Шако.ppt
- Количество слайдов: 45
 GLAUCOMA and PREGNANCY
GLAUCOMA and PREGNANCY
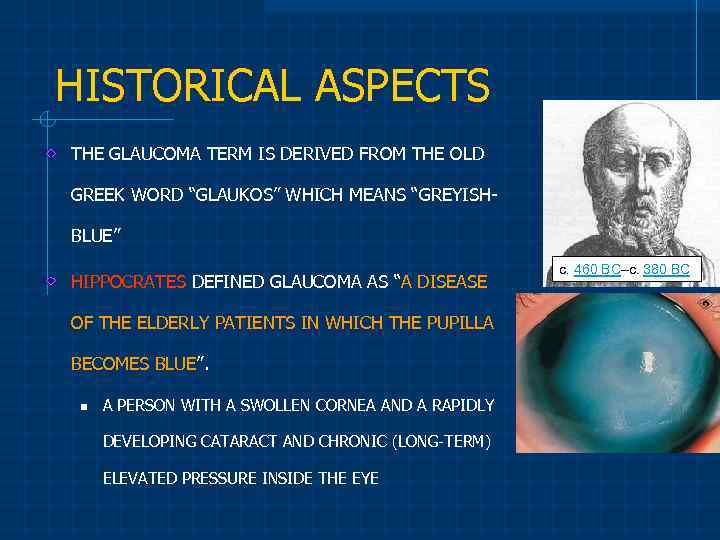 HISTORICAL ASPECTS THE GLAUCOMA TERM IS DERIVED FROM THE OLD GREEK WORD “GLAUKOS” WHICH MEANS “GREYISHBLUE” HIPPOCRATES DEFINED GLAUCOMA AS “A DISEASE OF THE ELDERLY PATIENTS IN WHICH THE PUPILLA BECOMES BLUE”. n A PERSON WITH A SWOLLEN CORNEA AND A RAPIDLY DEVELOPING CATARACT AND CHRONIC (LONG-TERM) ELEVATED PRESSURE INSIDE THE EYE c. 460 BC–c. 380 BC
HISTORICAL ASPECTS THE GLAUCOMA TERM IS DERIVED FROM THE OLD GREEK WORD “GLAUKOS” WHICH MEANS “GREYISHBLUE” HIPPOCRATES DEFINED GLAUCOMA AS “A DISEASE OF THE ELDERLY PATIENTS IN WHICH THE PUPILLA BECOMES BLUE”. n A PERSON WITH A SWOLLEN CORNEA AND A RAPIDLY DEVELOPING CATARACT AND CHRONIC (LONG-TERM) ELEVATED PRESSURE INSIDE THE EYE c. 460 BC–c. 380 BC
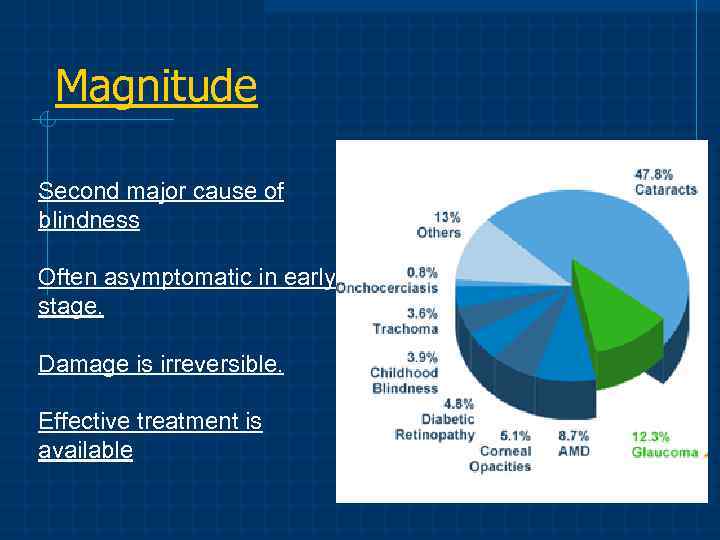 Magnitude Second major cause of blindness Often asymptomatic in early stage. Damage is irreversible. Effective treatment is available
Magnitude Second major cause of blindness Often asymptomatic in early stage. Damage is irreversible. Effective treatment is available
 How many people suffer from Glaucoma? According to WHO, about 100 million person in the world suffer from glaucoma and until 2030 this figure will double
How many people suffer from Glaucoma? According to WHO, about 100 million person in the world suffer from glaucoma and until 2030 this figure will double
 WHAT IS THE INTRAOCULAR PRESSURE? PRESSURE INSIDE THE EYE IS TERMED ”INTRAOCULAR PRESSURE (IOP)” EYE PRESSURE IS MEASURED IN MILLIMETERS OF MERCURY (mm. Hg) “NORMAL EYE PRESSURE” IS NOT A STABLE NUMBER(S), IT RANGES FROM 10 to 21 mm. Hg ELEVATED IOP IS AN EYE PRESSURE OF “GREATER THAN 21 mm. Hg”
WHAT IS THE INTRAOCULAR PRESSURE? PRESSURE INSIDE THE EYE IS TERMED ”INTRAOCULAR PRESSURE (IOP)” EYE PRESSURE IS MEASURED IN MILLIMETERS OF MERCURY (mm. Hg) “NORMAL EYE PRESSURE” IS NOT A STABLE NUMBER(S), IT RANGES FROM 10 to 21 mm. Hg ELEVATED IOP IS AN EYE PRESSURE OF “GREATER THAN 21 mm. Hg”
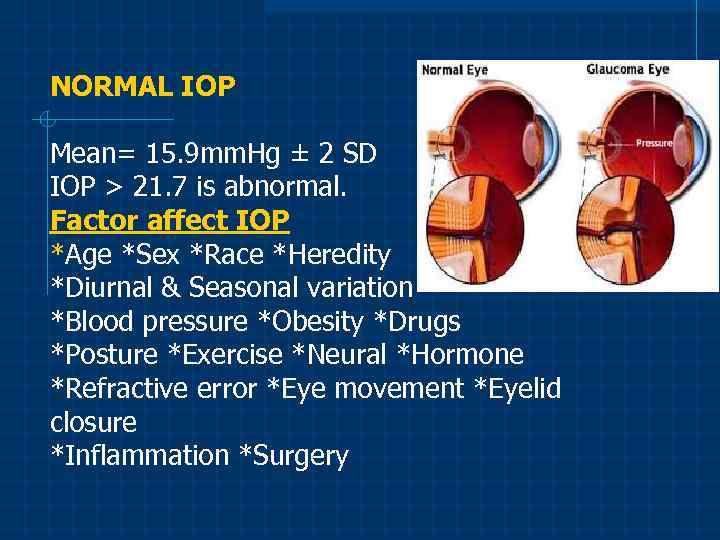 NORMAL IOP Mean= 15. 9 mm. Hg ± 2 SD IOP > 21. 7 is abnormal. Factor affect IOP *Age *Sex *Race *Heredity *Diurnal & Seasonal variation *Blood pressure *Obesity *Drugs *Posture *Exercise *Neural *Hormone *Refractive error *Eye movement *Eyelid closure *Inflammation *Surgery
NORMAL IOP Mean= 15. 9 mm. Hg ± 2 SD IOP > 21. 7 is abnormal. Factor affect IOP *Age *Sex *Race *Heredity *Diurnal & Seasonal variation *Blood pressure *Obesity *Drugs *Posture *Exercise *Neural *Hormone *Refractive error *Eye movement *Eyelid closure *Inflammation *Surgery
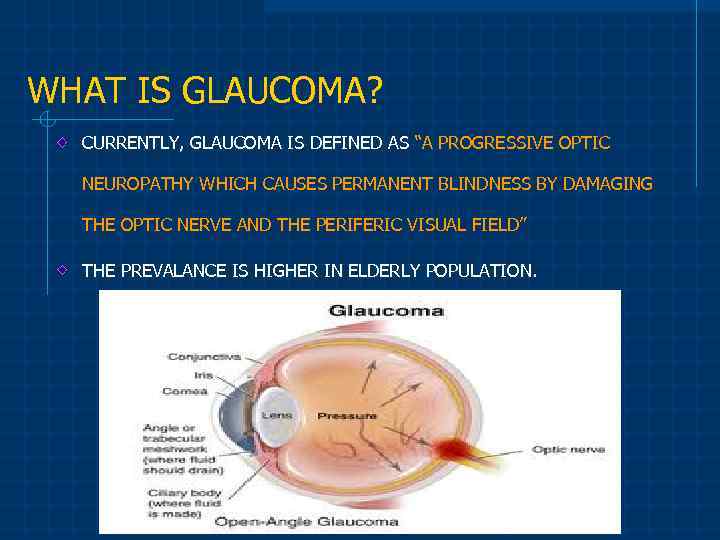 WHAT IS GLAUCOMA? CURRENTLY, GLAUCOMA IS DEFINED AS “A PROGRESSIVE OPTIC NEUROPATHY WHICH CAUSES PERMANENT BLINDNESS BY DAMAGING THE OPTIC NERVE AND THE PERIFERIC VISUAL FIELD” THE PREVALANCE IS HIGHER IN ELDERLY POPULATION.
