929fe308a0b0f674ca30deaee10e2dbe.ppt
- Количество слайдов: 22
 H. P. I. -M. Z 9/9 -11 a. m. l 40 y/o male with swelling, redness, and drainage from the left eye for last few days. l E. O. M. ’s intact. ”No suspicion of deep infection at this time”. l Treatment Keflex 500 mg Q 6 hr P. O. and check with Ophthalmology in the a. m. l (1 gram of Rocephin i. m. )
H. P. I. -M. Z 9/9 -11 a. m. l 40 y/o male with swelling, redness, and drainage from the left eye for last few days. l E. O. M. ’s intact. ”No suspicion of deep infection at this time”. l Treatment Keflex 500 mg Q 6 hr P. O. and check with Ophthalmology in the a. m. l (1 gram of Rocephin i. m. )
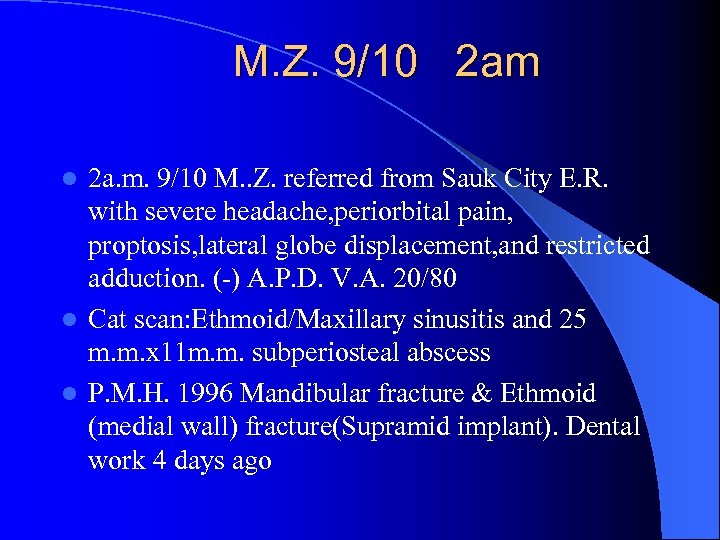 M. Z. 9/10 2 am 2 a. m. 9/10 M. . Z. referred from Sauk City E. R. with severe headache, periorbital pain, proptosis, lateral globe displacement, and restricted adduction. (-) A. P. D. V. A. 20/80 l Cat scan: Ethmoid/Maxillary sinusitis and 25 m. m. x 11 m. m. subperiosteal abscess l P. M. H. 1996 Mandibular fracture & Ethmoid (medial wall) fracture(Supramid implant). Dental work 4 days ago l
M. Z. 9/10 2 am 2 a. m. 9/10 M. . Z. referred from Sauk City E. R. with severe headache, periorbital pain, proptosis, lateral globe displacement, and restricted adduction. (-) A. P. D. V. A. 20/80 l Cat scan: Ethmoid/Maxillary sinusitis and 25 m. m. x 11 m. m. subperiosteal abscess l P. M. H. 1996 Mandibular fracture & Ethmoid (medial wall) fracture(Supramid implant). Dental work 4 days ago l
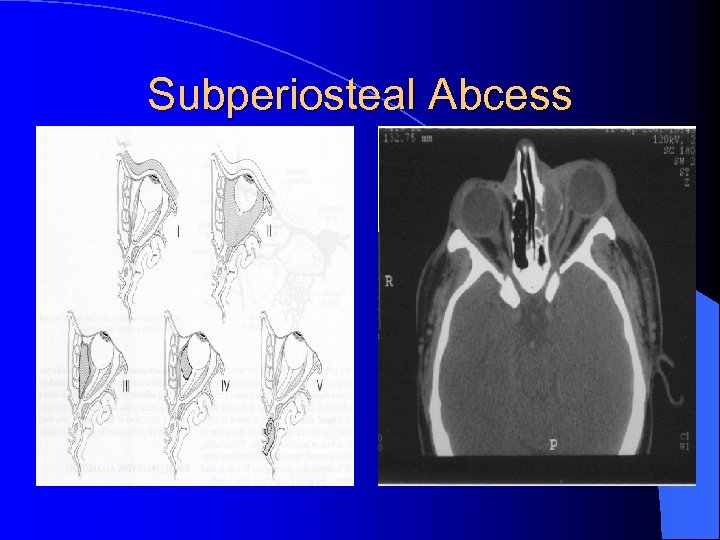 Subperiosteal Abcess
Subperiosteal Abcess
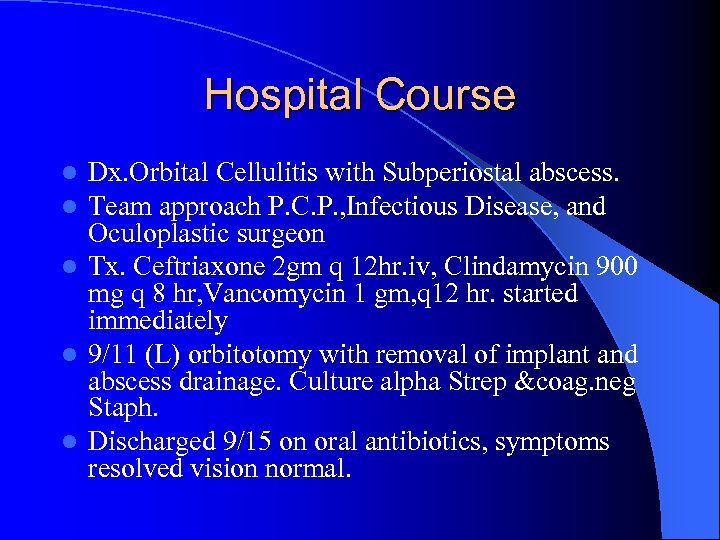 Hospital Course Dx. Orbital Cellulitis with Subperiostal abscess. Team approach P. C. P. , Infectious Disease, and Oculoplastic surgeon l Tx. Ceftriaxone 2 gm q 12 hr. iv, Clindamycin 900 mg q 8 hr, Vancomycin 1 gm, q 12 hr. started immediately l 9/11 (L) orbitotomy with removal of implant and abscess drainage. Culture alpha Strep &coag. neg Staph. l Discharged 9/15 on oral antibiotics, symptoms resolved vision normal. l l
