Gastric and duodenal ulcer disease Anatomy Arterial blood

Gastric and duodenal ulcer disease
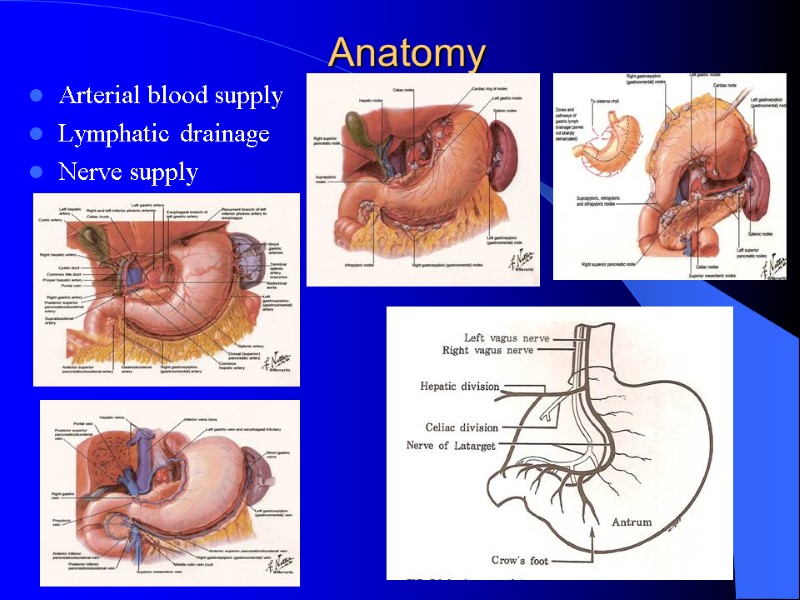
Anatomy Arterial blood supply Lymphatic drainage Nerve supply
PHYSIOLOGY Function: Digestion of food, reduce the size of food Acts as reservoir Absorption of Vit. 12, iron and calcium Stimulant of Gastric secretion: Gastrin -----> (+) parietal cell Acetylcholine (vagus) ---> (+) gastric cells Histamine (mast cells) ---> parietal & chief cells
PHYSIOLOGY BAO: 2 – 5 meq of acid/hr. (vagal tone and basal histamine secretion) MAO: Cephalic (vagus) ---> (+) parietal & G cell 10 meq acid/hr. Gastric: ---> (+) vagus & G cell 15 – 25 meq of acid/hr pH = < 2.0 Intestinal: Chyme enters the duodenum (-) gastric release Secretin, gastric inhibitory peptide, peptide YY ACID condition sterilized the area, except for HELICOBACTER PYLORI
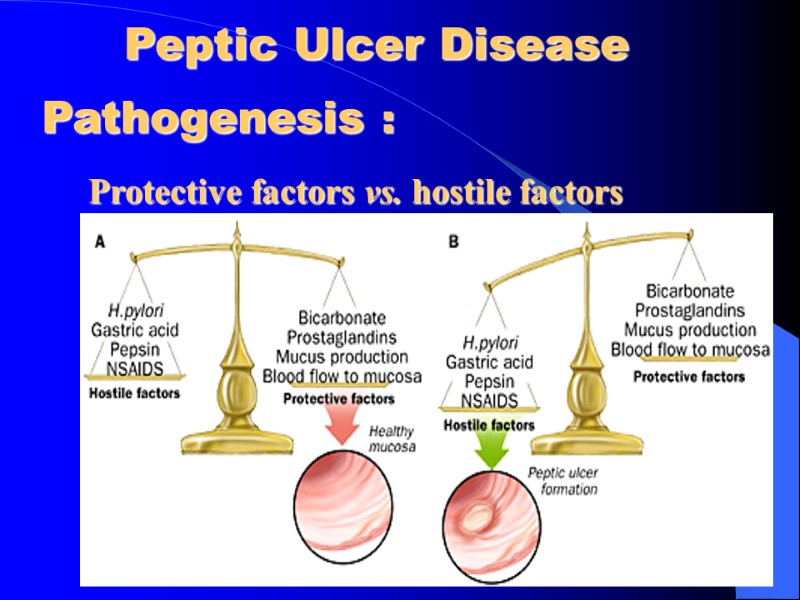
Protective factors vs. hostile factors
Peptic ulcer Pathogenesis: For both Duodenal & Gastric Ulcers: Infection w/ H. pylori: Decreases resistance of mucus layer from acid permeation (hydrophobicity) Increase acid secretion Slow duodenal emptying Reduced both duodenal and gastric bicarbonate secretion
