e9796aa0c000da633d01e45f013c2de0.ppt
- Количество слайдов: 92

Gas Conditioning During Mechanical Ventilation BY AHMAD YOUNES PROFESSOR OF THORACIC MEDICINE Mansoura Faculty of Medicine
Introduction • In 1871, Friedrich Trendelenburg described the first endo-tracheal intubation for administration of general anesthesia. Since then, there has been a growing body of literature addressing the effect of dry gases on respiratory tract of intubated patients. • After three hours of exposure to dry anesthetic gas, respiratory epithelial cells had 39% cilliary damage, 39% cytoplasmic changes, and 48% nuclear changes In the group exposed to dry gas, mucous flow had reduced clearance velocity compared to the group that inhaled completely humidified gas. • Due to unfavorable effects of inadequate humidification of exposure to dry anesthetic gas on the respiratory tract , humidification during invasive mechanical ventilation is currently an accepted standard of care
Physiological Airway Control of Heat and Humidity • Humidity is the amount of water in vaporous state contained in a gas. • Absolute humidity (AH) is the weight of water present in a given volume of gas and it is usually expressed in mg/L. • Relative humidity (RH) is the ratio of the actual weight of water vapor (AH) relative to the gas capacity to keep water vapour at a specific temperature. • Whenever the amount of gas contained in a sample is equal to its water vapor capacity, the RH is 100% and the gas is completely saturated. • It is important to understand that water vapor capacity of a sample will increase exponentially to the temperature Therefore, if the absolute humidity remains constant, RH will decrease whenever the temperature increases (because the denominator increases), and RH will increase when the temperature decreases (because the capacity to hold water vapor decreases).
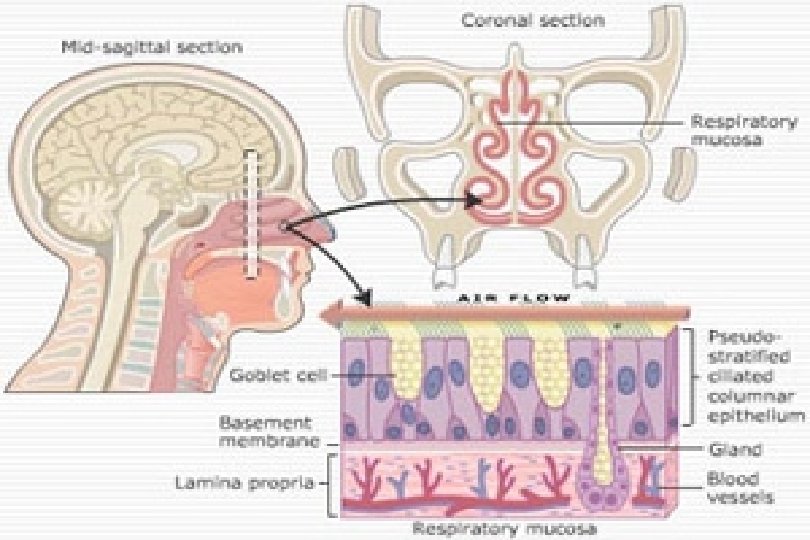
Physiological Airway Control of Heat and Humidity • The connective tissue of the nose is characterized by a rich vascular system of numerous and thin walled veins. This system is responsible for warming the inspired air to increase its humidity carrying capacity. • As the inspired air goes down the respiratory tract, it reaches a point at which its temperature is 37 ∘C and its relative humidity is 100%. This point is known as the isothermic saturation boundary (ISB), and it is usually located 5 cm below the carina.
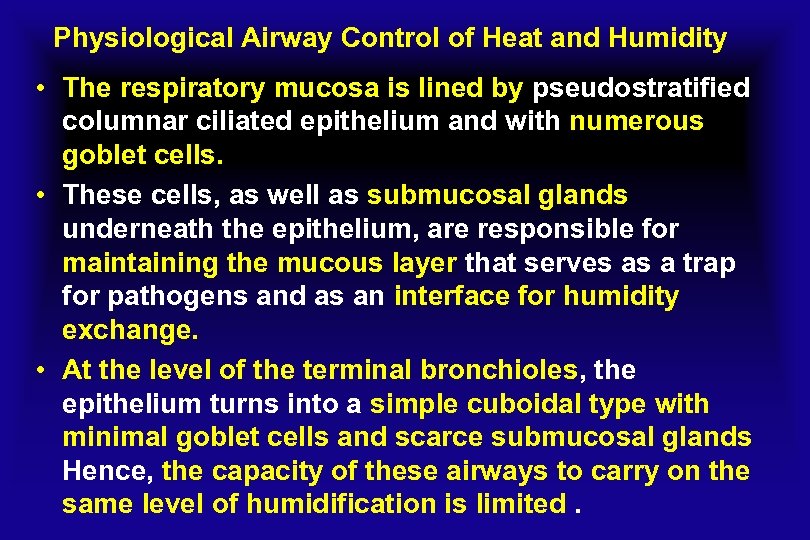
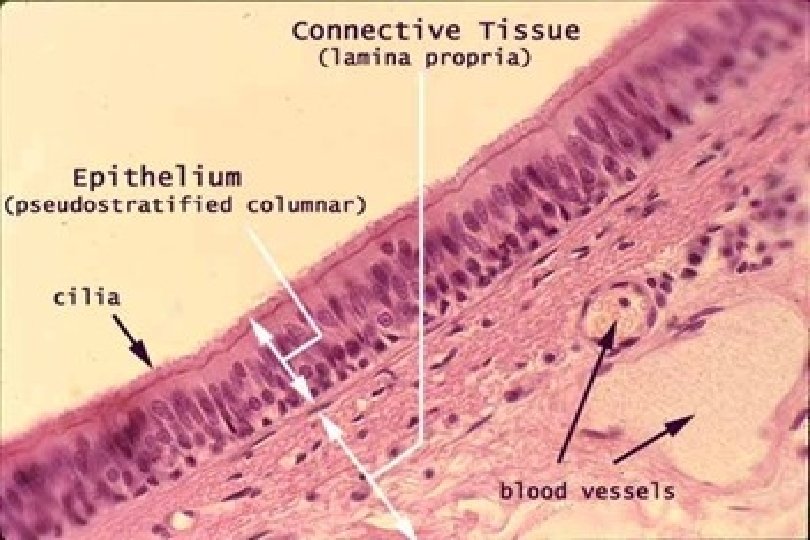
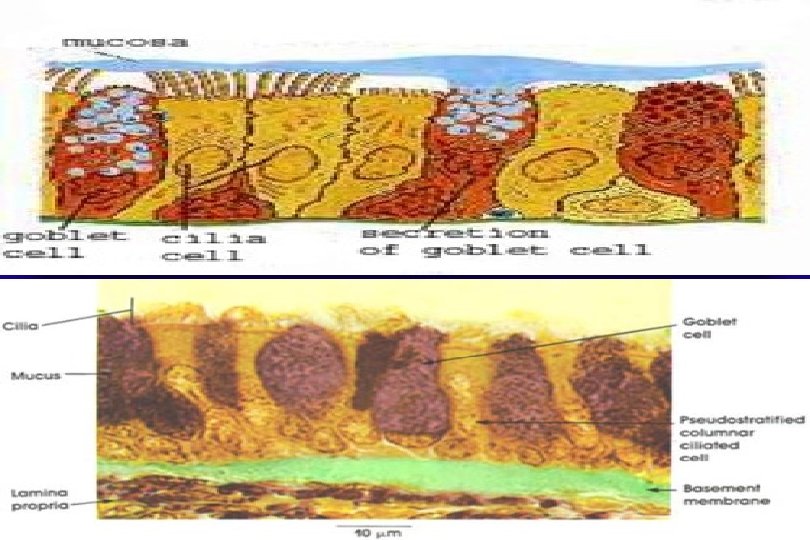
Physiological Airway Control of Heat and Humidity • The respiratory mucosa is lined by pseudostratified columnar ciliated epithelium and with numerous goblet cells. • These cells, as well as submucosal glands underneath the epithelium, are responsible for maintaining the mucous layer that serves as a trap for pathogens and as an interface for humidity exchange. • At the level of the terminal bronchioles, the epithelium turns into a simple cuboidal type with minimal goblet cells and scarce submucosal glands Hence, the capacity of these airways to carry on the same level of humidification is limited.
