4194799b7d19e1db4c9cfe5b63064f5d.ppt
- Количество слайдов: 32
 Hormonal Disease in Pregnancy
Hormonal Disease in Pregnancy
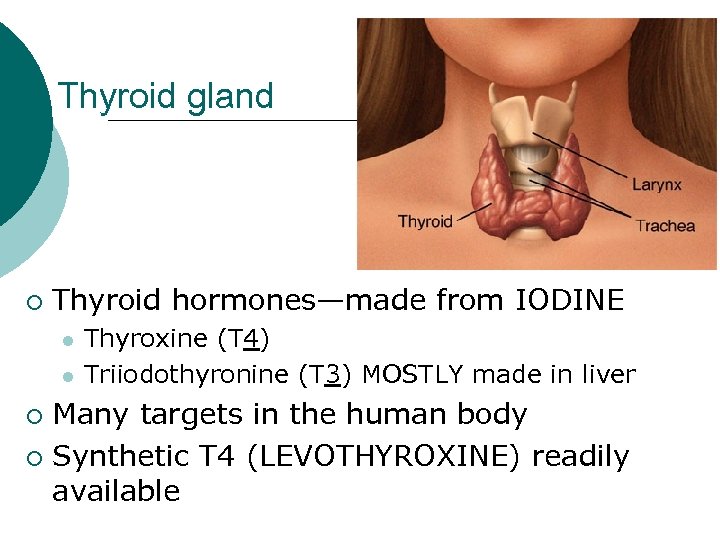 Thyroid gland ¡ Thyroid hormones—made from IODINE l l Thyroxine (T 4) Triiodothyronine (T 3) MOSTLY made in liver Many targets in the human body ¡ Synthetic T 4 (LEVOTHYROXINE) readily available ¡
Thyroid gland ¡ Thyroid hormones—made from IODINE l l Thyroxine (T 4) Triiodothyronine (T 3) MOSTLY made in liver Many targets in the human body ¡ Synthetic T 4 (LEVOTHYROXINE) readily available ¡
 2011 Guidelines: Endocrine Society American Thyroid Association Pre conception education of hypothyroid women and optimization of LT 4 dosage ¡ Check thyroid function tests as soon as pregnancy confirmed and consider empirically increasing LT 4 dose by taking 2 additional LT 4 tablets per week ¡
2011 Guidelines: Endocrine Society American Thyroid Association Pre conception education of hypothyroid women and optimization of LT 4 dosage ¡ Check thyroid function tests as soon as pregnancy confirmed and consider empirically increasing LT 4 dose by taking 2 additional LT 4 tablets per week ¡
 Thyroid health in pregnant women without thyroid disease ¡ Daily iodine requirements increase in pregnancy l l WHO 250 mcg/day Institute of Medicine 220 mcg/day NOT all prenatal vitamins contain iodine! ¡ In the USA, as of 2009, only 51% of prenatal vitamins labeled to contain iodine ¡ Measured iodine content was only 75% of labeled content! ¡ Leung A et al N Engl J Med 2009 360: 9
Thyroid health in pregnant women without thyroid disease ¡ Daily iodine requirements increase in pregnancy l l WHO 250 mcg/day Institute of Medicine 220 mcg/day NOT all prenatal vitamins contain iodine! ¡ In the USA, as of 2009, only 51% of prenatal vitamins labeled to contain iodine ¡ Measured iodine content was only 75% of labeled content! ¡ Leung A et al N Engl J Med 2009 360: 9
 2011 Guidelines: Endocrine Society American Thyroid Association ¡ All women attempting to conceive and pregnant women take a prenatal vitamin containing 150 mcg of potassium iodine
2011 Guidelines: Endocrine Society American Thyroid Association ¡ All women attempting to conceive and pregnant women take a prenatal vitamin containing 150 mcg of potassium iodine
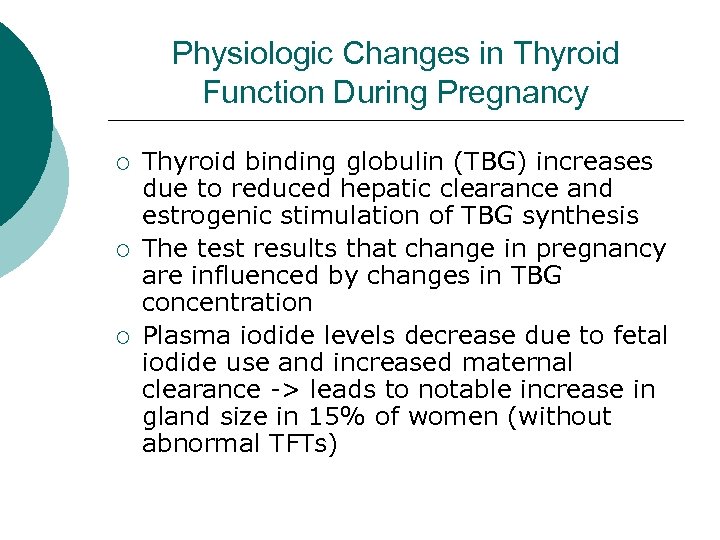 Physiologic Changes in Thyroid Function During Pregnancy ¡ ¡ ¡ Thyroid binding globulin (TBG) increases due to reduced hepatic clearance and estrogenic stimulation of TBG synthesis The test results that change in pregnancy are influenced by changes in TBG concentration Plasma iodide levels decrease due to fetal iodide use and increased maternal clearance -> leads to notable increase in gland size in 15% of women (without abnormal TFTs)
