Копия total.ppt
- Количество слайдов: 68
 Gastroenteritis, Infections of the GI Tract, and Diarrhea 2/8/2018 1
Gastroenteritis, Infections of the GI Tract, and Diarrhea 2/8/2018 1
 Gastroenteritis is a nonspecific term for various pathologic states of the gastrointestinal tract. n The primary manifestation is diarrhea, but it may be accompanied by nausea, vomiting, and abdominal pain. n A universal definition of diarrhea does not exist, although patients seem to have no difficulty defining their own situation. n n 2/8/2018 Although most definitions center on the frequency, consistency, and water content of stools 2
Gastroenteritis is a nonspecific term for various pathologic states of the gastrointestinal tract. n The primary manifestation is diarrhea, but it may be accompanied by nausea, vomiting, and abdominal pain. n A universal definition of diarrhea does not exist, although patients seem to have no difficulty defining their own situation. n n 2/8/2018 Although most definitions center on the frequency, consistency, and water content of stools 2
 Gastroenteritis Defined as- Inflammation of the mucous membrane of both the stomach and intestine, usually causing nausea, vomiting, and diarrhea. n Acute gastroenteritis usually causes profuse watery diarrhea, often c nausea and vomiting, but without localized findings. n Between cramps, the abdomen is completely relaxed. n 2/8/2018 3
Gastroenteritis Defined as- Inflammation of the mucous membrane of both the stomach and intestine, usually causing nausea, vomiting, and diarrhea. n Acute gastroenteritis usually causes profuse watery diarrhea, often c nausea and vomiting, but without localized findings. n Between cramps, the abdomen is completely relaxed. n 2/8/2018 3
 Cause of Gastroenteritis n n Infectious agents usually cause acute gastroenteritis. These agents cause diarrhea by adherence, mucosal invasion, enterotoxin production, and/or cytotoxin production. These mechanisms result in increased fluid secretion and/or decreased absorption. This produces an increased luminal fluid content that cannot be adequately reabsorbed, leading to dehydration and the loss of electrolytes and nutrients. 2/8/2018 4
Cause of Gastroenteritis n n Infectious agents usually cause acute gastroenteritis. These agents cause diarrhea by adherence, mucosal invasion, enterotoxin production, and/or cytotoxin production. These mechanisms result in increased fluid secretion and/or decreased absorption. This produces an increased luminal fluid content that cannot be adequately reabsorbed, leading to dehydration and the loss of electrolytes and nutrients. 2/8/2018 4
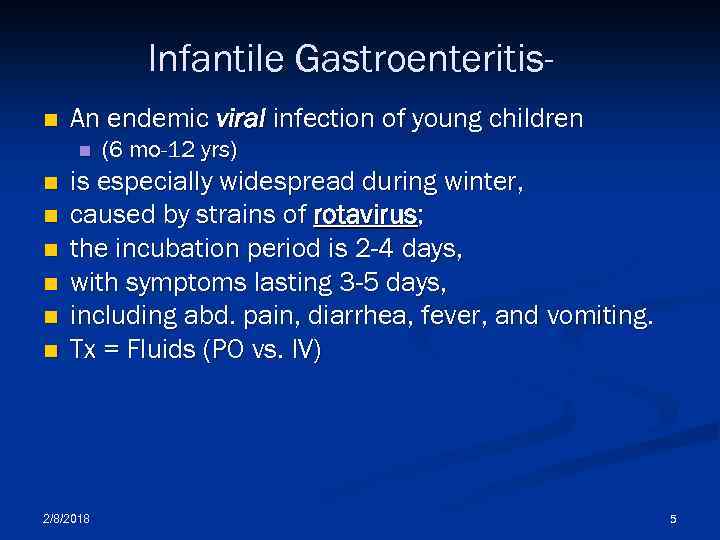 Infantile Gastroenteritisn An endemic viral infection of young children n n n (6 mo-12 yrs) is especially widespread during winter, caused by strains of rotavirus; the incubation period is 2 -4 days, with symptoms lasting 3 -5 days, including abd. pain, diarrhea, fever, and vomiting. Tx = Fluids (PO vs. IV) 2/8/2018 5
Infantile Gastroenteritisn An endemic viral infection of young children n n n (6 mo-12 yrs) is especially widespread during winter, caused by strains of rotavirus; the incubation period is 2 -4 days, with symptoms lasting 3 -5 days, including abd. pain, diarrhea, fever, and vomiting. Tx = Fluids (PO vs. IV) 2/8/2018 5
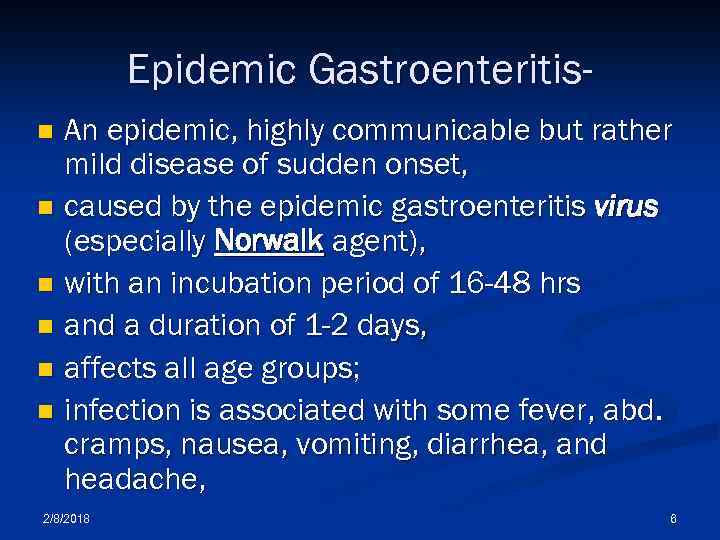 Epidemic Gastroenteritis. An epidemic, highly communicable but rather mild disease of sudden onset, n caused by the epidemic gastroenteritis virus (especially Norwalk agent), n with an incubation period of 16 -48 hrs n and a duration of 1 -2 days, n affects all age groups; n infection is associated with some fever, abd. cramps, nausea, vomiting, diarrhea, and headache, n 2/8/2018 6
Epidemic Gastroenteritis. An epidemic, highly communicable but rather mild disease of sudden onset, n caused by the epidemic gastroenteritis virus (especially Norwalk agent), n with an incubation period of 16 -48 hrs n and a duration of 1 -2 days, n affects all age groups; n infection is associated with some fever, abd. cramps, nausea, vomiting, diarrhea, and headache, n 2/8/2018 6
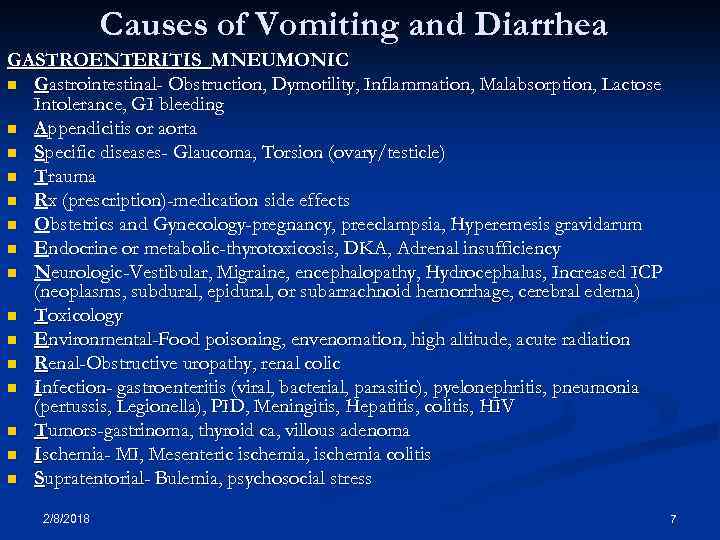 Causes of Vomiting and Diarrhea GASTROENTERITIS MNEUMONIC n Gastrointestinal- Obstruction, Dymotility, Inflammation, Malabsorption, Lactose Intolerance, GI bleeding n Appendicitis or aorta n Specific diseases- Glaucoma, Torsion (ovary/testicle) n Trauma n Rx (prescription)-medication side effects n Obstetrics and Gynecology-pregnancy, preeclampsia, Hyperemesis gravidarum n Endocrine or metabolic-thyrotoxicosis, DKA, Adrenal insufficiency n Neurologic-Vestibular, Migraine, encephalopathy, Hydrocephalus, Increased ICP (neoplasms, subdural, epidural, or subarrachnoid hemorrhage, cerebral edema) n Toxicology n Environmental-Food poisoning, envenomation, high altitude, acute radiation n Renal-Obstructive uropathy, renal colic n Infection- gastroenteritis (viral, bacterial, parasitic), pyelonephritis, pneumonia (pertussis, Legionella), PID, Meningitis, Hepatitis, colitis, HIV n Tumors-gastrinoma, thyroid ca, villous adenoma n Ischemia- MI, Mesenteric ischemia, ischemia colitis n Supratentorial- Bulemia, psychosocial stress 2/8/2018 7
Causes of Vomiting and Diarrhea GASTROENTERITIS MNEUMONIC n Gastrointestinal- Obstruction, Dymotility, Inflammation, Malabsorption, Lactose Intolerance, GI bleeding n Appendicitis or aorta n Specific diseases- Glaucoma, Torsion (ovary/testicle) n Trauma n Rx (prescription)-medication side effects n Obstetrics and Gynecology-pregnancy, preeclampsia, Hyperemesis gravidarum n Endocrine or metabolic-thyrotoxicosis, DKA, Adrenal insufficiency n Neurologic-Vestibular, Migraine, encephalopathy, Hydrocephalus, Increased ICP (neoplasms, subdural, epidural, or subarrachnoid hemorrhage, cerebral edema) n Toxicology n Environmental-Food poisoning, envenomation, high altitude, acute radiation n Renal-Obstructive uropathy, renal colic n Infection- gastroenteritis (viral, bacterial, parasitic), pyelonephritis, pneumonia (pertussis, Legionella), PID, Meningitis, Hepatitis, colitis, HIV n Tumors-gastrinoma, thyroid ca, villous adenoma n Ischemia- MI, Mesenteric ischemia, ischemia colitis n Supratentorial- Bulemia, psychosocial stress 2/8/2018 7
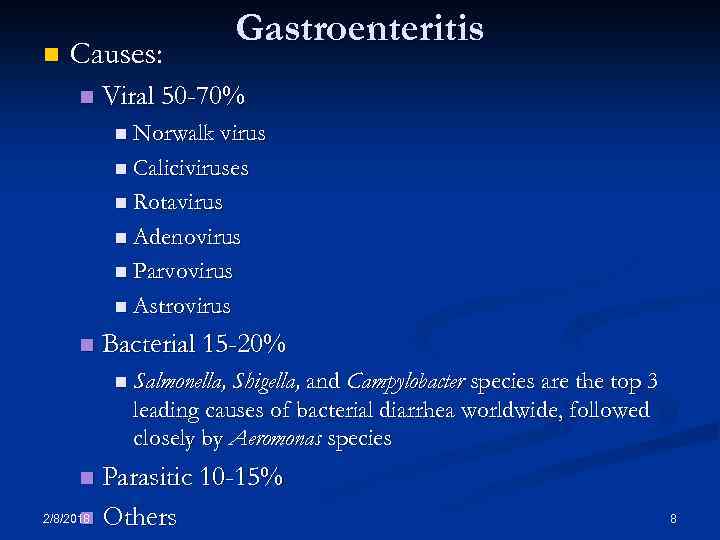 n Causes: n Gastroenteritis Viral 50 -70% n Norwalk virus n Caliciviruses n Rotavirus n Adenovirus n Parvovirus n Astrovirus n Bacterial 15 -20% n Salmonella, Shigella, and Campylobacter species are the top 3 leading causes of bacterial diarrhea worldwide, followed closely by Aeromonas species Parasitic 10 -15% 2/8/2018 Others n n 8
n Causes: n Gastroenteritis Viral 50 -70% n Norwalk virus n Caliciviruses n Rotavirus n Adenovirus n Parvovirus n Astrovirus n Bacterial 15 -20% n Salmonella, Shigella, and Campylobacter species are the top 3 leading causes of bacterial diarrhea worldwide, followed closely by Aeromonas species Parasitic 10 -15% 2/8/2018 Others n n 8
 Gastroenteritis Acute symptoms may follow a wide variety of infectious & chemical agents n Ingestion may occur as a result of person to person contact, more commonly via water or food n The majority of food borne illnesses are caused by staphylococcus from contaminated food aureus being allowed to stand, producing endotoxins. n Salmonella & Clostridium follow staph poisoning as most common. They are found in meats. n 2/8/2018 9