WHAT IS GLAUCOMA? CURRENTLY, GLAUCOMA IS DEFINED AS “A PROGRESSIVE OPTIC NEUROPATHY WHICH CAUSES PERMANENT BLINDNESS BY DAMAGING THE OPTIC NERVE AND THE PERIFERIC VISUAL FIELD” THE PREVALANCE IS HIGHER IN ELDERLY POPULATION.
 GLAUCOMA Intraocular pressure is not the only factor responsible for glaucoma! v v v 95% of people with elevated IOP will never have the damage associated with glaucoma. One-third of patients with glaucoma do not have elevated IOP. Most of the ocular findings that occur in people with glaucoma also occur in people without glaucoma.
GLAUCOMA Intraocular pressure is not the only factor responsible for glaucoma! v v v 95% of people with elevated IOP will never have the damage associated with glaucoma. One-third of patients with glaucoma do not have elevated IOP. Most of the ocular findings that occur in people with glaucoma also occur in people without glaucoma.
 Glaucoma - the main cause of blindness in the world
Glaucoma - the main cause of blindness in the world
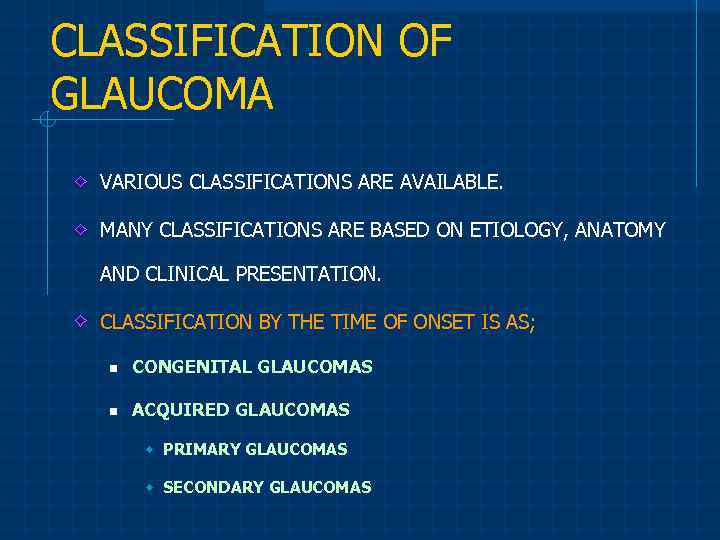 CLASSIFICATION OF GLAUCOMA VARIOUS CLASSIFICATIONS ARE AVAILABLE. MANY CLASSIFICATIONS ARE BASED ON ETIOLOGY, ANATOMY AND CLINICAL PRESENTATION. CLASSIFICATION BY THE TIME OF ONSET IS AS; n CONGENITAL GLAUCOMAS n ACQUIRED GLAUCOMAS w PRIMARY GLAUCOMAS w SECONDARY GLAUCOMAS
CLASSIFICATION OF GLAUCOMA VARIOUS CLASSIFICATIONS ARE AVAILABLE. MANY CLASSIFICATIONS ARE BASED ON ETIOLOGY, ANATOMY AND CLINICAL PRESENTATION. CLASSIFICATION BY THE TIME OF ONSET IS AS; n CONGENITAL GLAUCOMAS n ACQUIRED GLAUCOMAS w PRIMARY GLAUCOMAS w SECONDARY GLAUCOMAS
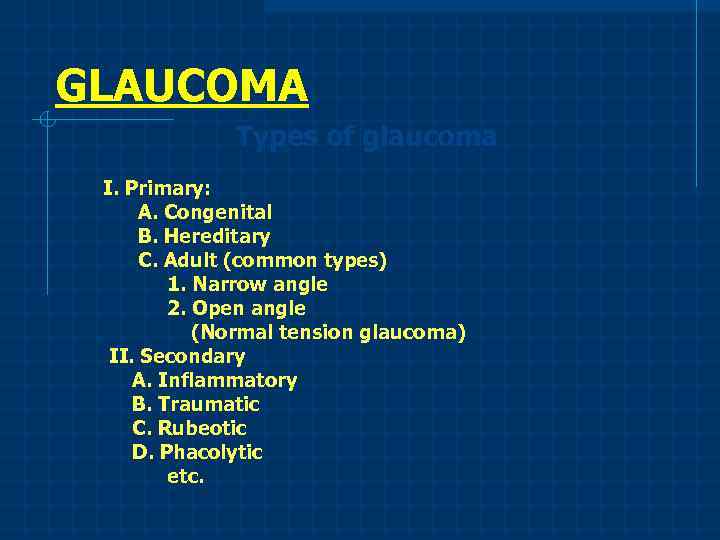 GLAUCOMA Types of glaucoma I. Primary: A. Congenital B. Hereditary C. Adult (common types) 1. Narrow angle 2. Open angle (Normal tension glaucoma) II. Secondary A. Inflammatory B. Traumatic C. Rubeotic D. Phacolytic etc.
GLAUCOMA Types of glaucoma I. Primary: A. Congenital B. Hereditary C. Adult (common types) 1. Narrow angle 2. Open angle (Normal tension glaucoma) II. Secondary A. Inflammatory B. Traumatic C. Rubeotic D. Phacolytic etc.
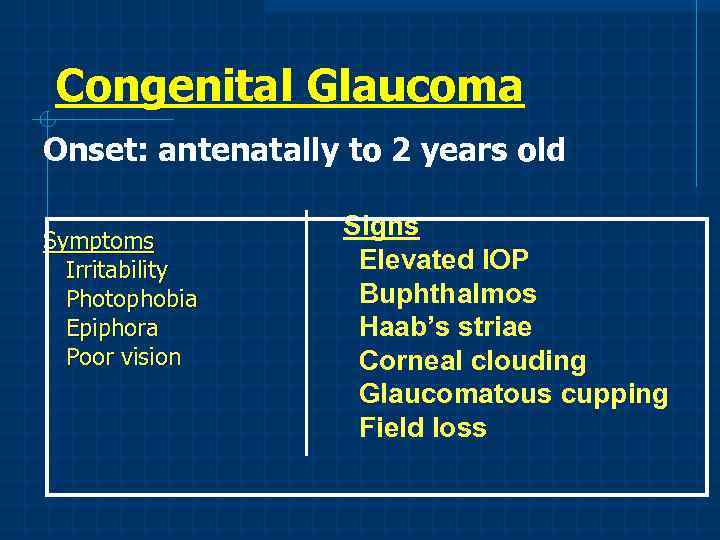 Congenital Glaucoma Onset: antenatally to 2 years old Symptoms Irritability Photophobia Epiphora Poor vision Signs Elevated IOP Buphthalmos Haab’s striae Corneal clouding Glaucomatous cupping Field loss
Congenital Glaucoma Onset: antenatally to 2 years old Symptoms Irritability Photophobia Epiphora Poor vision Signs Elevated IOP Buphthalmos Haab’s striae Corneal clouding Glaucomatous cupping Field loss
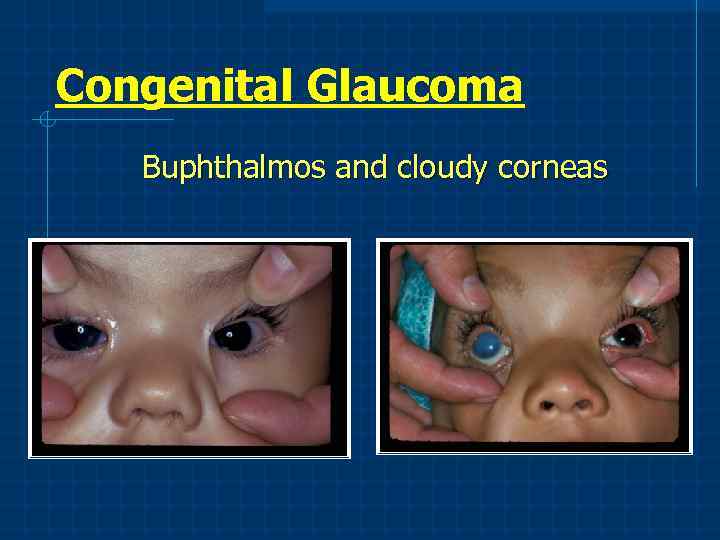 Congenital Glaucoma Buphthalmos and cloudy corneas
Congenital Glaucoma Buphthalmos and cloudy corneas
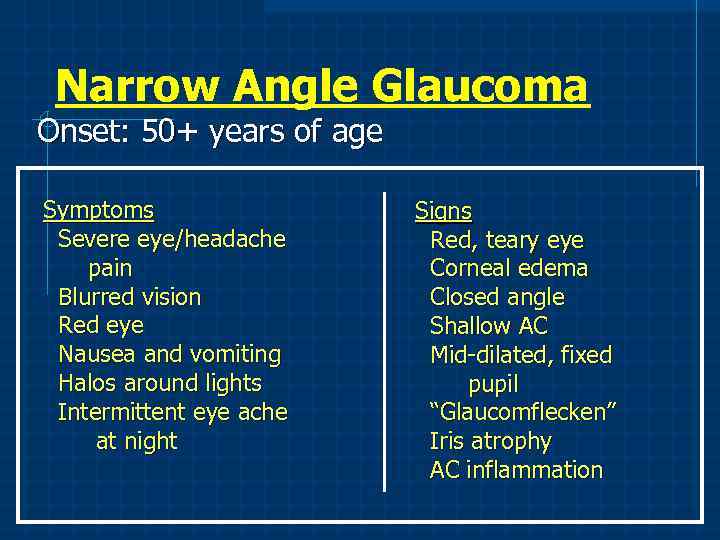 Narrow Angle Glaucoma Onset: 50+ years of age Symptoms Severe eye/headache pain Blurred vision Red eye Nausea and vomiting Halos around lights Intermittent eye ache at night Signs Red, teary eye Corneal edema Closed angle Shallow AC Mid-dilated, fixed pupil “Glaucomflecken” Iris atrophy AC inflammation
