96725351c7fa96ca80cb18eb0092d83a.ppt
- Количество слайдов: 32
GLAUCOMA RN Elisa Urruchi ORBIS International 1 | ORBIS International
GLAUCOMA What is it? A disease of progressive optic neuropathy involving: Structural changes in the optic nerve head Visual field loss Resulting in blindness if left untreated. 2 | ORBIS International
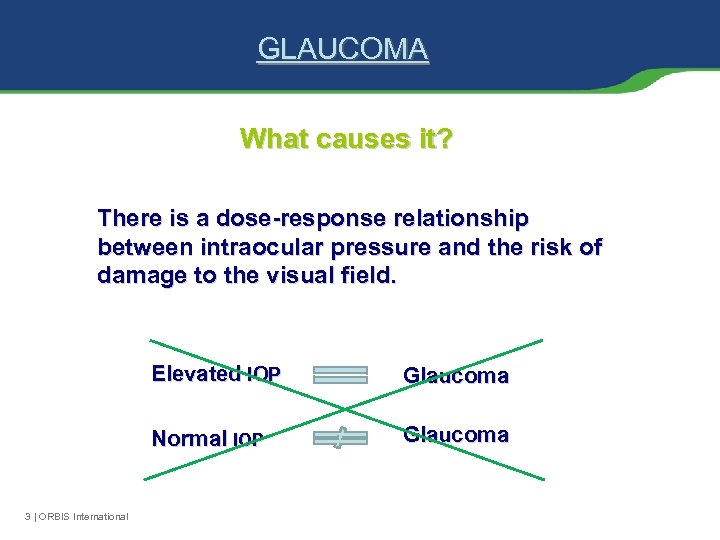
GLAUCOMA What causes it? There is a dose-response relationship between intraocular pressure and the risk of damage to the visual field. Elevated IOP Normal IOP 3 | ORBIS International Glaucoma
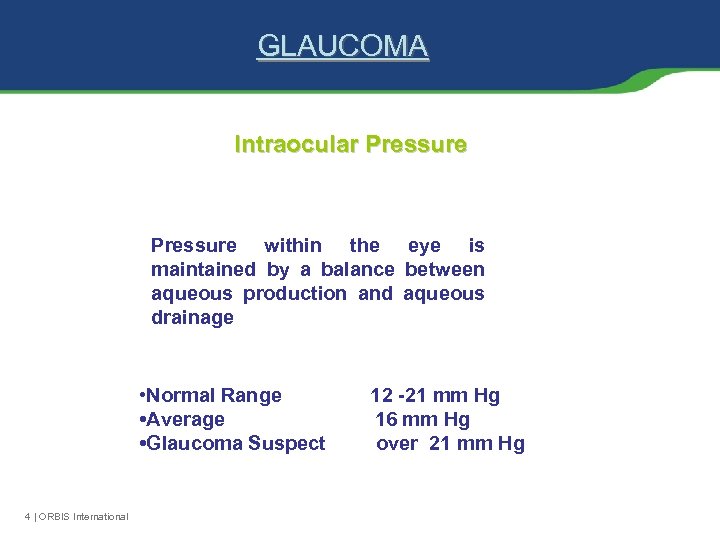
GLAUCOMA Intraocular Pressure within the eye is maintained by a balance between aqueous production and aqueous drainage • Normal Range • Average • Glaucoma Suspect 4 | ORBIS International 12 -21 mm Hg 16 mm Hg over 21 mm Hg
DIAGNOSING GLAUCOMA How do we measure IOP? • Goldman applanation tonometry • Tono - pen • Schiotz tonometer • No contact tonometer 5 | ORBIS International