Gastroenteritis Acute symptoms may follow a wide variety of infectious & chemical agents n Ingestion may occur as a result of person to person contact, more commonly via water or food n The majority of food borne illnesses are caused by staphylococcus from contaminated food aureus being allowed to stand, producing endotoxins. n Salmonella & Clostridium follow staph poisoning as most common. They are found in meats. n 2/8/2018 9
 Gastroenteritis n Invasive Infection: The organism enters the mucosal cells, destroys them, causing diarrhea usually with blood in the stool. n Enterotoxic syndromes: The organisms do not invade the mucosa, but produce enterotoxins of which act as chemical mediators causing hypersecretion of the fluid. Little damage to the tissue is done. 2/8/2018 10
Gastroenteritis n Invasive Infection: The organism enters the mucosal cells, destroys them, causing diarrhea usually with blood in the stool. n Enterotoxic syndromes: The organisms do not invade the mucosa, but produce enterotoxins of which act as chemical mediators causing hypersecretion of the fluid. Little damage to the tissue is done. 2/8/2018 10
 Gastroenteritis Key Symptoms n Viral n n n n 2/8/2018 Abdominal cramps (#1) Vomiting Profuse watery stools Myalgias Fever Headaches Arthralgias n Bacterial Dysentery n n n Small volume stools Fever Tenesmus Bloody mucoid stools Suprapubic pain relieved by BM 11
Gastroenteritis Key Symptoms n Viral n n n n 2/8/2018 Abdominal cramps (#1) Vomiting Profuse watery stools Myalgias Fever Headaches Arthralgias n Bacterial Dysentery n n n Small volume stools Fever Tenesmus Bloody mucoid stools Suprapubic pain relieved by BM 11
 Gastroenteritis (cont. ) n Historical Information n 2/8/2018 History of suspicious food eaten within the last 48 hrs, eating an unusual food (special fish) in a restaurant, or preparing food in an unconventional container (copper). Or a hx of similar illness in others who ate with the patient. 12
Gastroenteritis (cont. ) n Historical Information n 2/8/2018 History of suspicious food eaten within the last 48 hrs, eating an unusual food (special fish) in a restaurant, or preparing food in an unconventional container (copper). Or a hx of similar illness in others who ate with the patient. 12
 Gastroenteritis (cont. ) n Physical Exam Findings Minimally helpful n Abdominal tenderness n Diarrhea causing dehydration n Fever- usually indicates organism invasion n Hypotension- usually indicates dehydration and electrolyte imbalance n Rectal Exam- “to bleed or not to bleed” n 2/8/2018 13
Gastroenteritis (cont. ) n Physical Exam Findings Minimally helpful n Abdominal tenderness n Diarrhea causing dehydration n Fever- usually indicates organism invasion n Hypotension- usually indicates dehydration and electrolyte imbalance n Rectal Exam- “to bleed or not to bleed” n 2/8/2018 13
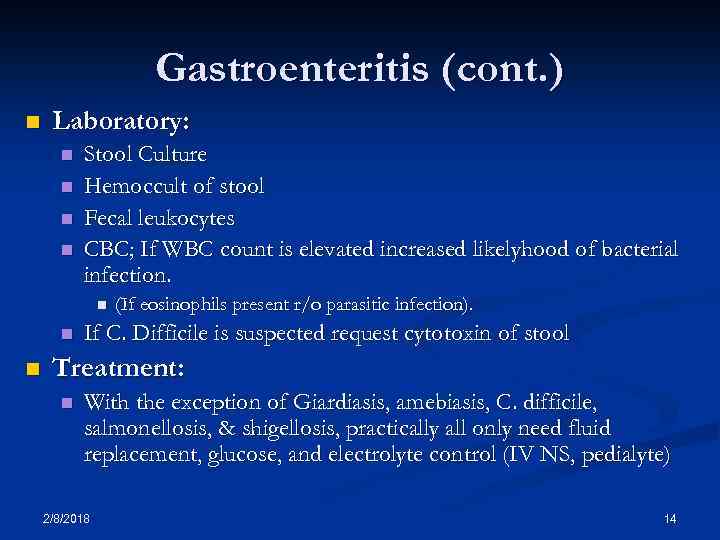 Gastroenteritis (cont. ) n Laboratory: n n Stool Culture Hemoccult of stool Fecal leukocytes CBC; If WBC count is elevated increased likelyhood of bacterial infection. n n n (If eosinophils present r/o parasitic infection). If C. Difficile is suspected request cytotoxin of stool Treatment: n With the exception of Giardiasis, amebiasis, C. difficile, salmonellosis, & shigellosis, practically all only need fluid replacement, glucose, and electrolyte control (IV NS, pedialyte) 2/8/2018 14
Gastroenteritis (cont. ) n Laboratory: n n Stool Culture Hemoccult of stool Fecal leukocytes CBC; If WBC count is elevated increased likelyhood of bacterial infection. n n n (If eosinophils present r/o parasitic infection). If C. Difficile is suspected request cytotoxin of stool Treatment: n With the exception of Giardiasis, amebiasis, C. difficile, salmonellosis, & shigellosis, practically all only need fluid replacement, glucose, and electrolyte control (IV NS, pedialyte) 2/8/2018 14
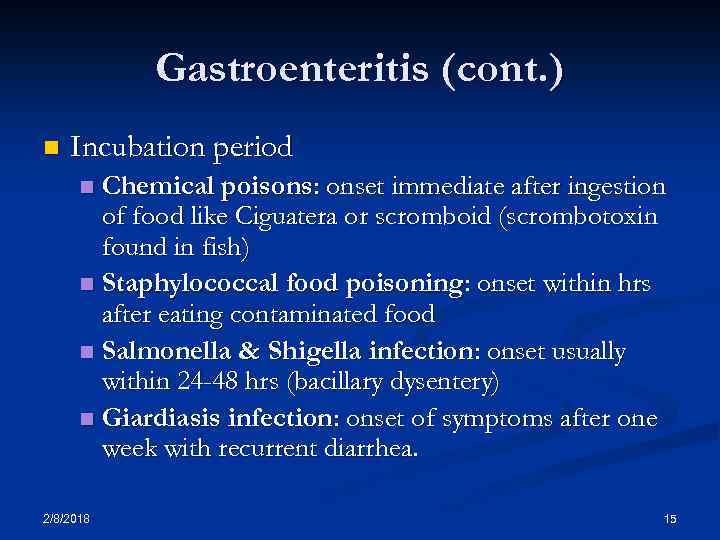 Gastroenteritis (cont. ) n Incubation period Chemical poisons: onset immediate after ingestion of food like Ciguatera or scromboid (scrombotoxin found in fish) n Staphylococcal food poisoning: onset within hrs after eating contaminated food n Salmonella & Shigella infection: onset usually within 24 -48 hrs (bacillary dysentery) n Giardiasis infection: onset of symptoms after one week with recurrent diarrhea. n 2/8/2018 15
Gastroenteritis (cont. ) n Incubation period Chemical poisons: onset immediate after ingestion of food like Ciguatera or scromboid (scrombotoxin found in fish) n Staphylococcal food poisoning: onset within hrs after eating contaminated food n Salmonella & Shigella infection: onset usually within 24 -48 hrs (bacillary dysentery) n Giardiasis infection: onset of symptoms after one week with recurrent diarrhea. n 2/8/2018 15
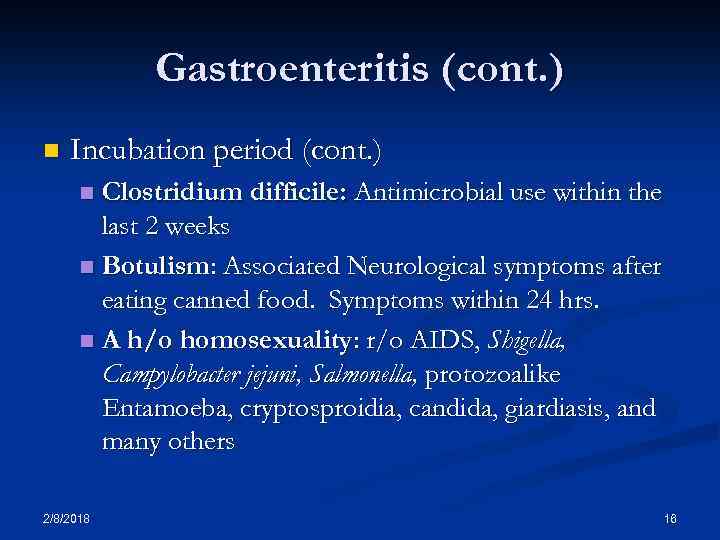 Gastroenteritis (cont. ) n Incubation period (cont. ) Clostridium difficile: Antimicrobial use within the last 2 weeks n Botulism: Associated Neurological symptoms after eating canned food. Symptoms within 24 hrs. n A h/o homosexuality: r/o AIDS, Shigella, Campylobacter jejuni, Salmonella, protozoalike Entamoeba, cryptosproidia, candida, giardiasis, and many others n 2/8/2018 16
Gastroenteritis (cont. ) n Incubation period (cont. ) Clostridium difficile: Antimicrobial use within the last 2 weeks n Botulism: Associated Neurological symptoms after eating canned food. Symptoms within 24 hrs. n A h/o homosexuality: r/o AIDS, Shigella, Campylobacter jejuni, Salmonella, protozoalike Entamoeba, cryptosproidia, candida, giardiasis, and many others n 2/8/2018 16
 Gastrointestinal Infectious Disorders Viral n Staphlococcal n Cholera n Shigellosis n Salmonella n Hemorrhagic Colitis (E. coli O 157: H 7) n Pseudomembranous Colitis (C. difficile) n Enterotoxigenic E. coli n 2/8/2018 17
Gastrointestinal Infectious Disorders Viral n Staphlococcal n Cholera n Shigellosis n Salmonella n Hemorrhagic Colitis (E. coli O 157: H 7) n Pseudomembranous Colitis (C. difficile) n Enterotoxigenic E. coli n 2/8/2018 17
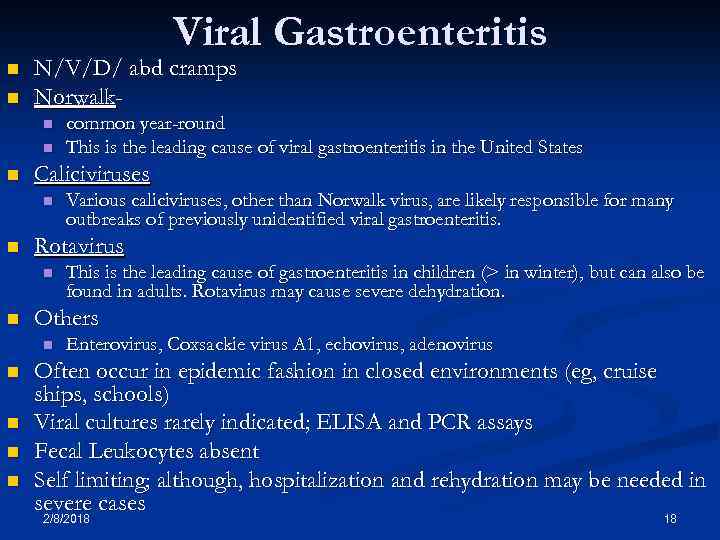 Viral Gastroenteritis n n N/V/D/ abd cramps Norwalkn n n Caliciviruses n n n This is the leading cause of gastroenteritis in children (> in winter), but can also be found in adults. Rotavirus may cause severe dehydration. Others n n Various caliciviruses, other than Norwalk virus, are likely responsible for many outbreaks of previously unidentified viral gastroenteritis. Rotavirus n n common year-round This is the leading cause of viral gastroenteritis in the United States Enterovirus, Coxsackie virus A 1, echovirus, adenovirus Often occur in epidemic fashion in closed environments (eg, cruise ships, schools) Viral cultures rarely indicated; ELISA and PCR assays Fecal Leukocytes absent Self limiting; although, hospitalization and rehydration may be needed in severe cases 2/8/2018 18
