95a6daa18791a673d2d3dcafe4730559.ppt
- Количество слайдов: 69
Heart Failure Bill Cayley, Jr MD MDiv
Learning objectives Participants will be able to discuss 1. Evaluation & management of acute heart failure 2. Causes & classification of heart failure 3. Diagnosis of heart failure 4. Management of chronic heart failure
Guidelines n n n 2009 focused update incorporated into the ACC/AHA 2005 Guidelines forthe Diagnosis and Management of Heart Failure in Adults. Circulation. 2009 Apr 14; 119(14). PMID: 19324966. (http: //circ. ahajournals. org/cgi/content/full/119/14/e 391) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J. 2008 Oct; 29(19): 2388442. PMID: 18799522. (http: //eurheartj. oxfordjournals. org/cgi/content/full/29/19/2388) ALCS Resource Text. Dallas, TX: American Heart Association, 2008.
John 50 year old traffic accident victim n n Ø Ø Ø Awake, moderate distress, c/o chest pain & SOB PMH: Hypertension, diabetes. SH: ½ ppd cigarettes, taxi driver Exam: HR 120, BP 80/40. PERRLA. Lips cut. Heart irregular. Chest has wet crackles. Abdomen tender. What is the clinical syndrome? What could be the underlying diagnoses? Why? What do you do? Why?
Shock & heart failure n n Shock: Insufficient circulation of oxygenated blood to meet metabolic demands. (Crit Care. 2006; 10(4): 221) Heart failure: a complex clinical syndrome due to a structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. (Circulation. 2009 Apr 14; 119(14))
Heart failure (HF): Definition Features of HF: n n n Shortness of breath at rest or during exertion or fatigue (A) (B) Signs of fluid retention such as pulmonary congestion or ankle swelling (A) (B) Objective evidence of an abnormality of the structure or function of the heart at rest (B) (A) ACC/AHA 2009 Update (B) ESC 2008 Guidelines
HF – a few more points… ACC/AHA Update… Ø Because not all patients have volume overload at the time of initial or subsequent evaluation, the term "heart failure" is preferred over the older term "congestive heart failure. " Ø It should be emphasized that HF is not equivalent to cardiomyopathy or to LV dysfunction; these latter terms describe possible structural or functional reasons for the development of HF. ESC Guidelines Ø A clinical response to treatment directed at HF alone is not sufficient for the diagnosis. . . Ø HF should never be a sole diagnosis. The cause should always be sought.
