bf9b970442da1cf44039583a68f7bcec.ppt
- Количество слайдов: 38
 Heel Pressure Ulcers Prevalence, Cost, Etiology and Risk Factors
Heel Pressure Ulcers Prevalence, Cost, Etiology and Risk Factors
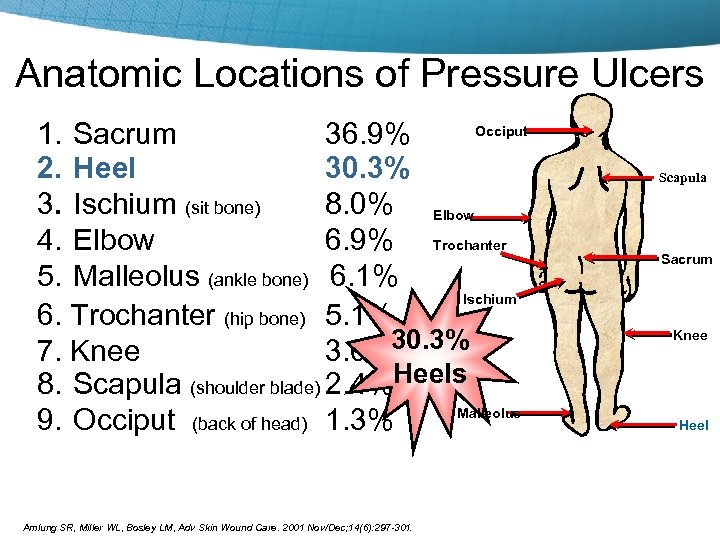 Anatomic Locations of Pressure Ulcers Occiput 1. Sacrum 36. 9% 2. Heel 30. 3% 3. Ischium (sit bone) 8. 0% Elbow 4. Elbow 6. 9% Trochanter 5. Malleolus (ankle bone) 6. 1% Ischium 6. Trochanter (hip bone) 5. 1% 7. Knee 3. 0%30. 3% 8. Scapula (shoulder blade) 2. 4%Heels Malleolus 9. Occiput (back of head) 1. 3% Amlung SR, Miller WL, Bosley LM, Adv Skin Wound Care. 2001 Nov/Dec; 14(6): 297 -301. Scapula Sacrum Knee Heel
Anatomic Locations of Pressure Ulcers Occiput 1. Sacrum 36. 9% 2. Heel 30. 3% 3. Ischium (sit bone) 8. 0% Elbow 4. Elbow 6. 9% Trochanter 5. Malleolus (ankle bone) 6. 1% Ischium 6. Trochanter (hip bone) 5. 1% 7. Knee 3. 0%30. 3% 8. Scapula (shoulder blade) 2. 4%Heels Malleolus 9. Occiput (back of head) 1. 3% Amlung SR, Miller WL, Bosley LM, Adv Skin Wound Care. 2001 Nov/Dec; 14(6): 297 -301. Scapula Sacrum Knee Heel
 Prevention – Who is at risk? • • ICU population Orthopedics Neurosurgery LTC Units Co-morbidities: PVD, Diabetes, Immobility The “Vent” patient (7 M days*) Operating Room – 2 hour+ procedures *Source: Principal Procedure outcomes for respiratory intubation and ventilation: Healthcare Cost and Utilization Project (HCUP), 2004, http: //hcupnet. ahrq. gov/HCUPnet. jsp
Prevention – Who is at risk? • • ICU population Orthopedics Neurosurgery LTC Units Co-morbidities: PVD, Diabetes, Immobility The “Vent” patient (7 M days*) Operating Room – 2 hour+ procedures *Source: Principal Procedure outcomes for respiratory intubation and ventilation: Healthcare Cost and Utilization Project (HCUP), 2004, http: //hcupnet. ahrq. gov/HCUPnet. jsp
 Diabetes • Affects 16 million Americans • Millions at risk for skin breakdown • 15% of diabetics develop foot ulcers • Foot lesions = #1 reason for hospitalization • Lower extremity amputations 15 times more likely to occur in diabetics vs. non-diabetic Mulder G, Armstron D, Seaman S, Wounds 15 (4): 92 -106, 2003
Diabetes • Affects 16 million Americans • Millions at risk for skin breakdown • 15% of diabetics develop foot ulcers • Foot lesions = #1 reason for hospitalization • Lower extremity amputations 15 times more likely to occur in diabetics vs. non-diabetic Mulder G, Armstron D, Seaman S, Wounds 15 (4): 92 -106, 2003
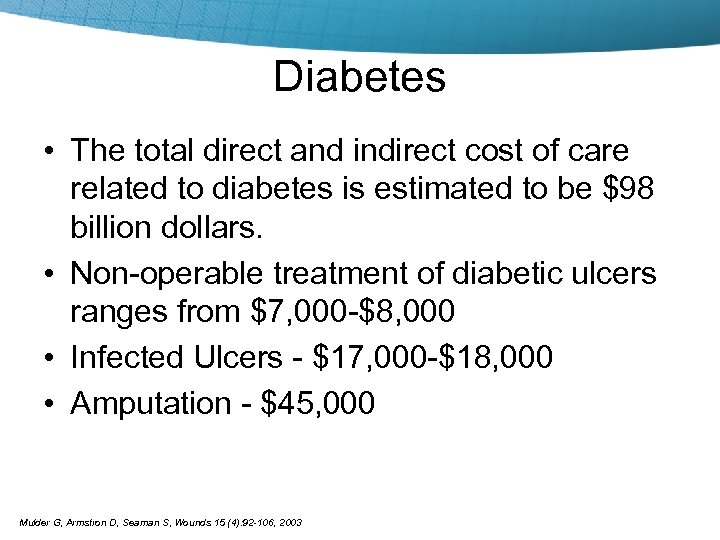 Diabetes • The total direct and indirect cost of care related to diabetes is estimated to be $98 billion dollars. • Non-operable treatment of diabetic ulcers ranges from $7, 000 -$8, 000 • Infected Ulcers - $17, 000 -$18, 000 • Amputation - $45, 000 Mulder G, Armstron D, Seaman S, Wounds 15 (4): 92 -106, 2003
Diabetes • The total direct and indirect cost of care related to diabetes is estimated to be $98 billion dollars. • Non-operable treatment of diabetic ulcers ranges from $7, 000 -$8, 000 • Infected Ulcers - $17, 000 -$18, 000 • Amputation - $45, 000 Mulder G, Armstron D, Seaman S, Wounds 15 (4): 92 -106, 2003
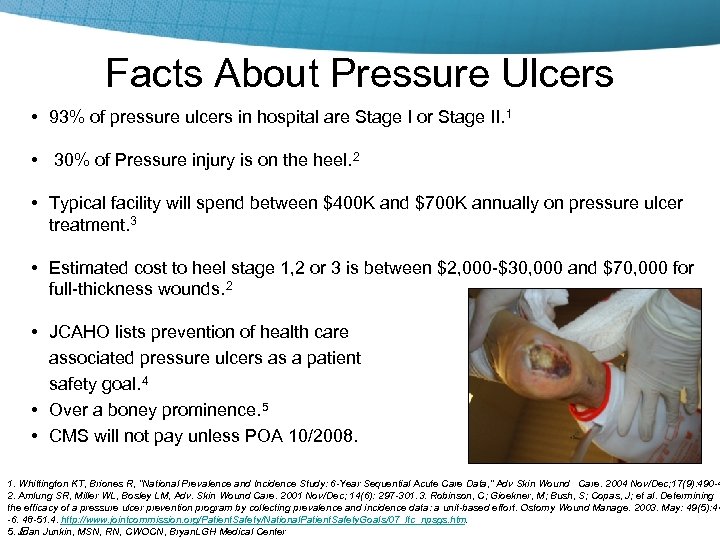 Facts About Pressure Ulcers • 93% of pressure ulcers in hospital are Stage I or Stage II. 1 • 30% of Pressure injury is on the heel. 2 • Typical facility will spend between $400 K and $700 K annually on pressure ulcer treatment. 3 • Estimated cost to heel stage 1, 2 or 3 is between $2, 000 -$30, 000 and $70, 000 for full-thickness wounds. 2 • JCAHO lists prevention of health care associated pressure ulcers as a patient safety goal. 4 • Over a boney prominence. 5 • CMS will not pay unless POA 10/2008. 1. Whittington KT, Briones R, “National Prevalence and Incidence Study: 6 -Year Sequential Acute Care Data, ” Adv Skin Wound Care. 2004 Nov/Dec; 17(9): 490 -4 2. Amlung SR, Miller WL, Bosley LM, Adv. Skin Wound Care. 2001 Nov/Dec; 14(6): 297 -301. 3. Robinson, C; Gioekner, M; Bush, S; Copas, J; et al. Determining the efficacy of a pressure ulcer prevention program by collecting prevalence and incidence data: a unit-based effort. Ostomy Wound Manage. 2003. May: 49(5): 44 -6. 48 -51. 4. http: //www. jointcommission. org/Patient. Safety/National. Patient. Safety. Goals/07_ltc_npsgs. htm. 5. Junkin, MSN, RN, CWOCN, Bryan. LGH Medical Center Joan