Viral Gastroenteritis n n N/V/D/ abd cramps Norwalkn n n Caliciviruses n n n This is the leading cause of gastroenteritis in children (> in winter), but can also be found in adults. Rotavirus may cause severe dehydration. Others n n Various caliciviruses, other than Norwalk virus, are likely responsible for many outbreaks of previously unidentified viral gastroenteritis. Rotavirus n n common year-round This is the leading cause of viral gastroenteritis in the United States Enterovirus, Coxsackie virus A 1, echovirus, adenovirus Often occur in epidemic fashion in closed environments (eg, cruise ships, schools) Viral cultures rarely indicated; ELISA and PCR assays Fecal Leukocytes absent Self limiting; although, hospitalization and rehydration may be needed in severe cases 2/8/2018 18
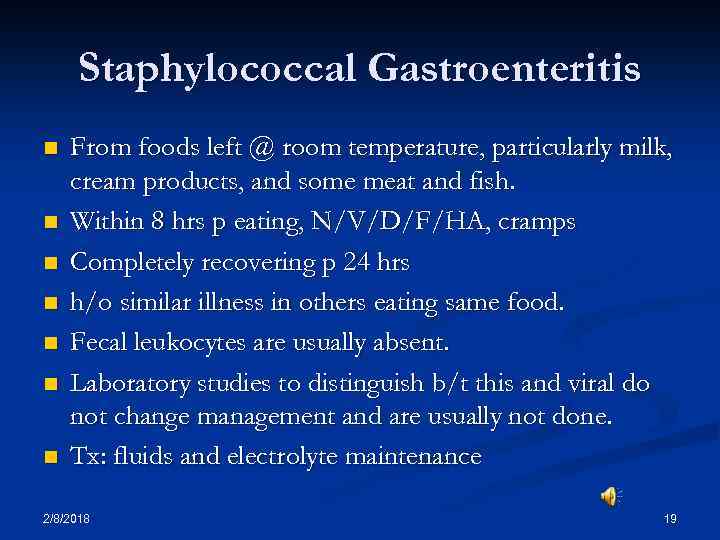 Staphylococcal Gastroenteritis n n n n From foods left @ room temperature, particularly milk, cream products, and some meat and fish. Within 8 hrs p eating, N/V/D/F/HA, cramps Completely recovering p 24 hrs h/o similar illness in others eating same food. Fecal leukocytes are usually absent. Laboratory studies to distinguish b/t this and viral do not change management and are usually not done. Tx: fluids and electrolyte maintenance 2/8/2018 19
Staphylococcal Gastroenteritis n n n n From foods left @ room temperature, particularly milk, cream products, and some meat and fish. Within 8 hrs p eating, N/V/D/F/HA, cramps Completely recovering p 24 hrs h/o similar illness in others eating same food. Fecal leukocytes are usually absent. Laboratory studies to distinguish b/t this and viral do not change management and are usually not done. Tx: fluids and electrolyte maintenance 2/8/2018 19
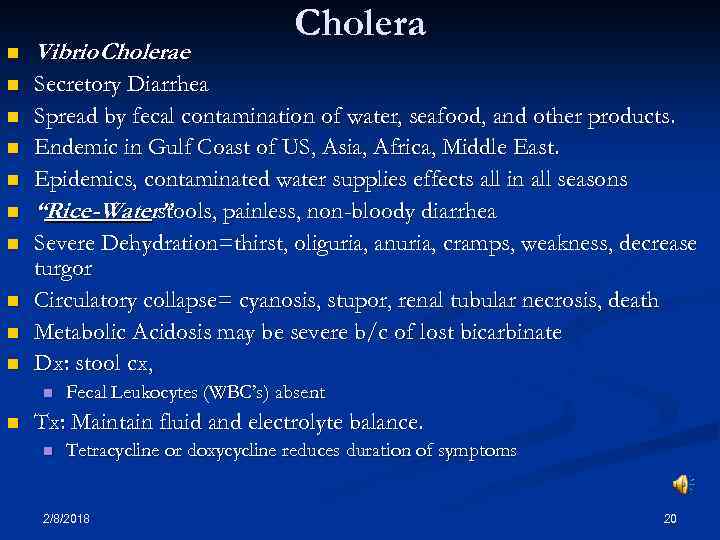 Cholera n Vibrio Cholerae n Secretory Diarrhea Spread by fecal contamination of water, seafood, and other products. Endemic in Gulf Coast of US, Asia, Africa, Middle East. Epidemics, contaminated water supplies effects all in all seasons “Rice-Water” stools, painless, non-bloody diarrhea Severe Dehydration=thirst, oliguria, anuria, cramps, weakness, decrease turgor Circulatory collapse= cyanosis, stupor, renal tubular necrosis, death Metabolic Acidosis may be severe b/c of lost bicarbinate Dx: stool cx, n n n n n Fecal Leukocytes (WBC’s) absent Tx: Maintain fluid and electrolyte balance. n Tetracycline or doxycycline reduces duration of symptoms 2/8/2018 20
Cholera n Vibrio Cholerae n Secretory Diarrhea Spread by fecal contamination of water, seafood, and other products. Endemic in Gulf Coast of US, Asia, Africa, Middle East. Epidemics, contaminated water supplies effects all in all seasons “Rice-Water” stools, painless, non-bloody diarrhea Severe Dehydration=thirst, oliguria, anuria, cramps, weakness, decrease turgor Circulatory collapse= cyanosis, stupor, renal tubular necrosis, death Metabolic Acidosis may be severe b/c of lost bicarbinate Dx: stool cx, n n n n n Fecal Leukocytes (WBC’s) absent Tx: Maintain fluid and electrolyte balance. n Tetracycline or doxycycline reduces duration of symptoms 2/8/2018 20
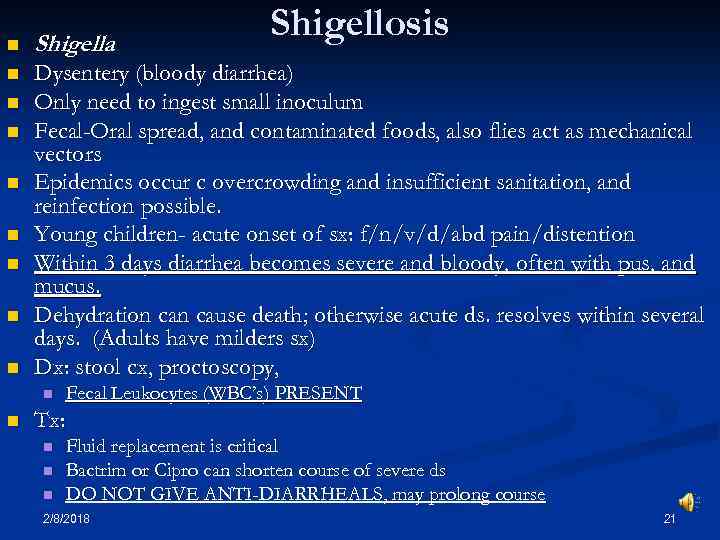 Shigellosis n Shigella n Dysentery (bloody diarrhea) Only need to ingest small inoculum Fecal-Oral spread, and contaminated foods, also flies act as mechanical vectors Epidemics occur c overcrowding and insufficient sanitation, and reinfection possible. Young children- acute onset of sx: f/n/v/d/abd pain/distention Within 3 days diarrhea becomes severe and bloody, often with pus, and mucus. Dehydration cause death; otherwise acute ds. resolves within several days. (Adults have milders sx) Dx: stool cx, proctoscopy, n n n n n Fecal Leukocytes (WBC’s) PRESENT Tx: n n n Fluid replacement is critical Bactrim or Cipro can shorten course of severe ds DO NOT GIVE ANTI-DIARRHEALS, may prolong course 2/8/2018 21
Shigellosis n Shigella n Dysentery (bloody diarrhea) Only need to ingest small inoculum Fecal-Oral spread, and contaminated foods, also flies act as mechanical vectors Epidemics occur c overcrowding and insufficient sanitation, and reinfection possible. Young children- acute onset of sx: f/n/v/d/abd pain/distention Within 3 days diarrhea becomes severe and bloody, often with pus, and mucus. Dehydration cause death; otherwise acute ds. resolves within several days. (Adults have milders sx) Dx: stool cx, proctoscopy, n n n n n Fecal Leukocytes (WBC’s) PRESENT Tx: n n n Fluid replacement is critical Bactrim or Cipro can shorten course of severe ds DO NOT GIVE ANTI-DIARRHEALS, may prolong course 2/8/2018 21
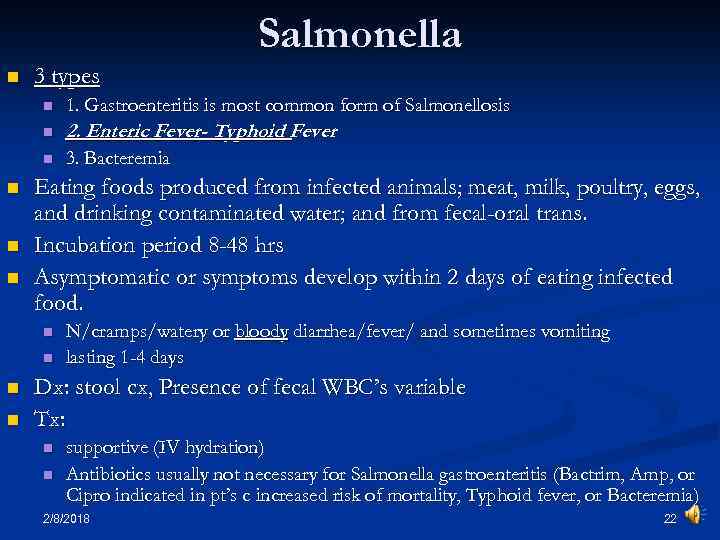 Salmonella n 3 types n n 2. Enteric Fever- Typhoid Fever n n 1. Gastroenteritis is most common form of Salmonellosis 3. Bacteremia Eating foods produced from infected animals; meat, milk, poultry, eggs, and drinking contaminated water; and from fecal-oral trans. Incubation period 8 -48 hrs Asymptomatic or symptoms develop within 2 days of eating infected food. n n N/cramps/watery or bloody diarrhea/fever/ and sometimes vomiting lasting 1 -4 days Dx: stool cx, Presence of fecal WBC’s variable Tx: n n supportive (IV hydration) Antibiotics usually not necessary for Salmonella gastroenteritis (Bactrim, Amp, or Cipro indicated in pt’s c increased risk of mortality, Typhoid fever, or Bacteremia) 2/8/2018 22
Salmonella n 3 types n n 2. Enteric Fever- Typhoid Fever n n 1. Gastroenteritis is most common form of Salmonellosis 3. Bacteremia Eating foods produced from infected animals; meat, milk, poultry, eggs, and drinking contaminated water; and from fecal-oral trans. Incubation period 8 -48 hrs Asymptomatic or symptoms develop within 2 days of eating infected food. n n N/cramps/watery or bloody diarrhea/fever/ and sometimes vomiting lasting 1 -4 days Dx: stool cx, Presence of fecal WBC’s variable Tx: n n supportive (IV hydration) Antibiotics usually not necessary for Salmonella gastroenteritis (Bactrim, Amp, or Cipro indicated in pt’s c increased risk of mortality, Typhoid fever, or Bacteremia) 2/8/2018 22
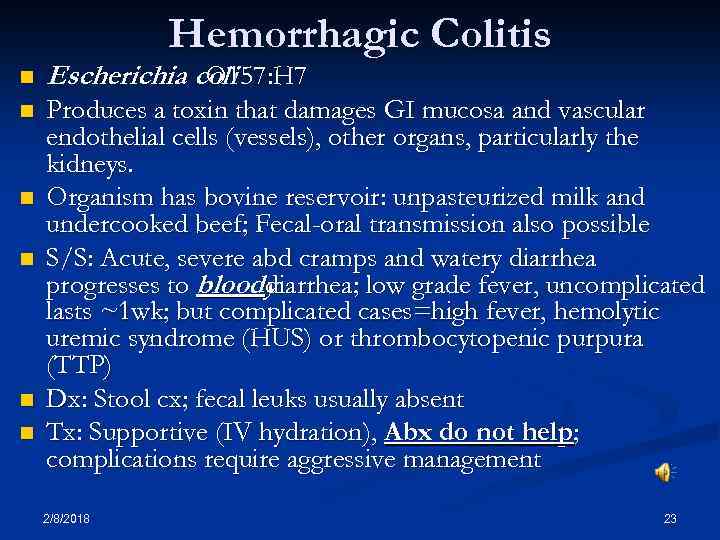 Hemorrhagic Colitis n Escherichia coli O 157: H 7 n Produces a toxin that damages GI mucosa and vascular endothelial cells (vessels), other organs, particularly the kidneys. Organism has bovine reservoir: unpasteurized milk and undercooked beef; Fecal-oral transmission also possible S/S: Acute, severe abd cramps and watery diarrhea progresses to bloody diarrhea; low grade fever, uncomplicated lasts ~1 wk; but complicated cases=high fever, hemolytic uremic syndrome (HUS) or thrombocytopenic purpura (TTP) Dx: Stool cx; fecal leuks usually absent Tx: Supportive (IV hydration), Abx do not help; complications require aggressive management n n 2/8/2018 23
Hemorrhagic Colitis n Escherichia coli O 157: H 7 n Produces a toxin that damages GI mucosa and vascular endothelial cells (vessels), other organs, particularly the kidneys. Organism has bovine reservoir: unpasteurized milk and undercooked beef; Fecal-oral transmission also possible S/S: Acute, severe abd cramps and watery diarrhea progresses to bloody diarrhea; low grade fever, uncomplicated lasts ~1 wk; but complicated cases=high fever, hemolytic uremic syndrome (HUS) or thrombocytopenic purpura (TTP) Dx: Stool cx; fecal leuks usually absent Tx: Supportive (IV hydration), Abx do not help; complications require aggressive management n n 2/8/2018 23
