305d3f7ad8d37d854209f003946124ec.ppt
- Количество слайдов: 70
 HIV / AIDS – 2006 An Overview for International Volunteers Allen Mc. Cutchan, MD, MSc Professor Of Medicine UCSD
HIV / AIDS – 2006 An Overview for International Volunteers Allen Mc. Cutchan, MD, MSc Professor Of Medicine UCSD
 Outline of Lecture l Origins of HIV l Virology and Clinical Features of HIV infection l History of AIDS Epidemic l Responses to the HIV Epidemic
Outline of Lecture l Origins of HIV l Virology and Clinical Features of HIV infection l History of AIDS Epidemic l Responses to the HIV Epidemic
 Origins of HIV From SIV chimpanzee Humans and chimps share ~ 98 % DNA sequences HIV from humans is similar to SIV found in chimps HIV transferred from chimps to man in 1920 s - 30 s
Origins of HIV From SIV chimpanzee Humans and chimps share ~ 98 % DNA sequences HIV from humans is similar to SIV found in chimps HIV transferred from chimps to man in 1920 s - 30 s
 Origins of HIV From SIV chimpanzee l Group M (main) HIV-1, the cause of the AIDS epidemic, passed from chimps to humans in the ~ 1920 s or 1930 s l HIV-1 emerged from Africa in the ~ mid 1970’s and was spread to Europe and American by gay men l HIV-2 , a less virulent retrovirus related to SIV African green monkey is epidemic in West Africa l Chimp to human transmission of HIV on 2 other occasions created related HIV-1 minor groups O and N
Origins of HIV From SIV chimpanzee l Group M (main) HIV-1, the cause of the AIDS epidemic, passed from chimps to humans in the ~ 1920 s or 1930 s l HIV-1 emerged from Africa in the ~ mid 1970’s and was spread to Europe and American by gay men l HIV-2 , a less virulent retrovirus related to SIV African green monkey is epidemic in West Africa l Chimp to human transmission of HIV on 2 other occasions created related HIV-1 minor groups O and N
 HIV may have infected the first persons thru “bushmeat” l Killing, butchering, and preparing primates exposes people to simian (monkey) viruses that are more deadly to people than to monkeys E 2
HIV may have infected the first persons thru “bushmeat” l Killing, butchering, and preparing primates exposes people to simian (monkey) viruses that are more deadly to people than to monkeys E 2
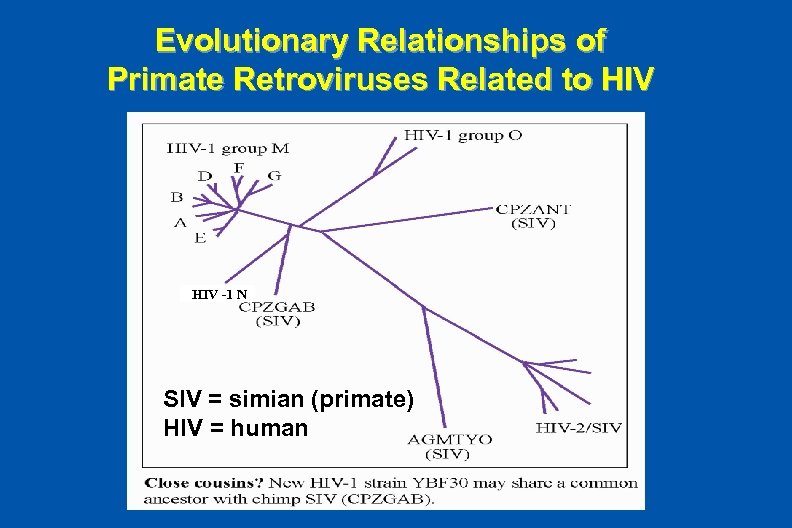 Evolutionary Relationships of Primate Retroviruses Related to HIV -1 N SIV = simian (primate) HIV = human
Evolutionary Relationships of Primate Retroviruses Related to HIV -1 N SIV = simian (primate) HIV = human
 HIV Clades l HIV rapidly evolves by two mechanisms: – Mutation - changes in single nucleosides of the RNA – Recombination – combinations of long RNA sequences from two distinct HIV strains l Distinct clades (genetic subgroups) of the M group of HIV have evolved and become dominate in specific geographic regions – A in Central Africa – B in North American and Europe – C in Southern and Eastern Africa l Several clades (eg, A/G ad A/E) are recombinants
HIV Clades l HIV rapidly evolves by two mechanisms: – Mutation - changes in single nucleosides of the RNA – Recombination – combinations of long RNA sequences from two distinct HIV strains l Distinct clades (genetic subgroups) of the M group of HIV have evolved and become dominate in specific geographic regions – A in Central Africa – B in North American and Europe – C in Southern and Eastern Africa l Several clades (eg, A/G ad A/E) are recombinants
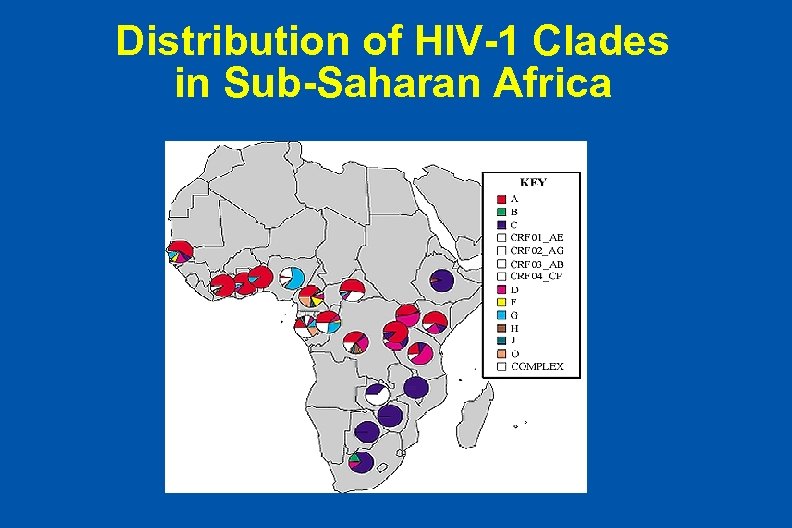 Distribution of HIV-1 Clades in Sub-Saharan Africa
Distribution of HIV-1 Clades in Sub-Saharan Africa
 Faces of HIV / AIDS Russian Mother and Daughter
Faces of HIV / AIDS Russian Mother and Daughter
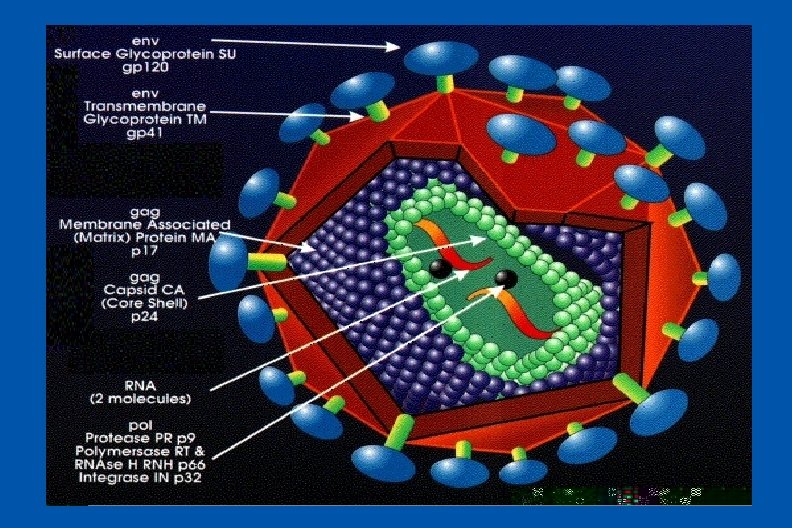
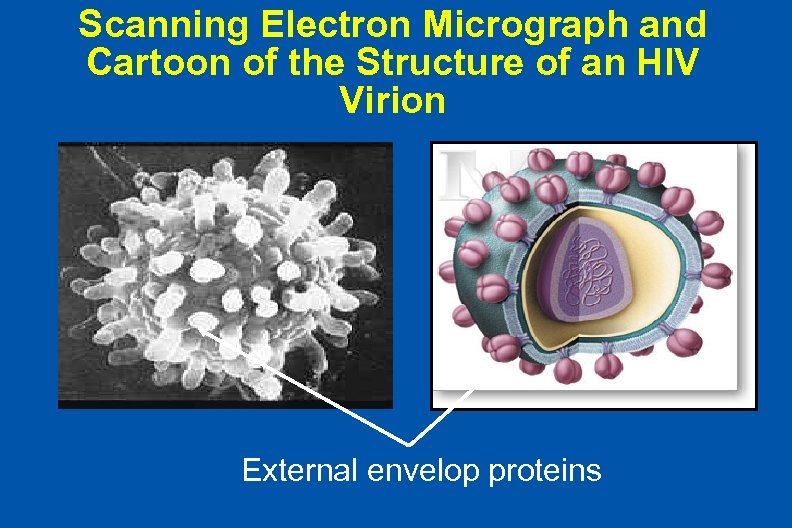 Scanning Electron Micrograph and Cartoon of the Structure of an HIV Virion External envelop proteins
Scanning Electron Micrograph and Cartoon of the Structure of an HIV Virion External envelop proteins
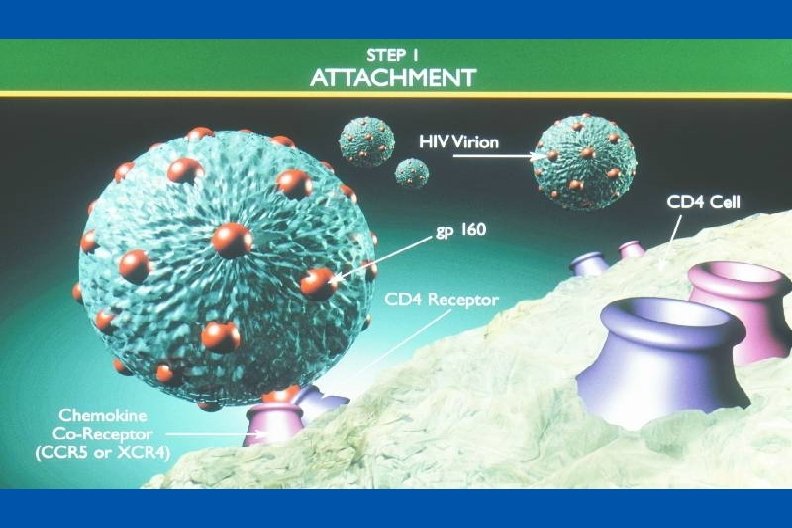
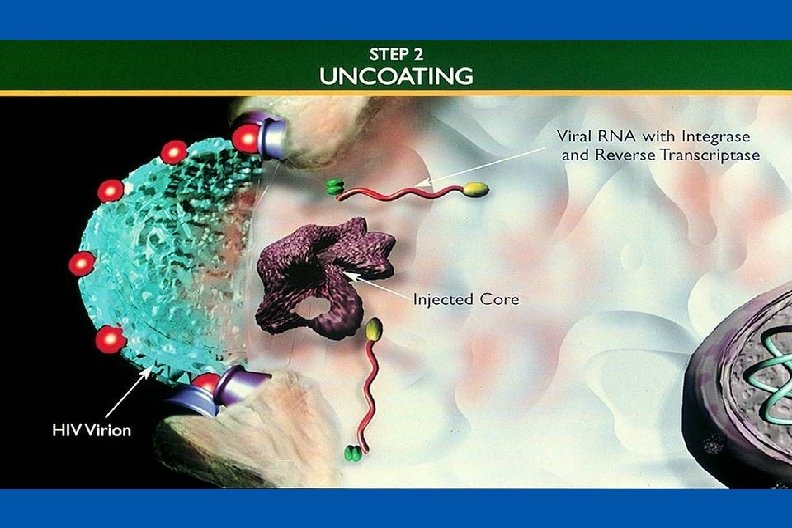
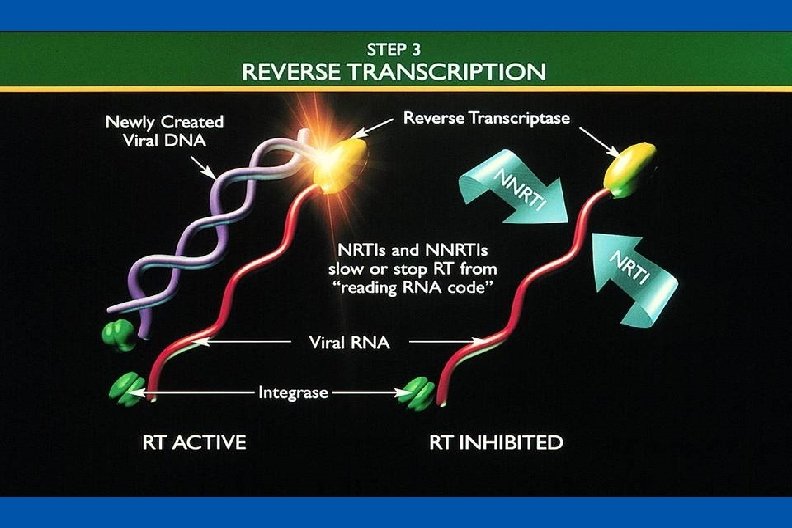
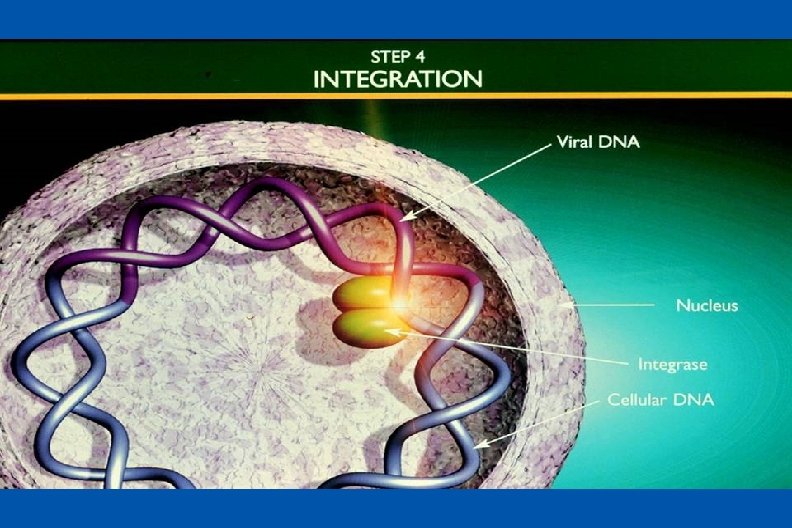
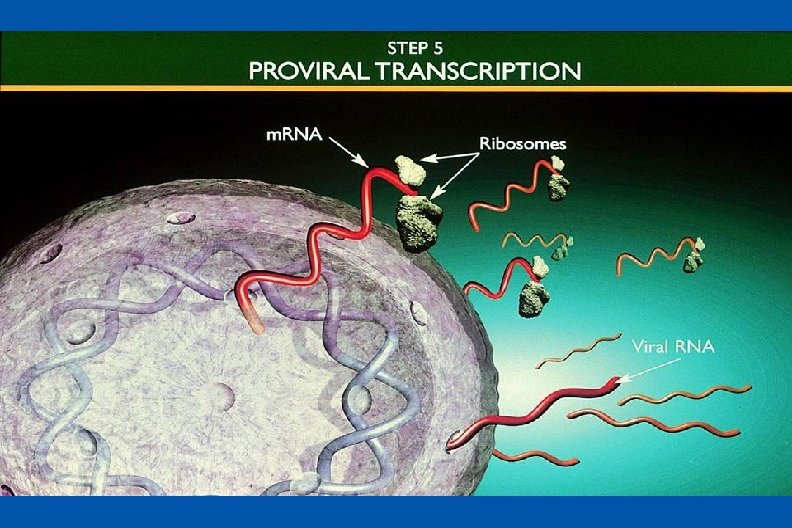
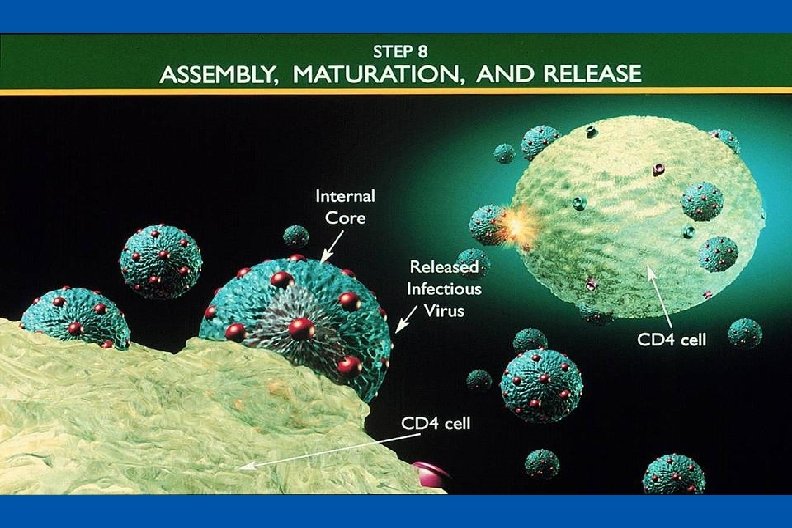
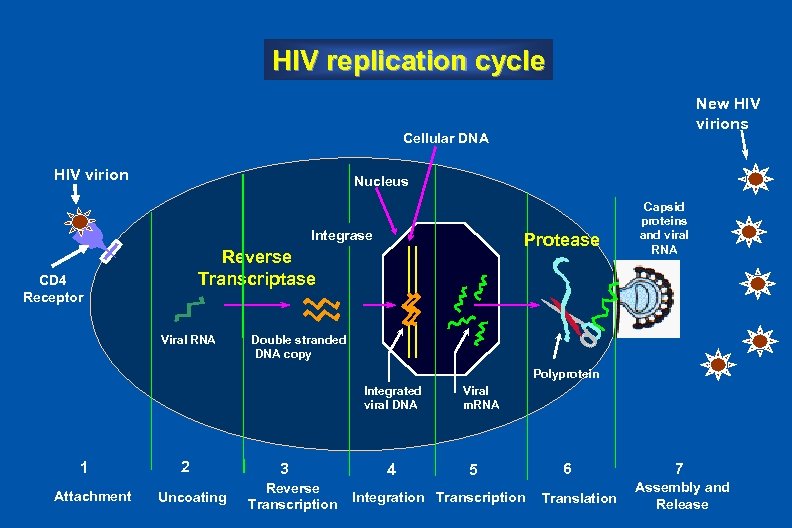 HIV replication cycle New HIV virions Cellular DNA HIV virion Nucleus HIV Virions Integrase Protease Reverse Transcriptase CD 4 Receptor Viral RNA Capsid proteins and viral RNA Double stranded DNA copy Polyprotein Integrated viral DNA 1 Attachment 2 Uncoating 3 Reverse Transcription 4 Viral m. RNA 5 Integration Transcription 6 Translation 7 Assembly and Release
HIV replication cycle New HIV virions Cellular DNA HIV virion Nucleus HIV Virions Integrase Protease Reverse Transcriptase CD 4 Receptor Viral RNA Capsid proteins and viral RNA Double stranded DNA copy Polyprotein Integrated viral DNA 1 Attachment 2 Uncoating 3 Reverse Transcription 4 Viral m. RNA 5 Integration Transcription 6 Translation 7 Assembly and Release
