08d9acc7486e265162ba4ee03a934ff4.ppt
- Количество слайдов: 69
Health Tech Prep Mosby’s Textbook for Nursing Assistants Chapter 24 Nutrition
Objectives Ø Ø Ø Ø Ø Define the key terms listed in this chapter Explain the purpose and use of the Food Guide Pyramid Explain how to use the Dietary Guidelines for Americans Describe the functions and major sources of nutrients Explain how to use food labels Explain the purpose of intake and output records Identify what is counted as fluid intake Explain how to assist with food and fluid needs Explain how to assist with calorie counts Ø Ø Ø Ø Describe factors that affect eating and nutrition Describe the special diets and between-meal nourishments Identify the signs, symptoms, and precautions relating to regurgitation and aspiration Describe fluid requirements and the causes of dehydration Explain what to do when the person has special fluid orders Describe the purpose, methods, and comfort measures for enteral nutrition and IV therapy Perform the procedures described in this chapter
BASIC NUTRITION Ø poor diet and poor eating habits: • Increase the risk of infection • Increase the risk for acute and chronic diseases • Cause chronic illnesses to become worse • Cause healing problems • Affect physical and mental function increasing risk for accidents and injuries
APPLICATION#1 FOOD DIARY Students will keep a food diary of their intake for 24 hrs and bring to class. While discussing the food guide pyramid students will try to put the foods that they have eaten in the food guide pyramid and determine if they have been provided with the daily value of nutrients and servings for the day.
BASIC NUTRITION Ø Nutrition • processes involved in the ingestion, digestion, absorption, and use of foods and fluids by the body. • needed for growth, healing, and body functions. Ø A well-balanced diet and correct calorie intake are necessary Ø A well-balanced diet has servings from levels 1, 2, and 3 of the Food Guide Pyramid. Ø The amount of energy that a nutrient provides is measured in calories. Ø calorie =amount of energy produced when the body burns food. • 1 gram of fat— 9 calories • 1 gram of protein— 4 calories • 1 gram of carbohydrate— 4 calories
BASIC NUTRITION Ø Nutrients • =a substance that is ingested, digested, absorbed, and used by the body • • • Carbohydrate Protein Fats Vitamins minerals
Nutrients Ø Protein • the most important nutrient. • needed for tissue growth and repair. • Sources of protein • Meat • Fish • Poultry • Eggs • Milk and milk products • Cereals • beans, peas, and nuts.
Nutrients Ø Carbohydrates • Provide energy and fiber for bowel elimination • found in fruits • Vegetables • Breads • Cereals • sugar Ø The fiber in fruits, vegetables, breads, and cereals provides the bulky part of chyme for elimination.
Nutrients Ø Fats • Fats provide energy • add flavor • help the body use certain vitamins. Ø Sources of fat include • Meats • Lard • Butter • shortening, oils, • Milk • Cheese • egg yolks • nuts. Ø Fat the body does not use is stored as adipose tissue.
Nutrients Ø Vitamins • Vitamins are needed for certain body functions. • Vitamins do not provide calories. Ø vitamins A, D, E, and K are stored by the body Ø Vitamin C and the B-complex vitamins are not stored. • These vitamins must be ingested daily. Ø ***Table 23 -1 in the textbook lists the sources/ major functions of vitamins.
Nutrients Ø Minerals • needed for: • (1) Bone and tooth formation • (2) Nerve and muscle function • (3) Fluid balance • (4) Other body processes Ø ***Table 23 -2 in the textbook lists the major functions and dietary sources
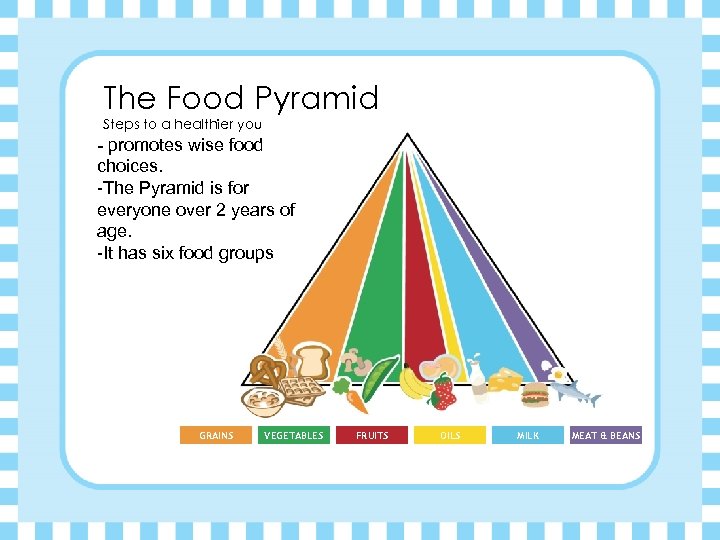
The Food Pyramid Steps to a healthier you - promotes wise food choices. -The Pyramid is for everyone over 2 years of age. -It has six food groups GRAINS VEGETABLES FRUITS OILS MILK MEAT & BEANS
Grains Make half of your grains whole Ø 6 to 11 servings are allowed a day. Ø See Box 23 -3 in the textbook. Ø provides • Protein • Carbohydrates • iron, thiamin, niacin, and riboflavin. • fats and sugars are small.
