05cc90fb5606068a7310e015e87b1d47.ppt
- Количество слайдов: 67
Hames Lecture 2011 Little r, Big R: Aristotle, Osler, and Einstein Thomas C. Rosenthal MD Professor and Chair, Family Medicine University at Buffalo Founding Director NYS AHEC System Editor: Journal of Rural Health 2000 -2009 Assoc. Editor: FP Audio Editor: Office Based Geriatrics Member: FM RRC "Medicine is a science of uncertainty and an art of probability. " Osler 1
Curtis G Hames Research Award z. Hames award recipients shall have contributed to the development of family medicine research through the course of their career. z. The Hames address will review the state of the art of family medicine research with emphasis on future developments. Thank you. 2
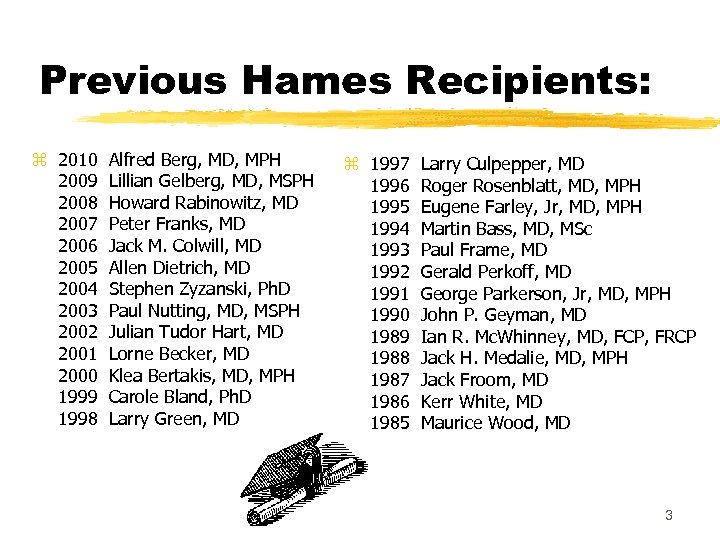
Previous Hames Recipients: z 2010 Alfred Berg, MD, MPH 2009 Lillian Gelberg, MD, MSPH 2008 Howard Rabinowitz, MD 2007 Peter Franks, MD 2006 Jack M. Colwill, MD 2005 Allen Dietrich, MD 2004 Stephen Zyzanski, Ph. D 2003 Paul Nutting, MD, MSPH 2002 Julian Tudor Hart, MD 2001 Lorne Becker, MD 2000 Klea Bertakis, MD, MPH 1999 Carole Bland, Ph. D 1998 Larry Green, MD z 1997 Larry Culpepper, MD 1996 Roger Rosenblatt, MD, MPH 1995 Eugene Farley, Jr, MD, MPH 1994 Martin Bass, MD, MSc 1993 Paul Frame, MD 1992 Gerald Perkoff, MD 1991 George Parkerson, Jr, MD, MPH 1990 John P. Geyman, MD 1989 Ian R. Mc. Whinney, MD, FCP, FRCP 1988 Jack H. Medalie, MD, MPH 1987 Jack Froom, MD 1986 Kerr White, MD 1985 Maurice Wood, MD 3
"If you see a turtle on a fence post, it had help getting there” The 150 employees of UB Family Medicine put me up onto the fence post. Thank you! 4
Family Medicine: Embracing a Continuum of FM Research z. Little ‘r’ research y. Creating new knowledge through the collection of available data from patients or records, generally in a limited time period. y. Results published. z. Big ‘R’ Research y. Creating new knowledge through the collection of data. Often involving an intervention. y. Results published. x. Often funded by external resources. x. Often funded with existing resources. Both generate important Facts. 5
Collecting new facts: EXAMPLES FROM OUR SHOP IN BUFFALO A continuum from little “r” to BIG “R”. 6
Post your question here: Family Medicine Research is Eclectic z. What do sarcomas look like before they are diagnosed? z Rosenthal TC, Kraybill W. Soft tissue sarcomas: Interfacing primary care recognition with tertiary care treatment. American Family Physician. 1999; 60: 567 -72. z. Is it time to use genetic tests to determine breast cancer risks? z Rosenthal TC, Puck SM. Breast Cancer: Screening for Genetic Risk. American Family Physician. 1999; 59: 99 -105. You have your own questions. Research starts with a systematic review, advances to a study, and expands to a publication. 7
Little “r” Research Office Funded z. Question: Does endometrial sampling by FPs produce results similar to GYNs? y 310 procedures were reviewed performed by 12 family physicians I knew. x. A personal PBRN. y. Indications, complications, and findings matched published GYN results. (Rosenthal, 1989) 8
Little “r” Research Small NYS AFP Grant z. A 76 yo woman, dies following cholecystectomy for asymptomatic gallstones. She is my patient. y 9 WNY FP Practices agree to have nurse find patients in files with asymptomatic gallstones. y. Patients charts were checked annually for 5 yrs. y 32 cases found. 8 developed symptoms. 7 had surgery. Average latency= 3 years 5 months. y Rosenthal, et al. Archives of Fam Med. 1997. 9
Little “r” Research Dept. Funding z. Will abdominal U/S improve outcomes of the “annual physical”. z. Abdominal u/s added to PEs in 189 consecutive asymptomatic patients. z 22% had unsuspected findings. y. Half of these were gallstones. x 6 (3%) patients underwent some Tx. z. U/S added little to a good physical exam. z Rosenthal TC, Siepel T, Zubler J, Horwitz M. The use of ultrasonography to scan the abdomen of patients presenting for routine physical exams. J Fam Pract. 10 1994; 38: 380 -385.
