671486567dfac7bd5de483ea7e4ead3d.ppt
- Количество слайдов: 32
HIV AND AIDS PREVENTION DR. DOREEN ASIMBA CHS, 28. 02. 2015
Historical Background • 1981 – CDC(USA): Unexplained PCP/KS in healthy homosexual men previously • 1984 – HIV virus clearly demonstrated to be the causative agent • 1984 – First case of AIDS was described in Kenya • 1986 - Human Immunodeficiency Virus (HIV) accepted as international designation for the retrovirus in a WHO consultative meeting
Modes of Transmission n Sexual contact most important mode of transmission/acquisition of HIV worldwide n n Parenteral n n n Blood or blood products Infected blood or body fluids through contaminated sharps IDU through needle-sharing or needle stick accidents Donated organs Traditional procedures Perinatal n n Heterosexual Homosexual Non-consensual sexual exposure (assault) Transplacental, during labor/delivery and breastfeeding HIV is not transmitted by casual contact, surface contact, or from insect bites
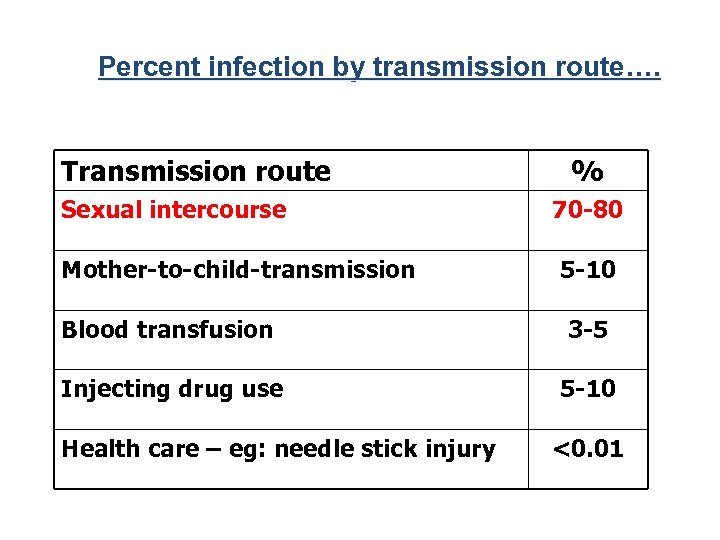
Percent infection by transmission route…. Transmission route Sexual intercourse Mother-to-child-transmission % 70 -80 5 -10 Blood transfusion 3 -5 Injecting drug use 5 -10 Health care – eg: needle stick injury <0. 01
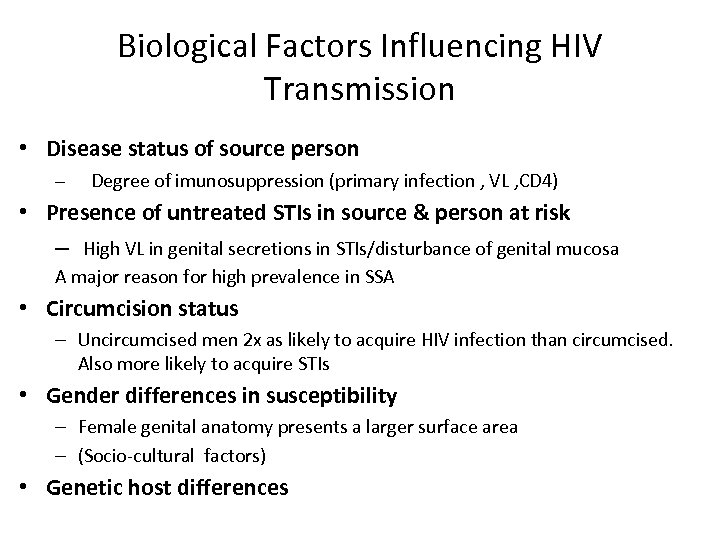
Biological Factors Influencing HIV Transmission • Disease status of source person – Degree of imunosuppression (primary infection , VL , CD 4) • Presence of untreated STIs in source & person at risk – High VL in genital secretions in STIs/disturbance of genital mucosa A major reason for high prevalence in SSA • Circumcision status – Uncircumcised men 2 x as likely to acquire HIV infection than circumcised. Also more likely to acquire STIs • Gender differences in susceptibility – Female genital anatomy presents a larger surface area – (Socio-cultural factors) • Genetic host differences
