bbeef2f5a3f810f2ee0c112784ca9067.ppt
- Количество слайдов: 78
 HEMORRHAGIC DIATHESIS
HEMORRHAGIC DIATHESIS
 HEMORRHAGIC DIATHESIS IS A DISEASE, CHARACTERIZED BY EXCESSIVE BLEEDING. ACCORDING TO PATHOGENESIS, IT IS CLASSIFIED INTO COAGULOPATHY, PLATELET DISORDER (THROMBOCYTOPENIA AND THROMBOCYTOPATHY) AND VASOPATHY. EACH TYPE IS SUBDIVIDED INTO CONGENITAL AND ACQUIRED.
HEMORRHAGIC DIATHESIS IS A DISEASE, CHARACTERIZED BY EXCESSIVE BLEEDING. ACCORDING TO PATHOGENESIS, IT IS CLASSIFIED INTO COAGULOPATHY, PLATELET DISORDER (THROMBOCYTOPENIA AND THROMBOCYTOPATHY) AND VASOPATHY. EACH TYPE IS SUBDIVIDED INTO CONGENITAL AND ACQUIRED.
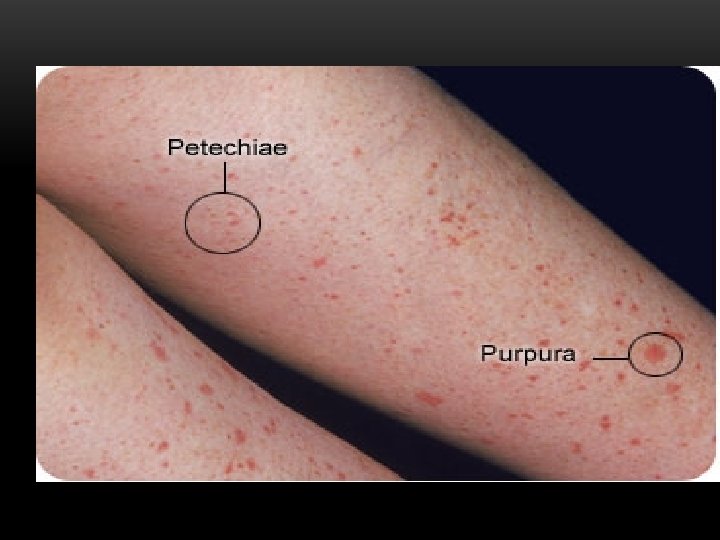
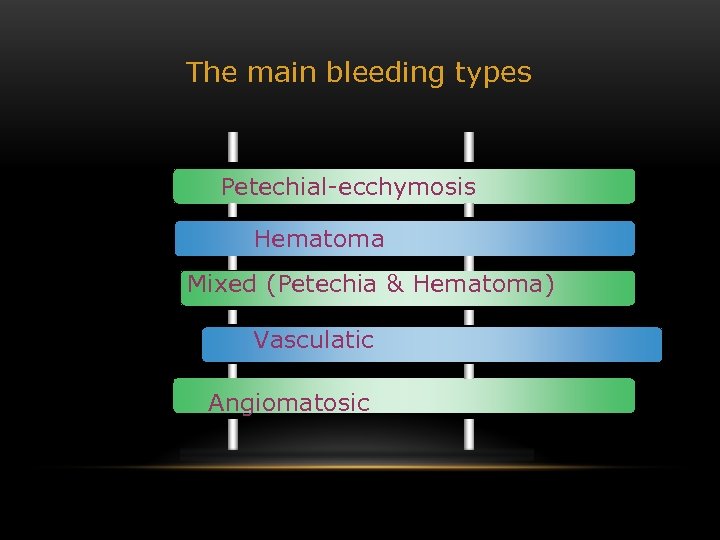 The main bleeding types Petechial-ecchymosis Hematoma Mixed (Petechia & Hematoma) Vasculatic Angiomatosic
The main bleeding types Petechial-ecchymosis Hematoma Mixed (Petechia & Hematoma) Vasculatic Angiomatosic
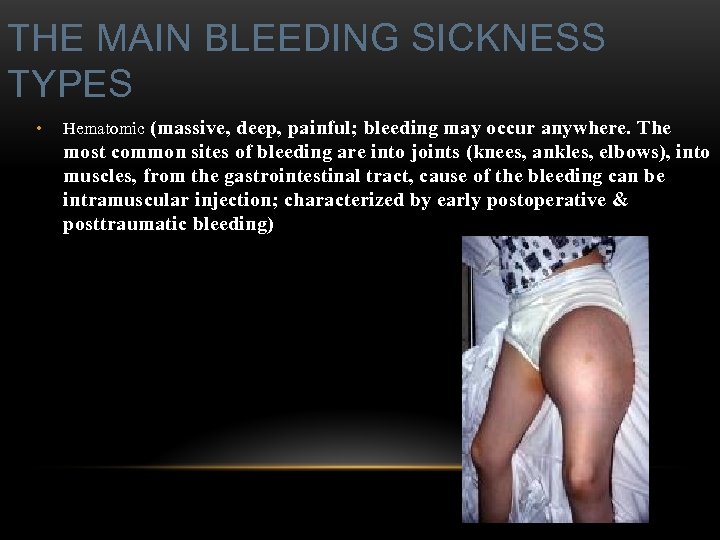 THE MAIN BLEEDING SICKNESS TYPES • Hematomic (massive, deep, painful; bleeding may occur anywhere. The most common sites of bleeding are into joints (knees, ankles, elbows), into muscles, from the gastrointestinal tract, cause of the bleeding can be intramuscular injection; characterized by early postoperative & posttraumatic bleeding)
THE MAIN BLEEDING SICKNESS TYPES • Hematomic (massive, deep, painful; bleeding may occur anywhere. The most common sites of bleeding are into joints (knees, ankles, elbows), into muscles, from the gastrointestinal tract, cause of the bleeding can be intramuscular injection; characterized by early postoperative & posttraumatic bleeding)
 • hematoma
• hematoma
 • petechia-spotted (macula)
• petechia-spotted (macula)
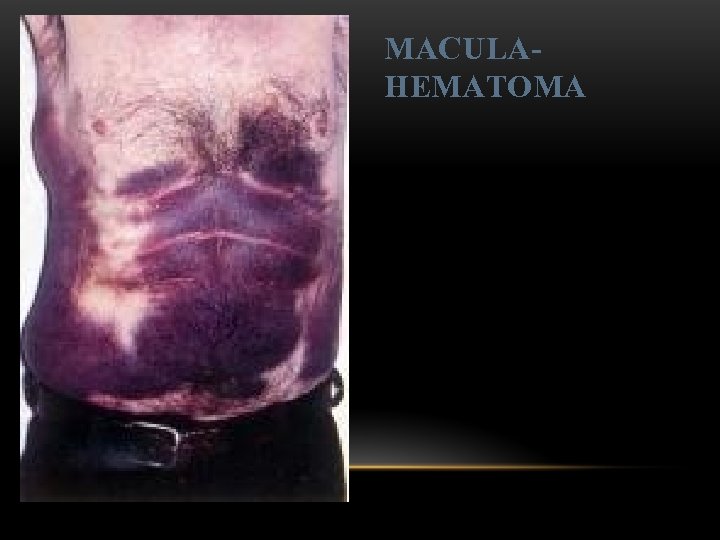 MACULAHEMATOMA
MACULAHEMATOMA
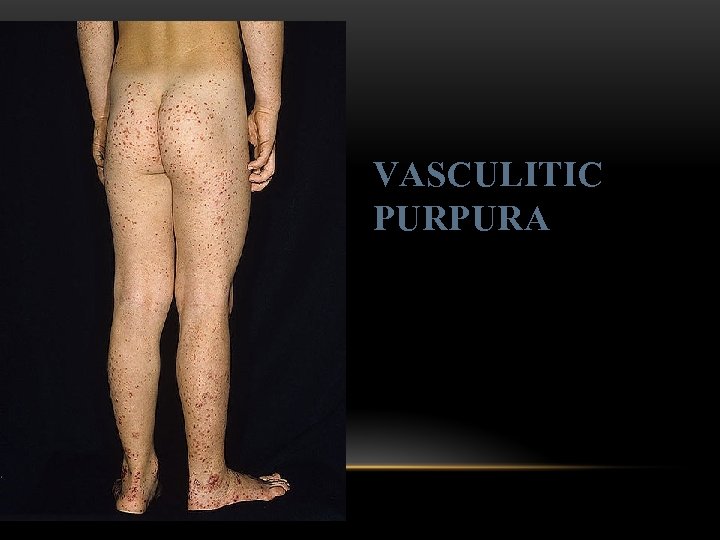 VASCULITIC PURPURA
VASCULITIC PURPURA
 ANGIOMA
ANGIOMA
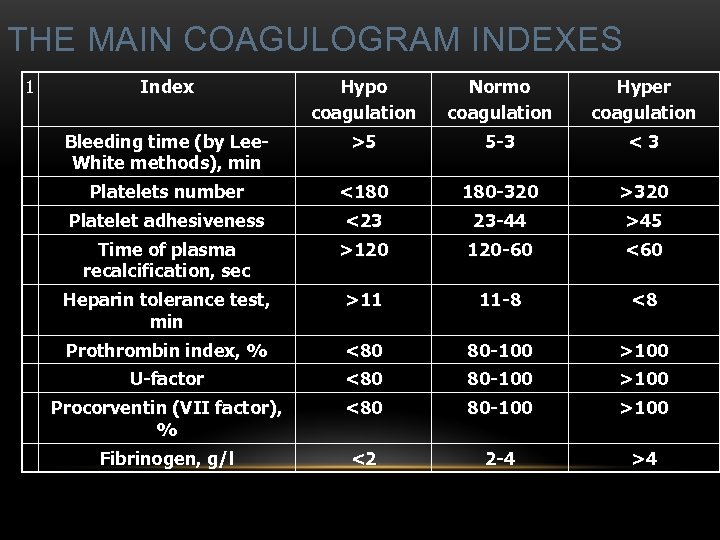 THE MAIN COAGULOGRAM INDEXES 1 Index Hypo coagulation Normo coagulation Hyper coagulation Bleeding time (by Lee. White methods), min >5 5 -3 <3 Platelets number <180 180 -320 >320 Platelet adhesiveness <23 23 -44 >45 Time of plasma recalcification, sec >120 120 -60 <60 Heparin tolerance test, min >11 11 -8 <8 Prothrombin index, % <80 80 -100 >100 U-factor <80 80 -100 >100 Procorventin (VII factor), % <80 80 -100 >100 Fibrinogen, g/l <2 2 -4 >4
THE MAIN COAGULOGRAM INDEXES 1 Index Hypo coagulation Normo coagulation Hyper coagulation Bleeding time (by Lee. White methods), min >5 5 -3 <3 Platelets number <180 180 -320 >320 Platelet adhesiveness <23 23 -44 >45 Time of plasma recalcification, sec >120 120 -60 <60 Heparin tolerance test, min >11 11 -8 <8 Prothrombin index, % <80 80 -100 >100 U-factor <80 80 -100 >100 Procorventin (VII factor), % <80 80 -100 >100 Fibrinogen, g/l <2 2 -4 >4
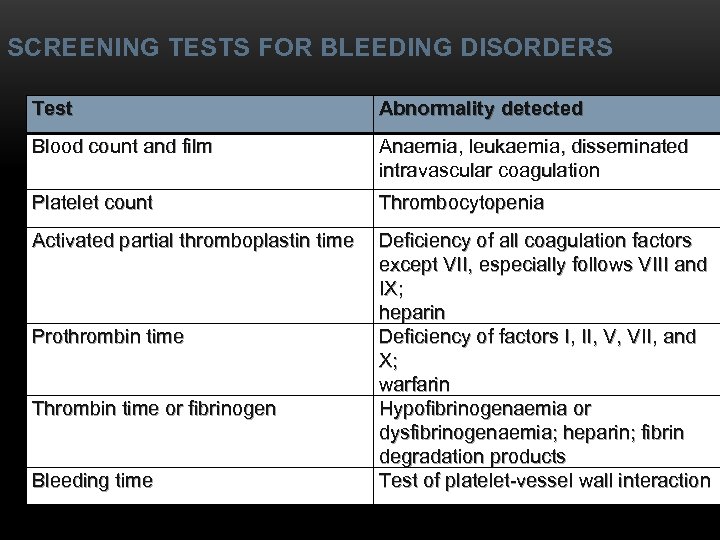 SCREENING TESTS FOR BLEEDING DISORDERS Test Abnormality detected Blood count and film Anaemia, leukaemia, disseminated intravascular coagulation Platelet count Thrombocytopenia Activated partial thromboplastin time Deficiency of all coagulation factors except VII, especially follows VIII and IX; heparin Deficiency of factors I, II, V, VII, and X; warfarin Hypofibrinogenaemia or dysfibrinogenaemia; heparin; fibrin degradation products Test of platelet-vessel wall interaction Prothrombin time Thrombin time or fibrinogen Bleeding time
SCREENING TESTS FOR BLEEDING DISORDERS Test Abnormality detected Blood count and film Anaemia, leukaemia, disseminated intravascular coagulation Platelet count Thrombocytopenia Activated partial thromboplastin time Deficiency of all coagulation factors except VII, especially follows VIII and IX; heparin Deficiency of factors I, II, V, VII, and X; warfarin Hypofibrinogenaemia or dysfibrinogenaemia; heparin; fibrin degradation products Test of platelet-vessel wall interaction Prothrombin time Thrombin time or fibrinogen Bleeding time
 COAGULOPATHY • I. Congenital • Deficiency of coagulation factor VIII (hemophilia A) • Deficiency of coagulation factor IX (hemophilia B) • Deficiency of coagulation factor XI (hemophilia C) • Deficiency of other coagulation factors (I, II, V, VII, IX, X and XIII) • Deficiency of XII factor, prekallikrein or kininogen, protein C and S (without excessive bleeding) • von Willebrand’s disease (angiohemophilia)
COAGULOPATHY • I. Congenital • Deficiency of coagulation factor VIII (hemophilia A) • Deficiency of coagulation factor IX (hemophilia B) • Deficiency of coagulation factor XI (hemophilia C) • Deficiency of other coagulation factors (I, II, V, VII, IX, X and XIII) • Deficiency of XII factor, prekallikrein or kininogen, protein C and S (without excessive bleeding) • von Willebrand’s disease (angiohemophilia)
 COAGULOPATHY • II. Acquired • 1) Hypoprothrombinemia • • Deficiency of vitamin K due to acholia of GIT (in cholestatic jaundice) • In overdose of indirect anticoagulant (antagonist of vitamin K) • In liver cirrhosis (due to reduced protein production) • 2) Consumption of coagulation factors (II stage of DIC) • 3) Heparin overdose • 4) Activation of fibrinolytic system • • In administration of streptokinase etc. • In trauma, obstetrical or surgical operations • In malignant neoplasms • In shock, sepsis, hematological malignancies, III stage of DIC
