c1cde53f57686a07bdfe12c0ec798871.ppt
- Количество слайдов: 59
G lobal INitiative for A sthma
GINA Workshop Report Topics: Definition Burden of Asthma Risk Factors Mechanisms Diagnosis and Classification Education and Delivery of Care Six Part Asthma Management Plan Research Recommendations
Definition of Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role Chronic inflammation causes an associated increase in airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment

Mechanisms Underlying the Definition of Asthma Risk Factors (for development of asthma) INFLAMMATION Airway Hyperresponsiveness Risk Factors (for exacerbations) Airflow Obstruction Symptoms
Burden of Asthma is one of the most common chronic diseases worldwide Prevalence increasing in many countries, especially in children A major cause of school/work absence An overall increase in severity of asthma increases the pool of patients at risk for death
Burden of Asthma Health care expenditures very high Developed economies might expect to spend 1 -2 percent of total health care expenditures on asthma. Developing economies likely to face increased demand Poorly controlled asthma is expensive; investment in prevention medication likely to yield cost savings in emergency care
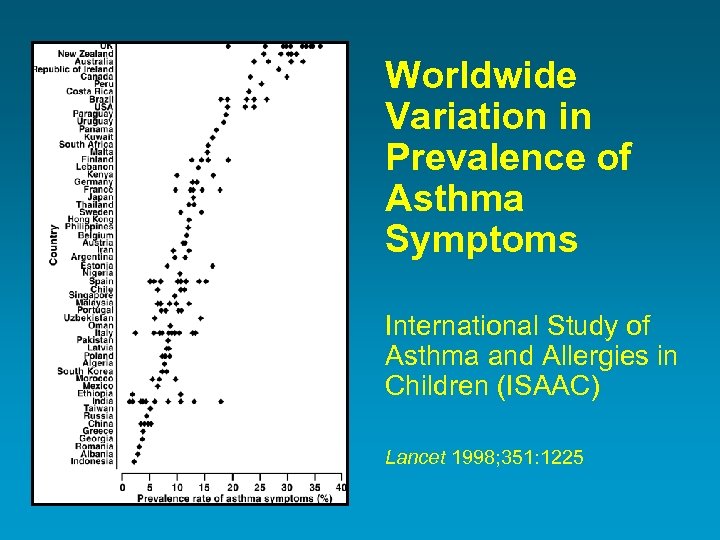
Worldwide Variation in Prevalence of Asthma Symptoms International Study of Asthma and Allergies in Children (ISAAC) Lancet 1998; 351: 1225
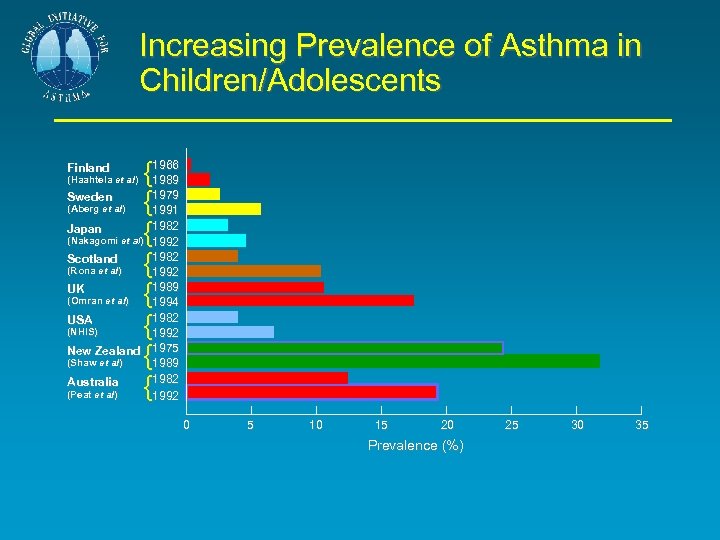
Increasing Prevalence of Asthma in Children/Adolescents {1966 1989 Sweden {1979 1991 Japan {1982 1992 Scotland {1982 1992 UK {1989 1994 USA {1982 1992 New Zealand 1975 {1989 Australia {1982 1992 Finland (Haahtela et al) (Aberg et al) (Nakagomi et al) (Rona et al) (Omran et al) (NHIS) (Shaw et al) (Peat et al) 0 5 10 15 20 Prevalence (%) 25 30 35
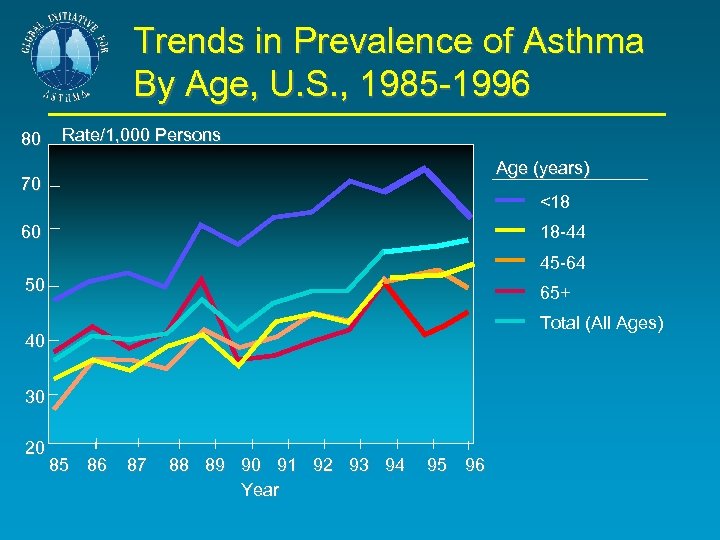
Trends in Prevalence of Asthma By Age, U. S. , 1985 -1996 80 Rate/1, 000 Persons Age (years) 70 <18 60 18 -44 45 -64 50 65+ Total (All Ages) 40 30 20 85 86 87 88 89 90 91 92 93 94 Year 95 96
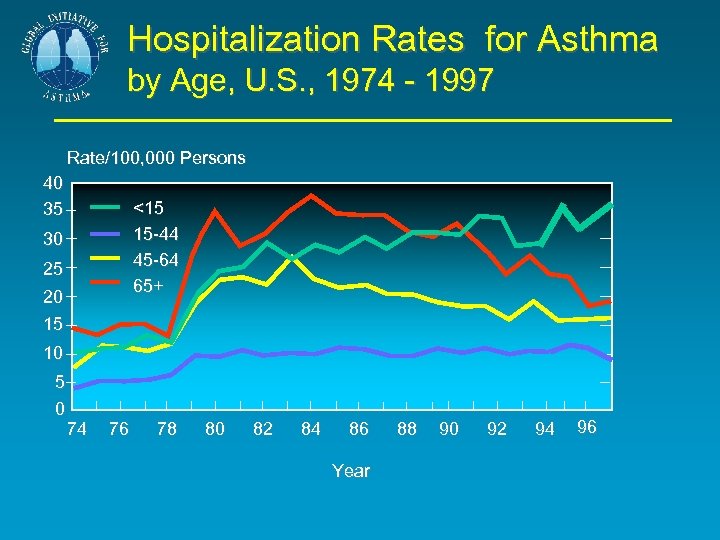
Hospitalization Rates for Asthma by Age, U. S. , 1974 - 1997 Rate/100, 000 Persons 40 35 <15 15 -44 45 -64 65+ 30 25 20 15 10 5 0 74 76 78 80 82 84 86 Year 88 90 92 94 96
