1c63d2ace094d0610739b3b006d79aac.ppt
- Количество слайдов: 47
 Hoarding in the Elderly: A Challenge to Home Care Mary Ann Forciea MD, FACP Associate Professor of Clinical Medicine Division of Geriatric Medicine UPHS
Hoarding in the Elderly: A Challenge to Home Care Mary Ann Forciea MD, FACP Associate Professor of Clinical Medicine Division of Geriatric Medicine UPHS
 Why am I (or my team) here? • This is a common and frustrating problem for us • Hoping to learn some diagnostic tips • Hoping to learn some management tips • Want a chance to vent frustration at the system of care available to these patients. • Like to see my colleagues. • Always wanted to try this restaurant
Why am I (or my team) here? • This is a common and frustrating problem for us • Hoping to learn some diagnostic tips • Hoping to learn some management tips • Want a chance to vent frustration at the system of care available to these patients. • Like to see my colleagues. • Always wanted to try this restaurant
 Why am I (or my team) here? 1. 2. 3. 4. 5. This is a challenging problem for us Want a chance to vent about these patients Like to see my colleagues Always wanted to try this restaurant Want to see if UPHS has any better ideas than we do
Why am I (or my team) here? 1. 2. 3. 4. 5. This is a challenging problem for us Want a chance to vent about these patients Like to see my colleagues Always wanted to try this restaurant Want to see if UPHS has any better ideas than we do
 Key questions for this seminar • Is hoarding in older patients different than in younger patients • What are the critical clinical questions in the evaluation of patients with hoarding? • What treatment strategies can be attempted? • What resources are available in the Delaware Valley?
Key questions for this seminar • Is hoarding in older patients different than in younger patients • What are the critical clinical questions in the evaluation of patients with hoarding? • What treatment strategies can be attempted? • What resources are available in the Delaware Valley?
 Case- DR • 78 yr old lady, widow with 2 children • Living in Senior housing • Call from facility SW (Friday at 4 PM) – Increasing complaints from neighbors about ‘cleanliness’ of apartment – Apartment visit that day • Toilet overflow, clutter, attire – Home health aide refusing to return – Facility considering eviction
