical Care Consultant, Clinical Director of ICU department Omdurman military Hospital kamalmergani@gmail. com
Hospital-Acquired Pneumonia (HAP) & Ventilator-Associated Pneumonia (VAP) Thursday 18 April 2013 Kamal Mergani, MD, FSCCM Internal Medicine & Critical Care Consultant, Clinical Director of ICU department Omdurman military Hospital kamalmergani@gmail. com
 Definitions n HAP > 48 hours after admission n VAP > 48– 72 hours after endotracheal intubation n HCAP u hospitalized > 2 days within 90 days of the infection u nursing home or long-term care facility u recent IV antibiotic therapy, chemotherapy, or wound care < 30 days u attended a hospital or hemodialysis clinic Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J Respir Crit Care Med 2005; 171: 388– 416
Definitions n HAP > 48 hours after admission n VAP > 48– 72 hours after endotracheal intubation n HCAP u hospitalized > 2 days within 90 days of the infection u nursing home or long-term care facility u recent IV antibiotic therapy, chemotherapy, or wound care < 30 days u attended a hospital or hemodialysis clinic Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J Respir Crit Care Med 2005; 171: 388– 416
 HAP: Impact Incidence n n n Accounts for ~15% of all nosocomial infections (2 nd most common cause of NI’s after UTI’s) Number of cases per year in US: ~275, 000 Extra days in the hospital: 4 -9 days Average extra days in ICU: 4. 3 days Direct cost (estimated) of excess hospital stay = $1. 5 billion per year
HAP: Impact Incidence n n n Accounts for ~15% of all nosocomial infections (2 nd most common cause of NI’s after UTI’s) Number of cases per year in US: ~275, 000 Extra days in the hospital: 4 -9 days Average extra days in ICU: 4. 3 days Direct cost (estimated) of excess hospital stay = $1. 5 billion per year
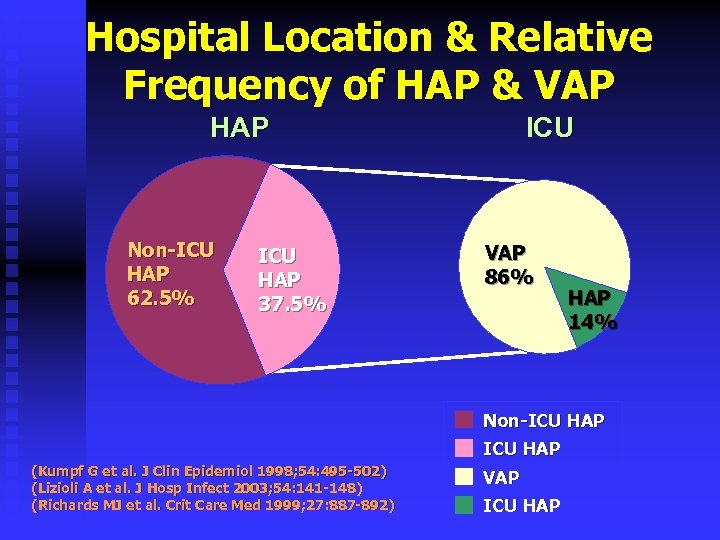 Hospital Location & Relative Frequency of HAP & VAP HAP Non-ICU HAP 62. 5% ICU HAP 37. 5% ICU VAP 86% HAP 14% Non-ICU HAP (Kumpf G et al. J Clin Epidemiol 1998; 54: 495 -502) (Lizioli A et al. J Hosp Infect 2003; 54: 141 -148) (Richards MJ et al. Crit Care Med 1999; 27: 887 -892) VAP ICU HAP
Hospital Location & Relative Frequency of HAP & VAP HAP Non-ICU HAP 62. 5% ICU HAP 37. 5% ICU VAP 86% HAP 14% Non-ICU HAP (Kumpf G et al. J Clin Epidemiol 1998; 54: 495 -502) (Lizioli A et al. J Hosp Infect 2003; 54: 141 -148) (Richards MJ et al. Crit Care Med 1999; 27: 887 -892) VAP ICU HAP
 Risk Factors for HAP & VAP
Risk Factors for HAP & VAP
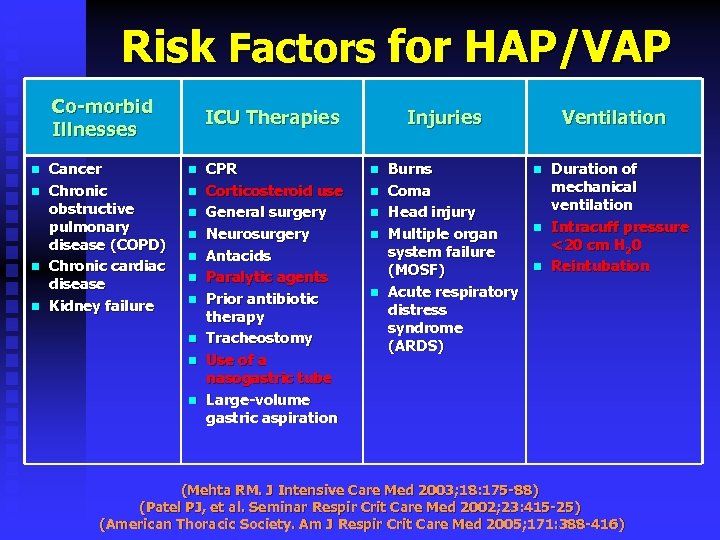 Risk Factors for HAP/VAP Co-morbid Illnesses n n Cancer Chronic obstructive pulmonary disease (COPD) Chronic cardiac disease Kidney failure ICU Therapies n n n n n CPR Corticosteroid use General surgery Neurosurgery Antacids Paralytic agents Prior antibiotic therapy Tracheostomy Use of a nasogastric tube Large-volume gastric aspiration Injuries n n n Burns Coma Head injury Multiple organ system failure (MOSF) Acute respiratory distress syndrome (ARDS) Ventilation n Duration of mechanical ventilation Intracuff pressure <20 cm H 20 Reintubation (Mehta RM. J Intensive Care Med 2003; 18: 175 -88) (Patel PJ, et al. Seminar Respir Crit Care Med 2002; 23: 415 -25) (American Thoracic Society. Am J Respir Crit Care Med 2005; 171: 388 -416)
Risk Factors for HAP/VAP Co-morbid Illnesses n n Cancer Chronic obstructive pulmonary disease (COPD) Chronic cardiac disease Kidney failure ICU Therapies n n n n n CPR Corticosteroid use General surgery Neurosurgery Antacids Paralytic agents Prior antibiotic therapy Tracheostomy Use of a nasogastric tube Large-volume gastric aspiration Injuries n n n Burns Coma Head injury Multiple organ system failure (MOSF) Acute respiratory distress syndrome (ARDS) Ventilation n Duration of mechanical ventilation Intracuff pressure <20 cm H 20 Reintubation (Mehta RM. J Intensive Care Med 2003; 18: 175 -88) (Patel PJ, et al. Seminar Respir Crit Care Med 2002; 23: 415 -25) (American Thoracic Society. Am J Respir Crit Care Med 2005; 171: 388 -416)