Clinical Manifestation Abdominal pain: Due to irritation of afferent nerves w/in the ulcer by the acid or due to peristaltic waves passing through the ulcer Duodenal: colicky or burning pain relieved w/ food intake Gastric: gnawing or burning usually during or after eating. N/V Weight loss Epigastric tenderness
Peptic ulcer Pathogenesis: Effects of NSAIDs Decreases Prostagladin Prostaglandin – inhibits acid secretion, stimulates mucus and HCO3 secretion and mucosal blood flow Zollinger-Ellison Syndrome (1%): Massive secretion of HCL due to ectopic gastrin production from non-beta islet cell tumor (gastrinoma) Associated w/ type I (MEN) PPP 20% multiple, 2/3 malignant, w/ slow growing Parietal cell mass is increased > gastrin 3-6 x the normal
Symptoms of gastric ulcer disease: epigastric pain after meal or during meal upper dyspeptic syndrome – loss of appetite, nauzea, vomiting, flatulence vomiting brings relief reduced nutrition loss of weight
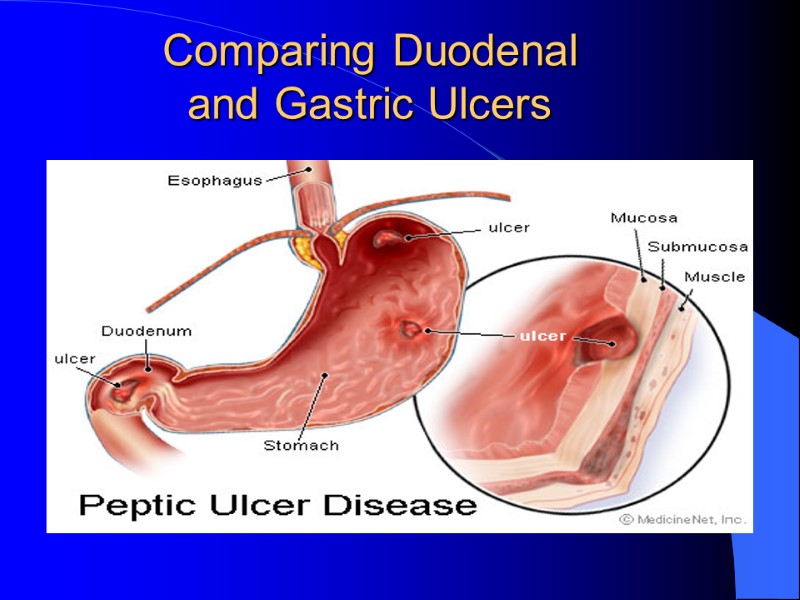
Comparing Duodenal and Gastric Ulcers
