9ca7f6f849e26da6f22febd84de96339.ppt
- Количество слайдов: 53
 Gender: male v Age: 12 y/o v
Gender: male v Age: 12 y/o v
 Chief compliant Neck mass noted about 1 year
Chief compliant Neck mass noted about 1 year
 Present illness v This 12 y/o boy 何o銳 suffered from right neck mass (initial size: 3 cm) for about 1 years. Therefore he came to KMUH for help in Oct 2006 and NP biopsy was done, it showed chronic inflammation. Biopsy of lymph node over right side of neck showed metastatic carcinoma. The primary lesion was unknown after a series of exam were done there. He had also been to CGMH and PET was arranged, which showed no primary site. Then he came to our ENT OPD for help in Aug 2007. PE showed previous op scar over right neck and bulging mass over nasopharynx. Then he received NP biopsy, and it showed nonkeratinizing undifferentiated carcinoma.
Present illness v This 12 y/o boy 何o銳 suffered from right neck mass (initial size: 3 cm) for about 1 years. Therefore he came to KMUH for help in Oct 2006 and NP biopsy was done, it showed chronic inflammation. Biopsy of lymph node over right side of neck showed metastatic carcinoma. The primary lesion was unknown after a series of exam were done there. He had also been to CGMH and PET was arranged, which showed no primary site. Then he came to our ENT OPD for help in Aug 2007. PE showed previous op scar over right neck and bulging mass over nasopharynx. Then he received NP biopsy, and it showed nonkeratinizing undifferentiated carcinoma.
 Present illness v Under the impression of NPC with right neck metastasis, he was admitted for tumor survey in Oct 2007. MRI revealed NPC with right side skull base involvement and multiple lymph nodes over carotid space and posterior triangle of bil. submandibular and neck region, the maxium one size about 2 cm over the right side, and above 1. 5 cm over the left side noted. Abdominal sono showed hyperechoic area (1. 2 cm) in right lobe of liver, hemangioma or focal fatty liver change was suspected. Whole body bone scan showed no distant bony metastases except direct basal skull invasion. Radiotherapy was suggested then, but his family preferred traditional therapy. However, the mass over right side of neck progressed in size. So he was brought to our hospital again and he was referred to our department for further survey and CCRT.
Present illness v Under the impression of NPC with right neck metastasis, he was admitted for tumor survey in Oct 2007. MRI revealed NPC with right side skull base involvement and multiple lymph nodes over carotid space and posterior triangle of bil. submandibular and neck region, the maxium one size about 2 cm over the right side, and above 1. 5 cm over the left side noted. Abdominal sono showed hyperechoic area (1. 2 cm) in right lobe of liver, hemangioma or focal fatty liver change was suspected. Whole body bone scan showed no distant bony metastases except direct basal skull invasion. Radiotherapy was suggested then, but his family preferred traditional therapy. However, the mass over right side of neck progressed in size. So he was brought to our hospital again and he was referred to our department for further survey and CCRT.
 Past and personal history: – – – DM/HTN: denied habit of Smoking: denied habit of drinking: denied habit of betel nuts chewing: (-) drug allergy: unkown Previous op history: (-)
Past and personal history: – – – DM/HTN: denied habit of Smoking: denied habit of drinking: denied habit of betel nuts chewing: (-) drug allergy: unkown Previous op history: (-)