 Pathogenesis of HAP/VAP
Pathogenesis of HAP/VAP
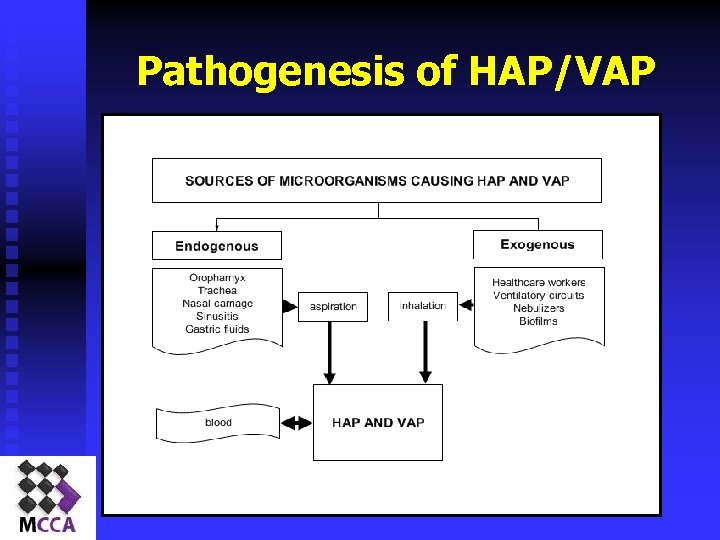 Pathogenesis of HAP/VAP
Pathogenesis of HAP/VAP
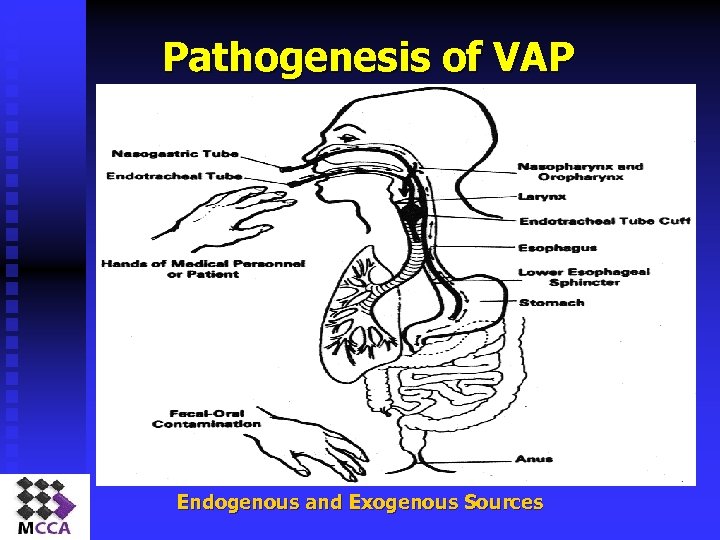 Pathogenesis of VAP Endogenous and Exogenous Sources
Pathogenesis of VAP Endogenous and Exogenous Sources
 Causative Pathogens
Causative Pathogens
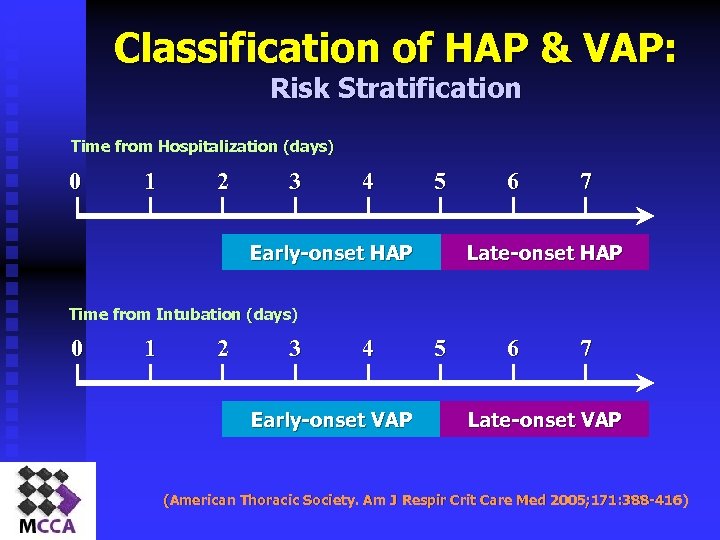 Classification of HAP & VAP: Risk Stratification Time from Hospitalization (days) 0 1 2 3 4 5 Early-onset HAP 6 7 Late-onset HAP Time from Intubation (days) 0 1 2 3 4 Early-onset VAP 5 6 7 Late-onset VAP (American Thoracic Society. Am J Respir Crit Care Med 2005; 171: 388 -416)
Classification of HAP & VAP: Risk Stratification Time from Hospitalization (days) 0 1 2 3 4 5 Early-onset HAP 6 7 Late-onset HAP Time from Intubation (days) 0 1 2 3 4 Early-onset VAP 5 6 7 Late-onset VAP (American Thoracic Society. Am J Respir Crit Care Med 2005; 171: 388 -416)
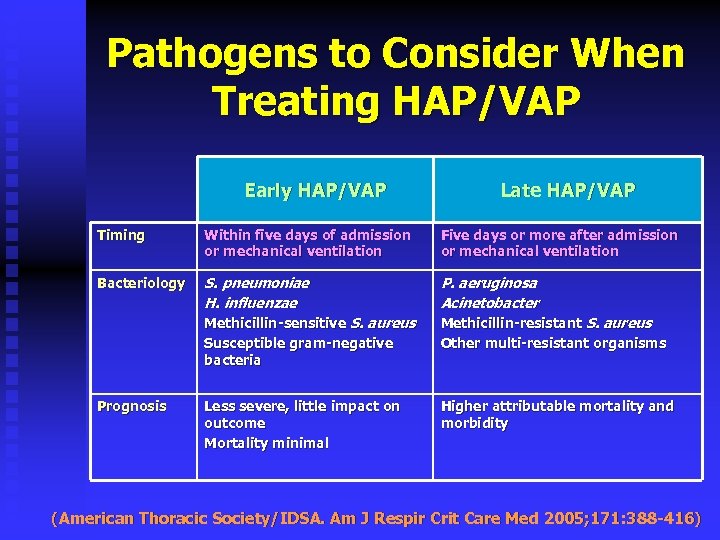 Pathogens to Consider When Treating HAP/VAP Early HAP/VAP Late HAP/VAP Timing Within five days of admission or mechanical ventilation Five days or more after admission or mechanical ventilation Bacteriology S. pneumoniae H. influenzae P. aeruginosa Acinetobacter Methicillin-sensitive S. aureus Susceptible gram-negative bacteria Methicillin-resistant S. aureus Other multi-resistant organisms Less severe, little impact on outcome Mortality minimal Higher attributable mortality and morbidity Prognosis (American Thoracic Society/IDSA. Am J Respir Crit Care Med 2005; 171: 388 -416)
Pathogens to Consider When Treating HAP/VAP Early HAP/VAP Late HAP/VAP Timing Within five days of admission or mechanical ventilation Five days or more after admission or mechanical ventilation Bacteriology S. pneumoniae H. influenzae P. aeruginosa Acinetobacter Methicillin-sensitive S. aureus Susceptible gram-negative bacteria Methicillin-resistant S. aureus Other multi-resistant organisms Less severe, little impact on outcome Mortality minimal Higher attributable mortality and morbidity Prognosis (American Thoracic Society/IDSA. Am J Respir Crit Care Med 2005; 171: 388 -416)
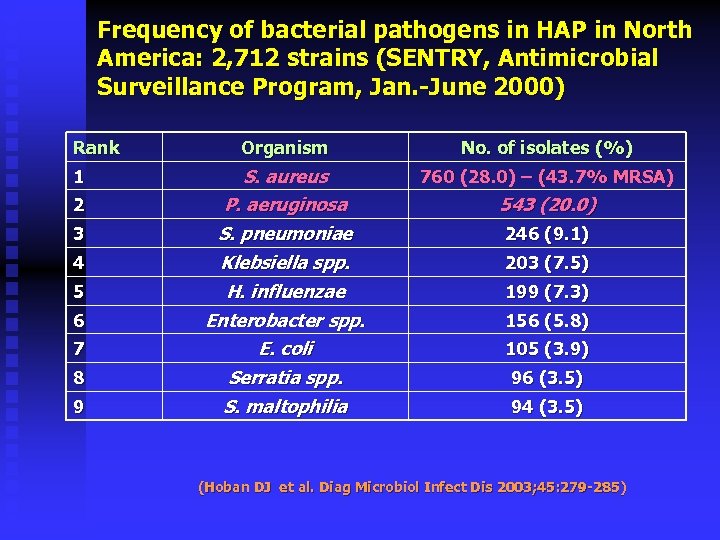 Frequency of bacterial pathogens in HAP in North America: 2, 712 strains (SENTRY, Antimicrobial Surveillance Program, Jan. -June 2000) Rank Organism No. of isolates (%) S. aureus P. aeruginosa 760 (28. 0) – (43. 7% MRSA) S. pneumoniae Klebsiella spp. 246 (9. 1) H. influenzae Enterobacter spp. 199 (7. 3) 105 (3. 9) 8 E. coli Serratia spp. 9 S. maltophilia 94 (3. 5) 1 2 3 4 5 6 7 543 (20. 0) 203 (7. 5) 156 (5. 8) 96 (3. 5) (Hoban DJ et al. Diag Microbiol Infect Dis 2003; 45: 279 -285)
Frequency of bacterial pathogens in HAP in North America: 2, 712 strains (SENTRY, Antimicrobial Surveillance Program, Jan. -June 2000) Rank Organism No. of isolates (%) S. aureus P. aeruginosa 760 (28. 0) – (43. 7% MRSA) S. pneumoniae Klebsiella spp. 246 (9. 1) H. influenzae Enterobacter spp. 199 (7. 3) 105 (3. 9) 8 E. coli Serratia spp. 9 S. maltophilia 94 (3. 5) 1 2 3 4 5 6 7 543 (20. 0) 203 (7. 5) 156 (5. 8) 96 (3. 5) (Hoban DJ et al. Diag Microbiol Infect Dis 2003; 45: 279 -285)
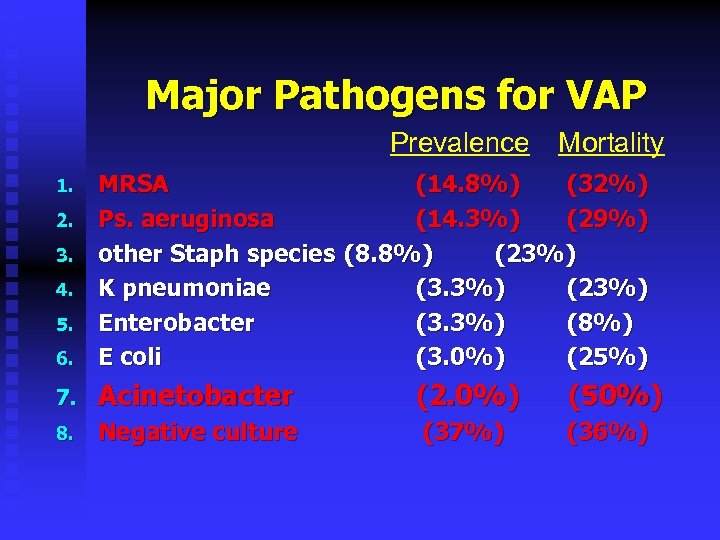 Major Pathogens for VAP Prevalence Mortality 6. MRSA (14. 8%) (32%) Ps. aeruginosa (14. 3%) (29%) other Staph species (8. 8%) (23%) K pneumoniae (3. 3%) (23%) Enterobacter (3. 3%) (8%) E coli (3. 0%) (25%) 7. Acinetobacter (2. 0%) (50%) 8. Negative culture (37%) (36%) 1. 2. 3. 4. 5.