DIAGNOSING GLAUCOMA Incorrect IOP reading can be caused by: ØCornea being thicker or thinner than normal ØA history of eye surgery, such as LASIK 6 | ORBIS International
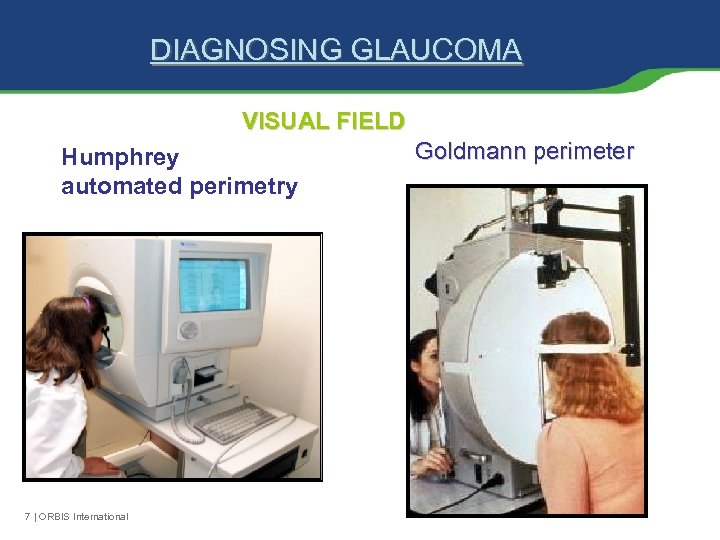
DIAGNOSING GLAUCOMA VISUAL FIELD Humphrey automated perimetry 7 | ORBIS International Goldmann perimeter
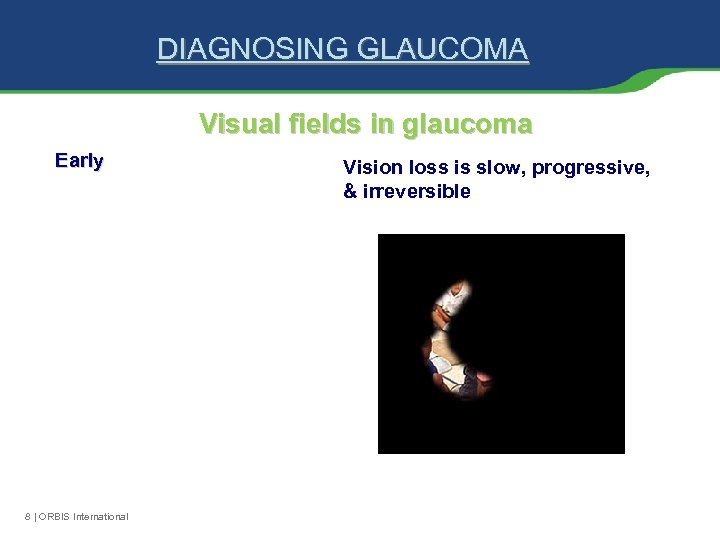
DIAGNOSING GLAUCOMA Visual fields in glaucoma Early 8 | ORBIS International Vision loss is slow, progressive, & irreversible
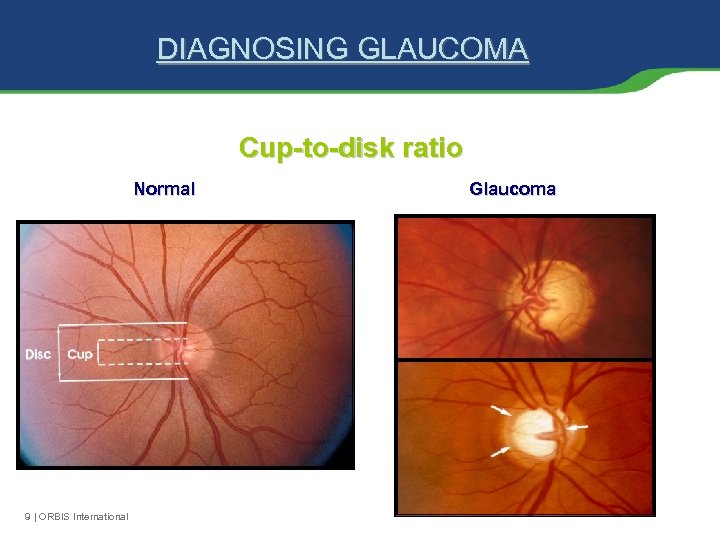
DIAGNOSING GLAUCOMA Cup-to-disk ratio Normal 9 | ORBIS International Glaucoma
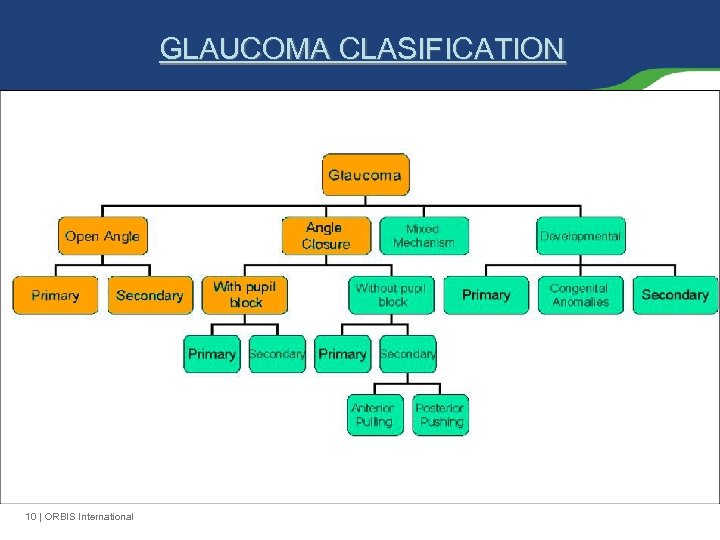
GLAUCOMA CLASIFICATION 10 | ORBIS International
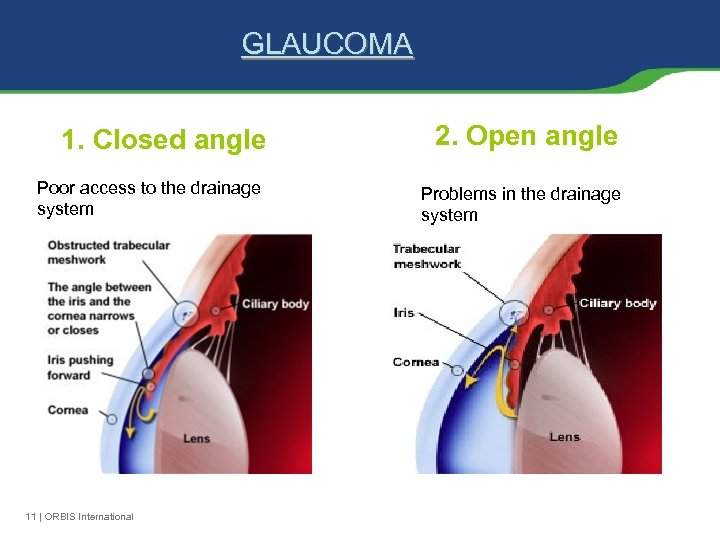
GLAUCOMA 1. Closed angle Poor access to the drainage system 11 | ORBIS International 2. Open angle Problems in the drainage system
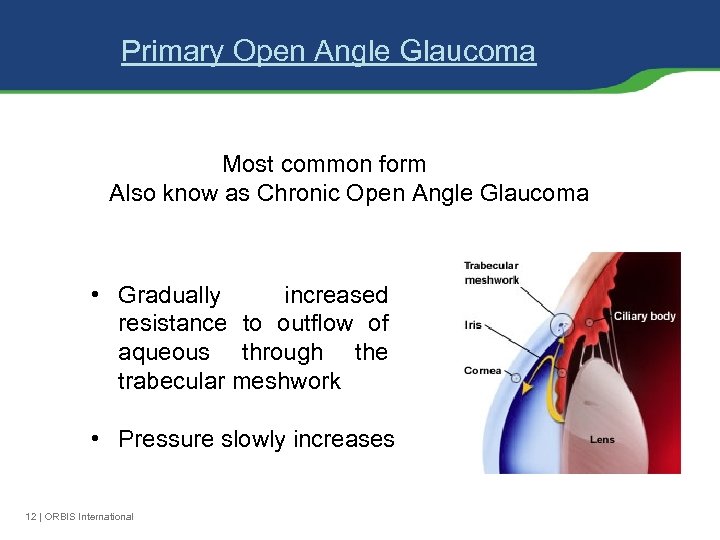
