1b2d5084baca71c3e28f302900b371eb.ppt
- Количество слайдов: 164
Guide to diabetes Dr. Hussein Kamal An internist & endocrinologist
Definition • Diabetes mellitus is a syndrome characterised by chronic hyperglycaemia and disturbance of carbohydrate, fat and protein metabolism associated with absolute or relative deficiency in in insulin secretion andor insulin action.
Insulin allows glucose (sugar) to enter body cells to convert it into energy. Insulin is also needed to synthesize protein and store fats. In un controlled diabetes, glucose and lipids (fats) remain in the blood stream and, with time damage the body’s vital organs and contribute to heart disease.
Classification Diabetes is classified into three main types: • Type 1 previously called insulin-dependent diabetes mellitus (IDDM) • Type 2 previously called non-insulindependent diabetes mellitus(NIDDM) • Gestational Diabetes Mellitus(GDM)
Type 1 Diabetes Occurrence: • Autoimmune disease wherein the immune system attacks B-cells of pancreas and destroys them. The pancreas then produce little or no insulin. • Scientists do not know exactly what causes the body’s immune system to attack the B-cells, but they believe that both genetic factors and environmental factors and possibly viruses, are involved.
Characteristics: • Often develops in children and young adults, but the disorder can appear at any age. • Symptoms usually develop over a short period, although B-cell destruction can begin year earlier. • If not diagnosed and treated with insulin, a person can lapse into a life-threatening diabetic coma, also known as diabetic ketoacidosis.
Type 2 diabetes Occurrence: • The most common form of diabetes. • Due to reduce insulin secretion or peripheral resistance to action of insulin. • The result is the same as for Type 1 diabetes, glucose builds up in the blood and the body cannot make efficient use of its main source of fuel.
• Often part of a metabolic syndrome that includes obesity, elevated blood pressure, and high levels of blood lipids.
Characteristics: • Contributes 90 to 95% of total diabetes and onethird not been diagnosed. • This form of diabetes usually develops in adults. • About 80% of people with Type 2 diabetes are overweight. • Increase in incidence of childhood obesity leads to Type 2 diabetes becoming more common in young people
Symptoms & Management for Type 1 and Type 2 Diabetes Symptoms: • Increased thirst and urination. • Constant hunger. • Weight loss. • Blurred vision • Extreme fatigue. • Slow healing of wounds or sores.
Management: • Diet • Exercise • Insulin for Type 1 and OHAs or insulin in Type 2 • Education • Monitoring blood glucose and therapy
Gestational Diabetes: Occurrence: • Develops in pregnancy and disappears after delivery, however with increased risk in getting later in life • Insulin resistance due to pregnancy. • Genetic predisposition.
Management: • Diet: provide adequate calories which will not lead to hyperglycemia or ketonemia. • Exercise: that does not cause fetal distress, contractions or hypertension. • Insulin: to maintain blood glucose, fasting<=95 mg/dl (<=5. 3 mmol/l); one hour post prandially <=120 mg/dl(<=6. 7 mmol/l).
Diagnosis The fasting plasma glucose test in the preferred test for diagnosis Type 1 or Type 2 diabetes. However, a diagnosis of diabetes is made by an one of the three positive tests, with a second positive on a different day:
• A random Plasma glucose value (taken any time of day) of 200 mg/dl or more, along with the presence of diabetes symptoms. • A plasma glucose value of 126/mgd. L or more, after a person has fasted for 8 hours
• An oral glucose tolerance test (OGTT) plasma glucose value of 200 mg/d. L or more in the blood sample, taken 2 hours after a person has consumed a drink containing 75 grams of glucose dissolved in water. This test, taken in a laboratory or the doctor’s office, measures plasma glucose at timed intervals over a 3 -hour period.
Gestational Diabetes Diagnosed based on plasma glucose values measured during the OGTT. Glucose levels are normally lower during pregnancy, so the threshold values for diagnosis of diabetes in pregnancy are lower. If women has two plasma glucose values equal to or more than any of the following values after a 100 gm OGTT, she has gestational diabetes:
• 1 -hour level of 180 mg/d. L • 2 -hour level of 155 mg/d. L or 3 -hour level of 140 mg/d. L • Fasting plasma glucose level of 95 mg/d. L
People with impaired glucose metabolism, a state between normal and diabetes are at risk for developing diabetes, heart attacks, and strokes. There are two forms of impaired glucose metabolism.
Impaired Fasting Glucose (IFG): • Fasting plasma glucose level of 110 to 125 mg/d. L, a level higher than normal but less than the level indicating a diagnosis of diabetes.
Impared Glucose Tolerance (IGT) Means that blood glucose during the oral glucose tolerance test is higher than normal but not high enough for a diagnosis of diabetes. IGT is diagnosed when the glucose level is 141 to 199 mg/d. L, 2 hours after a person is given a drink containing 75 grams of glucose.
OGTT • OGTT is performed using a 75 or 100 gm oral glucose load in the morning after a noncaloric 8 hour fast. Water is allowed, but not coffee or smoking. • Test should be performed on an individual without underlying illness and/or interfering drugs. OGTT is not appropriate for a patient who is malnourished, on a restricted carbohydrate diet, or with acute and chronic illness.
• Patient should be ambulatory and not to bed rest, hospitalized , or immobilized. During the test, patient should be resting comfortably. • Patient should consume an unrestricted diet containing at least 150 g carbohydrate daily for three days before test. • Just a confirmatory test, not to be done regularly.
Glycated Hemoglobin (Hb. A 1 c) Test • Indicates blood glucose control over a period of approximately 3 months. • Normal range varies depending on the method the lab uses: usually 4 -7%, correlating to average blood glucose of 60150 mg/dl (3. 3 -8. 3 mmol/l)
• Should be prescribed by health care provider every three months for Type 1 diabetes and at 3 -6 months intervals for Type 2, to help determine overall control. • Patient does not need to be fasting to have this blood test performed
Ketone Test • Ketone is by product of fat metabolism; presence of ketone indicates that the body is not metabolizing food properly because of lack of available insulin or carbohydrate; may indicate impeding or established diabetic ketoacidosis (DKA), a condition that requires immediate medical attention.
Method: Dipstick When to test: • When blood glucose level is consistently >300 mg/dl (16. 7 mmol/l). • During period of acute illness (illness is a stress that can cause and hyperglycemia). • When symptoms of hyperglycemia accompanied by nausea, vomiting and abdominal pain are present.

Treatment strategy
Goals Of Treatment • Control high blood glucose (hyperglycemia) • Avoid low blood glucose (hypoglycemia). • Treatment of associated conditions, such as high blood pressure, cholesterol disorder and obesity. • Prevent or retard the progression of complications of diabetes such as blindness, kidney failure, heart disease, stroke and amputation of legs.
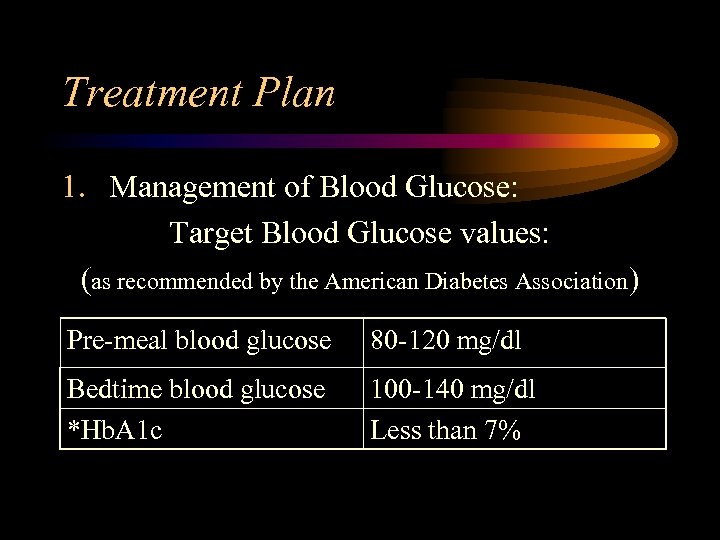
Treatment Plan 1. Management of Blood Glucose: Target Blood Glucose values: (as recommended by the American Diabetes Association) Pre-meal blood glucose 80 -120 mg/dl Bedtime blood glucose *Hb. A 1 c 100 -140 mg/dl Less than 7%
• However, not every person is a candidate for such tight blood glucose control. This should not be attempted in: • Frail, elderly person who have already developed the complications of diabetes such as blindness and end-stage kidney failure. • Elderly patients having frequent low blood glucose episodes.
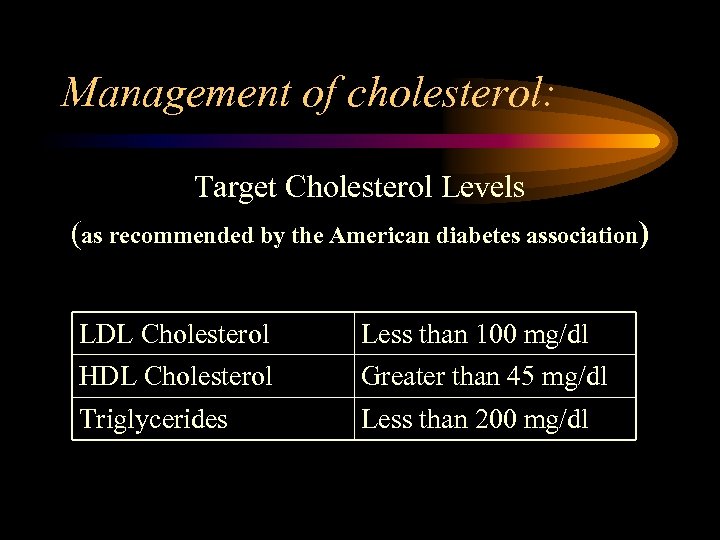
Management of cholesterol: Target Cholesterol Levels (as recommended by the American diabetes association) LDL Cholesterol Less than 100 mg/dl HDL Cholesterol Greater than 45 mg/dl Triglycerides Less than 200 mg/dl
Management of High Blood Pressure • Target blood pressure in diabetic patients should be less than systolic 130/ diastolic 85 mm Hg, as recommended by the American diabetes Association. • The treatment strategy also involves correct nutrition, moderate exercise and proper medication.