Major Pathogens for VAP Prevalence Mortality 6. MRSA (14. 8%) (32%) Ps. aeruginosa (14. 3%) (29%) other Staph species (8. 8%) (23%) K pneumoniae (3. 3%) (23%) Enterobacter (3. 3%) (8%) E coli (3. 0%) (25%) 7. Acinetobacter (2. 0%) (50%) 8. Negative culture (37%) (36%) 1. 2. 3. 4. 5.

 Diagnosis of HAP/VAP n Clinical approach Vs. n Invasive approach
Diagnosis of HAP/VAP n Clinical approach Vs. n Invasive approach
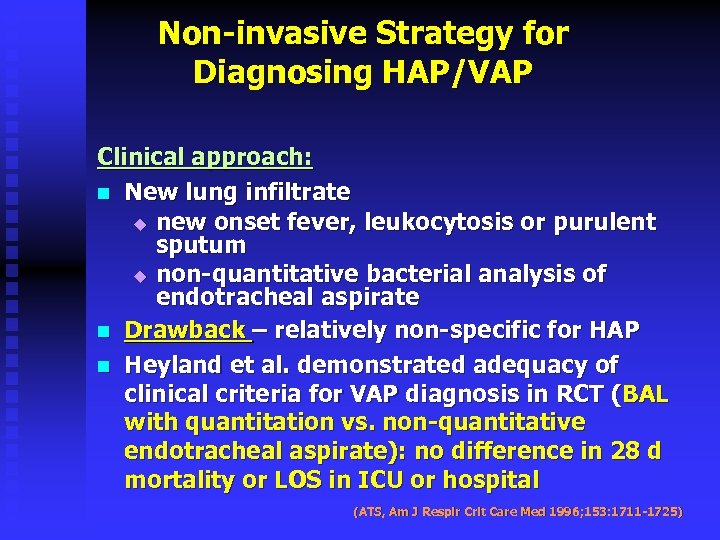 Non-invasive Strategy for Diagnosing HAP/VAP Clinical approach: n New lung infiltrate u new onset fever, leukocytosis or purulent sputum u non-quantitative bacterial analysis of endotracheal aspirate n Drawback – relatively non-specific for HAP n Heyland et al. demonstrated adequacy of clinical criteria for VAP diagnosis in RCT (BAL with quantitation vs. non-quantitative endotracheal aspirate): no difference in 28 d mortality or LOS in ICU or hospital (ATS, Am J Respir Crit Care Med 1996; 153: 1711 -1725)
Non-invasive Strategy for Diagnosing HAP/VAP Clinical approach: n New lung infiltrate u new onset fever, leukocytosis or purulent sputum u non-quantitative bacterial analysis of endotracheal aspirate n Drawback – relatively non-specific for HAP n Heyland et al. demonstrated adequacy of clinical criteria for VAP diagnosis in RCT (BAL with quantitation vs. non-quantitative endotracheal aspirate): no difference in 28 d mortality or LOS in ICU or hospital (ATS, Am J Respir Crit Care Med 1996; 153: 1711 -1725)
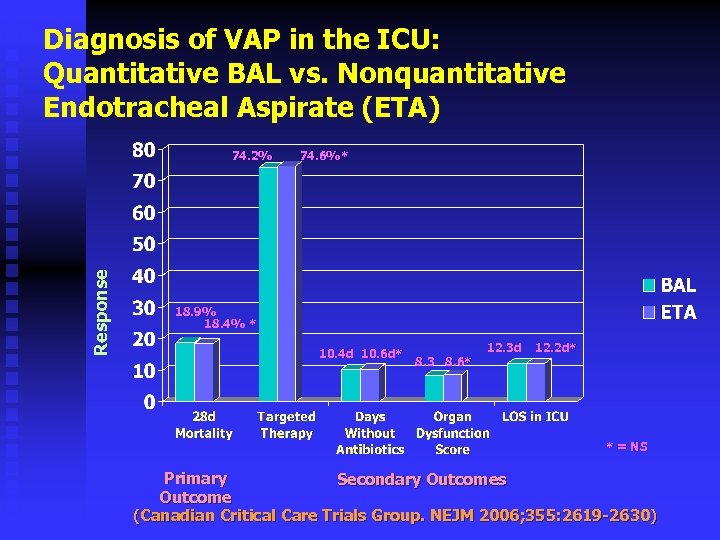 Diagnosis of VAP in the ICU: Quantitative BAL vs. Nonquantitative Endotracheal Aspirate (ETA) Response 74. 2% 74. 6%* 18. 9% 18. 4% * 10. 4 d 10. 6 d* 8. 3 8. 6* 12. 3 d 12. 2 d* * = NS Primary Secondary Outcomes Outcome (Canadian Critical Care Trials Group. NEJM 2006; 355: 2619 -2630)
Diagnosis of VAP in the ICU: Quantitative BAL vs. Nonquantitative Endotracheal Aspirate (ETA) Response 74. 2% 74. 6%* 18. 9% 18. 4% * 10. 4 d 10. 6 d* 8. 3 8. 6* 12. 3 d 12. 2 d* * = NS Primary Secondary Outcomes Outcome (Canadian Critical Care Trials Group. NEJM 2006; 355: 2619 -2630)
 Initial Therapy of HAP/VAP
Initial Therapy of HAP/VAP
 n We have new 2012/2013 septic shock guidlienes
n We have new 2012/2013 septic shock guidlienes
 Kollef MH et al. Chest 2006
Kollef MH et al. Chest 2006
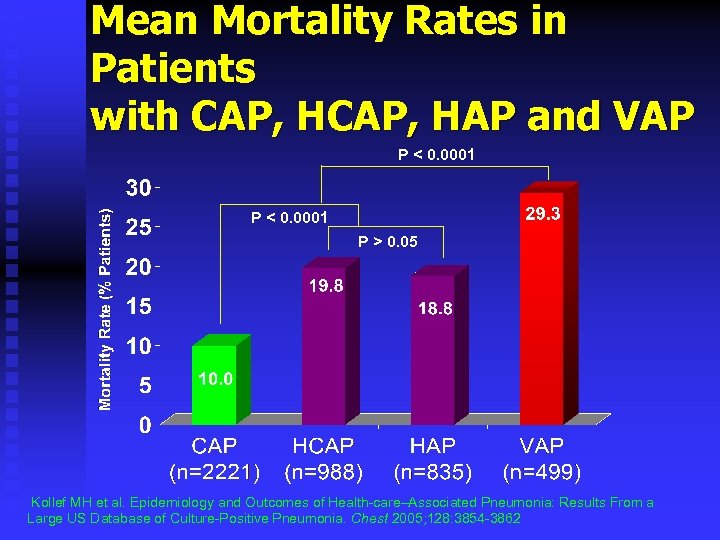 Mean Mortality Rates in Patients with CAP, HAP and VAP P < 0. 0001 P > 0. 05 Kollef MH et al. Epidemiology and Outcomes of Health-care–Associated Pneumonia: Results From a Large US Database of Culture-Positive Pneumonia. Chest 2005; 128: 3854 -3862
Mean Mortality Rates in Patients with CAP, HAP and VAP P < 0. 0001 P > 0. 05 Kollef MH et al. Epidemiology and Outcomes of Health-care–Associated Pneumonia: Results From a Large US Database of Culture-Positive Pneumonia. Chest 2005; 128: 3854 -3862
 How Wrong Is Our Initial Antibiotic Treatment?
How Wrong Is Our Initial Antibiotic Treatment?