COAGULOPATHY • II. Acquired • 1) Hypoprothrombinemia • • Deficiency of vitamin K due to acholia of GIT (in cholestatic jaundice) • In overdose of indirect anticoagulant (antagonist of vitamin K) • In liver cirrhosis (due to reduced protein production) • 2) Consumption of coagulation factors (II stage of DIC) • 3) Heparin overdose • 4) Activation of fibrinolytic system • • In administration of streptokinase etc. • In trauma, obstetrical or surgical operations • In malignant neoplasms • In shock, sepsis, hematological malignancies, III stage of DIC
 PLATELET DISORDERS • Thrombocytopathy • I. Congenital (deficiency of platelet membrane glycoprotein) – Glanzmann's Thrombasthenia • II. Acquired (normal platelet count in blood and bone marrow but its functions are decreased) • • Drugs (after intake of antiplatelet agents: aspirin, Ticlide®); • Immune, toxic, septic processes; • Hematological malignancies and anemias • Thrombocytopenia (decrease in the number of platelets) • I. Werlhof’s disease - autoimmune thrombocytopenic purpura • II. Symptomatic • • Immune (heteroimmune, isoimmune, ) • Toxic (in phosphorus poisoning etc. ) • Methaplastic (in hematological malignancies or myelocarcinosis) • Drug-induced (cytostatics)
PLATELET DISORDERS • Thrombocytopathy • I. Congenital (deficiency of platelet membrane glycoprotein) – Glanzmann's Thrombasthenia • II. Acquired (normal platelet count in blood and bone marrow but its functions are decreased) • • Drugs (after intake of antiplatelet agents: aspirin, Ticlide®); • Immune, toxic, septic processes; • Hematological malignancies and anemias • Thrombocytopenia (decrease in the number of platelets) • I. Werlhof’s disease - autoimmune thrombocytopenic purpura • II. Symptomatic • • Immune (heteroimmune, isoimmune, ) • Toxic (in phosphorus poisoning etc. ) • Methaplastic (in hematological malignancies or myelocarcinosis) • Drug-induced (cytostatics)
 THROMBOCYTOPENIA o Thrombocytopenia (decrease in the number of platelets) o - Idiopathic thrombocytopenic purpura (ITP) o - Thombotic thrombocytopenic purpura (TTP) o - Heparin-induced thrombocytopenia (HIT) o - Hemolytic-Uremic Syndrome o - Chronic liver disease
THROMBOCYTOPENIA o Thrombocytopenia (decrease in the number of platelets) o - Idiopathic thrombocytopenic purpura (ITP) o - Thombotic thrombocytopenic purpura (TTP) o - Heparin-induced thrombocytopenia (HIT) o - Hemolytic-Uremic Syndrome o - Chronic liver disease
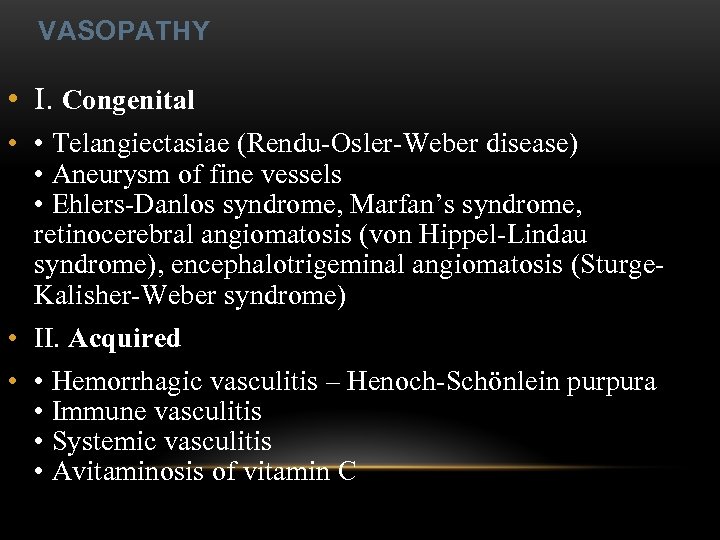 VASOPATHY • I. Congenital • • Telangiectasiae (Rendu-Osler-Weber disease) • Aneurysm of fine vessels • Ehlers-Danlos syndrome, Marfan’s syndrome, retinocerebral angiomatosis (von Hippel-Lindau syndrome), encephalotrigeminal angiomatosis (Sturge. Kalisher-Weber syndrome) • II. Acquired • • Hemorrhagic vasculitis – Henoch-Schönlein purpura • Immune vasculitis • Systemic vasculitis • Avitaminosis of vitamin C
VASOPATHY • I. Congenital • • Telangiectasiae (Rendu-Osler-Weber disease) • Aneurysm of fine vessels • Ehlers-Danlos syndrome, Marfan’s syndrome, retinocerebral angiomatosis (von Hippel-Lindau syndrome), encephalotrigeminal angiomatosis (Sturge. Kalisher-Weber syndrome) • II. Acquired • • Hemorrhagic vasculitis – Henoch-Schönlein purpura • Immune vasculitis • Systemic vasculitis • Avitaminosis of vitamin C
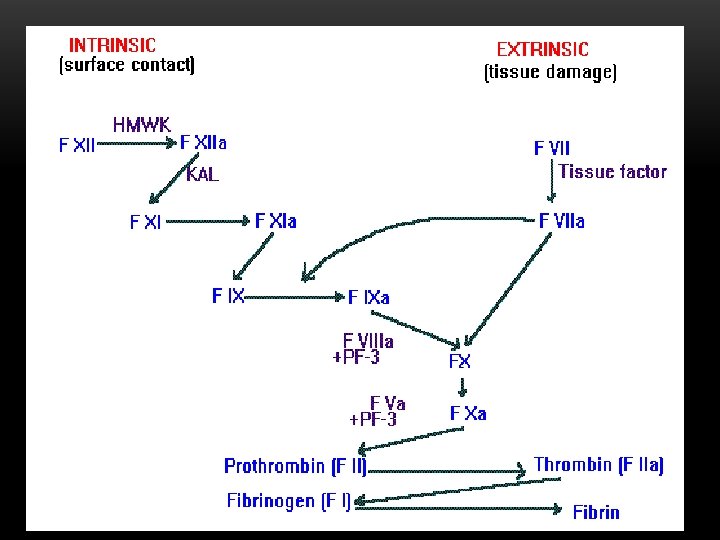
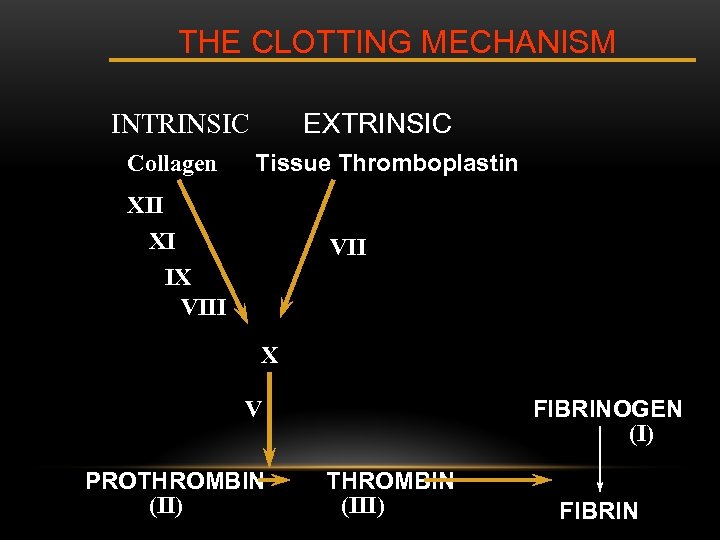 THE CLOTTING MECHANISM EXTRINSIC INTRINSIC Collagen Tissue Thromboplastin XII XI IX VIII VII X FIBRINOGEN (I) V PROTHROMBIN (II) THROMBIN (III) FIBRIN
THE CLOTTING MECHANISM EXTRINSIC INTRINSIC Collagen Tissue Thromboplastin XII XI IX VIII VII X FIBRINOGEN (I) V PROTHROMBIN (II) THROMBIN (III) FIBRIN
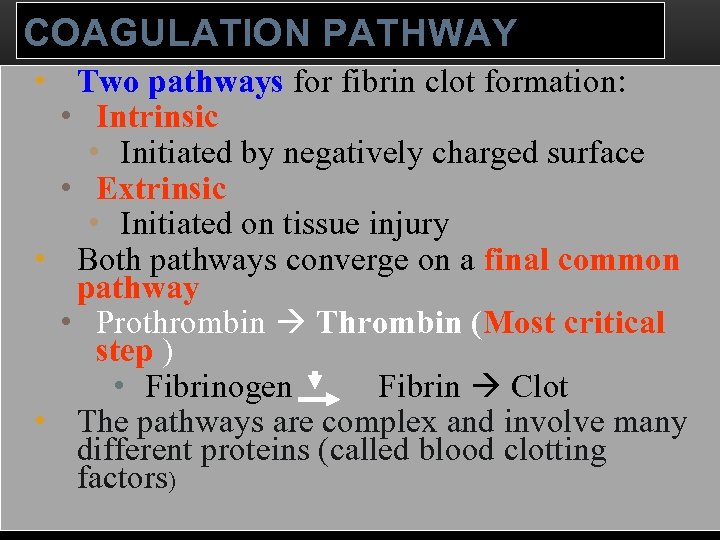 COAGULATION PATHWAY • Two pathways for fibrin clot formation: • Intrinsic • Initiated by negatively charged surface • Extrinsic • Initiated on tissue injury • Both pathways converge on a final common pathway • Prothrombin Thrombin (Most critical step ) • Fibrinogen Fibrin Clot • The pathways are complex and involve many different proteins (called blood clotting factors)
COAGULATION PATHWAY • Two pathways for fibrin clot formation: • Intrinsic • Initiated by negatively charged surface • Extrinsic • Initiated on tissue injury • Both pathways converge on a final common pathway • Prothrombin Thrombin (Most critical step ) • Fibrinogen Fibrin Clot • The pathways are complex and involve many different proteins (called blood clotting factors)
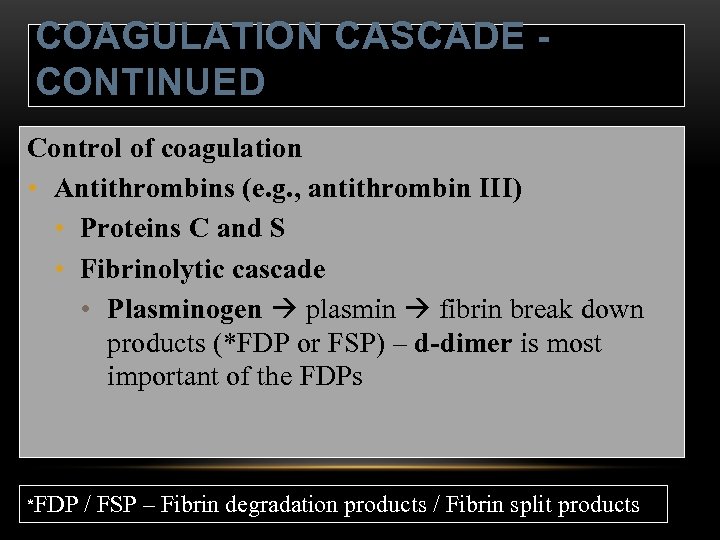 COAGULATION CASCADE CONTINUED Control of coagulation • Antithrombins (e. g. , antithrombin III) • Proteins C and S • Fibrinolytic cascade • Plasminogen plasmin fibrin break down products (*FDP or FSP) – d-dimer is most important of the FDPs *FDP / FSP – Fibrin degradation products / Fibrin split products
COAGULATION CASCADE CONTINUED Control of coagulation • Antithrombins (e. g. , antithrombin III) • Proteins C and S • Fibrinolytic cascade • Plasminogen plasmin fibrin break down products (*FDP or FSP) – d-dimer is most important of the FDPs *FDP / FSP – Fibrin degradation products / Fibrin split products
