a81d11ea7b7b3bef2d604467c74eacc6.ppt
- Количество слайдов: 44
Gestational Diabetes By: Kevin Rabey
Gestational Diabetes is Carbohydrate Intolerance n n Begins/detected in pregnancy insulin resistance/hyperinsulinemia during pregnancy.
Gestational Diabetes n n Metabolic adaptations occur in normal pregnant women to ensure adequate fuel and nutrients to the fetus throughout the pregnancy Placental secretions of diabetogenic hormones help facilitate insulin resistance w growth hormone w corticotropin-releasing hormone w placental lactogen w progesterone
Prevalence United States prevalence is between 1. 4 and 14 % Higher in Black, Latino, Native American and Asian as compared to white women
Screening for Gestational Diabetes American Diabetic Association (ADA) American College of Obstetrics (ACOG) United States Preventative Service Task Force (USPSTF)
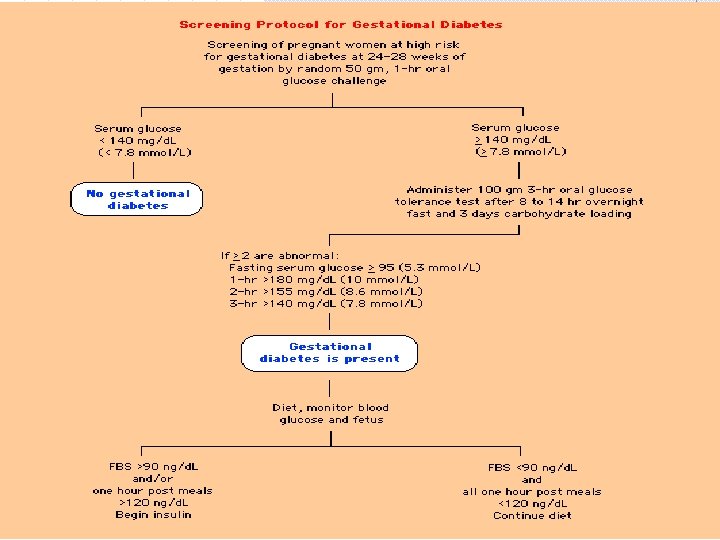
Screening At the Fourth International Workshop on Gestational Diabetes it was also recommended that further evaluation be conducted on any woman with: n n Random serum glucose >200 Fasting serum glucose >126
Screening Carbohydrate loading for 3 days prior to the OGTT has been recommended but is probably not necessary. should fast for 12 hours Universal Screening threshold of values for GCT and GTT
Effects of Gestational Diabetes Preeclampsia Fetal Macrosomia Operative Delivery Polyhydramnios Birth Trauma Perinatal Mortality Neonatal Metabolic Complications n n Hypoglycemia Hyperbilirubinemia Hypocalcemia Erythremia Development of obesity and diabetes in childhood

Treatment of Gestational Diabetes Diet and exercise Glucose Monitoring Insulin Therapy Oral Hypoglycemic agents
Diet Therapy Goals of an Effective diet n n Normoglycemia prevent ketosis adequate wt gain good fetal health Blood glucose concentrations fall about 20% during pregnancy n Average FBS in a pregnancy is 56 and 1 hour never exceeded 105
Diet Therapy FBS > 95 is high in pregnancy FBS >90 with normal GTT: Studies showed a higher risk of an infant with macrosomia Thus treatment with small elevations in sugar should be considered High maternal Glucose n n n fetal hyperglycemia increased fetal growth even in the absence of gestational diabetes