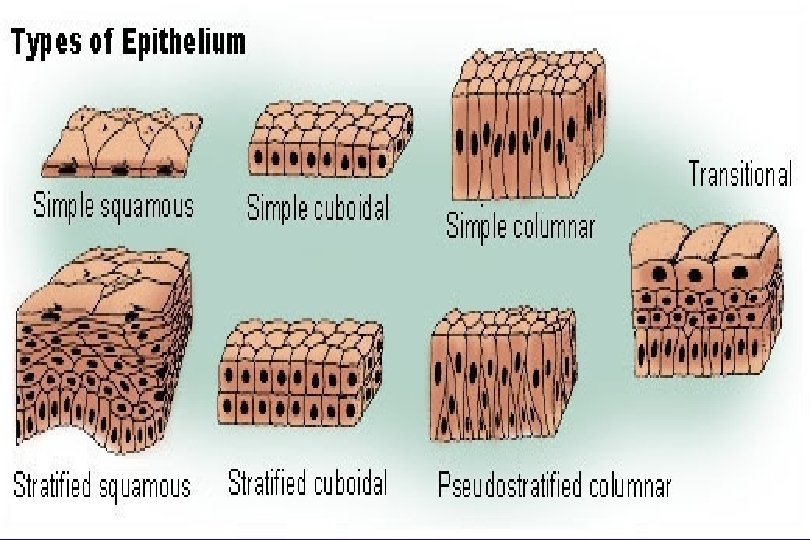
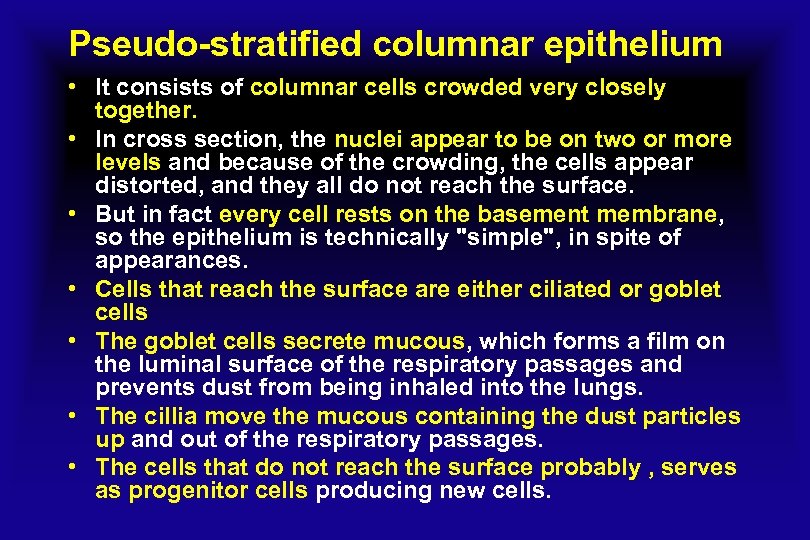
Pseudo-stratified columnar epithelium • It consists of columnar cells crowded very closely together. • In cross section, the nuc. Iei appear to be on two or more levels and because of the crowding, the cells appear distorted, and they all do not reach the surface. • But in fact every cell rests on the basement membrane, so the epithelium is technically "simple", in spite of appearances. • Cells that reach the surface are either ciliated or goblet cells • The goblet cells secrete mucous, which forms a film on the luminal surface of the respiratory passages and prevents dust from being inhaled into the lungs. • The cillia move the mucous containing the dust particles up and out of the respiratory passages. • The cells that do not reach the surface probably , serves as progenitor cells producing new cells.
Physiological Airway Control of Heat and Humidity • After endotracheal intubation, as the upper airway loses its capacity to heat and moisture inhaled gas, the ISB is shifted down the respiratory tract. • This imposes a burden on the lower respiratory tract, as it is not well prepared for the humidification process. Consequently, delivery of partially cold and dry medical gases brings about potential damage to the respiratory epithelium, manifested by increased work of breathing, atelectasis, thick and dehydrated secretions, and cough and / or bronchospasm. • Notably, there are other factors that may shift the ISB distally producing the same effects, such as mouth breathing, cold and dry air breathing, and/or high minute ventilation. • inhalation of large volumes of cold air during exercise is thought to be the inciting event of exercise-induced asthma.
Physiological Airway Control of Heat and Humidity • During the exhalation process, the expired gas transfers heat back to the upper airway mucosa. • As the airway temperature decreases, the capacity to hold water also decreases. Therefore, condensed water is reabsorbed by the mucosa, recovering its hydration. • Importantly, in periods of cold weather, the amount of water condensation may exceed the mucosal capacity to accept water. Therefore, the remaining water accumulates in the upper airway with consequent rhinorrhea. • In order to avoid the aforementioned consequences associated with lack of humidification in mechanically ventilated patients, a variety of devices (humidifiers) have been introduced in clinical practice. • The human airway must provide gas at core temperature and 100% RH at the alveolar surface in order to optimize gas exchange and protect lung tissue.
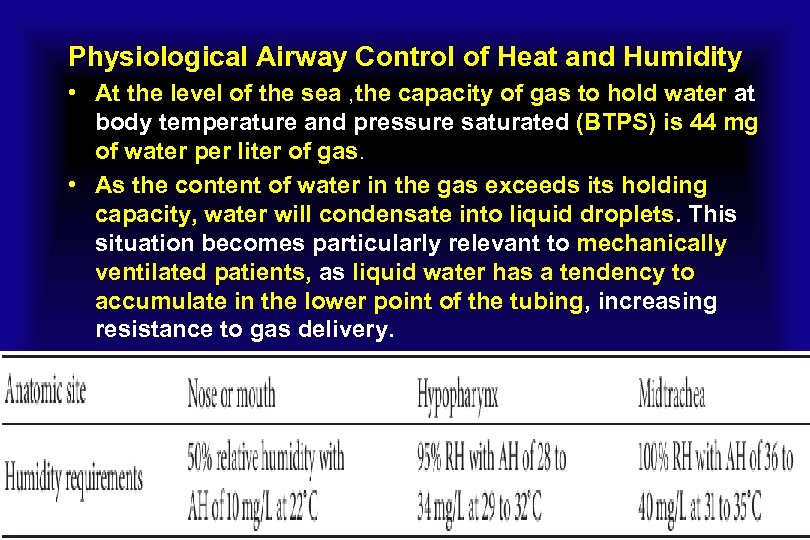
Physiological Airway Control of Heat and Humidity • At the level of the sea , the capacity of gas to hold water at body temperature and pressure saturated (BTPS) is 44 mg of water per liter of gas. • As the content of water in the gas exceeds its holding capacity, water will condensate into liquid droplets. This situation becomes particularly relevant to mechanically ventilated patients, as liquid water has a tendency to accumulate in the lower point of the tubing, increasing resistance to gas delivery.

Effects of inefficient gas conditioning during non-invasive ventilation • Non-invasive ventilation (NIV) is a mechanical ventilation modality that does not utilize an invasive artificial airway (endotracheal tube or tracheostomy tube). • NIV is usually delivered through a nasal or oro-nasal mask so the inspired gas passes through the upper airway where it is conditioned. • Like during spontaneous breathing, patients under NIV require adequate humidification and heating of the inspired air (that is, gas conditioning). • NIV delivers inspired air at high flow rates, which may overwhelm the usual airway humidification mechanisms. • Inadequate gas conditioning has been associated with negative effects on tolerance to NIV when a patient breathes inadequately humidified air.
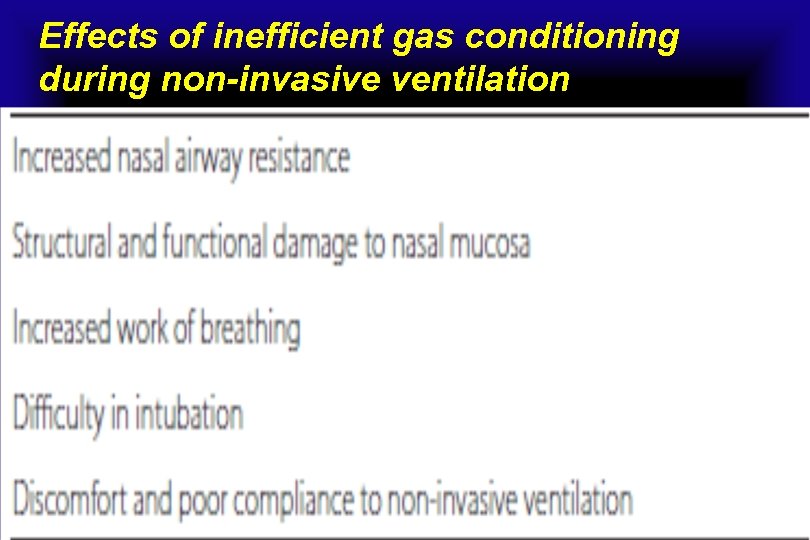
Effects of inefficient gas conditioning during non-invasive ventilation
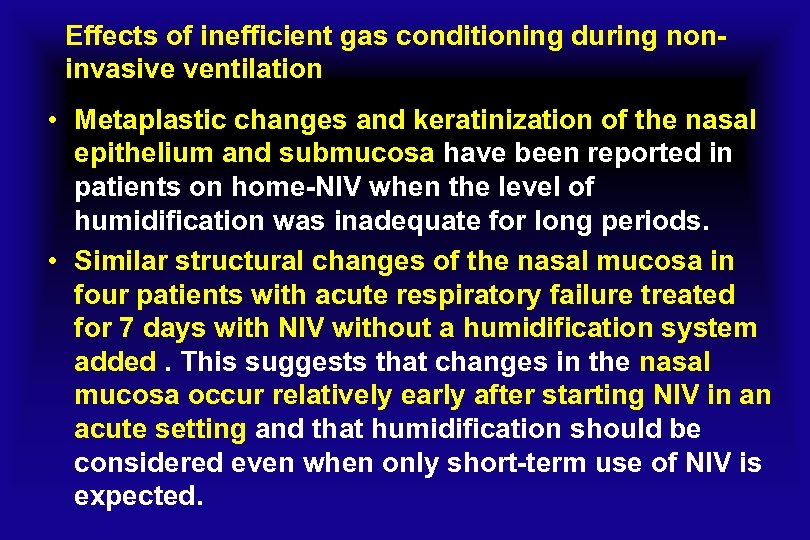
Effects of inefficient gas conditioning during noninvasive ventilation • Metaplastic changes and keratinization of the nasal epithelium and submucosa have been reported in patients on home-NIV when the level of humidification was inadequate for long periods. • Similar structural changes of the nasal mucosa in four patients with acute respiratory failure treated for 7 days with NIV without a humidification system added. This suggests that changes in the nasal mucosa occur relatively early after starting NIV in an acute setting and that humidification should be considered even when only short-term use of NIV is expected.