Primary Open Angle Glaucoma Most common form Also know as Chronic Open Angle Glaucoma • Gradually increased resistance to outflow of aqueous through the trabecular meshwork • Pressure slowly increases 12 | ORBIS International
Primary Open Angle Glaucoma Risk factors v. Elevated IOP v. Increases with age v. Positive family history v. African American background 13 | ORBIS International
Primary Open Angle Glaucoma Onset: 50+ years of age Symptoms • • Usually none May have loss of central and peripheral vision 14 | ORBIS International Signs • • • Elevated IOP Visual field loss Glaucomatous disk changes
TREATMENT Goal To preserve vision by reducing IOP to a level thought to be safe for the optic nerve. Ø Medical Ø Laser Ø Surgical 15 | ORBIS International
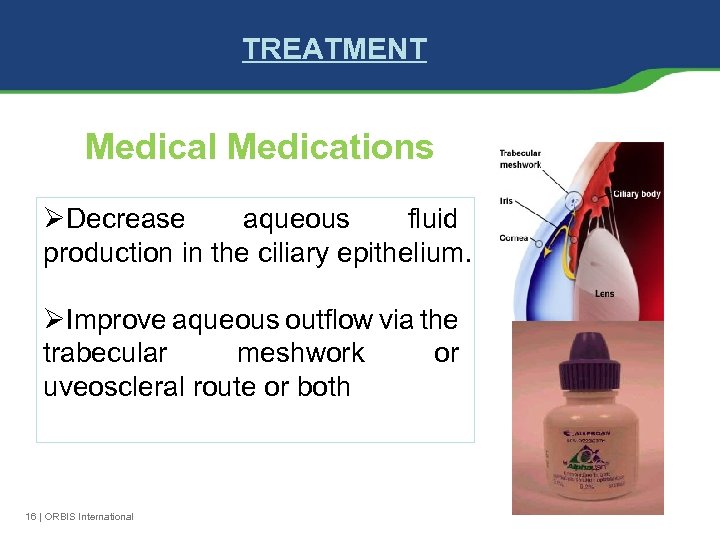
TREATMENT Medical Medications ØDecrease aqueous fluid production in the ciliary epithelium. ØImprove aqueous outflow via the trabecular meshwork or uveoscleral route or both 16 | ORBIS International