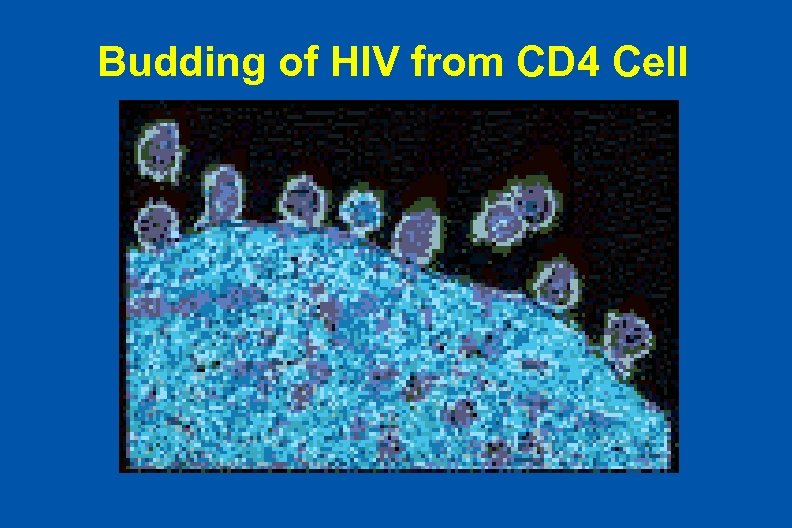 Budding of HIV from CD 4 Cell
Budding of HIV from CD 4 Cell
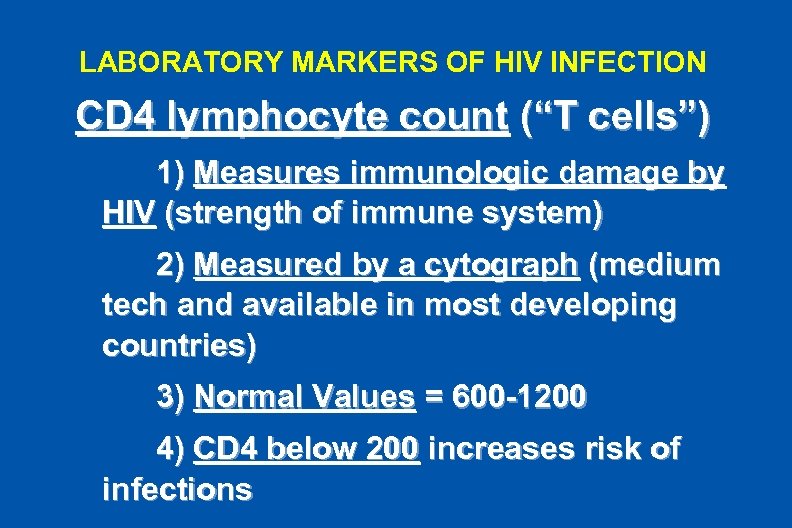 LABORATORY MARKERS OF HIV INFECTION CD 4 lymphocyte count (“T cells”) 1) Measures immunologic damage by HIV (strength of immune system) 2) Measured by a cytograph (medium tech and available in most developing countries) 3) Normal Values = 600 -1200 4) CD 4 below 200 increases risk of infections
LABORATORY MARKERS OF HIV INFECTION CD 4 lymphocyte count (“T cells”) 1) Measures immunologic damage by HIV (strength of immune system) 2) Measured by a cytograph (medium tech and available in most developing countries) 3) Normal Values = 600 -1200 4) CD 4 below 200 increases risk of infections
 Cytograph in Ethiopian Army Hospital Laboratory
Cytograph in Ethiopian Army Hospital Laboratory
 LABORATORY MARKERS OF HIV INFECTION Viral load (or HIV RNA Levels) 1) Measures concentration of HIV in blood and expressed in logarithms 100 = 2 logs 100, 000 = 5 logs) 2 ) Measured by high tech PCR Assay and thus, not widely available in developing countries
LABORATORY MARKERS OF HIV INFECTION Viral load (or HIV RNA Levels) 1) Measures concentration of HIV in blood and expressed in logarithms 100 = 2 logs 100, 000 = 5 logs) 2 ) Measured by high tech PCR Assay and thus, not widely available in developing countries
 LABORATORY MARKERS OF HIV INFECTION Uses of “viral load” a) Diagnosis - detects primary (early) infection before antibodies to HIV appear b) Prognosis - predicts CD 4 decline, clinical events, and time to death c) Monitoring treatment – measures effects of drugs
LABORATORY MARKERS OF HIV INFECTION Uses of “viral load” a) Diagnosis - detects primary (early) infection before antibodies to HIV appear b) Prognosis - predicts CD 4 decline, clinical events, and time to death c) Monitoring treatment – measures effects of drugs
 Dynamics of HIV Infections l l Rapid HIV production and human cell destruction without treatment – About 1010 (10 billion) virions are produced daily – Average life-span of HIV in plasma (free virus) is ~ 6 hours – Average life-span of an HIV-infected CD 4 lymphocytes is ~ 1. 6 days Long HIV latency and survival in human cells – HIV lies dormant even during treatment, but can revive if treatment is stopped, making cures impossible thus far
Dynamics of HIV Infections l l Rapid HIV production and human cell destruction without treatment – About 1010 (10 billion) virions are produced daily – Average life-span of HIV in plasma (free virus) is ~ 6 hours – Average life-span of an HIV-infected CD 4 lymphocytes is ~ 1. 6 days Long HIV latency and survival in human cells – HIV lies dormant even during treatment, but can revive if treatment is stopped, making cures impossible thus far
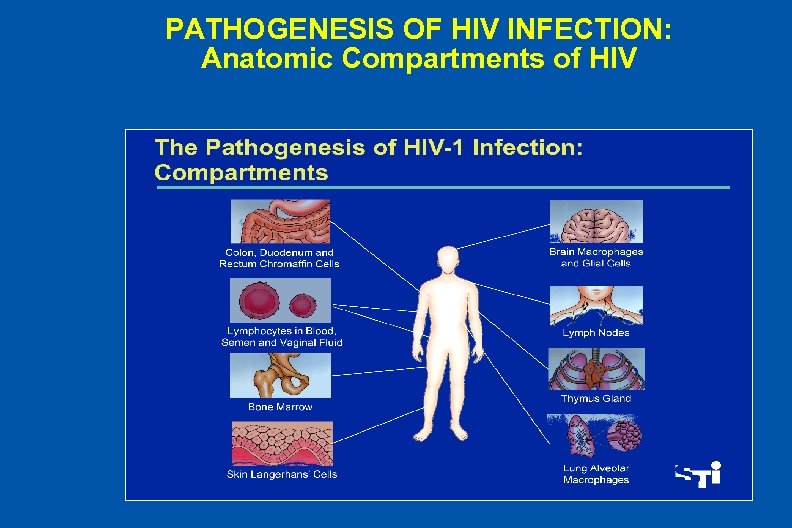 PATHOGENESIS OF HIV INFECTION: Anatomic Compartments of HIV
PATHOGENESIS OF HIV INFECTION: Anatomic Compartments of HIV
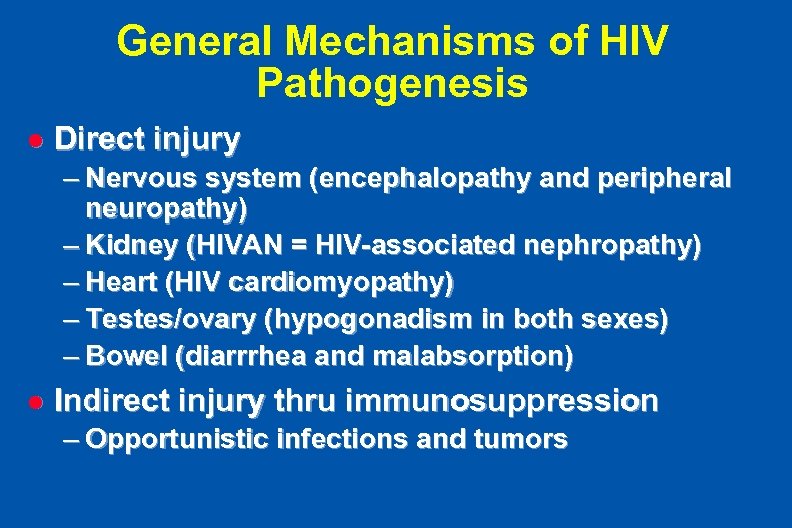 General Mechanisms of HIV Pathogenesis l Direct injury – Nervous system (encephalopathy and peripheral neuropathy) – Kidney (HIVAN = HIV-associated nephropathy) – Heart (HIV cardiomyopathy) – Testes/ovary (hypogonadism in both sexes) – Bowel (diarrrhea and malabsorption) l Indirect injury thru immunosuppression – Opportunistic infections and tumors
General Mechanisms of HIV Pathogenesis l Direct injury – Nervous system (encephalopathy and peripheral neuropathy) – Kidney (HIVAN = HIV-associated nephropathy) – Heart (HIV cardiomyopathy) – Testes/ovary (hypogonadism in both sexes) – Bowel (diarrrhea and malabsorption) l Indirect injury thru immunosuppression – Opportunistic infections and tumors
 General principles of Immune Dysfunction in HIV l l l Marked disruption of immune tissues (lymph nodes) Most cell types of the immune system are dysfunctional Persons with advanced HIV (AIDS) have – Impaired ability to respond to new infections or vaccines – Impaired ability to maintain memory responses to old infections – Susceptibility to opportunistic infections – Loss of containment of HIV replication
General principles of Immune Dysfunction in HIV l l l Marked disruption of immune tissues (lymph nodes) Most cell types of the immune system are dysfunctional Persons with advanced HIV (AIDS) have – Impaired ability to respond to new infections or vaccines – Impaired ability to maintain memory responses to old infections – Susceptibility to opportunistic infections – Loss of containment of HIV replication