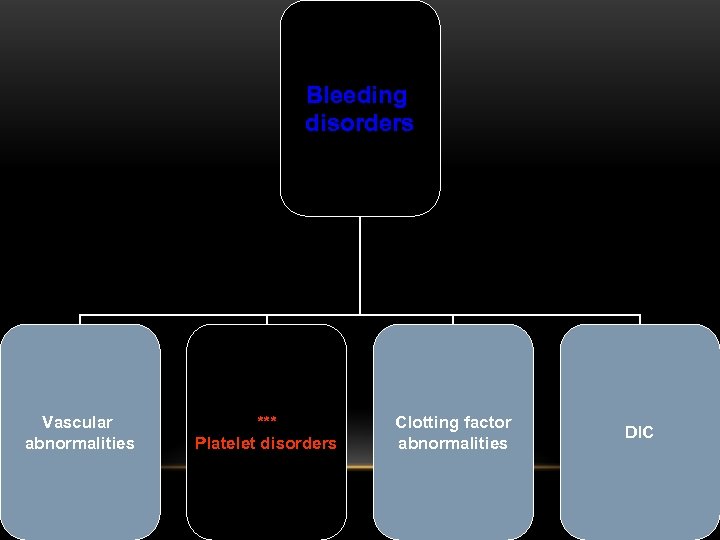
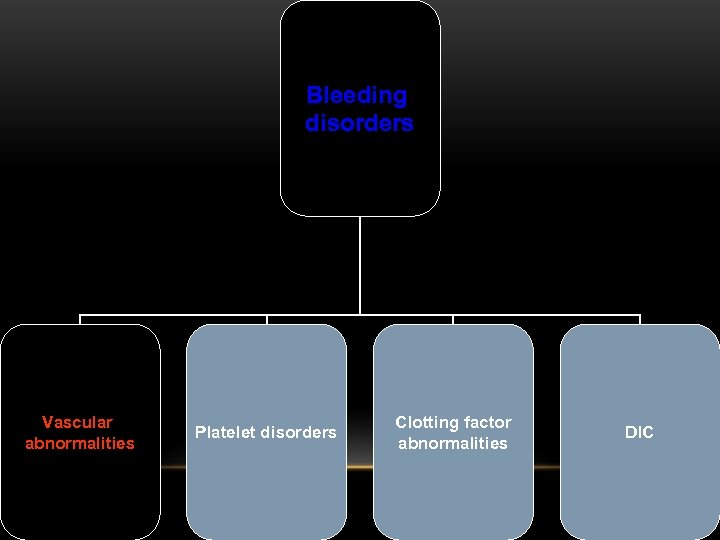
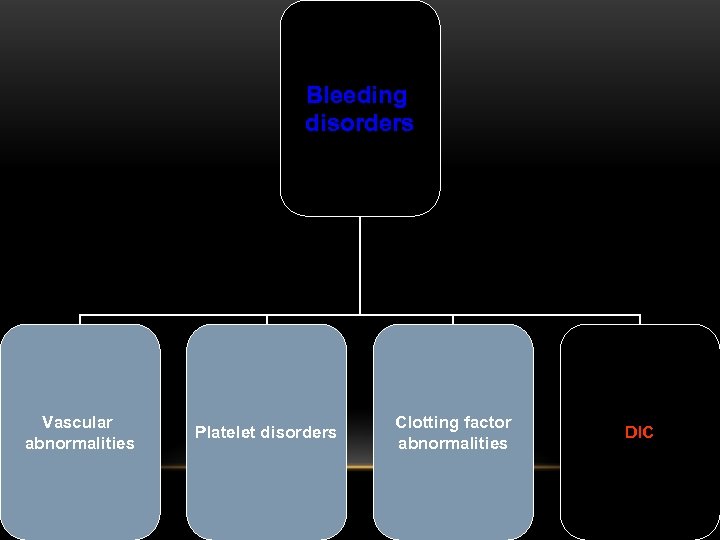
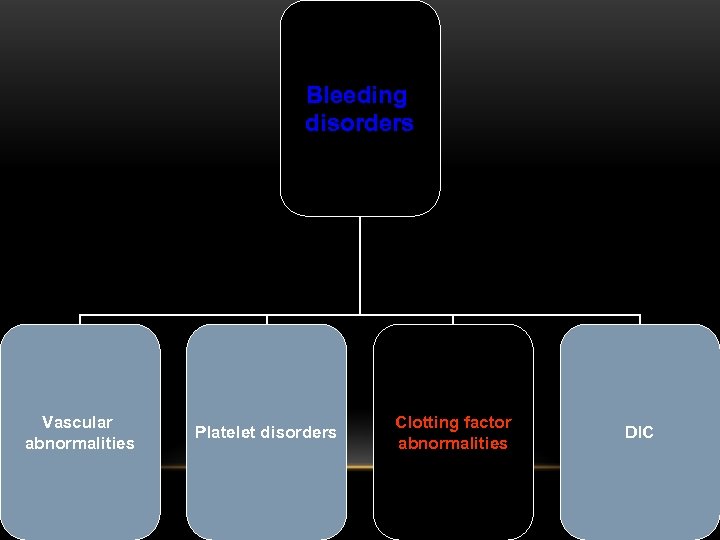 Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
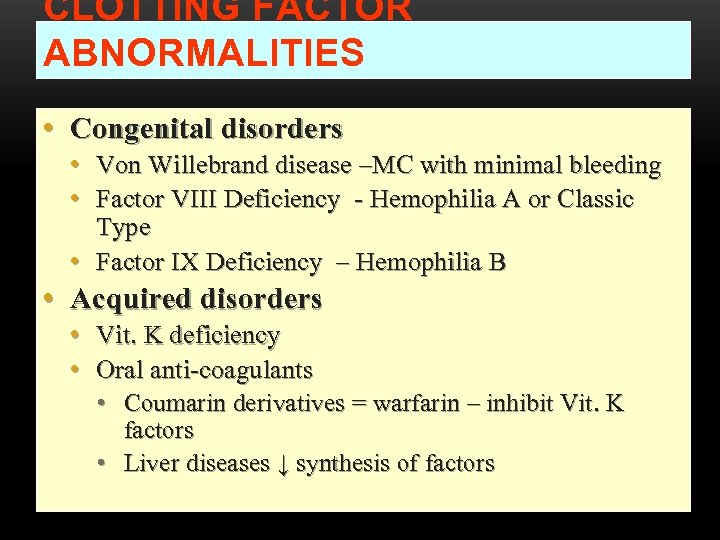 CLOTTING FACTOR ABNORMALITIES • Congenital disorders • Von Willebrand disease –MC with minimal bleeding • Factor VIII Deficiency - Hemophilia A or Classic Type • Factor IX Deficiency – Hemophilia B • Acquired disorders • Vit. K deficiency • Oral anti-coagulants • Coumarin derivatives = warfarin – inhibit Vit. K factors • Liver diseases ↓ synthesis of factors
CLOTTING FACTOR ABNORMALITIES • Congenital disorders • Von Willebrand disease –MC with minimal bleeding • Factor VIII Deficiency - Hemophilia A or Classic Type • Factor IX Deficiency – Hemophilia B • Acquired disorders • Vit. K deficiency • Oral anti-coagulants • Coumarin derivatives = warfarin – inhibit Vit. K factors • Liver diseases ↓ synthesis of factors
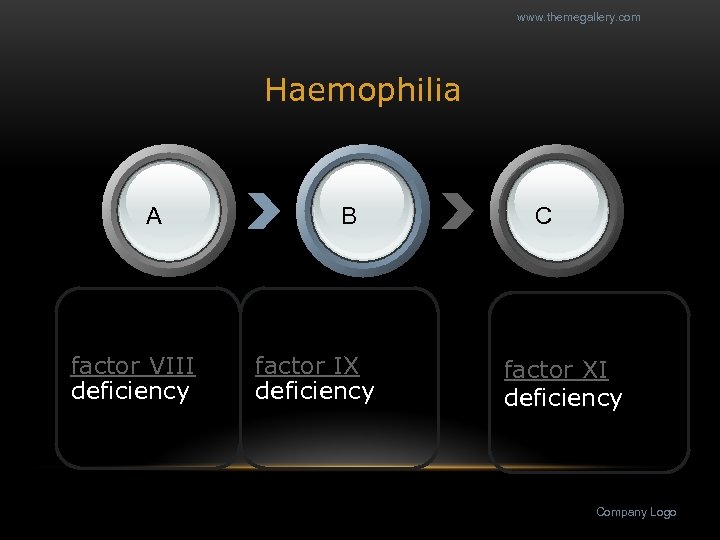 www. themegallery. com Haemophilia А factor VIII deficiency В factor IX deficiency С factor XI deficiency Company Logo
www. themegallery. com Haemophilia А factor VIII deficiency В factor IX deficiency С factor XI deficiency Company Logo
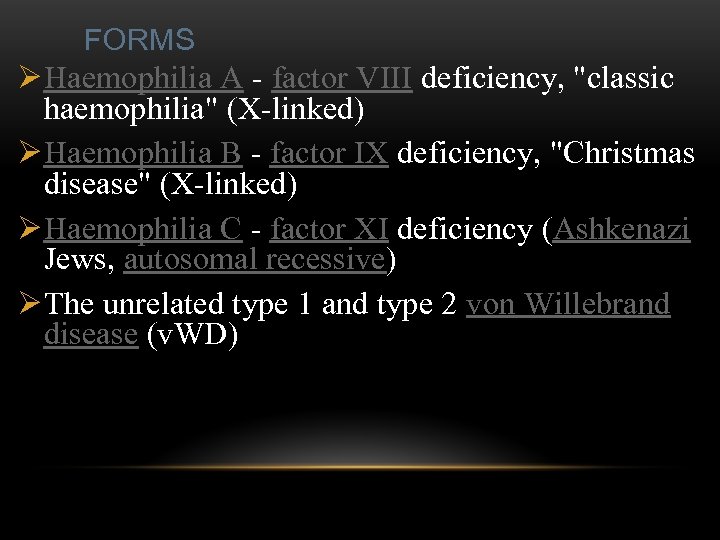 FORMS Ø Haemophilia A - factor VIII deficiency, "classic haemophilia" (X-linked) Ø Haemophilia B - factor IX deficiency, "Christmas disease" (X-linked) Ø Haemophilia C - factor XI deficiency (Ashkenazi Jews, autosomal recessive) Ø The unrelated type 1 and type 2 von Willebrand disease (v. WD)
FORMS Ø Haemophilia A - factor VIII deficiency, "classic haemophilia" (X-linked) Ø Haemophilia B - factor IX deficiency, "Christmas disease" (X-linked) Ø Haemophilia C - factor XI deficiency (Ashkenazi Jews, autosomal recessive) Ø The unrelated type 1 and type 2 von Willebrand disease (v. WD)
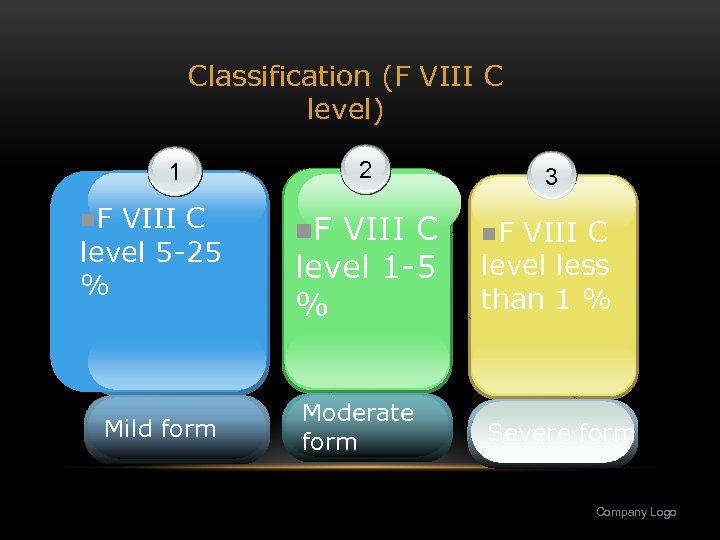 Classification (F VIII C level) 2 1 n. F VIII C level 5 -25 % Mild form n. F VIII C level 1 -5 % Moderate form 3 n. F VIII C level less than 1 % Severe form Company Logo
Classification (F VIII C level) 2 1 n. F VIII C level 5 -25 % Mild form n. F VIII C level 1 -5 % Moderate form 3 n. F VIII C level less than 1 % Severe form Company Logo
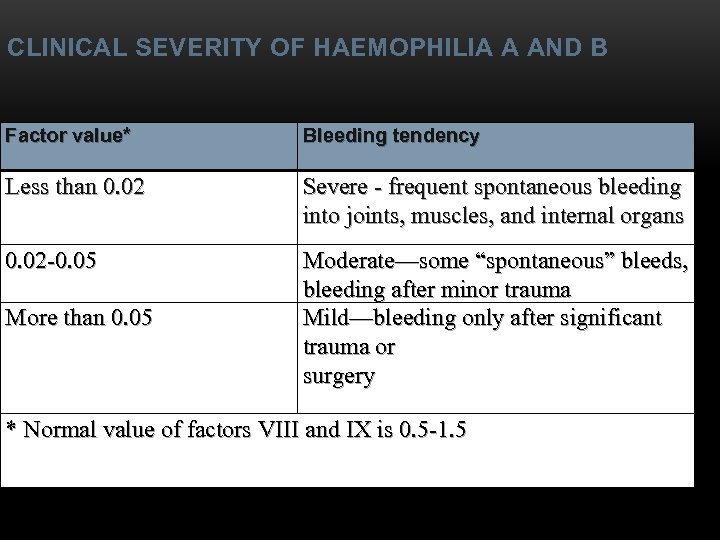 CLINICAL SEVERITY OF HAEMOPHILIA A AND B Factor value* Bleeding tendency Less than 0. 02 Severe - frequent spontaneous bleeding into joints, muscles, and internal organs 0. 02 -0. 05 Moderate—some “spontaneous” bleeds, bleeding after minor trauma Mild—bleeding only after significant trauma or surgery More than 0. 05 * Normal value of factors VIII and IX is 0. 5 -1. 5
CLINICAL SEVERITY OF HAEMOPHILIA A AND B Factor value* Bleeding tendency Less than 0. 02 Severe - frequent spontaneous bleeding into joints, muscles, and internal organs 0. 02 -0. 05 Moderate—some “spontaneous” bleeds, bleeding after minor trauma Mild—bleeding only after significant trauma or surgery More than 0. 05 * Normal value of factors VIII and IX is 0. 5 -1. 5
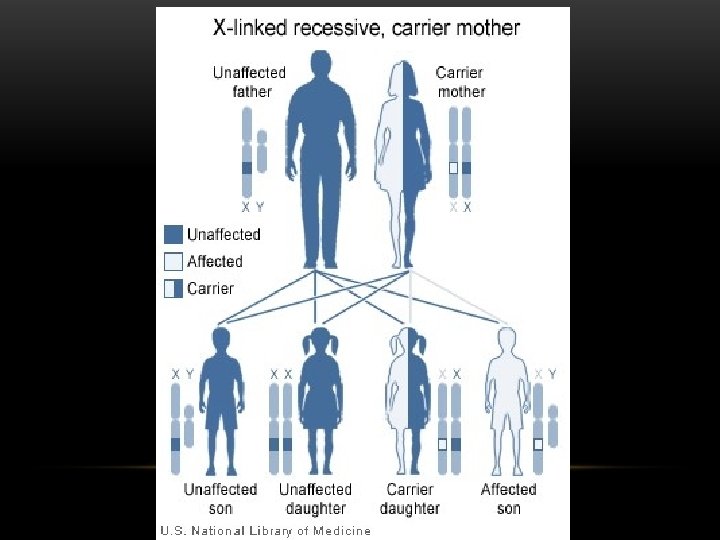
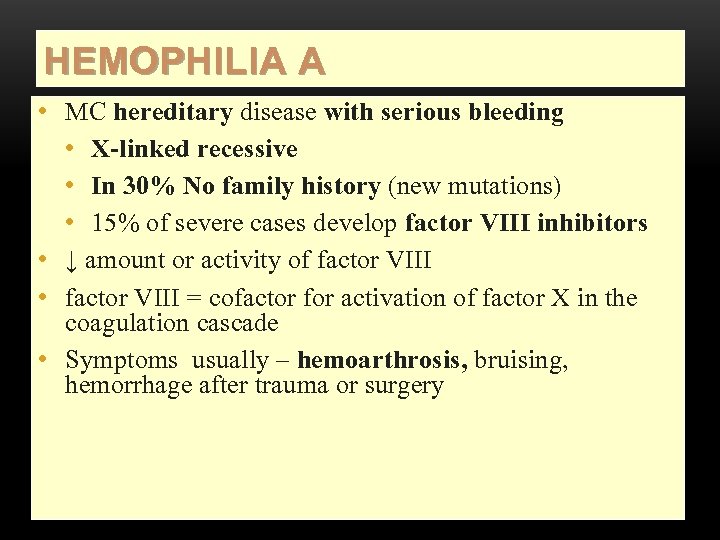 HEMOPHILIA A • MC hereditary disease with serious bleeding • X-linked recessive • In 30% No family history (new mutations) • 15% of severe cases develop factor VIII inhibitors • ↓ amount or activity of factor VIII • factor VIII = cofactor for activation of factor X in the coagulation cascade • Symptoms usually – hemoarthrosis, bruising, hemorrhage after trauma or surgery
HEMOPHILIA A • MC hereditary disease with serious bleeding • X-linked recessive • In 30% No family history (new mutations) • 15% of severe cases develop factor VIII inhibitors • ↓ amount or activity of factor VIII • factor VIII = cofactor for activation of factor X in the coagulation cascade • Symptoms usually – hemoarthrosis, bruising, hemorrhage after trauma or surgery
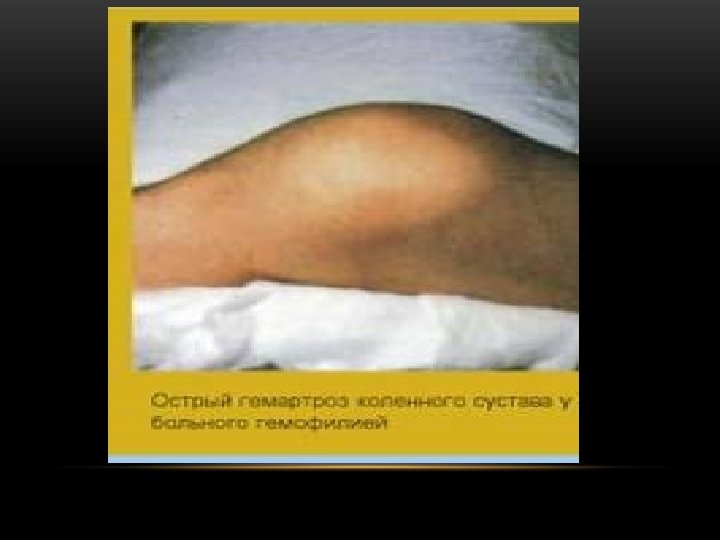
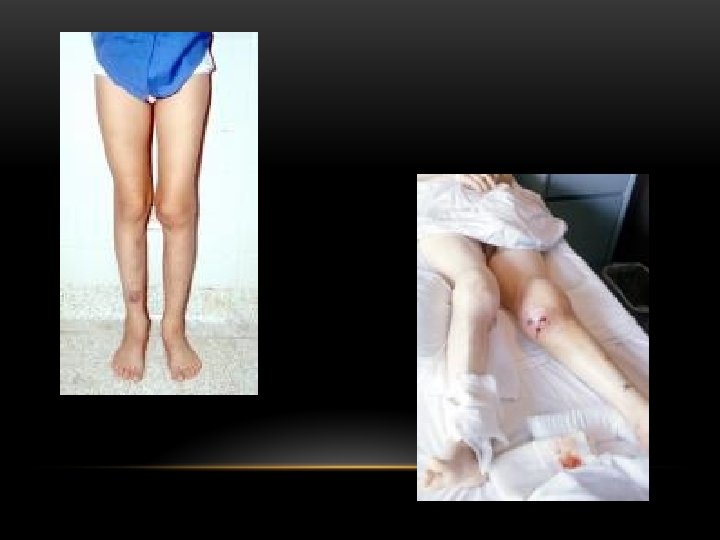
 SIGNS & SYMPTOMS • Symptoms of hemophilia are usually first noticed during infancy or childhood. However, some people with milder forms of hemophilia may not develop symptoms until later on. The following are signs of hemophilia that may be noticed shortly after birth: Bleeding into the muscle, resulting in a deep bruise after receiving a routine vitamin K shot. Prolonged bleeding after a male child is circumcised. • Other symptoms of hemophilia include: Bleeding into a joint or muscle that causes pain and swelling. Abnormal bleeding after an injury. Easy bruising. Frequent nosebleeds. Blood in the urine (hematuria). • The most common bleeding problem a person with severe hemophilia has is bleeding into a joint (hemarthrosis), often
SIGNS & SYMPTOMS • Symptoms of hemophilia are usually first noticed during infancy or childhood. However, some people with milder forms of hemophilia may not develop symptoms until later on. The following are signs of hemophilia that may be noticed shortly after birth: Bleeding into the muscle, resulting in a deep bruise after receiving a routine vitamin K shot. Prolonged bleeding after a male child is circumcised. • Other symptoms of hemophilia include: Bleeding into a joint or muscle that causes pain and swelling. Abnormal bleeding after an injury. Easy bruising. Frequent nosebleeds. Blood in the urine (hematuria). • The most common bleeding problem a person with severe hemophilia has is bleeding into a joint (hemarthrosis), often