Facts About Pressure Ulcers • 93% of pressure ulcers in hospital are Stage I or Stage II. 1 • 30% of Pressure injury is on the heel. 2 • Typical facility will spend between $400 K and $700 K annually on pressure ulcer treatment. 3 • Estimated cost to heel stage 1, 2 or 3 is between $2, 000 -$30, 000 and $70, 000 for full-thickness wounds. 2 • JCAHO lists prevention of health care associated pressure ulcers as a patient safety goal. 4 • Over a boney prominence. 5 • CMS will not pay unless POA 10/2008. 1. Whittington KT, Briones R, “National Prevalence and Incidence Study: 6 -Year Sequential Acute Care Data, ” Adv Skin Wound Care. 2004 Nov/Dec; 17(9): 490 -4 2. Amlung SR, Miller WL, Bosley LM, Adv. Skin Wound Care. 2001 Nov/Dec; 14(6): 297 -301. 3. Robinson, C; Gioekner, M; Bush, S; Copas, J; et al. Determining the efficacy of a pressure ulcer prevention program by collecting prevalence and incidence data: a unit-based effort. Ostomy Wound Manage. 2003. May: 49(5): 44 -6. 48 -51. 4. http: //www. jointcommission. org/Patient. Safety/National. Patient. Safety. Goals/07_ltc_npsgs. htm. 5. Junkin, MSN, RN, CWOCN, Bryan. LGH Medical Center Joan
 The CMS 10 Commandments: If It’s Not POA, We Won’t Pay 1. Pressure Ulcers 2. Catheter-associated urinary tract infections (UTI) 3. Objects left in surgery 4. Air embolism 5. Blood incompatibility 6. Vascular-catheter associated blood stream infection 7. Surgical site infections: Mediastinitis (after CABG), certain orthopedic procedures and bariatric surgeries 8. Falls 9. Deep Vein Thrombosis (DVT) 10. Poor glycemic control Federal Register, Vol 73, No. 161 pgs: 48473 -48474 , August 19, 2008
The CMS 10 Commandments: If It’s Not POA, We Won’t Pay 1. Pressure Ulcers 2. Catheter-associated urinary tract infections (UTI) 3. Objects left in surgery 4. Air embolism 5. Blood incompatibility 6. Vascular-catheter associated blood stream infection 7. Surgical site infections: Mediastinitis (after CABG), certain orthopedic procedures and bariatric surgeries 8. Falls 9. Deep Vein Thrombosis (DVT) 10. Poor glycemic control Federal Register, Vol 73, No. 161 pgs: 48473 -48474 , August 19, 2008
 Who is Focused on Skin Breakdown? CMS State Operations Manual, F 314 “Because the heels and elbows have relatively little surface area, it is difficult to redistribute pressure on these two surfaces. Therefore, it is important to pay particular attention to reducing the pressure on these areas for the resident at risk in accord with resident’s overall goals and condition. ” “Based on the comprehensive assessment of a resident, the facility must ensure that-(1) A resident who enters the facility without pressure sores does not develop pressure sores unless the individual’s clinical condition demonstrates that they were unavoidable; and (2) A resident having pressure sores receives necessary treatment and services to promote healing, prevent infection and prevent new sores from developing. ” Centers for Medicare & Medicaid Svcs, CMS Manual System, Pub. 100 -07 State Operations, Provider Certification, Appendix PP Guidance to Surveyors for LTC Facilities, F 314 483. 25(c) Pressure Sores, (Rev. 4, Issued/Effective 11 -12 -2004). Dept of Health & Human Svcs, Transmittal 12, 14 Oct 2005: 144 (available at new. cms. hhs. gov/transmittals/downloads/R 12 SOM. pdf).
Who is Focused on Skin Breakdown? CMS State Operations Manual, F 314 “Because the heels and elbows have relatively little surface area, it is difficult to redistribute pressure on these two surfaces. Therefore, it is important to pay particular attention to reducing the pressure on these areas for the resident at risk in accord with resident’s overall goals and condition. ” “Based on the comprehensive assessment of a resident, the facility must ensure that-(1) A resident who enters the facility without pressure sores does not develop pressure sores unless the individual’s clinical condition demonstrates that they were unavoidable; and (2) A resident having pressure sores receives necessary treatment and services to promote healing, prevent infection and prevent new sores from developing. ” Centers for Medicare & Medicaid Svcs, CMS Manual System, Pub. 100 -07 State Operations, Provider Certification, Appendix PP Guidance to Surveyors for LTC Facilities, F 314 483. 25(c) Pressure Sores, (Rev. 4, Issued/Effective 11 -12 -2004). Dept of Health & Human Svcs, Transmittal 12, 14 Oct 2005: 144 (available at new. cms. hhs. gov/transmittals/downloads/R 12 SOM. pdf).