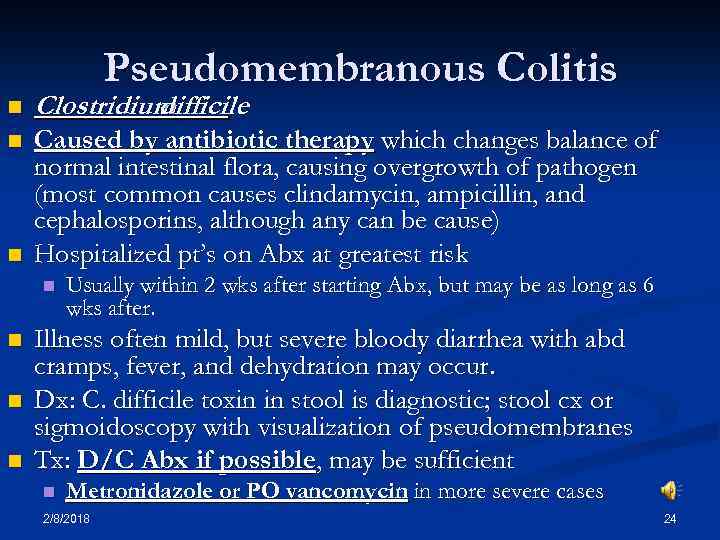 Pseudomembranous Colitis n Clostridium difficile n Caused by antibiotic therapy which changes balance of normal intestinal flora, causing overgrowth of pathogen (most common causes clindamycin, ampicillin, and cephalosporins, although any can be cause) Hospitalized pt’s on Abx at greatest risk n n n Usually within 2 wks after starting Abx, but may be as long as 6 wks after. Illness often mild, but severe bloody diarrhea with abd cramps, fever, and dehydration may occur. Dx: C. difficile toxin in stool is diagnostic; stool cx or sigmoidoscopy with visualization of pseudomembranes Tx: D/C Abx if possible, may be sufficient n Metronidazole or PO vancomycin in more severe cases 2/8/2018 24
Pseudomembranous Colitis n Clostridium difficile n Caused by antibiotic therapy which changes balance of normal intestinal flora, causing overgrowth of pathogen (most common causes clindamycin, ampicillin, and cephalosporins, although any can be cause) Hospitalized pt’s on Abx at greatest risk n n n Usually within 2 wks after starting Abx, but may be as long as 6 wks after. Illness often mild, but severe bloody diarrhea with abd cramps, fever, and dehydration may occur. Dx: C. difficile toxin in stool is diagnostic; stool cx or sigmoidoscopy with visualization of pseudomembranes Tx: D/C Abx if possible, may be sufficient n Metronidazole or PO vancomycin in more severe cases 2/8/2018 24
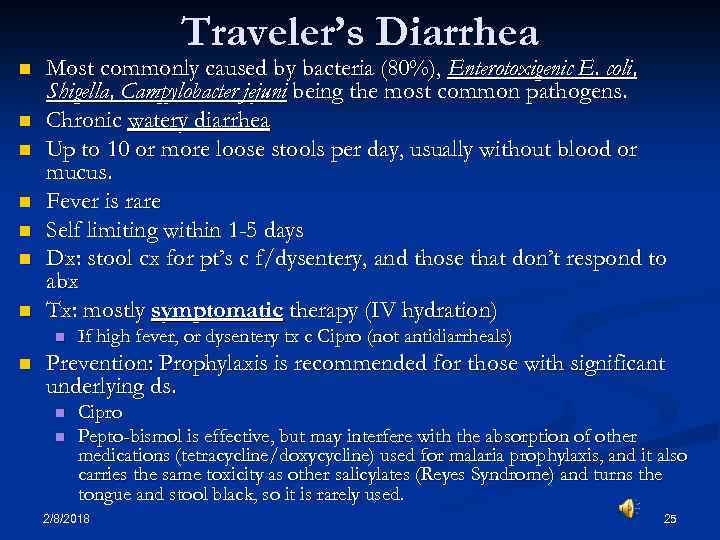 Traveler’s Diarrhea n n n n Most commonly caused by bacteria (80%), Enterotoxigenic E. coli, Shigella, Campylobacter jejuni being the most common pathogens. Chronic watery diarrhea Up to 10 or more loose stools per day, usually without blood or mucus. Fever is rare Self limiting within 1 -5 days Dx: stool cx for pt’s c f/dysentery, and those that don’t respond to abx Tx: mostly symptomatic therapy (IV hydration) n n If high fever, or dysentery tx c Cipro (not antidiarrheals) Prevention: Prophylaxis is recommended for those with significant underlying ds. n n Cipro Pepto-bismol is effective, but may interfere with the absorption of other medications (tetracycline/doxycycline) used for malaria prophylaxis, and it also carries the same toxicity as other salicylates (Reyes Syndrome) and turns the tongue and stool black, so it is rarely used. 2/8/2018 25
Traveler’s Diarrhea n n n n Most commonly caused by bacteria (80%), Enterotoxigenic E. coli, Shigella, Campylobacter jejuni being the most common pathogens. Chronic watery diarrhea Up to 10 or more loose stools per day, usually without blood or mucus. Fever is rare Self limiting within 1 -5 days Dx: stool cx for pt’s c f/dysentery, and those that don’t respond to abx Tx: mostly symptomatic therapy (IV hydration) n n If high fever, or dysentery tx c Cipro (not antidiarrheals) Prevention: Prophylaxis is recommended for those with significant underlying ds. n n Cipro Pepto-bismol is effective, but may interfere with the absorption of other medications (tetracycline/doxycycline) used for malaria prophylaxis, and it also carries the same toxicity as other salicylates (Reyes Syndrome) and turns the tongue and stool black, so it is rarely used. 2/8/2018 25
 General Bacterial Overgrowth Treatment Usually self limiting n IV hydration n Correct the anatomic defect when possible. n Empiric antibiotic trial can be used as a diagnostic and therapeutic maneuver. n Ciprofloxacin (or combo c Metronidazole) n (However often not necessary, unless dysenteric) 2/8/2018 26
General Bacterial Overgrowth Treatment Usually self limiting n IV hydration n Correct the anatomic defect when possible. n Empiric antibiotic trial can be used as a diagnostic and therapeutic maneuver. n Ciprofloxacin (or combo c Metronidazole) n (However often not necessary, unless dysenteric) 2/8/2018 26
 Protozoal Infection 2/8/2018 27
Protozoal Infection 2/8/2018 27
 Protozoal infection signs/symptoms n n n Abdominal pain Wheezing or hemoptysis due to pulmonary migration of larva (lofflers syndrome) Dermatitis Diarrhea Dysentery 2/8/2018 n n n Pruritis Rectal Prolapse Steatorrhea Passage of parasites Bowel obstruction (as found in taenia and ascarisis) 28
Protozoal infection signs/symptoms n n n Abdominal pain Wheezing or hemoptysis due to pulmonary migration of larva (lofflers syndrome) Dermatitis Diarrhea Dysentery 2/8/2018 n n n Pruritis Rectal Prolapse Steatorrhea Passage of parasites Bowel obstruction (as found in taenia and ascarisis) 28
 Protozoal Infections n History n n n n 2/8/2018 Travel to underdeveloped areas Outbreak of associated illness (Giardia, Trichinella) Daycare exposure (Giardia) Homosexual behavior (Giardia, Entamoebia) Animal Exposure Diet: uncooked foods Immunocompromised n Physical Findings n n n Weight loss Excessive gas or abdominal distention Hyperperistalsis Perianal infection Wheezing 29
Protozoal Infections n History n n n n 2/8/2018 Travel to underdeveloped areas Outbreak of associated illness (Giardia, Trichinella) Daycare exposure (Giardia) Homosexual behavior (Giardia, Entamoebia) Animal Exposure Diet: uncooked foods Immunocompromised n Physical Findings n n n Weight loss Excessive gas or abdominal distention Hyperperistalsis Perianal infection Wheezing 29
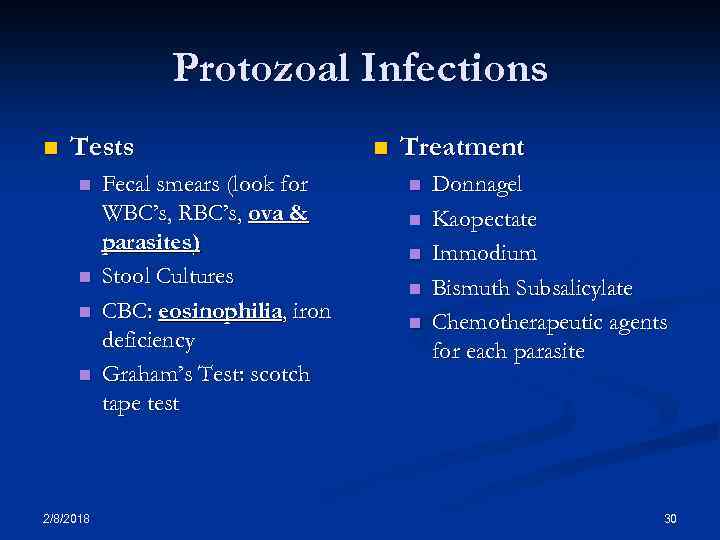 Protozoal Infections n Tests n n 2/8/2018 Fecal smears (look for WBC’s, RBC’s, ova & parasites) Stool Cultures CBC: eosinophilia, iron deficiency Graham’s Test: scotch tape test n Treatment n n n Donnagel Kaopectate Immodium Bismuth Subsalicylate Chemotherapeutic agents for each parasite 30
Protozoal Infections n Tests n n 2/8/2018 Fecal smears (look for WBC’s, RBC’s, ova & parasites) Stool Cultures CBC: eosinophilia, iron deficiency Graham’s Test: scotch tape test n Treatment n n n Donnagel Kaopectate Immodium Bismuth Subsalicylate Chemotherapeutic agents for each parasite 30
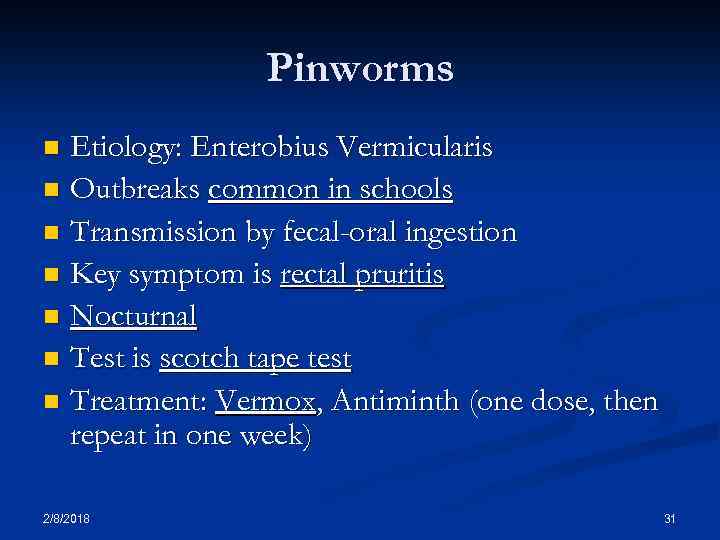 Pinworms Etiology: Enterobius Vermicularis n Outbreaks common in schools n Transmission by fecal-oral ingestion n Key symptom is rectal pruritis n Nocturnal n Test is scotch tape test n Treatment: Vermox, Antiminth (one dose, then repeat in one week) n 2/8/2018 31
Pinworms Etiology: Enterobius Vermicularis n Outbreaks common in schools n Transmission by fecal-oral ingestion n Key symptom is rectal pruritis n Nocturnal n Test is scotch tape test n Treatment: Vermox, Antiminth (one dose, then repeat in one week) n 2/8/2018 31
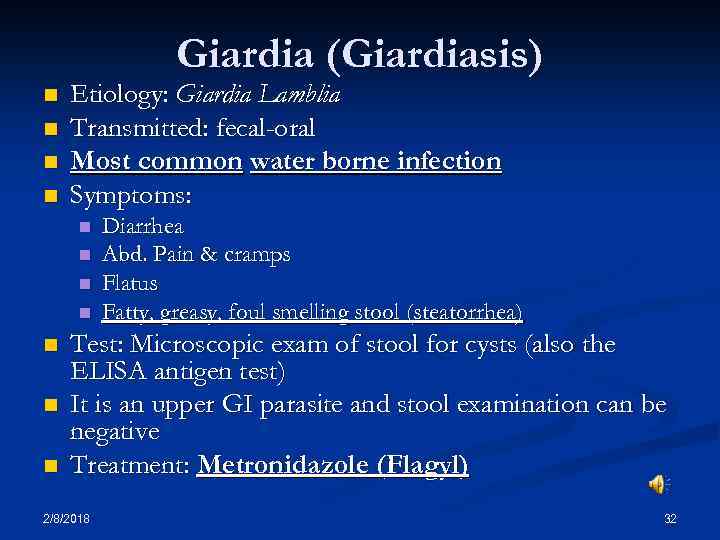 Giardia (Giardiasis) n n Etiology: Giardia Lamblia Transmitted: fecal-oral Most common water borne infection Symptoms: n n n n Diarrhea Abd. Pain & cramps Flatus Fatty, greasy, foul smelling stool (steatorrhea) Test: Microscopic exam of stool for cysts (also the ELISA antigen test) It is an upper GI parasite and stool examination can be negative Treatment: Metronidazole (Flagyl) 2/8/2018 32
Giardia (Giardiasis) n n Etiology: Giardia Lamblia Transmitted: fecal-oral Most common water borne infection Symptoms: n n n n Diarrhea Abd. Pain & cramps Flatus Fatty, greasy, foul smelling stool (steatorrhea) Test: Microscopic exam of stool for cysts (also the ELISA antigen test) It is an upper GI parasite and stool examination can be negative Treatment: Metronidazole (Flagyl) 2/8/2018 32