 Physical examination General: consciousness clear HEENT: no pale conjunctiva, no icteric sclera v v – – Nasopharynx: bulging mass over right side Neck: • v v A neck mass about 3 x 6. 5 cm over right side of upper neck, firm, immovable Chest: clear breathing sound, no rales, no wheezing Heart: regular heart beats, no murmurs Abdomen: soft & flat, no tenderness, normoactive bowel sound Karnofsky scale: 90%
Physical examination General: consciousness clear HEENT: no pale conjunctiva, no icteric sclera v v – – Nasopharynx: bulging mass over right side Neck: • v v A neck mass about 3 x 6. 5 cm over right side of upper neck, firm, immovable Chest: clear breathing sound, no rales, no wheezing Heart: regular heart beats, no murmurs Abdomen: soft & flat, no tenderness, normoactive bowel sound Karnofsky scale: 90%
 Lab data v EB-VCA Ig. A: 5. 68(+), Ig. G: 5. 63 (+)
Lab data v EB-VCA Ig. A: 5. 68(+), Ig. G: 5. 63 (+)
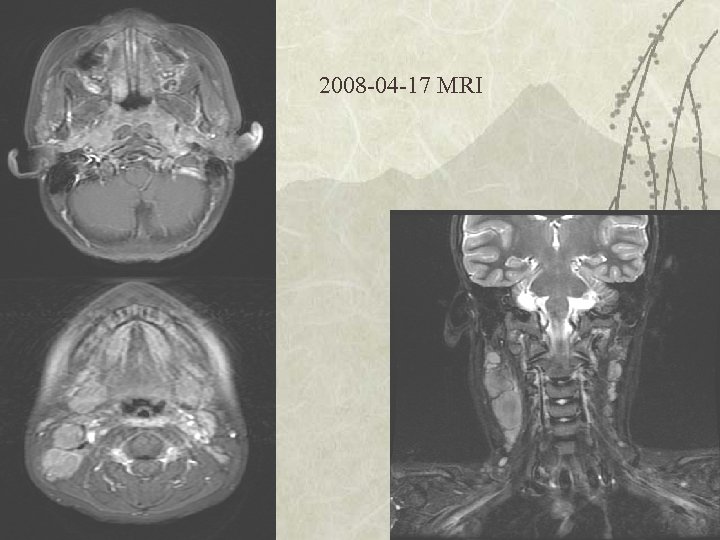
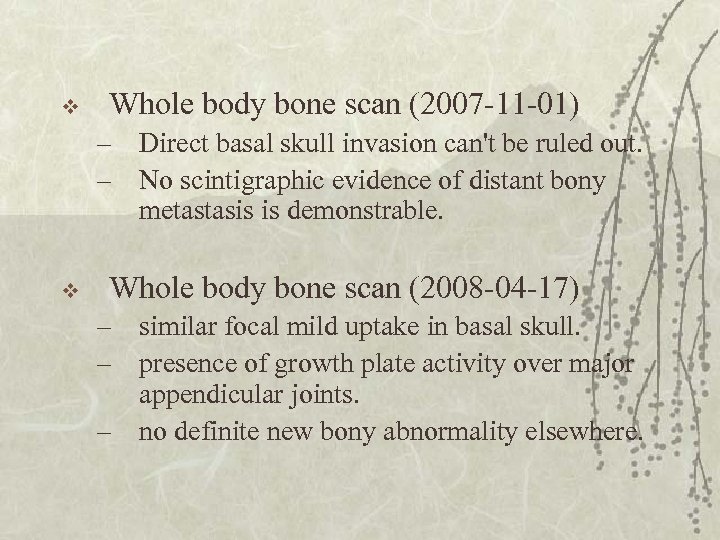
 v MRI (N/Y contrast), Nasopharynx (200710 -31) (2008 -04 -17) – lymph nodes noted over the carotid space and posterior triangle of bil. submandibular and neck region • • Right side: 2 cm 2. 7 cm Left side: 1. 5 cm 1. 7 cm
v MRI (N/Y contrast), Nasopharynx (200710 -31) (2008 -04 -17) – lymph nodes noted over the carotid space and posterior triangle of bil. submandibular and neck region • • Right side: 2 cm 2. 7 cm Left side: 1. 5 cm 1. 7 cm
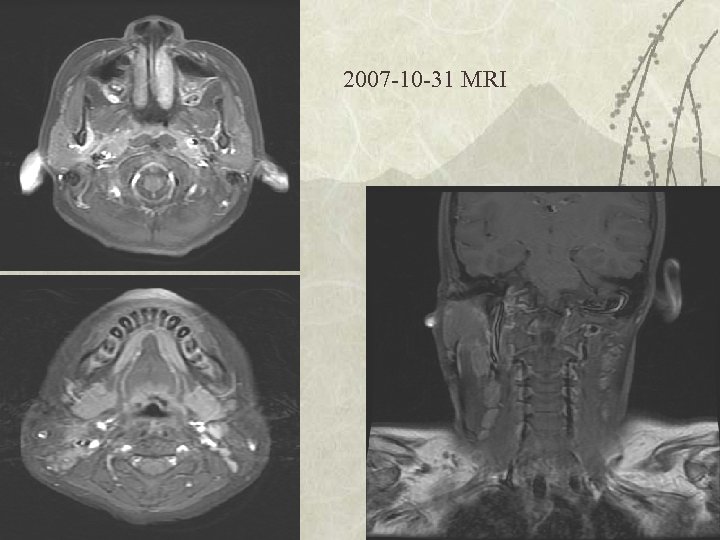 2007 -10 -31 MRI
2007 -10 -31 MRI
 2008 -04 -17 MRI
2008 -04 -17 MRI
 v Whole body bone scan (2007 -11 -01) – Direct basal skull invasion can't be ruled out. – No scintigraphic evidence of distant bony metastasis is demonstrable. v Whole body bone scan (2008 -04 -17) – similar focal mild uptake in basal skull. – presence of growth plate activity over major appendicular joints. – no definite new bony abnormality elsewhere.
v Whole body bone scan (2007 -11 -01) – Direct basal skull invasion can't be ruled out. – No scintigraphic evidence of distant bony metastasis is demonstrable. v Whole body bone scan (2008 -04 -17) – similar focal mild uptake in basal skull. – presence of growth plate activity over major appendicular joints. – no definite new bony abnormality elsewhere.
 v Sono, Upper abdomen (2007 -10 -31) – A small hyperechoic area (1. 2 cm) in right lobe of liver, hemangioma or focal fatty liver change was first considered, regular ultrasound F/U was suggested, no other focal lesion in upper abdomen
v Sono, Upper abdomen (2007 -10 -31) – A small hyperechoic area (1. 2 cm) in right lobe of liver, hemangioma or focal fatty liver change was first considered, regular ultrasound F/U was suggested, no other focal lesion in upper abdomen
 Treatment planning v v Energy and purpose: 6 MVX-rays with curative intent Position: supine with mask Technique: SAD 100 cm, IMRT with ? portals to cover tumor in nasopahrynx Dosage: – – Tumor in nasopahrynx and LN over bil. neck: 70 Gy/35 Fx/7 weeks Bilateral level II , III, IV and 1/2 of postrior nasal cavity and 1/3 of maxillary sinus: 63 Gy/35 Fx/7 weeks
Treatment planning v v Energy and purpose: 6 MVX-rays with curative intent Position: supine with mask Technique: SAD 100 cm, IMRT with ? portals to cover tumor in nasopahrynx Dosage: – – Tumor in nasopahrynx and LN over bil. neck: 70 Gy/35 Fx/7 weeks Bilateral level II , III, IV and 1/2 of postrior nasal cavity and 1/3 of maxillary sinus: 63 Gy/35 Fx/7 weeks
 Childhood nasopharyngeal carcinoma: from biology to treatment Lancet Oncol 2003; 4: 13– 21
Childhood nasopharyngeal carcinoma: from biology to treatment Lancet Oncol 2003; 4: 13– 21
 Childhood NPC v close association with EBV infection – high titer of Ig. G, Ig. A Undifferentiated histology v High incidence of locoregionally advanced disease and distant metastases v
