716b8331910d4fcd0615180ccd31f251.ppt
- Количество слайдов: 83
Glaucoma is not a single disease but consist of a large group of disorders wherein the intraocular pressure is too high for the structure and normal functioning of the optic nerve head. In healthy human eyes the normal pressure varies between 10 -20 mm Hg. Values of 21 mm of Hg or higher (applanation) or 22. 4 mm of Hg (indentation) should be regarded with suspicion. It must be recalled that aqueous humour which is secreted by the ciliary processes first inters the posterior chamber.
Glaucoma It then passes forward through the pupil to the AC where it leaves the eye by way of the trabecular meshwork in the angle of AC, canal of Schlemm , aqueous veins and mixes with the blood in the episcleral vessels.
Glaucoma occurs 1)Commonly when there is resistant to the flow of aqueous at any level during its pathway. 2)Rarely when more of aqueous is produced.
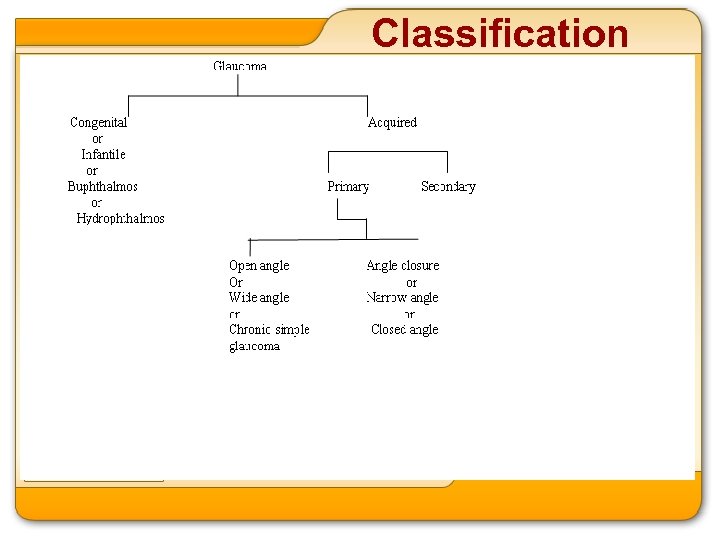
Classification
NB : Absolute glaucoma : it is the end stage of all neglected glaucomas and is characterized by 1)Absence of perception of light 2)High intraocular pressure
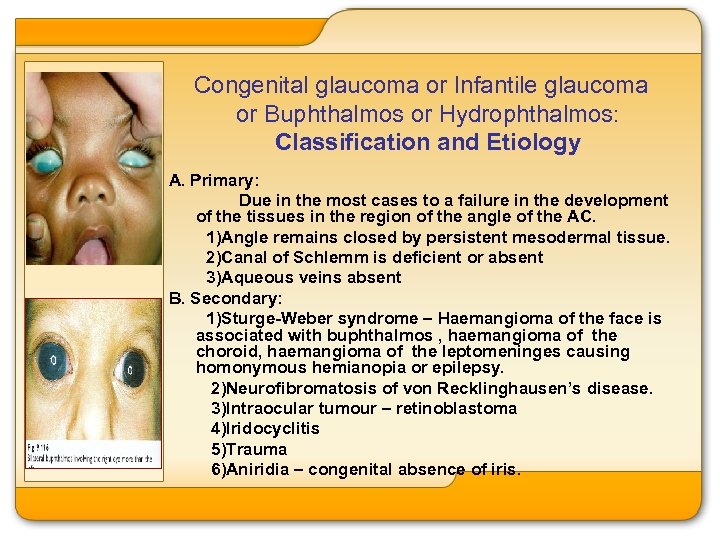
Congenital glaucoma or Infantile glaucoma or Buphthalmos or Hydrophthalmos: Classification and Etiology A. Primary: Due in the most cases to a failure in the development of the tissues in the region of the angle of the AC. 1)Angle remains closed by persistent mesodermal tissue. 2)Canal of Schlemm is deficient or absent 3)Aqueous veins absent B. Secondary: 1)Sturge-Weber syndrome – Haemangioma of the face is associated with buphthalmos , haemangioma of the choroid, haemangioma of the leptomeninges causing homonymous hemianopia or epilepsy. 2)Neurofibromatosis of von Recklinghausen’s disease. 3)Intraocular tumour – retinoblastoma 4)Iridocyclitis 5)Trauma 6)Aniridia – congenital absence of iris.
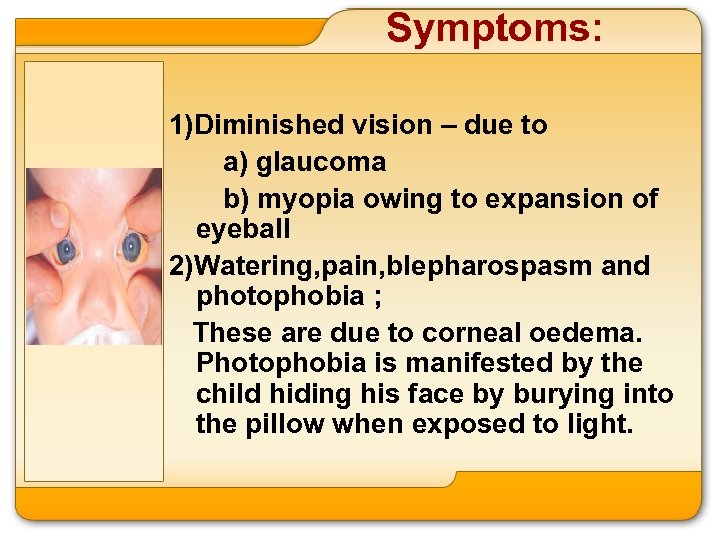
Symptoms: 1)Diminished vision – due to a) glaucoma b) myopia owing to expansion of eyeball 2)Watering, pain, blepharospasm and photophobia ; These are due to corneal oedema. Photophobia is manifested by the child hiding his face by burying into the pillow when exposed to light.
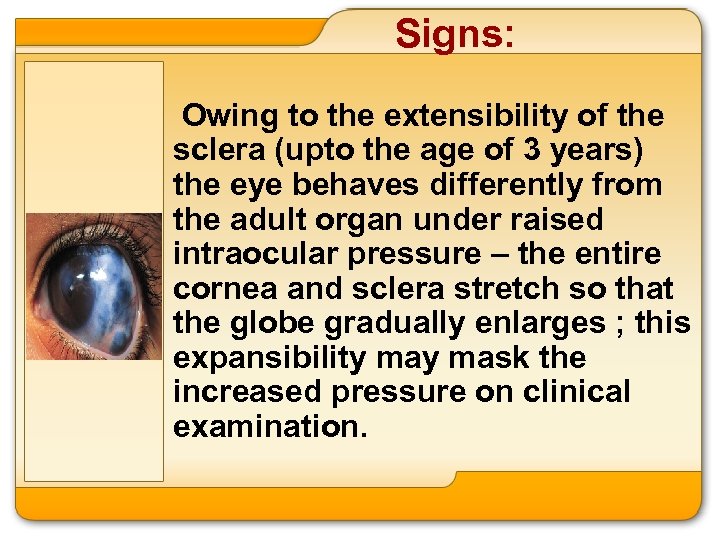
Signs: Owing to the extensibility of the sclera (upto the age of 3 years) the eye behaves differently from the adult organ under raised intraocular pressure – the entire cornea and sclera stretch so that the globe gradually enlarges ; this expansibility mask the increased pressure on clinical examination.
