f24e87d0f731bbad93f1bc377d6f1ae8.ppt
- Количество слайдов: 55
(HA)ART Making ART Possible An Update on Assisted Reproductive Technology and HIV Nikole D. Gettings, MSN, CNM Clinical Services Coordinator Memphis Center for Reproductive Health 1726 Poplar Ave Memphis TN 38104 ngettings@mcrh-tn. org
Objectives • • • After today’s sessions the learner will: Understand the history of fertility recommendations for individuals living with HIV Understand updated guidelines regarding fertility recommendations for individuals living with HIV from Center for Disease Control [CDC], American Congress of Obstetricians and Gynecologists [ACOG], and American Society for Reproductive Medicine [ASRM]. Gain awareness of assisted reproductive technology [ART] procedures available to individuals living with HIV Identify resources in literature for clinical guidance in care and expected outcomes of fertility programs offering services to individuals living with HIV Discuss applicability of guideline recommendations for fertility planning in adolescent populations and identify local resources, or gap in resources for fertility services for HIV positive individuals.
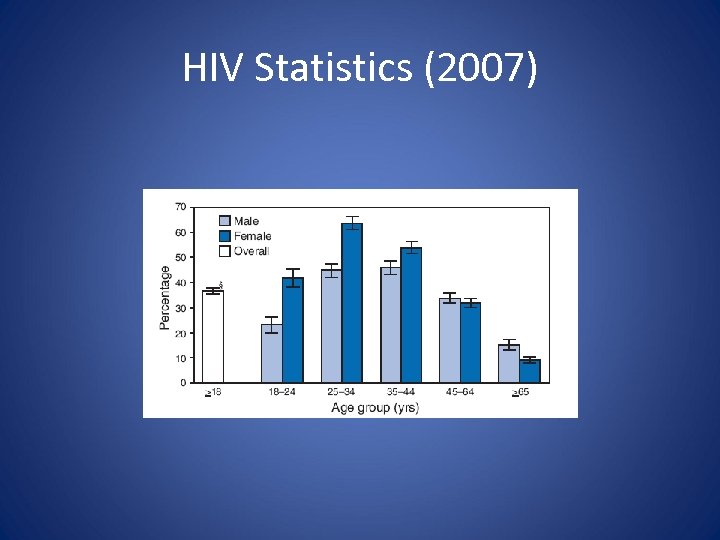
HIV Statistics (2007)
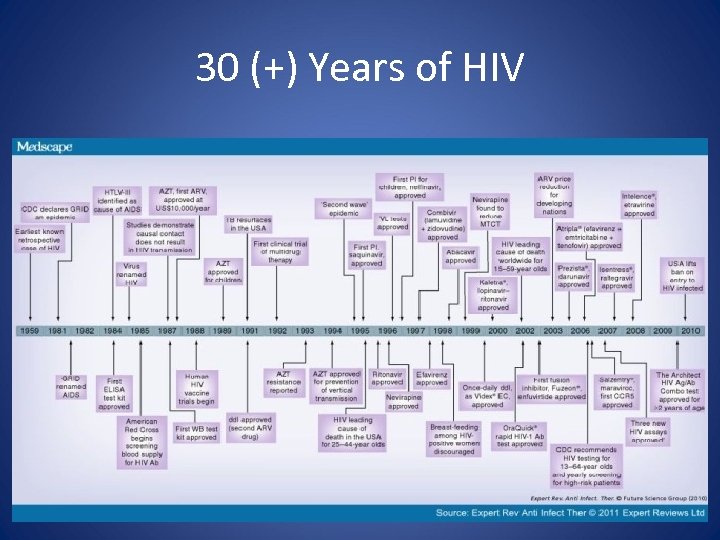
30 (+) Years of HIV
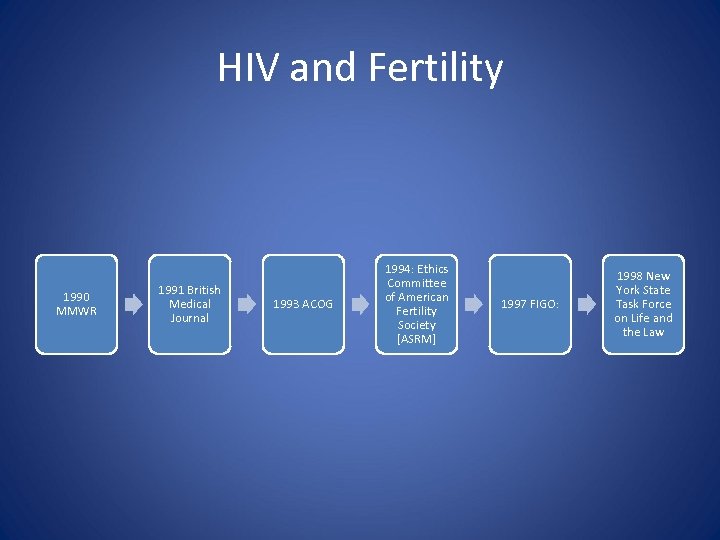
HIV and Fertility 1990 MMWR 1991 British Medical Journal 1993 ACOG 1994: Ethics Committee of American Fertility Society [ASRM] 1997 FIGO: 1998 New York State Task Force on Life and the Law
![[Procreation] is central to personal identity, to dignity and to the meaning of one’s [Procreation] is central to personal identity, to dignity and to the meaning of one’s](https://present5.com/presentation/f24e87d0f731bbad93f1bc377d6f1ae8/image-6.jpg)
[Procreation] is central to personal identity, to dignity and to the meaning of one’s life ~ Robertson (1994)

Italy, 1992 Augusto E. Semprini
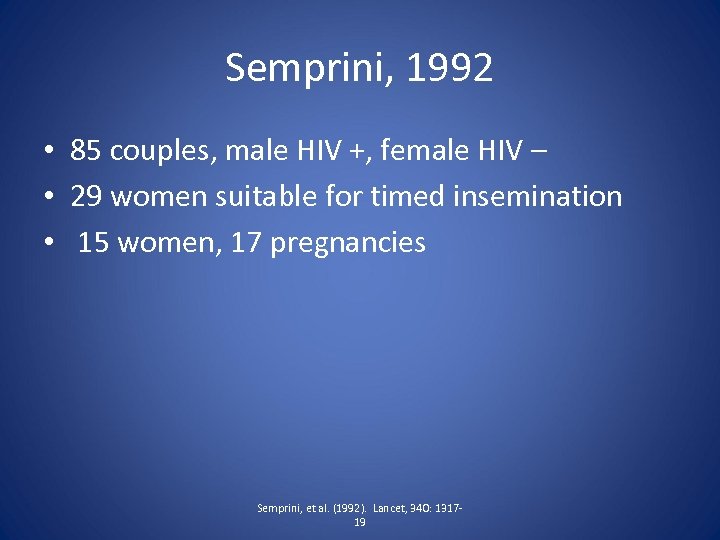
Semprini, 1992 • 85 couples, male HIV +, female HIV – • 29 women suitable for timed insemination • 15 women, 17 pregnancies Semprini, et al. (1992). Lancet, 340: 131719