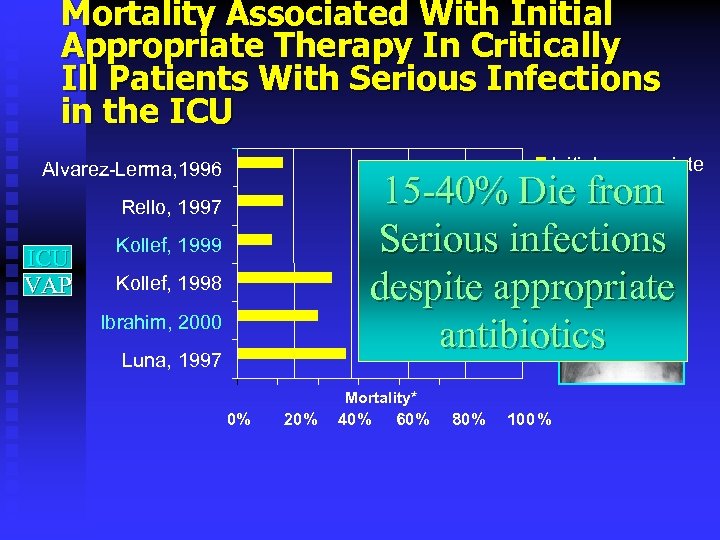 Mortality Associated With Initial Appropriate Therapy In Critically Ill Patients With Serious Infections in the ICU Initial appropriate therapy Alvarez-Lerma, 1996 15 -40% Die from Serious infections despite appropriate antibiotics Rello, 1997 ICU VAP Kollef, 1999 Kollef, 1998 Ibrahim, 2000 Luna, 1997 Mortality* 0% 20% 40% 60% 80% 100%
Mortality Associated With Initial Appropriate Therapy In Critically Ill Patients With Serious Infections in the ICU Initial appropriate therapy Alvarez-Lerma, 1996 15 -40% Die from Serious infections despite appropriate antibiotics Rello, 1997 ICU VAP Kollef, 1999 Kollef, 1998 Ibrahim, 2000 Luna, 1997 Mortality* 0% 20% 40% 60% 80% 100%
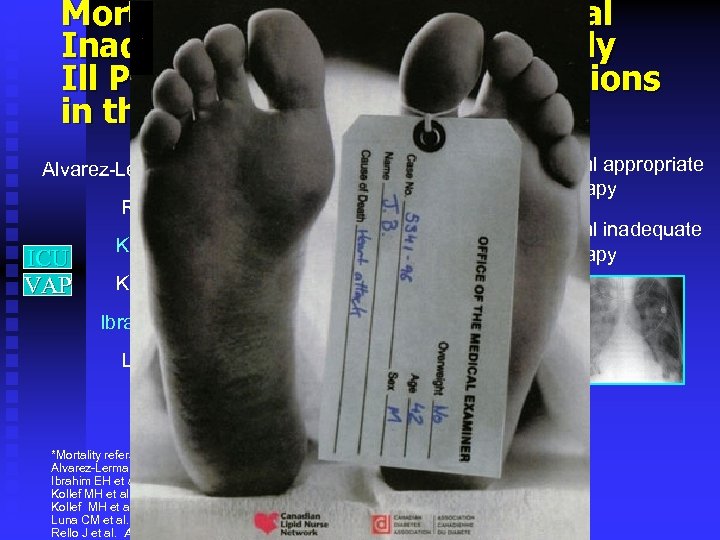 Mortality Associated With Initial Inadequate Therapy In Critically Ill Patients With Serious Infections in the ICU Initial appropriate therapy Alvarez-Lerma, 1996 Rello, 1997 ICU VAP Initial inadequate therapy Kollef, 1999 Kollef, 1998 Ibrahim, 2000 Luna, 1997 Mortality* 0% 20% 40% *Mortality refers to crude or infection-related mortality Alvarez-Lerma F et al. Intensive Care Med 1996; 22: 387 -394. Ibrahim EH et al. Chest 2000; 118 L 146 -155. Kollef MH et al. Chest 1999; 115: 462 -474 Kollef MH et al. Chest 1998; 113: 412 -420. Luna CM et al. Chest 1997; 111: 676 -685. Rello J et al. Am J Resp Crit Care Med 1997; 156: 196 -200. 60% 80% 100%
Mortality Associated With Initial Inadequate Therapy In Critically Ill Patients With Serious Infections in the ICU Initial appropriate therapy Alvarez-Lerma, 1996 Rello, 1997 ICU VAP Initial inadequate therapy Kollef, 1999 Kollef, 1998 Ibrahim, 2000 Luna, 1997 Mortality* 0% 20% 40% *Mortality refers to crude or infection-related mortality Alvarez-Lerma F et al. Intensive Care Med 1996; 22: 387 -394. Ibrahim EH et al. Chest 2000; 118 L 146 -155. Kollef MH et al. Chest 1999; 115: 462 -474 Kollef MH et al. Chest 1998; 113: 412 -420. Luna CM et al. Chest 1997; 111: 676 -685. Rello J et al. Am J Resp Crit Care Med 1997; 156: 196 -200. 60% 80% 100%
 Timing
Timing
 THE Message Time is life Timing
THE Message Time is life Timing
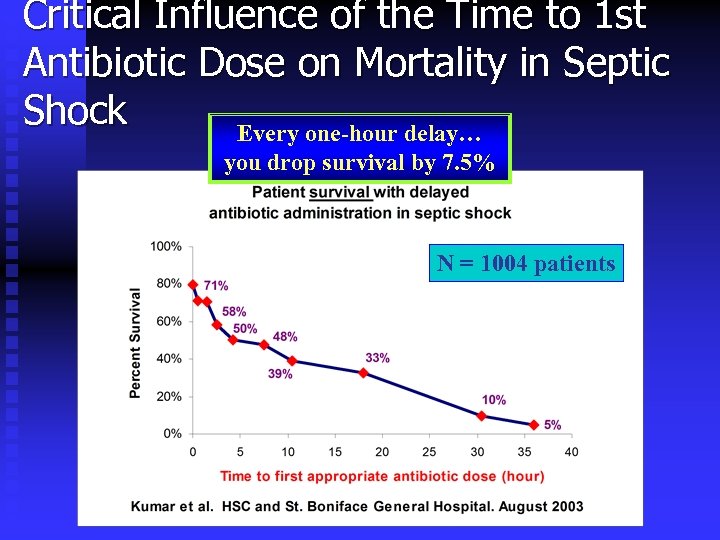 Critical Influence of the Time to 1 st Antibiotic Dose on Mortality in Septic Shock Every one-hour delay… you drop survival by 7. 5% N = 1004 patients
Critical Influence of the Time to 1 st Antibiotic Dose on Mortality in Septic Shock Every one-hour delay… you drop survival by 7. 5% N = 1004 patients
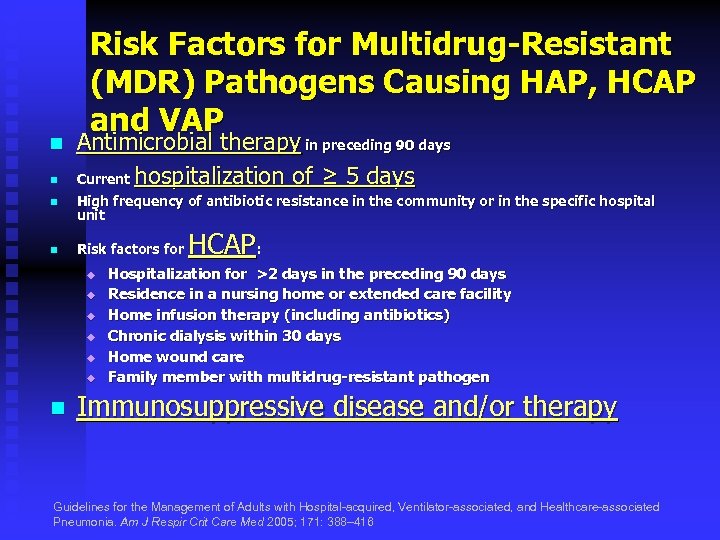 n n Risk Factors for Multidrug-Resistant (MDR) Pathogens Causing HAP, HCAP and VAP Antimicrobial therapy in preceding 90 days Current hospitalization of ≥ 5 days n High frequency of antibiotic resistance in the community or in the specific hospital unit n Risk factors for u u u n HCAP: Hospitalization for >2 days in the preceding 90 days Residence in a nursing home or extended care facility Home infusion therapy (including antibiotics) Chronic dialysis within 30 days Home wound care Family member with multidrug-resistant pathogen Immunosuppressive disease and/or therapy Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J Respir Crit Care Med 2005; 171: 388– 416
n n Risk Factors for Multidrug-Resistant (MDR) Pathogens Causing HAP, HCAP and VAP Antimicrobial therapy in preceding 90 days Current hospitalization of ≥ 5 days n High frequency of antibiotic resistance in the community or in the specific hospital unit n Risk factors for u u u n HCAP: Hospitalization for >2 days in the preceding 90 days Residence in a nursing home or extended care facility Home infusion therapy (including antibiotics) Chronic dialysis within 30 days Home wound care Family member with multidrug-resistant pathogen Immunosuppressive disease and/or therapy Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J Respir Crit Care Med 2005; 171: 388– 416
