dbac26f82301f610019bcddf64140b61.ppt
- Количество слайдов: 66
Hematuria in children Abbas Al. Abbad, M. D. Manama, Bahrain 7 May 2009


Urine Colors
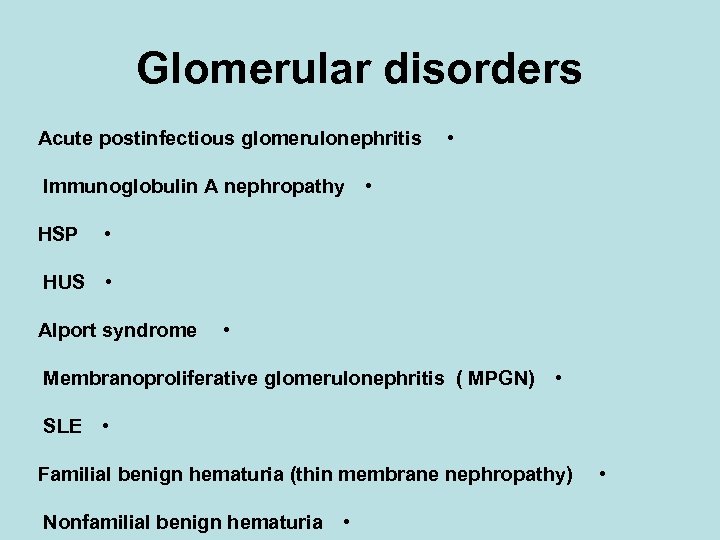
Glomerular disorders Acute postinfectious glomerulonephritis Immunoglobulin A nephropathy HSP • • • HUS • Alport syndrome • Membranoproliferative glomerulonephritis ( MPGN) • SLE • Familial benign hematuria (thin membrane nephropathy) Nonfamilial benign hematuria • •
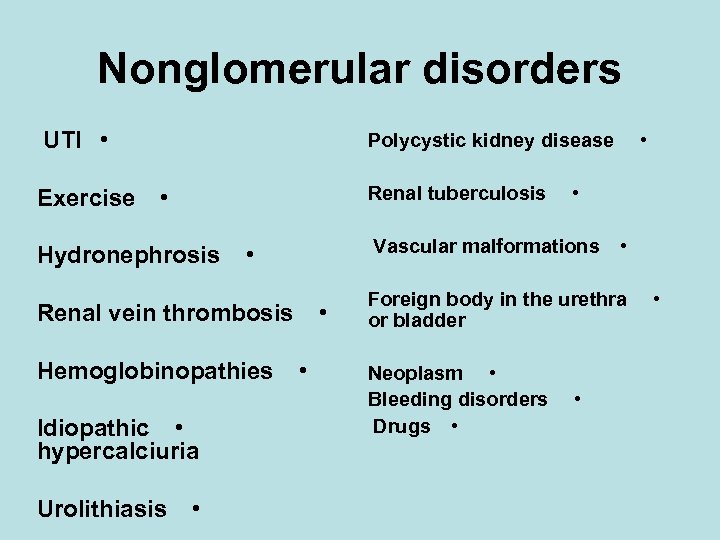
Nonglomerular disorders UTI • Exercise • Polycystic kidney disease Renal tuberculosis • Hydronephrosis Vascular malformations • • Renal vein thrombosis Hemoglobinopathies Idiopathic • hypercalciuria Urolithiasis • • Foreign body in the urethra or bladder Neoplasm • Bleeding disorders Drugs • • •
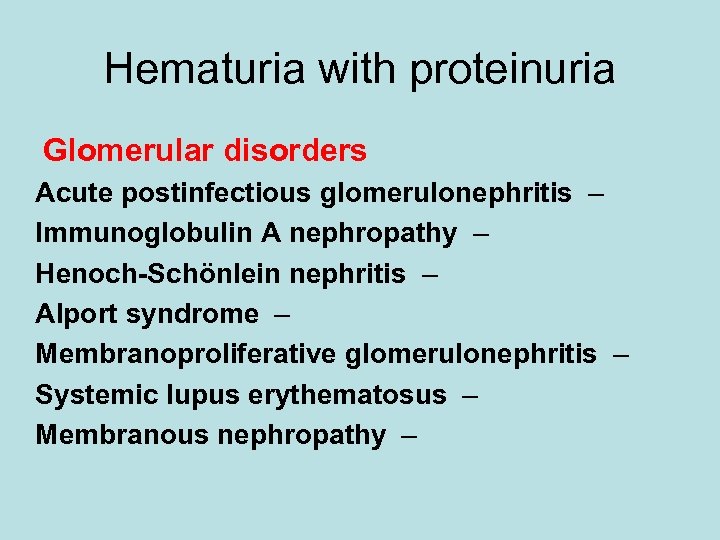
Hematuria with proteinuria Glomerular disorders Acute postinfectious glomerulonephritis – Immunoglobulin A nephropathy – Henoch-Schönlein nephritis – Alport syndrome – Membranoproliferative glomerulonephritis – Systemic lupus erythematosus – Membranous nephropathy –
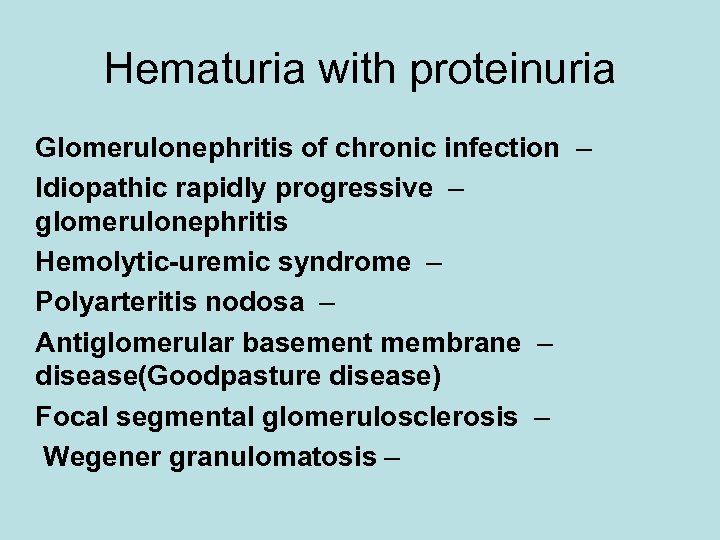
