304a63626f332b7779bf0240febaa452.ppt
- Количество слайдов: 91
Health Informatics had a favorable impact on patient care. Agree or Disagree? BCS Health Informatics Forum October 4, 2005 Denis Protti - University of Victoria 1
Before we begin the debate, we need to set the rules Denis Protti - University of Victoria 3
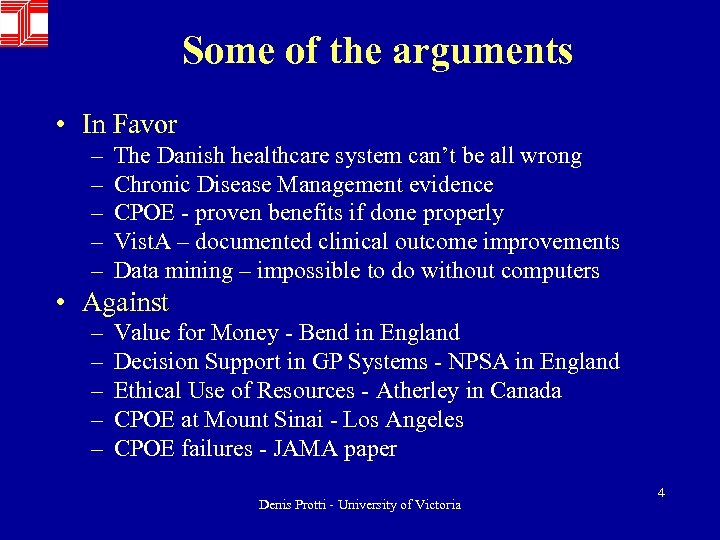
Some of the arguments • In Favor – – – The Danish healthcare system can’t be all wrong Chronic Disease Management evidence CPOE - proven benefits if done properly Vist. A – documented clinical outcome improvements Data mining – impossible to do without computers • Against – – – Value for Money - Bend in England Decision Support in GP Systems - NPSA in England Ethical Use of Resources - Atherley in Canada CPOE at Mount Sinai - Los Angeles CPOE failures - JAMA paper Denis Protti - University of Victoria 4
Arguments in Favor The Danish Health Care System Can’t Be All Wrong Denis Protti - University of Victoria 5
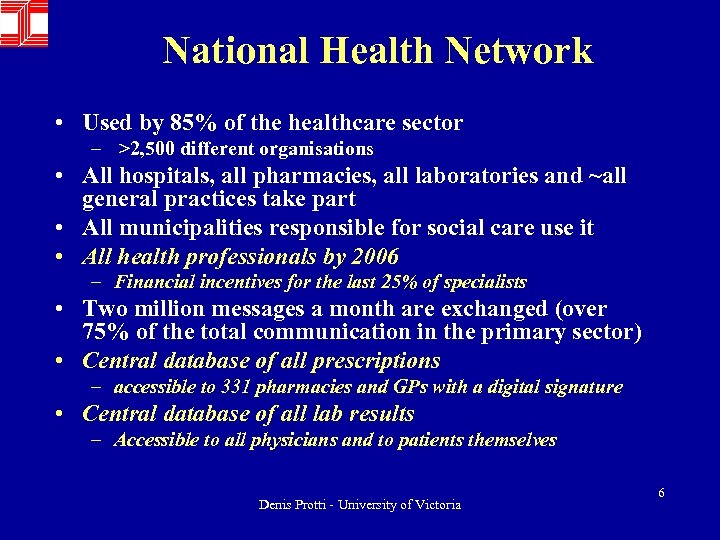
National Health Network • Used by 85% of the healthcare sector – >2, 500 different organisations • All hospitals, all pharmacies, all laboratories and ~all general practices take part • All municipalities responsible for social care use it • All health professionals by 2006 – Financial incentives for the last 25% of specialists • Two million messages a month are exchanged (over 75% of the total communication in the primary sector) • Central database of all prescriptions – accessible to 331 pharmacies and GPs with a digital signature • Central database of all lab results – Accessible to all physicians and to patients themselves Denis Protti - University of Victoria 6
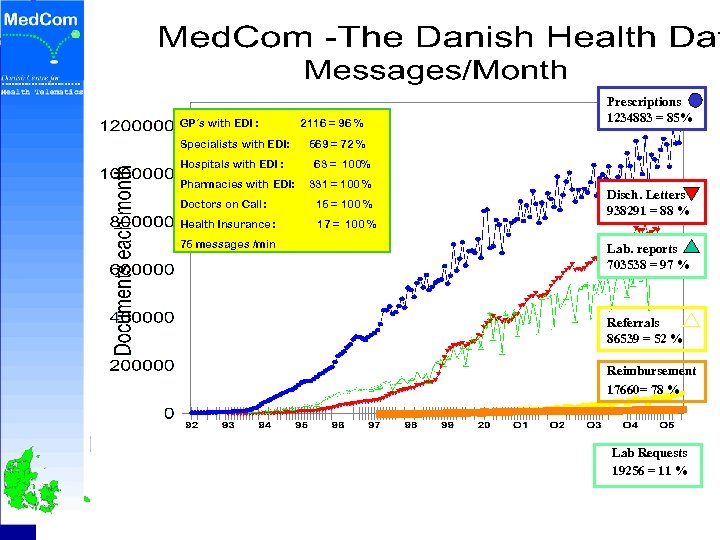
GP´s with EDI : Specialists with EDI: Hospitals with EDI : Pharmacies with EDI: 2116 = 96 % Prescriptions 1234883 85% 1039105 = 73% 569 = 72 % 63 = 100% 331 = 100 % Doctors on Call: 15 = 100 % Health Insurance : 17 = 100 % 75 messages /min Disch. Letters 938291 88 682923 = 85 % Lab. reports 703538 97 543040 = 82 % Referrals 86539 = 52 % Reimbursement 17660= 78 % Lab Requests 19256 = 11 % Denis Protti - University of Victoria 7
From handwritten prescriptions to. . Denis Protti - University of Victoria 8
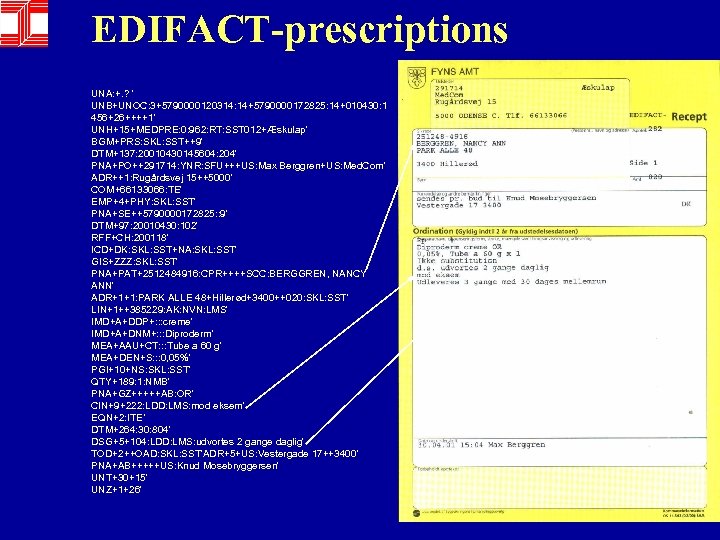
EDIFACT-prescriptions UNA: +. ? ' UNB+UNOC: 3+5790000120314: 14+5790000172825: 14+010430: 1 456+26++++1' UNH+15+MEDPRE: 0: 962: RT: SST 012+Æskulap' BGM+PRS: SKL: SST++9' DTM+137: 20010430145604: 204' PNA+PO++291714: YNR: SFU+++US: Max Berggren+US: Med. Com' ADR++1: Rugårdsvej 15++5000' COM+66133066: TE' EMP+4+PHY: SKL: SST' PNA+SE++5790000172825: : 9' DTM+97: 20010430: 102' RFF+CH: 200118' ICD+DK: SKL: SST+NA: SKL: SST' GIS+ZZZ: SKL: SST' PNA+PAT+2512484916: CPR++++SCC: BERGGREN, NANCY ANN' ADR+1+1: PARK ALLE 48+Hillerød+3400++020: SKL: SST' LIN+1++385229: AK: NVN: LMS' IMD+A+DDP+: : : creme' IMD+A+DNM+: : : Diproderm' MEA+AAU+CT: : : Tube a 60 g' MEA+DEN+S: : : 0, 05%' PGI+10+NS: SKL: SST' QTY+189: 1: NMB' PNA+GZ+++++AB: OR' CIN+9+222: LDD: LMS: mod eksem' EQN+2: ITE’ DTM+264: 30: 804' DSG+5+104: LDD: LMS: udvortes 2 gange daglig' TOD+2++OAD: SKL: SST'ADR+5+US: Vestergade 17++3400' PNA+AB+++++US: Knud Mosebryggersen' UNT+30+15' UNZ+1+26'
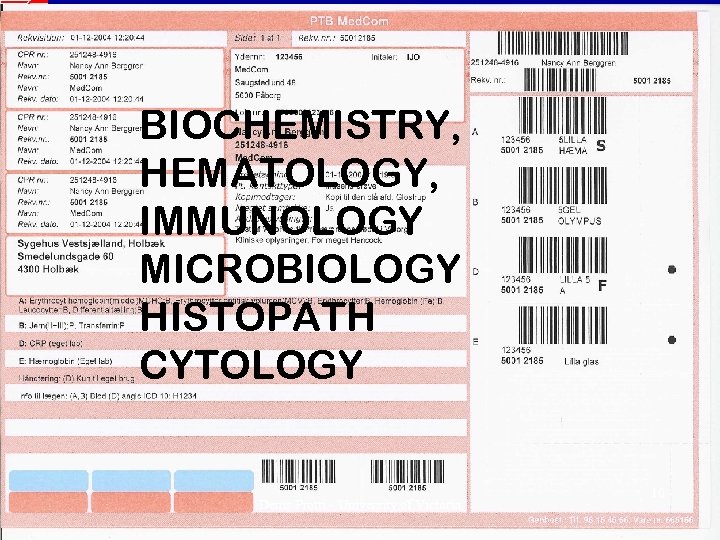
BIOCHEMISTRY, HEMATOLOGY, IMMUNOLOGY MICROBIOLOGY HISTOPATH CYTOLOGY Denis Protti - University of Victoria 10
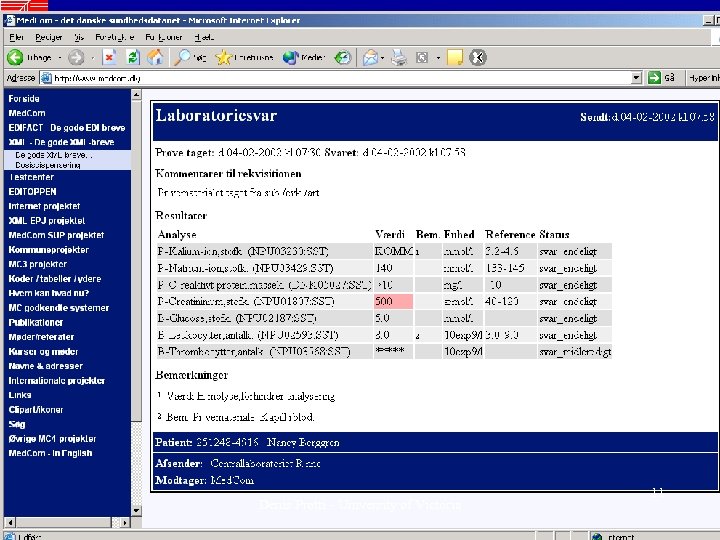
Denis Protti - University of Victoria 11
VPN- Internet based Health Data Network by 2005 • Structured clinical messages UNA: +. ? ' UNB+UNOC: 3+5790000120284: 14+57 UNH+80901082504854+MEDRPT: D: 93 BGM+LRP++9+NA' DTM+137: 200001141247: 203' S 01+01' NAD+SLA+4201050: SKS: SST++Sygeh SEQ++1' SPR+ORG+60: SKS: SST+RPT 01: SKS: S S 01+01' • Clinical e-mail • Booking at GP´s / Specialists • Look up – across regions: – Lab results, Lab requisitions, X-ray reports • Health Portal • Patient monitoring, clinical databases • Telemedicine Denis Protti - University of Victoria 12
Arguments in Favor Chronic Disease Management Evidence of Benefits Denis Protti - University of Victoria 13
One of many Chronic Disease Management success stories Denis Protti - University of Victoria 14