Case- DR • 78 yr old lady, widow with 2 children • Living in Senior housing • Call from facility SW (Friday at 4 PM) – Increasing complaints from neighbors about ‘cleanliness’ of apartment – Apartment visit that day • Toilet overflow, clutter, attire – Home health aide refusing to return – Facility considering eviction
 Case continues 2 • >40 yr history of bipolar disorder – Has medications – Multiple barriers to ongoing psychiatric care • Diabetes mellitus with peripheral neuropathy] • Venous stasis • DJD of knees, hips, LS spine – increasing immobility
Case continues 2 • >40 yr history of bipolar disorder – Has medications – Multiple barriers to ongoing psychiatric care • Diabetes mellitus with peripheral neuropathy] • Venous stasis • DJD of knees, hips, LS spine – increasing immobility
 Case 3 – prior history • Third dwelling while part of our primary care program (8 yrs) • ‘Clutter’ an issue in each site – Mania associated with requests for DME • Progressive mobility dependence – Third move precipitated by loss of driving privileges
Case 3 – prior history • Third dwelling while part of our primary care program (8 yrs) • ‘Clutter’ an issue in each site – Mania associated with requests for DME • Progressive mobility dependence – Third move precipitated by loss of driving privileges
 Added information • Visited patient one week ago • Called patient after SW call – Admits to overwhelming apartment ‘situation’ – Blame exclusively on building management – Admits to progressive URI over past week – Reluctant to agree to ED or hospital visit • Home care team urgent conference call
Added information • Visited patient one week ago • Called patient after SW call – Admits to overwhelming apartment ‘situation’ – Blame exclusively on building management – Admits to progressive URI over past week – Reluctant to agree to ED or hospital visit • Home care team urgent conference call
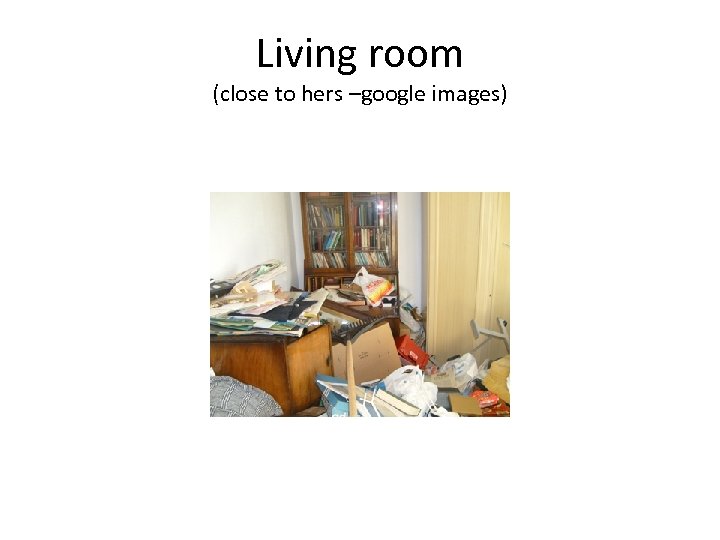 Living room (close to hers –google images)
Living room (close to hers –google images)
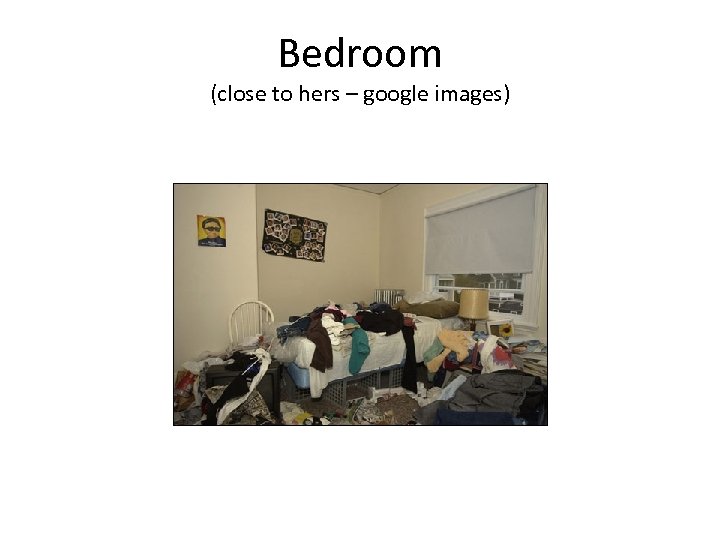 Bedroom (close to hers – google images)
