9278b4792fdd1e6d2e058b94032e8d3a.ppt
- Количество слайдов: 46
 Healthcare Insurance Past , Present & Future 1
Healthcare Insurance Past , Present & Future 1
 “ It is not pieces of gold & silver but health that is the real wealth ” Mahatma Gandhi 2
“ It is not pieces of gold & silver but health that is the real wealth ” Mahatma Gandhi 2
 Economic growth is an indicator of a country’s well being and development • Empirical evidence suggests that a significant portion of economic growth is contributed by human capital – the elements of which are level of education and health of the people 3
Economic growth is an indicator of a country’s well being and development • Empirical evidence suggests that a significant portion of economic growth is contributed by human capital – the elements of which are level of education and health of the people 3
 Health Scenario in India • India with a population of 1. 2 billion possesses around 16. 6% of the global population and 20% of the global disease burden. • Health care expenditure in India is around 5% of GDPI as compared to 8. 4%in UK, 7. 5% IN Brazil In USA and Japan the Govt. spending on Health is around 80%. MORE THAN 70% OF HEALTHCARE EXPENDITURE IN INDIA TODAY IS MET OUT OF INDIVIDUALS’ POCKETS. • Given the implication that a healthy and productive population has on economic development, there is need to step up health care funding mechanism 4
Health Scenario in India • India with a population of 1. 2 billion possesses around 16. 6% of the global population and 20% of the global disease burden. • Health care expenditure in India is around 5% of GDPI as compared to 8. 4%in UK, 7. 5% IN Brazil In USA and Japan the Govt. spending on Health is around 80%. MORE THAN 70% OF HEALTHCARE EXPENDITURE IN INDIA TODAY IS MET OUT OF INDIVIDUALS’ POCKETS. • Given the implication that a healthy and productive population has on economic development, there is need to step up health care funding mechanism 4
 History of Health Insurance • Medical Insurance was first offered in the United States in 1850 and insured injuries arising from railroad and steamboat accidents. • In India the formal health insurance started with the ESIS (Employees State Insurance Scheme) under the ESIS Act 1948 and with the CGHS (Central Govt Health Scheme) 1954. • In 1981, a limited cover was devised for individuals and families. This was structured formally in 1986 when 4 subsidiaries of GIC launched the Mediclaim policy (HDH) both for individuals and Groups 5
History of Health Insurance • Medical Insurance was first offered in the United States in 1850 and insured injuries arising from railroad and steamboat accidents. • In India the formal health insurance started with the ESIS (Employees State Insurance Scheme) under the ESIS Act 1948 and with the CGHS (Central Govt Health Scheme) 1954. • In 1981, a limited cover was devised for individuals and families. This was structured formally in 1986 when 4 subsidiaries of GIC launched the Mediclaim policy (HDH) both for individuals and Groups 5
 Milestones for Mediclaim since 1986 : Changes introduced from 1991 • Removal of Sub limits • Introduction of Family Floater Concept • Critical Ilness Cover • Tailormade Policies for Corporates • Hike in Premium and Sum Insured 6
Milestones for Mediclaim since 1986 : Changes introduced from 1991 • Removal of Sub limits • Introduction of Family Floater Concept • Critical Ilness Cover • Tailormade Policies for Corporates • Hike in Premium and Sum Insured 6
 the next phase ( 2000 – 2005 ) Ø Opening up of the Insurance Sector Ø Introduction of TPAS Ø Govt Health Insurance Schemes 7
the next phase ( 2000 – 2005 ) Ø Opening up of the Insurance Sector Ø Introduction of TPAS Ø Govt Health Insurance Schemes 7
 Latest Trends - 2005 onwards A) PRODUCT MODIFICATION : - Three products for different age groups Family Package Cover Pre-existing Disease Cover Disease Specific Policy Senior Citizens Policy B) CO-BRANDED PRODUCTS WITH BANKS 8
Latest Trends - 2005 onwards A) PRODUCT MODIFICATION : - Three products for different age groups Family Package Cover Pre-existing Disease Cover Disease Specific Policy Senior Citizens Policy B) CO-BRANDED PRODUCTS WITH BANKS 8
 Latest Trends - 2005 onwards C) Stand Alone HEALTH INSURANCE COS. D) Life Insurance Companies providing Health Cover E) Govt Schemes : • • • - Weavers & Artisans Cover Universal Health Ins. Cover Rajiv Aarogyashri – AP Govt. Yeshasvini Scheme – Farmers in Karnataka Rashtriya Swasthya Bima Yojona ( RSBY) 9
Latest Trends - 2005 onwards C) Stand Alone HEALTH INSURANCE COS. D) Life Insurance Companies providing Health Cover E) Govt Schemes : • • • - Weavers & Artisans Cover Universal Health Ins. Cover Rajiv Aarogyashri – AP Govt. Yeshasvini Scheme – Farmers in Karnataka Rashtriya Swasthya Bima Yojona ( RSBY) 9
 Tax Benefits : As it stands today • Under Section 80 D, Premium upto Rs 15, 000 paid for Self + spouse + dependent children qualifies for Tax Benefit. (This amount is likely to be increased to Rs 50, 000 through DTC in 2012. ) • Additional premium paid upto Rs 15, 000/= for parents’ health insurance also qualifies and in case of Sr Citizens parents, premium paid upto Rs 20, 000 qualifies for tax deduction. • As per Section 80 DD a fixed total of Rs 50, 000 qualifies as deduction irrespective of amount incurred towards expenditure / investment for medical treatment of handicapped dependent and in case of severe disability this is increased to Rs 75, 000 • As per Section 80 DDB, deduction of upto Rs 40, 000 ( For Sr citizens Rs 60, 000/) is allowed for medical treatment of specified diseases certified by Govt hospitals. 10