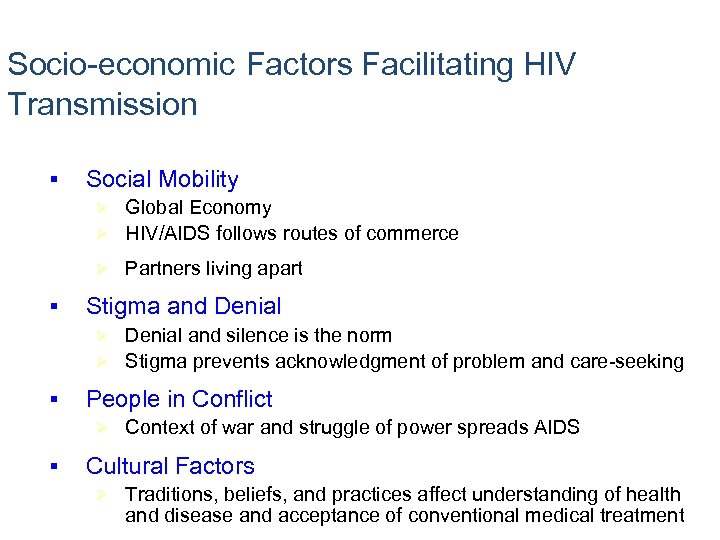
Socio-economic Factors Facilitating HIV Transmission § Social Mobility Global Economy Ø HIV/AIDS follows routes of commerce Ø Ø § Partners living apart Stigma and Denial and silence is the norm Ø Stigma prevents acknowledgment of problem and care-seeking Ø § People in Conflict Ø § Context of war and struggle of power spreads AIDS Cultural Factors Ø Traditions, beliefs, and practices affect understanding of health and disease and acceptance of conventional medical treatment
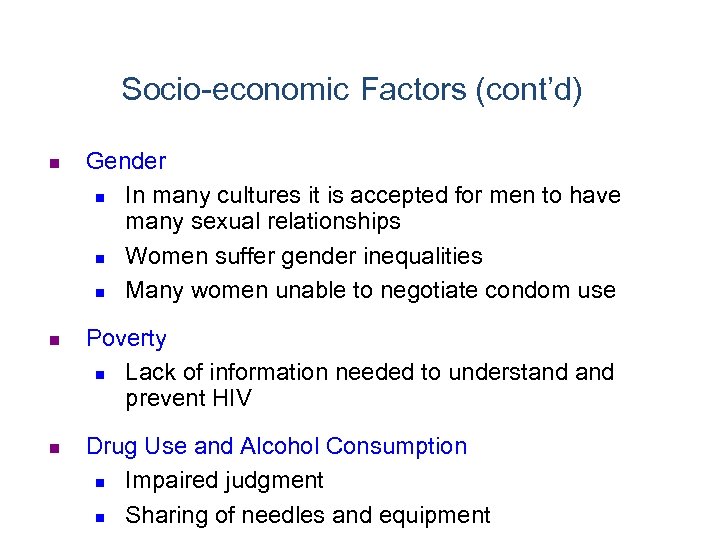
Socio-economic Factors (cont’d) n n n Gender n In many cultures it is accepted for men to have many sexual relationships n Women suffer gender inequalities n Many women unable to negotiate condom use Poverty n Lack of information needed to understand prevent HIV Drug Use and Alcohol Consumption n Impaired judgment n Sharing of needles and equipment
Behavioral Factors n n n Multiple sexual partners Unprotected sexual intercourse Large age difference between sexual partners
Natural History and Progression Of HIV Infection
HIV AND AIDS • The hallmark of HIV and AIDS is a profound immunodeficiency as a result depletion of CD 4+ T lymphocytes. • The CD 4+ T cell depletion is two fold – Reduction in numbers – Impairment in function
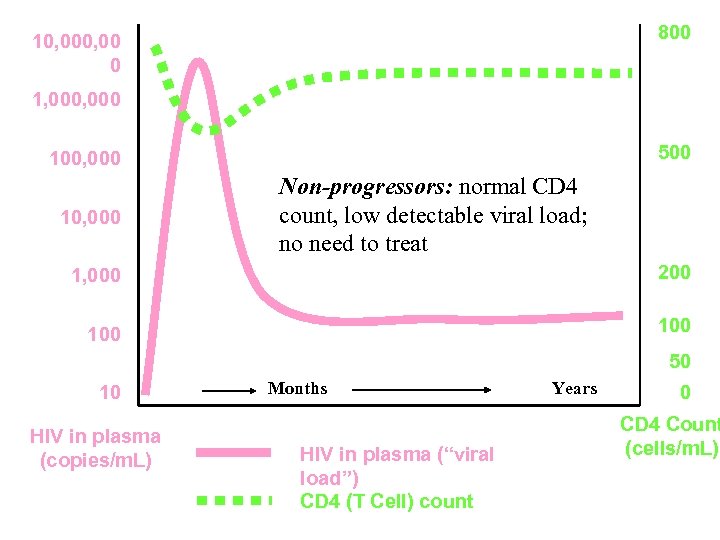