Online Provider Directory PUBLIC KEY INFRASTRUCTURE Pharmacy Discharge Summaries Patient Status Reports GP Practice ISP Government or Private Health Insurer EDI Message Exchange Pathology Lab Test Reports Orders Online Services and Databases ISP GP Practice AGPAL ACCREDITED VPN GP Practice Child Immunisation Diabetes Infectious Disease Management Systems Radiology Service Test Reports Orders Denis Protti - University of Victoria Public Health Monitoring and Surveillance Systems 15

New Zealand Facts • Used by 80% of all healthcare sector organizations in New Zealand – All hospitals, radiology clinics, private laboratories – ~1, 800 general practices. – > 600 specialists, physiotherapists, other allied health workers • Over 3 million messages a month exchanged – 95% of the communication in the primary health care sector. Denis Protti - University of Victoria 16
New Zealand Facts • Over 95% of GP offices are using one of nine Practice Management Systems – 75% use their systems to electronically send and receive clinical messages such as laboratory results, radiology results, discharge letters, referrals, etc. • ~ 50% of GPs now use the Internet on a regular basis from their offices - including communicating with their patients. Denis Protti - University of Victoria 17
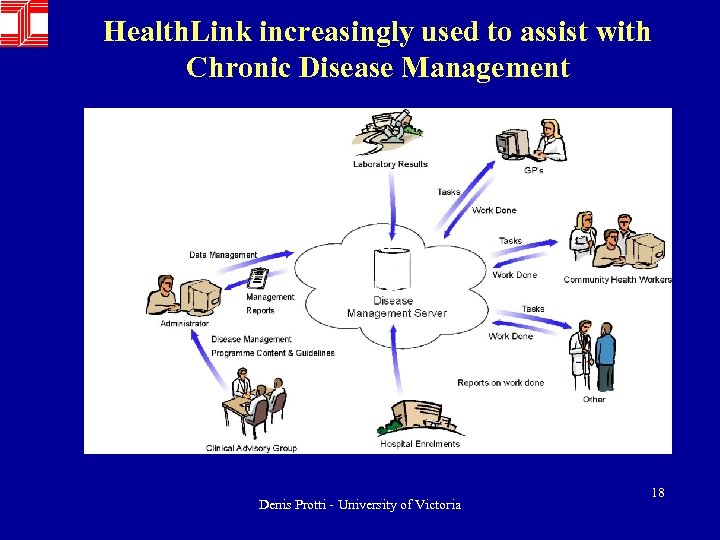
Health. Link increasingly used to assist with Chronic Disease Management Denis Protti - University of Victoria 18
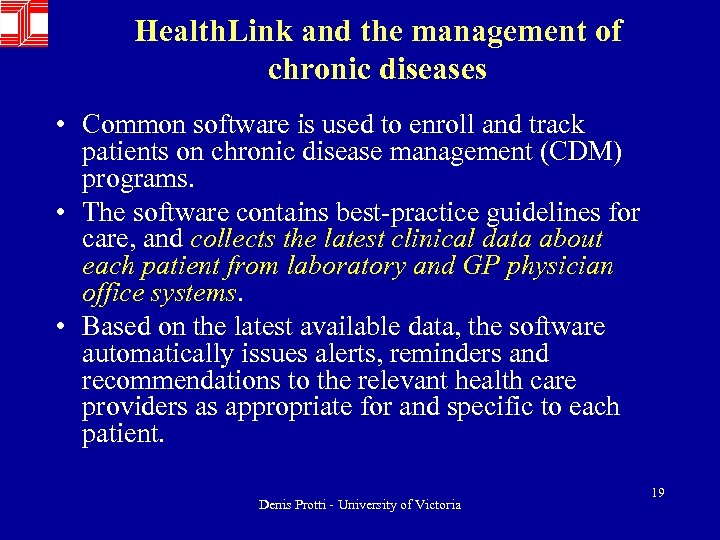
Health. Link and the management of chronic diseases • Common software is used to enroll and track patients on chronic disease management (CDM) programs. • The software contains best-practice guidelines for care, and collects the latest clinical data about each patient from laboratory and GP physician office systems. • Based on the latest available data, the software automatically issues alerts, reminders and recommendations to the relevant health care providers as appropriate for and specific to each patient. Denis Protti - University of Victoria 19
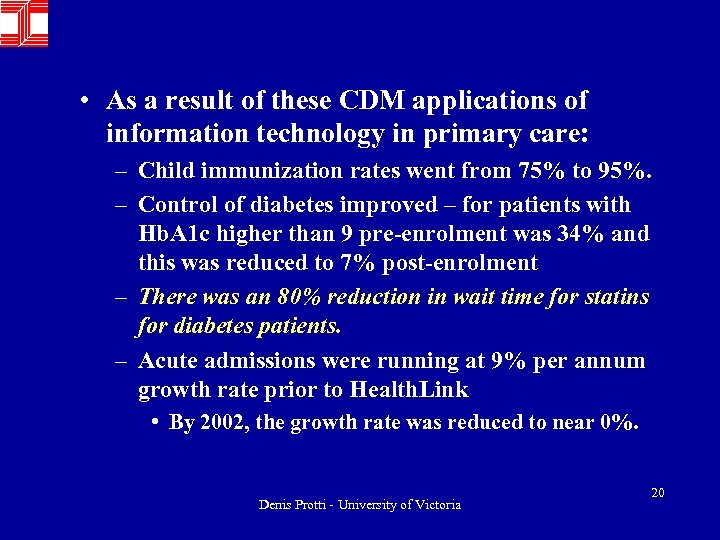
• As a result of these CDM applications of information technology in primary care: – Child immunization rates went from 75% to 95%. – Control of diabetes improved – for patients with Hb. A 1 c higher than 9 pre-enrolment was 34% and this was reduced to 7% post-enrolment – There was an 80% reduction in wait time for statins for diabetes patients. – Acute admissions were running at 9% per annum growth rate prior to Health. Link • By 2002, the growth rate was reduced to near 0%. Denis Protti - University of Victoria 20
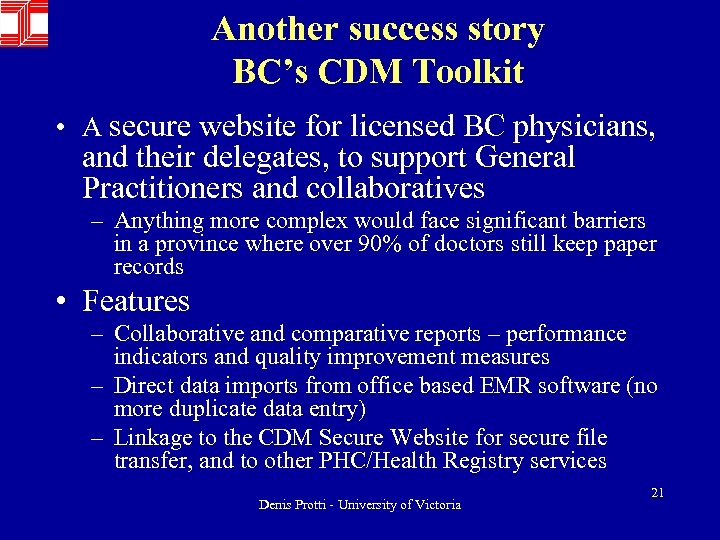
Another success story BC’s CDM Toolkit • A secure website for licensed BC physicians, and their delegates, to support General Practitioners and collaboratives – Anything more complex would face significant barriers in a province where over 90% of doctors still keep paper records • Features – Collaborative and comparative reports – performance indicators and quality improvement measures – Direct data imports from office based EMR software (no more duplicate data entry) – Linkage to the CDM Secure Website for secure file transfer, and to other PHC/Health Registry services Denis Protti - University of Victoria 21
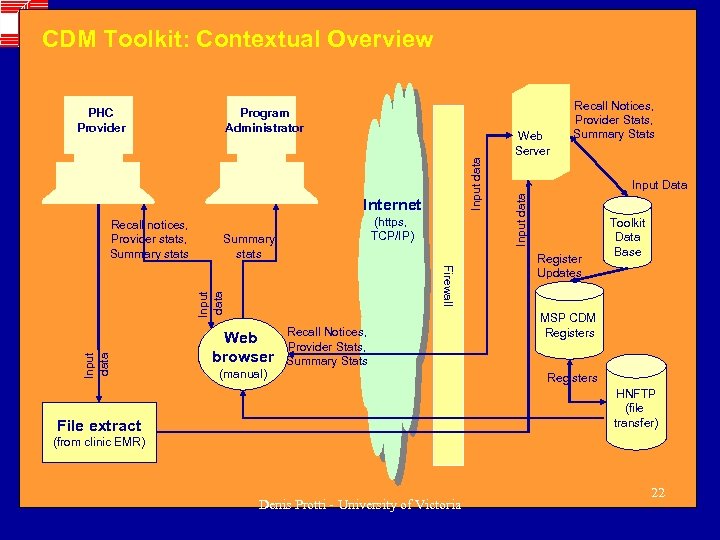
CDM Toolkit: Contextual Overview Internet (https, TCP/IP) Summary stats Firewall Input data Recall notices, Provider stats, Summary stats Web browser (manual) Recall Notices, Provider Stats, Summary Stats Web Server Recall Notices, Provider Stats, Summary Stats Input Data Input data Program Administrator Input data PHC Provider Register Updates Toolkit Data Base MSP CDM Registers HNFTP (file transfer) File extract (from clinic EMR) Denis Protti - University of Victoria 22
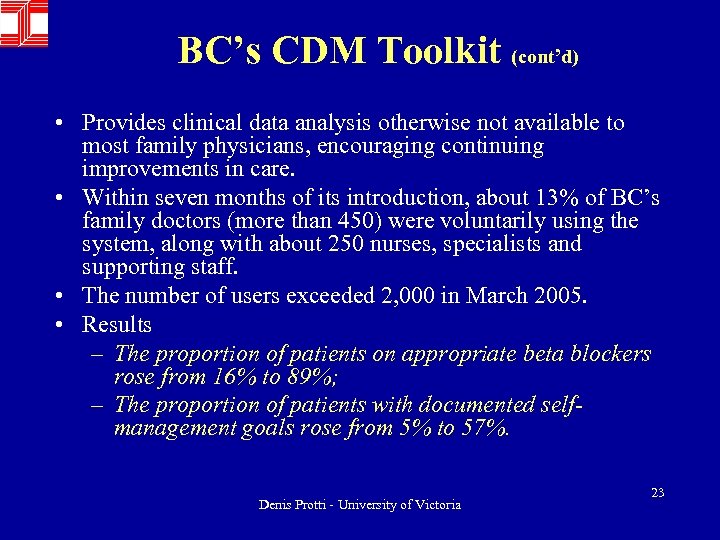
BC’s CDM Toolkit (cont’d) • Provides clinical data analysis otherwise not available to most family physicians, encouraging continuing improvements in care. • Within seven months of its introduction, about 13% of BC’s family doctors (more than 450) were voluntarily using the system, along with about 250 nurses, specialists and supporting staff. • The number of users exceeded 2, 000 in March 2005. • Results – The proportion of patients on appropriate beta blockers rose from 16% to 89%; – The proportion of patients with documented selfmanagement goals rose from 5% to 57%. Denis Protti - University of Victoria 23
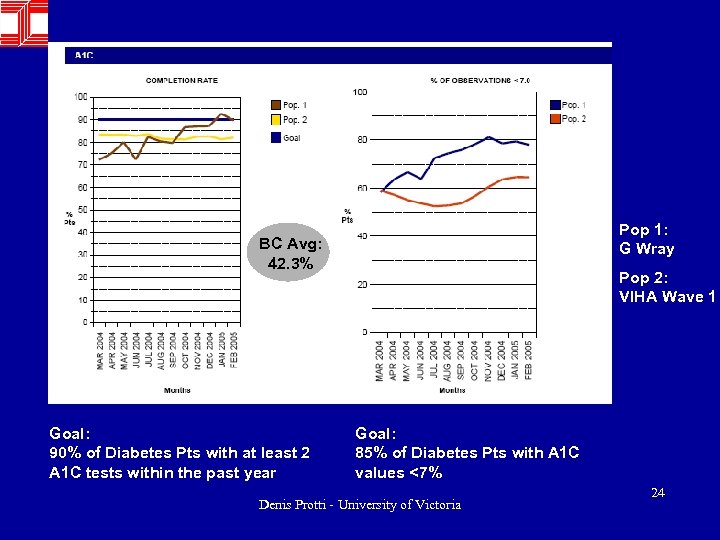