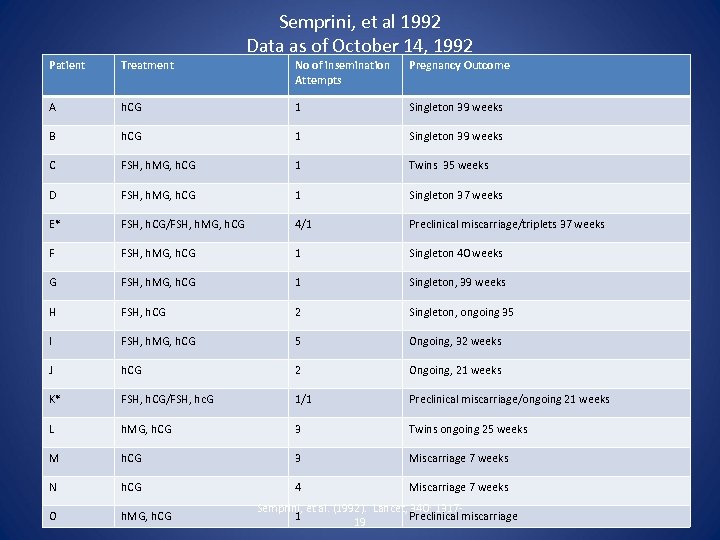
Semprini, et al 1992 Data as of October 14, 1992 Patient Treatment No of insemination Attempts Pregnancy Outcome A h. CG 1 Singleton 39 weeks B h. CG 1 Singleton 39 weeks C FSH, h. MG, h. CG 1 Twins 35 weeks D FSH, h. MG, h. CG 1 Singleton 37 weeks E* FSH, h. CG/FSH, h. MG, h. CG 4/1 Preclinical miscarriage/triplets 37 weeks F FSH, h. MG, h. CG 1 Singleton 40 weeks G FSH, h. MG, h. CG 1 Singleton, 39 weeks H FSH, h. CG 2 Singleton, ongoing 35 I FSH, h. MG, h. CG 5 Ongoing, 32 weeks J h. CG 2 Ongoing, 21 weeks K* FSH, h. CG/FSH, hc. G 1/1 Preclinical miscarriage/ongoing 21 weeks L h. MG, h. CG 3 Twins ongoing 25 weeks M h. CG 3 Miscarriage 7 weeks N h. CG 4 Miscarriage 7 weeks O h. MG, h. CG Semprini, et al. (1992). Lancet, 340: 13171 Preclinical miscarriage 19
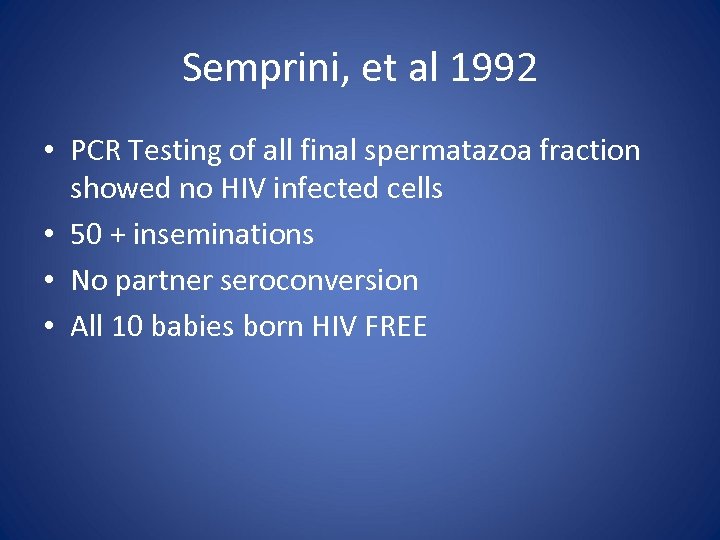
Semprini, et al 1992 • PCR Testing of all final spermatazoa fraction showed no HIV infected cells • 50 + inseminations • No partner seroconversion • All 10 babies born HIV FREE
Mandelbrot et al. , 1997 • • • 92 HIV serodiscordant couples (male HIV +) unprotected intercourse only at ovulation Protected intercourse at all other times 104 pregnancies 4 maternal seroconversions (4. 3%) Mandelbrot, L, Heard I, Henrion-Geant, E, Henrion, R (1997). Natural conception in HIV-negative women with HIV-infected
1999 International Perinatal HIV Group • 1: 500 to 1: 1000 for each single act of intercourse The International Perinatal HIV Group. (1999) The mode of delivery and the risk of vertical transmission of human immunodeficiency virus type 1, a meta-analysis of 15 prospective cohort studies. New England Journal of Medicine; 340: 977 -987
Reproductive Desire • 1440 HIV patients • 29% of both women and men desired children • 69% of women and 59% of men realistically expected to have 1 or more children Chen, JL (2001): Fertility desires and intentions of HIV-positive men and women. (2001) Family Planning Perpectives; 33: 144