 Heel Ulcer Prevention: Current Practice • Pillows…nursing standard • Booties…many • Orthotics…doctor and clinician request and expensive • Prevention…protocols: too general or inaccurate. Ownership. • Treatment…ulcers and foot drop • Nothing…
Heel Ulcer Prevention: Current Practice • Pillows…nursing standard • Booties…many • Orthotics…doctor and clinician request and expensive • Prevention…protocols: too general or inaccurate. Ownership. • Treatment…ulcers and foot drop • Nothing…
 Heel Protector or Orthotic? • • • DM Systems Gaymar KCI Spanamerica EHOB • • Hollister Posey L’Nard Anatomical Concepts • De. Royal • Multi Podus
Heel Protector or Orthotic? • • • DM Systems Gaymar KCI Spanamerica EHOB • • Hollister Posey L’Nard Anatomical Concepts • De. Royal • Multi Podus
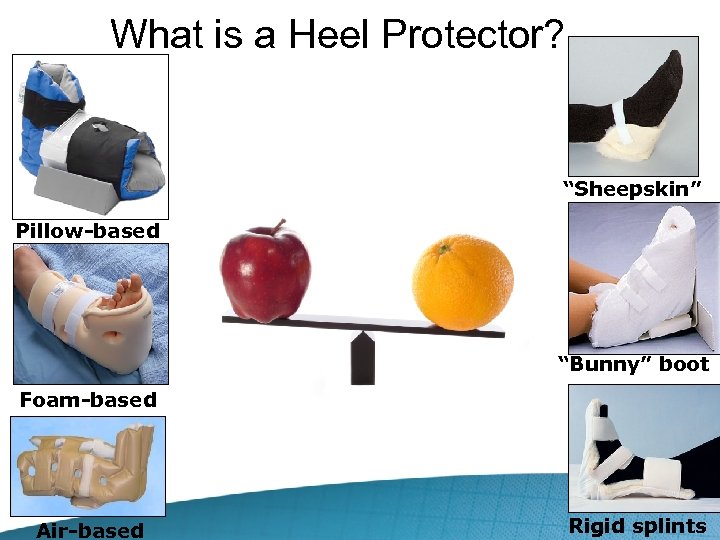 What is a Heel Protector? “Sheepskin” Pillow-based “Bunny” boot Foam-based Air-based Rigid splints
What is a Heel Protector? “Sheepskin” Pillow-based “Bunny” boot Foam-based Air-based Rigid splints
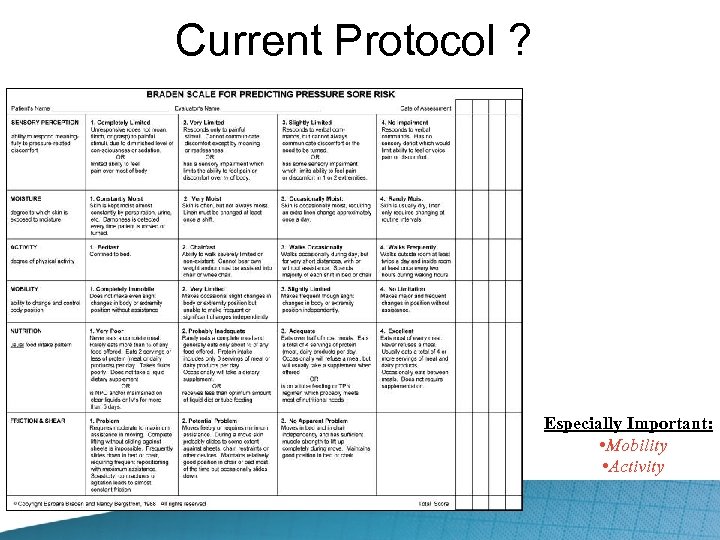 Current Protocol ? Especially Important: • Mobility • Activity
Current Protocol ? Especially Important: • Mobility • Activity
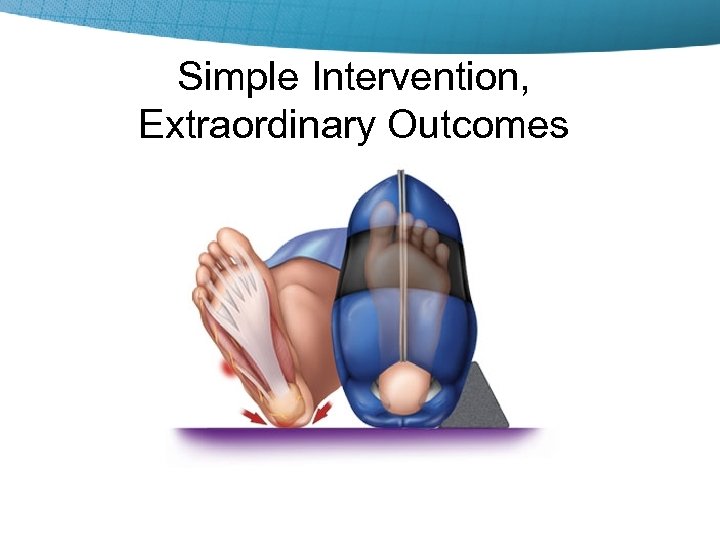 Simple Intervention, Extraordinary Outcomes
Simple Intervention, Extraordinary Outcomes
 Jill Walsh, JWOCN March 2007 • Objective: To identify risk factors (Braden score and co-morbidities) • Study Method: Two year Retrospective chart review of patients admitted with or developed heel ulcers. Pts. on HU Prevention protocol for 10 days. Braden + co-morbidity. Compared Prevalon to Waffle-boot • Results: 53 patients. 0 Heel Ulcers. 8 hip fractures. Prevalon preferred: comfort, warmth, heel protection, DVT compression compatibility. • Conclusion: Heel Ulcer prevention protocol (Braden’s 16 -18 and co-morbidities) and the use of a pressure-relieving device is effective in reducing the rate of heel pressure ulcers. Prevalon outperformed the ‘control’ product (p>. 05; stat. sign. )
Jill Walsh, JWOCN March 2007 • Objective: To identify risk factors (Braden score and co-morbidities) • Study Method: Two year Retrospective chart review of patients admitted with or developed heel ulcers. Pts. on HU Prevention protocol for 10 days. Braden + co-morbidity. Compared Prevalon to Waffle-boot • Results: 53 patients. 0 Heel Ulcers. 8 hip fractures. Prevalon preferred: comfort, warmth, heel protection, DVT compression compatibility. • Conclusion: Heel Ulcer prevention protocol (Braden’s 16 -18 and co-morbidities) and the use of a pressure-relieving device is effective in reducing the rate of heel pressure ulcers. Prevalon outperformed the ‘control’ product (p>. 05; stat. sign. )
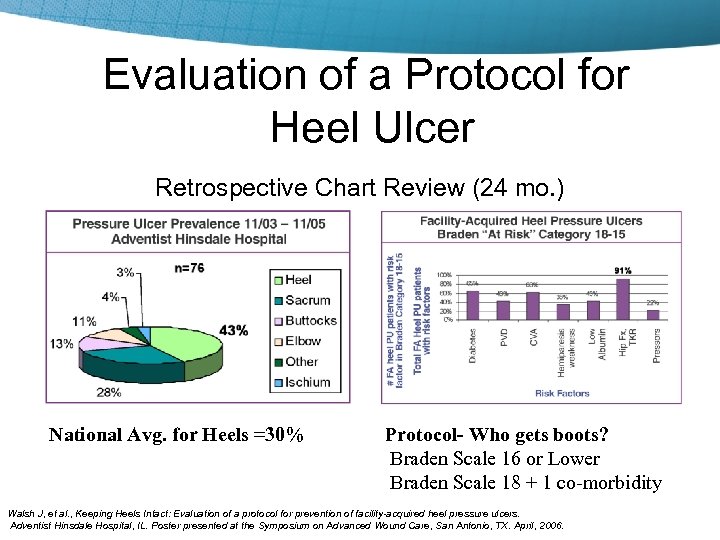 Evaluation of a Protocol for Heel Ulcer Retrospective Chart Review (24 mo. ) National Avg. for Heels =30% Protocol- Who gets boots? Braden Scale 16 or Lower Braden Scale 18 + 1 co-morbidity Walsh J, et al. , Keeping Heels Intact: Evaluation of a protocol for prevention of facility-acquired heel pressure ulcers. Adventist Hinsdale Hospital, IL. Poster presented at the Symposium on Advanced Wound Care, San Antonio, TX. April, 2006.
Evaluation of a Protocol for Heel Ulcer Retrospective Chart Review (24 mo. ) National Avg. for Heels =30% Protocol- Who gets boots? Braden Scale 16 or Lower Braden Scale 18 + 1 co-morbidity Walsh J, et al. , Keeping Heels Intact: Evaluation of a protocol for prevention of facility-acquired heel pressure ulcers. Adventist Hinsdale Hospital, IL. Poster presented at the Symposium on Advanced Wound Care, San Antonio, TX. April, 2006.
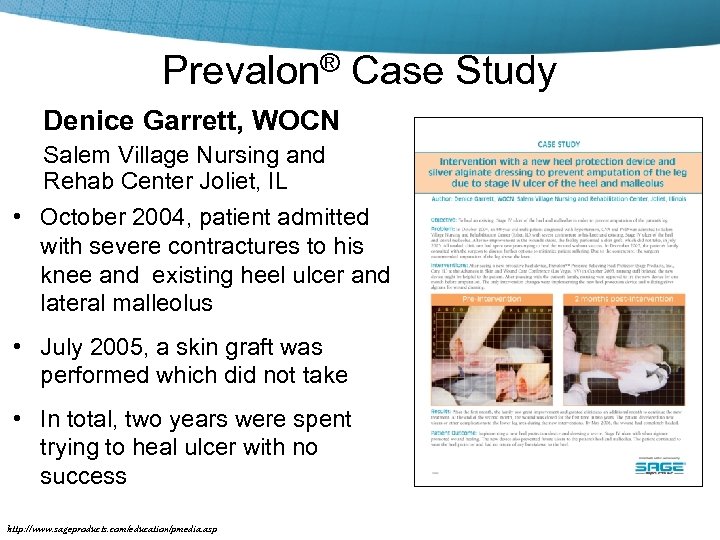 Prevalon® Case Study Denice Garrett, WOCN Salem Village Nursing and Rehab Center Joliet, IL • October 2004, patient admitted with severe contractures to his knee and existing heel ulcer and lateral malleolus • July 2005, a skin graft was performed which did not take • In total, two years were spent trying to heal ulcer with no success http: //www. sageproducts. com/education/pmedia. asp
Prevalon® Case Study Denice Garrett, WOCN Salem Village Nursing and Rehab Center Joliet, IL • October 2004, patient admitted with severe contractures to his knee and existing heel ulcer and lateral malleolus • July 2005, a skin graft was performed which did not take • In total, two years were spent trying to heal ulcer with no success http: //www. sageproducts. com/education/pmedia. asp
