8bb9a7fce34f04877b0a66819b9d7d4d.ppt
- Количество слайдов: 16
 HIV EPIDEMIC AND RESPONSE IN SOUTH SUDAN: 2015 UPDATE
HIV EPIDEMIC AND RESPONSE IN SOUTH SUDAN: 2015 UPDATE
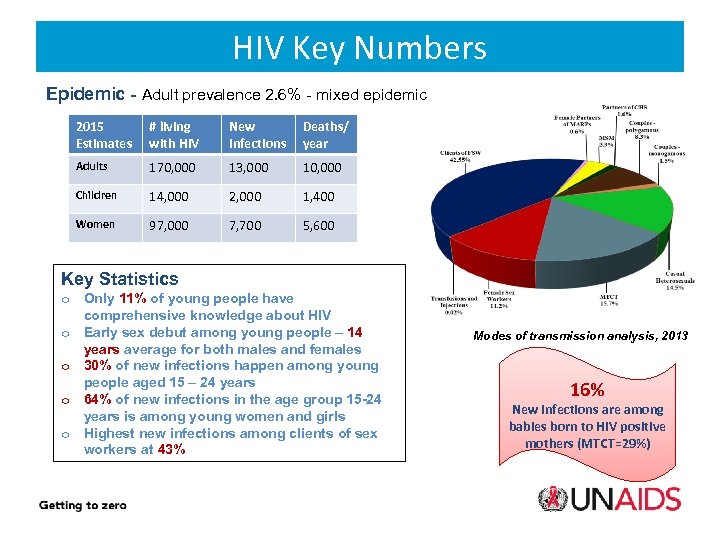 HIV Key Numbers Epidemic - Adult prevalence 2. 6% - mixed epidemic 2015 Estimates # living with HIV New Infections Deaths/ year Adults 170, 000 13, 000 10, 000 Children 14, 000 2, 000 1, 400 Women 97, 000 7, 700 5, 600 Key Statistics o Only 11% of young people have comprehensive knowledge about HIV o Early sex debut among young people – 14 years average for both males and females o 30% of new infections happen among young people aged 15 – 24 years o 64% of new infections in the age group 15 -24 years is among young women and girls o Highest new infections among clients of sex workers at 43% Modes of transmission analysis, 2013 16% New infections are among babies born to HIV positive mothers (MTCT=29%)
HIV Key Numbers Epidemic - Adult prevalence 2. 6% - mixed epidemic 2015 Estimates # living with HIV New Infections Deaths/ year Adults 170, 000 13, 000 10, 000 Children 14, 000 2, 000 1, 400 Women 97, 000 7, 700 5, 600 Key Statistics o Only 11% of young people have comprehensive knowledge about HIV o Early sex debut among young people – 14 years average for both males and females o 30% of new infections happen among young people aged 15 – 24 years o 64% of new infections in the age group 15 -24 years is among young women and girls o Highest new infections among clients of sex workers at 43% Modes of transmission analysis, 2013 16% New infections are among babies born to HIV positive mothers (MTCT=29%)
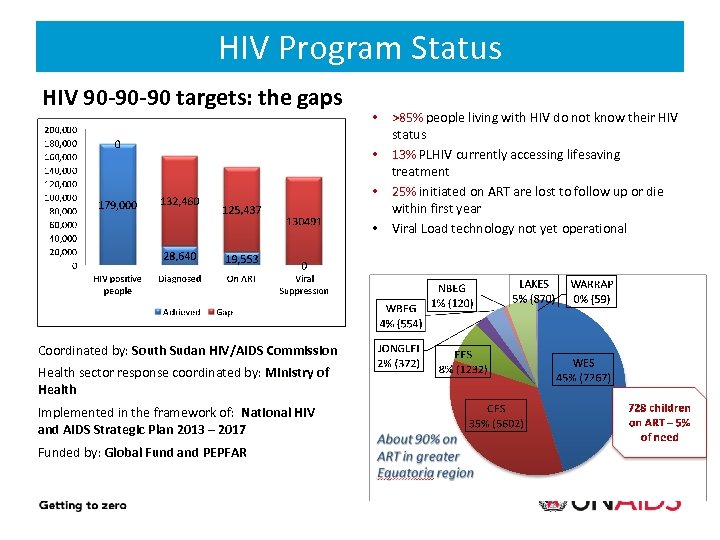 HIV Program Status HIV 90 -90 -90 targets: the gaps • • 18% 13. 4% No VL • • Coordinated by: South Sudan HIV/AIDS Commission Health sector response coordinated by: Ministry of Health Implemented in the framework of: National HIV and AIDS Strategic Plan 2013 – 2017 Funded by: Global Fund and PEPFAR >85% people living with HIV do not know their HIV status 13% PLHIV currently accessing lifesaving treatment 25% initiated on ART are lost to follow up or die within first year Viral Load technology not yet operational
HIV Program Status HIV 90 -90 -90 targets: the gaps • • 18% 13. 4% No VL • • Coordinated by: South Sudan HIV/AIDS Commission Health sector response coordinated by: Ministry of Health Implemented in the framework of: National HIV and AIDS Strategic Plan 2013 – 2017 Funded by: Global Fund and PEPFAR >85% people living with HIV do not know their HIV status 13% PLHIV currently accessing lifesaving treatment 25% initiated on ART are lost to follow up or die within first year Viral Load technology not yet operational