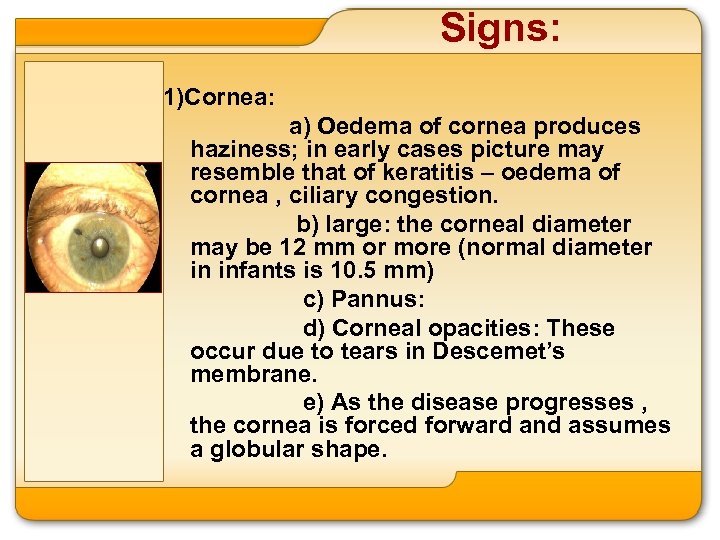
Signs: 1)Cornea: a) Oedema of cornea produces haziness; in early cases picture may resemble that of keratitis – oedema of cornea , ciliary congestion. b) large: the corneal diameter may be 12 mm or more (normal diameter in infants is 10. 5 mm) c) Pannus: d) Corneal opacities: These occur due to tears in Descemet’s membrane. e) As the disease progresses , the cornea is forced forward and assumes a globular shape.
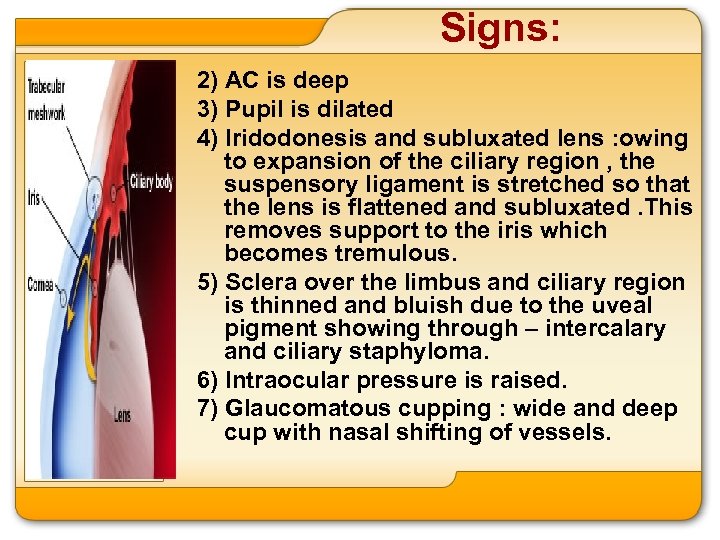
Signs: 2) AC is deep 3) Pupil is dilated 4) Iridodonesis and subluxated lens : owing to expansion of the ciliary region , the suspensory ligament is stretched so that the lens is flattened and subluxated. This removes support to the iris which becomes tremulous. 5) Sclera over the limbus and ciliary region is thinned and bluish due to the uveal pigment showing through – intercalary and ciliary staphyloma. 6) Intraocular pressure is raised. 7) Glaucomatous cupping : wide and deep cup with nasal shifting of vessels.
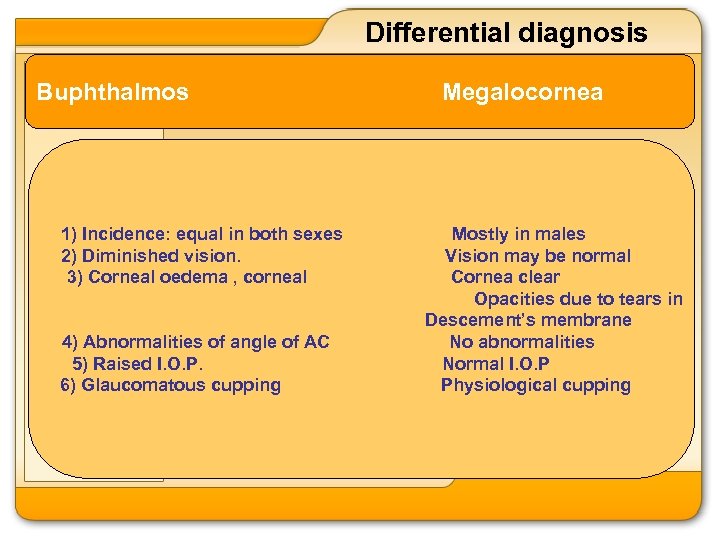
Differential diagnosis Buphthalmos 1) Incidence: equal in both sexes 2) Diminished vision. 3) Corneal oedema , corneal 4) Abnormalities of angle of AC 5) Raised I. O. P. 6) Glaucomatous cupping Megalocornea Mostly in males Vision may be normal Cornea clear Opacities due to tears in Descement’s membrane No abnormalities Normal I. O. P Physiological cupping
Treatment A) Medical : 1) Miotics are useless 2) Tab. diamox 5 -10 mg/kg body weight. B) Surgical: is more important 1) Goniotomy : Consists of incising the abnormal tissue at the angle by a goniotomy knife introduced through the opposite limbus , under direct visualization with the aid of gonioscope. 2) Trabeculotomy : The Schlemm’s canal is entered by means of an instrument called trabeculotome , which is then rotated towards AC so as to break the inner wall of the Schlemm’s canal. Aqueous from the AC can then drain into Schlemm’s canal. 3) Filtering operation such as trabeculectomy , if the above operation fail. However , prognosis is often unfavourable. 4) ‘Nowadays , a combination of trabeculectomy with trabeculectomy is being done with fairly good success’. If obstruction to aqueous outflow is incomplete , signs sometimes are delayed till puberty when it is known as juvenile glaucoma.