Nutrition • Nutrition is an important element in diabetes management. • Diet content should be 10 -2 -% protein, 60% carbohydrates and 20% fats.
Do’s of diabetic diets • Consistency in diet and meal timings according to medicines. • Multivitamin containing an antioxidant such as vitamin , beta-carotene, vitamins C and E. • Minimum of 1200 kcal/day for women and 1500 kcal/day for men.
• Sodium level (salt intake) should be maintained between 2. 4 and 3. 0 gm/day for people without hypertension and >2. 4 gm/day for people with mild to moderate hypertension. • Fibre of approximately 20 - 35 gm/day from a variety of food sources should be consumed
Don’ts of diabetic diets • Avoid alcohol especially if diabetes is not in control. • Avoid in-between meals. Adhere to the time and size of the meal decided. • Avoid fasts and fasting alters body metabolism, adversely affecting the diabetic state.
Exercise • Exercise can improve the health and outlook of life. Regular and controlled exercise not only helps to increase glucose utilization but also helps to maintain desirable health.
Do’s in exercise • Check the patients for blood pressure, blood fat levels, Hb. A 1 c, health of heart, circulatory and nervous systems, kidney function, eyes and feet. • Choose exercises that fit the patient’s health. • Exercise should be preceded and followed by 5 -10 minutes of slow, continuous, aerobic activities.
• Remember the feet. Advice them to wear the comfortable shoes for the sport. • Watch the low blood sugar, insulin or oral diabetes medicine may lead to low blood sugar levels. • Advice the patients to keep a snack handy to avoid low blood sugar levels during the exercise.
Don’ts in exercise • Advise not to snack unnecessarily before exercise. • Uncomfortable shoes should not be worn while exercising. • Avoid exercising in extreme cold or heat. • Exceeding target heart rate of 60 to 80% of estimated maximum heart rate.
Oral Hypoglycemic Agents • OHAs are primarily used in type 2 diabetes adjunct to nutrition therapy and exercise. • Oral agents are broadly classified as follows:
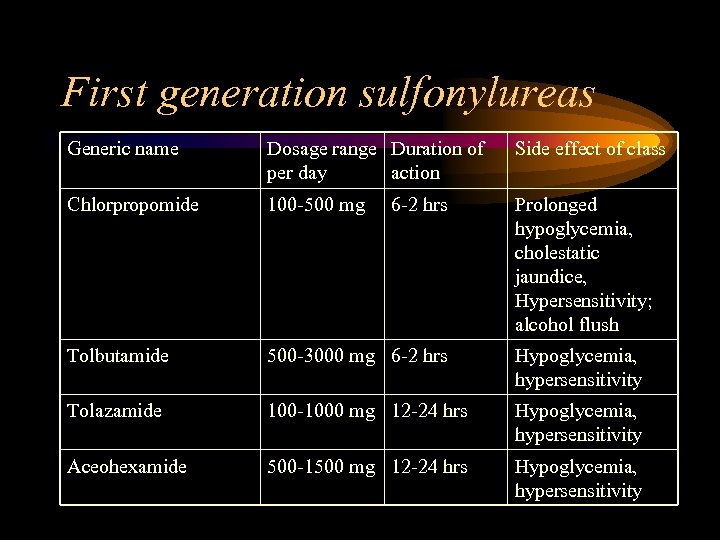
First generation sulfonylureas Generic name Dosage range Duration of per day action Side effect of class Chlorpropomide 100 -500 mg Prolonged hypoglycemia, cholestatic jaundice, Hypersensitivity; alcohol flush Tolbutamide 500 -3000 mg 6 -2 hrs Hypoglycemia, hypersensitivity Tolazamide 100 -1000 mg 12 -24 hrs Hypoglycemia, hypersensitivity Aceohexamide 500 -1500 mg 12 -24 hrs Hypoglycemia, hypersensitivity 6 -2 hrs
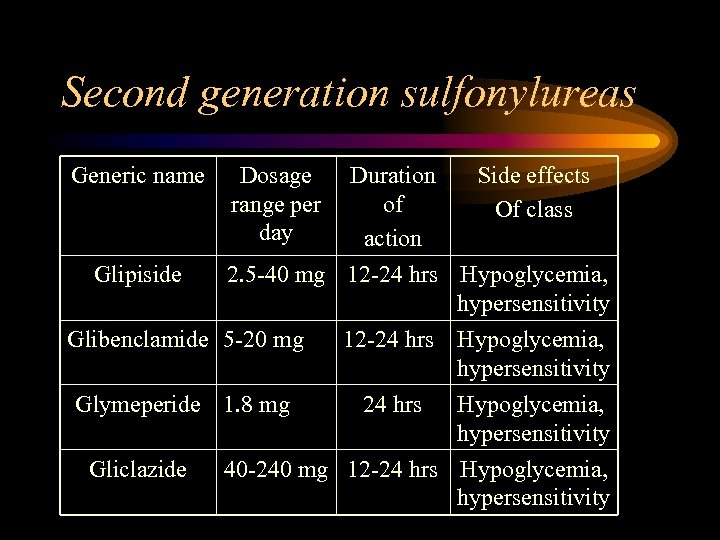
Second generation sulfonylureas Generic name Glipiside Dosage range per day Duration Side effects of Of class action 2. 5 -40 mg 12 -24 hrs Hypoglycemia, hypersensitivity Glibenclamide 5 -20 mg Glymeperide 1. 8 mg Gliclazide 12 -24 hrs Hypoglycemia, hypersensitivity 40 -240 mg 12 -24 hrs Hypoglycemia, hypersensitivity
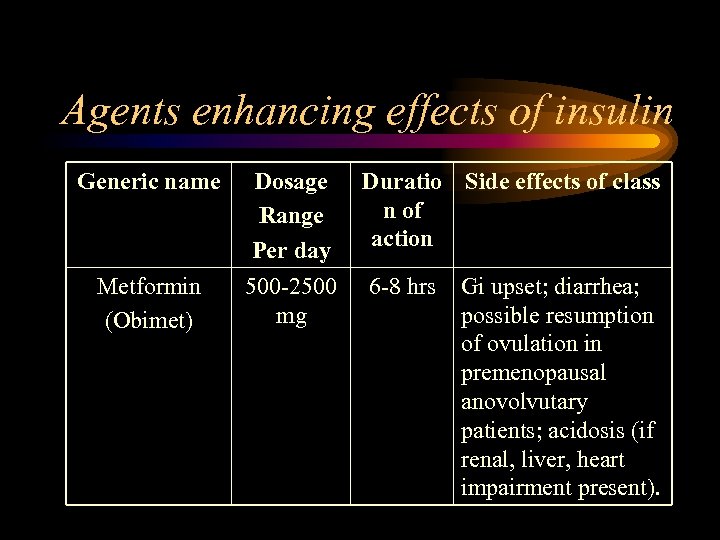
Agents enhancing effects of insulin Generic name Metformin (Obimet) Dosage Range Per day 500 -2500 mg Duratio Side effects of class n of action 6 -8 hrs Gi upset; diarrhea; possible resumption of ovulation in premenopausal anovolvutary patients; acidosis (if renal, liver, heart impairment present).
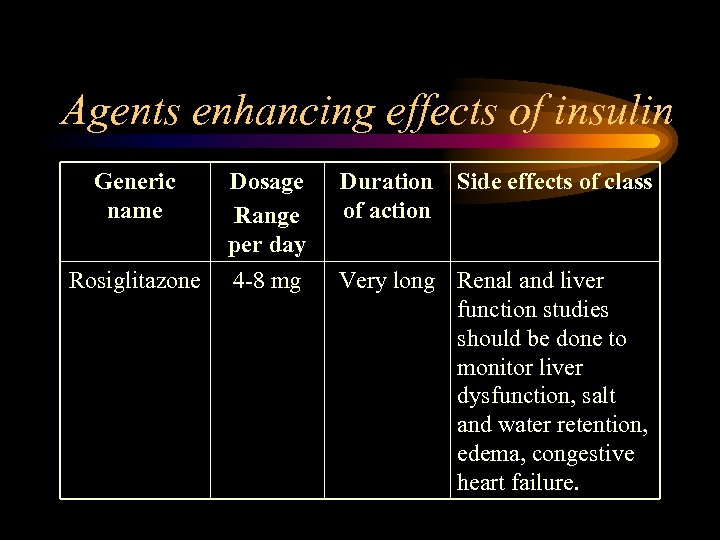
Agents enhancing effects of insulin Generic name Rosiglitazone Dosage Range per day 4 -8 mg Duration Side effects of class of action Very long Renal and liver function studies should be done to monitor liver dysfunction, salt and water retention, edema, congestive heart failure.
