2bccfa160c43aab26bcc8a7c5da0ead1.ppt
- Количество слайдов: 60
FVA for Students with Multiple Disabilities to include Cerebral Visual Impairment (CVI): A Collaborative Approach Across Disciplines Part II- Perkins Webinar Rajiv K. Panikkar, MA, CLVT, COMS, TVI Joanne Szabo PT, DPT, MHA, PCS Arizona State School for the Deaf & Blind
Objectives Participants will: • Understand challenges TVIs / O&M face completing FVAs for students with CVI • Recognize the importance of team collaboration • Discuss how to build an FVA for a student identified with CVI. • Apply collaborative strategies • Understand the importance of reassessment
Challenges • TVI has lack of familiarity with student • Student may not receive O & M • Lack of familiarity with CVI • Visual functioning with CVI looks different depending upon area of brain damaged (Dutton, 2003) • Routines may require equipment and staff support • Optimal learning conditions can be very specific and difficult to set up • Student may not be able to help or take part in the assessment process secondary to additional disabilities
Solution COLLABORATION!! Use the team that knows the child, including his or her family and caregivers. YOU CANNOT DO THIS ALONE! Erin & Topor 2010
Difference between traditional FVA & FVA for CVI • In early stages, CVI will cover up any other ocular impairment (cannot perform traditional FVA) • The TVI/O&M are the lead for the FVA but other trained professionals are needed since CVI affects many behavioral areas • The teams job is to “ensure that the full range of effects of CVI are appraised” (Lueck & Dutton, 2015)
FVA for CVI • A solid understanding of CVI is critical when assessing / administering testing to a student with CVI • Testing items requiring the student to use vision must be within the student’s visual capabilities Lueck & Dutton, 2015
Preparation for FVA Gather information • Medical records review • Interview • Family / caregiver • School team members • Observations • Home (may be via interview) • Lead evaluator to bring info back to the team • School • Direct Assessment
Medical Records Review • Reports from eye care specialist • TVI can assist in interpretation of eye report • Not a complete picture of vision use —uncertainty may be documented • Eye report may be “normal” • Evaluation important for health of eye and to document pathology • Often can determine if refractive error present—if glasses prescribed they should be worn during assessment
Medical Records Review Cont. • Medical reports – neurologist + • Are there conditions associated with CVI? • Asphyxia • Perinatal hypoxic-ischemic encephalopathy • Intraventricular hemorrhage • Periventricular leukomalacia • CNS infection • Trauma • Cerebral vascular accident • Structural abnormalities Teplin, S. W. (1995)
Interview—Family / Caregiver • Parents provide critical information for CVI assessment • Visual behaviors may be different at home • Parents may know how to elicit visual responses • Know likes and dislikes very well • Information gathered about CVI behaviors will later help with the assessment at school • Parents are key to helping their child learn to use his or her vision so keep them in the loop!
Interview—Family / Caregiver Cont. • Questions that help ID CVI behaviors • What does child prefer to look at? • Does their child have a preferred color? • When is the child at his or her best e. g. most visually alert? • Will the child look into their faces? • Does the child notice things that are moving more than stationary objects? • Is there a side he or she sees better from? • Guide to Parent Interview Questions (Roman-Lantzy, 2007 p. 41)
Interview—School team • Teachers / therapists • Lead uses Multidisciplinary Team Interview Form • Helps meet the team member’s needs • Areas of concern are documented • Questions about vision use are asked • Goals are identified
Multidisciplinary Team Interview Form • Develops a picture of the whole child • Current participation at school • Physical abilities • Communication mode • How providers see student’s vision use • What modifications are being used • Behaviors / medication that may affect testing • Any other concerns / questions
Form Contents • Use of vision and working distances • Changes in vision • Additional disabilities • Reading level • Visual difficulties with school tasks • Favorite tasks and visual difficulties with tasks • Low vision devices • Best lighting • Glare protection • Mobility concerns • Student’s daily schedule- home and school • Goals for FVA
What Information can be Gathered From The Form • The tools you will need for the FVA • The environments you will need to include for observation / assessment • Possible obstacles or behaviors • Who or what can help minimize them • Motivators • Is pre-practice necessary? • If yes, give materials to staff • Which staff will need to assist you?