Hematuria with proteinuria Glomerulonephritis of chronic infection – Idiopathic rapidly progressive – glomerulonephritis Hemolytic-uremic syndrome – Polyarteritis nodosa – Antiglomerular basement membrane – disease(Goodpasture disease) Focal segmental glomerulosclerosis – Wegener granulomatosis –
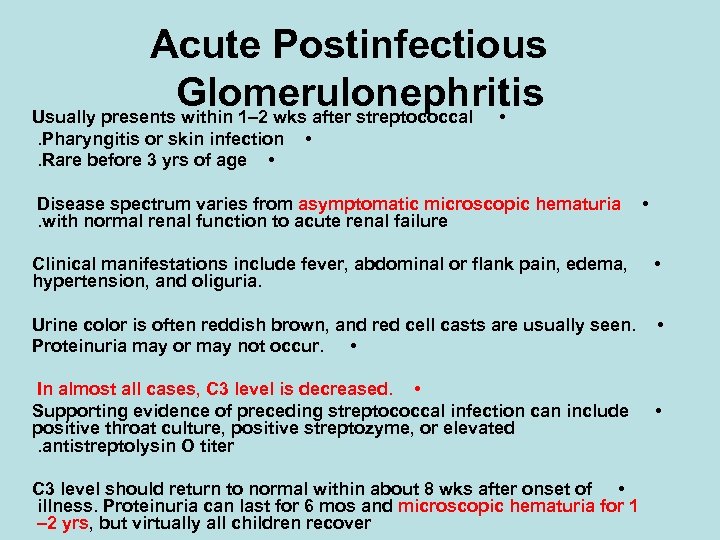
Acute Postinfectious Glomerulonephritis Usually presents within 1– 2 wks after streptococcal • . Pharyngitis or skin infection. Rare before 3 yrs of age • • Disease spectrum varies from asymptomatic microscopic hematuria. with normal renal function to acute renal failure • Clinical manifestations include fever, abdominal or flank pain, edema, hypertension, and oliguria. • Urine color is often reddish brown, and red cell casts are usually seen. Proteinuria may or may not occur. • • In almost all cases, C 3 level is decreased. • Supporting evidence of preceding streptococcal infection can include positive throat culture, positive streptozyme, or elevated. antistreptolysin O titer C 3 level should return to normal within about 8 wks after onset of • illness. Proteinuria can last for 6 mos and microscopic hematuria for 1 – 2 yrs, but virtually all children recover •

