Glomerulonephropathy.pptx
- Количество слайдов: 62
Glomerulonephropathy Paul D. Bradford, PA-C Philadelphia University Physician Assistant Studies Program
Glomerular Disease Catagories? Nephritic Spectrum Nephrotic Spectrum
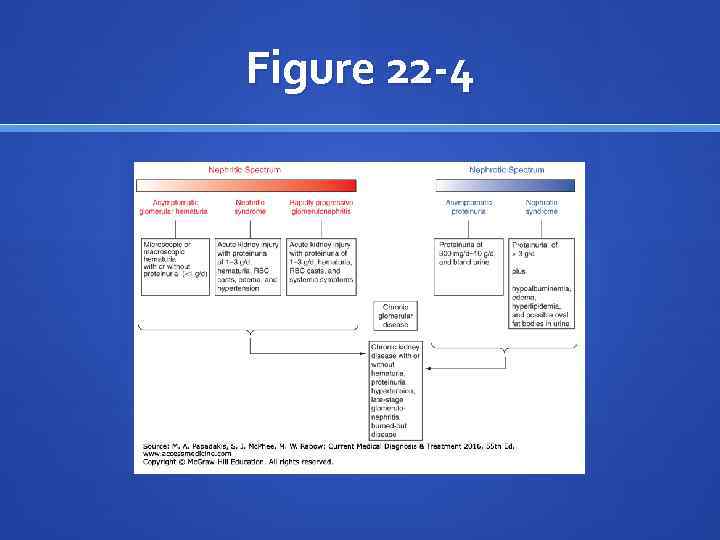
Figure 22 -4
Quick Info Nephritic Syndrome Components Edema (some) (first in areas of low tissue pressure) Hypertension (decrease in GFR leads to sodium retention) Hematuria Proteinuria
Nephrotic Syndrome: Quick Association N E P H R Pr. Oteinuria T I C
“Poor Man’s Renal Biopsy” Urinalysis helps us toward diagnosis.
Nephritic Syndrome: What’s in the cup? Protein WBCs RBCs (some dysmorphic) RBC Casts
Nephrotic Syndrome: What’s in the cup? Proteinuria Because there is a lot in the urine, where is there much less than normal? That’s called: hypoalbunimemia
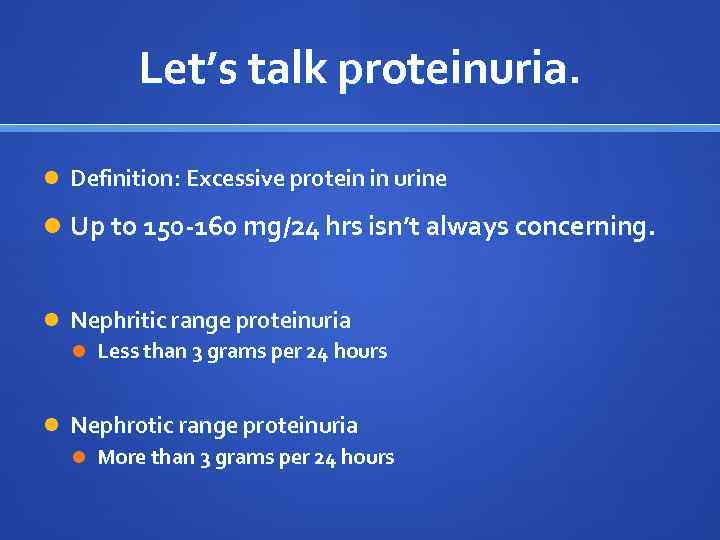
Let’s talk proteinuria. Definition: Excessive protein in urine Up to 150 -160 mg/24 hrs isn’t always concerning. Nephritic range proteinuria Less than 3 grams per 24 hours Nephrotic range proteinuria More than 3 grams per 24 hours
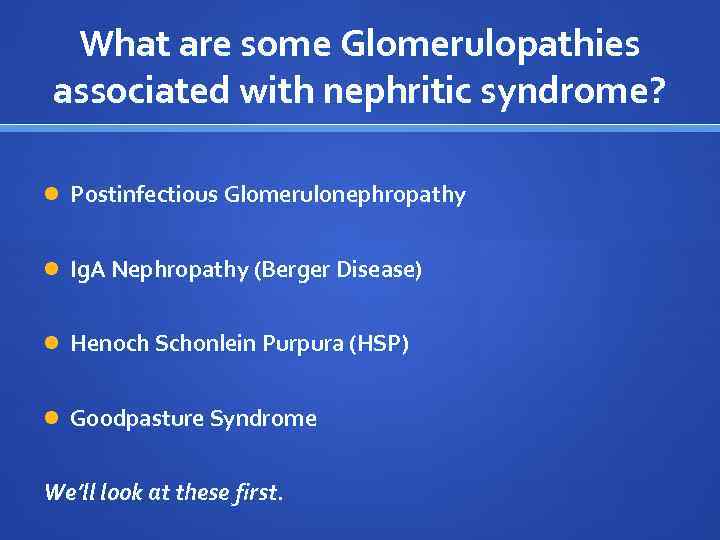
What are some Glomerulopathies associated with nephritic syndrome? Postinfectious Glomerulonephropathy Ig. A Nephropathy (Berger Disease) Henoch Schonlein Purpura (HSP) Goodpasture Syndrome We’ll look at these first.