Narrow Angle Glaucoma Onset: 50+ years of age Symptoms Severe eye/headache pain Blurred vision Red eye Nausea and vomiting Halos around lights Intermittent eye ache at night Signs Red, teary eye Corneal edema Closed angle Shallow AC Mid-dilated, fixed pupil “Glaucomflecken” Iris atrophy AC inflammation
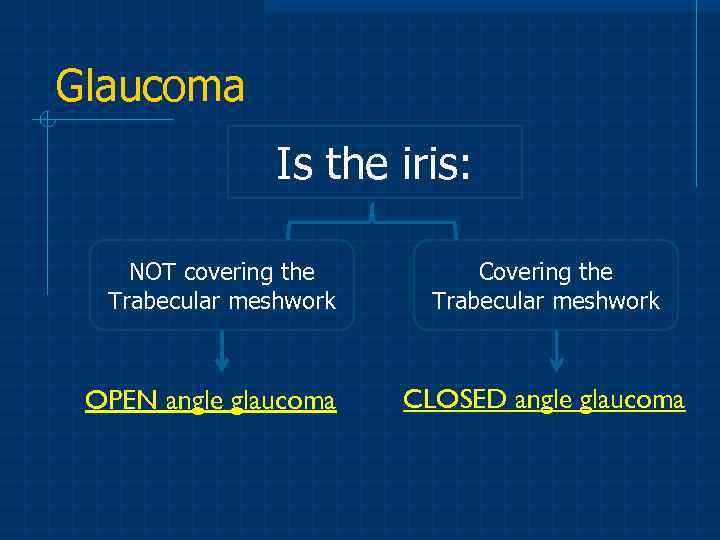 Glaucoma Is the iris: NOT covering the Trabecular meshwork OPEN angle glaucoma Covering the Trabecular meshwork CLOSED angle glaucoma
Glaucoma Is the iris: NOT covering the Trabecular meshwork OPEN angle glaucoma Covering the Trabecular meshwork CLOSED angle glaucoma
 CLASSIFICATION OF THE ACQUIRED GLAUCOMAS PRIMARY OPEN ANGLE GLAUCOMA NORMAL PRESSURE GLAUCOMA OCULAR HYPERTENSION SECONDARY OPEN ANGLE GLAUCOMAS PSEUDOEXFOLIATION GLAUCOMA PIGMENTARY GLAUCOMA PHACOLYTIC GLAUCOMA SECONDARY TO OCULAR INFLAMMATION SECONDARY TO HIGH EPISCLERAL VENOUS PRESSURE SECONDARY TO STEROID THERAPY PRIMARY ANGLE CLOSURE GLAUCOMAS • ACUTE ANGLE CLOSURE GLAUCOMA • SUBACUTE ANGLE CLOSURE GLAUCOMA SECONDARY ANGLE CLOSURE GLAUCOMAS DUE TO PERIPHERAL ANTERIOR SYNECHIAE SWOLLEN LENS OR PUPILLARY SECLUSION ANTERIOR MOVEMENT OF THE IRIS-LENS DIAPHRAGM NEOVASCULAR GLAUCOMA PLATEAU IRIS SYNDROME
CLASSIFICATION OF THE ACQUIRED GLAUCOMAS PRIMARY OPEN ANGLE GLAUCOMA NORMAL PRESSURE GLAUCOMA OCULAR HYPERTENSION SECONDARY OPEN ANGLE GLAUCOMAS PSEUDOEXFOLIATION GLAUCOMA PIGMENTARY GLAUCOMA PHACOLYTIC GLAUCOMA SECONDARY TO OCULAR INFLAMMATION SECONDARY TO HIGH EPISCLERAL VENOUS PRESSURE SECONDARY TO STEROID THERAPY PRIMARY ANGLE CLOSURE GLAUCOMAS • ACUTE ANGLE CLOSURE GLAUCOMA • SUBACUTE ANGLE CLOSURE GLAUCOMA SECONDARY ANGLE CLOSURE GLAUCOMAS DUE TO PERIPHERAL ANTERIOR SYNECHIAE SWOLLEN LENS OR PUPILLARY SECLUSION ANTERIOR MOVEMENT OF THE IRIS-LENS DIAPHRAGM NEOVASCULAR GLAUCOMA PLATEAU IRIS SYNDROME
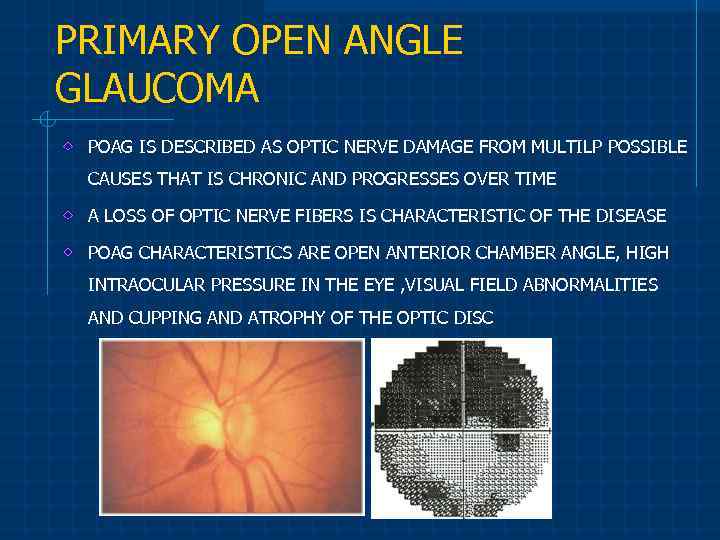 PRIMARY OPEN ANGLE GLAUCOMA POAG IS DESCRIBED AS OPTIC NERVE DAMAGE FROM MULTILP POSSIBLE CAUSES THAT IS CHRONIC AND PROGRESSES OVER TIME A LOSS OF OPTIC NERVE FIBERS IS CHARACTERISTIC OF THE DISEASE POAG CHARACTERISTICS ARE OPEN ANTERIOR CHAMBER ANGLE, HIGH INTRAOCULAR PRESSURE IN THE EYE , VISUAL FIELD ABNORMALITIES AND CUPPING AND ATROPHY OF THE OPTIC DISC
PRIMARY OPEN ANGLE GLAUCOMA POAG IS DESCRIBED AS OPTIC NERVE DAMAGE FROM MULTILP POSSIBLE CAUSES THAT IS CHRONIC AND PROGRESSES OVER TIME A LOSS OF OPTIC NERVE FIBERS IS CHARACTERISTIC OF THE DISEASE POAG CHARACTERISTICS ARE OPEN ANTERIOR CHAMBER ANGLE, HIGH INTRAOCULAR PRESSURE IN THE EYE , VISUAL FIELD ABNORMALITIES AND CUPPING AND ATROPHY OF THE OPTIC DISC
 CAUSES ? THE EXACT CAUSE OF POAG IS UNKNOWN THE MOST IMPORTANT (AND WELL KNOWN) CAUSE OF POAG IS INCREASED IOP THE CAUSE OF THE HIGH IOP IS GENERALLY ACCEPTED TO BE BECAUSE OF AN IMBALANCE IN THE PRODUCTION AND DRAINAGE OF FLUID IN THE EYE (AQUEOUS HUMOR) THE FLUID IS CONTINUALLY BEING PRODUCED BUT CANNOT BE DRAINED BECAUSE OF THE IMPROPERLY FUNCTIONING DRAINAGE CHANNELS (CALLED TRABECULAR MESHWORK) RAISING THE IOP!!