Pop 1: G Wray BC Avg: 42. 3% Goal: 90% of Diabetes Pts with at least 2 A 1 C tests within the past year Pop 2: VIHA Wave 1 Goal: 85% of Diabetes Pts with A 1 C values <7% Denis Protti - University of Victoria 24
VIHA Outcomes • Diabetes - % with > 1 Hb. A 1 c in 1 yr – BC (’ 02 -03) = 39 % – VIHA (March/05) = 79 % • CHF - Patients on recommended drugs (ACE-I): – BC (’ 02 -03) = 50 % – VIHA (March/05) = 85 % Denis Protti - University of Victoria 25
Arguments in Favor Computerised Physician Order Entry (CPOE) – Has Proven Value Denis Protti - University of Victoria 26
Effect of Physician Order Entry (CPOE) • 3 recent white papers on use of CPOE • Medication errors are the low hanging fruit of patient safety • CPOE shown to reduce serious, nonintercepted drug errors by 55% • In US, States are demanding it! Denis Protti - University of Victoria 27
The evidence that IT can enhance patient safety is mounting • Boston’s Brigham and Women’s Hospital, demonstrated that CPOE reduced error rates by 55% -- from 10. 7 to 4. 9 per 1000 patient days. – Rates of serious medication errors fell by 88% in a subsequent study by the same group. – The prevention of errors was attributed to the CPOE system’s structured orders and medication checks. • LDS Hospital in Salt Lake City demonstrated a 70% reduction in ADEs after implementation of a CPOE system. Denis Protti - University of Victoria 28
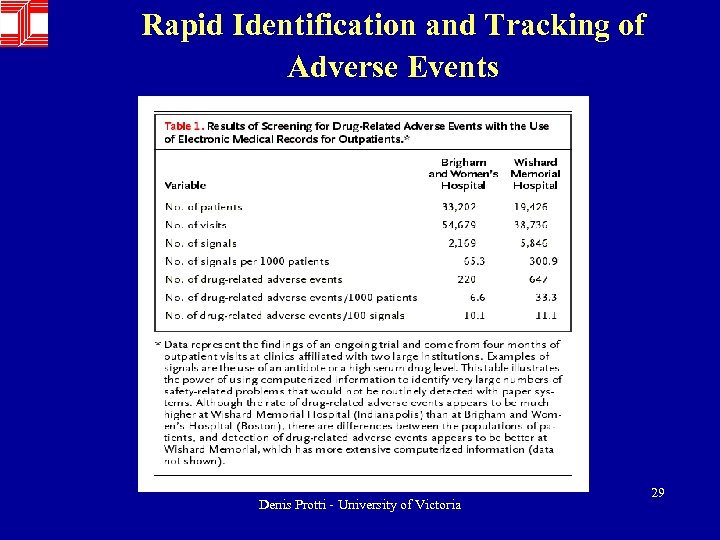
Rapid Identification and Tracking of Adverse Events Denis Protti - University of Victoria 29
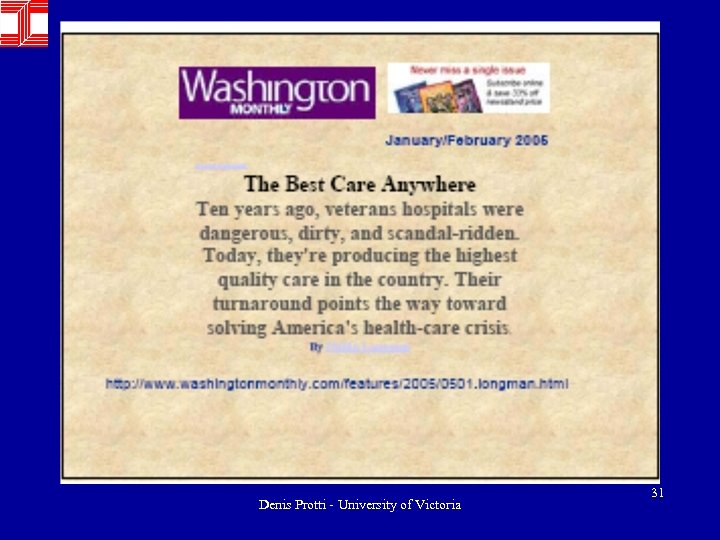
Arguments in Favor The EHR system (Vist. A) at the Veteran’s Administration is the gold standard when it comes to measuring clinical outcomes Denis Protti - University of Victoria 30
Denis Protti - University of Victoria 31
Comparison of Quality of Care for VA Patients • VA patients scored significantly higher for: – Adjusted overall quality (67% vs 51%) – Chronic disease care (72% vs 59%) – Preventive care (64% vs 44%) • The VA advantage was most prominent in areas where the VA has established performance measures and active performance monitoring • Other studies suggest contributions from: – EHR, clinician reminders, structured templates, standing orders, improved inter-provider communication, facility performance profiling, accountability for performance and more integrated delivery systems Steven Asch, Elizabeth Mc. Glynn et al Comparison of Quality of Care for Patients in the Veterans’ Health Administration and Patients in a National Sample Annals of Internal Medicine 2004; 141: 939 -945 Denis Protti - University of Victoria 32
The VA Computerized Patient Record System • Integrated computer-based medical record developed by Department of Veterans Affairs • Includes clinician order entry, note entry, results review, imaging, decision support, remote data • Integrated with pharmacy, laboratory, dietetics, vital signs, nursing and bar code medication administration programs • Includes user authentication with signature codes, business rules for user classes to ensure security and appropriate use Denis Protti - University of Victoria 33
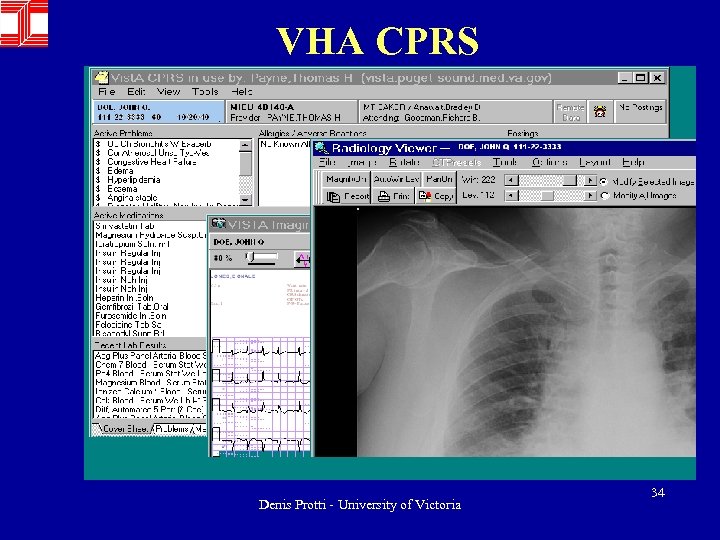
VHA CPRS Denis Protti - University of Victoria 34
• The VA's Quality Enhancement Research Initiative (QUERI) is a large-scale, multidisciplinary quality improvement initiative designed to ensure excellence in all areas where VA provides health care services, including inpatient, outpatient, and long-term care settings. • The role of information systems is critical to this quality improvement process. Hynes DM et al Informatics Resources to Support Health Care Quality Improvement in the Veterans Health Administration J Am Med Inform Assoc. 2004; 11: 344 -350 Denis Protti - University of Victoria 35
QUERI in action • QUERI's development of information technology tools is an important component of (and contributor to) VA's overall informatics strategy. • The resulting databases and data elements and information technology tools provide valuable information for patient care, quality improvement, research, and management decisions, including high-level policy formulation and resource allocation. • An example from the Ischemic Heart Disease (IHD) QUERI's experience illustrates this point. Denis Protti - University of Victoria 36