Childhood NPC v close association with EBV infection – high titer of Ig. G, Ig. A Undifferentiated histology v High incidence of locoregionally advanced disease and distant metastases v
 Epidemiology and aetiology v Children under 16 years of age – 1– 2% of all patients with NPC in China, – 2. 4% in the UK – 7. 2% in Turkey – 10% in the USA – 12%in Israel – 13% in Kenya – 14. 5% in Tunisia – 18% in Uganda
Epidemiology and aetiology v Children under 16 years of age – 1– 2% of all patients with NPC in China, – 2. 4% in the UK – 7. 2% in Turkey – 10% in the USA – 12%in Israel – 13% in Kenya – 14. 5% in Tunisia – 18% in Uganda
 Epidemiology and aetiology v NPC constitutes 20– 50% of all primary nasopharyngeal malignant tumors in children –Median age: 13 years –Male : female = 1. 8: 1 –Black people
Epidemiology and aetiology v NPC constitutes 20– 50% of all primary nasopharyngeal malignant tumors in children –Median age: 13 years –Male : female = 1. 8: 1 –Black people
 Epidemiology and aetiology v Genetic Risk factor: – HLA A 2 Bsin 2 haplotype, Aw 19, Bw 46, and B 17 types –deletions of chromosomes 3 p, 9 p, 11 q, 13 q, and 14 q –inactivation of p 53, rearrangements in retinoblastoma (RB 2/p 130) tumor suppressor genes, and genetic polymorphism of the CYP 2 E 1 gene
Epidemiology and aetiology v Genetic Risk factor: – HLA A 2 Bsin 2 haplotype, Aw 19, Bw 46, and B 17 types –deletions of chromosomes 3 p, 9 p, 11 q, 13 q, and 14 q –inactivation of p 53, rearrangements in retinoblastoma (RB 2/p 130) tumor suppressor genes, and genetic polymorphism of the CYP 2 E 1 gene
 v Invasiveness: – Gains of genes on chromosome 12 – allelic loss on 11 q, 13 q, and 16 q v metastatic disease –mutation of p 53 –aberrant expression of cadherins
v Invasiveness: – Gains of genes on chromosome 12 – allelic loss on 11 q, 13 q, and 16 q v metastatic disease –mutation of p 53 –aberrant expression of cadherins
 v High titer of Ig. A, Ig. G –particularly those with the undifferentiated form of the disease –Ig. A antibodies specific to EBV are used as markers for screening –Good indicator for disease activity v High concentrations of antibodies against ZEBRA (Bam. H 1 Z Epstein-Barr replication activator) –ZEBRA is a nuclear transactivator that induces viral production by infected cells –Ig. GZ may be a useful marker for the follow-up of young patients with NPC
v High titer of Ig. A, Ig. G –particularly those with the undifferentiated form of the disease –Ig. A antibodies specific to EBV are used as markers for screening –Good indicator for disease activity v High concentrations of antibodies against ZEBRA (Bam. H 1 Z Epstein-Barr replication activator) –ZEBRA is a nuclear transactivator that induces viral production by infected cells –Ig. GZ may be a useful marker for the follow-up of young patients with NPC
 NPC & EBV v Clonal EBV genomes are found in cells that form early preinvasive dysplastic lesions –EBV infection is an early event in multistep carcinogenesis of NPC v EBV –double-stranded DNA molecule that encodes more than 100 genes of which only 10 are expressed in latently infected cells in vitro – 6 nuclear proteins (EBNAs), – 2 membrane proteins (LMPs), – 2 non-translated RNA molecules (EBER)
NPC & EBV v Clonal EBV genomes are found in cells that form early preinvasive dysplastic lesions –EBV infection is an early event in multistep carcinogenesis of NPC v EBV –double-stranded DNA molecule that encodes more than 100 genes of which only 10 are expressed in latently infected cells in vitro – 6 nuclear proteins (EBNAs), – 2 membrane proteins (LMPs), – 2 non-translated RNA molecules (EBER)