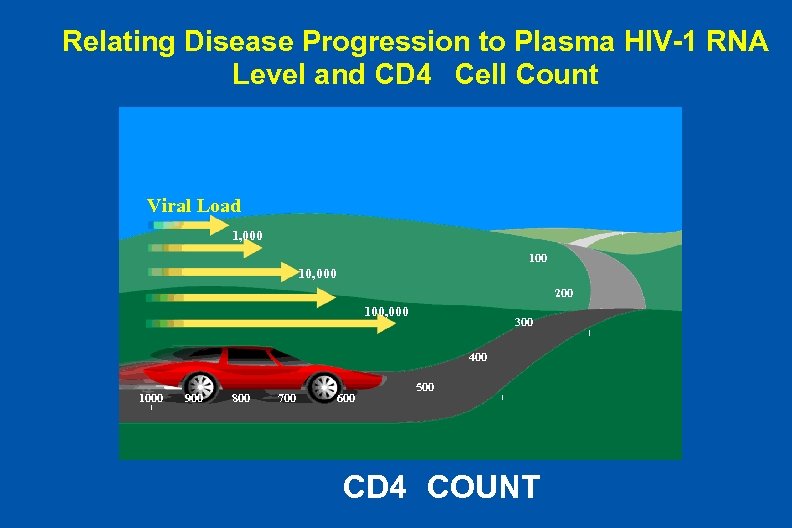 Relating Disease Progression to Plasma HIV-1 RNA Level and CD 4 Cell Count Viral Load 1, 000 10, 000 200 100, 000 300 400 1000 900 800 700 600 500 CD 4 COUNT
Relating Disease Progression to Plasma HIV-1 RNA Level and CD 4 Cell Count Viral Load 1, 000 10, 000 200 100, 000 300 400 1000 900 800 700 600 500 CD 4 COUNT
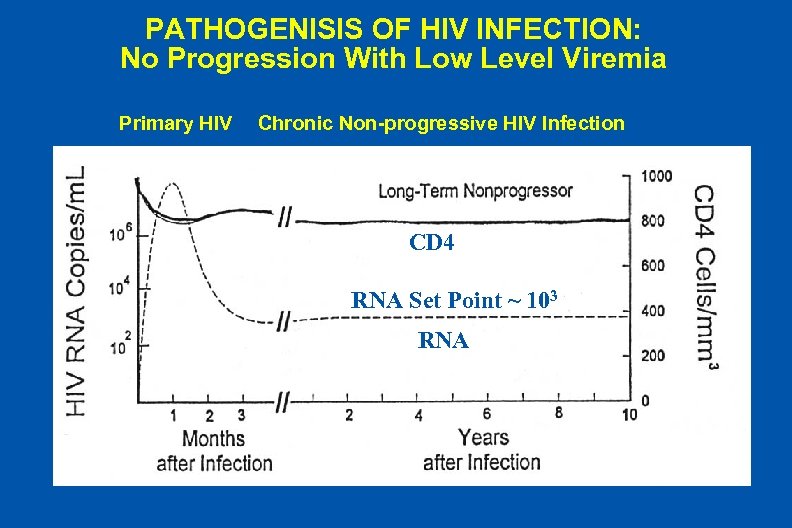 PATHOGENISIS OF HIV INFECTION: No Progression With Low Level Viremia Primary HIV Chronic Non-progressive HIV Infection CD 4 RNA Set Point ~ 103 RNA
PATHOGENISIS OF HIV INFECTION: No Progression With Low Level Viremia Primary HIV Chronic Non-progressive HIV Infection CD 4 RNA Set Point ~ 103 RNA
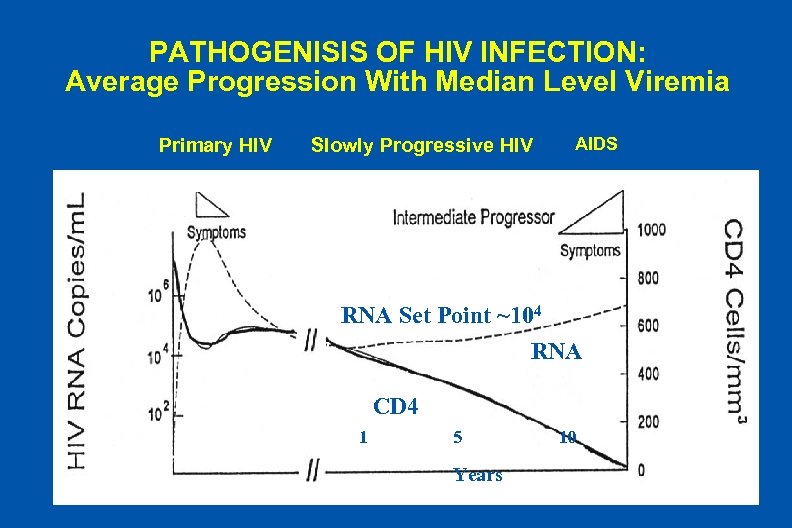 PATHOGENISIS OF HIV INFECTION: Average Progression With Median Level Viremia Primary HIV Slowly Progressive HIV AIDS RNA Set Point ~104 RNA CD 4 1 5 Years 10
PATHOGENISIS OF HIV INFECTION: Average Progression With Median Level Viremia Primary HIV Slowly Progressive HIV AIDS RNA Set Point ~104 RNA CD 4 1 5 Years 10
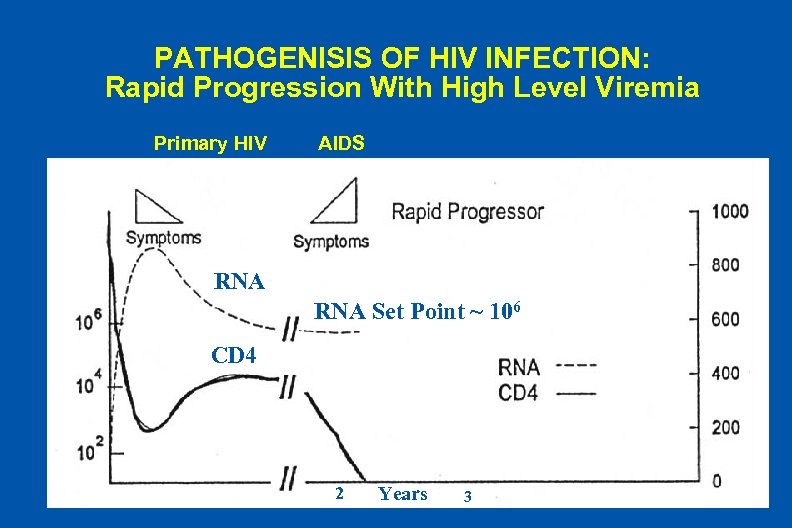 PATHOGENISIS OF HIV INFECTION: Rapid Progression With High Level Viremia Primary HIV AIDS RNA Set Point ~ 106 CD 4 2 Years 3
PATHOGENISIS OF HIV INFECTION: Rapid Progression With High Level Viremia Primary HIV AIDS RNA Set Point ~ 106 CD 4 2 Years 3
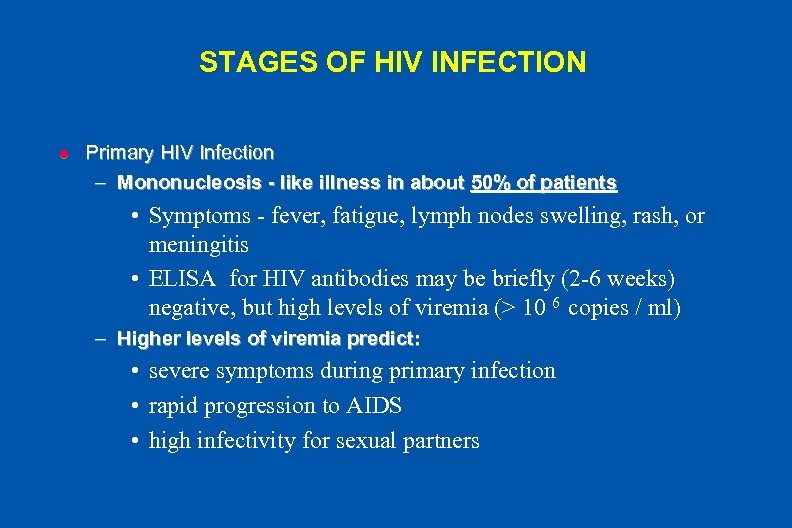 STAGES OF HIV INFECTION l Primary HIV Infection – Mononucleosis - like illness in about 50% of patients • Symptoms - fever, fatigue, lymph nodes swelling, rash, or meningitis • ELISA for HIV antibodies may be briefly (2 -6 weeks) negative, but high levels of viremia (> 10 6 copies / ml) – Higher levels of viremia predict: • severe symptoms during primary infection • rapid progression to AIDS • high infectivity for sexual partners
STAGES OF HIV INFECTION l Primary HIV Infection – Mononucleosis - like illness in about 50% of patients • Symptoms - fever, fatigue, lymph nodes swelling, rash, or meningitis • ELISA for HIV antibodies may be briefly (2 -6 weeks) negative, but high levels of viremia (> 10 6 copies / ml) – Higher levels of viremia predict: • severe symptoms during primary infection • rapid progression to AIDS • high infectivity for sexual partners
 STAGES OF HIV INFECTION l Asymptomatic Chronic Infection (Stage A) – Not always asymptomatic - patients may be vigorously healthy or have mild fatigue or low grade fevers (eg, occasional night sweats), but no illnesses indicating immunosuppression – CD 4 counts may range from normal (>500) to very low (<50) – Plasma HIV RNA levels are highly variable (5, 000 to > 106)
STAGES OF HIV INFECTION l Asymptomatic Chronic Infection (Stage A) – Not always asymptomatic - patients may be vigorously healthy or have mild fatigue or low grade fevers (eg, occasional night sweats), but no illnesses indicating immunosuppression – CD 4 counts may range from normal (>500) to very low (<50) – Plasma HIV RNA levels are highly variable (5, 000 to > 106)
 STAGES OF HIV INFECTION l Symptomatic Chronic Infection (Stages B and C) – B = History of “Minor” Opportunistic Infections (eg oral candidiasis or recurrent Herpes zoster) - see appendix 1 to lecture outline – C = History of AIDS defining opportunistic infections or tumors (eg, pneumocystis pneumonia or Kaposi Sarcoma) - see appendix 2 to lecture outline – AIDS (Acquired Immunodeficiency Syndrome) = either less than 200 CD 4+ T cells/µL or Stage C (history of any category AIDS defining condition)
STAGES OF HIV INFECTION l Symptomatic Chronic Infection (Stages B and C) – B = History of “Minor” Opportunistic Infections (eg oral candidiasis or recurrent Herpes zoster) - see appendix 1 to lecture outline – C = History of AIDS defining opportunistic infections or tumors (eg, pneumocystis pneumonia or Kaposi Sarcoma) - see appendix 2 to lecture outline – AIDS (Acquired Immunodeficiency Syndrome) = either less than 200 CD 4+ T cells/µL or Stage C (history of any category AIDS defining condition)
 CAUSES OF MORBIDITY AND MORTALITY Without sophisticated medical treatment: 1. In much of the underdeveloped world, opportunistic infections (esp, tuberculosis and diarrheal diseases) are often the first and fatal events 2. Both lead to wasting, malnutrition, and death from starvation, dehydration, and secondary pneumonias
CAUSES OF MORBIDITY AND MORTALITY Without sophisticated medical treatment: 1. In much of the underdeveloped world, opportunistic infections (esp, tuberculosis and diarrheal diseases) are often the first and fatal events 2. Both lead to wasting, malnutrition, and death from starvation, dehydration, and secondary pneumonias