Bedroom (close to hers – google images)
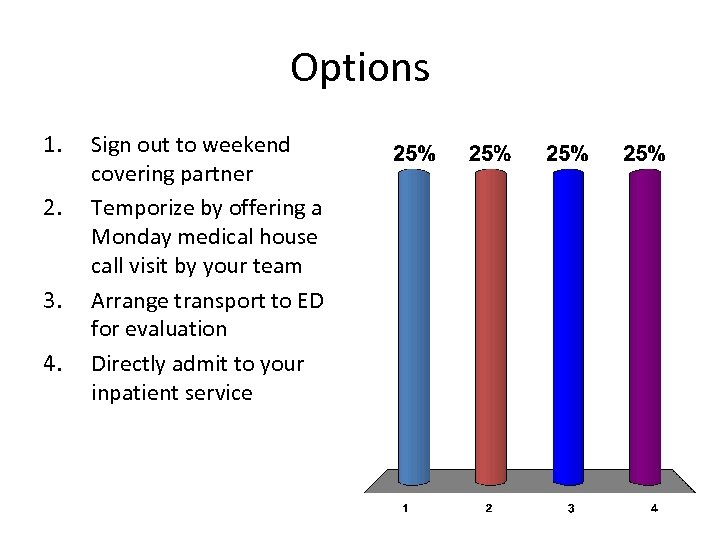 Options 1. 2. 3. 4. Sign out to weekend covering partner Temporize by offering a Monday medical house call visit by your team Arrange transport to ED for evaluation Directly admit to your inpatient service
Options 1. 2. 3. 4. Sign out to weekend covering partner Temporize by offering a Monday medical house call visit by your team Arrange transport to ED for evaluation Directly admit to your inpatient service
 Hoarding – Definition Saxena 2007 • Collecting – excessive quantities of – Poorly useable items – Of little value • Failing to discard items • Interference with function
Hoarding – Definition Saxena 2007 • Collecting – excessive quantities of – Poorly useable items – Of little value • Failing to discard items • Interference with function
 Excessive acquisition • Buying • Accumulation of ‘free’ things – Received – Sought out (dumpster diving • Motivation – “thrill” – ‘therapy’ for unpleasant feelings (? ‘retail’ therapy) – Fear of missed opportunities
Excessive acquisition • Buying • Accumulation of ‘free’ things – Received – Sought out (dumpster diving • Motivation – “thrill” – ‘therapy’ for unpleasant feelings (? ‘retail’ therapy) – Fear of missed opportunities
 Failure to discard • Most easily recognized • Motivation – Sentimental value – Wasteful to discard – Might be useful in the future • Decreased ability to group/sort items • Poor organizational skills
Failure to discard • Most easily recognized • Motivation – Sentimental value – Wasteful to discard – Might be useful in the future • Decreased ability to group/sort items • Poor organizational skills
 Interference with function • Clutter – cannot use space or object for its intended purpose • Functional status – cannot walk through apartment, bathe, cook • Consequences – Eviction, health concerns, fire risks
Interference with function • Clutter – cannot use space or object for its intended purpose • Functional status – cannot walk through apartment, bathe, cook • Consequences – Eviction, health concerns, fire risks
 Risks of hoarding • • • Social dysfunction Functional disability Falls Fires Unsanitary conditions