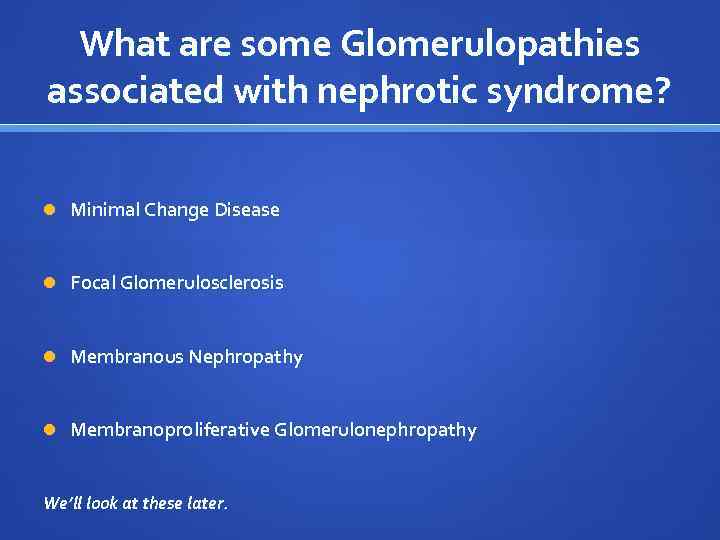
What are some Glomerulopathies associated with nephrotic syndrome? Minimal Change Disease Focal Glomerulosclerosis Membranous Nephropathy Membranoproliferative Glomerulonephropathy We’ll look at these later.
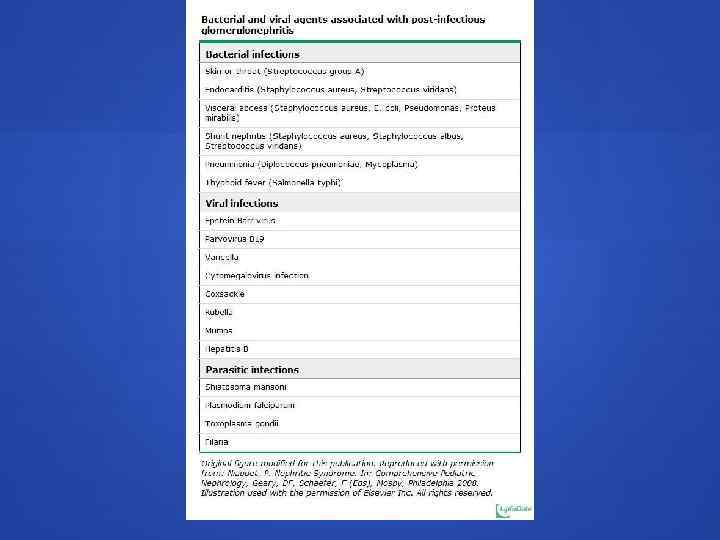
Postinfectious Glomerulonephritis Lots of organisms can cause this (see next slide), but the most common is… Group A beta-hemolytic streptococci (GABS)
Postinfectious Glomerulonephritis (Change in term) When Group A beta-hemolytic streptococci (GABS) is the postinfectious cause of glomerulonephritis, the term often used in PSGN. Can you guess what that stands for?