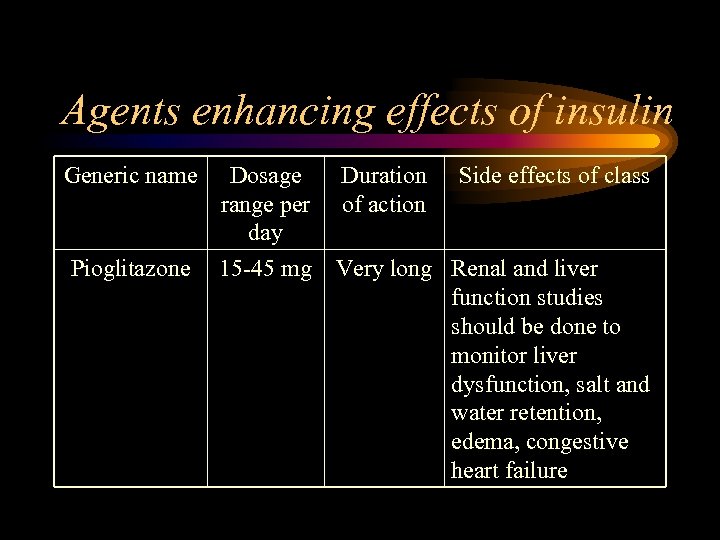
Agents enhancing effects of insulin Generic name Dosage range per day Duration of action Side effects of class Pioglitazone 15 -45 mg Very long Renal and liver function studies should be done to monitor liver dysfunction, salt and water retention, edema, congestive heart failure
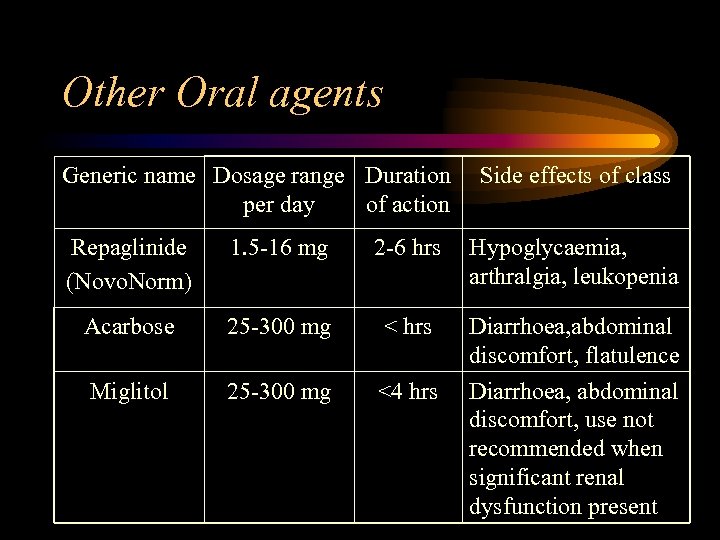
Other Oral agents Generic name Dosage range Duration per day of action Side effects of class Repaglinide (Novo. Norm) 1. 5 -16 mg 2 -6 hrs Hypoglycaemia, arthralgia, leukopenia Acarbose 25 -300 mg < hrs Miglitol 25 -300 mg <4 hrs Diarrhoea, abdominal discomfort, flatulence Diarrhoea, abdominal discomfort, use not recommended when significant renal dysfunction present
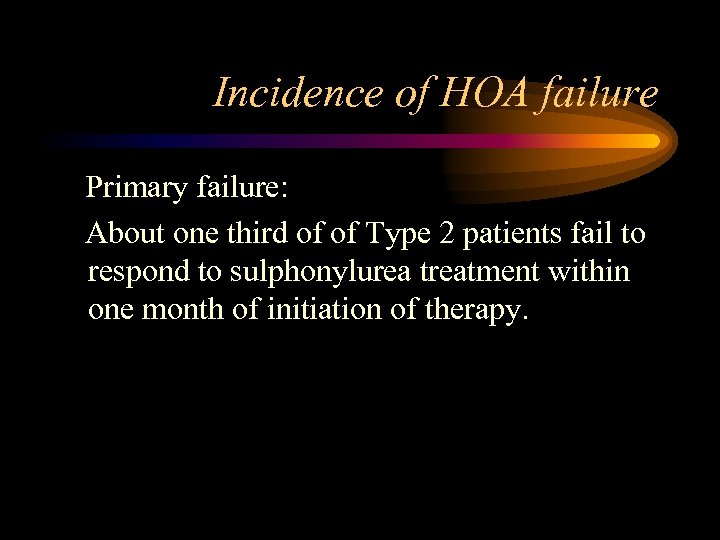
Incidence of HOA failure Primary failure: About one third of of Type 2 patients fail to respond to sulphonylurea treatment within one month of initiation of therapy.
Secondary failure: • Of the patients that initially achieve satisfactory glycaemic control, about 5 to 10% go on to develop secondary failure each year, so that after 10 years only about half of the patients continue to have satisfactory response.
Secondary failure: (continued) • From the data of the UKPD study, it appears by the sixth year, approximately 50% of the patients randomized to sulphonylurea needed supplemental insulin to maintain adequate glycemic control.
Diagnosis OHA failure: • It is a condition in which an individual does not respond adequately/ satisfactorily with OHAs. • Clinically, following parameters can be of great relevance in diagnosing OHA failure: 1. Inadequate improvement in the classical signs and symptoms of diabetes viz. , polydypsia, polyuria, polyphagia and fatigue.
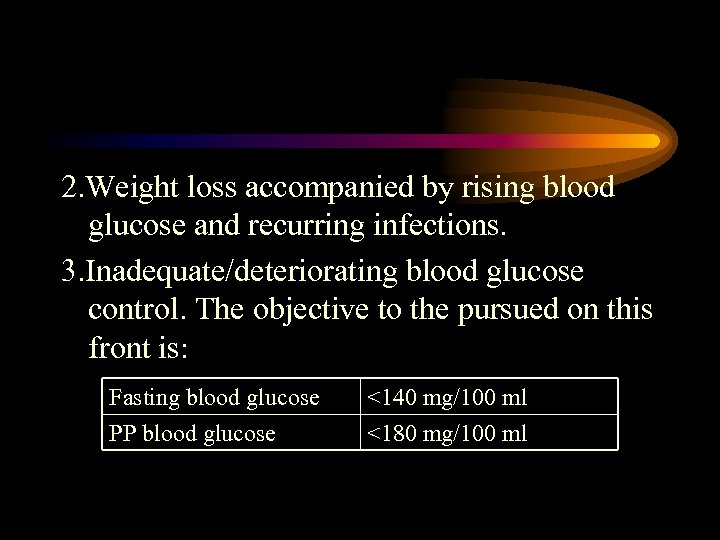
2. Weight loss accompanied by rising blood glucose and recurring infections. 3. Inadequate/deteriorating blood glucose control. The objective to the pursued on this front is: Fasting blood glucose PP blood glucose <140 mg/100 ml <180 mg/100 ml
4. High and increasing number of tablets with inadequate control; especially exceeding two to two and a half tablets in case of commonly used OHA.
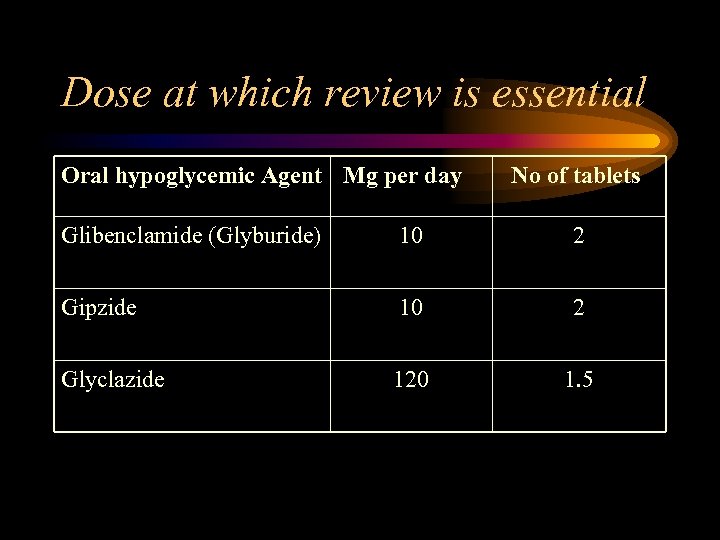
Dose at which review is essential Oral hypoglycemic Agent Mg per day No of tablets Glibenclamide (Glyburide) 10 2 Gipzide 10 2 Glyclazide 120 1. 5
Dose at which review is essential • Poor performance with the above doses indicates the necessity to review the entire therapy and therapeutic alternative to be considered at this point of time is initiation of insulin therapy
In case of Type 2 diabetes, there are 2 possibilities: • Stop HOA treatment and start insulin therapy (substitution) or • Continue OHA treatment and add insulin therapy (supplement)
Oral antidiabetics are contraindicated in Type 1 diabetes and in Type 2 diabetes undergoing surgery, serve infections, liver and kidney disease, and gestational diabetes.
Insulin are always used in patients with Type 1 diabetes and may be required in patients with Type 2 diabetes or gestational diabetes. Insulin can be broadly classified on the basis of species, action profile and strength.