Little “r” Research Dept. Funding z What is the exposure and reaction to bashing among third-year medical students. z A survey about bashing was completed by 105 students. z 79% believed bashing was unprofessional. Bashing occurred during all clerkships. It is most common during the surgery clerkship. Object of bashing: Fam med (72%), internal medicine (40%), psychiatry (39%), and surgery (36%). z Holmes D, Tumiel-Berhalter L, Zayas LE, Watkins R. Bashing of Medical Specialties: Students’ Experiences and Recommendations. Fam Med 2008; 40(6): 400 -6. ) 11
Big “R” Research Federal Office of Rural Health z. Do rural training tracks (1 -2) graduates practice in rural communities? z. Mail survey of RTT PDs. z 76% of graduates enter rural practice. y. They pass the boards. y. Most practice within 1 mile of a hospital. z. Rural 1 -2 residencies achieve their goal. z Rosenthal TC, et. al. One-two rural residency tracks in family medicine: Are they getting the job done? Family Medicine 1998; 30: 90 -3. 12
Bid “R” Research NRSA Funded z Are poorly controlled diabetics more likely to be depressed? z The PHQ-9 was mailed to 454 patients. Responses were compared with Hb. A 1 c% and fasting blood glucose levels. z There is a modest but significant correlation between FBG and PHQ-9 scores. (p = 0. 015). z Poorly controlled diabetes should be screened for depression. Kahn, L. et. al. Fasting Blood Glucose and Depressive Mood Among Patients with Mental Illness in a Medicaid Managed Care Program. Depression Research and Treatment Journal. 2011 13
Big “R” Research NIH Funded Research z Buprenorphine or methadone: Is one more effective for opiate withdrawal? z Observational study evaluated completion rates of patients over a 13 -month period when buprenorphine replaced methadone for shortterm opiate detoxification. z The pts treated with buprenorphine were more likely to complete detoxification. (P<. 001). z Blondell RD, Smith SJ, Servoss TJ, De. Vaul SK, Simons RL. Buprenorphine and Methadone: A Comparison of Patient Completion Rates During Inpatient Detoxification. Journal of Addictive Diseases. 2007; 26(2): 3 -11. 14
Big “R” Research Funded by New York State Department of Mental Health funds. z If patients with psychiatric emergencies are also connected to primary care do they do better? z Patients were randomized to case management or usual care. Variables tracked: primary care entry, comorbidity, insurance, hospital admission, case management and mental health linkages. z At 3 months 57% of the case management group was linked to primary care compared with 16% of the usual care group (P <. 001) z Griswold KS, et. al. Connections to primary medical care after psychiatric crisis. J Am Board Fam Pract. 2005 May-Jun; 18(3): 166 -72. 15