Women Living Positive Survey, December 2006 -March 2007 700 Women 227 had been pregnant 39% had children 48% “never asked by provider if they were pregnant or thinking about getting pregnant” • 57% never discussed appropriate treatment before becoming pregnant • 61% personally believed they could have children with appropriate medical care • 59% felt society strongly urges them not to have children • • Squires, et al. (2011). Health needs of HIV-infected women in the United XStates: Insights from the women living positive survey. AIDS Patient Care and STDs: 25: 1 -7
CDC 1990 For any couple with one or both partners infected with HIV abstain from engaging in sexual activities or consistently use condoms Center for Disease Control. (1990). HIV-1 infection and artificial insemination with processed semen. MMWR; 39: 249 -256
Ethical Concerns • Creation of child infected with HIV • Premature death of parents • Transmission of virus: Medical staff, partner, other couples
Sperm Washing Thanks to the work of Semprini and others, there has been a large shift in fertility options for HIV affected couples and the biomedical ethics around this issue
Principles of Bioethics • Autonomy • Beneficence • Justice
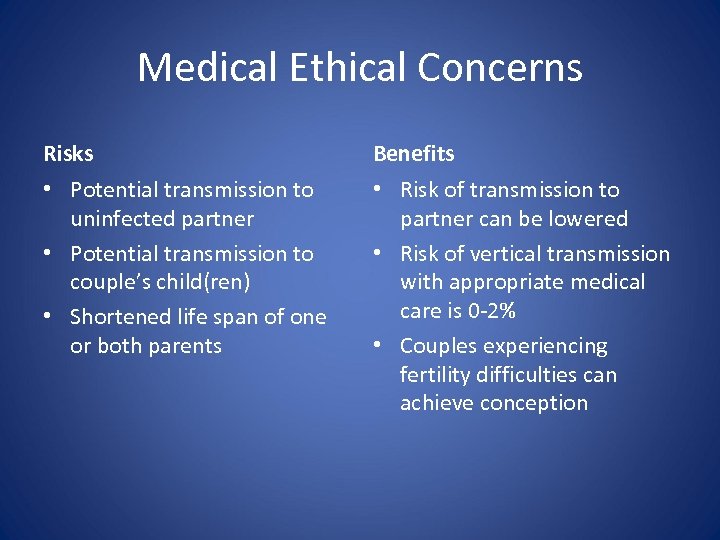
Medical Ethical Concerns Risks Benefits • Potential transmission to uninfected partner • Potential transmission to couple’s child(ren) • Shortened life span of one or both parents • Risk of transmission to partner can be lowered • Risk of vertical transmission with appropriate medical care is 0 -2% • Couples experiencing fertility difficulties can achieve conception
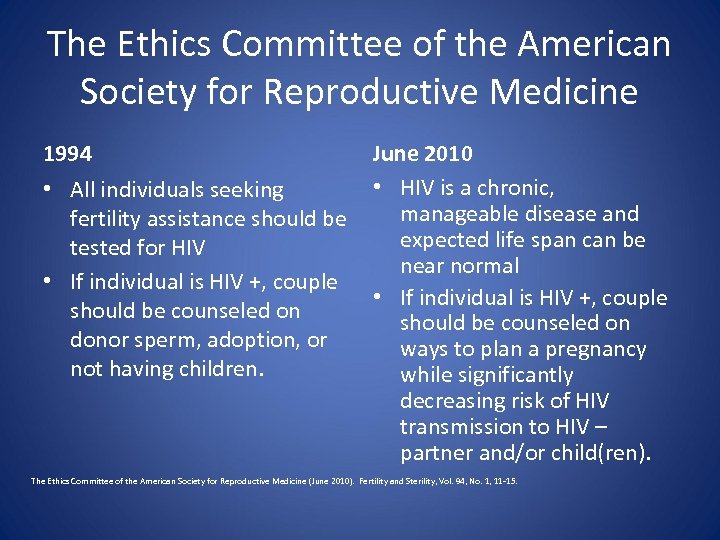
The Ethics Committee of the American Society for Reproductive Medicine 1994 • All individuals seeking fertility assistance should be tested for HIV • If individual is HIV +, couple should be counseled on donor sperm, adoption, or not having children. June 2010 • HIV is a chronic, manageable disease and expected life span can be near normal • If individual is HIV +, couple should be counseled on ways to plan a pregnancy while significantly decreasing risk of HIV transmission to HIV – partner and/or child(ren). The Ethics Committee of the American Society for Reproductive Medicine (June 2010). Fertility and Sterility, Vol. 94, No. 1, 11 -15.