Tax Benefits : As it stands today • Under Section 80 D, Premium upto Rs 15, 000 paid for Self + spouse + dependent children qualifies for Tax Benefit. (This amount is likely to be increased to Rs 50, 000 through DTC in 2012. ) • Additional premium paid upto Rs 15, 000/= for parents’ health insurance also qualifies and in case of Sr Citizens parents, premium paid upto Rs 20, 000 qualifies for tax deduction. • As per Section 80 DD a fixed total of Rs 50, 000 qualifies as deduction irrespective of amount incurred towards expenditure / investment for medical treatment of handicapped dependent and in case of severe disability this is increased to Rs 75, 000 • As per Section 80 DDB, deduction of upto Rs 40, 000 ( For Sr citizens Rs 60, 000/) is allowed for medical treatment of specified diseases certified by Govt hospitals. 10
 Health Insurance Claims settlement process: • Cashless : For availing cashless treatment (only at authorized network hospitals), the TPA has to be notified in advance (for planned hospitalization) or within the stipulated time limits (for emergencies). The claim amount needs to be approved by the TPA, and the hospital settles the amount with the TPA/ Insurer. Typically there will be exclusions and such amount will have to be settled directly at the hospital. • Reimbursement : Reimbursement facility can be availed at both the network and non-network hospitals. Here the insured avails the treatment and settles the hospital bills directly at the hospital • Self administered portfolio : Insured may opt to purchase Health Insurance policy without TPA in which case the settlement would be on reimbursement basis by the insuring Office concerned. 11
Health Insurance Claims settlement process: • Cashless : For availing cashless treatment (only at authorized network hospitals), the TPA has to be notified in advance (for planned hospitalization) or within the stipulated time limits (for emergencies). The claim amount needs to be approved by the TPA, and the hospital settles the amount with the TPA/ Insurer. Typically there will be exclusions and such amount will have to be settled directly at the hospital. • Reimbursement : Reimbursement facility can be availed at both the network and non-network hospitals. Here the insured avails the treatment and settles the hospital bills directly at the hospital • Self administered portfolio : Insured may opt to purchase Health Insurance policy without TPA in which case the settlement would be on reimbursement basis by the insuring Office concerned. 11
 Role of Third Party Administrator (TPA) • TPAs licensed by IRDA are the intermediary between Insured and Insurance Company and responsible for providing value added services to policy holders including all aspects of claim arising out of health insurance policies. • The work of the TPA starts once the Policy is issued. • TPAs have helped insurance companies provide better service to their policyholders through their efficiency in claim settlement. • There at present 29 IRDA registered TPAs • 12
Role of Third Party Administrator (TPA) • TPAs licensed by IRDA are the intermediary between Insured and Insurance Company and responsible for providing value added services to policy holders including all aspects of claim arising out of health insurance policies. • The work of the TPA starts once the Policy is issued. • TPAs have helped insurance companies provide better service to their policyholders through their efficiency in claim settlement. • There at present 29 IRDA registered TPAs • 12
 Functions of Third Party Administrator (TPA) 1) TPA issues ID cards to all their policyholders in order to validate their identity at the time of Claim. 2) In case of a claim, policyholder will have to inform TPA on their 24 hr toll free line . In case of a network hospital the TPA issues authorization letter to the hospital for admission of policyholder and also pays for treatment. At the time of discharge all the bills are sent to TPA for processing the claim. In case of Emergency hospitalization in a hospital outside the network, cashless facility cannot be extended and claim is reimbursed after submission of documents . 3) After making the payment to the hospital, the TPA sends all necessary • • documents of claims to insurance company and the Insurance company then reimburses TPA. . 13
Functions of Third Party Administrator (TPA) 1) TPA issues ID cards to all their policyholders in order to validate their identity at the time of Claim. 2) In case of a claim, policyholder will have to inform TPA on their 24 hr toll free line . In case of a network hospital the TPA issues authorization letter to the hospital for admission of policyholder and also pays for treatment. At the time of discharge all the bills are sent to TPA for processing the claim. In case of Emergency hospitalization in a hospital outside the network, cashless facility cannot be extended and claim is reimbursed after submission of documents . 3) After making the payment to the hospital, the TPA sends all necessary • • documents of claims to insurance company and the Insurance company then reimburses TPA. . 13
 The Preferred Provider Network (PPN) of hospitals is an initiative of the 4 Public Sector General Insurance Companies (PSGICs) taken in July 2010 to introduce • Discipline on the pricing of hospital services charges; • Pre-negotiated rates for medical procedures and • overall standardisation of hospital facilities. The Agreement is entered into with Hospitals which are then listed under the PPN Network. Presently the PPN Facility operates in Delhi, Mumbai, Chennai and Bangalore and will be extended to four more cities, viz. Hyderabad, Kolkata, Ahmedabad and Chandigarh from 1 July 2011. • • . • 14
The Preferred Provider Network (PPN) of hospitals is an initiative of the 4 Public Sector General Insurance Companies (PSGICs) taken in July 2010 to introduce • Discipline on the pricing of hospital services charges; • Pre-negotiated rates for medical procedures and • overall standardisation of hospital facilities. The Agreement is entered into with Hospitals which are then listed under the PPN Network. Presently the PPN Facility operates in Delhi, Mumbai, Chennai and Bangalore and will be extended to four more cities, viz. Hyderabad, Kolkata, Ahmedabad and Chandigarh from 1 July 2011. • • . • 14