Postinfectious Glomerulonephritis Poststreptococcal glomerular nephritis (PSGN) Most common cause of acute nephritis worldwide. Primarily occurs in the developing world. Risk of PSGN is greatest in children between 5 and 12 years of age, and older adults greater than 60 years of age.
Postinfectious Glomerulonephritis PSGN Occurs during disease epidemics.
Postinfectious Glomerulonephritis PSGN Clinical Picture Edema (possibly gross) hematuria HTN Usually presents 1 -3 weeks after infection
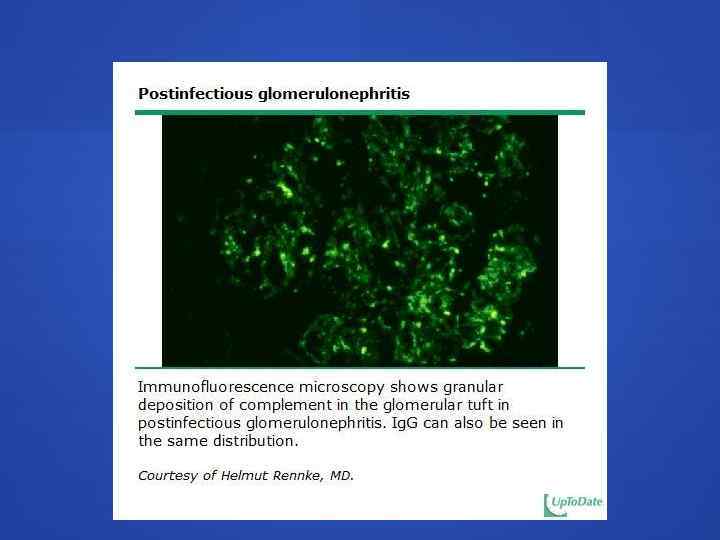
Postinfectious Glomerulonephritis characteristic pathologic features of PSGN demonstrated by electron microscopy: dome-shaped subepithelial deposits (“humps”)
Postinfectious Glomerulonephritis PSGN Treatment: Supportive Care Perhaps including: antihypertensives, salt restriction, diuretics Prognosis is good for children
Ig. A Nephropathy (Berger Disease) Most common cause of primary glomerulonephritis. More common among Asians and Caucasians. 2 or 3 – to - 1 male to female predominance. Peak incidence: second and third decades of life
Ig. A Nephropathy (Berger Disease) deposits of Ig. A in the glomerular mesangium. Inciting cause is unknown. Associated with: hepatic cirrhosis, celiac disease, HIV, cytomegalovirus, and other infections.
Ig. A Nephropathy (Berger Disease) Most common presenting complaint: an episode of gross hematuria. Frequently associated with concurrent URI (50%). “synpharyngitic hematuria” Onset often noted 1 -2 days after onset of concurrent illness This differentiates the clinical picture from PSGN.
Ig. A Nephropathy (Berger Disease) Labs Serum Ig. A elevated in 50%, so normal Ig. A does not rule out disease UA: hematuria, proteinuria Proteinuria range varies and prognostic >1 g/24 hrs = worse prognosis Diagnosis Renal biopsy
Ig. A Nephropathy (Berger Disease) Treatment ACE Inhibitors ARBs Corticosteroids Fish Oil? Prognosis: Approximately 50% will progress to chronic kidney disease
Henoch-Schonlein Purpura Most common systemic vasculitis of childhood. Self-limiting. Characterized by a tetrad of clinical manifestations that vary in their occurrence and order of presentation. “Classic Triad” Palpable purpura Arthralgia and/or arthritis Abdominal pain +/- Renal disease
Henoch-Schonlein Purpura Occurs primarily between the ages of 3 and 15 years. The annual incidence is 10 to 20 per 100, 000 in children <17 years of age Peak incidence: 4 to 6 y/o. Male > Female 10 % of HSP cases occur in adults.