Physiologic Changes in Thyroid Function During Pregnancy ¡ ¡ ¡ Thyroid binding globulin (TBG) increases due to reduced hepatic clearance and estrogenic stimulation of TBG synthesis The test results that change in pregnancy are influenced by changes in TBG concentration Plasma iodide levels decrease due to fetal iodide use and increased maternal clearance -> leads to notable increase in gland size in 15% of women (without abnormal TFTs)
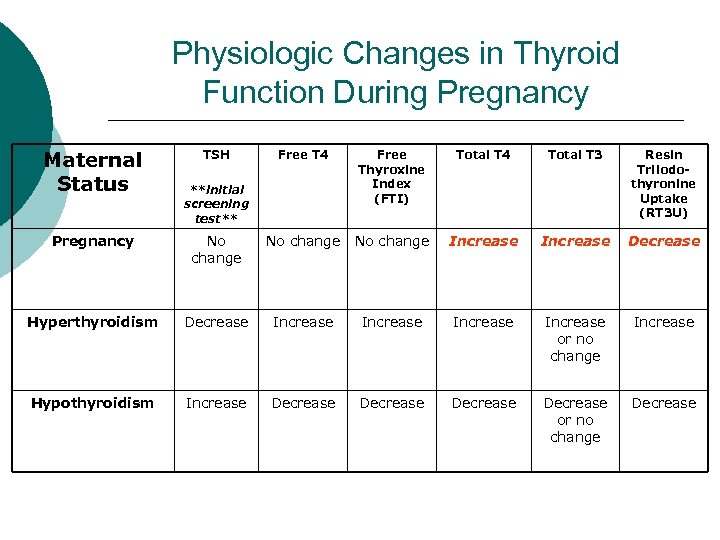 Physiologic Changes in Thyroid Function During Pregnancy Maternal Status TSH Free T 4 Free Thyroxine Index (FTI) Total T 4 Total T 3 Resin Triiodothyronine Uptake (RT 3 U) **initial screening test** Pregnancy No change Increase Decrease Hyperthyroidism Decrease Increase or no change Increase Hypothyroidism Increase Decrease or no change Decrease
Physiologic Changes in Thyroid Function During Pregnancy Maternal Status TSH Free T 4 Free Thyroxine Index (FTI) Total T 4 Total T 3 Resin Triiodothyronine Uptake (RT 3 U) **initial screening test** Pregnancy No change Increase Decrease Hyperthyroidism Decrease Increase or no change Increase Hypothyroidism Increase Decrease or no change Decrease
 The Fetal Thyroid Begins concentrating iodine at 1012 weeks ¡ Controlled by pituitary TSH by approximately 20 weeks ¡
The Fetal Thyroid Begins concentrating iodine at 1012 weeks ¡ Controlled by pituitary TSH by approximately 20 weeks ¡
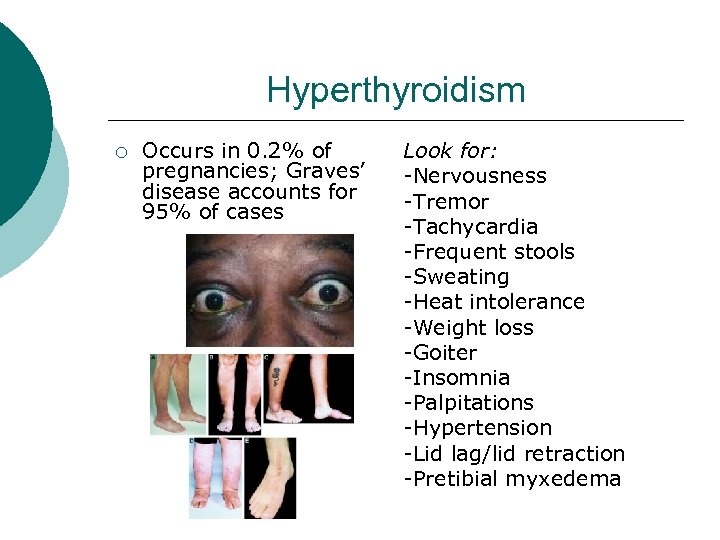 Hyperthyroidism ¡ Occurs in 0. 2% of pregnancies; Graves’ disease accounts for 95% of cases Look for: -Nervousness -Tremor -Tachycardia -Frequent stools -Sweating -Heat intolerance -Weight loss -Goiter -Insomnia -Palpitations -Hypertension -Lid lag/lid retraction -Pretibial myxedema
Hyperthyroidism ¡ Occurs in 0. 2% of pregnancies; Graves’ disease accounts for 95% of cases Look for: -Nervousness -Tremor -Tachycardia -Frequent stools -Sweating -Heat intolerance -Weight loss -Goiter -Insomnia -Palpitations -Hypertension -Lid lag/lid retraction -Pretibial myxedema
 Fetal & Neonatal Effects of Hyperthyroidism ¡ ¡ ¡ Associated with preterm delivery, low birth weight, fetal loss Fetal thyrotoxicosis (related to disease itself or treatment) Risk of immune-mediated hypo/hyperthyroidism (due to antibodies crossing the placenta, esp. in Graves or chronic autoimmune thyroiditis) l l Antibodies in Graves’ disease can be either stimulatory or inhibitory Neonates of women with Graves’ who have been surgically/radioactively treated are at higher risk, b/c not taking suppression