Observation • Important points to consider • Noisy vs quiet times • Near vs distance activities • Simple vs cluttered background • Familiar vs novel objects • Stationary vs moving objects • Watch for CVI behaviors • Color Preference • Non-purposeful gaze • Interested in moving or shiny / reflective surfaces or objects Roman-Lantzy, 2007
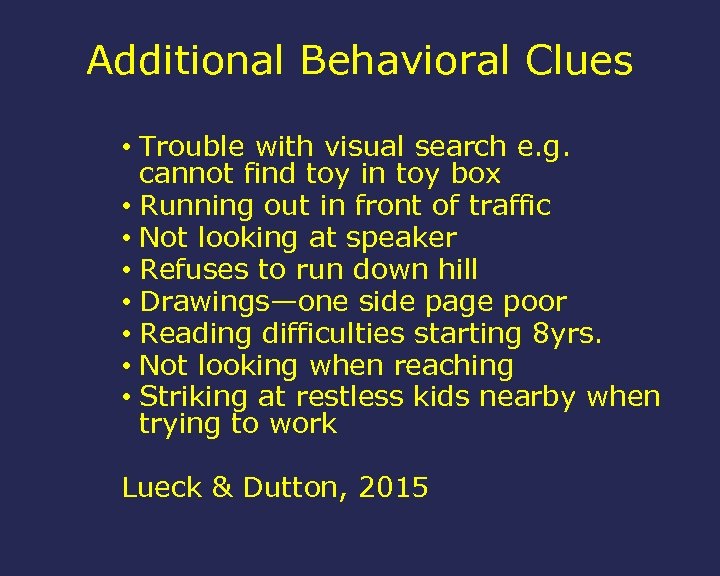
Additional Behavioral Clues • Trouble with visual search e. g. cannot find toy in toy box • Running out in front of traffic • Not looking at speaker • Refuses to run down hill • Drawings—one side page poor • Reading difficulties starting 8 yrs. • Not looking when reaching • Striking at restless kids nearby when trying to work Lueck & Dutton, 2015
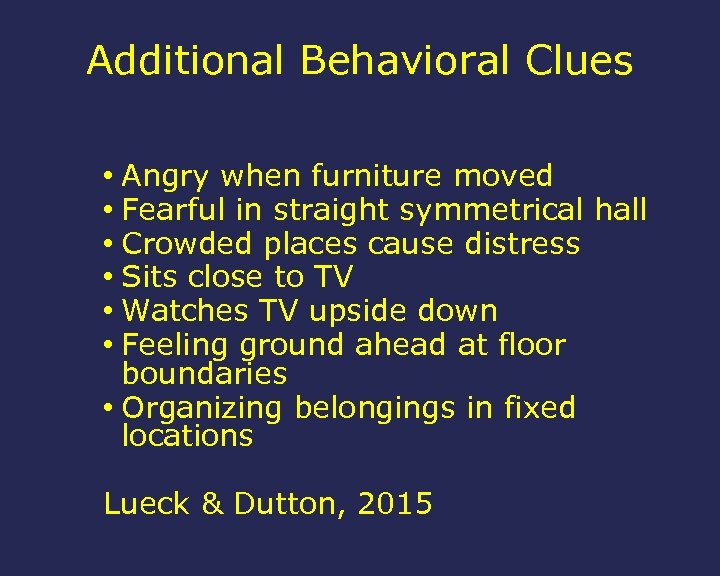
Additional Behavioral Clues • Angry when furniture moved • Fearful in straight symmetrical hall • Crowded places cause distress • Sits close to TV • Watches TV upside down • Feeling ground ahead at floor boundaries • Organizing belongings in fixed locations Lueck & Dutton, 2015
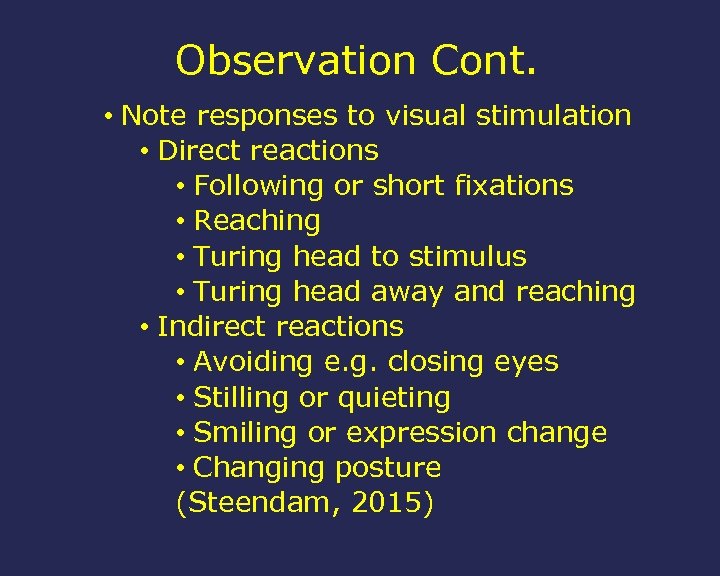
Observation Cont. • Note responses to visual stimulation • Direct reactions • Following or short fixations • Reaching • Turing head to stimulus • Turing head away and reaching • Indirect reactions • Avoiding e. g. closing eyes • Stilling or quieting • Smiling or expression change • Changing posture (Steendam, 2015)
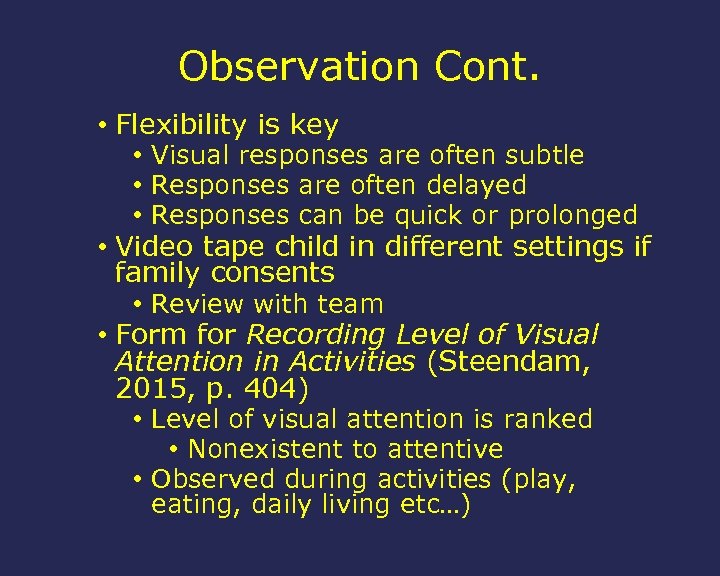
Observation Cont. • Flexibility is key • Visual responses are often subtle • Responses are often delayed • Responses can be quick or prolonged • Video tape child in different settings if family consents • Review with team • Form for Recording Level of Visual Attention in Activities (Steendam, 2015, p. 404) • Level of visual attention is ranked • Nonexistent to attentive • Observed during activities (play, eating, daily living etc…)