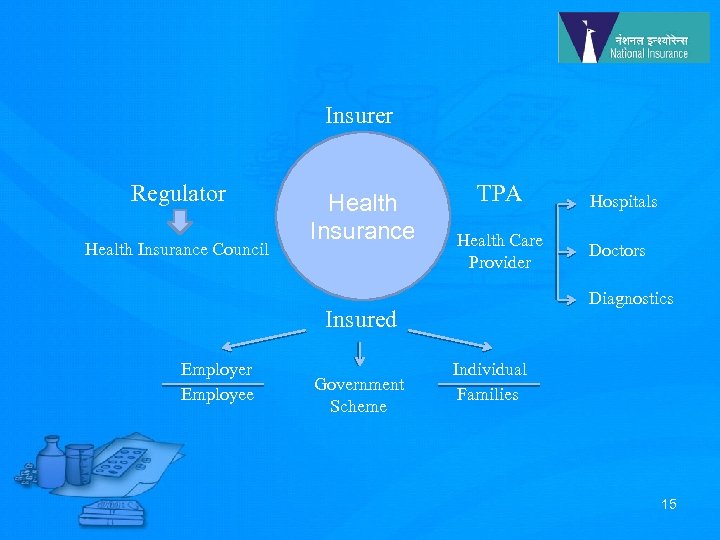 Insurer Regulator Health Insurance Council Health Insurance TPA Health Care Provider Government Scheme Doctors Diagnostics Insured Employer Employee Hospitals Individual Families 15
Insurer Regulator Health Insurance Council Health Insurance TPA Health Care Provider Government Scheme Doctors Diagnostics Insured Employer Employee Hospitals Individual Families 15
 Financing Health care: In India healthcare is financed through a combination of sources like : - 1) 2) 3) 4) 5) Household and Individual out of pocket payments Central & State Government tax revenue Mandatory Social & Voluntary Health Insurance like ESI, CGHS, Micro Insurance Other Employees / Mutual Schemes not using public or private Insurance companies 16
Financing Health care: In India healthcare is financed through a combination of sources like : - 1) 2) 3) 4) 5) Household and Individual out of pocket payments Central & State Government tax revenue Mandatory Social & Voluntary Health Insurance like ESI, CGHS, Micro Insurance Other Employees / Mutual Schemes not using public or private Insurance companies 16
 Necessity of Health Insurance: Life style diseases v Every one needs medical care. Of all the risks facing a household, health risk probably poses the greatest threat to lives & livelihoods. v Sedentary life style, hectic schedules, long working hours and eating habits are leading to silent diseases and causing rise in number of people suffering from obesity, diabetes and cardiovascular diseases. v As per Government of India Report 2006, the morbidity rate for males is 8. 3% (Rural) and 9. 1% (Urban) and for females 9. 3% (Rural) and 10. 8% (Urban). v 2. 5 million hospitalization in 2005 due to road accident. Projected 3 million by 2010 and 3. 5 million by 2015 – National Medical Journal 2008 17
Necessity of Health Insurance: Life style diseases v Every one needs medical care. Of all the risks facing a household, health risk probably poses the greatest threat to lives & livelihoods. v Sedentary life style, hectic schedules, long working hours and eating habits are leading to silent diseases and causing rise in number of people suffering from obesity, diabetes and cardiovascular diseases. v As per Government of India Report 2006, the morbidity rate for males is 8. 3% (Rural) and 9. 1% (Urban) and for females 9. 3% (Rural) and 10. 8% (Urban). v 2. 5 million hospitalization in 2005 due to road accident. Projected 3 million by 2010 and 3. 5 million by 2015 – National Medical Journal 2008 17
 Necessity of Health Insurance: Mediflation v High escalation in medical costs due to advancement & high tech intervention in health, diagnostic & therapeutic procedures, prescription drugs leading to Mediflation. v The explosion of knowledge in genetic engineering & Bio technology, Nanotechnology, Medical Informatics & Gene therapy will further escalate health care costs beyond the reach of most people in future. v Medical Tourism : As more and more patients from Europe, the US and other affluent nations with high medicare costs look for effective options, a blend of top-class medical expertise at attractive prices is helping a growing number of Indian corporate hospitals lure foreign patients. Costs would escalate for the Indian insured. 18
Necessity of Health Insurance: Mediflation v High escalation in medical costs due to advancement & high tech intervention in health, diagnostic & therapeutic procedures, prescription drugs leading to Mediflation. v The explosion of knowledge in genetic engineering & Bio technology, Nanotechnology, Medical Informatics & Gene therapy will further escalate health care costs beyond the reach of most people in future. v Medical Tourism : As more and more patients from Europe, the US and other affluent nations with high medicare costs look for effective options, a blend of top-class medical expertise at attractive prices is helping a growing number of Indian corporate hospitals lure foreign patients. Costs would escalate for the Indian insured. 18
 Necessity of Health Insurance: Mediflation • Expenses towards medical expenses is the second highest cause of rural indebtedness after agriculture. Major portion of the country’s poor (over 45%) had to borrow / sell assets to meet costs of care. • This huge out of pocket expenditure does not pass through any pooling mechanism and thus needs to be channeled through Health Insurance. 19
Necessity of Health Insurance: Mediflation • Expenses towards medical expenses is the second highest cause of rural indebtedness after agriculture. Major portion of the country’s poor (over 45%) had to borrow / sell assets to meet costs of care. • This huge out of pocket expenditure does not pass through any pooling mechanism and thus needs to be channeled through Health Insurance. 19
 Health Insurance Figures According to figures upto Feb 2011, the total health insurance premiums written by non-life companies and standalone health insurance companies grew by 22. 95 %. The health insurance market continues to be dominated by the four state -owned general insurers, which together accounted for almost 58. 39 per cent of the premiums. March 11 figures reveal that National Insurance Company, led the Health Portfolio pie with 1492 crores registering a sharp Growth of 46. 47 % cent this fiscal with an exceptional Accretion of 473 crores. ICICI Lombard, Bajaj Allianz General and HDFC ERGO are the top players amongst private non life insurers. 20