I. Acute heart failure & shock
Acute HF and shock n 50 year old traffic accident victim, short of breath, chest crackles. n What do you do? ABCD – initial approach n Airway n n Breathing n n Adequate ventilation? Provide O 2. Circulation n n Maintaining airway? Trauma or obstruction? Assess BP, Heart Rate, Rhythm Diagnosis
Differential diagnosis n AMPLE History and Physical n n n Allergies Medications Past illnesses / Pregnancy Last meal Events / Environment n What happened? When? Where?
Possible causes: Hs & Ts n n n Hypovolemia Hypoxia Hydrogen ion n n Acidiosis Hypo/Hyperkalemia Hypoglycemia Hypothermia n n Toxin Tamponade n n n Tension pneumothorax Thrombosis n n Cardiac or pulmonary Trauma
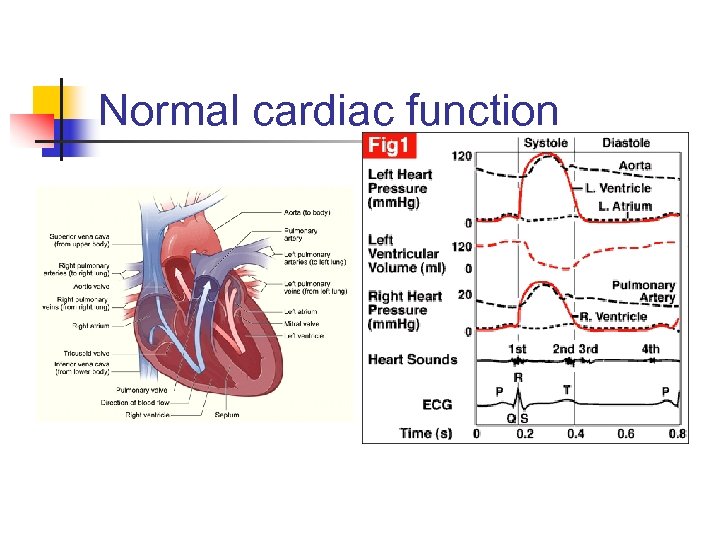
Normal cardiac function
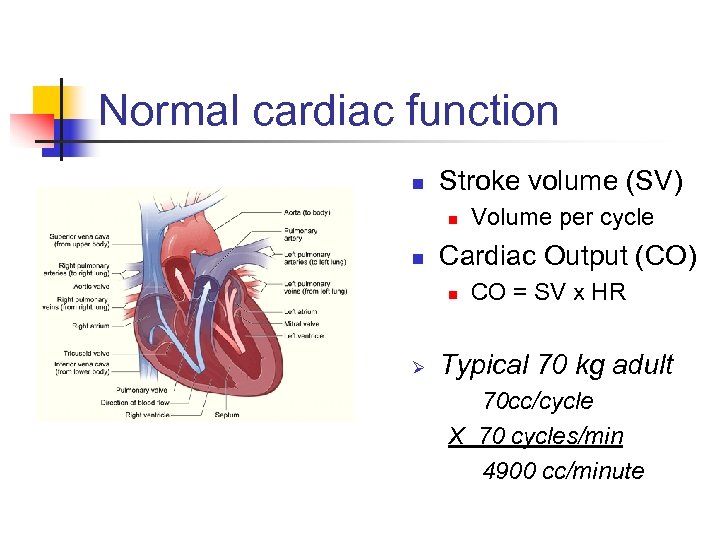
Normal cardiac function n Stroke volume (SV) n n Cardiac Output (CO) n Ø Volume per cycle CO = SV x HR Typical 70 kg adult 70 cc/cycle X 70 cycles/min 4900 cc/minute
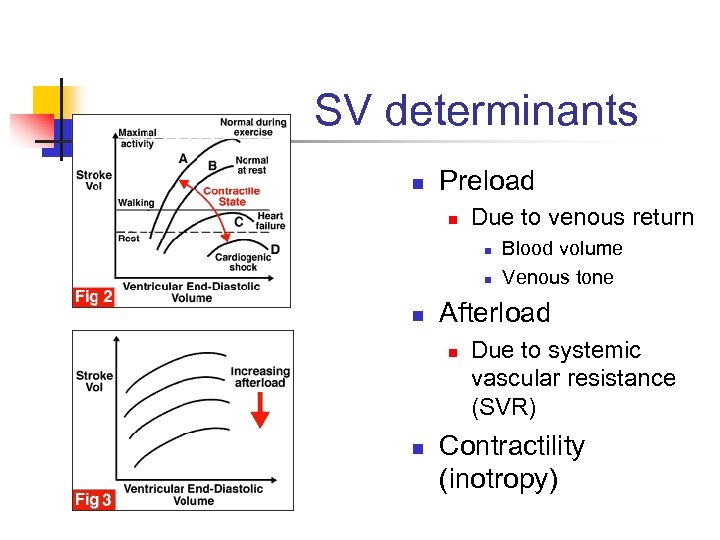
SV determinants n Preload n Due to venous return n Afterload n n Blood volume Venous tone Due to systemic vascular resistance (SVR) Contractility (inotropy)
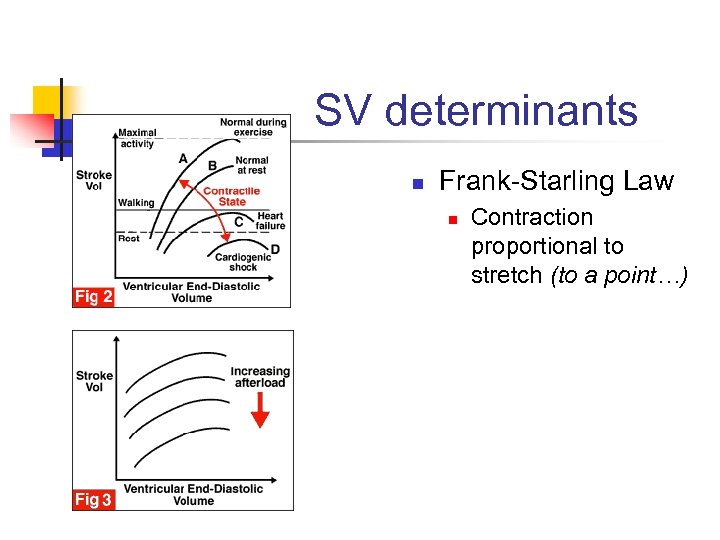
SV determinants n Frank-Starling Law n Contraction proportional to stretch (to a point…)
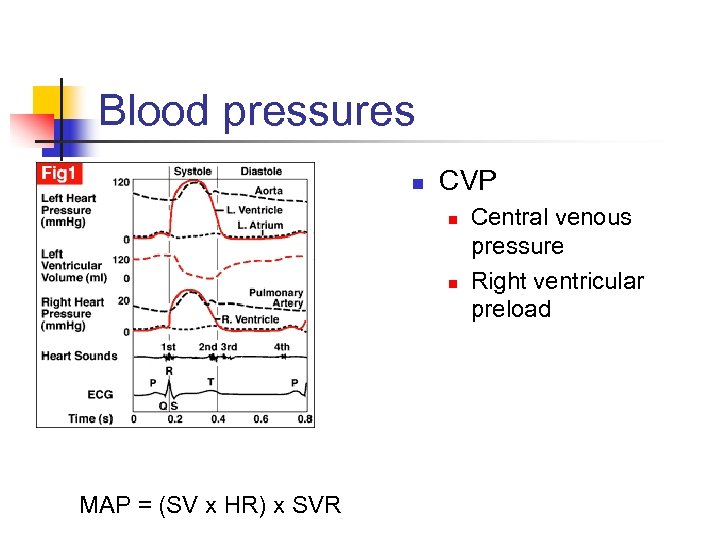
Blood pressures n CVP n n MAP = (SV x HR) x SVR Central venous pressure Right ventricular preload
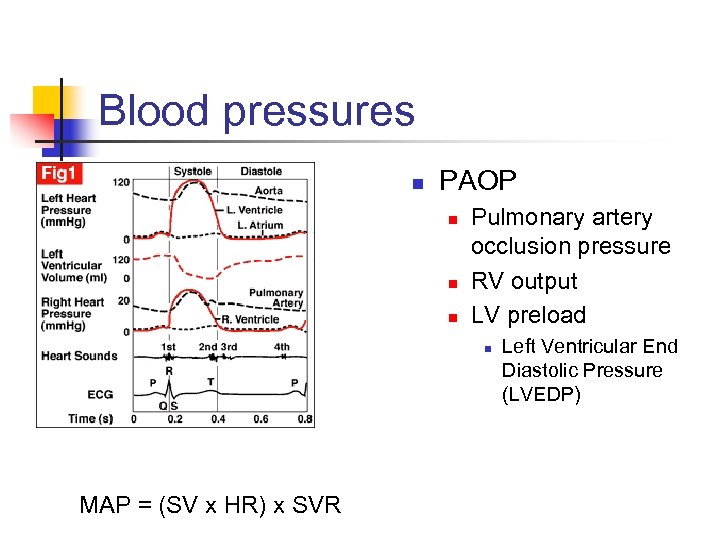
Blood pressures n PAOP n n n Pulmonary artery occlusion pressure RV output LV preload n MAP = (SV x HR) x SVR Left Ventricular End Diastolic Pressure (LVEDP)
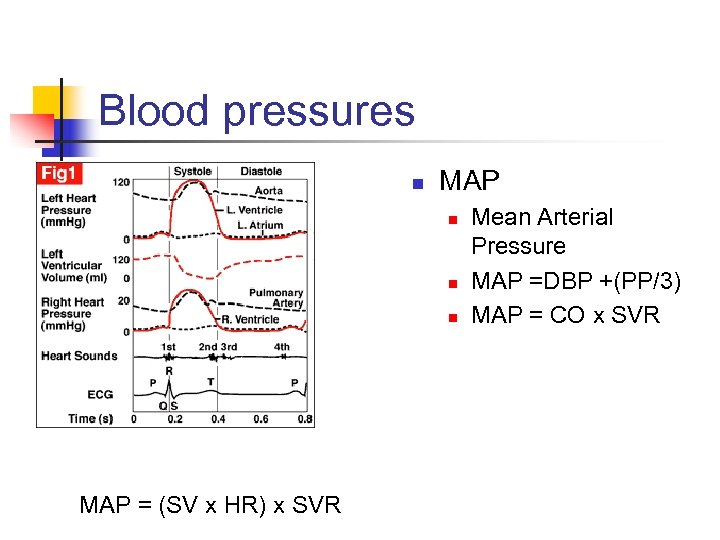
Blood pressures n MAP n n n MAP = (SV x HR) x SVR Mean Arterial Pressure MAP =DBP +(PP/3) MAP = CO x SVR
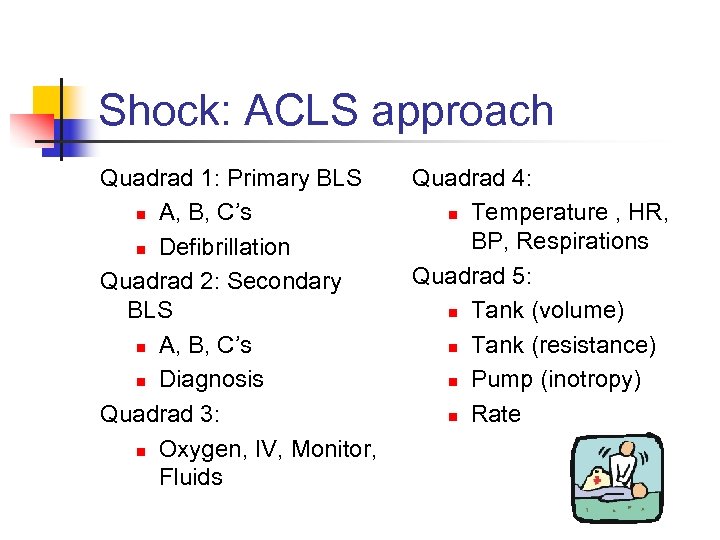
Shock: ACLS approach Quadrad 1: Primary BLS n A, B, C’s n Defibrillation Quadrad 2: Secondary BLS n A, B, C’s n Diagnosis Quadrad 3: n Oxygen, IV, Monitor, Fluids Quadrad 4: n Temperature , HR, BP, Respirations Quadrad 5: n Tank (volume) n Tank (resistance) n Pump (inotropy) n Rate
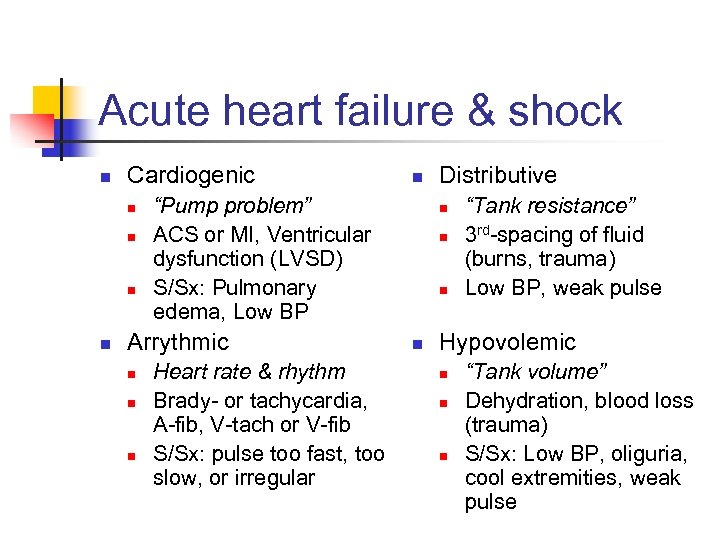