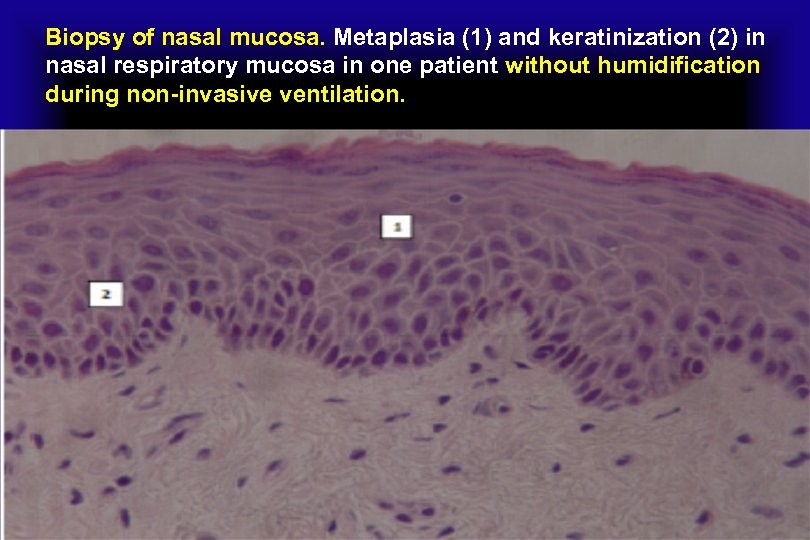
Biopsy of nasal mucosa. Metaplasia (1) and keratinization (2) in nasal respiratory mucosa in one patient without humidification during non-invasive ventilation.
Metaplasia versus Dysplasia • Dysplasia comes from the root Greek term meaning ‘bad formation’. It is a pathological term used to refer to an irregularity that hinders cell maturation within a particular tissue; • Dysplasia in general comprises of the increased growth of immature cells with a simultaneous reduction in the growth of mature cells, their numbers and their site of growth. • Dysplasia is the indication of a premature neo-plastic progression. It directly indicates a state when the cellular defect is constrained within the tissue origin, for instance in case of an in-situ neoplasm. • Dysplasia basically comprises of four distinct stages of pathological change. These are, Anisocytosis or the growth of cells of disproportionate size, Poikilocytosis or the growth of unusually shaped cells, Hyperchromatism and lastly the presence of mitotic lumps of cells that continuously keep on dividing
Metaplasia versus Dysplasia • Metaplasia derives from the original Greek term denoting ‘change in form’. It is the process of the reversible substitution of a distinct kind of cell with another mature cell of another differentiated kind. • The transformation from one cell type to another in Metaplasia is often the result of the initiation caused by an unusual stimulus. • The original cells in this case are not strong enough to survive in a new environment comprising of unknown and abnormal stimuli. • A condition of Dysplasia where the growth and differentiation of cells are delayed are compared with Metaplasia where a mature cell of a distinct kind is replaced by another mature cell of yet another distinguished type.
Metaplasia versus Dysplasia • Dysplasia is a pathological term used to refer to an irregularity that hinders cell maturation within a particular tissue whereas Metaplasia is the process of the reversible substitution of a distinct kind of cell with another mature cell of the similar distinct kind. • Dysplasia is cancerous whereas Metaplasia is non-cancerous. • Metaplasia can be stopped by removing the abnormal stimulus, but Dysplasia is a nonreversible process.
Keratinized versus Non-keratinized Epithelium • Keratinized tissue like the skin has lots of vessicles containing keratohyaline, a protein that eventually turns into keratine when the cell dies, providing that epithelium with protection and resistance to traction and friction, and it makes it impermeable. • The only epithelium that keratinizes is stratified squamous, and it only happens in the skin (in normal conditions). • Non keratinized tissue does not offer as much protection and allows the diffusion of materials through the cell junctions and the cell's body.
Keratinized versus Non-keratinized Epithelium Kertinized Suamous Epithelium: 1. The cells of few outer layers of stratified squamous epithetium replace their cytoplasm with a hard water proof protein 2. The layers of flat dead cells-stratum corneum or horney layers are present. 3. It forms epidermis of the skin of land vertebrates. 4. It prevents loss of water and mechanical injury. Non-kertinized Epithelium: 1. It has living squamous cells at the surface. 2. Strtum corneum absent as non-kertinization or cornification occurs. 3. It is formed in lining of cornea, mouth, pharynx, oesophagus, vocal cords, vigina, cervix etc. 4. It provides mechanical protection from injury.
Effects of inefficient gas conditioning during non-invasive ventilation • Inadequate airway gas conditioning may have serious consequences in critically ill patients using NIV. • Difficulties were recently reported with intubation in patients failing a trial of NIV delivered at high inspiratory oxygen fraction with a low level of humidification. • One case study showed inspissated secretions, causing lifethreatening airway obstruction in a patient using NIV for hypoxemic respiratory failure. • A high fraction of inspired oxygen was also entrained into the NIV circuit and this extra anhydrous gas may have contributed to the airway obstruction. • Inadequate humidification can also cause significant discomfort for chronic NIV users.
Effects of inefficient gas conditioning during noninvasive ventilation • Dryness elated symptoms started to appear when AH was lower than 15 mg H 2 O/L. • This was associated with increased nasal airway resistance (NAWR). • Heated Humidification improved comfort and compliance to NIV. • In healthy subjects under CPAP delivered by a oro-nasal mask, when a humidification device was applied and AH was higher than 10 to 12 mg. H 2 O/L , comfort was significantly better.
Effects of inefficient gas conditioning during non-invasive ventilation • In home-NIV, comparing two humidification systems, HH and a heat and moisture exchange filter (HME); compliance was much better (75% of patients) with the former. However, other symptoms, such as dry throat, the number of hospital admissions and the rate of complications caused by infection (mainly pneumonia), were similar with the two systems. • Similar results were published stressed the importance of ‘early’ humidification from the very start of ventilator treatment, so as to ensure the best possible compliance in home-NIV patients.
Contributors to gas conditioning during non-invasive ventilation • Analysis of the need for gas conditioning during NIV must clearly take account of the following parameters: 1 ) Air leaks; 2) Interface for NIV delivery; 3) Type of ventilator; 4) Room temperature; 5) Temperatures of inhaled gas and the vaporization chamber; 6) Airflow and pressure at the entrance of the humidification system; and 7) Type of humidification system.