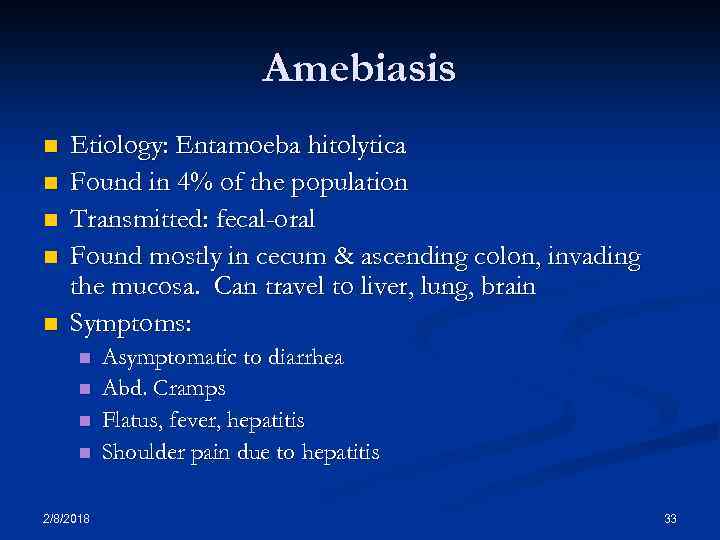 Amebiasis n n n Etiology: Entamoeba hitolytica Found in 4% of the population Transmitted: fecal-oral Found mostly in cecum & ascending colon, invading the mucosa. Can travel to liver, lung, brain Symptoms: n n 2/8/2018 Asymptomatic to diarrhea Abd. Cramps Flatus, fever, hepatitis Shoulder pain due to hepatitis 33
Amebiasis n n n Etiology: Entamoeba hitolytica Found in 4% of the population Transmitted: fecal-oral Found mostly in cecum & ascending colon, invading the mucosa. Can travel to liver, lung, brain Symptoms: n n 2/8/2018 Asymptomatic to diarrhea Abd. Cramps Flatus, fever, hepatitis Shoulder pain due to hepatitis 33
 Amebiasis (cont. ) n Signs: range n n n Test: n n No symptoms – no signs Bloody diarrhea Perianal ulcers RUQ tenderness Pulmonary (pneumonia- emphysema) Examine stool for cyst –trophozoites Treatment: n 2/8/2018 Metronidazole (Flagyl) 34
Amebiasis (cont. ) n Signs: range n n n Test: n n No symptoms – no signs Bloody diarrhea Perianal ulcers RUQ tenderness Pulmonary (pneumonia- emphysema) Examine stool for cyst –trophozoites Treatment: n 2/8/2018 Metronidazole (Flagyl) 34
 Ascariasis n n n Most common intestinal helminth Etiology: Ascaris lumbricoides (the large intestine round worm) Transmitted by contaminated food n n n Human feces as fertilizer Pulmonary phase (Loffler’s syndrome) Intestinal phase (eggs in stool) Penetrate the intestine & invade liver, lung, heart Tx: Albendazole and Pyrantel pamoate 2/8/2018 35
Ascariasis n n n Most common intestinal helminth Etiology: Ascaris lumbricoides (the large intestine round worm) Transmitted by contaminated food n n n Human feces as fertilizer Pulmonary phase (Loffler’s syndrome) Intestinal phase (eggs in stool) Penetrate the intestine & invade liver, lung, heart Tx: Albendazole and Pyrantel pamoate 2/8/2018 35
 Tapeworms Cestodes (segmented worms) n Taenia solium n Adults live in GI tract, larvae can be found in almost any organ (neuro, muscle, eye) (cysticercosis ) n Fish, beef, pork, dog , cats, fleas, snakes, birds, and other mammals can carry the tapeworm larva, humans can be the definitive host or the intermediate host n From 5 mm to over 25 meters in length n 2/8/2018 36
Tapeworms Cestodes (segmented worms) n Taenia solium n Adults live in GI tract, larvae can be found in almost any organ (neuro, muscle, eye) (cysticercosis ) n Fish, beef, pork, dog , cats, fleas, snakes, birds, and other mammals can carry the tapeworm larva, humans can be the definitive host or the intermediate host n From 5 mm to over 25 meters in length n 2/8/2018 36
 Whipworm (Trichuriasis) n n n n Humans are the only host for this whipworm and one of the most common parasitic infections in the U. S. The worm lives in the cecum and appendix One female produces several thousand eggs/day Fecal-oral transm. , uncooked veggies, & water Symptoms: allergic rxns, anemia, vague GI complaints, diarrhea & abd. distention Diagnosis: stool examination Tx: Albendazole, Mebendazole 2/8/2018 37
Whipworm (Trichuriasis) n n n n Humans are the only host for this whipworm and one of the most common parasitic infections in the U. S. The worm lives in the cecum and appendix One female produces several thousand eggs/day Fecal-oral transm. , uncooked veggies, & water Symptoms: allergic rxns, anemia, vague GI complaints, diarrhea & abd. distention Diagnosis: stool examination Tx: Albendazole, Mebendazole 2/8/2018 37
 Diarrhea 2/8/2018 38
Diarrhea 2/8/2018 38
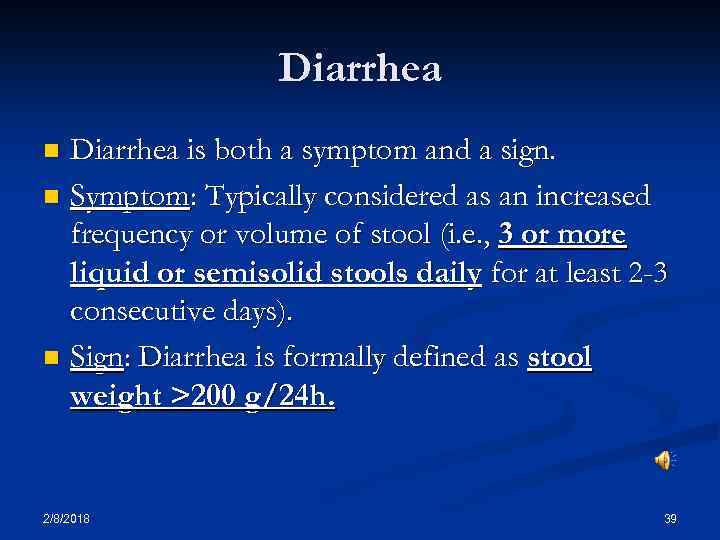 Diarrhea is both a symptom and a sign. n Symptom: Typically considered as an increased frequency or volume of stool (i. e. , 3 or more liquid or semisolid stools daily for at least 2 -3 consecutive days). n Sign: Diarrhea is formally defined as stool weight >200 g/24 h. n 2/8/2018 39
Diarrhea is both a symptom and a sign. n Symptom: Typically considered as an increased frequency or volume of stool (i. e. , 3 or more liquid or semisolid stools daily for at least 2 -3 consecutive days). n Sign: Diarrhea is formally defined as stool weight >200 g/24 h. n 2/8/2018 39
 Diarrhea n Causes of diarrhea n n n Psychogenic Surgical Endocrine Carcinoid tumors Mechanical n Neoplasm Foreign body n n Chemical n n Bacterial Parasitic Saline Cathartics Dietary Allergic Malabsorption n 2/8/2018 Tropical sprue Celiac ds. Whipple’s ds. 40
Diarrhea n Causes of diarrhea n n n Psychogenic Surgical Endocrine Carcinoid tumors Mechanical n Neoplasm Foreign body n n Chemical n n Bacterial Parasitic Saline Cathartics Dietary Allergic Malabsorption n 2/8/2018 Tropical sprue Celiac ds. Whipple’s ds. 40
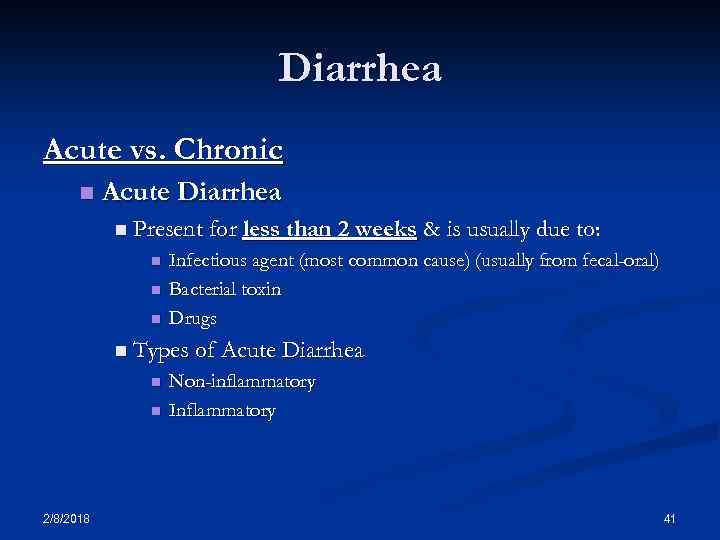 Diarrhea Acute vs. Chronic n Acute Diarrhea n Present for less than 2 weeks n n n & is usually due to: Infectious agent (most common cause) (usually from fecal-oral) Bacterial toxin Drugs n Types of Acute Diarrhea n n 2/8/2018 Non-inflammatory Inflammatory 41
Diarrhea Acute vs. Chronic n Acute Diarrhea n Present for less than 2 weeks n n n & is usually due to: Infectious agent (most common cause) (usually from fecal-oral) Bacterial toxin Drugs n Types of Acute Diarrhea n n 2/8/2018 Non-inflammatory Inflammatory 41
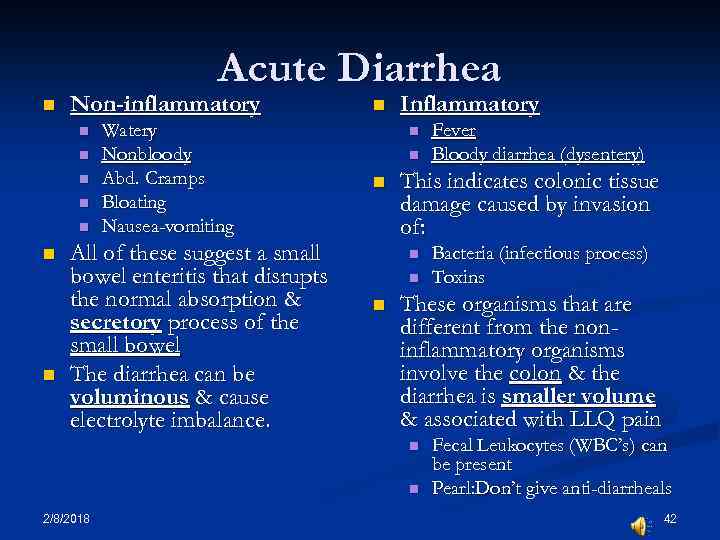 Acute Diarrhea n Non-inflammatory n n n n Watery Nonbloody Abd. Cramps Bloating Nausea-vomiting All of these suggest a small bowel enteritis that disrupts the normal absorption & secretory process of the small bowel The diarrhea can be voluminous & cause electrolyte imbalance. n Inflammatory n n n This indicates colonic tissue damage caused by invasion of: n n n Bacteria (infectious process) Toxins These organisms that are different from the noninflammatory organisms involve the colon & the diarrhea is smaller volume & associated with LLQ pain n n 2/8/2018 Fever Bloody diarrhea (dysentery) Fecal Leukocytes (WBC’s) can be present Pearl: Don’t give anti-diarrheals 42
Acute Diarrhea n Non-inflammatory n n n n Watery Nonbloody Abd. Cramps Bloating Nausea-vomiting All of these suggest a small bowel enteritis that disrupts the normal absorption & secretory process of the small bowel The diarrhea can be voluminous & cause electrolyte imbalance. n Inflammatory n n n This indicates colonic tissue damage caused by invasion of: n n n Bacteria (infectious process) Toxins These organisms that are different from the noninflammatory organisms involve the colon & the diarrhea is smaller volume & associated with LLQ pain n n 2/8/2018 Fever Bloody diarrhea (dysentery) Fecal Leukocytes (WBC’s) can be present Pearl: Don’t give anti-diarrheals 42
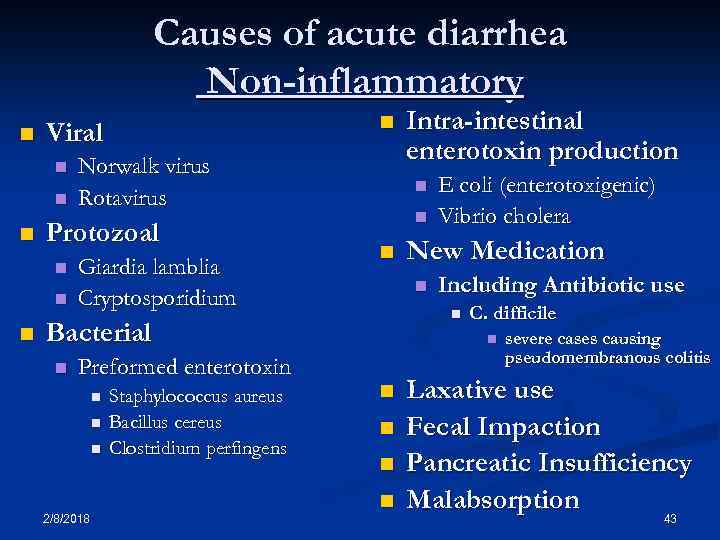 Causes of acute diarrhea Non-inflammatory n n Norwalk virus Rotavirus Protozoal n n Viral Giardia lamblia Cryptosporidium n n n Preformed enterotoxin n 2/8/2018 Staphylococcus aureus Bacillus cereus Clostridium perfingens E coli (enterotoxigenic) Vibrio cholera New Medication n Including Antibiotic use n Bacterial n Intra-intestinal enterotoxin production C. difficile n n n severe cases causing pseudomembranous colitis Laxative use Fecal Impaction Pancreatic Insufficiency Malabsorption 43
Causes of acute diarrhea Non-inflammatory n n Norwalk virus Rotavirus Protozoal n n Viral Giardia lamblia Cryptosporidium n n n Preformed enterotoxin n 2/8/2018 Staphylococcus aureus Bacillus cereus Clostridium perfingens E coli (enterotoxigenic) Vibrio cholera New Medication n Including Antibiotic use n Bacterial n Intra-intestinal enterotoxin production C. difficile n n n severe cases causing pseudomembranous colitis Laxative use Fecal Impaction Pancreatic Insufficiency Malabsorption 43