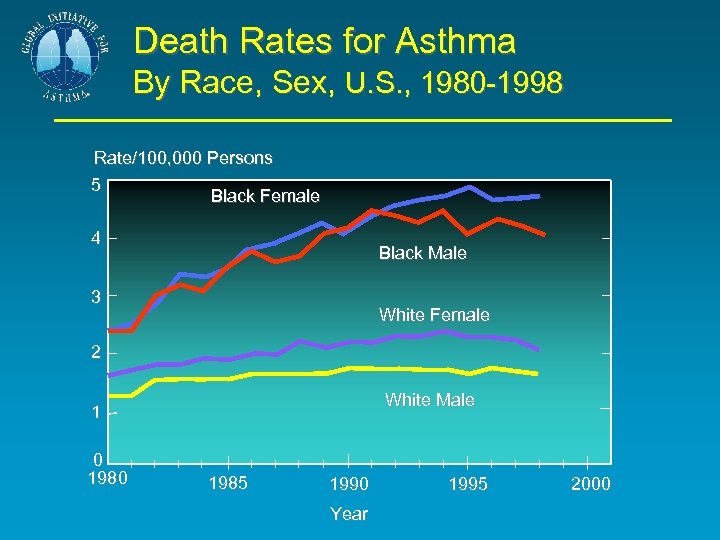
Death Rates for Asthma By Race, Sex, U. S. , 1980 -1998 Rate/100, 000 Persons 5 Black Female 4 Black Male 3 White Female 2 White Male 1 0 1985 1990 Year 1995 2000
Risk Factors for Asthma Host factors: predispose individuals to, or protect them from, developing asthma Environmental factors: influence susceptibility to development of asthma in predisposed individuals, precipitate asthma exacerbations, and/or cause symptoms to persist

Factors that Exacerbate Asthma Allergens Air Pollutants Respiratory infections Exercise and hyperventilation Weather changes Sulfur dioxide Food, additives, drugs
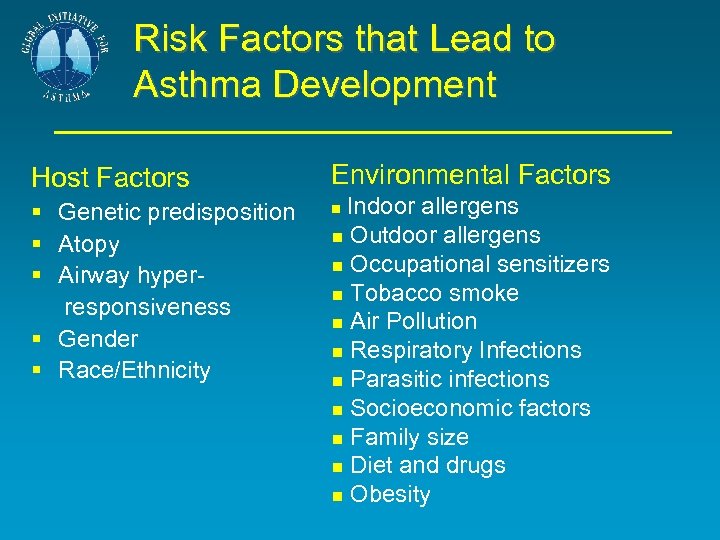
Risk Factors that Lead to Asthma Development Host Factors Environmental Factors § Genetic predisposition § Atopy § Airway hyperresponsiveness § Gender § Race/Ethnicity Indoor allergens Outdoor allergens Occupational sensitizers Tobacco smoke Air Pollution Respiratory Infections Parasitic infections Socioeconomic factors Family size Diet and drugs Obesity

Is it Asthma? Recurrent episodes of wheezing Troublesome cough at night Cough or wheeze after exercise Cough, wheeze or chest tightness after exposure to airborne allergens or pollutants Colds “go to the chest” or take more than 10 days to clear
Asthma Diagnosis History and patterns of symptoms Physical examination Measurements of lung function Measurements of allergic status to identify risk factors
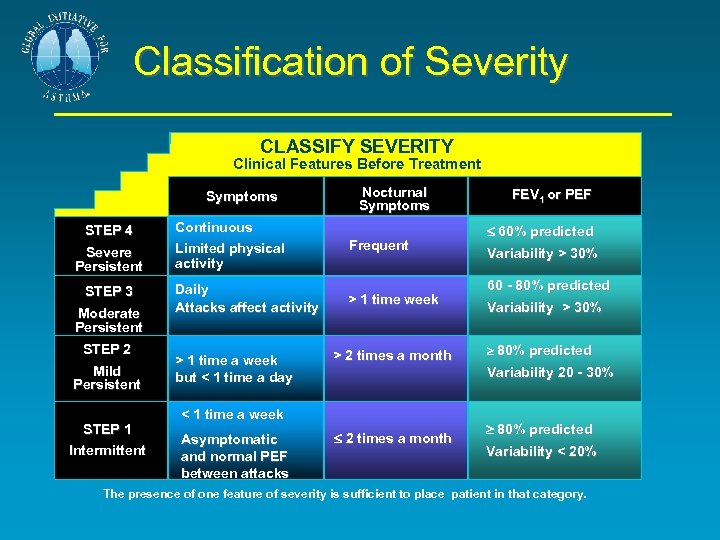
Classification of Severity CLASSIFY SEVERITY Clinical Features Before Treatment Symptoms STEP 4 Severe Persistent STEP 3 Moderate Persistent STEP 2 Mild Persistent STEP 1 Intermittent Continuous Limited physical activity Daily Attacks affect activity > 1 time a week but < 1 time a day Nocturnal Symptoms Frequent > 1 time week > 2 times a month 60% predicted Variability > 30% 60 - 80% predicted Variability > 30% 80% predicted Variability 20 - 30% < 1 time a week Asymptomatic and normal PEF between attacks FEV 1 or PEF 2 times a month 80% predicted Variability < 20% The presence of one feature of severity is sufficient to place patient in that category.

