38044ff918f8c0a77d2774a918558d71.ppt
- Количество слайдов: 52
GUJARAT STATE NUTRITION MISSION (GSNM) Presentation to Hon’ble Chief Minister Departments of H&FW and WCD
Agenda of the Meeting 1. Overview of the nutrition status in Gujarat-High incidence of undernutrition in Gujarat 2. Nodal Departments for Gujarat State Nutrition Mission - HFWD & DWCD. 3. To decide the Roles, Responsibilities and Structure of Nutrition Mission 4. To evolve Concept and Approach to achieve the objective : - 3 –Tier Approach. 5. Human and Financial resources for the Mission 6. Maharashtra & Other Models – successful case study. 7. Any other agenda items from the Chair 16 -Mar-18 Health & FW 2
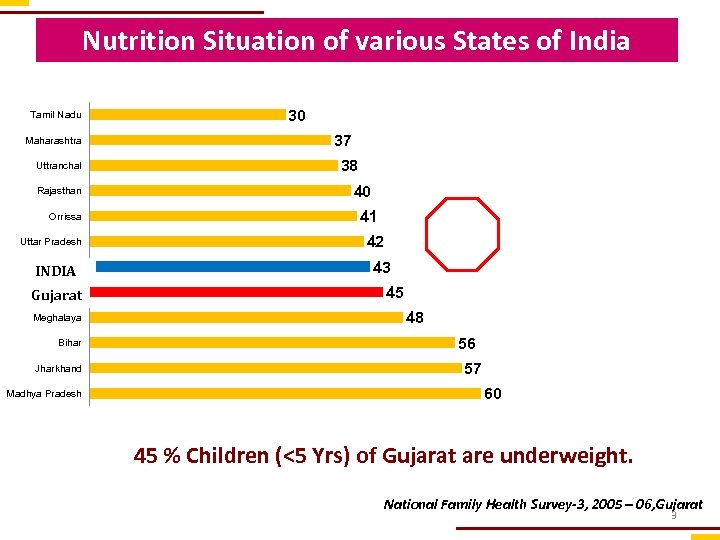
Nutrition Situation of various States of India Tamil Nadu Maharashtra Uttranchal Rajasthan Orrissa Uttar Pradesh INDIA Gujarat Meghalaya Bihar Jharkhand Madhya Pradesh 30 37 38 40 41 42 43 45 48 56 57 60 45 % Children (<5 Yrs) of Gujarat are underweight. National Family Health Survey-3, 2005 – 06, Gujarat 3
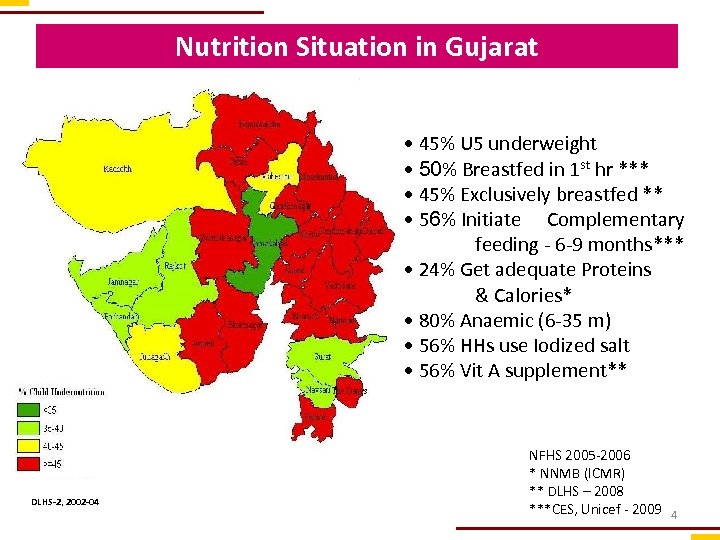
Nutrition Situation in Gujarat • 45% U 5 underweight • 50% Breastfed in 1 st hr *** • 45% Exclusively breastfed ** • 56% Initiate Complementary feeding - 6 -9 months*** • 24% Get adequate Proteins & Calories* • 80% Anaemic (6 -35 m) • 56% HHs use Iodized salt • 56% Vit A supplement** DLHS-2, 2002 -04 NFHS 2005 -2006 * NNMB (ICMR) ** DLHS – 2008 ***CES, Unicef - 2009 4
Types of Malnutrition • Underweight- A composite measure – Low Weight for Age • Stunting- An indicator of past growth failure – Low Height for Age • Wasting- Current or Acute malnutrition – Low Weight for Height • Micronutrient deficiencies- Iron(Anaemia), Iodine (Hypothyroidism, Cretinism-Mental retardation), Vit-A (Night Blindness)
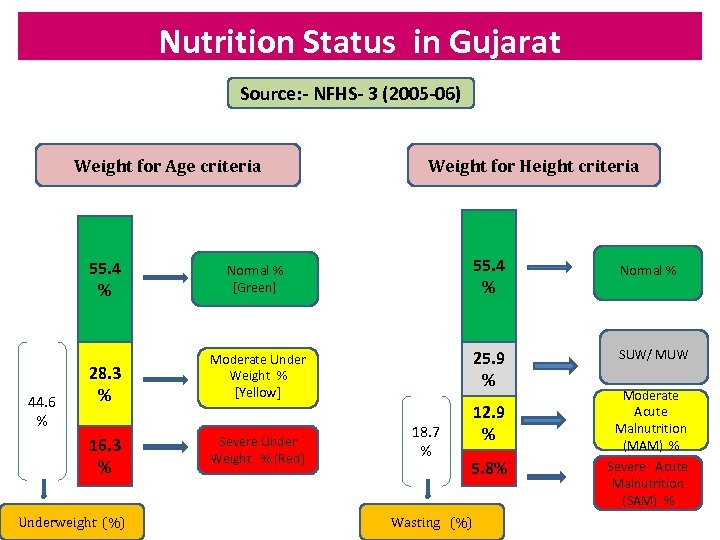
Nutrition Status in Gujarat Source: - NFHS- 3 (2005 -06) Weight for Age criteria 55. 4 % 44. 6 % 28. 3 % 16. 3 % Underweight (%) Weight for Height criteria 55. 4 % Normal % [Green] 25. 9 % Moderate Under Weight % [Yellow] Severe Under Weight % (Red) 18. 7 % 12. 9 % 5. 8% Wasting (%) Normal % SUW/ MUW Moderate Acute Malnutrition (MAM) % Severe Acute Malnutrition (SAM) %
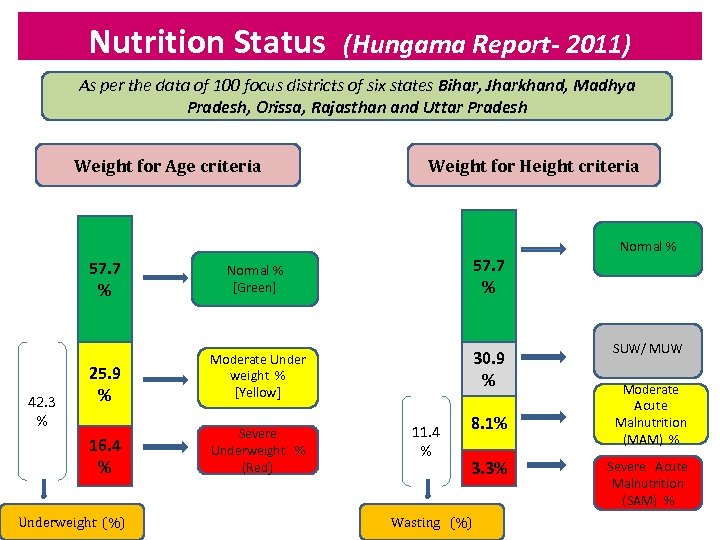
Nutrition Status (Hungama Report- 2011) As per the data of 100 focus districts of six states Bihar, Jharkhand, Madhya Pradesh, Orissa, Rajasthan and Uttar Pradesh Weight for Age criteria 57. 7 % Normal % [Green] 25. 9 % Severe Underweight % (Red) 30. 9 % Moderate Under weight % [Yellow] 16. 4 % 42. 3 % Weight for Height criteria Underweight (%) 11. 4 % 8. 1% 3. 3% Wasting (%) Normal % SUW/ MUW Moderate Acute Malnutrition (MAM) % Severe Acute Malnutrition (SAM) %
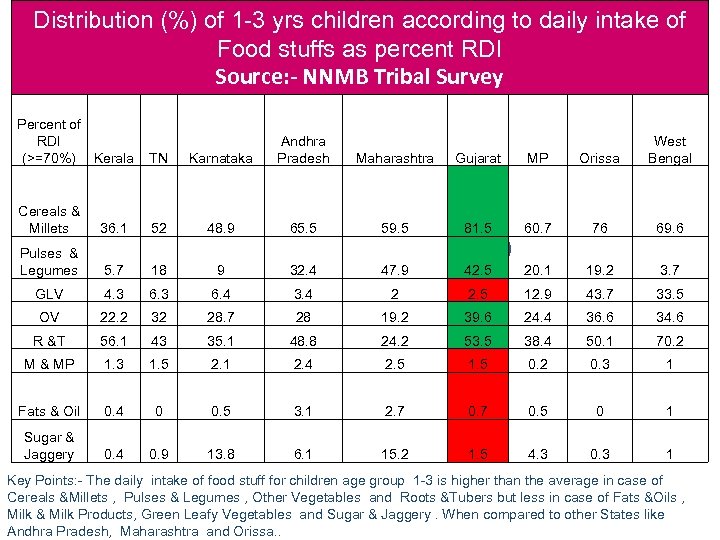
Distribution (%) of 1 -3 yrs children according to daily intake of Food stuffs as percent RDI Source: - NNMB Tribal Survey Percent of RDI (>=70%) Kerala TN Cereals & Millets 36. 1 Pulses & Legumes Karnataka Andhra Pradesh Maharashtra Gujarat MP Orissa West Bengal 52 48. 9 65. 5 59. 5 81. 5 60. 7 76 69. 6 5. 7 18 9 32. 4 47. 9 42. 5 20. 1 19. 2 3. 7 GLV 4. 3 6. 4 3. 4 2 2. 5 12. 9 43. 7 33. 5 OV 22. 2 32 28. 7 28 19. 2 39. 6 24. 4 36. 6 34. 6 R &T 56. 1 43 35. 1 48. 8 24. 2 53. 5 38. 4 50. 1 70. 2 M & MP 1. 3 1. 5 2. 1 2. 4 2. 5 1. 5 0. 2 0. 3 1 Fats & Oil 0. 4 0 0. 5 3. 1 2. 7 0. 5 0 1 Sugar & Jaggery 0. 4 0. 9 13. 8 6. 1 15. 2 1. 5 4. 3 0. 3 1 Key Points: - The daily intake of food stuff for children age group 1 -3 is higher than the average in case of Cereals &Millets , Pulses & Legumes , Other Vegetables and Roots &Tubers but less in case of Fats &Oils , Milk & Milk Products, Green Leafy Vegetables and Sugar & Jaggery. When compared to other States like Andhra Pradesh, Maharashtra and Orissa. .