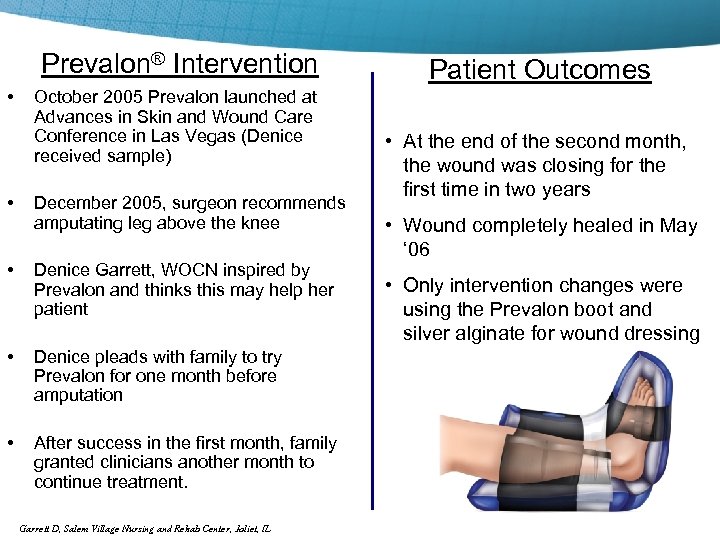 Prevalon® Intervention • • October 2005 Prevalon launched at Advances in Skin and Wound Care Conference in Las Vegas (Denice received sample) December 2005, surgeon recommends amputating leg above the knee • Denice Garrett, WOCN inspired by Prevalon and thinks this may help her patient • Denice pleads with family to try Prevalon for one month before amputation • After success in the first month, family granted clinicians another month to continue treatment. Garrett D, Salem Village Nursing and Rehab Center, Joliet, IL Patient Outcomes • At the end of the second month, the wound was closing for the first time in two years • Wound completely healed in May ‘ 06 • Only intervention changes were using the Prevalon boot and silver alginate for wound dressing
Prevalon® Intervention • • October 2005 Prevalon launched at Advances in Skin and Wound Care Conference in Las Vegas (Denice received sample) December 2005, surgeon recommends amputating leg above the knee • Denice Garrett, WOCN inspired by Prevalon and thinks this may help her patient • Denice pleads with family to try Prevalon for one month before amputation • After success in the first month, family granted clinicians another month to continue treatment. Garrett D, Salem Village Nursing and Rehab Center, Joliet, IL Patient Outcomes • At the end of the second month, the wound was closing for the first time in two years • Wound completely healed in May ‘ 06 • Only intervention changes were using the Prevalon boot and silver alginate for wound dressing
 Vicki Burda Poster Presentation at SAWC in APRIL 2007 Three Key Take-Aways: 1) Prevalon significantly reduces the risk of developing heel pressure ulcers in a high-risk population – 95% reduction of heel ulcer incidence! (From 39 to 2) 2) Positive outcomes attributed to protocol and Prevalon 3) Process improvement for heel ulcer prevention can be effective
Vicki Burda Poster Presentation at SAWC in APRIL 2007 Three Key Take-Aways: 1) Prevalon significantly reduces the risk of developing heel pressure ulcers in a high-risk population – 95% reduction of heel ulcer incidence! (From 39 to 2) 2) Positive outcomes attributed to protocol and Prevalon 3) Process improvement for heel ulcer prevention can be effective
 Poster Presentation at 2007 WOCN by Dr Harriett Loehne Three Key Take-Aways: 1) Prevalon® effective for treatment and prevention of heel ulcers 2) 0 Heel pressure ulcers during 10 -week trial on 8 “high-risk patients” 3) Staff and patients prefer: Standardized all units to Prevalon
Poster Presentation at 2007 WOCN by Dr Harriett Loehne Three Key Take-Aways: 1) Prevalon® effective for treatment and prevention of heel ulcers 2) 0 Heel pressure ulcers during 10 -week trial on 8 “high-risk patients” 3) Staff and patients prefer: Standardized all units to Prevalon
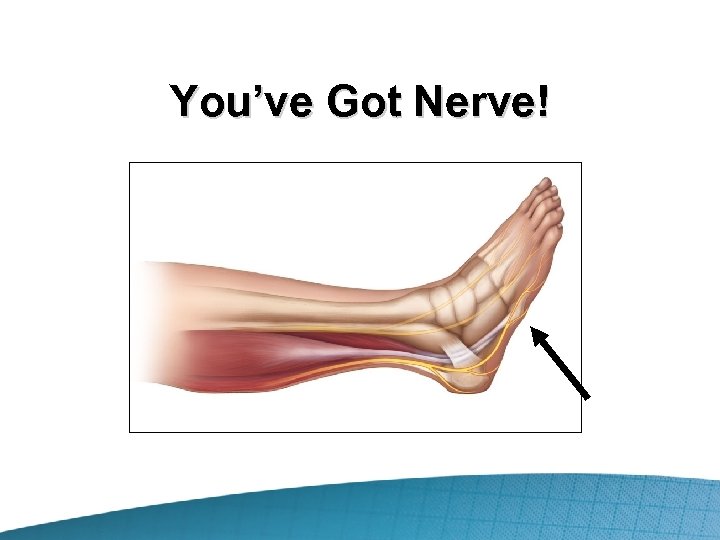 You’ve Got Nerve!
You’ve Got Nerve!
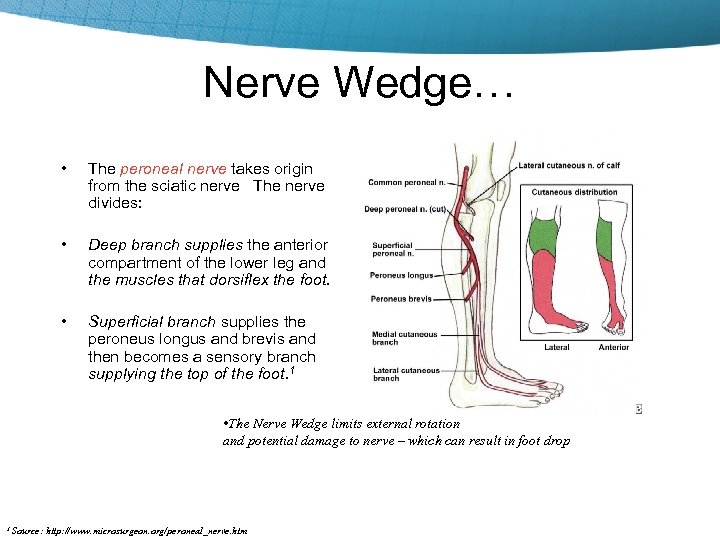 Nerve Wedge… • The peroneal nerve takes origin from the sciatic nerve The nerve divides: • Deep branch supplies the anterior compartment of the lower leg and the muscles that dorsiflex the foot. • Superficial branch supplies the peroneus longus and brevis and then becomes a sensory branch supplying the top of the foot. 1 • The Nerve Wedge limits external rotation and potential damage to nerve – which can result in foot drop 1 Source: http: //www. microsurgeon. org/peroneal_nerve. htm
Nerve Wedge… • The peroneal nerve takes origin from the sciatic nerve The nerve divides: • Deep branch supplies the anterior compartment of the lower leg and the muscles that dorsiflex the foot. • Superficial branch supplies the peroneus longus and brevis and then becomes a sensory branch supplying the top of the foot. 1 • The Nerve Wedge limits external rotation and potential damage to nerve – which can result in foot drop 1 Source: http: //www. microsurgeon. org/peroneal_nerve. htm
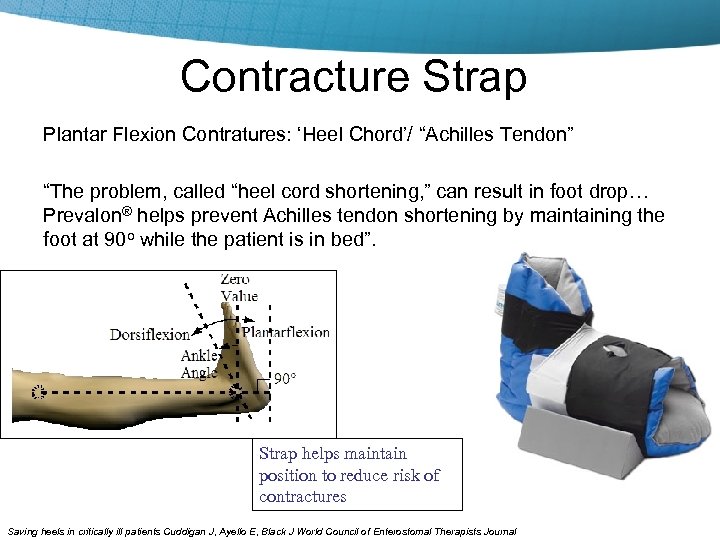 Contracture Strap Plantar Flexion Contratures: ‘Heel Chord’/ “Achilles Tendon” “The problem, called “heel cord shortening, ” can result in foot drop… Prevalon® helps prevent Achilles tendon shortening by maintaining the foot at 90 o while the patient is in bed”. Strap helps maintain position to reduce risk of contractures Saving heels in critically ill patients Cuddigan J, Ayello E, Black J World Council of Enterostomal Therapists Journal