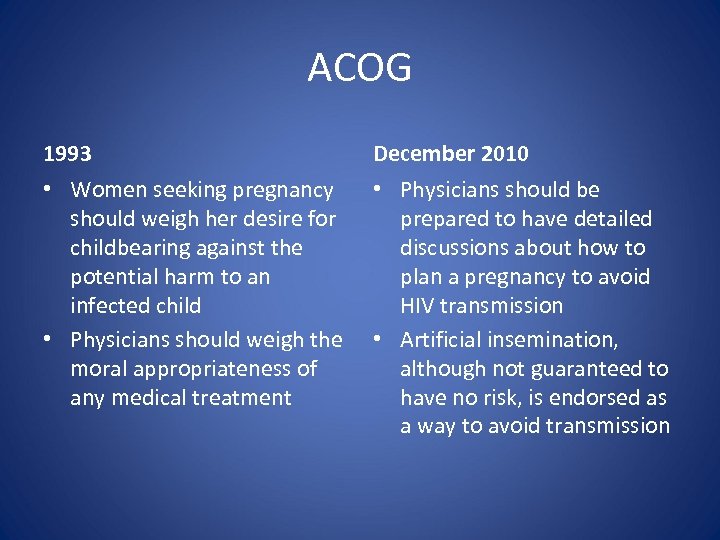
ACOG 1993 December 2010 • Women seeking pregnancy should weigh her desire for childbearing against the potential harm to an infected child • Physicians should weigh the moral appropriateness of any medical treatment • Physicians should be prepared to have detailed discussions about how to plan a pregnancy to avoid HIV transmission • Artificial insemination, although not guaranteed to have no risk, is endorsed as a way to avoid transmission
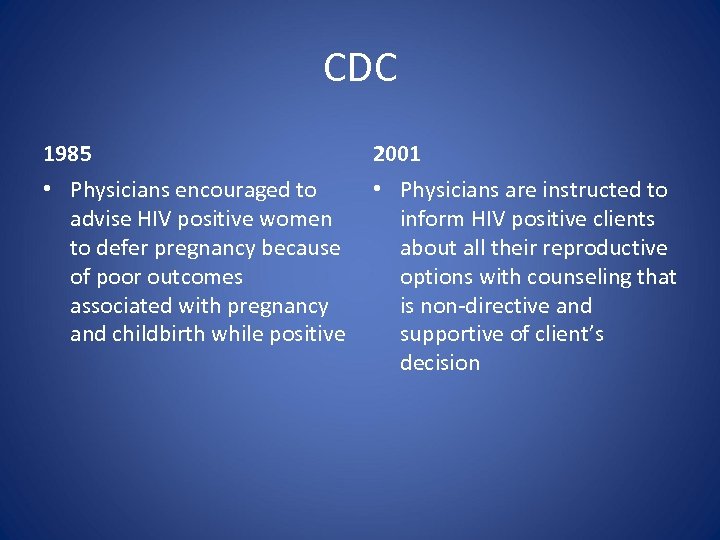
CDC 1985 2001 • Physicians encouraged to advise HIV positive women to defer pregnancy because of poor outcomes associated with pregnancy and childbirth while positive • Physicians are instructed to inform HIV positive clients about all their reproductive options with counseling that is non-directive and supportive of client’s decision
Preconception Care No smoking Avoidance of STD’s Avoid substance abuse Increase folic acid Vaccines for hepatitis A & B Pneumococcal and influenza
STD Testing

Eligibility for ART Programs
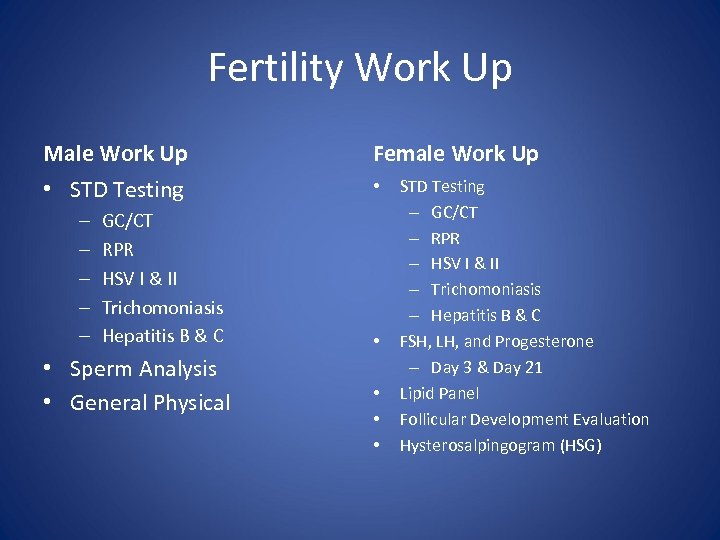
Fertility Work Up Male Work Up Female Work Up • STD Testing • – – – GC/CT RPR HSV I & II Trichomoniasis Hepatitis B & C • Sperm Analysis • General Physical • • STD Testing – GC/CT – RPR – HSV I & II – Trichomoniasis – Hepatitis B & C FSH, LH, and Progesterone – Day 3 & Day 21 Lipid Panel Follicular Development Evaluation Hysterosalpingogram (HSG)
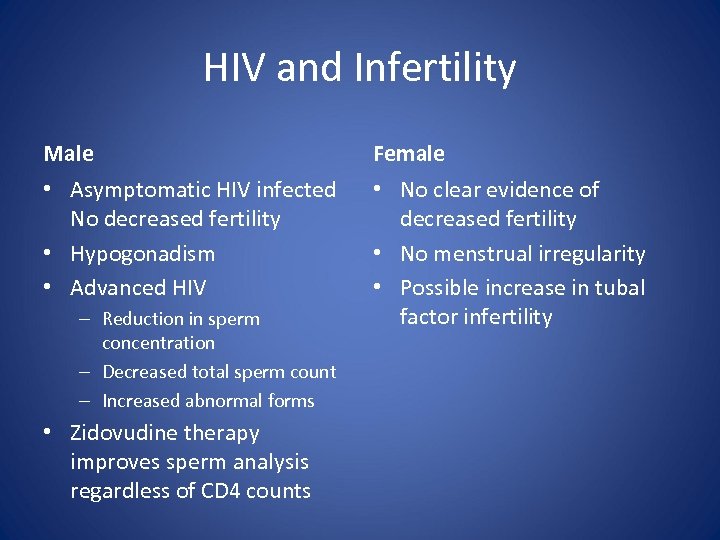
HIV and Infertility Male Female • Asymptomatic HIV infected No decreased fertility • Hypogonadism • Advanced HIV • No clear evidence of decreased fertility • No menstrual irregularity • Possible increase in tubal factor infertility – Reduction in sperm concentration – Decreased total sperm count – Increased abnormal forms • Zidovudine therapy improves sperm analysis regardless of CD 4 counts
Serodiscordant: HIV + Female/HIV - Male • Insemination with partner’s sperm at ovulation • Insemination with donor sperm • In-vitro Fertilization • Intracytoplasmic sperm injection