 v EBNA 1 –Expressed in nearly all cases of EBV-positive NPC –important in replication and maintenance of the viral genome during cell division v LMP 1 –Oncogenic substance • upregulates several cellular proteins that inhibit apoptosis, including BCL-2 and A 20, and binds to numerous • Binds to proteins associated with the tumor necrosis-factor receptor –expressed in almost two thirds of EBV positive NPC tumors
v EBNA 1 –Expressed in nearly all cases of EBV-positive NPC –important in replication and maintenance of the viral genome during cell division v LMP 1 –Oncogenic substance • upregulates several cellular proteins that inhibit apoptosis, including BCL-2 and A 20, and binds to numerous • Binds to proteins associated with the tumor necrosis-factor receptor –expressed in almost two thirds of EBV positive NPC tumors
 v LMP 2 –Prevents reactivation of the virus by blocking phosphorylation by tyrosine kinases v EBER –Do not encode proteins –important for oncogenesis and resistance to programmed cell death (apoptosis).
v LMP 2 –Prevents reactivation of the virus by blocking phosphorylation by tyrosine kinases v EBER –Do not encode proteins –important for oncogenesis and resistance to programmed cell death (apoptosis).
 v pathogenesis of childhood NPC –multistep process involving EBV infection that leads to increased expression of LMP 1 and p 53 in epithelial cells –oncoprotein BCL-2 is highly expressed in 80% of adults with NPC, it is probably not associated with paediatric NPC.
v pathogenesis of childhood NPC –multistep process involving EBV infection that leads to increased expression of LMP 1 and p 53 in epithelial cells –oncoprotein BCL-2 is highly expressed in 80% of adults with NPC, it is probably not associated with paediatric NPC.
 Immune suppression v T-cell immunity to EBV –suppression of EBV-infected B-cell proliferation and the growth and invasion of NPC tumors –ratio of CD 4 to CD 8 is reduced –production of interleukin 2 and its receptor is decreased –the numbers of CD 8 -positive cells in peripheral blood and the tumor are increased v interferon-β could be useful for immunostimulation because of its direct and indirect effects on tumor cells
Immune suppression v T-cell immunity to EBV –suppression of EBV-infected B-cell proliferation and the growth and invasion of NPC tumors –ratio of CD 4 to CD 8 is reduced –production of interleukin 2 and its receptor is decreased –the numbers of CD 8 -positive cells in peripheral blood and the tumor are increased v interferon-β could be useful for immunostimulation because of its direct and indirect effects on tumor cells
 Histopathology v Type I: keratinising squamous-cell carcinoma –Keratin production v type II : non-keratinising epidermoid carcinoma –IIa: pleiomorphism –IIb: lymphoid infiltration v type III : undifferentiated carcinoma –IIIa: Large nucleoli and eosinophilic cytoplasm –IIIb: small nucleoli and basophilic structure
Histopathology v Type I: keratinising squamous-cell carcinoma –Keratin production v type II : non-keratinising epidermoid carcinoma –IIa: pleiomorphism –IIb: lymphoid infiltration v type III : undifferentiated carcinoma –IIIa: Large nucleoli and eosinophilic cytoplasm –IIIb: small nucleoli and basophilic structure
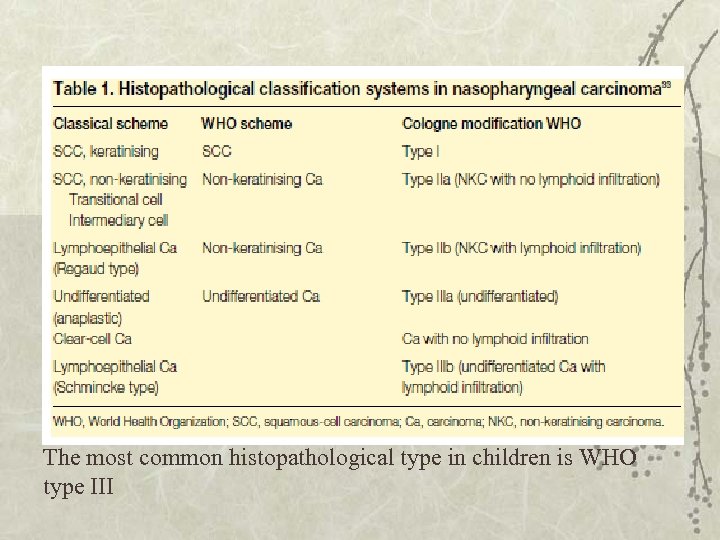 The most common histopathological type in children is WHO type III
The most common histopathological type in children is WHO type III
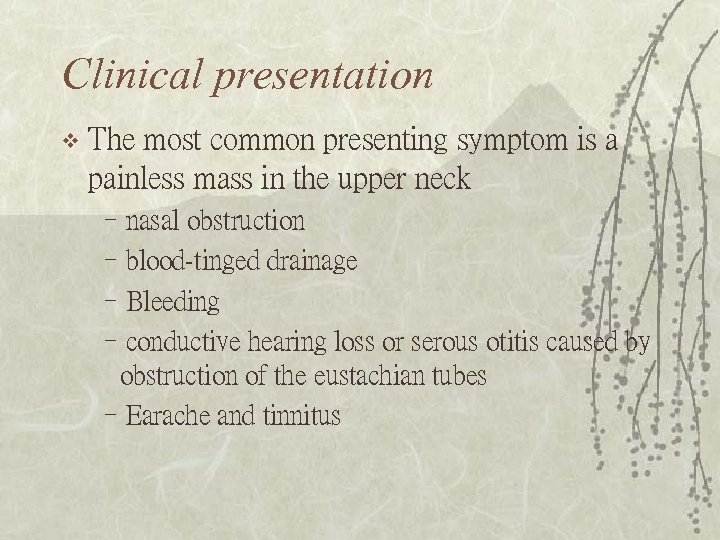 Clinical presentation v The most common presenting symptom is a painless mass in the upper neck –nasal obstruction –blood-tinged drainage –Bleeding –conductive hearing loss or serous otitis caused by obstruction of the eustachian tubes –Earache and tinnitus