Hospital Course Dx. Orbital Cellulitis with Subperiostal abscess. Team approach P. C. P. , Infectious Disease, and Oculoplastic surgeon l Tx. Ceftriaxone 2 gm q 12 hr. iv, Clindamycin 900 mg q 8 hr, Vancomycin 1 gm, q 12 hr. started immediately l 9/11 (L) orbitotomy with removal of implant and abscess drainage. Culture alpha Strep &coag. neg Staph. l Discharged 9/15 on oral antibiotics, symptoms resolved vision normal. l l
 MRSA l Community acquired – Increased potential for tissue invasion – Found in young athletes and inmates – Progresses despite appropriate treatment
MRSA l Community acquired – Increased potential for tissue invasion – Found in young athletes and inmates – Progresses despite appropriate treatment
 Case Review Day 1: 44 yr old male squeezed a pustule in his nose Day 3: fever and chills developed, treated with TMP/SMX DS and Rifampin Day 4: Admitted for eyelid swelling, WBC 24, 000. Rx- Vancomycin + Ceftriaxone + Metronidazole Day 5: Massive proptosis, ophthalmoplegia, bilateral vision loss
Case Review Day 1: 44 yr old male squeezed a pustule in his nose Day 3: fever and chills developed, treated with TMP/SMX DS and Rifampin Day 4: Admitted for eyelid swelling, WBC 24, 000. Rx- Vancomycin + Ceftriaxone + Metronidazole Day 5: Massive proptosis, ophthalmoplegia, bilateral vision loss
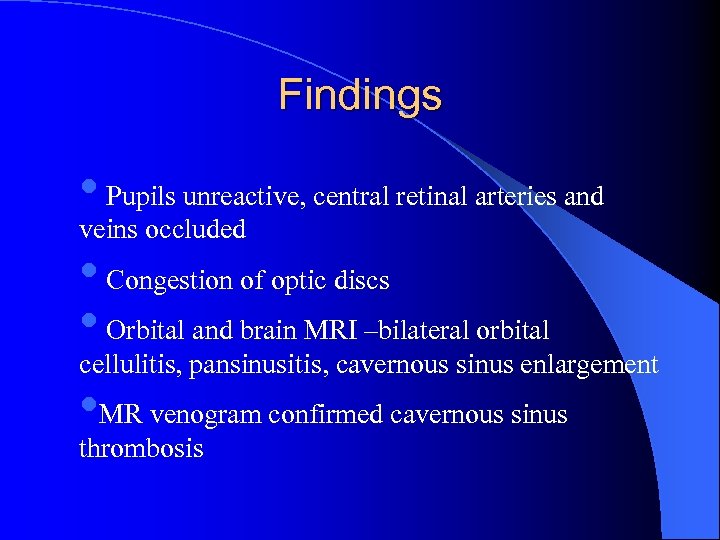 Findings • Pupils unreactive, central retinal arteries and veins occluded • Congestion of optic discs • Orbital and brain MRI –bilateral orbital cellulitis, pansinusitis, cavernous sinus enlargement • MR venogram confirmed cavernous sinus thrombosis
Findings • Pupils unreactive, central retinal arteries and veins occluded • Congestion of optic discs • Orbital and brain MRI –bilateral orbital cellulitis, pansinusitis, cavernous sinus enlargement • MR venogram confirmed cavernous sinus thrombosis
 Hospital course l Paranasal l Day l In sinuses drained endoscopically 13: iv heparin and methylprednisolone retrospect, may have benefited from orbital decompression sooner