 Hemophilia Diagnostic criteria Hematomic bleeding sickness types Arhtropathy
Hemophilia Diagnostic criteria Hematomic bleeding sickness types Arhtropathy


 BIOCHEMICAL ASPECTS: • Factor VIII circulates in the plasma as a complex of factor VIII and von Willebrand factor. The molecular weight of human factor VIII has been estimated to be 285, 000. Hemophelia A in which factor VIII (antihemophelic factor) is either absent or dysfunctional is transmitted by X chromosomal inheritance. Hemophelia A is at least four times more common than hemophelia B.
BIOCHEMICAL ASPECTS: • Factor VIII circulates in the plasma as a complex of factor VIII and von Willebrand factor. The molecular weight of human factor VIII has been estimated to be 285, 000. Hemophelia A in which factor VIII (antihemophelic factor) is either absent or dysfunctional is transmitted by X chromosomal inheritance. Hemophelia A is at least four times more common than hemophelia B.
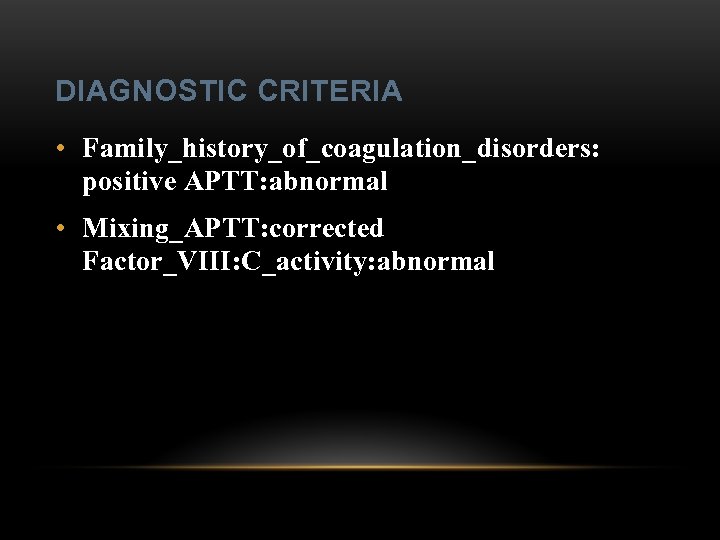 DIAGNOSTIC CRITERIA • Family_history_of_coagulation_disorders: positive APTT: abnormal • Mixing_APTT: corrected Factor_VIII: C_activity: abnormal
DIAGNOSTIC CRITERIA • Family_history_of_coagulation_disorders: positive APTT: abnormal • Mixing_APTT: corrected Factor_VIII: C_activity: abnormal
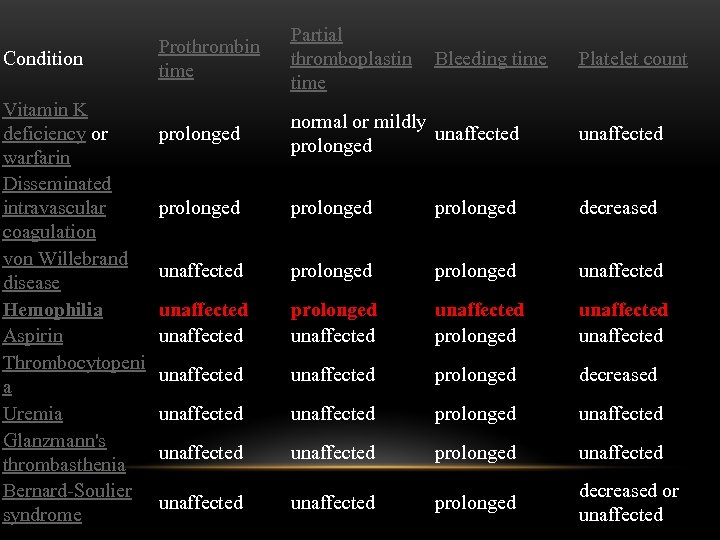 Condition Vitamin K deficiency or warfarin Disseminated intravascular coagulation von Willebrand disease Hemophilia Aspirin Thrombocytopeni a Uremia Glanzmann's thrombasthenia Bernard-Soulier syndrome Prothrombin time Partial thromboplastin Bleeding time Platelet count prolonged normal or mildly unaffected prolonged decreased unaffected prolonged unaffected unaffected prolonged decreased unaffected unaffected prolonged decreased or unaffected
Condition Vitamin K deficiency or warfarin Disseminated intravascular coagulation von Willebrand disease Hemophilia Aspirin Thrombocytopeni a Uremia Glanzmann's thrombasthenia Bernard-Soulier syndrome Prothrombin time Partial thromboplastin Bleeding time Platelet count prolonged normal or mildly unaffected prolonged decreased unaffected prolonged unaffected unaffected prolonged decreased unaffected unaffected prolonged decreased or unaffected
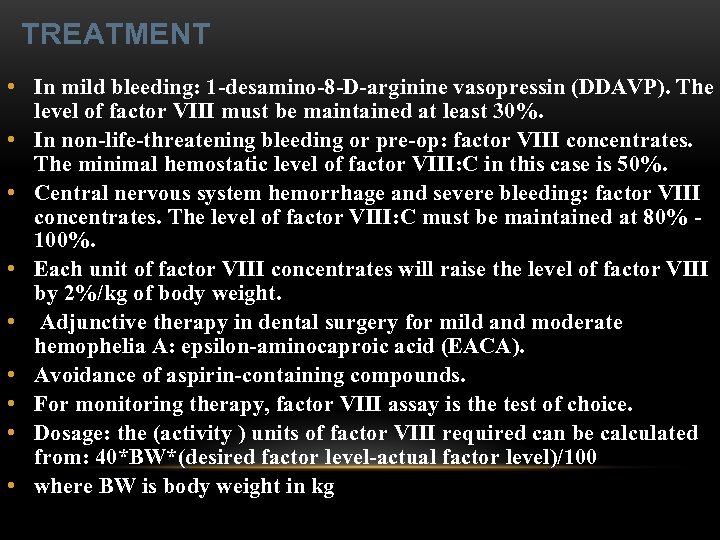 TREATMENT • In mild bleeding: 1 -desamino-8 -D-arginine vasopressin (DDAVP). The level of factor VIII must be maintained at least 30%. • In non-life-threatening bleeding or pre-op: factor VIII concentrates. The minimal hemostatic level of factor VIII: C in this case is 50%. • Central nervous system hemorrhage and severe bleeding: factor VIII concentrates. The level of factor VIII: C must be maintained at 80% 100%. • Each unit of factor VIII concentrates will raise the level of factor VIII by 2%/kg of body weight. • Adjunctive therapy in dental surgery for mild and moderate hemophelia A: epsilon-aminocaproic acid (EACA). • Avoidance of aspirin-containing compounds. • For monitoring therapy, factor VIII assay is the test of choice. • Dosage: the (activity ) units of factor VIII required can be calculated from: 40*BW*(desired factor level-actual factor level)/100 • where BW is body weight in kg
TREATMENT • In mild bleeding: 1 -desamino-8 -D-arginine vasopressin (DDAVP). The level of factor VIII must be maintained at least 30%. • In non-life-threatening bleeding or pre-op: factor VIII concentrates. The minimal hemostatic level of factor VIII: C in this case is 50%. • Central nervous system hemorrhage and severe bleeding: factor VIII concentrates. The level of factor VIII: C must be maintained at 80% 100%. • Each unit of factor VIII concentrates will raise the level of factor VIII by 2%/kg of body weight. • Adjunctive therapy in dental surgery for mild and moderate hemophelia A: epsilon-aminocaproic acid (EACA). • Avoidance of aspirin-containing compounds. • For monitoring therapy, factor VIII assay is the test of choice. • Dosage: the (activity ) units of factor VIII required can be calculated from: 40*BW*(desired factor level-actual factor level)/100 • where BW is body weight in kg
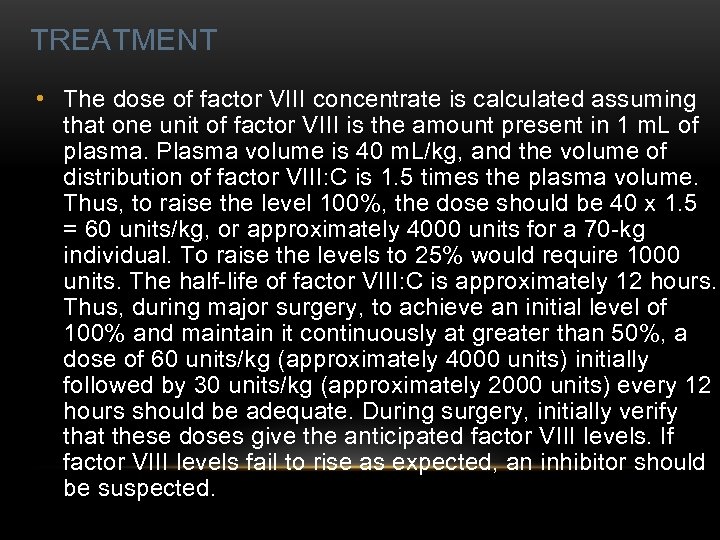 TREATMENT • The dose of factor VIII concentrate is calculated assuming that one unit of factor VIII is the amount present in 1 m. L of plasma. Plasma volume is 40 m. L/kg, and the volume of distribution of factor VIII: C is 1. 5 times the plasma volume. Thus, to raise the level 100%, the dose should be 40 x 1. 5 = 60 units/kg, or approximately 4000 units for a 70 -kg individual. To raise the levels to 25% would require 1000 units. The half-life of factor VIII: C is approximately 12 hours. Thus, during major surgery, to achieve an initial level of 100% and maintain it continuously at greater than 50%, a dose of 60 units/kg (approximately 4000 units) initially followed by 30 units/kg (approximately 2000 units) every 12 hours should be adequate. During surgery, initially verify that these doses give the anticipated factor VIII levels. If factor VIII levels fail to rise as expected, an inhibitor should be suspected.