Fetal & Neonatal Effects of Hyperthyroidism ¡ ¡ ¡ Associated with preterm delivery, low birth weight, fetal loss Fetal thyrotoxicosis (related to disease itself or treatment) Risk of immune-mediated hypo/hyperthyroidism (due to antibodies crossing the placenta, esp. in Graves or chronic autoimmune thyroiditis) l l Antibodies in Graves’ disease can be either stimulatory or inhibitory Neonates of women with Graves’ who have been surgically/radioactively treated are at higher risk, b/c not taking suppression
 Causes & Diagnosis of Hyperthyroidism ¡ Most common cause of hyperthyroidism is Graves’ disease l l ¡ Document elevated FT 4 or elevated FTI with suppressed TSH, in absence of goiter/mass Most patients have antibodies to TSH receptor, antimicrosomal, or antithyroid peroxidase antibodies, but measurement of these is not required (though some endocrinologists recommend measuring TSI, which are stimulatory antibodies to TSH receptor) Other causes: l Excess TSH production, gestational trophoplastic disease, hyperfunctioning thyroid adenoma, toxic goiter, subacute thyroiditis, extrathyroid source of TH
Causes & Diagnosis of Hyperthyroidism ¡ Most common cause of hyperthyroidism is Graves’ disease l l ¡ Document elevated FT 4 or elevated FTI with suppressed TSH, in absence of goiter/mass Most patients have antibodies to TSH receptor, antimicrosomal, or antithyroid peroxidase antibodies, but measurement of these is not required (though some endocrinologists recommend measuring TSI, which are stimulatory antibodies to TSH receptor) Other causes: l Excess TSH production, gestational trophoplastic disease, hyperfunctioning thyroid adenoma, toxic goiter, subacute thyroiditis, extrathyroid source of TH
 Treatment of Hyperthyroidism ¡ ¡ ¡ Goal is to maintain FT 4/FTI in high normal range using lowest possible dose (minimize fetal exposure) Measure FT 4/FTI q 2 -4 weeks and titrate Thioamides (PTU/methimazole) -> decrease thyroid hormone synthesis by blocking organification of iodide l l PTU also reduces T 4 ->T 3 and may work more quickly PTU traditionally preferred (older studies found that methimazole crossed placenta more readily and was associated with fetal aplasia cutis; newer studies refute this)