 Challenges to the HIV Response Limited infrastructure and systems to provide HIV services such as laboratory services, logistics and supply chain management Low levels of investment in HIV response High level of stigma and discrimination towards and among people living with HIV and key affected populations Low knowledge, low literacy and harmful socio-cultural practices impede HIV prevention efforts Lack of community support systems for adherence and psychosocial support to address stigma Humanitarian crisis and population displacement is having a reversal effect on the response, whilst making women and girls more vulnerable to infection
Challenges to the HIV Response Limited infrastructure and systems to provide HIV services such as laboratory services, logistics and supply chain management Low levels of investment in HIV response High level of stigma and discrimination towards and among people living with HIV and key affected populations Low knowledge, low literacy and harmful socio-cultural practices impede HIV prevention efforts Lack of community support systems for adherence and psychosocial support to address stigma Humanitarian crisis and population displacement is having a reversal effect on the response, whilst making women and girls more vulnerable to infection
 HIV AND THE CURRENT CRISIS: (POTENTIAL) IMPACT AND CONCERNS
HIV AND THE CURRENT CRISIS: (POTENTIAL) IMPACT AND CONCERNS
 HIV and AIDS, Crises and Vulnerability 6 Vulnerability to HIV infection: Emergencies generate situations of high risk to HIV infection Negative coping mechanisms Sexual and gender-based violence Disruption of social networks Inaccessible HIV prevention commodities Most at risk group Vulnerability to crisis: HIV and AIDS undermines existing coping strategies; may reduce social stability, available services and resources Disruption of health care services Disruption of care and support services e. g. food & livelihoods to ART/TB patients; HBC and OVC Impact of humanitarian situation on HIV affected households.
HIV and AIDS, Crises and Vulnerability 6 Vulnerability to HIV infection: Emergencies generate situations of high risk to HIV infection Negative coping mechanisms Sexual and gender-based violence Disruption of social networks Inaccessible HIV prevention commodities Most at risk group Vulnerability to crisis: HIV and AIDS undermines existing coping strategies; may reduce social stability, available services and resources Disruption of health care services Disruption of care and support services e. g. food & livelihoods to ART/TB patients; HBC and OVC Impact of humanitarian situation on HIV affected households.