800 10, 00 0 1, 000 500 100, 000 10, 000 Non-progressors: normal CD 4 count, low detectable viral load; no need to treat 1, 000 200 100 50 10 HIV in plasma (copies/m. L) Months HIV in plasma (“viral load”) CD 4 (T Cell) count Years 0 CD 4 Count (cells/m. L)
Natural History of HIV Infection • Rapid Progressors 5– 10%, AIDS 1 -2 years • Intermediate Progressors 80 -90%, Asymptomatic 5 -8 years • Slow Progressors 5 -10%, Good immune responses 10 -15 years, Rare
Symptomatic Disease and AIDS n Viral load continues to rise causing n Increased demands on immune system as production of CD 4 cells cannot match destruction n Increased susceptibility to common infections (URTI, pneumonia, skin etc) n Late-stage disease is characterized by a CD 4 count <200 cells/mm 3 and the development of opportunistic infections, selected tumors, wasting, and neurological complications).
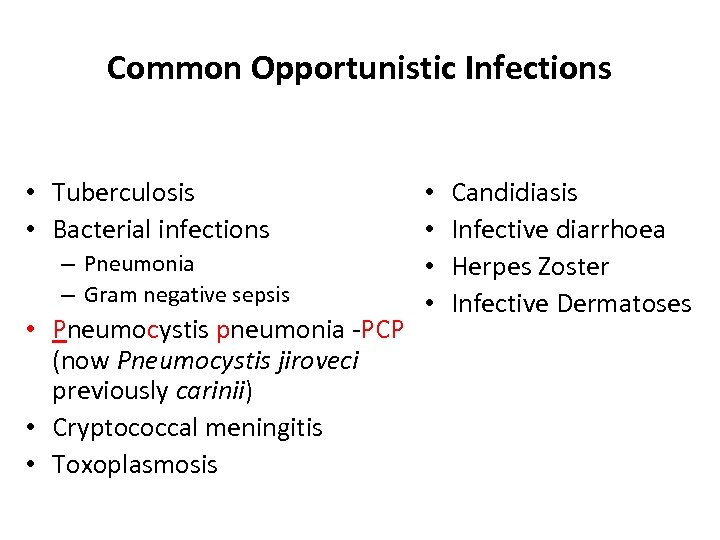
Common Opportunistic Infections • Tuberculosis • Bacterial infections – Pneumonia – Gram negative sepsis • Pneumocystis pneumonia -PCP (now Pneumocystis jiroveci previously carinii) • Cryptococcal meningitis • Toxoplasmosis • • Candidiasis Infective diarrhoea Herpes Zoster Infective Dermatoses
Opportunistic Infections • The infections are an indication of how advance the HIV disease is • Hence an indication of when to start ARVs • A major cause of stigmatization • Prevention of OIs with ARVs
Important Messages about OIs • Opportunistic infections cause the vast majority of the morbidity and mortality associated with HIV • Most are readily treatable and/or preventable • Most of these treatments are simple, available and affordable