Henoch-Schonlein Purpura Diagnosis of HSP is usually based upon clinical manifestations of the disease. In unusual presentation, biopsy of the affected organ (skin or kidney) demonstrating predominantly Ig. A deposition supports the diagnosis of HSP.
Henoch-Schonlein Purpura Labs UA: RBC, WBC, casts, and proteinuria. Serum Ig. A elevated in 50% - 70% of patients with HSP.
Henoch-Schonlein Purpura Labs UA: RBC, WBC, casts, and proteinuria. Serum Ig. A elevated in 50% - 70% of patients with HSP.
Henoch-Schonlein Purpura Treatment is supportive with good prognosis, as this is generally self-limiting.
Case Example A 45 -year-old man was admitted to the intensive care unit with respiratory failure secondary to massive hemoptysis and acute renal failure. Antiglomerular basement membrane antibodies were strongly positive. Autopsy showed consolidated lung from extensive bleeding, which led to asphyxiation.
Goodpasture Syndrome (Anti-GBM Disease) Glomerulonephritis And Pulmonary Hemorrhage
Goodpasture Syndrome What is responsible? Anti-GBM antibodies However, up to one third of patients with anti-GBM nephritis have no evidence of lung injury
Goodpasture Syndrome Genetics play an important role. Patients with specific human leukocyte antigen (HLA) types are more susceptible to disease and may have a worse prognosis HLA-DR 2 and –B 7 Males 6 x more than Females. Wide range of affected ages, but most commonly 2 nd and 3 rd decades.
Goodpasture Syndrome Presentation Preceded by URI in 20 -60% of cases 60 -80% of patients present with pulmonary and renal disease 20 -40% have renal disease alone 10% or less have disease that is limited to the lungs.
Goodpasture Syndrome Physical Exam Tachypnea Inspiratory crackles over lung bases Cyanosis Hypertension (present in 20% of cases) Rash Edema
Goodpasture Syndrome Studies ID anemia (secondary to hemorrhage) and/or leukocytosis Increased BUN and creatinine UA: low-grade proteinuria, gross or microscopic hematuria, and red blood cell casts Circulating anti-GBM antibodies confirms diagnosis If diagnosis is unclear kidney biopsy is an option
Goodpasture Syndrome Treatment Plasma exchange (to remove circulating antibodies) Immunosuppressive drugs Corticosteroids Anti-GB< titers should decrease as the clinical course improves.
Goodpasture Syndrome Prognosis varies and is closely associated with condition at diagnosis. 5 -year survival rate exceeds 80% fewer than 30% of patients require long-term dialysis. Patients presenting with serum creatinine levels greater than 4 mg/d. L, oliguria, and more than 50% crescents on renal biopsy rarely recover.
Nephrotic Syndrome
Quick Info Nephrotic Syndrome Components Proteinuria Hypoalbuminemia Hyperlipidemia Edema