TREATMENT • The dose of factor VIII concentrate is calculated assuming that one unit of factor VIII is the amount present in 1 m. L of plasma. Plasma volume is 40 m. L/kg, and the volume of distribution of factor VIII: C is 1. 5 times the plasma volume. Thus, to raise the level 100%, the dose should be 40 x 1. 5 = 60 units/kg, or approximately 4000 units for a 70 -kg individual. To raise the levels to 25% would require 1000 units. The half-life of factor VIII: C is approximately 12 hours. Thus, during major surgery, to achieve an initial level of 100% and maintain it continuously at greater than 50%, a dose of 60 units/kg (approximately 4000 units) initially followed by 30 units/kg (approximately 2000 units) every 12 hours should be adequate. During surgery, initially verify that these doses give the anticipated factor VIII levels. If factor VIII levels fail to rise as expected, an inhibitor should be suspected.
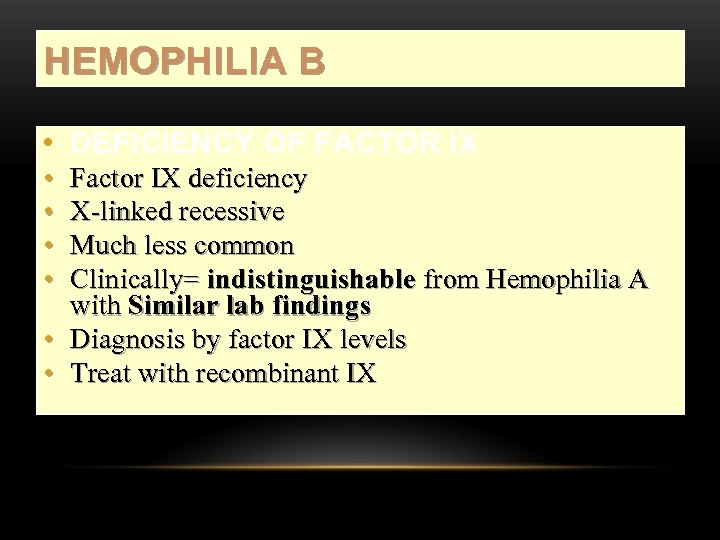 HEMOPHILIA B • DEFICIENCY OF FACTOR IX • • Factor IX deficiency X-linked recessive Much less common Clinically= indistinguishable from Hemophilia A with Similar lab findings • Diagnosis by factor IX levels • Treat with recombinant IX
HEMOPHILIA B • DEFICIENCY OF FACTOR IX • • Factor IX deficiency X-linked recessive Much less common Clinically= indistinguishable from Hemophilia A with Similar lab findings • Diagnosis by factor IX levels • Treat with recombinant IX
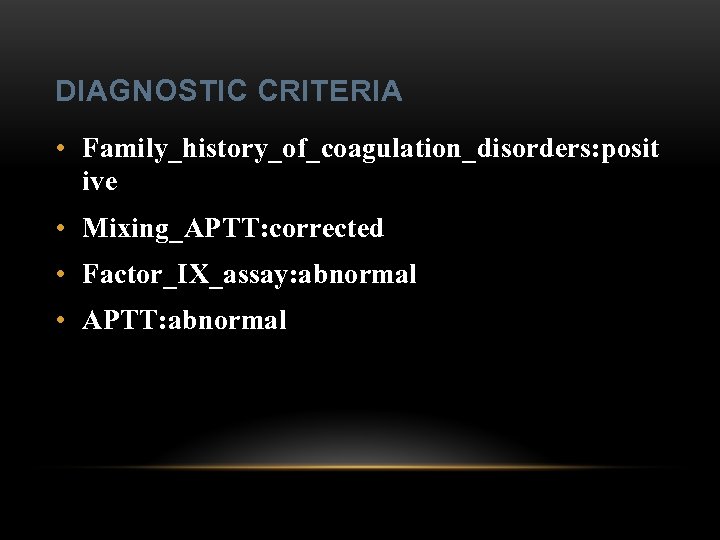 DIAGNOSTIC CRITERIA • Family_history_of_coagulation_disorders: posit ive • Mixing_APTT: corrected • Factor_IX_assay: abnormal • APTT: abnormal
DIAGNOSTIC CRITERIA • Family_history_of_coagulation_disorders: posit ive • Mixing_APTT: corrected • Factor_IX_assay: abnormal • APTT: abnormal
 TREATMENT • For patients with mild form of factor IX deficiency with non-life-threatening bleeding, the treatment of choice is FFP. For the severe form of hemophelia B or in life- threatening situation, prothrombin complex concentrates are the treatment of choice.
TREATMENT • For patients with mild form of factor IX deficiency with non-life-threatening bleeding, the treatment of choice is FFP. For the severe form of hemophelia B or in life- threatening situation, prothrombin complex concentrates are the treatment of choice.
 TREATMENT • Target levels of factor IX for therapy: Severe hemorrhage: 20% - 50% for 3 -5 days, then 10% - 20% for the next 10 days. • Minor hemorrhage: 20% for 7 days. • Surgery: 50% - 70% for 2 days, then 30% 40% for 3 days, then 20% for 7 days.
TREATMENT • Target levels of factor IX for therapy: Severe hemorrhage: 20% - 50% for 3 -5 days, then 10% - 20% for the next 10 days. • Minor hemorrhage: 20% for 7 days. • Surgery: 50% - 70% for 2 days, then 30% 40% for 3 days, then 20% for 7 days.
 TREATMENT • Dosage: the (activity) units of factor IX required can be calculated from: 80*BW*(desired factor level-actual factor level)/100 • where BW is body weight in kg • Note that in-vivo recovery of factor IX is about 50%.
TREATMENT • Dosage: the (activity) units of factor IX required can be calculated from: 80*BW*(desired factor level-actual factor level)/100 • where BW is body weight in kg • Note that in-vivo recovery of factor IX is about 50%.
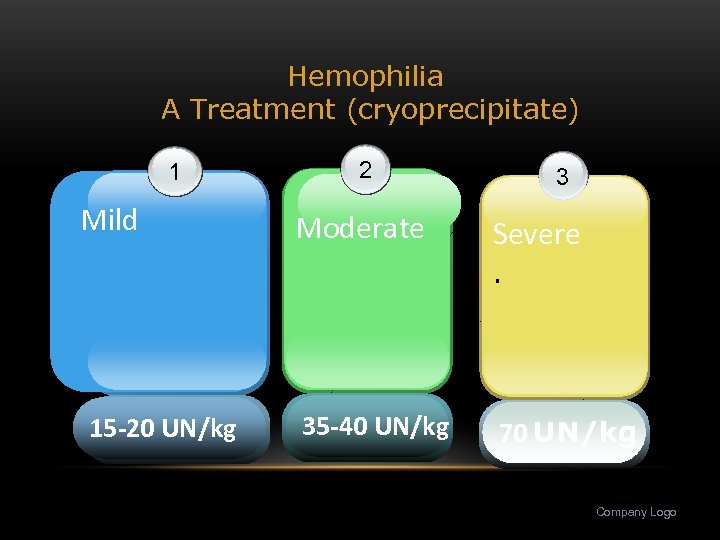 Hemophilia A Treatment (cryoprecipitate) 1 Mild 15 -20 UN/kg 2 3 Moderate Severe. 35 -40 UN/kg 70 UN/kg Company Logo
Hemophilia A Treatment (cryoprecipitate) 1 Mild 15 -20 UN/kg 2 3 Moderate Severe. 35 -40 UN/kg 70 UN/kg Company Logo
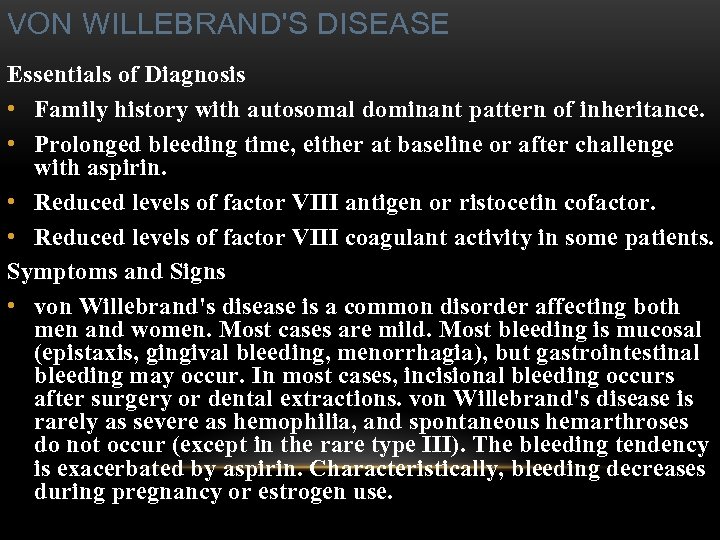 VON WILLEBRAND'S DISEASE Essentials of Diagnosis • Family history with autosomal dominant pattern of inheritance. • Prolonged bleeding time, either at baseline or after challenge with aspirin. • Reduced levels of factor VIII antigen or ristocetin cofactor. • Reduced levels of factor VIII coagulant activity in some patients. Symptoms and Signs • von Willebrand's disease is a common disorder affecting both men and women. Most cases are mild. Most bleeding is mucosal (epistaxis, gingival bleeding, menorrhagia), but gastrointestinal bleeding may occur. In most cases, incisional bleeding occurs after surgery or dental extractions. von Willebrand's disease is rarely as severe as hemophilia, and spontaneous hemarthroses do not occur (except in the rare type III). The bleeding tendency is exacerbated by aspirin. Characteristically, bleeding decreases during pregnancy or estrogen use.