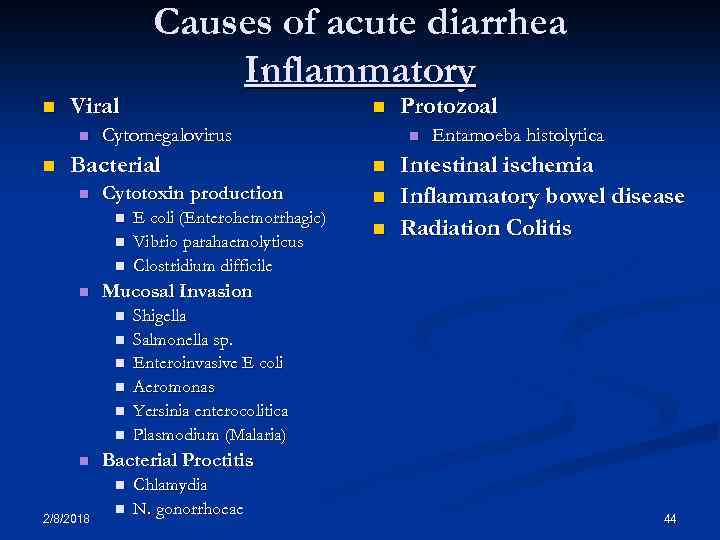 n Viral n n Causes of acute diarrhea Inflammatory n Cytomegalovirus Bacterial n Cytotoxin production n n n Entamoeba histolytica Intestinal ischemia Inflammatory bowel disease Radiation Colitis Shigella Salmonella sp. Enteroinvasive E coli Aeromonas Yersinia enterocolitica Plasmodium (Malaria) Bacterial Proctitis n 2/8/2018 n Mucosal Invasion n n E coli (Enterohemorrhagic) Vibrio parahaemolyticus Clostridium difficile Protozoal n Chlamydia N. gonorrhoeae 44
n Viral n n Causes of acute diarrhea Inflammatory n Cytomegalovirus Bacterial n Cytotoxin production n n n Entamoeba histolytica Intestinal ischemia Inflammatory bowel disease Radiation Colitis Shigella Salmonella sp. Enteroinvasive E coli Aeromonas Yersinia enterocolitica Plasmodium (Malaria) Bacterial Proctitis n 2/8/2018 n Mucosal Invasion n n E coli (Enterohemorrhagic) Vibrio parahaemolyticus Clostridium difficile Protozoal n Chlamydia N. gonorrhoeae 44
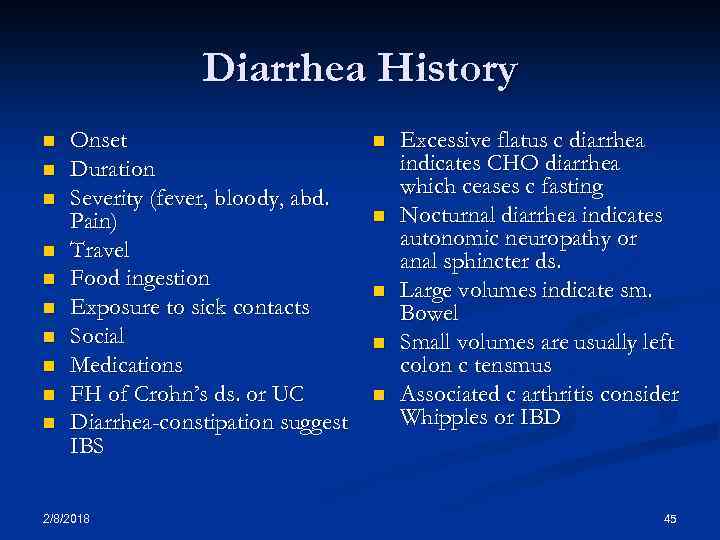 Diarrhea History n n n n n Onset Duration Severity (fever, bloody, abd. Pain) Travel Food ingestion Exposure to sick contacts Social Medications FH of Crohn’s ds. or UC Diarrhea-constipation suggest IBS 2/8/2018 n n n Excessive flatus c diarrhea indicates CHO diarrhea which ceases c fasting Nocturnal diarrhea indicates autonomic neuropathy or anal sphincter ds. Large volumes indicate sm. Bowel Small volumes are usually left colon c tensmus Associated c arthritis consider Whipples or IBD 45
Diarrhea History n n n n n Onset Duration Severity (fever, bloody, abd. Pain) Travel Food ingestion Exposure to sick contacts Social Medications FH of Crohn’s ds. or UC Diarrhea-constipation suggest IBS 2/8/2018 n n n Excessive flatus c diarrhea indicates CHO diarrhea which ceases c fasting Nocturnal diarrhea indicates autonomic neuropathy or anal sphincter ds. Large volumes indicate sm. Bowel Small volumes are usually left colon c tensmus Associated c arthritis consider Whipples or IBD 45
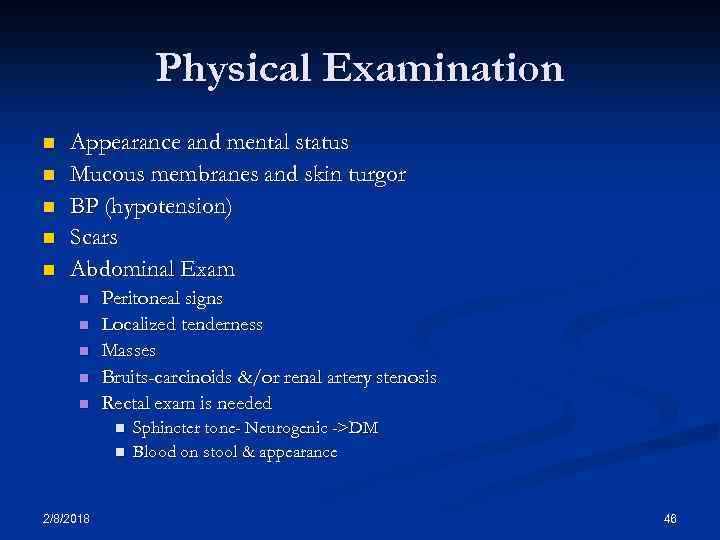 Physical Examination n n Appearance and mental status Mucous membranes and skin turgor BP (hypotension) Scars Abdominal Exam n n n Peritoneal signs Localized tenderness Masses Bruits-carcinoids &/or renal artery stenosis Rectal exam is needed n n 2/8/2018 Sphincter tone- Neurogenic ->DM Blood on stool & appearance 46
Physical Examination n n Appearance and mental status Mucous membranes and skin turgor BP (hypotension) Scars Abdominal Exam n n n Peritoneal signs Localized tenderness Masses Bruits-carcinoids &/or renal artery stenosis Rectal exam is needed n n 2/8/2018 Sphincter tone- Neurogenic ->DM Blood on stool & appearance 46
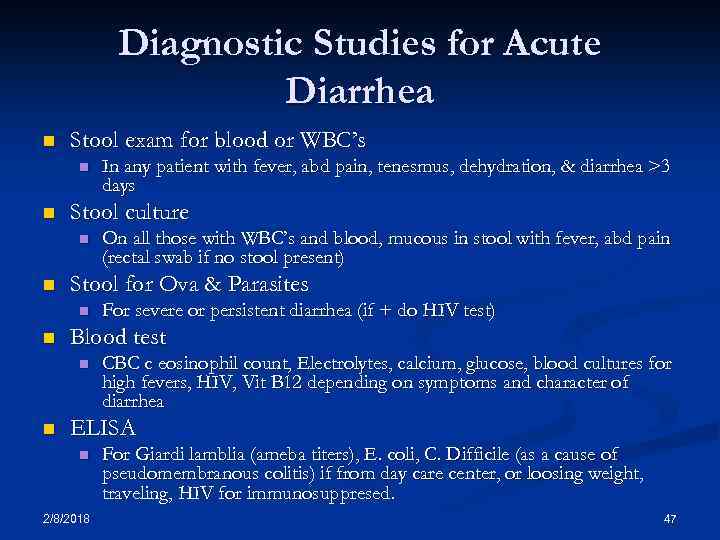 Diagnostic Studies for Acute Diarrhea n Stool exam for blood or WBC’s n n Stool culture n n For severe or persistent diarrhea (if + do HIV test) Blood test n n On all those with WBC’s and blood, mucous in stool with fever, abd pain (rectal swab if no stool present) Stool for Ova & Parasites n n In any patient with fever, abd pain, tenesmus, dehydration, & diarrhea >3 days CBC c eosinophil count, Electrolytes, calcium, glucose, blood cultures for high fevers, HIV, Vit B 12 depending on symptoms and character of diarrhea ELISA n 2/8/2018 For Giardi lamblia (ameba titers), E. coli, C. Difficile (as a cause of pseudomembranous colitis) if from day care center, or loosing weight, traveling, HIV for immunosuppresed. 47
Diagnostic Studies for Acute Diarrhea n Stool exam for blood or WBC’s n n Stool culture n n For severe or persistent diarrhea (if + do HIV test) Blood test n n On all those with WBC’s and blood, mucous in stool with fever, abd pain (rectal swab if no stool present) Stool for Ova & Parasites n n In any patient with fever, abd pain, tenesmus, dehydration, & diarrhea >3 days CBC c eosinophil count, Electrolytes, calcium, glucose, blood cultures for high fevers, HIV, Vit B 12 depending on symptoms and character of diarrhea ELISA n 2/8/2018 For Giardi lamblia (ameba titers), E. coli, C. Difficile (as a cause of pseudomembranous colitis) if from day care center, or loosing weight, traveling, HIV for immunosuppresed. 47
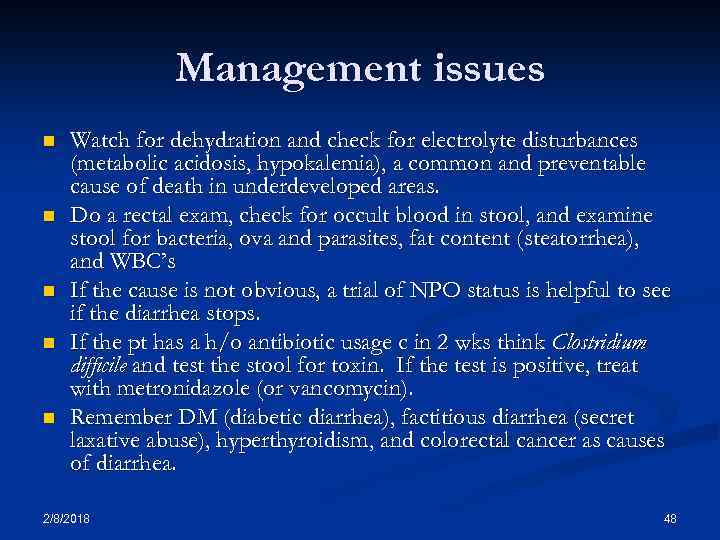 Management issues n n n Watch for dehydration and check for electrolyte disturbances (metabolic acidosis, hypokalemia), a common and preventable cause of death in underdeveloped areas. Do a rectal exam, check for occult blood in stool, and examine stool for bacteria, ova and parasites, fat content (steatorrhea), and WBC’s If the cause is not obvious, a trial of NPO status is helpful to see if the diarrhea stops. If the pt has a h/o antibiotic usage c in 2 wks think Clostridium difficile and test the stool for toxin. If the test is positive, treat with metronidazole (or vancomycin). Remember DM (diabetic diarrhea), factitious diarrhea (secret laxative abuse), hyperthyroidism, and colorectal cancer as causes of diarrhea. 2/8/2018 48
Management issues n n n Watch for dehydration and check for electrolyte disturbances (metabolic acidosis, hypokalemia), a common and preventable cause of death in underdeveloped areas. Do a rectal exam, check for occult blood in stool, and examine stool for bacteria, ova and parasites, fat content (steatorrhea), and WBC’s If the cause is not obvious, a trial of NPO status is helpful to see if the diarrhea stops. If the pt has a h/o antibiotic usage c in 2 wks think Clostridium difficile and test the stool for toxin. If the test is positive, treat with metronidazole (or vancomycin). Remember DM (diabetic diarrhea), factitious diarrhea (secret laxative abuse), hyperthyroidism, and colorectal cancer as causes of diarrhea. 2/8/2018 48
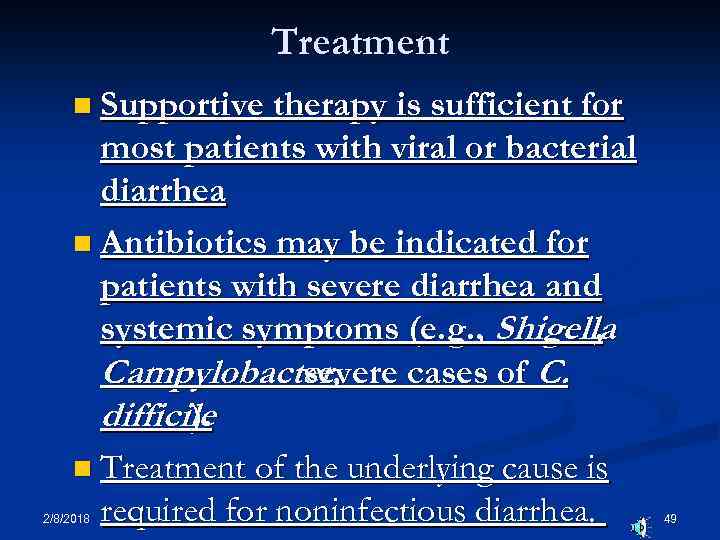 Treatment n Supportive therapy is sufficient for most patients with viral or bacterial diarrhea n Antibiotics may be indicated for patients with severe diarrhea and systemic symptoms (e. g. , Shigella , Campylobacter, severe cases of C. difficile ). n Treatment of the underlying cause is required for noninfectious diarrhea. 2/8/2018 49
Treatment n Supportive therapy is sufficient for most patients with viral or bacterial diarrhea n Antibiotics may be indicated for patients with severe diarrhea and systemic symptoms (e. g. , Shigella , Campylobacter, severe cases of C. difficile ). n Treatment of the underlying cause is required for noninfectious diarrhea. 2/8/2018 49
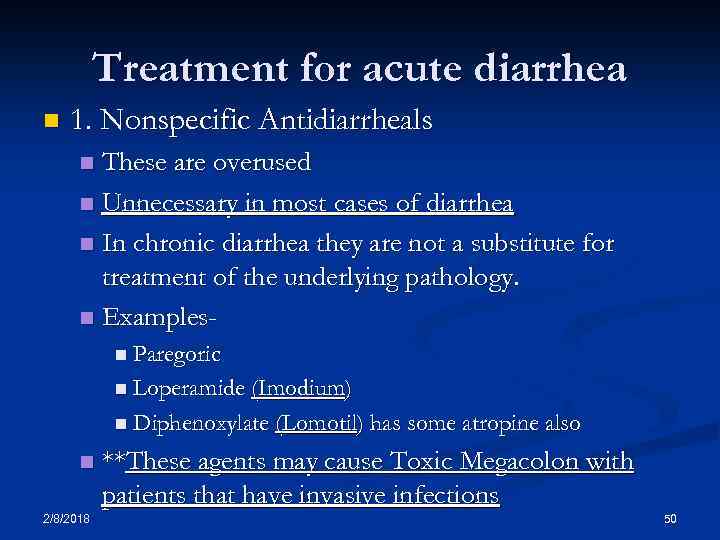 Treatment for acute diarrhea n 1. Nonspecific Antidiarrheals These are overused n Unnecessary in most cases of diarrhea n In chronic diarrhea they are not a substitute for treatment of the underlying pathology. n Examplesn n Paregoric n Loperamide (Imodium) n Diphenoxylate (Lomotil) has some atropine also n 2/8/2018 **These agents may cause Toxic Megacolon with patients that have invasive infections 50