Risks of hoarding • • • Social dysfunction Functional disability Falls Fires Unsanitary conditions
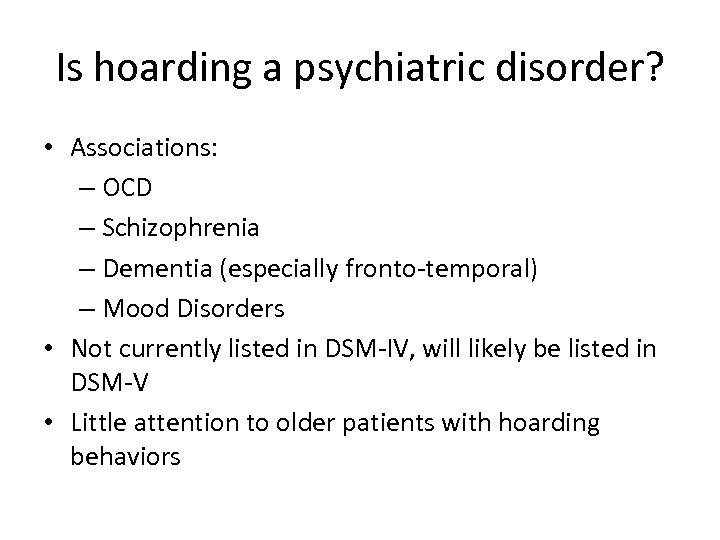 Is hoarding a psychiatric disorder? • Associations: – OCD – Schizophrenia – Dementia (especially fronto-temporal) – Mood Disorders • Not currently listed in DSM-IV, will likely be listed in DSM-V • Little attention to older patients with hoarding behaviors
Is hoarding a psychiatric disorder? • Associations: – OCD – Schizophrenia – Dementia (especially fronto-temporal) – Mood Disorders • Not currently listed in DSM-IV, will likely be listed in DSM-V • Little attention to older patients with hoarding behaviors
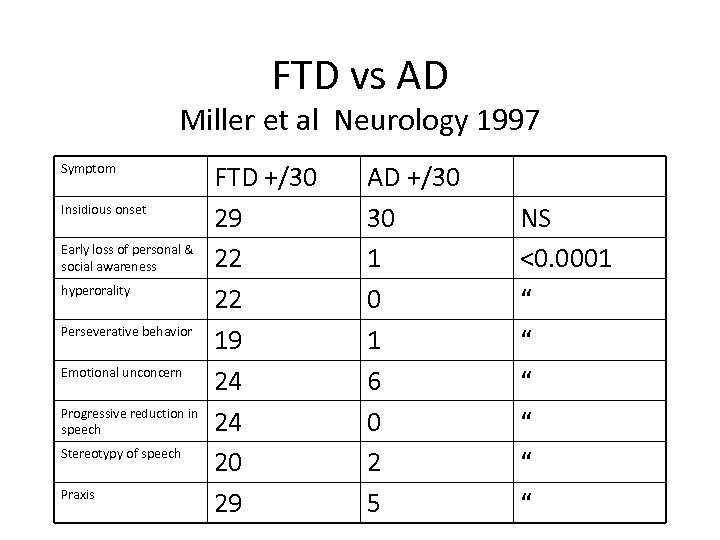 FTD vs AD Miller et al Neurology 1997 Symptom Insidious onset Early loss of personal & social awareness hyperorality Perseverative behavior Emotional unconcern Progressive reduction in speech Stereotypy of speech Praxis FTD +/30 29 22 22 19 24 24 20 29 AD +/30 30 1 6 0 2 5 NS <0. 0001 “ “ “
FTD vs AD Miller et al Neurology 1997 Symptom Insidious onset Early loss of personal & social awareness hyperorality Perseverative behavior Emotional unconcern Progressive reduction in speech Stereotypy of speech Praxis FTD +/30 29 22 22 19 24 24 20 29 AD +/30 30 1 6 0 2 5 NS <0. 0001 “ “ “
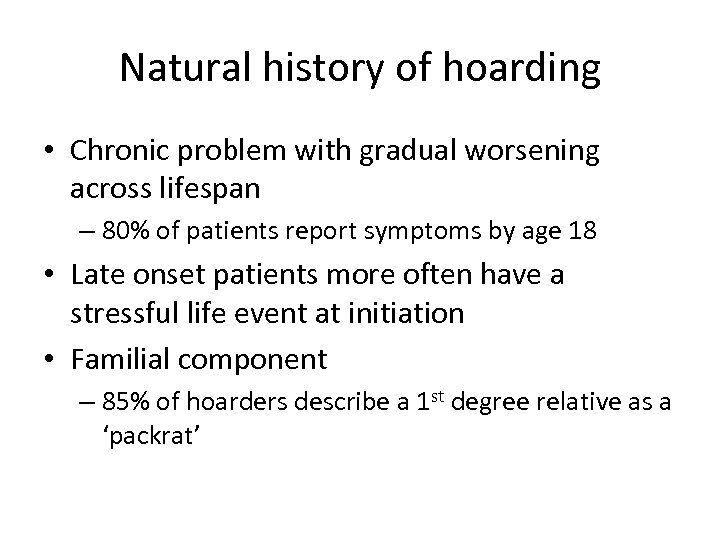 Natural history of hoarding • Chronic problem with gradual worsening across lifespan – 80% of patients report symptoms by age 18 • Late onset patients more often have a stressful life event at initiation • Familial component – 85% of hoarders describe a 1 st degree relative as a ‘packrat’
Natural history of hoarding • Chronic problem with gradual worsening across lifespan – 80% of patients report symptoms by age 18 • Late onset patients more often have a stressful life event at initiation • Familial component – 85% of hoarders describe a 1 st degree relative as a ‘packrat’
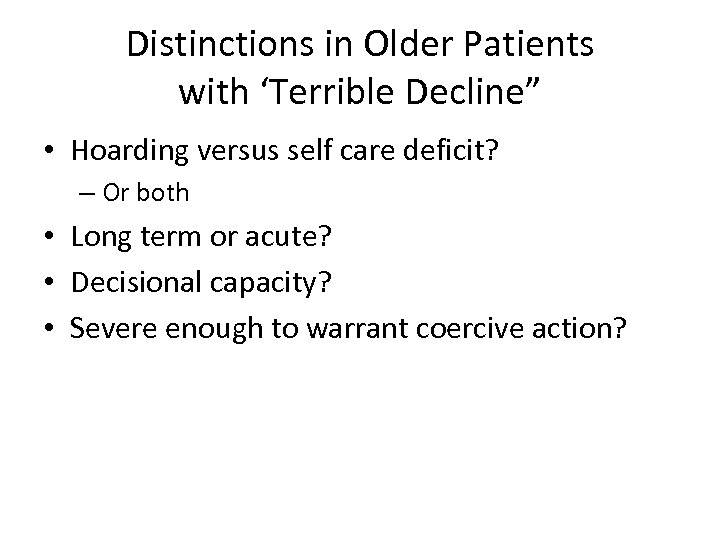 Distinctions in Older Patients with ‘Terrible Decline” • Hoarding versus self care deficit? – Or both • Long term or acute? • Decisional capacity? • Severe enough to warrant coercive action?
Distinctions in Older Patients with ‘Terrible Decline” • Hoarding versus self care deficit? – Or both • Long term or acute? • Decisional capacity? • Severe enough to warrant coercive action?