Symptoms of duodenal ulcer disease: epigastric pain 2 hours after meal or on a empty stomach or during night pyrosis good nutrition obstipation seasonal dependence (spring, autumn)
Diagnosis: UGIS (double contrast) Endoscopy
Therapy: Conservative regular lifestyle prohibition of the smoking and alcohol diet (proteins, milk and milky products) pharmacology (antagonists of H2 receptors, antacids, anticholinergics Surgical BI, BII resection proximal selective vagotomy vagotomy with pyloroplastic suture of perforated or haemorrhagic ulcer
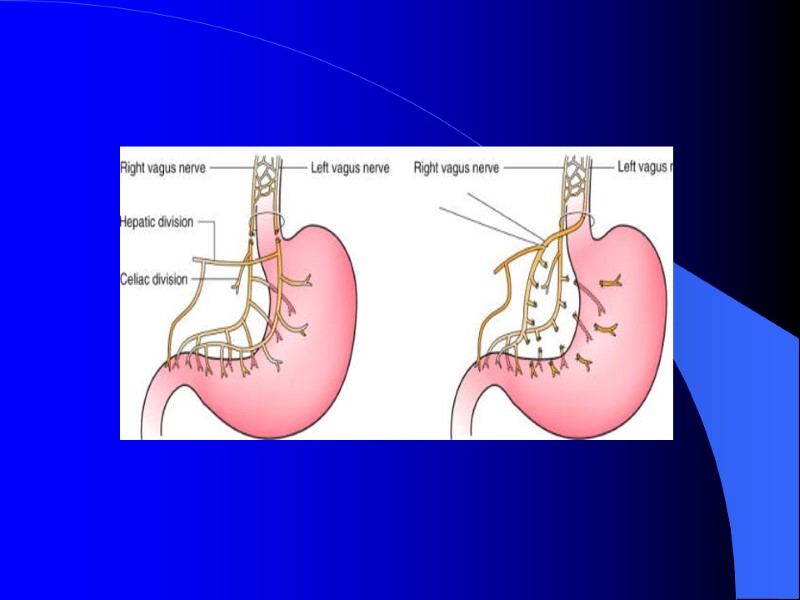
Stomach resections: Billroth I (BI) – gastro-duodenoanastomosis end-to-end Billroth II (BII) – gastro-jejunoanastomosis end-to-side with blind closure of duodenum Proximal selective vagotomy – denervation of parietal gastric cells
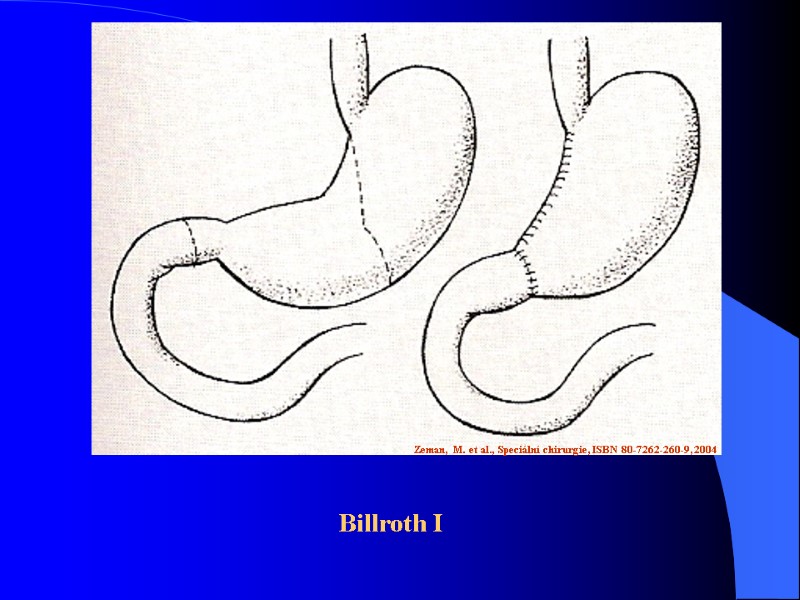
Zeman, M. et al., Speciální chirurgie, ISBN 80-7262-260-9, 2004 Billroth I
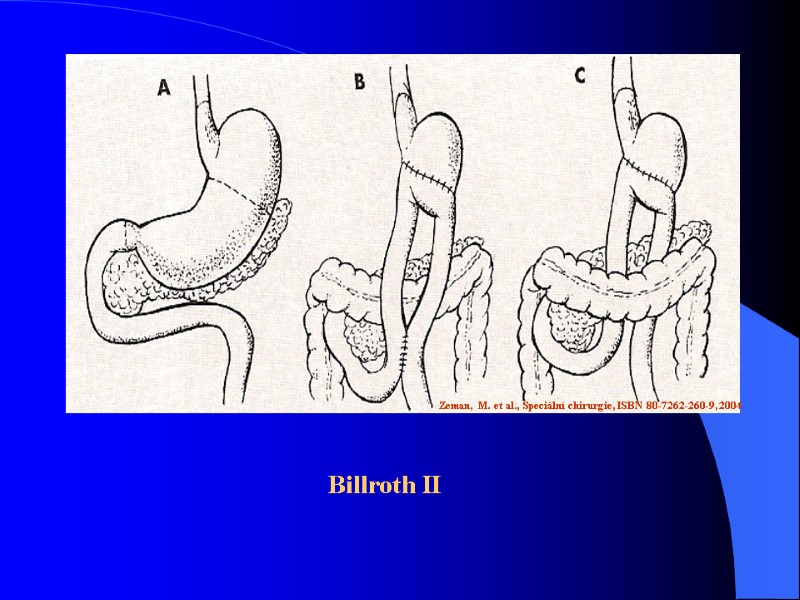
Billroth II Zeman, M. et al., Speciální chirurgie, ISBN 80-7262-260-9, 2004
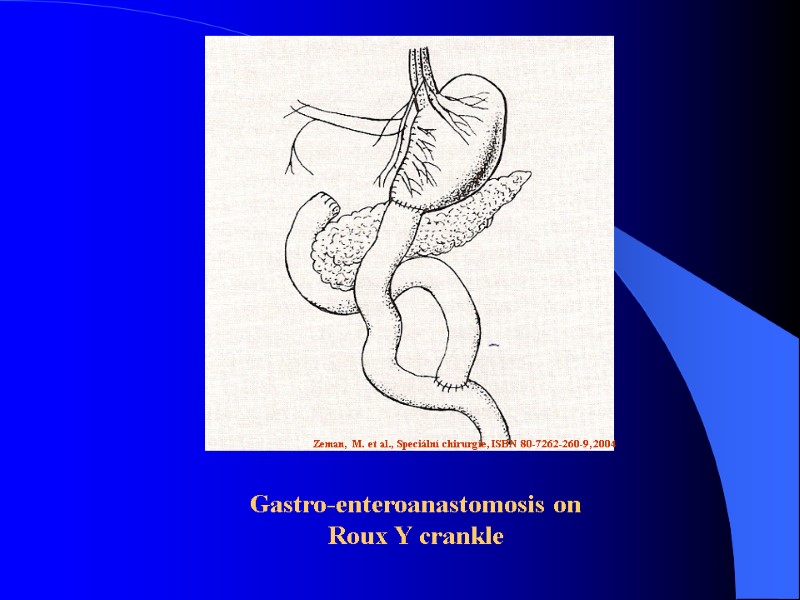
Zeman, M. et al., Speciální chirurgie, ISBN 80-7262-260-9, 2004 Gastro-enteroanastomosis on Roux Y crankle