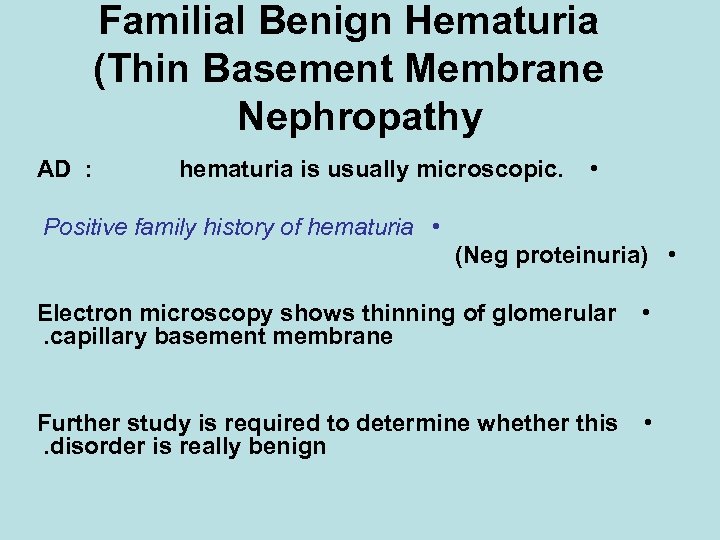
Familial Benign Hematuria (Thin Basement Membrane Nephropathy AD : hematuria is usually microscopic. • Positive family history of hematuria • (Neg proteinuria) • Electron microscopy shows thinning of glomerular. capillary basement membrane • Further study is required to determine whether this. disorder is really benign •
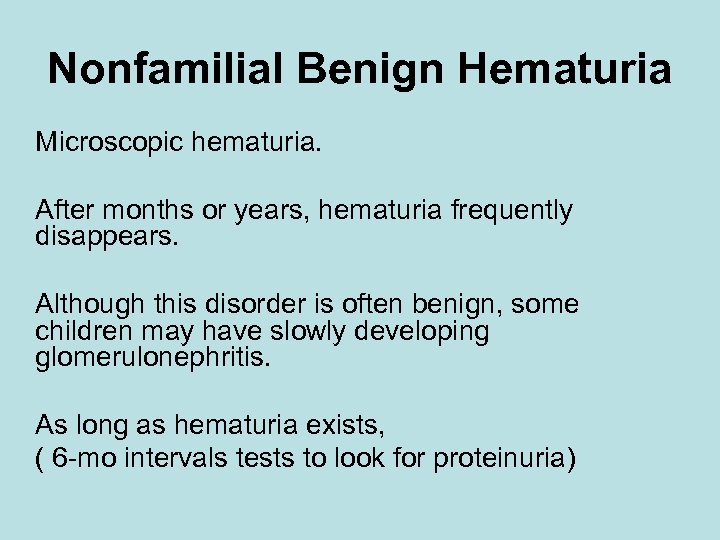
Nonfamilial Benign Hematuria Microscopic hematuria. After months or years, hematuria frequently disappears. Although this disorder is often benign, some children may have slowly developing glomerulonephritis. As long as hematuria exists, ( 6 -mo intervals tests to look for proteinuria)
Alport Syndrome Recurrent gross hematuria or asymptomatic microscopic hematuria. ensorineural hearing loss. S X-linked ( AD or AR <10 %) X-linked phenotype ( alpha-5 Collagen IV) • Progressive renal insufficiency (? ? delayed by ACEI, ARB) Kidney Transplant • •
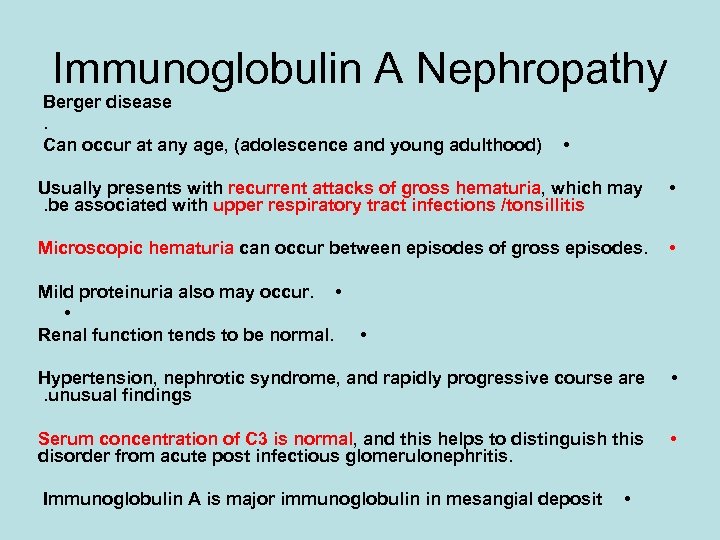