Clinical presentation v The most common presenting symptom is a painless mass in the upper neck –nasal obstruction –blood-tinged drainage –Bleeding –conductive hearing loss or serous otitis caused by obstruction of the eustachian tubes –Earache and tinnitus
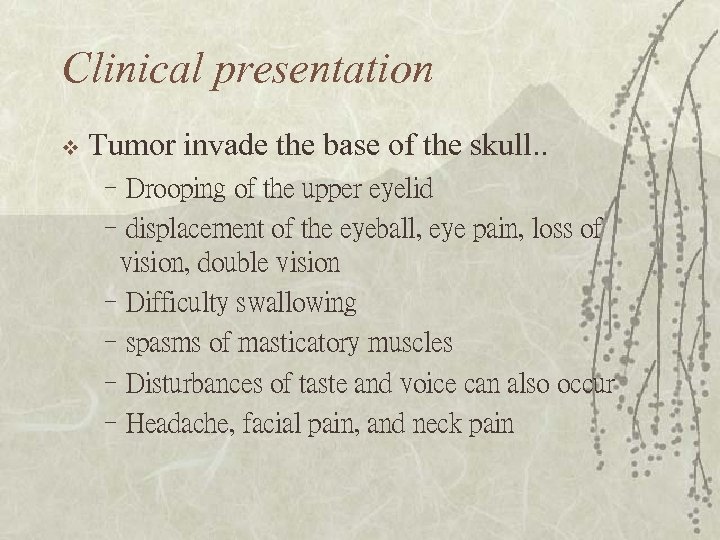 Clinical presentation v Tumor invade the base of the skull. . –Drooping of the upper eyelid –displacement of the eyeball, eye pain, loss of vision, double vision –Difficulty swallowing –spasms of masticatory muscles –Disturbances of taste and voice can also occur –Headache, facial pain, and neck pain
Clinical presentation v Tumor invade the base of the skull. . –Drooping of the upper eyelid –displacement of the eyeball, eye pain, loss of vision, double vision –Difficulty swallowing –spasms of masticatory muscles –Disturbances of taste and voice can also occur –Headache, facial pain, and neck pain
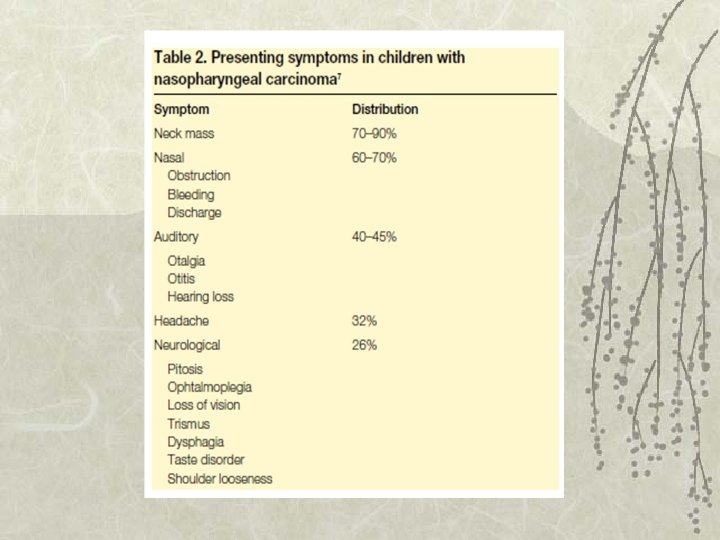
 Clinical presentation v Distant metastatic regions –bones (67%) –liver(30%) –bone marrow (23%) –lungs (20%), and mediastinum
Clinical presentation v Distant metastatic regions –bones (67%) –liver(30%) –bone marrow (23%) –lungs (20%), and mediastinum
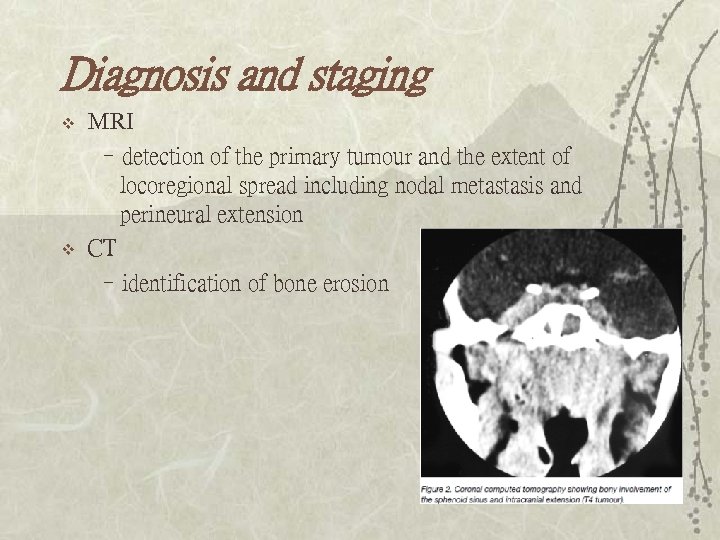 Diagnosis and staging v v MRI –detection of the primary tumour and the extent of locoregional spread including nodal metastasis and perineural extension CT –identification of bone erosion
Diagnosis and staging v v MRI –detection of the primary tumour and the extent of locoregional spread including nodal metastasis and perineural extension CT –identification of bone erosion
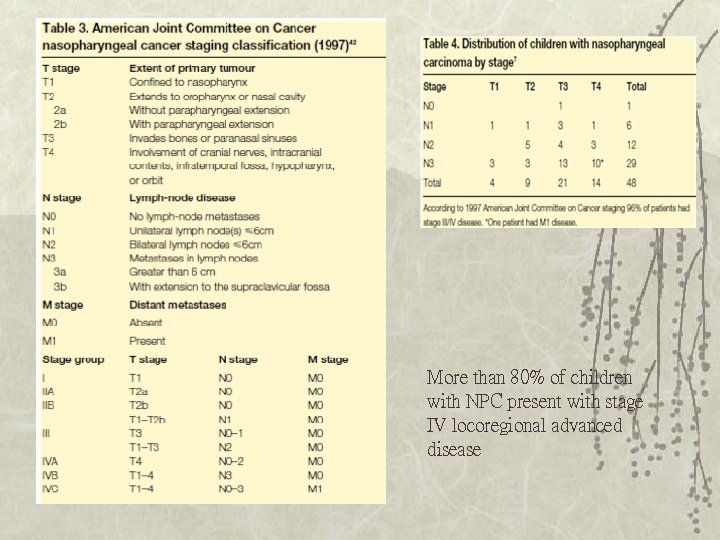 More than 80% of children with NPC present with stage IV locoregional advanced disease
More than 80% of children with NPC present with stage IV locoregional advanced disease
 v Lab data – LDH > 500 IU/ml poor prognosis – Viral caspid antigen Ig. A and ZEBRA protein concentration • Monitoring disease recurrence
v Lab data – LDH > 500 IU/ml poor prognosis – Viral caspid antigen Ig. A and ZEBRA protein concentration • Monitoring disease recurrence
 Treatment and prognosis v Surgical therapy –unresectable due to complex anatomical location of disease –radical neck dissection is appropriate • primary tumor seems to be controlled • persistent neck nodes following chemoradiation • isolated recurrence in the neck occurs after radiotherapy
Treatment and prognosis v Surgical therapy –unresectable due to complex anatomical location of disease –radical neck dissection is appropriate • primary tumor seems to be controlled • persistent neck nodes following chemoradiation • isolated recurrence in the neck occurs after radiotherapy
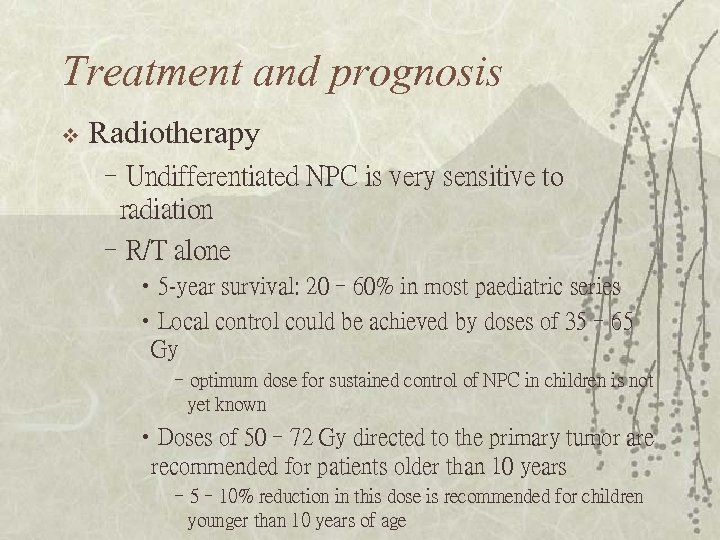 Treatment and prognosis v Radiotherapy –Undifferentiated NPC is very sensitive to radiation –R/T alone • 5 -year survival: 20– 60% in most paediatric series • Local control could be achieved by doses of 35– 65 Gy –optimum dose for sustained control of NPC in children is not yet known • Doses of 50– 72 Gy directed to the primary tumor are recommended for patients older than 10 years – 5– 10% reduction in this dose is recommended for children younger than 10 years of age
Treatment and prognosis v Radiotherapy –Undifferentiated NPC is very sensitive to radiation –R/T alone • 5 -year survival: 20– 60% in most paediatric series • Local control could be achieved by doses of 35– 65 Gy –optimum dose for sustained control of NPC in children is not yet known • Doses of 50– 72 Gy directed to the primary tumor are recommended for patients older than 10 years – 5– 10% reduction in this dose is recommended for children younger than 10 years of age