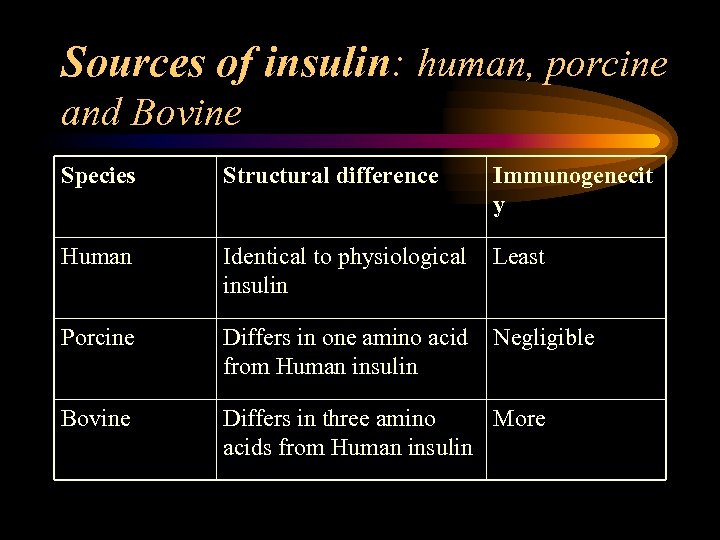
Sources of insulin: human, porcine and Bovine Species Structural difference Immunogenecit y Human Identical to physiological insulin Least Porcine Differs in one amino acid from Human insulin Negligible Bovine Differs in three amino More acids from Human insulin
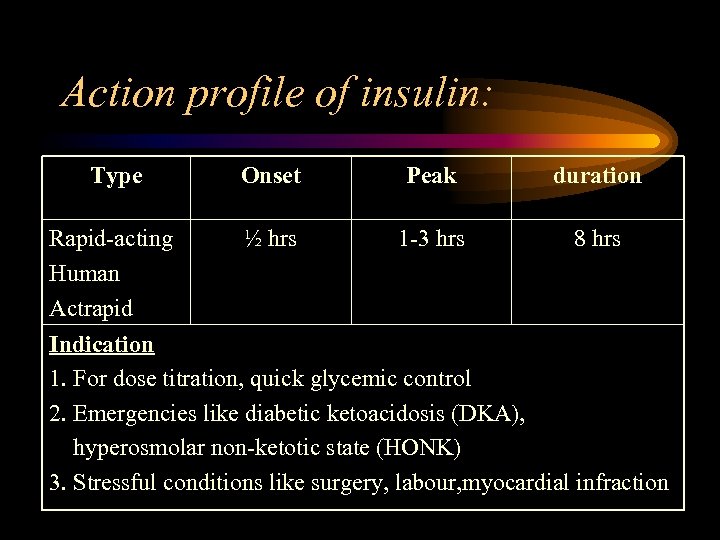
Action profile of insulin: Type Onset Peak duration Rapid-acting Human Actrapid ½ hrs 1 -3 hrs 8 hrs Indication 1. For dose titration, quick glycemic control 2. Emergencies like diabetic ketoacidosis (DKA), hyperosmolar non-ketotic state (HONK) 3. Stressful conditions like surgery, labour, myocardial infraction
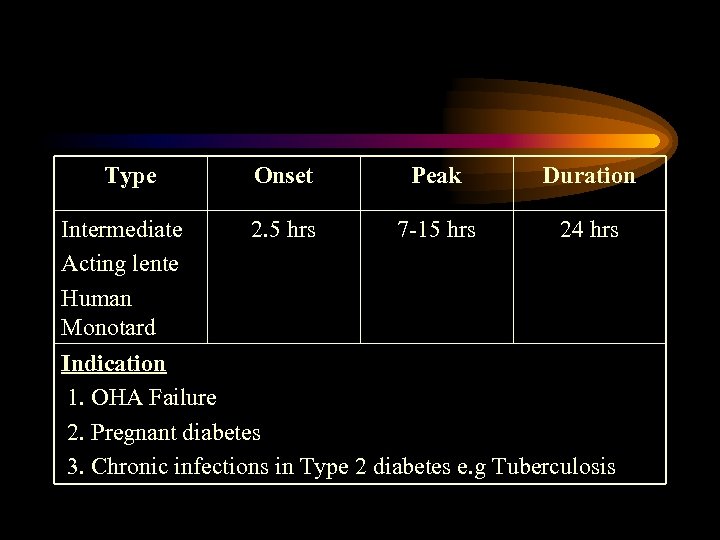
Type Intermediate Acting lente Human Monotard Onset Peak Duration 2. 5 hrs 7 -15 hrs 24 hrs Indication 1. OHA Failure 2. Pregnant diabetes 3. Chronic infections in Type 2 diabetes e. g Tuberculosis
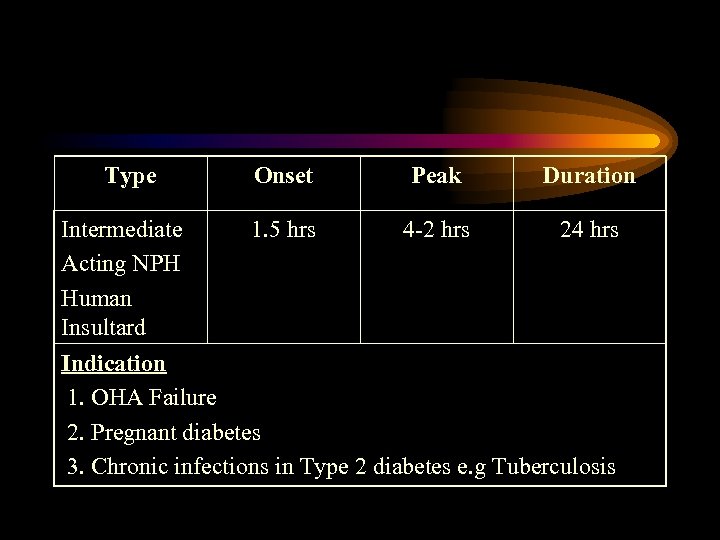
Type Intermediate Acting NPH Human Insultard Onset Peak Duration 1. 5 hrs 4 -2 hrs 24 hrs Indication 1. OHA Failure 2. Pregnant diabetes 3. Chronic infections in Type 2 diabetes e. g Tuberculosis
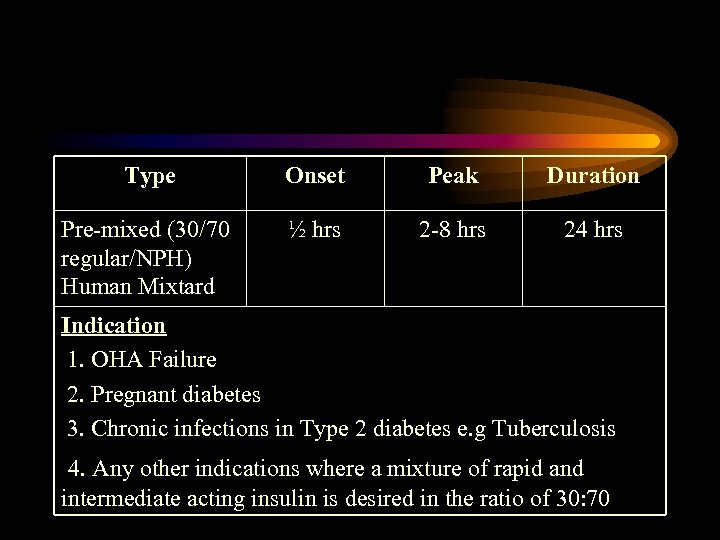
Type Onset Peak Duration Pre-mixed (30/70 regular/NPH) Human Mixtard ½ hrs 2 -8 hrs 24 hrs Indication 1. OHA Failure 2. Pregnant diabetes 3. Chronic infections in Type 2 diabetes e. g Tuberculosis 4. Any other indications where a mixture of rapid and intermediate acting insulin is desired in the ratio of 30: 70
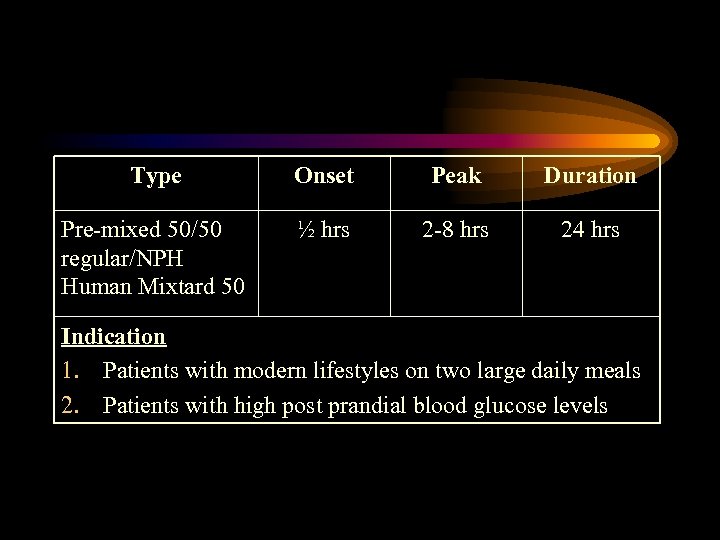
Type Onset Peak Duration Pre-mixed 50/50 regular/NPH Human Mixtard 50 ½ hrs 2 -8 hrs 24 hrs Indication 1. Patients with modern lifestyles on two large daily meals 2. Patients with high post prandial blood glucose levels
Amounts of insulin • Insulin regimen should be individualized depending on lifestyle, activity level and eating pattern. • Continuous treatment and monitoring are the main stay. • Efforts should be taken to keep blood glucose as close to the target range (72 mg/dl before a meal, 180 or less two hours after a meal).
Insulin Initiation Substitutions • Stop OHA tablets. • Start with Intermediate insulin 0. 2 units /kg body weight before breakfast or at bed time (upto a maximum of 20 units). • Increases by 2 -6 units every 3 -4 days if necessary.
Note: • If post prandial blood glucose levels are too high add Rapid action insulin. Alternatively, Pre-mixed insulin could be used. If the dose exceeds 30 -40 units, divide the dose into daily injections 2/3 rd before breakfast and 1/3 rd before dinner.
Supplement • Continue with OHA tablet with out any change in dose. • Start with 0. 1 to 0. 2 units of intermediate insulin per Kg body weight before breakfast or bed time.