QUERI in action • When the IHD QUERI team proposed to develop a national clinical reminder for lipid level management, it quickly became clear that then-existing formal protocols and procedures for clinical reminder development were incomplete. • An organizational realignment resulted in formal links and collaborations leading to formalized, well-documented processes for developing, testing, and implementing national clinical reminders in the clinical information system. Denis Protti - University of Victoria 37
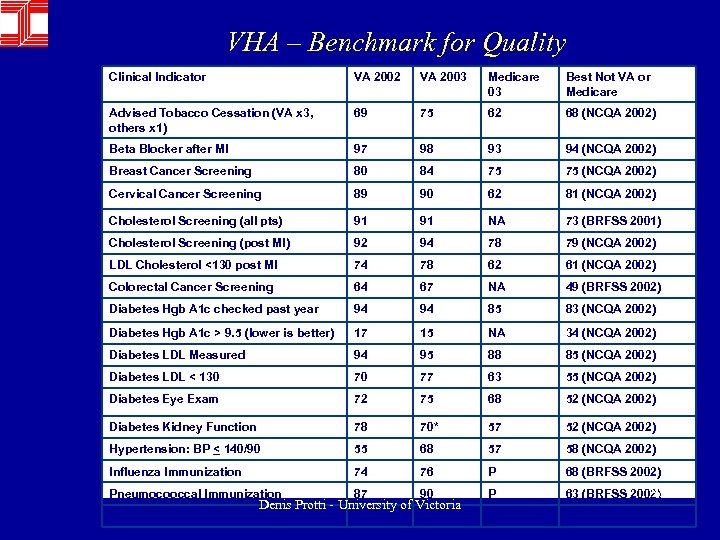
VHA – Benchmark for Quality Clinical Indicator VA 2002 VA 2003 Medicare 03 Best Not VA or Medicare Advised Tobacco Cessation (VA x 3, others x 1) 69 75 62 68 (NCQA 2002) Beta Blocker after MI 97 98 93 94 (NCQA 2002) Breast Cancer Screening 80 84 75 75 (NCQA 2002) Cervical Cancer Screening 89 90 62 81 (NCQA 2002) Cholesterol Screening (all pts) 91 91 NA 73 (BRFSS 2001) Cholesterol Screening (post MI) 92 94 78 79 (NCQA 2002) LDL Cholesterol <130 post MI 74 78 62 61 (NCQA 2002) Colorectal Cancer Screening 64 67 NA 49 (BRFSS 2002) Diabetes Hgb A 1 c checked past year 94 94 85 83 (NCQA 2002) Diabetes Hgb A 1 c > 9. 5 (lower is better) 17 15 NA 34 (NCQA 2002) Diabetes LDL Measured 94 95 88 85 (NCQA 2002) Diabetes LDL < 130 70 77 63 55 (NCQA 2002) Diabetes Eye Exam 72 75 68 52 (NCQA 2002) Diabetes Kidney Function 78 70* 57 52 (NCQA 2002) Hypertension: BP < 140/90 55 68 57 58 (NCQA 2002) Influenza Immunization 74 76 P 68 (BRFSS 2002) Pneumocooccal Immunization 87 90 P 38 63 (BRFSS 2002) Mental Health F/U 30 D post D/C 81 77* 61 74 (NCQA 2002) Denis Protti - University of Victoria
Denis Protti - University of Victoria 39
Arguments in Favor Data Mining benefits are impossible without computer technology Denis Protti - University of Victoria 40
• 20 Hospitals • 100+ Clinics • 450 employed physicians • + Affiliated physicians • Health Plans • One million members and affiliates • Utah and southern Idaho • $3. 1 B in annual revenue • 25, 000 employees Denis Protti - University of Victoria 41
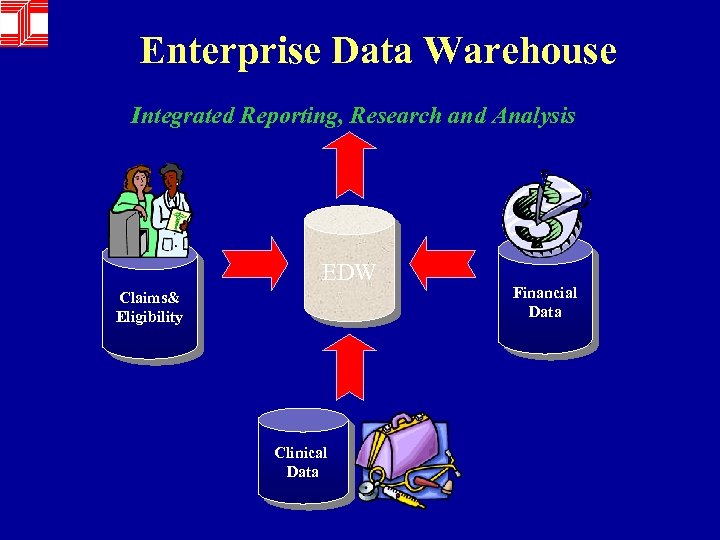
Enterprise Data Warehouse Integrated Reporting, Research and Analysis EDW Claims& Eligibility Clinical Data Financial Data
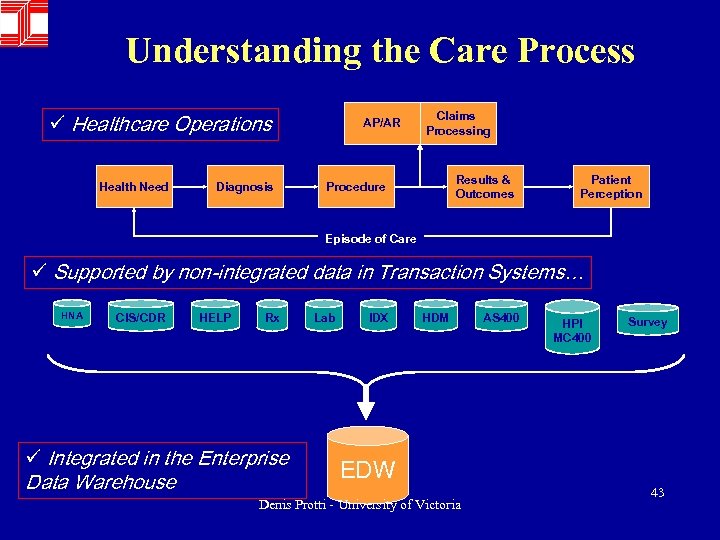
Understanding the Care Process ü Healthcare Operations Health Need Diagnosis AP/AR Claims Processing Results & Outcomes Procedure Patient Perception Episode of Care ü Supported by non-integrated data in Transaction Systems… HNA CIS/CDR HELP Rx ü Integrated in the Enterprise Data Warehouse Lab IDX HDM EDW Denis Protti - University of Victoria AS 400 HPI MC 400 Survey 43
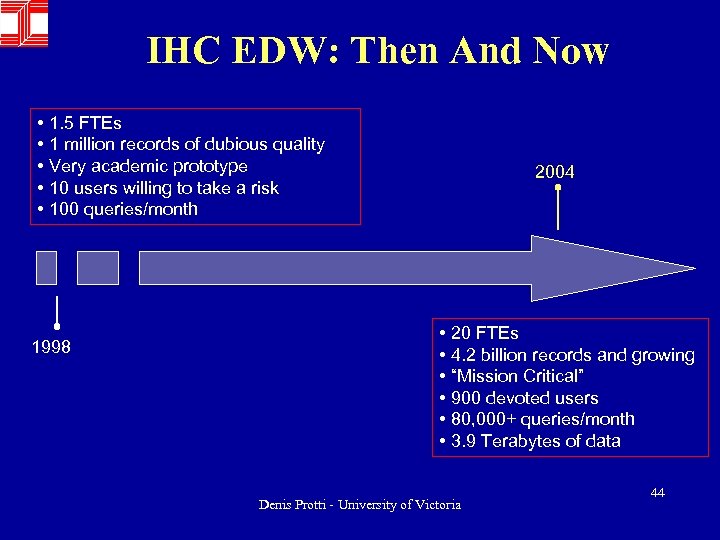
IHC EDW: Then And Now • 1. 5 FTEs • 1 million records of dubious quality • Very academic prototype • 10 users willing to take a risk • 100 queries/month 1998 2004 • 20 FTEs • 4. 2 billion records and growing • “Mission Critical” • 900 devoted users • 80, 000+ queries/month • 3. 9 Terabytes of data Denis Protti - University of Victoria 44
Motives Behind EDW & BI • Fundamentally – Drive healthcare costs down, quality up • Sub themes – Patient quality of life and safety, compliance, evidence-based medicine, etc. Reduce Mean Time To Improvement (MTTI) Denis Protti - University of Victoria 45
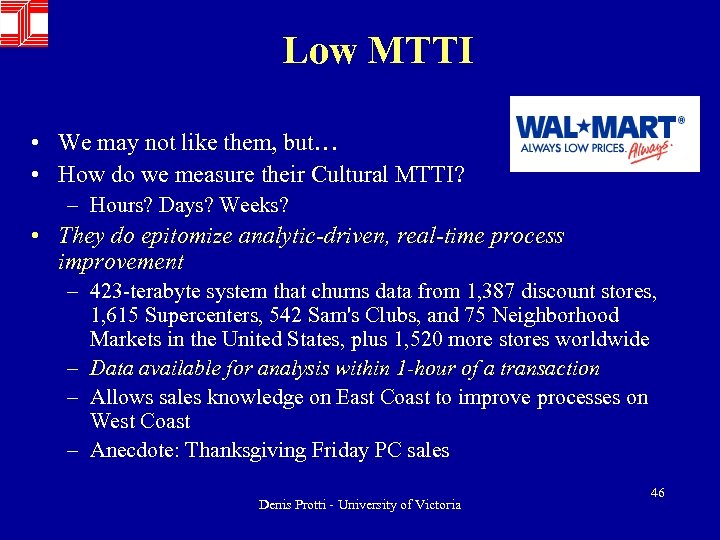
Low MTTI • We may not like them, but… • How do we measure their Cultural MTTI? – Hours? Days? Weeks? • They do epitomize analytic-driven, real-time process improvement – 423 -terabyte system that churns data from 1, 387 discount stores, 1, 615 Supercenters, 542 Sam's Clubs, and 75 Neighborhood Markets in the United States, plus 1, 520 more stores worldwide – Data available for analysis within 1 -hour of a transaction – Allows sales knowledge on East Coast to improve processes on West Coast – Anecdote: Thanksgiving Friday PC sales Denis Protti - University of Victoria 46
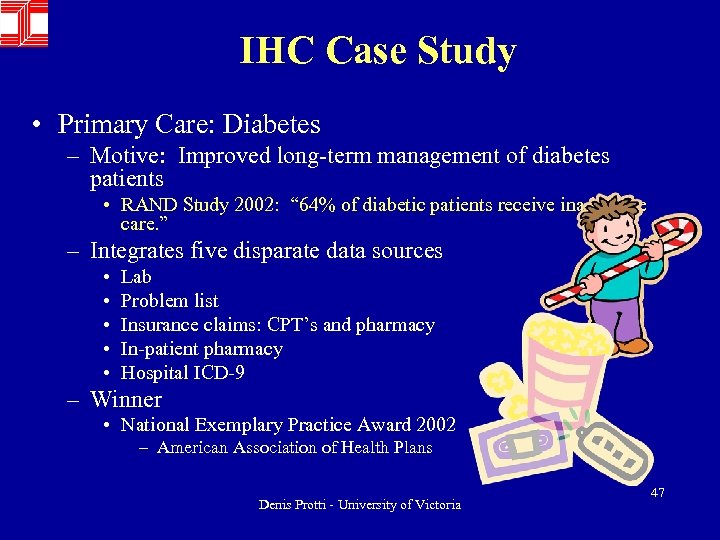
IHC Case Study • Primary Care: Diabetes – Motive: Improved long-term management of diabetes patients • RAND Study 2002: “ 64% of diabetic patients receive inadequate care. ” – Integrates five disparate data sources • • • Lab Problem list Insurance claims: CPT’s and pharmacy In-patient pharmacy Hospital ICD-9 – Winner • National Exemplary Practice Award 2002 – American Association of Health Plans Denis Protti - University of Victoria 47