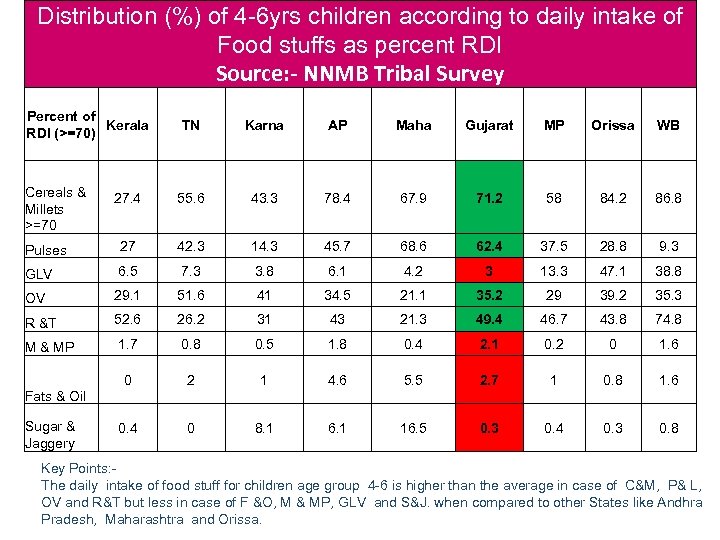
Distribution (%) of 4 -6 yrs children according to daily intake of Food stuffs as percent RDI Source: - NNMB Tribal Survey Percent of Kerala RDI (>=70) TN Karna AP Maha Gujarat MP Orissa WB 27. 4 55. 6 43. 3 78. 4 67. 9 71. 2 58 84. 2 86. 8 Pulses 27 42. 3 14. 3 45. 7 68. 6 62. 4 37. 5 28. 8 9. 3 GLV 6. 5 7. 3 3. 8 6. 1 4. 2 3 13. 3 47. 1 38. 8 OV 29. 1 51. 6 41 34. 5 21. 1 35. 2 29 39. 2 35. 3 R &T 52. 6 26. 2 31 43 21. 3 49. 4 46. 7 43. 8 74. 8 M & MP 1. 7 0. 8 0. 5 1. 8 0. 4 2. 1 0. 2 0 1. 6 0 2 1 4. 6 5. 5 2. 7 1 0. 8 1. 6 0. 4 0 8. 1 6. 1 16. 5 0. 3 0. 4 0. 3 0. 8 Cereals & Millets >=70 Fats & Oil Sugar & Jaggery Key Points: The daily intake of food stuff for children age group 4 -6 is higher than the average in case of C&M, P& L, OV and R&T but less in case of F &O, M & MP, GLV and S&J. when compared to other States like Andhra Pradesh, Maharashtra and Orissa.
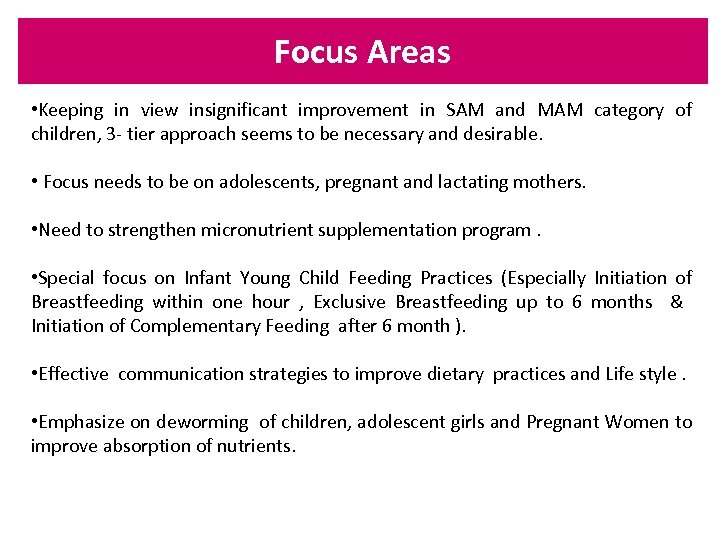
Focus Areas • Keeping in view insignificant improvement in SAM and MAM category of children, 3 - tier approach seems to be necessary and desirable. • Focus needs to be on adolescents, pregnant and lactating mothers. • Need to strengthen micronutrient supplementation program. • Special focus on Infant Young Child Feeding Practices (Especially Initiation of Breastfeeding within one hour , Exclusive Breastfeeding up to 6 months & Initiation of Complementary Feeding after 6 month ). • Effective communication strategies to improve dietary practices and Life style. • Emphasize on deworming of children, adolescent girls and Pregnant Women to improve absorption of nutrients.