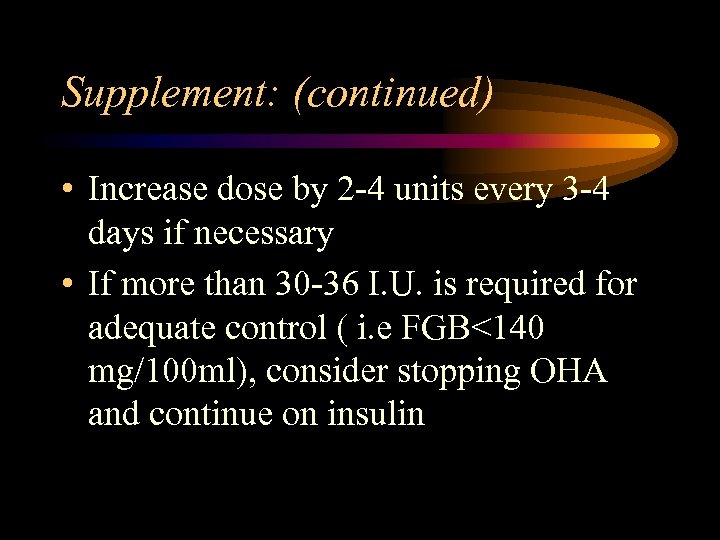
Supplement: (continued) • Increase dose by 2 -4 units every 3 -4 days if necessary • If more than 30 -36 I. U. is required for adequate control ( i. e FGB<140 mg/100 ml), consider stopping OHA and continue on insulin
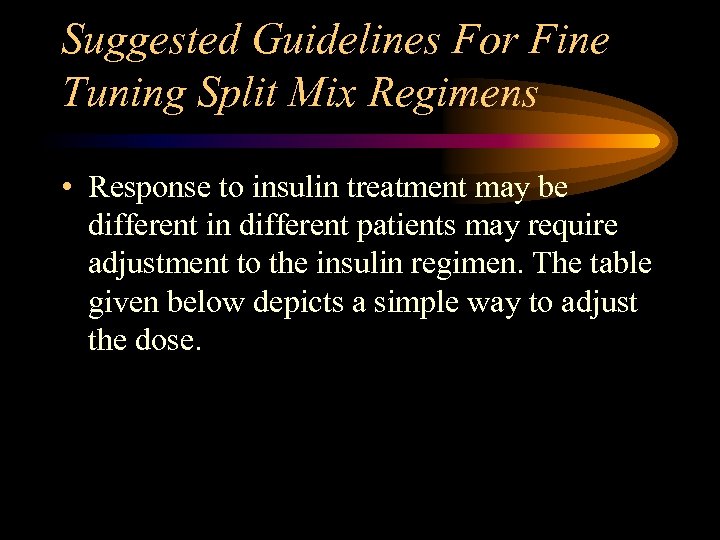
Suggested Guidelines For Fine Tuning Split Mix Regimens • Response to insulin treatment may be different in different patients may require adjustment to the insulin regimen. The table given below depicts a simple way to adjust the dose.
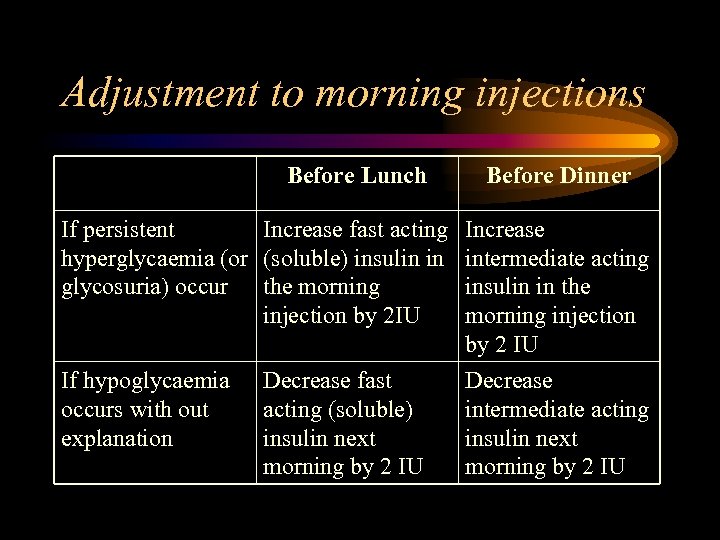
Adjustment to morning injections Before Lunch Before Dinner If persistent Increase fast acting hyperglycaemia (or (soluble) insulin in glycosuria) occur the morning injection by 2 IU Increase intermediate acting insulin in the morning injection by 2 IU If hypoglycaemia occurs with out explanation Decrease intermediate acting insulin next morning by 2 IU Decrease fast acting (soluble) insulin next morning by 2 IU
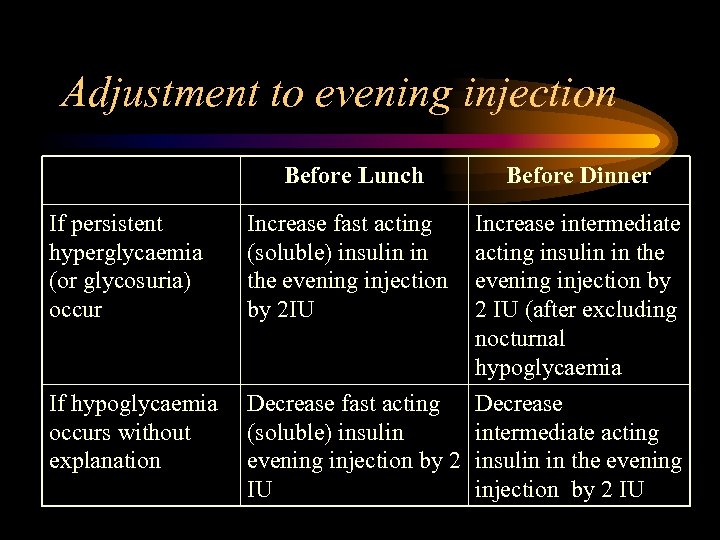
Adjustment to evening injection Before Lunch If persistent hyperglycaemia (or glycosuria) occur If hypoglycaemia occurs without explanation Increase fast acting (soluble) insulin in the evening injection by 2 IU Before Dinner Increase intermediate acting insulin in the evening injection by 2 IU (after excluding nocturnal hypoglycaemia Decrease fast acting Decrease (soluble) insulin intermediate acting evening injection by 2 insulin in the evening IU injection by 2 IU
Mixing Insulin • NPH and short-acting insulin formulations when mixed may be used immediately or stored up to 2 weeks. • Mixing of regular and lente is not recommended unless injected immediately after preparation; binding action of regular and lente begins immediately and effect of regular may be blunted.
Insulin Administration • Choose a syringe compatible with the insulin strength (i. e. 40 I. U. insulin) • For cloudy insulin (suspension) invert the vial a few times until the suspension has been mixed well. • Draw air into syringe corresponding to the prescribed dose of insulin and slowly inject air into vial held vertically at eye level, then draw up insulin
Insulin Administration: continued • Inject excess amount of insulin back into the vial held vertically at eye level and pull out the needle. • Lift up the skin at the injection site in a broad fold and insert needle at an angle of 45 into the subcutaneous tissue, inject insulin slowly. • In order not to injure the tissue beneath the skin rotate the injection site in the chosen area.
Delivery Devises Needle and Syringe • A common way of administering insulin is with a needle and syringe. • Syringes come in a range of capacities (1 ml, 0. 5 ml, or 0. 3 ml) and different strengths. • Most suitable size can be selected to deliver the insulin dosage as per the requirement.
• Needles also come in different gauges and lengths, and have very fine points and special coatings to make them relatively pain-free although some people find them daunting and not very convenient.
Insulin Pens (Novo. Pen 3) • Easiest and the most convenient way of administrating insulin. • Accurate even at extremely low dosage. • Novo. Pen 3 reduces the insulin administration to mere two step procedure: Dial the dose and inject.
Advantages: • Combination of insulin pens and Penfills completely eliminates the need to handle syringes and vials. • No need to mix and measure and therefore improves dosage accuracy. • Novo. Pen 3 is compact enough to fit easily into a purse or pocket and convenient to carry anywhere.
• Launch of single penfills has further enhanced convenience to buy and has also offered economy to the patient by avoiding huge investment at one single time.
Disposable Pens (Novo. Let): • Premixed, prefilled and ready to use disposable insulin delivery devices. • Patients just have to dial dose, inject and dispose the pen after use of 300 units of insulin. Novo. Lets useful in initiating insulin therapy in
• OHA inadequacy and failure • Pre and post operative conditions • Gestational diabetes mellitus Novo. Lets are available in all the varieties of insulin viz. Mixtard 30 Novo. Let, Mixtard 50 Novo. Let, Actrapid Novo. Let, Insulatard Novo. Let
Storage of Insulin • Refrigerate unopened insulin (will be good until the expiration date on the vial). • The vial of insulin is used within 30 days of opening, may be stored at room temperature (>2 degree Celsius and <30 degree Celsius); insulin ac activity decreases after 30 days at room temperature. • Unlike other medications insulin requires a special storage and transportation arrangement.
• Needs to be stored between 2 degree Celsius to 8 degree Celsius without dampness and direct exposure to sunlight. • In transportation it is to be dispatched with coolants and thermocol boxes.
• Neutral insulin should be a clear solution whereas premixed and intermediate insulin are suspensions. • Magnus Novo Nordisk offer complete range of insulin with C 4 (Complete care cool chain) guarantee.
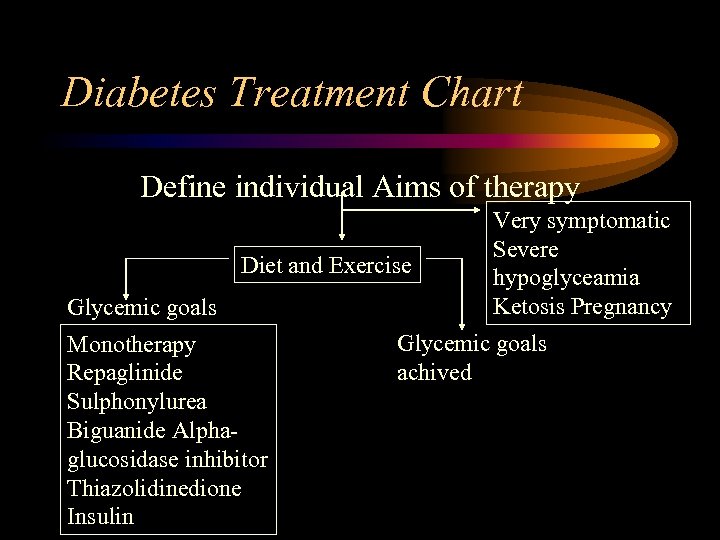
Diabetes Treatment Chart Define individual Aims of therapy Diet and Exercise Glycemic goals Monotherapy Repaglinide Sulphonylurea Biguanide Alphaglucosidase inhibitor Thiazolidinedione Insulin Very symptomatic Severe hypoglyceamia Ketosis Pregnancy Glycemic goals achived
Traditional Medicines Due to chronic nature of the disease, patients try various therapies available in the market, which are clinically not proven. The basis of the usage of these medicines is “no sideeffects” but then “efficacy” is always a question mark. Some of the traditional medicines used in the treatment are:
• Better substances like Neem leaves, Bittergourd, Methi etc. • Ayurvedic drugs viz. Vijasar, Bittergourd, Jamoon Seeds and Nisha Amlakki are used commonly. However their clinical results have not been either conclusive or not published. • Spirulina (fresh water algae) that grows in water tanks is used, but not significant effect seen on blood sugar.