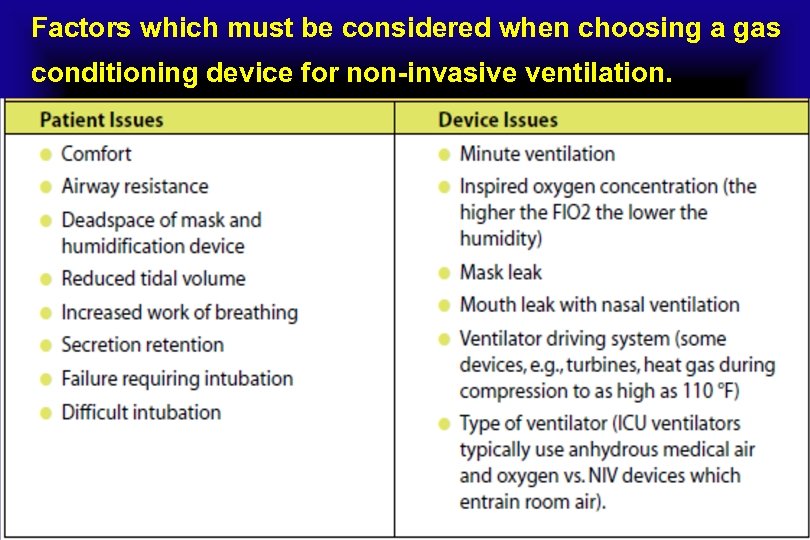
Factors which must be considered when choosing a gas conditioning device for non-invasive ventilation.
How to convert Fahrenheit to Celsius • The temperature T in degrees Celsius (°C) is equal to the temperature T in degrees Fahrenheit (°F) minus 32, times 5/9: • T(°C) = (T(°F) - 32) × 5/9
Air leaks • Mouth and / or peripheral mask air leaks, especially in tachypneic patients under NIV, cause unidirectional nasal airflow, so the mucosa recovers less heat and moisture during expiration. This may cause a continuous drop in AH. • An increase in NAWR is the typical consequence of large mouth air leaks during NIV from a nasal mask. This reflects the nasal vaso-constrictive response to prolonged inhalation of dry air. • The flow of cold air through the nose dries the mucosa, resulting in the release of vaso-active and pro-inflammatory mediators. These boost superficial mucosal blood flow and cause engorgement of deeper capacitance vessels, leading to increased nasal resistance. This in turn promotes mouth breathing, setting up a vicious circle. • Increased NAWR is likely to lead to unsuccessful acclimatization to NIV.
Air leaks • Most current CPAP devices come with an integrated HH system. As these deliver more moisture than cold pass-over humidifiers, they may be more effective in patients with mouth leak and nasal congestion. • HH reduces nasal symptoms and nasal resistance , consequently attenuating inflammatory cell infiltration and fibrosis of the nasal mucosa. Therefore, the American Academy of Sleep Medicine has recommended the use of HH to improve CPAP compliance and adherence as a standard of practice.
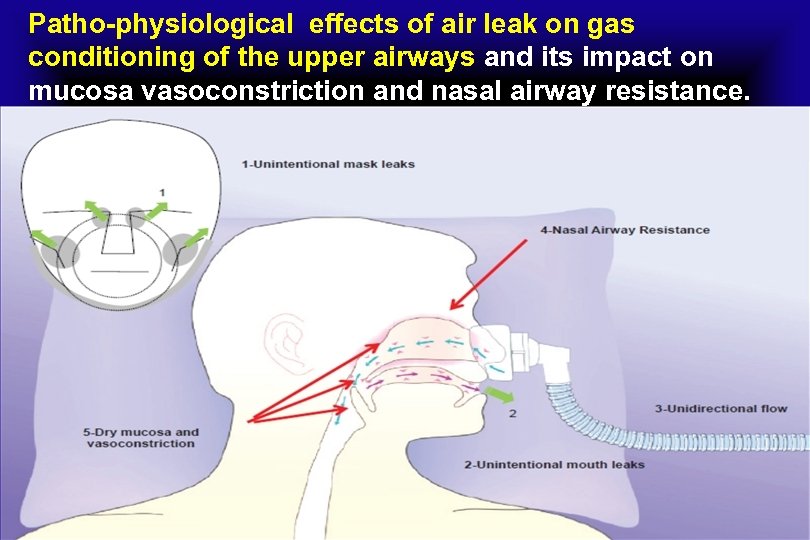
Patho-physiological effects of air leak on gas conditioning of the upper airways and its impact on mucosa vasoconstriction and nasal airway resistance.
Air leaks • Air leaks affect the performance of HMEs because the HME recovers less moisture when the expired air is drier. • The site of the leak, either unintentional (around the mask) or intentional (mask or circuit) also affects humidity. • While the unintentional leaks are likely to have a substantial impact on AH because of the compensatory increase in inspiratory flow, the intentional leaks are not known to contribute to insufficient humidification of air during NIV. • We can only speculate that inefficient washout of the exhaled air throughout an unintentional leak system (that is, plateau valve, anti-rebreathing valve) is likely to involve a substantial degree of humidity, especially in interfaces with high dead space, such as a total face mask.
Air leaks • In a study in adult volunteers, nasal CPAP with a mouth leak resulted in a three-fold increase in NAWR that was substantially attenuated by effective humidification. • This high NAWR would result in substantially lower effective pressure being transmitted to the nasopharynx and subsequently to the distal airway.
Interfaces • The most common interfaces used to deliver NIV are nasal and facial masks, the former being tolerated better in the chronic than the acute setting. • Nasal masks tend to have more leaks than face masks, and this can result in inadequate gas conditioning of inspired air. • The use of an oro-nasal mask avoids the changes in RH related to mouth leaks. This choice is likely to be crucial to the success of NIV in selected categories of acute patients (for example, need for prolonged ventilator support, difficulty in spontaneously clearing secretions , mouth-breathers).
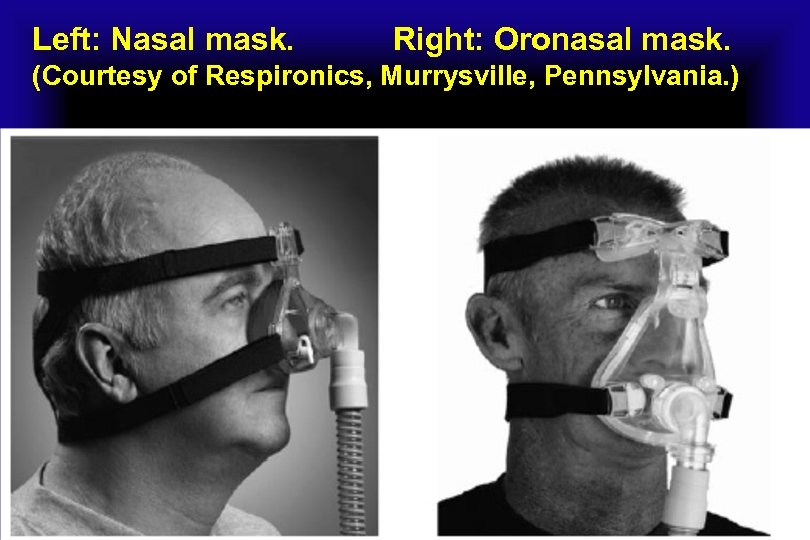
Left: Nasal mask. Right: Oronasal mask. (Courtesy of Respironics, Murrysville, Pennsylvania. )
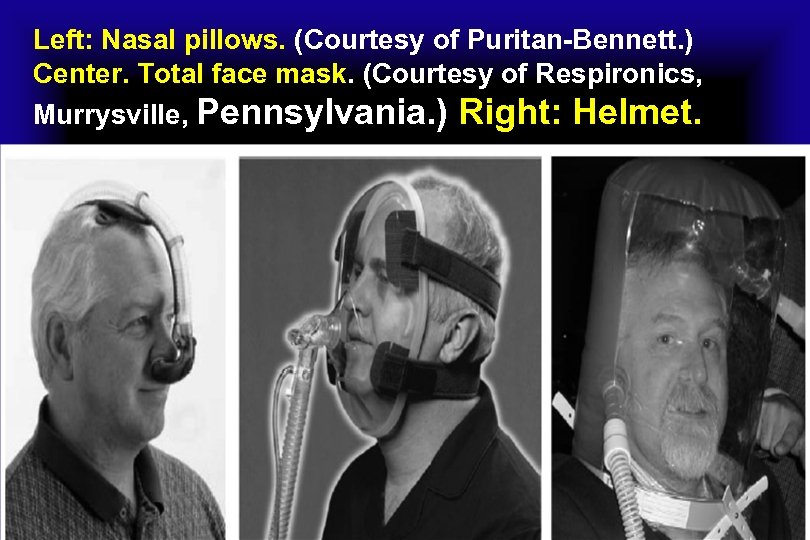
Left: Nasal pillows. (Courtesy of Puritan-Bennett. ) Center. Total face mask. (Courtesy of Respironics, Murrysville, Pennsylvania. ) Right: Helmet.
Interfaces • • Compared to the other more popular interfaces (nasal, oro-nasal, total face masks), the helmet has a much larger inner space (more than 10 liters), which may act as a ‘reservoir’ of humidity because of the amount of exhaled gas that remains there. The clinician must therefore carefully adjust the humidification of the inhaled gas depending on the type of interface and the resulting leak pattern.