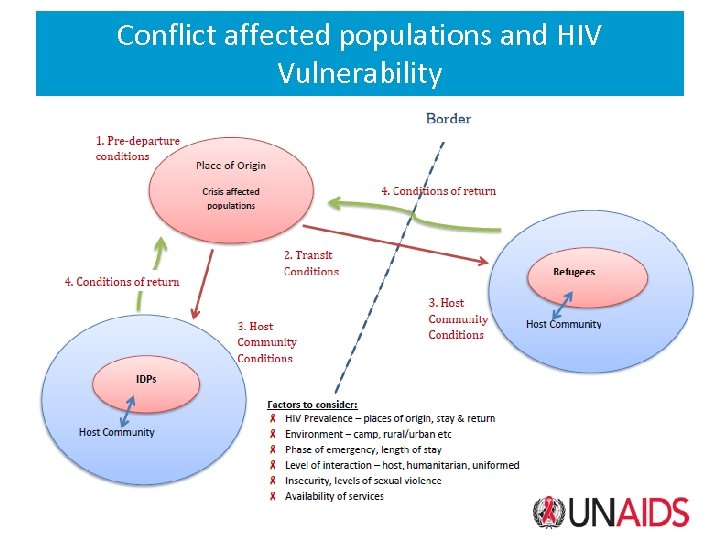 Conflict affected populations and HIV Vulnerability
Conflict affected populations and HIV Vulnerability
 Heightened Risk of HIV Infection Condom programming may be disrupted, decreasing easy access to The risk of acquiring HIV is increased if Sexually Transmitted Infections are left untreated Risk of unsafe blood transfusions: The number of transfusions may increase due to injuries after a disaster or a conflict, while blood safety measures can break down in humanitarian situations. Disruption of Prevention of Mother to Child Transmission (PMTCT) programming can result in infants becoming infected with HIV Survivors of rape and sexual violence, specifically women and girls, may not have access to post-exposure prophylaxis (PEP) to prevent HIV transmission result of widespread violence or conflict Negative coping mechanisms may expose vulnerable groups to high risk of HIV infection e. g. sex work or transactional sex, casual sex, migration to urban areas which may have higher HIV prevalence etc.
Heightened Risk of HIV Infection Condom programming may be disrupted, decreasing easy access to The risk of acquiring HIV is increased if Sexually Transmitted Infections are left untreated Risk of unsafe blood transfusions: The number of transfusions may increase due to injuries after a disaster or a conflict, while blood safety measures can break down in humanitarian situations. Disruption of Prevention of Mother to Child Transmission (PMTCT) programming can result in infants becoming infected with HIV Survivors of rape and sexual violence, specifically women and girls, may not have access to post-exposure prophylaxis (PEP) to prevent HIV transmission result of widespread violence or conflict Negative coping mechanisms may expose vulnerable groups to high risk of HIV infection e. g. sex work or transactional sex, casual sex, migration to urban areas which may have higher HIV prevalence etc.
 Increased Vulnerability of PLHIV Disruption of health care services leads to PLHIV not accessing prevention and treatment services, including treatment of opportunistic infections such as TB, STIs, Malaria etc Disruption of ART may lead to adverse side effects and further deterioration of health status through opportunistic infections Shortages of basic commodities such as food, water and safe shelter may have a severe socio-economic impact on individuals and families already affected by AIDS Food insecurity may lead to malnutrition in PLHIV, further deteriorating their health status, and increasing the risk of disease outbreaks such as TB, cholera etc Stigma, discrimination and social exclusion against PLHIV and their families increased in confined living conditions such as IDP camps. This may prevent them from accessing vital services, such as healthcare
Increased Vulnerability of PLHIV Disruption of health care services leads to PLHIV not accessing prevention and treatment services, including treatment of opportunistic infections such as TB, STIs, Malaria etc Disruption of ART may lead to adverse side effects and further deterioration of health status through opportunistic infections Shortages of basic commodities such as food, water and safe shelter may have a severe socio-economic impact on individuals and families already affected by AIDS Food insecurity may lead to malnutrition in PLHIV, further deteriorating their health status, and increasing the risk of disease outbreaks such as TB, cholera etc Stigma, discrimination and social exclusion against PLHIV and their families increased in confined living conditions such as IDP camps. This may prevent them from accessing vital services, such as healthcare
 Impact of the Crisis on HIV Epidemic & Response Crisis in the Equatoria region with highest burden of HIV, thousands of ART clients potentially lost to follow up ART sites non-functional – health workers, drugs, diagnostics etc High numbers of refugees in Uganda and DRC impacting on ability to ensure treatment continuation Food and nutrition insecurity is impacting on the ability of PLHIV to take their drugs Sexual violence and risk of HIV transmission Negative coping mechanisms can lead to high risk of HIV infection e. g. transactional sex, sex work, casual sex (especially among young people), migration to urban centers etc