Observation at Home • Going to the home is best option • Interview of family—back up • Observation begins when you arrive • How is the child using vision? • How is the child reacting to stimuli? • Observe during typical routine or activity—no intervention • Observe after modification • Positioning • Materials • Environmental changes • Altering presentation (Steendam, 2015)
Observation at School • Determine areas of education • Cafeteria, transitions (mobility), class, PE, spontaneous play etc… • Select optimal times / situations • Competing sensory input can distract the use of vision • Initially observe with familiar / organic activities • Seek to understand distractions • Control and observe • Fatigue is a factor for students with multiple disabilities and CVI— opportunities may be limited
Direct Assessment • Assessment team will vary depending upon: • Student’s unique needs • The range of CVI behaviors noted • Areas included in the assessment: • Visual functions (ex: visual fields) • Functional vision (during routines) • Visual processing • Motor function (task performance and mobility) • Auditory processing (sound localization can be affected) • Environment (competing sensory stimuli) • Social / emotional issues (Lueck & Dutton, 2015)
Visual Functions Direct Assessment • Students with profound involvement may be difficult to test as CVI dominates the visual responses—may have to wait until some resolution has occurred. • Areas included in possible assessment • Functional Acuity • Oculomotor
FUNCTIONAL ACUITY REVIEW • 3 Types of Functional Acuity: • Awareness Acuity • Identification Acuity • Preferred Viewing Distance

AWARENESS ACUITY • Definition: • The furthest possible distance at which the presence of any form is first detected
AWARENESS ACUITY • Example of excerpt from report: • Location: Indoors in N’s home • Lighting: Two West-facing windows with blinds halfway closed in one window. Other window blinds open on a partly cloudy day. No additional lighting indoors. • N was first aware of a person at 15 feet. He indicated this by smiling. Due to indoor space constraints, he could be aware of an individual from a further distance. These results may vary based on lighting conditions.