Vegetables Vary your veggies Ø 3 to 5 servings a day. • See Box 23 -3 in the textbook. Ø Fiber Ø vitamins A and C Ø Carbohydrates Ø minerals. Ø low in fat. Ø **Vegetables can become high in fat from food preparation
Fruits Focus on fruits Ø 2 to 4 fruit servings a day. • See Box 23 -3 in the textbook. Ø contains some sugar and is low in fat. Ø Carbohydrates Ø vitamins A and C Ø potassium, and other minerals
Oils Know your fats Ø Fats, oils, and sweets Ø used sparingly and as little as possible. • high in calories • Nutrients are few Ø Use food labels to find the fat content of foods.
Milk Get your calcium rich foods Ø Included • Milk • Skim milk has less fat than whole milk • Yogurt • Cheese • Ice cream (although higher in fat content) Ø See Box 23 -3 in the textbook. Ø 2 -3 servings per day Ø high in protein, carbohydrates, fat, calcium, and riboflavin.
Meat and Beans Go lean on protein Ø 2 to 3 servings a day. Ø See Box 23 -3 in the textbook. Ø high in protein, fat, iron, and thiamin. Ø Serving size is important. ** Culture, appetite, personal choice, and recipe affect serving size. Ø Nuts and peanut butter have the most fat in this group Ø lowest peas and cooked dry beans
THE GOAL=Better health Follow the Dietary Guidelines for Americans to reduce the risk for many diseases (See Box 23 -2 in the textbook. )
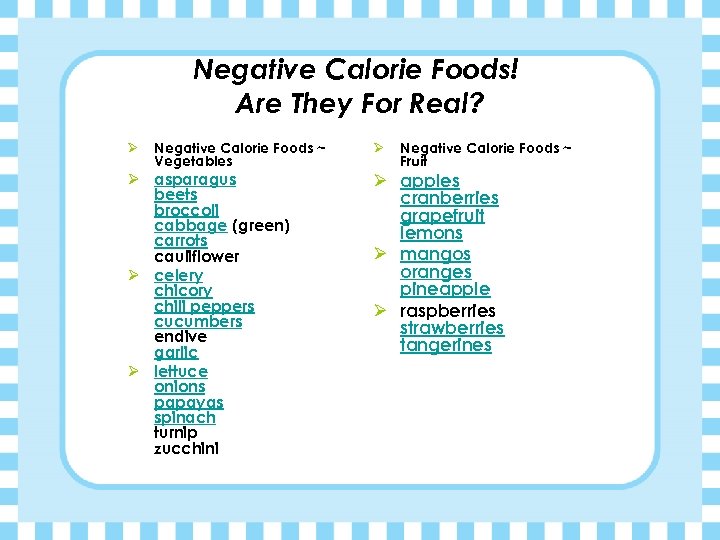
Negative Calorie Foods! Are They For Real? Ø Negative Calorie Foods ~ Vegetables Ø asparagus beets broccoli cabbage (green) carrots cauliflower Ø celery chicory chili peppers cucumbers endive garlic Ø lettuce onions papayas spinach turnip zucchini Ø Negative Calorie Foods ~ Fruit Ø apples cranberries grapefruit lemons Ø mangos oranges pineapple Ø raspberries strawberries tangerines
APPLICATION #2: Menu Planning Plan a nutritious, well-balanced menu for 1 day using the Food Guide Pyramid. Menus should include three meals and two snacks and equal approximately 2000 calories. APPLICATION #3: Food Guide Pyramid Worksheet Food Guide Pyramid Internet
Food labels Ø Figure 23 -5 in the textbook Ø Food labels are used to plan diets. Ø contain the following; • Serving size • How the serving fits into the daily diet • Calories per serving and number of calories from fat • The total amount of fat and the amount of saturated fat • Amount of cholesterol, sodium, and protein • Total amount of carbohydrates • Amount of vitamin A and C, calcium, and iron

Food labels Ø Daily Value(DV). = How a serving fits into the daily diet Ø expressed in a percentage based on a daily diet of 2000 calories. Ø Daily Reference Values (DRVs)= maximum daily intake values for total Ø fat, saturated fat, cholesterol, sodium, carbohydrate, and dietary fiber.