Acute heart failure & shock n Cardiogenic n n “Pump problem” ACS or MI, Ventricular dysfunction (LVSD) S/Sx: Pulmonary edema, Low BP Arrythmic n n Heart rate & rhythm Brady- or tachycardia, A-fib, V-tach or V-fib S/Sx: pulse too fast, too slow, or irregular Distributive n n “Tank resistance” 3 rd-spacing of fluid (burns, trauma) Low BP, weak pulse Hypovolemic n n n “Tank volume” Dehydration, blood loss (trauma) S/Sx: Low BP, oliguria, cool extremities, weak pulse
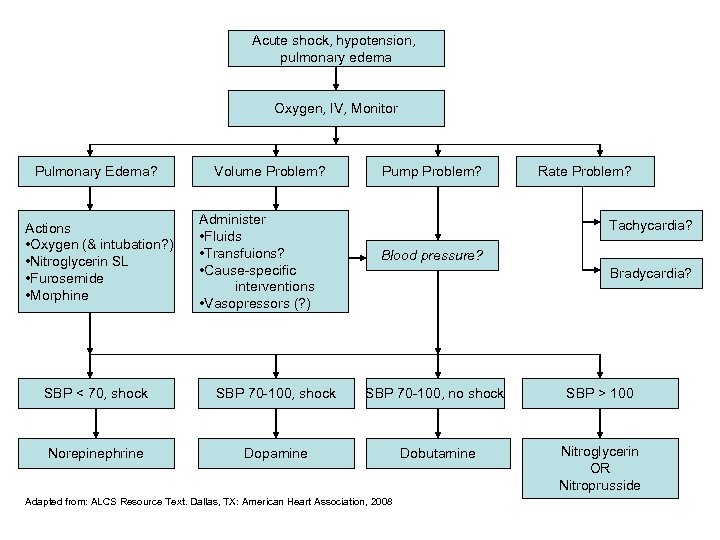
Acute shock, hypotension, pulmonary edema Oxygen, IV, Monitor Pulmonary Edema? Actions • Oxygen (& intubation? ) • Nitroglycerin SL • Furosemide • Morphine Volume Problem? Administer • Fluids • Transfuions? • Cause-specific interventions • Vasopressors (? ) Pump Problem? Rate Problem? Tachycardia? Blood pressure? Bradycardia? SBP < 70, shock SBP 70 -100, no shock SBP > 100 Norepinephrine Dopamine Dobutamine Nitroglycerin OR Nitroprusside Adapted from: ALCS Resource Text. Dallas, TX: American Heart Association, 2008
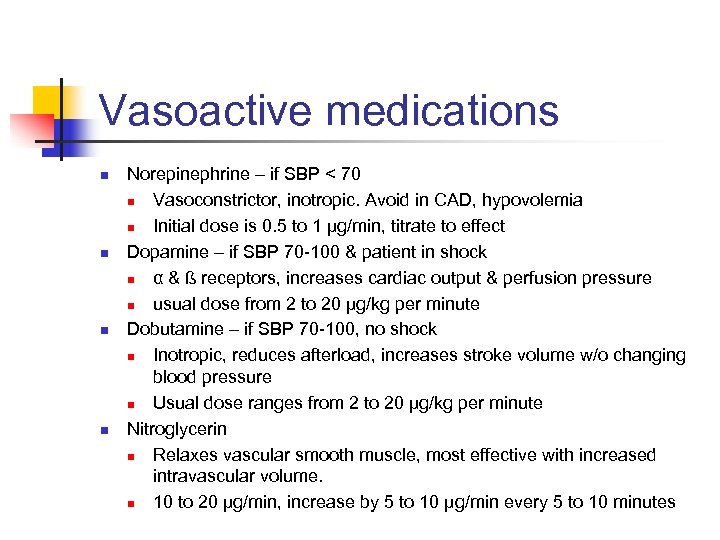
Vasoactive medications n n Norepinephrine – if SBP < 70 n Vasoconstrictor, inotropic. Avoid in CAD, hypovolemia n Initial dose is 0. 5 to 1 µg/min, titrate to effect Dopamine – if SBP 70 -100 & patient in shock n α & ß receptors, increases cardiac output & perfusion pressure n usual dose from 2 to 20 µg/kg per minute Dobutamine – if SBP 70 -100, no shock n Inotropic, reduces afterload, increases stroke volume w/o changing blood pressure n Usual dose ranges from 2 to 20 µg/kg per minute Nitroglycerin n Relaxes vascular smooth muscle, most effective with increased intravascular volume. n 10 to 20 µg/min, increase by 5 to 10 µg/min every 5 to 10 minutes
II. Causes & classification
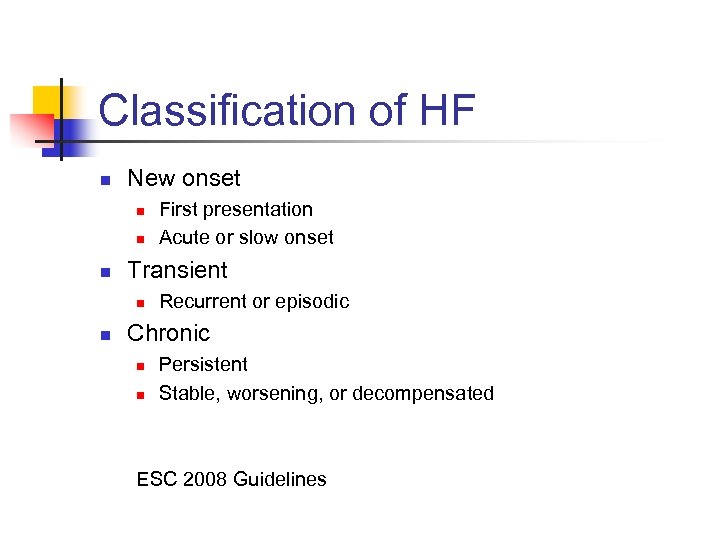
Classification of HF n New onset n n n Transient n n First presentation Acute or slow onset Recurrent or episodic Chronic n n Persistent Stable, worsening, or decompensated ESC 2008 Guidelines
Chronic HF and systolic function n n “A distinction is frequently made between systolic and diastolic HF. The distinction is somewhat arbitrary. ” Diastolic HF: n n n Symptoms and/or signs of HF and a preserved left ventricular ejection fraction (LVEF) >40– 50%. No consensus as to the cut-off for preserved EF. In the past most patients admitted to hospitals for investigation or entered into clinical trials have had dilated hearts with a reduced EF <35 or 40%. Most patients with HF have evidence of both systolic and diastolic dysfunction at rest or on exercise. Diastolic and systolic HFs should not be considered as separate entities. ESC 2008 Guidelines