Treatment of Hyperthyroidism ¡ ¡ ¡ Goal is to maintain FT 4/FTI in high normal range using lowest possible dose (minimize fetal exposure) Measure FT 4/FTI q 2 -4 weeks and titrate Thioamides (PTU/methimazole) -> decrease thyroid hormone synthesis by blocking organification of iodide l l PTU also reduces T 4 ->T 3 and may work more quickly PTU traditionally preferred (older studies found that methimazole crossed placenta more readily and was associated with fetal aplasia cutis; newer studies refute this)
 Treatment of Hyperthyroidism ¡ Effect of treatment on fetal thyroid function: l l ¡ Possible transient suppression of thyroid function Fetal goiter associated with Graves’ (usually drug-induced fetal hypothyroidism) Fetal thyrotoxicosis due to maternal antibodies is rare -> screen for growth and normal FHR Neonate at risk for thyroid dysfunction; notify pediatrician Breastfeeding safe when taking PTU/methimazole
Treatment of Hyperthyroidism ¡ Effect of treatment on fetal thyroid function: l l ¡ Possible transient suppression of thyroid function Fetal goiter associated with Graves’ (usually drug-induced fetal hypothyroidism) Fetal thyrotoxicosis due to maternal antibodies is rare -> screen for growth and normal FHR Neonate at risk for thyroid dysfunction; notify pediatrician Breastfeeding safe when taking PTU/methimazole
 Treatment of Hyperthyroidism ¡ ¡ ¡ Beta-blockers can be used for symptomatic relief (usually Propanolol) Reserve thyroidectomy for women in whom thioamide treatment unsuccessful Iodine 131 contraindicated (risk of fetal thyroid ablation especially if exposed after 10 weeks); avoid pregnancy/breastfeeding for 4 months after radioactive ablation
Treatment of Hyperthyroidism ¡ ¡ ¡ Beta-blockers can be used for symptomatic relief (usually Propanolol) Reserve thyroidectomy for women in whom thioamide treatment unsuccessful Iodine 131 contraindicated (risk of fetal thyroid ablation especially if exposed after 10 weeks); avoid pregnancy/breastfeeding for 4 months after radioactive ablation
 Hypothyroidism ¡ ¡ Symptoms: fatigue, constipation, cold intolerance, muscle cramps, hair loss, dry skin, slow reflexes, weight gain, intellectual slowness, voice changes, insomnia Can progress to myxedema and coma Subclinical hypothyroidism: elevated TSH, normal FTI in asymptomatic patient Associated with other autoimmune disorders l Type 1 DM -> 5 -8% risk of hypothyroidism; 25% postpartum thyroid dysfunction
Hypothyroidism ¡ ¡ Symptoms: fatigue, constipation, cold intolerance, muscle cramps, hair loss, dry skin, slow reflexes, weight gain, intellectual slowness, voice changes, insomnia Can progress to myxedema and coma Subclinical hypothyroidism: elevated TSH, normal FTI in asymptomatic patient Associated with other autoimmune disorders l Type 1 DM -> 5 -8% risk of hypothyroidism; 25% postpartum thyroid dysfunction