CAUSES ? THE EXACT CAUSE OF POAG IS UNKNOWN THE MOST IMPORTANT (AND WELL KNOWN) CAUSE OF POAG IS INCREASED IOP THE CAUSE OF THE HIGH IOP IS GENERALLY ACCEPTED TO BE BECAUSE OF AN IMBALANCE IN THE PRODUCTION AND DRAINAGE OF FLUID IN THE EYE (AQUEOUS HUMOR) THE FLUID IS CONTINUALLY BEING PRODUCED BUT CANNOT BE DRAINED BECAUSE OF THE IMPROPERLY FUNCTIONING DRAINAGE CHANNELS (CALLED TRABECULAR MESHWORK) RAISING THE IOP!!
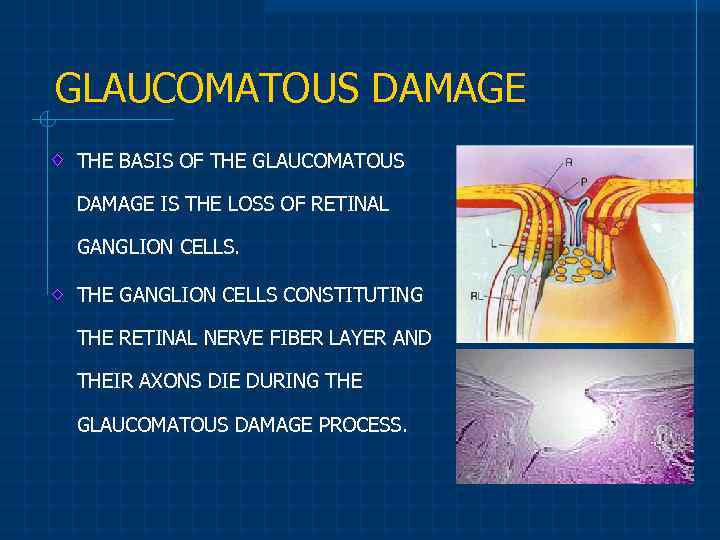 GLAUCOMATOUS DAMAGE THE BASIS OF THE GLAUCOMATOUS DAMAGE IS THE LOSS OF RETINAL GANGLION CELLS. THE GANGLION CELLS CONSTITUTING THE RETINAL NERVE FIBER LAYER AND THEIR AXONS DIE DURING THE GLAUCOMATOUS DAMAGE PROCESS.
GLAUCOMATOUS DAMAGE THE BASIS OF THE GLAUCOMATOUS DAMAGE IS THE LOSS OF RETINAL GANGLION CELLS. THE GANGLION CELLS CONSTITUTING THE RETINAL NERVE FIBER LAYER AND THEIR AXONS DIE DURING THE GLAUCOMATOUS DAMAGE PROCESS.
 SYMPTOMS MOST CASES ARE ASYMPTOMATIC UNTIL THE VISUAL FIELD ABNORMALITIES BECOME PROMINENT AND AFFECT CENTRAL VISION. THUS, ANNUAL ROUTINE EXAMINATION IS ESSENTIAL FOR EARLY DIAGNOSIS.
SYMPTOMS MOST CASES ARE ASYMPTOMATIC UNTIL THE VISUAL FIELD ABNORMALITIES BECOME PROMINENT AND AFFECT CENTRAL VISION. THUS, ANNUAL ROUTINE EXAMINATION IS ESSENTIAL FOR EARLY DIAGNOSIS.
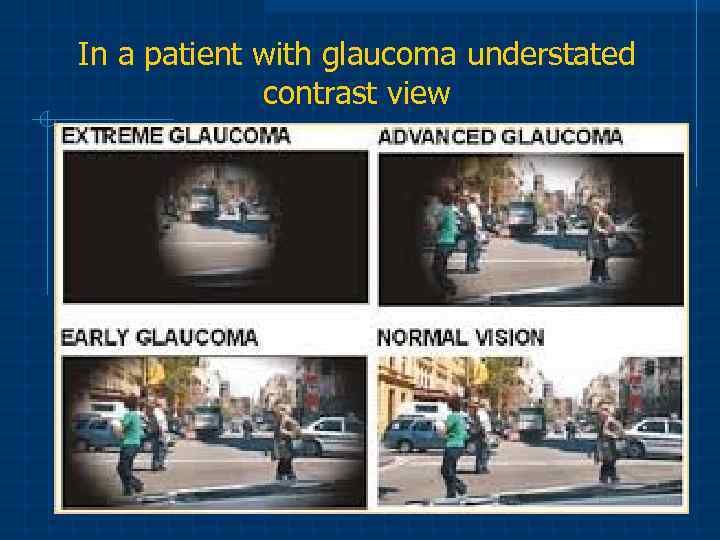 In a patient with glaucoma understated contrast view
In a patient with glaucoma understated contrast view
 Stages of pregnancy Ideally, a discussion of the treatment plan of a woman’s glaucoma should be initiated before pregnancy begins. In this way, the adverse effects of medications can be prevented during the first trimester, when most organogenesis is occurring. Additionally, alternate effective methods to lower IOP (including surgery if necessary) can be explored or achieved prior to pregnancy beginning. Women of childbearing age should inform their doctor immediately should they suspect they are pregnant, or if they are planning to start or add to their family.
Stages of pregnancy Ideally, a discussion of the treatment plan of a woman’s glaucoma should be initiated before pregnancy begins. In this way, the adverse effects of medications can be prevented during the first trimester, when most organogenesis is occurring. Additionally, alternate effective methods to lower IOP (including surgery if necessary) can be explored or achieved prior to pregnancy beginning. Women of childbearing age should inform their doctor immediately should they suspect they are pregnant, or if they are planning to start or add to their family.
 First Trimester A discussion of the risks of medication and the best strategy for IOP-lowering should occur as soon as pregnancy is noted, as organogenesis has often begun when pregnancy is first identified, and medications taken during organogenesis can result in birth defects. Pregnancy discussions should include a discussion of medication concentration/dosage, methods to minimize systemic drug absorption, and if medication can be withheld for parts of the pregnancy.
First Trimester A discussion of the risks of medication and the best strategy for IOP-lowering should occur as soon as pregnancy is noted, as organogenesis has often begun when pregnancy is first identified, and medications taken during organogenesis can result in birth defects. Pregnancy discussions should include a discussion of medication concentration/dosage, methods to minimize systemic drug absorption, and if medication can be withheld for parts of the pregnancy.
 Brimonidine, a Category B drug, may be the safest option for the first trimester. Other anti glaucoma medications such as beta-blocker, prostaglandins and carbonic anhydrase inhibitors should be avoided when possible in first trimester to reduce potential teratogenic effects or premature abortion. Discussions with the patient may include observation off treatment in this critical period.
Brimonidine, a Category B drug, may be the safest option for the first trimester. Other anti glaucoma medications such as beta-blocker, prostaglandins and carbonic anhydrase inhibitors should be avoided when possible in first trimester to reduce potential teratogenic effects or premature abortion. Discussions with the patient may include observation off treatment in this critical period.