Immunoglobulin A Nephropathy Berger disease. Can occur at any age, (adolescence and young adulthood) • Usually presents with recurrent attacks of gross hematuria, which may. be associated with upper respiratory tract infections /tonsillitis • Microscopic hematuria can occur between episodes of gross episodes. • Mild proteinuria also may occur. • • Renal function tends to be normal. • Hypertension, nephrotic syndrome, and rapidly progressive course are. unusual findings • Serum concentration of C 3 is normal, and this helps to distinguish this disorder from acute post infectious glomerulonephritis. • Immunoglobulin A is major immunoglobulin in mesangial deposit •
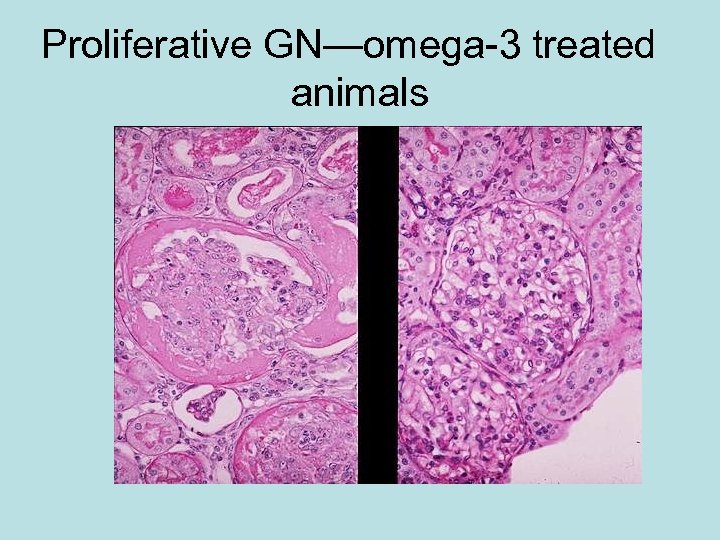
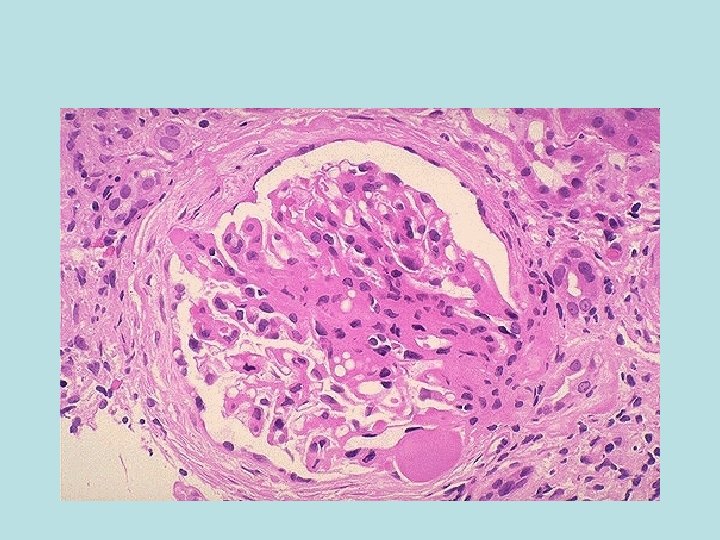
Proliferative GN—omega-3 treated animals
NON GLOMERULAR (Not Nephritis) UTI • ysuria, frequency, urgency, fever, pain, flank pain, and vomiting. • Microscopic or gross hematuria can occur • . pyuria and bacteriuria Positive urine culture confirms the diagnosis •
Hydronephrosis In children with hydronephrosis, microscopicor gross hematuria may occur following mild flank or abdominal Trauma or even NON traumatic
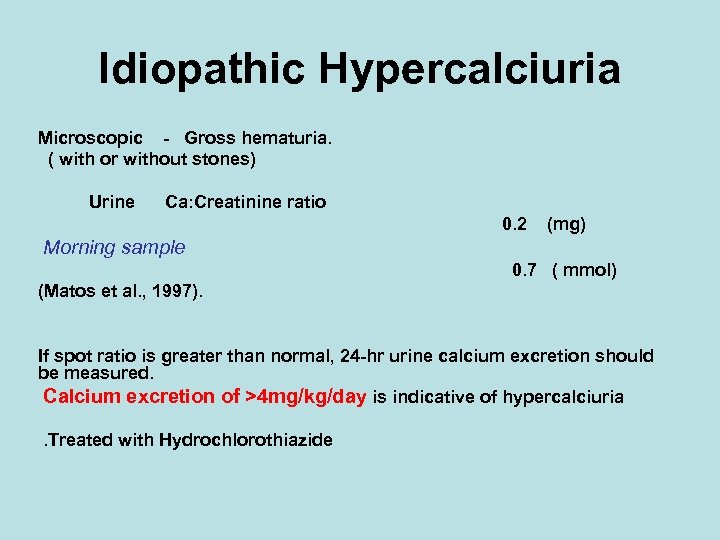
