5a7da0934806d9495d87c4d8b8fe8edf.ppt
- Количество слайдов: 42
Get Covered Kentucky The Affordable Care Act: What It Means for Kentuckians Erin Hoben, Esq.
Outline Part 1 – The Big Picture: Understanding the Affordable Care Act (A. C. A. ) Part 2 – Gaining Perspective: Kentucky and the A. C. A. Part 3 – The Nuts and Bolts: Getting Covered with Kynect Part 4 – Truths about the Affordable Care Act
Part I Understanding the Affordable Care Act 1) On a scale of one to ten, how would you rate your overall level of comfort explaining the Affordable Care Act to others? 2) Approximately how many Kentuckians currently lack health insurance? a) 310, 000 b) 460, 000 c) 550, 000 d) 640, 000
Supreme Court The ACA was challenged in the Supreme Court in March 2012 and was upheld in June 2012 The Supreme Court upheld the ACA in its entirety, except for the provision requiring states to expand Medicaid or lose federal funding States were then able to choose whether or not they would expand Medicaid for their residents 26 states have decided to expand
Affordable Care Act (ACA) Establishes a marketplace for individuals, families and small businesses to purchase affordable and quality healthcare, called Exchanges Kentucky is operating a state-based exchange, known as the Kentucky Health Benefit Exchange (KHBE) Beginning in 2014, individuals and large employers will be required to purchase insurance or pay a penalty