APPLICATION FOOD LABEL ACTIVITY
FACTORS AFFECTING EATING AND NUTRITION Ø Age • children: factors affecting eating and nutrition • Infants are breast-fed or bottle-fed. (1) For bottle-fed babies, the doctor orders the formula to use. • Solid foods are introduced at 4 to 6 months. (1) The nurse tells you what foods the infant can have.
FACTORS AFFECTING EATING AND NUTRITION Ø Culture • influences dietary practices, food choices, and food preparation. Ø Religion • Selecting, preparing, and eating food often involve religious practices. Ø See Box 23 -4 in the textbook.
FACTORS AFFECTING EATING AND NUTRITION Ø Finances • People with limited incomes often buy the cheaper carbohydrate foods. Ø Appetite • the desire for food. • Aromas and thoughts of food can stimulate the appetite. • Loss of appetite (anorexia) can occur from • illness • drugs • anxiety • pain • depression • unpleasant sights, thoughts, and smells.
FACTORS AFFECTING EATING AND NUTRITION Ø Personal choice • Food likes and dislikes are personal. • Foods served in the home influence food preferences. • People usually avoid foods that cause allergic reactions, nausea, vomiting, diarrhea, indigestion, or headaches.
FACTORS AFFECTING EATING AND NUTRITION Ø Illness • Appetite usually decreases during illness and recovery from injuries. • Nutritional needs increase to fight infection, heal tissue, and replace lost blood cells. • Nutrients lost through vomiting and diarrhea need replacement. • A sore mouth, tooth loss, or poorly fitting dentures affect chewing. • Illness can affect the ability to prepare and serve meals.
FACTORS AFFECTING EATING AND NUTRITION Ø Focus on home care: factors affecting eating and nutrition Ø You may be assigned to shop for groceries, plan meals, and cook. (1) Understand the Food Guide Pyramid, basic nutrition, and food labels (2) Know food preferences and eating habits (3) Review those that are allowed on the person’s diet (4) Consider eating and digestive problems (5) Plan menus for a full week. (6) Save grocery receipts for the person or family member. (7) Properly store foods.
FACTORS AFFECTING EATING AND NUTRITION Ø **Focus on long-term care: factors affecting eating and nutrition Ø OBRA has the following requirements for food served in longt erm care centers: Ø The person’s diet: • Is well balanced, nourishing and tastes good • Food is appetizing and attractive • Hot food is served hot; cold food is served cold. • Food is served promptly. • Food is prepared to meet each person’s needs. • Each person receives at least three meals a day. • The center provides any special eating equipment and utensils. Ø -Some centers have areas where the resident can dine with a spouse, family
SPECIAL DIETS Ø Doctors may order special diets: 1. For a nutritional deficiency or a disease 2. For weight control 3. To eliminate or decrease certain substances in the diet Ø The doctor, nurses, and dietitian work together to meet the person’s nutritional needs.
SPECIAL DIETS-Regular Ø Regular diet, general diet • no dietary limits or restrictions Ø Special diets may be needed • Person’s with certain diseases • Wound healing • Elimination • Swallowing problems • Allergies, excess weight, and other problems
SPECIAL DIETS-Sodium controlled Ø Diseases that require this type • Heart • Liver • kidney disease • hypertension Ø Sodium causes the body to retain water. Ø Less water reduces the heart’s workload.