 n Why Do We Need Combination Therapy? Achieve synergy* n Prevent emergence of resistance** n Better chance to initial appropriate therapy Achieve synergy* * Paul M et al: Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for sepsis in immunocompetent patients: Systematic review and meta-analysis of randomised trials. BMJ 2004; 328: 668 ** Bliziotis IA et al: Effect of aminoglycoside and beta-lactam combination therapy versus beta-lactam monotherapy on the emergence of antimicrobial resistance: A meta-analysis of randomized, controlled trials. Clin Infect Dis 2005; 41: 149
n Why Do We Need Combination Therapy? Achieve synergy* n Prevent emergence of resistance** n Better chance to initial appropriate therapy Achieve synergy* * Paul M et al: Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for sepsis in immunocompetent patients: Systematic review and meta-analysis of randomised trials. BMJ 2004; 328: 668 ** Bliziotis IA et al: Effect of aminoglycoside and beta-lactam combination therapy versus beta-lactam monotherapy on the emergence of antimicrobial resistance: A meta-analysis of randomized, controlled trials. Clin Infect Dis 2005; 41: 149
 Crit Care Med 2007; 35: 1888– 1895
Crit Care Med 2007; 35: 1888– 1895
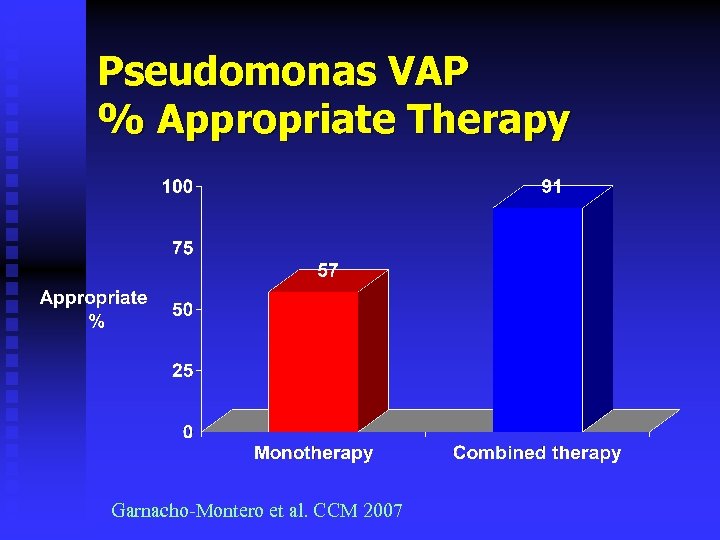 Pseudomonas VAP % Appropriate Therapy Garnacho-Montero et al. CCM 2007
Pseudomonas VAP % Appropriate Therapy Garnacho-Montero et al. CCM 2007
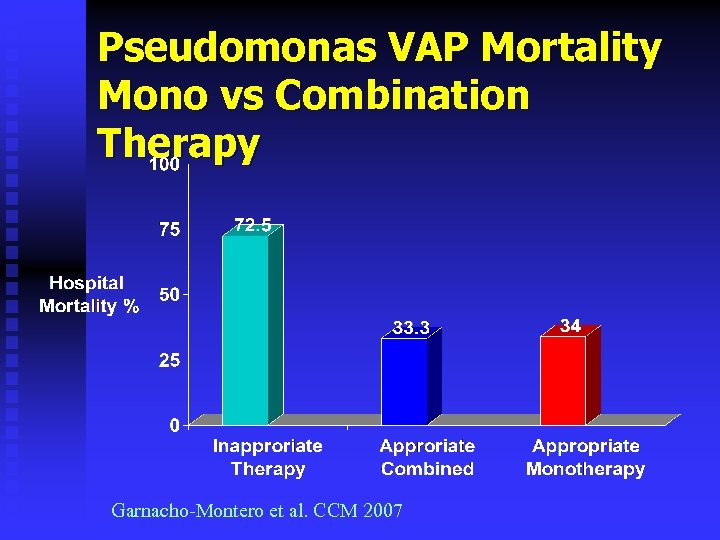 Pseudomonas VAP Mortality Mono vs Combination Therapy Garnacho-Montero et al. CCM 2007
Pseudomonas VAP Mortality Mono vs Combination Therapy Garnacho-Montero et al. CCM 2007
 How Long Should We Treat VAP? 7, 14, 21 days
How Long Should We Treat VAP? 7, 14, 21 days
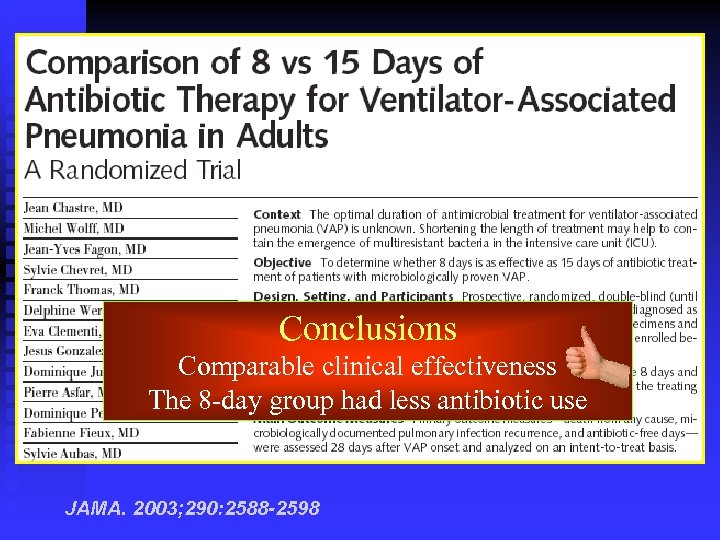 Conclusions Comparable clinical effectiveness The 8 -day group had less antibiotic use JAMA. 2003; 290: 2588 -2598
Conclusions Comparable clinical effectiveness The 8 -day group had less antibiotic use JAMA. 2003; 290: 2588 -2598
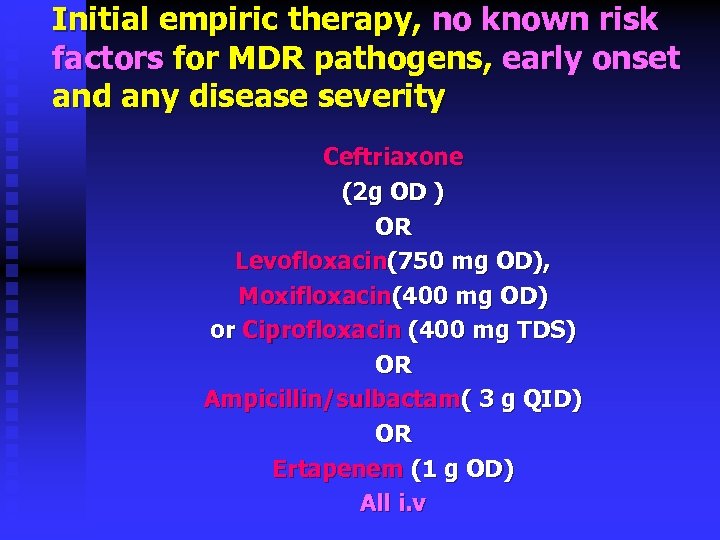 Initial empiric therapy, no known risk factors for MDR pathogens, early onset and any disease severity Ceftriaxone (2 g OD ) OR Levofloxacin(750 mg OD), Moxifloxacin(400 mg OD) or Ciprofloxacin (400 mg TDS) OR Ampicillin/sulbactam( 3 g QID) OR Ertapenem (1 g OD) All i. v
Initial empiric therapy, no known risk factors for MDR pathogens, early onset and any disease severity Ceftriaxone (2 g OD ) OR Levofloxacin(750 mg OD), Moxifloxacin(400 mg OD) or Ciprofloxacin (400 mg TDS) OR Ampicillin/sulbactam( 3 g QID) OR Ertapenem (1 g OD) All i. v
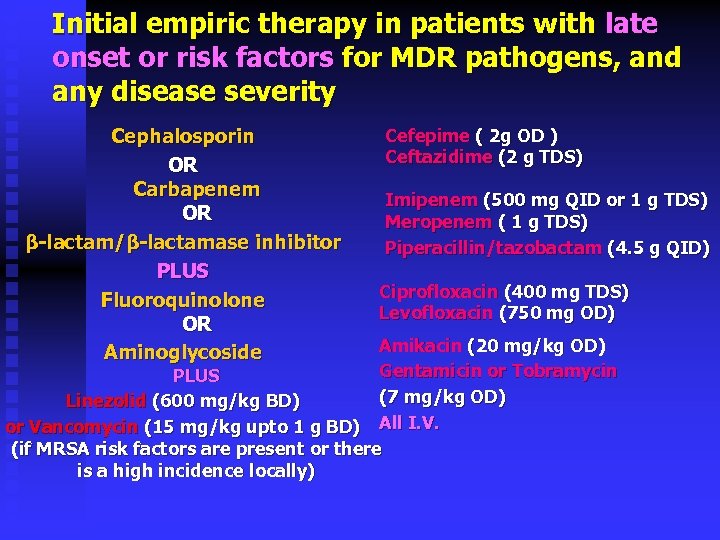 Initial empiric therapy in patients with late onset or risk factors for MDR pathogens, and any disease severity Cephalosporin OR Carbapenem OR β-lactam/β-lactamase inhibitor PLUS Fluoroquinolone OR Aminoglycoside Cefepime ( 2 g OD ) Ceftazidime (2 g TDS) Imipenem (500 mg QID or 1 g TDS) Meropenem ( 1 g TDS) Piperacillin/tazobactam (4. 5 g QID) Ciprofloxacin (400 mg TDS) Levofloxacin (750 mg OD) Amikacin (20 mg/kg OD) Gentamicin or Tobramycin PLUS (7 mg/kg OD) Linezolid (600 mg/kg BD) or Vancomycin (15 mg/kg upto 1 g BD) All I. V. (if MRSA risk factors are present or there is a high incidence locally)
Initial empiric therapy in patients with late onset or risk factors for MDR pathogens, and any disease severity Cephalosporin OR Carbapenem OR β-lactam/β-lactamase inhibitor PLUS Fluoroquinolone OR Aminoglycoside Cefepime ( 2 g OD ) Ceftazidime (2 g TDS) Imipenem (500 mg QID or 1 g TDS) Meropenem ( 1 g TDS) Piperacillin/tazobactam (4. 5 g QID) Ciprofloxacin (400 mg TDS) Levofloxacin (750 mg OD) Amikacin (20 mg/kg OD) Gentamicin or Tobramycin PLUS (7 mg/kg OD) Linezolid (600 mg/kg BD) or Vancomycin (15 mg/kg upto 1 g BD) All I. V. (if MRSA risk factors are present or there is a high incidence locally)
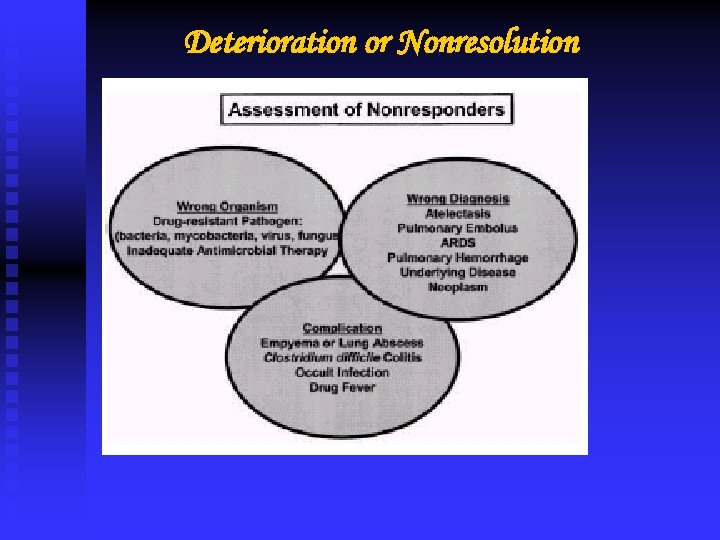 Deterioration or Nonresolution
Deterioration or Nonresolution
 VAP Prevention
VAP Prevention
 HOB Elevation HOB at 30 -45º CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005
HOB Elevation HOB at 30 -45º CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005