Six-Part Asthma Management Program 1. Educate Patients 2. Assess and Monitor Severity 3. Avoid Exposure to Risk Factors 4. Establish Medication Plans for Chronic Management: Adults and Children 5. Establish Plans for Managing Exacerbations 6. Provide Regular Follow-up Care

Six-Part Asthma Management Program 1. Educate patients to develop a partnership in asthma management 2. Assess and monitor asthma severity with symptom reports and measures of lung function as much as possible 3. Avoid exposure to risk factors 4. Establish medication plans for chronic management in children and adults 5. Establish individual plans for managing exacerbations 6. Provide regular follow-up care
Six-part Asthma Management Program Goals of Long-term Management Achieve and maintain control of symptoms Prevent asthma episodes or attacks Maintain pulmonary function as close to normal levels as possible Maintain normal activity levels, including exercise Avoid adverse effects from asthma medications Prevent development of irreversible airflow limitation Prevent asthma mortality
Six-part Asthma Management Program Control of Asthma Minimal (ideally no) chronic symptoms Minimal (infrequent) exacerbations No emergency visits Minimal (ideally no) need for “as needed” use of β 2 -agonist No limitations on activities, including exercise PEF circadian variation of less than 20 percent (Near) normal PEF Minimal (or no) adverse effects from medicine

Six-Part Asthma Management Program . The most effective management is to prevent airway inflammation by eliminating the causal factors Asthma can be effectively controlled in most patients, although it can not be cured The major factors contributing to asthma morbidity and mortality are underdiagnosis and inappropriate treatment
Six-Part Asthma Management Program Any asthma more severe than intermittent asthma is more effectively controlled by treatment to suppress and reverse airway inflammation than by treatment only of acute bronchoconstriction and symptoms
Six-part Asthma Management Program Part 1: Educate Patients to Develop a Partnership § Aim is guided self-management – giving patients the ability to control their asthma § Interventions, including use of written action plans, have been shown to reduce morbidity in both children and adults
Six-part Asthma Management Program Part 1: Educate Patients to Develop a Partnership Educate continually Include the family Provide information about asthma Provide training on self-management skills Emphasize a partnership among health care providers, the patient, and the patient’s family
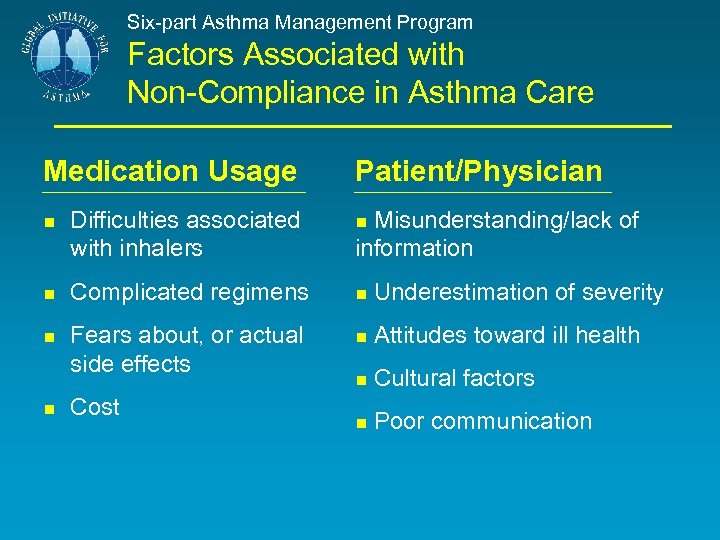
Six-part Asthma Management Program Factors Associated with Non-Compliance in Asthma Care Medication Usage Patient/Physician Misunderstanding/lack of information Difficulties associated with inhalers Complicated regimens Underestimation of severity Fears about, or actual side effects Attitudes toward ill health Cultural factors Poor communication Cost

Six-part Asthma Management Program Part 2: Assess and Monitor Asthma Severity with Symptom Reports and Measures of Lung Function Symptom reports Use of reliever medication Nighttime symptoms Activity limitations Spirometry follow-up: Assess severity Assess response to therapy PEF for initial assessment. Peak Expiratory Flow for monitoring at home Important for those with poor perception of symptoms Daily measurement recorded in a diary Assesses the severity and predicts worsening Guides the use of a zone system for asthma self-management Arterial blood gas for severe exacerbations
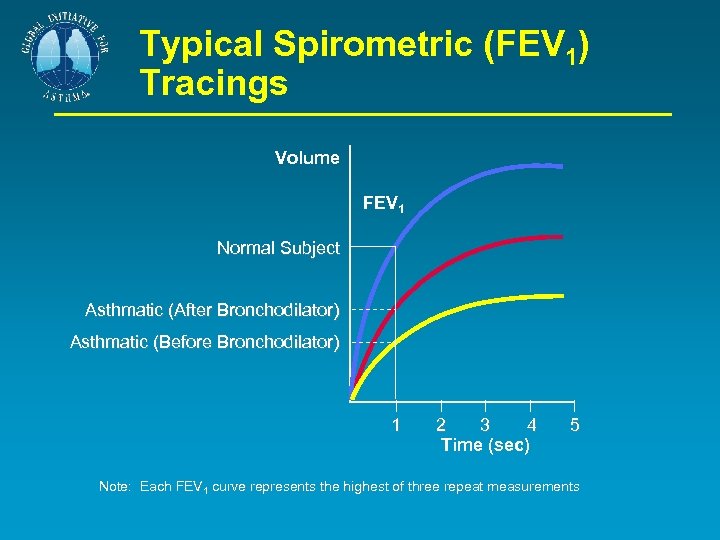