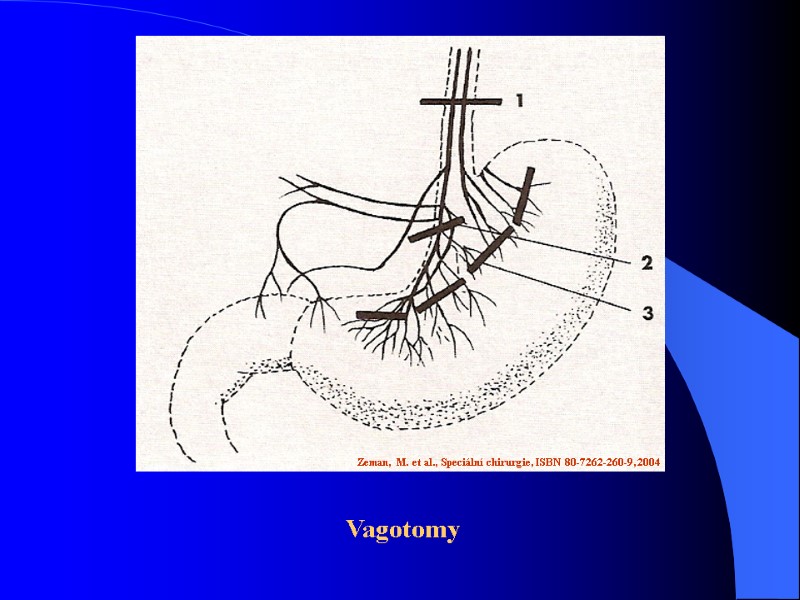
Zeman, M. et al., Speciální chirurgie, ISBN 80-7262-260-9, 2004 Vagotomy
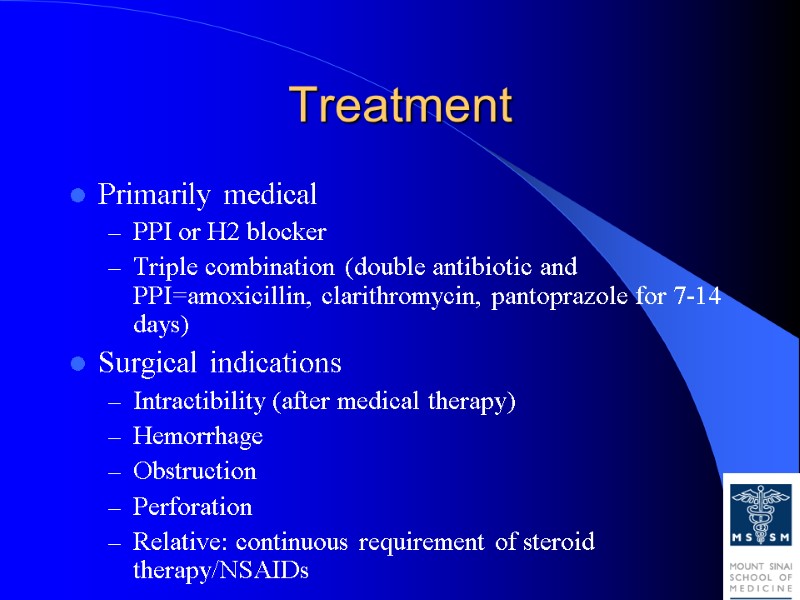
Treatment Primarily medical PPI or H2 blocker Triple combination (double antibiotic and PPI=amoxicillin, clarithromycin, pantoprazole for 7-14 days) Surgical indications Intractibility (after medical therapy) Hemorrhage Obstruction Perforation Relative: continuous requirement of steroid therapy/NSAIDs
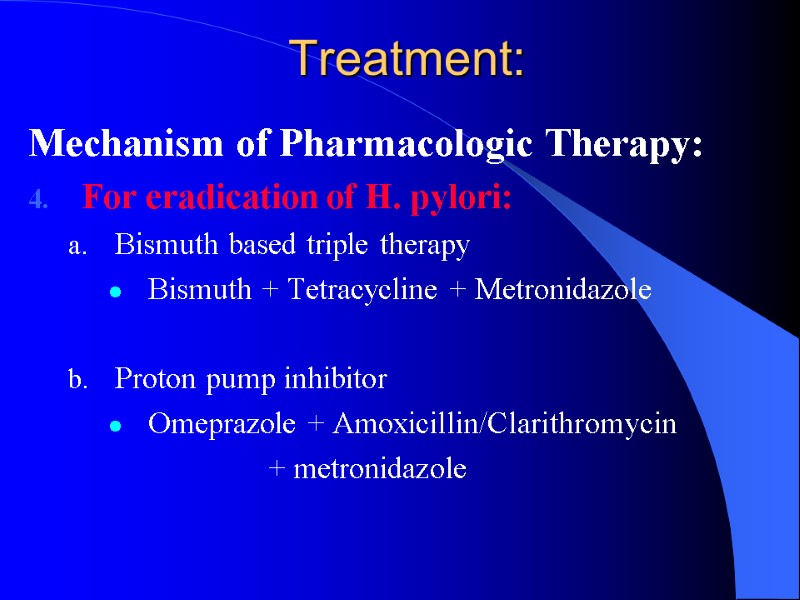
Treatment: Mechanism of Pharmacologic Therapy: For eradication of H. pylori: Bismuth based triple therapy Bismuth + Tetracycline + Metronidazole Proton pump inhibitor Omeprazole + Amoxicillin/Clarithromycin + metronidazole
Treatment: Surgical Treatment: Indication: Intractability: Highly selective vagotomy Low septic complication, (-) dumping and diarrhea For gastric ulcer: Total or subtotal gastrectomy w/ or w/o vagotomy
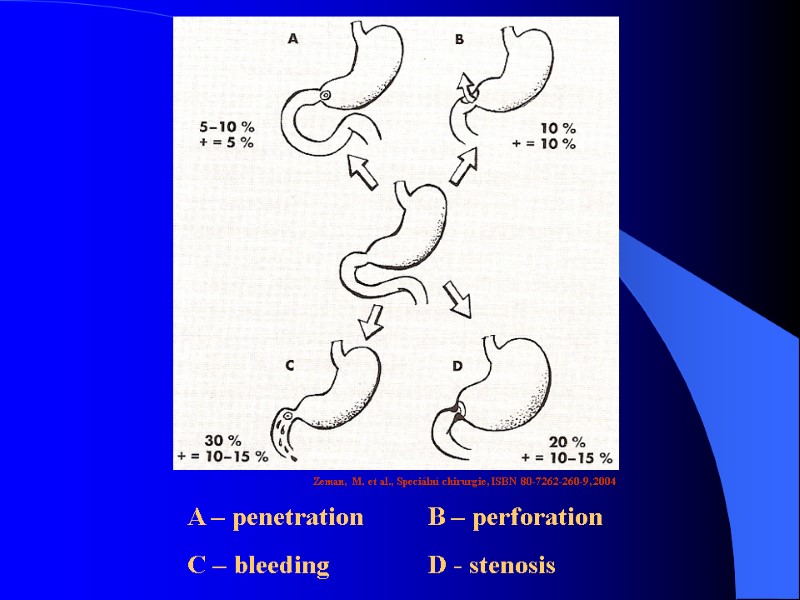
Zeman, M. et al., Speciální chirurgie, ISBN 80-7262-260-9, 2004 A – penetration B – perforation C – bleeding D - stenosis
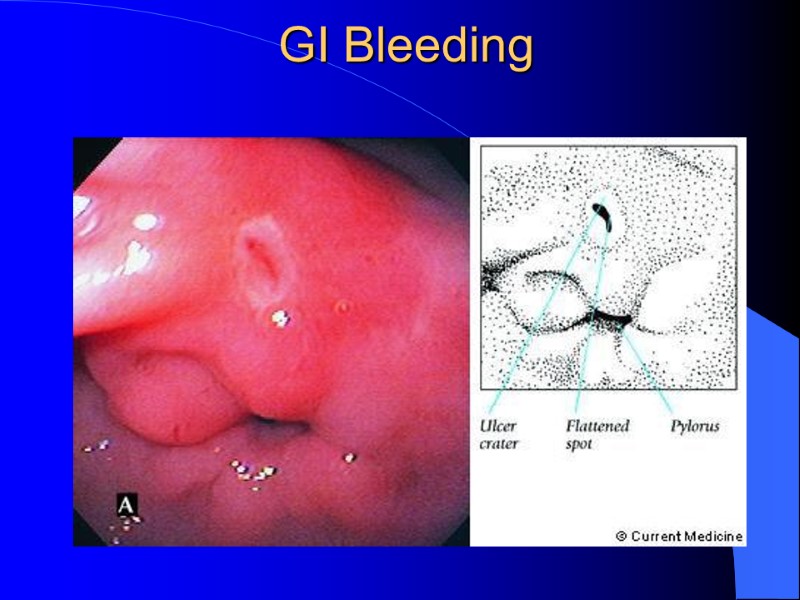
GI Bleeding