SPECIAL DIETS-Regular Ø See Box 23 -5 in the textbook. Ø 2000 to 3000 mg sodium diet • Also called: low-salt or no added- salt diet • Sodium control is mild. • All high-sodium foods are omitted • A small amount of salt is used in cooking. • Salt is not added to foods at the table. Ø 1000 mg sodium diet • Food is cooked without salt. • Foods high in sodium are omitted. • Vegetables high in sodium are restricted in amount. • Salt-free products are used. • Diet planning is necessary.
SPECIAL DIETS-Diabetic Ø for people with diabetes. Ø involves: • The person’s food preferences • Limiting amounts or changing the way food is prepared • The same amount of carbohydrates, protein, and fat are eaten each day. • Eating meals and snacks at regular times • Meal and snack times are the same from day to day. Ø The nurse will tell you what to give the person for a snack. ***The amount of insulin given depends on daily food intake. Tell the nurse about changes in the person’s eating habits. ***
SPECIAL DIETS-Dysphagia Ø Dysphagia=difficulty swallowing • A slow swallow =difficulty getting enough food and fluids for good nutrition • unsafe swallow= food enters the airway could cause aspiration Ø Food thickness is changed to meet the person’s needs Ø Diet is determined by the health team • MD, nurse, SLP, OT
SPECIAL DIETS-Dysphagia Ø safety: • Know the signs and symptoms of dysphagia. • See Box 23 -7 in the textbook. • Position the person’s head and neck correctly. • Follow the care plan. • Feed the person according to the care plan. • Follow aspiration precautions. • See Box 23 -8 in the textbook.
FLUID BALANCE Ø Water is needed to live. Ø Death can result from too much or too little water. . Ø Normal fluid requirements • adult needs 1500 ml of water daily to survive. • 2000 to 2500 ml of fluid per day are needed for normal fluid balance. Ø Water requirements increase • hot weather • exercise • fever • illness • excess fluid loss.
FLUID BALANCE Ø The amount of fluid taken in (intake) and the amount lost (output) must be equal. Ø Edema • If fluid intake exceeds fluid output • tissues swell with water. Ø Dehydration • decrease in the amount of water in body tissues. • Fluid output exceeds intake.
FLUID BALANCE Ø ** Focus on children: normal fluid requirements • requirements vary with age. • Infants and young children need more fluids than adults. • Excess fluid losses quickly cause death in an infant or child.
FLUID BALANCE Ø ** Focus on older persons: normal fluid requirements • The amount of body water decreases with age. • diseases affect fluid balance. • drugs cause the body to lose fluids; others cause the body to retain water. • increased risk for dehydration and edema.
FLUID BALANCE -Special orders Ø Found in the care plan Ø Will give specific instructions on what to give the resident • Encourage fluids • drinks an increased amount of fluid. • Intake records are kept. • given a variety of fluids. • kept within the person’s reach. • correct temperature. • Fluids are offered regularly to persons who cannot feed themselves.
FLUID BALANCE-Restrict fluids Ø restricted to a certain amount. • offered in small amounts and in small containers. • water pitcher is removed from the room or kept out of sight. • Intake records are kept. • The person needs frequent oral hygiene.
FLUID BALANCE-NPO Ø The person cannot eat or drink anything. Ø NPO is often ordered: • Before and after surgery • Before some laboratory tests and diagnostic procedures • In treating certain illnesses Ø An NPO sign is posted above the bed. Ø The water pitcher and glass are removed. Ø Frequent oral hygiene is needed. Ø Fluids are not swallowed.
FLUID BALANCE Ø Intake and output (I&O) records Ø order by MD for I&O measurements. Ø I&O records are used: • To evaluate fluid balance and kidney function • To help in evaluating and planning medical treatment • When the person has special fluid orders
FLUID BALANCE-Intake and Output Ø Intake • fluids taken by mouth. • IV fluids • tubefeedings. Ø Output • urine • vomitus • diarrhea • wound drainage.
FLUID BALANCE-Measuring I&O Ø #measured in milliliters (ml) or in cubic centimeters(cc). • 1 ounce equals 30 ml • A pint is about 500 ml • A quart is about 1000 ml • the serving size of the bowls, dishes, cups, pitchers, glasses, and other containers.