ACA Timeline: Current Provisions Progress toward closing of the Medicare donut hole Tax credits to small businesses with up to 25 employees Pre-existing condition insurance plan Assistance to employers providing coverage to retirees over age 55 Young adults can remain on parents insurance up to age 26 Covered preventive services on new health plans Increase in payments to rural health providers Funding for community health centers Increase in payments to primary care providers (2013)
ACA Timeline: Current Provisions Health insurers are prohibited from: Denying coverage to children because of pre-existing conditions Placing lifetime dollar limits on coverage Dropping people from health coverage when they get sick Health insurers must spend at least 80% of the premiums they collect on medical services or give customer rebates
Preventive Care Private health plans are required to cover preventive services without any costsharing By eliminating cost-sharing for preventive services, it reduces barriers to prevention for low-income communities An estimated 975, 000 Kentuckians with private health insurance have received preventive care without having to pay any out-of-pockets costs
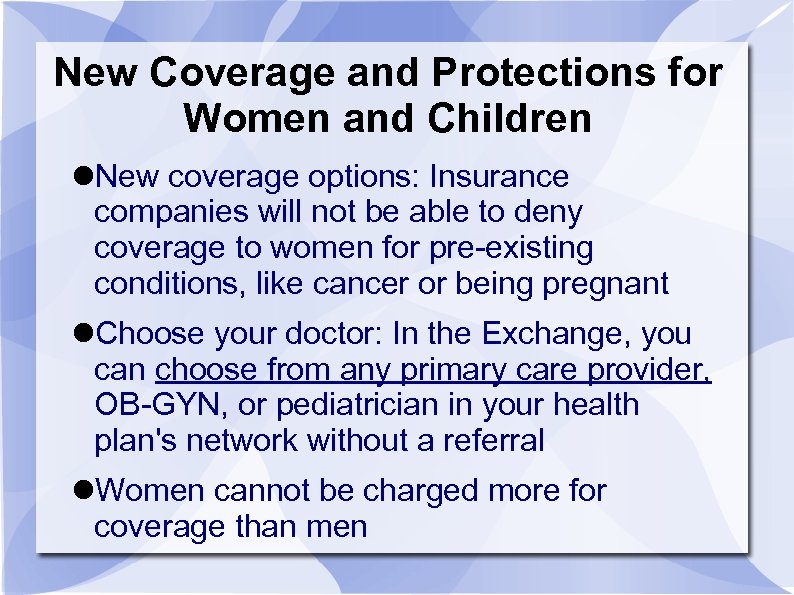
New Coverage and Protections for Women and Children New coverage options: Insurance companies will not be able to deny coverage to women for pre-existing conditions, like cancer or being pregnant Choose your doctor: In the Exchange, you can choose from any primary care provider, OB-GYN, or pediatrician in your health plan's network without a referral Women cannot be charged more for coverage than men
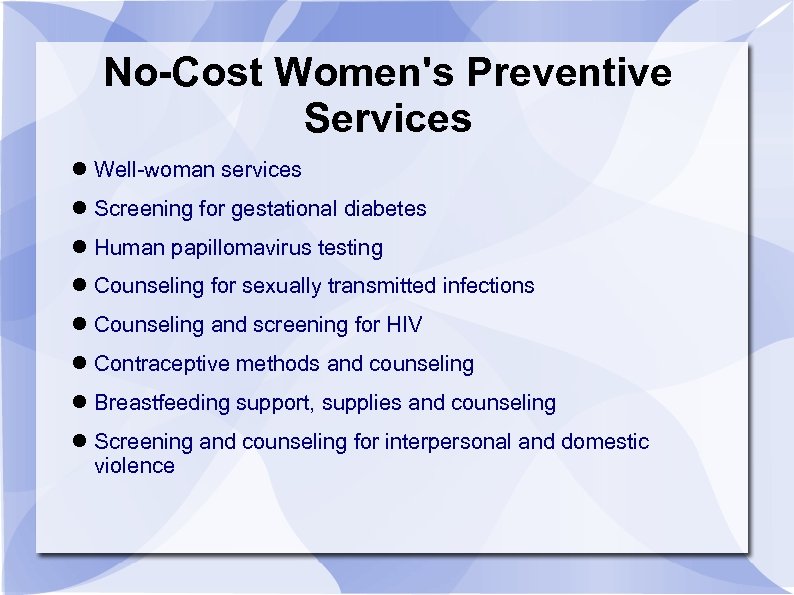