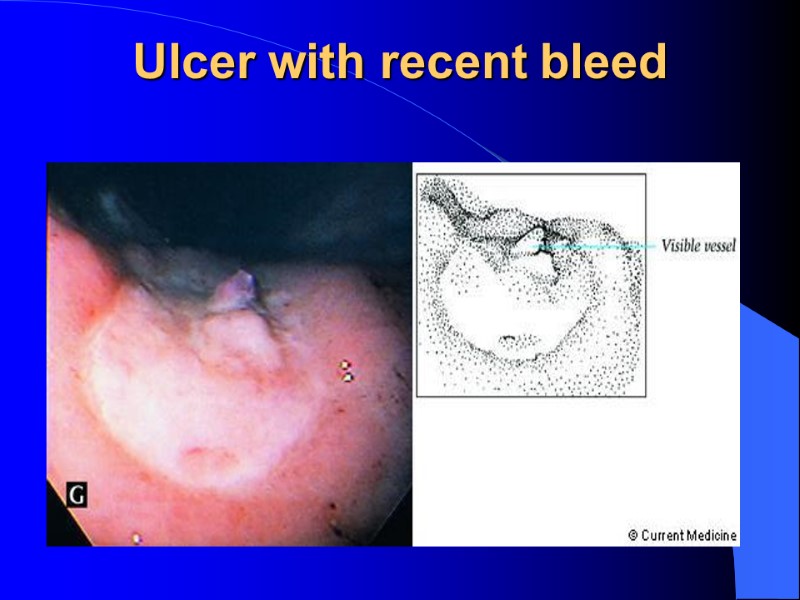
Ulcer with recent bleed
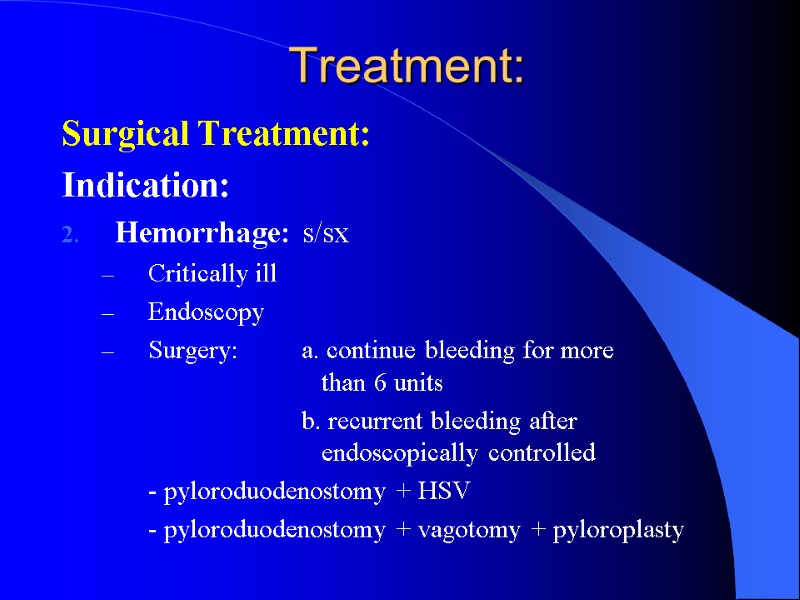
Treatment: Surgical Treatment: Indication: Hemorrhage: s/sx Critically ill Endoscopy Surgery: a. continue bleeding for more than 6 units b. recurrent bleeding after endoscopically controlled - pyloroduodenostomy + HSV - pyloroduodenostomy + vagotomy + pyloroplasty
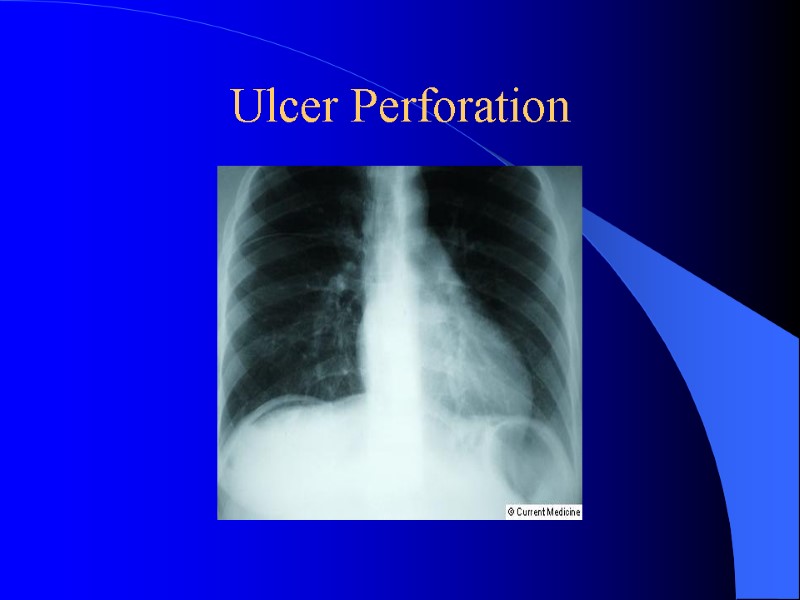
Ulcer Perforation
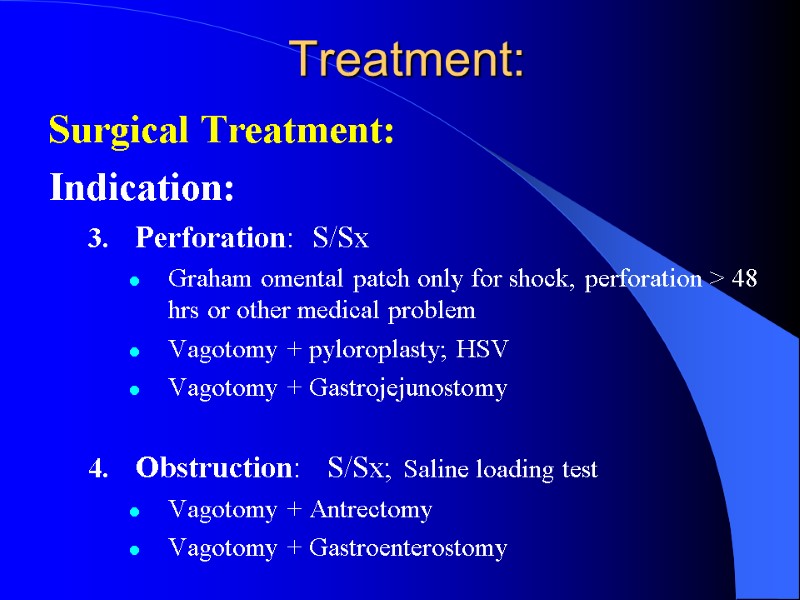
Treatment: Surgical Treatment: Indication: Perforation: S/Sx Graham omental patch only for shock, perforation > 48 hrs or other medical problem Vagotomy + pyloroplasty; HSV Vagotomy + Gastrojejunostomy Obstruction: S/Sx; Saline loading test Vagotomy + Antrectomy Vagotomy + Gastroenterostomy
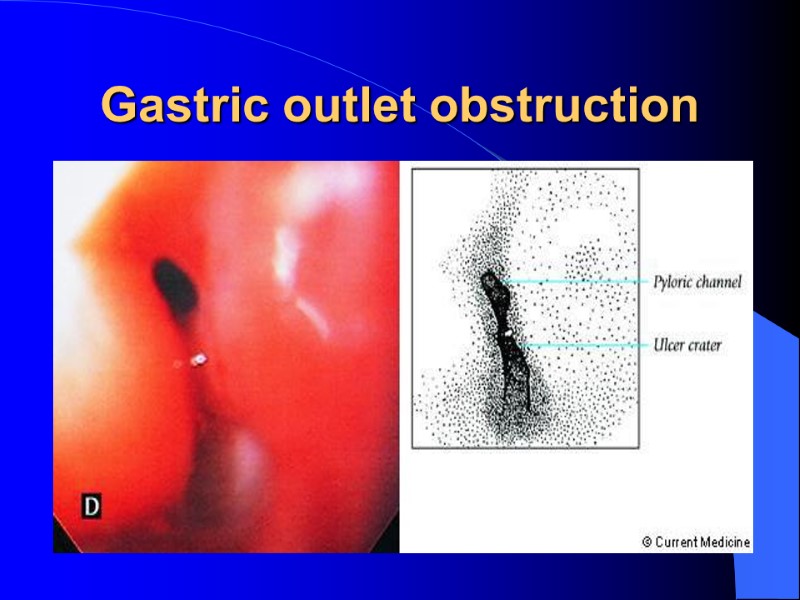
Gastric outlet obstruction
Elective Surgical Therapy Rare; most uncomplicated ulcers heal within 12 weeks If don’t, change medication, observe addition 12 weeks Check serum gastrin (antral G-cell hyperplasia or gastrinoma) EGD: biopsy all 4 quadrants of ulcer (rule out malignant ulcer) if refractory
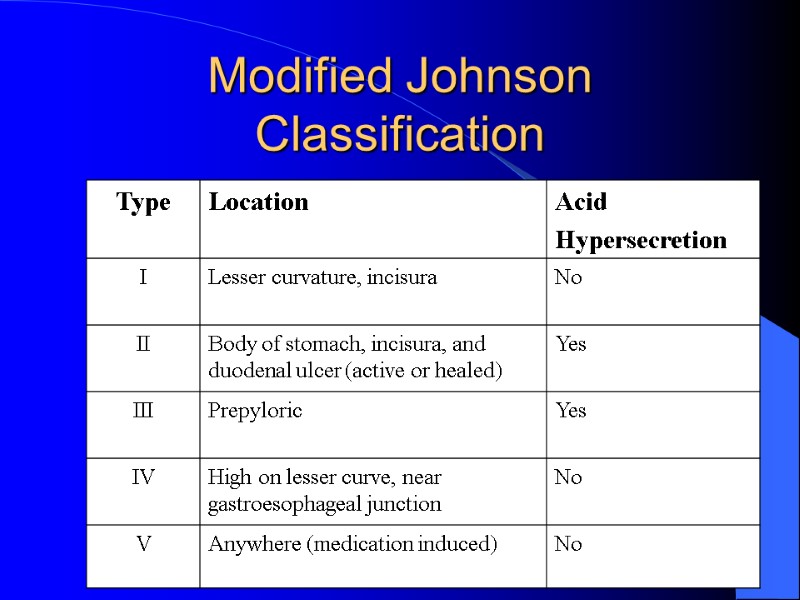