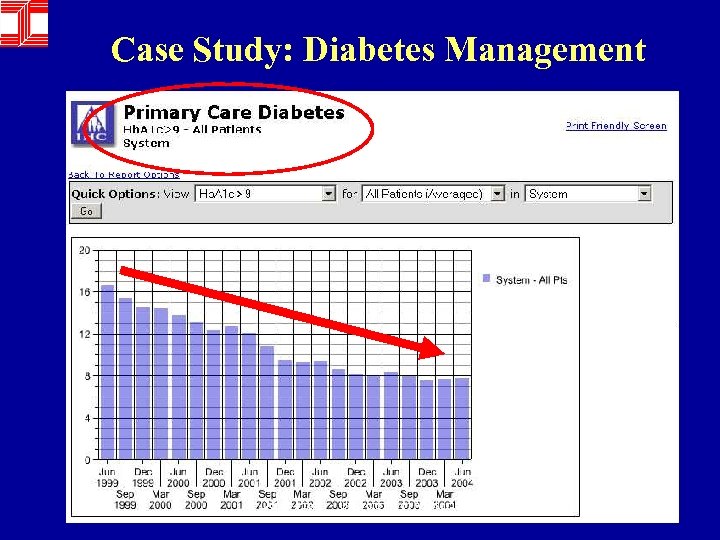
Case Study: Diabetes Management Denis Protti - University of Victoria 48
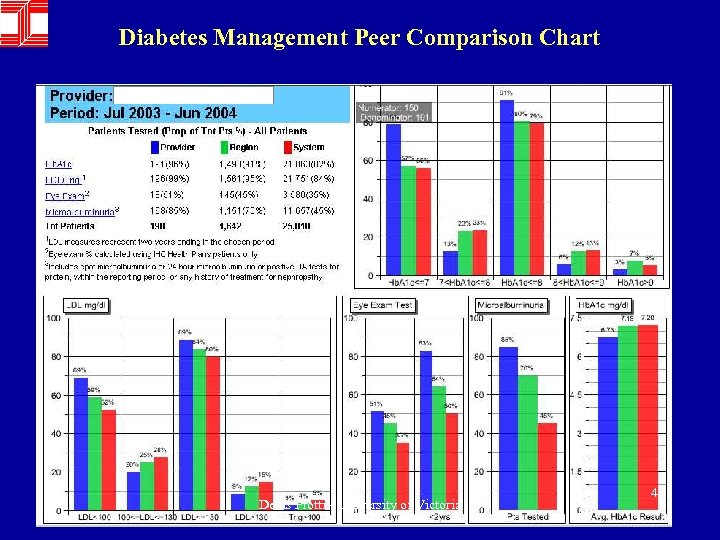
Diabetes Management Peer Comparison Chart Denis Protti - University of Victoria 49
IHC Case Study 2 • CV Discharge Medications – Motive: Basic protocol adherence • Appropriate discharge meds ordered following CV (IHD and MI) diagnosis and treatment – Results • 1994: 15% (estimate, no hard data) • 2004: 98% (hard data) Denis Protti - University of Victoria 50
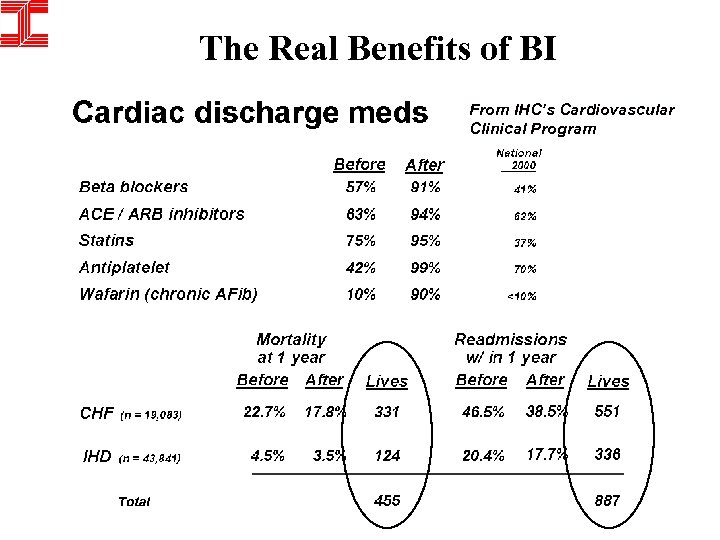
The Real Benefits of BI From IHC’s Cardiovascular Clinical Program
Arguments Against Denis Protti - University of Victoria 52
There are those who prefer proven technology Denis Protti - University of Victoria 53
Arguments Against Plenty of past failures to point to Denis Protti - University of Victoria 54

Past Clinical Information System Failures Around The World • • • Over budget / Delayed implementation Partial implementation / Limited functionality Replication failures - pilot succeeds, others fail Temporary setback / Regroup - Redesign Isolated system errors lead to patient harm Major system outage / failure Change CIS systems / vendors Stop work on CISs Total failure: Hospital closes due to system failure Denis Protti - University of Victoria 55

Public Health System New South Wales, Australia • NSW - 7 million people; Sidney - 3 million people • Public Health System provides integrated hospital & community services • Budget $5 billion (US); 100, 000 employees • Geographically divisionalized structure • Considerable dissatisfaction with current basic clinical & administrative systems – in-flexible, no Management Information – Supplementary apps being developed Southon et al. JAMIA 1997; 4: 112 -124. Denis Protti - University of Victoria 56
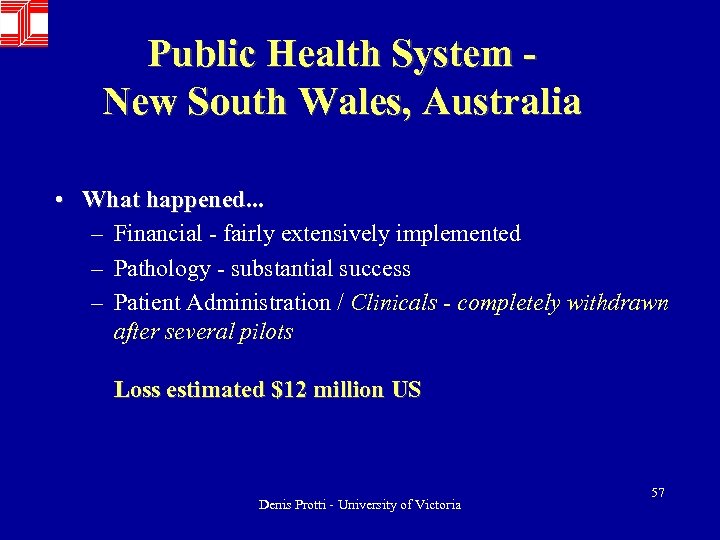
Public Health System New South Wales, Australia • What happened. . . – Financial - fairly extensively implemented – Pathology - substantial success – Patient Administration / Clinicals - completely withdrawn after several pilots Loss estimated $12 million US Denis Protti - University of Victoria 57
Lessons Learned. . . • Difficulties Organizational NOT Technical – Differences in business & operational environments • NSW cost control rather than cost allocation • NSW much larger span of control • Main benefits due to integration of systems • NSW no clerks available to enter orders • Clinicians - some. . . not enough use to learn Others. . . rotated out before they learned system • Strategy developed at local hospital, formulated centrally – Goal - cost-effective resource allocation – Organizational structure - decentralized • Local organizations focus on healthcare delivery, not costs • Result: System selected did not meet local needs Denis Protti - University of Victoria 58
Denis Protti - University of Victoria 59
Arguments Against Lack of evidence of public value Denis Protti - University of Victoria 60
• “The absence of a coherent body of evidence demonstrating that effective use of ICT in health can deliver real public value presents serious problems. . . , it hampers public and political debate on the use of ICT, potentially preventing appropriate spending on ICT in the future. ” (p. 83) Jamie Bend Public Value and e-Health Institute for Public Policy Research 2004 Denis Protti - University of Victoria 61
• “Until now, greater use of ICT has often been seen as a good in of itself as part of a process of modernisation. This is unlikely to be the case in future and appropriate use of ICT will have to be argued for and supported with evidence that spending on ICT will deliver benefits. ” (p. 12) Denis Protti - University of Victoria 62
Protti’s formula for the future • With deference and apologies to Albert E. , perhaps the safest predictor of the future will be to posit that it will be very much about Eb. M 2 C – Evidence-based Medicine – Evidence-based Management – Evidence-based Computing Denis Protti - University of Victoria 63
• “When the rapid development of ICT and the ability of some systems to adapt to or be altered for the specific environment in which they will be used is also taken into account, it becomes clear that evaluation of a new computer system presents different challenges to those faced when testing a new drug. ” (p. 58) Denis Protti - University of Victoria 65