Idiopathic Hypercalciuria Microscopic - Gross hematuria. ( with or without stones) Urine Ca: Creatinine ratio 0. 2 (mg) Morning sample 0. 7 ( mmol) (Matos et al. , 1997). If spot ratio is greater than normal, 24 -hr urine calcium excretion should be measured. Calcium excretion of >4 mg/kg/day is indicative of hypercalciuria. Treated with Hydrochlorothiazide
Nephrocalcinosis Nephrouro-lithiasis UTI Hypercalciuria Hyperuricosuria, Cystinuria, . Hyperoxaluria Microscopic or gross hematuria Treatment will depend on the cause •
Hemoglobinopathies Sickle cell anemia or trait Sickle beta-thalassemia can produce renal bleeding and microscopic or. gross hematuria Hemoglobin electrophoresis should be • performed in any child of unknown. cause of hematuria
Drugs Penicillins Sulfonamides, Cephalosporins, Rifampin, Tetracycline, Cisplatin, Lithium) Cyclophosphamide (hemorrhagic cystitis)

Diagnostic Approach Hematuria without Proteinuria • Hematuria with Proteinuria •


Blood tests Renal function Ca Po Uric acid Mg p. H Oxalate Citrate
Others C 3 • C 4 • ANA profile • ANCA • STREPTOZYME • DNAse B • ( More specific. esp. in skin lesions) OTHERS •
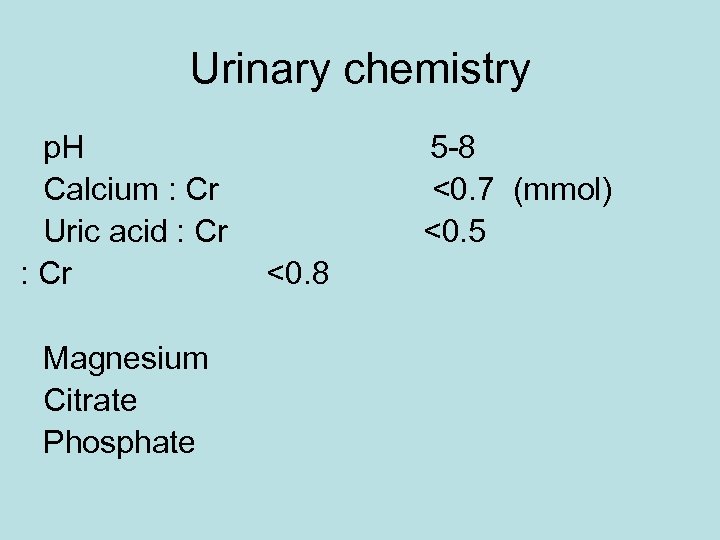