Typical Spirometric (FEV 1) Tracings Volume FEV 1 Normal Subject Asthmatic (After Bronchodilator) Asthmatic (Before Bronchodilator) 1 2 3 4 Time (sec) 5 Note: Each FEV 1 curve represents the highest of three repeat measurements

A Simple Index of PEF Variation
Six-part Asthma Management Program Part 3: Avoid Exposure to Risk Factors § Methods to prevent onset of asthma are not yet available but this remains an important goal § Measures to reduce exposure to causes of asthma exacerbations (e. g. allergens, pollutants, foods and medications) should be implemented whenever possible
Six-part Asthma Management Program Part 3: Avoid Exposure to Risk Factors Reduce exposure to indoor allergens Avoid tobacco smoke Avoid vehicle emission Identify irritants in the workplace Explore role of infections on asthma development, especially in children and young infants
Six-part Asthma Management Program Part 4: Establish Medication Plans for Long-Term Asthma Management A stepwise approach to pharmacological therapy is recommended The aim is to accomplish the goals of therapy with the least possible medication Although in many countries traditional methods of healing are used, their efficacy has not yet been established and their use can therefore not be recommended
Part 4: Long-term Asthma Management Stepwise Approach to Asthma Therapy The choice of treatment should be guided by: Severity of the patient’s asthma Patient’s current treatment Pharmacological properties and availability of the various forms of asthma treatment Economic considerations Cultural preferences and differing health care systems need to be considered.

Part 4: Long-term Asthma Management Pharmacologic Therapy Controller Medications: Inhaled glucocorticosteroids Systemic glucocorticosteroids Cromones Methylxanthines Long-acting inhaled β 2 -agonists Long-acting oral β 2 -agonists Leukotriene modifiers Anti-Ig. E
Part 4: Long-term Asthma Management Pharmacologic Therapy Reliever Medications: Rapid-acting inhaled β 2 -agonists Systemic glucocorticosteroids Anticholinergics Methylxanthines Short-acting oral β 2 -agonists
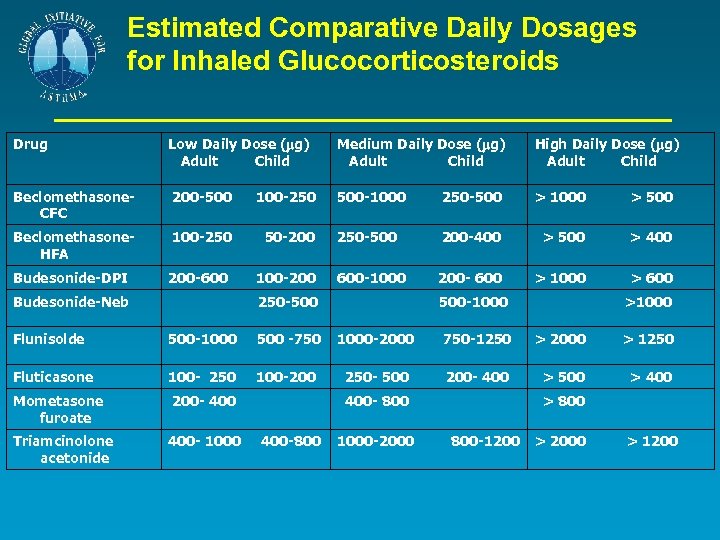
Estimated Comparative Daily Dosages for Inhaled Glucocorticosteroids Drug Low Daily Dose ( g) Adult Child Medium Daily Dose ( g) Adult Child High Daily Dose ( g) Adult Child Beclomethasone. CFC 200 -500 100 -250 500 -1000 250 -500 > 1000 > 500 Beclomethasone. HFA 100 -250 50 -200 250 -500 200 -400 > 500 > 400 Budesonide-DPI 200 -600 100 -200 600 -1000 200 - 600 > 1000 > 600 Budesonide-Neb 250 -500 500 -1000 >1000 Flunisolde 500 -1000 500 -750 1000 -2000 750 -1250 > 2000 > 1250 Fluticasone 100 - 250 100 -200 250 - 500 200 - 400 > 500 > 400 Mometasone furoate 200 - 400 Triamcinolone acetonide 400 - 1000 400 - 800 400 -800 1000 -2000 > 800 -1200 > 2000 > 1200
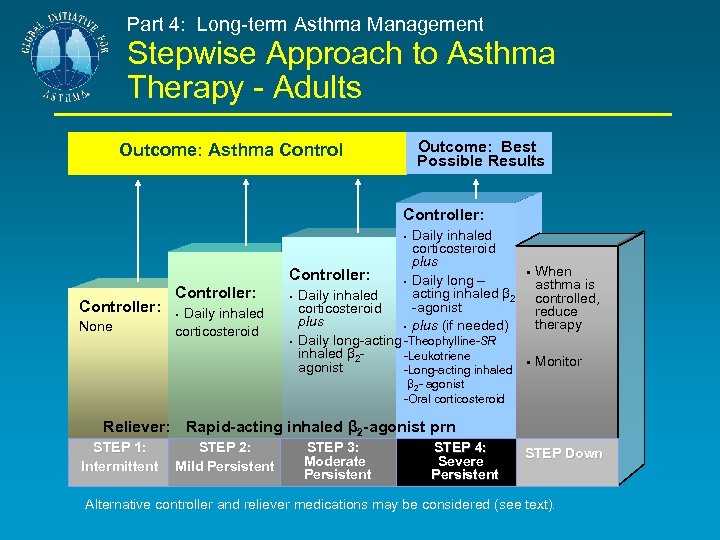
Part 4: Long-term Asthma Management Stepwise Approach to Asthma Therapy - Adults Outcome: Best Possible Results Outcome: Asthma Controller: § Controller: None Controller: Daily inhaled corticosteroid § § Daily inhaled corticosteroid plus Daily long – acting inhaled β 2 -agonist plus (if needed) Daily inhaled corticosteroid plus § Daily long-acting -Theophylline-SR inhaled β 2 -Leukotriene agonist -Long-acting inhaled § § When asthma is controlled, reduce therapy Monitor β 2 - agonist -Oral corticosteroid Reliever: Rapid-acting inhaled β 2 -agonist prn STEP 1: Intermittent STEP 2: Mild Persistent STEP 3: Moderate Persistent STEP 4: Severe Persistent STEP Down Alternative controller and reliever medications may be considered (see text).