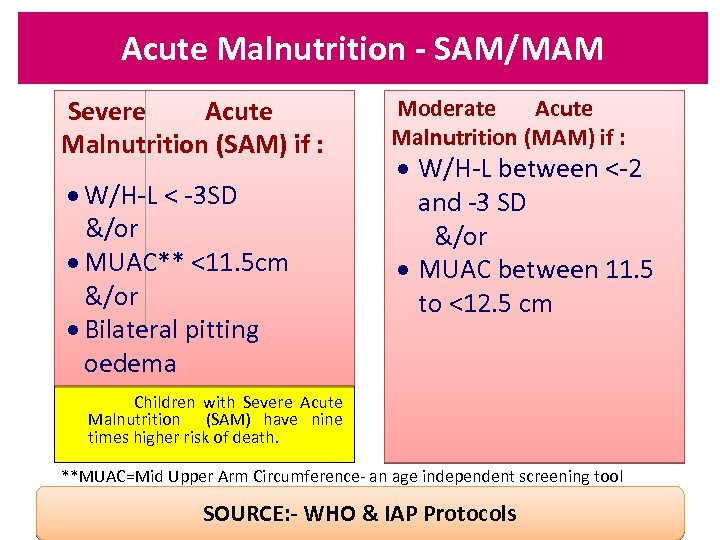
Acute Malnutrition - SAM/MAM Severe Acute Malnutrition (SAM) if : · W/H-L < -3 SD &/or · MUAC** <11. 5 cm &/or · Bilateral pitting oedema Moderate Acute Malnutrition (MAM) if : · W/H-L between <-2 and -3 SD &/or · MUAC between 11. 5 to <12. 5 cm Children with Severe Acute Malnutrition (SAM) have nine times higher risk of death. **MUAC=Mid Upper Arm Circumference- an age independent screening tool SOURCE: - WHO & IAP Protocols
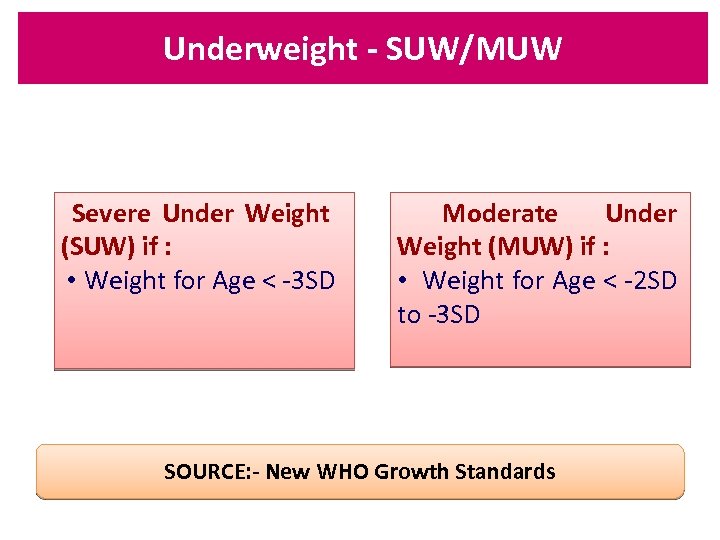
Underweight - SUW/MUW Severe Under Weight (SUW) if : • Weight for Age < -3 SD Moderate Under Weight (MUW) if : • Weight for Age < -2 SD to -3 SD SOURCE: - New WHO Growth Standards
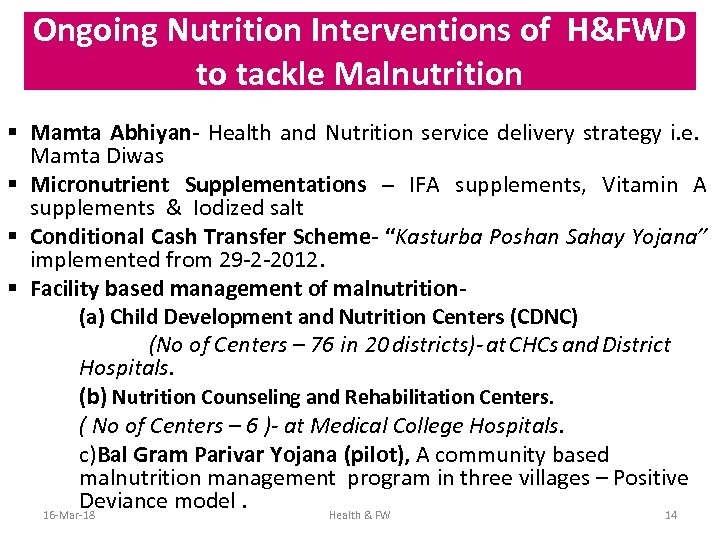
Ongoing Nutrition Interventions of H&FWD to tackle Malnutrition § Mamta Abhiyan- Health and Nutrition service delivery strategy i. e. Mamta Diwas § Micronutrient Supplementations – IFA supplements, Vitamin A supplements & Iodized salt § Conditional Cash Transfer Scheme- “Kasturba Poshan Sahay Yojana” implemented from 29 -2 -2012. § Facility based management of malnutrition(a) Child Development and Nutrition Centers (CDNC) (No of Centers – 76 in 20 districts)- at CHCs and District Hospitals. (b) Nutrition Counseling and Rehabilitation Centers. ( No of Centers – 6 )- at Medical College Hospitals. c)Bal Gram Parivar Yojana (pilot), A community based malnutrition management program in three villages – Positive Deviance model. 16 -Mar-18 Health & FW 14
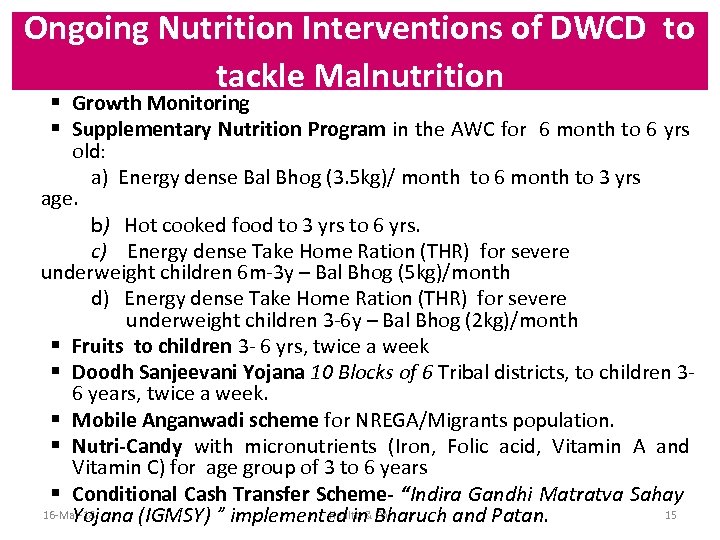
Ongoing Nutrition Interventions of DWCD to tackle Malnutrition § Growth Monitoring § Supplementary Nutrition Program in the AWC for 6 month to 6 yrs old: a) Energy dense Bal Bhog (3. 5 kg)/ month to 6 month to 3 yrs age. b) Hot cooked food to 3 yrs to 6 yrs. c) Energy dense Take Home Ration (THR) for severe underweight children 6 m-3 y – Bal Bhog (5 kg)/month d) Energy dense Take Home Ration (THR) for severe underweight children 3 -6 y – Bal Bhog (2 kg)/month § Fruits to children 3 - 6 yrs, twice a week § Doodh Sanjeevani Yojana 10 Blocks of 6 Tribal districts, to children 36 years, twice a week. § Mobile Anganwadi scheme for NREGA/Migrants population. § Nutri-Candy with micronutrients (Iron, Folic acid, Vitamin A and Vitamin C) for age group of 3 to 6 years § Conditional Cash Transfer Scheme- “Indira Gandhi Matratva Sahay 16 -Mar-18 Health & FW 15 Yojana (IGMSY) ” implemented in Bharuch and Patan.
Gujarat State Nutrition Mission Concept and Approach 16 -Mar-18 Health & FW 16
Gujarat State Nutrition Mission Structure Autonomous and independent structure of the Mission • An independent structure with autonomy in decision making and planning-in the form of Society /Trust ? • Three Tier Approach • Mission Director/Director General – a dedicated senior official of the level of a Principal Secretary / Secretary & not on additional charge. • Joint responsibility of HFWD & DWCD • Convergence with other line departments – Education, Food & Civil Supplies, Water Supply, Panchayat and Rural Development, Urban Development etc. 16 -Mar-18 Health & FW. 17
Gujarat State Nutrition Mission Structure The operational structure of the Mission should include A. State Level – 12 persons - Mission Director/Director General (IAS), Deputy Directors-3, Consultants and Project Officers -4, M&E Asst. -1, Data Entry Operators 2, Finance Asst. -1, Office Asst-1. Aim is to have specialists on board. B. District Level- 3 persons – District Nutrition Officer, Dist. M&E Asst. , Data entry operator, reporting to both CDHO and PO- ICDS to ensure convergence. C. Taluka Level- 2 persons – Taluka Nutrition Assistant, Date Entry Operator reporting to Taluka Health Officer 16 -Mar-18 Health & FW 18 and designate Taluka CDPO.