Urinary chemistry p. H Calcium : Cr Uric acid : Cr Magnesium Citrate Phosphate 5 -8 <0. 7 (mmol) <0. 5 <0. 8
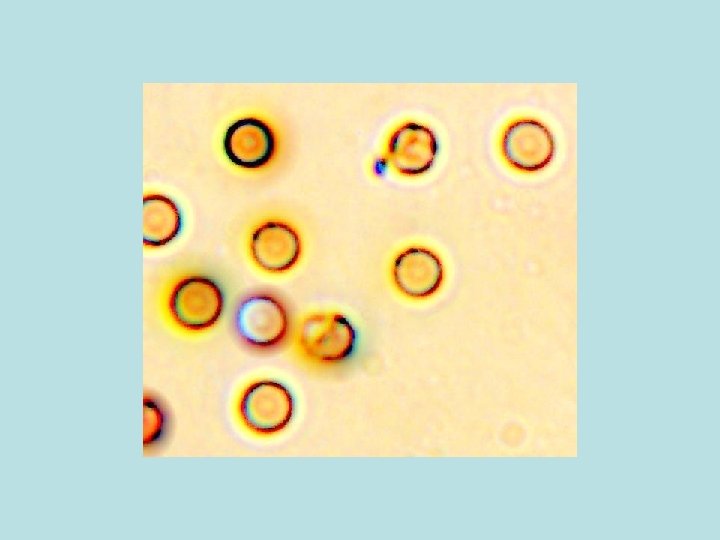
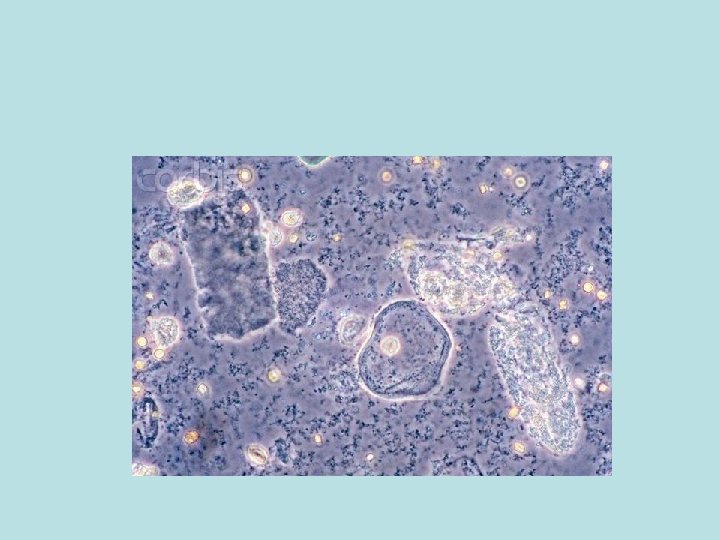
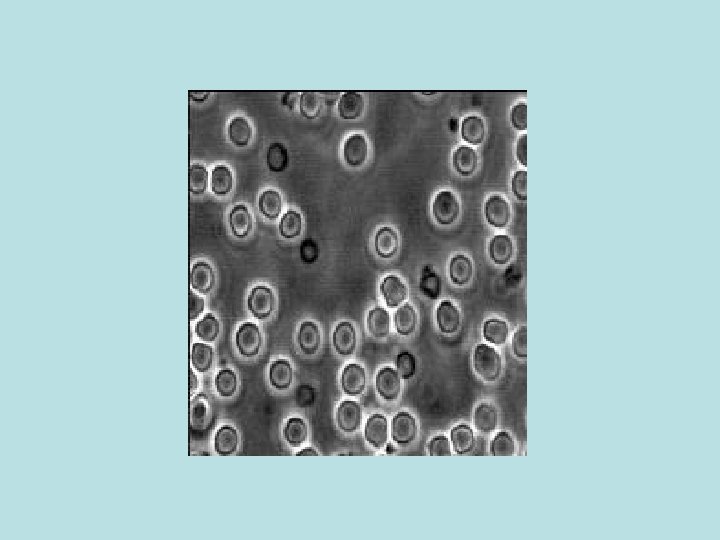
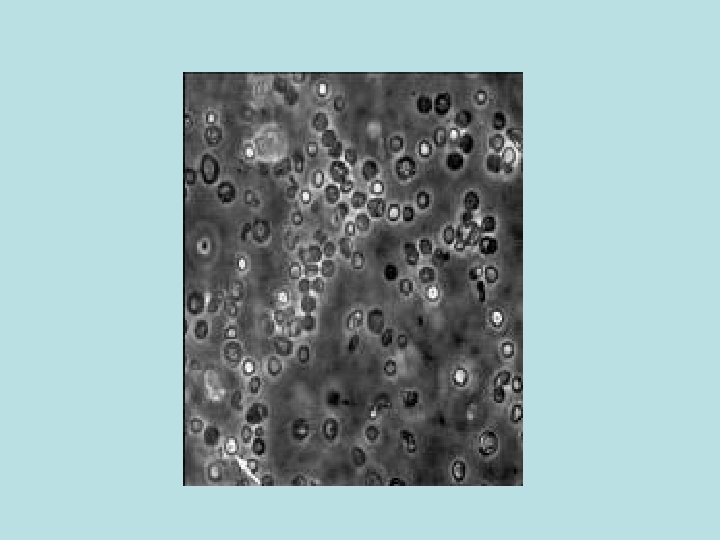
Differential Interference Contrast Microscopy
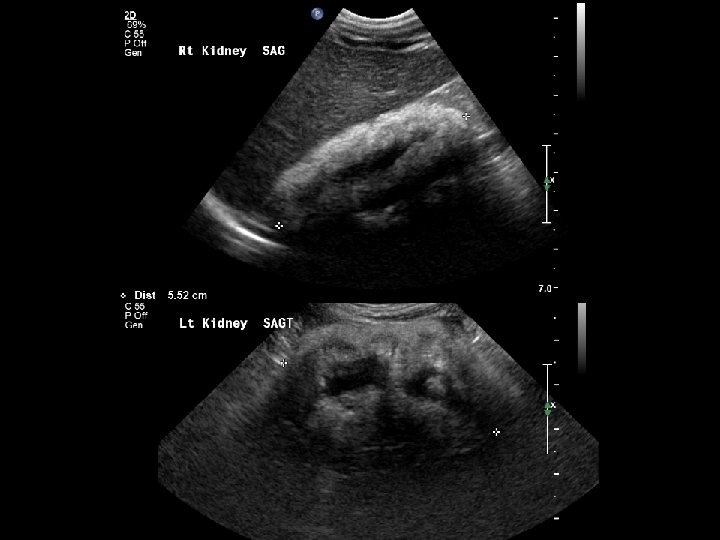
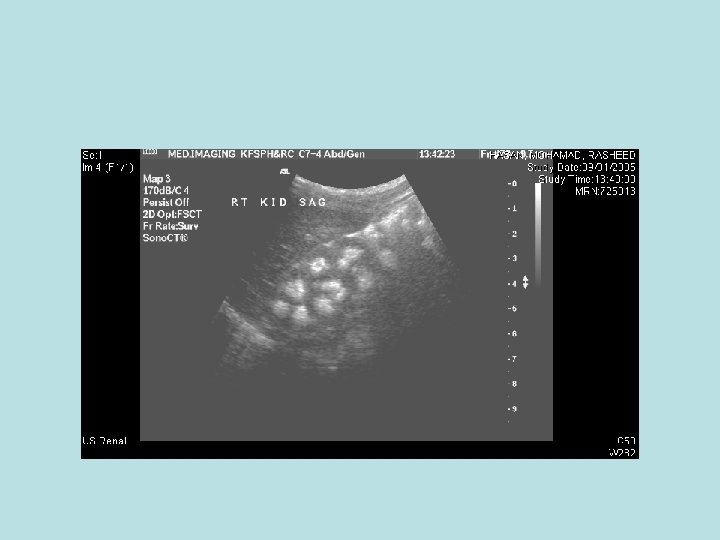
Radiological Studies Abdominal US KUB CT MRI/A

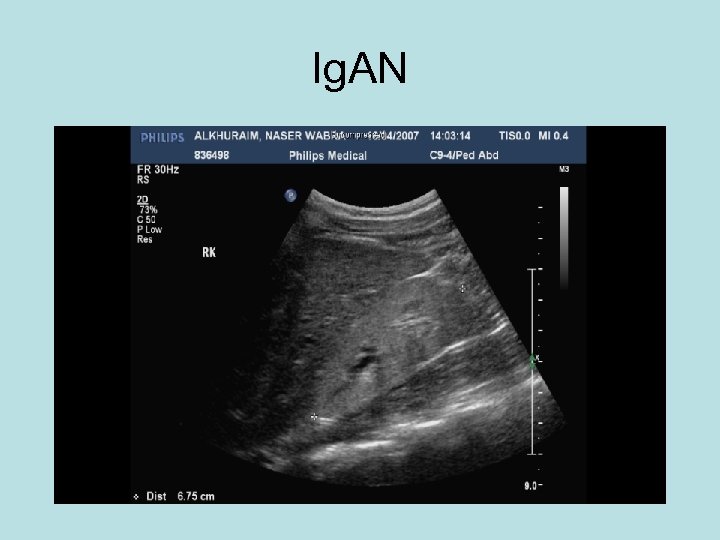
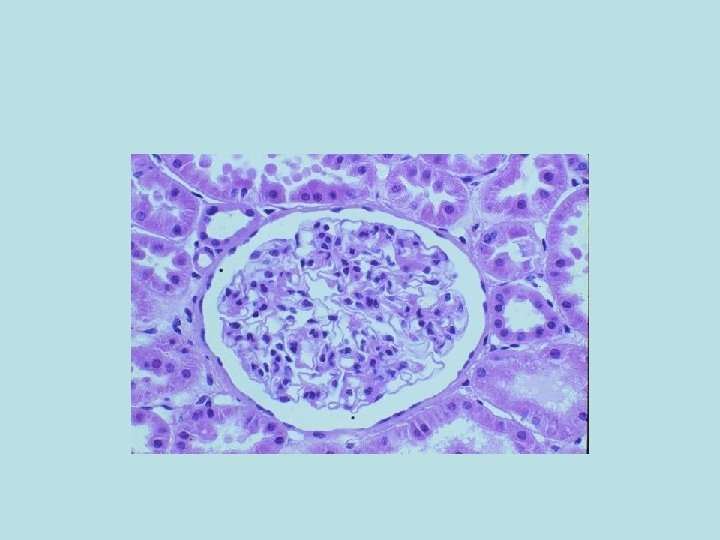
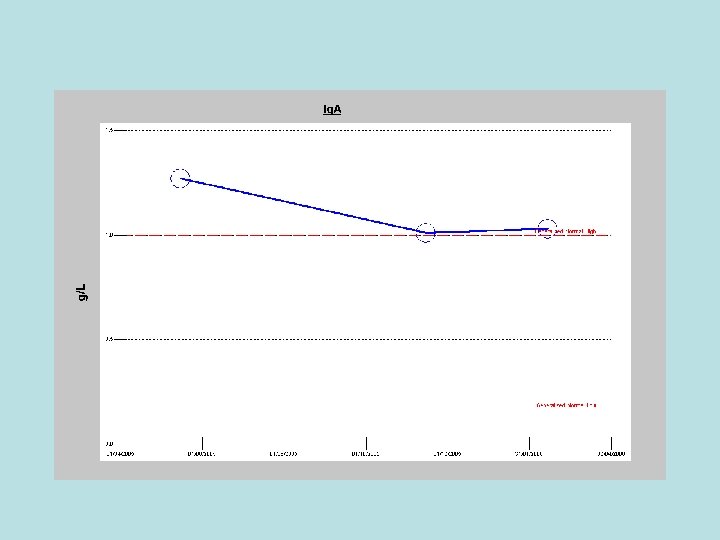
Ig. AN
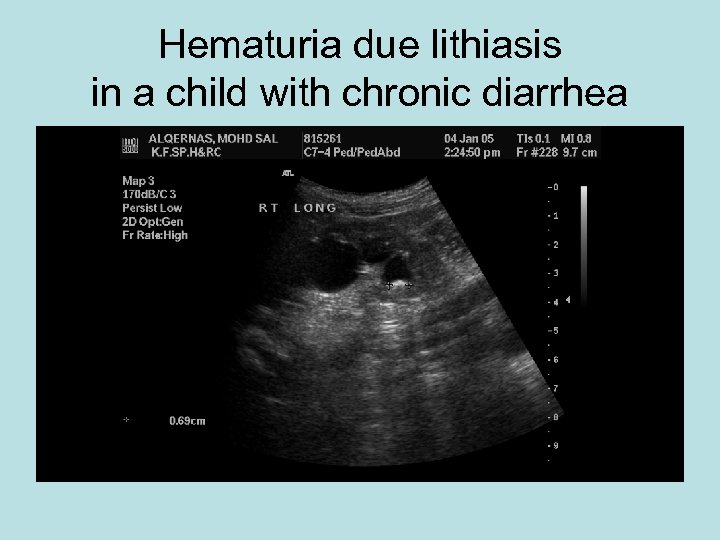
Hematuria due lithiasis in a child with chronic diarrhea
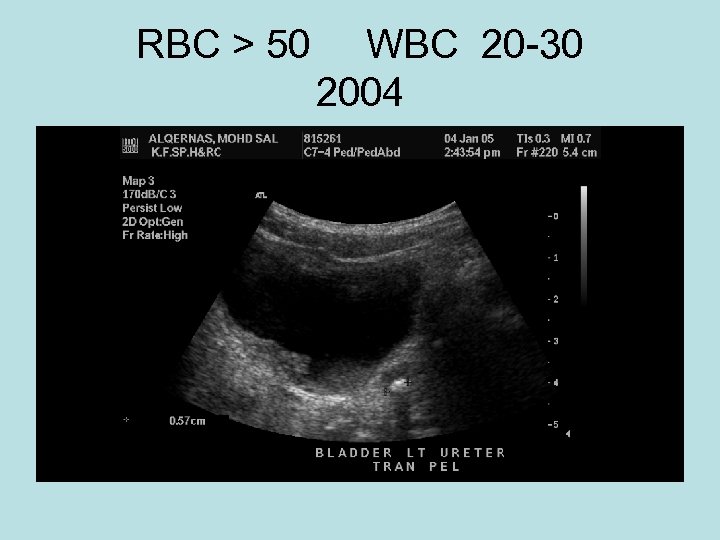
RBC > 50 WBC 20 -30 2004
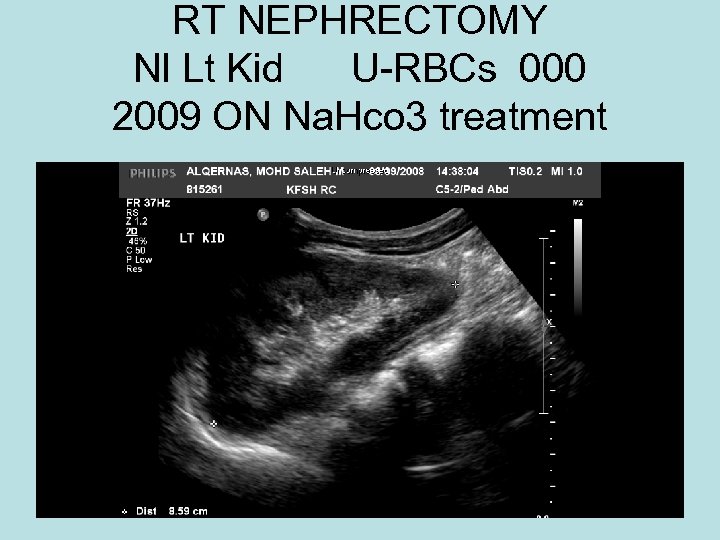
RT NEPHRECTOMY Nl Lt Kid U-RBCs 000 2009 ON Na. Hco 3 treatment
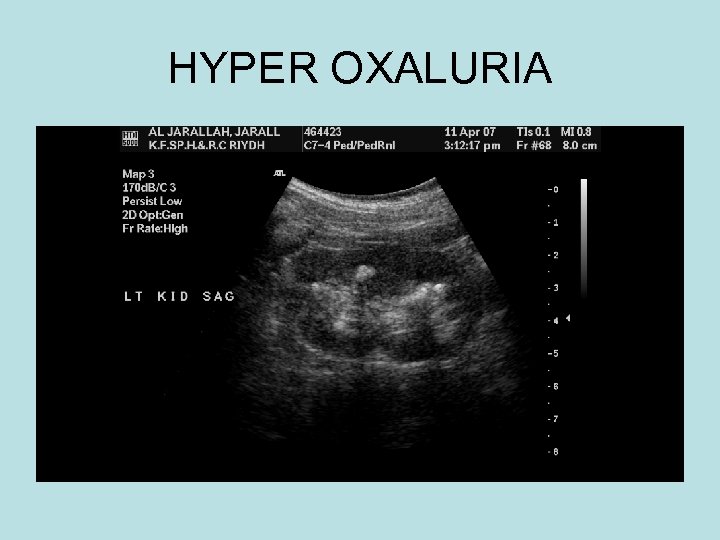
HYPER OXALURIA
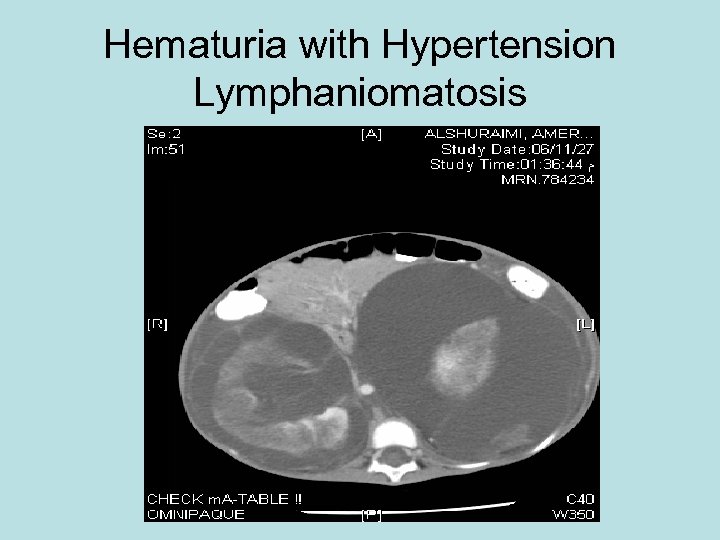
Hematuria with Hypertension Lymphaniomatosis
Case evidence 9 yr old boy Recurrent abd. Pain Microscopic hematuria Concentrated urine Referred with NEG: US, CT, BARIUM, ENDOSCOPY. NL GFR.