Impact of the Crisis on HIV Epidemic & Response Crisis in the Equatoria region with highest burden of HIV, thousands of ART clients potentially lost to follow up ART sites non-functional – health workers, drugs, diagnostics etc High numbers of refugees in Uganda and DRC impacting on ability to ensure treatment continuation Food and nutrition insecurity is impacting on the ability of PLHIV to take their drugs Sexual violence and risk of HIV transmission Negative coping mechanisms can lead to high risk of HIV infection e. g. transactional sex, sex work, casual sex (especially among young people), migration to urban centers etc
 Actions On-going ART facility mapping – functionality, capacity, commodities etc Partner mapping – who is in areas where ART sites are not functional to help with ART continuation Community mobilisation and mapping – to help trace and return to treatment HIV (and TB) clients Re-programming of GFATM grant – to address emerging needs Updating ART contingency plan and standard operating procedures for displacement emergencies Application for emergency funds for South Sudanese refugees in DRC for HIV treatment Data collection on South Sudanese refugees in Uganda and lobbying for emergency funds to address HIV treatment needs
Actions On-going ART facility mapping – functionality, capacity, commodities etc Partner mapping – who is in areas where ART sites are not functional to help with ART continuation Community mobilisation and mapping – to help trace and return to treatment HIV (and TB) clients Re-programming of GFATM grant – to address emerging needs Updating ART contingency plan and standard operating procedures for displacement emergencies Application for emergency funds for South Sudanese refugees in DRC for HIV treatment Data collection on South Sudanese refugees in Uganda and lobbying for emergency funds to address HIV treatment needs
 Priority (immediate) Actions Required Mobilise networks/associations of PLHIV, CBOs and FBOs in areas affected by the crisis to trace and provide drugs to both ART and TB clients. Provide linkages to (new) health facilities in areas of displacement and support mobile clinics for ART, TB treatment and basic health care Activate service delivery models that allow for multi-month scripting and community drug distributions for stable patients Partnerships for logistical support to distribute and preposition ARVs and other commodities at state/county/facility levels Provide supplementary food to clients on ART and TB who are in need of additional food/nutritional support Ensure access to PEP for survivors of rape and sexual violence Community mobilisation and awareness for continuation of ART, HIV prevention and PEP – both at community level and using media
Priority (immediate) Actions Required Mobilise networks/associations of PLHIV, CBOs and FBOs in areas affected by the crisis to trace and provide drugs to both ART and TB clients. Provide linkages to (new) health facilities in areas of displacement and support mobile clinics for ART, TB treatment and basic health care Activate service delivery models that allow for multi-month scripting and community drug distributions for stable patients Partnerships for logistical support to distribute and preposition ARVs and other commodities at state/county/facility levels Provide supplementary food to clients on ART and TB who are in need of additional food/nutritional support Ensure access to PEP for survivors of rape and sexual violence Community mobilisation and awareness for continuation of ART, HIV prevention and PEP – both at community level and using media
 Health Sector Response A number of national and international guidelines outline the essential actions that the health sector must take to prevent HIV transmission and to provide care and support to people living with HIV in the minimum initial response and beyond.
Health Sector Response A number of national and international guidelines outline the essential actions that the health sector must take to prevent HIV transmission and to provide care and support to people living with HIV in the minimum initial response and beyond.