Gujarat State Nutrition Mission Structure D. Urban Level – (1) Corporation level- 3 persons – Corporation Nutrition Officer, Corporation M&E Asst & Data entry operator, reporting to both MO- Urban Health and PO- Urban ICDS to ensure convergence. (2) Zonal Level- 2 persons – Zonal Nutrition Assistant and Date Entry Operator reporting to Corporation Nutrition Officer. 16 -Mar-18 Health & FW 19
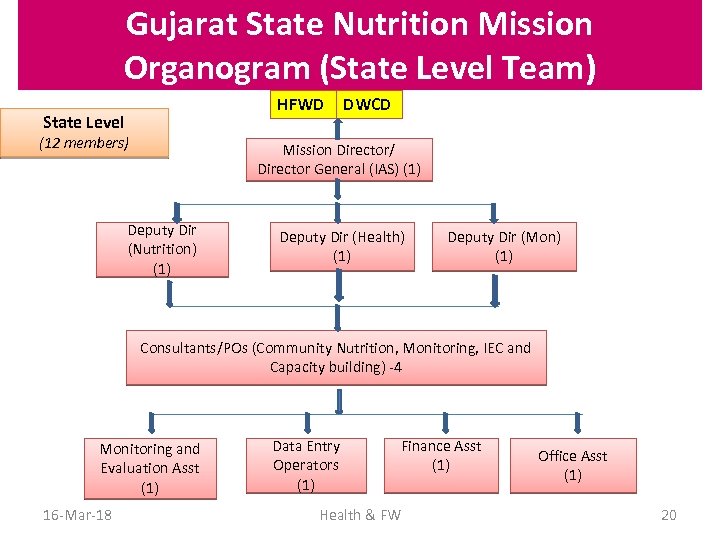
Gujarat State Nutrition Mission Organogram (State Level Team) HFWD State Level (12 members) DWCD Mission Director/ Director General (IAS) (1) Deputy Dir (Nutrition) (1) Deputy Dir (Health) (1) Deputy Dir (Mon) (1) Consultants/POs (Community Nutrition, Monitoring, IEC and Capacity building) -4 Monitoring and Evaluation Asst (1) 16 -Mar-18 Data Entry Operators (1) Finance Asst (1) Health & FW Office Asst (1) 20
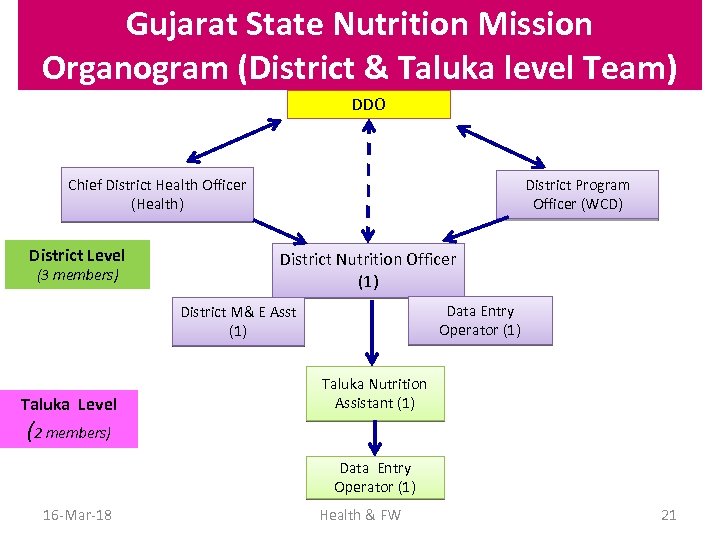
Gujarat State Nutrition Mission Organogram (District & Taluka level Team) DDO Chief District Health Officer (Health) District Level (3 members) District Program Officer (WCD) District Nutrition Officer (1) Data Entry Operator (1) District M& E Asst (1) Taluka Level Taluka Nutrition Assistant (1) (2 members) Data Entry Operator (1) 16 -Mar-18 Health & FW 21
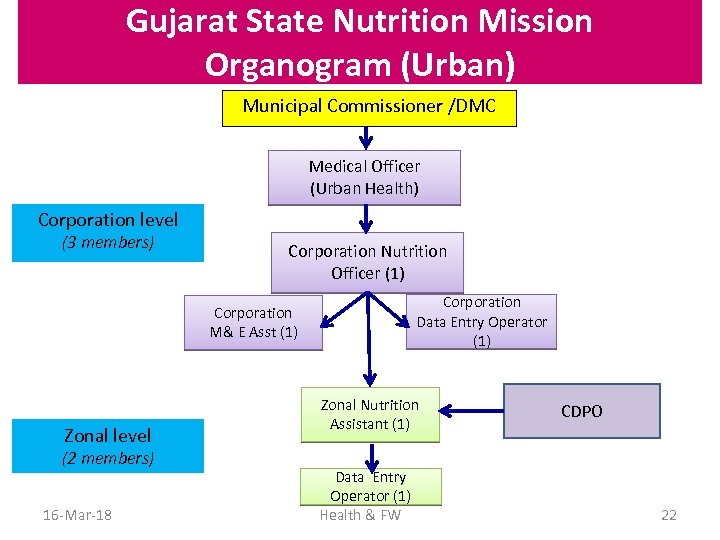
Gujarat State Nutrition Mission Organogram (Urban) Municipal Commissioner /DMC Medical Officer (Urban Health) Corporation level (3 members) Corporation Nutrition Officer (1) Corporation M& E Asst (1) Zonal level (2 members) 16 -Mar-18 Corporation Data Entry Operator (1) Zonal Nutrition Assistant (1) Data Entry Operator (1) Health & FW CDPO 22
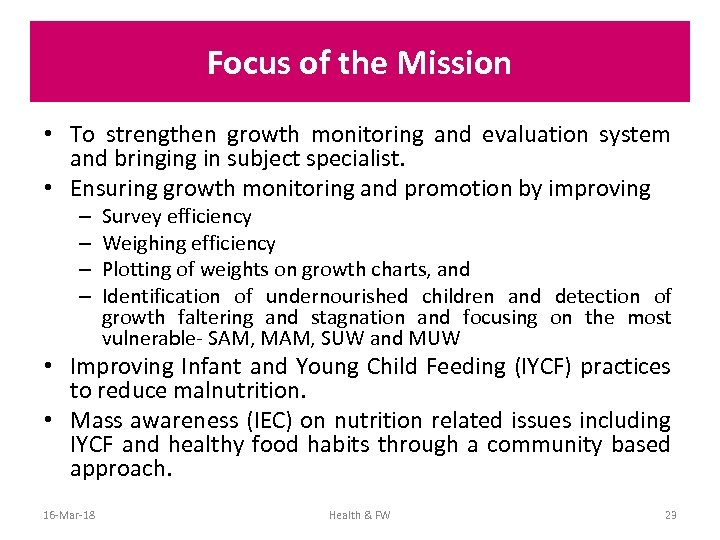
Focus of the Mission • To strengthen growth monitoring and evaluation system and bringing in subject specialist. • Ensuring growth monitoring and promotion by improving – – Survey efficiency Weighing efficiency Plotting of weights on growth charts, and Identification of undernourished children and detection of growth faltering and stagnation and focusing on the most vulnerable- SAM, MAM, SUW and MUW • Improving Infant and Young Child Feeding (IYCF) practices to reduce malnutrition. • Mass awareness (IEC) on nutrition related issues including IYCF and healthy food habits through a community based approach. 16 -Mar-18 Health & FW 23

Malnutrition Screening Tools & Equipments Weight for Height SAM if W/H <-3 SD MAM if W/H <-2 SD to -3 SD Indigenous Board: - Rs 1000/16 -Mar-18 Digital Weighing Scale : Cost Rs 4000/Spring Scale Rs 800 - 1500/- 24 Health & FW
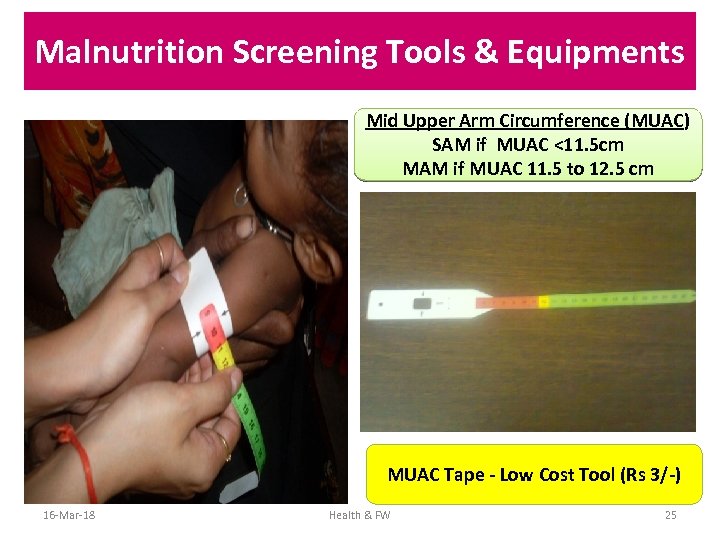
Malnutrition Screening Tools & Equipments Mid Upper Arm Circumference (MUAC) SAM if MUAC <11. 5 cm MAM if MUAC 11. 5 to 12. 5 cm MUAC Tape - Low Cost Tool (Rs 3/-) 16 -Mar-18 Health & FW 25
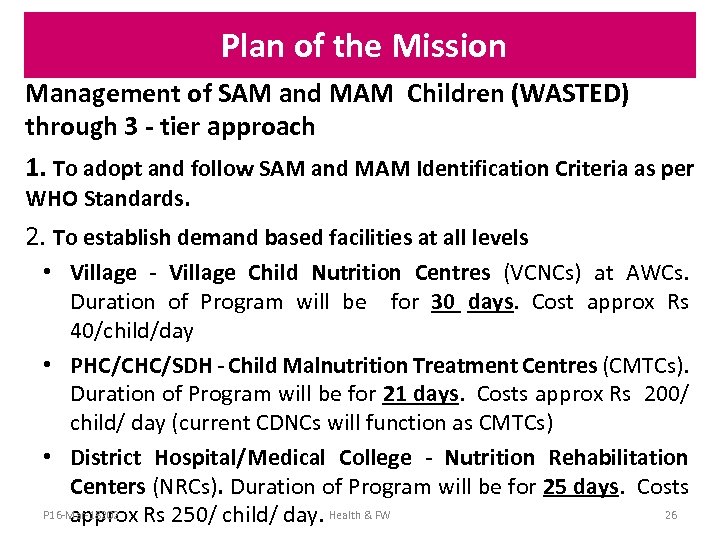
Plan of the Mission Management of SAM and MAM Children (WASTED) through 3 - tier approach 1. To adopt and follow SAM and MAM Identification Criteria as per WHO Standards. 2. To establish demand based facilities at all levels • Village - Village Child Nutrition Centres (VCNCs) at AWCs. Duration of Program will be for 30 days. Cost approx Rs 40/child/day • PHC/CHC/SDH - Child Malnutrition Treatment Centres (CMTCs). Duration of Program will be for 21 days. Costs approx Rs 200/ child/ day (current CDNCs will function as CMTCs) • District Hospital/Medical College - Nutrition Rehabilitation Centers (NRCs). Duration of Program will be for 25 days. Costs P 16 -Mar-18202 26 approx Rs 250/ child/ day. Health & FW