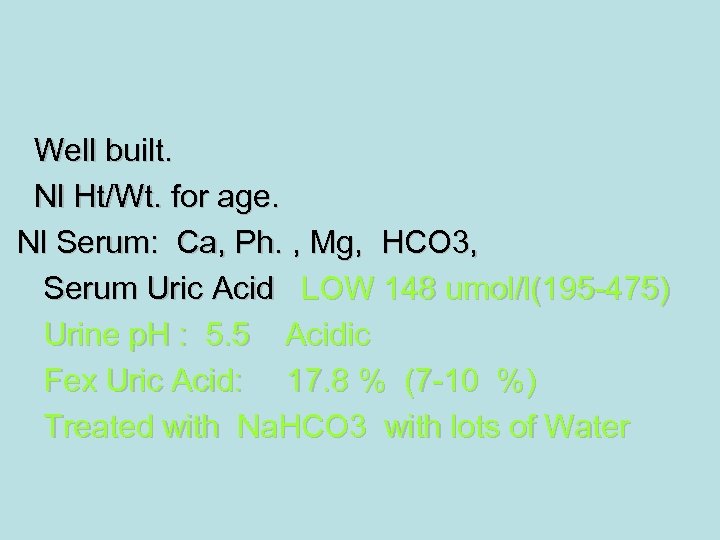
Well built. Nl Ht/Wt. for age. Nl Serum: Ca, Ph. , Mg, HCO 3, Serum Uric Acid LOW 148 umol/l(195 -475) Urine p. H : 5. 5 Acidic Fex Uric Acid: 17. 8 % (7 -10 %) Treated with Na. HCO 3 with lots of Water
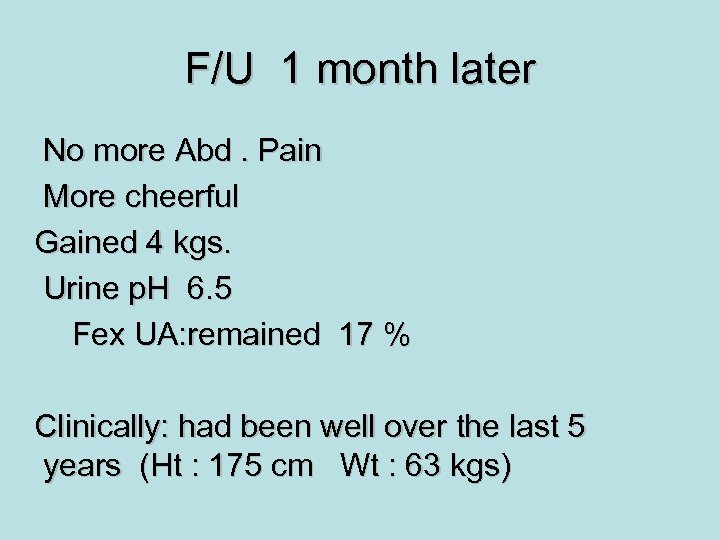
F/U 1 month later No more Abd. Pain More cheerful Gained 4 kgs. Urine p. H 6. 5 Fex UA: remained 17 % Clinically: had been well over the last 5 years (Ht : 175 cm Wt : 63 kgs)
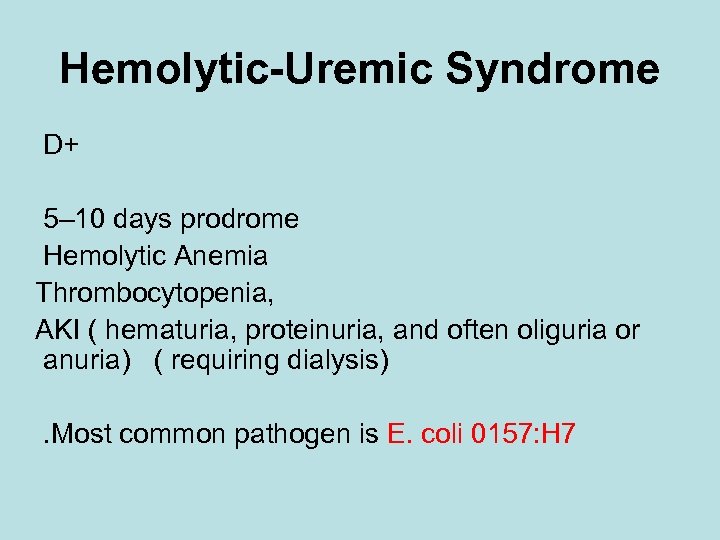
Hemolytic-Uremic Syndrome D+ 5– 10 days prodrome Hemolytic Anemia Thrombocytopenia, AKI ( hematuria, proteinuria, and often oliguria or anuria) ( requiring dialysis). Most common pathogen is E. coli 0157: H 7
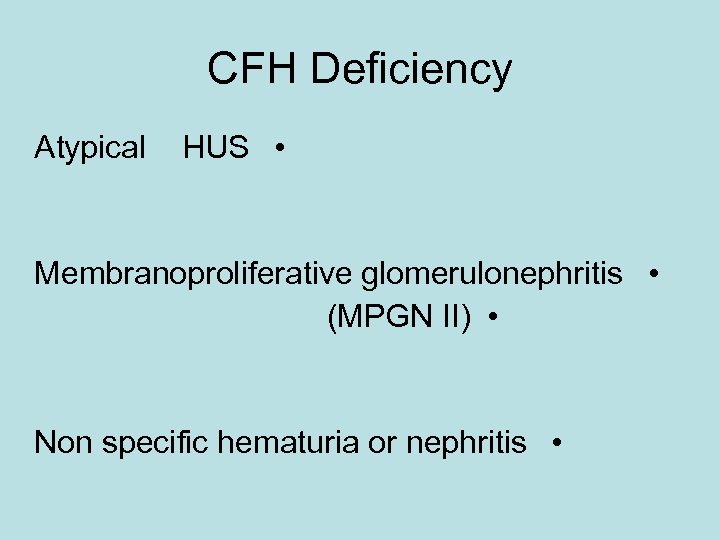
CFH Deficiency Atypical HUS • Membranoproliferative glomerulonephritis • (MPGN II) • Non specific hematuria or nephritis •
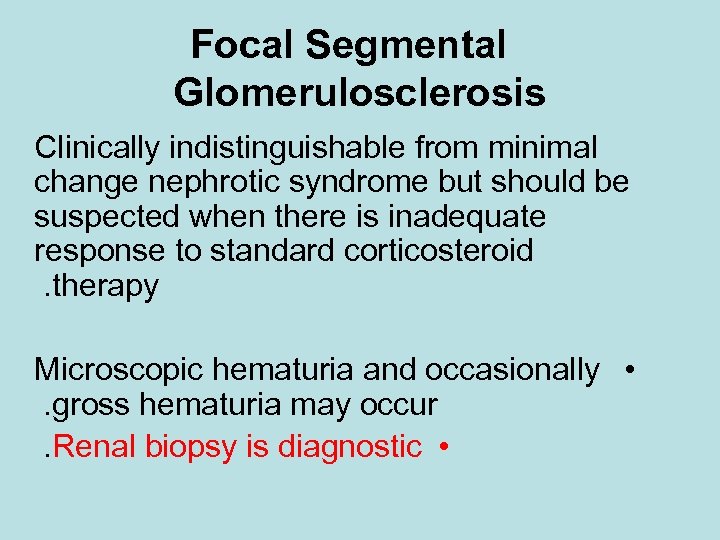
Focal Segmental Glomerulosclerosis Clinically indistinguishable from minimal change nephrotic syndrome but should be suspected when there is inadequate response to standard corticosteroid. therapy Microscopic hematuria and occasionally • . gross hematuria may occur. Renal biopsy is diagnostic •
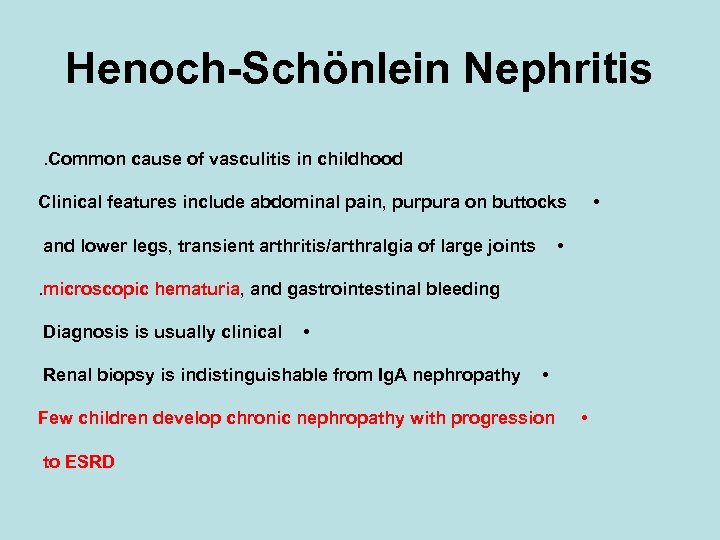
Henoch-Schönlein Nephritis. Common cause of vasculitis in childhood • Clinical features include abdominal pain, purpura on buttocks • and lower legs, transient arthritis/arthralgia of large joints. microscopic hematuria, and gastrointestinal bleeding Diagnosis is usually clinical • Renal biopsy is indistinguishable from Ig. A nephropathy • Few children develop chronic nephropathy with progression to ESRD •
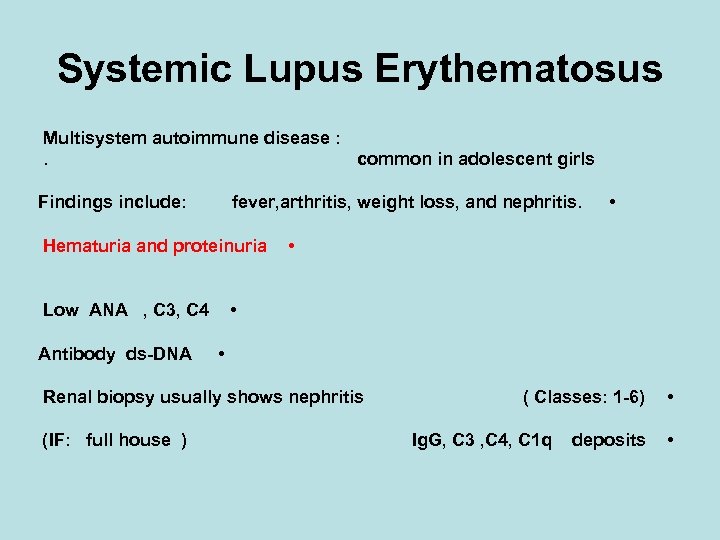
Systemic Lupus Erythematosus Multisystem autoimmune disease : . common in adolescent girls Findings include: fever, arthritis, weight loss, and nephritis. Hematuria and proteinuria • • Low ANA , C 3, C 4 Antibody ds-DNA • Renal biopsy usually shows nephritis ( IF: full house ) • ( Classes: 1 -6) Ig. G, C 3 , C 4, C 1 q deposits • •