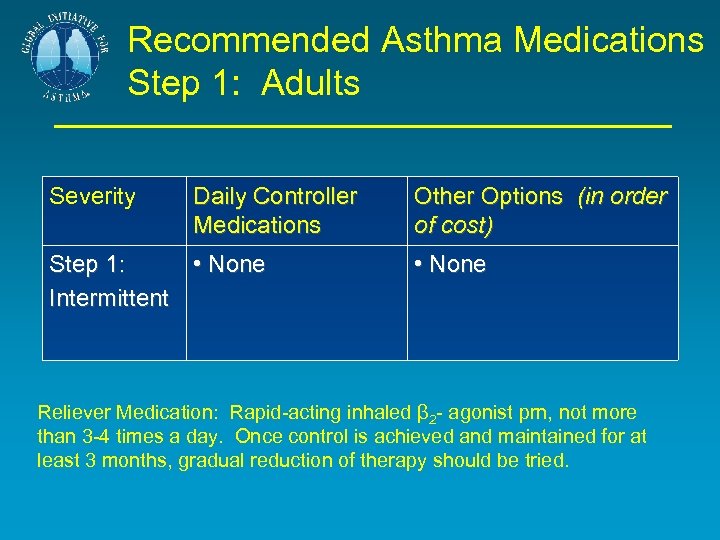
Recommended Asthma Medications Step 1: Adults Severity Daily Controller Medications Step 1: • None Intermittent Other Options (in order of cost) • None Reliever Medication: Rapid-acting inhaled β 2 - agonist prn, not more than 3 -4 times a day. Once control is achieved and maintained for at least 3 months, gradual reduction of therapy should be tried.
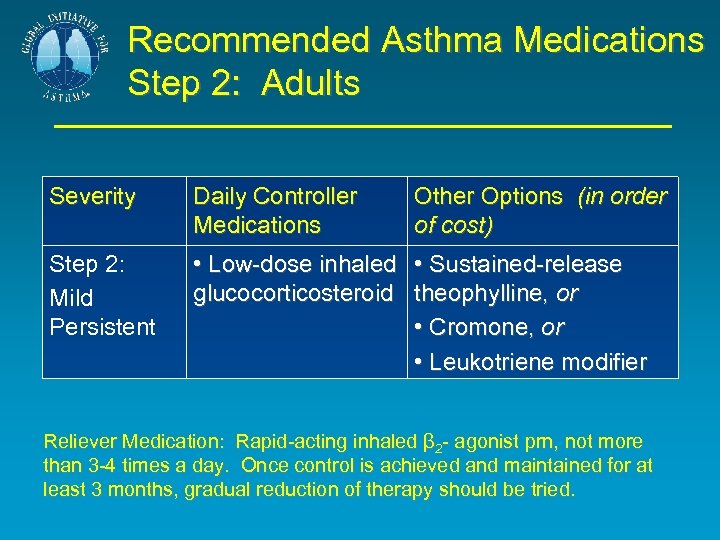
Recommended Asthma Medications Step 2: Adults Severity Daily Controller Medications Other Options (in order of cost) Step 2: Mild Persistent • Low-dose inhaled • Sustained-release glucocorticosteroid theophylline, or • Cromone, or • Leukotriene modifier Reliever Medication: Rapid-acting inhaled β 2 - agonist prn, not more than 3 -4 times a day. Once control is achieved and maintained for at least 3 months, gradual reduction of therapy should be tried.
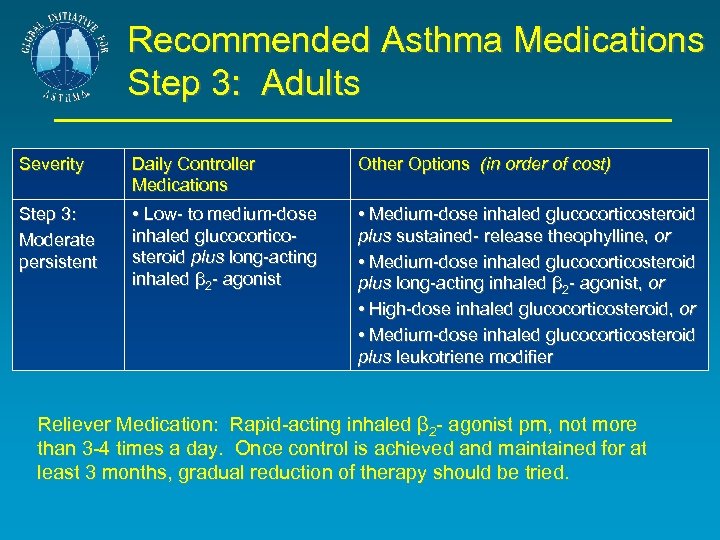
Recommended Asthma Medications Step 3: Adults Severity Daily Controller Medications Other Options (in order of cost) Step 3: Moderate persistent • Low- to medium-dose inhaled glucocorticosteroid plus long-acting inhaled β 2 - agonist • Medium-dose inhaled glucocorticosteroid plus sustained- release theophylline, or • Medium-dose inhaled glucocorticosteroid plus long-acting inhaled β 2 - agonist, or • High-dose inhaled glucocorticosteroid, or • Medium-dose inhaled glucocorticosteroid plus leukotriene modifier Reliever Medication: Rapid-acting inhaled β 2 - agonist prn, not more than 3 -4 times a day. Once control is achieved and maintained for at least 3 months, gradual reduction of therapy should be tried.