Chronic HF and systolic function Clinical Heart Failure
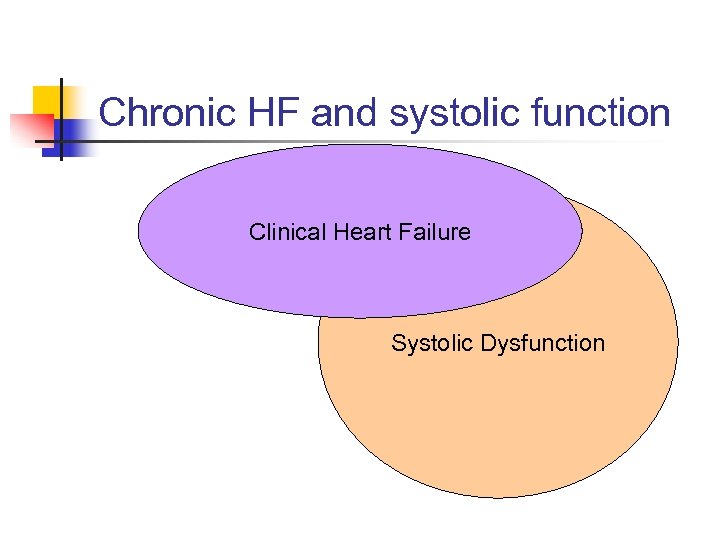
Chronic HF and systolic function Clinical Heart Failure Systolic Dysfunction
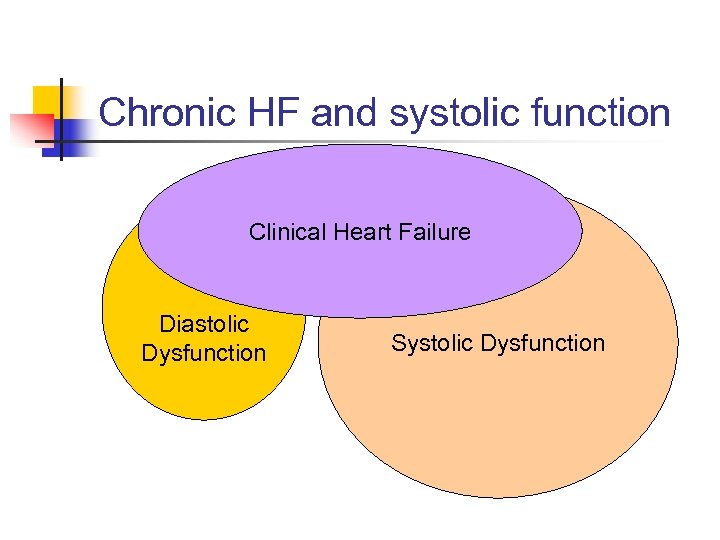
Chronic HF and systolic function Clinical Heart Failure Diastolic Dysfunction Systolic Dysfunction
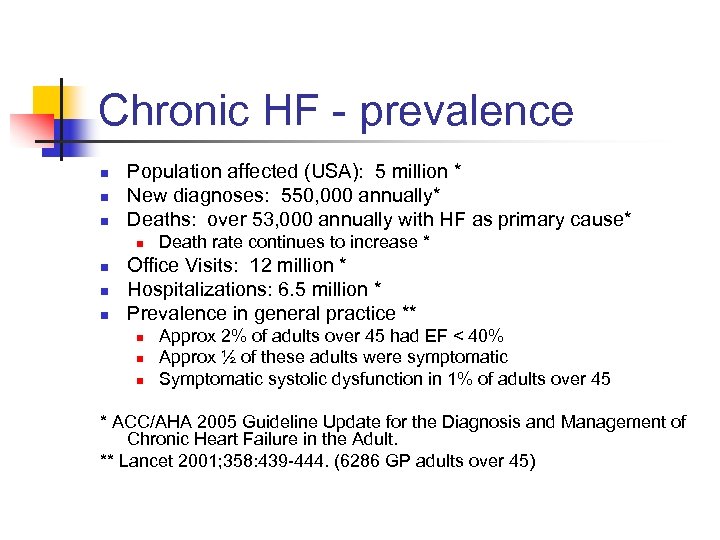
Chronic HF - prevalence n n n Population affected (USA): 5 million * New diagnoses: 550, 000 annually* Deaths: over 53, 000 annually with HF as primary cause* n n Death rate continues to increase * Office Visits: 12 million * Hospitalizations: 6. 5 million * Prevalence in general practice ** n n n Approx 2% of adults over 45 had EF < 40% Approx ½ of these adults were symptomatic Symptomatic systolic dysfunction in 1% of adults over 45 * ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. ** Lancet 2001; 358: 439 -444. (6286 GP adults over 45)
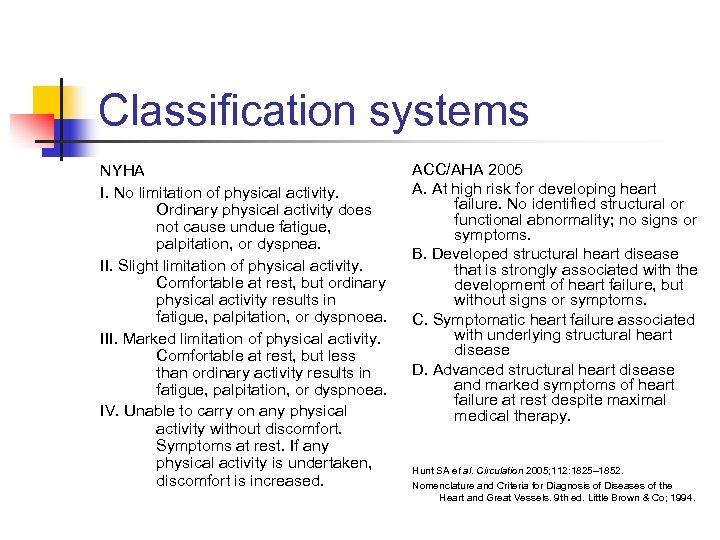
Classification systems NYHA I. No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea. II. Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnoea. III. Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity results in fatigue, palpitation, or dyspnoea. IV. Unable to carry on any physical activity without discomfort. Symptoms at rest. If any physical activity is undertaken, discomfort is increased. ACC/AHA 2005 A. At high risk for developing heart failure. No identified structural or functional abnormality; no signs or symptoms. B. Developed structural heart disease that is strongly associated with the development of heart failure, but without signs or symptoms. C. Symptomatic heart failure associated with underlying structural heart disease D. Advanced structural heart disease and marked symptoms of heart failure at rest despite maximal medical therapy. Hunt SA et al. Circulation 2005; 112: 1825– 1852. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels. 9 th ed. Little Brown & Co; 1994.