No-Cost Women's Preventive Services Well-woman services Screening for gestational diabetes Human papillomavirus testing Counseling for sexually transmitted infections Counseling and screening for HIV Contraceptive methods and counseling Breastfeeding support, supplies and counseling Screening and counseling for interpersonal and domestic violence
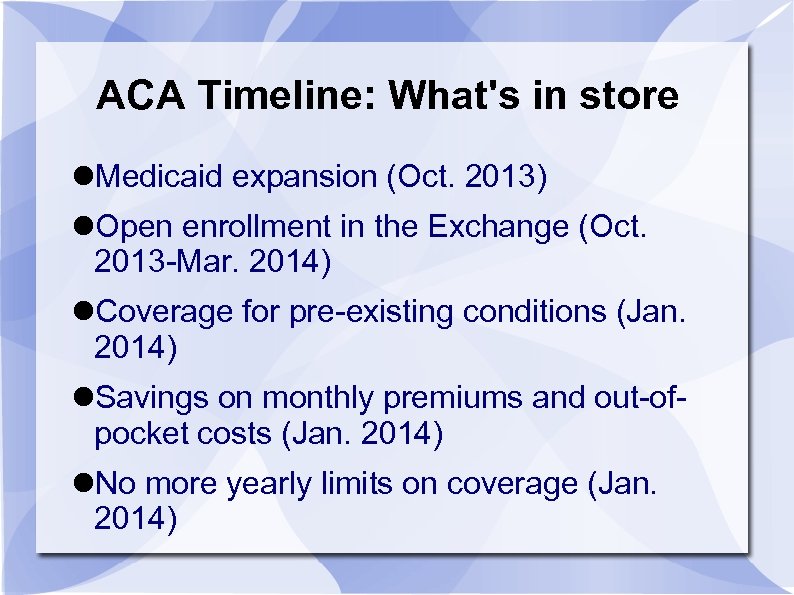
ACA Timeline: What's in store Medicaid expansion (Oct. 2013) Open enrollment in the Exchange (Oct. 2013 -Mar. 2014) Coverage for pre-existing conditions (Jan. 2014) Savings on monthly premiums and out-ofpocket costs (Jan. 2014) No more yearly limits on coverage (Jan. 2014)
Part 2 Kentucky and the Affordable Care Act
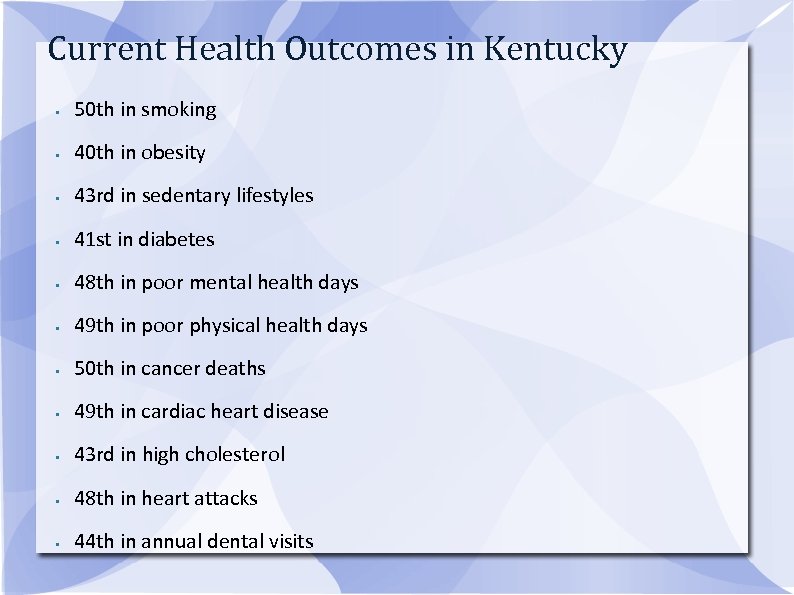
Current Health Outcomes in Kentucky • 50 th in smoking • 40 th in obesity • 43 rd in sedentary lifestyles • 41 st in diabetes • 48 th in poor mental health days • 49 th in poor physical health days • 50 th in cancer deaths • 49 th in cardiac heart disease • 43 rd in high cholesterol • 48 th in heart attacks • 44 th in annual dental visits
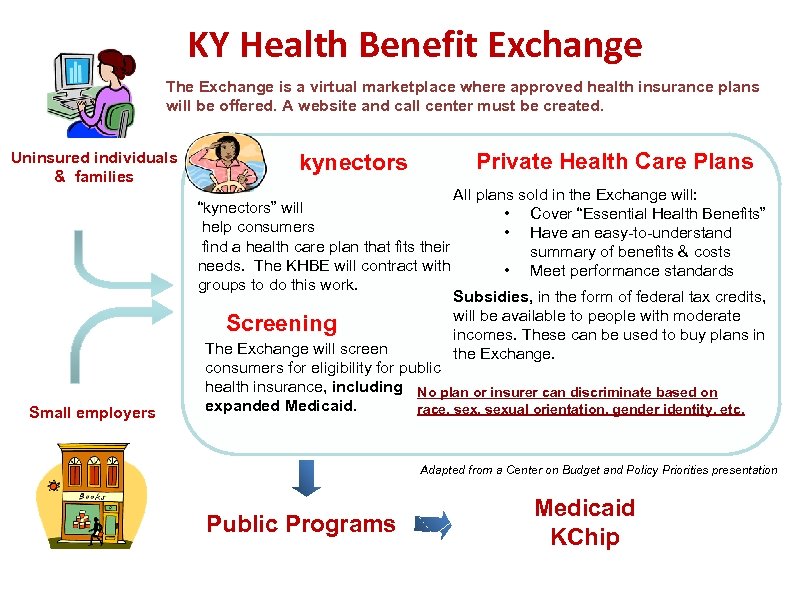
KY Health Benefit Exchange The Exchange is a virtual marketplace where approved health insurance plans will be offered. A website and call center must be created. Uninsured individuals & families Small employers kynectors Private Health Care Plans All plans sold in the Exchange will: “kynectors” will • Cover “Essential Health Benefits” help consumers • Have an easy-to-understand find a health care plan that fits their summary of benefits & costs needs. The KHBE will contract with • Meet performance standards groups to