Precautions • It is essential to provide the efficacy and safety of traditional medicines in wide variety of patents and to look for long term safety and efficacy in human beings. • Any system of medicine that claims that it has cure or relief for Diabetes has to under go the clinical safety tests before it is accepted.
• Scientific proof and clinical study should authenticate any such claims in magazines and newspapers.
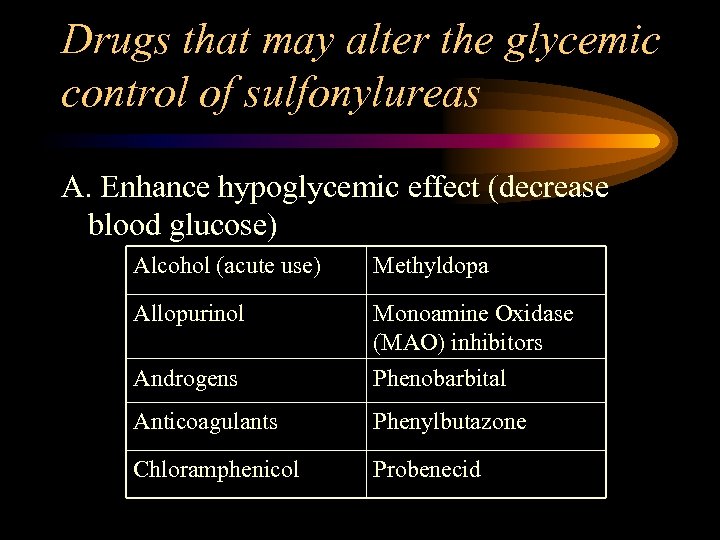
Drugs that may alter the glycemic control of sulfonylureas A. Enhance hypoglycemic effect (decrease blood glucose) Alcohol (acute use) Methyldopa Allopurinol Monoamine Oxidase (MAO) inhibitors Androgens Phenobarbital Anticoagulants Phenylbutazone Chloramphenicol Probenecid
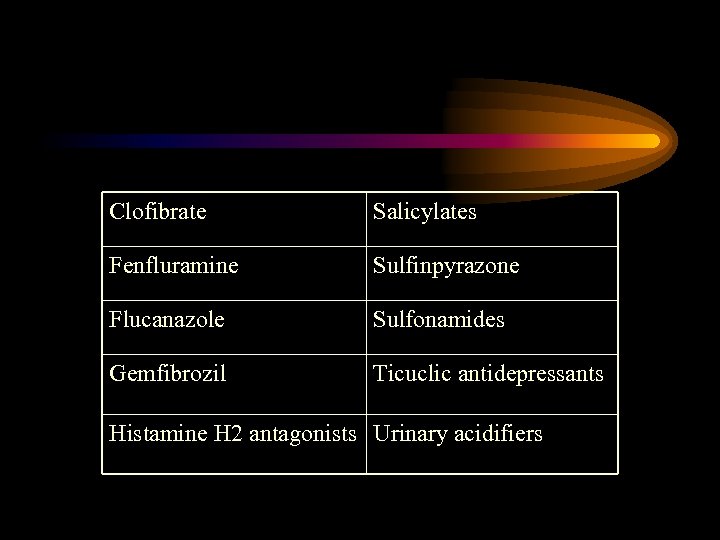
Clofibrate Salicylates Fenfluramine Sulfinpyrazone Flucanazole Sulfonamides Gemfibrozil Ticuclic antidepressants Histamine H 2 antagonists Urinary acidifiers
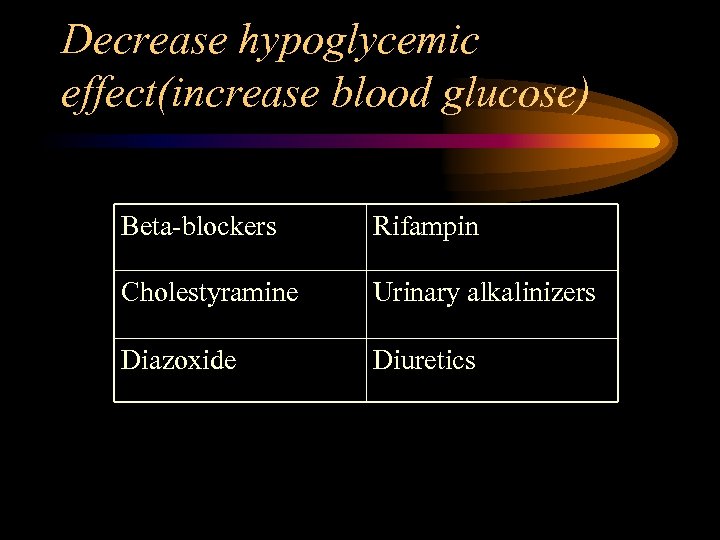
Decrease hypoglycemic effect(increase blood glucose) Beta-blockers Rifampin Cholestyramine Urinary alkalinizers Diazoxide Diuretics
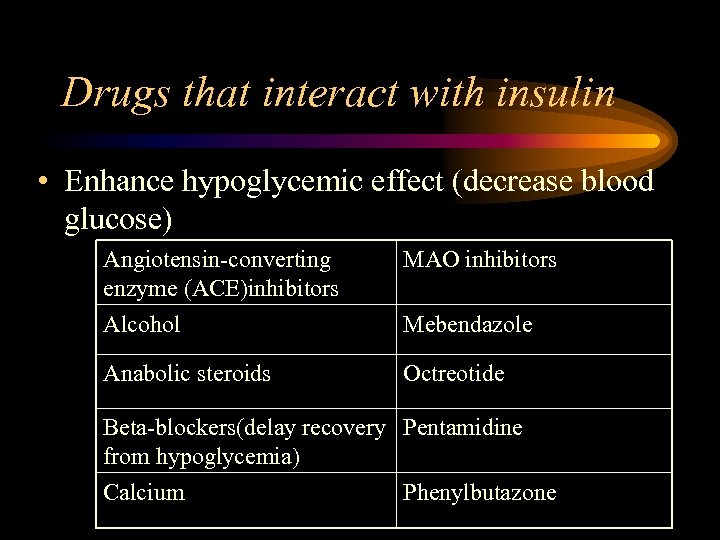
Drugs that interact with insulin • Enhance hypoglycemic effect (decrease blood glucose) Angiotensin-converting enzyme (ACE)inhibitors Alcohol MAO inhibitors Anabolic steroids Octreotide Mebendazole Beta-blockers(delay recovery Pentamidine from hypoglycemia) Calcium Phenylbutazone
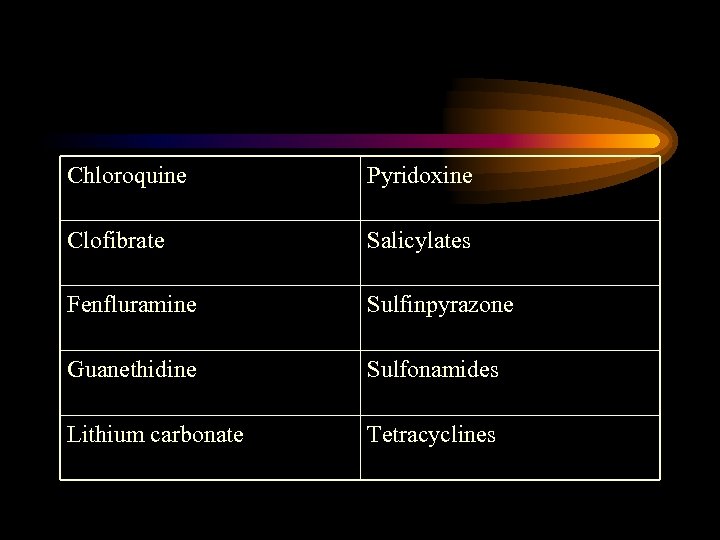
Chloroquine Pyridoxine Clofibrate Salicylates Fenfluramine Sulfinpyrazone Guanethidine Sulfonamides Lithium carbonate Tetracyclines
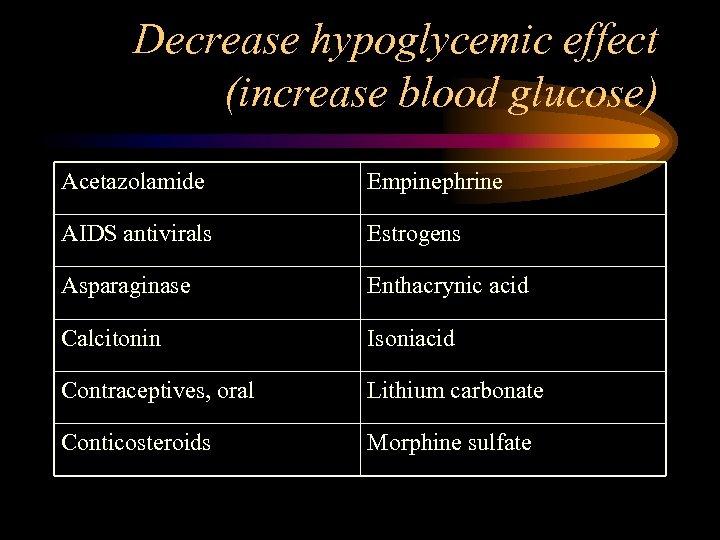
Decrease hypoglycemic effect (increase blood glucose) Acetazolamide Empinephrine AIDS antivirals Estrogens Asparaginase Enthacrynic acid Calcitonin Isoniacid Contraceptives, oral Lithium carbonate Conticosteroids Morphine sulfate
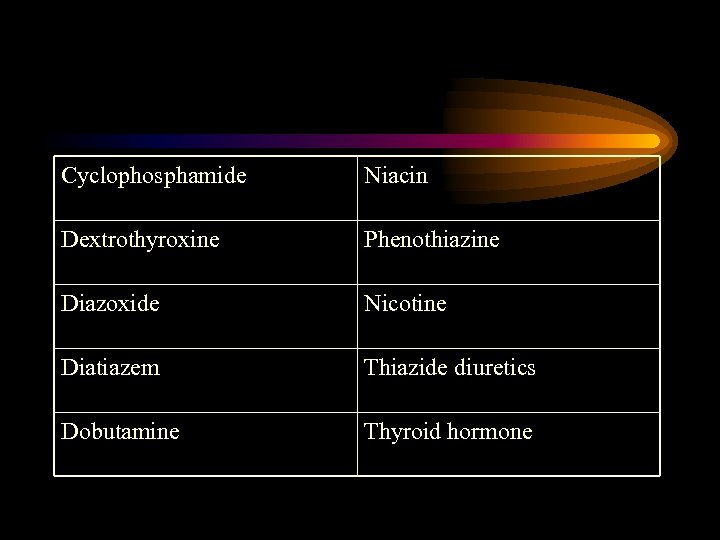
Cyclophosphamide Niacin Dextrothyroxine Phenothiazine Diazoxide Nicotine Diatiazem Thiazide diuretics Dobutamine Thyroid hormone
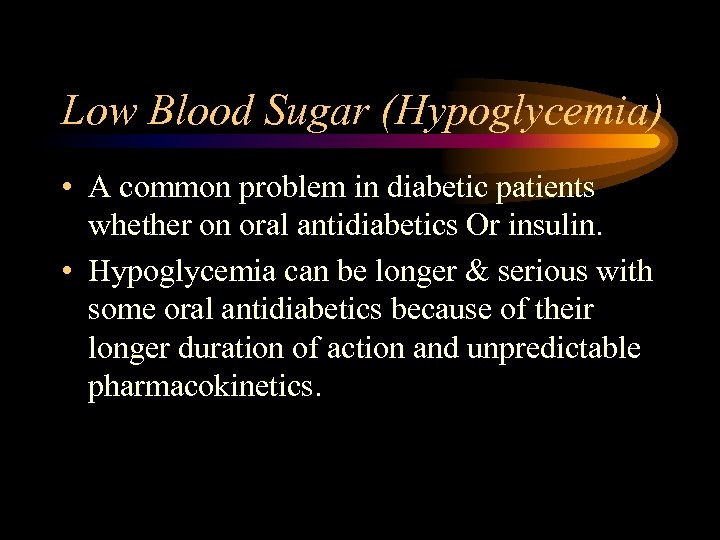
Low Blood Sugar (Hypoglycemia) • A common problem in diabetic patients whether on oral antidiabetics Or insulin. • Hypoglycemia can be longer & serious with some oral antidiabetics because of their longer duration of action and unpredictable pharmacokinetics.