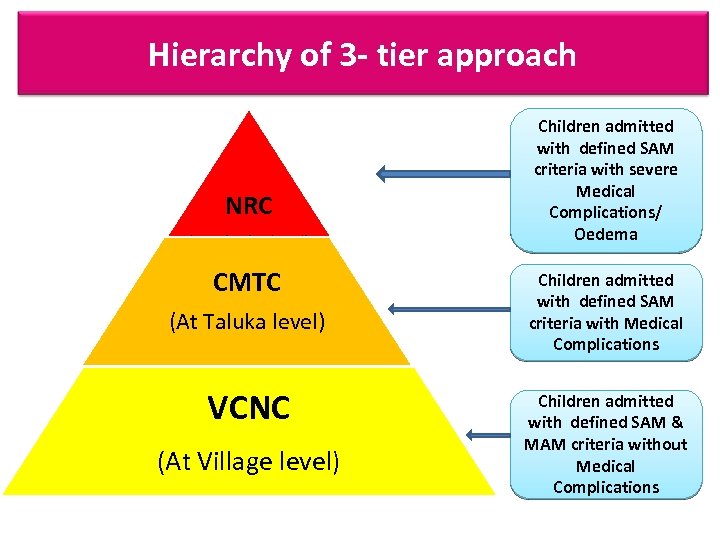
Hierarchy of 3 - tier approach NRC (At District level) CMTC (At Taluka level) VCNC (At Village level) Children admitted with defined SAM criteria with severe Medical Complications/ Oedema Children admitted with defined SAM criteria with Medical Complications Children admitted with defined SAM & MAM criteria without Medical Complications
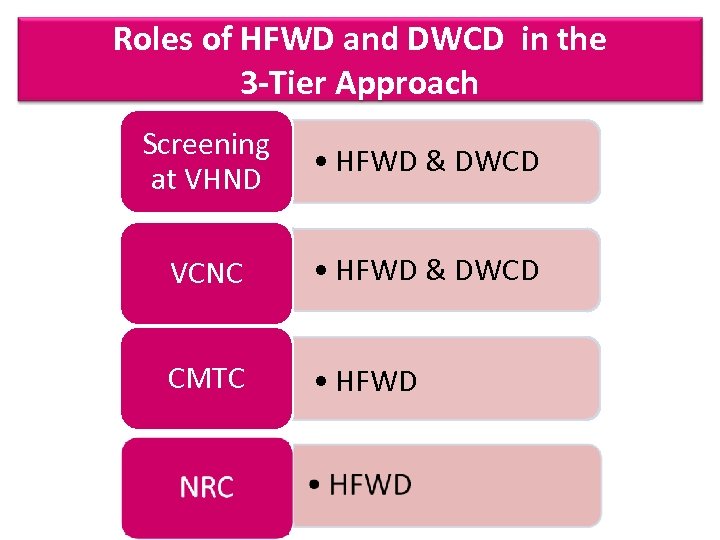
Roles of HFWD and DWCD in the 3 -Tier Approach Screening at VHND • HFWD & DWCD VCNC • HFWD & DWCD CMTC • HFWD
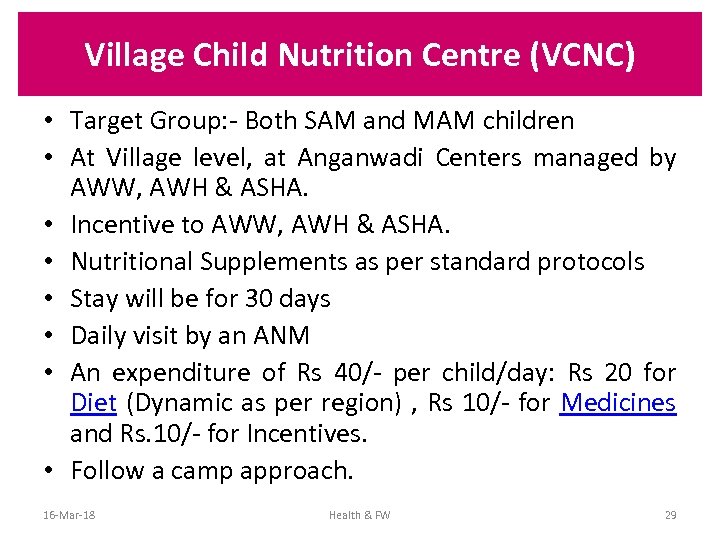
Village Child Nutrition Centre (VCNC) • Target Group: - Both SAM and MAM children • At Village level, at Anganwadi Centers managed by AWW, AWH & ASHA. • Incentive to AWW, AWH & ASHA. • Nutritional Supplements as per standard protocols • Stay will be for 30 days • Daily visit by an ANM • An expenditure of Rs 40/- per child/day: Rs 20 for Diet (Dynamic as per region) , Rs 10/- for Medicines and Rs. 10/- for Incentives. • Follow a camp approach. 16 -Mar-18 Health & FW 29
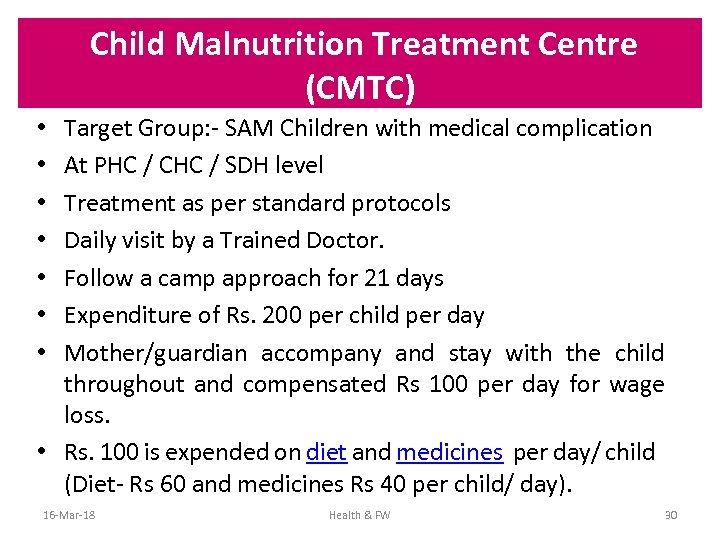
Child Malnutrition Treatment Centre (CMTC) Target Group: - SAM Children with medical complication At PHC / CHC / SDH level Treatment as per standard protocols Daily visit by a Trained Doctor. Follow a camp approach for 21 days Expenditure of Rs. 200 per child per day Mother/guardian accompany and stay with the child throughout and compensated Rs 100 per day for wage loss. • Rs. 100 is expended on diet and medicines per day/ child (Diet- Rs 60 and medicines Rs 40 per child/ day). • • 16 -Mar-18 Health & FW 30
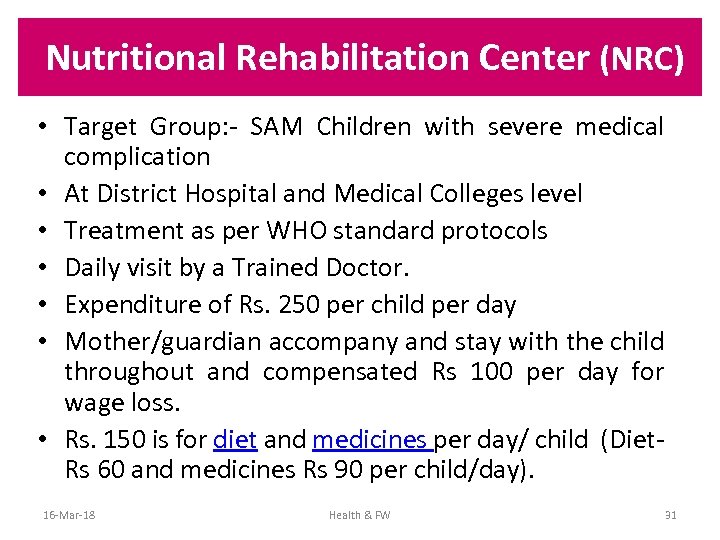
Nutritional Rehabilitation Center (NRC) • Target Group: - SAM Children with severe medical complication • At District Hospital and Medical Colleges level • Treatment as per WHO standard protocols • Daily visit by a Trained Doctor. • Expenditure of Rs. 250 per child per day • Mother/guardian accompany and stay with the child throughout and compensated Rs 100 per day for wage loss. • Rs. 150 is for diet and medicines per day/ child (Diet- Rs 60 and medicines Rs 90 per child/day). 16 -Mar-18 Health & FW 31
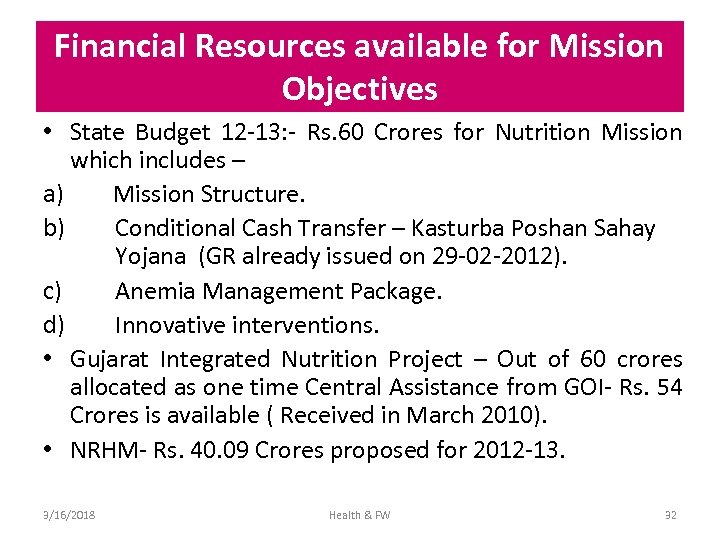
Financial Resources available for Mission Objectives • State Budget 12 -13: - Rs. 60 Crores for Nutrition Mission which includes – a) Mission Structure. b) Conditional Cash Transfer – Kasturba Poshan Sahay Yojana (GR already issued on 29 -02 -2012). c) Anemia Management Package. d) Innovative interventions. • Gujarat Integrated Nutrition Project – Out of 60 crores allocated as one time Central Assistance from GOI- Rs. 54 Crores is available ( Received in March 2010). • NRHM- Rs. 40. 09 Crores proposed for 2012 -13. 3/16/2018 Health & FW 32
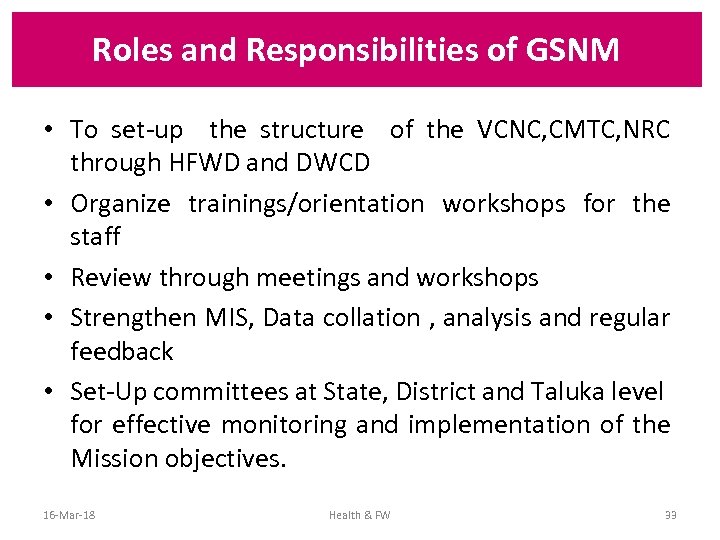
Roles and Responsibilities of GSNM • To set-up the structure of the VCNC, CMTC, NRC through HFWD and DWCD • Organize trainings/orientation workshops for the staff • Review through meetings and workshops • Strengthen MIS, Data collation , analysis and regular feedback • Set-Up committees at State, District and Taluka level for effective monitoring and implementation of the Mission objectives. 16 -Mar-18 Health & FW 33