Home Insemination (HIV + Female/HIV – Male) • Male ejaculates in clean, dry container (glass jar, sterile urine cup) • Fresh sperm is drawn up into syringe (no needle) • Place syringe into vagina and depress plunger or place sperm in cervical cap or diaphragm and place in vagina • Recommendations regarding timing: Based on ovulation (every other day starting at cycle day 5 until menses or + pregnancy test) • Syringe is re-useable but should be cleaned and dried thoroughly
Donor Sperm
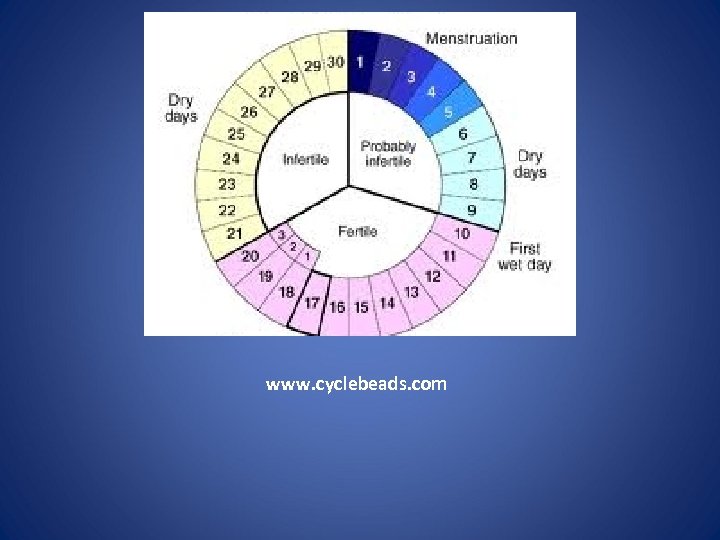
www. cyclebeads. com

www. fertilityfriend. com
Serodiscordant: HIV + Male/HIV - Female • Sperm washing followed by insemination via intrauterine insemination or intracytoplasmic sperm injection (ICSI) • Timed, unprotected intercourse around ovulation • PEP • Donor insemination
Sperm Washing
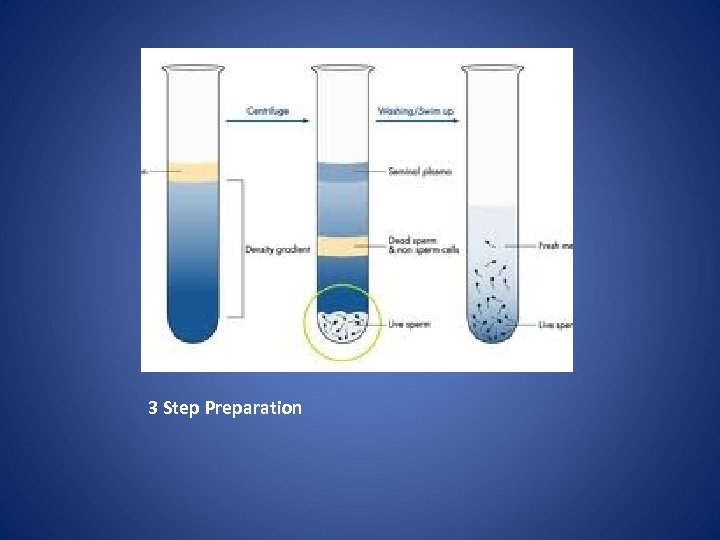
3 Step Preparation
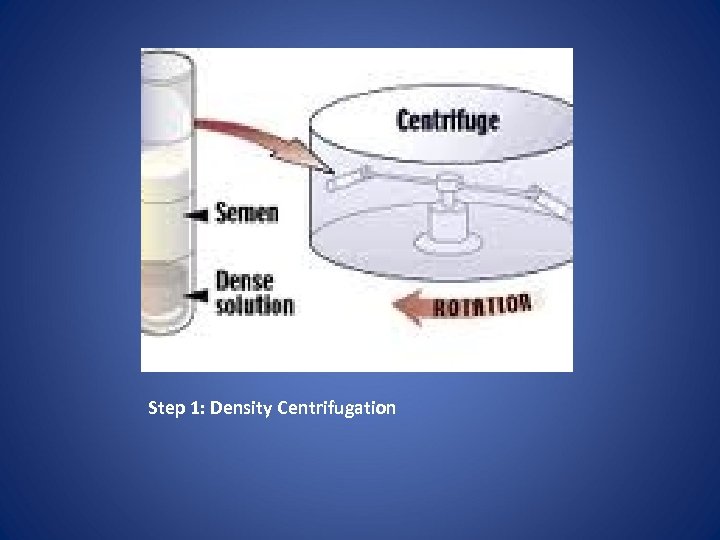
Step 1: Density Centrifugation
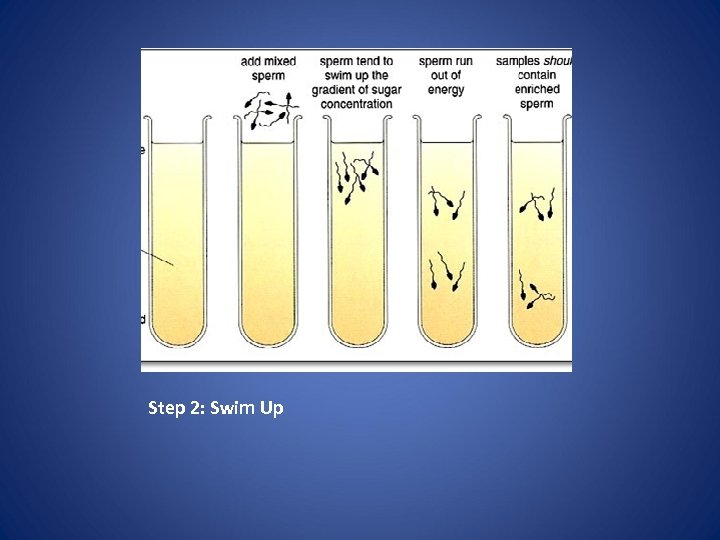
Step 2: Swim Up
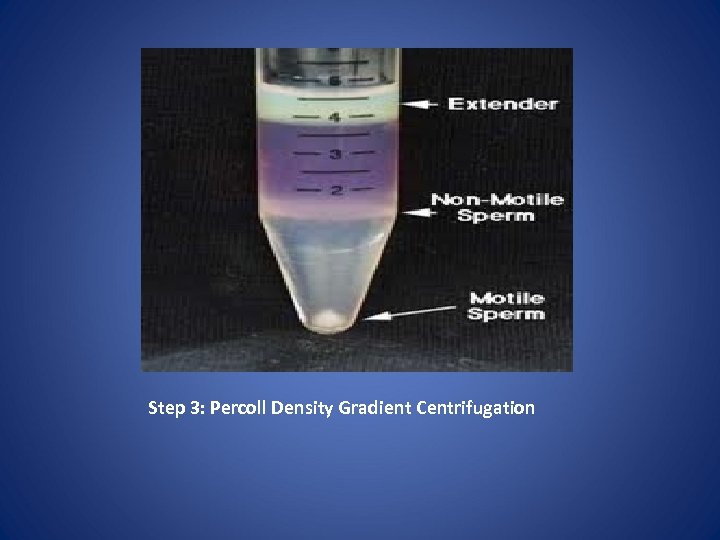
Step 3: Percoll Density Gradient Centrifugation
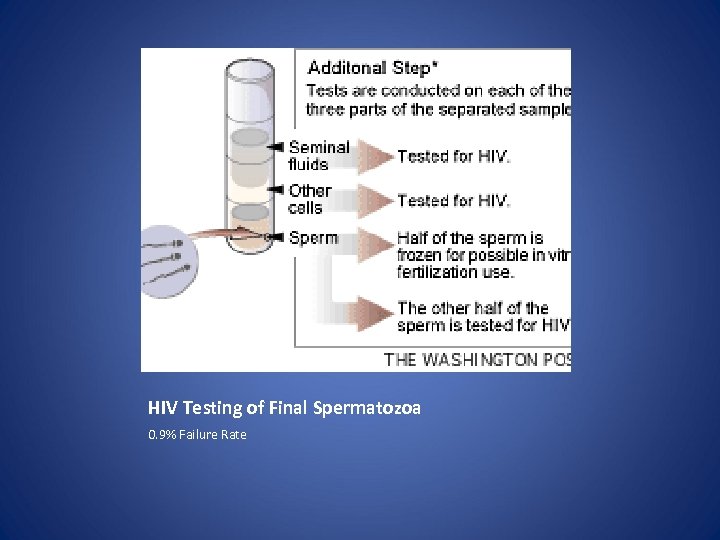
HIV Testing of Final Spermatozoa 0. 9% Failure Rate
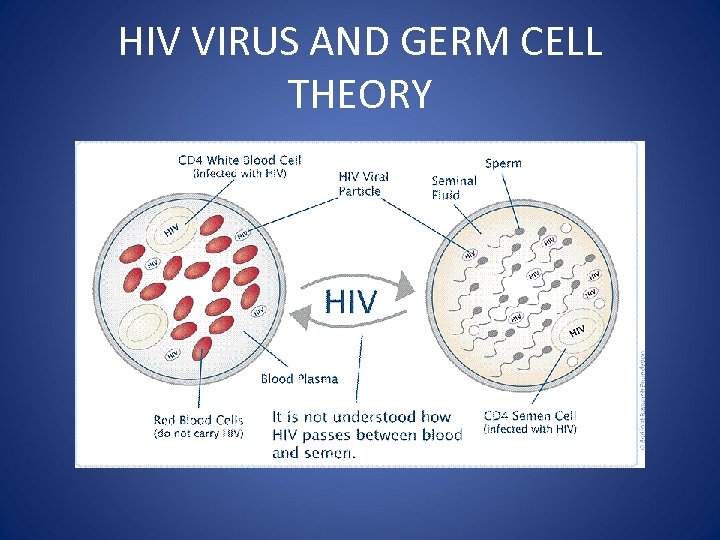
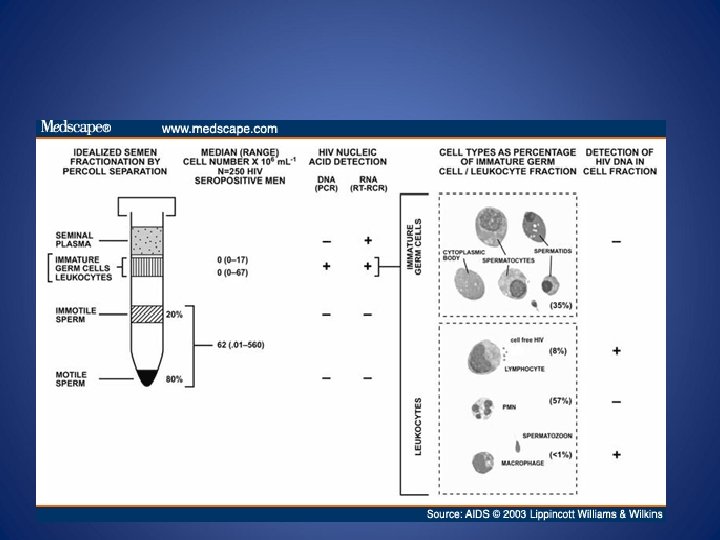
HIV VIRUS AND GERM CELL THEORY
Intrauterine Insemination (IUI)
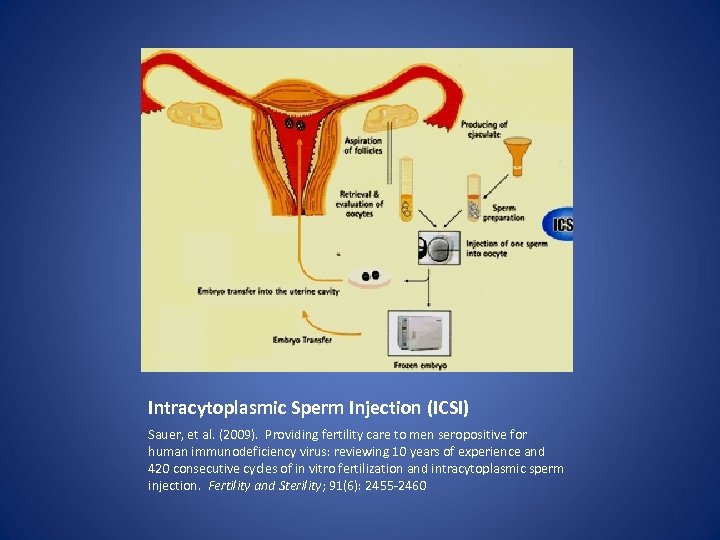
Intracytoplasmic Sperm Injection (ICSI) Sauer, et al. (2009). Providing fertility care to men seropositive for human immunodeficiency virus: reviewing 10 years of experience and 420 consecutive cycles of in vitro fertilization and intracytoplasmic sperm injection. Fertility and Sterility; 91(6): 2455 -2460
3000
Lack of Providers Sauer, M (2006). American physicians remain slow to embrace the reproductive needs of human immunodeficiency-virus patients. Fertility and Sterility; 85(2): 295 -297
Access to Fertility Services for HIV
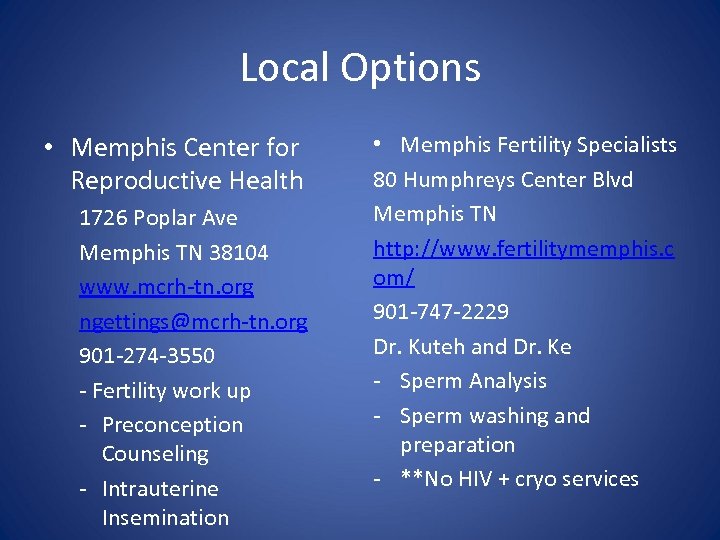
