865a92b6f1bdd0f13bc4b67efef7eda1.ppt
- Количество слайдов: 74
 Hospice and Palliative Care: The Quality Imperative Diane E. Meier, MD Professor, Departments of Geriatrics and Medicine Gaisman Professor of Medical Ethics Director, Center to Advance Palliative Care Mount Sinai School of Medicine 04. 26. 06
Hospice and Palliative Care: The Quality Imperative Diane E. Meier, MD Professor, Departments of Geriatrics and Medicine Gaisman Professor of Medical Ethics Director, Center to Advance Palliative Care Mount Sinai School of Medicine 04. 26. 06
 NHPCO and Quality • Vision: A world where individuals and families facing serious illness, death, and grief will experience the best that humankind can offer. • Mission: To lead and mobilize social change for improved care at the end of life. Enabling themes: • Quality: continuous improvement in the quality of hospice and palliative care services, and business practices; • Access: Increasing use of palliative and hospice care and integration of end-of-life care into the health care continuum
NHPCO and Quality • Vision: A world where individuals and families facing serious illness, death, and grief will experience the best that humankind can offer. • Mission: To lead and mobilize social change for improved care at the end of life. Enabling themes: • Quality: continuous improvement in the quality of hospice and palliative care services, and business practices; • Access: Increasing use of palliative and hospice care and integration of end-of-life care into the health care continuum
 National Consensus Project For Quality Palliative Care Going National: Bringing the National Consensus Project for Quality Palliative Care into the Mainstream www. nationalconsensusproject. org
National Consensus Project For Quality Palliative Care Going National: Bringing the National Consensus Project for Quality Palliative Care into the Mainstream www. nationalconsensusproject. org
 NCP Guidelines for Quality Palliative Care In order to achieve a consensus on what we meant by quality palliative care, a partnership of NHPCO, AAHPM, HPNA, CAPC conducted a 2 -year guideline development process including a review of over 2000 citations from the literature, 31 consensus documents and standards, and peer review by a steering committee of 20 professionals and 200 experts in the field. The resulting guidelines, published in 2004, serve as a framework for research, education, QI projects and health policy.
NCP Guidelines for Quality Palliative Care In order to achieve a consensus on what we meant by quality palliative care, a partnership of NHPCO, AAHPM, HPNA, CAPC conducted a 2 -year guideline development process including a review of over 2000 citations from the literature, 31 consensus documents and standards, and peer review by a steering committee of 20 professionals and 200 experts in the field. The resulting guidelines, published in 2004, serve as a framework for research, education, QI projects and health policy.
 NCP Goals 1. Build national consensus concerning the definition, philosophy and principles of palliative care through an open and inclusive process that includes the array of professionals, providers and consumers involved in, and affected by, palliative care. Completed April 2004
NCP Goals 1. Build national consensus concerning the definition, philosophy and principles of palliative care through an open and inclusive process that includes the array of professionals, providers and consumers involved in, and affected by, palliative care. Completed April 2004
 NCP Goals 2. Create voluntary clinical practice guidelines for palliative care that describe the highest quality services to patients and families. Completed April 2004 3. Broadly disseminate the clinical practice guidelines to enable existing and future programs to better define their program organization, resource requirements and performance measures. In Process
NCP Goals 2. Create voluntary clinical practice guidelines for palliative care that describe the highest quality services to patients and families. Completed April 2004 3. Broadly disseminate the clinical practice guidelines to enable existing and future programs to better define their program organization, resource requirements and performance measures. In Process
 NCP Goals 4. Help clinicians provide key elements of palliative care. In process 5. Promote recognition, stable reimbursement structures and accreditation initiatives through projects such as the National Quality Forum (NQF). In process
NCP Goals 4. Help clinicians provide key elements of palliative care. In process 5. Promote recognition, stable reimbursement structures and accreditation initiatives through projects such as the National Quality Forum (NQF). In process
 Formal Approval and Endorsement by Major Organizations • • • Center to Advance Palliative Care National Hospice and Palliative Care Coalition including: American Academy of Hospice and Palliative Medicine, Hospice and Palliative Nurses Association, National Hospice and Palliative Care Organization Academy of Medical-Surgical Nurses American Academy of Ambulatory Care Nursing American Alliance of Cancer Pain Initiatives American Association of Colleges of Nursing American Association of Critical Care Nurses American Association of Neonatal Nurses American Association of Spinal Cord Injury Nurses American Board of Hospice and Palliative Medicine American College of Nurse Practitioners • • • • American Nephrology Nurses' Association American Pain Society American Society for Bioethics and Humanities American Society for Pain Management Nursing American Society of Plastic Surgical Nurses Association of Nurses in AIDS Care Association of Pediatric Oncology Nursing Hospital Corporation of America International Association for Hospice and Palliative Care National Association of Directors of Nursing Administration for Long-Term Care Oncology Nursing Society Sigma Theta Tau (Honorary Nursing Society) Society of Critical Care Medicine List in formation.
Formal Approval and Endorsement by Major Organizations • • • Center to Advance Palliative Care National Hospice and Palliative Care Coalition including: American Academy of Hospice and Palliative Medicine, Hospice and Palliative Nurses Association, National Hospice and Palliative Care Organization Academy of Medical-Surgical Nurses American Academy of Ambulatory Care Nursing American Alliance of Cancer Pain Initiatives American Association of Colleges of Nursing American Association of Critical Care Nurses American Association of Neonatal Nurses American Association of Spinal Cord Injury Nurses American Board of Hospice and Palliative Medicine American College of Nurse Practitioners • • • • American Nephrology Nurses' Association American Pain Society American Society for Bioethics and Humanities American Society for Pain Management Nursing American Society of Plastic Surgical Nurses Association of Nurses in AIDS Care Association of Pediatric Oncology Nursing Hospital Corporation of America International Association for Hospice and Palliative Care National Association of Directors of Nursing Administration for Long-Term Care Oncology Nursing Society Sigma Theta Tau (Honorary Nursing Society) Society of Critical Care Medicine List in formation.
 The National Quality Forum Palliative and Hospice Care Framework • NQF= Voluntary consensus standards-setting organization – public+private support • 5 -step process: consensus standard development; widespread review; member voting and council approval; Board of Directors action; evaluation. • Characterized by openness, balance, due process, consensus, and appeals mechanism. • NQF endorsement has payment and policy implications. • NCP Guidelines developed into an NQF Framework, final vote expected in June 2006.
The National Quality Forum Palliative and Hospice Care Framework • NQF= Voluntary consensus standards-setting organization – public+private support • 5 -step process: consensus standard development; widespread review; member voting and council approval; Board of Directors action; evaluation. • Characterized by openness, balance, due process, consensus, and appeals mechanism. • NQF endorsement has payment and policy implications. • NCP Guidelines developed into an NQF Framework, final vote expected in June 2006.
 Implications of NQF Endorsement • Legitimacy in the eyes of policy makers • Legitimacy and coverage implications for payers • Support for development of actionable measures for QI, benchmarking, and public reporting
Implications of NQF Endorsement • Legitimacy in the eyes of policy makers • Legitimacy and coverage implications for payers • Support for development of actionable measures for QI, benchmarking, and public reporting
 The National Consensus Project for Quality Palliative Care: A Good Beginning • What was needed? Consensus within our field on what quality means. • Who were the partners? NHPCO, AAHPM, HPNA, CAPC • What were the outcomes? www. nationalconsensusproject. org dissemination, endorsement and an NQF Framework This work has positioned us to lead rather than follow in defining and measuring quality.
The National Consensus Project for Quality Palliative Care: A Good Beginning • What was needed? Consensus within our field on what quality means. • Who were the partners? NHPCO, AAHPM, HPNA, CAPC • What were the outcomes? www. nationalconsensusproject. org dissemination, endorsement and an NQF Framework This work has positioned us to lead rather than follow in defining and measuring quality.
 But what is quality? • “I know it when I see it!” • But if patients and families are to have reliably high quality care, there has to be a way to measure it. • How do we measure quality?
But what is quality? • “I know it when I see it!” • But if patients and families are to have reliably high quality care, there has to be a way to measure it. • How do we measure quality?
 Dr. M, an 89 year old practicing psychoanalyst • Admitted to the hospital for scleroderma and progressive kidney failure. • Declined hemodialysis. Palliative care consult called to assess patient’s capacity to refuse dialysis and to assure that she was not suicidal. • Discharged home with hospice on day 5 of hospital stay. • Did well at home for 4 months, remained in active clinical practice. • Said good bye to her patients, her son, and her friends, then died quietly at home 3 days later.
Dr. M, an 89 year old practicing psychoanalyst • Admitted to the hospital for scleroderma and progressive kidney failure. • Declined hemodialysis. Palliative care consult called to assess patient’s capacity to refuse dialysis and to assure that she was not suicidal. • Discharged home with hospice on day 5 of hospital stay. • Did well at home for 4 months, remained in active clinical practice. • Said good bye to her patients, her son, and her friends, then died quietly at home 3 days later.
 Dr. M- a typical patient • She received good hospital palliative care- goals of care assessment and development of a care plan that met her goals, symptom management. • Transitioned effectively to, and received good care from, hospice at home- Meticulous symptom management, psychosocial support from hospice RN, SW, MD to patient and her distressed family and friends. Assured a peaceful dignified death at home. Demonstrates how the palliative care quality continuum works well from the perspective of the patient and family, the providers, and the payers.
Dr. M- a typical patient • She received good hospital palliative care- goals of care assessment and development of a care plan that met her goals, symptom management. • Transitioned effectively to, and received good care from, hospice at home- Meticulous symptom management, psychosocial support from hospice RN, SW, MD to patient and her distressed family and friends. Assured a peaceful dignified death at home. Demonstrates how the palliative care quality continuum works well from the perspective of the patient and family, the providers, and the payers.