 Hypothyroidism: Fetal & Neonatal Effects Higher incidence of LBW (due to medically indicated preterm delivery, pre-eclampsia, abruption) ¡ Iodine deficient hypothyroidism -> congenital cretinism (growth failure, mental retardation, other neuropsychological deficits) ¡
Hypothyroidism: Fetal & Neonatal Effects Higher incidence of LBW (due to medically indicated preterm delivery, pre-eclampsia, abruption) ¡ Iodine deficient hypothyroidism -> congenital cretinism (growth failure, mental retardation, other neuropsychological deficits) ¡
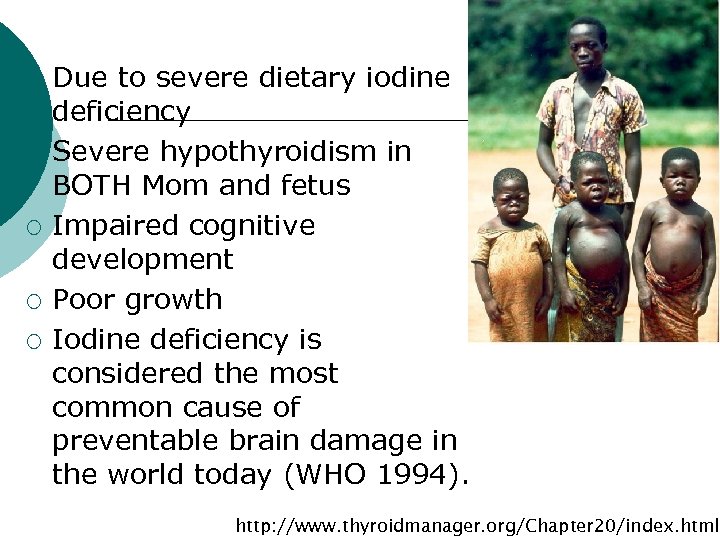 Cretinism ¡ ¡ ¡ Due to severe dietary iodine deficiency Severe hypothyroidism in BOTH Mom and fetus Impaired cognitive development Poor growth Iodine deficiency is considered the most common cause of preventable brain damage in the world today (WHO 1994). http: //www. thyroidmanager. org/Chapter 20/index. html
Cretinism ¡ ¡ ¡ Due to severe dietary iodine deficiency Severe hypothyroidism in BOTH Mom and fetus Impaired cognitive development Poor growth Iodine deficiency is considered the most common cause of preventable brain damage in the world today (WHO 1994). http: //www. thyroidmanager. org/Chapter 20/index. html
 Causes & Diagnosis of Hypothyroidism ¡ Causes: l l Hashimoto’s (chronic thyroiditis; most common in developed countries) & iodine deficiency -> both associated with goiter Subacute thyroiditis -> not associated with goiter Thyroidectomy, radioactive iodine treatment Iodine deficiency (most common worldwide; rare in US)
Causes & Diagnosis of Hypothyroidism ¡ Causes: l l Hashimoto’s (chronic thyroiditis; most common in developed countries) & iodine deficiency -> both associated with goiter Subacute thyroiditis -> not associated with goiter Thyroidectomy, radioactive iodine treatment Iodine deficiency (most common worldwide; rare in US)
 Spectrum l Mild “subclinical” hypothyroidism 1: 50 pregnancies l Severe “overt” hypothyroidism 1: 500 pregnancies
Spectrum l Mild “subclinical” hypothyroidism 1: 50 pregnancies l Severe “overt” hypothyroidism 1: 500 pregnancies
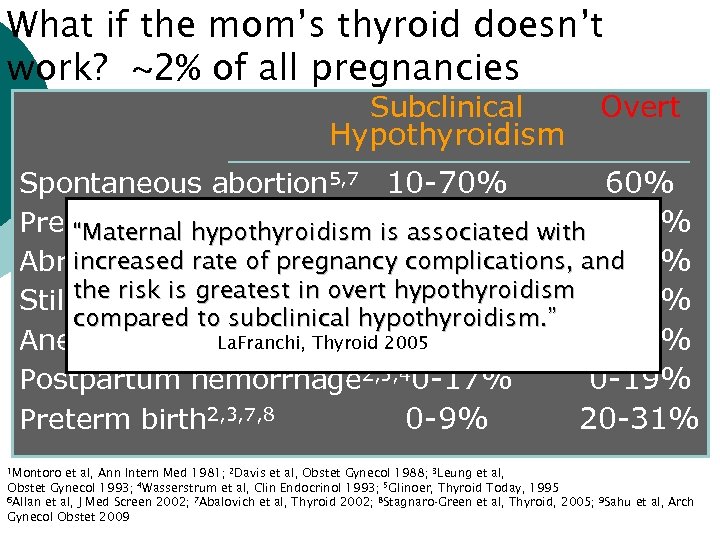 What if the mom’s thyroid doesn’t work? ~2% of all pregnancies Subclinical Hypothyroidism Overt Spontaneous abortion 5, 7 10 -70% 60% Preeclampsia 1, 2, 4, 6, 9 “Maternal hypothyroidism is 0 -17% associated with 0 -44% increased rate Abruption 2, 3, 4, 6, 7 of pregnancy complications, and 0% 0 -19% the risk is greatest in overt hypothyroidism Stillbirth/fetal loss 1, 2, 3, 6 0 -3% 0 -12% compared to subclinical hypothyroidism. ” La. Franchi, Thyroid 