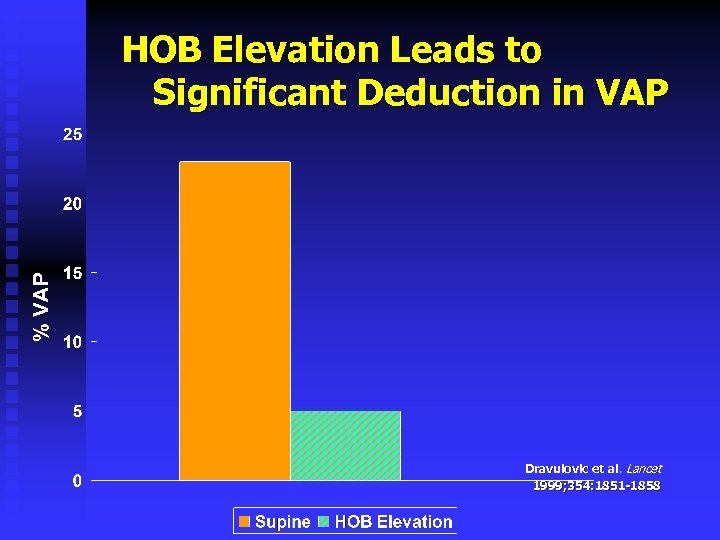 HOB Elevation Leads to Significant Deduction in VAP Dravulovic et al. Lancet 1999; 354: 1851 -1858
HOB Elevation Leads to Significant Deduction in VAP Dravulovic et al. Lancet 1999; 354: 1851 -1858
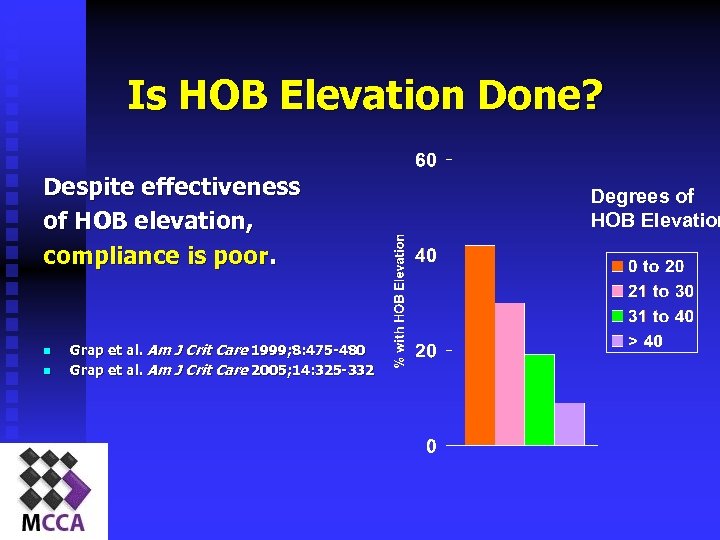 Is HOB Elevation Done? Despite effectiveness of HOB elevation, compliance is poor. n n Grap et al. Am J Crit Care 1999; 8: 475 -480 Grap et al. Am J Crit Care 2005; 14: 325 -332 Degrees of HOB Elevation
Is HOB Elevation Done? Despite effectiveness of HOB elevation, compliance is poor. n n Grap et al. Am J Crit Care 1999; 8: 475 -480 Grap et al. Am J Crit Care 2005; 14: 325 -332 Degrees of HOB Elevation
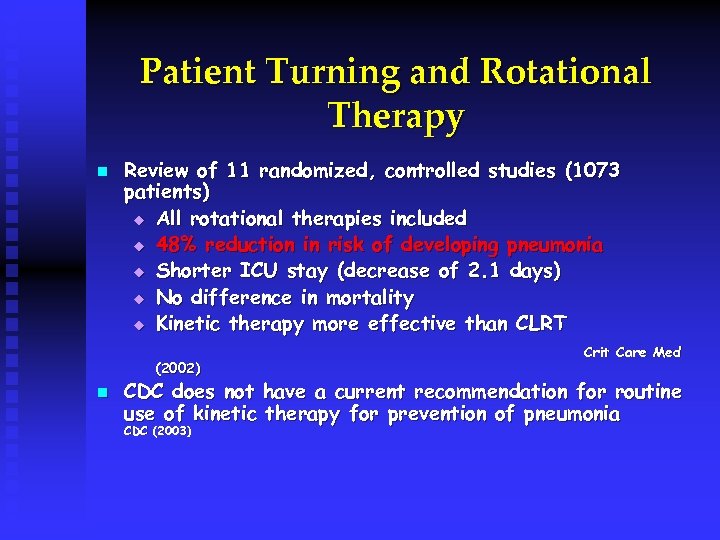 Patient Turning and Rotational Therapy n Review of 11 randomized, controlled studies (1073 patients) u All rotational therapies included u 48% reduction in risk of developing pneumonia u Shorter ICU stay (decrease of 2. 1 days) u No difference in mortality u Kinetic therapy more effective than CLRT (2002) n Crit Care Med CDC does not have a current recommendation for routine use of kinetic therapy for prevention of pneumonia CDC (2003)
Patient Turning and Rotational Therapy n Review of 11 randomized, controlled studies (1073 patients) u All rotational therapies included u 48% reduction in risk of developing pneumonia u Shorter ICU stay (decrease of 2. 1 days) u No difference in mortality u Kinetic therapy more effective than CLRT (2002) n Crit Care Med CDC does not have a current recommendation for routine use of kinetic therapy for prevention of pneumonia CDC (2003)
 Patient Turning… n n Rotational therapy is beneficial for patients at high risk for atelectasis and pneumonia, including patients who are: u sedated and ventilated > 3 – 4 days u difficult to turn u have head injury u in traction When rotational beds are not used, turn at least q 2 hours
Patient Turning… n n Rotational therapy is beneficial for patients at high risk for atelectasis and pneumonia, including patients who are: u sedated and ventilated > 3 – 4 days u difficult to turn u have head injury u in traction When rotational beds are not used, turn at least q 2 hours
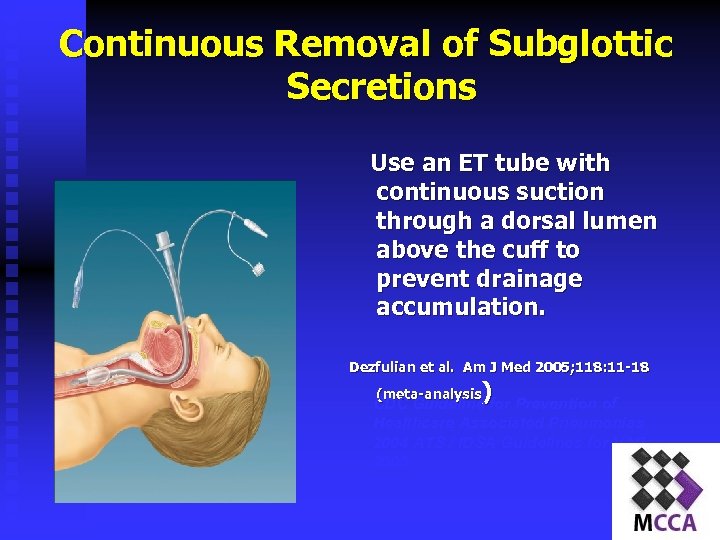 Continuous Removal of Subglottic Secretions Use an ET tube with continuous suction through a dorsal lumen above the cuff to prevent drainage accumulation. Dezfulian et al. Am J Med 2005; 118: 11 -18 ) (meta-analysis CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005
Continuous Removal of Subglottic Secretions Use an ET tube with continuous suction through a dorsal lumen above the cuff to prevent drainage accumulation. Dezfulian et al. Am J Med 2005; 118: 11 -18 ) (meta-analysis CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 ATS / IDSA Guidelines for VAP 2005
 Continuous Removal of Subglottic Secretions n n ET tubes with an additional lumen for the removal of subglottic secretions have been found to decrease VAP in some studies by as much as 20 to 40% Extra cost of the tubes will more than be paid for by the decrease in VAP costs. ) Dezfulian et al. Am J Med 2005; 118: 11 -18 (meta-analysis
Continuous Removal of Subglottic Secretions n n ET tubes with an additional lumen for the removal of subglottic secretions have been found to decrease VAP in some studies by as much as 20 to 40% Extra cost of the tubes will more than be paid for by the decrease in VAP costs. ) Dezfulian et al. Am J Med 2005; 118: 11 -18 (meta-analysis
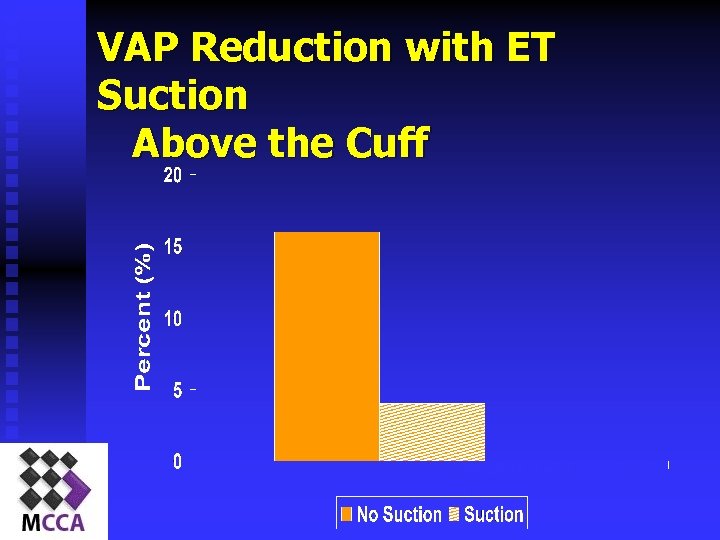 VAP Reduction with ET Suction Above the Cuff Smulders et al. Chest; 121: 858 -862
VAP Reduction with ET Suction Above the Cuff Smulders et al. Chest; 121: 858 -862
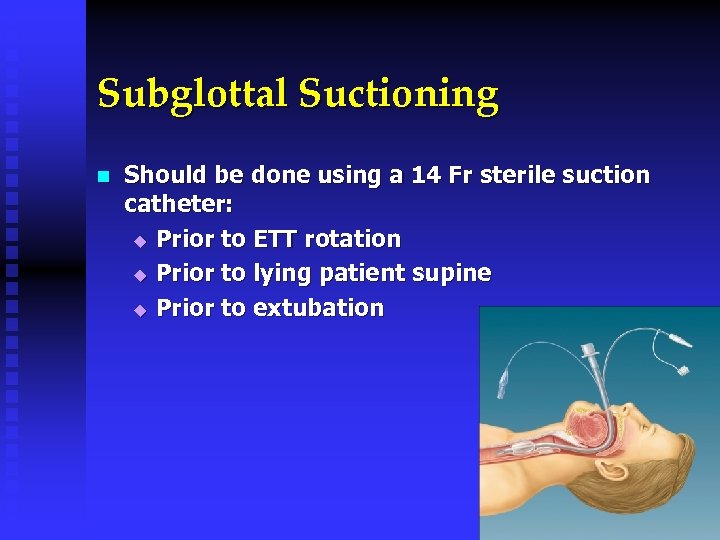 Subglottal Suctioning n Should be done using a 14 Fr sterile suction catheter: u Prior to ETT rotation u Prior to lying patient supine u Prior to extubation
Subglottal Suctioning n Should be done using a 14 Fr sterile suction catheter: u Prior to ETT rotation u Prior to lying patient supine u Prior to extubation