Big “R” Research Funded by Agency for Health Research and Quality z How can Family Medicine office teams identify and improve on patient safety concerns? z Staff and providers identified office functions that suggest patient safety risk. Qualitatively analyzed responses were presented to providers and staff in joint session. z There was high concordance between priorities identified by physicians, nursing and staff yet each site was unique. z Identified areas of concern decreased by 35% over 12 months. z Singh, R. , A. Singh, et al. (2006). "Building learning practices with self-empowered teams for improving patient safety. " J Health Management 8(1): 91 -118. 16
Big “R” Research Agency for Health Research and Quality: AHRQ R 03 H 5016031 z Can FP offices do more to help patients with CKD? z Using practice enhancement assistants, computer decision support, and academic detailing, a rapid-cycle quality improvement process was implemented. z Recognition and treatment of CKD led to lower GFRs! z Fox, C. J Am Board Fam Med 2008; 21: 522– 30. 17
Family Physicians Must Seek Answers to Clinical Questions z“No matter how many molecular discoveries we make at the laboratory bench, they can only be translated into remedies by physicians who engage in clinical investigation” (Levine, 2004) To Meet the Challenge: 1. Understand what we do. 2. Champion the difference in our research. 18
Understanding we do. And why our research is so important. 19
The Einstein Effect Consilience Gradually a sense of unity has been lost in the increasing fragmentation and specialization of knowledge. E. O. Wilson, 1998 20
Our perspective is undifferentiated 21
Family Medicine is Complex 22
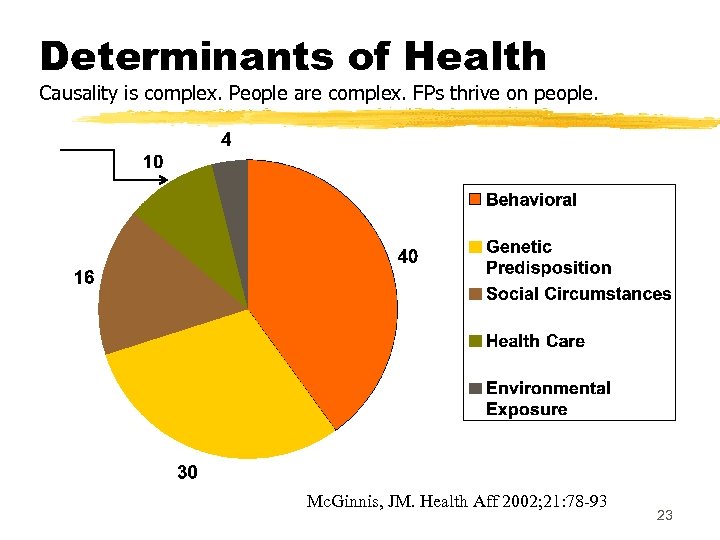
Determinants of Health Causality is complex. People are complex. FPs thrive on people. Mc. Ginnis, JM. Health Aff 2002; 21: 78 -93 23
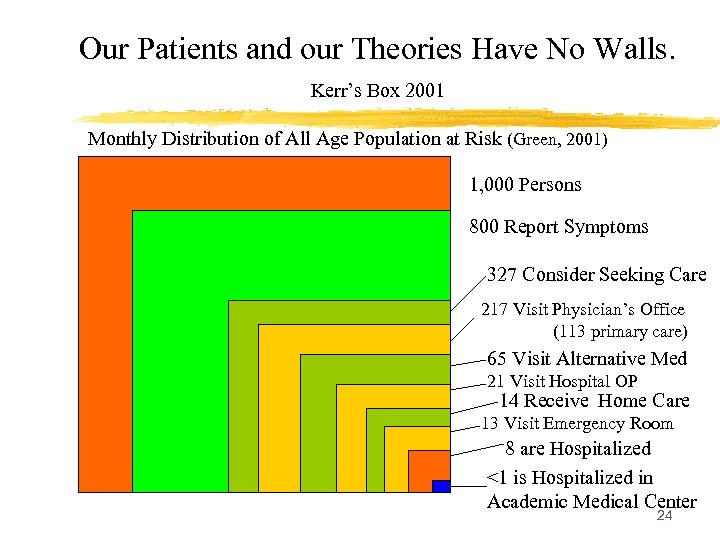
Our Patients and our Theories Have No Walls. Kerr’s Box 2001 Monthly Distribution of All Age Population at Risk (Green, 2001) 1, 000 Persons 800 Report Symptoms 327 Consider Seeking Care 217 Visit Physician’s Office (113 primary care) 65 Visit Alternative Med 21 Visit Hospital OP 14 Receive Home Care 13 Visit Emergency Room 8 are Hospitalized <1 is Hospitalized in Academic Medical Center 24
Complexity z “The higher we go on the scale of specialized practice, the less complex medical decision making becomes. ” z How Doctors Think by Jerome Groopman, M. D. pg. 99 z 80% of Medicare patients have 4 or more chronic conditions. – Valderas, 2009 z Family physicians’ patients are different. y. CHF with normal LVEF is common. (James, 1999) z Every office visit is complicated by Competing Demands. (Jaen, 1994) 25
Randomized Controlled Trials Great for understanding disease and drugs. Not so good for understanding People. z. The RCT selects a thousand patients and one disease in order to screen out individual patient variables. z. Family docs encounter one patient and attempt to understand a dozen variables that impact one or several conditions. 26