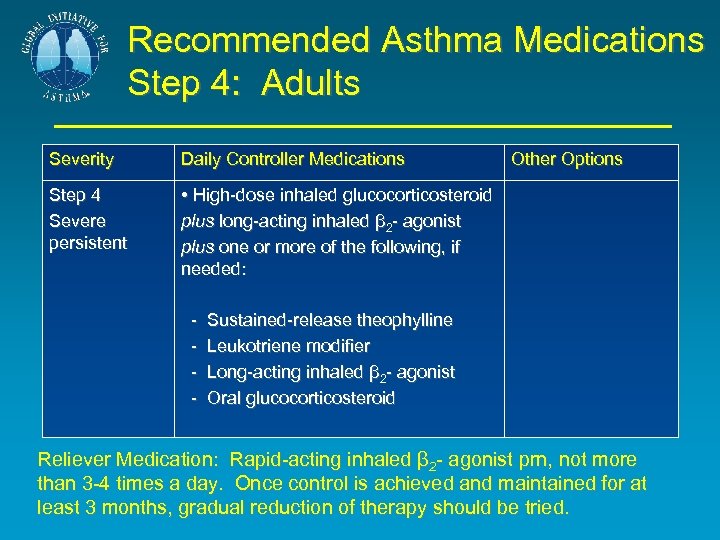
Recommended Asthma Medications Step 4: Adults Severity Daily Controller Medications Step 4 Severe persistent • High-dose inhaled glucocorticosteroid plus long-acting inhaled β 2 - agonist plus one or more of the following, if needed: - Other Options Sustained-release theophylline Leukotriene modifier Long-acting inhaled β 2 - agonist Oral glucocorticosteroid Reliever Medication: Rapid-acting inhaled β 2 - agonist prn, not more than 3 -4 times a day. Once control is achieved and maintained for at least 3 months, gradual reduction of therapy should be tried.
Six-part Asthma Management Program Part 4: Establish Medication Plans for Long-Term Asthma Management in Infants and Children § Childhood and adult asthma share the same underlying mechanisms. However, because of processes of growth and development, effects of asthma treatments in children differ from those in adults.

Six-part Asthma Management Program Part 4: Establish Medication Plans for Long-Term Asthma Management in Infants and Children § Many asthma medications (e. g. glucocorticosteroids, β 2 - agonists, theophylline) are metabolized faster in children than in adults, and younger children tend to metabolize medications faster than older children
Six-part Asthma Management Program Part 4: Establish Medication Plans for Long-Term Asthma Management in Infants and Children § Long-term treatment with inhaled glucocorticosteroids has not been shown to be associated with any increase in osteoporosis or bone fracture § Studies including a total of over 3, 500 children treated for periods of 1 – 13 years have found no sustained adverse effect of inhaled glucocorticosteroids on growth
Six-part Asthma Management Program Part 4: Establish Medication Plans for Long-Term Asthma Management in Infants and Children § Rapid-acting inhaled β 2 - agonists are the most effective reliever therapy for children § These medications are the most effective bronchodilators available and are the treatment of choice for acute asthma symptoms
Six-part Asthma Management Program Part 5: Establish Plans for Managing Exacerbations Treatment of exacerbations depends on: § The patient § Experience of the health care professional § Therapies that are the most effective for the particular patient § Availability of medications § Emergency facilities
Six-part Asthma Management Program Part 5: Establish Plans for Managing Exacerbations Primary therapies for exacerbations: • Repetitive administration of rapid-acting inhaled β 2 -agonist • Early introduction of systemic glucocorticosteroids • Oxygen supplementation Closely monitor response to treatment with serial measures of lung function
Six-part Asthma Management Program Part 5: Managing Severe Asthma Exacerbations § Severe exacerbations are lifethreatening medical emergencies § Care must be expeditious and treatment is often most safely undertaken in a hospital or hospital-based emergency department