Contracture Strap Plantar Flexion Contratures: ‘Heel Chord’/ “Achilles Tendon” “The problem, called “heel cord shortening, ” can result in foot drop… Prevalon® helps prevent Achilles tendon shortening by maintaining the foot at 90 o while the patient is in bed”. Strap helps maintain position to reduce risk of contractures Saving heels in critically ill patients Cuddigan J, Ayello E, Black J World Council of Enterostomal Therapists Journal
 Prevalon® with Wedge I. Prevents Pressure Ulcers of the Heel! • • • II. Stays in Place! Floats the Heel! Stretch Panel – No Trauma! Reduces Risk of Plantar Flexion Contractures! • • • Foot Remains Upright! Contracture Strap Adjusts Tension Boot is Stabilized; Nerve Wedge
Prevalon® with Wedge I. Prevents Pressure Ulcers of the Heel! • • • II. Stays in Place! Floats the Heel! Stretch Panel – No Trauma! Reduces Risk of Plantar Flexion Contractures! • • • Foot Remains Upright! Contracture Strap Adjusts Tension Boot is Stabilized; Nerve Wedge
 Tina Meyers BSN, RN, CWOCN, ACHRN Harris County Hospital District, Houston, Texas • Title: Successful Prevention or Heel Ulcers and Plantar Flexion Contractures in High Risk Ventilator Population • Objective: Targeted reduction of heel injury and plantar flexion contractures in the sedated, ICU patient • Intervention: Use of heel protector with contracture strap on 53 high risk patients • Results: 0 PF contractures; 0 Heel Ulcers; 5 patients with abnormal ankle ROM improved; Revenue Preservation of $1. 9 MM • Conclusion: New Heel Protector with Contracture Strap effectively reduced the risk of heel ulcers and PF contractures in 53 patients Presenting at NPUAP Educational Conference; March 2009 Washington DC Presented at World Union of Wound Healing Society Meeting in Toronto, May 2008
Tina Meyers BSN, RN, CWOCN, ACHRN Harris County Hospital District, Houston, Texas • Title: Successful Prevention or Heel Ulcers and Plantar Flexion Contractures in High Risk Ventilator Population • Objective: Targeted reduction of heel injury and plantar flexion contractures in the sedated, ICU patient • Intervention: Use of heel protector with contracture strap on 53 high risk patients • Results: 0 PF contractures; 0 Heel Ulcers; 5 patients with abnormal ankle ROM improved; Revenue Preservation of $1. 9 MM • Conclusion: New Heel Protector with Contracture Strap effectively reduced the risk of heel ulcers and PF contractures in 53 patients Presenting at NPUAP Educational Conference; March 2009 Washington DC Presented at World Union of Wound Healing Society Meeting in Toronto, May 2008
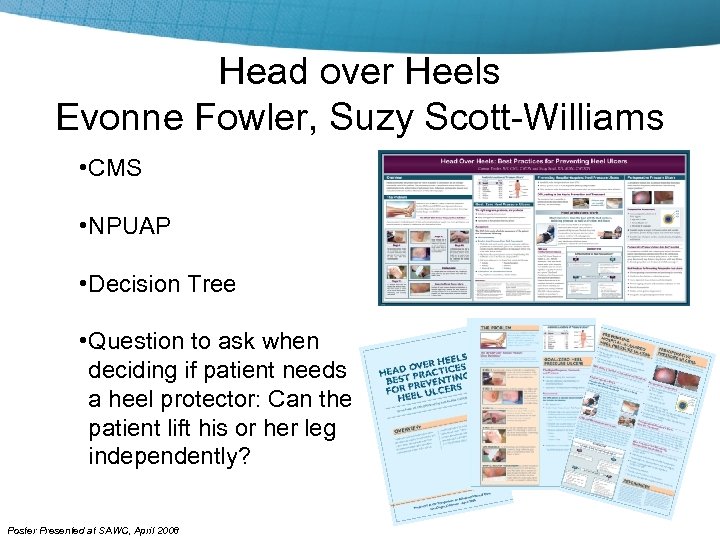 Head over Heels Evonne Fowler, Suzy Scott-Williams • CMS • NPUAP • Decision Tree • Question to ask when deciding if patient needs a heel protector: Can the patient lift his or her leg independently? Poster Presented at SAWC, April 2008
Head over Heels Evonne Fowler, Suzy Scott-Williams • CMS • NPUAP • Decision Tree • Question to ask when deciding if patient needs a heel protector: Can the patient lift his or her leg independently? Poster Presented at SAWC, April 2008
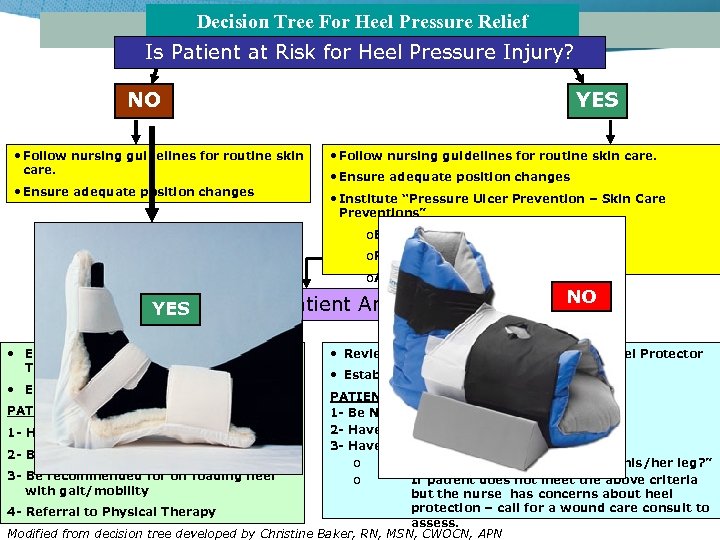 Decision Tree For Heel Pressure Relief Is Patient at Risk for Heel Pressure Injury? NO YES • Follow nursing guidelines for routine skin care. • Ensure adequate position changes • Institute “Pressure Ulcer Prevention – Skin Care Preventions” o Elevate heels off bed o Reposition every 2 hours o Assess skin integrity every shift YES Is Patient Ambulatory? • Educate Patient on Pressure Reducing Techniques • Establish patient appropriateness NO NO • Review Criteria for Pressure-Relieving Heel Protector • Establish patient appropriateness PATIENT MUST: 1 - Be NON-AMBULATORY 2 - Have a total Braden Score of 15 or less 1 - Have the potential to be AMBULATORY 3 - Have TWO or more co-morbidities 2 - Be AMBULATORY o Determine “Can the patient lift his/her leg? ” 3 - Be recommended for off loading heel o If patient does not meet the above criteria with gait/mobility but the nurse has concerns about heel protection – call for a wound care consult to 4 - Referral to Physical Therapy assess. Modified from decision tree developed by Christine Baker, RN, MSN, CWOCN, APN PATIENT MUST:
Decision Tree For Heel Pressure Relief Is Patient at Risk for Heel Pressure Injury? NO YES • Follow nursing guidelines for routine skin care. • Ensure adequate position changes • Institute “Pressure Ulcer Prevention – Skin Care Preventions” o Elevate heels off bed o Reposition every 2 hours o Assess skin integrity every shift YES Is Patient Ambulatory? • Educate Patient on Pressure Reducing Techniques • Establish patient appropriateness NO NO • Review Criteria for Pressure-Relieving Heel Protector • Establish patient appropriateness PATIENT MUST: 1 - Be NON-AMBULATORY 2 - Have a total Braden Score of 15 or less 1 - Have the potential to be AMBULATORY 3 - Have TWO or more co-morbidities 2 - Be AMBULATORY o Determine “Can the patient lift his/her leg? ” 3 - Be recommended for off loading heel o If patient does not meet the above criteria with gait/mobility but the nurse has concerns about heel protection – call for a wound care consult to 4 - Referral to Physical Therapy assess. Modified from decision tree developed by Christine Baker, RN, MSN, CWOCN, APN PATIENT MUST:
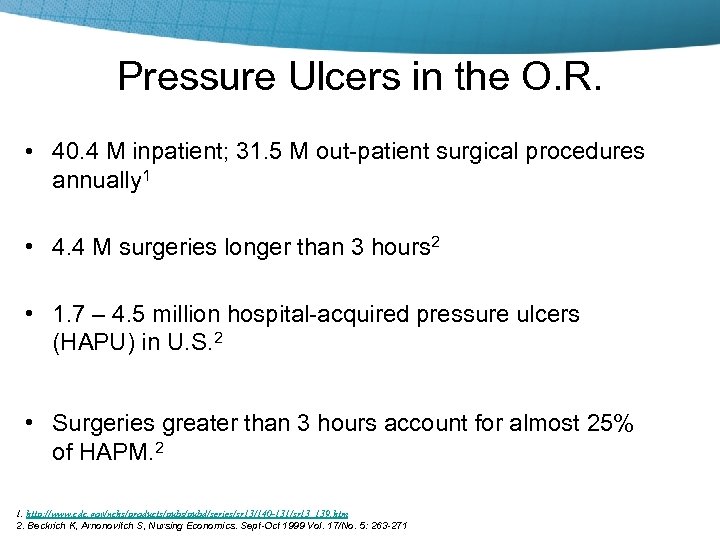 Pressure Ulcers in the O. R. • 40. 4 M inpatient; 31. 5 M out-patient surgical procedures annually 1 • 4. 4 M surgeries longer than 3 hours 2 • 1. 7 – 4. 5 million hospital-acquired pressure ulcers (HAPU) in U. S. 2 • Surgeries greater than 3 hours account for almost 25% of HAPM. 2 1. http: //www. cdc. gov/nchs/products/pubd/series/sr 13/140 -131/sr 13_139. htm 2. Beckrich K, Arnonovitch S, Nursing Economics. Sept-Oct 1999 Vol. 17/No. 5: 263 -271
Pressure Ulcers in the O. R. • 40. 4 M inpatient; 31. 5 M out-patient surgical procedures annually 1 • 4. 4 M surgeries longer than 3 hours 2 • 1. 7 – 4. 5 million hospital-acquired pressure ulcers (HAPU) in U. S. 2 • Surgeries greater than 3 hours account for almost 25% of HAPM. 2 1. http: //www. cdc. gov/nchs/products/pubd/series/sr 13/140 -131/sr 13_139. htm 2. Beckrich K, Arnonovitch S, Nursing Economics. Sept-Oct 1999 Vol. 17/No. 5: 263 -271
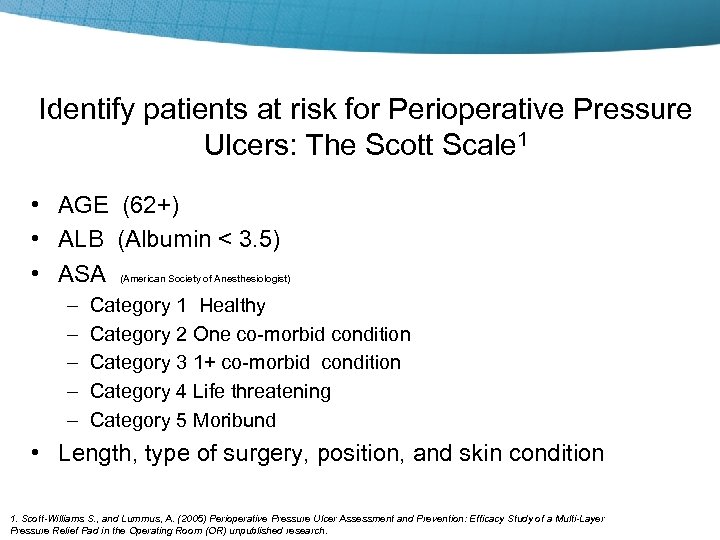 Identify patients at risk for Perioperative Pressure Ulcers: The Scott Scale 1 • AGE (62+) • ALB (Albumin < 3. 5) • ASA (American Society of Anesthesiologist) – – – Category 1 Healthy Category 2 One co-morbid condition Category 3 1+ co-morbid condition Category 4 Life threatening Category 5 Moribund • Length, type of surgery, position, and skin condition 1. Scott-Williams S. , and Lummus, A. (2005) Perioperative Pressure Ulcer Assessment and Prevention: Efficacy Study of a Multi-Layer Pressure Relief Pad in the Operating Room (OR) unpublished research.
Identify patients at risk for Perioperative Pressure Ulcers: The Scott Scale 1 • AGE (62+) • ALB (Albumin < 3. 5) • ASA (American Society of Anesthesiologist) – – – Category 1 Healthy Category 2 One co-morbid condition Category 3 1+ co-morbid condition Category 4 Life threatening Category 5 Moribund • Length, type of surgery, position, and skin condition 1. Scott-Williams S. , and Lummus, A. (2005) Perioperative Pressure Ulcer Assessment and Prevention: Efficacy Study of a Multi-Layer Pressure Relief Pad in the Operating Room (OR) unpublished research.
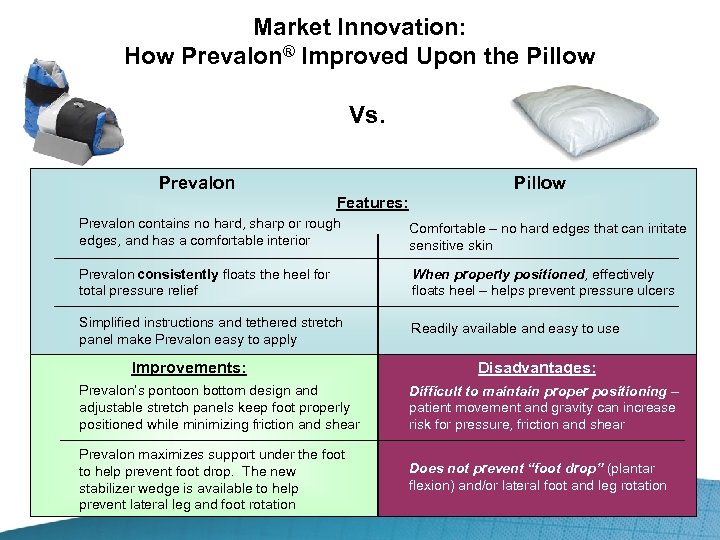 Market Innovation: How Prevalon® Improved Upon the Pillow Vs. Prevalon Pillow Features: Prevalon contains no hard, sharp or rough edges, and has a comfortable interior Comfortable – no hard edges that can irritate sensitive skin Prevalon consistently floats the heel for total pressure relief When properly positioned, effectively floats heel – helps prevent pressure ulcers Simplified instructions and tethered stretch panel make Prevalon easy to apply Readily available and easy to use Improvements: Disadvantages: Prevalon’s pontoon bottom design and adjustable stretch panels keep foot properly positioned while minimizing friction and shear Difficult to maintain proper positioning – patient movement and gravity can increase risk for pressure, friction and shear Prevalon maximizes support under the foot to help prevent foot drop. The new stabilizer wedge is available to help prevent lateral leg and foot rotation Does not prevent “foot drop” (plantar flexion) and/or lateral foot and leg rotation