Primary Glaucomas They have the following features: 1) They are not associated with obvious intraocular disorder that might account for the high IOP. 2) They are typically bilateral. 3) They are generally believed to have a genetic basis
There are 2 types of primary glaucomas 1)Primary open angle glaucoma 1) Age: 50 – 60 years … 2) Sex : Mostly equal in … both sexes but there is slight preponderance of males. 3) Types of individuals-affects … people who are generally the subjects of vascular sclerosis – diabetes mellitus. 4) Types of eyes usually … myopic , angle of AC wide open , AC normal depth 5) Onset of symptoms … Insidious 2) Primary angle closure glaucoma 40 -50 years Women are more affected than men Highly strung , anxious, sympathetictonic in type Usually hypermetropic eyeball small (cornea small) angle of AC narrow AC shadow Sudden – pain , redness diminision of vision
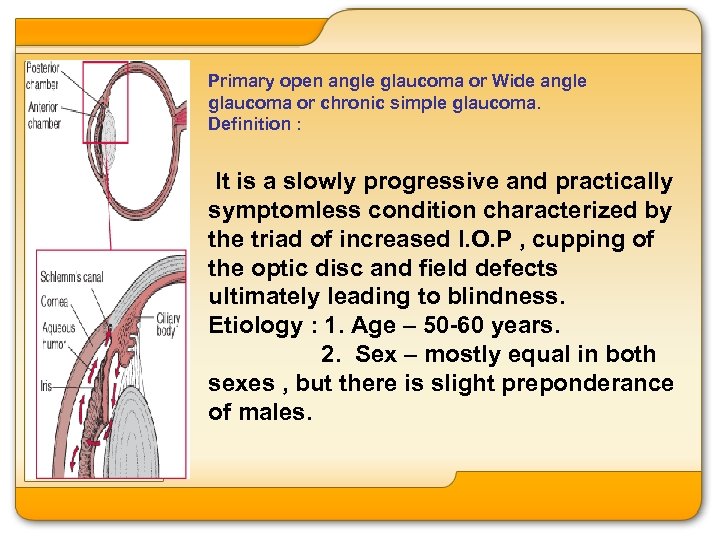
Primary open angle glaucoma or Wide angle glaucoma or chronic simple glaucoma. Definition : It is a slowly progressive and practically symptomless condition characterized by the triad of increased I. O. P , cupping of the optic disc and field defects ultimately leading to blindness. Etiology : 1. Age – 50 -60 years. 2. Sex – mostly equal in both sexes , but there is slight preponderance of males.
3. Type of individual affected : people who are generally the subjects of • vascular sclerosis. A combined process of vascular sclerosis of the optic nerve head and sclerosis of the trabecular mesh-work and adjoining structures ( canal of Schlemm , aqueous veins ) has been proposed. 4. Type of eye affected – usually • myopic , angle of Ac wide open , AC normal depth. 5. Predisposing factors • a) Family history of glaucoma • b) Diabetes mellitus •
Symptoms : The onset of the disease is • insidious ; it develops very gradually and may last for sometime before the patient becomes aware of the existence of an abnormal condition. 1) Painless progressive dimension • of vision ( refer senile cataract ) 2) Mild eye ache , headache. •
Symptoms : 3)Frequent change of presbyopic glasses ( • normally they require change once in 3 years ). This is due to weakness of accommodation as a result of : a) pressure upon the ciliary muscle and its • nerve supply b) decreased blood supply to the ciliary • muscle. 4)Coloured halos around light bulb due to • corneal oedema. 5) Defective dark adaptation , night • blindness. 6) An observant person may notice a • defect in the visual field. •
Signs : The eye may appears perfectly normal • externally or there may be a slight ciliary congestion. moderate dilatation of the episcleral veins. The pupil may be slightly or moderately • dilated and reacts sluggishly to light. The important signs which point to the • diagnosis are : 1) I. O. P. the tension in chronic simple • glaucoma requires careful study and repeated observation. Hospitalization of the patient for 24 hours is advisable.
Signs : The initial change is not so much a rise of • tension asan eaaggeration of the normal diurnal variation (2 mm of Hg ). Avariation in the oculare tension of over 5 mm Hg ( Schiotz)should always excite suspicion of glaucoma even though the whole excusion lies under the limits generally accepted as normal (22. 4 mm Hg). Some 20% of cases show the rise in • tension in the morning , some 25% in the afternoon and majority shows a biphasic curve , rising at both times. In most cases, however , the tension falls during the evening and night.
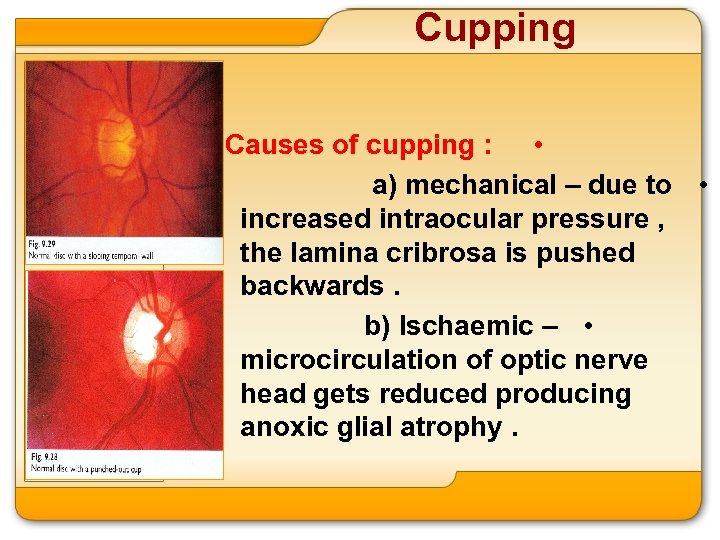
Cupping Causes of cupping : • a) mechanical – due to • increased intraocular pressure , the lamina cribrosa is pushed backwards. b) Ischaemic – • microcirculation of optic nerve head gets reduced producing anoxic glial atrophy.
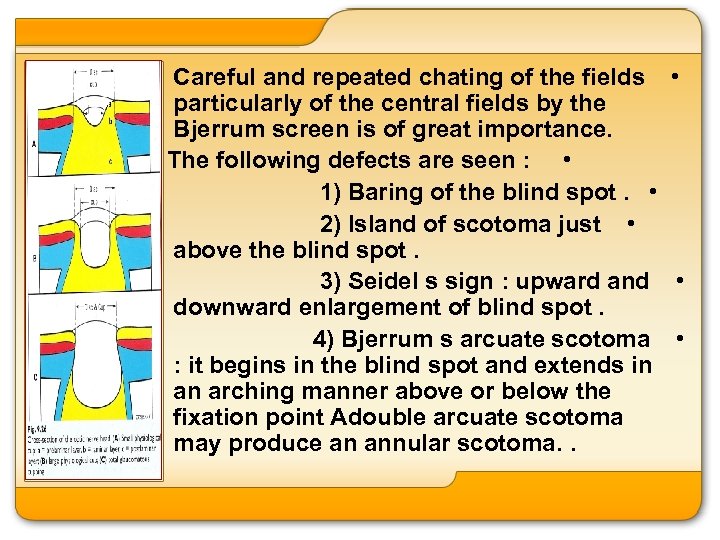
Careful and repeated chating of the fields • particularly of the central fields by the Bjerrum screen is of great importance. The following defects are seen : • 1) Baring of the blind spot. • 2) Island of scotoma just • above the blind spot. 3) Seidel s sign : upward and • downward enlargement of blind spot. 4) Bjerrum s arcuate scotoma • : it begins in the blind spot and extends in an arching manner above or below the fixation point Adouble arcuate scotoma may produce an annular scotoma. .