Ventilator types • Intensive care ventilators, home-care mechanical ventilators, and high-flow CPAP systems operate by providing a very high inspiratory flow to compensate for the inspiratory demand of a patient with acute respiratory failure and the air leaks when applied in a NIV mode. • Single-circuit home ventilators and/or dedicated NIV ventilators equipped with a turbine or piston differ from double-circuit ICU ventilators, which are pneumatic and supplied with high-pressure sources of gas. • Home models - that is, blower-based devices - compress room air and have higher humidity than ICU ventilators, which obtain dry gas directly from a mains hospital outlet. • So , ICU ventilators provided a lower level of AH during NIV than turbine mechanical ventilators (5 versus 13 mg. H 2 O/L).
Ventilator types • we have to bear in mind that AH lower than 5 mg. H 2 O/L is ‘critical’ for the likelihood of complications related to inadequate gas conditioning of inspired air. • Physicians have also to remember that the higher the oxygen fraction delivered during NIV, the greater the risk of inadequate gas conditioning without the addition of HH or a HME.
Ambient temperature • Even though insufficient humidification during NIV can be caused by specific climatic or environmental conditions in the place where the treatment is implemented (for example, an excessively cold sleeping area), the majority of cases suffering from excessive airway dryness are due to technical factors related to the ventilation process itself and its interaction with the patient (interface, leaks, inspired oxygen fraction, respiratory rate, use of humidifiers). • The effects of ambient temperature probably only need be considered for patients who sleep in very cold premises.
Res Med Climate Line™ • Unique to Res. Med, the Climate Line heated tube works with our exclusive Climate Control system* to deliver a constant comfortable temperature at the mask throughout the night, even as temperature and humidity levels change. • The Climate Line heated tube is smaller, slimmer and sleeker than your average mask tubing, resulting in increased flexibility and less mask drag for a more comfortable night’s sleep. • *The Climate Control system is available in Res. Med’s S 9™ Series of devices
Res. Med Climate Line Air • Climate Line Air is our most advanced heated tubing and it’s the key that unlocks Res. Med's Climate Control solution for the Air. Sense™ 10 and Air Curve™ 10 series of devices. • Climate Line Air Oxy is a variant of Climate Line Air that comes with a built‐in oxygen connector for patients who require supplemental oxygen.
Climate Line™ Max Oxy Air Tubing • The Climate Line™ Max Oxy Air Tubing with Supplemental Oxygen Port is a 19 mm inner diameter, heated tubing with a port to add oxygen to the air stream. It is for use ONLY with a Res Med S 9 Series machine using an H 5 i Heated Humidifier. • The Climate Line tubing uses a sensor that measures humidity to maintain a uniform temperature from the machine all the way to the mask. • The temperature in the tube itself is warmed by a thin copper wire on the outside of the tube. • The Climate Line™ Max Oxy Air Tubing can easily support higher pressures, such as though frequently found in Bi. Level therapy. • The Climate Line™ Max Oxy Air Tubing with Supplemental Oxygen Port is a latex free product.
Temperature of the inhaled gas • Conditioning inspired gas involves both heating and humidification. • To facilitate gas exchange and protect lung tissue, inspired gas must reach body temperature by the time it arrives at the alveolar surface. How easily this can be achieved depends on the temperature of the inhaled gas. • The ventilator power source affects gas temperature, as turbine-driven systems create more heat than piston-driven ventilators.
Temperature of the inhaled gas • Increasing levels of IPAP have also been reported to raise the gas temperature with a turbine-driven NIV device. This tended to preserve AH at high IPAP levels, but it was not sufficient to maintain adequate humidity when ambient RH was low. • HH set at its highest temperature was most effective in countering the deleterious effects of NIV on delivered humidity. In clinical practice the temperature setting for HH may be based on the patient’s tolerance.
Airflow at the entrance to the humidifier • The impact of the airflow entering the HH humidification chamber is one of the most important physical phenomena affecting airway humidity. • By analyzing the factors underlying humidification capacity over a variable range of airflows at the entrance to the humidification chamber (20, 55, and 90 L/minute). At high flow rates, many commercial humidifiers were unable to generate adequate RH. • This suggests that a humidifier alone may not be enough to ensure adequate humidification of inspired gases, particularly at high flow rates.
Types of Humidifiers • Humidifiers are devices that add molecules of water to gas. They are classified as active or passive based on the presence of external sources of heat and water (active humidifiers), or the utilization of patients’ own temperature and hydration to achieve humidification in successive breaths (passive humidifiers). • Active Humidifiers act by allowing air passage inside a heated water reservoir. These devices are placed in the inspiratory limb of the ventilator circuit, proximal to the ventilator. After the air is loaded with water vapor in the reservoir, it travels along the inspiratory limb to the patient’s airway. • As condensation of water vapor may accumulate as the surrounding temperature of the inspiratory limb decreases, these systems are used with the addition of water traps, which require frequent evacuation to avoid risk of contamination of the circuit.
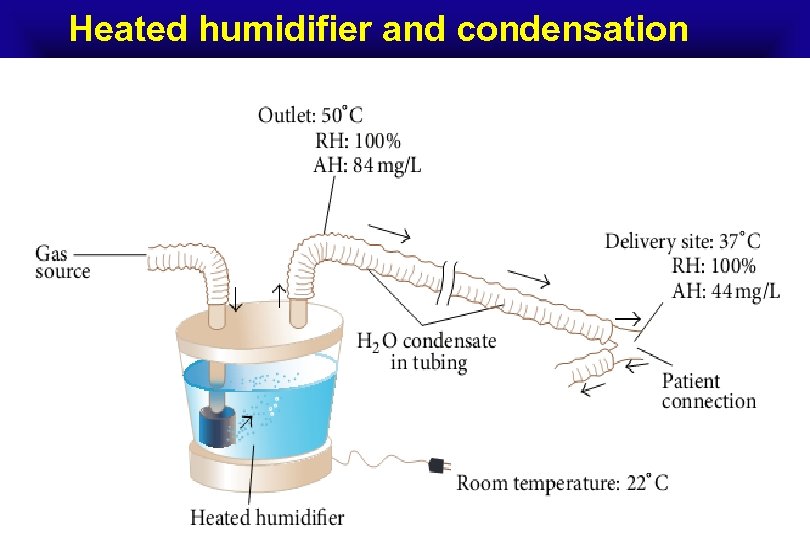
Heated humidifier and condensation
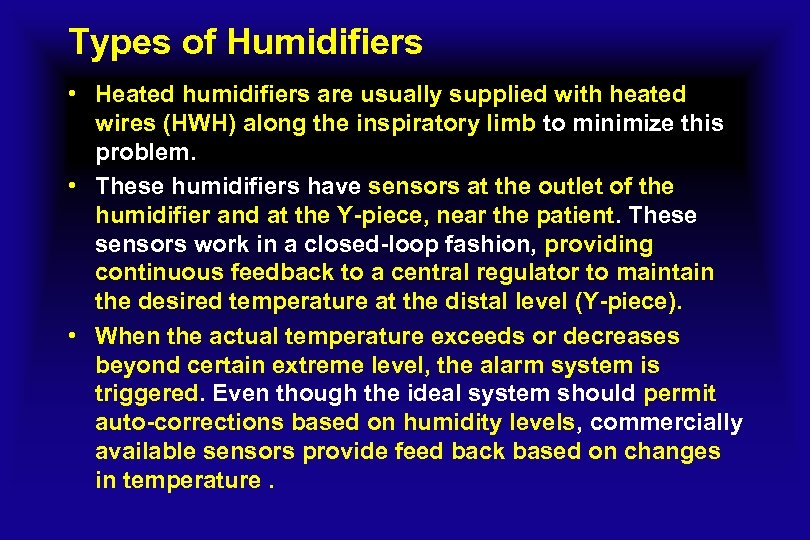
Types of Humidifiers • Heated humidifiers are usually supplied with heated wires (HWH) along the inspiratory limb to minimize this problem. • These humidifiers have sensors at the outlet of the humidifier and at the Y-piece, near the patient. These sensors work in a closed-loop fashion, providing continuous feedback to a central regulator to maintain the desired temperature at the distal level (Y-piece). • When the actual temperature exceeds or decreases beyond certain extreme level, the alarm system is triggered. Even though the ideal system should permit auto-corrections based on humidity levels, commercially available sensors provide feed back based on changes in temperature.