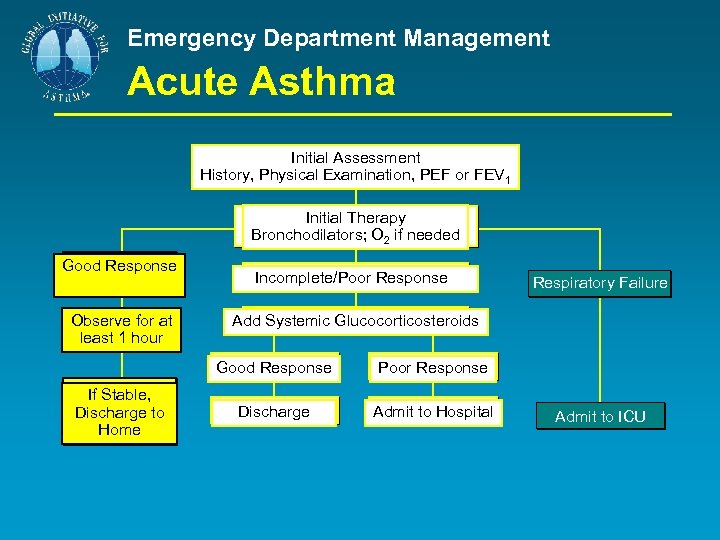
Emergency Department Management Acute Asthma Initial Assessment History, Physical Examination, PEF or FEV 1 Initial Therapy Bronchodilators; O 2 if needed Good Response Observe for at least 1 hour Incomplete/Poor Response Add Systemic Glucocorticosteroids Good Response If Stable, Discharge to Home Respiratory Failure Poor Response Discharge Admit to Hospital Admit to ICU
Six-part Asthma Management Program Part 6: Provide Regular Follow-up Care Continual monitoring is essential to assure that therapeutic goals are met. Frequent follow-up visits are necessary to review: § Home PEF and symptom records § Techniques in use of medications § Risk factors and their control Once asthma control is established, follow-up visits should be scheduled (at 1 to 6 month intervals as appropriate)
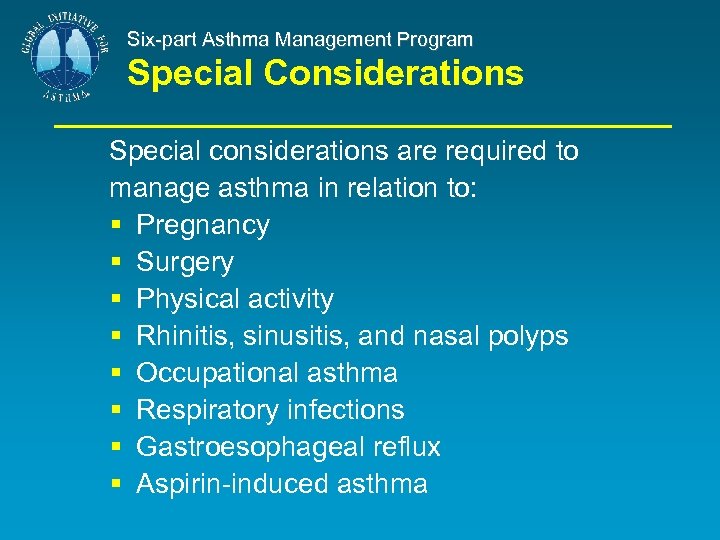
Six-part Asthma Management Program Special Considerations Special considerations are required to manage asthma in relation to: § Pregnancy § Surgery § Physical activity § Rhinitis, sinusitis, and nasal polyps § Occupational asthma § Respiratory infections § Gastroesophageal reflux § Aspirin-induced asthma
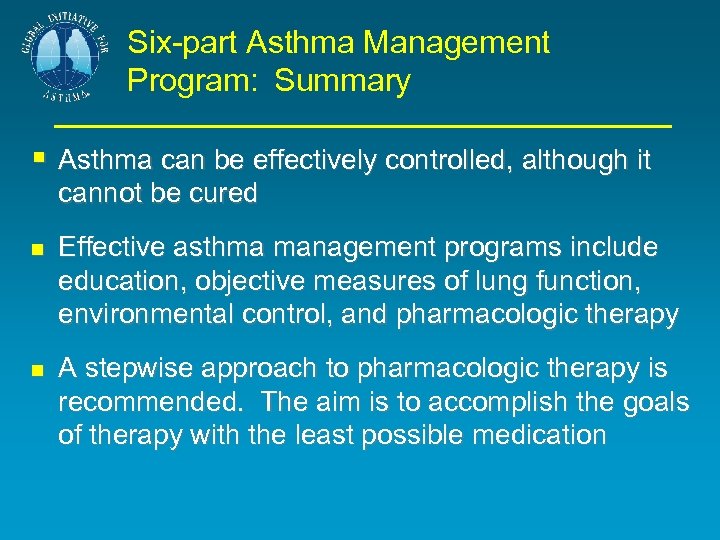
Six-part Asthma Management Program: Summary § Asthma can be effectively controlled, although it cannot be cured Effective asthma management programs include education, objective measures of lung function, environmental control, and pharmacologic therapy A stepwise approach to pharmacologic therapy is recommended. The aim is to accomplish the goals of therapy with the least possible medication

Six-part Asthma Management Program: Summary (continued) Anything more than mild, occasional asthma is more effectively controlled by suppressing inflammation than by only treating acute bronchospasm The availability of varying forms of treatment, cultural preferences, and differing health care systems need to be considered

http: //www. ginasthma. com

Part 4: Long-term Asthma Management Stepwise Approach to Asthma Therapy - Adults Outcome: Best Possible Results Outcome: Asthma Controller: § Controller: None Controller: Daily inhaled corticosteroid § § Daily inhaled corticosteroid Daily long – acting inhaled β 2 -agonist plus(if needed) Daily inhaled corticosteroid § Daily long-acting inhaled β 2 -Theophylline-SR agonist -Leukotriene -Long-acting inhaled β 2 - agonist -Oral corticosteroid § § When asthma is controlled, reduce therapy Monitor Reliever: Rapid-acting inhaled β 2 -agonist prn STEP 1: Intermittent STEP 2: Mild Persistent STEP 3: Moderate Persistent STEP 4: Severe Persistent STEP Down Alternative controller and reliever medications may be considered (see text).
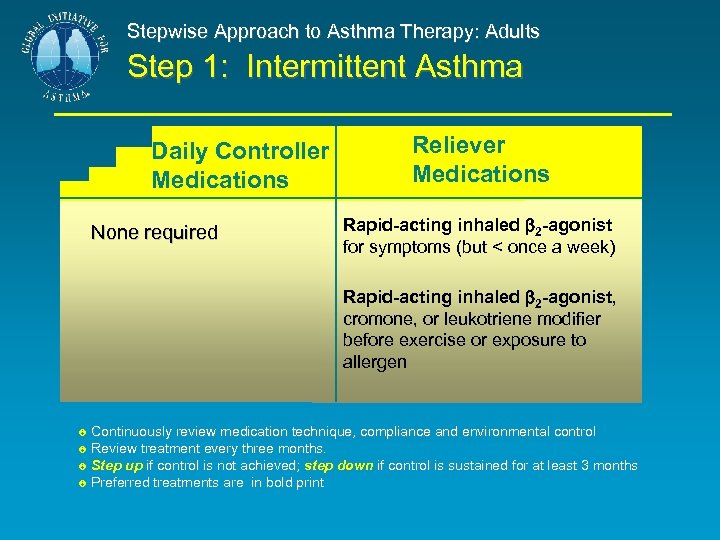