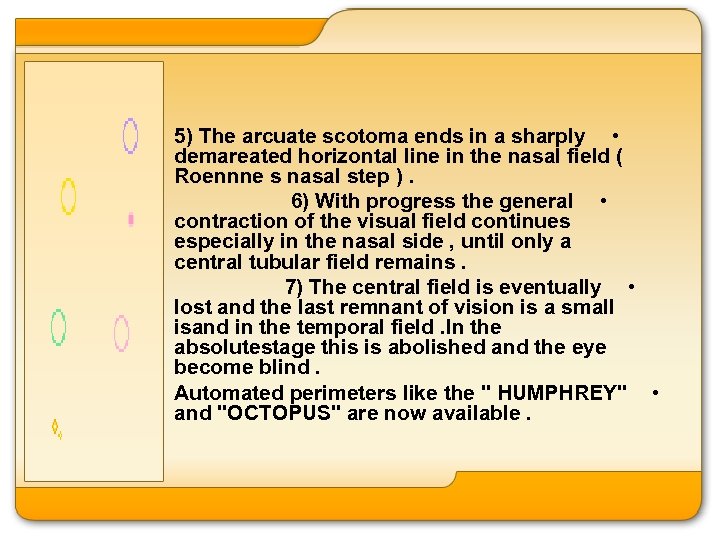
5) The arcuate scotoma ends in a sharply • demareated horizontal line in the nasal field ( Roennne s nasal step ). 6) With progress the general • contraction of the visual field continues especially in the nasal side , until only a central tubular field remains. 7) The central field is eventually • lost and the last remnant of vision is a small isand in the temporal field. In the absolutestage this is abolished and the eye become blind. Automated perimeters like the " HUMPHREY" • and "OCTOPUS" are now available.
Differential diagnosis 1. Senile cataract (refer lens) • 2. Optic atrophy • 3. Other causes of painless progressive • dimension of vision ( refer examination of an eye patient ) 4. Low Tension Glaucoma : Low vascular • perfusion pressure sometimes makes the optic nerve head susceptible to damage even with normal IOP. To prevent damage to the optic nerve head , IOP has to be maintained at 12 mm Hg. The Disc and field changes are similar to primary openangle glaucoma.
5. Ocular hypertension : In this condition • , the IOP is high but there are no disc and field changes. Such eyes need long term follow – up. Investigations : • 1. Tonography – The eye is compressed • by a weightes tonometer for 4 minutes and the IOP before and after the procedure is measured. In the normal eye , there is a gradual fall in the IOP but in eyes where drainage is impeded , the fall in the IOP remains insignificant.
2. Provocative test : Water drinking • test – after 8 hours fast. the patient is instructed to drink about 1 liter of water , following which the IOP is measured every 15 minutes for 1 hour. A rise of more than 8 mm Hg after 15 -30 mts. is considered to be positive.
Treatment The key to effecticve treatment is a • careful and regular follow – up reqiring recording of visiual acuity , tonometry, evaluation of optic disc by funduscopy and perimetry at periodic intervals. These help us to decide the dosage and combination of drugs and also the necessity for surgical intervention. Modes of treatment available for POAG are : 1. Medical • 2. Lser Trabeculoplasty • •
3. Filtering surgery • 1. medical : is the first and basic line og • management. 1) Miotics : ( parasympathomimetics) • a) Pilocarpine nitrate or hydrochloride ( 2 to 4 • %) Meechanism of action : • i) Contraction of ciliary muscle pulls the scleral • spur and opens the canal of Schlemm. ii) a histamine like action causing leakiness of the • trabeculare meshwork. iii) Contaction of ciliary muscle causes • compression of blood vessels in it , Thereby decreasing the production of aqueous. Action of Pilocarpine lasts for 6 hours •
Side effects : 1. Miosis – interferes with vision in patients • with nuclear cataract. 2. Ciliary spasm and cosequent • myopia 3. Folliculare conjunctivitis • b) Eserine or physotigmine (0. 25%) is • usually used in combination with pilocarpine. 2) Epinephrine 1 to 2 % (Sympathomimetic) • Mechanism of action : 1) Increased outflow of • aqueous 2) Decreased its • production Twice a day administration is sufficient and • produces mild mydriasis.
Side Effects : i) Conjunetival irritation and • pigmentation ii) Maculopathy • 3) Beta blockers : These • form the first line of medical therapy nowadays , They act by reducing aqueous production which in turn lowers IOP.
Advantages: i) no effect onpupillary size : no ciliary • spasm ii) Action lasts for 12 hours , therefore has to be instilled twice a day only a)Timolo maleate ( 0. 25% to 0. 5%) is • nonseective beta adrenergic blocker. Side effects : Local – superficial punctuate keratitis , corneal anaesthesia Systemic – bradycardia and bronchospasm. Hence contraindicated in asthma and cardiac patients. 4 ) Acetazolamide ( diamox) : It is a carbonic anhydrase inhibitor and reduces aqueous formation. • • •
Dose : Tab. 250 mg t. d. s. or q. i. d. • Side effects : 1) Numbness and • paraesthesia of extremities 2) Vomiting , diarrhea • 3) Renal calculi • II. Laser trabeculoplasty : Argon laser • trabeculoplasty causes a shrinkage of the collagen on the inner surface of the trabecular ring and contracts it , thereby opening the inter- trabeculare spaces and increasing the aqueous outflow.
In this out-patient procedure , the cornea • is anaesthetized and a Goldmann single mirror goniolens is inserted and laser burns of spot size um and duration 0. 1 second and power setting between 500 and 750 mw are applied over the trabecular meshwork. Usually about 180 of the angle is covered • in one sitting and the rest is done in the next session after about 4 weeks.
Side effects : 1) Transient rise of intraocular pressure, • 2) mild iritis, • 3) Peripheral anterior synechiae if • burns are placed very posteriorly. III. Surgical • Indications : • 1) When gross variation of tension • occurs in spite of medical treatment. 2) When base pressure cannot be kept • below 22. 4 mm of Hg with medical treatment
3) When deterioration in visual fields • urs in spite of medical treatment 4) Poor patient compliance – • patient does not use or cannot afford to buy drugs used in medical treatment. Principle: Trabeculectomy is the surgery • of choice. A rectangular piece of trabecular meshwork is removed under a partial thickness scleral flap to enable aqueous to filter from the anterior chamber into the subconjunctival space.