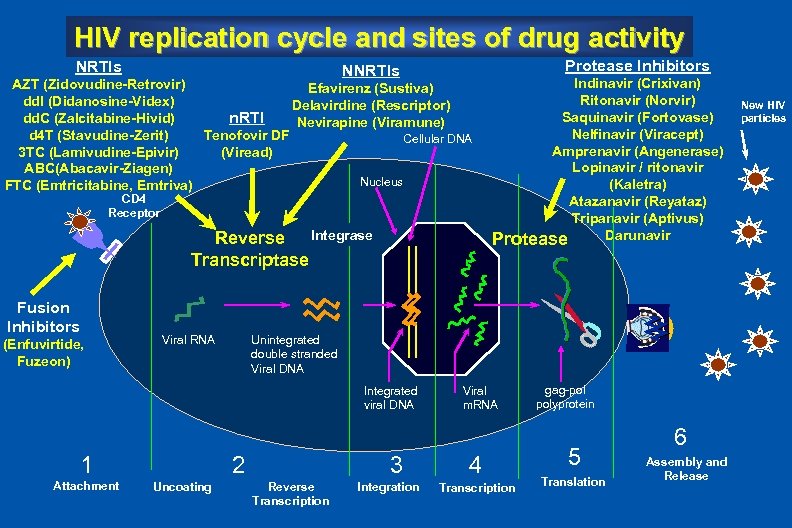 HIV replication cycle and sites of drug activity NRTIs Protease Inhibitors NNRTIs AZT (Zidovudine-Retrovir) Efavirenz (Sustiva) dd. I (Didanosine-Videx) Delavirdine (Rescriptor) n. RTI dd. C (Zalcitabine-Hivid) Nevirapine (Viramune) d 4 T (Stavudine-Zerit) Tenofovir DF Cellular DNA 3 TC (Lamivudine-Epivir) (Viread) ABC(Abacavir-Ziagen) Nucleus FTC (Emtricitabine, Emtriva) HIV Virions CD 4 Receptor Reverse Integrase Transcriptase Fusion Inhibitors (Enfuvirtide, Fuzeon) Viral RNA Unintegrated double stranded Viral DNA Integrated viral DNA 1 Attachment 3 2 Uncoating Indinavir (Crixivan) Ritonavir (Norvir) Saquinavir (Fortovase) Nelfinavir (Viracept) Amprenavir (Angenerase) Lopinavir / ritonavir (Kaletra) Atazanavir (Reyataz) Tripanavir (Aptivus) Darunavir Protease Reverse Transcription Integration Viral m. RNA 4 Transcription gag-pol polyprotein 5 Translation 6 Assembly and Release New HIV particles
HIV replication cycle and sites of drug activity NRTIs Protease Inhibitors NNRTIs AZT (Zidovudine-Retrovir) Efavirenz (Sustiva) dd. I (Didanosine-Videx) Delavirdine (Rescriptor) n. RTI dd. C (Zalcitabine-Hivid) Nevirapine (Viramune) d 4 T (Stavudine-Zerit) Tenofovir DF Cellular DNA 3 TC (Lamivudine-Epivir) (Viread) ABC(Abacavir-Ziagen) Nucleus FTC (Emtricitabine, Emtriva) HIV Virions CD 4 Receptor Reverse Integrase Transcriptase Fusion Inhibitors (Enfuvirtide, Fuzeon) Viral RNA Unintegrated double stranded Viral DNA Integrated viral DNA 1 Attachment 3 2 Uncoating Indinavir (Crixivan) Ritonavir (Norvir) Saquinavir (Fortovase) Nelfinavir (Viracept) Amprenavir (Angenerase) Lopinavir / ritonavir (Kaletra) Atazanavir (Reyataz) Tripanavir (Aptivus) Darunavir Protease Reverse Transcription Integration Viral m. RNA 4 Transcription gag-pol polyprotein 5 Translation 6 Assembly and Release New HIV particles
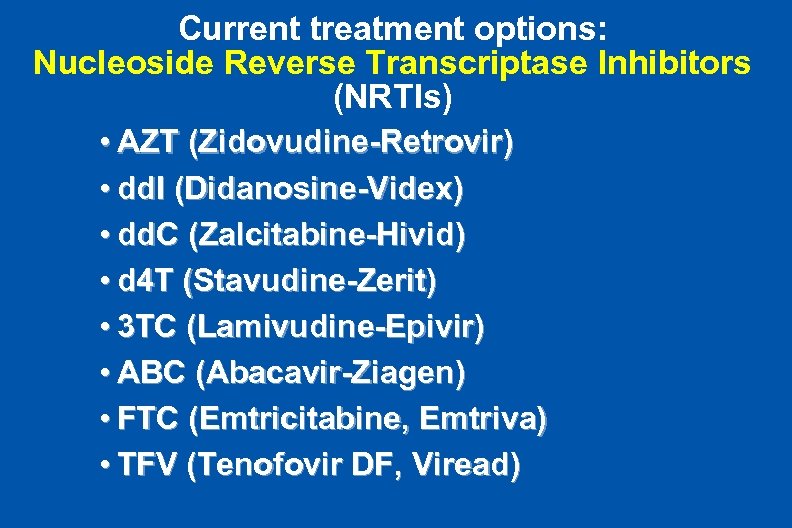 Current treatment options: Nucleoside Reverse Transcriptase Inhibitors (NRTIs) • AZT (Zidovudine-Retrovir) • dd. I (Didanosine-Videx) • dd. C (Zalcitabine-Hivid) • d 4 T (Stavudine-Zerit) • 3 TC (Lamivudine-Epivir) • ABC (Abacavir-Ziagen) • FTC (Emtricitabine, Emtriva) • TFV (Tenofovir DF, Viread)
Current treatment options: Nucleoside Reverse Transcriptase Inhibitors (NRTIs) • AZT (Zidovudine-Retrovir) • dd. I (Didanosine-Videx) • dd. C (Zalcitabine-Hivid) • d 4 T (Stavudine-Zerit) • 3 TC (Lamivudine-Epivir) • ABC (Abacavir-Ziagen) • FTC (Emtricitabine, Emtriva) • TFV (Tenofovir DF, Viread)
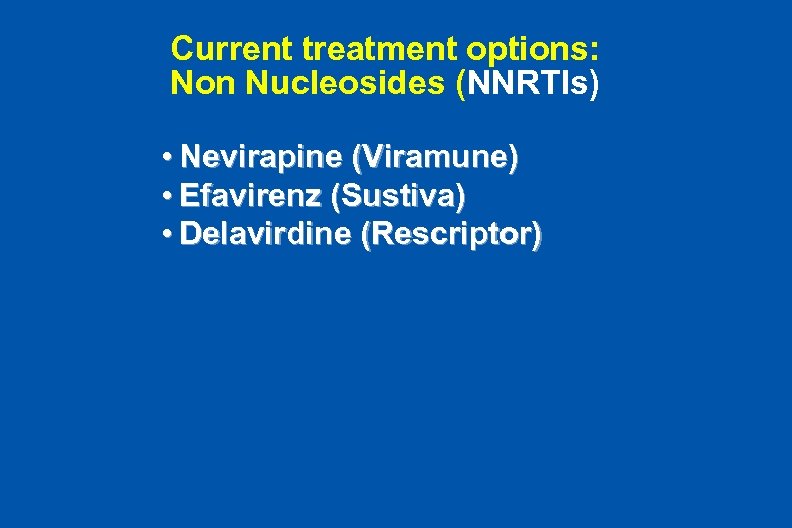 Current treatment options: Non Nucleosides (NNRTIs) • Nevirapine (Viramune) • Efavirenz (Sustiva) • Delavirdine (Rescriptor)
Current treatment options: Non Nucleosides (NNRTIs) • Nevirapine (Viramune) • Efavirenz (Sustiva) • Delavirdine (Rescriptor)
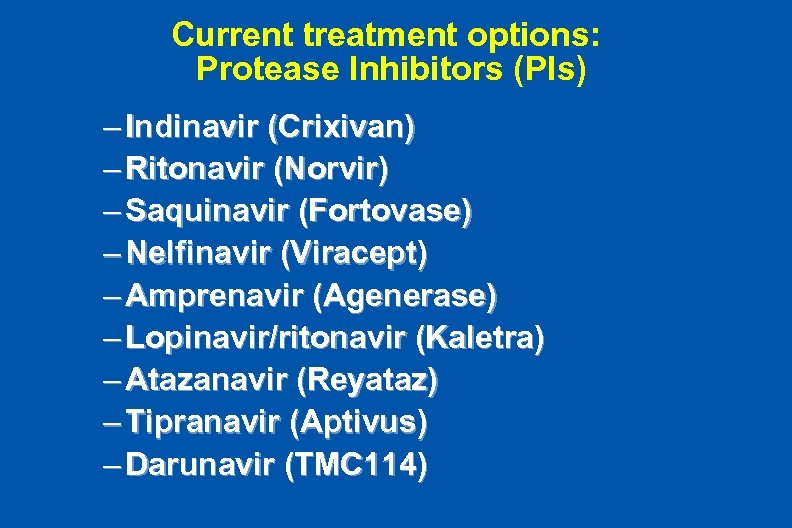 Current treatment options: Protease Inhibitors (PIs) PIs – Indinavir (Crixivan) – Ritonavir (Norvir) – Saquinavir (Fortovase) – Nelfinavir (Viracept) – Amprenavir (Agenerase) – Lopinavir/ritonavir (Kaletra) – Atazanavir (Reyataz) – Tipranavir (Aptivus) – Darunavir (TMC 114)
Current treatment options: Protease Inhibitors (PIs) PIs – Indinavir (Crixivan) – Ritonavir (Norvir) – Saquinavir (Fortovase) – Nelfinavir (Viracept) – Amprenavir (Agenerase) – Lopinavir/ritonavir (Kaletra) – Atazanavir (Reyataz) – Tipranavir (Aptivus) – Darunavir (TMC 114)
 Principles of Antiretroviral Therapy l Give ARVs in combinations of 2 -4 drugs for adequate potency to completely suppress HIV replication l Maintain adherence > 95 -98 % to avoid – failure of suppression of HIV replication – selection of drug resistant HIV because patients failing twice don’t often respond to further changes in ARVs
Principles of Antiretroviral Therapy l Give ARVs in combinations of 2 -4 drugs for adequate potency to completely suppress HIV replication l Maintain adherence > 95 -98 % to avoid – failure of suppression of HIV replication – selection of drug resistant HIV because patients failing twice don’t often respond to further changes in ARVs
 Principles of Antiretroviral Therapy l Monitor patients regularly (every 2 -6 months) for: – Symptoms of opportunistic infections (OIs such as TB ) and tumors (such as lymphoma or Kaposi’s Sarcoma) – Toxicity (blood tests and symptoms) – Adherence (question about taking ARV generally and in detail for the past 3 days)
Principles of Antiretroviral Therapy l Monitor patients regularly (every 2 -6 months) for: – Symptoms of opportunistic infections (OIs such as TB ) and tumors (such as lymphoma or Kaposi’s Sarcoma) – Toxicity (blood tests and symptoms) – Adherence (question about taking ARV generally and in detail for the past 3 days)
 Principles of Antiretroviral Therapy l Monitor patients for – Symptoms of toxicity (blood tests and symptoms) – Adherence (question about taking ARV generally and in detail for the past 3 days) – Use of other drug that might change metabolism of ARV drugs