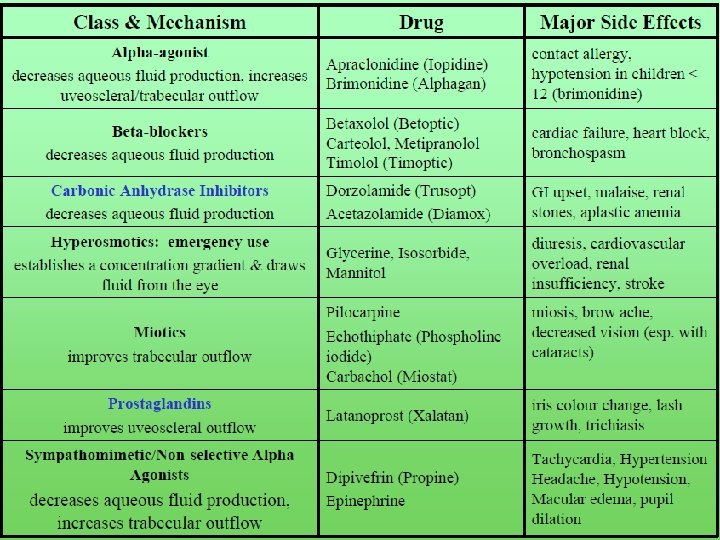
17 | ORBIS International
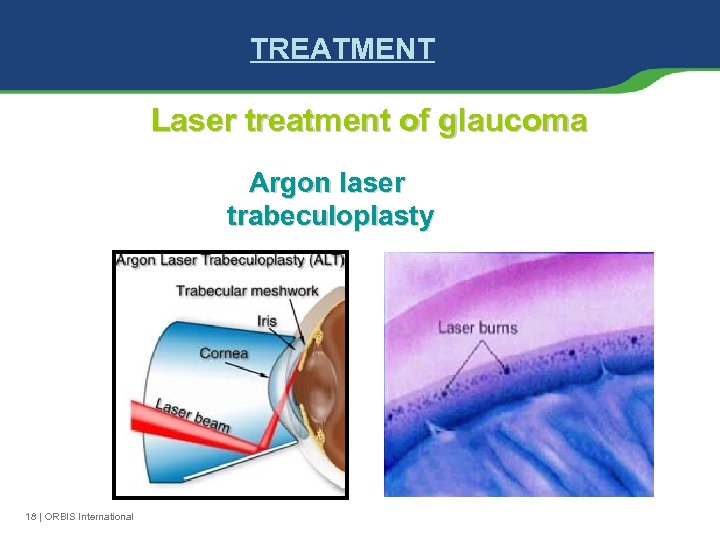
TREATMENT Laser treatment of glaucoma Argon laser trabeculoplasty 18 | ORBIS International
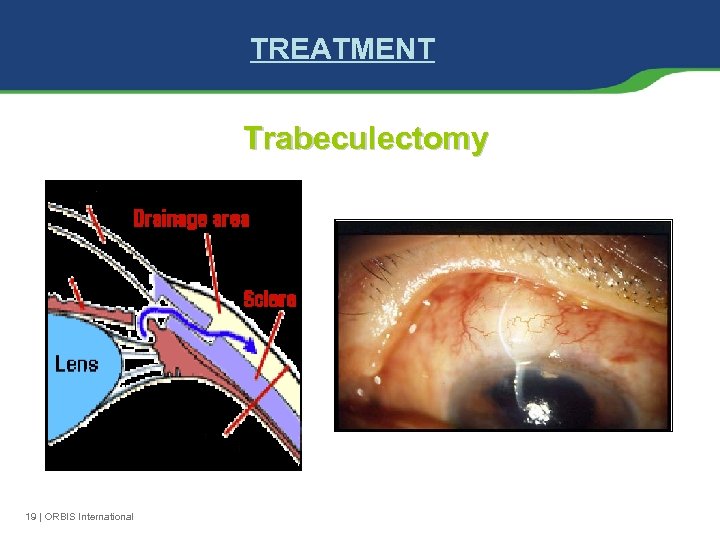
TREATMENT Trabeculectomy 19 | ORBIS International
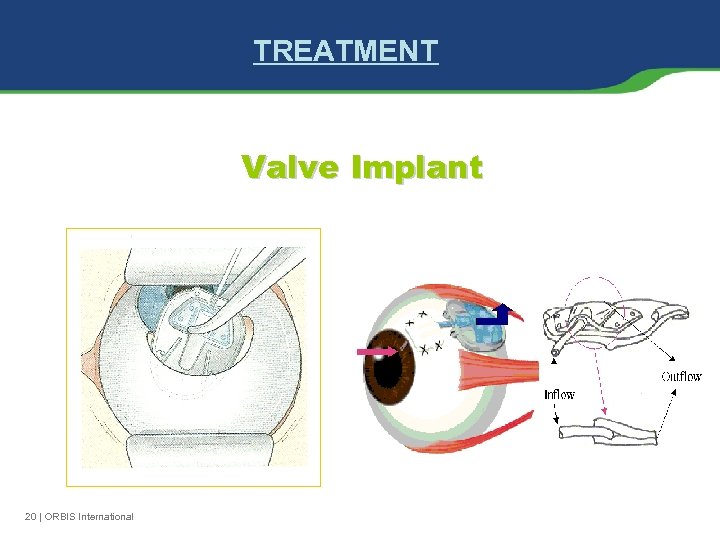
TREATMENT Valve Implant 20 | ORBIS International
Postoperative Care Ø Glaucoma medications are usually discontinued to improve aqueous humor flow to the bleb. Ø Topical medications consist typically of antibiotic drops 4 times per day and anti-inflammatory therapy e. g. with prednisolone drops every 2 hours. Ø A shield is applied to cover the eye until anesthesia has worn off (that also anesthetizes the optic nerve) and vision resumes. Ø Patients are instructed to call immediately for pain that cannot be controlled with over the counter pain medication or if vision decreases Ø do not rub the eye and to wear the shield at night for several days after surgery. 21 | ORBIS International