Treatment for acute diarrhea n 1. Nonspecific Antidiarrheals These are overused n Unnecessary in most cases of diarrhea n In chronic diarrhea they are not a substitute for treatment of the underlying pathology. n Examplesn n Paregoric n Loperamide (Imodium) n Diphenoxylate (Lomotil) has some atropine also n 2/8/2018 **These agents may cause Toxic Megacolon with patients that have invasive infections 50
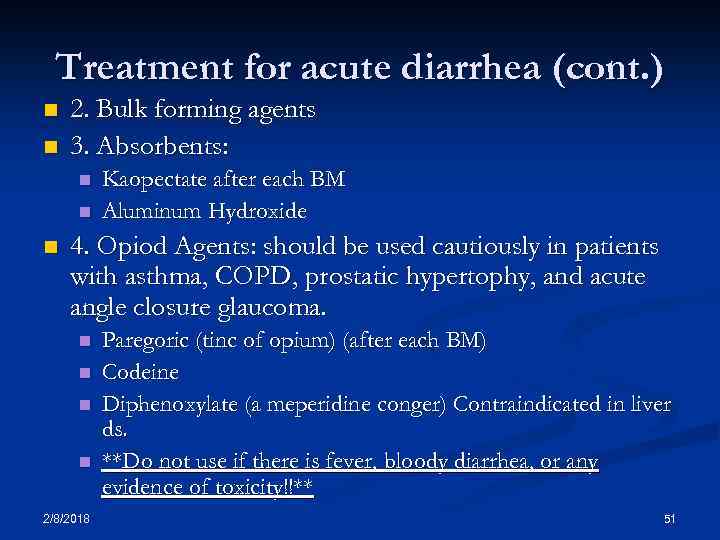 Treatment for acute diarrhea (cont. ) n n 2. Bulk forming agents 3. Absorbents: n n n Kaopectate after each BM Aluminum Hydroxide 4. Opiod Agents: should be used cautiously in patients with asthma, COPD, prostatic hypertophy, and acute angle closure glaucoma. n n 2/8/2018 Paregoric (tinc of opium) (after each BM) Codeine Diphenoxylate (a meperidine conger) Contraindicated in liver ds. **Do not use if there is fever, bloody diarrhea, or any evidence of toxicity!!** 51
Treatment for acute diarrhea (cont. ) n n 2. Bulk forming agents 3. Absorbents: n n n Kaopectate after each BM Aluminum Hydroxide 4. Opiod Agents: should be used cautiously in patients with asthma, COPD, prostatic hypertophy, and acute angle closure glaucoma. n n 2/8/2018 Paregoric (tinc of opium) (after each BM) Codeine Diphenoxylate (a meperidine conger) Contraindicated in liver ds. **Do not use if there is fever, bloody diarrhea, or any evidence of toxicity!!** 51
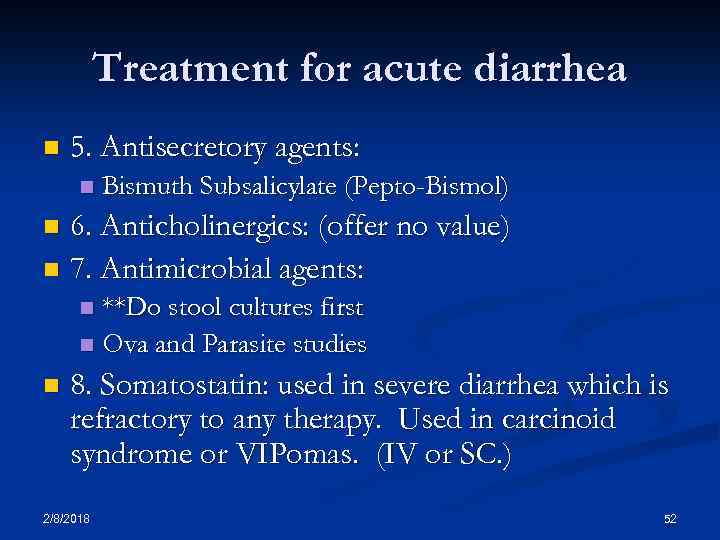 Treatment for acute diarrhea n 5. Antisecretory agents: n Bismuth Subsalicylate (Pepto-Bismol) 6. Anticholinergics: (offer no value) n 7. Antimicrobial agents: n **Do stool cultures first n Ova and Parasite studies n n 8. Somatostatin: used in severe diarrhea which is refractory to any therapy. Used in carcinoid syndrome or VIPomas. (IV or SC. ) 2/8/2018 52
Treatment for acute diarrhea n 5. Antisecretory agents: n Bismuth Subsalicylate (Pepto-Bismol) 6. Anticholinergics: (offer no value) n 7. Antimicrobial agents: n **Do stool cultures first n Ova and Parasite studies n n 8. Somatostatin: used in severe diarrhea which is refractory to any therapy. Used in carcinoid syndrome or VIPomas. (IV or SC. ) 2/8/2018 52
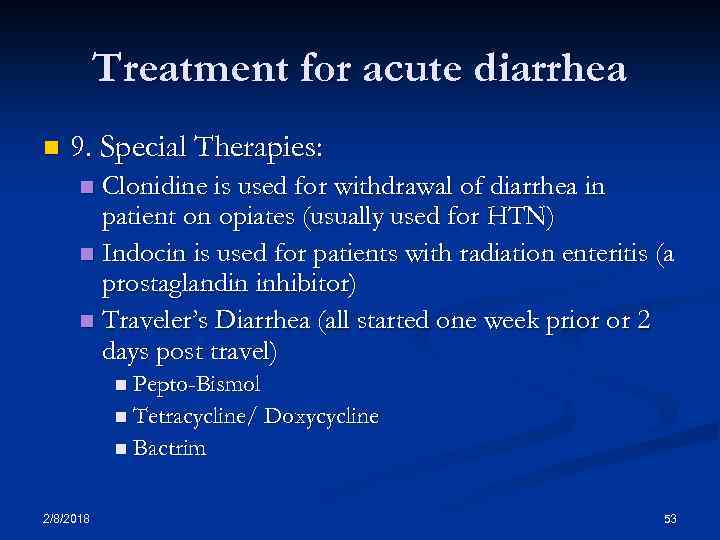 Treatment for acute diarrhea n 9. Special Therapies: Clonidine is used for withdrawal of diarrhea in patient on opiates (usually used for HTN) n Indocin is used for patients with radiation enteritis (a prostaglandin inhibitor) n Traveler’s Diarrhea (all started one week prior or 2 days post travel) n n Pepto-Bismol n Tetracycline/ Doxycycline n Bactrim 2/8/2018 53
Treatment for acute diarrhea n 9. Special Therapies: Clonidine is used for withdrawal of diarrhea in patient on opiates (usually used for HTN) n Indocin is used for patients with radiation enteritis (a prostaglandin inhibitor) n Traveler’s Diarrhea (all started one week prior or 2 days post travel) n n Pepto-Bismol n Tetracycline/ Doxycycline n Bactrim 2/8/2018 53
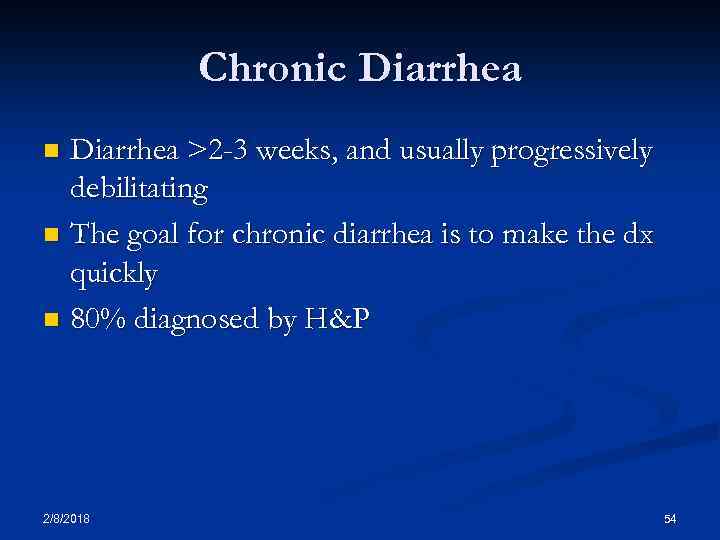 Chronic Diarrhea >2 -3 weeks, and usually progressively debilitating n The goal for chronic diarrhea is to make the dx quickly n 80% diagnosed by H&P n 2/8/2018 54
Chronic Diarrhea >2 -3 weeks, and usually progressively debilitating n The goal for chronic diarrhea is to make the dx quickly n 80% diagnosed by H&P n 2/8/2018 54
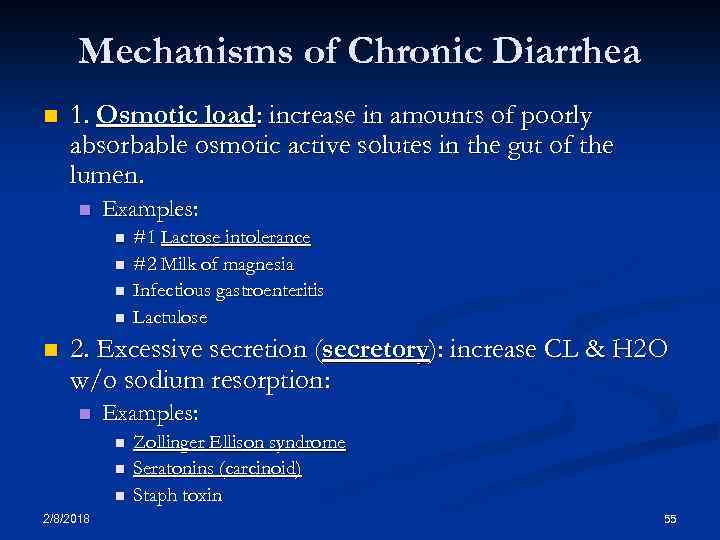 Mechanisms of Chronic Diarrhea n 1. Osmotic load: increase in amounts of poorly absorbable osmotic active solutes in the gut of the lumen. n Examples: n n n #1 Lactose intolerance #2 Milk of magnesia Infectious gastroenteritis Lactulose 2. Excessive secretion (secretory): increase CL & H 2 O w/o sodium resorption: n Examples: n n n 2/8/2018 Zollinger Ellison syndrome Seratonins (carcinoid) Staph toxin 55
Mechanisms of Chronic Diarrhea n 1. Osmotic load: increase in amounts of poorly absorbable osmotic active solutes in the gut of the lumen. n Examples: n n n #1 Lactose intolerance #2 Milk of magnesia Infectious gastroenteritis Lactulose 2. Excessive secretion (secretory): increase CL & H 2 O w/o sodium resorption: n Examples: n n n 2/8/2018 Zollinger Ellison syndrome Seratonins (carcinoid) Staph toxin 55
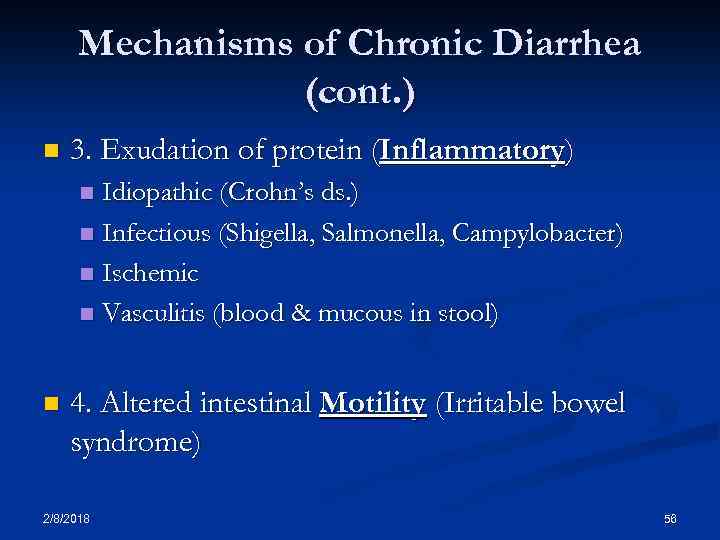 Mechanisms of Chronic Diarrhea (cont. ) n 3. Exudation of protein (Inflammatory) Idiopathic (Crohn’s ds. ) n Infectious (Shigella, Salmonella, Campylobacter) n Ischemic n Vasculitis (blood & mucous in stool) n n 4. Altered intestinal Motility (Irritable bowel syndrome) 2/8/2018 56
Mechanisms of Chronic Diarrhea (cont. ) n 3. Exudation of protein (Inflammatory) Idiopathic (Crohn’s ds. ) n Infectious (Shigella, Salmonella, Campylobacter) n Ischemic n Vasculitis (blood & mucous in stool) n n 4. Altered intestinal Motility (Irritable bowel syndrome) 2/8/2018 56
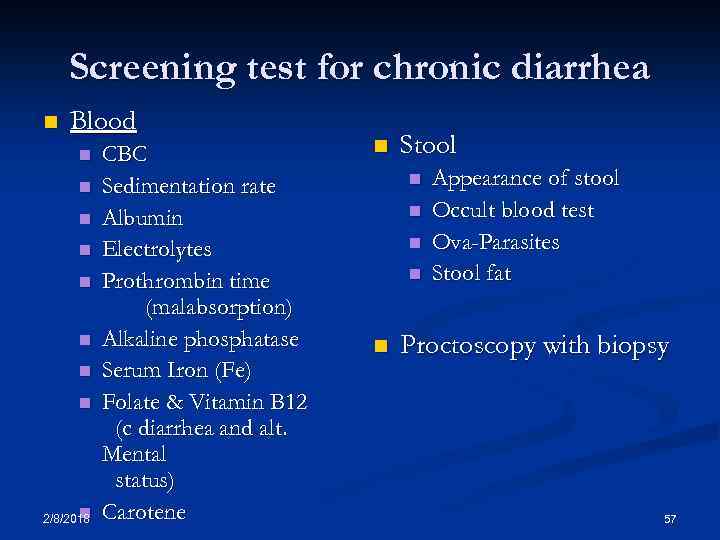 Screening test for chronic diarrhea n Blood n n n n n 2/8/2018 CBC Sedimentation rate Albumin Electrolytes Prothrombin time (malabsorption) Alkaline phosphatase Serum Iron (Fe) Folate & Vitamin B 12 (c diarrhea and alt. Mental status) Carotene n Stool n n n Appearance of stool Occult blood test Ova-Parasites Stool fat Proctoscopy with biopsy 57
Screening test for chronic diarrhea n Blood n n n n n 2/8/2018 CBC Sedimentation rate Albumin Electrolytes Prothrombin time (malabsorption) Alkaline phosphatase Serum Iron (Fe) Folate & Vitamin B 12 (c diarrhea and alt. Mental status) Carotene n Stool n n n Appearance of stool Occult blood test Ova-Parasites Stool fat Proctoscopy with biopsy 57
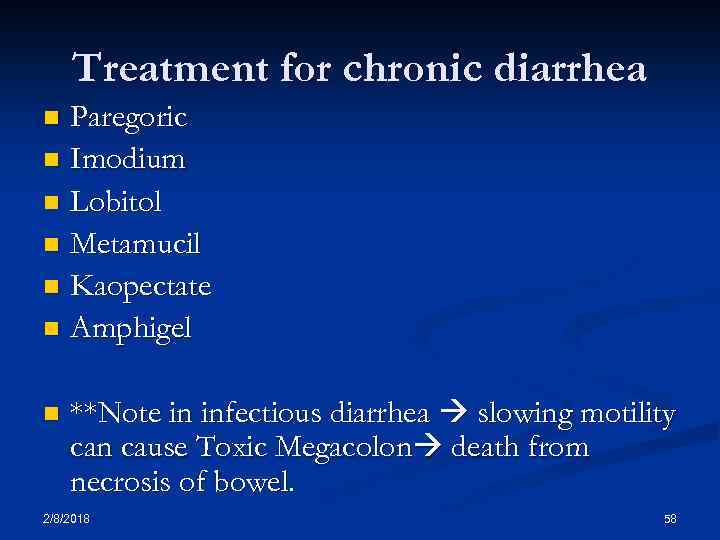 Treatment for chronic diarrhea Paregoric n Imodium n Lobitol n Metamucil n Kaopectate n Amphigel n n **Note in infectious diarrhea slowing motility can cause Toxic Megacolon death from necrosis of bowel. 2/8/2018 58
Treatment for chronic diarrhea Paregoric n Imodium n Lobitol n Metamucil n Kaopectate n Amphigel n n **Note in infectious diarrhea slowing motility can cause Toxic Megacolon death from necrosis of bowel. 2/8/2018 58
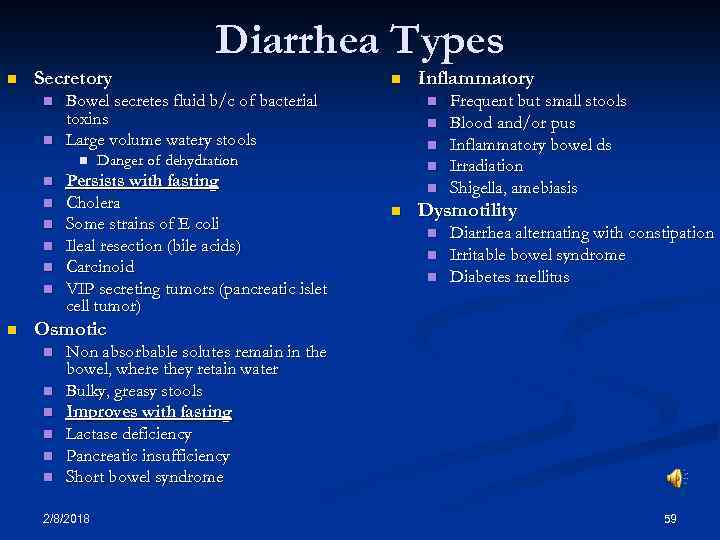 Diarrhea Types n Secretory n n Bowel secretes fluid b/c of bacterial toxins Large volume watery stools n n n Danger of dehydration Persists with fasting Cholera Some strains of E coli Ileal resection (bile acids) Carcinoid VIP secreting tumors (pancreatic islet cell tumor) Inflammatory n n n Frequent but small stools Blood and/or pus Inflammatory bowel ds Irradiation Shigella, amebiasis Dysmotility n n n Diarrhea alternating with constipation Irritable bowel syndrome Diabetes mellitus Osmotic n n n Non absorbable solutes remain in the bowel, where they retain water Bulky, greasy stools Improves with fasting Lactase deficiency Pancreatic insufficiency Short bowel syndrome 2/8/2018 59
Diarrhea Types n Secretory n n Bowel secretes fluid b/c of bacterial toxins Large volume watery stools n n n Danger of dehydration Persists with fasting Cholera Some strains of E coli Ileal resection (bile acids) Carcinoid VIP secreting tumors (pancreatic islet cell tumor) Inflammatory n n n Frequent but small stools Blood and/or pus Inflammatory bowel ds Irradiation Shigella, amebiasis Dysmotility n n n Diarrhea alternating with constipation Irritable bowel syndrome Diabetes mellitus Osmotic n n n Non absorbable solutes remain in the bowel, where they retain water Bulky, greasy stools Improves with fasting Lactase deficiency Pancreatic insufficiency Short bowel syndrome 2/8/2018 59