 Suctioning n SET UP n YANKAUER STORAGE
Suctioning n SET UP n YANKAUER STORAGE
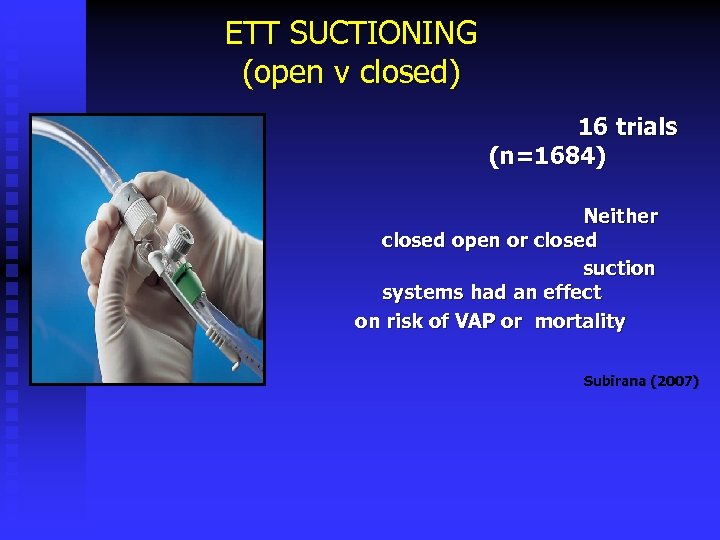 ETT SUCTIONING (open v closed) 16 trials (n=1684) Neither closed open or closed suction systems had an effect on risk of VAP or mortality Subirana (2007)
ETT SUCTIONING (open v closed) 16 trials (n=1684) Neither closed open or closed suction systems had an effect on risk of VAP or mortality Subirana (2007)
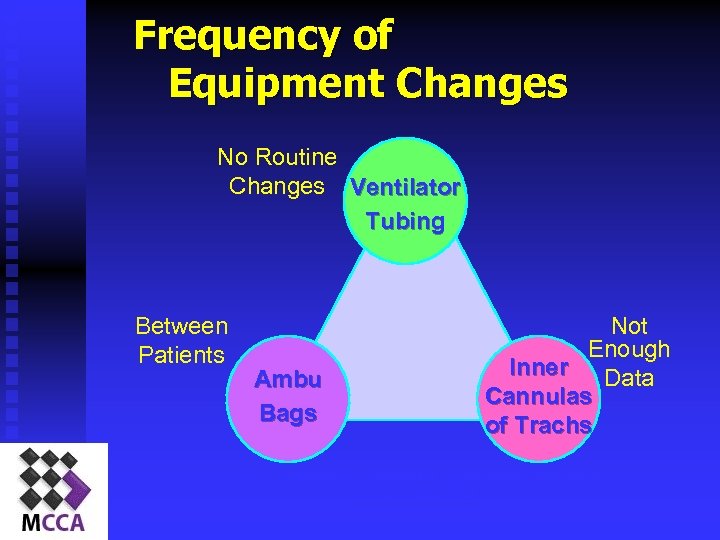 Frequency of Equipment Changes No Routine Changes Ventilator Tubing Between Patients Ambu Bags Not Enough Inner Data Cannulas of Trachs CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004
Frequency of Equipment Changes No Routine Changes Ventilator Tubing Between Patients Ambu Bags Not Enough Inner Data Cannulas of Trachs CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004
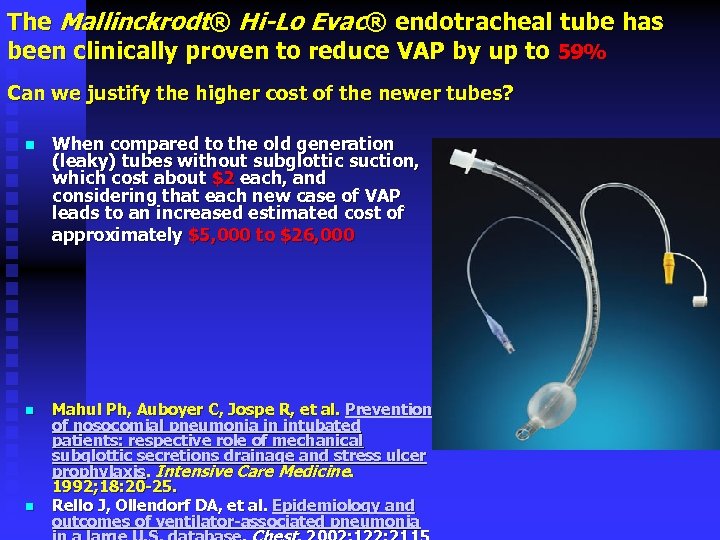 The Mallinckrodt® Hi-Lo Evac® endotracheal tube has been clinically proven to reduce VAP by up to 59% Can we justify the higher cost of the newer tubes? n When compared to the old generation (leaky) tubes without subglottic suction, which cost about $2 each, and considering that each new case of VAP leads to an increased estimated cost of approximately $5, 000 to $26, 000 n Mahul Ph, Auboyer C, Jospe R, et al. Prevention of nosocomial pneumonia in intubated patients: respective role of mechanical subglottic secretions drainage and stress ulcer prophylaxis. Intensive Care Medicine. 1992; 18: 20 -25. Rello J, Ollendorf DA, et al. Epidemiology and outcomes of ventilator-associated pneumonia n
The Mallinckrodt® Hi-Lo Evac® endotracheal tube has been clinically proven to reduce VAP by up to 59% Can we justify the higher cost of the newer tubes? n When compared to the old generation (leaky) tubes without subglottic suction, which cost about $2 each, and considering that each new case of VAP leads to an increased estimated cost of approximately $5, 000 to $26, 000 n Mahul Ph, Auboyer C, Jospe R, et al. Prevention of nosocomial pneumonia in intubated patients: respective role of mechanical subglottic secretions drainage and stress ulcer prophylaxis. Intensive Care Medicine. 1992; 18: 20 -25. Rello J, Ollendorf DA, et al. Epidemiology and outcomes of ventilator-associated pneumonia n
 Handwashing What role does handwashing play in nosocomial pneumonias? Albert, NEJM 1981; Preston, AJM 1981; CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004
Handwashing What role does handwashing play in nosocomial pneumonias? Albert, NEJM 1981; Preston, AJM 1981; CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004
 New CDC guideline recommends frequent use of alcohol-based handrubs n New guideline developed by the Centers for Disease Control and Prevention (CDC) and infection control organizations recommends that healthcare workers use an alcoholbased handrub (a gel, rinse or foam) to routinely clean their hands between patient contacts, as long as hands are not dirty.
New CDC guideline recommends frequent use of alcohol-based handrubs n New guideline developed by the Centers for Disease Control and Prevention (CDC) and infection control organizations recommends that healthcare workers use an alcoholbased handrub (a gel, rinse or foam) to routinely clean their hands between patient contacts, as long as hands are not dirty.
 Oral Care n n n Role of oral care, colonization of the oropharynx, and VAP unclear. Dental plaque may be involved as a reservoir Limited research on impact of rigorous oral care to alter VAP rates n CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 Grap M. Amer J of Critical Care 2003; 12: 113 -119.
Oral Care n n n Role of oral care, colonization of the oropharynx, and VAP unclear. Dental plaque may be involved as a reservoir Limited research on impact of rigorous oral care to alter VAP rates n CDC Guideline for Prevention of Healthcare Associated Pneumonias 2004 Grap M. Amer J of Critical Care 2003; 12: 113 -119.