TREATMENT Laser Cyclophotocoagulation • Reduces aqueous production by destruction of the ciliary body • Used in severe glaucoma when conventional treatment fails to control IOP 22 | ORBIS International
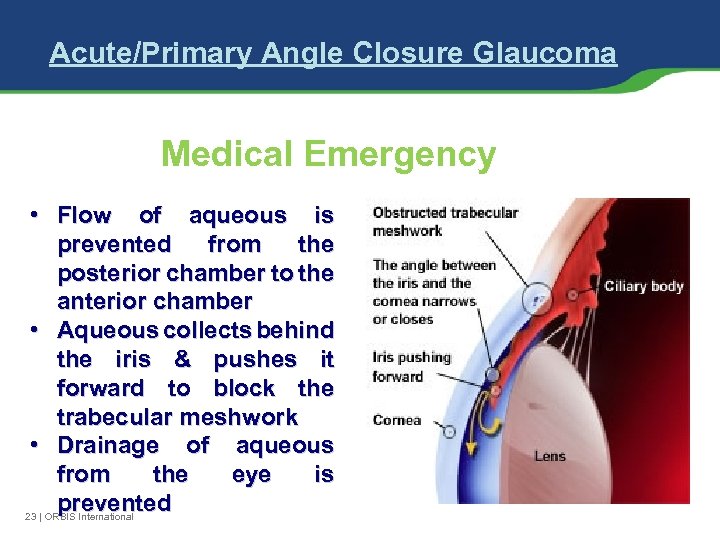
Acute/Primary Angle Closure Glaucoma Medical Emergency • Flow of aqueous is prevented from the posterior chamber to the anterior chamber • Aqueous collects behind the iris & pushes it forward to block the trabecular meshwork • Drainage of aqueous from the eye is prevented 23 | ORBIS International
Acute/Primary Angle Closure Glaucoma Risk factors v. Hyperopia v. Elderly v. Woman v. Family history v. African American background 24 | ORBIS International
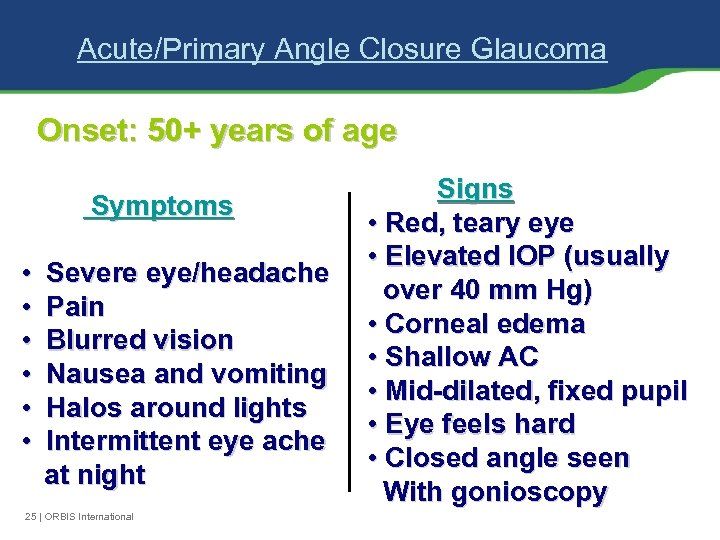