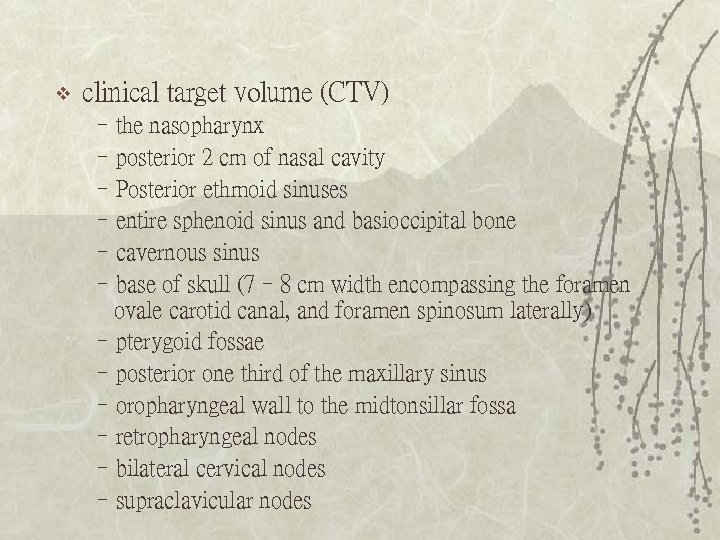 v clinical target volume (CTV) –the nasopharynx –posterior 2 cm of nasal cavity –Posterior ethmoid sinuses –entire sphenoid sinus and basioccipital bone –cavernous sinus –base of skull (7– 8 cm width encompassing the foramen ovale carotid canal, and foramen spinosum laterally) –pterygoid fossae –posterior one third of the maxillary sinus –oropharyngeal wall to the midtonsillar fossa –retropharyngeal nodes –bilateral cervical nodes –supraclavicular nodes
v clinical target volume (CTV) –the nasopharynx –posterior 2 cm of nasal cavity –Posterior ethmoid sinuses –entire sphenoid sinus and basioccipital bone –cavernous sinus –base of skull (7– 8 cm width encompassing the foramen ovale carotid canal, and foramen spinosum laterally) –pterygoid fossae –posterior one third of the maxillary sinus –oropharyngeal wall to the midtonsillar fossa –retropharyngeal nodes –bilateral cervical nodes –supraclavicular nodes
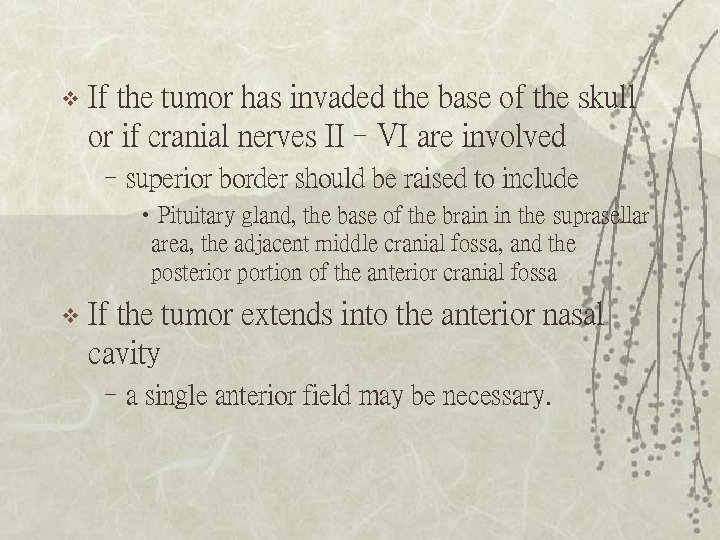 v If the tumor has invaded the base of the skull or if cranial nerves II–VI are involved –superior border should be raised to include • Pituitary gland, the base of the brain in the suprasellar area, the adjacent middle cranial fossa, and the posterior portion of the anterior cranial fossa v If the tumor extends into the anterior nasal cavity –a single anterior field may be necessary.
v If the tumor has invaded the base of the skull or if cranial nerves II–VI are involved –superior border should be raised to include • Pituitary gland, the base of the brain in the suprasellar area, the adjacent middle cranial fossa, and the posterior portion of the anterior cranial fossa v If the tumor extends into the anterior nasal cavity –a single anterior field may be necessary.

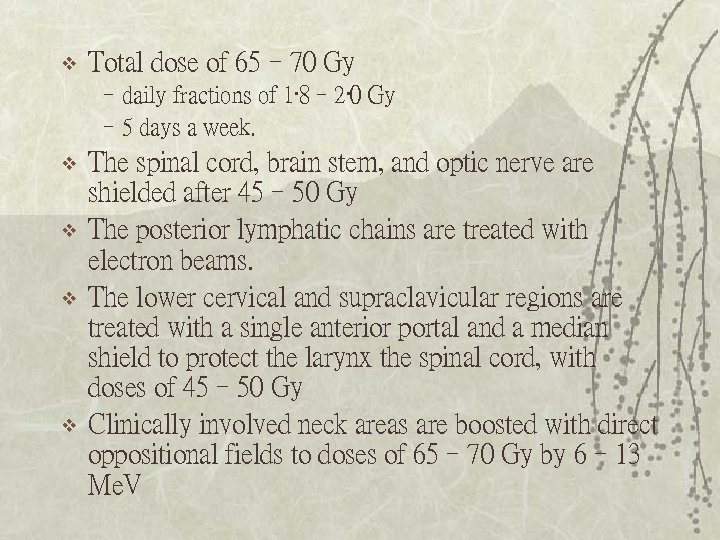 v Total dose of 65– 70 Gy –daily fractions of 1· 8– 2· 0 Gy – 5 days a week. v v The spinal cord, brain stem, and optic nerve are shielded after 45– 50 Gy The posterior lymphatic chains are treated with electron beams. The lower cervical and supraclavicular regions are treated with a single anterior portal and a median shield to protect the larynx the spinal cord, with doses of 45– 50 Gy Clinically involved neck areas are boosted with direct oppositional fields to doses of 65– 70 Gy by 6– 13 Me. V
v Total dose of 65– 70 Gy –daily fractions of 1· 8– 2· 0 Gy – 5 days a week. v v The spinal cord, brain stem, and optic nerve are shielded after 45– 50 Gy The posterior lymphatic chains are treated with electron beams. The lower cervical and supraclavicular regions are treated with a single anterior portal and a median shield to protect the larynx the spinal cord, with doses of 45– 50 Gy Clinically involved neck areas are boosted with direct oppositional fields to doses of 65– 70 Gy by 6– 13 Me. V
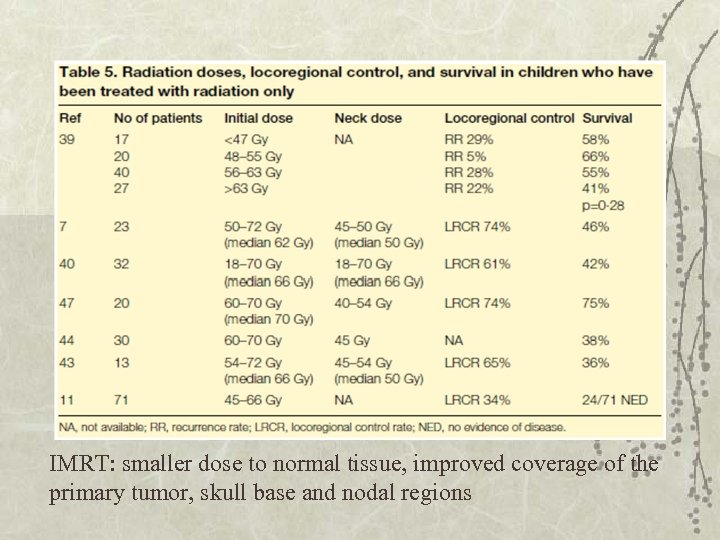 IMRT: smaller dose to normal tissue, improved coverage of the primary tumor, skull base and nodal regions
IMRT: smaller dose to normal tissue, improved coverage of the primary tumor, skull base and nodal regions
 Survival rate v Stage: –T stage • T 1– 2 : 75% • T 3– 4: 37% –N stage • N 0: 64% • N 3: 36% –Metastatic disease at presentation : <10% v Irradiation dose: –< 60 Gy: 10 -36% –> 60 Gy: 60 -76%
Survival rate v Stage: –T stage • T 1– 2 : 75% • T 3– 4: 37% –N stage • N 0: 64% • N 3: 36% –Metastatic disease at presentation : <10% v Irradiation dose: –< 60 Gy: 10 -36% –> 60 Gy: 60 -76%
 Relapses! Most occur in the first 2 years v > 50 % patients have overt distant metastases v
