9e012fc767ef068f02fd07ed79fbe15d.ppt
- Количество слайдов: 42
GAIT DISTURBANCES AND FALLS IN OLDER ADULTS
OBJECTIVES Know and understand: • How to perform a diagnostic evaluation of gait dysfunction • How to conduct a gait assessment of the older adult • The importance of falls by older persons • How to assess and treat falls by an older person Slide 2
TOPICS COVERED • Gait Disorders • Gait Assessment • Epidemiology of Falls • Causes of Falls • Evaluation and Treatment of Falls • Clinical Guidelines for Preventing Falls Slide 3
GAIT IMPAIRMENT • Gait disorders are common and a predictor of functional decline • Certain gait-related mobility disorders progress with age and are associated with morbidity and mortality • Community-dwelling older adults with gait disorders, particularly neurologically abnormal gaits, are at higher risk of institutionalization and death Slide 4
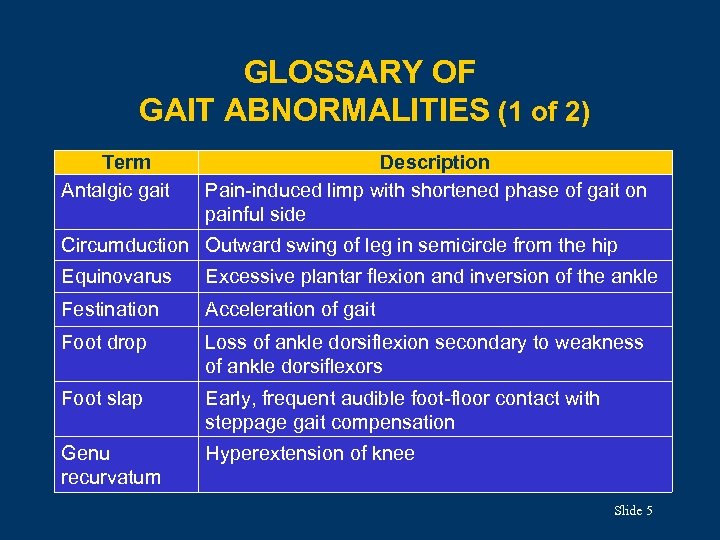
GLOSSARY OF GAIT ABNORMALITIES (1 of 2) Term Antalgic gait Description Pain-induced limp with shortened phase of gait on painful side Circumduction Outward swing of leg in semicircle from the hip Equinovarus Excessive plantar flexion and inversion of the ankle Festination Acceleration of gait Foot drop Loss of ankle dorsiflexion secondary to weakness of ankle dorsiflexors Foot slap Early, frequent audible foot-floor contact with steppage gait compensation Genu recurvatum Hyperextension of knee Slide 5
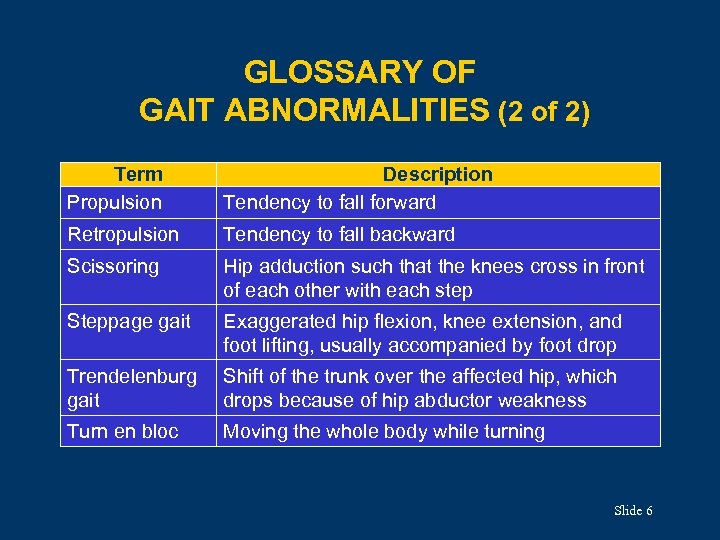