Stepwise Approach to Asthma Therapy: Adults Step 1: Intermittent Asthma Daily Controller Medications None required Reliever Medications Rapid-acting inhaled 2 -agonist for symptoms (but < once a week) Rapid-acting inhaled 2 -agonist, cromone, or leukotriene modifier before exercise or exposure to allergen Continuously review medication technique, compliance and environmental control Review treatment every three months. Step up if control is not achieved; step down if control is sustained for at least 3 months Preferred treatments are in bold print
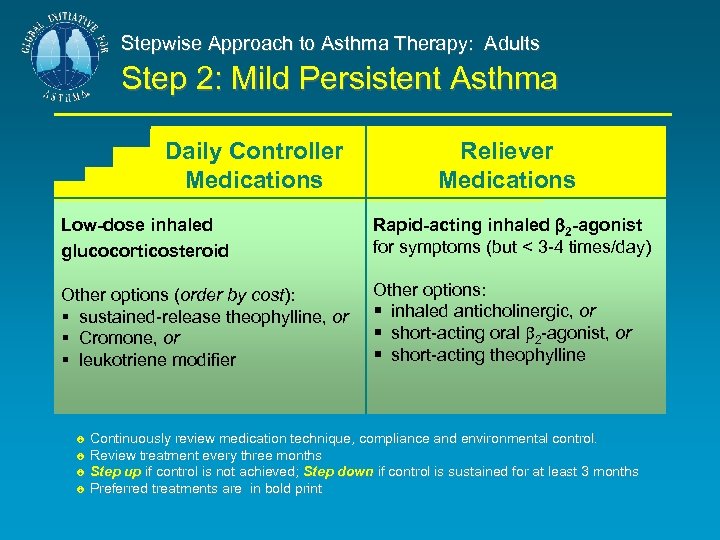
Stepwise Approach to Asthma Therapy: Adults Step 2: Mild Persistent Asthma Daily Controller Medications Reliever Medications Low-dose inhaled glucocorticosteroid Rapid-acting inhaled 2 -agonist for symptoms (but < 3 -4 times/day) Other options (order by cost): § sustained-release theophylline, or § Cromone, or § leukotriene modifier Other options: § inhaled anticholinergic, or § short-acting oral 2 -agonist, or § short-acting theophylline Continuously review medication technique, compliance and environmental control. Review treatment every three months Step up if control is not achieved; Step down if control is sustained for at least 3 months Preferred treatments are in bold print
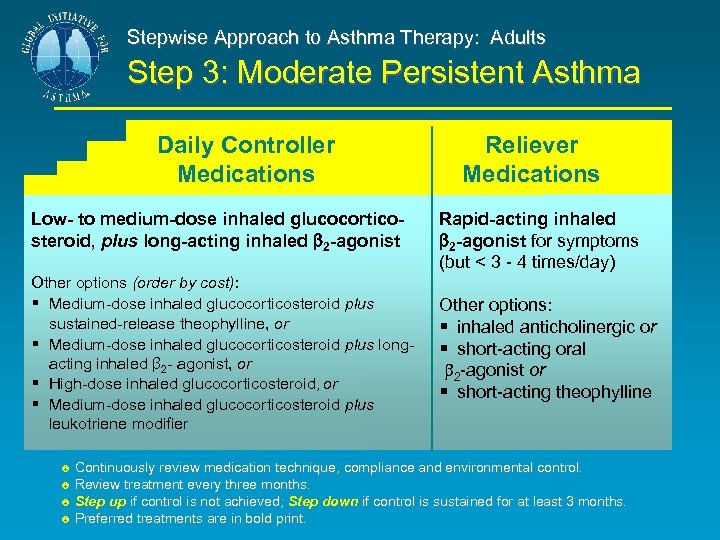
Stepwise Approach to Asthma Therapy: Adults Step 3: Moderate Persistent Asthma Daily Controller Medications Low- to medium-dose inhaled glucocorticosteroid, plus long-acting inhaled 2 -agonist Other options (order by cost): § Medium-dose inhaled glucocorticosteroid plus sustained-release theophylline, or § Medium-dose inhaled glucocorticosteroid plus longacting inhaled β 2 - agonist, or § High-dose inhaled glucocorticosteroid, or § Medium-dose inhaled glucocorticosteroid plus leukotriene modifier Reliever Medications Rapid-acting inhaled 2 -agonist for symptoms (but < 3 - 4 times/day) Other options: § inhaled anticholinergic or § short-acting oral 2 -agonist or § short-acting theophylline Continuously review medication technique, compliance and environmental control. Review treatment every three months. Step up if control is not achieved; Step down if control is sustained for at least 3 months. Preferred treatments are in bold print.
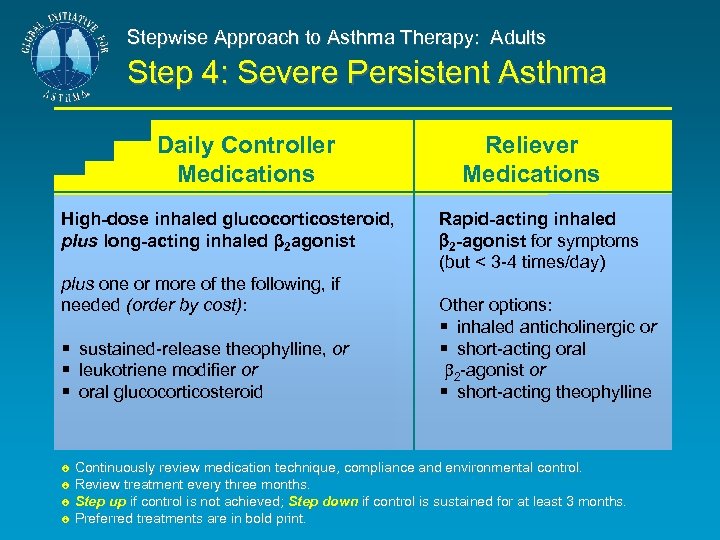
Stepwise Approach to Asthma Therapy: Adults Step 4: Severe Persistent Asthma Daily Controller Medications High-dose inhaled glucocorticosteroid, plus long-acting inhaled β 2 agonist plus one or more of the following, if needed (order by cost): § sustained-release theophylline, or § leukotriene modifier or § oral glucocorticosteroid Reliever Medications Rapid-acting inhaled 2 -agonist for symptoms (but < 3 -4 times/day) Other options: § inhaled anticholinergic or § short-acting oral 2 -agonist or § short-acting theophylline Continuously review medication technique, compliance and environmental control. Review treatment every three months. Step up if control is not achieved; Step down if control is sustained for at least 3 months. Preferred treatments are in bold print.
c1cde53f57686a07bdfe12c0ec798871.ppt