Principles of Antiretroviral Therapy l Monitor patients for – Symptoms of toxicity (blood tests and symptoms) – Adherence (question about taking ARV generally and in detail for the past 3 days) – Use of other drug that might change metabolism of ARV drugs
 Causes of Treatment Failure Patient: Non-adherence, poor access, intolerability, advanced immunosuppression (low CD 4 counts) Drugs: Low potency, poor absorption, drug interactions, toxicities, complex dosing regimens HIV strains: High viral load, transmitted (preexisting) resistance
Causes of Treatment Failure Patient: Non-adherence, poor access, intolerability, advanced immunosuppression (low CD 4 counts) Drugs: Low potency, poor absorption, drug interactions, toxicities, complex dosing regimens HIV strains: High viral load, transmitted (preexisting) resistance
 Principles of Antiretroviral Therapy l If failure is detected as increasing viral load (HIV levels in blood) – Measure a second blood sample for viral load to confirm - ? error or brief “blip” – Question patient about adherence toxicity, and other drugs, – If applicable, provide adherence counseling and /or change to new drugs
Principles of Antiretroviral Therapy l If failure is detected as increasing viral load (HIV levels in blood) – Measure a second blood sample for viral load to confirm - ? error or brief “blip” – Question patient about adherence toxicity, and other drugs, – If applicable, provide adherence counseling and /or change to new drugs
 Adherence l Newer name for “compliance” to various components of medical care: – Attending clinic – Filling prescriptions – Taking medications as prescribed – Reporting new symptoms accurately and quickly to providers l Poor compliance with anti retroviral drugs can have serious, irreversible consequences (resistance or toxicity)
Adherence l Newer name for “compliance” to various components of medical care: – Attending clinic – Filling prescriptions – Taking medications as prescribed – Reporting new symptoms accurately and quickly to providers l Poor compliance with anti retroviral drugs can have serious, irreversible consequences (resistance or toxicity)
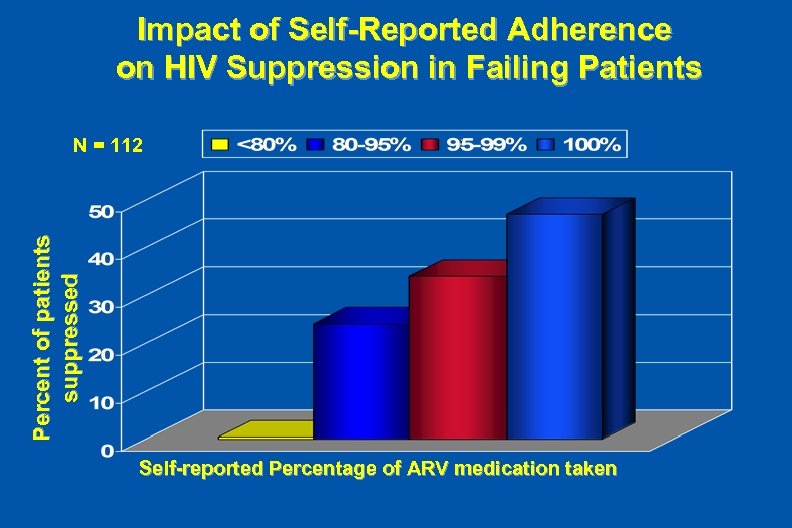 Impact of Self-Reported Adherence on HIV Suppression in Failing Patients Percent of patients suppressed N = 112 Self-reported Percentage of ARV medication taken
Impact of Self-Reported Adherence on HIV Suppression in Failing Patients Percent of patients suppressed N = 112 Self-reported Percentage of ARV medication taken
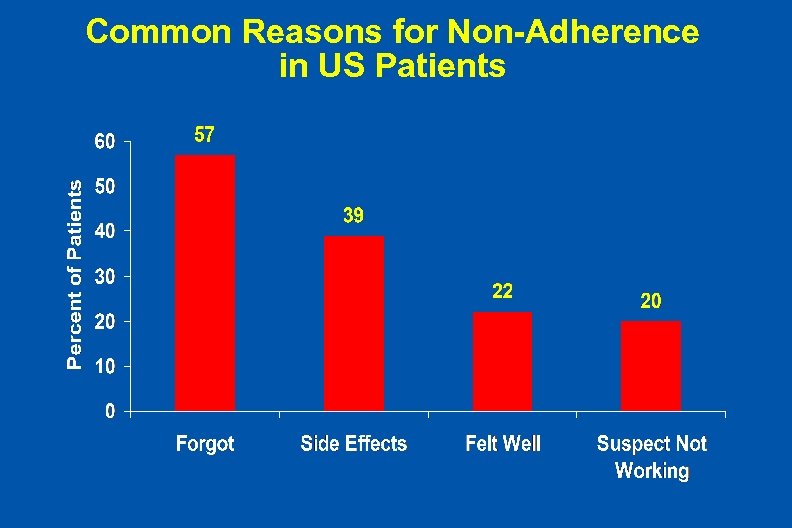 Common Reasons for Non-Adherence in US Patients
Common Reasons for Non-Adherence in US Patients
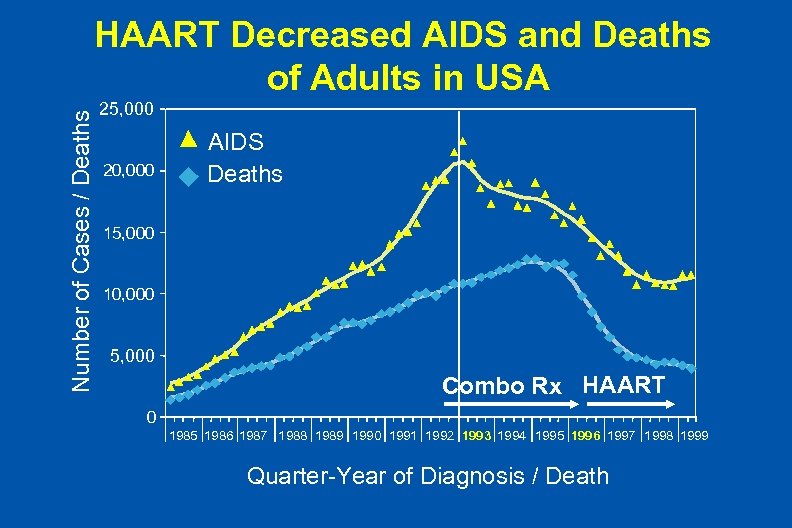 Number of Cases / Deaths HAART Decreased AIDS and Deaths of Adults in USA 25, 000 20, 000 AIDS Deaths 15, 000 10, 000 5, 000 Combo Rx HAART 0 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 Quarter-Year of Diagnosis / Death
Number of Cases / Deaths HAART Decreased AIDS and Deaths of Adults in USA 25, 000 20, 000 AIDS Deaths 15, 000 10, 000 5, 000 Combo Rx HAART 0 1985 1986 1987 1988 1989 1990 1991 1992 1993 1994 1995 1996 1997 1998 1999 Quarter-Year of Diagnosis / Death
 Russians at Summer School for HIV Volunteers
Russians at Summer School for HIV Volunteers
 History of the AIDS Epidemic – Initial definitions of a new disease 25 years ago • Case series of unusual opportunistic tumors and infections (Kaposi’s Sarcoma, PCP, HSV) in gay men in the United States (1981). – Expanded recognition (1982 -88) of: • Risk groups including transfusion recipients (including hemophiliacs), IV drug users, Haitians, and heterosexual Africans seeking treatment in Europe (1982 -84). • Clinical manifestations in new organs (eg, brain, gut, heart, kidney, and endocrine glands) • New opportunistic infections (eg, cryptococcal meningitis) were identified
History of the AIDS Epidemic – Initial definitions of a new disease 25 years ago • Case series of unusual opportunistic tumors and infections (Kaposi’s Sarcoma, PCP, HSV) in gay men in the United States (1981). – Expanded recognition (1982 -88) of: • Risk groups including transfusion recipients (including hemophiliacs), IV drug users, Haitians, and heterosexual Africans seeking treatment in Europe (1982 -84). • Clinical manifestations in new organs (eg, brain, gut, heart, kidney, and endocrine glands) • New opportunistic infections (eg, cryptococcal meningitis) were identified