GLOSSARY OF GAIT ABNORMALITIES (2 of 2) Term Propulsion Description Tendency to fall forward Retropulsion Tendency to fall backward Scissoring Hip adduction such that the knees cross in front of each other with each step Steppage gait Exaggerated hip flexion, knee extension, and foot lifting, usually accompanied by foot drop Trendelenburg gait Shift of the trunk over the affected hip, which drops because of hip abductor weakness Turn en bloc Moving the whole body while turning Slide 6
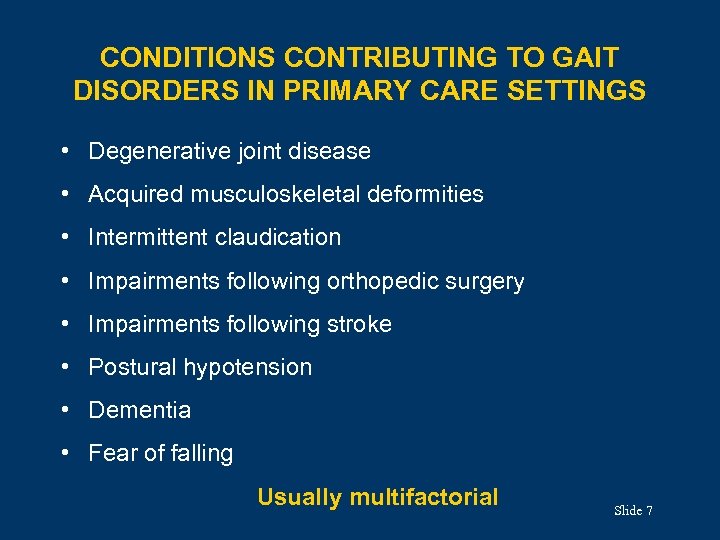
CONDITIONS CONTRIBUTING TO GAIT DISORDERS IN PRIMARY CARE SETTINGS • Degenerative joint disease • Acquired musculoskeletal deformities • Intermittent claudication • Impairments following orthopedic surgery • Impairments following stroke • Postural hypotension • Dementia • Fear of falling Usually multifactorial Slide 7
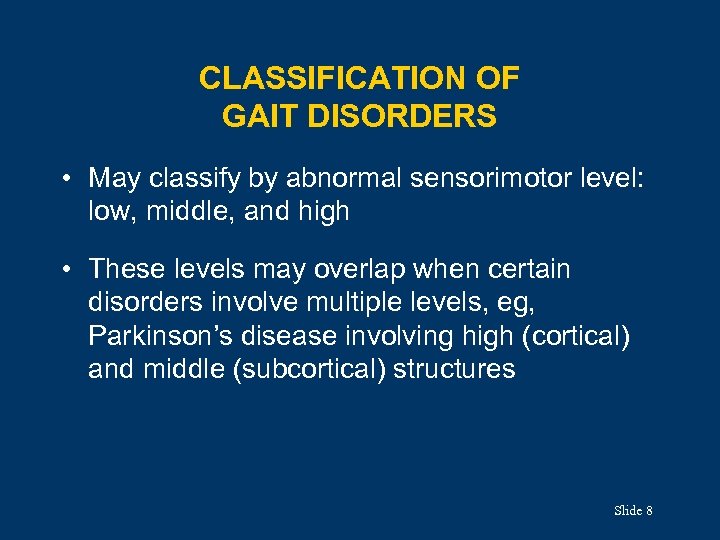
CLASSIFICATION OF GAIT DISORDERS • May classify by abnormal sensorimotor level: low, middle, and high • These levels may overlap when certain disorders involve multiple levels, eg, Parkinson’s disease involving high (cortical) and middle (subcortical) structures Slide 8
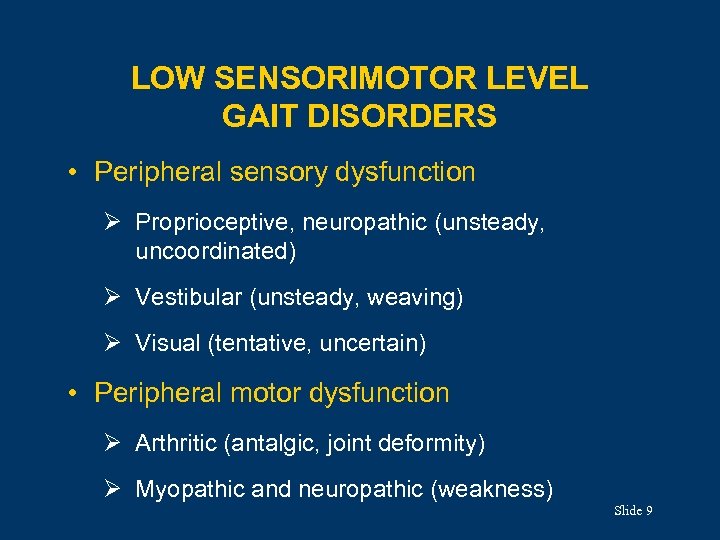
LOW SENSORIMOTOR LEVEL GAIT DISORDERS • Peripheral sensory dysfunction Ø Proprioceptive, neuropathic (unsteady, uncoordinated) Ø Vestibular (unsteady, weaving) Ø Visual (tentative, uncertain) • Peripheral motor dysfunction Ø Arthritic (antalgic, joint deformity) Ø Myopathic and neuropathic (weakness) Slide 9
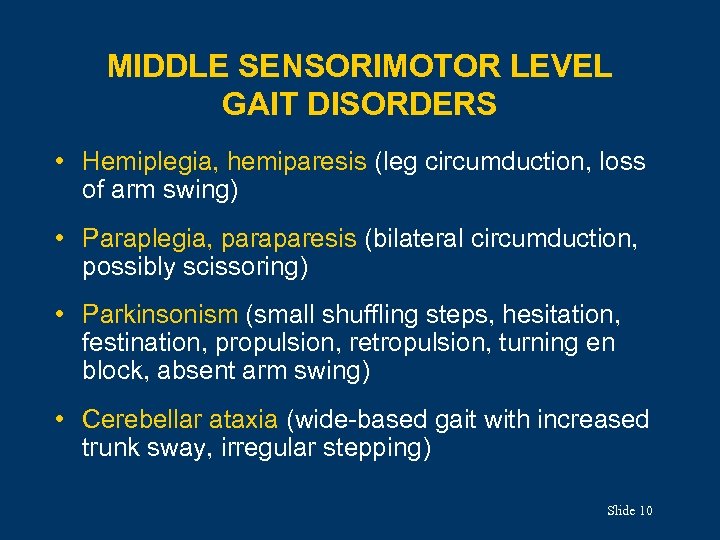
MIDDLE SENSORIMOTOR LEVEL GAIT DISORDERS • Hemiplegia, hemiparesis (leg circumduction, loss of arm swing) • Paraplegia, paraparesis (bilateral circumduction, possibly scissoring) • Parkinsonism (small shuffling steps, hesitation, festination, propulsion, retropulsion, turning en block, absent arm swing) • Cerebellar ataxia (wide-based gait with increased trunk sway, irregular stepping) Slide 10