 How Quality is Assessed Degree to which health services increase the likelihood of desired health outcomes and are consistent with current professional standards of care. Evaluated on the basis of 3 components: • Structure: (presence of an IDT) • Process: (patient seen by RN, MD, SW +other members of the IDT as indicated) • Outcome: (pain and satisfaction improve as a result)
How Quality is Assessed Degree to which health services increase the likelihood of desired health outcomes and are consistent with current professional standards of care. Evaluated on the basis of 3 components: • Structure: (presence of an IDT) • Process: (patient seen by RN, MD, SW +other members of the IDT as indicated) • Outcome: (pain and satisfaction improve as a result)
 The Link Between Structure, Process, and Outcome • Structure and process measures are most useful as quality indicators if changes in them demonstrably improve patient outcomes. • Outcomes are most useful as quality indicators if they can be linked to specific process or structural measures that, if altered, change the outcome.
The Link Between Structure, Process, and Outcome • Structure and process measures are most useful as quality indicators if changes in them demonstrably improve patient outcomes. • Outcomes are most useful as quality indicators if they can be linked to specific process or structural measures that, if altered, change the outcome.
 The Purpose of Measurement • External Quality Assessment: Payers, regulators want to selectively pay or accredit providers based on their quality and cost effectiveness. Does this palliative care program assess and treat symptoms in a timely manner? • Internal Quality Assessment: Is our hospice effectively identifying and treating shortness of breath?
The Purpose of Measurement • External Quality Assessment: Payers, regulators want to selectively pay or accredit providers based on their quality and cost effectiveness. Does this palliative care program assess and treat symptoms in a timely manner? • Internal Quality Assessment: Is our hospice effectively identifying and treating shortness of breath?
 Definition of Quality in Healthcare In healthcare, defined as care that is: • Patient-centered • Beneficial • Timely • Safe • Equitable • Efficient National Quality Forum www. qualityforum. org Institute for Healthcare Improvement www. ihi. org
Definition of Quality in Healthcare In healthcare, defined as care that is: • Patient-centered • Beneficial • Timely • Safe • Equitable • Efficient National Quality Forum www. qualityforum. org Institute for Healthcare Improvement www. ihi. org
 1. Is Palliative Care Patient and Family-Centered? To answer this question we need to know what persons with serious illness want from our healthcare system.
1. Is Palliative Care Patient and Family-Centered? To answer this question we need to know what persons with serious illness want from our healthcare system.
 Impact of Illness on Family Caregivers 2004 United States estimates: 26 million caregivers deliver care at home to a seriously ill relative ØAverage hours of caregiving per week: 18 ØCost equivalent of uncompensated care: $257 billion (@ $8/hr) Levine C. Loneliness of the long-term caregiver N Engl J Med 1999; 340: 1587 AARP Caregiving in the U. S. 2004 www. caregiving. org Report to Congress: Medicare Payment Policy Medpac; March 2003 www. medpac. gov 90.
Impact of Illness on Family Caregivers 2004 United States estimates: 26 million caregivers deliver care at home to a seriously ill relative ØAverage hours of caregiving per week: 18 ØCost equivalent of uncompensated care: $257 billion (@ $8/hr) Levine C. Loneliness of the long-term caregiver N Engl J Med 1999; 340: 1587 AARP Caregiving in the U. S. 2004 www. caregiving. org Report to Congress: Medicare Payment Policy Medpac; March 2003 www. medpac. gov 90.
 Caregiver Characteristics 900 family caregivers of seriously ill persons at 6 sites across the U. S. • • • Women: 61% Work full time: 60% Close family member: 96% Over age 65: 33% In poor health: 33% Emanuel et al. N Engl J Med 1999; 341: 956. Caregiving in the U. S. 2005 www. caregiving. org
Caregiver Characteristics 900 family caregivers of seriously ill persons at 6 sites across the U. S. • • • Women: 61% Work full time: 60% Close family member: 96% Over age 65: 33% In poor health: 33% Emanuel et al. N Engl J Med 1999; 341: 956. Caregiving in the U. S. 2005 www. caregiving. org
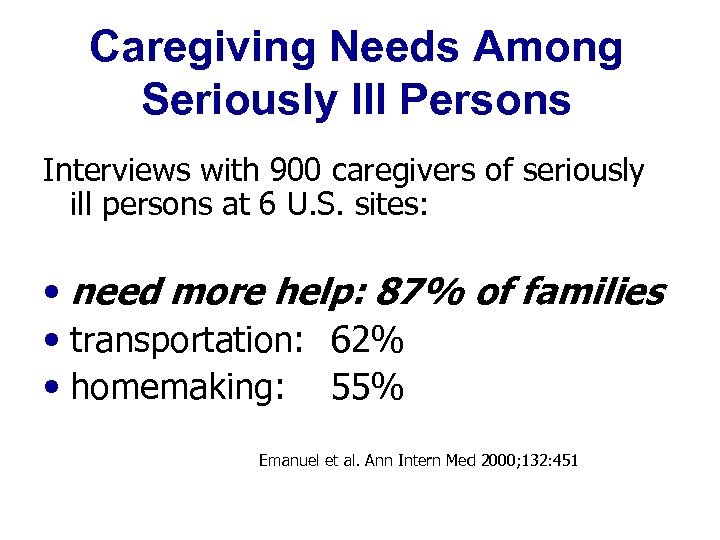 Caregiving Needs Among Seriously Ill Persons Interviews with 900 caregivers of seriously ill persons at 6 U. S. sites: • need more help: 87% of families • transportation: 62% • homemaking: 55% Emanuel et al. Ann Intern Med 2000; 132: 451
Caregiving Needs Among Seriously Ill Persons Interviews with 900 caregivers of seriously ill persons at 6 U. S. sites: • need more help: 87% of families • transportation: 62% • homemaking: 55% Emanuel et al. Ann Intern Med 2000; 132: 451
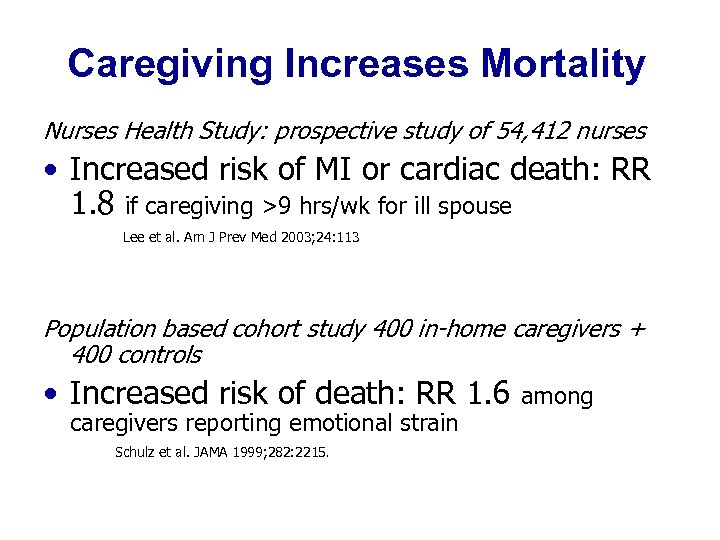 Caregiving Increases Mortality Nurses Health Study: prospective study of 54, 412 nurses • Increased risk of MI or cardiac death: RR 1. 8 if caregiving >9 hrs/wk for ill spouse Lee et al. Am J Prev Med 2003; 24: 113 Population based cohort study 400 in-home caregivers + 400 controls • Increased risk of death: RR 1. 6 among caregivers reporting emotional strain Schulz et al. JAMA 1999; 282: 2215.
Caregiving Increases Mortality Nurses Health Study: prospective study of 54, 412 nurses • Increased risk of MI or cardiac death: RR 1. 8 if caregiving >9 hrs/wk for ill spouse Lee et al. Am J Prev Med 2003; 24: 113 Population based cohort study 400 in-home caregivers + 400 controls • Increased risk of death: RR 1. 6 among caregivers reporting emotional strain Schulz et al. JAMA 1999; 282: 2215.