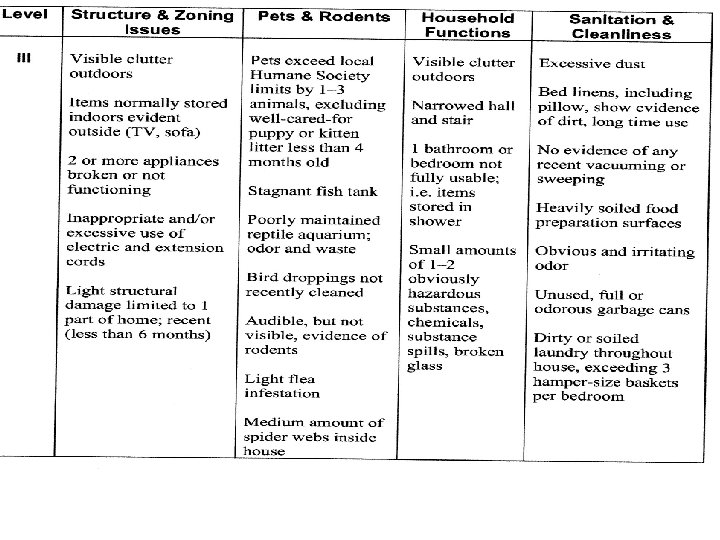
 Assessment tools Clutter Hoarding Scale Institute for Challenging Disorganization
Assessment tools Clutter Hoarding Scale Institute for Challenging Disorganization
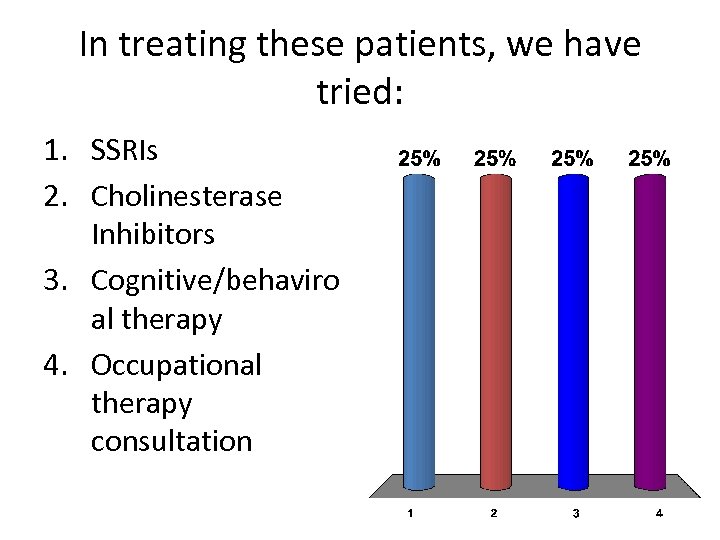 In treating these patients, we have tried: 1. SSRIs 2. Cholinesterase Inhibitors 3. Cognitive/behaviro al therapy 4. Occupational therapy consultation
In treating these patients, we have tried: 1. SSRIs 2. Cholinesterase Inhibitors 3. Cognitive/behaviro al therapy 4. Occupational therapy consultation
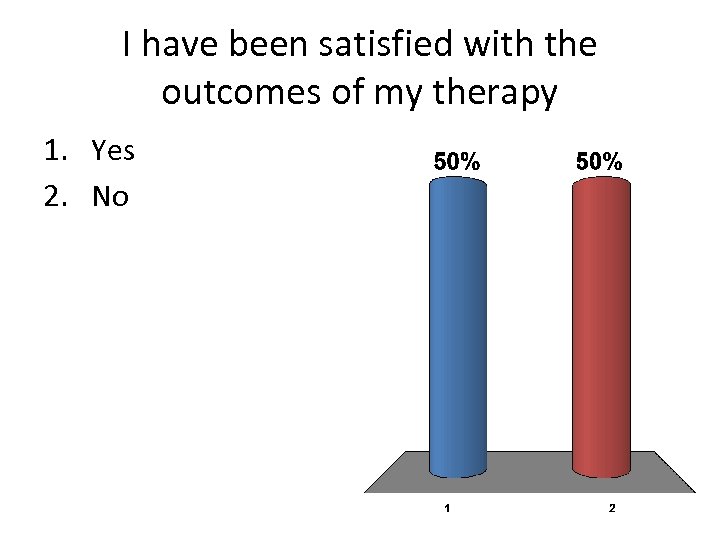 I have been satisfied with the outcomes of my therapy 1. Yes 2. No
I have been satisfied with the outcomes of my therapy 1. Yes 2. No
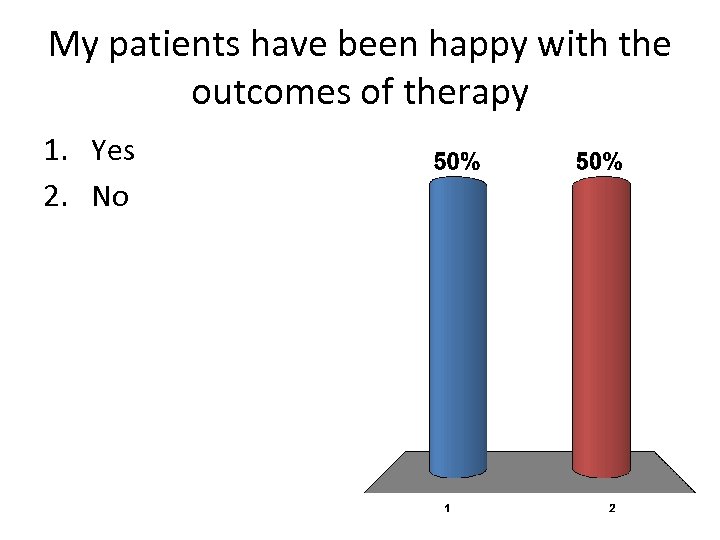 My patients have been happy with the outcomes of therapy 1. Yes 2. No
My patients have been happy with the outcomes of therapy 1. Yes 2. No
 Treatment • Medications – SSRI – possibly less effective in older patients • Cognitive behavioral therapy – Information processing deficits • Help sort into larger clusters – Maladaptive beliefs • I am a craftsman because I own tools – Attachment to possessions • Sentiment, control • Interprofessional team management
Treatment • Medications – SSRI – possibly less effective in older patients • Cognitive behavioral therapy – Information processing deficits • Help sort into larger clusters – Maladaptive beliefs • I am a craftsman because I own tools – Attachment to possessions • Sentiment, control • Interprofessional team management
 Self care deficit “The result of an adult’s inability due to diminished capacity to perform essential self-care tasks such as providing essential food, clothing, shelter, and medical care; obtaining goods and services necessary to maintain physical health, mental health, emotional well-being and general safety; and/or manage financial affairs. ” -APS
Self care deficit “The result of an adult’s inability due to diminished capacity to perform essential self-care tasks such as providing essential food, clothing, shelter, and medical care; obtaining goods and services necessary to maintain physical health, mental health, emotional well-being and general safety; and/or manage financial affairs. ” -APS