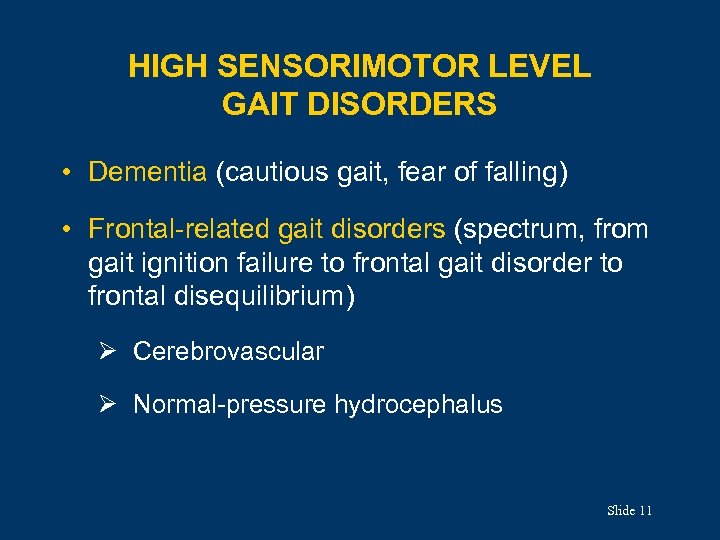
HIGH SENSORIMOTOR LEVEL GAIT DISORDERS • Dementia (cautious gait, fear of falling) • Frontal-related gait disorders (spectrum, from gait ignition failure to frontal gait disorder to frontal disequilibrium) Ø Cerebrovascular Ø Normal-pressure hydrocephalus Slide 11
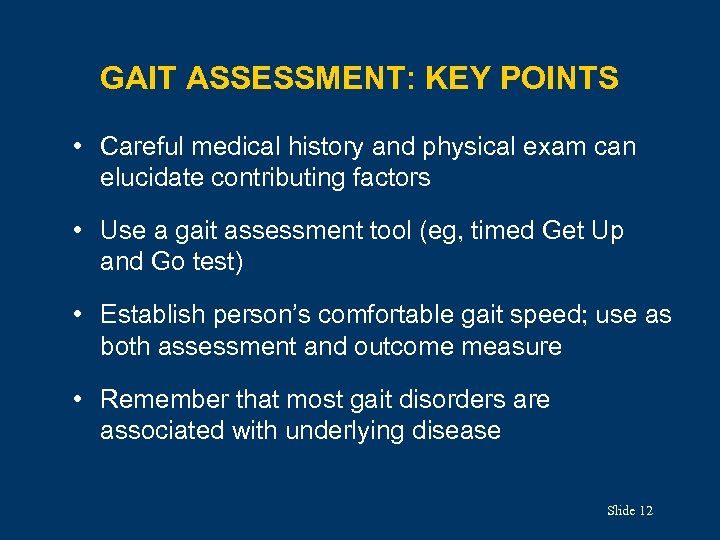
GAIT ASSESSMENT: KEY POINTS • Careful medical history and physical exam can elucidate contributing factors • Use a gait assessment tool (eg, timed Get Up and Go test) • Establish person’s comfortable gait speed; use as both assessment and outcome measure • Remember that most gait disorders are associated with underlying disease Slide 12
COMFORTABLE GAIT SPEED • Measure as part of a timed walk Ø For a short distance (eg, 10 feet) or Ø As a distance walked over time (eg, 6 min) • Predicts disease activity (eg, arthritis), cardiac and pulmonary function, mobility and ADL disability, institutionalization, and mortality Slide 13
THE TIMED GET UP AND GO TEST (1 of 2) Record the time it takes a person to: 1. Rise from a hard-backed chair with arms 2. Walk 10 feet (3 meters) 3. Turn 4. Return to the chair 5. Sit down Slide 14
THE TIMED GET UP AND GO TEST (2 of 2) • Most adults can complete in 10 sec • Most frail elderly adults can complete in 11 to 20 sec • ≥ 14 sec = falls risk • >20 sec comprehensive evaluation • Results are strongly associated with functional independence in ADLs Slide 15