Health Insurance Figures According to figures upto Feb 2011, the total health insurance premiums written by non-life companies and standalone health insurance companies grew by 22. 95 %. The health insurance market continues to be dominated by the four state -owned general insurers, which together accounted for almost 58. 39 per cent of the premiums. March 11 figures reveal that National Insurance Company, led the Health Portfolio pie with 1492 crores registering a sharp Growth of 46. 47 % cent this fiscal with an exceptional Accretion of 473 crores. ICICI Lombard, Bajaj Allianz General and HDFC ERGO are the top players amongst private non life insurers. 20
 Rashtriya Bima Yojana Policy Health Insurance for the Poor • RSBY has been launched by Ministry of Labour and Employment, Govt of India to provide health insurance coverage for Below Poverty Line (BPL) families. • RSBY started rolling from 1 st April 2008. • The objective of RSBY is to provide protection to BPL households from financial liabilities arising out of health shocks that involve hospitalization. • Beneficiaries under RSBY are entitled to hospitalization coverage up to Rs. 30, 000/- for most of the diseases that require hospitalization. Government has even fixed the package rates for the hospitals for a large number of interventions. • Pre-existing conditions are covered from day one and there is no age limit. Coverage extends to five members of the family which includes the head of household, spouse and up to three dependents. • Beneficiaries need to pay only Rs. 30/- as registration fee while Central and State Government pays the premium to the insurer selected by the State Government on the basis of a competitive bidding. 21
Rashtriya Bima Yojana Policy Health Insurance for the Poor • RSBY has been launched by Ministry of Labour and Employment, Govt of India to provide health insurance coverage for Below Poverty Line (BPL) families. • RSBY started rolling from 1 st April 2008. • The objective of RSBY is to provide protection to BPL households from financial liabilities arising out of health shocks that involve hospitalization. • Beneficiaries under RSBY are entitled to hospitalization coverage up to Rs. 30, 000/- for most of the diseases that require hospitalization. Government has even fixed the package rates for the hospitals for a large number of interventions. • Pre-existing conditions are covered from day one and there is no age limit. Coverage extends to five members of the family which includes the head of household, spouse and up to three dependents. • Beneficiaries need to pay only Rs. 30/- as registration fee while Central and State Government pays the premium to the insurer selected by the State Government on the basis of a competitive bidding. 21
 Unique Features of RSBY • Empowering the Beneficiary : Freedom of choice to BPL Policy holder to choose hospitals and be treated as a significant provider of revenue • Business Model for all Stakeholders : Insurers/Hospitals/ Intermediaries/Govt. : Incentives have been built for all stakeholders . Conducive both in terms of expansion of the scheme as well as for its sustainability. • IT intensive : Every beneficiary family is issued a biometric enabled smart card containing their photographs and fingerprints. All hospitals empanelled under RSBY are IT Enabled and connected to the server at the district level. 22
Unique Features of RSBY • Empowering the Beneficiary : Freedom of choice to BPL Policy holder to choose hospitals and be treated as a significant provider of revenue • Business Model for all Stakeholders : Insurers/Hospitals/ Intermediaries/Govt. : Incentives have been built for all stakeholders . Conducive both in terms of expansion of the scheme as well as for its sustainability. • IT intensive : Every beneficiary family is issued a biometric enabled smart card containing their photographs and fingerprints. All hospitals empanelled under RSBY are IT Enabled and connected to the server at the district level. 22
 Unique Features of RSBY • Safe and Foolproof The use of the biometric cared and a key management system makes this scheme safe and foolproof. • Portability A beneficiary will be able to use his/her smart card in any RSBY empanelled hospital across India. This is of great help to migrant workers • Cashless and Paperless transaction No payment is to be made by the beneficiary and participating providers may send online claims to the insurer and get paid electronically. • Robust Monitoring and Evaluation: An elaborate data management system is being put in place which can track any transaction across India and provide periodic analytical reports. This should allow for mid course improvements in the Scheme. 23
Unique Features of RSBY • Safe and Foolproof The use of the biometric cared and a key management system makes this scheme safe and foolproof. • Portability A beneficiary will be able to use his/her smart card in any RSBY empanelled hospital across India. This is of great help to migrant workers • Cashless and Paperless transaction No payment is to be made by the beneficiary and participating providers may send online claims to the insurer and get paid electronically. • Robust Monitoring and Evaluation: An elaborate data management system is being put in place which can track any transaction across India and provide periodic analytical reports. This should allow for mid course improvements in the Scheme. 23
 Financing for RSBY • The majority of the financing, about 75 percent, is provided by the Government of India (GOI), while the remainder is paid by the respective state government. Government of India’s contribution is 90 percent in case of North-eastern states and Jammu and Kashmir and respective state Governments need to pay only 10% of the premium. • Beneficiaries need to pay only Rs. 30 as the registration fee. This amount shall be used for incurring administrative expenses under the scheme. 24