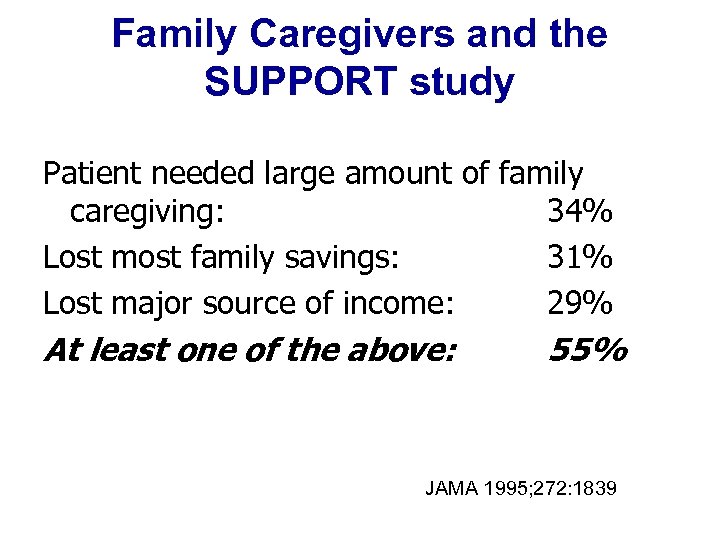 Family Caregivers and the SUPPORT study Patient needed large amount of family caregiving: 34% Lost most family savings: 31% Lost major source of income: 29% At least one of the above: 55% JAMA 1995; 272: 1839
Family Caregivers and the SUPPORT study Patient needed large amount of family caregiving: 34% Lost most family savings: 31% Lost major source of income: 29% At least one of the above: 55% JAMA 1995; 272: 1839
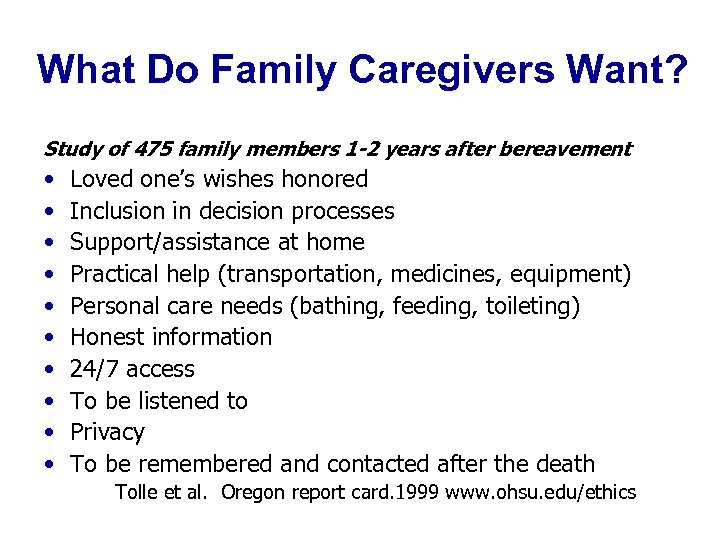 What Do Family Caregivers Want? Study of 475 family members 1 -2 years after bereavement • • • Loved one’s wishes honored Inclusion in decision processes Support/assistance at home Practical help (transportation, medicines, equipment) Personal care needs (bathing, feeding, toileting) Honest information 24/7 access To be listened to Privacy To be remembered and contacted after the death Tolle et al. Oregon report card. 1999 www. ohsu. edu/ethics
What Do Family Caregivers Want? Study of 475 family members 1 -2 years after bereavement • • • Loved one’s wishes honored Inclusion in decision processes Support/assistance at home Practical help (transportation, medicines, equipment) Personal care needs (bathing, feeding, toileting) Honest information 24/7 access To be listened to Privacy To be remembered and contacted after the death Tolle et al. Oregon report card. 1999 www. ohsu. edu/ethics
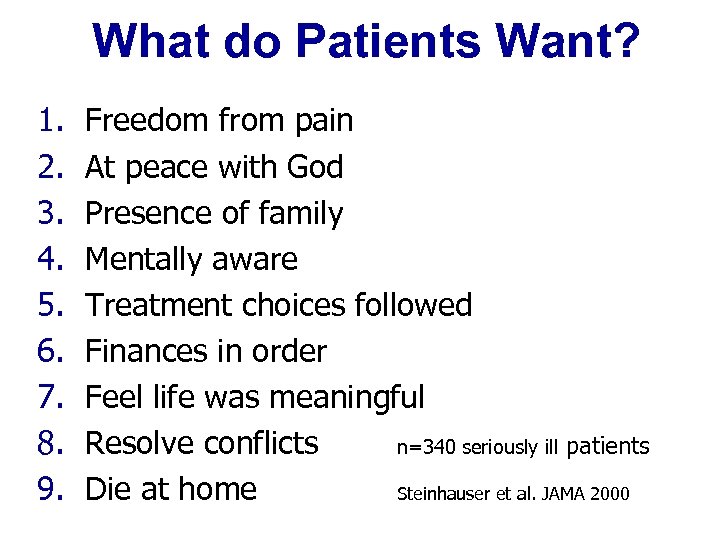 What do Patients Want? 1. 2. 3. 4. 5. 6. 7. 8. 9. Freedom from pain At peace with God Presence of family Mentally aware Treatment choices followed Finances in order Feel life was meaningful Resolve conflicts n=340 seriously ill patients Die at home Steinhauser et al. JAMA 2000
What do Patients Want? 1. 2. 3. 4. 5. 6. 7. 8. 9. Freedom from pain At peace with God Presence of family Mentally aware Treatment choices followed Finances in order Feel life was meaningful Resolve conflicts n=340 seriously ill patients Die at home Steinhauser et al. JAMA 2000
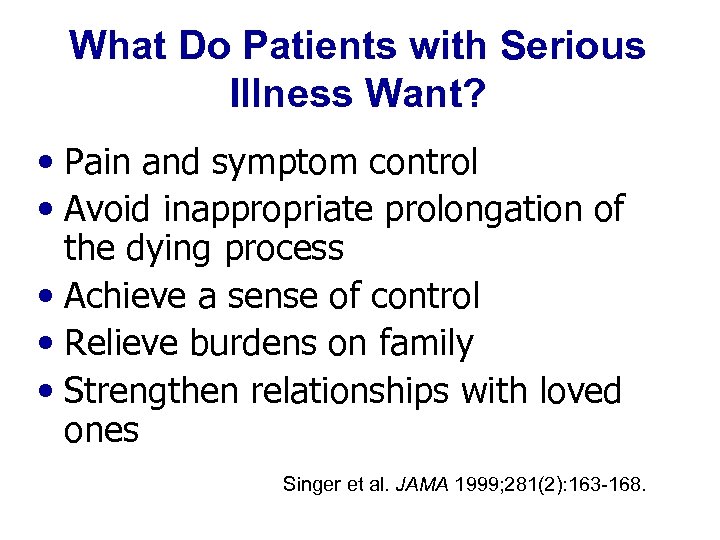 What Do Patients with Serious Illness Want? • Pain and symptom control • Avoid inappropriate prolongation of the dying process • Achieve a sense of control • Relieve burdens on family • Strengthen relationships with loved ones Singer et al. JAMA 1999; 281(2): 163 -168.
What Do Patients with Serious Illness Want? • Pain and symptom control • Avoid inappropriate prolongation of the dying process • Achieve a sense of control • Relieve burdens on family • Strengthen relationships with loved ones Singer et al. JAMA 1999; 281(2): 163 -168.
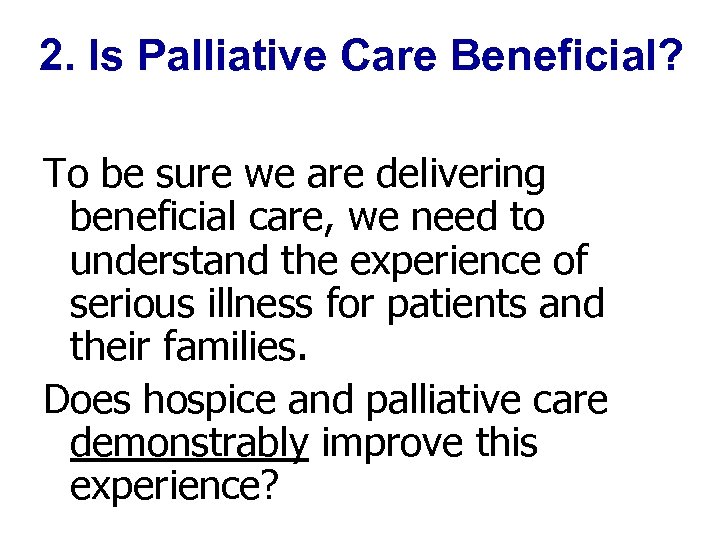 2. Is Palliative Care Beneficial? To be sure we are delivering beneficial care, we need to understand the experience of serious illness for patients and their families. Does hospice and palliative care demonstrably improve this experience?
2. Is Palliative Care Beneficial? To be sure we are delivering beneficial care, we need to understand the experience of serious illness for patients and their families. Does hospice and palliative care demonstrably improve this experience?
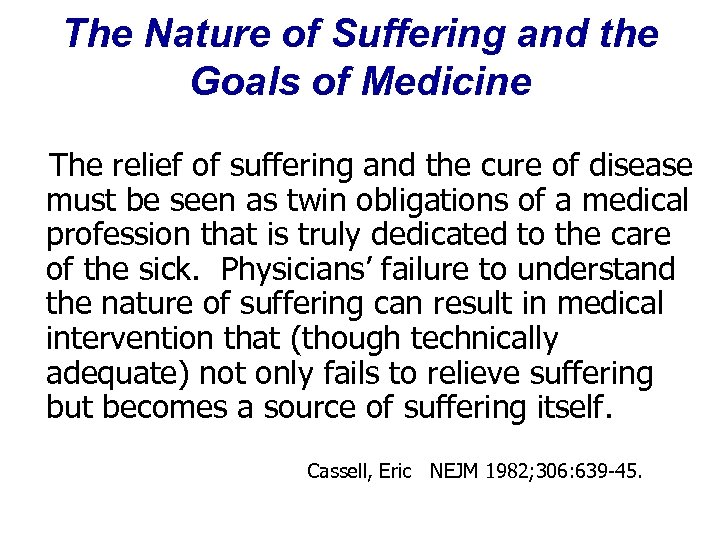 The Nature of Suffering and the Goals of Medicine The relief of suffering and the cure of disease must be seen as twin obligations of a medical profession that is truly dedicated to the care of the sick. Physicians’ failure to understand the nature of suffering can result in medical intervention that (though technically adequate) not only fails to relieve suffering but becomes a source of suffering itself. Cassell, Eric NEJM 1982; 306: 639 -45.
The Nature of Suffering and the Goals of Medicine The relief of suffering and the cure of disease must be seen as twin obligations of a medical profession that is truly dedicated to the care of the sick. Physicians’ failure to understand the nature of suffering can result in medical intervention that (though technically adequate) not only fails to relieve suffering but becomes a source of suffering itself. Cassell, Eric NEJM 1982; 306: 639 -45.
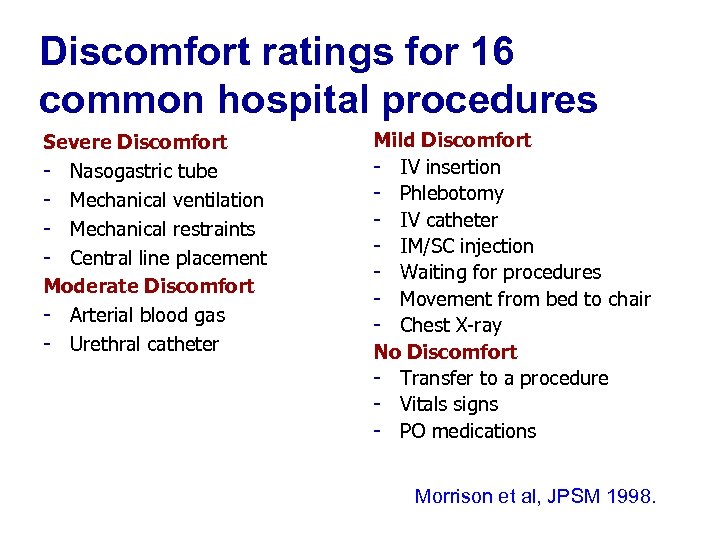 Discomfort ratings for 16 common hospital procedures Severe Discomfort - Nasogastric tube - Mechanical ventilation - Mechanical restraints - Central line placement Moderate Discomfort - Arterial blood gas - Urethral catheter Mild Discomfort - IV insertion - Phlebotomy - IV catheter - IM/SC injection - Waiting for procedures - Movement from bed to chair - Chest X-ray No Discomfort - Transfer to a procedure - Vitals signs - PO medications Morrison et al, JPSM 1998.