Modified Johnson Classification
Elective Surgical Therapy Type I
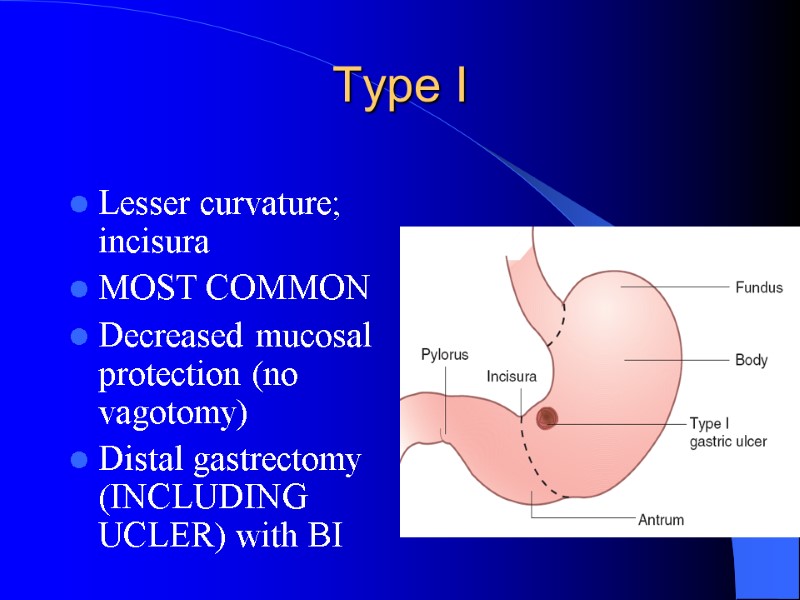
Type I Lesser curvature; incisura MOST COMMON Decreased mucosal protection (no vagotomy) Distal gastrectomy (INCLUDING UCLER) with BI

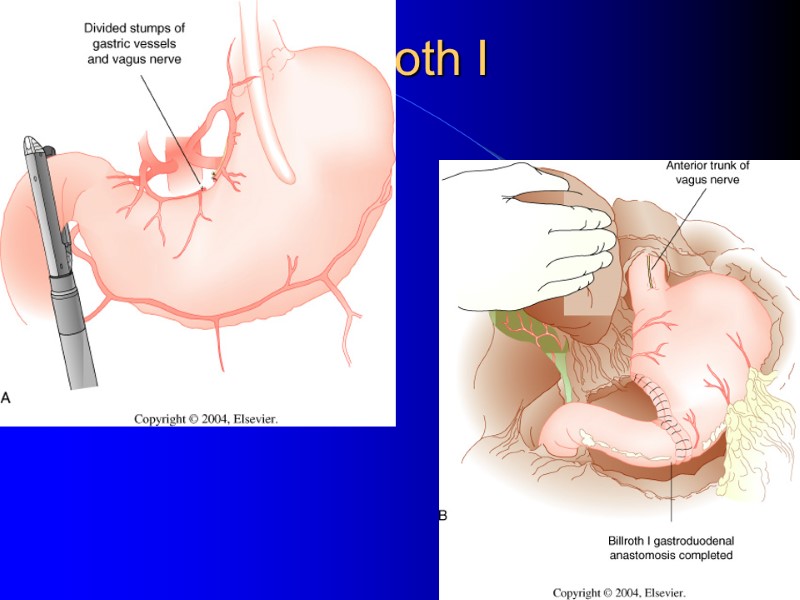
Billroth I
Elective Surgical Therapy Type II/III
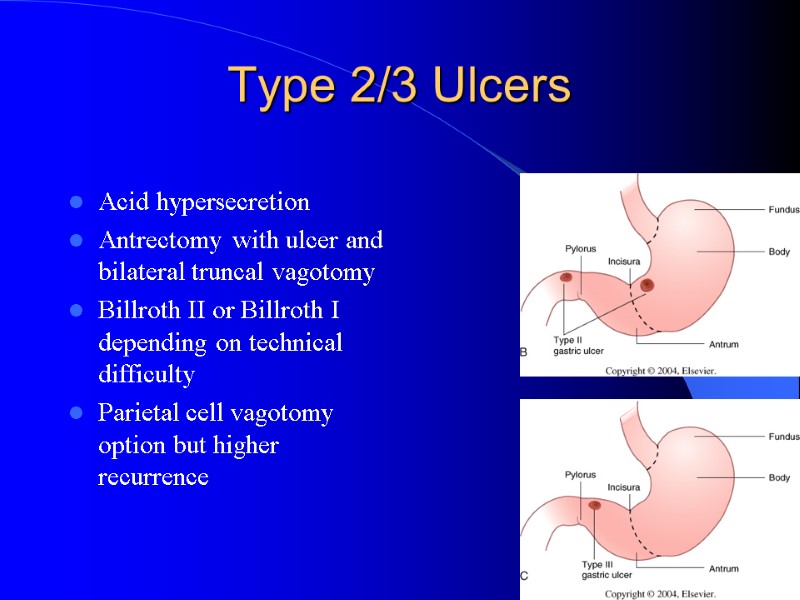
Type 2/3 Ulcers Acid hypersecretion Antrectomy with ulcer and bilateral truncal vagotomy Billroth II or Billroth I depending on technical difficulty Parietal cell vagotomy option but higher recurrence
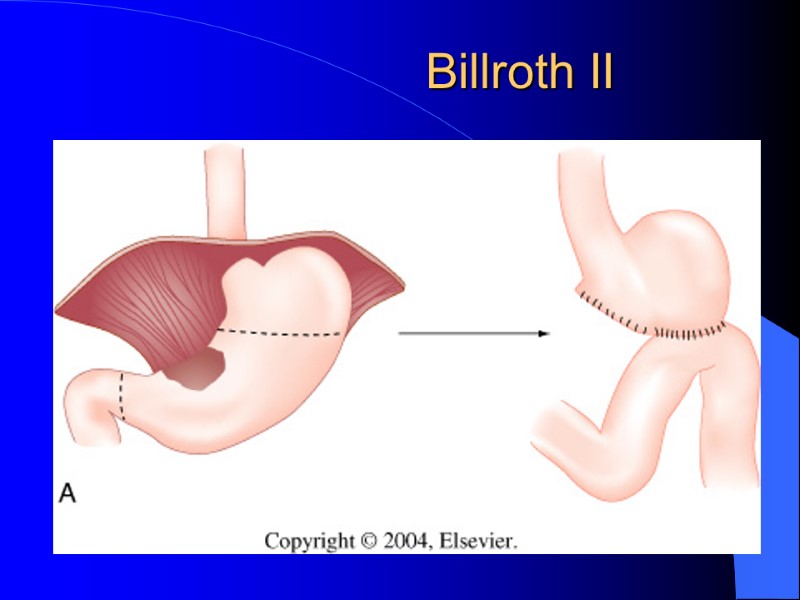
Billroth II
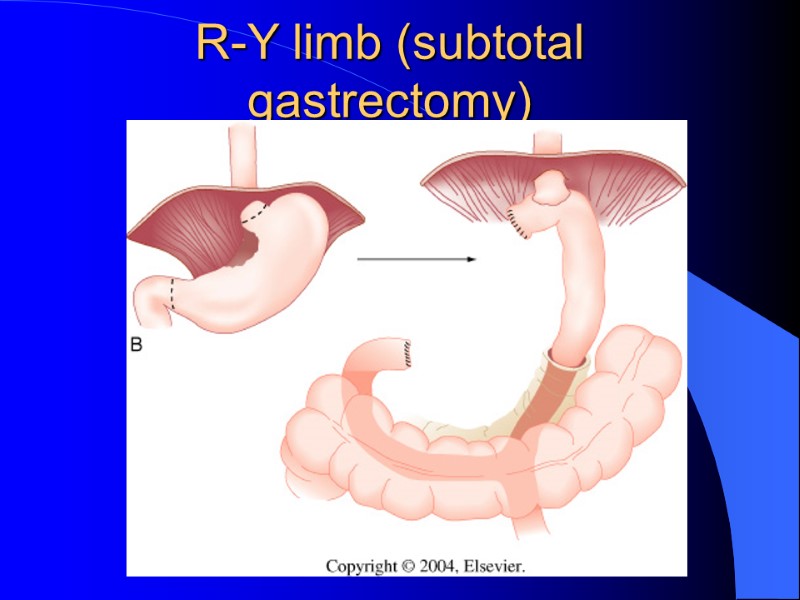
R-Y limb (subtotal gastrectomy)
Elective Surgical Therapy Type IV
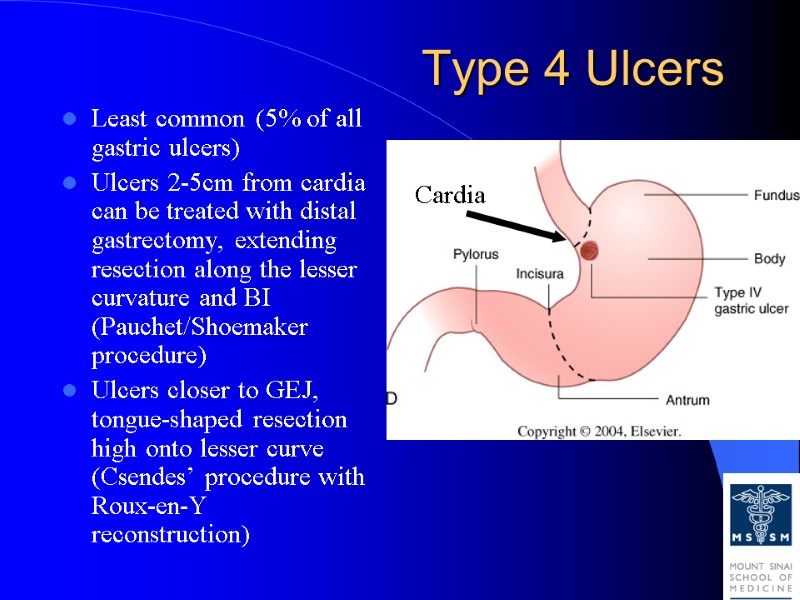
Type 4 Ulcers Least common (5% of all gastric ulcers) Ulcers 2-5cm from cardia can be treated with distal gastrectomy, extending resection along the lesser curvature and BI (Pauchet/Shoemaker procedure) Ulcers closer to GEJ, tongue-shaped resection high onto lesser curve (Csendes’ procedure with Roux-en-Y reconstruction) Cardia
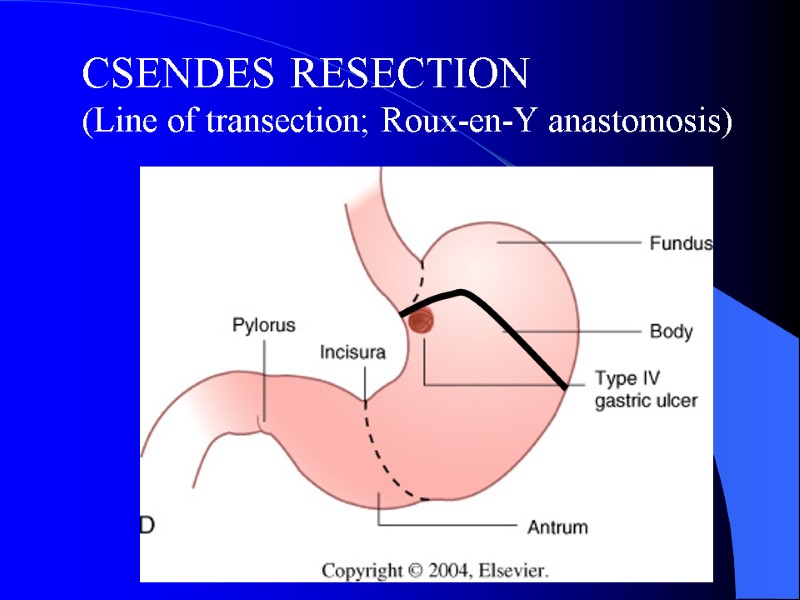