Financing for RSBY • The majority of the financing, about 75 percent, is provided by the Government of India (GOI), while the remainder is paid by the respective state government. Government of India’s contribution is 90 percent in case of North-eastern states and Jammu and Kashmir and respective state Governments need to pay only 10% of the premium. • Beneficiaries need to pay only Rs. 30 as the registration fee. This amount shall be used for incurring administrative expenses under the scheme. 24
 RSBY Facts • More than 376 districts in 29 states in India are covered under this scheme • There are 8096 private and public hospitals empanelled as Health Care Providers • As of April 2011 the number of Active smart cards issued is 2, 33, 46, 929. • National Insurance, Oriental Insurance and United India Insurance are the 3 major non life insurance players with ICICI leading the private non life insurer group. 25
RSBY Facts • More than 376 districts in 29 states in India are covered under this scheme • There are 8096 private and public hospitals empanelled as Health Care Providers • As of April 2011 the number of Active smart cards issued is 2, 33, 46, 929. • National Insurance, Oriental Insurance and United India Insurance are the 3 major non life insurance players with ICICI leading the private non life insurer group. 25
 Rising Claims Ratio : • RSBY, has been witnessing an increase in its Claim ratio. • Several states have reportedly exceeded 100 percent mark, a pointer to be concerned with future premium rate setting. The number of Hospitalisation cases reported as on April 11 is 16, 82, 391 • rate of hospitals is extremely low. 26
Rising Claims Ratio : • RSBY, has been witnessing an increase in its Claim ratio. • Several states have reportedly exceeded 100 percent mark, a pointer to be concerned with future premium rate setting. The number of Hospitalisation cases reported as on April 11 is 16, 82, 391 • rate of hospitals is extremely low. 26
 Health Insurance : Future Initiatives for Holistic Health care • Portability of Mediclaim in India w. e. f. 1 st July 2011. This is to ensure that a customer continues to enjoy benefits under the Health Policy even if he wishes to change his insurance provider. • Traditional Healthcare practices to be brought under Mediclaim fold. A panel has been set up by the General Insurance council to examine the merits of reccognizing Ayurveda, Unani, Siddha and Homeopathy forms of Healthcare. These alternative practices though recognised by GOI have yet to be brought under the Mediclaim list. • Clinical Establishment Registration and Regulation Act This law passed last year aims to regulate standards at private hospitals and check overcharging, unnecessary tests, negligence and other malpractices. Since health is a state subject the State Assemblies need to pass a resolution before the central law can apply in that State 27
Health Insurance : Future Initiatives for Holistic Health care • Portability of Mediclaim in India w. e. f. 1 st July 2011. This is to ensure that a customer continues to enjoy benefits under the Health Policy even if he wishes to change his insurance provider. • Traditional Healthcare practices to be brought under Mediclaim fold. A panel has been set up by the General Insurance council to examine the merits of reccognizing Ayurveda, Unani, Siddha and Homeopathy forms of Healthcare. These alternative practices though recognised by GOI have yet to be brought under the Mediclaim list. • Clinical Establishment Registration and Regulation Act This law passed last year aims to regulate standards at private hospitals and check overcharging, unnecessary tests, negligence and other malpractices. Since health is a state subject the State Assemblies need to pass a resolution before the central law can apply in that State 27
 Health Insurance : Future IRDA Initiatives IRDA is working on a set of comprehensive health insurance guidelines which would cover : • Standard Treatment Guidelines (‘STGs’) for common causes of hospitalisation like diarrhoea, asthma, cataract surgery and typhoid. FICCI has recommended 22 STGs to the regulator. • A list of items as part of common exclusions under non-medical expenses may include costs for diabetic chart, external durable devices like walking aids and cervical collar, eye kits and X-ray films. • Standard definitions of 11 critical illnesses such as cancer, first heart attack, open heart replacement and major organ/bone marrow transplant. Insurers would be required to cover these under their critical illness plans. • A common form for claim settlement including claim settlement protocol. 28
Health Insurance : Future IRDA Initiatives IRDA is working on a set of comprehensive health insurance guidelines which would cover : • Standard Treatment Guidelines (‘STGs’) for common causes of hospitalisation like diarrhoea, asthma, cataract surgery and typhoid. FICCI has recommended 22 STGs to the regulator. • A list of items as part of common exclusions under non-medical expenses may include costs for diabetic chart, external durable devices like walking aids and cervical collar, eye kits and X-ray films. • Standard definitions of 11 critical illnesses such as cancer, first heart attack, open heart replacement and major organ/bone marrow transplant. Insurers would be required to cover these under their critical illness plans. • A common form for claim settlement including claim settlement protocol. 28
 Health Insurance : Future IRDA Initiatives Health Insurance Councils : • IRDA is working on setting up of Health Councils through provision of Section 14(f) of the IRDA Act. • This proposed common health body is envisaged to help in ensuring harmonized growth of business and also in reducing differences arising between stakeholders like TPAs , Insurers, Hospitals and the public. • In addition to other functions, the council will also set up mechanisms to enforce strict vigilance on attempts to defraud the insurance system and take effective and concrete action thereupon. 29