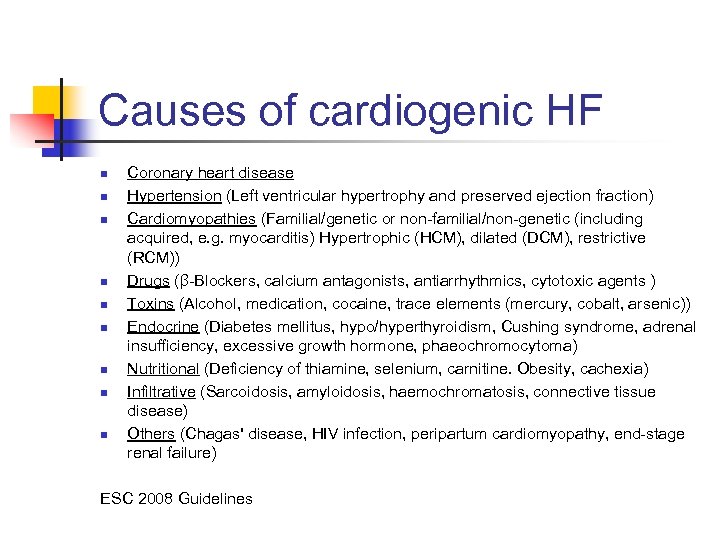
Causes of cardiogenic HF n n n n n Coronary heart disease Hypertension (Left ventricular hypertrophy and preserved ejection fraction) Cardiomyopathies (Familial/genetic or non-familial/non-genetic (including acquired, e. g. myocarditis) Hypertrophic (HCM), dilated (DCM), restrictive (RCM)) Drugs (β-Blockers, calcium antagonists, antiarrhythmics, cytotoxic agents ) Toxins (Alcohol, medication, cocaine, trace elements (mercury, cobalt, arsenic)) Endocrine (Diabetes mellitus, hypo/hyperthyroidism, Cushing syndrome, adrenal insufficiency, excessive growth hormone, phaeochromocytoma) Nutritional (Deficiency of thiamine, selenium, carnitine. Obesity, cachexia) Infiltrative (Sarcoidosis, amyloidosis, haemochromatosis, connective tissue disease) Others (Chagas' disease, HIV infection, peripartum cardiomyopathy, end-stage renal failure) ESC 2008 Guidelines
III. Diagnosis of heart failure
Fred HPI: 64 year old man, presents as new patient with fatigue for 3 weeks, shortness of breath with exertion that is worse over the past 3 months, vague chest discomfort, and mild ankle swelling. Also has back pain and erectile dysfunction. PMH: Type II DM, Htn, depression, hyperlipidemia. FH: No CAD or CVAs, MGM had Diabetes. SH: Former trucker, quit tobacco 27 years ago, minimal Et. OH, no drugs. Meds: Metformin 500 mg BID, HTCZ 25 mg daily, bupropion 100 mg daily, metoprolol 25 mg bid.