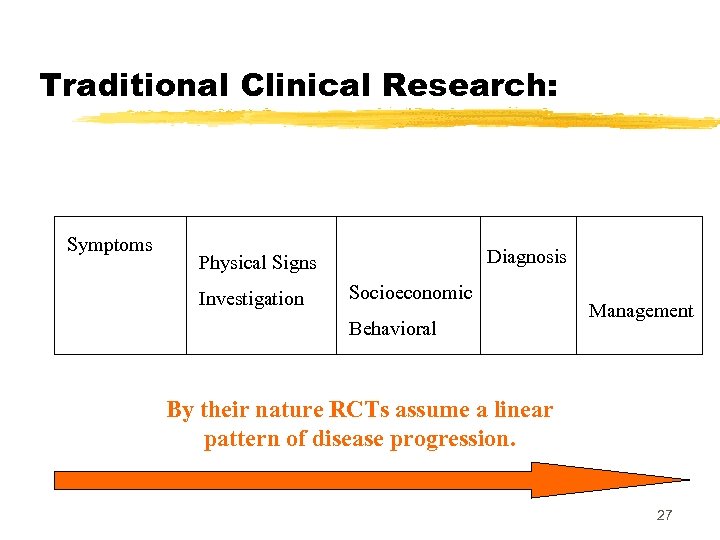
Traditional Clinical Research: Symptoms Diagnosis Physical Signs Investigation Socioeconomic Behavioral Management By their nature RCTs assume a linear pattern of disease progression. 27
Are Patients linear creatures? 28
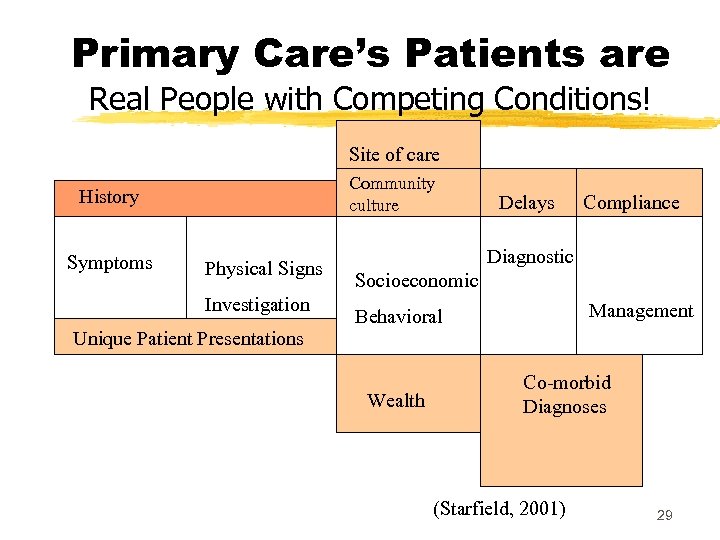
Primary Care’s Patients are Real People with Competing Conditions! Site of care Community culture History Symptoms Physical Signs Investigation Unique Patient Presentations Delays Compliance Diagnostic Socioeconomic Management Behavioral Wealth Co-morbid Diagnoses (Starfield, 2001) 29
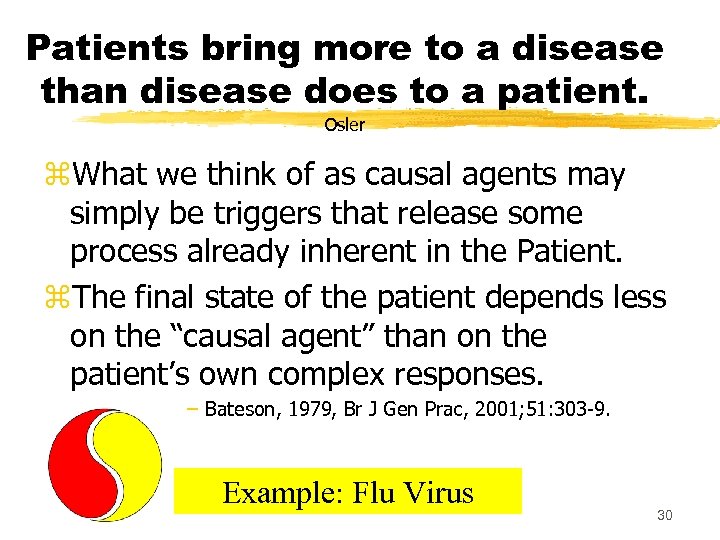
Patients bring more to a disease than disease does to a patient. Osler z. What we think of as causal agents may simply be triggers that release some process already inherent in the Patient. z. The final state of the patient depends less on the “causal agent” than on the patient’s own complex responses. – Bateson, 1979, Br J Gen Prac, 2001; 51: 303 -9. Example: Flu Virus 30
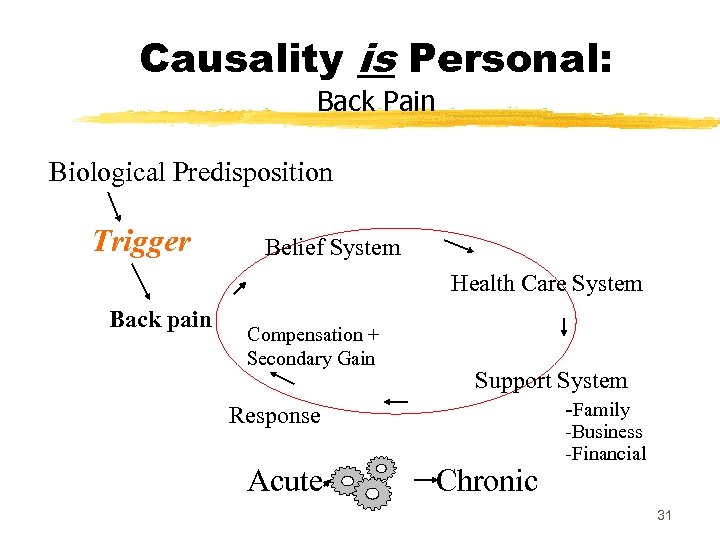
Causality is Personal: Back Pain Biological Predisposition Trigger Belief System Health Care System Back pain Compensation + Secondary Gain Response Acute Support System -Family Chronic -Business -Financial 31
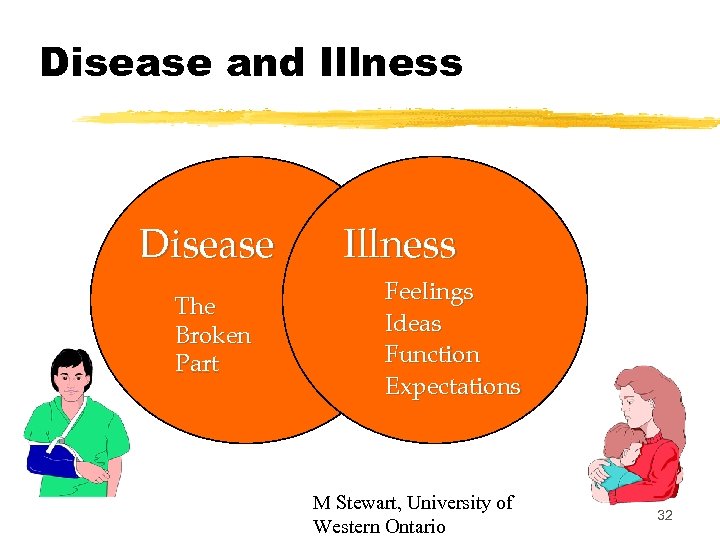
Disease and Illness Disease The Broken Part Illness Feelings Ideas Function Expectations M Stewart, University of Western Ontario 32
Not only do we see problems differently, but: Family Physician Solve Problems Differently 33
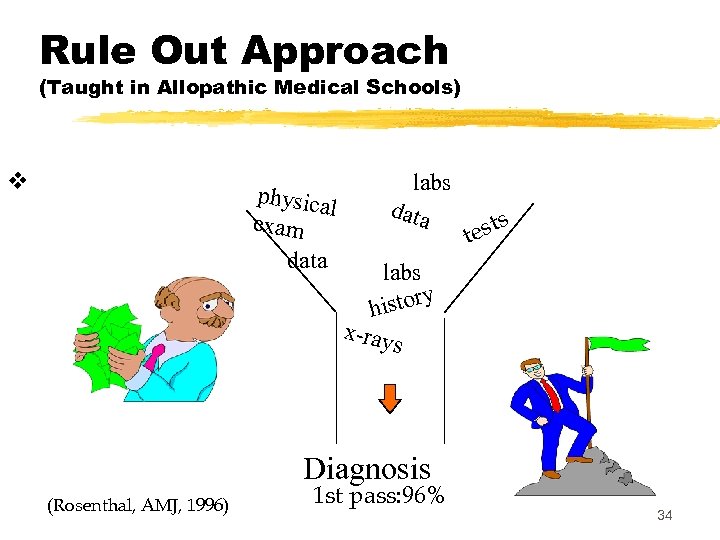
Rule Out Approach (Taught in Allopathic Medical Schools) v physica l exam data labs data sts te labs istory h x-ray s Diagnosis (Rosenthal, AMJ, 1996) 1 st pass: 96% 34
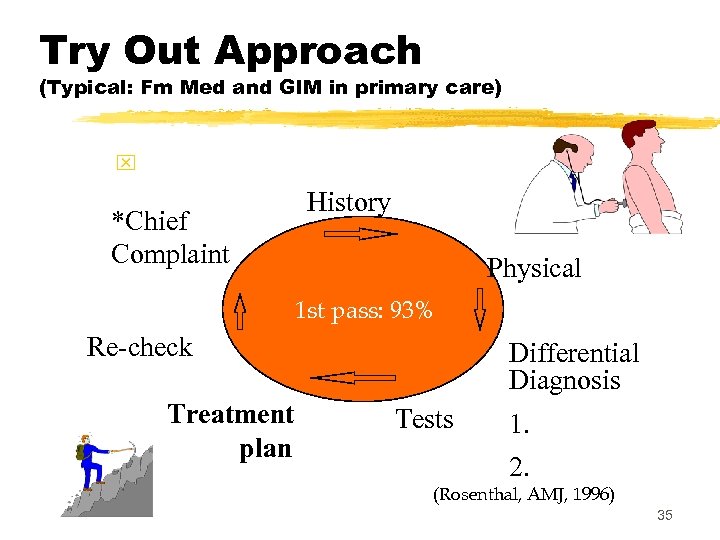
Try Out Approach (Typical: Fm Med and GIM in primary care) x *Chief Complaint History Physical 1 st pass: 93% Re-check Treatment plan Differential Diagnosis Tests 1. 2. (Rosenthal, AMJ, 1996) 35
The Specialist’s Task vs the Generalist’s Task z. Specialists do the right thing to the patient. z. Family doctors get the patient to do the right thing. These activities require: ~ Communication skills. ~ Continuity relationships with patients. ~ Passions for different career rewards. 36
Change, Continuity, Time z. Change takes time! y. Patients have capacity to change in their own best interest. y. A doctor-patient relationship develops like scaffolding, incrementally, like all human relationships. (Pink, 2006) y. Continuity of care improves outcomes. x. Meta-analysis of continuity + 81 care outcomes: • 41 were significantly improved by continuity. – Expenditures were significantly lower. (Saultz, 2005) Chinese Proverb: A journey of a 1000 miles starts one step at a time. 37