An active humidifier with a heated wire in the inspiratory limb; both temperature sensors, one at the side of the patient and the other at the outlet of the heated reservoir, are shown ,
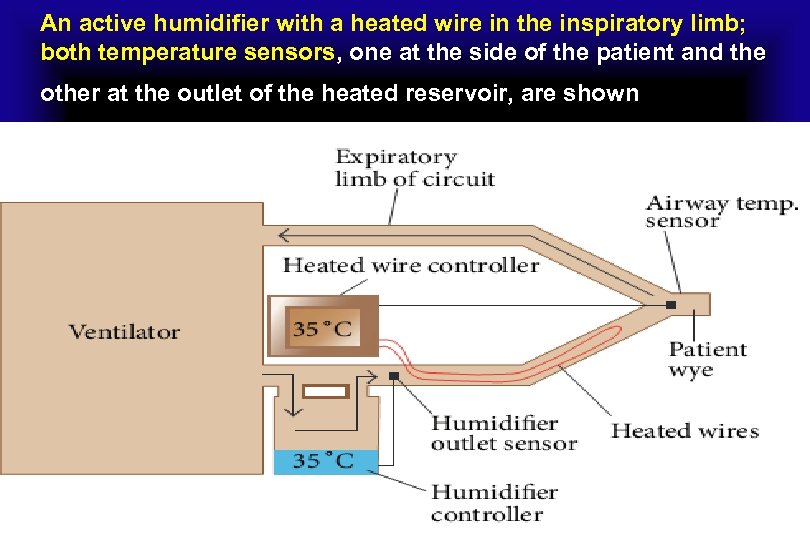
Types of Humidifiers • Usual temperature setting for the current heated humidifiers is 37 ∘C. • The performance of humidifiers may be affected by room temperature, as well as patient minute ventilation. In the last situation, an increase in minute ventilation preserving the same temperature of the heated reservoir may not be adequate to deliver appropriate AH to the patient. • Some humidifiers are supplemented with automatic compensation systems, which compute the amount of thermal energy needed to humidify certain volume of gas and change the temperature of the water reservoir accordingly.
Heated humidifiers are classified as • (1) Bubble. Gas is forced down a tube into the bottom of a water container. The gas escapes from the distal end of the tube under water surface forming bubbles, which gain humidity as they rise to the water surface. • Some of these humidifiers have a diffuser at the distal end of the tube that breaks gas into smaller bubbles. • The smaller the bubbles, the larger the gas-water interface Allowing for higher water vapor content. • Other factors that influence water vapor content of the produced gas are the amount of water in the container and the flow rate. Simply , the higher the water column in the container, the more gas-water interface will ensue, so water levels should be checked on a frequent basis. • In terms of flow rate, when slow flows are delivered, there is more time for gas humidification.
Bubble humidifiers may be unheated or heated . • Typically, unheated bubble humidifiers are used with low-flow oral-nasal oxygen delivery systems. • Heated bubble humidifiers provide higher absolute humidity. They are designed to work with flow rates as high as 100 L/min. These humidifiers usually use diffusers to increase the liquid-air interface. • A problem with heated bubble humidifiers is that they exhibit high resistance to Air flow imposing higher work of breathing than passover ones. Furthermore, they may generate microaerosol. Nevertheless, the amount of aerosol produced by these types of humidifiers may not be clinically significant • Despite this, the use of bubble humidifiers during mechanical ventilation has fallen in favor of passover ones.

(2) Passover • In passover humidifiers , gas passes over a heated water reservoir carrying water vapor to the patient. These are typically used for the purpose of invasive and noninvasive mechanical ventilation. • Another variant of passover humidifiers is the wick one. In this type of device, the gas enters a reservoir and passes over a wick that acts as a sponge that has its distal end immersed in water. • The wick pores provide more gas-water interface allowing for more humidification compared to simple passover humidifiers.
(2) Passover • The water reservoir is fed through a closed system. This system can be supplied with water either manually through a port or float feed system that ensures the water level remains constant all the time. • As dry gas enters the chamber and travels through the wick, heat and moisture increase. Due to the fact that gas does not emerge underneath the water surface, no bubbles are generated.
(2) Passover • A third type of passover humidifier involves a hydrophobic membrane. As with the wick device, dry gas passes through a membrane. • Nevertheless, its hydrophobic characteristic only allows passage of water vapor, precluding liquid water to travel through it. • Similarly to the wick humidifier, bubbles and aerosols are not generated. • These humidifiers are more commonly used during mechanical ventilation than bubble ones due to their lower flow resistance and absence of micro-aerosols.
In all cases • A temperature probe is placed near the Y piece of the ventilator circuit to ensure delivery of gas with optimal temperature. • The presence of condensate in the tubing may increase resistance, which can decrease volume delivered in pressure controlled, or increase peak pressure in volume controlled modes. • The use of these wires does not come without thermal risks. • The AARC clinical practice guidelines recommend gas delivery with a maximum temperature of 37∘C and 100% RH (44 mg. H 2 O/L).
Currently there are 6 types of humidifier heating systems devices • The hot plate element , which sits at the bottom of the humidifier, is one of the most commonly used. Other devices include the wrap around element, which surrounds the humidifier chamber; a collar element, which sits between the reservoir and the outlet; the immersion heater, which is placed directly inside the water reservoir; and the heated wire, which is placed in the inspiratory limb of the ventilator.

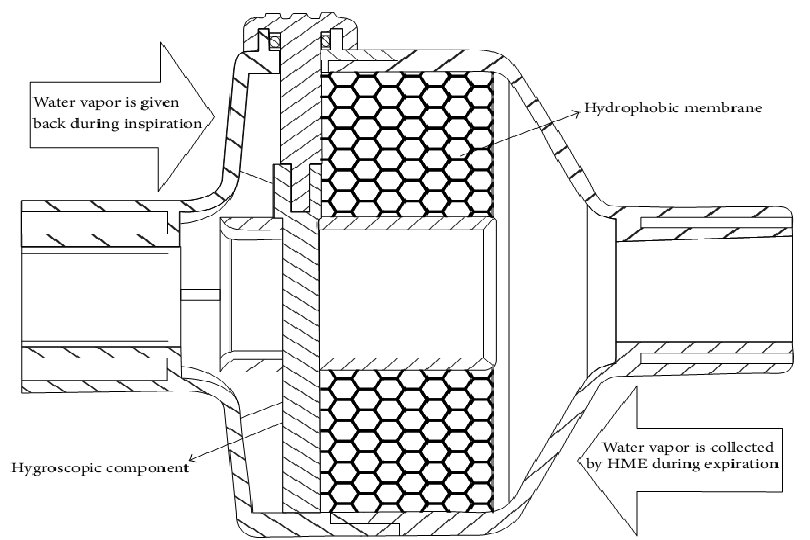
Passive Humidifiers • Heat and Moisture Exchangers (HMEs) are also called artificial noses because they mimic the action of nasal cavity in gas humidification. • They operate on the same physical principle , as they contain a condenser element, which retains moisture from every exhaled breath and returns it back to the next inspired breath. • Unlike heat humidifiers, which are placed in the inspiratory limb of the circuit, these devices are placed between the Y Piece and the patient. • This may increase resistance to airflow not only during inspiration, but also during the expiratory phase.
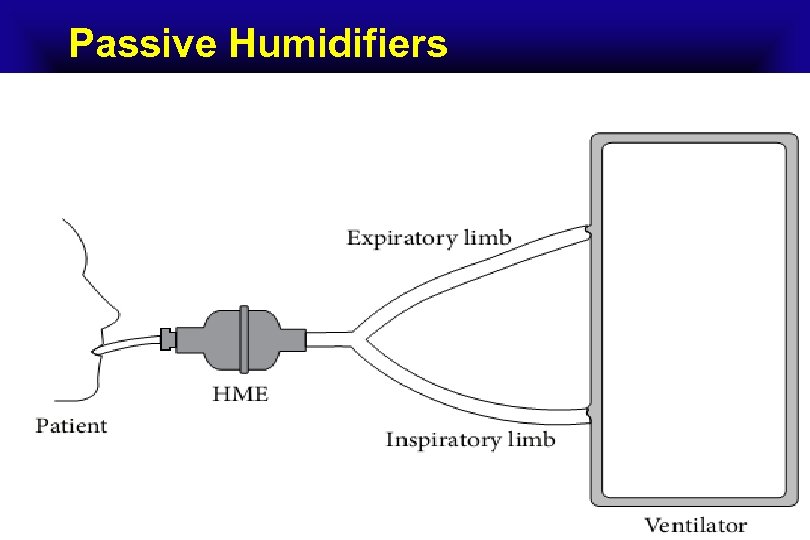
Passive Humidifiers
Passive Humidifiers • In situations in which administration of aerosolized medications is needed, HMEs need to be removed from the circuit to avoid aerosol deposition in HME filters. Otherwise, HMEs with capability to change from “HME function” to “aerosol function” should be used. • Initial designs of HMEs used condensers made of metallic elements that had high thermal conductivity. Thus, they were able to recapture only 50% of the patient’s exhaled moisture. Hence, they provided humidification of 10– 14 mg. H 2 O/L, at tidal volumes (VT) ranging between 500 m. L and 1000 m. L. These devices were known as simple HMEs.