 Daily Sedation vocation
Daily Sedation vocation
 Daily “Sedation Vacation” and Daily Assessment of Readiness to Wean n n Correlated with reduction in rate of VAP Sedation vacation results in significant reduction in time on mechanical ventilation Duration of mv decreased from 7. 3 days to 4. 9 days-study by Kress et al. NEJM 2000 Weaning is easier when patients are able to assist themselves at extubation with coughing and control of secretions
Daily “Sedation Vacation” and Daily Assessment of Readiness to Wean n n Correlated with reduction in rate of VAP Sedation vacation results in significant reduction in time on mechanical ventilation Duration of mv decreased from 7. 3 days to 4. 9 days-study by Kress et al. NEJM 2000 Weaning is easier when patients are able to assist themselves at extubation with coughing and control of secretions
 HME v HEATED CIRCUITS >20 studies in past twenty years Contradictory but the larger trials show no statistical difference However > 5 days ventilated reduced patency in ETT with HME Jaber et al (2004)
HME v HEATED CIRCUITS >20 studies in past twenty years Contradictory but the larger trials show no statistical difference However > 5 days ventilated reduced patency in ETT with HME Jaber et al (2004)
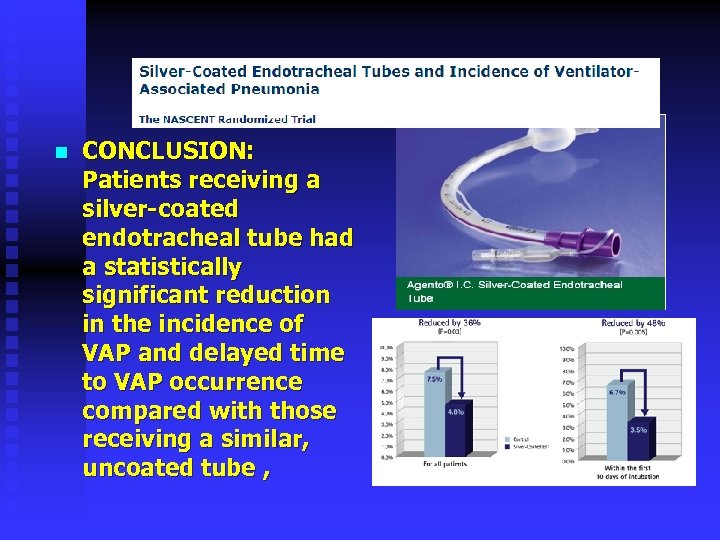 n CONCLUSION: Patients receiving a silver-coated endotracheal tube had a statistically significant reduction in the incidence of VAP and delayed time to VAP occurrence compared with those receiving a similar, uncoated tube ,
n CONCLUSION: Patients receiving a silver-coated endotracheal tube had a statistically significant reduction in the incidence of VAP and delayed time to VAP occurrence compared with those receiving a similar, uncoated tube ,
 n Pedro Caruso, MD, Ph. D; Silvia Denari, Ph. D; Soraia A. L. Ruiz, RT; Sergio E. Demarzo, MD, Ph. D; Daniel Deheinzelin, MD, Ph. D n. Crit Care Med 2009 Vol. 37, No. 1
n Pedro Caruso, MD, Ph. D; Silvia Denari, Ph. D; Soraia A. L. Ruiz, RT; Sergio E. Demarzo, MD, Ph. D; Daniel Deheinzelin, MD, Ph. D n. Crit Care Med 2009 Vol. 37, No. 1
 n The relative risk reduction of VAP in the saline instillation group was ▼ 54% (95% confidence interval [CI] 18%– 74%) and the number needed to treat was 8 (95% CI 5– 27).
n The relative risk reduction of VAP in the saline instillation group was ▼ 54% (95% confidence interval [CI] 18%– 74%) and the number needed to treat was 8 (95% CI 5– 27).
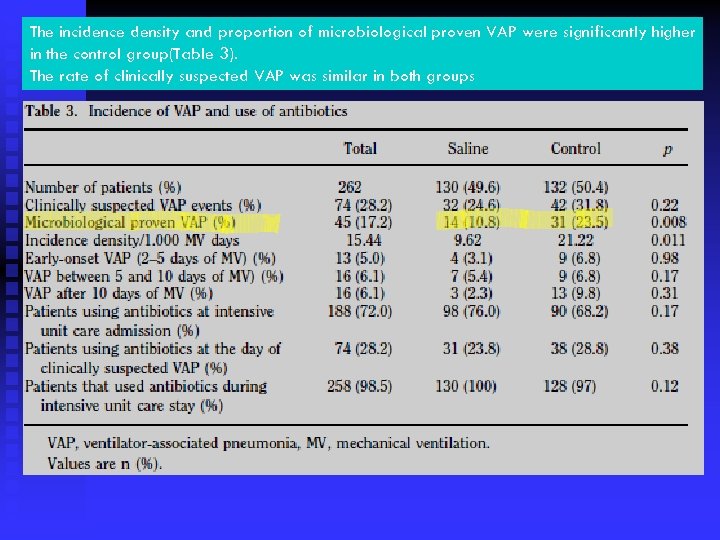 The incidence density and proportion of microbiological proven VAP were significantly higher in the control group(Table 3). The rate of clinically suspected VAP was similar in both groups
The incidence density and proportion of microbiological proven VAP were significantly higher in the control group(Table 3). The rate of clinically suspected VAP was similar in both groups
 PLEASE NOTE ? ? ? You have to teach the nurses again and again , rather than simply putting rules and protocols.
PLEASE NOTE ? ? ? You have to teach the nurses again and again , rather than simply putting rules and protocols.
 EDUCATION PROGRAMMES Demonstrated to reduce incidences of VAP by +/- 50% Apisarnthanarak et al (2007); Zack et al (2002)
EDUCATION PROGRAMMES Demonstrated to reduce incidences of VAP by +/- 50% Apisarnthanarak et al (2007); Zack et al (2002)
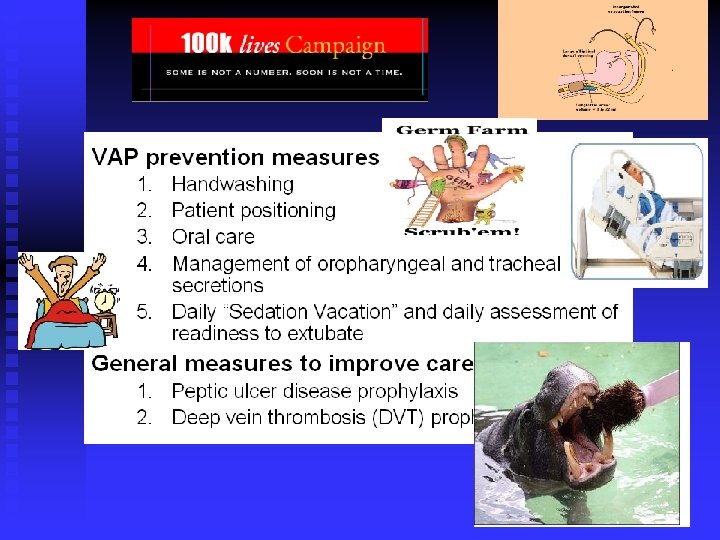 Ventilator Bundle
Ventilator Bundle
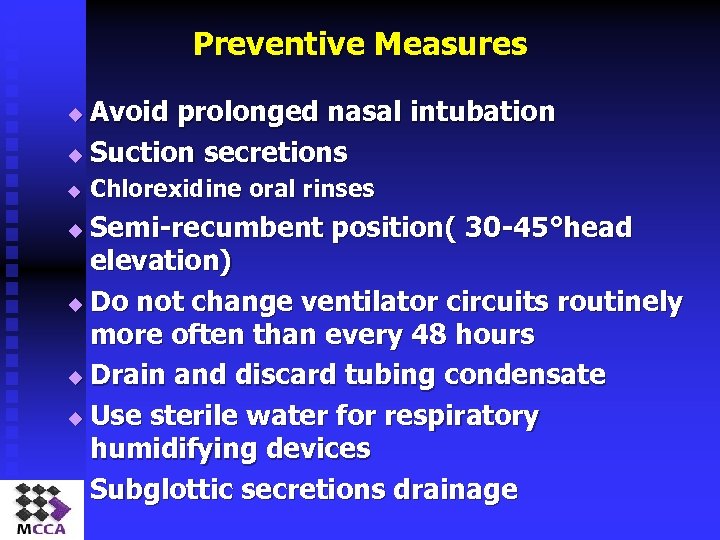 Preventive Measures Avoid prolonged nasal intubation u Suction secretions u u Chlorexidine oral rinses Semi-recumbent position( 30 -45°head elevation) u Do not change ventilator circuits routinely more often than every 48 hours u Drain and discard tubing condensate u Use sterile water for respiratory humidifying devices u Subglottic secretions drainage u
Preventive Measures Avoid prolonged nasal intubation u Suction secretions u u Chlorexidine oral rinses Semi-recumbent position( 30 -45°head elevation) u Do not change ventilator circuits routinely more often than every 48 hours u Drain and discard tubing condensate u Use sterile water for respiratory humidifying devices u Subglottic secretions drainage u
 DEC 2011 MV course
DEC 2011 MV course
 2013 Critical care symposium? ?
2013 Critical care symposium? ?
 THANKS FOR YOUR ATTENTION
THANKS FOR YOUR ATTENTION