VON WILLEBRAND'S DISEASE Essentials of Diagnosis • Family history with autosomal dominant pattern of inheritance. • Prolonged bleeding time, either at baseline or after challenge with aspirin. • Reduced levels of factor VIII antigen or ristocetin cofactor. • Reduced levels of factor VIII coagulant activity in some patients. Symptoms and Signs • von Willebrand's disease is a common disorder affecting both men and women. Most cases are mild. Most bleeding is mucosal (epistaxis, gingival bleeding, menorrhagia), but gastrointestinal bleeding may occur. In most cases, incisional bleeding occurs after surgery or dental extractions. von Willebrand's disease is rarely as severe as hemophilia, and spontaneous hemarthroses do not occur (except in the rare type III). The bleeding tendency is exacerbated by aspirin. Characteristically, bleeding decreases during pregnancy or estrogen use.

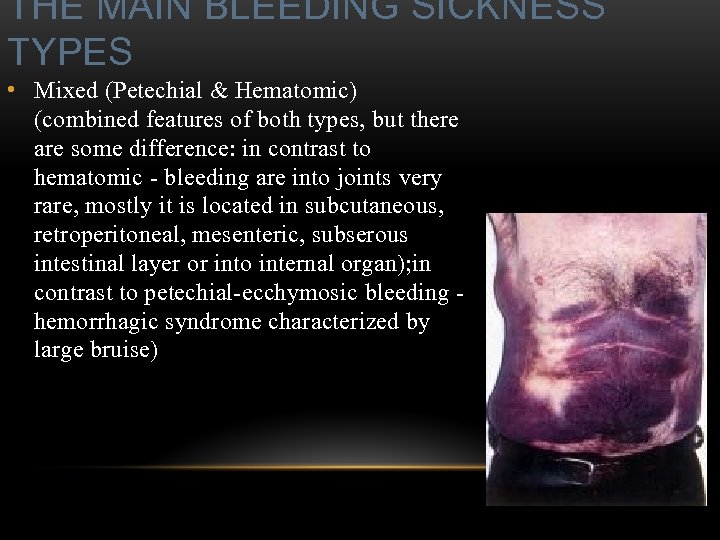 THE MAIN BLEEDING SICKNESS TYPES • Mixed (Petechial & Hematomic) (combined features of both types, but there are some difference: in contrast to hematomic - bleeding are into joints very rare, mostly it is located in subcutaneous, retroperitoneal, mesenteric, subserous intestinal layer or into internal organ); in contrast to petechial-ecchymosic bleeding - hemorrhagic syndrome characterized by large bruise)
THE MAIN BLEEDING SICKNESS TYPES • Mixed (Petechial & Hematomic) (combined features of both types, but there are some difference: in contrast to hematomic - bleeding are into joints very rare, mostly it is located in subcutaneous, retroperitoneal, mesenteric, subserous intestinal layer or into internal organ); in contrast to petechial-ecchymosic bleeding - hemorrhagic syndrome characterized by large bruise)
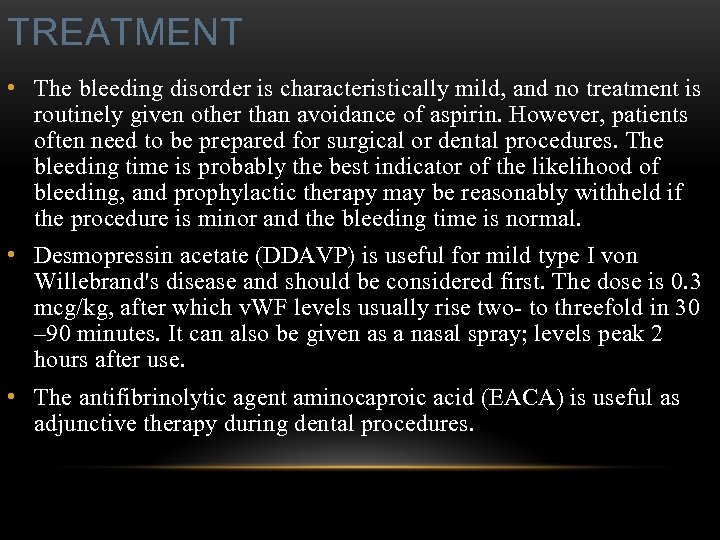 TREATMENT • The bleeding disorder is characteristically mild, and no treatment is routinely given other than avoidance of aspirin. However, patients often need to be prepared for surgical or dental procedures. The bleeding time is probably the best indicator of the likelihood of bleeding, and prophylactic therapy may be reasonably withheld if the procedure is minor and the bleeding time is normal. • Desmopressin acetate (DDAVP) is useful for mild type I von Willebrand's disease and should be considered first. The dose is 0. 3 mcg/kg, after which v. WF levels usually rise two- to threefold in 30 – 90 minutes. It can also be given as a nasal spray; levels peak 2 hours after use. • The antifibrinolytic agent aminocaproic acid (EACA) is useful as adjunctive therapy during dental procedures.
TREATMENT • The bleeding disorder is characteristically mild, and no treatment is routinely given other than avoidance of aspirin. However, patients often need to be prepared for surgical or dental procedures. The bleeding time is probably the best indicator of the likelihood of bleeding, and prophylactic therapy may be reasonably withheld if the procedure is minor and the bleeding time is normal. • Desmopressin acetate (DDAVP) is useful for mild type I von Willebrand's disease and should be considered first. The dose is 0. 3 mcg/kg, after which v. WF levels usually rise two- to threefold in 30 – 90 minutes. It can also be given as a nasal spray; levels peak 2 hours after use. • The antifibrinolytic agent aminocaproic acid (EACA) is useful as adjunctive therapy during dental procedures.
 PLATELET HEMOSTATIC ACTIVITY • 1. Pl stimulate vasoconstriction of injured vessels • 2. Pl form hemostatic plug (platelet adhesion) + platelet aggregation to seal small vessel wall • 3. Pl play role in fibrin clot formation
PLATELET HEMOSTATIC ACTIVITY • 1. Pl stimulate vasoconstriction of injured vessels • 2. Pl form hemostatic plug (platelet adhesion) + platelet aggregation to seal small vessel wall • 3. Pl play role in fibrin clot formation
 Bleeding disorders Vascular abnormalities *** Platelet disorders Clotting factor abnormalities DIC
Bleeding disorders Vascular abnormalities *** Platelet disorders Clotting factor abnormalities DIC
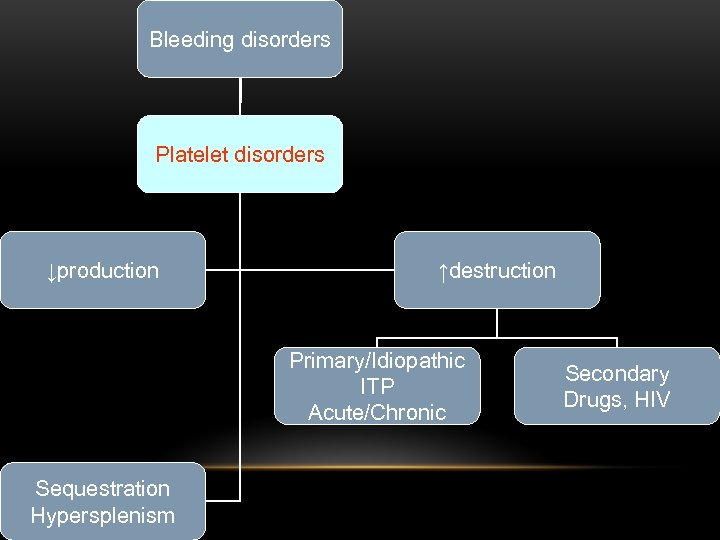 Bleeding disorders Platelet disorders ↓production ↑destruction Primary/Idiopathic ITP Acute/Chronic Sequestration Hypersplenism Secondary Drugs, HIV
Bleeding disorders Platelet disorders ↓production ↑destruction Primary/Idiopathic ITP Acute/Chronic Sequestration Hypersplenism Secondary Drugs, HIV
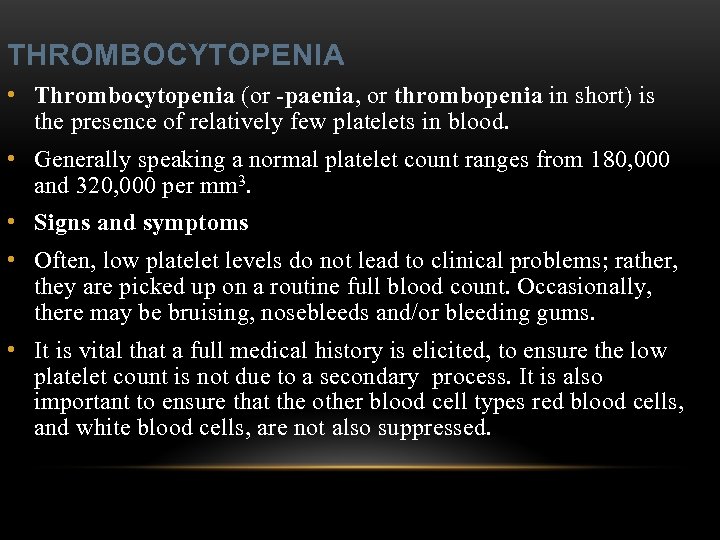 THROMBOCYTOPENIA • Thrombocytopenia (or -paenia, or thrombopenia in short) is the presence of relatively few platelets in blood. • Generally speaking a normal platelet count ranges from 180, 000 and 320, 000 per mm 3. • Signs and symptoms • Often, low platelet levels do not lead to clinical problems; rather, they are picked up on a routine full blood count. Occasionally, there may be bruising, nosebleeds and/or bleeding gums. • It is vital that a full medical history is elicited, to ensure the low platelet count is not due to a secondary process. It is also important to ensure that the other blood cell types red blood cells, and white blood cells, are not also suppressed.
THROMBOCYTOPENIA • Thrombocytopenia (or -paenia, or thrombopenia in short) is the presence of relatively few platelets in blood. • Generally speaking a normal platelet count ranges from 180, 000 and 320, 000 per mm 3. • Signs and symptoms • Often, low platelet levels do not lead to clinical problems; rather, they are picked up on a routine full blood count. Occasionally, there may be bruising, nosebleeds and/or bleeding gums. • It is vital that a full medical history is elicited, to ensure the low platelet count is not due to a secondary process. It is also important to ensure that the other blood cell types red blood cells, and white blood cells, are not also suppressed.
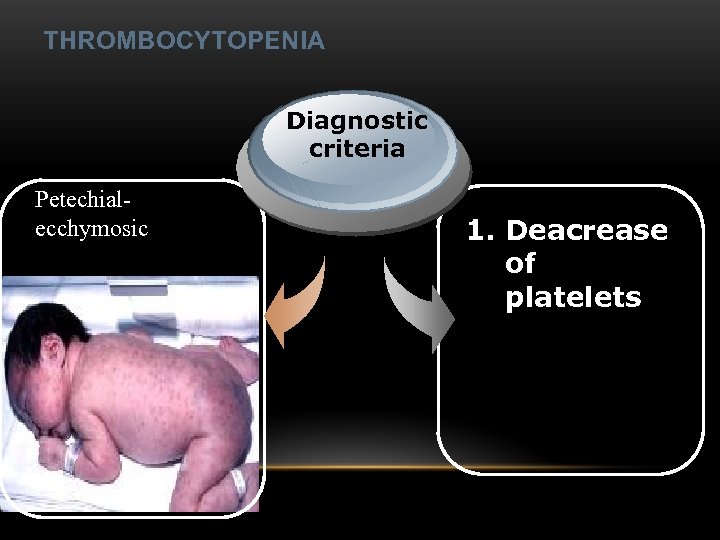 THROMBOCYTOPENIA Diagnostic criteria Petechialecchymosic 1. Deacrease of platelets
THROMBOCYTOPENIA Diagnostic criteria Petechialecchymosic 1. Deacrease of platelets
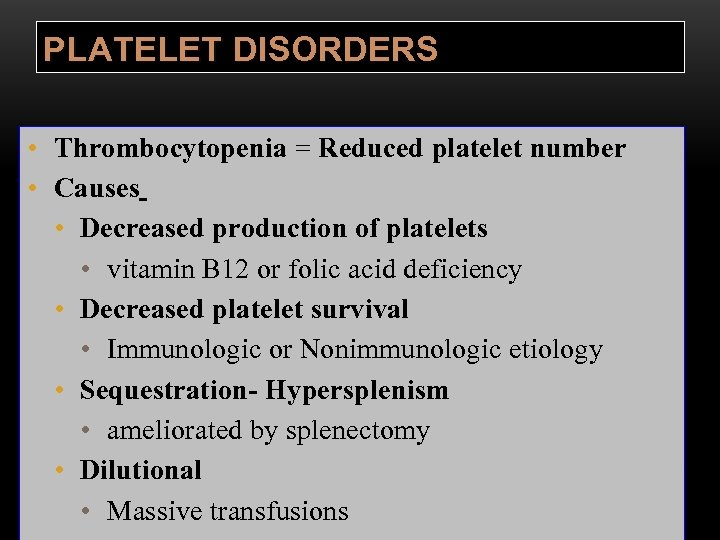 PLATELET DISORDERS • Thrombocytopenia = Reduced platelet number • Causes • Decreased production of platelets • vitamin B 12 or folic acid deficiency • Decreased platelet survival • Immunologic or Nonimmunologic etiology • Sequestration- Hypersplenism • ameliorated by splenectomy • Dilutional • Massive transfusions
PLATELET DISORDERS • Thrombocytopenia = Reduced platelet number • Causes • Decreased production of platelets • vitamin B 12 or folic acid deficiency • Decreased platelet survival • Immunologic or Nonimmunologic etiology • Sequestration- Hypersplenism • ameliorated by splenectomy • Dilutional • Massive transfusions
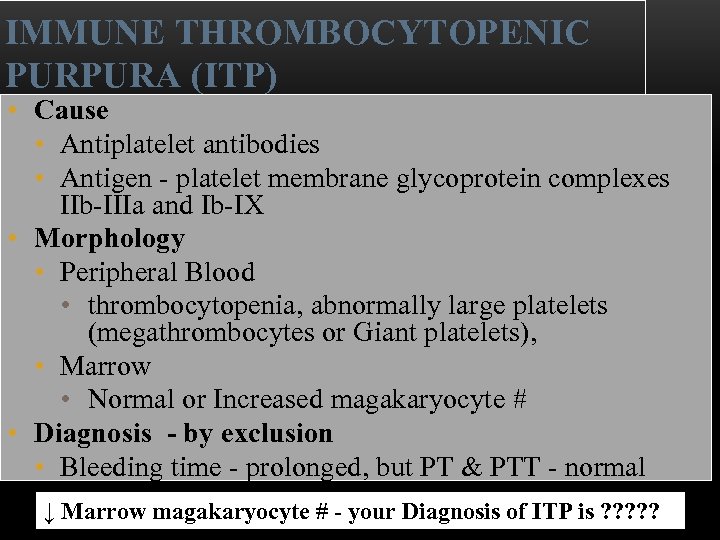 IMMUNE THROMBOCYTOPENIC PURPURA (ITP) • Cause • Antiplatelet antibodies • Antigen - platelet membrane glycoprotein complexes IIb-IIIa and Ib-IX • Morphology • Peripheral Blood • thrombocytopenia, abnormally large platelets (megathrombocytes or Giant platelets), • Marrow • Normal or Increased magakaryocyte # • Diagnosis - by exclusion • Bleeding time - prolonged, but PT & PTT - normal ↓ Marrow magakaryocyte # - your Diagnosis of ITP is ? ? ?