IDENTIFICATION ACUITY • Definition: • The furthest possible distance at which a detected form is first correctly identified
IDENTIFICATION ACUITY • Example of excerpt from report: • N gave his mom a different smile than he did when looking at the evaluator from 10 feet away. This suggests he could possibly identify his mom from this distance.
PREFERRED VIEWING DISTANCE • Definition: • The most comfortable distance for viewing a detected form
PREFERRED VIEWING DISTANCE • Example of excerpt from report: • From between 3 -5 feet away, N was able to hold his gaze on his mom for approximately 2 -4 minutes.
OCULOMOTOR FUNCTION (ABILITY TO MOVE THE EYES) • Fixation • Establishing and maintaining gaze on a visual target. • Accommodation • Changes in lighting conditions that affect near, Intermediate and distance vision • Tracking • Visually following a moving target.
OCULOMOTOR FUNCTION (ABILITY TO MOVE THE EYES) • Shift of Gaze • Looking from one visual target to another • Scanning • Repeatedly fixating to look at a series of visual targets • Eye Preference • Preferred eye for most tasks

RESOURCE *CURRENTLY OUT OF PRINT? ? • Look at Me: A Resource Manual for the Development of Residual Vision in Multiply Impaired Children • Smith, Audrey J. , and Karen Shane. Cote. Look at Me: a Resource Manual for the Development of Residual Vision in Multiply Impaired Children. Pennsylvania College of Optometry Press, 1984

Functional Vision Direct Assessment • A systematic presentation of visual stimuli • Choose environments that afford best performance • Start with natural light • Darken room if no response—use additional light on viewing object • Position student supported to reduce fatigue • Goal is to document visual potential in optimal conditions • Information from observations should tell us what to eliminate from this process e. g. complex backgrounds, noise etc…
Functional Vision Assessment Approaches • Tools must allow for the observation and assessment of functional vision • Different types of tools available • CVI Range (Roman-Lantzy, 2007) • Allows monitoring of behaviors over time • Comprehensive model for assessment — 3 tiers (Lueck & Dutton, 2015) • The Sensory Learning Kit (Smith, 2009) • Focuses on sensory motor routines • Part of this kit has a functional Vision observational assessment