CSENDES RESECTION (Line of transection; Roux-en-Y anastomosis)
Elective Surgical Therapy Giant Gastric Ulcer
Giant Gastric Ulcer Giant gastric ulcer: >3cm; 30% malignancy risk Subtotal gastrectomy with Roux-en-Y (high morbidity and mortality) Kelling-Madlener procedure: less aggressive, antrectomy, BI reconstruction, bilateral truncal vagotomy, leave ulcer, multiple biopsies, cautery of ulcer
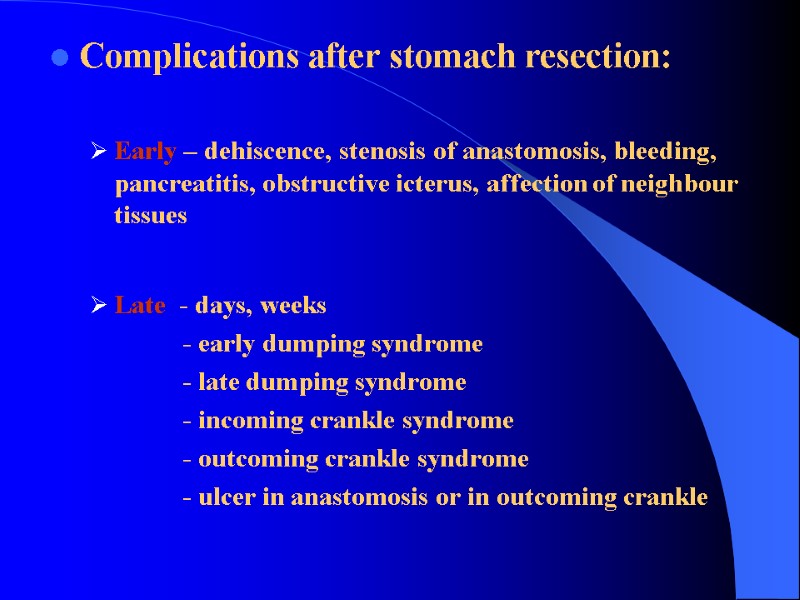
Complications after stomach resection: Early – dehiscence, stenosis of anastomosis, bleeding, pancreatitis, obstructive icterus, affection of neighbour tissues Late - days, weeks - early dumping syndrome - late dumping syndrome - incoming crankle syndrome - outcoming crankle syndrome - ulcer in anastomosis or in outcoming crankle
Early Complications (1) 1. Failure of the stomach or stomach remnant to empty occurs after any procedure. It was formerly common after vagotomy and drainage. Causes are: A. Prolonged paralysis of stomach (doubtful) B. Edema at a stoma C. Fluid and electrolyte disorder, especially hypokalaemia. Management is conservative with NG suction, fluid, electrolyte and nutritional replacement.