Acute/Primary Angle Closure Glaucoma Onset: 50+ years of age Symptoms • • • Severe eye/headache Pain Blurred vision Nausea and vomiting Halos around lights Intermittent eye ache at night 25 | ORBIS International Signs • Red, teary eye • Elevated IOP (usually over 40 mm Hg) • Corneal edema • Shallow AC • Mid-dilated, fixed pupil • Eye feels hard • Closed angle seen With gonioscopy
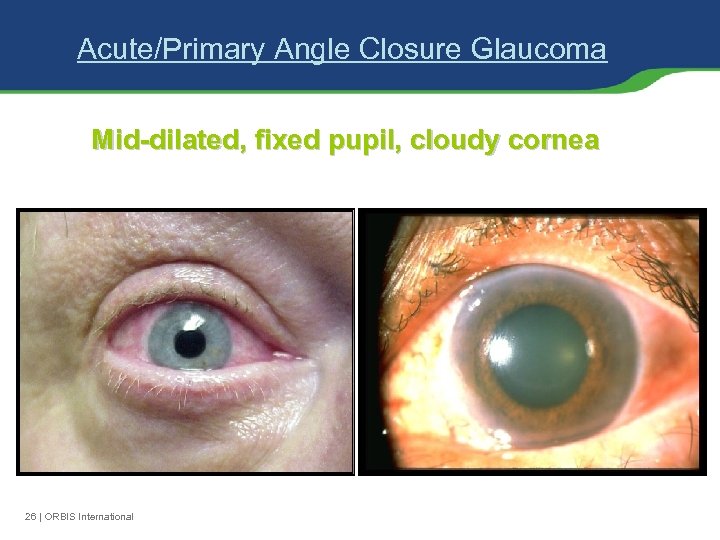
Acute/Primary Angle Closure Glaucoma Mid-dilated, fixed pupil, cloudy cornea 26 | ORBIS International
Acute/Primary Angle Closure Glaucoma Treatment v. Aqueous suppressants (timoptic, betagan, trusopt) v. Miotic (pilocarpine alone may be sufficient in mild attacks) v. Intravenous or oral carbonic anhydrase inhibitors v. Intravenous or oral hyperosmotic agents 27 | ORBIS International
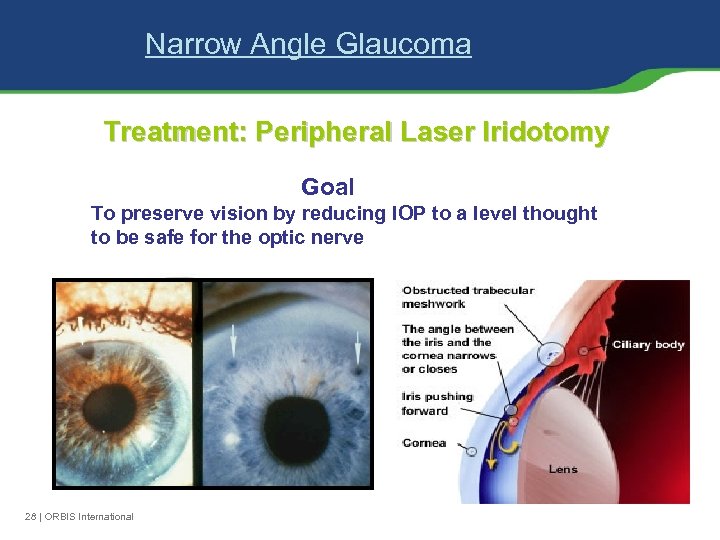
Narrow Angle Glaucoma Treatment: Peripheral Laser Iridotomy Goal To preserve vision by reducing IOP to a level thought to be safe for the optic nerve 28 | ORBIS International
Key Points ØOnce peripheral or central vision is lost from glaucoma, it can never be restored by any form of treatment. ØEarly detection of glaucoma is critical. Progression of the disease & permanent blindness can be prevented by appropriate treatment. ØGlaucoma is an increasingly important public health concern due to our aging population demographics 29 | ORBIS International
Glaucoma Quiz Ø Glaucoma is more common in Blacks than in Whites Ø Glaucoma tends to run in families Ø A person can have glaucoma and not know It Ø People over age 60 are more likely to get glaucoma Ø Eye pain is often a symptom of glaucoma Ø Glaucoma can be controlled Ø Glaucoma is caused by increased eye pressure Ø Vision lost from glaucoma can be restored Ø A complete glaucoma exam consists only of measuring eye pressure 30 | ORBIS International
THANK YOU ALL FOR LISTENING! 31 | ORBIS International

32 | ORBIS International
96725351c7fa96ca80cb18eb0092d83a.ppt