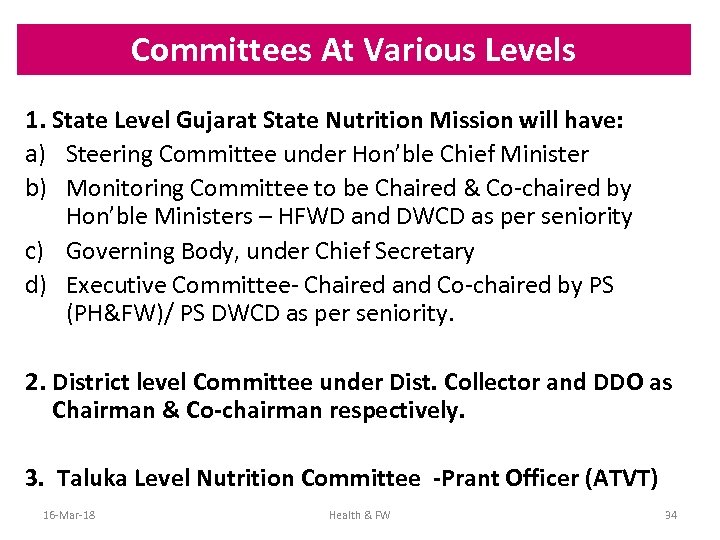
Committees At Various Levels 1. State Level Gujarat State Nutrition Mission will have: a) Steering Committee under Hon’ble Chief Minister b) Monitoring Committee to be Chaired & Co-chaired by Hon’ble Ministers – HFWD and DWCD as per seniority c) Governing Body, under Chief Secretary d) Executive Committee- Chaired and Co-chaired by PS (PH&FW)/ PS DWCD as per seniority. 2. District level Committee under Dist. Collector and DDO as Chairman & Co-chairman respectively. 3. Taluka Level Nutrition Committee -Prant Officer (ATVT) 16 -Mar-18 Health & FW 34
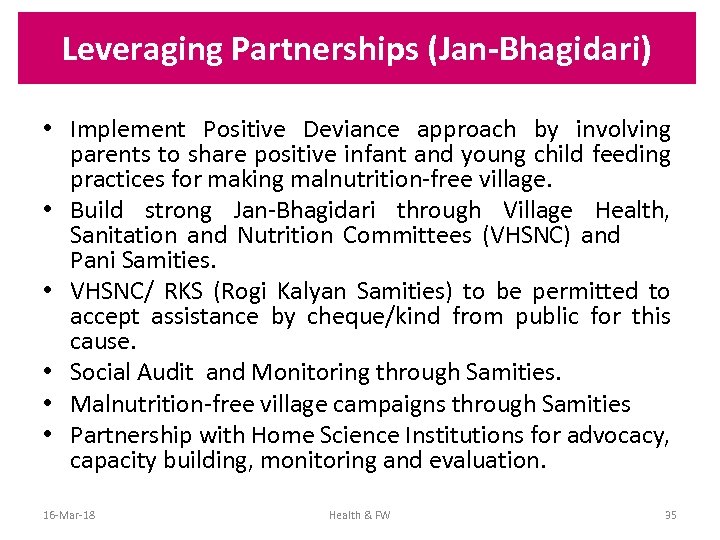
Leveraging Partnerships (Jan-Bhagidari) • Implement Positive Deviance approach by involving parents to share positive infant and young child feeding practices for making malnutrition-free village. • Build strong Jan-Bhagidari through Village Health, Sanitation and Nutrition Committees (VHSNC) and Pani Samities. • VHSNC/ RKS (Rogi Kalyan Samities) to be permitted to accept assistance by cheque/kind from public for this cause. • Social Audit and Monitoring through Samities. • Malnutrition-free village campaigns through Samities • Partnership with Home Science Institutions for advocacy, capacity building, monitoring and evaluation. 16 -Mar-18 Health & FW 35
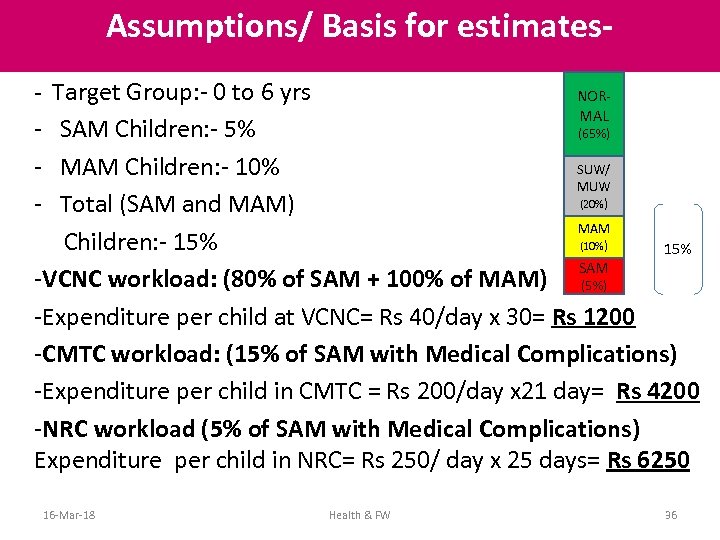
Assumptions/ Basis for estimates- - Target Group: - 0 to 6 yrs NORMAL - SAM Children: - 5% (65%) SUW/ - MAM Children: - 10% MUW (20%) - Total (SAM and MAM) MAM Children: - 15% (10%) 15% SAM -VCNC workload: (80% of SAM + 100% of MAM) (5%) -Expenditure per child at VCNC= Rs 40/day x 30= Rs 1200 -CMTC workload: (15% of SAM with Medical Complications) -Expenditure per child in CMTC = Rs 200/day x 21 day= Rs 4200 -NRC workload (5% of SAM with Medical Complications) Expenditure per child in NRC= Rs 250/ day x 25 days= Rs 6250 16 -Mar-18 Health & FW 36
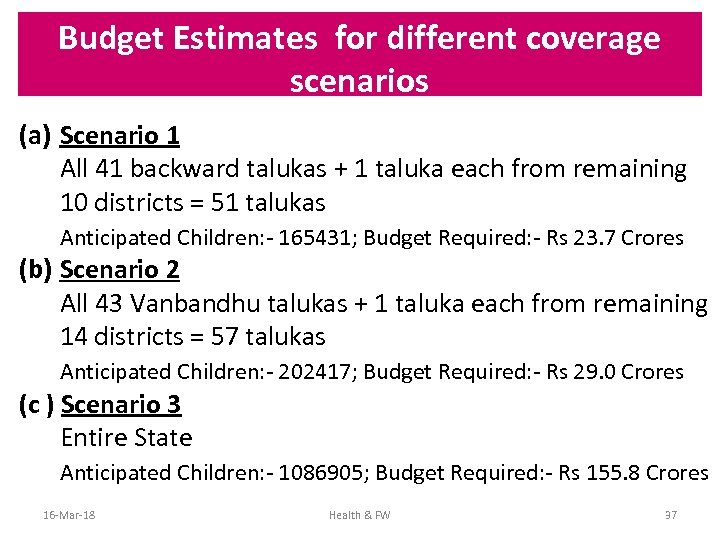
Budget Estimates for different coverage scenarios (a) Scenario 1 All 41 backward talukas + 1 taluka each from remaining 10 districts = 51 talukas Anticipated Children: - 165431; Budget Required: - Rs 23. 7 Crores (b) Scenario 2 All 43 Vanbandhu talukas + 1 taluka each from remaining 14 districts = 57 talukas Anticipated Children: - 202417; Budget Required: - Rs 29. 0 Crores (c ) Scenario 3 Entire State Anticipated Children: - 1086905; Budget Required: - Rs 155. 8 Crores 16 -Mar-18 Health & FW 37
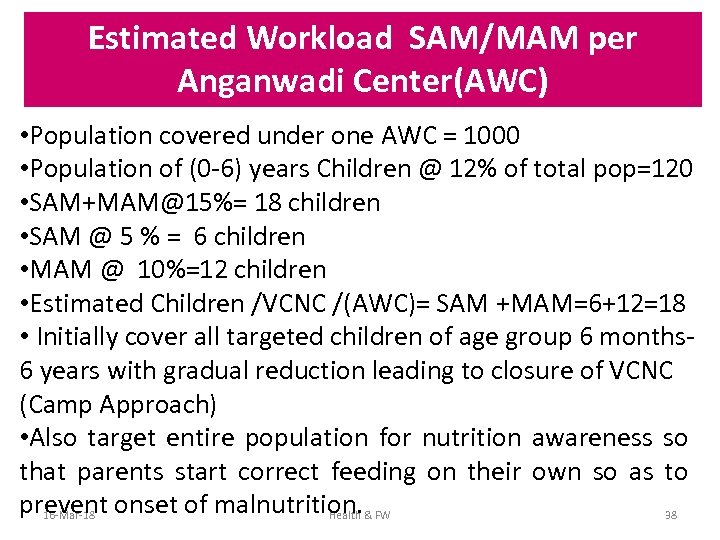
Estimated Workload SAM/MAM per Anganwadi Center(AWC) • Population covered under one AWC = 1000 • Population of (0 -6) years Children @ 12% of total pop=120 • SAM+MAM@15%= 18 children • SAM @ 5 % = 6 children • MAM @ 10%=12 children • Estimated Children /VCNC /(AWC)= SAM +MAM=6+12=18 • Initially cover all targeted children of age group 6 months- 6 years with gradual reduction leading to closure of VCNC (Camp Approach) • Also target entire population for nutrition awareness so that parents start correct feeding on their own so as to prevent onset of malnutrition. 16 -Mar-18 Health & FW 38
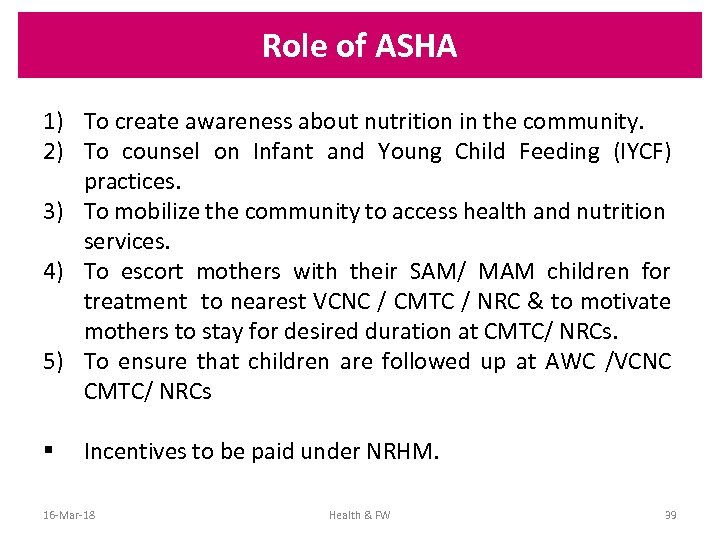