 History of the AIDS Epidemic – Retroviral cause of AIDS (HIV) discovered in 3 laboratories (Montagnier, Gallo, and Levi, 1985) – Diagnostic methods devised to assess HIV infection by detecting antibodies and levels of immunosuppression • ELISA and immunoblotting for HIV infection developed soon after HIV was isolated (1986) • Criteria for case definitions for AIDS, opportunistic infections (OIs), organ-specific syndromes (e. g. , dementia), and acute HIV infections followed (1987 -88) • CD 4 lymphocyte depletion noted initially (1981) were found to predict risk of progression to OIs and death
History of the AIDS Epidemic – Retroviral cause of AIDS (HIV) discovered in 3 laboratories (Montagnier, Gallo, and Levi, 1985) – Diagnostic methods devised to assess HIV infection by detecting antibodies and levels of immunosuppression • ELISA and immunoblotting for HIV infection developed soon after HIV was isolated (1986) • Criteria for case definitions for AIDS, opportunistic infections (OIs), organ-specific syndromes (e. g. , dementia), and acute HIV infections followed (1987 -88) • CD 4 lymphocyte depletion noted initially (1981) were found to predict risk of progression to OIs and death
 History of the AIDS Epidemic – Anti-OI and Anti-retroviral therapy • Treatment and prophylaxis of opportunistic infections (eg, PCP, MAC, and CMV) (1983 -90) • Antiretroviral drugs of several classes - [1987 (AZT), 1996 (Protease Inhibitors (= PI) and NNRTI), presently 21 agents approved • Perinatal prophylaxis to prevent maternal-child transmission (1992) • Assays for HIV in blood improve management of ARV drugs by providing feedback of their effects (1996) • Delayed treatment strategy adopted because: – Safety demonstrated for patients with high CD 4 counts – Metabolic complications of long term ARV therapy
History of the AIDS Epidemic – Anti-OI and Anti-retroviral therapy • Treatment and prophylaxis of opportunistic infections (eg, PCP, MAC, and CMV) (1983 -90) • Antiretroviral drugs of several classes - [1987 (AZT), 1996 (Protease Inhibitors (= PI) and NNRTI), presently 21 agents approved • Perinatal prophylaxis to prevent maternal-child transmission (1992) • Assays for HIV in blood improve management of ARV drugs by providing feedback of their effects (1996) • Delayed treatment strategy adopted because: – Safety demonstrated for patients with high CD 4 counts – Metabolic complications of long term ARV therapy
 Faces of HIV/AIDS HIV-infected Activist from Chad
Faces of HIV/AIDS HIV-infected Activist from Chad
 Future of the HIV Epidemic l Major current and future interventions against HIV – behavioral prevention - both a sociopolitical and technical (social marketing) problem – treatment - a complex, but soluble problem, with current medications dependent on massive aid and technical assistance – vaccines - a technical problem, not likely to be available soon
Future of the HIV Epidemic l Major current and future interventions against HIV – behavioral prevention - both a sociopolitical and technical (social marketing) problem – treatment - a complex, but soluble problem, with current medications dependent on massive aid and technical assistance – vaccines - a technical problem, not likely to be available soon
 Principles of Responding to the HIV Eidemic l Test - increase voluntary testing in health care settings and tie to accessible treatment, start with interruption of maternal transmission to neonates with simple, short oral regimens l Treat - provide drugs and support medical and public health infrastructure for treating HIV , TB, and related diseases, using donations from developed world and beginning in Africa l Prevent - focus on infected persons as vectors and drugs to prevent maternal-child transmission l Count - build surveillance and research into delivery of all the above interventions to assess and improve each component
Principles of Responding to the HIV Eidemic l Test - increase voluntary testing in health care settings and tie to accessible treatment, start with interruption of maternal transmission to neonates with simple, short oral regimens l Treat - provide drugs and support medical and public health infrastructure for treating HIV , TB, and related diseases, using donations from developed world and beginning in Africa l Prevent - focus on infected persons as vectors and drugs to prevent maternal-child transmission l Count - build surveillance and research into delivery of all the above interventions to assess and improve each component
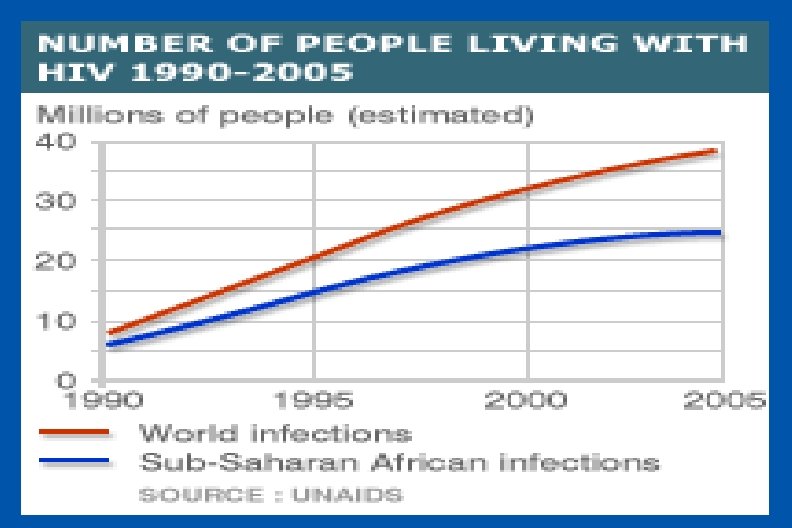
 Current Responses to the Global HIV Epidemic l Total support of anti-HIV activity has increased rapidly over past 5 years thru aid from USG and UN Global Fund – Initial aid was targeted only to HIV prevention – HIV treatment now supported as prices of generic drugs made in India and Brazil have dropped (350 -500 US$/year) – Tuberculosis, the major complication of HIV in Africans, is being simultaneously addressed – Some countries such as Thailand, Uganda and Botswana have reduced rates of new HIV infections thru public education, but many other countries have responded inadequately