Discomfort ratings for 16 common hospital procedures Severe Discomfort - Nasogastric tube - Mechanical ventilation - Mechanical restraints - Central line placement Moderate Discomfort - Arterial blood gas - Urethral catheter Mild Discomfort - IV insertion - Phlebotomy - IV catheter - IM/SC injection - Waiting for procedures - Movement from bed to chair - Chest X-ray No Discomfort - Transfer to a procedure - Vitals signs - PO medications Morrison et al, JPSM 1998.
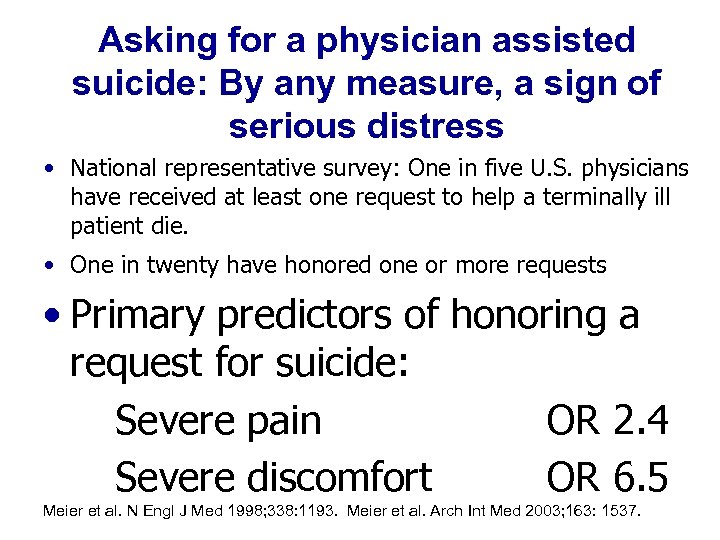 Asking for a physician assisted suicide: By any measure, a sign of serious distress • National representative survey: One in five U. S. physicians have received at least one request to help a terminally ill patient die. • One in twenty have honored one or more requests • Primary predictors of honoring a request for suicide: Severe pain OR 2. 4 Severe discomfort OR 6. 5 Meier et al. N Engl J Med 1998; 338: 1193. Meier et al. Arch Int Med 2003; 163: 1537.
Asking for a physician assisted suicide: By any measure, a sign of serious distress • National representative survey: One in five U. S. physicians have received at least one request to help a terminally ill patient die. • One in twenty have honored one or more requests • Primary predictors of honoring a request for suicide: Severe pain OR 2. 4 Severe discomfort OR 6. 5 Meier et al. N Engl J Med 1998; 338: 1193. Meier et al. Arch Int Med 2003; 163: 1537.
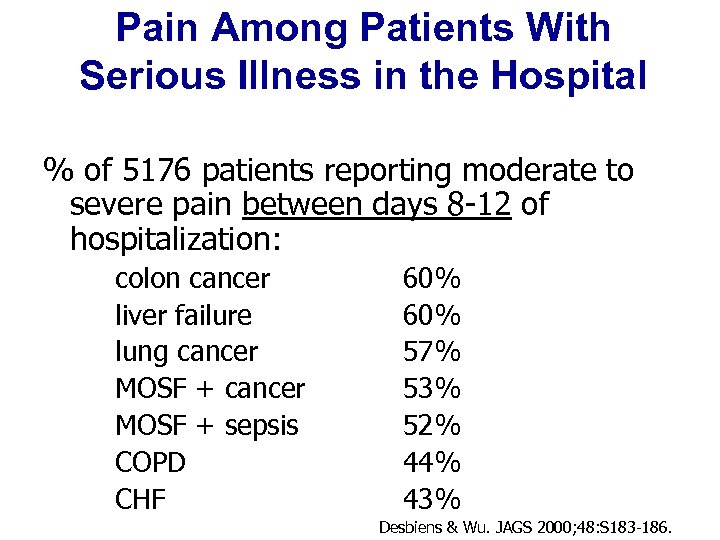 Pain Among Patients With Serious Illness in the Hospital % of 5176 patients reporting moderate to severe pain between days 8 -12 of hospitalization: colon cancer liver failure lung cancer MOSF + sepsis COPD CHF 60% 57% 53% 52% 44% 43% Desbiens & Wu. JAGS 2000; 48: S 183 -186.
Pain Among Patients With Serious Illness in the Hospital % of 5176 patients reporting moderate to severe pain between days 8 -12 of hospitalization: colon cancer liver failure lung cancer MOSF + sepsis COPD CHF 60% 57% 53% 52% 44% 43% Desbiens & Wu. JAGS 2000; 48: S 183 -186.
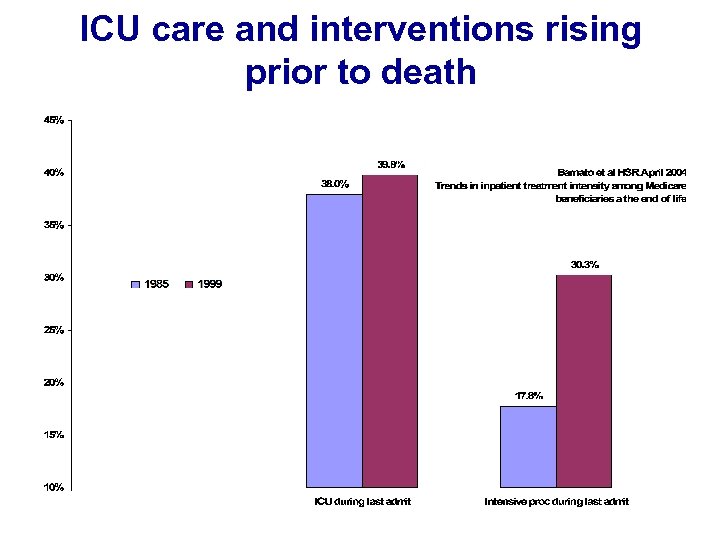 ICU care and interventions rising prior to death
ICU care and interventions rising prior to death
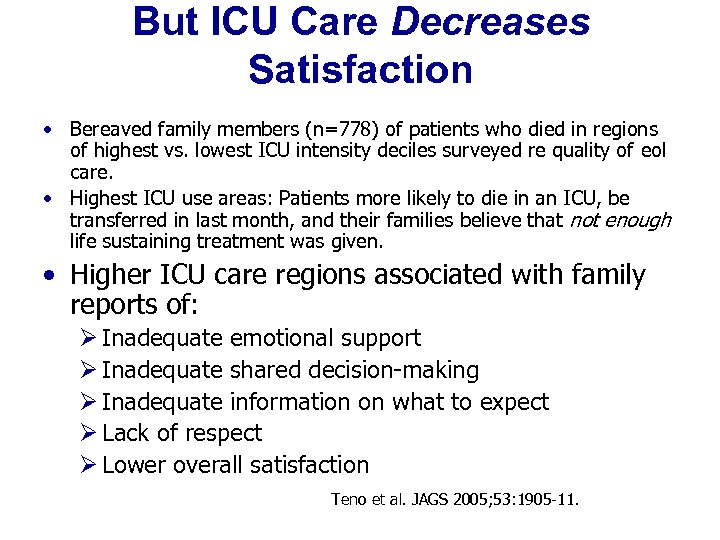 But ICU Care Decreases Satisfaction • Bereaved family members (n=778) of patients who died in regions of highest vs. lowest ICU intensity deciles surveyed re quality of eol care. • Highest ICU use areas: Patients more likely to die in an ICU, be transferred in last month, and their families believe that not enough life sustaining treatment was given. • Higher ICU care regions associated with family reports of: Ø Inadequate emotional support Ø Inadequate shared decision-making Ø Inadequate information on what to expect Ø Lack of respect Ø Lower overall satisfaction Teno et al. JAGS 2005; 53: 1905 -11.
But ICU Care Decreases Satisfaction • Bereaved family members (n=778) of patients who died in regions of highest vs. lowest ICU intensity deciles surveyed re quality of eol care. • Highest ICU use areas: Patients more likely to die in an ICU, be transferred in last month, and their families believe that not enough life sustaining treatment was given. • Higher ICU care regions associated with family reports of: Ø Inadequate emotional support Ø Inadequate shared decision-making Ø Inadequate information on what to expect Ø Lack of respect Ø Lower overall satisfaction Teno et al. JAGS 2005; 53: 1905 -11.