Relapses! Most occur in the first 2 years v > 50 % patients have overt distant metastases v
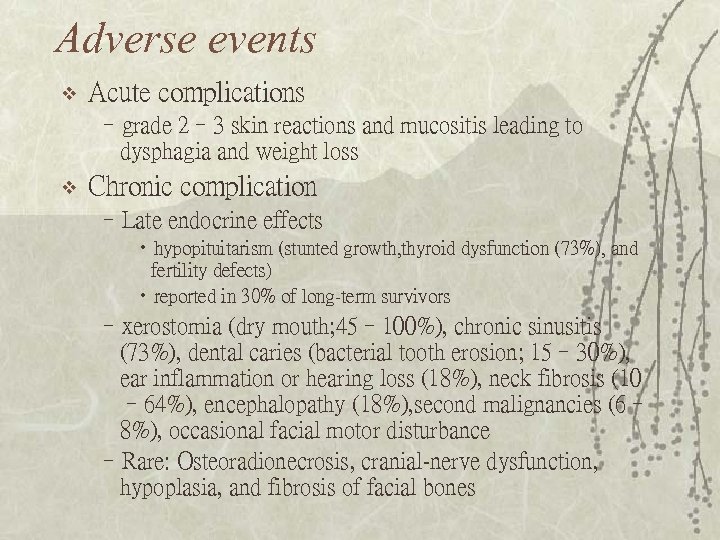 Adverse events v Acute complications –grade 2– 3 skin reactions and mucositis leading to dysphagia and weight loss v Chronic complication –Late endocrine effects • hypopituitarism (stunted growth, thyroid dysfunction (73%), and fertility defects) • reported in 30% of long-term survivors –xerostomia (dry mouth; 45– 100%), chronic sinusitis (73%), dental caries (bacterial tooth erosion; 15– 30%), ear inflammation or hearing loss (18%), neck fibrosis (10 – 64%), encephalopathy (18%), second malignancies (6– 8%), occasional facial motor disturbance –Rare: Osteoradionecrosis, cranial-nerve dysfunction, hypoplasia, and fibrosis of facial bones
Adverse events v Acute complications –grade 2– 3 skin reactions and mucositis leading to dysphagia and weight loss v Chronic complication –Late endocrine effects • hypopituitarism (stunted growth, thyroid dysfunction (73%), and fertility defects) • reported in 30% of long-term survivors –xerostomia (dry mouth; 45– 100%), chronic sinusitis (73%), dental caries (bacterial tooth erosion; 15– 30%), ear inflammation or hearing loss (18%), neck fibrosis (10 – 64%), encephalopathy (18%), second malignancies (6– 8%), occasional facial motor disturbance –Rare: Osteoradionecrosis, cranial-nerve dysfunction, hypoplasia, and fibrosis of facial bones
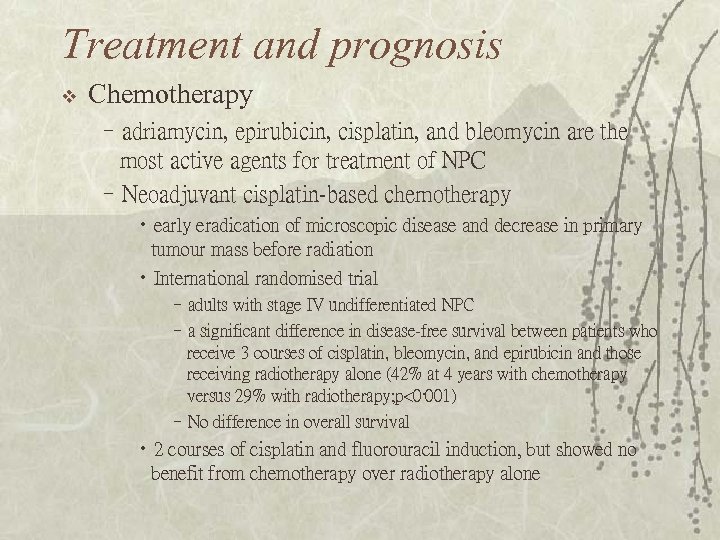 Treatment and prognosis v Chemotherapy –adriamycin, epirubicin, cisplatin, and bleomycin are the most active agents for treatment of NPC –Neoadjuvant cisplatin-based chemotherapy • early eradication of microscopic disease and decrease in primary tumour mass before radiation • International randomised trial –adults with stage IV undifferentiated NPC –a significant difference in disease-free survival between patients who receive 3 courses of cisplatin, bleomycin, and epirubicin and those receiving radiotherapy alone (42% at 4 years with chemotherapy versus 29% with radiotherapy; p<0· 001) –No difference in overall survival • 2 courses of cisplatin and fluorouracil induction, but showed no benefit from chemotherapy over radiotherapy alone
Treatment and prognosis v Chemotherapy –adriamycin, epirubicin, cisplatin, and bleomycin are the most active agents for treatment of NPC –Neoadjuvant cisplatin-based chemotherapy • early eradication of microscopic disease and decrease in primary tumour mass before radiation • International randomised trial –adults with stage IV undifferentiated NPC –a significant difference in disease-free survival between patients who receive 3 courses of cisplatin, bleomycin, and epirubicin and those receiving radiotherapy alone (42% at 4 years with chemotherapy versus 29% with radiotherapy; p<0· 001) –No difference in overall survival • 2 courses of cisplatin and fluorouracil induction, but showed no benefit from chemotherapy over radiotherapy alone
 –Concomitant chemoradiotherapy • eradicate local occult metastatic disease by radiosensitisation • the systemic effects of cytotoxic agents. • concomitant cisplatin and radiotherapy followed by 3 courses of adjuvant cisplatin and fluorouracil is now the standard of care for adults with NPC in the USA –childhood NPC: not yet been determined
–Concomitant chemoradiotherapy • eradicate local occult metastatic disease by radiosensitisation • the systemic effects of cytotoxic agents. • concomitant cisplatin and radiotherapy followed by 3 courses of adjuvant cisplatin and fluorouracil is now the standard of care for adults with NPC in the USA –childhood NPC: not yet been determined