History and exam n Typical Symptoms of HF on presentation n Decreased exercise tolerance n Dyspnea? Fatigue? n Fluid retention n Abd Swelling? Leg Swelling n Asymptomatic n Cardiac dysfunction incidentally discovered ACC/AHA 2009 Update
Initial evaluation: History n n n A thorough history and physical examination should be obtained/performed in patients presenting with HF to identify cardiac and noncardiac disorders or behaviors that might cause or accelerate the development or progression of HF. A careful history of current and past use of alcohol, illicit drugs, current or past standard or "alternative therapies, " and chemotherapy drugs should be obtained from patients presenting with HF. In patients presenting with HF, initial assessment should be made of the patient's ability to perform routine and desired activities of daily living. ACC/AHA 2009 Update
Initial evaluation: Exam n Initial examination of patients presenting with HF should include: n assessment of the patient's volume status n orthostatic blood pressure changes n measurement of weight and height n calculation of body mass index ACC/AHA 2009 Update
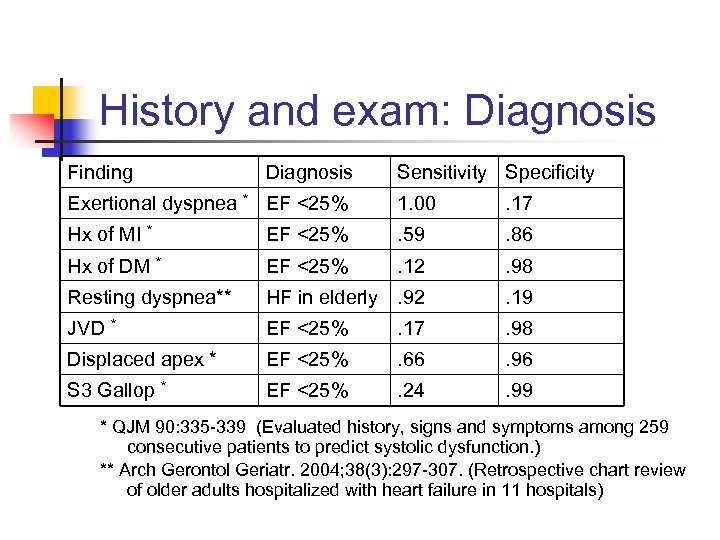
History and exam: Diagnosis Finding Diagnosis Sensitivity Specificity Exertional dyspnea * EF <25% 1. 00 . 17 Hx of MI * EF <25% . 59 . 86 Hx of DM * EF <25% . 12 . 98 Resting dyspnea** HF in elderly. 92 . 19 JVD * EF <25% . 17 . 98 Displaced apex * EF <25% . 66 . 96 S 3 Gallop * EF <25% . 24 . 99 * QJM 90: 335 -339 (Evaluated history, signs and symptoms among 259 consecutive patients to predict systolic dysfunction. ) ** Arch Gerontol Geriatr. 2004; 38(3): 297 -307. (Retrospective chart review of older adults hospitalized with heart failure in 11 hospitals)
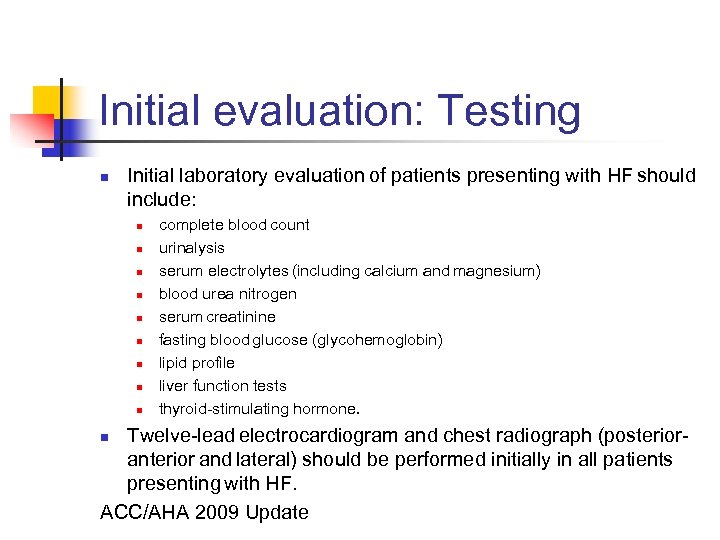
Initial evaluation: Testing n Initial laboratory evaluation of patients presenting with HF should include: n n n n n complete blood count urinalysis serum electrolytes (including calcium and magnesium) blood urea nitrogen serum creatinine fasting blood glucose (glycohemoglobin) lipid profile liver function tests thyroid-stimulating hormone. Twelve-lead electrocardiogram and chest radiograph (posterioranterior and lateral) should be performed initially in all patients presenting with HF. ACC/AHA 2009 Update n
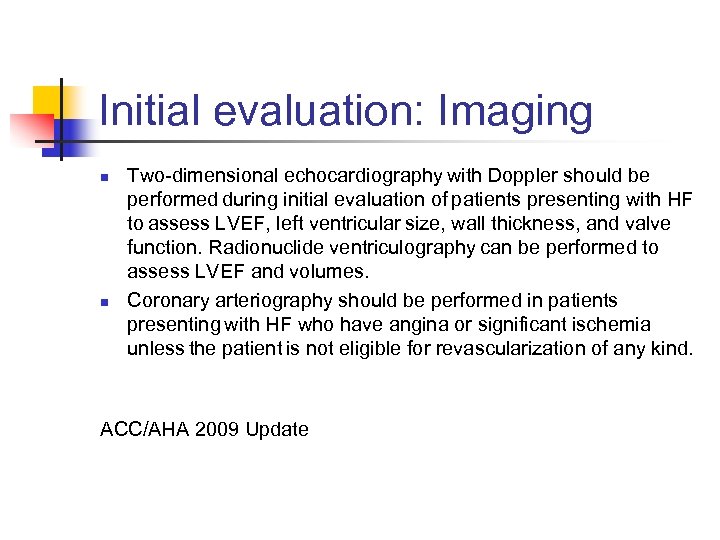
Initial evaluation: Imaging n n Two-dimensional echocardiography with Doppler should be performed during initial evaluation of patients presenting with HF to assess LVEF, left ventricular size, wall thickness, and valve function. Radionuclide ventriculography can be performed to assess LVEF and volumes. Coronary arteriography should be performed in patients presenting with HF who have angina or significant ischemia unless the patient is not eligible for revascularization of any kind. ACC/AHA 2009 Update
What about BNP? n n n B-type natriuretic peptide 32 amino acid polypeptide Secreted from the ventricles Response to volume expansion & pressure overload Natriuretic and vasodilatory Suppress renin-angiotensin-aldosterone system J Am Board Fam Pract 2003; 16: 327 -333.
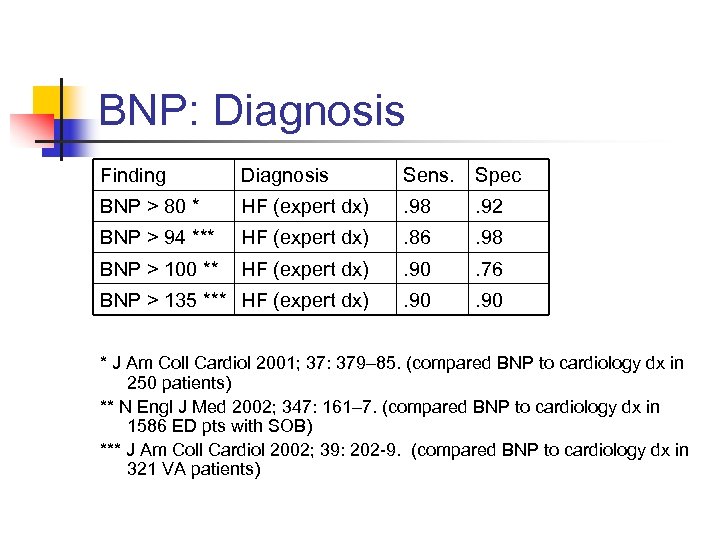
BNP: Diagnosis Finding Diagnosis Sens. Spec BNP > 80 * HF (expert dx) . 98 . 92 BNP > 94 *** HF (expert dx) . 86 . 98 BNP > 100 ** HF (expert dx) . 90 . 76 BNP > 135 *** HF (expert dx) . 90 * J Am Coll Cardiol 2001; 37: 379– 85. (compared BNP to cardiology dx in 250 patients) ** N Engl J Med 2002; 347: 161– 7. (compared BNP to cardiology dx in 1586 ED pts with SOB) *** J Am Coll Cardiol 2002; 39: 202 -9. (compared BNP to cardiology dx in 321 VA patients)
BUT. . . n n A word of caution… n Patients with pulmonary embolism, lung cancer, and pulmonary TB had mean BNP 90 or higher *** n Mean BNP of 141 * – 348 ** in patients with LVSD but no clinical heart failure Thus… n BNP aids in diagnosis but is not the end of the story! * J Am Coll Cardiol 2001; 37: 379– 85. ** N Engl J Med 2002; 347: 161– 7. *** J Am Coll Cardiol 2002; 39: 202 -9.