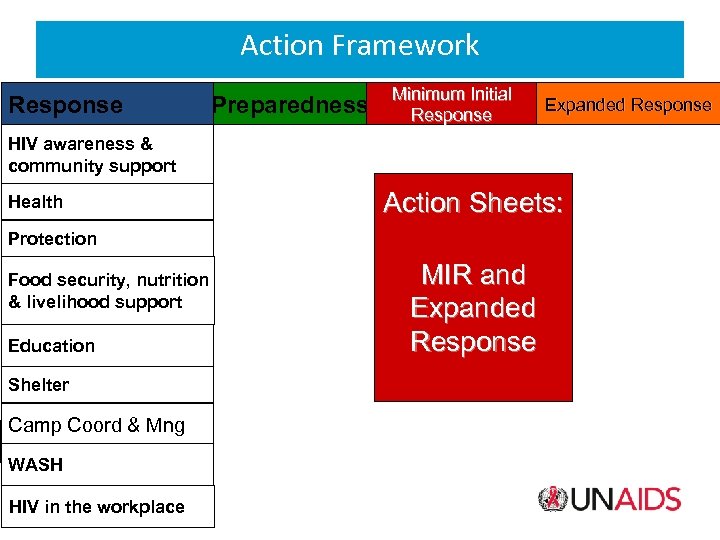 Action Framework Response Preparedness Minimum Initial Response Expanded Response HIV awareness & community support Health Action Sheets: Protection Food security, nutrition & livelihood support Education Shelter Camp Coord & Mng WASH HIV in the workplace MIR and Expanded Response
Action Framework Response Preparedness Minimum Initial Response Expanded Response HIV awareness & community support Health Action Sheets: Protection Food security, nutrition & livelihood support Education Shelter Camp Coord & Mng WASH HIV in the workplace MIR and Expanded Response
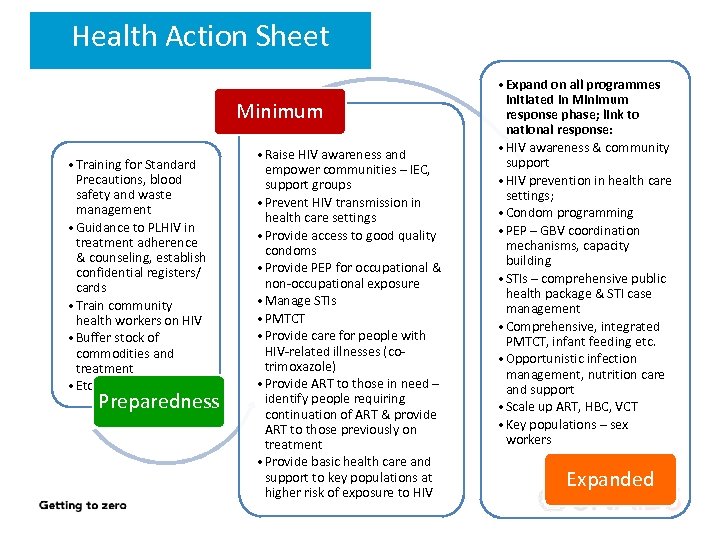 Health Action Sheet Minimum • Training for Standard Precautions, blood safety and waste management • Guidance to PLHIV in treatment adherence & counseling, establish confidential registers/ cards • Train community health workers on HIV • Buffer stock of commodities and treatment • Etc. Preparedness • Raise HIV awareness and empower communities – IEC, support groups • Prevent HIV transmission in health care settings • Provide access to good quality condoms • Provide PEP for occupational & non-occupational exposure • Manage STIs • PMTCT • Provide care for people with HIV-related illnesses (cotrimoxazole) • Provide ART to those in need – identify people requiring continuation of ART & provide ART to those previously on treatment • Provide basic health care and support to key populations at higher risk of exposure to HIV • Expand on all programmes initiated in Minimum response phase; link to national response: • HIV awareness & community support • HIV prevention in health care settings; • Condom programming • PEP – GBV coordination mechanisms, capacity building • STIs – comprehensive public health package & STI case management • Comprehensive, integrated PMTCT, infant feeding etc. • Opportunistic infection management, nutrition care and support • Scale up ART, HBC, VCT • Key populations – sex workers Expanded
Health Action Sheet Minimum • Training for Standard Precautions, blood safety and waste management • Guidance to PLHIV in treatment adherence & counseling, establish confidential registers/ cards • Train community health workers on HIV • Buffer stock of commodities and treatment • Etc. Preparedness • Raise HIV awareness and empower communities – IEC, support groups • Prevent HIV transmission in health care settings • Provide access to good quality condoms • Provide PEP for occupational & non-occupational exposure • Manage STIs • PMTCT • Provide care for people with HIV-related illnesses (cotrimoxazole) • Provide ART to those in need – identify people requiring continuation of ART & provide ART to those previously on treatment • Provide basic health care and support to key populations at higher risk of exposure to HIV • Expand on all programmes initiated in Minimum response phase; link to national response: • HIV awareness & community support • HIV prevention in health care settings; • Condom programming • PEP – GBV coordination mechanisms, capacity building • STIs – comprehensive public health package & STI case management • Comprehensive, integrated PMTCT, infant feeding etc. • Opportunistic infection management, nutrition care and support • Scale up ART, HBC, VCT • Key populations – sex workers Expanded
 SHUKRAN
SHUKRAN