Diet Therapy Calorie Allotment: wt dependent at initial presentation (Kg/Day) n n 30 kcal 80 – 120% ideal body 24 kcal 120 – 150% ideal body 12 -15 kcal >150% ideal body 40 kcal < 80% of ideal body wt
Diet Therapy Calories: n n n Carbohydrate 40% Protein 20% Fat 40% (postprandial glucose) 75 to 80% gestational diabetes/glucose intolerance : normoglycemia Complex carbohydrates (starches/veget) nutrient dense: less effect on postprandial sugars then simple sugars
Diet Therapy Calorie distribution: n n n 3 meals and 3 snacks Over wt: 3 meals no snacks Breakfast: very small meal (10% total daily calories) Higher postprandial glucose significantly increase the risk of macrosomia Remaining calories: n n 30% lunch and dinner Remaining divided evenly between snacks
Glucose Monitoring Gestational diabetes/glucose intolerance n n n Measure glucose when wake in am (FBS) Measure 2 hours after each meal/snack Diet diary Two criteria to prevent macrosomia n n Fasting glucose <90 1 hour postprandial <120
Exercise Therapy Gestational Diabetes n n Type 2 diabetes unmasked in pregnancy exercise that diminishes peripheral resistance to insulin would be beneficial: cardiovascular conditioning increase affinity and receptor binding Reduction in both fasting and postprandial glucose n may decrease need for otherapies in Gestational Diabetes
Exercise Therapy Safety and Exercise in pregnancy n Increase CO and Bld volume n Exercise: divert oxygen and nutrients n Fetal bradycardia
Exercise Therapy Safe exercise does not cause n n fetal distress low birth wt uterine contractions maternal hypertension Teach woman to: n n n palpate their uterus for contractions cease exercise should they occur Avoid exercise in supine position
Exercise therapy Contraindications to exercise in Pregnancy n n n Preg-induced HTN Premature rupture of membranes Preterm labor Incompetent cervix Persistent second or third trimester bleeding Intra-uterine growth retardation
Exercise Therapy Exercises n walking seem the most appropriate Arm exercises against resistance are safe and effective n Study cardiovascular fitness program n
Insulin therapy Initiate insulin therapy when the following occur on 2 or more occasions in a 2 week period: (4 th international work shop GDM) n n Fasting glucose >90 1 hour postprandial >120 The ADA and ACOG use 95 fasting and 2 hour >120 Macrosomia decreased from 42% to 12% and C-Section decrease b/c of cephalopelvic dispropotion from 36% to 12%