IMMUNE THROMBOCYTOPENIC PURPURA (ITP) • Cause • Antiplatelet antibodies • Antigen - platelet membrane glycoprotein complexes IIb-IIIa and Ib-IX • Morphology • Peripheral Blood • thrombocytopenia, abnormally large platelets (megathrombocytes or Giant platelets), • Marrow • Normal or Increased magakaryocyte # • Diagnosis - by exclusion • Bleeding time - prolonged, but PT & PTT - normal ↓ Marrow magakaryocyte # - your Diagnosis of ITP is ? ? ?
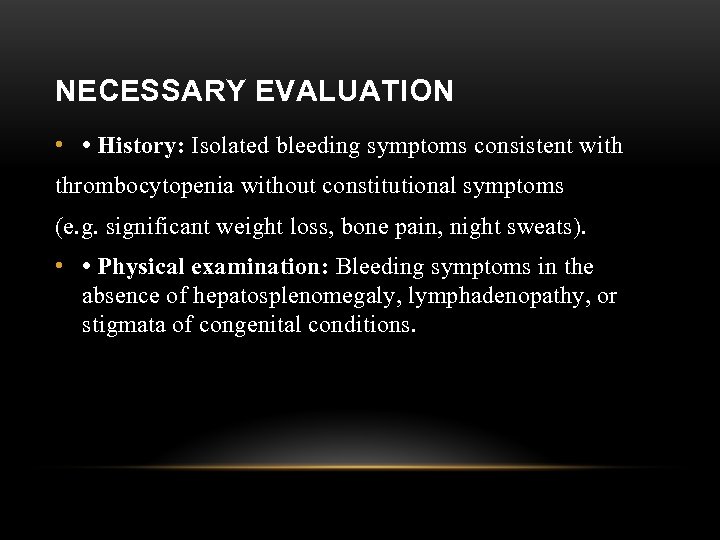 NECESSARY EVALUATION • • History: Isolated bleeding symptoms consistent with thrombocytopenia without constitutional symptoms (e. g. significant weight loss, bone pain, night sweats). • • Physical examination: Bleeding symptoms in the absence of hepatosplenomegaly, lymphadenopathy, or stigmata of congenital conditions.
NECESSARY EVALUATION • • History: Isolated bleeding symptoms consistent with thrombocytopenia without constitutional symptoms (e. g. significant weight loss, bone pain, night sweats). • • Physical examination: Bleeding symptoms in the absence of hepatosplenomegaly, lymphadenopathy, or stigmata of congenital conditions.
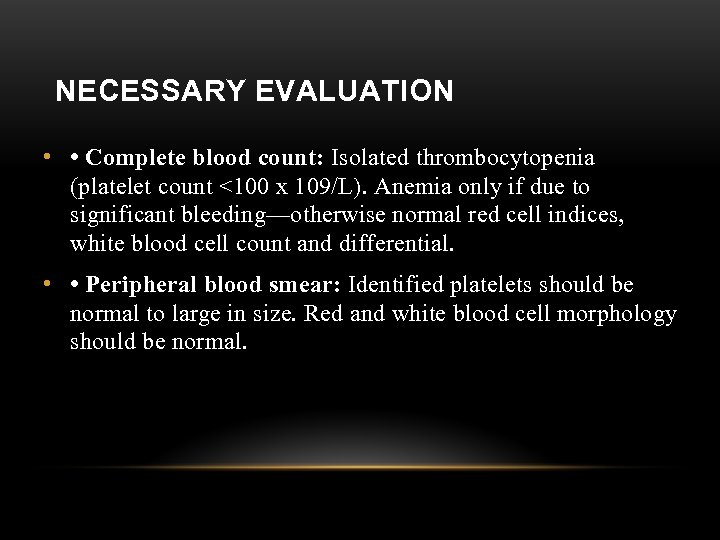 NECESSARY EVALUATION • • Complete blood count: Isolated thrombocytopenia (platelet count <100 x 109/L). Anemia only if due to significant bleeding—otherwise normal red cell indices, white blood cell count and differential. • • Peripheral blood smear: Identified platelets should be normal to large in size. Red and white blood cell morphology should be normal.
NECESSARY EVALUATION • • Complete blood count: Isolated thrombocytopenia (platelet count <100 x 109/L). Anemia only if due to significant bleeding—otherwise normal red cell indices, white blood cell count and differential. • • Peripheral blood smear: Identified platelets should be normal to large in size. Red and white blood cell morphology should be normal.
 BONE MARROW EVALUATION • • Bone marrow examination is unnecessary in patients with the typical features of ITP outlined above, irrespective of the age of the patient. • • Bone marrow examination is felt to be unnecessary in children with typical ITP prior to initiation of treatment with corticosteroids, prior to splenectomy, or in patients who fail intravenous immunoglobulin (IVIg) therapy.
BONE MARROW EVALUATION • • Bone marrow examination is unnecessary in patients with the typical features of ITP outlined above, irrespective of the age of the patient. • • Bone marrow examination is felt to be unnecessary in children with typical ITP prior to initiation of treatment with corticosteroids, prior to splenectomy, or in patients who fail intravenous immunoglobulin (IVIg) therapy.
 BONE MARROW EVALUATION • • The presence of abnormalities in the history, physical examination, or the complete blood count and peripheral blood smear should be further investigated, e. g. with a bone marrow examination or other appropriate investigations, before the diagnosis of ITP is made.
BONE MARROW EVALUATION • • The presence of abnormalities in the history, physical examination, or the complete blood count and peripheral blood smear should be further investigated, e. g. with a bone marrow examination or other appropriate investigations, before the diagnosis of ITP is made.
 ADDITIONAL EVALUATIONS • • All adult patients with newly diagnosed ITP should undergo testing for HIV and HCV. • • There is insufficient evidence to support the routine use of anti-platelet, antiphospholipid, and anti-nuclear antibodies, thrombopoietin levels, or platelet parameters obtained on automated analyzers in the evaluation of patients with suspected ITP.
ADDITIONAL EVALUATIONS • • All adult patients with newly diagnosed ITP should undergo testing for HIV and HCV. • • There is insufficient evidence to support the routine use of anti-platelet, antiphospholipid, and anti-nuclear antibodies, thrombopoietin levels, or platelet parameters obtained on automated analyzers in the evaluation of patients with suspected ITP.
 DIAGNOSTIC CRITERIA: • Plt_count: abnormal (low) • Peripheral blood smear: no increase in schistocytes • Bone_marrow: megakaryocytosis
DIAGNOSTIC CRITERIA: • Plt_count: abnormal (low) • Peripheral blood smear: no increase in schistocytes • Bone_marrow: megakaryocytosis
 THE MAIN BLEEDING SICKNESS TYPES • Petechia-ecchymosis (is usually localized to superficial sites such as the skin and mucous membranes, wich often combined with menorrhagia, nose bleeding, gumms bleeding; rare – with gastrointestinal bleeding or brain hemorrhage; it is small, painless, provoked by simple action like skin cleaning, measure of blood pressure etc; pinch test is positive)
THE MAIN BLEEDING SICKNESS TYPES • Petechia-ecchymosis (is usually localized to superficial sites such as the skin and mucous membranes, wich often combined with menorrhagia, nose bleeding, gumms bleeding; rare – with gastrointestinal bleeding or brain hemorrhage; it is small, painless, provoked by simple action like skin cleaning, measure of blood pressure etc; pinch test is positive)
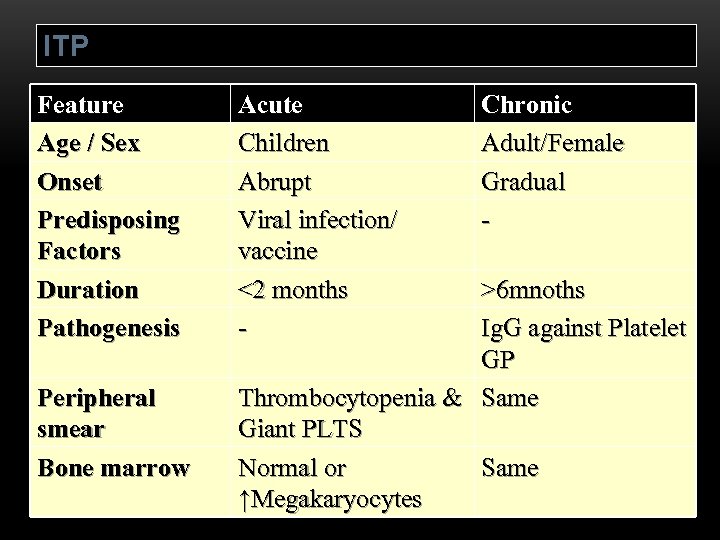 ITP Feature Age / Sex Onset Predisposing Factors Duration Pathogenesis Peripheral smear Bone marrow Acute Children Abrupt Viral infection/ vaccine <2 months - Chronic Adult/Female Gradual - >6 mnoths Ig. G against Platelet GP Thrombocytopenia & Same Giant PLTS Normal or Same ↑Megakaryocytes
ITP Feature Age / Sex Onset Predisposing Factors Duration Pathogenesis Peripheral smear Bone marrow Acute Children Abrupt Viral infection/ vaccine <2 months - Chronic Adult/Female Gradual - >6 mnoths Ig. G against Platelet GP Thrombocytopenia & Same Giant PLTS Normal or Same ↑Megakaryocytes
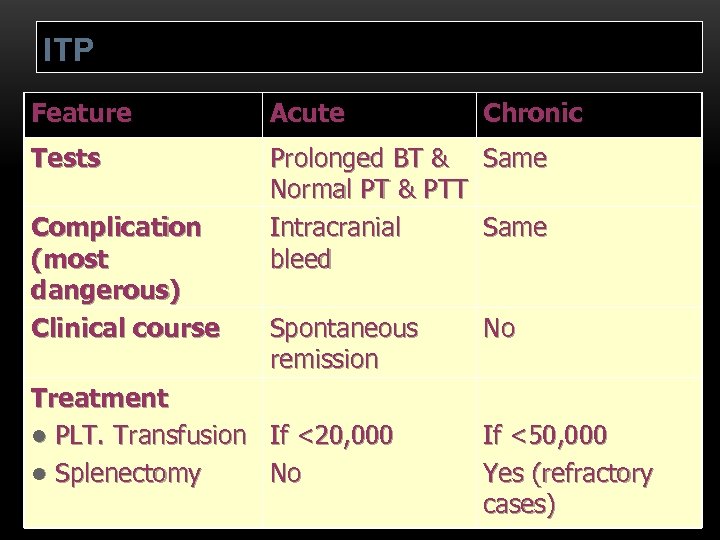 ITP Feature Acute Tests Prolonged BT & Same Normal PT & PTT Intracranial Same bleed Complication (most dangerous) Clinical course Spontaneous remission Treatment l PLT. Transfusion If <20, 000 l Splenectomy No Chronic No If <50, 000 Yes (refractory cases)
ITP Feature Acute Tests Prolonged BT & Same Normal PT & PTT Intracranial Same bleed Complication (most dangerous) Clinical course Spontaneous remission Treatment l PLT. Transfusion If <20, 000 l Splenectomy No Chronic No If <50, 000 Yes (refractory cases)
 Condition Partial Prothrombin thromboplast Bleeding time in time Platelet count Vitamin K deficiency or prolonged warfarin normal or mildly prolonged unaffected Disseminated prolonged intravascular coagulation prolonged decreased von Willebrand disease unaffected prolonged unaffected Hemophilia unaffected prolonged unaffected Aspirin unaffected prolonged unaffected Thrombocytopeni unaffected prolonged a Uremia Glanzmann's thrombasthenia Bernard-Soulier syndrome decreased unaffected unaffected prolonged decreased or unaffected
Condition Partial Prothrombin thromboplast Bleeding time in time Platelet count Vitamin K deficiency or prolonged warfarin normal or mildly prolonged unaffected Disseminated prolonged intravascular coagulation prolonged decreased von Willebrand disease unaffected prolonged unaffected Hemophilia unaffected prolonged unaffected Aspirin unaffected prolonged unaffected Thrombocytopeni unaffected prolonged a Uremia Glanzmann's thrombasthenia Bernard-Soulier syndrome decreased unaffected unaffected prolonged decreased or unaffected
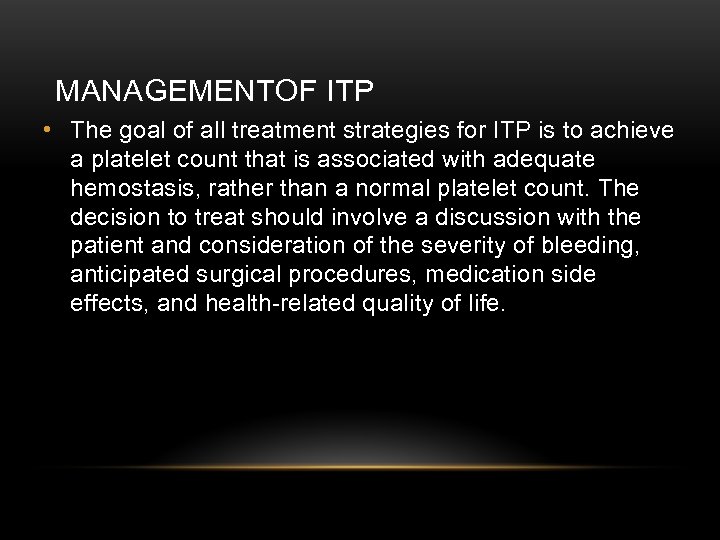 MANAGEMENTOF ITP • The goal of all treatment strategies for ITP is to achieve a platelet count that is associated with adequate hemostasis, rather than a normal platelet count. The decision to treat should involve a discussion with the patient and consideration of the severity of bleeding, anticipated surgical procedures, medication side effects, and health-related quality of life.