 Self-Neglect – Definition Pavlou and Lachs JGIM 2008 • A Self-neglector is a person who exhibits 1 or more of the following: – 1) persistent inattention to personal hygiene and/or environment – 2) repeated refusal of some/all indicated services which can reasonably be expected to improve quality of life – 3) self endangerment through the manifestation of unsafe behaviors (e. g. persistent refusal to care for a wound, creating fire hazards in the home)
Self-Neglect – Definition Pavlou and Lachs JGIM 2008 • A Self-neglector is a person who exhibits 1 or more of the following: – 1) persistent inattention to personal hygiene and/or environment – 2) repeated refusal of some/all indicated services which can reasonably be expected to improve quality of life – 3) self endangerment through the manifestation of unsafe behaviors (e. g. persistent refusal to care for a wound, creating fire hazards in the home)
 Self-neglect Annual incidence: 5. 2 per 1000 elders Self-neglect 50 -75% of elder mistreatment 90% of all self-neglect APS ≥ 65 y/o ♀>♂ Decreased survival 40. 3% died within 13 years follow-up • Self-neglect patients more likely to die in NH • • • Lachs et al. JAMA 1998
Self-neglect Annual incidence: 5. 2 per 1000 elders Self-neglect 50 -75% of elder mistreatment 90% of all self-neglect APS ≥ 65 y/o ♀>♂ Decreased survival 40. 3% died within 13 years follow-up • Self-neglect patients more likely to die in NH • • • Lachs et al. JAMA 1998
 Clinical evaluation • Dementia • Depression • If acute, look for medical problem – Stroke, infection, medication effect • Determination of decisional capacity
Clinical evaluation • Dementia • Depression • If acute, look for medical problem – Stroke, infection, medication effect • Determination of decisional capacity
 Treatment • Often emergency-related – Hip fracture, pneumonia, police incident • If incapable of decisions – Refer for competency determination and guardianship • Placement likely • If capable – Inform of helpful services – Documentation of preferences for Advance Directive