 Second Trimester In second trimester, brimonidine can be applied and beta-blockers can be used with regular fetal heart rate and fetal growth monitoring. If prostaglandin analogues are used, premature labor symptoms and signs should be described to the patient, and the medication should be stopped if such symptoms are noted. When topical or oral carbonic anhydrase inhibitors are used, fetal growth retardation monitoring may be considered.
Second Trimester In second trimester, brimonidine can be applied and beta-blockers can be used with regular fetal heart rate and fetal growth monitoring. If prostaglandin analogues are used, premature labor symptoms and signs should be described to the patient, and the medication should be stopped if such symptoms are noted. When topical or oral carbonic anhydrase inhibitors are used, fetal growth retardation monitoring may be considered.
 Third Trimester Brimonidine, beta-blocker, or topical carbonic anhydrase inhibitors, can be used with caution. Avoidance of prostaglandins may decrease the risk of premature labor, which is particularly important early in the third trimester. Late in the third trimester, brimonidine should be discontinued because it can induce central nervous system depression in newborns. Topical carbonic anhydrase inhibitors may be the optimal choice in this period.
Third Trimester Brimonidine, beta-blocker, or topical carbonic anhydrase inhibitors, can be used with caution. Avoidance of prostaglandins may decrease the risk of premature labor, which is particularly important early in the third trimester. Late in the third trimester, brimonidine should be discontinued because it can induce central nervous system depression in newborns. Topical carbonic anhydrase inhibitors may be the optimal choice in this period.
 Postpartum Carbonic anhydrase inhibitors and beta-blockers are certified by the American Academy of Pediatrics for use during nursing. However, low doses of these medications should be considered when used in the breast feeding period. Brimonidine is contraindicated for use in lactating mothers due to the risk of central nervous system depression in the newborn.
Postpartum Carbonic anhydrase inhibitors and beta-blockers are certified by the American Academy of Pediatrics for use during nursing. However, low doses of these medications should be considered when used in the breast feeding period. Brimonidine is contraindicated for use in lactating mothers due to the risk of central nervous system depression in the newborn.
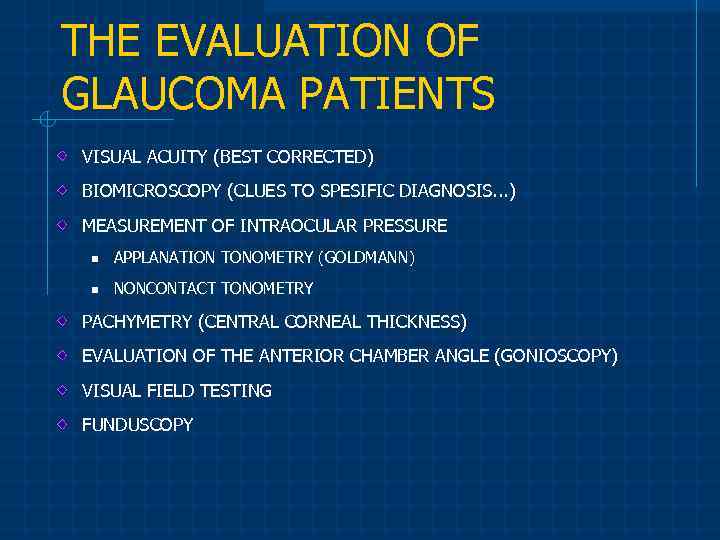 THE EVALUATION OF GLAUCOMA PATIENTS VISUAL ACUITY (BEST CORRECTED) BIOMICROSCOPY (CLUES TO SPESIFIC DIAGNOSIS. . . ) MEASUREMENT OF INTRAOCULAR PRESSURE n APPLANATION TONOMETRY (GOLDMANN) n NONCONTACT TONOMETRY PACHYMETRY (CENTRAL CORNEAL THICKNESS) EVALUATION OF THE ANTERIOR CHAMBER ANGLE (GONIOSCOPY) VISUAL FIELD TESTING FUNDUSCOPY
THE EVALUATION OF GLAUCOMA PATIENTS VISUAL ACUITY (BEST CORRECTED) BIOMICROSCOPY (CLUES TO SPESIFIC DIAGNOSIS. . . ) MEASUREMENT OF INTRAOCULAR PRESSURE n APPLANATION TONOMETRY (GOLDMANN) n NONCONTACT TONOMETRY PACHYMETRY (CENTRAL CORNEAL THICKNESS) EVALUATION OF THE ANTERIOR CHAMBER ANGLE (GONIOSCOPY) VISUAL FIELD TESTING FUNDUSCOPY
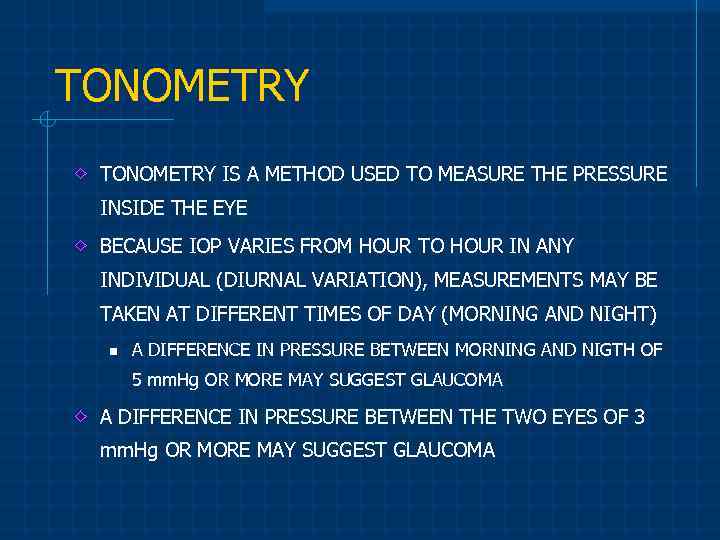 TONOMETRY IS A METHOD USED TO MEASURE THE PRESSURE INSIDE THE EYE BECAUSE IOP VARIES FROM HOUR TO HOUR IN ANY INDIVIDUAL (DIURNAL VARIATION), MEASUREMENTS MAY BE TAKEN AT DIFFERENT TIMES OF DAY (MORNING AND NIGHT) n A DIFFERENCE IN PRESSURE BETWEEN MORNING AND NIGTH OF 5 mm. Hg OR MORE MAY SUGGEST GLAUCOMA A DIFFERENCE IN PRESSURE BETWEEN THE TWO EYES OF 3 mm. Hg OR MORE MAY SUGGEST GLAUCOMA
TONOMETRY IS A METHOD USED TO MEASURE THE PRESSURE INSIDE THE EYE BECAUSE IOP VARIES FROM HOUR TO HOUR IN ANY INDIVIDUAL (DIURNAL VARIATION), MEASUREMENTS MAY BE TAKEN AT DIFFERENT TIMES OF DAY (MORNING AND NIGHT) n A DIFFERENCE IN PRESSURE BETWEEN MORNING AND NIGTH OF 5 mm. Hg OR MORE MAY SUGGEST GLAUCOMA A DIFFERENCE IN PRESSURE BETWEEN THE TWO EYES OF 3 mm. Hg OR MORE MAY SUGGEST GLAUCOMA
 APPLANATION TONOMETRY PERRKINS HAND HELD TONOMETER SCHIOTZ TONOMETER NON CONTACT TONOMETER THE TECHNIQUES OF IOP MEASUREMENTS TONOPEN XL
APPLANATION TONOMETRY PERRKINS HAND HELD TONOMETER SCHIOTZ TONOMETER NON CONTACT TONOMETER THE TECHNIQUES OF IOP MEASUREMENTS TONOPEN XL
 PACHYMETRY NORMAL CENTRAL CORNEAL THICKNESS IS VARIABLE 500 -520 MICRONS n THINNER CORNEA (CCT < 500 m) CAN GIVE FALSELY LOW PRESSURE READINGS n SEVERE GLAUCOMA PATIENTS MAY BE FAILED DIAGNOSE n A THICK CORNEA (>600 m) CAN GIVE FALSELY HIGH PRESSURE READINGS n UNNECESSARY TREATMENTS !!
PACHYMETRY NORMAL CENTRAL CORNEAL THICKNESS IS VARIABLE 500 -520 MICRONS n THINNER CORNEA (CCT < 500 m) CAN GIVE FALSELY LOW PRESSURE READINGS n SEVERE GLAUCOMA PATIENTS MAY BE FAILED DIAGNOSE n A THICK CORNEA (>600 m) CAN GIVE FALSELY HIGH PRESSURE READINGS n UNNECESSARY TREATMENTS !!