Role of ASHA 1) To create awareness about nutrition in the community. 2) To counsel on Infant and Young Child Feeding (IYCF) practices. 3) To mobilize the community to access health and nutrition services. 4) To escort mothers with their SAM/ MAM children for treatment to nearest VCNC / CMTC / NRC & to motivate mothers to stay for desired duration at CMTC/ NRCs. 5) To ensure that children are followed up at AWC /VCNC CMTC/ NRCs § Incentives to be paid under NRHM. 16 -Mar-18 Health & FW 39
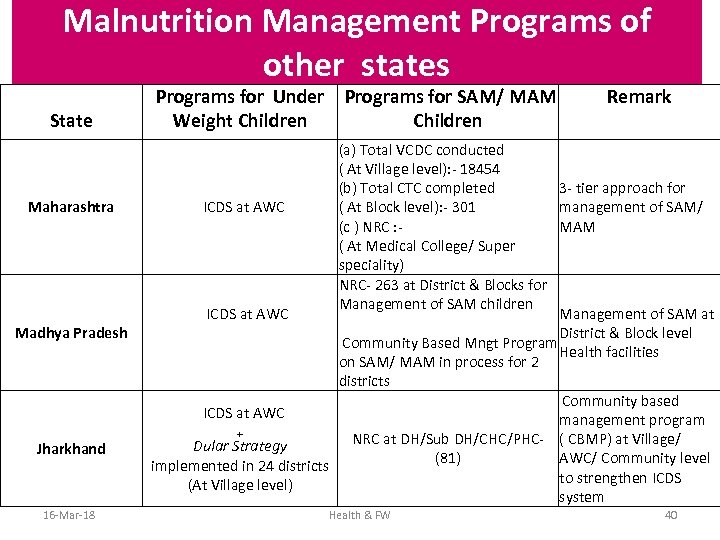
Malnutrition Management Programs of other states State Maharashtra Madhya Pradesh Jharkhand 16 -Mar-18 Programs for Under Weight Children Programs for SAM/ MAM Children Remark (a) Total VCDC conducted ( At Village level): - 18454 3 - tier approach for (b) Total CTC completed ICDS at AWC ( At Block level): - 301 management of SAM/ (c ) NRC : - MAM ( At Medical College/ Super speciality) NRC- 263 at District & Blocks for Management of SAM children ICDS at AWC Management of SAM at District & Block level Community Based Mngt Program Health facilities on SAM/ MAM in process for 2 districts Community based ICDS at AWC management program + NRC at DH/Sub DH/CHC/PHC- ( CBMP) at Village/ Dular Strategy (81) AWC/ Community level implemented in 24 districts to strengthen ICDS (At Village level) system Health & FW 40
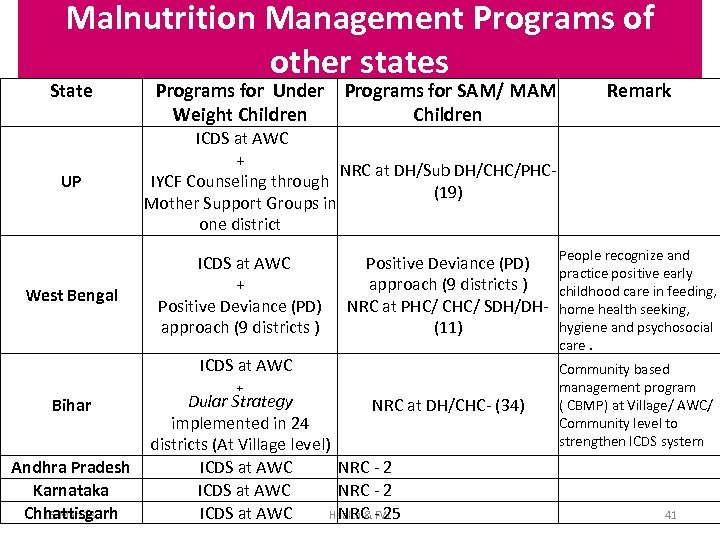
Malnutrition Management Programs of other states State UP West Bengal Programs for Under Weight Children Programs for SAM/ MAM Children ICDS at AWC + NRC at DH/Sub DH/CHC/PHC- IYCF Counseling through (19) Mother Support Groups in one district ICDS at AWC + Positive Deviance (PD) approach (9 districts ) Positive Deviance (PD) People recognize and practice positive early approach (9 districts ) childhood care in feeding, NRC at PHC/ CHC/ SDH/DH- home health seeking, hygiene and psychosocial (11) ICDS at AWC Bihar Andhra Pradesh Karnataka Chhattisgarh 16 -Mar-18 Remark + Dular Strategy NRC at DH/CHC- (34) implemented in 24 districts (At Village level) ICDS at AWC NRC - 25 Health & FW care. Community based management program ( CBMP) at Village/ AWC/ Community level to strengthen ICDS system 41
Rajmata Jijau Mother –Child Health and Nutrition (RJMCHN) Mission, Maharashtra-Case Study 16 -Mar-18 Health & FW 42
Operational Facets (Maharashtra) • Independent and autonomous Mission Structure. • Neither Society nor Trust, steering by CM • Headed by a very senior IAS Officer of PS/Secretary level on full time basis as Director-General of the Mission • Committed Officers (3 to 4) identified and posted in the Mission to assist the Director -General. • Champions (people willing to contribute) identified in all Depts. • Nodal Department is DWCD. • Funding from multiple sources like DWCD, NRHM, TSP, SCSP, District Planning Boards, etc. 16 -Mar-18 Health & FW 43
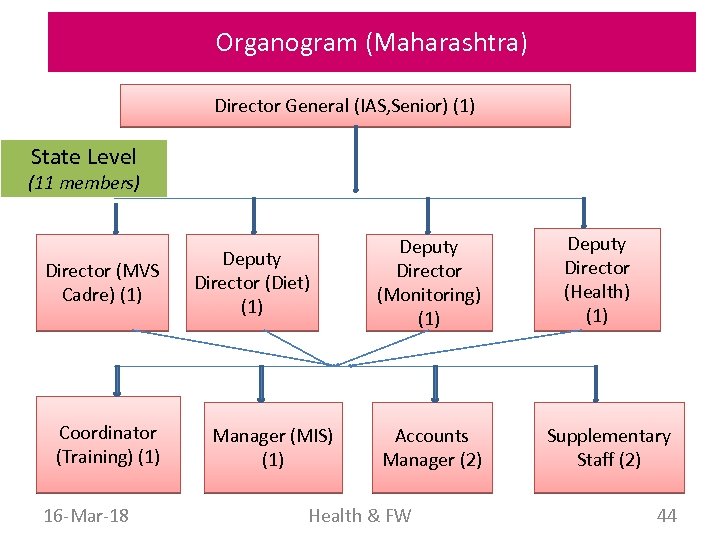
Organogram (Maharashtra) Director General (IAS, Senior) (1) State Level (11 members) Director (MVS Cadre) (1) Coordinator (Training) (1) 16 -Mar-18 Deputy Director (Diet) (1) Manager (MIS) (1) Deputy Director (Monitoring) (1) Accounts Manager (2) Health & FW Deputy Director (Health) (1) Supplementary Staff (2) 44