Treatment • Often emergency-related – Hip fracture, pneumonia, police incident • If incapable of decisions – Refer for competency determination and guardianship • Placement likely • If capable – Inform of helpful services – Documentation of preferences for Advance Directive
 Assessment tools Self neglect severity scale -Houston Geriatrics group
Assessment tools Self neglect severity scale -Houston Geriatrics group
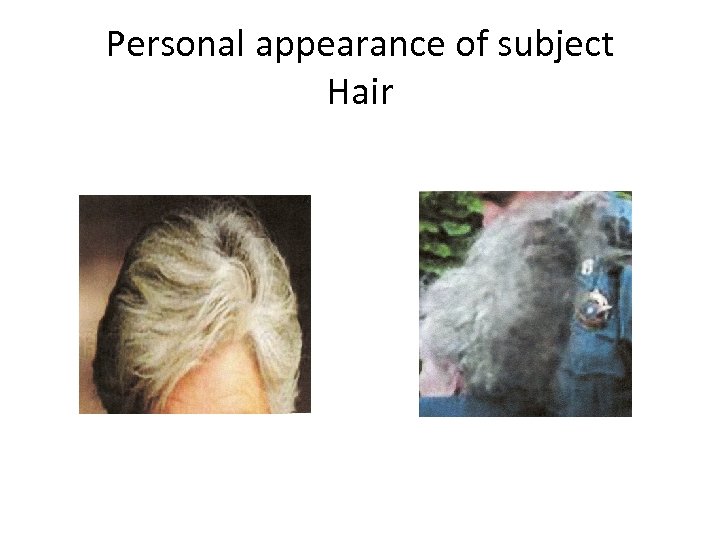 Personal appearance of subject Hair
Personal appearance of subject Hair
 Nails
Nails
 House
House
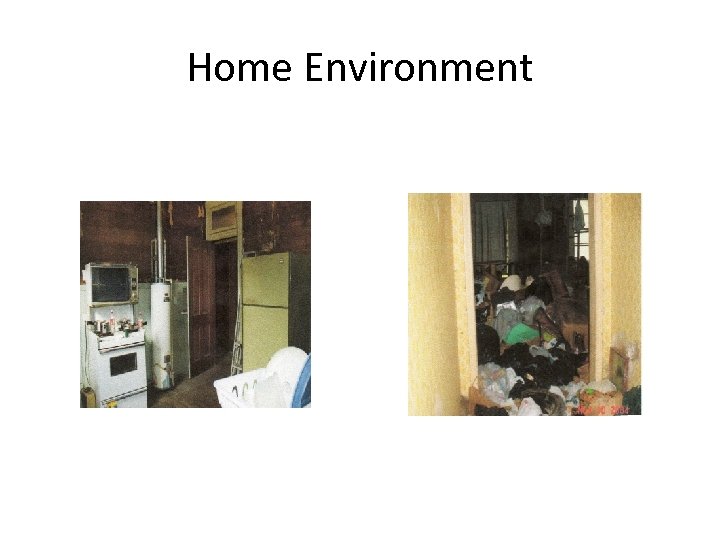 Home Environment
Home Environment
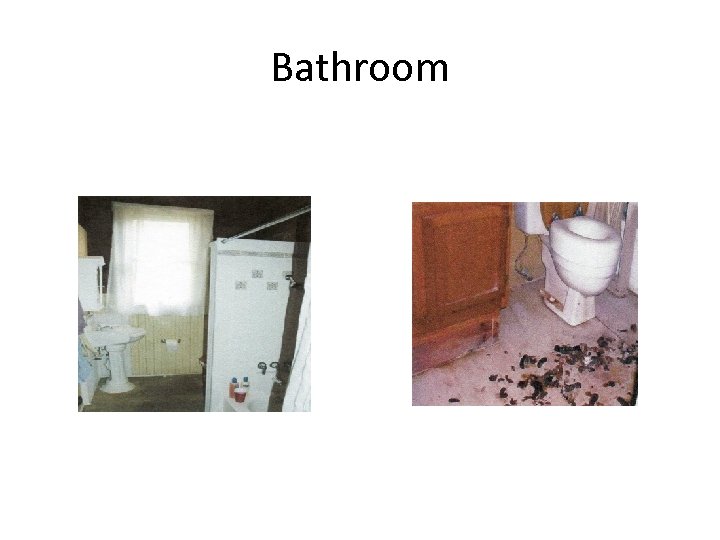 Bathroom
Bathroom
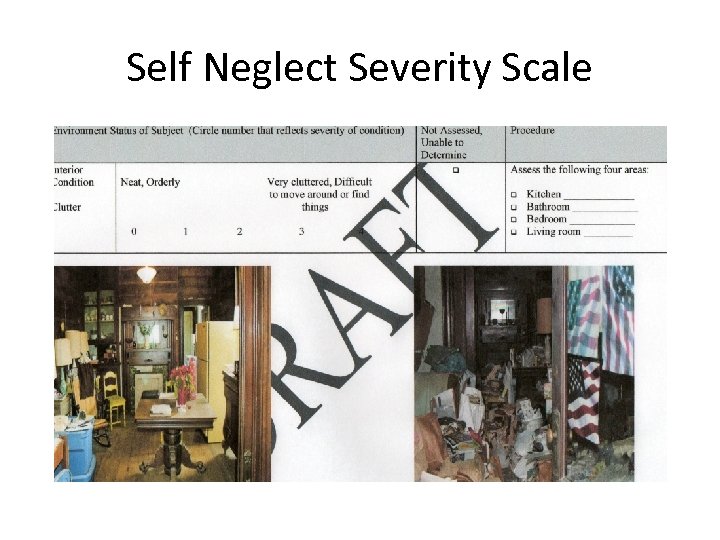 Self Neglect Severity Scale
Self Neglect Severity Scale
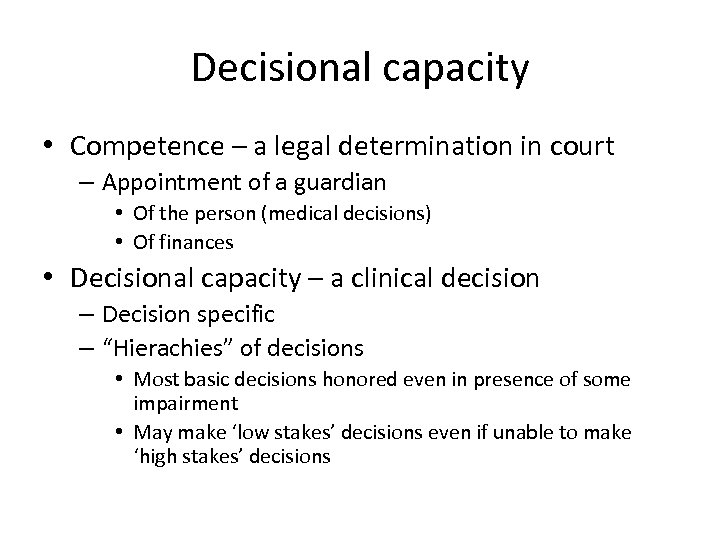 Decisional capacity • Competence – a legal determination in court – Appointment of a guardian • Of the person (medical decisions) • Of finances • Decisional capacity – a clinical decision – Decision specific – “Hierachies” of decisions • Most basic decisions honored even in presence of some impairment • May make ‘low stakes’ decisions even if unable to make ‘high stakes’ decisions
Decisional capacity • Competence – a legal determination in court – Appointment of a guardian • Of the person (medical decisions) • Of finances • Decisional capacity – a clinical decision – Decision specific – “Hierachies” of decisions • Most basic decisions honored even in presence of some impairment • May make ‘low stakes’ decisions even if unable to make ‘high stakes’ decisions
 Elements of Decision Making • Ability to communicate a choice • Ability to understand retain relevant information • Ability to appreciate the situation and consequences for oneself • Ability to manipulate information rationally
Elements of Decision Making • Ability to communicate a choice • Ability to understand retain relevant information • Ability to appreciate the situation and consequences for oneself • Ability to manipulate information rationally
 Ability to appreciate situation for oneself • Acknowledge that condition is present • Realizes that risks and benefits apply to him/her • May involve understanding of motives for choices • What will happen if you refuse treatment? If you accept?