Complex Skills: Family Medicine z. Life Skills: Those skills that cut across life’s relationships. y. Communicating y. Motivating y. Engaging y. Problem solving y. Multi-tasking z. Treatment Skills: Those skills used in the treatment of disease. y. Diagnosing y. Medicating y. Operating y. Referring All are important to primary care and researchable! 38
Epistemology Theory of Knowledge: We use information differently. z There are 2 distinct types of knowledge: y. Knowing “that” as in “I know that. ” x. Ex: 2+2=4. Accumulated facts. x. Demanded of Specialists. y. Knowing “how” as in “I know how. ” x. Ex: Knowing how to add any number. Problem Solving. x. Demanded of Generalists. Facts Knowledge Experience 39
Champion our difference in our research. 40
Getting to Research in 31 days. The one month plan. Aka: The little r plan. Aka: The “Osler Plan”. (Gordon, 1978) A protocol for initiating research in practice. 41
Creation: Your Researchable Question z. Day One through Five y. Every working hour write a patient management question you encountered. y. Use Post-ups: One question per post-up. z. Day Six (Saturday#1) y. Arrange, re-arrange post-ups according to categories. y. Consolidate repeats and near repeats. y. Match your curiosity and passion to a question. 42
Creation: Your Researchable Question z. Day 7 (Sunday #1 and RRC compliant) y. Rest and contemplate. z. Day 8 and 9 y. See patients again. z. Day 10 (one hour) y. Present question to a multidisciplinary research team. y. Refine question. y. Review compatible research methods. 43
Creation: Your Researchable Question z. Day 13 (Saturday#2) y. Literature search. z. Day 14 (Sunday #2) y. Rest and contemplate. z. Day 17 (one hour) y. Present results of literature search to team. y. Refine methodology. 44
Creation: Your Researchable Question z. Day 20 (Saturday #3) y. Draft Research Plan with team. y. Draft Anticipated Results. x. In this step calculate power, refine methods, define bias. z. Day 21 (Sunday #3) y. Rest and contemplate. z. Day 24 (one hour) y. Review protocol and anticipated results with team, identify gaps. 45
Creation: Your Researchable Question z. Day 27 (Saturday #4) y. Fill in gaps. y. Draft IRB approval forms. z. Day 28 (Sunday #4) y. Rest and contemplate. z. Day 31 (one hour) y. Team drafts time line, need for resources and project start date. x See work sheet: (Gordon, 1978) 46
Comparing Observation to RCTs z. Generally: Good correlation between RCTs and non-RCTs. y 84% within calculated study error margin. x. Non-RCTs tend to show greater treatment effects. z. Non-RCTs include more heterogeneous study populations. (Ioannidis, 2001)(Starfield, 2001) z. Mixed Methods (Qual + Quant) (Creswell, 2004) “There is tenure in observation for all of us. ” Larry Green, 1987 47
Comparative Effectiveness Research z. Treatment is a balance of benefits and harms. z. When the risks associated with one procedure outweigh its clinical benefits or the clinical benefits of an alternate treatment, it is appropriate and ethical to limit its use. An Emerging Opportunity for Family Medicine 48