Symptoms of Hypoglycemia: • • • Sweating Palpitations Shakiness Blurry vision Headache • Frequent hunger • Feeling of “passing out” • Decreased “concentrating ability” • Inappropriate behavior • Loss of conciousness
Treatment of Hypoglycemia: • Check blood glucose to exclude other reasons. • If glucose meter not readily available, then presume hypoglycemia and institute testament immediately. • Provide glucose tablets, fruit juices, candy, etc. • If the patient becomes unconscious, a Glucagon injection (Gluca. Gen Hypokit) Should be administered. • Recheck blood glucose after 30 minutes.
• Hypoglycemia can be recurrent on administration of long acting insulin or drugs such as Glyburide, Glipizide especially if patients also have kidney disease. • Patients are generally monitored in the hospital for 24 48 hours for any recurrent hypoglycemia.
Diabetic ketoacidosis Symptoms: • Anorexia, nausea, vomiting • Thirst, Polyuria • Weakness • Abdominal pain • Visual disturbance • Weight loss
Signs: • • Elevated blood glucose (>250 mg/dl) Ketonuria/Ketonemia Plasma bicarbonate <15 meq/L Dehydration Warm dry skin Tachycardia Rapid/deep breathing, acetone odour Somnolence, coma
Treatment: • Replacement of fluid loss to correct dehydration & hyperosmolarity • Replacement of electrolysis with potassium containing saline • Correction of hyperglycemia by insulin and fluid replacement • Ketosis and acidosis are simultaneously corrected by above measures • Identification and correction of precipitatory causes.
Complications: Long Term • Diabetes is the silent killer as it affects almost all the organs of the body and usually leads to a host of complications if not controlled aggressively.
Kidney Disease Symptoms: • Hypertension, edema, proteinuria and renal insufficiency
Diagnosis: • Urinary microalbumin excretion testing • Spot urine sample testing
Treatment: • Tight control of blood glucose in most diabetic patients. • Dietary protein restrictions. • Excessive urinary microalbumin excretion should be treated with an ACE-inhibitor agent (provided there are no contraindications) even if their blood pressure is not elevated. This helps to control intraglomerular hypertension. • High blood pressure should be aggressively treated in diabetic patients and target blood pressure should be less than 130/85 mg Hg.
Monitoring: • Urinary albumin excretion test on a yearly basis
Eye Disease • Symptoms: • Diminished visual activity; frequent change in power of lens, painful eye
Diagnosis: • Check visual acuity with Snellens chart, seperately for each eye • Dilate pupils • Examine fundi by ophthalmoscope • Microaneurysms, retinal hemorrhages, hard exudates from eye.
Treatment: • Aggressive control of blood glucose and blood pressure in most diabetic patients. • Laser photocoagulation surgery for diabetic macular edema or proliferative retinopathy. • Vitrectomy surgery for vitreous hemorrhage or severe progressive neovascularization.
Monitoring: • Yearly eye examination of the diabetic patient by an ophthalmologist
Foot Problem Symptoms: • Tingling, pins & needle sensation, burning sensation, numbness or pain.
Diagnosis: • Carefully inspect the feet (whole foot, nails) • Check peripheral pulses • Examine for neuropathy i. e touch and vibration

Treatment: • Best treatment is regular care of the feet. • Tight blood glucose control is crucial. • The mode of treatment depends upon – the degree of lesions, – neuropathic & vascular assessment – and X-ray. • Treatment can range from bed rest, antibiotics according to culture and sensitivity, plaster, special shoes to ampulation.
Mentoring: • A podiatrist should be visited for regular foot checking.
Erectile Dysfunction • Erectile dysfunction is the most common male sexual dysfunction in diabetes.
Treatment options for diabetic erectile dysfunction General measures • Improving diabetic control • Reduce alcohol intake • Withdraw causative drugs Nonhormonal therapy • Alpha-2 -adgrenergic blocking agents (yohimbine hydrochloride) • Type-specific phosphodiesterase inhibitors (sildenafil citrate)
Noninvasive Therapy: • Vacuum erection devices • Intracavernosal injection of vasoactive agents (mixture of papaverine, phentolamine, prostaglandin E 1) Invasive therapy: • Penile prosthesis (malleable versus inflatable device) • Microvascular arterial bypass surgery
Heart Disease • Symptoms: • Augina symptoms: chest, arm, and/or jaw pain (discomfort), Shortness of breath, cold clammy sweat • Myocardial infraction (ML)- “silent”ML more common.
Diagnosis: • Examine blood pressure • Electrocardiogram monitoring particularly ambulatory • ECG monitoring for silent ischemia • Stress testing for coronary heart disease • Echocardiography (with Doppler) • Testing of cholesterol
Treatment • Antiplatelet / anticoagulants: • Start Aspirin 80 to 325 mg/d if not contraindicated Manage warfarin to international normalised ratio 2 to 3. 5 for post ML-patients not able to take aspirin
ACE inhibitors in post-ML patients: • Start early post-ML in stable high risk patients (anterior ML, previous ML, Killip class II • Continue indefinitely for all with LV dysfunction • Use as needed to manage blood pressure or symptoms in all other patients
Beta-blockers: • Start in high risk post-ML patients (arrhythymia, LV dysfunction, inducible ischemia) at 5 to 28 days with continuation for six months minimum • Use as needed to manage angina, rhythym, or blood pressure in all other patients
Pregnancy and Diabetes Insulin treated diabetes Planned Pregnancy • Good glycemic control be obtained before conception. In some situations intensive stabilization pre-pregnancy may be necessary • Good glycemic control before and throughout pregnancy reduces the risk of complications for the mother and foetus.

• For pre-pregnancy stabilization use at least a twice daily mixtures of short and intermediate acting insulin. • Reinforce education on diet and insulin self adjustment.
Preconception goal for glycemic control • Premeal glucose 70 to 100 mg/100 ml (3. 8 to 5. 5 mmol/l) • 1 to 2 hour post meal glucose at or below 150 mg/100 ml(< 8. 3 mmol/ol) • Serial H BA 1 c levels to be maintained at the normal or near normal value.