Wegener Granulomatosis Vasculitis that affects upper and lower respiratory tract and kidneys Clinically: Fever, malaise, weight loss, hemoptysis, dyspnea, hematuria, and proteinuria. are characteristic findings Antineutrophil circulating antibodies (ANCA) • Kidney biopsy: necrotizing granulomatous lesions •
Renal Vein Thrombosis Predisposing factors: perinatal asphyxia dehydration septicemia shock coagulopathies: e. g. , protein C, S deficiency Gross hematuria +/- palpable unilateral or bilateral • Kidneys • Renal U/S with Doppler •
Trauma Blunt or penetrating injury to kidney or any portion of urinary tract can cause gross or microscopic hematuria Renal U/S is mandatory • URETHERAL INJURY • (Urethrography or cystoscopy) •
Exercise Vigorous exercise can produce gross or • Microscopic hematuria • . ( usually resolves within 1– 2 days)
Polycystic Kidney Disease ARPKD ADPKD Common findings in neonates: gross or microscopic hematuria bilateral flank masses, hypertension +/- renal impairment Renal U/S Cysts are microscopic • Congenital hepatic fibrosis (CHF)
Glomerulonephritis of Chronic Infection Endocarditis. Shunt infections Clinically: Acute GN • Chronic renal insufficiency. • . Serum C 3 is often decreased
Others Renal Tuberculosis • Vascular Malformations • Foreign Body in Urethra or Bladder Wilms tumor Gross hematuria occurs in small number of cases. Renal U/S or CT shows renal mass Renal hemangioma is rare ( recurrent hematuria) Renal carcinoma is rare in pediatric population, Bladder tumors are exceedingly rare in children
Others Bleeding Disorders • (hemophilias, thrombocytopenia, DIC) • Uncommon to be isolated hematuria •
Summary Isolated hematuria is not a common presentation in children. If so, it needs thorough investigation and all effort to be applied in order to prevent renal damage. • Proteinuria has to be looked at carefully in any child with hematuria. • Non glomerular causes are common in children and usually are due to congenital anomalies or crystalluria. • Early referral to nephrology/urology service is advisable and family members need to be investigated in all children with hematuria. Proper investigations and treatment at early stages is of paramount importance in order to prevent chronic kidney disease. • •
THANK YOU

THANK YOU
dbac26f82301f610019bcddf64140b61.ppt