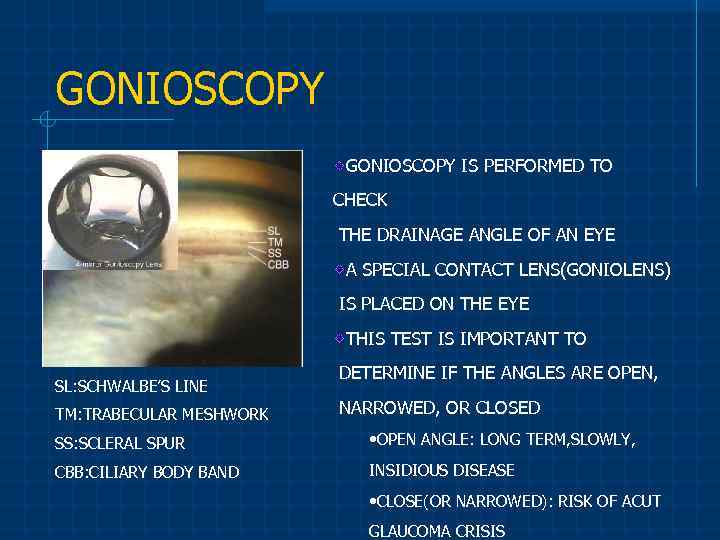 GONIOSCOPY IS PERFORMED TO CHECK THE DRAINAGE ANGLE OF AN EYE A SPECIAL CONTACT LENS(GONIOLENS) IS PLACED ON THE EYE THIS TEST IS IMPORTANT TO SL: SCHWALBE’S LINE TM: TRABECULAR MESHWORK DETERMINE IF THE ANGLES ARE OPEN, NARROWED, OR CLOSED SS: SCLERAL SPUR • OPEN ANGLE: LONG TERM, SLOWLY, CBB: CILIARY BODY BAND INSIDIOUS DISEASE • CLOSE(OR NARROWED): RISK OF ACUT GLAUCOMA CRISIS
GONIOSCOPY IS PERFORMED TO CHECK THE DRAINAGE ANGLE OF AN EYE A SPECIAL CONTACT LENS(GONIOLENS) IS PLACED ON THE EYE THIS TEST IS IMPORTANT TO SL: SCHWALBE’S LINE TM: TRABECULAR MESHWORK DETERMINE IF THE ANGLES ARE OPEN, NARROWED, OR CLOSED SS: SCLERAL SPUR • OPEN ANGLE: LONG TERM, SLOWLY, CBB: CILIARY BODY BAND INSIDIOUS DISEASE • CLOSE(OR NARROWED): RISK OF ACUT GLAUCOMA CRISIS
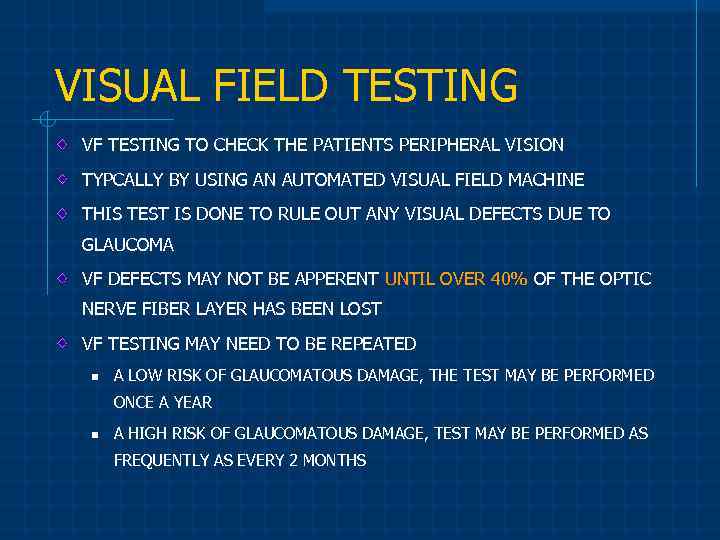 VISUAL FIELD TESTING VF TESTING TO CHECK THE PATIENTS PERIPHERAL VISION TYPCALLY BY USING AN AUTOMATED VISUAL FIELD MACHINE THIS TEST IS DONE TO RULE OUT ANY VISUAL DEFECTS DUE TO GLAUCOMA VF DEFECTS MAY NOT BE APPERENT UNTIL OVER 40% OF THE OPTIC NERVE FIBER LAYER HAS BEEN LOST VF TESTING MAY NEED TO BE REPEATED n A LOW RISK OF GLAUCOMATOUS DAMAGE, THE TEST MAY BE PERFORMED ONCE A YEAR n A HIGH RISK OF GLAUCOMATOUS DAMAGE, TEST MAY BE PERFORMED AS FREQUENTLY AS EVERY 2 MONTHS
VISUAL FIELD TESTING VF TESTING TO CHECK THE PATIENTS PERIPHERAL VISION TYPCALLY BY USING AN AUTOMATED VISUAL FIELD MACHINE THIS TEST IS DONE TO RULE OUT ANY VISUAL DEFECTS DUE TO GLAUCOMA VF DEFECTS MAY NOT BE APPERENT UNTIL OVER 40% OF THE OPTIC NERVE FIBER LAYER HAS BEEN LOST VF TESTING MAY NEED TO BE REPEATED n A LOW RISK OF GLAUCOMATOUS DAMAGE, THE TEST MAY BE PERFORMED ONCE A YEAR n A HIGH RISK OF GLAUCOMATOUS DAMAGE, TEST MAY BE PERFORMED AS FREQUENTLY AS EVERY 2 MONTHS
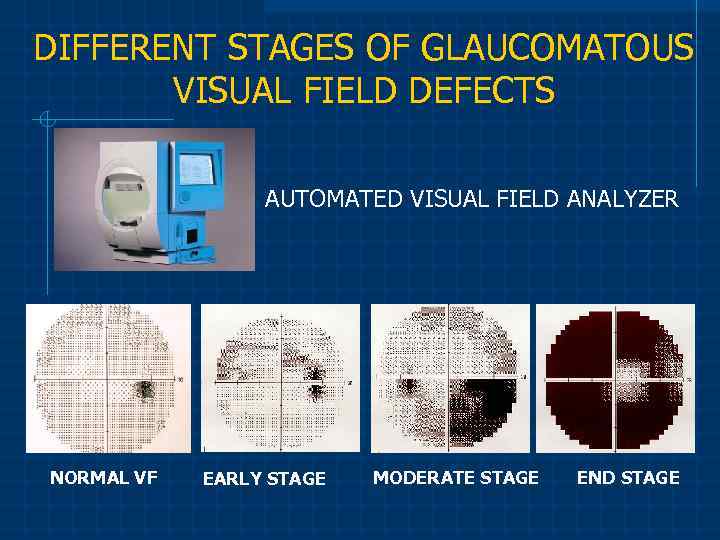 DIFFERENT STAGES OF GLAUCOMATOUS VISUAL FIELD DEFECTS AUTOMATED VISUAL FIELD ANALYZER NORMAL VF EARLY STAGE MODERATE STAGE END STAGE
DIFFERENT STAGES OF GLAUCOMATOUS VISUAL FIELD DEFECTS AUTOMATED VISUAL FIELD ANALYZER NORMAL VF EARLY STAGE MODERATE STAGE END STAGE
 OPTIC NERVE HEAD EXAMINATION EACH OPTIC NERVE HEAD IS EXAMINED FOR ANY DAMAGE OR ABNORMALITIES THIS MAY REQUIRE DILATION OF THE PUPILS TO ENSURE AN ADEQUATE EXAMINATION OF THE OPTIC NERVES FUNDUS PHOTOGRAPHS, WHICH ARE PICTURES OF YOUR OPTIC DISC ARE TAKEN FOR FUTURE REFERENCE AND COMPARISON DIFFERENT IMAGING STUDIES MAY BE CONDUCTED TO DOCUMENT THE STATUS OF OPTIC NERVE AND TO DETECT CHANGES OVER TIME
OPTIC NERVE HEAD EXAMINATION EACH OPTIC NERVE HEAD IS EXAMINED FOR ANY DAMAGE OR ABNORMALITIES THIS MAY REQUIRE DILATION OF THE PUPILS TO ENSURE AN ADEQUATE EXAMINATION OF THE OPTIC NERVES FUNDUS PHOTOGRAPHS, WHICH ARE PICTURES OF YOUR OPTIC DISC ARE TAKEN FOR FUTURE REFERENCE AND COMPARISON DIFFERENT IMAGING STUDIES MAY BE CONDUCTED TO DOCUMENT THE STATUS OF OPTIC NERVE AND TO DETECT CHANGES OVER TIME