Other Assesments • Asses for any diabetic complications (hypertension, ischemic heart disease, nephropathy, neuropathy, retinopathy and severe gastroenteropathy). • Obsteric assessment • Thyroid function test as per local practice
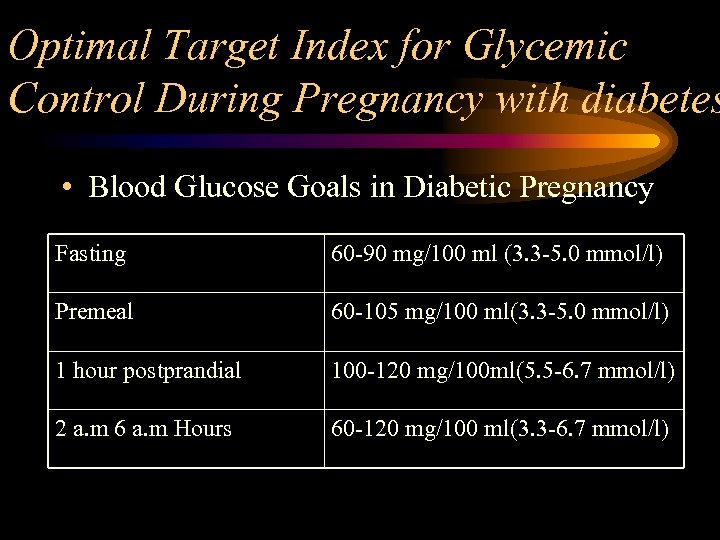
Optimal Target Index for Glycemic Control During Pregnancy with diabetes • Blood Glucose Goals in Diabetic Pregnancy Fasting 60 -90 mg/100 ml (3. 3 -5. 0 mmol/l) Premeal 60 -105 mg/100 ml(3. 3 -5. 0 mmol/l) 1 hour postprandial 100 -120 mg/100 ml(5. 5 -6. 7 mmol/l) 2 a. m 6 a. m Hours 60 -120 mg/100 ml(3. 3 -6. 7 mmol/l)
Oral hypoglycemic treated diabetes • Oral hypoglycemic drugs should be discontinued and human insulin therapy instituted. • Planning for pregnancy; preconceptions goals for glycemic control; other assessment; and Optimal Target Index for glycemic control during pregnancy with diabetes.
Gestational diabetes • Gestational diabetes mellitus develops in approximately 2 -5% of pregnant women. GDM are at increased risk for the development of Type 2 diabetes later in life and their infants are at risk for macrosomia.
Screening, diagnosis and treatement • All pregnant women should be screened for glucose intolerance between 24 th and 28 th week
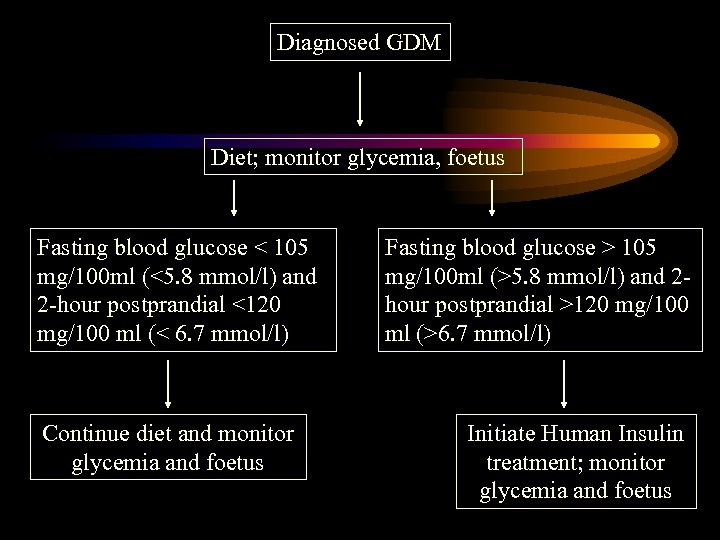
Diagnosed GDM Diet; monitor glycemia, foetus Fasting blood glucose < 105 mg/100 ml (<5. 8 mmol/l) and 2 -hour postprandial <120 mg/100 ml (< 6. 7 mmol/l) Continue diet and monitor glycemia and foetus Fasting blood glucose > 105 mg/100 ml (>5. 8 mmol/l) and 2 hour postprandial >120 mg/100 ml (>6. 7 mmol/l) Initiate Human Insulin treatment; monitor glycemia and foetus
• Diabetes is frequently associated with infections as seen in clinical practice, but not clearly proved. Defects in both cell mediated immunity and polymorphonuclear functions have seen experimentally shown, but their exact role in human beings is yet to be clearly shown.
• A decreased perfusion due to abnormality in microvascular circulation and neuropathy may worsen the prognosis as infection sets in. • The entire immune system is altered to defense against microbial invasion, certain defects may be more directly associated with certain infections in diabetes.
Skin infections • Due to compromised host defense and high blood sugars, microbes withy low virulence easily cause infections of the damaged skin. • Staphylococcus aurous infection causing boils, carbuncles and abscesses are the most common skin infections.
Diagnosis: • Confirmation is by biopsy of the affected area Treatment: • Board-spectrum antibiotics, antifungul agents
Tuberculosis • Tuberculosis is common with diabetes in India. Diagnosis: • Chest X-ray • Sputum and urine examination • Hematology

Symptoms: • • Weight loss Fever with chills Weakness Excessive urination
Treatment: • Antitubercular therapy of INH, Rifampicin, Ethambutol and Pyrazinamide. • Rifampicin and INH interact with OHAs and therefore choose insulin to initiate antidiabetic treatment.
Surgery • During surgery utmost care is required from the family physician in co-ordination with anesthetist to achieve proper glycemic control and avoid complications. The management differs as per the current treatment and status of diabetes. Broadly surgery management in diabetics is undertaken in following three phases:
Pre-operative Management • In patients managed on diet, assess for metabolic control with proper diet. If uncontrolled, admit patient 1 -2 days before operation and initiate Human Actrapid. • In patients managed on oral anti-diabetics, shift to shorter acting sulphonylurea. Biguanide should be stopped one week before and the patient should be shifted to insulin for stabilisation
• In patients on insulin, shift from intermediate acting insulin to short acting insulin (Human Actrapid) • Frequent monitoring is required. • If optimal control is not achieved with subcutaneous Human Actrapid, considered intervevous infusion.
Peri-operative (during surgery) Management • In patients only managed on diet institute insulin if hyperglycemia develops & persists post operatively. • In patients managed on oral medication, avoid breakfast and no medication on day of treatment. Treats as non diabetic if blood glucose is<126 mg/dl. • If blood glucose increase more than 126 mg/dl then initiate insulin (human Actrapid) • In major surgery set up Human Actrapid insulin infusion.
• In patients managed on insulin, set up i. V, infusion (10% Dextrose 500 ml + I. U. Human Actrapid+10 mmol KCL) and regimen adjust as per patient’s requirement. • Monitor patient frequently (1 -2 times every hour) during operation.
Post-operative (after surgery) Management • In diet treated diabetics, return to preoperative dietary management incase of minor surgery. In major surgery, treat with Human Actrpid (8 -12 units) t. d. s before each meal. Further titrate the dose as per the requirement.
• In patients managed on oral medication recommence sulphonylureas with first meal in case of minor surgery. In major surgery, treat with Human Actrapid (8 -12 units) t. d. s. before each meal. Further titrate the dose as per the requirement.
• In patients managed on insulin, continue the infusion at the same rate until oral feeding commences. If infusion is prolonged (24 hrs), check electrolytes daily (Na/K). • Initiate Human Actrapid (equivalent to preoperative dose) with oral feeding • After 2 -3 days, restabilise on suitable regimen for the patients. • Measure Ketone bodies and blood glucose frequently
• Being sick can make the blood glucose level go up very high. • It can also cause serious conditions that can put up the patient in a coma.
What Happens When the Patient is Sick • Patient when sick is under stress leading to release of hormones, which raises blood glucose levels, and interferes with the glucose-lowering effects of insulin. • Easy to lose control of the diabetes leading to ketoacidosis and diabetic coma particularly in people with Type 1 diabetes. • People with Type 2 diabetes, especially older people, can develop a similar condition called hyperosmolar hyperglycemic nonketotic coma.
Diabetes Medicines • Type 1 diabetes, it is advisable to take extra insulin to bring down the higher blood sugar levels. • Type 2 diabetes, may be able to take pills, or may need to use insulin for a short time.
Food • Eating and drinking can be a big problem. But it is important to stick to the normal meal plan. • Easy to run low on fluids when one is vomiting or has fever or diarrhea. Extra fluids will also helps get rid of the extra sugar (and possibly ketones) in the blood.
Medicines to Watch Out For • Advice to check the label of over- the-counter medicines before buying them to see if they have sugar. Small doses of medicines with sugar are usually okey. • Many medicines when taken for short-term illnesses can affect blood sugar levels, even if they don’t contain sugar. For example, aspirin In large doses can lower blood sugar levels
• Some antibiotics lower blood sugar levels in people with Type 2 diabetes who take diabetes pills. • Decongestant and some products for treating colds raise blood sugar levels. Monitoring Glucose level • Regular / frequent monitoring required
Travel • Before a long trip, medical examination is necessary to make sure diabetes is in good control.
Packing Tips Whether traveling by car, plane, boat, bike, or foot, the patient will want keep this “carry-on” bag with him at all times. Pack this bag with: • All the insulin and syringes needed for the trip blood and urine testing supplies (include extra batteries for the glucose meter) • All Oral medications (an extra supply is a good idea)
• Other medications or medical supplies, such as glucagon, antidiarrhea medication, antibiotic ointment, antiemetic drugs • ID and Diabetes identity card • A well-wrapped, air-tight snack pack of crackers or cheese, peanut butter, fruit, a juice box, and some form of sugar (hard candy or glucose tablets) to treat low blood glucose.
Insulin During Travel • Insulin stored in very hot or very cold temperature may lose strength. Don’t store insulin in the glove compartment or trunk of the car • Insulin used in India are of the strength 40 and 100 I. U. • In foreign countries, insulin may come as I. U. 40 or I. u. 80. If the patient needs to use these insulin, one must buy new syringes to match the new insulin to avoid mistake in the insulin dose.
Crossing Time Zones If one takes insulin shots and will be crossing the time zones, remember: • Eastward travel means a shorter day, less insulin may be needed. • Westward travel means a longer day, so more insulin may be needed. • To keep track of shots and meals through changing time zones, advice the patient to keep his watch on his home time zone until the morning after he arrives.
After Arrival • After a long flight, it is advisable to take it easy for a few days. Test the blood sugar often. • If one takes insulin, plan the activities so that one can adjust insulin dose and meals. • Ask for a list of ingredients for unfamiliar foods. Some foods may upset the stomach and hurt the diabetes control. • Always advice to wear comfortable shoes and never go barefoot. Check the feet every day.
1b2d5084baca71c3e28f302900b371eb.ppt