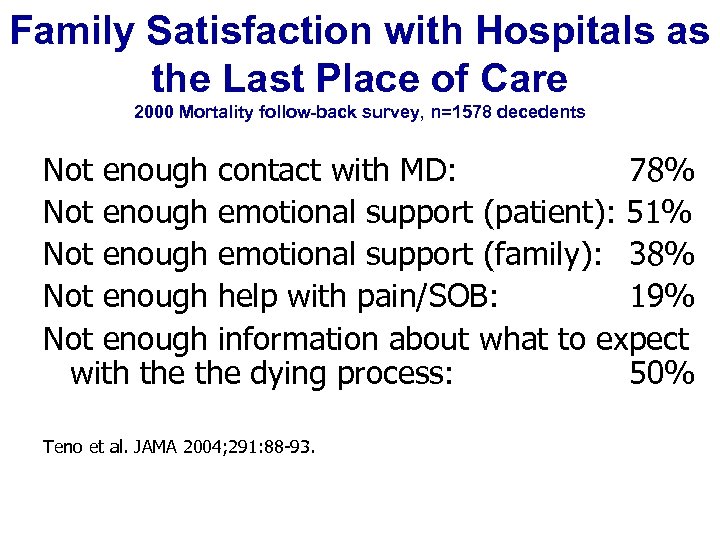 Family Satisfaction with Hospitals as the Last Place of Care 2000 Mortality follow-back survey, n=1578 decedents Not enough contact with MD: 78% Not enough emotional support (patient): 51% Not enough emotional support (family): 38% Not enough help with pain/SOB: 19% Not enough information about what to expect with the dying process: 50% Teno et al. JAMA 2004; 291: 88 -93.
Family Satisfaction with Hospitals as the Last Place of Care 2000 Mortality follow-back survey, n=1578 decedents Not enough contact with MD: 78% Not enough emotional support (patient): 51% Not enough emotional support (family): 38% Not enough help with pain/SOB: 19% Not enough information about what to expect with the dying process: 50% Teno et al. JAMA 2004; 291: 88 -93.
 Are Hospice and Palliative Care Demonstrably Beneficial? The Evidence Base: • Reduction in symptom burden • Improved patient and family satisfaction • Reduced costs
Are Hospice and Palliative Care Demonstrably Beneficial? The Evidence Base: • Reduction in symptom burden • Improved patient and family satisfaction • Reduced costs
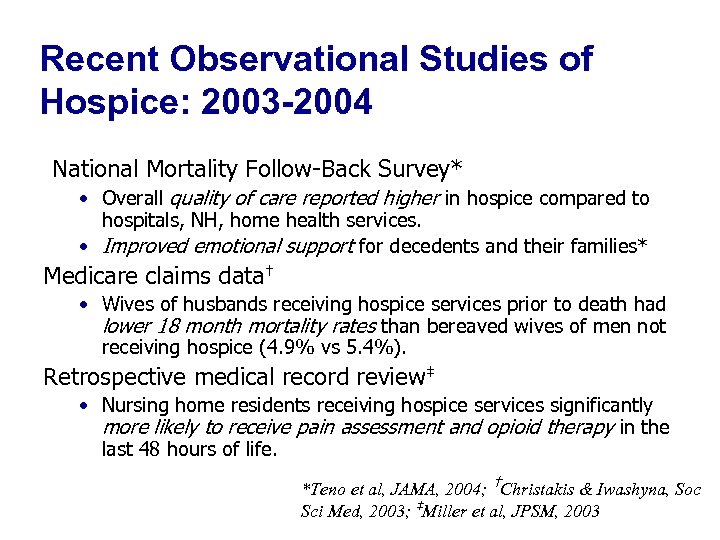 Recent Observational Studies of Hospice: 2003 -2004 National Mortality Follow-Back Survey* • Overall quality of care reported higher in hospice compared to hospitals, NH, home health services. • Improved emotional support for decedents and their families* Medicare claims data† • Wives of husbands receiving hospice services prior to death had lower 18 month mortality rates than bereaved wives of men not receiving hospice (4. 9% vs 5. 4%). Retrospective medical record review‡ • Nursing home residents receiving hospice services significantly more likely to receive pain assessment and opioid therapy in the last 48 hours of life. *Teno et al, JAMA, 2004; †Christakis & Iwashyna, Soc Sci Med, 2003; ‡Miller et al, JPSM, 2003
Recent Observational Studies of Hospice: 2003 -2004 National Mortality Follow-Back Survey* • Overall quality of care reported higher in hospice compared to hospitals, NH, home health services. • Improved emotional support for decedents and their families* Medicare claims data† • Wives of husbands receiving hospice services prior to death had lower 18 month mortality rates than bereaved wives of men not receiving hospice (4. 9% vs 5. 4%). Retrospective medical record review‡ • Nursing home residents receiving hospice services significantly more likely to receive pain assessment and opioid therapy in the last 48 hours of life. *Teno et al, JAMA, 2004; †Christakis & Iwashyna, Soc Sci Med, 2003; ‡Miller et al, JPSM, 2003
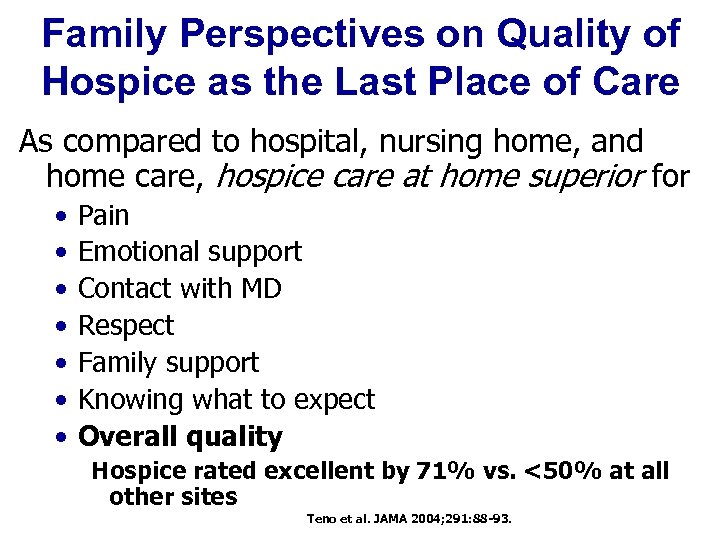 Family Perspectives on Quality of Hospice as the Last Place of Care As compared to hospital, nursing home, and home care, hospice care at home superior for • • Pain Emotional support Contact with MD Respect Family support Knowing what to expect Overall quality Hospice rated excellent by 71% vs. <50% at all other sites Teno et al. JAMA 2004; 291: 88 -93.
Family Perspectives on Quality of Hospice as the Last Place of Care As compared to hospital, nursing home, and home care, hospice care at home superior for • • Pain Emotional support Contact with MD Respect Family support Knowing what to expect Overall quality Hospice rated excellent by 71% vs. <50% at all other sites Teno et al. JAMA 2004; 291: 88 -93.
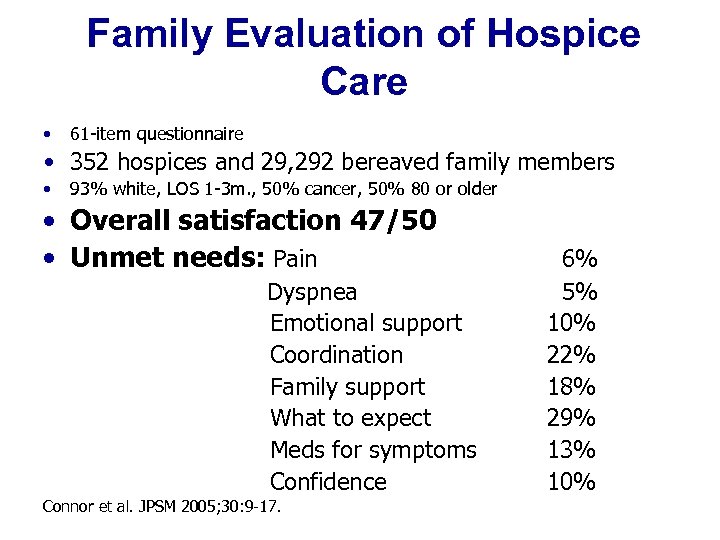 Family Evaluation of Hospice Care • 61 -item questionnaire • 352 hospices and 29, 292 bereaved family members • 93% white, LOS 1 -3 m. , 50% cancer, 50% 80 or older • Overall satisfaction 47/50 • Unmet needs: Pain Dyspnea Emotional support Coordination Family support What to expect Meds for symptoms Confidence Connor et al. JPSM 2005; 30: 9 -17. 6% 5% 10% 22% 18% 29% 13% 10%
Family Evaluation of Hospice Care • 61 -item questionnaire • 352 hospices and 29, 292 bereaved family members • 93% white, LOS 1 -3 m. , 50% cancer, 50% 80 or older • Overall satisfaction 47/50 • Unmet needs: Pain Dyspnea Emotional support Coordination Family support What to expect Meds for symptoms Confidence Connor et al. JPSM 2005; 30: 9 -17. 6% 5% 10% 22% 18% 29% 13% 10%
 State of the Science: U. S. Hospice Programs Results: Higher overall satisfaction, improved family support, + impact on pain management
State of the Science: U. S. Hospice Programs Results: Higher overall satisfaction, improved family support, + impact on pain management
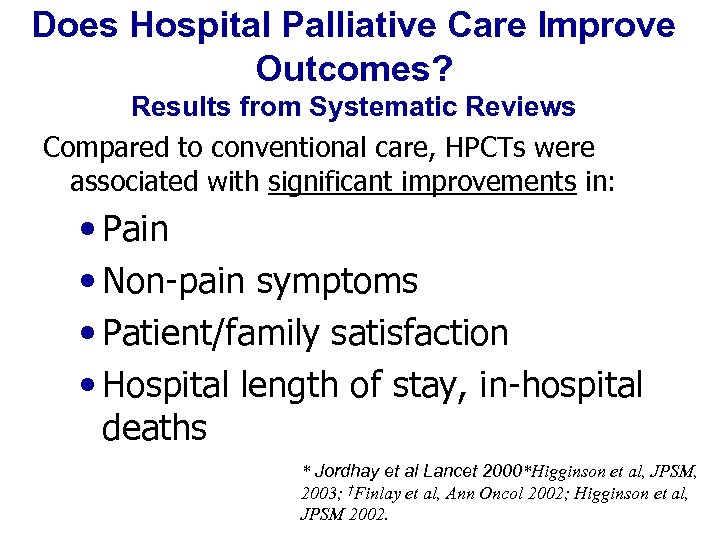 Does Hospital Palliative Care Improve Outcomes? Results from Systematic Reviews Compared to conventional care, HPCTs were associated with significant improvements in: • Pain • Non-pain symptoms • Patient/family satisfaction • Hospital length of stay, in-hospital deaths * Jordhay et al Lancet 2000*Higginson et al, JPSM, 2003; †Finlay et al, Ann Oncol 2002; Higginson et al, JPSM 2002.