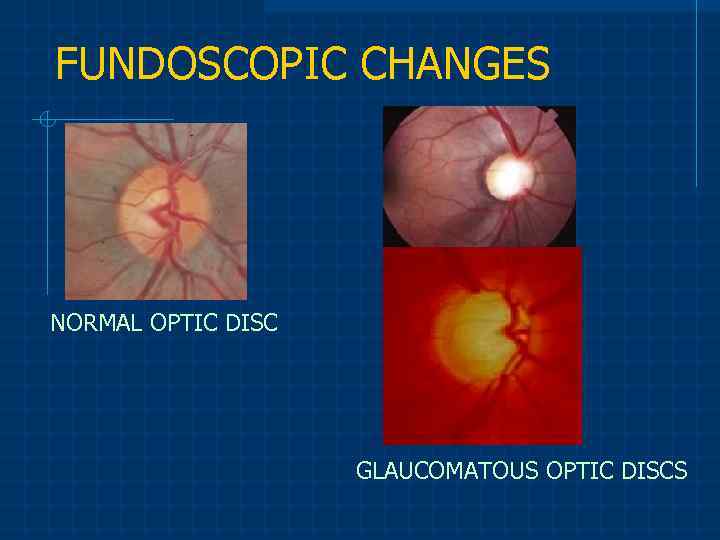 FUNDOSCOPIC CHANGES NORMAL OPTIC DISC GLAUCOMATOUS OPTIC DISCS
FUNDOSCOPIC CHANGES NORMAL OPTIC DISC GLAUCOMATOUS OPTIC DISCS
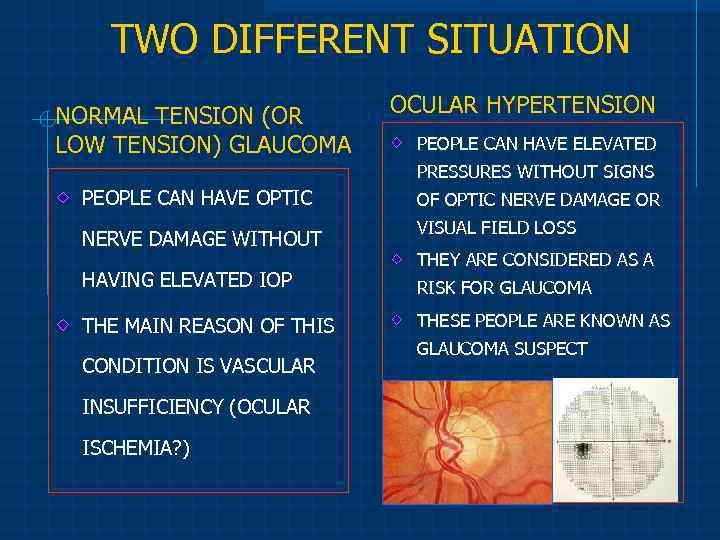 TWO DIFFERENT SITUATION NORMAL TENSION (OR OCULAR HYPERTENSION PEOPLE CAN HAVE ELEVATED LOW TENSION) GLAUCOMA PRESSURES WITHOUT SIGNS PEOPLE CAN HAVE OPTIC NERVE DAMAGE WITHOUT HAVING ELEVATED IOP THE MAIN REASON OF THIS CONDITION IS VASCULAR INSUFFICIENCY (OCULAR ISCHEMIA? ) OF OPTIC NERVE DAMAGE OR VISUAL FIELD LOSS THEY ARE CONSIDERED AS A RISK FOR GLAUCOMA THESE PEOPLE ARE KNOWN AS GLAUCOMA SUSPECT
TWO DIFFERENT SITUATION NORMAL TENSION (OR OCULAR HYPERTENSION PEOPLE CAN HAVE ELEVATED LOW TENSION) GLAUCOMA PRESSURES WITHOUT SIGNS PEOPLE CAN HAVE OPTIC NERVE DAMAGE WITHOUT HAVING ELEVATED IOP THE MAIN REASON OF THIS CONDITION IS VASCULAR INSUFFICIENCY (OCULAR ISCHEMIA? ) OF OPTIC NERVE DAMAGE OR VISUAL FIELD LOSS THEY ARE CONSIDERED AS A RISK FOR GLAUCOMA THESE PEOPLE ARE KNOWN AS GLAUCOMA SUSPECT
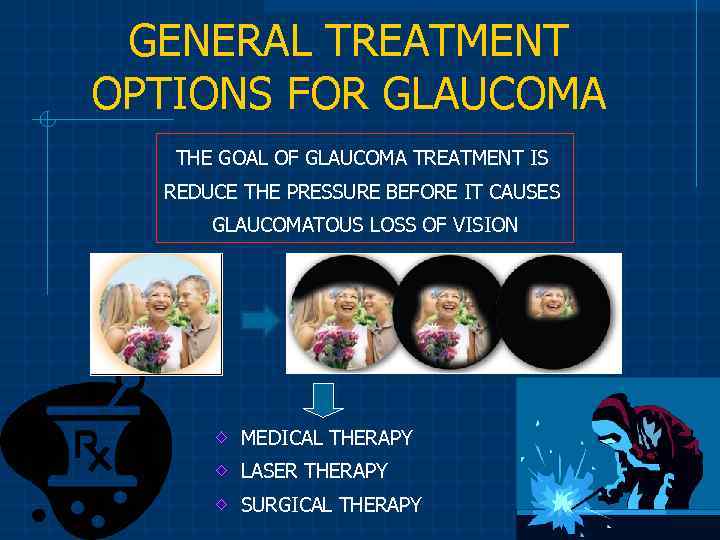 GENERAL TREATMENT OPTIONS FOR GLAUCOMA THE GOAL OF GLAUCOMA TREATMENT IS REDUCE THE PRESSURE BEFORE IT CAUSES GLAUCOMATOUS LOSS OF VISION MEDICAL THERAPY LASER THERAPY SURGICAL THERAPY
GENERAL TREATMENT OPTIONS FOR GLAUCOMA THE GOAL OF GLAUCOMA TREATMENT IS REDUCE THE PRESSURE BEFORE IT CAUSES GLAUCOMATOUS LOSS OF VISION MEDICAL THERAPY LASER THERAPY SURGICAL THERAPY
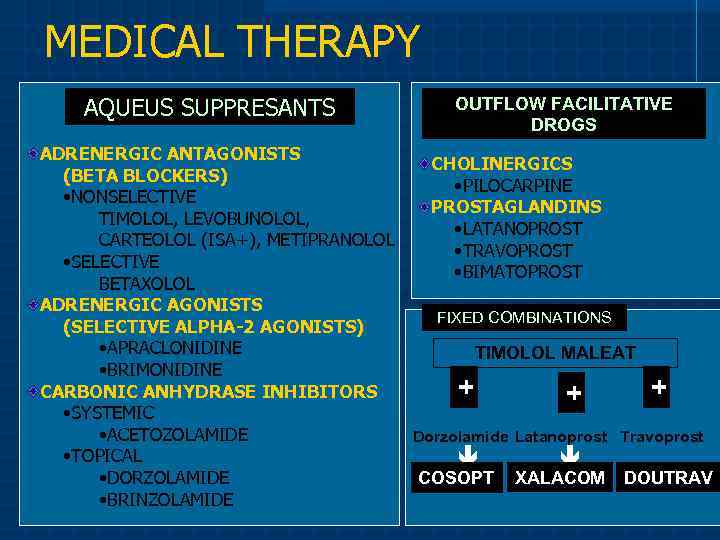 MEDICAL THERAPY AQUEUS SUPPRESANTS OUTFLOW FACILITATIVE DROGS ADRENERGIC ANTAGONISTS CHOLINERGICS (BETA BLOCKERS) • PILOCARPINE • NONSELECTIVE PROSTAGLANDINS TIMOLOL, LEVOBUNOLOL, • LATANOPROST CARTEOLOL (ISA+), METIPRANOLOL • TRAVOPROST • SELECTIVE • BIMATOPROST BETAXOLOL ADRENERGIC AGONISTS FIXED COMBINATIONS (SELECTIVE ALPHA-2 AGONISTS) • APRACLONIDINE TIMOLOL MALEAT • BRIMONIDINE + + CARBONIC ANHYDRASE INHIBITORS + • SYSTEMIC • ACETOZOLAMIDE Dorzolamide Latanoprost Travoprost • TOPICAL COSOPT XALACOM DOUTRAV • DORZOLAMIDE • BRINZOLAMIDE
MEDICAL THERAPY AQUEUS SUPPRESANTS OUTFLOW FACILITATIVE DROGS ADRENERGIC ANTAGONISTS CHOLINERGICS (BETA BLOCKERS) • PILOCARPINE • NONSELECTIVE PROSTAGLANDINS TIMOLOL, LEVOBUNOLOL, • LATANOPROST CARTEOLOL (ISA+), METIPRANOLOL • TRAVOPROST • SELECTIVE • BIMATOPROST BETAXOLOL ADRENERGIC AGONISTS FIXED COMBINATIONS (SELECTIVE ALPHA-2 AGONISTS) • APRACLONIDINE TIMOLOL MALEAT • BRIMONIDINE + + CARBONIC ANHYDRASE INHIBITORS + • SYSTEMIC • ACETOZOLAMIDE Dorzolamide Latanoprost Travoprost • TOPICAL COSOPT XALACOM DOUTRAV • DORZOLAMIDE • BRINZOLAMIDE