2005 Anemia 2, 3 0 -2% 0 -31% Postpartum hemorrhage 2, 3, 40 -17% 0 -19% Preterm birth 2, 3, 7, 8 0 -9% 20 -31% 1 Montoro et al, Ann Intern Med 1981; 2 Davis et al, Obstet Gynecol 1988; 3 Leung et al, Obstet Gynecol 1993; 4 Wasserstrum et al, Clin Endocrinol 1993; 5 Glinoer, Thyroid Today, 1995 6 Allan et al, J Med Screen 2002; 7 Abalovich et al, Thyroid 2002; 8 Stagnaro-Green et al, Thyroid, 2005; 9 Sahu et al, Arch Gynecol Obstet 2009
What if the mom’s thyroid doesn’t work? ~2% of all pregnancies Subclinical Hypothyroidism Overt Spontaneous abortion 5, 7 10 -70% 60% Preeclampsia 1, 2, 4, 6, 9 “Maternal hypothyroidism is 0 -17% associated with 0 -44% increased rate Abruption 2, 3, 4, 6, 7 of pregnancy complications, and 0% 0 -19% the risk is greatest in overt hypothyroidism Stillbirth/fetal loss 1, 2, 3, 6 0 -3% 0 -12% compared to subclinical hypothyroidism. ” La. Franchi, Thyroid 2005 Anemia 2, 3 0 -2% 0 -31% Postpartum hemorrhage 2, 3, 40 -17% 0 -19% Preterm birth 2, 3, 7, 8 0 -9% 20 -31% 1 Montoro et al, Ann Intern Med 1981; 2 Davis et al, Obstet Gynecol 1988; 3 Leung et al, Obstet Gynecol 1993; 4 Wasserstrum et al, Clin Endocrinol 1993; 5 Glinoer, Thyroid Today, 1995 6 Allan et al, J Med Screen 2002; 7 Abalovich et al, Thyroid 2002; 8 Stagnaro-Green et al, Thyroid, 2005; 9 Sahu et al, Arch Gynecol Obstet 2009
 Recent Developments Hypothyroidism for Subclinical MATERNAL HEALTH Negro R et al, Universal Screening vs Case Finding for Detection and Treatment of Thyroid Dysfunction During Pregnancy, J Clin Endocrinol Metabolism 2010 95: 1699 FETAL HEALTH Lazarus J et al. Controlled Antenatal Thyroid Screening (CATS) Study. 14 th International Thyroid Congress, Sept 2010
Recent Developments Hypothyroidism for Subclinical MATERNAL HEALTH Negro R et al, Universal Screening vs Case Finding for Detection and Treatment of Thyroid Dysfunction During Pregnancy, J Clin Endocrinol Metabolism 2010 95: 1699 FETAL HEALTH Lazarus J et al. Controlled Antenatal Thyroid Screening (CATS) Study. 14 th International Thyroid Congress, Sept 2010
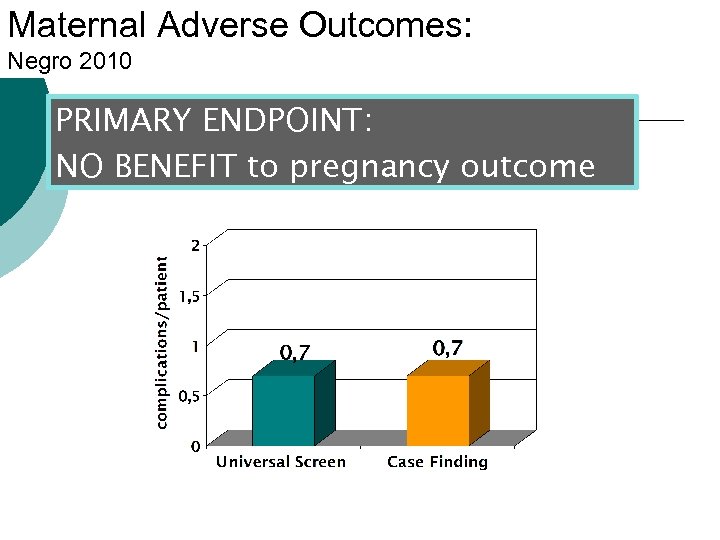 Maternal Adverse Outcomes: Negro 2010 PRIMARY ENDPOINT: NO BENEFIT to pregnancy outcome
Maternal Adverse Outcomes: Negro 2010 PRIMARY ENDPOINT: NO BENEFIT to pregnancy outcome
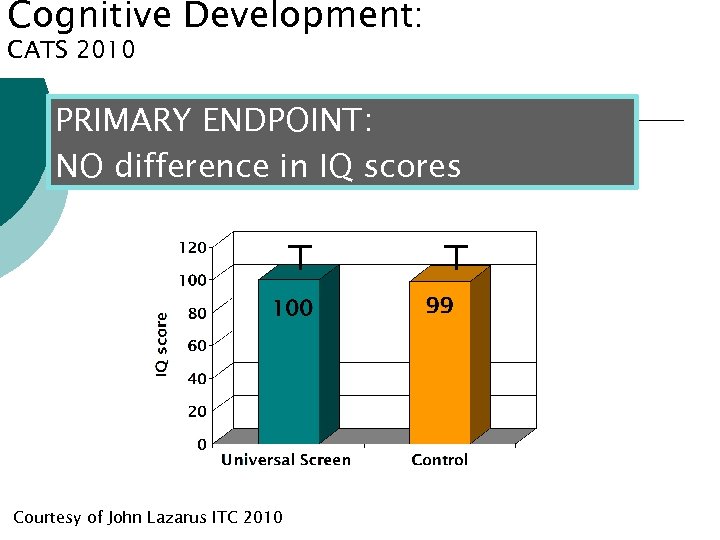 Cognitive Development: Cognitive development and Maternal Hypothyroidism CATS 2010 PRIMARY ENDPOINT: NO difference in IQ scores Courtesy of John Lazarus ITC 2010
Cognitive Development: Cognitive development and Maternal Hypothyroidism CATS 2010 PRIMARY ENDPOINT: NO difference in IQ scores Courtesy of John Lazarus ITC 2010