Current Responses to the Global HIV Epidemic l Total support of anti-HIV activity has increased rapidly over past 5 years thru aid from USG and UN Global Fund – Initial aid was targeted only to HIV prevention – HIV treatment now supported as prices of generic drugs made in India and Brazil have dropped (350 -500 US$/year) – Tuberculosis, the major complication of HIV in Africans, is being simultaneously addressed – Some countries such as Thailand, Uganda and Botswana have reduced rates of new HIV infections thru public education, but many other countries have responded inadequately
 Responding to AIDS In the Underdeveloped World l Major problems in the developing nations – Poorly educated populations without experience or skills in using medications for chronic diseases – Denial of seriousness and implications of epidemic – Political instability, war, and corruption – Poverty - limitations of infrastructure and trained personnel for delivery of a massive program of health care, especially in rural areas
Responding to AIDS In the Underdeveloped World l Major problems in the developing nations – Poorly educated populations without experience or skills in using medications for chronic diseases – Denial of seriousness and implications of epidemic – Political instability, war, and corruption – Poverty - limitations of infrastructure and trained personnel for delivery of a massive program of health care, especially in rural areas
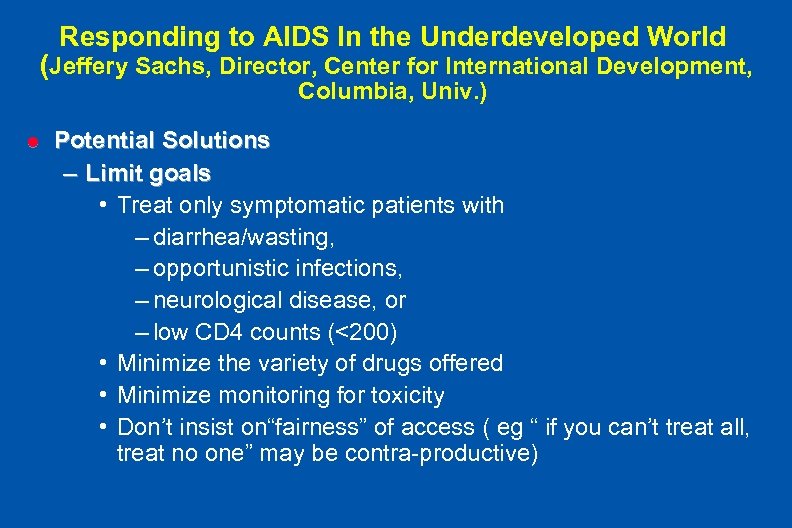 Responding to AIDS In the Underdeveloped World (Jeffery Sachs, Director, Center for International Development, Columbia, Univ. ) l Potential Solutions – Limit goals • Treat only symptomatic patients with – diarrhea/wasting, – opportunistic infections, – neurological disease, or – low CD 4 counts (<200) • Minimize the variety of drugs offered • Minimize monitoring for toxicity • Don’t insist on“fairness” of access ( eg “ if you can’t treat all, treat no one” may be contra-productive)
Responding to AIDS In the Underdeveloped World (Jeffery Sachs, Director, Center for International Development, Columbia, Univ. ) l Potential Solutions – Limit goals • Treat only symptomatic patients with – diarrhea/wasting, – opportunistic infections, – neurological disease, or – low CD 4 counts (<200) • Minimize the variety of drugs offered • Minimize monitoring for toxicity • Don’t insist on“fairness” of access ( eg “ if you can’t treat all, treat no one” may be contra-productive)
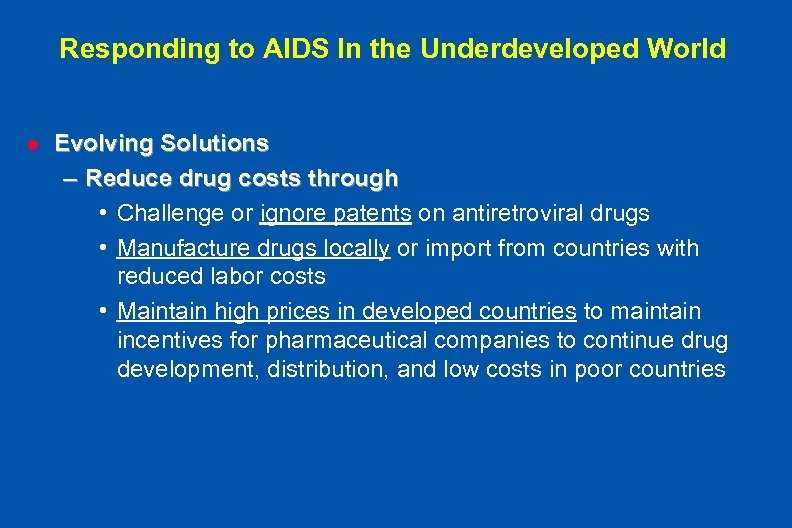 Responding to AIDS In the Underdeveloped World l Evolving Solutions – Reduce drug costs through • Challenge or ignore patents on antiretroviral drugs • Manufacture drugs locally or import from countries with reduced labor costs • Maintain high prices in developed countries to maintain incentives for pharmaceutical companies to continue drug development, distribution, and low costs in poor countries
Responding to AIDS In the Underdeveloped World l Evolving Solutions – Reduce drug costs through • Challenge or ignore patents on antiretroviral drugs • Manufacture drugs locally or import from countries with reduced labor costs • Maintain high prices in developed countries to maintain incentives for pharmaceutical companies to continue drug development, distribution, and low costs in poor countries
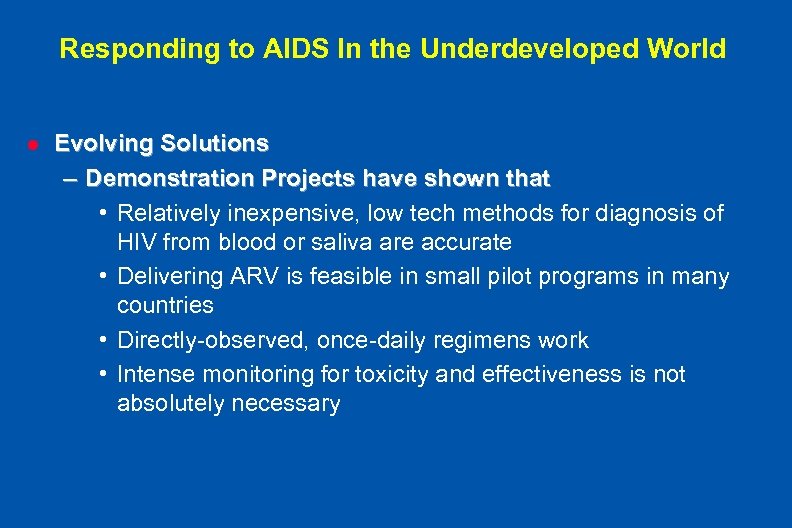 Responding to AIDS In the Underdeveloped World l Evolving Solutions – Demonstration Projects have shown that • Relatively inexpensive, low tech methods for diagnosis of HIV from blood or saliva are accurate • Delivering ARV is feasible in small pilot programs in many countries • Directly-observed, once-daily regimens work • Intense monitoring for toxicity and effectiveness is not absolutely necessary
Responding to AIDS In the Underdeveloped World l Evolving Solutions – Demonstration Projects have shown that • Relatively inexpensive, low tech methods for diagnosis of HIV from blood or saliva are accurate • Delivering ARV is feasible in small pilot programs in many countries • Directly-observed, once-daily regimens work • Intense monitoring for toxicity and effectiveness is not absolutely necessary
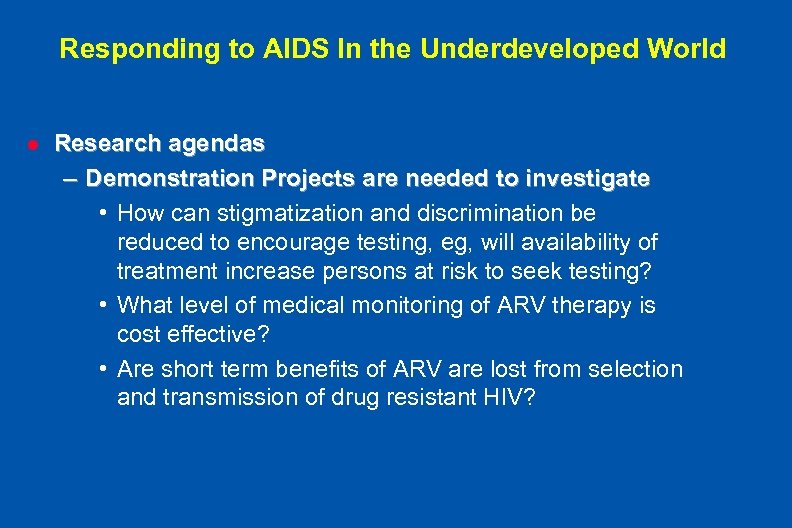 Responding to AIDS In the Underdeveloped World l Research agendas – Demonstration Projects are needed to investigate • How can stigmatization and discrimination be reduced to encourage testing, eg, will availability of treatment increase persons at risk to seek testing? • What level of medical monitoring of ARV therapy is cost effective? • Are short term benefits of ARV are lost from selection and transmission of drug resistant HIV?