MANAGEMENTOF ITP • The goal of all treatment strategies for ITP is to achieve a platelet count that is associated with adequate hemostasis, rather than a normal platelet count. The decision to treat should involve a discussion with the patient and consideration of the severity of bleeding, anticipated surgical procedures, medication side effects, and health-related quality of life.
 INITIAL MANAGEMENT OF ITP • Assessment of Disease Status: • • What bleeding is the patient experiencing? • • Determine the timing, location, and severity of • bleeding symptoms. • • Does this patient have any additional risk factors for bleeding such as use of antithrombotic agents or high-risk occupation? • • Is a surgical procedure anticipated? • • Is this patient likely to comply with recommended treatments? • • Is the bleeding experienced by this patient interfering with his or her daily activities or causing significant
INITIAL MANAGEMENT OF ITP • Assessment of Disease Status: • • What bleeding is the patient experiencing? • • Determine the timing, location, and severity of • bleeding symptoms. • • Does this patient have any additional risk factors for bleeding such as use of antithrombotic agents or high-risk occupation? • • Is a surgical procedure anticipated? • • Is this patient likely to comply with recommended treatments? • • Is the bleeding experienced by this patient interfering with his or her daily activities or causing significant
 GENERAL CONSIDERATIONS FOR INITIAL MANAGEMENT • • The majority of patients with no bleeding or mild bleeding (defined here as skin manifestations only, such as petechiae and bruising) can be treated with observation alone regardless of platelet count. • • First-line treatment includes observation, corticosteroids, IVIg, or anti-D immunoglobulin (anti-D). • • Anti-D should be used with caution given recent FDA warnings of severe hemolysis. It is therefore not advised in patients with bleeding causing a decline in hemoglobin, or those with evidence of autoimmune hemolysis.
GENERAL CONSIDERATIONS FOR INITIAL MANAGEMENT • • The majority of patients with no bleeding or mild bleeding (defined here as skin manifestations only, such as petechiae and bruising) can be treated with observation alone regardless of platelet count. • • First-line treatment includes observation, corticosteroids, IVIg, or anti-D immunoglobulin (anti-D). • • Anti-D should be used with caution given recent FDA warnings of severe hemolysis. It is therefore not advised in patients with bleeding causing a decline in hemoglobin, or those with evidence of autoimmune hemolysis.
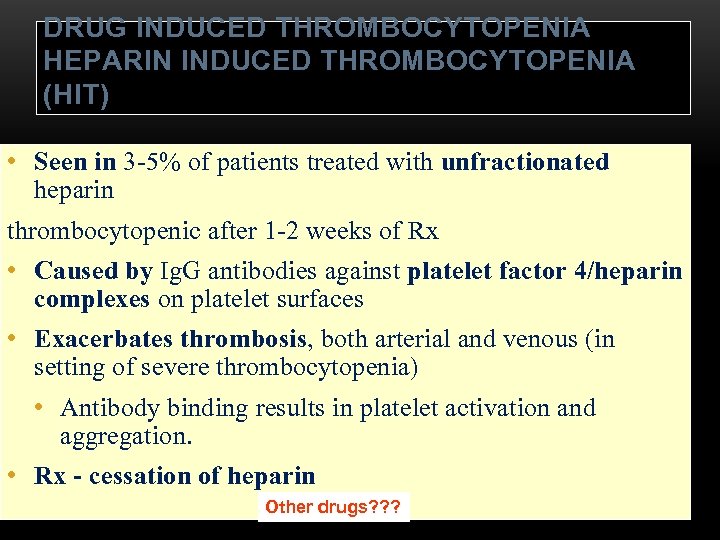 DRUG INDUCED THROMBOCYTOPENIA HEPARIN INDUCED THROMBOCYTOPENIA (HIT) • Seen in 3 -5% of patients treated with unfractionated heparin thrombocytopenic after 1 -2 weeks of Rx • Caused by Ig. G antibodies against platelet factor 4/heparin complexes on platelet surfaces • Exacerbates thrombosis, both arterial and venous (in setting of severe thrombocytopenia) • Antibody binding results in platelet activation and aggregation. • Rx - cessation of heparin Other drugs? ? ?
DRUG INDUCED THROMBOCYTOPENIA HEPARIN INDUCED THROMBOCYTOPENIA (HIT) • Seen in 3 -5% of patients treated with unfractionated heparin thrombocytopenic after 1 -2 weeks of Rx • Caused by Ig. G antibodies against platelet factor 4/heparin complexes on platelet surfaces • Exacerbates thrombosis, both arterial and venous (in setting of severe thrombocytopenia) • Antibody binding results in platelet activation and aggregation. • Rx - cessation of heparin Other drugs? ? ?
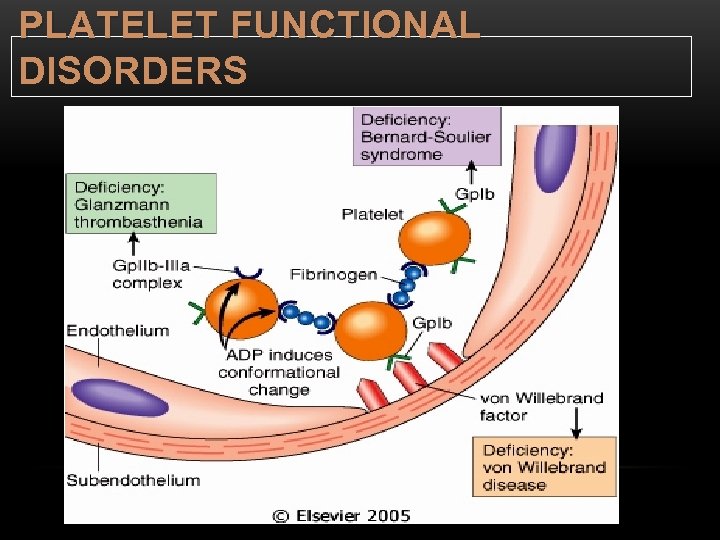 PLATELET FUNCTIONAL DISORDERS
PLATELET FUNCTIONAL DISORDERS
 Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
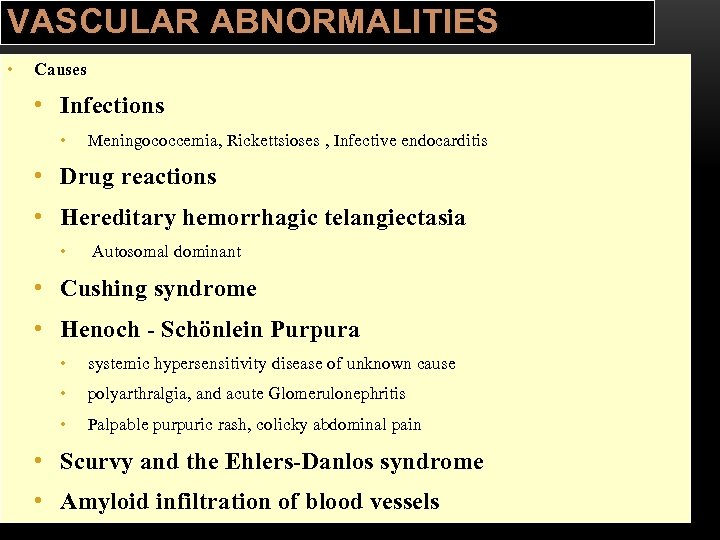 VASCULAR ABNORMALITIES • Causes • Infections • Meningococcemia, Rickettsioses , Infective endocarditis • Drug reactions • Hereditary hemorrhagic telangiectasia • Autosomal dominant • Cushing syndrome • Henoch - Schönlein Purpura • systemic hypersensitivity disease of unknown cause • polyarthralgia, and acute Glomerulonephritis • Palpable purpuric rash, colicky abdominal pain • Scurvy and the Ehlers-Danlos syndrome • Amyloid infiltration of blood vessels
VASCULAR ABNORMALITIES • Causes • Infections • Meningococcemia, Rickettsioses , Infective endocarditis • Drug reactions • Hereditary hemorrhagic telangiectasia • Autosomal dominant • Cushing syndrome • Henoch - Schönlein Purpura • systemic hypersensitivity disease of unknown cause • polyarthralgia, and acute Glomerulonephritis • Palpable purpuric rash, colicky abdominal pain • Scurvy and the Ehlers-Danlos syndrome • Amyloid infiltration of blood vessels
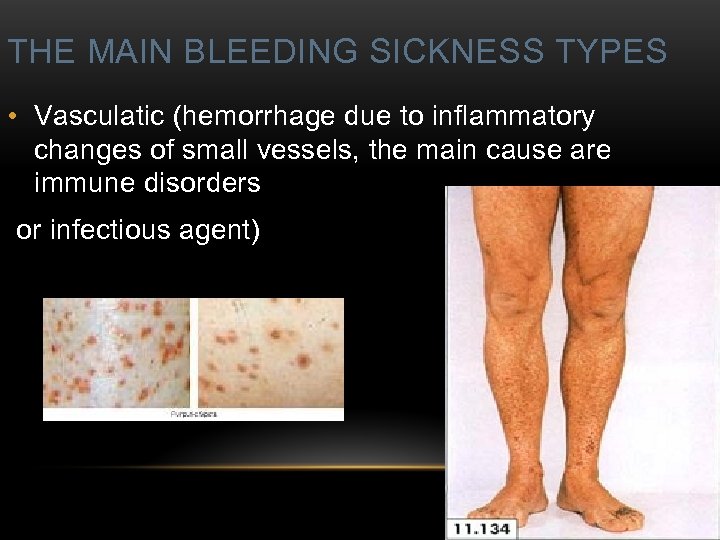 THE MAIN BLEEDING SICKNESS TYPES • Vasculatic (hemorrhage due to inflammatory changes of small vessels, the main cause are immune disorders or infectious agent)
THE MAIN BLEEDING SICKNESS TYPES • Vasculatic (hemorrhage due to inflammatory changes of small vessels, the main cause are immune disorders or infectious agent)
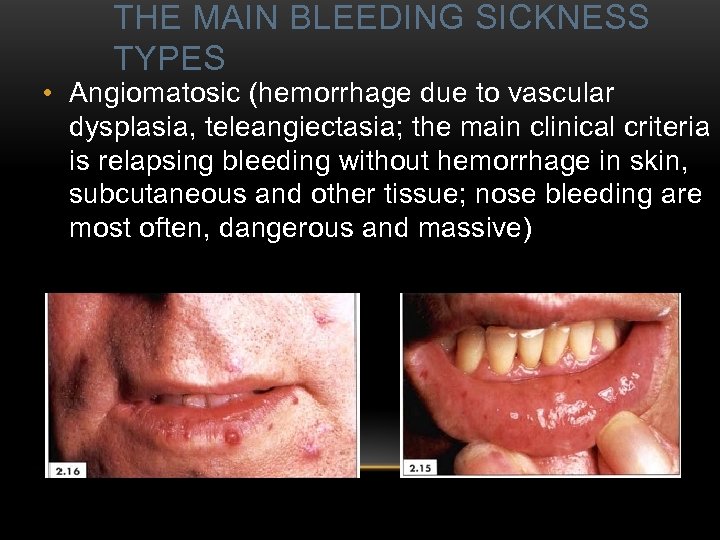 THE MAIN BLEEDING SICKNESS TYPES • Angiomatosic (hemorrhage due to vascular dysplasia, teleangiectasia; the main clinical criteria is relapsing bleeding without hemorrhage in skin, subcutaneous and other tissue; nose bleeding are most often, dangerous and massive)
THE MAIN BLEEDING SICKNESS TYPES • Angiomatosic (hemorrhage due to vascular dysplasia, teleangiectasia; the main clinical criteria is relapsing bleeding without hemorrhage in skin, subcutaneous and other tissue; nose bleeding are most often, dangerous and massive)
 Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
Bleeding disorders Vascular abnormalities Platelet disorders Clotting factor abnormalities DIC
 Thank you for attention!
Thank you for attention!