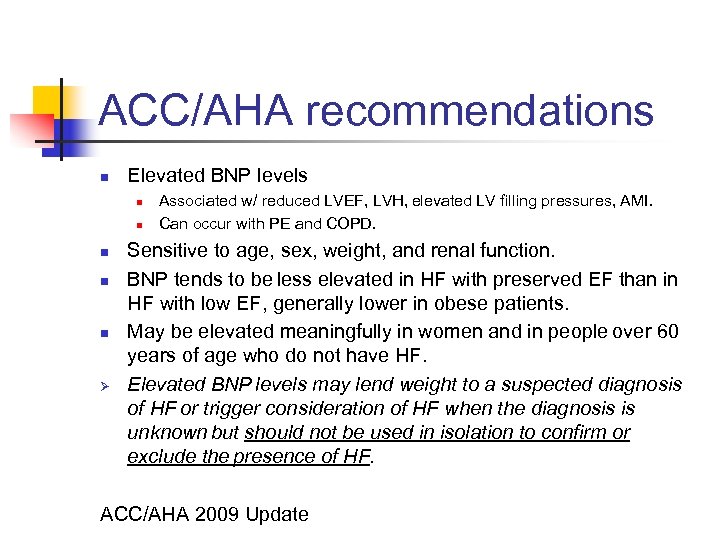
ACC/AHA recommendations n Elevated BNP levels n n n Ø Associated w/ reduced LVEF, LVH, elevated LV filling pressures, AMI. Can occur with PE and COPD. Sensitive to age, sex, weight, and renal function. BNP tends to be less elevated in HF with preserved EF than in HF with low EF, generally lower in obese patients. May be elevated meaningfully in women and in people over 60 years of age who do not have HF. Elevated BNP levels may lend weight to a suspected diagnosis of HF or trigger consideration of HF when the diagnosis is unknown but should not be used in isolation to confirm or exclude the presence of HF. ACC/AHA 2009 Update
Imaging: Diagnosis n First things first – what is the question? n Does the patient have heart failure? n Does the patient have systolic or diastolic dysfunction? n Will the patient benefit from revascularization? n What is the prognosis?
Imaging: Options n n Options n Two dimensional trans-thoracic echocardiogram n Stress testing with nuclear perfusion imaging n Stress testing and echocardiographic imaging n Angiography – to define need for revascularization Considerations n HF plus ischemia and angina n CABG improves morbidity and mortality n HF with uncertain ischemia n May need to define CAD if there is angina n If no angina, benefit of defining ischemia is unclear
IV. Management of chronic HF
Fran HPI: 60 year old woman, presents to free clinic with shortness of breath, mild leg swelling and history of “heart attack”. Off most medications since her husband died and she lost her insurance. Breathes OK at rest and walking around house, but SOB going to mailbox or carrying groceries. PMH: MI, Hypertension. FH: Hypertension, mom died of MI at 75. SH: Tobacco use 1 pack/day, minimal Et. OH. Meds: HTCZ 25 mg daily, was on some other “heart pills” but she can’t remember which ones.
Fran PE: Older female, appears older than stated age, NAD VS: Afebrile, BP 160/100, RR 24, 180#, 65” HEENT: Unremarkable Neck: Supple, no LA or TM, no obvious JVD Cor: Regular, no murmur Lungs: Basilar Crackles Legs: 1+ pitting edema
Fran CXR: Cardiomegally EKG: Q in II, III, F suggesting old MI Echo: (old records) LVEF 30%, inferior wall motion abnormality.
Fran n What would you do? Why?
ACEIs: Long-term results n n Multiple trials show short-term benefit of ACEIs for HF & MI Long-term outcomes: n Lancet. 2000 May 6; 355(9215): 1575 -81. n Systematic overview of long-term trials of ACEIs n For patients with HF or LVSD after MI n Outcomes: HF admission, MI, death n RCTs with 1000 or more patients n Compared 3 trials with SOLVD
ARBs and HF n Angiotensin receptor blockers: n Blockade angiotensin II type 1 receptor rather than inhibit angiotensin conversion n Theoretically superior blockade of renin-angiotensin system n Alternative for ACEI-intolerant patients? n Trials in HF have shown mixed results n 2002 meta-analysis: no statistically significant difference in mortality or heart failure hospitalization rates between ARBs and placebo in patients with heart failure and left ventricular systolic dysfunction (J Am Coll Cardiol. 2002; 39: 463 -70 )
Beta-blockers in HF n Summary n Reduce mortality n Reduce hospitalizations n Relative benefit between agents difficult to discern n Carvedilol appears superior to short-acting metoprolol n Adequate doses needed n Up to 25 mg BID of carvedilol n Up to 100 mg BID of metoprolol n Early initiation in stabilized patients does not increase risks
Digoxin and outcomes n n n Mortality n Not reduced by treating left ventricular systolic dysfunction with digoxin n May be decreased by low serum digoxin concentration (SDC) < 0. 9, but may be INCREASED by SDC >1. 1 Hospitalizations n Decreased by treating left ventricular systolic dysfunction with digoxin n Cardiac arrest risk increased with Digoxin if Cr > 1. 4 Symptoms and Quality of Life n Conflicting evidence on improvement in quality of life, but if digoxin is used levels < 0. 9 are most beneficial
Spironolactone & HF n Background n ACEIs and ARBs appear to reduce levels of aldosterone n Effect may be only short-term n Aldosterone may have adverse effects on heart structure and function n Suggested by experimental data n Spironolactone antagonizes aldosterone. n Recommended for Stage D HF
Diuretics n n n Increase sodium excretion Decrease signs of fluid retention Provide most rapid symptomatic relief No long-term trials on morbidity or mortality ACC/AHA recommends n Loop diuretics for symptom control n Diuretics should not be used for HF in isolation
Stage “A” HF n n n n n ACC/AHA 2009 Update Systolic and diastolic hypertension should be controlled in accordance with contemporary guidelines. Lipid disorders should be treated in accordance with contemporary guidelines. For patients with diabetes mellitus, blood sugar should be controlled in accordance with contemporary guidelines. Patients should be counseled to avoid behaviors that may increase the risk of HF (e. g. , smoking, excessive alcohol consumption, and illicit drug use). Ventricular rate should be controlled or sinus rhythm restored in patients with supraventricular tachyarrhythmias. Thyroid disorders should be treated. Periodic evaluation for signs and symptoms of HF. For patients with known CAD, follow current guidelines for secondary prevention. Perform a noninvasive evaluation of LV function (i. e. , LVEF) in patients with a strong family history of cardiomyopathy or in those receiving cardiotoxic interventions.