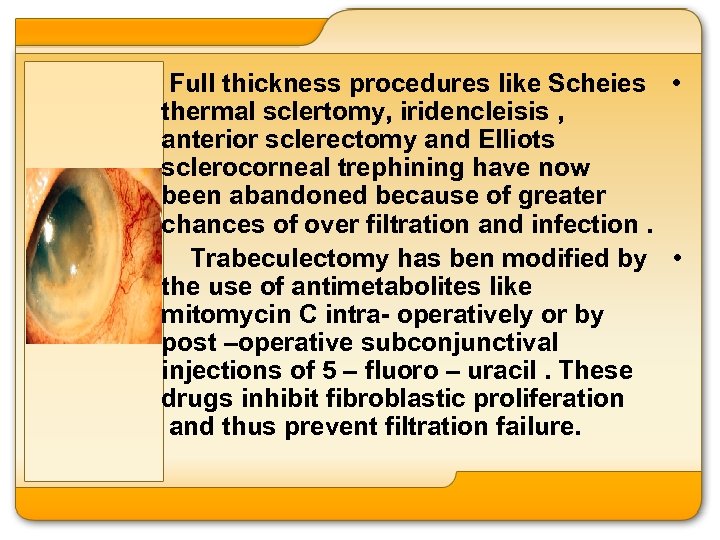
Full thickness procedures like Scheies • thermal sclertomy, iridencleisis , anterior sclerectomy and Elliots sclerocorneal trephining have now been abandoned because of greater chances of over filtration and infection. Trabeculectomy has ben modified by • the use of antimetabolites like mitomycin C intra- operatively or by post –operative subconjunctival injections of 5 – fluoro – uracil. These drugs inhibit fibroblastic proliferation and thus prevent filtration failure.
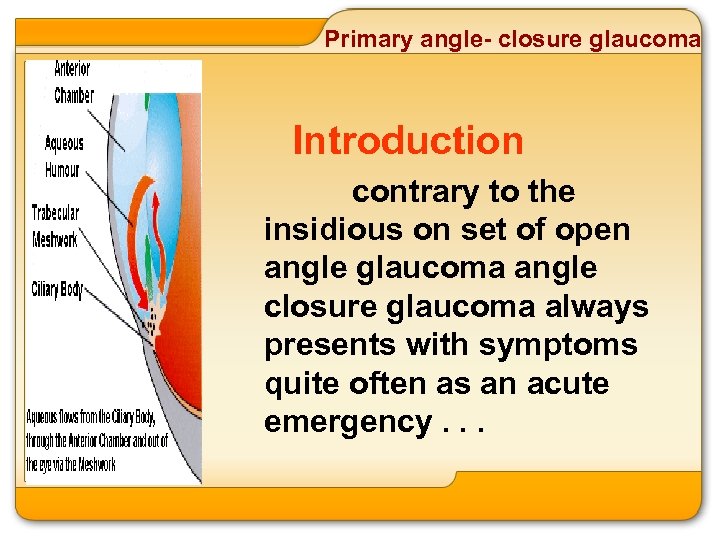
Primary angle- closure glaucoma Introduction contrary to the insidious on set of open angle glaucoma angle closure glaucoma always presents with symptoms quite often as an acute emergency. . .
Primary angle- closure glaucoma
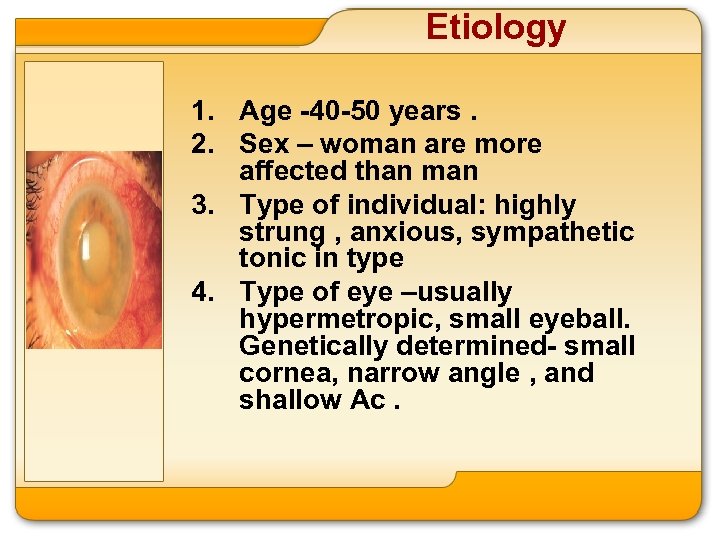
Etiology 1. Age -40 -50 years. 2. Sex – woman are more affected than man 3. Type of individual: highly strung , anxious, sympathetic tonic in type 4. Type of eye –usually hypermetropic, small eyeball. Genetically determined- small cornea, narrow angle , and shallow Ac.
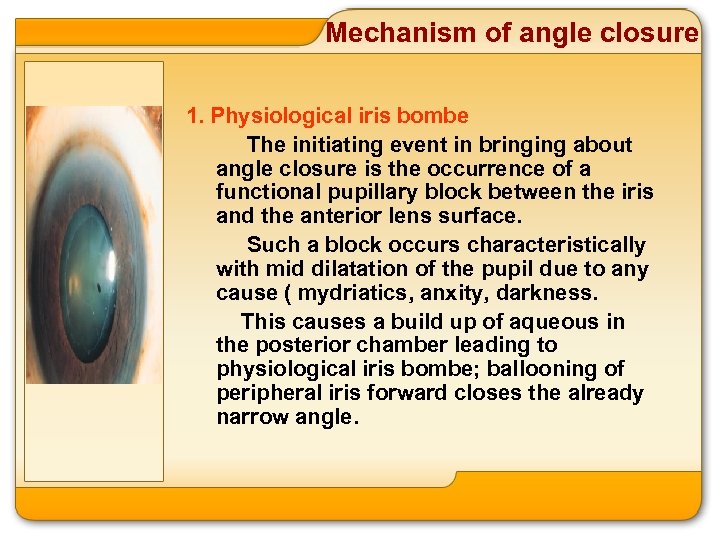
Mechanism of angle closure 1. Physiological iris bombe The initiating event in bringing about angle closure is the occurrence of a functional pupillary block between the iris and the anterior lens surface. Such a block occurs characteristically with mid dilatation of the pupil due to any cause ( mydriatics, anxity, darkness. This causes a build up of aqueous in the posterior chamber leading to physiological iris bombe; ballooning of peripheral iris forward closes the already narrow angle.
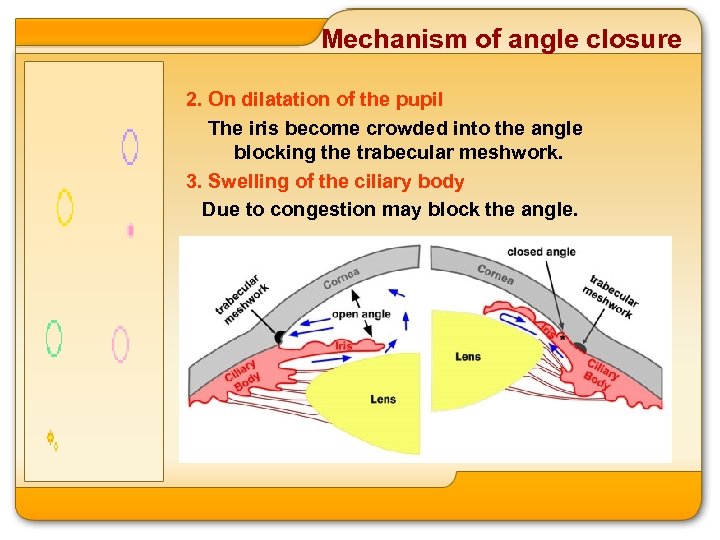
Mechanism of angle closure 2. On dilatation of the pupil The iris become crowded into the angle blocking the trabecular meshwork. 3. Swelling of the ciliary body Due to congestion may block the angle.