Responding to AIDS In the Underdeveloped World l Research agendas – Demonstration Projects are needed to investigate • How can stigmatization and discrimination be reduced to encourage testing, eg, will availability of treatment increase persons at risk to seek testing? • What level of medical monitoring of ARV therapy is cost effective? • Are short term benefits of ARV are lost from selection and transmission of drug resistant HIV?
 Responding to AIDS In the Underdeveloped World l Effects of treating – Motivates infected persons to seek testing – Decreases new infections by decreasing HIV in genital secretions – Conserves human capital for economic development
Responding to AIDS In the Underdeveloped World l Effects of treating – Motivates infected persons to seek testing – Decreases new infections by decreasing HIV in genital secretions – Conserves human capital for economic development
 Faces of HIV/AIDS HIV-infected Couple, India
Faces of HIV/AIDS HIV-infected Couple, India
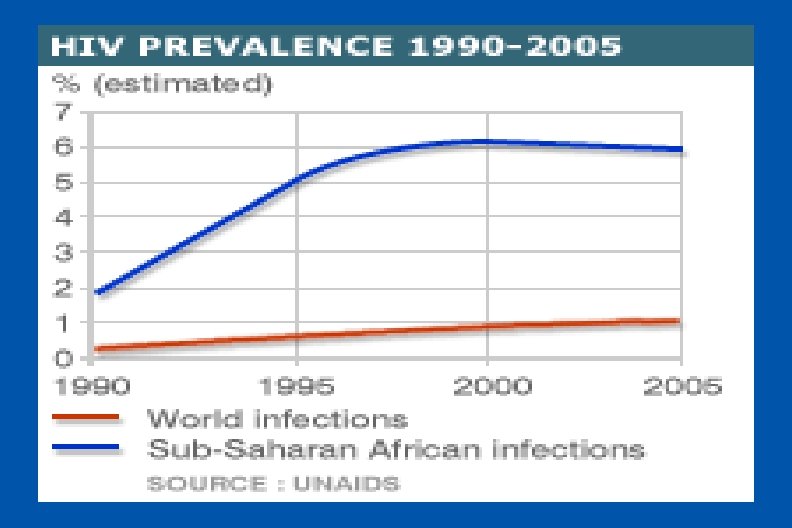
 Why Be Hopeful? l Prevention is working – prevalence is stabilizing or falling in many countres in sub-Saharan Africa l Technical progress has reduced costs of therapy – Costs of testing for HIV are low (<$10 / test ) – Costs of generic drugs is $300 - 500 / person / year – Therapy can be delivered by DOT and monitored for as little as $450 / person / year
Why Be Hopeful? l Prevention is working – prevalence is stabilizing or falling in many countres in sub-Saharan Africa l Technical progress has reduced costs of therapy – Costs of testing for HIV are low (<$10 / test ) – Costs of generic drugs is $300 - 500 / person / year – Therapy can be delivered by DOT and monitored for as little as $450 / person / year
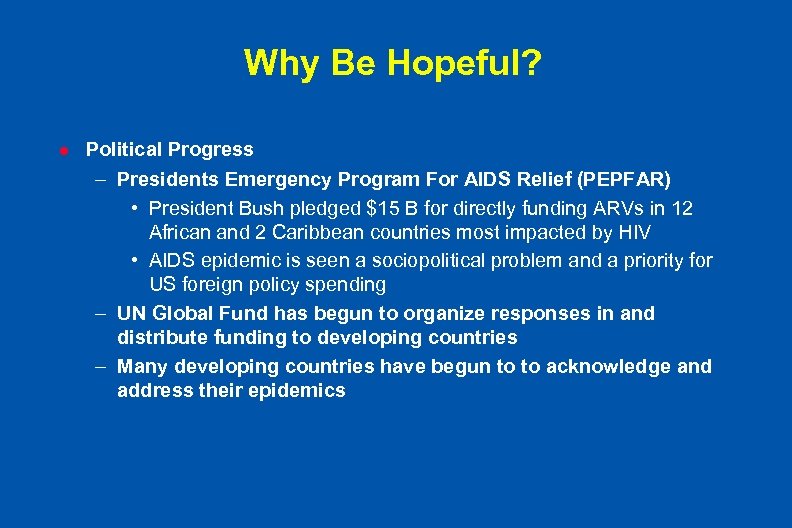 Why Be Hopeful? l Political Progress – Presidents Emergency Program For AIDS Relief (PEPFAR) • President Bush pledged $15 B for directly funding ARVs in 12 African and 2 Caribbean countries most impacted by HIV • AIDS epidemic is seen a sociopolitical problem and a priority for US foreign policy spending – UN Global Fund has begun to organize responses in and distribute funding to developing countries – Many developing countries have begun to to acknowledge and address their epidemics
Why Be Hopeful? l Political Progress – Presidents Emergency Program For AIDS Relief (PEPFAR) • President Bush pledged $15 B for directly funding ARVs in 12 African and 2 Caribbean countries most impacted by HIV • AIDS epidemic is seen a sociopolitical problem and a priority for US foreign policy spending – UN Global Fund has begun to organize responses in and distribute funding to developing countries – Many developing countries have begun to to acknowledge and address their epidemics
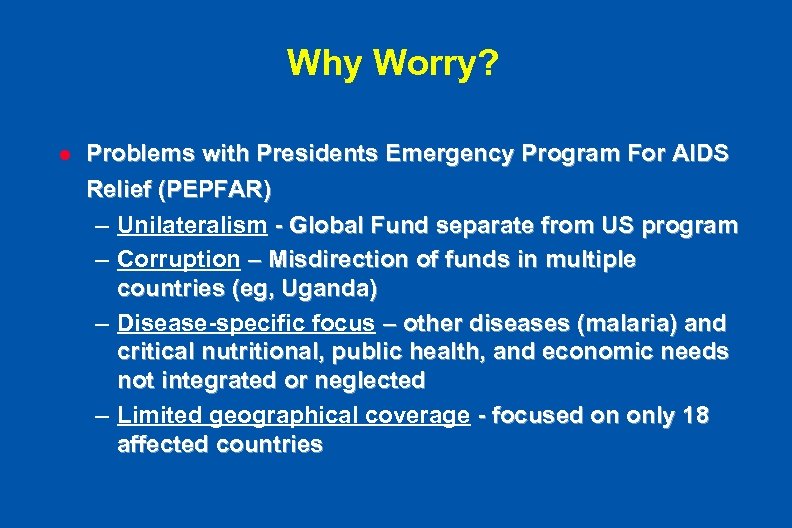 Why Worry? l Problems with Presidents Emergency Program For AIDS Relief (PEPFAR) – Unilateralism - Global Fund separate from US program – Corruption – Misdirection of funds in multiple countries (eg, Uganda) – Disease-specific focus – other diseases (malaria) and critical nutritional, public health, and economic needs not integrated or neglected – Limited geographical coverage - focused on only 18 affected countries
Why Worry? l Problems with Presidents Emergency Program For AIDS Relief (PEPFAR) – Unilateralism - Global Fund separate from US program – Corruption – Misdirection of funds in multiple countries (eg, Uganda) – Disease-specific focus – other diseases (malaria) and critical nutritional, public health, and economic needs not integrated or neglected – Limited geographical coverage - focused on only 18 affected countries
 Why Worry? l Consequences of Failure to Implement PEPFAR Effectively – Millions of lives lost and diminished – Socioeconomic development of Africa and Asia delayed – Future “medical foreign aid “ stigmatized
Why Worry? l Consequences of Failure to Implement PEPFAR Effectively – Millions of lives lost and diminished – Socioeconomic development of Africa and Asia delayed – Future “medical foreign aid “ stigmatized
 Information sources l UNAIDS web site (www. unaids. org) l Centers for Disease Control w. EB site (www. cdc. gov) l UCSD AIDS Research Institute web site (hsrd. ucsd. edu/cfar/admin. html)
Information sources l UNAIDS web site (www. unaids. org) l Centers for Disease Control w. EB site (www. cdc. gov) l UCSD AIDS Research Institute web site (hsrd. ucsd. edu/cfar/admin. html)