 LASER THERAPY LASER TRABECULOPLASTY n ARGON LASER TRABECULOPLASTY (ARGON LASER) n SELECTIVE LASER TRABECULOPLASTY (ND: YAG) ARGON LASER TRABECULOPLASTY CYCLOPHOTOCOAGULATION n TRANSSCLERAL (ND: YAG, DIODE) n TRANSPUPILLARY (ARGON) n TRANSVITREAL (DURING VITRECTOMY) n ENDOSCOPIC (ARGON) DIODE LASER TRANSSCLERAL CYCLOPHOTOCOAGULATION
LASER THERAPY LASER TRABECULOPLASTY n ARGON LASER TRABECULOPLASTY (ARGON LASER) n SELECTIVE LASER TRABECULOPLASTY (ND: YAG) ARGON LASER TRABECULOPLASTY CYCLOPHOTOCOAGULATION n TRANSSCLERAL (ND: YAG, DIODE) n TRANSPUPILLARY (ARGON) n TRANSVITREAL (DURING VITRECTOMY) n ENDOSCOPIC (ARGON) DIODE LASER TRANSSCLERAL CYCLOPHOTOCOAGULATION
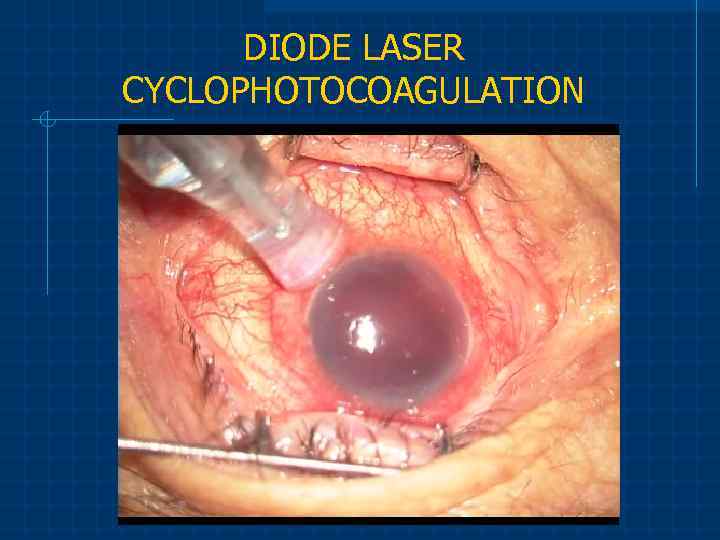 DIODE LASER CYCLOPHOTOCOAGULATION
DIODE LASER CYCLOPHOTOCOAGULATION
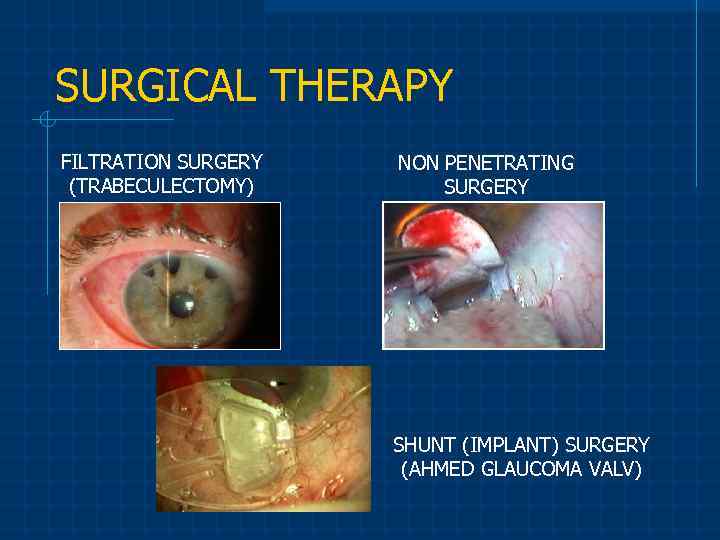 SURGICAL THERAPY FILTRATION SURGERY (TRABECULECTOMY) NON PENETRATING SURGERY SHUNT (IMPLANT) SURGERY (AHMED GLAUCOMA VALV)
SURGICAL THERAPY FILTRATION SURGERY (TRABECULECTOMY) NON PENETRATING SURGERY SHUNT (IMPLANT) SURGERY (AHMED GLAUCOMA VALV)
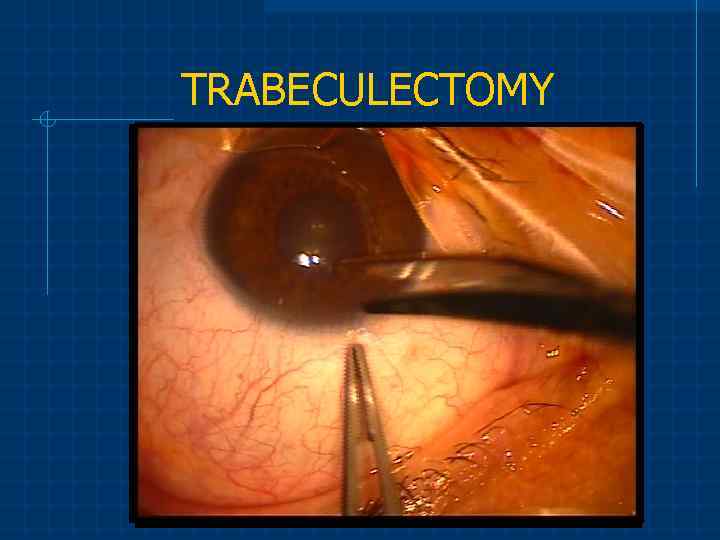 TRABECULECTOMY
TRABECULECTOMY
 What can I do to minimize risk to my baby? Work with your eye doctor. The first three months of pregnancy, when most of the infant’s organs initially form, are especially critical. It is important to get your eye doctor involved as early as possible in order to plan the best treatment regimen for your pregnancy. It is even better if you can let your eye doctor know if you are planning to conceive. That way, a medication regimen can be planned or adjusted even before the baby is conceived.
What can I do to minimize risk to my baby? Work with your eye doctor. The first three months of pregnancy, when most of the infant’s organs initially form, are especially critical. It is important to get your eye doctor involved as early as possible in order to plan the best treatment regimen for your pregnancy. It is even better if you can let your eye doctor know if you are planning to conceive. That way, a medication regimen can be planned or adjusted even before the baby is conceived.
 Used references Morozov VI, Yakovlev AA Pharmacotherapy Eye Diseases: A Handbook. - Ed. 4 th. - M. : Medicine, 2001. - 472 b. Nesterov AP Glaucoma M. : Medicine, 1995. Shkarlova SI Glaucoma and cataracts. A series of "Medicine for you. " Rostov N / A: Phoenix, 2001. - 192 s. The information posted on the website: (http: //www. vision-ua. com/); (http: //www. eyenews. ru/).
Used references Morozov VI, Yakovlev AA Pharmacotherapy Eye Diseases: A Handbook. - Ed. 4 th. - M. : Medicine, 2001. - 472 b. Nesterov AP Glaucoma M. : Medicine, 1995. Shkarlova SI Glaucoma and cataracts. A series of "Medicine for you. " Rostov N / A: Phoenix, 2001. - 192 s. The information posted on the website: (http: //www. vision-ua. com/); (http: //www. eyenews. ru/).