FALLS Definition: coming to rest inadvertently on the ground or at a lower level • One of the most common geriatric syndromes • Most falls are not associated with syncope • Falls literature usually excludes falls associated with loss of consciousness Slide 16
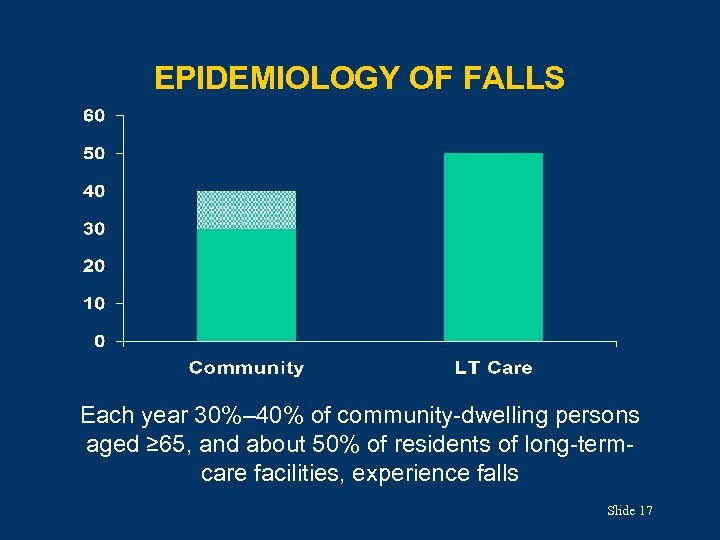
EPIDEMIOLOGY OF FALLS Each year 30%– 40% of community-dwelling persons aged ≥ 65, and about 50% of residents of long-termcare facilities, experience falls Slide 17
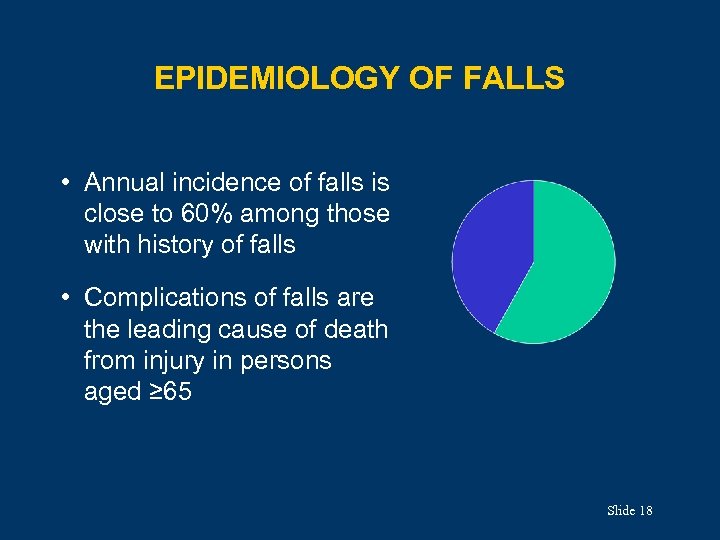
EPIDEMIOLOGY OF FALLS • Annual incidence of falls is close to 60% among those with history of falls • Complications of falls are the leading cause of death from injury in persons aged ≥ 65 Slide 18
MORBIDITY AND MORTALITY • Most falls by older adults result in some injury • 10%– 15% of falls by older adults result in fracture or other serious injury • The death rate attributable to falls increases with age • Mortality highest in white men aged ≥ 85: 180 deaths/100, 000 population Slide 19
SEQUELAE OF FALLS • Associated with: Ø Decline in functional status Ø Nursing home placement Ø Increased use of medical services Ø Fear of falling • Half of those who fall are unable to get up without help (“long lie”) • A “long lie” predicts lasting decline in functional status Slide 20

COSTS OF FALLS • Emergency department visits • Hospitalizations • Indirect cost from fall-related injuries like hip fractures is substantial Slide 21
CAUSES OF FALLS BY OLDER ADULTS • Rarely due to a single cause • May be due to the accumulated effect of impairments in multiple domains (such as other geriatric syndromes) • Complex interaction of: Ø Intrinsic factors (eg, chronic disease) Ø Challenges to postural control (eg, changing position) Ø Mediating factors (eg, risk taking, underlying mobility level) Slide 22