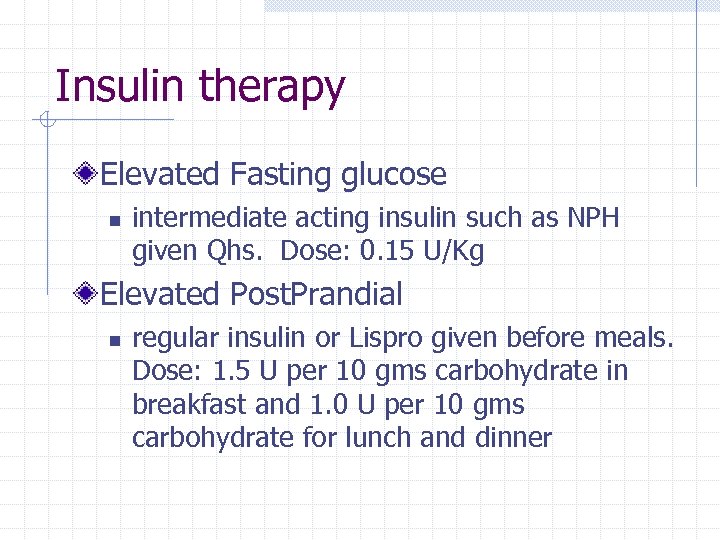
Insulin therapy Elevated Fasting glucose n intermediate acting insulin such as NPH given Qhs. Dose: 0. 15 U/Kg Elevated Post. Prandial n regular insulin or Lispro given before meals. Dose: 1. 5 U per 10 gms carbohydrate in breakfast and 1. 0 U per 10 gms carbohydrate for lunch and dinner
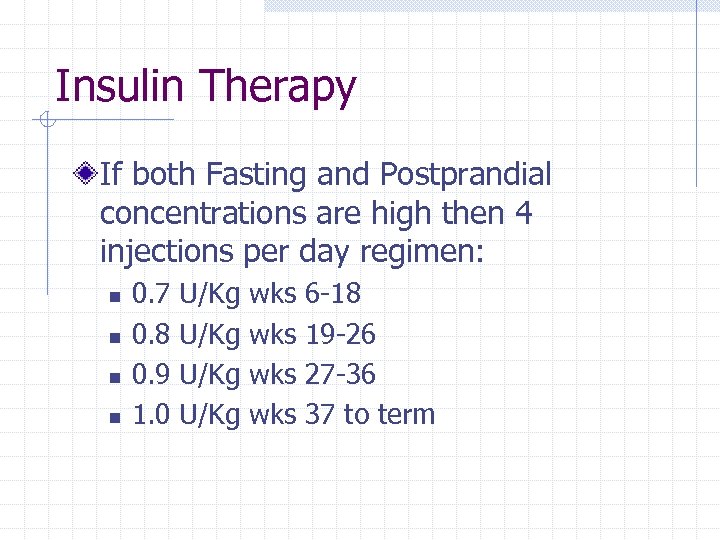
Insulin Therapy If both Fasting and Postprandial concentrations are high then 4 injections per day regimen: n n 0. 7 0. 8 0. 9 1. 0 U/Kg wks wks 6 -18 19 -26 27 -36 37 to term
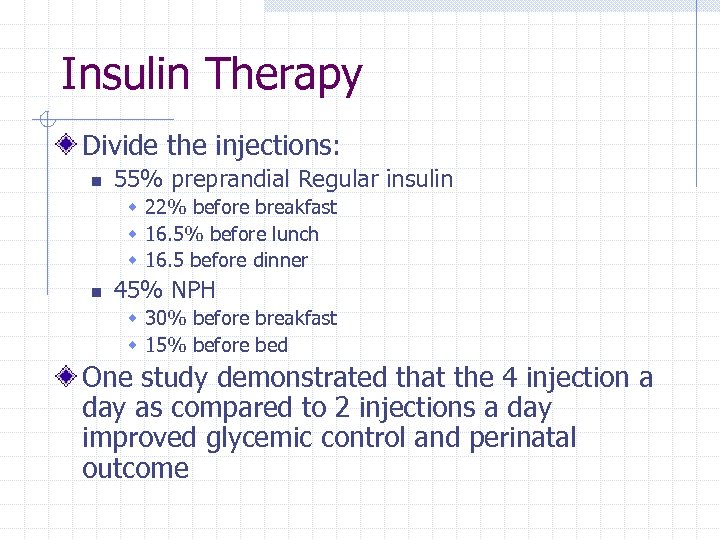
Insulin Therapy Divide the injections: n 55% preprandial Regular insulin w 22% before breakfast w 16. 5% before lunch w 16. 5 before dinner n 45% NPH w 30% before breakfast w 15% before bed One study demonstrated that the 4 injection a day as compared to 2 injections a day improved glycemic control and perinatal outcome
Oral Hypoglycemic Agents Further study required before Oral Hypoglycemic Agent may be used Sulfonylurea drug n Fetal hyperinsulinemia w Macrosomia w Neonatal hypoglycemia Glyburide n n Does not pass placenta May be safe: on going studies Metformin n Preeclampsia and still birth
Peripartum Concerns: Fetal Surveillance vasculopathy or significant potential fetal malformations increased risk of fetal malformations over the general population (1. 5% vs 4. 8%) Increased risk of prenatal complications n n n Fasting hyperglycemia Poor metabolic control Macrosomia (affect mode of delivery) Overall pregnancy outcome Increased risk pre eclampsia
Peripartum Concerns Fetal Surveillance Early Delivery Macrosomia and C-Section General Delivery Neonatal Issues
Peripartum Concerns: Fetal Surveillance Well controlled gestational diabetes n n Decreased risk antepartum fetal demise Decreased third trimester neonatal mortality Counting fetal movements is a simple way to assess fetal well being Fewer then 10 movements in 12 hours is associated with poor outcome The ACOG recommend fetal surveillance to be initiated in women with poor control, require insulin or have other complications of pregnancy