Hospital course l Paranasal l Day l In sinuses drained endoscopically 13: iv heparin and methylprednisolone retrospect, may have benefited from orbital decompression sooner
 Preseptal cellulitis RX Dicloxacillin Augmentin Macrolides Quinolones 3 rd gen. Cephalosporin
Preseptal cellulitis RX Dicloxacillin Augmentin Macrolides Quinolones 3 rd gen. Cephalosporin
 Orbital Cellulitis Ø Ceftriaxone & Metronidazole Vancomycin Ø Ampicillin/Sulbactam Ø Ticarcillin/Clavulanic acid & Vancomycin Ø Imipenen/Meropenem & Vancomycin Ø Fluoroquinolone & Clindamycin Ø Aztreonam Ø Amphotericin
Orbital Cellulitis Ø Ceftriaxone & Metronidazole Vancomycin Ø Ampicillin/Sulbactam Ø Ticarcillin/Clavulanic acid & Vancomycin Ø Imipenen/Meropenem & Vancomycin Ø Fluoroquinolone & Clindamycin Ø Aztreonam Ø Amphotericin




 Team Work EYE ENT ID NEUROSURGERY
Team Work EYE ENT ID NEUROSURGERY


 HEADS UP • Team Approach • History very important in determining the most likely organism. Culture may be difficult. • Frequent re-evaluations are necessary. • Imaging studies are very helpful in diagnosis and monitoring treatment. • Serious problem can result in death.
HEADS UP • Team Approach • History very important in determining the most likely organism. Culture may be difficult. • Frequent re-evaluations are necessary. • Imaging studies are very helpful in diagnosis and monitoring treatment. • Serious problem can result in death.
 Differential Dx. Proptosis Infection Orbital cellulitis Cavernous sinus thrombosis Neoplastic Metastatic Ca Lymphoma Rhabdomyosarcoma Retinoblastoma Leukemia Letterer-Siwe disease l Endocrine Orbital Inflammation l Pseudotumor l Orbital myositis l Wegener’ granulomatosis
Differential Dx. Proptosis Infection Orbital cellulitis Cavernous sinus thrombosis Neoplastic Metastatic Ca Lymphoma Rhabdomyosarcoma Retinoblastoma Leukemia Letterer-Siwe disease l Endocrine Orbital Inflammation l Pseudotumor l Orbital myositis l Wegener’ granulomatosis
 ANATOMY
ANATOMY

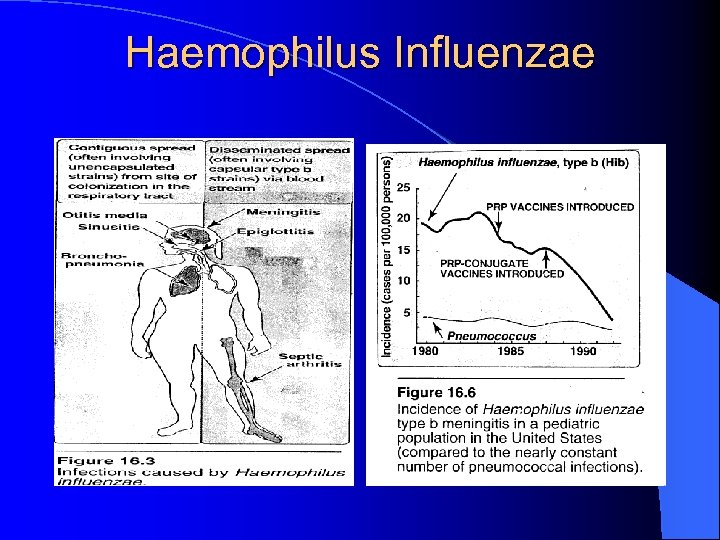 Haemophilus Influenzae
Haemophilus Influenzae