CAUSES: INTRINSIC • Age-related decline Ø Changes in visual function Ø Proprioceptive system, vestibular system • Chronic disease Ø Parkinson’s disease Ø Osteoarthritis Ø Cognitive impairment • Acute illness • Medication use (see next slide) Slide 23
CAUSES: MEDICATION USE • Specific classes, eg: Ø Ø Ø Benzodiazepines Antidepressants Antipsychotic drugs Cardiac medications Hypoglycemic agents • Recent medication dosage adjustments • Total number of medications Slide 24
FALLS ASSESSMENT (1 of 2) • Ask all older adults about falls in past year • Single fall: check for balance or gait disturbance • Recurrent falls or gait or balance disturbance: (1) Obtain relevant medical history, physical exam, cognitive and functional assessment Slide 25
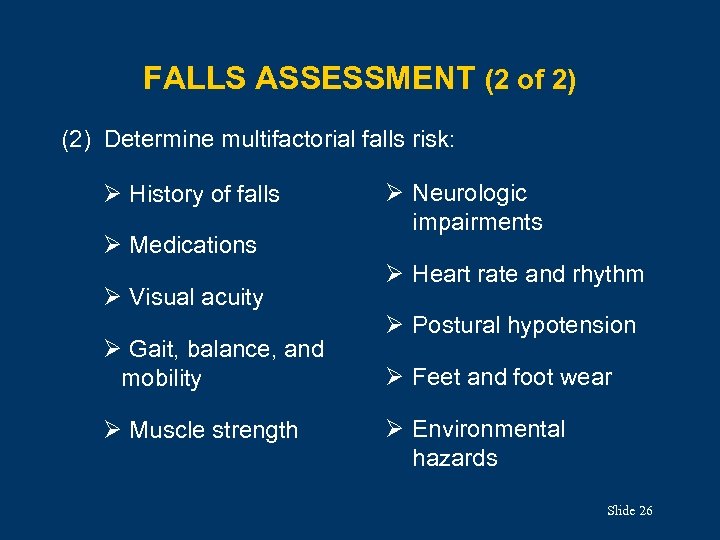
FALLS ASSESSMENT (2 of 2) (2) Determine multifactorial falls risk: Ø History of falls Ø Medications Ø Visual acuity Ø Gait, balance, and mobility Ø Muscle strength Ø Neurologic impairments Ø Heart rate and rhythm Ø Postural hypotension Ø Feet and foot wear Ø Environmental hazards Slide 26
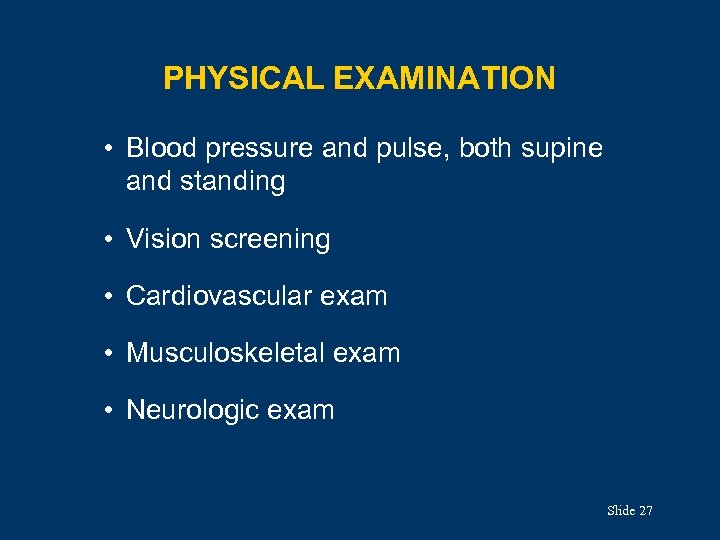
PHYSICAL EXAMINATION • Blood pressure and pulse, both supine and standing • Vision screening • Cardiovascular exam • Musculoskeletal exam • Neurologic exam Slide 27
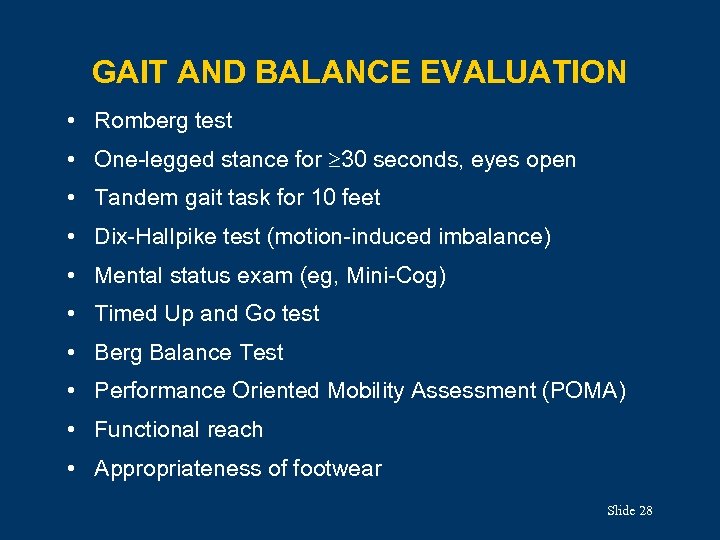
GAIT AND BALANCE EVALUATION • Romberg test • One-legged stance for 30 seconds, eyes open • Tandem gait task for 10 feet • Dix-Hallpike test (motion-induced imbalance) • Mental status exam (eg, Mini-Cog) • Timed Up and Go test • Berg Balance Test • Performance Oriented Mobility Assessment (POMA) • Functional reach • Appropriateness of footwear Slide 28