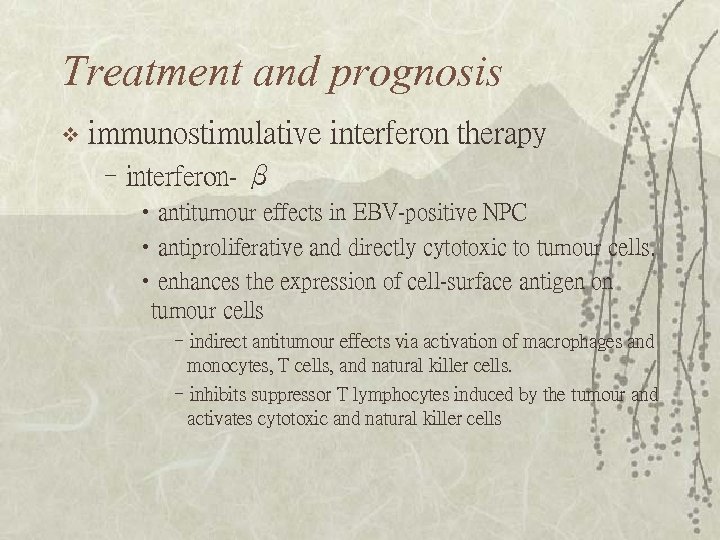 Treatment and prognosis v immunostimulative interferon therapy –interferon- β • antitumour effects in EBV-positive NPC • antiproliferative and directly cytotoxic to tumour cells. • enhances the expression of cell-surface antigen on tumour cells –indirect antitumour effects via activation of macrophages and monocytes, T cells, and natural killer cells. –inhibits suppressor T lymphocytes induced by the tumour and activates cytotoxic and natural killer cells
Treatment and prognosis v immunostimulative interferon therapy –interferon- β • antitumour effects in EBV-positive NPC • antiproliferative and directly cytotoxic to tumour cells. • enhances the expression of cell-surface antigen on tumour cells –indirect antitumour effects via activation of macrophages and monocytes, T cells, and natural killer cells. –inhibits suppressor T lymphocytes induced by the tumour and activates cytotoxic and natural killer cells
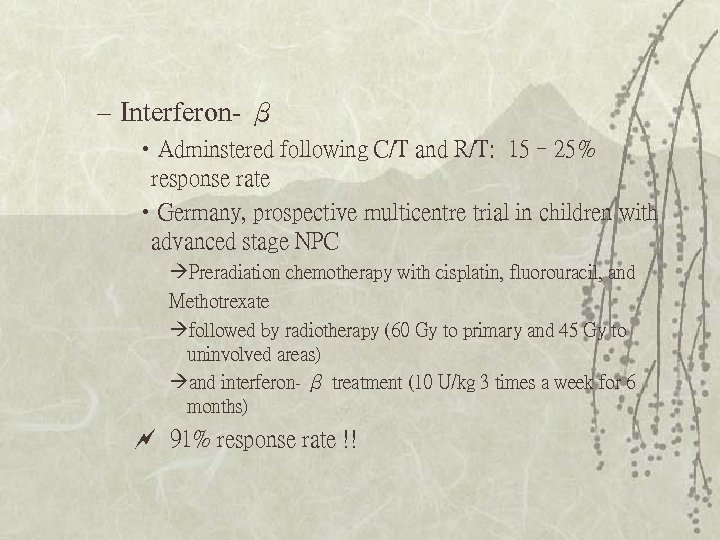 – Interferon- β • Adminstered following C/T and R/T: 15– 25% response rate • Germany, prospective multicentre trial in children with advanced stage NPC Preradiation chemotherapy with cisplatin, fluorouracil, and Methotrexate followed by radiotherapy (60 Gy to primary and 45 Gy to uninvolved areas) and interferon- β treatment (10 U/kg 3 times a week for 6 months) 91% response rate !!
– Interferon- β • Adminstered following C/T and R/T: 15– 25% response rate • Germany, prospective multicentre trial in children with advanced stage NPC Preradiation chemotherapy with cisplatin, fluorouracil, and Methotrexate followed by radiotherapy (60 Gy to primary and 45 Gy to uninvolved areas) and interferon- β treatment (10 U/kg 3 times a week for 6 months) 91% response rate !!
 Metastatic and recurrent disease v 20– 50% of patients still suffer from recurrent or metastatic disease –Most within 1 -2 years of diagnosis – 48% of relapses occurred at distant sites only – 43% at local and regional sites – 9% both at distant and locoregional regions. v Median survival – 3– 6 months in untreated patients – 8– 12 months for those treated by chemotherapy
Metastatic and recurrent disease v 20– 50% of patients still suffer from recurrent or metastatic disease –Most within 1 -2 years of diagnosis – 48% of relapses occurred at distant sites only – 43% at local and regional sites – 9% both at distant and locoregional regions. v Median survival – 3– 6 months in untreated patients – 8– 12 months for those treated by chemotherapy
 Metastatic and recurrent disease v Chemotherapy: –Cisplatin and ifosfamide, weekly PF (cisplatin, fluorouracil), and interferon are also combinations that are used in recurrent disease. • Response rates are around 60– 90% • Complete response about 20% v Second line irradiation or brachytherapy –Locoregional recurrence –Severe complication – 5 -year survival of about 40%
Metastatic and recurrent disease v Chemotherapy: –Cisplatin and ifosfamide, weekly PF (cisplatin, fluorouracil), and interferon are also combinations that are used in recurrent disease. • Response rates are around 60– 90% • Complete response about 20% v Second line irradiation or brachytherapy –Locoregional recurrence –Severe complication – 5 -year survival of about 40%
 Conclusion v Early administration of an effective chemotherapeutic agent is needed for treatment of childhood NPC – Advanced stage – This tumor type is sensitive to chemotherapy
Conclusion v Early administration of an effective chemotherapeutic agent is needed for treatment of childhood NPC – Advanced stage – This tumor type is sensitive to chemotherapy