do this work. Subsidies, in the form of federal tax credits, will be available to people with moderate Screening incomes. These can be used to buy plans in The Exchange will screen the Exchange. consumers for eligibility for public health insurance, including No plan or insurer can discriminate based on expanded Medicaid. race, sexual orientation, gender identity, etc. Adapted from a Center on Budget and Policy Priorities presentation Public Programs Medicaid KChip
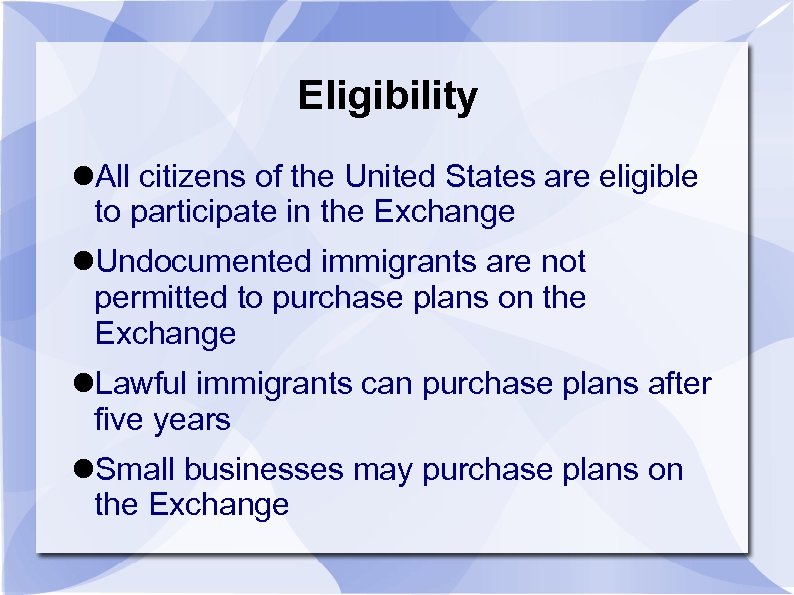
Eligibility All citizens of the United States are eligible to participate in the Exchange Undocumented immigrants are not permitted to purchase plans on the Exchange Lawful immigrants can purchase plans after five years Small businesses may purchase plans on the Exchange
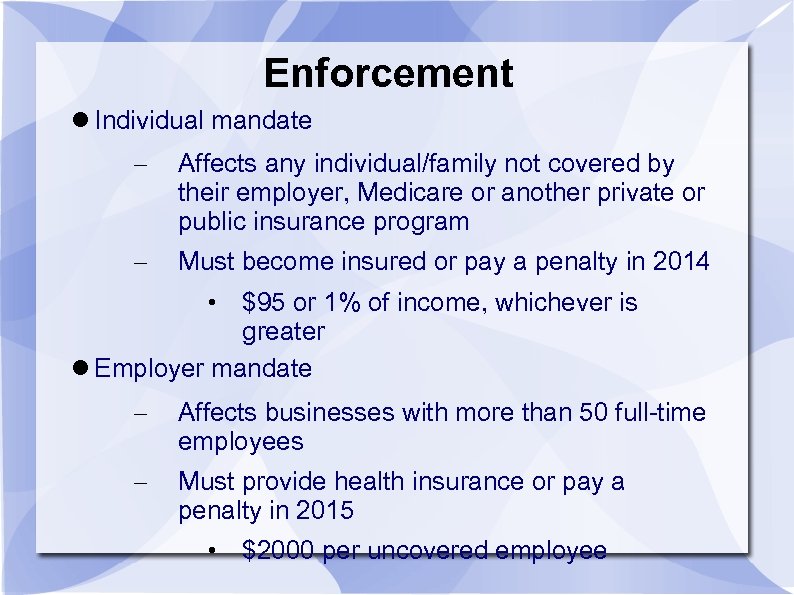
Enforcement Individual mandate – Affects any individual/family not covered by their employer, Medicare or another private or public insurance program – Must become insured or pay a penalty in 2014 • $95 or 1% of income, whichever is greater Employer mandate – Affects businesses with more than 50 full-time employees – Must provide health insurance or pay a penalty in 2015 • $2000 per uncovered employee
Medicaid Expansion
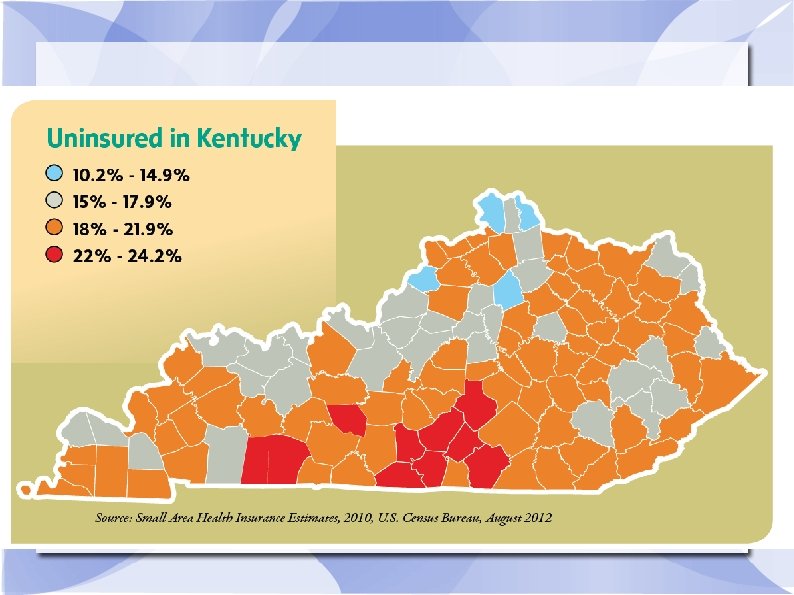
Medicaid Expansion Governor Beshear signed an executive order to expand Medicaid on May 9, 2013 Sets a floor of 138% FPL for eligibility Over 300, 000 people in Kentucky will benefit from the expansion Kentucky will benefit more than any other state, with 57% of its uninsured population becoming eligible under the expansion