Local Options • Memphis Center for Reproductive Health 1726 Poplar Ave Memphis TN 38104 www. mcrh-tn. org ngettings@mcrh-tn. org 901 -274 -3550 - Fertility work up - Preconception Counseling - Intrauterine Insemination • Memphis Fertility Specialists 80 Humphreys Center Blvd Memphis TN http: //www. fertilitymemphis. c om/ 901 -747 -2229 Dr. Kuteh and Dr. Ke - Sperm Analysis - Sperm washing and preparation - **No HIV + cryo services
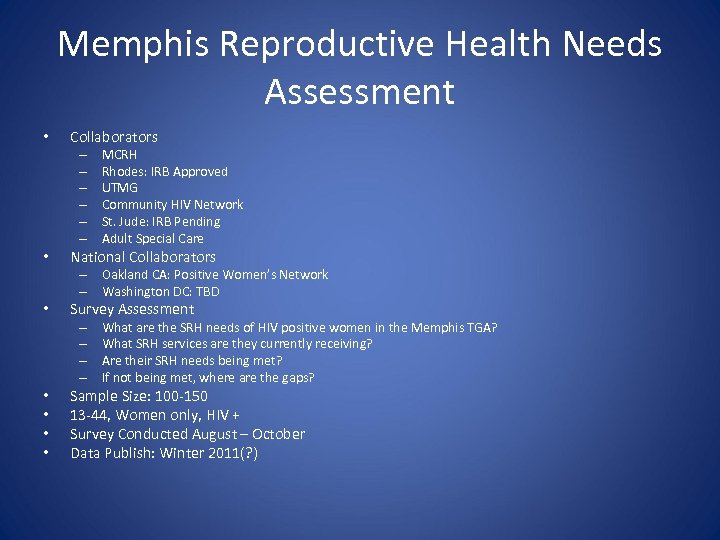
Memphis Reproductive Health Needs Assessment • Collaborators – – – • MCRH Rhodes: IRB Approved UTMG Community HIV Network St. Jude: IRB Pending Adult Special Care National Collaborators – Oakland CA: Positive Women’s Network – Washington DC: TBD • Survey Assessment – – • • What are the SRH needs of HIV positive women in the Memphis TGA? What SRH services are they currently receiving? Are their SRH needs being met? If not being met, where are the gaps? Sample Size: 100 -150 13 -44, Women only, HIV + Survey Conducted August – October Data Publish: Winter 2011(? )

Resources • • • www. creathe. org www. cyclebeads. com www. thewellproject. org www. hivcenternyc. org www. studiosemprini. com/ www. thebody. com
Special Populations
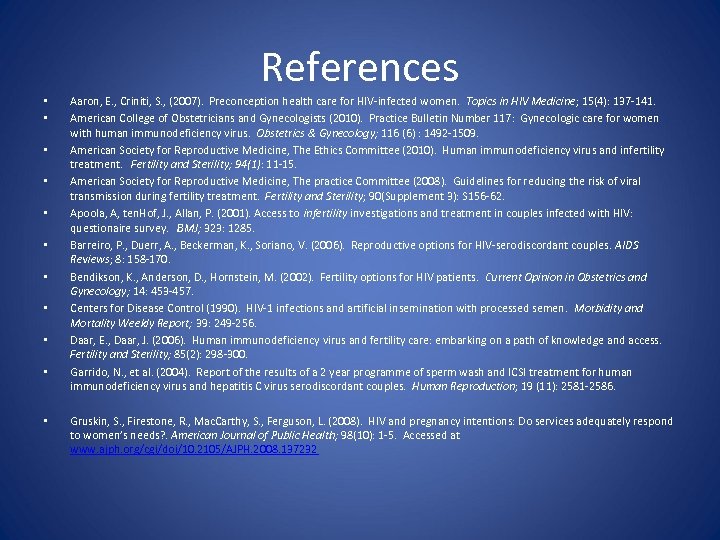
References • • • Aaron, E. , Criniti, S. , (2007). Preconception health care for HIV-infected women. Topics in HIV Medicine; 15(4): 137 -141. American College of Obstetricians and Gynecologists (2010). Practice Bulletin Number 117: Gynecologic care for women with human immunodeficiency virus. Obstetrics & Gynecology; 116 (6) : 1492 -1509. American Society for Reproductive Medicine, The Ethics Committee (2010). Human immunodeficiency virus and infertility treatment. Fertility and Sterility; 94(1): 11 -15. American Society for Reproductive Medicine, The practice Committee (2008). Guidelines for reducing the risk of viral transmission during fertility treatment. Fertility and Sterility; 90(Supplement 3): S 156 -62. Apoola, A, ten. Hof, J. , Allan, P. (2001). Access to infertility investigations and treatment in couples infected with HIV: questionaire