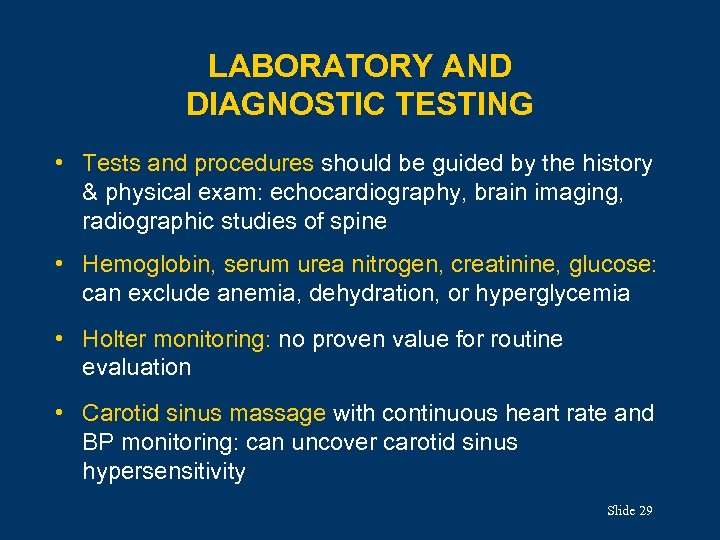
LABORATORY AND DIAGNOSTIC TESTING • Tests and procedures should be guided by the history & physical exam: echocardiography, brain imaging, radiographic studies of spine • Hemoglobin, serum urea nitrogen, creatinine, glucose: can exclude anemia, dehydration, or hyperglycemia • Holter monitoring: no proven value for routine evaluation • Carotid sinus massage with continuous heart rate and BP monitoring: can uncover carotid sinus hypersensitivity Slide 29
TREATMENT • Most favorable results with health screening followed by targeted interventions • Aim to reduce intrinsic and environmental risk factors • Interdisciplinary approach to falls prevention is most efficacious Slide 30
AGS FALLS PREVENTION GUIDELINES Recommendations include: • Assessment of all older adults • Assessment of anyone with history of falls • Multifactorial interventions including: Ø Ø Minimize medications Initiate individually tailored exercise program Treat vision impairment Manage postural hypotension, heart rate and rhythm abnormalities Ø Supplement vitamin D Ø Manage foot and footwear problems Ø Modify the house environment Slide 31
SUMMARY • Gait disorders are associated with many diseases and syndromes, including falls • Falls by older adults are common and usually multifactorial • Falls predict functional decline • Screening and targeted preventive interventions are most effective • AGS falls prevention guidelines are available and recommend multifactorial interventions Slide 32