Don’t forget: Case Reports z“Publish short notes on anything that is striking” William Osler MD y. A case report in 1978 led to a 1980 paper published in the NEJM relating tampon use to toxic shock syndrome. (Todd, 1978) y. AIDS first described in a case report in 1981. (Gottleib, 1981) Emphasizing the importance of each patient! 49
Family medicine reaches full potential through Research Aristotle: Modes of Persuasion from “Rhetoric” z. Pathos: Appeals to emotion and passion. z. Logos: Relies on reason, order and knowledge. y Can be replicated. z. Ethos: “Believability” y. Moral competence. y. Expertise. y. Acquired over time. y. Influenced by values of the culture. y. Ethos is granted by the audience. 50
Research Changes Ethos: z. Ethos responds to new ideas or forces. y. Practice rewards the clinician. y. Research rewards the scholar. y. Writing rewards everyone. z. Generate Pathos and Logos y. And you have done good. z. Change Ethos: and you have done Great! Does PCMH = Changed Ethos? 51
A Unique Knowledge Base for Family Medicine z. Self-reflective practice by clinicians. z. Involving the patient voice in generating research questions and interpreting data. z. Inquiry into the systems affecting health care. z. Investigation of disease phenomena and treatment effects in patients over time. Stange KC, Miller WL, Mc. Whinney I. Developing the Knowledge Base of Family Practice. Fam Med 2001; 33(4): 286 -97. 52
Conclusion: Good to great! z. Family medicine research is essential research. z. Like Einstein, we need to connect facts to concepts. z. Like Aristotle we need to write. z. Like Osler, we need to inspire fundamental change. 53
Seek and ye shall discover! “It is more important to understand what sort of patient has a disease that what sort of disease has a patient. ” Osler. 54
Bibliography z Aldrich R, Kemp L, Williams JS, Harris E, Simpson S, Wilson A, Mc. Gill K, Byles J, Lowe J, Jackson T. Using socioeconomic evidence in clinical practice guidelines. BMJ 2003; 327: 1283 -5. z Ayanian JZ. Generalists and specialists caring for patients with heart disease: United we stand, divided we fall. Am J Med 2000; 108: 25961. 55
Bibliography z Barnato AE, Labor RE, Freeborne NE, Jayes RL, Campbell DE, Lynn j. Qualitative analysis of Medicare claims in the last 3 years of life: a pilot study. J Am Geriatrics Soc. 2005; 53: 66. z Bertram DA, Rosenthal TC. Implementation of an in-patient case management program in rural hospitals. J Rural Health. 1996 Winter; 12: 54 -66. z Birtwhistle RV, Godwin MS, Delva MD, Casson RI, Lam M, Mac. Donald SE, Sequin R, Ruhland L. Randomized ewuivalence trial comparing three month and six month follow up of patients with hipertension by family practitioners. BMJ 2004; Jan 15. 56