FLUID BALANCE Ø A container called a graduate is used to measure fluids. Ø -Plastic urinals and emesis basins often have amount marks. Ø -An I&O record is kept at the bedside. Ø - Amounts are totaled at the end of the shift and recorded in the person’s chart. Ø -Remind the person: Ø # Not to urinate in the toilet Ø # Not to put toilet tissue into the receptacle
ØAPPLICATION #5: Determining intake and output
MEETING FOOD AND FLUIDS NEEDS Ø factors affect appetite and the ability to eat: Ø Weakness and illness Ø Unpleasant odors, sights, and sounds Ø Uncomfortable positions Ø The need for oral hygiene Ø The need to eliminate Ø Pain
Preparing for meals Ø -Patients and residents need: • To eliminate and have oral care • Dentures, eyeglasses, and hearing aids in place • To be clean and dry (if incontinent) • To be in a comfortable position for eating • A setting that is free of unpleasant sights, sounds and odors • Remove unpleasant equipment from the room.
Preparing the Person for Meals Ø Serving meal trays • Food is served in containers that keep foods at the correcttemperature. • You serve meal trays after preparing persons for meals. • If a meal tray is not served within 15 minutes, recheck food temperature. • If the food is not at the right temperature, get another tray. • Some agencies allow reheating in a microwave oven.
Feeding the person Ø Factors affecting the ability to feed oneself • Weakness • Paralysis • casts • other physical limits /illnesses
Rules and guidelines for feeding Ø Ø Serve food and fluids in the order the person prefers. Offer fluids during the meal. use Spoons= less likely to cause injury. respect the person • Are often angry, humiliated, and embarrassed • May be depressed, resentful, or refuse to eat • Let them do as much as possible. • Provide support and encouragement.
Rules and guidelines for feeding Ø Ø Allow time and privacy for prayer. Meals provide social contact with others. Engage the person in pleasant conversation. Give time for chewing and swallowing.
Rules and guidelines for feeding Ø Sit so you face the person. • This is more relaxing. • It shows the person that you have time. • You can see how well the person is eating. • You can see if the person has problems swallowing.
Rules and guidelines for feeding Ø visually impaired resident • Tell the person what is on the tray. • When feeding a visually impaired person, describe what you are offering. • If feed themselves describe foods and fluids and their place on the tray. • Use the numbers on a clock for the location of foods.
*Focus on long-term care: serving meal trays Ø Nursing centers have special dining programs. • Social dining • Residents eat at a dining room table with 4 to 6 others. • Food is served as it is in a restaurant. • for persons who are oriented and can feed themselves
Focus on long-term care: serving meal trays Ø Family dining • Food is served in bowls and on platters. • Residents serve themselves. Ø Assistive dining • The dining room has horseshoe-shaped tables. • They are for residents who need help eating.
Focus on long-term care: serving meal trays Ø Low-stimulation dining • The program prevents distractions during meals. • The health team decides on the best place for each person to sit

APPLICATION FEEDING A DEPENDENT RESIDENT
Between-meal nourishments Ø Ø . Many special diets involve between-meal nourishments. Serve nourishments when they arrive on the nursing unit. Provide needed eating utensils, a straw, and napkin. Follow the same considerations and procedures for serving meal trays and feeding
Providing drinking water Ø Patients and residents need fresh drinking water each shift. Ø They also need water whenever the pitcher is empty. Ø ask about any special orders before providing water Ø Practice medical asepsis. Ø Follow agency procedure.

APPLICATION PASSING FRESH WATER APPLICATION Care Planning considerations Worksheet
1 2 3 4 5 6 7 IN CLASS WORK Enteral nutrition Parenteral Nutrition (IV Therapy) NG tube Nasointestinal tube Gastrostomy tube Jejunostomy tube PEG tube Ø Provide the following information about the term from the text. Present the information to the class. • Definition • How it is inserted ? ( if relating to a feeding tube) • Who inserts it? ( if related to a feeding tube) • Why it used? • Any special precautions • Special Needs of the patient

RESEARCH 1. Monosodium Glutamate 2. Partially hydrogenated vegetable oil 3. Aspartame 4. Splenda 5. Olean 6. Nitrates 7. Organic foods 8. Nutrisweet 9. Saturated/Unsaturated Fats 10. Mono- and Di-glycerides
08d9acc7486e265162ba4ee03a934ff4.ppt