Medicaid Expansion The federal government will pay an enhanced federal funds participation (FFP) rate to states who expand Medicaid Currently, the FFP rate in Kentucky is 70%, with Kentucky paying 30% of the costs Under expansion, the FFP rate will be 100% and will phase out to 90% in 2020 This will enable Kentucky to provide coverage to both newly eligibles and those who enroll as a result of the “woodwork” effect
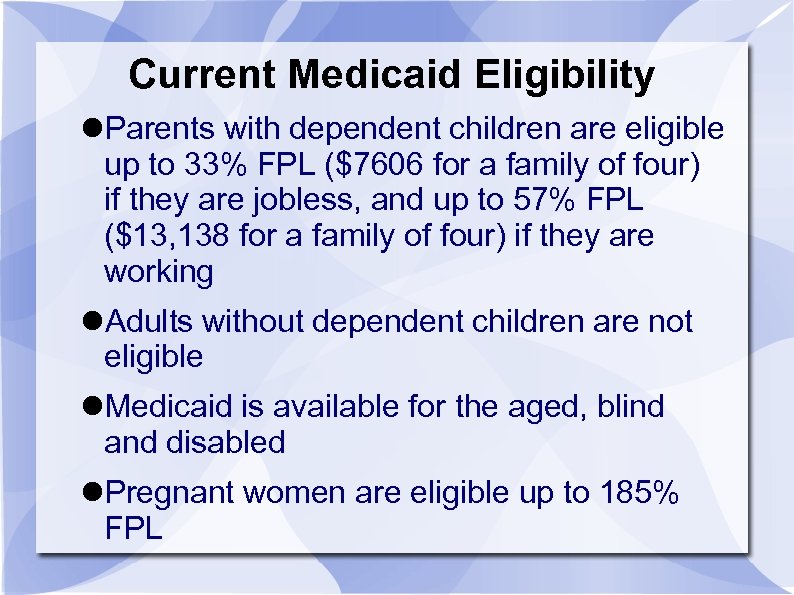
Current Medicaid Eligibility Parents with dependent children are eligible up to 33% FPL ($7606 for a family of four) if they are jobless, and up to 57% FPL ($13, 138 for a family of four) if they are working Adults without dependent children are not eligible Medicaid is available for the aged, blind and disabled Pregnant women are eligible up to 185% FPL
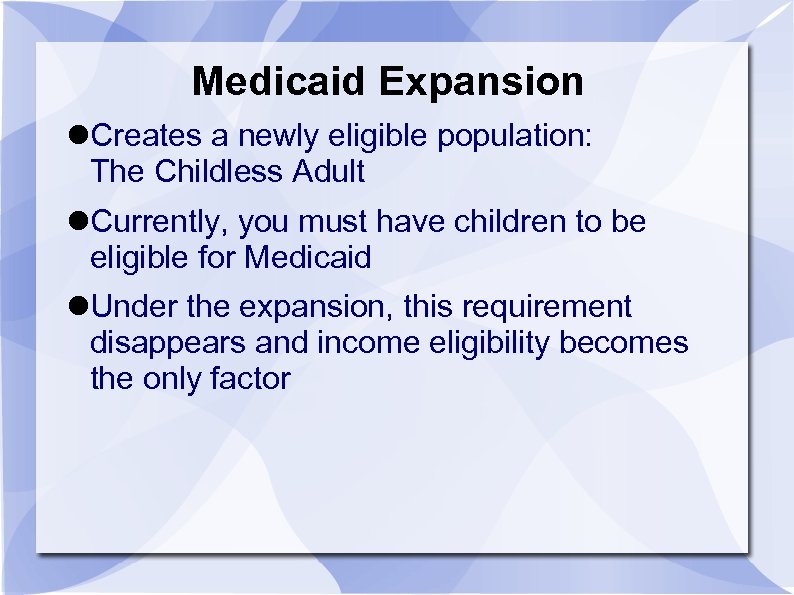
Medicaid Expansion Creates a newly eligible population: The Childless Adult Currently, you must have children to be eligible for Medicaid Under the expansion, this requirement disappears and income eligibility becomes the only factor
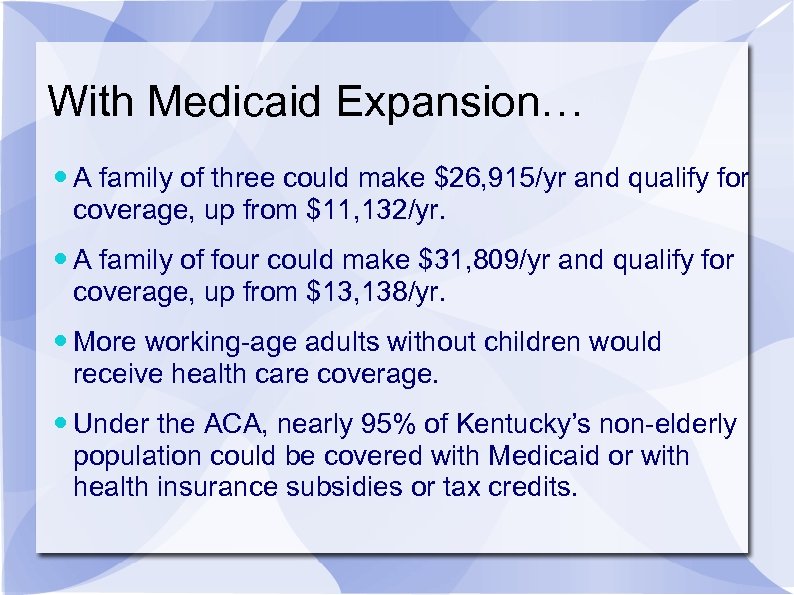
With Medicaid Expansion… A family of three could make $26, 915/yr and qualify for coverage, up from $11, 132/yr. A family of four could make $31, 809/yr and qualify for coverage, up from $13, 138/yr. More working-age adults without children would receive health care coverage. Under the ACA, nearly 95% of Kentucky’s non-elderly population could be covered with Medicaid or with health insurance subsidies or tax credits.