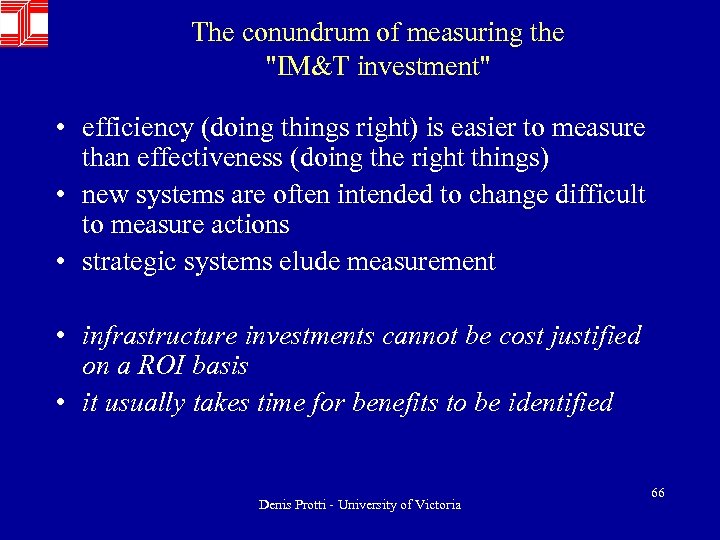
The conundrum of measuring the "IM&T investment" • efficiency (doing things right) is easier to measure than effectiveness (doing the right things) • new systems are often intended to change difficult to measure actions • strategic systems elude measurement • infrastructure investments cannot be cost justified on a ROI basis • it usually takes time for benefits to be identified Denis Protti - University of Victoria 66
• “It might take some time for the effects of a new system to become clear. Possible benefits of new ICT systems may only become apparent after working practices have altered to take advantage of the new resource and this process could take several months or years, presenting a particular problem for those looking to evaluate pilot projects. ” (p. 58). Denis Protti - University of Victoria 67
• “While these barriers all offer possible explanations for the fact that few benefits are evident from previous e-health projects and may yet adversely affect future projects, none is insurmountable. ” (p. 15). • “As we demonstrated in chapter three, few previous e-health projects have produced real evidence of public value. ” (p. 57). Denis Protti - University of Victoria 68
Arguments Against Decision Support System Failures Denis Protti - University of Victoria 69
Further warnings from England • A different form of caution comes in the December 2003 report released by the NPSA entitled “Realising the Potential of GP Computer Systems to Improve Patient Safety”. • Since over 95% of GP practices in England are automated and the most commonly used clinical application are medication prescriptions which are printed and carried to the pharmacy by the patient, there was a commonly held belief that medication errors were not a significant issue in primary care in England. Denis Protti - University of Victoria 70
• To the surprise of many, the assessment of GP computer systems revealed: – lack of alerts in relation to contraindications – for example, there was no warning of the risk of Reyes’ syndrome when prescribing aspirin to an eight-year old child – spurious alerts – for example a serious alert warning was given for a commonly used and relatively safe drug-drug combination – failures of drug allergy warnings – depending on how the allergy history had been recorded, warnings might or might not be displayed – risks of prescribing drugs with similar names – particularly with penicillin (frequently used) and penicillamine (rarely used and likely to do harm to some patients) – lack of warning for inappropriate dosages – for example, trying to prescribe methotrexate daily instead of weekly Denis Protti - University of Victoria 71
• Perhaps the most concerning finding was that English GPs have come to rely on their computers to provide alerts. • More than 90% of GPs regarded computerised alerts (including contraindication alerts) and systems for recall for patient monitoring to be important. • The survey revealed that some GPs are not fully aware of the safety features on their computer systems and only a minority has had training on the use of these safety features. Denis Protti - University of Victoria 72
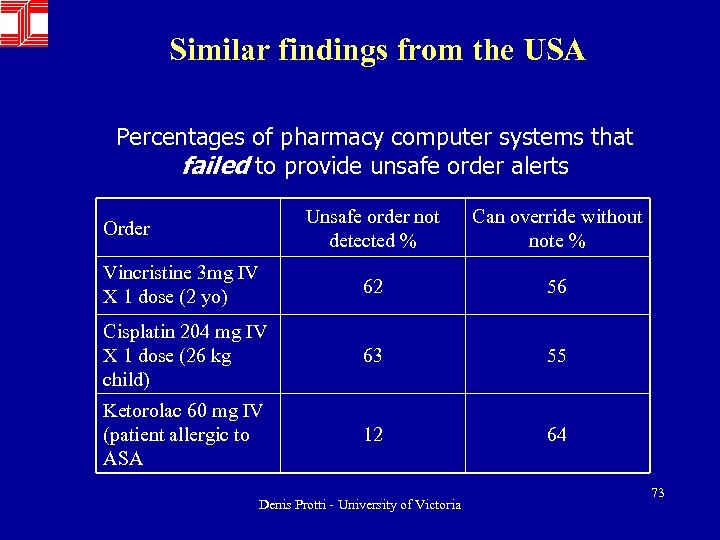
Similar findings from the USA Percentages of pharmacy computer systems that failed to provide unsafe order alerts Unsafe order not detected % Can override without note % Vincristine 3 mg IV X 1 dose (2 yo) 62 56 Cisplatin 204 mg IV X 1 dose (26 kg child) 63 55 Ketorolac 60 mg IV (patient allergic to ASA 12 64 Order Denis Protti - University of Victoria 73
Arguments Against Ethical Use of Resources Denis Protti - University of Victoria 74
• “Since 1999, the federal and other governments in Canada have repeatedly emphasized the value to healthcare of electronic health records. In 2004, a substantial UK investigation questioned the evidence of public value of large scale, government initiatives in healthcare information technology, and of electronic health records in particular. ” Atherley G Evidence of Public Value and Public Risk of Electronic Health Records: An Issue for Social Justice? Electronic. Healthcare Vol. 4, No. 1, 2005 Denis Protti - University of Victoria 75