 ¡ ¡ However, secondary analyses for both studies suggest a benefit Negative results could be due to screening and intervention at end of 1 st trimester—TOO LATE What to do
¡ ¡ However, secondary analyses for both studies suggest a benefit Negative results could be due to screening and intervention at end of 1 st trimester—TOO LATE What to do
 2011 Guidelines: Endocrine Society American Thyroid Association Insufficient evidence to recommend universal screening for thyroid disease in pregnant women ¡ Aggressive detection of women at high risk for thyroid dysfunction ¡
2011 Guidelines: Endocrine Society American Thyroid Association Insufficient evidence to recommend universal screening for thyroid disease in pregnant women ¡ Aggressive detection of women at high risk for thyroid dysfunction ¡
 Women at risk for hypothyroidism • History of thyroid dysfunction or prior thyroid surgery • Signs or symptoms of thyroid problem • Women older than age 30 • Presence of other autoimmune disorders – Type 1 diabetes, rheumatoid arthritis • Family history of thyroid dysfunction • History of miscarriage or preterm labor
Women at risk for hypothyroidism • History of thyroid dysfunction or prior thyroid surgery • Signs or symptoms of thyroid problem • Women older than age 30 • Presence of other autoimmune disorders – Type 1 diabetes, rheumatoid arthritis • Family history of thyroid dysfunction • History of miscarriage or preterm labor
 ¡ ¡ What is needed. . . Partnerships with public health, government and professional organizations to insure all prenatal vitamins contain 150 mcg of potassium iodine Exploration of the feasibility of a randomized controlled trial that screens, identifies, and treats thyroid dysfunction in women PRIOR to conception
¡ ¡ What is needed. . . Partnerships with public health, government and professional organizations to insure all prenatal vitamins contain 150 mcg of potassium iodine Exploration of the feasibility of a randomized controlled trial that screens, identifies, and treats thyroid dysfunction in women PRIOR to conception
 Treatment of Hypothyroidism Treat with Levothyroxine in sufficient dose to return TSH to normal ¡ Adjust dosage every 4 weeks ¡ Check TSH every trimester ¡
Treatment of Hypothyroidism Treat with Levothyroxine in sufficient dose to return TSH to normal ¡ Adjust dosage every 4 weeks ¡ Check TSH every trimester ¡
 ACOG Recommendations ¡ Screening of all pregnant women with a personal history, physical examination, or symptoms of a thyroid disorder.