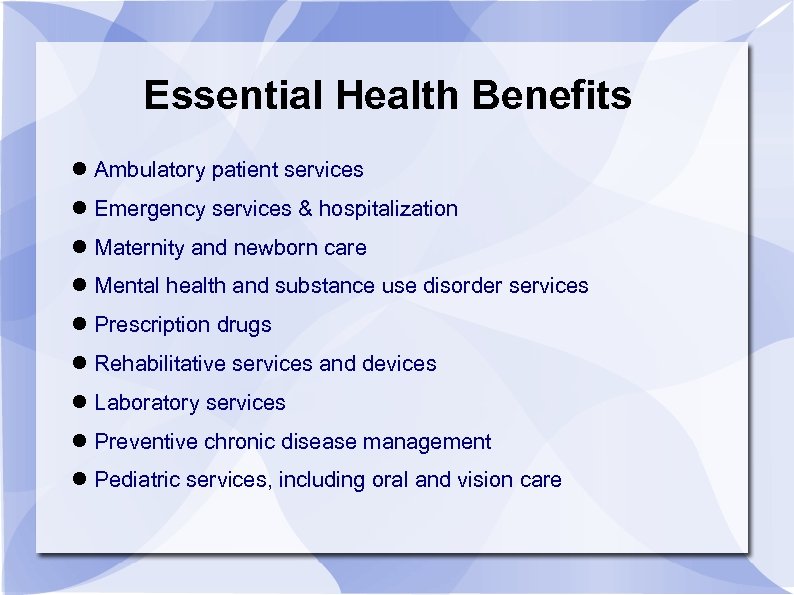
Essential Health Benefits Ambulatory patient services Emergency services & hospitalization Maternity and newborn care Mental health and substance use disorder services Prescription drugs Rehabilitative services and devices Laboratory services Preventive chronic disease management Pediatric services, including oral and vision care
Part 3 How to get coverage in Kentucky
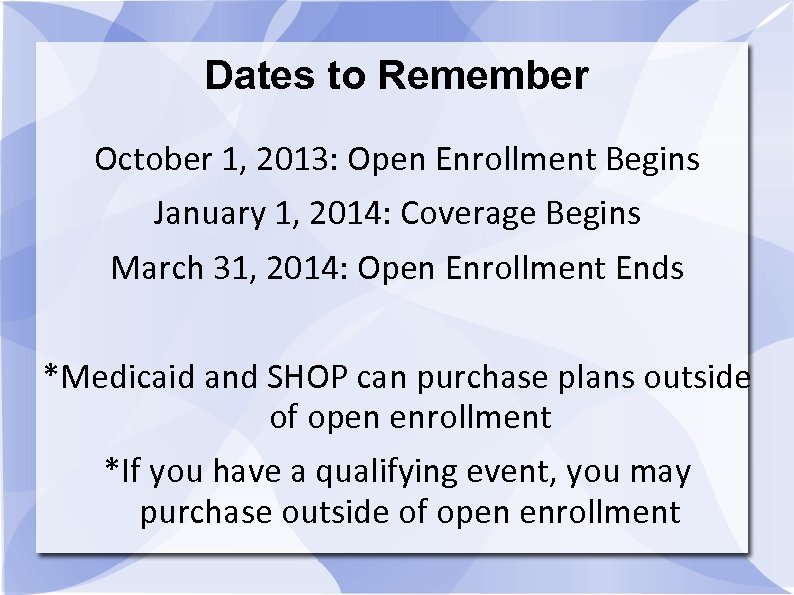
Dates to Remember October 1, 2013: Open Enrollment Begins January 1, 2014: Coverage Begins March 31, 2014: Open Enrollment Ends *Medicaid and SHOP can purchase plans outside of open enrollment *If you have a qualifying event, you may purchase outside of open enrollment
Kentucky Health Benefit Exchange: kynect Marketplace where Kentuckians can purchase insurance Travelocity for health insurance Allows consumers to compare and choose plans Promotes competition All insurance affordability programs will be accessed using kynect
The “Exchange Population” This term has been used to describe people who earn too much to qualify for Medicaid, but cannot afford to purchase private health insurance without government assistance Subsidies are available to this group between 138% and 400% FPL They will receive premium assistance in the form of tax credits
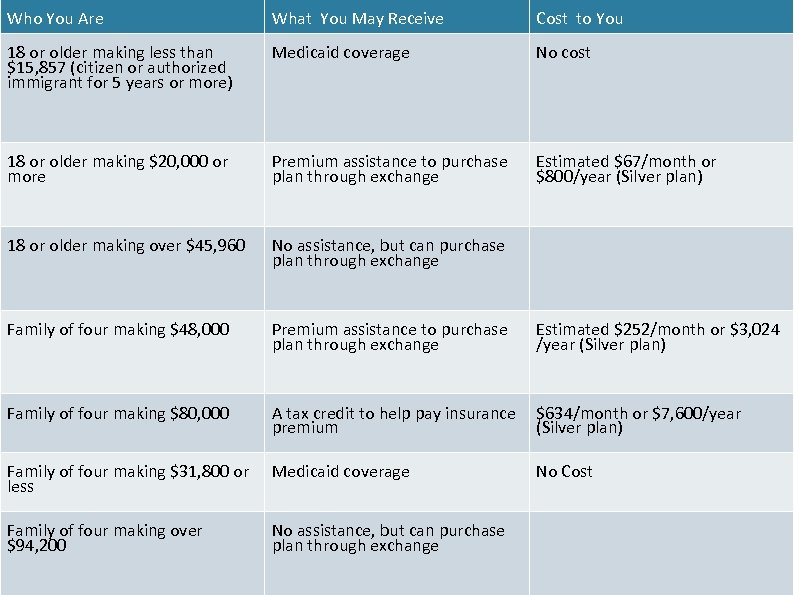
Who You Are What You May Receive Cost to You 18 or older making less than $15, 857 (citizen or authorized immigrant for 5 years or more) Medicaid coverage No cost 18 or older making $20, 000 or more Premium assistance to purchase plan through exchange Estimated $67/month or $800/year (Silver plan) 18 or older making over $45, 960 No assistance, but can purchase plan through exchange Family of four making $48, 000 Premium assistance to purchase plan through exchange Estimated $252/month or $3, 024 /year (Silver plan) Family of four making $80, 000 A tax credit to help pay insurance premium $634/month or $7, 600/year (Silver plan) Family of four making $31, 800 or less Medicaid coverage No Cost Family of four making over $94, 200 No assistance, but can purchase plan through exchange
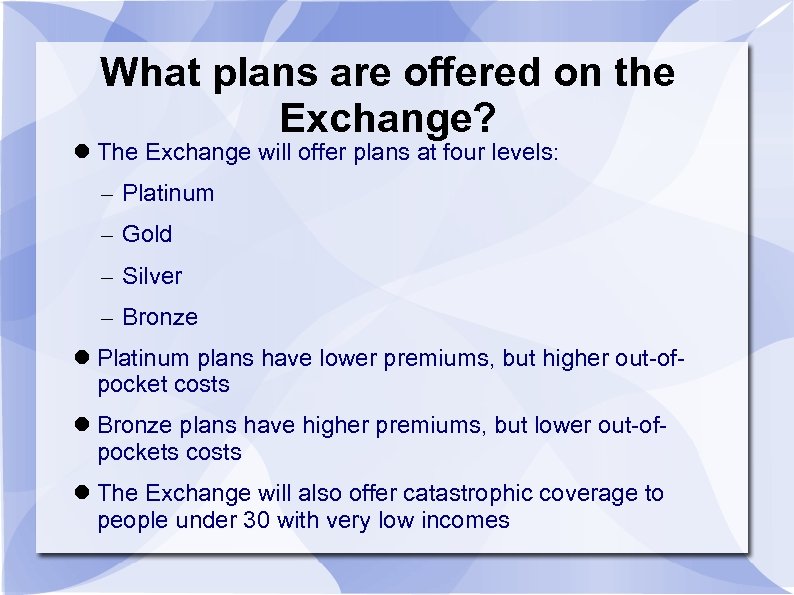