CASE 1 (1 of 3) • An 88 -yr-old man comes to the office because he has been feeling more tired than usual, and yesterday he fell in his bedroom. • He was hospitalized with pneumonia 2 months ago; he received daily physical and occupational therapy in a nursing facility for 4 weeks and was then discharged home at maximal function. • He has a history of Parkinson’s disease, hypertension, and osteoarthritis. Medications include carbidopa/ levodopa, hydrochlorothiazide, metoprolol, and acetaminophen. Slide 33
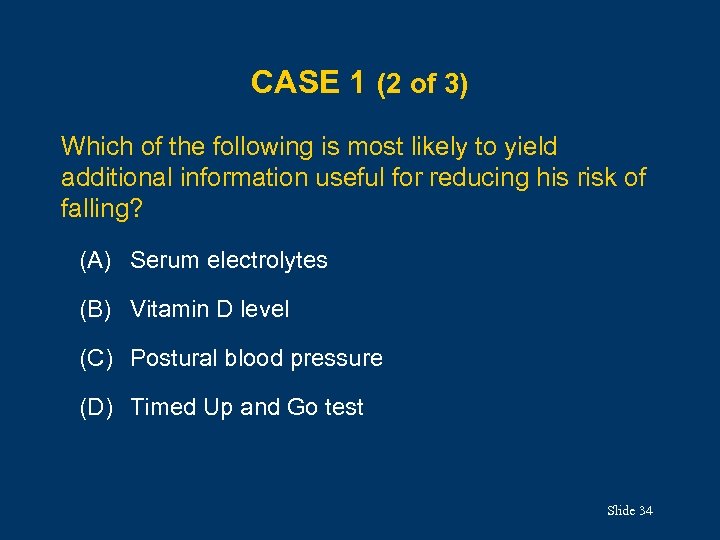
CASE 1 (2 of 3) Which of the following is most likely to yield additional information useful for reducing his risk of falling? (A) Serum electrolytes (B) Vitamin D level (C) Postural blood pressure (D) Timed Up and Go test Slide 34
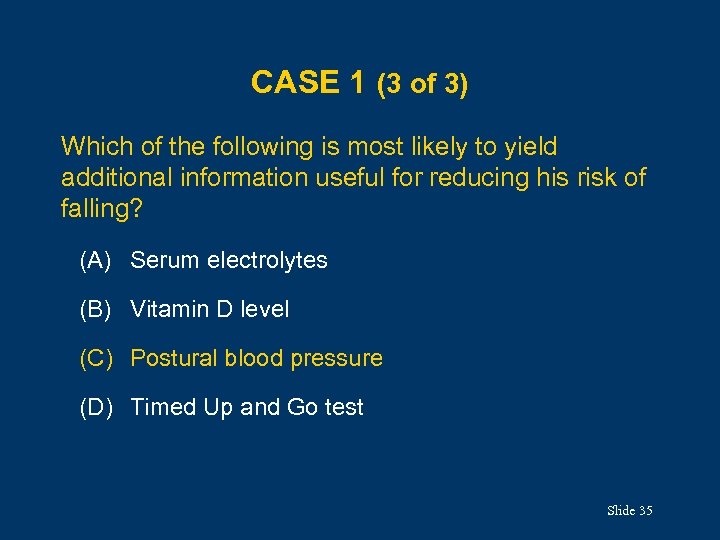
CASE 1 (3 of 3) Which of the following is most likely to yield additional information useful for reducing his risk of falling? (A) Serum electrolytes (B) Vitamin D level (C) Postural blood pressure (D) Timed Up and Go test Slide 35
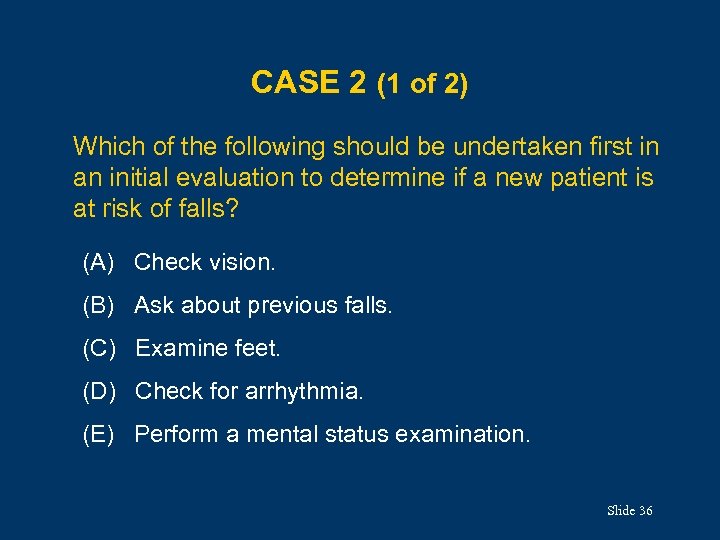
CASE 2 (1 of 2) Which of the following should be undertaken first in an initial evaluation to determine if a new patient is at risk of falls? (A) Check vision. (B) Ask about previous falls. (C) Examine feet. (D) Check for arrhythmia. (E) Perform a mental status examination. Slide 36
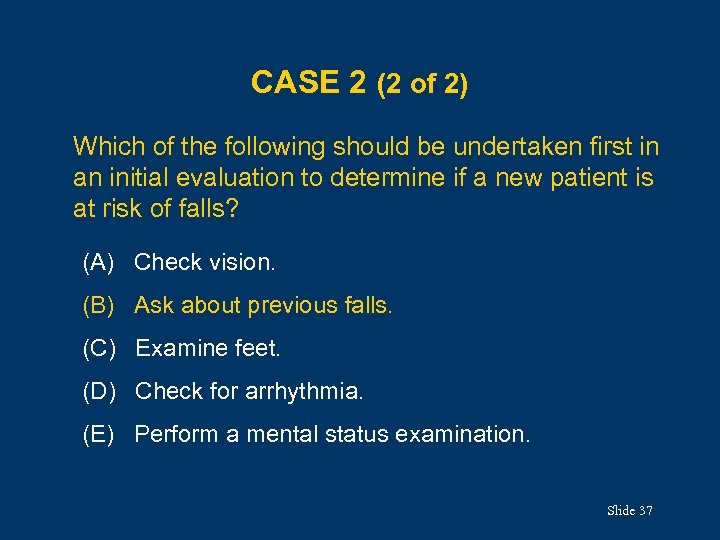
CASE 2 (2 of 2) Which of the following should be undertaken first in an initial evaluation to determine if a new patient is at risk of falls? (A) Check vision. (B) Ask about previous falls. (C) Examine feet. (D) Check for arrhythmia. (E) Perform a mental status examination. Slide 37