Bibliography z Borkan JM. Mixed Methods Studies: A Foundation for Primary Care Research Annals of Family Medicine 2: 4 -6 (2004) z Creswell JW, Fetters MD, Ivankova NV. Designing A Mixed Methods Study In Primary Care. Annals of Family Medicine 2: 7 -12 (2004) z Curtis P, Dickinson P, Steiner J, Lanphear B, Vu K. Building capacity for research in family medicine: is the blueprint faulty? Fam Med. Feb 2003; 35(2): 124 -130. z Doescher MP, Saver BG, Fiscella K, Franks P. Preventive Care: Does continuity count? J Gen Int Med. 2004; 19: 632. 57
Bibliography z Easterbrook G. The Progress Paradox: How life gets better while prople feel worse. Random House. 2003 z Ely JW, Osheroff JA, Ebell MH, et al. Obstacles to answering doctors’ questions about patient care with evidence: qualitative study. BMJ 2002; 324: 710. z Fan VS, Burman M, Dc. Donell MB, Fihn SD. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Int Med. 2005; 20: 226. 58
Bibliography z Godon MJ. Research Workbook: A guide for initial planning of clinical, social, and behavioral research projects. J Fam Pract. 1978; 7: 145 -60. z Gottlieb GJ, Ragaz A, Vogel JB, Friedman-Kien A, Rywiln AM, Weiner EA, Ackerman AB. A preliminary communication on extensively disseminated Kaposi’s sarcoma in a young homosexual men. Amer J Dermatopathology 1981; 3: 111 -4. z Green LA, Fryer GE, Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. NEJM 2001; 344: 2021 -2025. z Hjortdahl P, Borchgrevink CF. Continuity of care: influence of general practitioners’ knowledge about their patients on use of resources in consultations. BMJ. 1991; 303: 1181 -4. z Hurwitz B, Vass A. What’s a good doctor, and how can you make one? BMJ 2002; 325: 667 -8. 59
Bibliography z Ioannidis JPA, Haidich AB, Pappa M, Pantazis N, Kokori SI, Tektonidou MG, Contopoulos-Ioannidis DG, Lau J. Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA 2001; 286: 821 -30. z Institute of Medicine. A manpower policy for primary health care (IOM Publication 78 -02) Washington, DC: National Academy of Sciences. 1978. z Jaen, C. R. , K. C. Stange, et al. (1994). "Competing demands of primary care: a model for the delivery of clinical preventive services. " J Fam Pract 38(2): 166 -171. z Jan M. De Maeseneer, Lutgarde De Prins, Christiane Gosset, and Jozef Heyerick. Provider Continuity in Family Medicine: Does It Make a Difference for Total Health Care Costs? Ann Fam Med 2003 1: 144 -148. 60
Bibliography z James, P. A. , T. M. Cowan, et al. (1999). "Heart failure in primary care: measuring the quality of care. " J Fam Pract 48(10): 790 -798. z Kahn NB. The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004; 2(Supp 1): S 3 S 32. z Kwok RHM. Chinese-restaurant syndrome. N Eng J Med. 1968; 278: 796. z Leichter HM. “Evil Habits” and “Personal Choices”: Assigning responsibility for health in the 20 th century. Milbank Quarterly 2003; 81: 603 -626. z Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001; 322: 336 -342 61