What plans are offered on the Exchange? The Exchange will offer plans at four levels: – Platinum – Gold – Silver – Bronze Platinum plans have lower premiums, but higher out-ofpocket costs Bronze plans have higher premiums, but lower out-ofpockets costs The Exchange will also offer catastrophic coverage to people under 30 with very low incomes
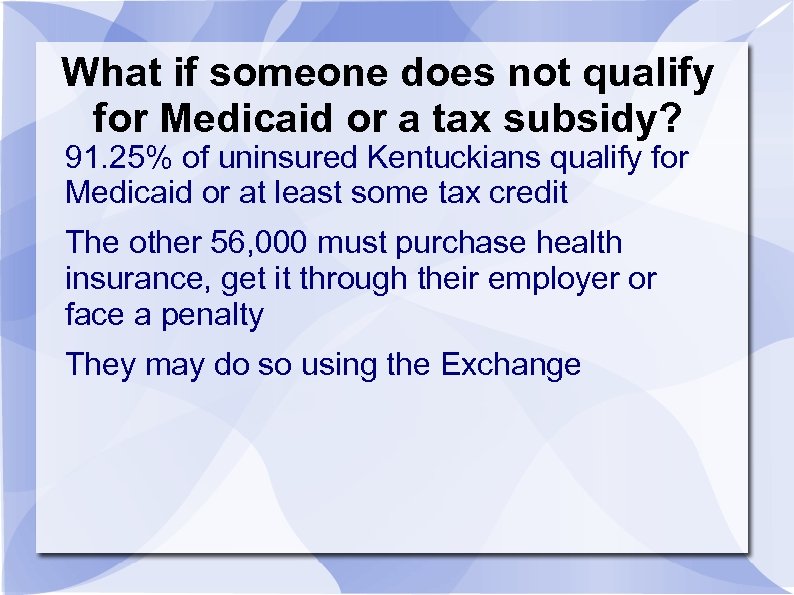
What if someone does not qualify for Medicaid or a tax subsidy? 91. 25% of uninsured Kentuckians qualify for Medicaid or at least some tax credit The other 56, 000 must purchase health insurance, get it through their employer or face a penalty They may do so using the Exchange
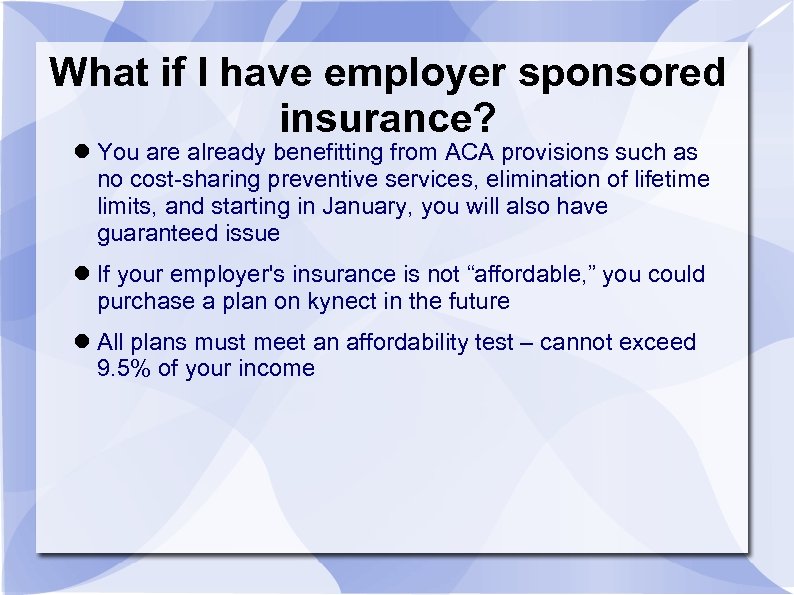
What if I have employer sponsored insurance? You are already benefitting from ACA provisions such as no cost-sharing preventive services, elimination of lifetime limits, and starting in January, you will also have guaranteed issue If your employer's insurance is not “affordable, ” you could purchase a plan on kynect in the future All plans must meet an affordability test – cannot exceed 9. 5% of your income
Okay, let's get everyone enrolled! Open enrollment begins October 1, 2013 and is available through March 31, 2014 Individuals can sign up: Online using kynect. ky. gov Over the phone by calling 1 -855 -4 kynect By visiting a kynector By mailing in their application
kynectors The ACA includes a provision to allow for states to implement an in-person assister (IPA) or navigator program Kentucky has coined these assisters “kynectors” Guidelines: – Must provide public education about QHPs – Must distribute fair and impartial information – Will be able to facilitate enrollment – Must refer Kentuckians to a consumer assistance program or ombudsmen to resolve grievances – Must be culturally and linguistically competent

kynectors These will be existing community organizations They are funded through the state and will receive training in August 2013 The program will be comprehensive, ensuring coverage in all eight Medicaid regions throughout the state
Small Business Health Options Program (SHOP) Simplifies the process of buying health insurance for your small business Open enrollment begins October 1, 2013 Insurance plans cannot turn you down based on the health status of your employees or their dependents, even if they have pre-existing conditions Cannot charge you higher premiums for women, or increase your group's premium for employees with high medical costs These protections do not apply to grandfathered plans