Market Innovation: How Prevalon® Improved Upon the Pillow Vs. Prevalon Pillow Features: Prevalon contains no hard, sharp or rough edges, and has a comfortable interior Comfortable – no hard edges that can irritate sensitive skin Prevalon consistently floats the heel for total pressure relief When properly positioned, effectively floats heel – helps prevent pressure ulcers Simplified instructions and tethered stretch panel make Prevalon easy to apply Readily available and easy to use Improvements: Disadvantages: Prevalon’s pontoon bottom design and adjustable stretch panels keep foot properly positioned while minimizing friction and shear Difficult to maintain proper positioning – patient movement and gravity can increase risk for pressure, friction and shear Prevalon maximizes support under the foot to help prevent foot drop. The new stabilizer wedge is available to help prevent lateral leg and foot rotation Does not prevent “foot drop” (plantar flexion) and/or lateral foot and leg rotation
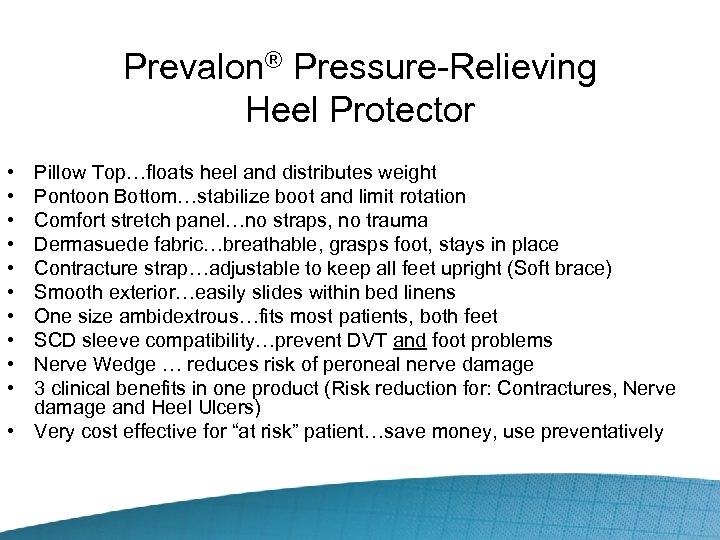 Prevalon® Pressure-Relieving Heel Protector • • • Pillow Top…floats heel and distributes weight Pontoon Bottom…stabilize boot and limit rotation Comfort stretch panel…no straps, no trauma Dermasuede fabric…breathable, grasps foot, stays in place Contracture strap…adjustable to keep all feet upright (Soft brace) Smooth exterior…easily slides within bed linens One size ambidextrous…fits most patients, both feet SCD sleeve compatibility…prevent DVT and foot problems Nerve Wedge … reduces risk of peroneal nerve damage 3 clinical benefits in one product (Risk reduction for: Contractures, Nerve damage and Heel Ulcers) • Very cost effective for “at risk” patient…save money, use preventatively
Prevalon® Pressure-Relieving Heel Protector • • • Pillow Top…floats heel and distributes weight Pontoon Bottom…stabilize boot and limit rotation Comfort stretch panel…no straps, no trauma Dermasuede fabric…breathable, grasps foot, stays in place Contracture strap…adjustable to keep all feet upright (Soft brace) Smooth exterior…easily slides within bed linens One size ambidextrous…fits most patients, both feet SCD sleeve compatibility…prevent DVT and foot problems Nerve Wedge … reduces risk of peroneal nerve damage 3 clinical benefits in one product (Risk reduction for: Contractures, Nerve damage and Heel Ulcers) • Very cost effective for “at risk” patient…save money, use preventatively
 Key Reference Accounts Cleveland Clinic Emory University Hospital MA General Hospital Conroe Med Center St. Luke’s Hospital Arrowhead Reg Med Ctr Creighton Medical Center Northwest Community Hospital Piedmont Hospital VA Medical Center Meritcare Med Center University of Chicago Cleveland, OH Atlanta, GA Boston, MA Conroe, TX Chesterfield, MO Colton, CA Omaha, NE Arlington Hts, IL Santa Rosa, CA Miami, FL Fargo, ND Chicago, IL
Key Reference Accounts Cleveland Clinic Emory University Hospital MA General Hospital Conroe Med Center St. Luke’s Hospital Arrowhead Reg Med Ctr Creighton Medical Center Northwest Community Hospital Piedmont Hospital VA Medical Center Meritcare Med Center University of Chicago Cleveland, OH Atlanta, GA Boston, MA Conroe, TX Chesterfield, MO Colton, CA Omaha, NE Arlington Hts, IL Santa Rosa, CA Miami, FL Fargo, ND Chicago, IL
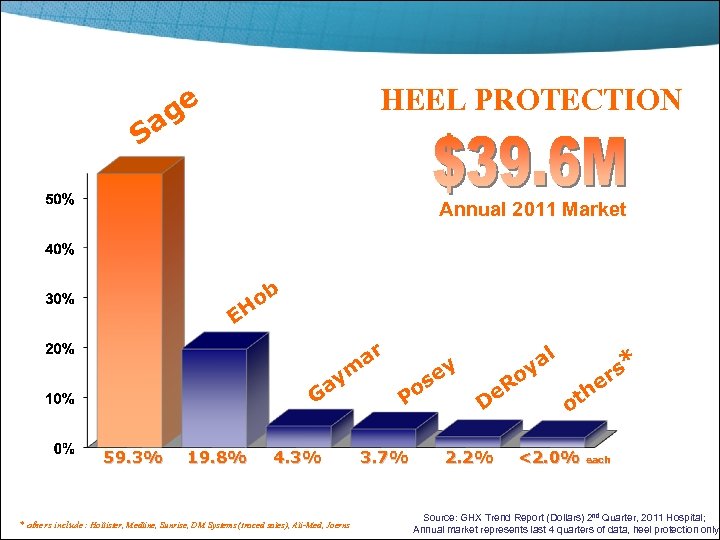 HEEL PROTECTION ge a S Annual 2011 Market ob H E ar ym Ga 59. 3% 19. 8% 4. 3% * others include: Hollister, Medline, Sunrise, DM Systems (traced sales), Ali-Med, Joerns ey os P 3. 7% l ya o e. R D 2. 2% s er * th o <2. 0% each Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data, heel protection only
HEEL PROTECTION ge a S Annual 2011 Market ob H E ar ym Ga 59. 3% 19. 8% 4. 3% * others include: Hollister, Medline, Sunrise, DM Systems (traced sales), Ali-Med, Joerns ey os P 3. 7% l ya o e. R D 2. 2% s er * th o <2. 0% each Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data, heel protection only
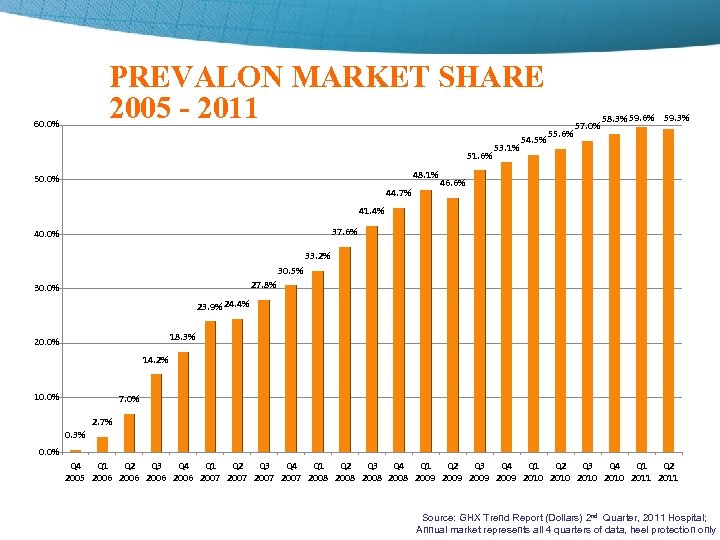 PREVALON MARKET SHARE 2005 - 2011 60. 0% 51. 6% 48. 1% 50. 0% 44. 7% 53. 1% 54. 5% 55. 6% 57. 0% 58. 3% 59. 6% 59. 3% 46. 6% 41. 4% 37. 6% 40. 0% 33. 2% 30. 5% 27. 8% 30. 0% 23. 9% 24. 4% 18. 3% 20. 0% 14. 2% 10. 0% 7. 0% 2. 7% 0. 3% 0. 0% Q 4 Q 1 Q 2 Q 3 Q 4 Q 1 Q 2 Q 3 Q 4 Q 1 Q 2 2005 2006 2007 2008 2009 2010 2011 Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents all 4 quarters of data, heel protection only
PREVALON MARKET SHARE 2005 - 2011 60. 0% 51. 6% 48. 1% 50. 0% 44. 7% 53. 1% 54. 5% 55. 6% 57. 0% 58. 3% 59. 6% 59. 3% 46. 6% 41. 4% 37. 6% 40. 0% 33. 2% 30. 5% 27. 8% 30. 0% 23. 9% 24. 4% 18. 3% 20. 0% 14. 2% 10. 0% 7. 0% 2. 7% 0. 3% 0. 0% Q 4 Q 1 Q 2 Q 3 Q 4 Q 1 Q 2 Q 3 Q 4 Q 1 Q 2 2005 2006 2007 2008 2009 2010 2011 Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents all 4 quarters of data, heel protection only