Health Insurance : Future IRDA Initiatives Health Insurance Councils : • IRDA is working on setting up of Health Councils through provision of Section 14(f) of the IRDA Act. • This proposed common health body is envisaged to help in ensuring harmonized growth of business and also in reducing differences arising between stakeholders like TPAs , Insurers, Hospitals and the public. • In addition to other functions, the council will also set up mechanisms to enforce strict vigilance on attempts to defraud the insurance system and take effective and concrete action thereupon. 29
 Health Insurance : Future Govt. Initiatives • The National Aids Control Organisation (NACO) has pressed for inclusive and universal healthcare for people living with HIV+. The Karnataka government has launched a health insurance scheme to benefit about 12, 000 HIV -positive children in collaboration with Star Health. • The Government is actively considering the scope for a public-funded health insurance scheme covering all citizens as part of the 12 th Five Year Plan, with premium rates linked to the beneficiary’s income levels. The ambitious scheme is planned to cover both hospitalisation expenses and treatment expenses at listed hospitals. 30
Health Insurance : Future Govt. Initiatives • The National Aids Control Organisation (NACO) has pressed for inclusive and universal healthcare for people living with HIV+. The Karnataka government has launched a health insurance scheme to benefit about 12, 000 HIV -positive children in collaboration with Star Health. • The Government is actively considering the scope for a public-funded health insurance scheme covering all citizens as part of the 12 th Five Year Plan, with premium rates linked to the beneficiary’s income levels. The ambitious scheme is planned to cover both hospitalisation expenses and treatment expenses at listed hospitals. 30
 Health Insurance : Future Govt. Initiatives • The Employees' State Insurance Corporation (ESIC), which provides health insurance to all workers whose monthly gross pay is up to Rs 15, 000, is gearing to improve its services. • All the beneficiaries will soon be issued a smart card to avail treatment at any ESI hospital or affiliated healthcare provider across the country. • The initiative, spearheaded with the help of the software company, Wipro, is to inter connect the 2, 200 ESI institutions across the country and launch an online portal. 31
Health Insurance : Future Govt. Initiatives • The Employees' State Insurance Corporation (ESIC), which provides health insurance to all workers whose monthly gross pay is up to Rs 15, 000, is gearing to improve its services. • All the beneficiaries will soon be issued a smart card to avail treatment at any ESI hospital or affiliated healthcare provider across the country. • The initiative, spearheaded with the help of the software company, Wipro, is to inter connect the 2, 200 ESI institutions across the country and launch an online portal. 31
 Health Insurance : Future Corporate Health Care Plans Preventive Health Care : Wellness initiatives. • The goal of these programmes is to make the workplace environment healthier, to improve the health of individual employees , to reduce healthcare costs and increase employee value. As part of the healthcare policy, organizations offer various benefits including Health insurances, mental health counselling , physical health camps, wellness camps etc Corporate Health Check Ups : • Earlier confined only to MNc or those industries with Health hazards such as paints, pesticides or manufacturing companies, today there is an increase in Corporate sponsored Health testing. Some employers make this annual check up compulsory for all above 40 as commonly hypertension, diabetes and deranged lipid profiles have begun to be diagnosed 32
Health Insurance : Future Corporate Health Care Plans Preventive Health Care : Wellness initiatives. • The goal of these programmes is to make the workplace environment healthier, to improve the health of individual employees , to reduce healthcare costs and increase employee value. As part of the healthcare policy, organizations offer various benefits including Health insurances, mental health counselling , physical health camps, wellness camps etc Corporate Health Check Ups : • Earlier confined only to MNc or those industries with Health hazards such as paints, pesticides or manufacturing companies, today there is an increase in Corporate sponsored Health testing. Some employers make this annual check up compulsory for all above 40 as commonly hypertension, diabetes and deranged lipid profiles have begun to be diagnosed 32
 Health Insurance : Future Scope for Employment in Health Care related Industry Considering that only 10% of the India population of more than 1 billion is insured under Health policies, the arena of Healthcare offers a large universe for employment • Specialisation in subjects like Hospital Administration, Risk Management, Actuarial Sciences will be the need of the day. • Insurance Companies, Health Specialists, Health Tourism centres, TPAs , Hospitals will be the potential employers. 33
Health Insurance : Future Scope for Employment in Health Care related Industry Considering that only 10% of the India population of more than 1 billion is insured under Health policies, the arena of Healthcare offers a large universe for employment • Specialisation in subjects like Hospital Administration, Risk Management, Actuarial Sciences will be the need of the day. • Insurance Companies, Health Specialists, Health Tourism centres, TPAs , Hospitals will be the potential employers. 33