Ability to appreciate situation for oneself • Acknowledge that condition is present • Realizes that risks and benefits apply to him/her • May involve understanding of motives for choices • What will happen if you refuse treatment? If you accept?
 Manipulates information rationally • Reaches conclusions that are logically consistent with starting premises • Again, may involve description of motives • Please help me to understand why you decided to accept/refuse treatment
Manipulates information rationally • Reaches conclusions that are logically consistent with starting premises • Again, may involve description of motives • Please help me to understand why you decided to accept/refuse treatment
 Summary • Older patients with hoarding behaviors have higher likelihood of co-existing dementia – Time course of progression is critical information • Hoarding and self neglect frequently co-exist in older patients – Assessment tools can help guide team planning and followup • The determination of decisional capacity is often critical • Local regulation about safety standards is important in action steps
Summary • Older patients with hoarding behaviors have higher likelihood of co-existing dementia – Time course of progression is critical information • Hoarding and self neglect frequently co-exist in older patients – Assessment tools can help guide team planning and followup • The determination of decisional capacity is often critical • Local regulation about safety standards is important in action steps
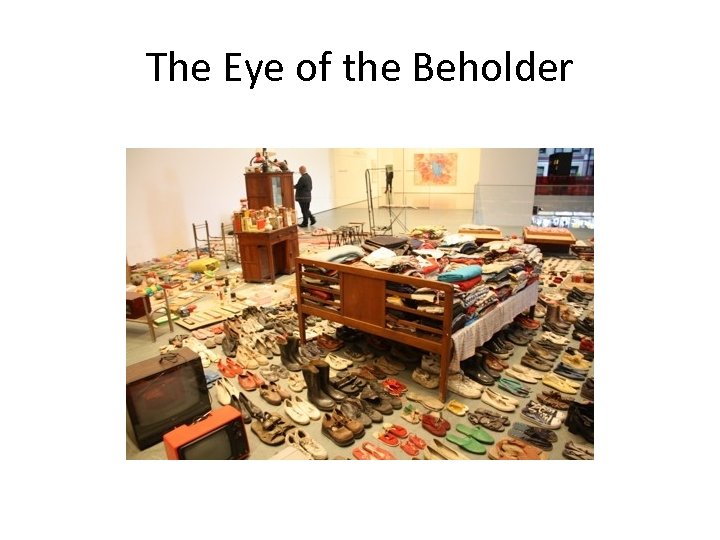 The Eye of the Beholder
The Eye of the Beholder
 Resources/References • The Institute for Challenging Disorganization: – www. challengingdisorganization. org • Valente, Sharon. The Hoarding Syndrome. Home Health Care Nurse 27: 432. 2009 – WWW. homehealthcarenurseonline. com • Guilliam, CM and Tolin, DF. Compulsive Hoarding. Bulletin of the Menniger Clinic 74: 93. 2010. • Dyer, CB et al. Self-neglect among the elderly; Am J of Public Health 97: 1671. 2007
Resources/References • The Institute for Challenging Disorganization: – www. challengingdisorganization. org • Valente, Sharon. The Hoarding Syndrome. Home Health Care Nurse 27: 432. 2009 – WWW. homehealthcarenurseonline. com • Guilliam, CM and Tolin, DF. Compulsive Hoarding. Bulletin of the Menniger Clinic 74: 93. 2010. • Dyer, CB et al. Self-neglect among the elderly; Am J of Public Health 97: 1671. 2007