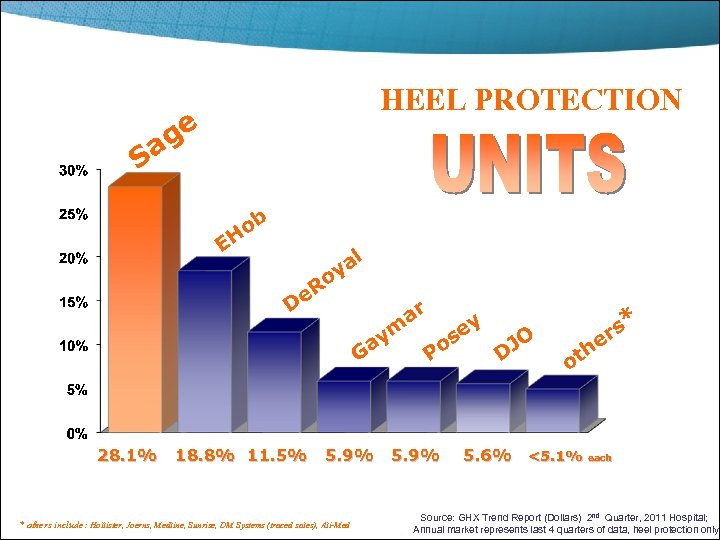 HEEL PROTECTION ge a S ob H E Ro De al y ar Ga ym 28. 1% 18. 8% 11. 5% 5. 9% * others include: Hollister, Joerns, Medline, Sunrise, DM Systems (traced sales), Ali-Med ey JO os P D 5. 9% rs e * h ot 5. 6% <5. 1% each Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data, heel protection only
HEEL PROTECTION ge a S ob H E Ro De al y ar Ga ym 28. 1% 18. 8% 11. 5% 5. 9% * others include: Hollister, Joerns, Medline, Sunrise, DM Systems (traced sales), Ali-Med ey JO os P D 5. 9% rs e * h ot 5. 6% <5. 1% each Source: GHX Trend Report (Dollars) 2 nd Quarter, 2011 Hospital; Annual market represents last 4 quarters of data, heel protection only
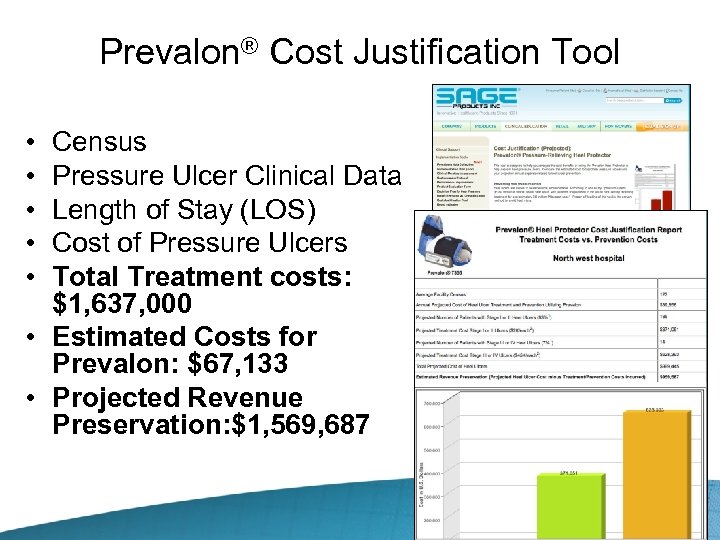 Prevalon® Cost Justification Tool • • • Census Pressure Ulcer Clinical Data Length of Stay (LOS) Cost of Pressure Ulcers Total Treatment costs: $1, 637, 000 • Estimated Costs for Prevalon: $67, 133 • Projected Revenue Preservation: $1, 569, 687
Prevalon® Cost Justification Tool • • • Census Pressure Ulcer Clinical Data Length of Stay (LOS) Cost of Pressure Ulcers Total Treatment costs: $1, 637, 000 • Estimated Costs for Prevalon: $67, 133 • Projected Revenue Preservation: $1, 569, 687
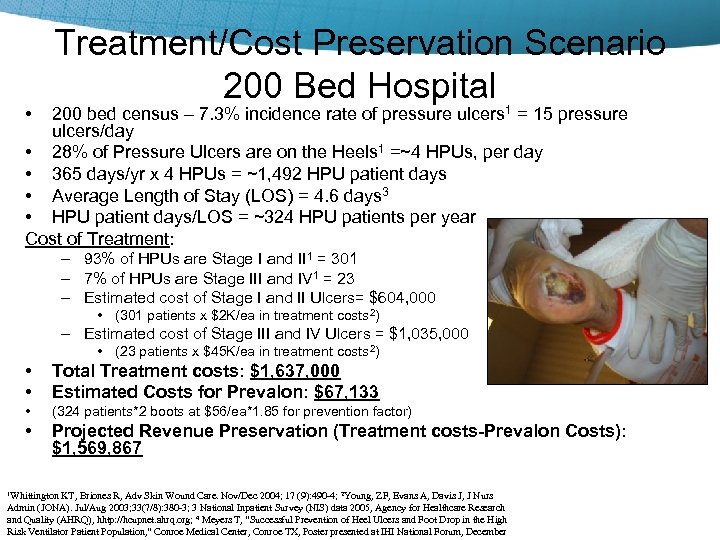 • Treatment/Cost Preservation Scenario 200 Bed Hospital 200 bed census – 7. 3% incidence rate of pressure ulcers 1 = 15 pressure ulcers/day • 28% of Pressure Ulcers are on the Heels 1 =~4 HPUs, per day • 365 days/yr x 4 HPUs = ~1, 492 HPU patient days • Average Length of Stay (LOS) = 4. 6 days 3 • HPU patient days/LOS = ~324 HPU patients per year Cost of Treatment: – 93% of HPUs are Stage I and II 1 = 301 – 7% of HPUs are Stage III and IV 1 = 23 – Estimated cost of Stage I and II Ulcers= $604, 000 • (301 patients x $2 K/ea in treatment costs 2) – Estimated cost of Stage III and IV Ulcers = $1, 035, 000 • (23 patients x $45 K/ea in treatment costs 2) • • Total Treatment costs: $1, 637, 000 Estimated Costs for Prevalon: $67, 133 • (324 patients*2 boots at $56/ea*1. 85 for prevention factor) • Projected Revenue Preservation (Treatment costs-Prevalon Costs): $1, 569, 867 1 Whittington KT, Briones R, Adv Skin Wound Care. Nov/Dec 2004; 17 (9): 490 -4; 2 Young, ZF, Evans A, Davis J, J Nurs Admin (JONA). Jul/Aug 2003; 33(7/8): 380 -3; 3 National Inpatient Survey (NIS) data 2005, Agency for Healthcare Research and Quality (AHRQ), hhtp: //hcupnet. ahrq. org; 4 Meyers T, “Successful Prevention of Heel Ulcers and Foot Drop in the High Risk Ventilator Patient Population, ” Conroe Medical Center, Conroe TX, Poster presented at IHI National Forum, December
• Treatment/Cost Preservation Scenario 200 Bed Hospital 200 bed census – 7. 3% incidence rate of pressure ulcers 1 = 15 pressure ulcers/day • 28% of Pressure Ulcers are on the Heels 1 =~4 HPUs, per day • 365 days/yr x 4 HPUs = ~1, 492 HPU patient days • Average Length of Stay (LOS) = 4. 6 days 3 • HPU patient days/LOS = ~324 HPU patients per year Cost of Treatment: – 93% of HPUs are Stage I and II 1 = 301 – 7% of HPUs are Stage III and IV 1 = 23 – Estimated cost of Stage I and II Ulcers= $604, 000 • (301 patients x $2 K/ea in treatment costs 2) – Estimated cost of Stage III and IV Ulcers = $1, 035, 000 • (23 patients x $45 K/ea in treatment costs 2) • • Total Treatment costs: $1, 637, 000 Estimated Costs for Prevalon: $67, 133 • (324 patients*2 boots at $56/ea*1. 85 for prevention factor) • Projected Revenue Preservation (Treatment costs-Prevalon Costs): $1, 569, 867 1 Whittington KT, Briones R, Adv Skin Wound Care. Nov/Dec 2004; 17 (9): 490 -4; 2 Young, ZF, Evans A, Davis J, J Nurs Admin (JONA). Jul/Aug 2003; 33(7/8): 380 -3; 3 National Inpatient Survey (NIS) data 2005, Agency for Healthcare Research and Quality (AHRQ), hhtp: //hcupnet. ahrq. org; 4 Meyers T, “Successful Prevention of Heel Ulcers and Foot Drop in the High Risk Ventilator Patient Population, ” Conroe Medical Center, Conroe TX, Poster presented at IHI National Forum, December
 Our Recipe… • Assessment – Identify High Risk • Evidence-based protocols • Targeted outcome Vs baseline • Educate • Implement interventions • Measure (PST, CJT) • Celebrate • Posters • Papers • Speakers, Web, Guidelines
Our Recipe… • Assessment – Identify High Risk • Evidence-based protocols • Targeted outcome Vs baseline • Educate • Implement interventions • Measure (PST, CJT) • Celebrate • Posters • Papers • Speakers, Web, Guidelines
 Thank You For Your Time
Thank You For Your Time