Stage “B” HF n n n n ACC/AHA 2009 Update Beta blockers and ACEIs should be used in all patients with a recent or remote history of MI regardless of EF or presence of HF. Beta blockers are indicated in all patients without a history of MI who have a reduced LVEF with no HF symptoms. Angiotensin converting enzyme inhibitors should be used in patients with a reduced EF and no symptoms of HF, even if they have not experienced MI. An ARB should be administered to post-MI patients without HF who are intolerant of ACEIs and have a low LVEF. Patients who have not developed HF symptoms should be treated according to contemporary guidelines after an acute MI. Coronary revascularization should be recommended in appropriate patients without symptoms of HF in accordance with contemporary guidelines. Valve replacement or repair should be recommended for patients with hemodynamically significant valvular stenosis or regurgitation and no symptoms of HF in accordance with contemporary guidelines.
Stage “C” HF n n n ACC/AHA 2009 Update Diuretics and salt restriction are indicated in patients with current or prior symptoms of HF and reduced LVEF who have evidence of fluid retention. Angiotensin-converting enzyme inhibitors are recommended for all patients with current or prior symptoms of HF and reduced LVEF, unless contraindicated. Use of 1 of the 3 beta blockers proven to reduce mortality (i. e. , bisoprolol, carvedilol, and sustained release metoprolol succinate) is recommended for all stable patients with current or prior symptoms of HF and reduced LVEF, unless contraindicated. Angiotensin II receptor blockers are recommended in patients with current or prior symptoms of HF and reduced LVEF who are ACEI-intolerant. Drugs known to adversely affect the clinical status of patients with current or prior symptoms of HF and reduced LVEF should be avoided or withdrawn whenever possible (e. g. , nonsteroidal anti-inflammatory drugs, most antiarrhythmic drugs, and most calcium channel blocking drugs). Exercise training is beneficial as an adjunctive approach to improve clinical status in ambulatory patients with current or prior symptoms of HF and reduced LVEF.
Stage “C” HF (2) n n ACC/AHA 2009 Update An implantable cardioverter-defibrillator is recommended: n As secondary prevention to prolong survival in patients with current or prior symptoms of HF and reduced LVEF who have a history of cardiac arrest, ventricular fibrillation, or hemodynamically destabilizing ventricular tachycardia. n For primary prevention of sudden cardiac death to reduce total mortality in patients with non-ischemic dilated cardiomyopathy or ischemic heart disease at least 40 days post-MI, a LVEF less than or equal to 35%, and NYHA functional class II or III symptoms while receiving chronic optimal medical therapy, and who have reasonable expectation of survival with a good functional status for more than 1 year. Patients with LVEF of less than or equal to 35%, sinus rhythm, and NYHA functional class III ambulatory class IV symptoms despite recommended optimal medical therapy and who have cardiac dyssynchrony, which is currently defined as a QRS duration greater than or equal to 0. 12 seconds, should receive cardiac resynchronization therapy, with or without an ICD, unless contraindicated.
Stage “C” HF (3) n n ACC/AHA 2009 Update Addition of an aldosterone antagonist is recommended in selected patients with moderately severe to severe symptoms of HF and reduced LVEF who can be carefully monitored for preserved renal function and normal potassium concentration. n Creatinine should be 2. 5 mg per d. L or less in men or 2. 0 mg per d. L or less in women and potassium should be less than 5. 0 m. Eq per liter. n Under circumstances where monitoring for hyperkalemia or renal dysfunction is not anticipated to be feasible, the risks may outweigh the benefits of aldosterone antagonists. The combination of hydralazine and nitrates is recommended to improve outcomes for patients self-described as African-Americans, with moderatesevere symptoms on optimal therapy with ACEIs, beta blockers, and diuretics.
Stage “D” HF n n n ACC/AHA 2009 Update Meticulous identification and control of fluid retention is recommended in patients with refractory end-stage HF. Referral for cardiac transplantation in potentially eligible patients is recommended for patients with refractory end-stage HF. Referral of patients with refractory end-stage HF to a HF program with expertise in the management of refractory HF is useful. Options for end-of-life care should be discussed with the patient and family when severe symptoms in patients with refractory end-stage HF persist despite application of all recommended therapies. Patients with refractory end-stage HF and implantable defibrillators should receive information about the option to inactivate the defibrillator.
In hospital ACC/AHA 2009 Update Factors that may precipitate acute HF and hospitalization: n Noncompliance with medical regimen, sodium and/or fluid restriction n Acute myocardial ischemia n Ucorrected high blood pressure n Atrial fibrillation and other arrhythmias n Recent addition of negative inotropic drugs (e. g. , verapamil, nifedipine, diltiazem, beta blockers) n Pulmonary embolus n Nonsteroidal anti-inflammatory drugs n Excessive alcohol or illicit drug use n Endocrine abnormalities (e. g. , diabetes mellitus, hyperthyroidism, hypothyroidism) n Concurrent infections (e. g. , pneumonia, viral illnesses)
Hospital discharge. ACC/AHA 2009 Update Comprehensive written discharge instructions for all patients with a hospitalization for HF and their caregivers is strongly recommended, with special emphasis on the following 6 aspects of care: n Diet n Discharge medications, with a special focus on adherence, persistence, and uptitration to recommended doses of ACEI/ARB and beta-blocker medication n Activity level n Follow-up appointments n Daily weight monitoring n What to do if HF symptoms worsen
End of life issues n n n ACC/AHA 2009 Update Ongoing patient and family education regarding prognosis for functional capacity and survival is recommended for patients with HF at the end of life. Patient and family education about options formulating and implementing advance directives and the role of palliative and hospice care services with reevaluation for changing clinical status is recommended for patients with HF at the end of life. Discussion is recommended regarding the option of inactivating ICDs for patients with HF at the end of life. It is important to ensure continuity of medical care between inpatient and outpatient settings for patients with HF at the end of life. Components of hospice care that are appropriate to the relief of suffering, including opiates, are recommended and do not preclude the options for use of inotropes and intravenous diuretics for symptom palliation for patients with HF at the end of life. All professionals working with HF patients should examine current end-of-life processes and work toward improvement in approaches to palliation and end-oflife care.
V. Heart failure summary
Heart failure summary n ABC’s n n Assess Airway, Breathing and Circulation Oxygen, IV Access, Monitor Treat Overload (Furosemide, Morphine, NTG) or Hypotension (Norepinephrine, Dopamine) Diagnosis: n n n History: DOE, Orthopnea? Exam: JVD, AJ Reflux, Apical Pulse? EKG: LBBB, Q waves? CXR (Cardiomegally, Edema? ) Imaging? Echo or perfusion scanning Biochemical Testing (BNP? )
Heart failure summary n Staged Management: n n n Behavioral Risk Factor Reduction Control Htn, Lipids, DM Medications n n n Digoxin – symptom control Diuretics – symptom control ACEI’s – improve symptoms and mortality Beta-blockers – improve mortality Spironolactone – improves mortality in severe HF Regular followup is vital!
THANKS!
95a6daa18791a673d2d3dcafe4730559.ppt