 Mediclaim : its shortcomings • Mediclaim, the traditional health insurance product accounting for more than 80% of total health insurance market in India, is short-term in nature and covers only inpatient costs. More than 70% of the total health spend ( Rs. 1700 crores – WHO-2007 estimates) is for outpatient cost and there are very few, products to cover these costs in India today. • Further, Mediclaim falls under the category of ‘protection’ products where there is no payment from the insurer if no claim is made. Many Indian people see less value in protection products like Mediclaim as compared to savings products like endowment policies. • There is need for long term health products to enable customers to provide for their health and long-term care costs, particularly after retirement 34
Mediclaim : its shortcomings • Mediclaim, the traditional health insurance product accounting for more than 80% of total health insurance market in India, is short-term in nature and covers only inpatient costs. More than 70% of the total health spend ( Rs. 1700 crores – WHO-2007 estimates) is for outpatient cost and there are very few, products to cover these costs in India today. • Further, Mediclaim falls under the category of ‘protection’ products where there is no payment from the insurer if no claim is made. Many Indian people see less value in protection products like Mediclaim as compared to savings products like endowment policies. • There is need for long term health products to enable customers to provide for their health and long-term care costs, particularly after retirement 34
 Health Insurance : Way Forward • Global experience both in highly industrialised countries as well as in low and middle income economies clearly demonstrate the importance of achieving universal coverage through either a purely tax based regime or social health mechanism or both. • Medical savings accounts or Health Savings Accounts : Much like Pension Funds, Health Savings accounts have been successful adapted in Singapore, USA, China and South Africa where the Govt. Extends tax concessions for savings on this account. 35
Health Insurance : Way Forward • Global experience both in highly industrialised countries as well as in low and middle income economies clearly demonstrate the importance of achieving universal coverage through either a purely tax based regime or social health mechanism or both. • Medical savings accounts or Health Savings Accounts : Much like Pension Funds, Health Savings accounts have been successful adapted in Singapore, USA, China and South Africa where the Govt. Extends tax concessions for savings on this account. 35
 Health Insurance : Way Forward ? • • • Health Savings Account Issues and applicability An HSA is a tax exempt savings account similar to an Individual pension account but earmarked for medical expenses. Deposits in the account are tax exempt and can be easily withdrawn to pay for routine medical bills. HSA works in conjunction with a special High deductible health insurance policy resulting in the provision of comprehensive health insurance coverage at the lowest possible net cost Health Savings Account, enables an insured to save his money, which he may use to meet the expenses when he falls sick. USA, China, Singapore and South Africa have adopted the HSA model for their citizens. 36
Health Insurance : Way Forward ? • • • Health Savings Account Issues and applicability An HSA is a tax exempt savings account similar to an Individual pension account but earmarked for medical expenses. Deposits in the account are tax exempt and can be easily withdrawn to pay for routine medical bills. HSA works in conjunction with a special High deductible health insurance policy resulting in the provision of comprehensive health insurance coverage at the lowest possible net cost Health Savings Account, enables an insured to save his money, which he may use to meet the expenses when he falls sick. USA, China, Singapore and South Africa have adopted the HSA model for their citizens. 36
 Utilization of funds in an HSA The balance in health savings accounts may only be used to pay medical expenses at any time during the account holders’ lifetime such as : • Medicines and drugs • Diagnostic expenses • Dental expenses • Co-pays or deductibles as part of the medical insurance cover • Other miscellaneous medical expenses not covered under medical insurance like medical cost for pre-existing diseases, maternity related expenses. • Specialist consultations fees • Long-term care expenses 37
Utilization of funds in an HSA The balance in health savings accounts may only be used to pay medical expenses at any time during the account holders’ lifetime such as : • Medicines and drugs • Diagnostic expenses • Dental expenses • Co-pays or deductibles as part of the medical insurance cover • Other miscellaneous medical expenses not covered under medical insurance like medical cost for pre-existing diseases, maternity related expenses. • Specialist consultations fees • Long-term care expenses 37
 HSA – The Indian Context • ‘Bhavishya Arogya’ was the first HSA type product introduced in the Indian market in 1990. The coverage under the policy was similar to Mediclaim, i. e. hospitalisation benefits, but with the difference that the utilisation of benefits was deferred up to the retirement age ( vesting age) between 55 and 60 years. • Introduction of HAS in the Indian market will help deepen health insurance penetration. • HSAs with ensuing tax benefits are likely to encourage people to start saving early for their old age health expenses since they would have an incentive to accumulate HSA balances. An early entry into the health insurance system would help address the systemic and contentious issue of pre-existing condition exclusions. • 38
HSA – The Indian Context • ‘Bhavishya Arogya’ was the first HSA type product introduced in the Indian market in 1990. The coverage under the policy was similar to Mediclaim, i. e. hospitalisation benefits, but with the difference that the utilisation of benefits was deferred up to the retirement age ( vesting age) between 55 and 60 years. • Introduction of HAS in the Indian market will help deepen health insurance penetration. • HSAs with ensuing tax benefits are likely to encourage people to start saving early for their old age health expenses since they would have an incentive to accumulate HSA balances. An early entry into the health insurance system would help address the systemic and contentious issue of pre-existing condition exclusions. • 38