survey. BMJ; 323: 1285. Barreiro, P. , Duerr, A. , Beckerman, K. , Soriano, V. (2006). Reproductive options for HIV-serodiscordant couples. AIDS Reviews; 8: 158 -170. Bendikson, K. , Anderson, D. , Hornstein, M. (2002). Fertility options for HIV patients. Current Opinion in Obstetrics and Gynecology; 14: 453 -457. Centers for Disease Control (1990). HIV-1 infections and artificial insemination with processed semen. Morbidity and Mortality Weekly Report; 39: 249 -256. Daar, E. , Daar, J. (2006). Human immunodeficiency virus and fertility care: embarking on a path of knowledge and access. Fertility and Sterility; 85(2): 298 -300. Garrido, N. , et al. (2004). Report of the results of a 2 year programme of sperm wash and ICSI treatment for human immunodeficiency virus and hepatitis C virus serodiscordant couples. Human Reproduction; 19 (11): 2581 -2586. Gruskin, S. , Firestone, R. , Mac. Carthy, S. , Ferguson, L. (2008). HIV and pregnancy intentions: Do services adequately respond to women’s needs? . American Journal of Public Health; 98(10): 1 -5. Accessed at www. ajph. org/cgi/doi/10. 2105/AJPH. 2008. 137232
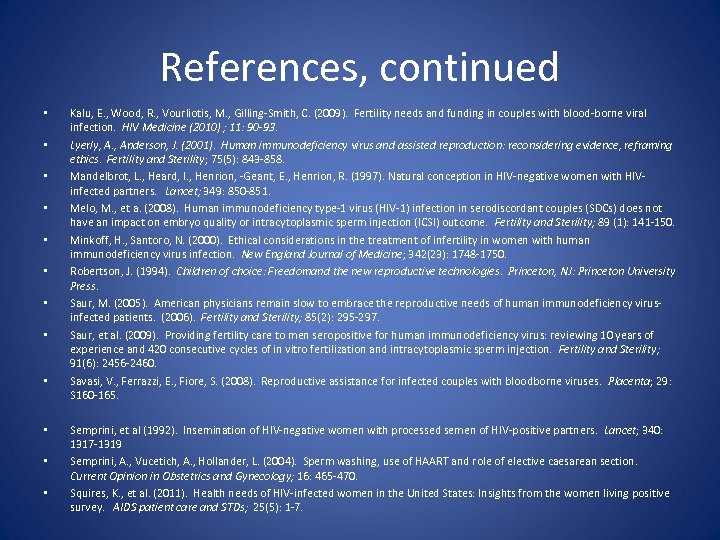
References, continued • • • Kalu, E. , Wood, R. , Vourliotis, M. , Gilling-Smith, C. (2009). Fertility needs and funding in couples with blood-borne viral infection. HIV Medicine (2010) ; 11: 90 -93. Lyerly, A. , Anderson, J. (2001). Human immunodeficiency virus and assisted reproduction: reconsidering evidence, reframing ethics. Fertility and Sterility; 75(5): 843 -858. Mandelbrot, L. , Heard, I. , Henrion, -Geant, E. , Henrion, R. (1997). Natural conception in HIV-negative women with HIVinfected partners. Lancet; 349: 850 -851. Melo, M. , et a. (2008). Human immunodeficiency type-1 virus (HIV-1) infection in serodiscordant couples (SDCs) does not have an impact on embryo quality or intracytoplasmic sperm injection (ICSI) outcome. Fertility and Sterility; 89 (1): 141 -150. Minkoff, H. , Santoro, N. (2000). Ethical considerations in the treatment of infertility