Does Hospital Palliative Care Improve Outcomes? Results from Systematic Reviews Compared to conventional care, HPCTs were associated with significant improvements in: • Pain • Non-pain symptoms • Patient/family satisfaction • Hospital length of stay, in-hospital deaths * Jordhay et al Lancet 2000*Higginson et al, JPSM, 2003; †Finlay et al, Ann Oncol 2002; Higginson et al, JPSM 2002.
 Other measures of success “The capacity to give one's attention to a sufferer is a very rare and difficult thing; it is almost a miracle; it is a miracle. ” Simone Weil
Other measures of success “The capacity to give one's attention to a sufferer is a very rare and difficult thing; it is almost a miracle; it is a miracle. ” Simone Weil
 3. Is palliative care timely?
3. Is palliative care timely?
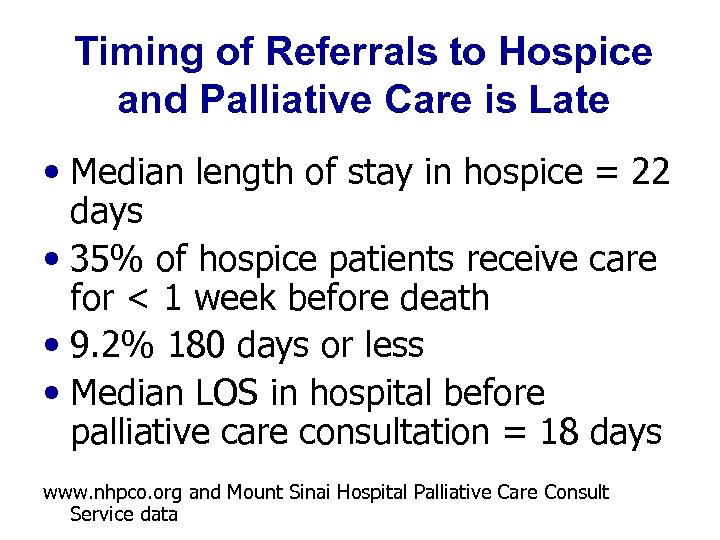 Timing of Referrals to Hospice and Palliative Care is Late • Median length of stay in hospice = 22 days • 35% of hospice patients receive care for < 1 week before death • 9. 2% 180 days or less • Median LOS in hospital before palliative care consultation = 18 days www. nhpco. org and Mount Sinai Hospital Palliative Care Consult Service data
Timing of Referrals to Hospice and Palliative Care is Late • Median length of stay in hospice = 22 days • 35% of hospice patients receive care for < 1 week before death • 9. 2% 180 days or less • Median LOS in hospital before palliative care consultation = 18 days www. nhpco. org and Mount Sinai Hospital Palliative Care Consult Service data
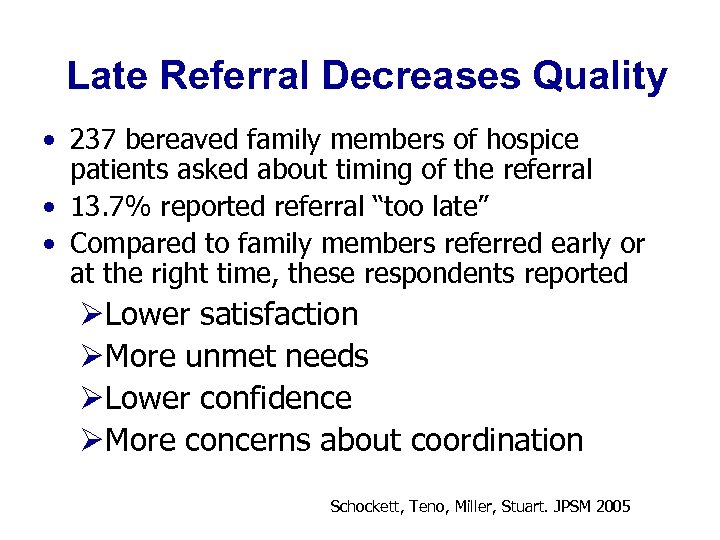 Late Referral Decreases Quality • 237 bereaved family members of hospice patients asked about timing of the referral • 13. 7% reported referral “too late” • Compared to family members referred early or at the right time, these respondents reported ØLower satisfaction ØMore unmet needs ØLower confidence ØMore concerns about coordination Schockett, Teno, Miller, Stuart. JPSM 2005
Late Referral Decreases Quality • 237 bereaved family members of hospice patients asked about timing of the referral • 13. 7% reported referral “too late” • Compared to family members referred early or at the right time, these respondents reported ØLower satisfaction ØMore unmet needs ØLower confidence ØMore concerns about coordination Schockett, Teno, Miller, Stuart. JPSM 2005
 4. Is Hospice and Palliative Care Safe? • No studies of medical error rate associated with palliative and hospice care • Studies do not show any difference in mortality rate or timing of death between palliative/hospice care patients and usual care groups. • Research needed.
4. Is Hospice and Palliative Care Safe? • No studies of medical error rate associated with palliative and hospice care • Studies do not show any difference in mortality rate or timing of death between palliative/hospice care patients and usual care groups. • Research needed.
 5. Is Hospice and Palliative Care Equitable? • Studies suggest that minorities (African. American, Hispanic-Latino, Asian) less likely to receive palliative + hospice care than whites. • Hospice data: 78% white (vs. 75% U. S. ); 8% AA (vs. 12. 3% U. S. ); 6% Hispanic (vs. 12. 5% U. S. ); 2% Asian (vs. 3. 6% U. S. ); 6. 4% multiracial. • No ethnic-racial data on hospital palliative care consult services
5. Is Hospice and Palliative Care Equitable? • Studies suggest that minorities (African. American, Hispanic-Latino, Asian) less likely to receive palliative + hospice care than whites. • Hospice data: 78% white (vs. 75% U. S. ); 8% AA (vs. 12. 3% U. S. ); 6% Hispanic (vs. 12. 5% U. S. ); 2% Asian (vs. 3. 6% U. S. ); 6. 4% multiracial. • No ethnic-racial data on hospital palliative care consult services
 6. Is Palliative-Hospice Care Efficient?
6. Is Palliative-Hospice Care Efficient?
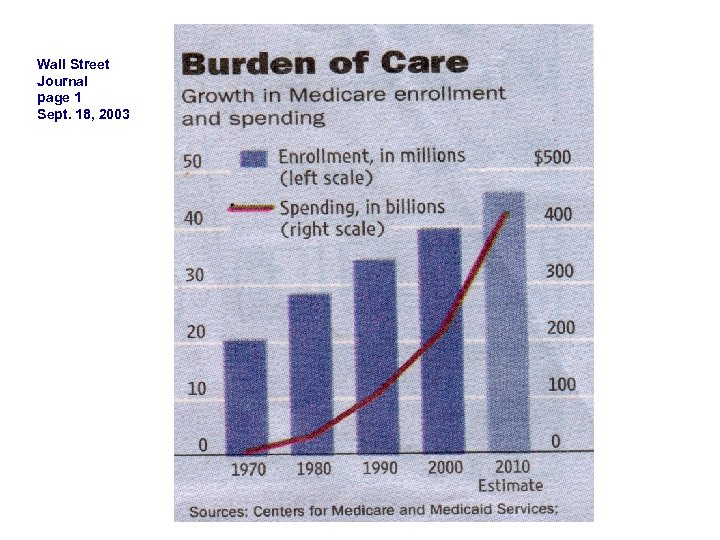 Wall Street Journal page 1 Sept. 18, 2003
Wall Street Journal page 1 Sept. 18, 2003

 Palliative Care Is Cost-Saving, supports transitions to more appropriate care settings • Palliative care lowers costs (for hospitals and payers) by reducing hospital and ICU length of stay, and direct (such as pharmacy) costs. • Palliative care improves continuity between settings and increases hospice/nursing home referral by supporting appropriate transition management. Lilly et al, Am J Med, 2000; Dowdy et al, Crit Care Med, 1998; Carlson et al, JAMA, 1988; Campbell et al, Heart Lung, 1991; Campbell et al, Crit Care Med, 1997; Bruera et al, J Pall Med, 2000; Finn et al, ASCO, 2002; Goldstein et al, Sup Care Cancer, 1996; Advisory Board 2002; Project Safe Conduct 2002, Smeenk et al Pat Educ Couns 2000; Von Gunten JAMA 2002; Schneiderman et al JAMA 2003; Campbell and Guzman, Chest 2003; Smith et al. JPM 2003; Smith, Hillner JCO 2002; www. capc. org; Gilmer et al. Health Affairs 2005. Campbell et al. Ann Int Med. 2004; Health Care Advisory Board. The New Medical Enterprise 2004.
Palliative Care Is Cost-Saving, supports transitions to more appropriate care settings • Palliative care lowers costs (for hospitals and payers) by reducing hospital and ICU length of stay, and direct (such as pharmacy) costs. • Palliative care improves continuity between settings and increases hospice/nursing home referral by supporting appropriate transition management. Lilly et al, Am J Med, 2000; Dowdy et al, Crit Care Med, 1998; Carlson et al, JAMA, 1988; Campbell et al, Heart Lung, 1991; Campbell et al, Crit Care Med, 1997; Bruera et al, J Pall Med, 2000; Finn et al, ASCO, 2002; Goldstein et al, Sup Care Cancer, 1996; Advisory Board 2002; Project Safe Conduct 2002, Smeenk et al Pat Educ Couns 2000; Von Gunten JAMA 2002; Schneiderman et al JAMA 2003; Campbell and Guzman, Chest 2003; Smith et al. JPM 2003; Smith, Hillner JCO 2002; www. capc. org; Gilmer et al. Health Affairs 2005. Campbell et al. Ann Int Med. 2004; Health Care Advisory Board. The New Medical Enterprise 2004.