 HSA – The Indian Context • Rationalizing and reducing healthcare expenses : With HSA providing greater discretion to individuals on their total healthcare spending, it is expected that patients would seek greater transparency and efficiency in the medical services accorded to them by healthcare providers eventually rationalizing and reducing healthcare expenses. • HSAs would provide greater emphasis to the insurance industry towards reviewing the need for providing high risk, catastrophic policies which will encourage individuals to self-insure for routine medical care. The corresponding reduction in premium costs would allow more individuals, households and employers to purchase health insurance, thus deepening health insurance penetration. 39
HSA – The Indian Context • Rationalizing and reducing healthcare expenses : With HSA providing greater discretion to individuals on their total healthcare spending, it is expected that patients would seek greater transparency and efficiency in the medical services accorded to them by healthcare providers eventually rationalizing and reducing healthcare expenses. • HSAs would provide greater emphasis to the insurance industry towards reviewing the need for providing high risk, catastrophic policies which will encourage individuals to self-insure for routine medical care. The corresponding reduction in premium costs would allow more individuals, households and employers to purchase health insurance, thus deepening health insurance penetration. 39
 HSA – The Indian Context • Learning from the Singapore and China model of HSA suggests that controlling healthcare demand should be achieved simultaneously with Government initiatives to implement health sector reforms. The reforms should include : • development of standard treatment guidelines (STGs), • accreditation of different layers of healthcare providers, • adoption of DRG (Diagnosis Related Group) and ICD (International Classification of Diseases) coding and quite importantly, • the revival of the Indian Medical Council of its original charter for enforcing ethics and professionalism in the medical profession. 40
HSA – The Indian Context • Learning from the Singapore and China model of HSA suggests that controlling healthcare demand should be achieved simultaneously with Government initiatives to implement health sector reforms. The reforms should include : • development of standard treatment guidelines (STGs), • accreditation of different layers of healthcare providers, • adoption of DRG (Diagnosis Related Group) and ICD (International Classification of Diseases) coding and quite importantly, • the revival of the Indian Medical Council of its original charter for enforcing ethics and professionalism in the medical profession. 40
 Challenges which hinder Growth of Health care services in India : • Low awareness of health insurance • Affordability • Lack of standardization of healthcare providers and Proper data for informed decisions • Limited understanding of the features of policy. • Consumers skeptical about tedious claim administration. • High loss ratio of health insurance particularly group 41
Challenges which hinder Growth of Health care services in India : • Low awareness of health insurance • Affordability • Lack of standardization of healthcare providers and Proper data for informed decisions • Limited understanding of the features of policy. • Consumers skeptical about tedious claim administration. • High loss ratio of health insurance particularly group 41
 Ushering in Change v Increasing consumer awareness v Standardization and accredition of health care providers v Enhancement of health care infrastructure v Building of Health Insurance repository 42
Ushering in Change v Increasing consumer awareness v Standardization and accredition of health care providers v Enhancement of health care infrastructure v Building of Health Insurance repository 42
 Enablers of growth v Technology v Innovation around products v Pricing & Channels of Distribution v Positive contribution of the Key stakeholders - Govt. , IRDA, Insurers, Healthcare Providers, Distribution channels, Health Centers, Media. 43
Enablers of growth v Technology v Innovation around products v Pricing & Channels of Distribution v Positive contribution of the Key stakeholders - Govt. , IRDA, Insurers, Healthcare Providers, Distribution channels, Health Centers, Media. 43
 IN CONCLUSION India has a great opportunity to spearhead a viable and competitive health insurance sector and encourage the development of a sound high quality health delivery system. What is required is a good understanding of the actuarial and other risks in the business , a long term vision for those entering it, simple product design , supportive regulation and sustained customer education. 44
IN CONCLUSION India has a great opportunity to spearhead a viable and competitive health insurance sector and encourage the development of a sound high quality health delivery system. What is required is a good understanding of the actuarial and other risks in the business , a long term vision for those entering it, simple product design , supportive regulation and sustained customer education. 44
 An Arab proverb says “ He who has health has hope. And he who has hope, has every thing” We say “ He who has a Health policy has hope. And he who has hope has every thing” 45
An Arab proverb says “ He who has health has hope. And he who has hope, has every thing” We say “ He who has a Health policy has hope. And he who has hope has every thing” 45
 THANK YOU 46
THANK YOU 46