Levels of Intervention (Maharashtra) Three tier approach adopted in Maharashtra: 1. Village Child Development Centres / Camps (VCDC) at AWCs- 30 days camp 2. Child Treatment Centres / Camps (CTC) – at PHC/ Subdistrict/ district hospitals- 21 days camp on residential basis 3. Nutrition Rehabilitation Centres (NRC)- Medical College / super specialty hospitals- as per need. 16 -Mar-18 Health & FW 45
Committee Structure (Maharashtra) There are three committees : - 1. Mission Steering Committee : Headed by Hon. Chief Minister of Maharashtra 2. Mission Monitoring Committee : Headed by Hon. Minister, DWCD 3. Mission Advisory Committee : Headed by Hon. ACS (Health) 16 -Mar-18 Health & FW 46
Village Child Development Camps /Centre (Maharashtra) • Both SAM and MAM children • At Village level, at Anganwadi Centres managed by AWW and Helper • Nutritional Supplements as per protocols • Incentive to AWW and AWH • Stay is for full 30 days • Daily visit by a Dr and an ANM • An expenditure of Rs 32/- per child/day: Rs 16 for diet (Dynamic as per region) , Rs 8/- for Medicines and Rs. 8/- for Incentives. • Done in a camp approach. 16 -Mar-18 Health & FW 47
Child Treatment Centre (Maharashtra) Child Treatment Camps CTC • At PHC / CHC / SDH level • Treatment as per protocols • Mother/guardian accompany and stay with the child throughout and compensated Rs 60 per day for wage loss. • Follow a camp approach for 21 days • Expenditure of Rs. 160 per child per day • Rs. 100 is expended per day on the diet and medicines of the child and mother/ guardian 16 -Mar-18 Health & FW 48
Efforts done on IEC/ BCC (Maharashtra) • IEC Action Plan of Rs. 6. 23 crores covering activities from state to village level for campaign. • Rajmata Jijau Malnutrition- Free Village Campaign Each village attaining malnutrition free status are selected for Malnutrition- Free village award scheme which comprises of award Rs. 1000/- and Rs 100/child as award for bringing each child in normal category. • Rajmata Jijau Excellence award for first 3 Malnutrition Free Villages in each district i. e. (a) -1 st Prize- Rs 1, 000 and Certificate. (b) - 2 nd Prize- Rs 50, 000 and Certificate. (c ) – 3 rd Prize- Rs 50, 000 and Certificate. A budget of Rs 10 crores /annum has been provided for this initiative 16 -Mar-18 Health & FW 49
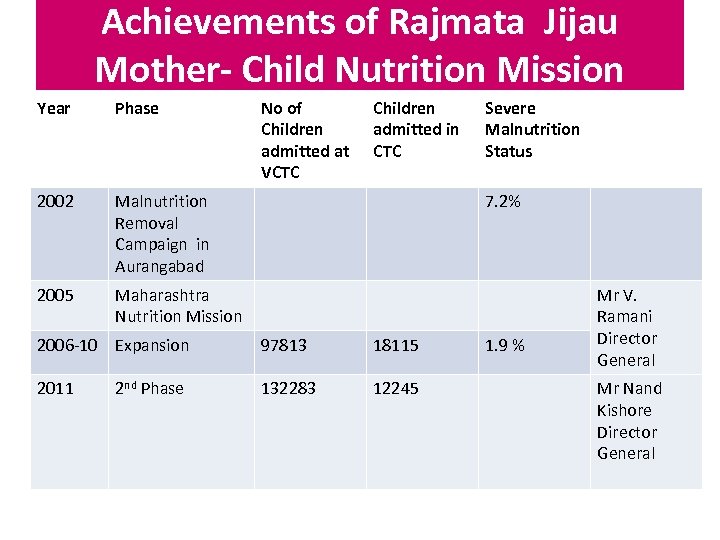
Achievements of Rajmata Jijau Mother- Child Nutrition Mission Year Phase 2002 Malnutrition Removal Campaign in Aurangabad 2005 No of Children admitted at VCTC Children admitted in CTC Maharashtra Nutrition Mission 7. 2% 2006 -10 Expansion 97813 18115 2011 132283 12245 2 nd Phase Severe Malnutrition Status 1. 9 % Mr V. Ramani Director General Mr Nand Kishore Director General
Way Forward…. . • Nodal Departments of Gujarat State Nutrition Mission- HFWD & WCD • A separate Nutrition Mission structure • Society Structure as suggested • A Full time Mission Director/Director General for Gujarat State Nutrition Mission • Screening criteria for SAM/MAM Children as per WHO Standard to be accepted in addition to SUW/MUW • 3 -Tier approach of Maharashtra namely VCNC, CMTC and NRC merits consideration. • Malnutrition- Free Village Campaign. • Strategy need to be separately workout by WCD and Health on Adolescent and Maternal Nutrition. 16 -Mar-18 Health & FW 51
Thanks 16 -Mar-18 Health & FW 52
38044ff918f8c0a77d2774a918558d71.ppt