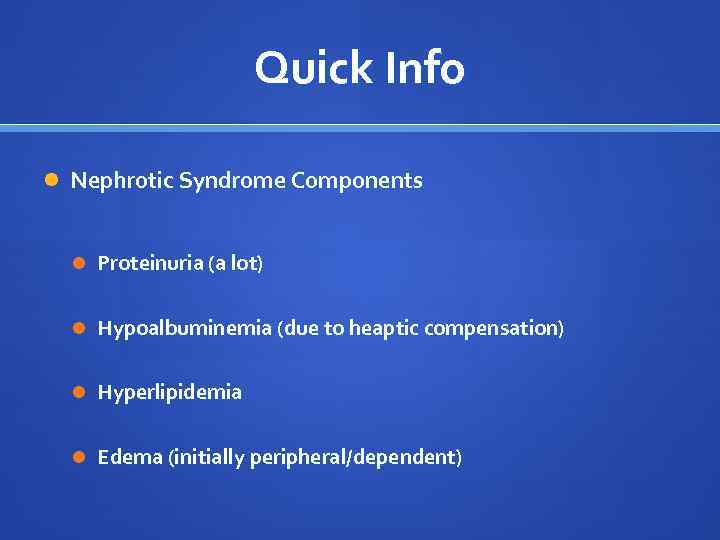
Quick Info Nephrotic Syndrome Components Proteinuria (a lot) Hypoalbuminemia (due to heaptic compensation) Hyperlipidemia Edema (initially peripheral/dependent)
Nephrotic Syndrome N E P H R Pr. Oteinuria T I C
Nephrotic Syndrome Principles of treatment - Consider increasing (to avoid negative nitrogen balance) or restricting dietary protein, dependent upon on proteinuria and/or GFR. - Salt restriction is essential. - ACE-I and/or ARBs – reduction of efferent arteriolar resistance. - Control coexisting hyperlipidemia
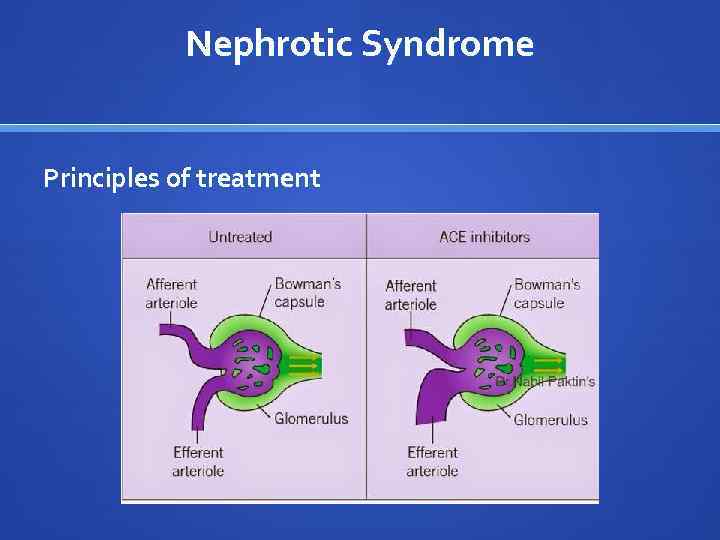
Nephrotic Syndrome Principles of treatment
Nephrotic Syndrome Be aware that hypoalbuminemia can lead to hypercoaguable state. Anticoagulation is considered in patients with evidence of thrombosis to prevent DVT/PE.
Minimal Change Disease Most commonly affects children, but can also affect adults with primary nephrotic syndrome. In children: M > F 24 -36 months of age = peak incidence
Minimal Change Disease Can be idiopathic Can occur following URI Can be associated with Hodgkin’s Lymphoma, heavy metal exposure (gold/lithium), hypersensitivity response.
Minimal Change Disease Clinical findings consistent with nephrotic syndrome. Proteinuria Hypoalbuminemia Hyperlipidemia Edema
Minimal Change Disease Histology “Minimal change” on light microscopy Characteristic foot process effacement on electron microscopy.

Minimal Change Disease Treatment Corticosteroids Kids need shorter course/dose than adults.
Membranous Nephropathy (MN) Common cause of nephrotic syndrome in nondiabetic adults. accounting for up to one-third of biopsy diagnoses. Often idiopathic, but can be associated with: hepatitis B, autoimmune diseases, malignancy, certain drugs such as gold, penicilins, captopril, and NSAIDs
Membranous Nephropathy (MN) Who? Most common in white males over 40 and rarely seen before age 30.
Membranous Nephropathy (MN) Clinical findings consistent with nephrotic syndrome. Proteinuria Hypoalbuminemia Hyperlipidemia Edema
Membranous Nephropathy (MN) Associations with: Occult cancer of lung, stomach, and colon in patients over 50 -60 y/o Higher incidence of renal vein thrombosis than other patients with nephrotic syndrome
Membranous Nephropathy (MN) Characteristic Labs - “spike and dome” pattern on kidney biopsy - Represents subepithelial deposits. - Ig. G and C 3 deposits along capillary loops.
Membranous Nephropathy (MN) Treatment – some controversy; review general principles of nephrotic syndrome treatment. Prognosis: 20 -50% of patients progress to ESRD in 3 -10 years


Resources https: //www. youtube. com/watch? v=1 nu. SSs. An. RVM
Glomerulonephropathy.pptx