TB and HIV • TB is the major opportunistic infection in Kenya • Since the onset of the HIV epidemic in the early eighties in Kenya, the prevalence of TB stopped falling and over the past 2 decades has risen sharply • HIV fuels the TB epidemic – HIV is the single most important risk factor for TB • >50% TB patients are HIV co-infected
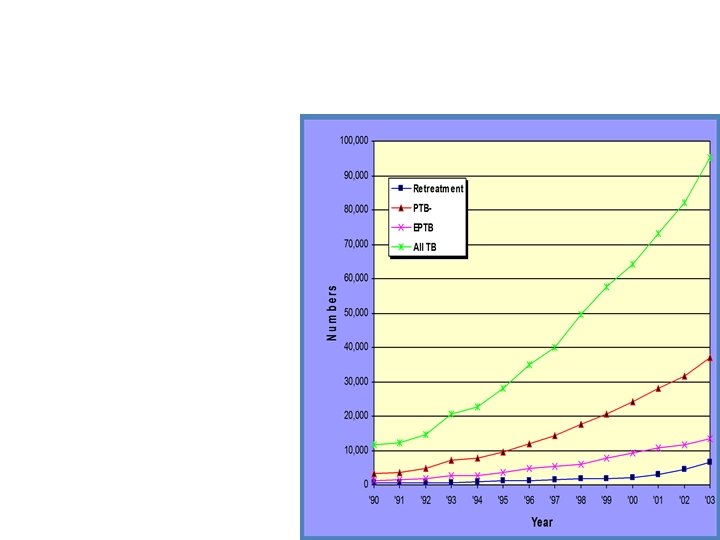
TB and HIV • TB occurs by – reactivation of latent infection – newly acquired infection • HIV increases the risk of TB progression • HIV increases the rate of TB progression • TB may speed the progression of HIV disease • ART reduces the incidence of TB in PLHA
TB/HIV: Conclusion • TB a major cause of morbidity and mortality in HIV patients • TB occurs at any stage of HIV infection • EPTB/atypical presentations of TB more common in severe HIV disease • All co-infected patients should be started on cotrimoxazole prophylaxis as it reduces mortality • HIV patients on ART remain at risk of developing TB; active case detection important
TB Preventive Strategies • Routine neonatal BCG in all children except for those with AIDS/severe immunosuppression • Effective case finding and treatment of infected and infectious people • Treatment of latent tuberculosis infection (LTBI) = INH prophylaxis – Reduces the risk of • progression of recently acquired TB • reactivation of latent TB infection – Particularly in individuals with a positive Mantoux test – Benefits last up to 2. 5 years
ART is recommended for prevention: • “ART also is recommended for HIV-infected individuals for the prevention of transmission of HIV. ” • HIV viral load directly related to probability of HIV transmission; increased ART use and lower community viral load associated with lower HIV incidence May 2014 22 www. aidsetc. org