Small Business Health Options Program (SHOP) There is a sliding scale tax credit of up to 35% of the employer's eligible premium expenses for tax years 2010 -2013 Currently, employers with 10 or fewer FTEs, paying annual wages of $25, 000 or less, qualify for the maximum credit if they offer coverage In 2014, the maximum tax credit increases to 50% of premium expenses and coverage MUST be purchased on kynect For tax-exempt employers, the same employee and wage requirements apply, but the maximum tax credit is 25% of eligible premium expenses for 2010 -2013, to 35% in 2014
Impact on Kentucky Medicaid expansion is estimated to create 17, 000 jobs annually Estimated economic impact of $15. 6 million through 2021 because of the federal government's assistance Will reduce enrollment in SSDI and SSI and incentivize those individuals to stay in the workforce Spillover effect of preventing absenteeism Allows workers to be mobile Stability and growth of small businesses
Part 4 ACA Truths
Truths about the ACA The Bill has withstood its legal challenges and has not been struck down, it is the law of the land. The government is not going to make me drop/change my existing coverage. Expanding Medicaid will benefit Kentucky's economy. Privacy protections are in place to ensure that our information is kept secure. kynect will offer robust and comprehensive health insurance options. Premiums on kynect will be more affordable than private health insurance sold on the individual market today. The ACA is puts consumer protections in place to benefit even those with employer-sponsored insurance.

Contact Information @Get. Covered. KY Facebook. com/getcoveredky www. getcovered-ky. org kvhmedicaidexpansion@gmail. com 502. 653. 9059
Useful Resources Official website of the Federal gov. : www. healthcare. gov Kaiser Family Foundation: http: //kff. org/health-reform/ Small Business Majority: www. smallbusinessmajority. org Families USA: www. familiesusa. org Kentucky Voices for Health: www. kyvoicesforhealth. org kynect: www. kynect. ky. gov Governor's White Paper on Medicaid Expansion: http: //governor. ky. gov/healthierky/Documents/Medicaid. Ex pansion. White. Paper. pdf
5a7da0934806d9495d87c4d8b8fe8edf.ppt