in women with human immunodeficiency virus infection. New England Journal of Medicine; 342(23): 1748 -1750. Robertson, J. (1994). Children of choice: Freedomand the new reproductive technologies. Princeton, NJ: Princeton University Press. Saur, M. (2005). American physicians remain slow to embrace the reproductive needs of human immunodeficiency virusinfected patients. (2006). Fertility and Sterility; 85(2): 295 -297. Saur, et al. (2009). Providing fertility care to men seropositive for human immunodeficiency virus: reviewing 10 years of experience and 420 consecutive cycles of in vitro fertilization and intracytoplasmic sperm injection. Fertility and Sterility; 91(6): 2456 -2460. Savasi, V. , Ferrazzi, E. , Fiore, S. (2008). Reproductive assistance for infected couples with bloodborne viruses. Placenta; 29: S 160 -165. Semprini, et al (1992). Insemination of HIV-negative women with processed semen of HIV-positive partners. Lancet; 340: 1317 -1319 Semprini, A. , Vucetich, A. , Hollander, L. (2004). Sperm washing, use of HAART and role of elective caesarean section. Current Opinion in Obstetrics and Gynecology; 16: 465 -470. Squires, K. , et al. (2011). Health needs of HIV-infected women in the United States: Insights from the women living positive survey. AIDS patient care and STDs; 25(5): 1 -7.
References, continued • • Thornton, A. , Fomanelli, F. , Collins, J. (2004). Reproduction decision making for couples affected by HIV: A review of the literature. Topics in HIV Medicine. 12(2): 61 -67. Van Leeuwen, E. , Repping, S. , Prins, J. M. , Reiss, P. , van der Veen, F. (unknown). Assisted reproductive technologies to establish pregnancies in couples with an HIV-I infected man. Van Zuiden Communications.
Thank You Thank you to St. Jude Children’s Research Facility Special thank you to Dr. Gaur, Sally Discenza, and Shelly Burrow Contact information: Nikole Gettings, MSN, CNM Memphis Center for Reproductive Health Phone: 901 -274 -3550 Email: ngettings@mcrh-tn. org
Questions?
f24e87d0f731bbad93f1bc377d6f1ae8.ppt