Clinical features The course of the disease may be divided into 5 stages. 1. Prodromal stage: occasional attacks of raised tension occure. Symptoms: Blurring of vision Coloured halos around lights due to corneal oedema Mild eyeache/ headache Signs: eye is white Cornea is hazy due to oedema IOP is raised.
Prodromal stage Treatment : Pilocarpine drops 2% t. d. s. ; it contracts the pupil and prevents crowding of the iris at the angle. Laser iridotomy Surgical: peripheral iridectomyhelps the aqueous humour to pass directly into the AC from posterior chamber therapy overcoming the pupillary block.
Clinical features 2. Stage of consistant instability: Intermittency in these attacks is replaced by regularity. Normal dirurnal variation of tension (2 mm. Hg)becomes exaggerated. Clinical features & Treatment: are same as in prodormal stage.
Clinical features 3. Acute congestion Attacks or acute congestive glaucoma: In a considerable number of cases both eyes are affected almost simultaneously, an attack in one eye being followed by similar targedy in the other.
Acute congestion Symptoms: - Sudden gross dimension of vision : in a few hours it may be reduced to hand movements close to face or even to perception of light. - Severe neuralgic pain in the eye radiating along the branches of the 5 th cranial nerve and causing violent headache; this pain sometimes is so severe that it is associated with nausea and vomiting. Such attacks have been mistaken for “bilious attacks” or acute abdomen. - Watering.
Acute congestion Signs - Oedema of lids - Marked congestion of the conjunctivaboth ciliary and conjunctival; chemosis of conjunctiva. - Cornea is steamy, and insensitive - AC is shallow - Pupil is dilated, vertically oval. Reaction to light and accommodation are absent.
Acute congestion Signs - Iris is congested and discolored. - IOP is markedly raised and eyeball is stony hard. - Fundus examination with an ophthalmoscope is not possible due to corneal oedema. The oedema may be temporarily cleared with glycerine drops. Fundus shows the picture of papilledema- disc margins are blurred, hyperemic, physiological cup is obscured. Arterial pulsations are seen.
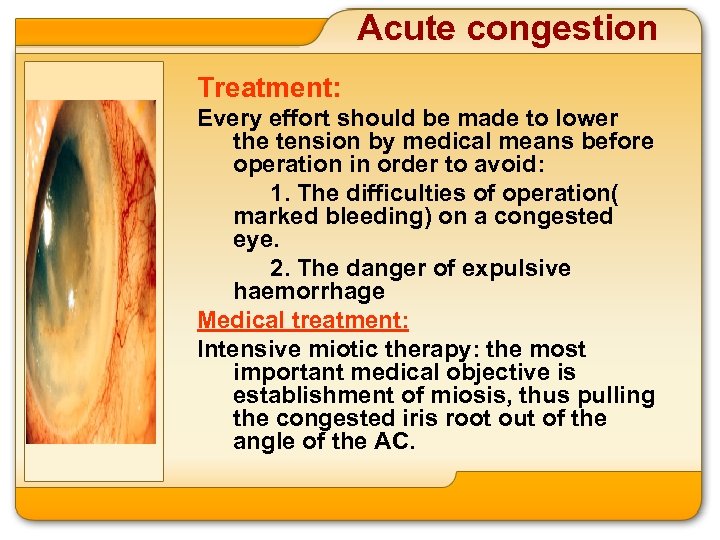
Acute congestion Treatment: Every effort should be made to lower the tension by medical means before operation in order to avoid: 1. The difficulties of operation( marked bleeding) on a congested eye. 2. The danger of expulsive haemorrhage Medical treatment: Intensive miotic therapy: the most important medical objective is establishment of miosis, thus pulling the congested iris root out of the angle of the AC.
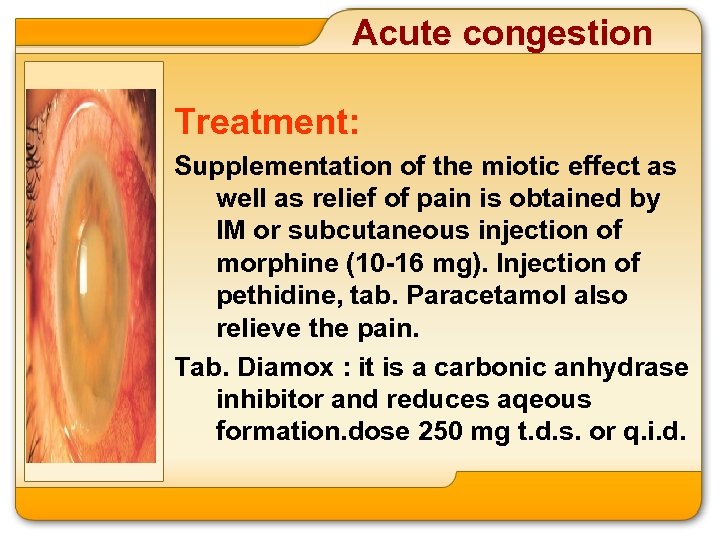
Acute congestion Treatment: Supplementation of the miotic effect as well as relief of pain is obtained by IM or subcutaneous injection of morphine (10 -16 mg). Injection of pethidine, tab. Paracetamol also relieve the pain. Tab. Diamox : it is a carbonic anhydrase inhibitor and reduces aqeous formation. dose 250 mg t. d. s. or q. i. d.
Acute congestion Treatment: Hyperosmotic agents: these cause deturgescenece of vitreous (by withdrawing fluid from it) and lower the IOP. They are very potent in this respect. I. V. Mannitol 20% 350 c. c. it should not be used in borderline cases of congestive cardiac failure. I. V. urea. It should not be used in kidney diseases
Acute congestion II. Surgical treatment: - If the IOP is not controlled within 12 -24 hours an operation has to be undertaken. - Filtering operation- trabeculectomy - Laser iridotomy to relieve pupillary block
Clinical features 4. Chronic congestive glaucoma: After a period of quiescence, another acute attack occurs, succeeded by others, each attack causes greater reduction of vision and permanent adhesion of the congested root of iris to the back of the cornea – peripheral anterior synchiae. If the peripheral anterior synchiae become extensive, the tension remains permanently elevated.