Post-Exposure Prophylaxis (PEP) ARV prophylaxis is recommended for occupational and non-occupational high risk exposure.
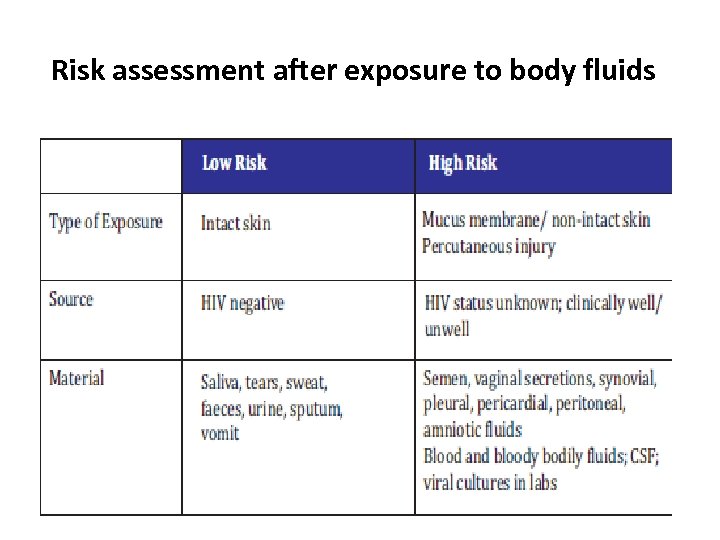
Risk assessment after exposure to body fluids
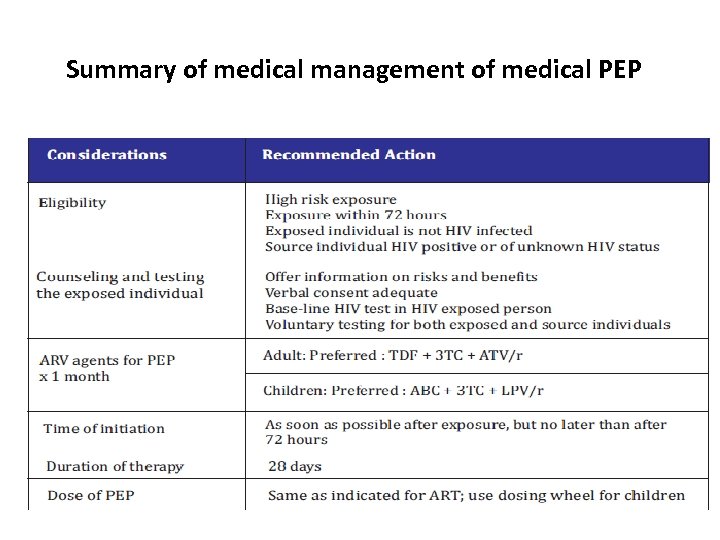
Summary of medical management of medical PEP
PRE-EXPOSURE PROPHYLAXIS (Pr. EP)
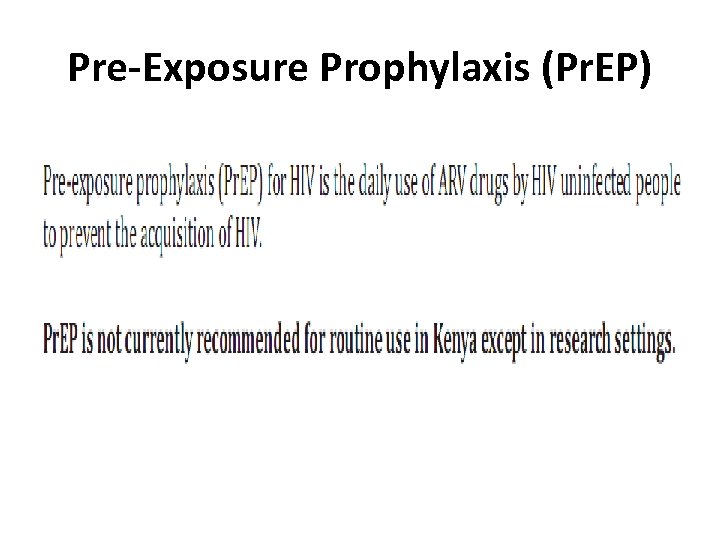
Pre-Exposure Prophylaxis (Pr. EP)
GOALS OF Pr. EP THERAPY • To reduce the acquisition of HIV infection with its resulting morbidity, mortality, and cost to individuals and society • MSM, heterosexually active men and women, and IDU who meet recommended criteria
STRATEGIES FOR PREVENTION OF HIV INFECTION: HIV NEGATIVE • Know your HIV status : HCT (testing & counseling) • • • BEHAVIOUR CHANGE & RISK REDUCTION : ABC, PMTCT: -ve children VMMC POST EXPOSURE PROPHYLAXIS PRE EXPOSURE PROPHYLAXIS CULTURAL PRACTICES (FGM, wife inheritance) EDUCATION/INFO (TBA, Public) EMPOWER THE GIRL CHILD (education) Commandment: DO NOT COMMIT ADULTERY
STRATEGIES FOR PREVENTION OF HIV TRANSMISSION : HIV POSITIVE • Behaviour change (consistent condom usage, safer sexual and drug-use practices) • Early diagnosis : HCT (testing & counseling) • Antiretroviral treatment(prevents OIs, ↓incidence of Tb, ↓ risk sexual transmission) • Detection and treatment of STIs • Early diagnosis & treatment of OIs • Stigma reduction
SUMMARY: PREVENTION STRATEGIES • • • BEHAVIOUR CHANGE & RISK REDUCTION ANTIRETROVIRAL THERAPY HCT: Early diagnosis, Early Rx POST EXPOSURE PROPHYLAXIS PMTCT VMMC
THANK YOU
671486567dfac7bd5de483ea7e4ead3d.ppt