Early Complications (2) 2. Intestinal obstruction. Causes are: A. Adhesive. B. As a consequences: (a) Twisting of the loop of a gastrojejunostomy after polya gastrectomy. (b) Herniation of loops through a mesenteric defect. (c) Retrograde intussusception of the efferent loop of a gastrojejunostomy (rare). Prophylaxis: avoid causes – such as mesenteric cul de sacs or holes Treatment: operative
Early Complications (3) 3. Fistulae. Can occur after any operation, which involves a suture line. Most usual sites are: 1. After polya gastrectomy i. Duodenal stump ii. Pancreases from trying to dissect out a difficult ulcer 2. Occasionally at a Pyloroplasty
Early Complications (4) 4. Acute pancreatitis. May follow any procedure. Its etiology is unknown, but some cases are traumatic
Late Complications (1) Anastomotic and recurrent ulceration Causes: Inadequate resection of parietal cell mass. Isolated antrum left after polya gastrectomy. Zollinger – Ellison syndrome. Incomplete vagotmy. Persistent suture in the anastomosis. More usually this is merely a suture exposed as a consequence of ulceration from another cause. Prophylaxis: adequate primary treatment. Management is related to cause and requires investigation to ascertain the level of acid secretion or the completeness of vagotomy. Recurrence after vagotomy is best managed by polya gastrectomy.
Late Complications (1) 2. Gastrojejunocolic fistulae. Occurs when a recurrent ulcer after gastrojejual anastomosis penetrates into the colon. It should arouse the suspicion of Zollinger-Ellison syndrome. Clinical features: Severe diarrhea occurs due to enteritis caused by cronic contents passing directly into the small bowel and acidosis, dehydration, potassium loss, anaemia and cachexia will result in death if the fastula is not interrupted surgically. Treatment: 1. Good risk patient. Excision of the gastric, jejunal and colonic components and the construction of a higher gastrectomy. 2. Poor risk patient. A staged procedure: (a) Stage 1: Proximal colostomy which, diverts the faecal stream from the fistula and thus stops the enteritis. (b) Stage 2: Excision of fistula and its visceral components and the construction of a higher gastrectomy and colonic anastomosis. (c) Stage 3: Closure of colostomy.
Early dumping syndrome: group of symptoms approved shortly after meal appears after BII resection vasomotoric sy. - face redness, fall of blood pressure, dizziness GI sy. - vomiting, diarrhoea Th.: diet, no sugar, low quantities of food, change BII to BI resection
Late dumping syndrome: hypoglycaemia (sugar is not enough digested) appears after BII resection weakness, perspiration, dizziness, tremor cca 3h after meal Th.: no sugar, change BII to BI resection
Anemia Partial gastrectomy and polya reconstruction interferes with duodenal absorption of iron and a macrocytic anemia may result More rarely, sufficient stomach has been removed to cause failure of release of intrinsic factor and thus a macrocytic anemia Malnutrition may contribute to both.
Weight loss and its complications Particulary after partial gastrectomy when patients are unwilling to eat sufficiently, weight loss is common Severe malnutrition is rare, but there is an increased risk of nutrition-associated diseases such as tuberculosis.
Bilious vomiting Any operation which, destroys or bypasses the pylorus allows bile to reach the stomach. Not only does this produce atrophic gastritis but also it may be associated with bilious vomiting. This is more likely after a polya gastrectomy where characteristically a patient eats a meal and some to 10 to 20 minutes later vomits bile only. In severe cases, either normal anatomy should be restored or the bile diverted more distally into the intestine.
Diarrhea Apart from the dumping syndrome, all vagotomies except highly selective ones seem to cause diarrhea Matters are made worse if cholecystectomy has been done or is subsequently done
Acute Gastritis (erosive) Stress erosions are usually multiple, small punctuate lesion in the proximal acid secreting portion of the stomach Clinical Settings: Severe illness, trauma, burns (Cushing ulcer) or sepsis Due to (-) mucosal defense (ischemia) Drug and Chemical ingestion Aspirin / NSAIDs CNS trauma: Increase gastrin ---> elevated acid secretion Curling ulcer
Acute Gastritis Pathogenesis: Aspirin, bile salts (backflow), alcohol Mucosal ischemia Clinical manifestations: Gastrointestinal bleeding Abdominal pain Diagnosis: Endoscopy / radionuclide scanning / visceral angiography
Acute Gastritis Treatment: NPO NGT / Saline lavage Antacids / omeprazole / sucralfate Intra-arterial infusion of vasopressin Surgery --> if 6-8 units over 24 hrs Mortality ---> 40% Near total gastrectomy Vagotomy + pyloroplasty + over sewing of bleeder Partial gastrectomy + vagotomy
Zollinger-Ellison Syndrome (Gastrinoma) Symptoms tends to be more severe, unrelenting and less responsive to therapy. Clinical Manifestation: Pain Diarrhea Steatorrhea Diagnosis: Acid secreting studies (50meq/hr) UGIS Radio-immuno assay for serum Gastrin level Diff: a) Pernicious anemia b) Renal insufficiency c) Antral gastrin hyperplasia or hyperfunction CT scan and angiography to localize gastrinoma Venous sampling
16066-darspeptic_ulcer.ppt
- Количество слайдов: 61