Chronic congestive glaucoma Signs: - Ciliary congestion Cornea hazy IOP is raised Fundus examination shows glaucomatous cupping. - Field defects appear- similar to those in chronic simple glaucoma
Chronic congestive glaucoma Treatment : medical : Miotic 2% pilocarpine drops Tab. Diamox one t. d. s. or q. i. d. Surgical : Filtering operation trabeclectomy
E. absolute glaucoma IT IS THE END STAGE and is characterised by: 1. Absence of perception of light … 2. High IOP…
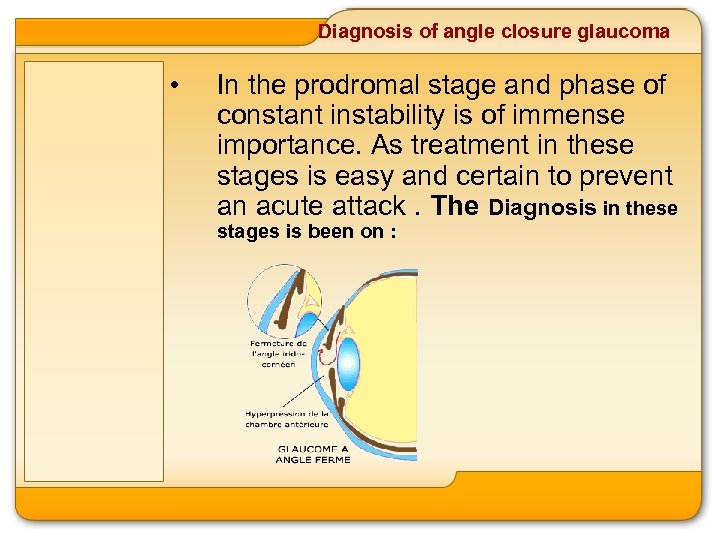
Diagnosis of angle closure glaucoma • In the prodromal stage and phase of constant instability is of immense importance. As treatment in these stages is easy and certain to prevent an acute attack. The Diagnosis in these stages is been on :
1. History of seeing coloured holes 2. Presence of small cornea 3. Provocative tests a)- mydriatic test: b)- dark room test
Absolute glaucoma Definition It is the end stage of all neglected glaucomas * primary angle closure, *primary open angle, buphthalmos *secondary glaucoma due to any cause. It is characterized by : 1. Absence of perception of light 2. High intraocular pressure eyeball is stony hard
Absolute glaucoma Symptoms: Pain in the eye, headache Complete blindness- cannot even per ceive light. Signs: 1. 2. Ciliary congestion Cornea is hazy (due to oedema) and is insensitive. It may show: l Bullous keratopathy- vesicles may be seen l Filamentary keratitis- filaments are formed by partialy shed epithelium.
Absolute glaucoma Signs: 3 - AC is shallow. 4 - Iris shows: Whitish patches of atrophy Ectropion of uveal pigment- dark pigmented zone around the pupil. Pupil is widely dilated, fixed (there is no reaction to light) and is grey or greenish. Lens is cataractous IOP is markedly raised. eyeball is stony hard. Intercalary, ciliary and equatorial staphylomas may be seen.
Absolute glaucoma Signs: Fundus shows glaucomatous optic atrophy. Sooner or later the eye becomes phthisical. The causes of phthisis bulbi are: 1. The tension becomes diminshed due to pressure atrophy of the ciliary body. 2. This leads to atrophic bulbi and later to phthisis bulbi. .
Absolute glaucoma Signs: 3. Due to corneal anaesthesia and persistent corneal oedema, corneal ulceration develops. Perforation of corneal ulcer leads to panophthalmitis and phthisis bulbi
Absolute glaucoma Treatment : Enucleation – since the eye ball is blind and painful. If this refused. 1. Tension may be lowered by cyclocryotherapy. The formation of aqueous can be reduced by inducing segmental atrophy of the ciliary body by application of cryo on the overlying sclera. 2. Pain may be relieved for a few months by a retrobulbar injection of 1 ml of 2% xylocaine followed 7 mts. Later by alcohol (80%0. a firm pad and bandage is applied for 24 hours.
Secondary glaucoma : have • the following features: they are characterised by assosiated ocular disorders that appear to be responsible for the raised iop e. g. iridocyclitis intumescent cataract ets. they are usually unilateral. they usually due to acquired and not inherited causes.
Causes and treatment of secondary glaucoma 1. Inflammatory and post inflammatory : Iridocyclitis: 1 - Clogging of trabecular meshwork by inflammatory exudate plasmoid aqueous 2 - Seclusio pupillae 3 - Seclusio pupillae produces iris bombe which gives rise to peripheral anterior synchiae. 4 - Occlusio pupillae 5 - Increased capillary hydrostatic pressure leading to increased aqueous formation.
Treatment 1 -local use of 1%atropine • corticosteroid hot fomentation. 2 -tab. diamox 250 mg t. d. s. • 3 -surgical paracentesis. Peripheral • iridectomy can be done to relieve the pupillary block in cases of iris bombe. in cases with extensive peripheral anterior synechiae due to iris bombe trabeculectomy may be required. earlier fuchs four dot iridotomy was done by passing von graefes knife across ac puncturing and counter puncturing both cornea and iris. this is now of historical interest only. •
Causes and treatment of secondary glaucoma • fuchs’ heterochromic uveitis: • In this condition, chronic uveitis is associated with a pale depigmented iris, secondary glaucoma and posterior subcapsular cataract. • Glaucomato – cyclitis- (posnerschlossman syndrome ) • Is characterized by recurrent attacks of secondary open angle glaucoma with mild anterior uveitis, but with symptoms of narrow angle glaucoma. Treatment is with topical steroids and antiglaucoma drugs
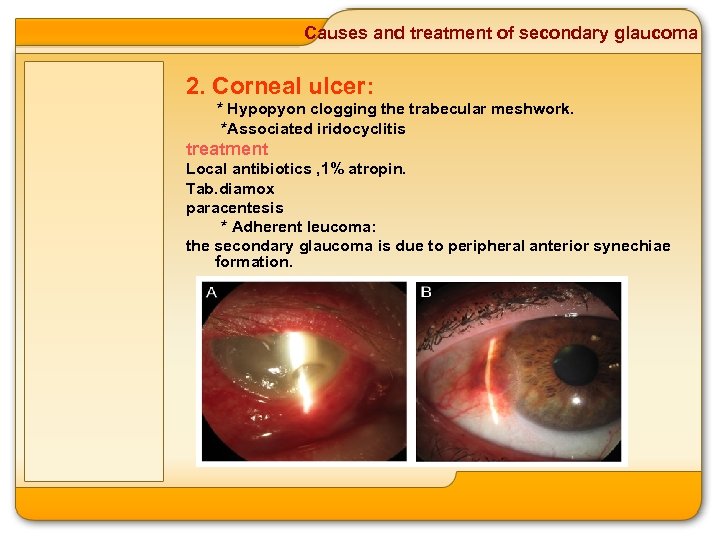
Causes and treatment of secondary glaucoma 2. Corneal ulcer: * Hypopyon clogging the trabecular meshwork. *Associated iridocyclitis treatment Local antibiotics , 1% atropin. Tab. diamox paracentesis * Adherent leucoma: the secondary glaucoma is due to peripheral anterior synechiae formation.
Causes and treatment of secondary glaucoma Treatment tab. diamox. Filtering surgery trabeculectomy Penetrating keratoplasty 3. Scleritis : The secondary glaucoma is due to associated iridocyclitis and treatment is the same as in iridocyclitis.