CASE 3 (1 of 4) • A 90 -year-old woman comes to the office because she has had increasing difficulty walking. Her gait is slower, and she feels as if she might fall backward at times. • She has hypertension, hypothyroidism, and osteoarthritis, and she had CABG 10 years ago, with no recurrence of angina. • She has moderate dorsal kyphosis and arthritic changes in her fingers and knees. Slide 38
CASE 3 (2 of 4) • Strength and reflexes are symmetric. The patient has some increased muscle tone. • She uses her arms to push up from the chair; once standing, she has difficulty starting to walk. • Her gait is symmetric, with a normal base, but her foot clearance and stride length are both decreased. • She turns slowly and carefully, with an increased number of steps. Slide 39
CASE 3 (3 of 4) Which of the following is the most likely cause of the patient’s gait abnormality? (A) Osteoarthritis (B) Proprioceptive deficits (C) Cerebrovascular disease (D) Parkinson’s disease (E) Cautious gait Slide 40
CASE 3 (4 of 4) Which of the following is the most likely cause of the patient’s gait abnormality? (A) Osteoarthritis (B) Proprioceptive deficits (C) Cerebrovascular disease (D) Parkinson’s disease (E) Cautious gait Slide 41
ACKNOWLEDGMENTS Editor: Annette Medina-Walpole, MD GRS 7 Chapter Authors: Neil B. Alexander, MD Sarah D. Berry, MD, MPH Douglas P. Kiel, MD, MPH GRS 7 Question Writer: Mary B. King, MD Pharmacotherapy Editor: Judith L. Beizer, Pharm. D Medical Writers: Beverly A. Caley Faith Reidenbach Managing Editor: Andrea N. Sherman, MS Copyright © 2010 American Geriatrics Society Slide 42
9e012fc767ef068f02fd07ed79fbe15d.ppt