CVI Range • CVI Range Assessment Form • infants to adults • Identifies the presence of visual behaviors • Determines what degree the CVI characteristics affect visual functioning • Identifies where the child falls on the continuum of visual functioning 0 _____CVI RANGE______10 No visual Near to Function (Roman-Lantzy, 2007, P. 57) typical function
CVI Range Cont. • Visual and behavioral characteristics included in assessment protocol: • • • Color preference Need for movement Visual latency Visual field preferences Difficulty with visual complexity Light gazing or non-purposeful gaze Difficulty with distance viewing Absent or atypical visual reflexes Difficulty with visual novelty Absence of visually guided reach (Roman-Lantzy, 2007)
CVI Range Cont. • This is a two part assessment • Across CVI Characteristics = Rating 1 • Overview of functional vision • Within CVI characteristics = Rating 2 • Extent to which CVI is affecting vision use • The two ratings create the CVI Range for the student • Higher functioning students scoring 7 -10 on the CVI Range • CVI Extension Chart (Roman-Lantzy, 2007, P. 69) • Allows gathering of more detailed information on visual skills for literacy • Study showed high interrater, test-retest, and internal consistency reliability (Newcome, 2010)
CVI Range Cont. • Phases—defined periods in the resolution of CVI • Phase 1 (score of 0 -3) Building consistent visual behavior • Phase 2 (score 3. 25 -7) Integrate the use of vision in functional routines • Phase 3 (score 7. 25 -10) Vision use with tasks / spontaneous / curious • CVI Resolution Chart • Findings documented here • Working document for IEP writing • Guides special instruction and targeted activities (Roman-Lantzy, 2007, P. 75)
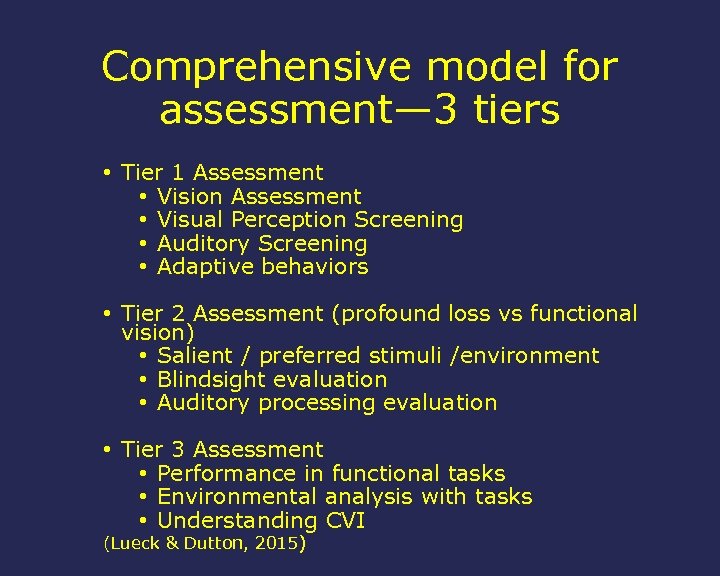
Comprehensive model for assessment— 3 tiers • Tier 1 Assessment • Vision Assessment • Visual Perception Screening • Auditory Screening • Adaptive behaviors • Tier 2 Assessment (profound loss vs functional vision) • Salient / preferred stimuli /environment • Blindsight evaluation • Auditory processing evaluation • Tier 3 Assessment • Performance in functional tasks • Environmental analysis with tasks • Understanding CVI (Lueck & Dutton, 2015)
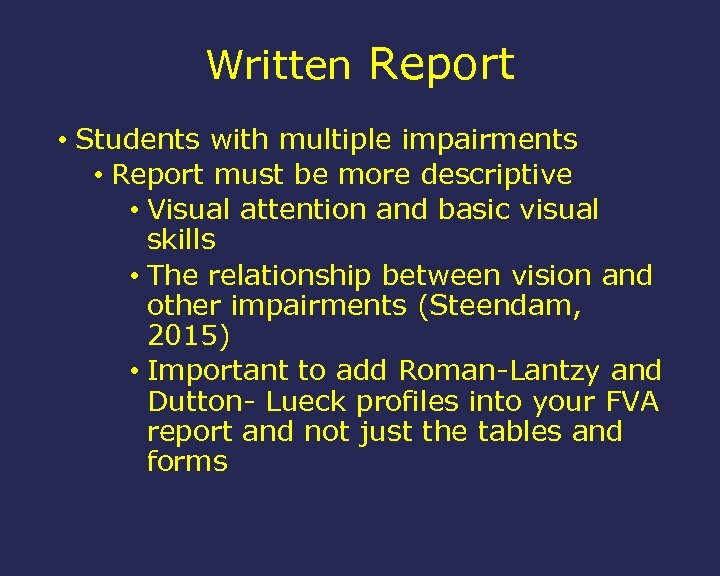