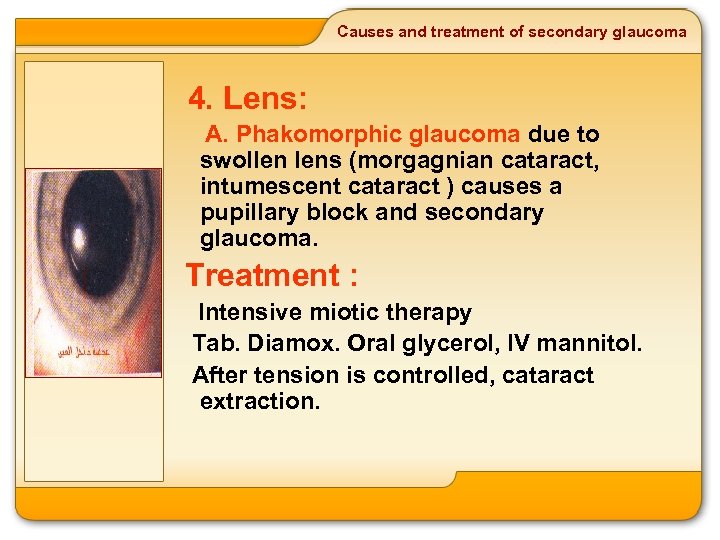
Causes and treatment of secondary glaucoma 4. Lens: A. Phakomorphic glaucoma due to swollen lens (morgagnian cataract, intumescent cataract ) causes a pupillary block and secondary glaucoma. Treatment : Intensive miotic therapy Tab. Diamox. Oral glycerol, IV mannitol. After tension is controlled, cataract extraction.
Causes and treatment of secondary glaucoma B. Phakolytik glaucoma: The lens matter in cases of hypermature cataract might leak out into the AC. Here it gets engulfed by macrophages which then go and block the trabecular meshwork. Treatment : Same as in phakomorphic glaucoma
Causes and treatment of secondary glaucoma C. Subluxated and dislocated lens : Irritation of ciliary body Posterior dislocated lens pushes iris forwards giving rise to peripheral anterior synechiae Treatment : Removal of lens with cryoprobe or wire vectis.
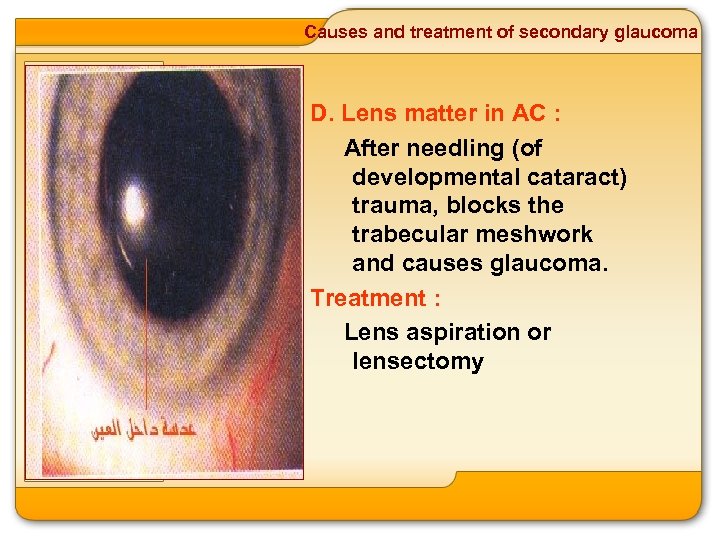
Causes and treatment of secondary glaucoma D. Lens matter in AC : After needling (of developmental cataract) trauma, blocks the trabecular meshwork and causes glaucoma. Treatment : Lens aspiration or lensectomy
Causes and treatment of secondary glaucoma E. Spherophakia : causes glaucoma in versus; since the lens is globular miotics cause pupillary block and raise the intraocular pressure. Treatment : Mydriatics
Causes and treatment of secondary glaucoma F. Aphakic glaucoma Peripheral anterior synechiae due to persistent post operative shallow AC. Vitreous loss Epithelialisation of AC. Treatment : Cyclodialysis 0
Causes and treatment of secondary glaucoma 5. Intraocular hemorrhage : a. Hyphaema : cellular elements clog the trabecular meshwork Treatment : Vit. C. , Injection Vit. K. , calcium gluconate, Tab. diamox Paracentesis b. Vitreous hemorrhage : the iris lens diaphragm is pushed forward giving rise to peripheral anterior synechiae tab diamox
Causes and treatment of secondary glaucoma 6. Haemorrhagic glaucoma : Due to central retinal vein and central retinal artery occlusion. Fibrovascular membrane blocks the trabecular meshwork. These new vessels are fragile and bleed producing recurrent hyphaema. Treatment : Prophylactic : by doing panretinal photocoagulating following central retinal vein occlusion. Cyclocryotherapy Enucleation
Causes and treatment of secondary glaucoma 7. Intraocular tumors : Retinoblastoma, malignant melanoma of choroid. the site of the tumor is more important than its size e. g. . Tumors near the site of exit of vortex veins tend to cause glaucoma. Involvement of vortex veins Involvement of the angle of ac by extension of growth. Iris lens diaphragm pushed forward by growth giving rise To peripheral anterior synechiae. Treatment : Enucleation
Causes and treatment of secondary glaucoma 8. Ocular trauma : In blunt injury secondary glaucoma may be due to traumatic iridocyclitis, intraocular haemorrhage, lens damage and damage to trabecular meshwork. Treatment : Tab. Diamox Filtering surgery – trabeculectomy Penetrating injuries and chemical burns also cause secondary glaucoma. Venous obstruction Orbital tumor meningioma. Orbital cellulites.
Causes and treatment of secondary glaucoma 10. Glaucoma capsulare or pseudoexfoliation glaucoma : the pseudoexfoliation syndrome is characterized by the deposition of dandrufflike material on the anterior lens capsular, the pupillary border, trabecular meshwork and other parts of the anterior segment of the eye. The origin of the material is believed to be ciliary body epithelium and the anterior subcapsular epithelium of the lens. pseudoexfoliation syndrome affects eldery patients and is frequently associated with open angle glaucoma.
This form of glaucoma presents like • primary open angle glaucoma and is believed to be caused by pigment and psefoliationudoex material bloking the trabecular meshwork. Psefoliationudoex glaucoma usually rspond Poorly to medical therapy and • trabeculectomy is often required. response to argon laser trabeculoplasty is usually good due to pigmentation of the trabecular meshwork. other association of the psefoliationudoex syndrome include nuclear cataract. subluxation of the lens poor mydriasis and pigment dispersion.
Causes and treatment of secondary glaucoma 9. Pigmentary glaucoma : It is typically seen in young male myopes. The clinical presentation resembles that of primary open angle glaucoma. It is characterized by excessive pigment dispersion from iris which blocks the trabecular meshwork producing elevated IOP. Slit lamp examination reveals krukenberg spindles on the back of cornea and gonioscopy shows an open angle with deposition of pigment on trabecular meshwork. The condition responds well to argon laser trabeculoplasty and tends to improve with age.
716b8331910d4fcd0615180ccd31f251.ppt