Passive Humidifiers • Newer designs of HMEs include: 1 - Hydrophobic HMEs, the condenser is made of a water repelling element with low thermal conductivity that maintains higher temperature gradients than in the case of simple HMEs. 2 - Combined hydrophobic hygroscopic HMEs, a hygroscopic salt (calcium or lithium chloride) is added inside the hydrophobic HME. These salts have a chemical affinity to attract water particles and thus increase the humidification capacity of the HME. 3 - Pure hygroscopic HMEs have only the hygroscopic compartment. • During exhalation, vapor condenses in the element as well as in the hygroscopic salts. During inspiration, water vapor is obtained from the salts, obtaining an absolute humidity ranging between 22 and 34 mg. H 2 O/L.
Passive Humidifiers • Hydrophobic HMEs were found to cause more narrowing in ETT diameter compared to hygroscopic ones. Therefore, the aforementioned HMEs are not frequently used. • Filters can be added to either hydrophobic or hygroscopic HMEs resulting in a heat and moisture exchanging filter (HMEF). These filters operate based on electrostatic or mechanical filtration. • Based on the predominant mechanism applied, these filters may be classified into pleated or electrostatic filters. • The pleated filters have more dense fibers and less electrostatic charges, whereas the electro-static filters have more electrostatic charges and less dense fibers.
Passive Humidifiers • Pleated filters function better as barriers to bacterial and viral pathogens than electrostatic filters. However, they confer higher airflow resistance. • The pleated nature of the membrane causes a turbulent air flow, which increases the pathogen’s deposition onto the inside of the filter. • The electrostatic filters are subjected to an electric field. Since bacteria and viruses carry electric charges, they get trapped within the electric field of these filters. These filters usually have larger pores than the pleated membranes, and they rely mainly on the electrostatic mechanism. • The previously described filter confers little to the humidification process and increases resistance. Therefore, they are mainly used as barriers to pathogens.
HMEs design and performance standards are defined by the International Organization for Standardization (ISO). • According to these standards, The appropriate HME should have at least 70% efficiency, providing at least 30 mg/L of water vapor. • In a recent study, assessment of the humidification capacity of 32 HMEs. Strikingly, 36% of tested HMEs had an AH of 4 mg. H 2 O/L lower than what was listed by the manufacturer. In fact, in some of them the difference was higher than 8 mg. H 2 O/L.
Passive Humidifiers • Intuitively, as HMEs eliminate the problem of tubing condensation, it may be considered as “elements of choice” to preventilator-associated pneumonia (VAP). Nevertheless, whether the presence of tubing condensate represents an important factor for the development of VAP in well-maintained circuits remains controversial. • HMEs present some shortcomings. Specifically, impaction of secretions or blood within the device may increase airway resistance and work of breathing. In extreme circumstances, complete airway obstruction has been reported. Therefore, patient selection becomes an essential component in the use of HMEs.
Contraindications for heat and moisture exchangers (i) Patients with thick or copious secretions. (ii) When there is loss in expired tidal volume (e. g. , large broncho-pleuro-cutaneous fistulas or presence of endotracheal tube cuff leak). (iii) In patients managed with low tidal volumes like those with ARDS. (iv) In difficult to wean patients and those with limited respiratory reserve. (v) Hypothermic patients with body temperature of<32 ∘C. (vi) In patients with high minute ventilations volumes (>10 L/min).
Passive Humidifiers • In certain devices , an active heated water source can be added to HMEs converting them from passive to active, increasing their humidification capacity. • If the external source of water runs out, these devices will still work as passive HMEs. • Several models exist, including the Booster, the Performer, the Humid Heat, and the Hygrovent Gold.
In the Booster model • The heating unit is incorporated between the HME and the patient. During inspiration the gas passes through the HME carrying water vapor based on the passive operation of the HME and then the heating unit adds to the humidity content of the gas before it reaches the patient. • As water enters the HME-Booster, it saturates the hydrophobic membrane contained in it. The moisture in the saturated membrane is then heated by the positive temperature control element connected to it. • It is thought that the utilization of this device may increase AH by 2 -3 mg/L of H 2 O more than passive HMEs
The performer • The Performer device is characterized by a metal plate in the middle of the HME, in between two hydrophobic and hygroscopic membranes. • This metal plate is heated by an external source that has three sets of temperature to deliver 40 ∘C, 50∘C, and 60 ∘C. • A water source provides it to one end of the humidifier. • The water reaches the two membranes and the metal plate heats it. Then, the water evaporates augmenting vapor content in the inspired gas. • The performer is able to deliver AH of 31. 9 to 34. 3 under normo-thermic conditions.
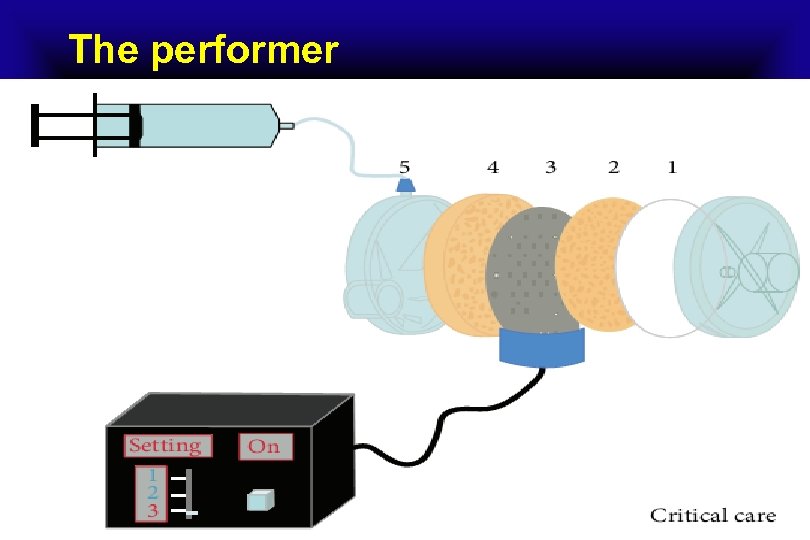
The performer
The Humid Heat • The Humid Heat is a hygroscopic HME that has an external heating source with the water being added at the patient side. • In one bench study, it was found to provide an absolute humidity of 34. 5 mg. H 2 O/L. • Humid Heat has preset values for temperature and humidity. • The only parameter that needs to be set is the value of minute volume of the ventilator, making its use very simple.

The Hygrovent Gold heat-and-moisture exchanger has an adapter into which a heating element is inserted, and a line that continuously supplies water.
Monitoring of Humidification Systems • American Association of Respiratory Care (AARC) recommend a temperature of 33 ± 2 ∘C with RH of 100% and a water vapor level of 44 mg/L. • The clinician commonly faces the issue of relying on different humidifiers without being certain about device accuracy. Independent assessments raise concerns about the validity of data included by the manufacturer. • The most reliable mean to measure humidity is by using a hygrometer-thermometer system. But these devices are not always available at the bedside for every patient.
Different surrogate markers have been suggested to monitor humidification levels. • The most popular surrogates are secretion characteristics, visual observation of condensate in tubing system, and requirement for saline instillation. • Excessive humidification will increase secretion volume, and suboptimal humidification will lead to crusting, inspissation of secretions, and a decrease in their volume. • As a matter of fact, secretion volume may be altered by administered aerosolized medications, frequency of suctioning, and saline instillation.