ACOG Recommendations ¡ Screening of all pregnant women with a personal history, physical examination, or symptoms of a thyroid disorder.
 Prolog Question #1 ¡ A 33 year-old G 3 P 2 at 10 weeks GA comes to the office for her 1 st prenatal visit. She reports that she had hypothyroidism in the distant past, but was never treated and is asymptomatic. Physical examination is normal. On bimanual examination her uterus is 10 weeks size and FHR is 150 bpm. Her TSH level is 13. 1 and, free T 4 level is 0. 7, and her anti-thyroid peroxidase antibody level is high. The next best step in the patient’s care is: l l A) Begin levothyroxine B) Repeat serum TSH and Free T 4 after 20 weeks of gestation C) Measure serum thyroid-stimulating immunoglobulins D) Perform ultrasonography of the maternal thyroid
Prolog Question #1 ¡ A 33 year-old G 3 P 2 at 10 weeks GA comes to the office for her 1 st prenatal visit. She reports that she had hypothyroidism in the distant past, but was never treated and is asymptomatic. Physical examination is normal. On bimanual examination her uterus is 10 weeks size and FHR is 150 bpm. Her TSH level is 13. 1 and, free T 4 level is 0. 7, and her anti-thyroid peroxidase antibody level is high. The next best step in the patient’s care is: l l A) Begin levothyroxine B) Repeat serum TSH and Free T 4 after 20 weeks of gestation C) Measure serum thyroid-stimulating immunoglobulins D) Perform ultrasonography of the maternal thyroid
 Answer ¡ A) Begin levothyroxine l l Although the patient is asymptomatic she has laboratory evidence of overt hypothyroidism with an elevated TSH and low free T 4 level She also has elevated anti-thyroid peroxidase antibody level which indicates that the likely cause of her hypothyroidism is chronic autoimmune thyroditis (Hashimoto’s disease) The anti-thyroid peroxidase antibodies also indicate an increased risk of her developing other autoimmune disease, such as adrena insufficiency or type 1 DM. Hypothyroidism in pregnancy has been associated with pre-eclampsia, GHTN, abruptio placentae, preterm delivery, and neuropsychologic deficits in the child.
Answer ¡ A) Begin levothyroxine l l Although the patient is asymptomatic she has laboratory evidence of overt hypothyroidism with an elevated TSH and low free T 4 level She also has elevated anti-thyroid peroxidase antibody level which indicates that the likely cause of her hypothyroidism is chronic autoimmune thyroditis (Hashimoto’s disease) The anti-thyroid peroxidase antibodies also indicate an increased risk of her developing other autoimmune disease, such as adrena insufficiency or type 1 DM. Hypothyroidism in pregnancy has been associated with pre-eclampsia, GHTN, abruptio placentae, preterm delivery, and neuropsychologic deficits in the child.
 And if the baby’s thyroid doesn’t work. . Congenital hypothyroidism affects 1: 3000 live births in the US ¡ Newborn screening programs in all 50 states ¡ Detection and treatment by 1 month of life results in normal outcomes ¡ THEREFORE, maternal thyroid hormone can protect fetal development in utero ¡
And if the baby’s thyroid doesn’t work. . Congenital hypothyroidism affects 1: 3000 live births in the US ¡ Newborn screening programs in all 50 states ¡ Detection and treatment by 1 month of life results in normal outcomes ¡ THEREFORE, maternal thyroid hormone can protect fetal development in utero ¡