• “Atherley examined the evidence pertaining specifically to electronic health records as represented in eight major health policy papers at the national level published in Canada from 1999 to early 2005. • He found during the period a decline in the concerns expressed in the 8 policy papers about privacy, security and availability of electronic health records systems. It also found that some risks were barely considered, if at all. • Yet, during the same period, the Auditor General of Canada issued strongly worded warnings about the wide range of risks affecting information technology in government. ” Denis Protti - University of Victoria 76
• Atherley concluded that a) evidence of public value and public risk of electronic health records should be subject to the standards increasingly used for and expected of evidence-based medicine, and of assessments of pharmaceuticals and medical devices; b) at the national level, Canada lacks an independent public accountability mechanism for analyzing public value and public risk from electronic health records; c) to the extent that, for electronic health records, the public risks are plausible and the public values are debatable, this lack is an issue of social justice. ” Denis Protti - University of Victoria 77
Arguments Against CPOE Failure at Mount Sinai Denis Protti - University of Victoria 78
Medical Center • Largest private hospital in California (850 -bed hospital) • Goals of $20 million Patient Care Expert (PCX) program: – Help reduce medical errors, – Allow physicians to electronically track their orders and – Provide alerts when physicians prescribe treatments that would prompt adverse reactions in patients. • Big Bang adoption required all physicians to show they could use the new system on 1 day or lose admitting privileges. • 600, 000 orders were logged on the system between October 2002 and January 2003 • Over 400 physicians complained that "it was endangering patient safety and required too much work, " • PCX was suspended because “it was not easy enough to use and it took too long to enter orders, " not because of patient safety concerns. Denis Protti - University of Victoria 79
Medical Center • Physician: “They poorly designed the system, poorly sold it and then jammed it down our throats and had the audacity to say everybody loves it and that it's a great system. ” • Administration: "Basically the hospital has decided to put on hold any further experience with CPOE at least until 2006 while they work on other aspects of the computer system to help with patient admissions, patient flow, billing and so on. ” • Lessons Learned: – Reinforces the importance of the cultural and organizational issues in successful implementation – Physicians must be the champions of this particular process in order to bring it successfully to conclusion. Denis Protti - University of Victoria 80
TDS 7000 Early Result Denis Protti - University of Victoria 81
Arguments Against CPOE – The Infamous JAMA Paper Denis Protti - University of Victoria 82
• In March 2005, Professor Ross Koppel and colleagues from the University of Pennsylvania published a paper on their assessment of a commercial computer-based provider orderentry (CPOE) system that had been implemented at their university hospital between 1997 and 2004. • Their study showed that ‘‘a leading CPOE system often facilitated medication error risks, with many reported to occur frequently. ’’ They concluded that ‘‘as CPOE systems are implemented, clinicians and hospital must attend to errors that these systems cause in addition to errors that they prevent. ’’ Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors Journal of the American Medical Association 2005: 293(10): 1197 -1203 Denis Protti - University of Victoria 83
• A main limitation of Koppel’s study is that it did not count errors or adverse events, but instead measured only perceptions of errors, which may or may not correlate with actual error rates. Further, it did not count the errors that were prevented. As such, it offers no insight into whether the error rate was higher or lower with CPOE. • Unfortunately, however, the press interpreted the study as suggesting that CPOE increases the medication error rate. While the authors did not state this, a press release put out by JAMA did so. Bates D Computerized physician order entry and medication errors: Finding a balance Journal of Biomedical Informatics June 16, 2005 Denis Protti - University of Victoria 84