Different surrogate markers have been suggested to monitor humidification levels. • Frequency of saline instillation has been proposed by some as a surrogate of gas humidity. • There was a significant correlation between the visual observation method and the hygroscopic measurements. • Despite the previously described data, there is still no clear consensus about a universal way to assess for humidity adequacy at the bedside
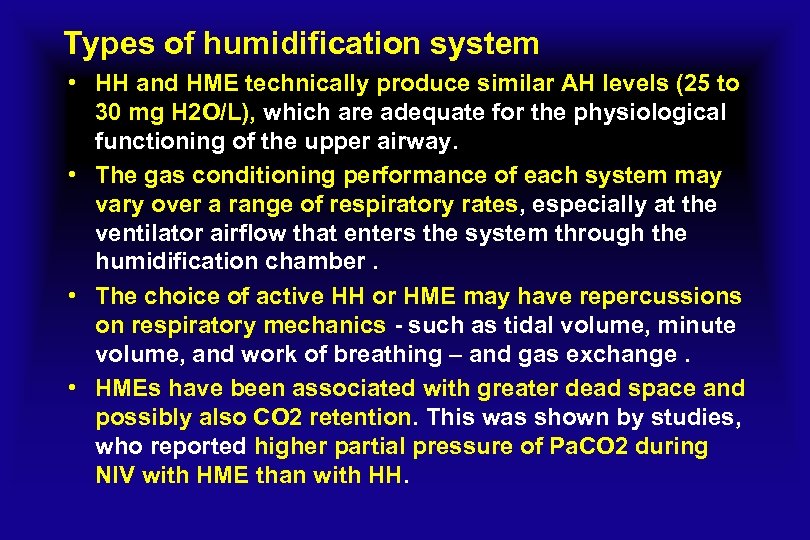
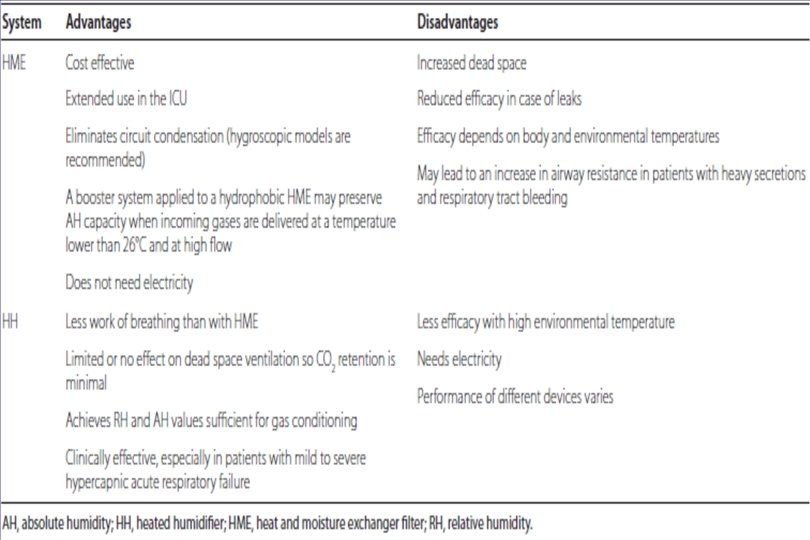
Types of humidification system • HH and HME technically produce similar AH levels (25 to 30 mg H 2 O/L), which are adequate for the physiological functioning of the upper airway. • The gas conditioning performance of each system may vary over a range of respiratory rates, especially at the ventilator airflow that enters the system through the humidification chamber. • The choice of active HH or HME may have repercussions on respiratory mechanics - such as tidal volume, minute volume, and work of breathing – and gas exchange. • HMEs have been associated with greater dead space and possibly also CO 2 retention. This was shown by studies, who reported higher partial pressure of Pa. CO 2 during NIV with HME than with HH.
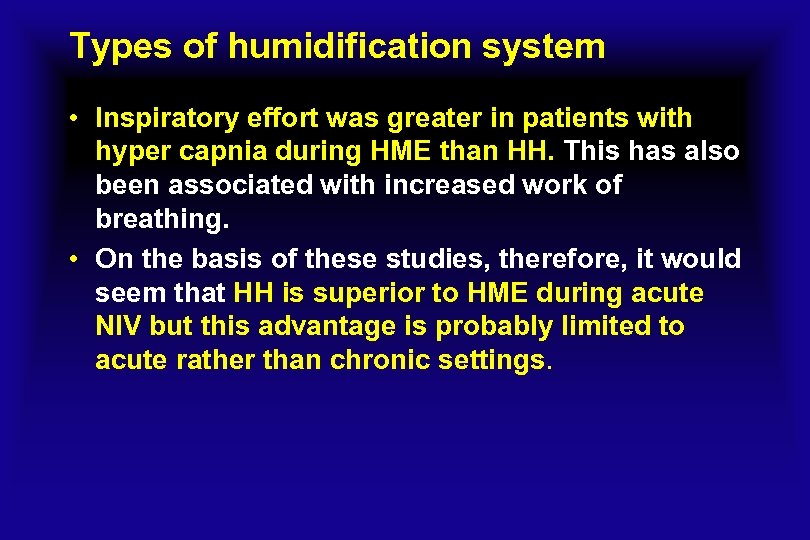
Types of humidification system • Inspiratory effort was greater in patients with hyper capnia during HME than HH. This has also been associated with increased work of breathing. • On the basis of these studies, therefore, it would seem that HH is superior to HME during acute NIV but this advantage is probably limited to acute rather than chronic settings.

Thermovent® T - Heat and Moisture Exchanger (HME) with 15 mm Female Connector. Humidifying Tracheostomy
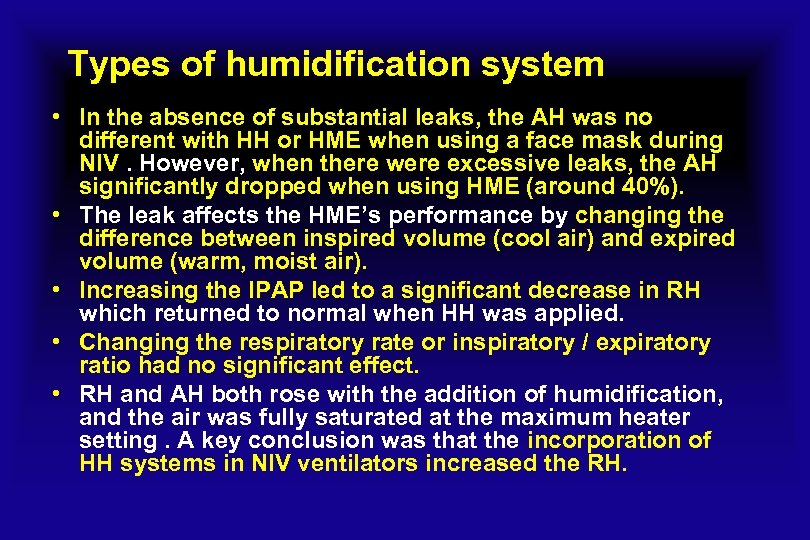
Types of humidification system • In the absence of substantial leaks, the AH was no different with HH or HME when using a face mask during NIV. However, when there were excessive leaks, the AH significantly dropped when using HME (around 40%). • The leak affects the HME’s performance by changing the difference between inspired volume (cool air) and expired volume (warm, moist air). • Increasing the IPAP led to a significant decrease in RH which returned to normal when HH was applied. • Changing the respiratory rate or inspiratory / expiratory ratio had no significant effect. • RH and AH both rose with the addition of humidification, and the air was fully saturated at the maximum heater setting. A key conclusion was that the incorporation of HH systems in NIV ventilators increased the RH.
Types of humidification system • By analyzing AH values in a series of patients with hypoxemic acute respiratory failure, with NIV administered by a turbine-driven ventilator and a face mask, in four different NIV environments: 1)without humidification; 2) with a HH-MR 850; 3) with a HH 730; 4) with a HME booster. The main findings were that the increase in inspired oxygen fraction led to a proportional decrease in AH and this effect was greater in an environment without humidification than during NIV delivered with HH and HMEbooster systems, and that AH levels were ‘critical’ when the inspired oxygen fraction was higher than 60%. AH was higher with a humidification system. • When HH and HME booster systems were compared, AH was higher with the latter; however, the HME booster caused more patient-ventilator asynchrony and hypercapnia.
Types of humidification system • The usual practice was to use HH more often than HME for acute NIV applications (53% versus 6. 6%). • Surprisingly, despite the importance of gas conditioning during NIV, there were relatively few hospital protocols referring to humidification practice in the participating centers (55%).
Selecting the Appropriate Humidifier • According to AARC guidelines , HHs should provide an absolute humidity level between 33 and 44 mg. H 2 O/L , whereas HMEs should provides minimum of 30 mg H 2 O/L. • Combined hydrophobic hygroscopic HMEs should be the first choice if passive humidification is selected, as they have better humidification capacity than the hydrophobic ones. • In terms of HME length of use, some concerns of decreased performance with their prolonged duration have been expressed. Hence, most manufacturers recommend exchanging HMEs every 24 hours.

Conclusion • Airway humidification represents a key intervention in mechanically ventilated patients. • Inappropriate humidifier settings or selection of devices may negatively impact clinical outcomes by damaging airway mucosa, prolonging mechanical ventilation, or increasing work of breathing. • Humidifier devices may function passively or actively, depending on the source of heat and humidity. • Depending on the clinical scenario, humidifier selection may change over time. Therefore , knowledge of the advantages and disadvantages of each of these devices is essential for respiratory care practitioners.
Conclusion • During NIV, adequate gas conditioning is essential because of the deleterious effects of inhalation of dry air , which may then negatively influence adherence to and the success of the ventilatory treatment. • Several parameters, mostly involving the technical aspects of NIV, are determinants of inefficient humidification. • The correct application of an appropriate humidification system may help prevent NIV-induced airway dryness. However , there are still open questions about when exactly to apply a humidifier in acute or chronic settings, the best type of humidification device in each situation, the interaction between the humidifier and the underlying disease and the effects of individual ventilators on delivered humidity.

e9796aa0c000da633d01e45f013c2de0.ppt