 How Palliative Care Reduces Hospital Length of Stay and Cost Palliative care: • Clarifies goals of care with patients and families • Helps families to select medical treatments and care settings that meet their goals • Assists with decisions to leave the hospital, or to withhold or withdraw death-prolonging treatments that don’t help to meet their goals
How Palliative Care Reduces Hospital Length of Stay and Cost Palliative care: • Clarifies goals of care with patients and families • Helps families to select medical treatments and care settings that meet their goals • Assists with decisions to leave the hospital, or to withhold or withdraw death-prolonging treatments that don’t help to meet their goals
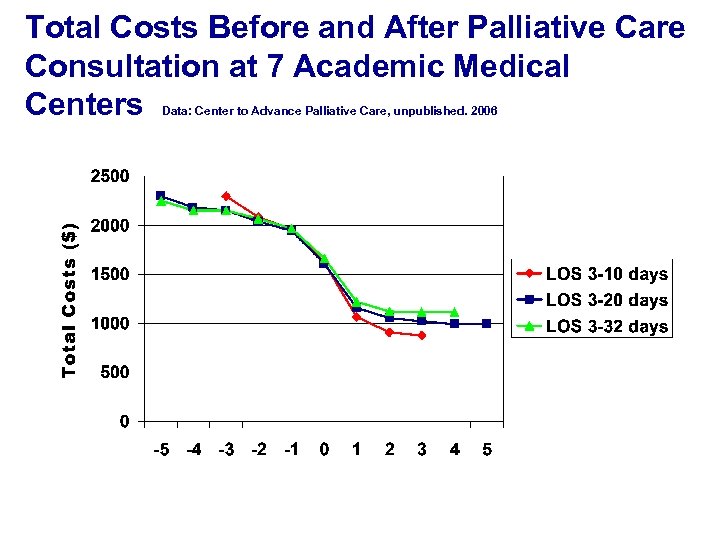 Total Costs Before and After Palliative Care Consultation at 7 Academic Medical Centers Data: Center to Advance Palliative Care, unpublished. 2006
Total Costs Before and After Palliative Care Consultation at 7 Academic Medical Centers Data: Center to Advance Palliative Care, unpublished. 2006
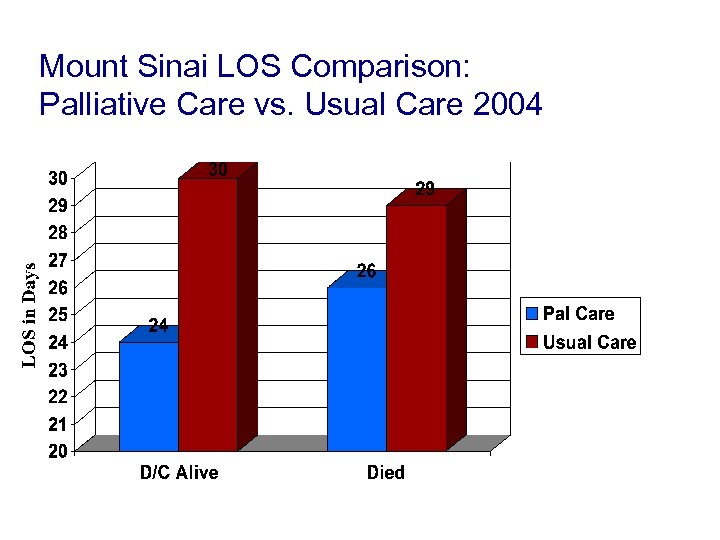 Mount Sinai LOS Comparison: Palliative Care vs. Usual Care 2004
Mount Sinai LOS Comparison: Palliative Care vs. Usual Care 2004
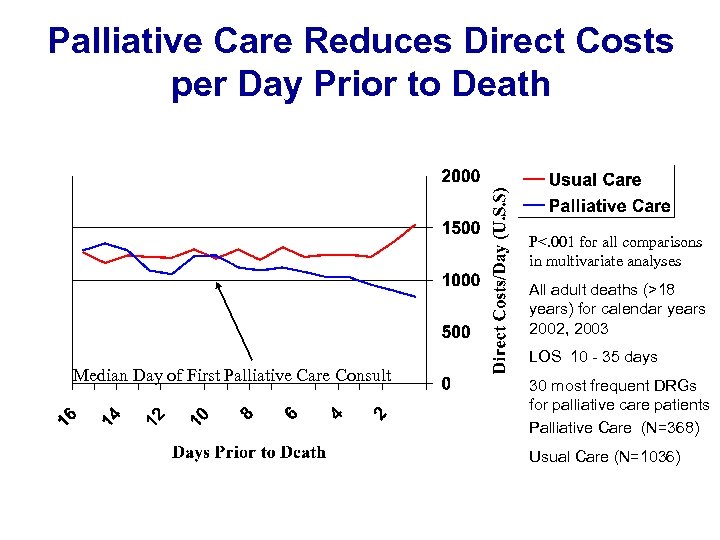 Palliative Care Reduces Direct Costs per Day Prior to Death P<. 001 for all comparisons in multivariate analyses All adult deaths (>18 years) for calendar years 2002, 2003 Median Day of First Palliative Care Consult LOS 10 - 35 days 30 most frequent DRGs for palliative care patients Palliative Care (N=368) Usual Care (N=1036)
Palliative Care Reduces Direct Costs per Day Prior to Death P<. 001 for all comparisons in multivariate analyses All adult deaths (>18 years) for calendar years 2002, 2003 Median Day of First Palliative Care Consult LOS 10 - 35 days 30 most frequent DRGs for palliative care patients Palliative Care (N=368) Usual Care (N=1036)
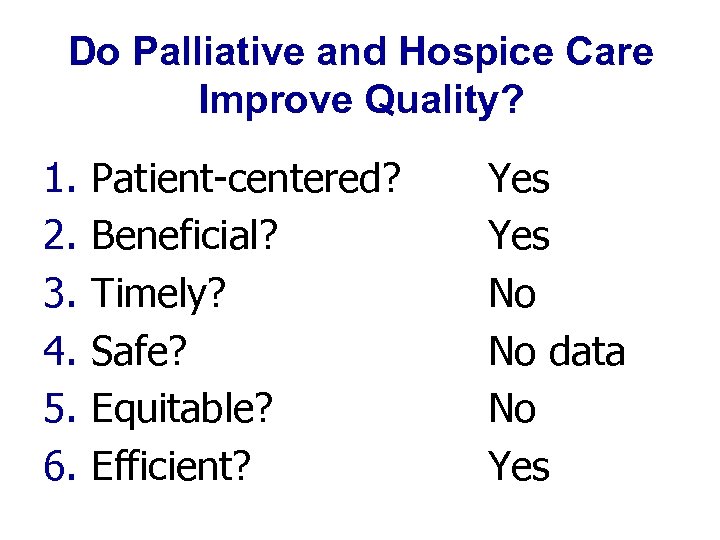 Do Palliative and Hospice Care Improve Quality? 1. 2. 3. 4. 5. 6. Patient-centered? Beneficial? Timely? Safe? Equitable? Efficient? Yes No No data No Yes
Do Palliative and Hospice Care Improve Quality? 1. 2. 3. 4. 5. 6. Patient-centered? Beneficial? Timely? Safe? Equitable? Efficient? Yes No No data No Yes
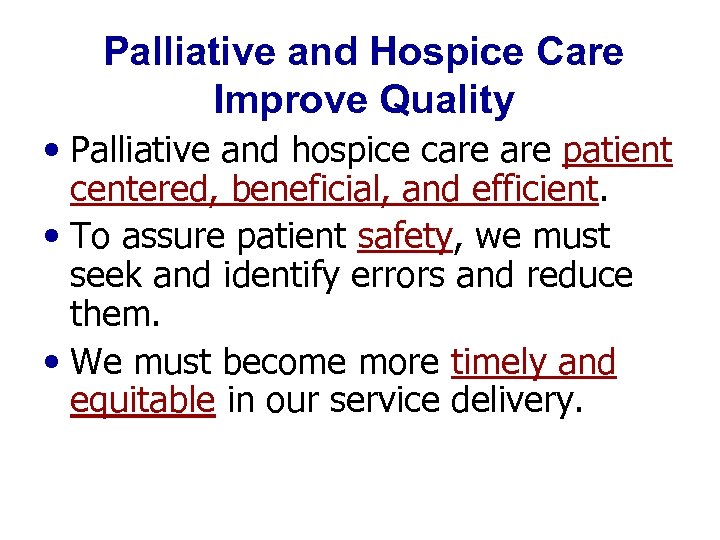 Palliative and Hospice Care Improve Quality • Palliative and hospice care patient centered, beneficial, and efficient. • To assure patient safety, we must seek and identify errors and reduce them. • We must become more timely and equitable in our service delivery.
Palliative and Hospice Care Improve Quality • Palliative and hospice care patient centered, beneficial, and efficient. • To assure patient safety, we must seek and identify errors and reduce them. • We must become more timely and equitable in our service delivery.
 State of the Science: Hospice and Palliative Care Programs Palliative and hospice care programs do something “Good” • Improved pain and other symptoms • Improved patient and family satisfaction • Improved resource utilization But… External quality measurement is coming. Are we ready for prime time?
State of the Science: Hospice and Palliative Care Programs Palliative and hospice care programs do something “Good” • Improved pain and other symptoms • Improved patient and family satisfaction • Improved resource utilization But… External quality measurement is coming. Are we ready for prime time?
 Are we Ready for Prime Time? External Quality Measures for Hospice + Palliative Care We need measures that are: Valid- The measure correlates with an important outcome. Reliable- The measure is consistent from center to center. Feasible- The burden of measurement is acceptable. Actionable- We can do something about it.
Are we Ready for Prime Time? External Quality Measures for Hospice + Palliative Care We need measures that are: Valid- The measure correlates with an important outcome. Reliable- The measure is consistent from center to center. Feasible- The burden of measurement is acceptable. Actionable- We can do something about it.