• “We evaluated a vendor-developed/vendor-built system, the predominant type in US hospitals, whereas several wellknown CPOE system studies were based on home-grown applications tailored to the institution at hand. • This useful distinction might explain some of the differences between our findings and those of other scholars because the constant re-evaluation, on-site research, and responsiveness needed for good CPOE systems are more likely to be found in the home-grown systems. ” Koppel R et al. Neither panacea nor black box: Responding to three Journal of Biomedical Informatics papers on computerized physician order entry systems Journal of Biomedical Informatics Article in Press - 2005 Denis Protti - University of Victoria 85
• “As Bates indicates, after the initial installation of the home-grown CPOE system at his institution, they routinely tracked errors and problems and made thousands of changes to the program, because ‘‘it is just impossible to get it all right at the outset, because the processes involved are so complex. ’’ • However, it is the vendor-developed/vendor-built systems that are being installed nationwide, generally in institutions with markedly lower capability to adapt them than a large teaching hospital like ours. ” Denis Protti - University of Victoria 97
Other Closing Arguments • In Favor – – – Telemedicine, wireless technologies, and remote monitoring Patient portals and Personal Health Records Bioinformatics (genomics and proteomics) Existing and Evolving Clinical Technologies Robotics and Virtual Reality Technologies Etc. • Opposed – – – – High costs of investment and wasted past expenditures Lack of evidence from RCTs Lack of clinician involvement and engagement Insufficient government funding and incentives Lack of change management strategies Insufficient training and on-going support Etc. Denis Protti - University of Victoria 98
Time for rebuttals and counter arguments THEN: Judging!! Denis Protti - University of Victoria 99
In conclusion • ‘We must stop blaming people and start looking at our systems. We must look at how we do things that cause errors and keep us from discovering them…. . before they cause further injury’ Lucian Leape Error in Medicine JAMA 1994 : 272 1851 -1857 Denis Protti - University of Victoria 100
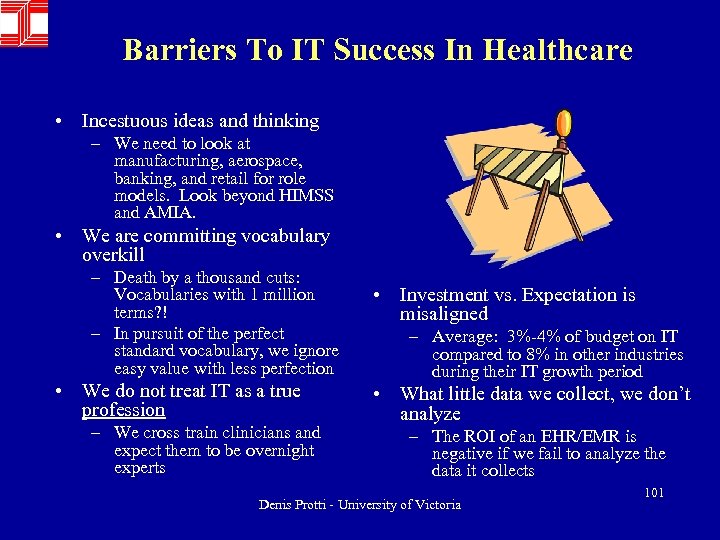
Barriers To IT Success In Healthcare • Incestuous ideas and thinking – We need to look at manufacturing, aerospace, banking, and retail for role models. Look beyond HIMSS and AMIA. • We are committing vocabulary overkill – Death by a thousand cuts: Vocabularies with 1 million terms? ! – In pursuit of the perfect standard vocabulary, we ignore easy value with less perfection • We do not treat IT as a true profession – We cross train clinicians and expect them to be overnight experts • Investment vs. Expectation is misaligned – Average: 3%-4% of budget on IT compared to 8% in other industries during their IT growth period • What little data we collect, we don’t analyze – The ROI of an EHR/EMR is negative if we fail to analyze the data it collects Denis Protti - University of Victoria 101
We must keep the faith • In hospitals in 1904 • It was not easy for all the doctors to make the change. To some of them the new way seemed more cumbersome than the old, just a lot of unnecessary red tape. • It seemed much simpler to jot down a few notes in a ledger lying open on the desk than to fill in all the blanks on a form sheet, much easier to pull out one's own volume and look up what old record was there than to call for an envelope and wait till it was brought from the file. Denis Protti - University of Victoria 102
• At first some doctors just forgot about the record blanks and used their ledgers when they were very busy, but in time they all saw the worth of the new system • (i. e. the medical record as we know it today), and it became a routine followed without question and with tremendous benefit. Those introducing IT in health care settings in the 21 st century can hope for as much success. Denis Protti - University of Victoria 103
Finite dprotti@uvic. ca Denis Protti - University of Victoria 104
304a63626f332b7779bf0240febaa452.ppt