Peripartum Concerns: Fetal Surveillance Nonstress tests (NSTs) or (BPP) n n 32 weeks of gestation with poor control 35 weeks with good control may increase to 2 x / week if indicated may start as early as 26 weeks complications/poor control Non reassuring fetal testing n n Reversible problem Non reversible situations Often pathologic heart patterns will revert to normal when maternal metabolic control is achieved
Peripartum Concerns: Early delivery Ideally deliver at 39 or 40 weeks Indications for early delivery n n poor glycemic control fetal abnormalities If early delivery is indicated n n Assess lung for maturity Delay delivery until lung maturity w Utilize steroids
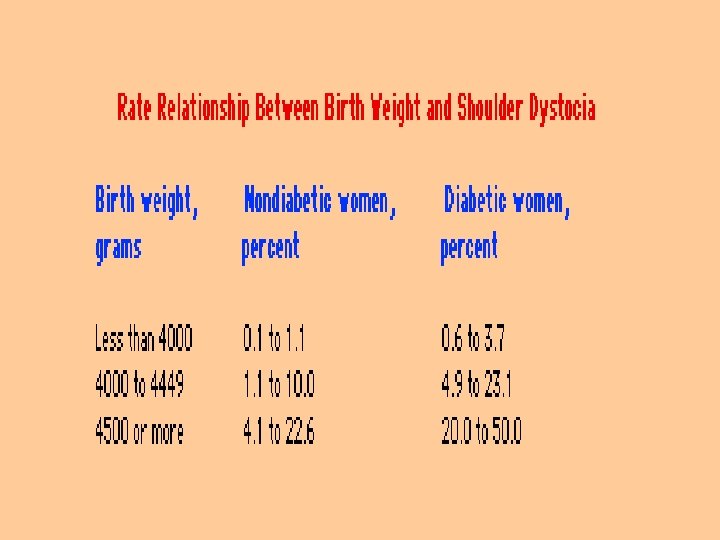
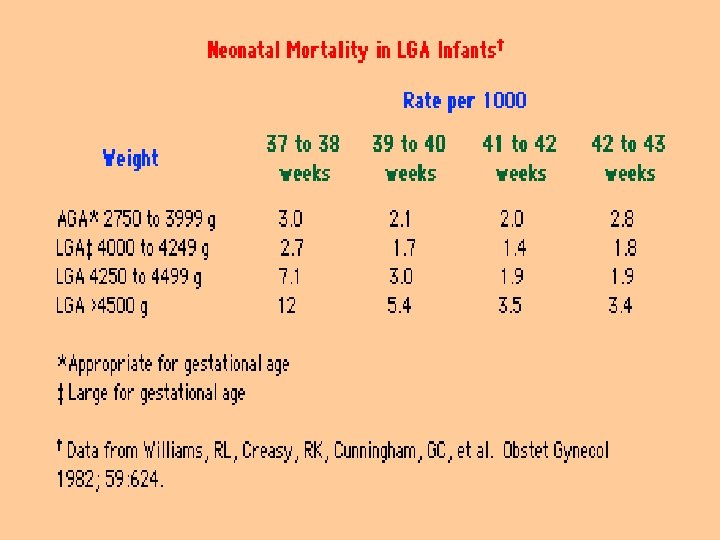
Peripartum Concerns: Macrosomia and C-Section Untreated GDM n Macrosomia is 17 to 29% (10% in general population) w C-Section to prevent shoulder dystocia is common for macrosomia Ultra Sound Elective C-Sections n n Estimated fetal wt is > 4. 5 Kg fetal wts of 4. 0 to 4. 5 Kg are at risk for shoulder dystocia

Peripartum Concerns: Delivery Goals n n GDM proceed to term and have an uneventful spontaneous vaginal deliver Avoid maternal hyperglycemia Insulin may be withheld during delivery and an IV of NS may be sufficient to maintain normoglycemia
Peripartum Concerns: Neonatal Issues The degree of maternal hyperglycemia correlates to the adverse outcomes Immediate n n Hypoglycemia Hyperbilirubinemia Hypocalcemia Polycythemia Long Term n Possibly impaired glucose intolerance and childhood obesity
Post. Partum Care Immediately after deliver n n glucose should be measured Fasting glucose should be < 110 and 1 hour post prandial <140 Resume regular diet but continue to measure and record bld sugars for several weeks after discharge 6 to 8 weeks following delivery n GCT; GTT
Post. Partuum concerns and future Risk After delivery n nearly all postpartum women will become normoglycemic 1/3 to 2/3 will have recurrent GDM in subsequent pregnancies 47 to 50% will develop DM within the first 5 years and is correlated to the glucose intolerance on the postpartum GTT 20% of GDM will have impaired glucose intolerance in early postpartum period GDM itself is a risk for development of DM. The HLA (DR 3 DR 4) may predispose to type 1 DM
Gestational Diabetes Questions? ? ?
a81d11ea7b7b3bef2d604467c74eacc6.ppt