 Unintended Consequences of Measurement • Burden and expense of measuring outcomes that we may not be able to tell someone how to alter • Results of a poor measure may look as authentic as the results of a good measure • The tyranny of the measurable: Risk of diverting resources to problems being assessed to the detriment of equally or more important problems not being assessed (e. g. measuring # of advance directives instead of occurrence of care consistent with patient goals) • “There are lies, damned lies, and statistics. ” Mark Twain
Unintended Consequences of Measurement • Burden and expense of measuring outcomes that we may not be able to tell someone how to alter • Results of a poor measure may look as authentic as the results of a good measure • The tyranny of the measurable: Risk of diverting resources to problems being assessed to the detriment of equally or more important problems not being assessed (e. g. measuring # of advance directives instead of occurrence of care consistent with patient goals) • “There are lies, damned lies, and statistics. ” Mark Twain
 External quality measures and end of life care - Are we ready for prime time? We providers should not measure nor be held accountable for: a) outcomes that have not been shown to be alterable by processes under our control b) processes that have not been shown to improve outcomes.
External quality measures and end of life care - Are we ready for prime time? We providers should not measure nor be held accountable for: a) outcomes that have not been shown to be alterable by processes under our control b) processes that have not been shown to improve outcomes.
 External Quality Measures A Good Example- Restraint Use • Studies demonstrate that restraints do not prevent falls. • Use of restraints associated with incontinence, injury, depression, discomfort, pain, and death. • Restraint use and falls selected as quality indicator for minimum data set (MDS)
External Quality Measures A Good Example- Restraint Use • Studies demonstrate that restraints do not prevent falls. • Use of restraints associated with incontinence, injury, depression, discomfort, pain, and death. • Restraint use and falls selected as quality indicator for minimum data set (MDS)
 External Quality Measures Restraints • Reduction in restraint use in nursing homes. • No resulting increase in falls or injuries.
External Quality Measures Restraints • Reduction in restraint use in nursing homes. • No resulting increase in falls or injuries.
 External Quality Measure A Bad Example- Weight Loss • Malnutrition and weight loss result in increased morbidity and mortality in the elderly • Nursing home residents are at increased risk for malnutrition and dehydration • Weight loss selected as quality indicator for minimum data set (MDS)
External Quality Measure A Bad Example- Weight Loss • Malnutrition and weight loss result in increased morbidity and mortality in the elderly • Nursing home residents are at increased risk for malnutrition and dehydration • Weight loss selected as quality indicator for minimum data set (MDS)
 Unintended Consequences Weight Loss in the Nursing Home • Dying patients lose weight. • Broad application of wt. loss as a quality indicator caused: ØIncreased use of feeding tubes ØIncreased transfers to hospital • Poorly selected measure results in worsened quality of care.
Unintended Consequences Weight Loss in the Nursing Home • Dying patients lose weight. • Broad application of wt. loss as a quality indicator caused: ØIncreased use of feeding tubes ØIncreased transfers to hospital • Poorly selected measure results in worsened quality of care.
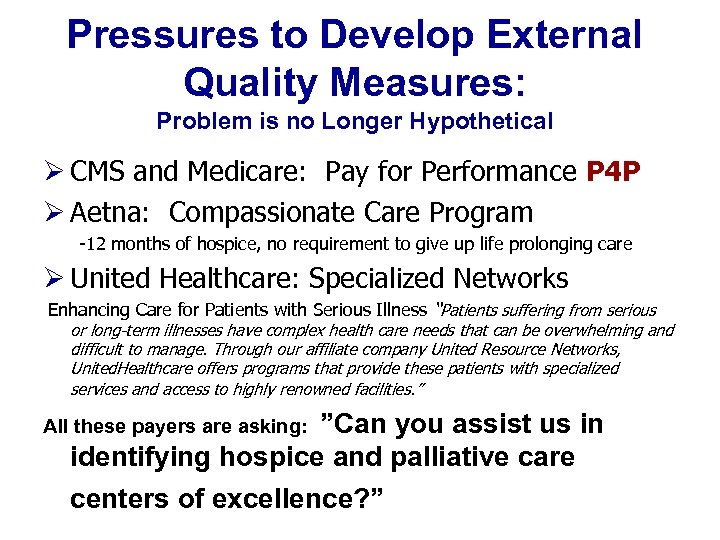 Pressures to Develop External Quality Measures: Problem is no Longer Hypothetical Ø CMS and Medicare: Pay for Performance P 4 P Ø Aetna: Compassionate Care Program -12 months of hospice, no requirement to give up life prolonging care Ø United Healthcare: Specialized Networks Enhancing Care for Patients with Serious Illness “Patients suffering from serious or long-term illnesses have complex health care needs that can be overwhelming and difficult to manage. Through our affiliate company United Resource Networks, United. Healthcare offers programs that provide these patients with specialized services and access to highly renowned facilities. ” All these payers are asking: ”Can you assist us in identifying hospice and palliative care centers of excellence? ”
Pressures to Develop External Quality Measures: Problem is no Longer Hypothetical Ø CMS and Medicare: Pay for Performance P 4 P Ø Aetna: Compassionate Care Program -12 months of hospice, no requirement to give up life prolonging care Ø United Healthcare: Specialized Networks Enhancing Care for Patients with Serious Illness “Patients suffering from serious or long-term illnesses have complex health care needs that can be overwhelming and difficult to manage. Through our affiliate company United Resource Networks, United. Healthcare offers programs that provide these patients with specialized services and access to highly renowned facilities. ” All these payers are asking: ”Can you assist us in identifying hospice and palliative care centers of excellence? ”
 Steps Forward and Challenges How should we respond to pressures of regulatory bodies and payers for measures given the current state of our field?
Steps Forward and Challenges How should we respond to pressures of regulatory bodies and payers for measures given the current state of our field?
 Palliative and Hospice Care Quality Collectively our field must develop and test measures that are feasible, reliable, actionable, and demonstrably linked to improved quality, or have them imposed upon us.
Palliative and Hospice Care Quality Collectively our field must develop and test measures that are feasible, reliable, actionable, and demonstrably linked to improved quality, or have them imposed upon us.

 Achieving Quality of Care • Patients and families want palliative and hospice care. • We know that palliative and hospice care improves quality. • Payers want to purchase quality palliative and hospice care for their beneficiaries. • We have to prove our quality through internal and external measurement and reporting. • The time to do that is now.
Achieving Quality of Care • Patients and families want palliative and hospice care. • We know that palliative and hospice care improves quality. • Payers want to purchase quality palliative and hospice care for their beneficiaries. • We have to prove our quality through internal and external measurement and reporting. • The time to do that is now.
 The Importance of Partnership From the Care of Dr. M to Assuring Access to Quality Palliative Care for All Americans • The commitment of NHPCO and the achievement of consensus for both the NCP and NQF processes was crucial to their success. • Collaborations between hospice and other palliative care providers and organizations will not only improve patient care but also define and test quality indicators. • Our partnership experience with both the NCP and NQF processes of consensus development is good preparation for the next stage of measure development and testing.
The Importance of Partnership From the Care of Dr. M to Assuring Access to Quality Palliative Care for All Americans • The commitment of NHPCO and the achievement of consensus for both the NCP and NQF processes was crucial to their success. • Collaborations between hospice and other palliative care providers and organizations will not only improve patient care but also define and test quality indicators. • Our partnership experience with both the NCP and NQF processes of consensus development is good preparation for the next stage of measure development and testing.
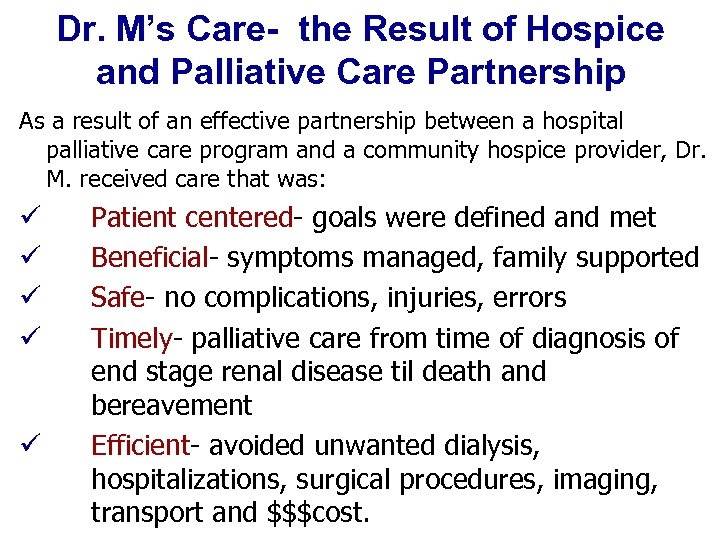 Dr. M’s Care- the Result of Hospice and Palliative Care Partnership As a result of an effective partnership between a hospital palliative care program and a community hospice provider, Dr. M. received care that was: ü ü ü Patient centered- goals were defined and met Beneficial- symptoms managed, family supported Safe- no complications, injuries, errors Timely- palliative care from time of diagnosis of end stage renal disease til death and bereavement Efficient- avoided unwanted dialysis, hospitalizations, surgical procedures, imaging, transport and $$$cost.
Dr. M’s Care- the Result of Hospice and Palliative Care Partnership As a result of an effective partnership between a hospital palliative care program and a community hospice provider, Dr. M. received care that was: ü ü ü Patient centered- goals were defined and met Beneficial- symptoms managed, family supported Safe- no complications, injuries, errors Timely- palliative care from time of diagnosis of end stage renal disease til death and bereavement Efficient- avoided unwanted dialysis, hospitalizations, surgical procedures, imaging, transport and $$$cost.
 Although the world is full of suffering, it is also full of the overcoming of it. Helen Keller Optimism 1903
Although the world is full of suffering, it is also full of the overcoming of it. Helen Keller Optimism 1903