Bibliography z Magee M, D’Antonio M. The Best Medicine. St. Martin’s Press, NY. 1999 z Maguire P, Pitceathly C. Key communication skills and how to acquire them. BMJ 2002; 325: 697 -700. z Mahoney MC, Verma P, Morantz S. Research Productivity Among Recipients of AAFP Foundation Grants. Ann Fam Med 2006; 5: 143 -145. z Nutting PA, Meredith A. Goodwin, Susan A. Flocke, Stephen J. Zyzanski, and Kurt C. Stange. Continuity of Primary Care: To Whom Does It Matter and When? Ann Fam Med 2003 1: 149 -155. 62
Bibliography z Parchman M, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med 2004; 36: 22 -7. z Pellegrino ED. Ethics and the moral center of the medical enterprise. Bull NY Acad Med. 1978; 54: 625 -40 Piccone G, Sloan F, Taylor D. Effects of risk and time preference and expected longevity on demand for medical tests. J Risk and Uncertainty. 2004; 28(1): 39 -53. 63
Bibliography z Rosenthal TC. Localized fibrous mesothelioma in the post partum period. J Fam Med, 1987; 25: 174 -175. z Rosenthal TC, et al. Endometrial Sampling: a retrospective chart review of 310 procedures performed by family physicians. J Fam Pract 1989; 29: 249 -256. z Rosenthal TC, Riemenschneider T, Feather J. A generalist-patientspecialist alliance for the nineties. Amer J Med. 1996 March; 100: 338 -343. z Rosenthal TC, Kraybill W. Soft tissue sarcomas: Interfacing primary care recognition with tertiary care treatment. American Family Physician. 1999; 60: 567 -72. 64
Bibliography z Shaughnessy AF, Slawson DC, Bennett JG. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994; 39: 489 -99. z Stange KC, Hekelman FP. Mentoring needs and family medicine faculty. Fam Med. May-Jun 1990; 22(3): 183 -185. z Starfield, B. New paradigms for quality in primary care. Br. Jour. GP 2001; 51: 303 -9. z Starfield, B. , L. Shi, et al. (2005). "The Effects Of Specialist Supply On Populations' Health: Assessing The Evidence. " Health Aff (Millwood). 65
References z Thomas P, The Research needs of primary care. BMJ. 2000; 321: 2 -3. z Todd J, Fishaut M, Kapral F, Welch T. Toxic-shock syndrome associated with phage-group-1 staphylococci. Lancet 1978; 2: 1116 -8. z Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003; 290: 1624 -32. 66

Bibliography z Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: Implications for understanding health and health services. Ann Fam Med 2009; 7: 357 -63. z Volk RJ, Spann SJ, Cass AR, Hawley ST. Patient Education for Informed Decision Making About Prostate Cancer Screening: A Randomized Controlled Trial with 1 -Year Follow-Up. Annals of Family Medicine 2003; 1: 22 -28. z Warburton RN. What do we gain from the sixth coronary heart disease drug? BMJ 2003; 327: 1237 -8. z Wilson EO. Consilience: The Unity of Knowledge, 1998 z Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Services Research 2002; 37: 1509 -1529. 67
05cc90fb5606068a7310e015e87b1d47.ppt