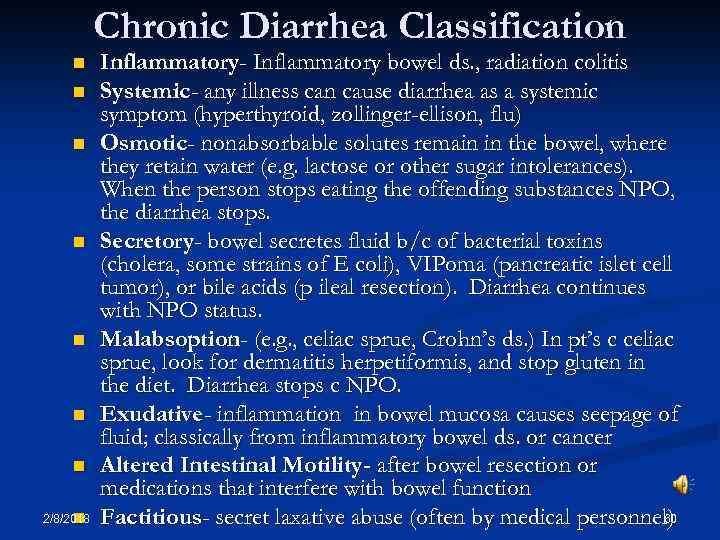 Chronic Diarrhea Classification n n n 2/8/2018 n Inflammatory- Inflammatory bowel ds. , radiation colitis Systemic- any illness can cause diarrhea as a systemic symptom (hyperthyroid, zollinger-ellison, flu) Osmotic- nonabsorbable solutes remain in the bowel, where they retain water (e. g. lactose or other sugar intolerances). When the person stops eating the offending substances NPO, the diarrhea stops. Secretory- bowel secretes fluid b/c of bacterial toxins (cholera, some strains of E coli), VIPoma (pancreatic islet cell tumor), or bile acids (p ileal resection). Diarrhea continues with NPO status. Malabsoption- (e. g. , celiac sprue, Crohn’s ds. ) In pt’s c celiac sprue, look for dermatitis herpetiformis, and stop gluten in the diet. Diarrhea stops c NPO. Exudative- inflammation in bowel mucosa causes seepage of fluid; classically from inflammatory bowel ds. or cancer Altered Intestinal Motility- after bowel resection or medications that interfere with bowel function 60 Factitious- secret laxative abuse (often by medical personnel)
Chronic Diarrhea Classification n n n 2/8/2018 n Inflammatory- Inflammatory bowel ds. , radiation colitis Systemic- any illness can cause diarrhea as a systemic symptom (hyperthyroid, zollinger-ellison, flu) Osmotic- nonabsorbable solutes remain in the bowel, where they retain water (e. g. lactose or other sugar intolerances). When the person stops eating the offending substances NPO, the diarrhea stops. Secretory- bowel secretes fluid b/c of bacterial toxins (cholera, some strains of E coli), VIPoma (pancreatic islet cell tumor), or bile acids (p ileal resection). Diarrhea continues with NPO status. Malabsoption- (e. g. , celiac sprue, Crohn’s ds. ) In pt’s c celiac sprue, look for dermatitis herpetiformis, and stop gluten in the diet. Diarrhea stops c NPO. Exudative- inflammation in bowel mucosa causes seepage of fluid; classically from inflammatory bowel ds. or cancer Altered Intestinal Motility- after bowel resection or medications that interfere with bowel function 60 Factitious- secret laxative abuse (often by medical personnel)
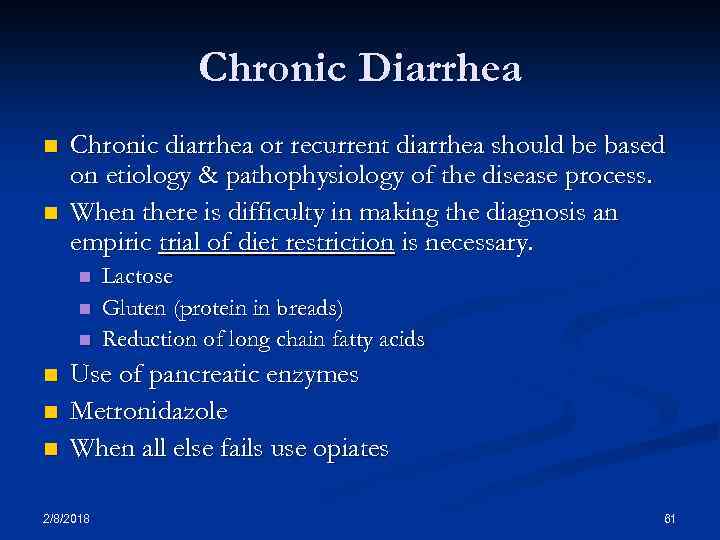 Chronic Diarrhea n n Chronic diarrhea or recurrent diarrhea should be based on etiology & pathophysiology of the disease process. When there is difficulty in making the diagnosis an empiric trial of diet restriction is necessary. n n n Lactose Gluten (protein in breads) Reduction of long chain fatty acids Use of pancreatic enzymes Metronidazole When all else fails use opiates 2/8/2018 61
Chronic Diarrhea n n Chronic diarrhea or recurrent diarrhea should be based on etiology & pathophysiology of the disease process. When there is difficulty in making the diagnosis an empiric trial of diet restriction is necessary. n n n Lactose Gluten (protein in breads) Reduction of long chain fatty acids Use of pancreatic enzymes Metronidazole When all else fails use opiates 2/8/2018 61
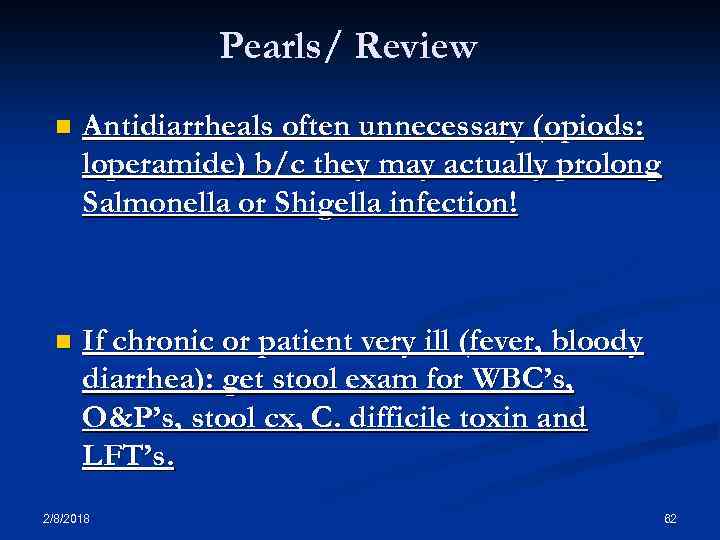 Pearls/ Review n Antidiarrheals often unnecessary (opiods: loperamide) b/c they may actually prolong Salmonella or Shigella infection! n If chronic or patient very ill (fever, bloody diarrhea): get stool exam for WBC’s, O&P’s, stool cx, C. difficile toxin and LFT’s. 2/8/2018 62
Pearls/ Review n Antidiarrheals often unnecessary (opiods: loperamide) b/c they may actually prolong Salmonella or Shigella infection! n If chronic or patient very ill (fever, bloody diarrhea): get stool exam for WBC’s, O&P’s, stool cx, C. difficile toxin and LFT’s. 2/8/2018 62
 Pearls (cont. ) n AID’s patients: diarrhea is often due to Cryptosporidium, Isospora or CMV n Diarrhea of any cause may lead to transient lactase deficiency (advise patient to avoid milk) n Bismuth subsalicylate (Pepto-Bismol) may prevent infection with enterotoxin producing E. coli. Great for travelers to exotic countries. 2/8/2018 63
Pearls (cont. ) n AID’s patients: diarrhea is often due to Cryptosporidium, Isospora or CMV n Diarrhea of any cause may lead to transient lactase deficiency (advise patient to avoid milk) n Bismuth subsalicylate (Pepto-Bismol) may prevent infection with enterotoxin producing E. coli. Great for travelers to exotic countries. 2/8/2018 63
 Pearls Diarrhea in elderly patients can indicate an obstruction or fecal impaction. n Acute Diarrhea: Lg amts. of stool Small bowel Sm amts. of stool Lg bowel n Gastroenteritis symptoms #1. abd. pain #2. diameter n Celiac sprue Gluten sensative enteropathy proximal small bowel n 2/8/2018 64
Pearls Diarrhea in elderly patients can indicate an obstruction or fecal impaction. n Acute Diarrhea: Lg amts. of stool Small bowel Sm amts. of stool Lg bowel n Gastroenteritis symptoms #1. abd. pain #2. diameter n Celiac sprue Gluten sensative enteropathy proximal small bowel n 2/8/2018 64
 Pearls In >90% of cases, acute diarrhea is mild and self -limiting, and diagnostic investigation is unnecessary. n Prompt sigmoidoscopy for severe proctitis (tenesmus, discharge, rectal pain) or suspected C. difficile colitis, ulcerative colitis, or ischemic colitis n When traveling 4 “P’s”, Pepto-bismol, and eat only peeled, packaged, and piping hot foods. n 2/8/2018 65
Pearls In >90% of cases, acute diarrhea is mild and self -limiting, and diagnostic investigation is unnecessary. n Prompt sigmoidoscopy for severe proctitis (tenesmus, discharge, rectal pain) or suspected C. difficile colitis, ulcerative colitis, or ischemic colitis n When traveling 4 “P’s”, Pepto-bismol, and eat only peeled, packaged, and piping hot foods. n 2/8/2018 65
 Review Infectious: noninflammatory (nonbloody) n Viruses: Norwalk virus, rotavirus, adenoviruses, astrovirus, coronavirus n Preformed toxin (food poisoning): Staphylococcus aureus, Bacillus cereus, Clostridium perfringens n Toxin production: enterotoxigenic E. coli, Vibrio cholerae, Vibrio parahaemolyticus n Protozoa: Giardia lamblia, Cryptosporidium, Cyclospora, Isospora n 2/8/2018 66
Review Infectious: noninflammatory (nonbloody) n Viruses: Norwalk virus, rotavirus, adenoviruses, astrovirus, coronavirus n Preformed toxin (food poisoning): Staphylococcus aureus, Bacillus cereus, Clostridium perfringens n Toxin production: enterotoxigenic E. coli, Vibrio cholerae, Vibrio parahaemolyticus n Protozoa: Giardia lamblia, Cryptosporidium, Cyclospora, Isospora n 2/8/2018 66
 Review Infectious: invasive or inflammatory n Shigella, Salmonella, Campylobacter, enteroinvasive E. coli, E. coli O 157: H 7, Yersinia enterocolitica, Clostridium difficile (e. g. , pseudomembranous colitis), Entamoeba histolytica, Neisseria gonorrhoeae, Listeria monocytogenes n 2/8/2018 67
Review Infectious: invasive or inflammatory n Shigella, Salmonella, Campylobacter, enteroinvasive E. coli, E. coli O 157: H 7, Yersinia enterocolitica, Clostridium difficile (e. g. , pseudomembranous colitis), Entamoeba histolytica, Neisseria gonorrhoeae, Listeria monocytogenes n 2/8/2018 67
 Pearl Bloody Diarrhea DDx n Shigella, n Salmonella, n Campylobacter, n enteroinvasive E. coli, (E. coli O 157: H 7), n Yersinia enterocolitica, n 2/8/2018 68
Pearl Bloody Diarrhea DDx n Shigella, n Salmonella, n Campylobacter, n enteroinvasive E. coli, (E. coli O 157: H 7), n Yersinia enterocolitica, n 2/8/2018 68