Written Report • Students with multiple impairments • Report must be more descriptive • Visual attention and basic visual skills • The relationship between vision and other impairments (Steendam, 2015) • Important to add Roman-Lantzy and Dutton- Lueck profiles into your FVA report and not just the tables and forms
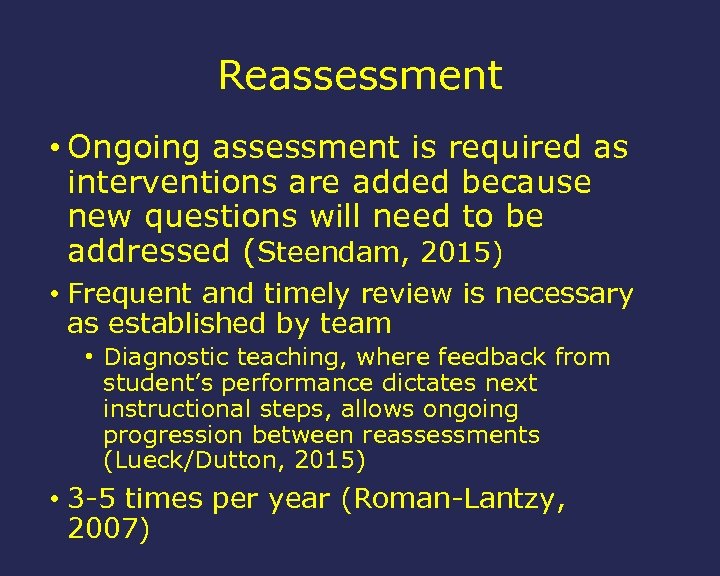
Reassessment • Ongoing assessment is required as interventions are added because new questions will need to be addressed (Steendam, 2015) • Frequent and timely review is necessary as established by team • Diagnostic teaching, where feedback from student’s performance dictates next instructional steps, allows ongoing progression between reassessments (Lueck/Dutton, 2015) • 3 -5 times per year (Roman-Lantzy, 2007)
Case Study CVI
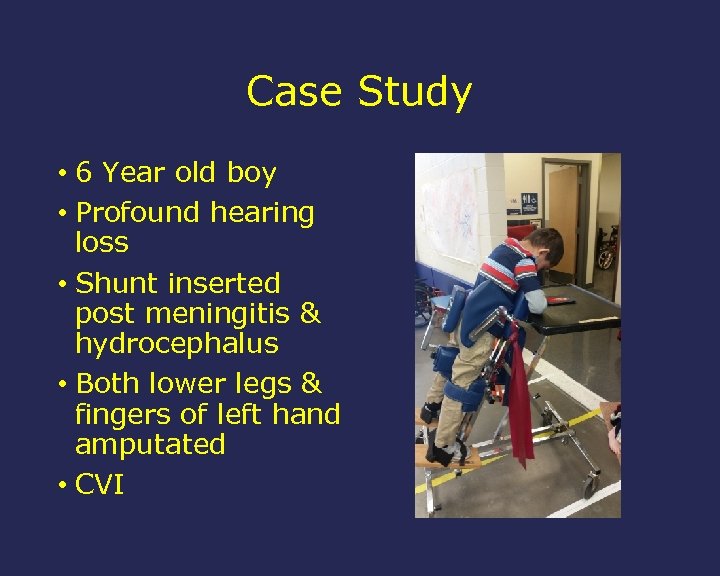
Case Study • 6 Year old boy • Profound hearing loss • Shunt inserted post meningitis & hydrocephalus • Both lower legs & fingers of left hand amputated • CVI

WHERE TO START? ?
Start Collaboration Question to be answered “How does damage to the brain affect vision? ” (Roman-Lantzy 2007 p. 51) • FVA focuses on the visual behaviors and associated CVI characteristics • Utilization of the CVI Range • Utilize the Multidisciplinary Team Form to gather information • Assessment completed by team
Work In Collaboration • Initially, most environments had trouble stopping student’s light gazing and finger flicking. No real purposeful use of vision in classroom • Team form revealed that SLP and PT were teaming to adapt environment to get visual responses Start where it’s working!!

Determine Visual Abilities as a Team • Standing in stander student focused his attention to target briefly • Preferred colors red & yellow • Throwing a ball interested him as he needed movement • Baseline Range completed by PT & SLP as that’s where he would work initially
Determine Tolerance • Fatigue is a huge issue • Identify optimal positioning for visual work • Identify optimal environment • Communicate what is working and what is not working with the team frequently!
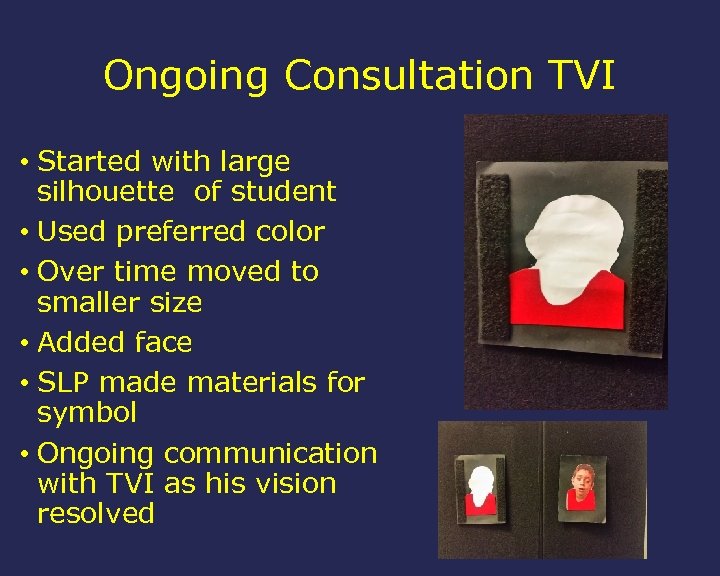
Ongoing Consultation TVI • Started with large silhouette of student • Used preferred color • Over time moved to smaller size • Added face • SLP made materials for symbol • Ongoing communication with TVI as his vision resolved
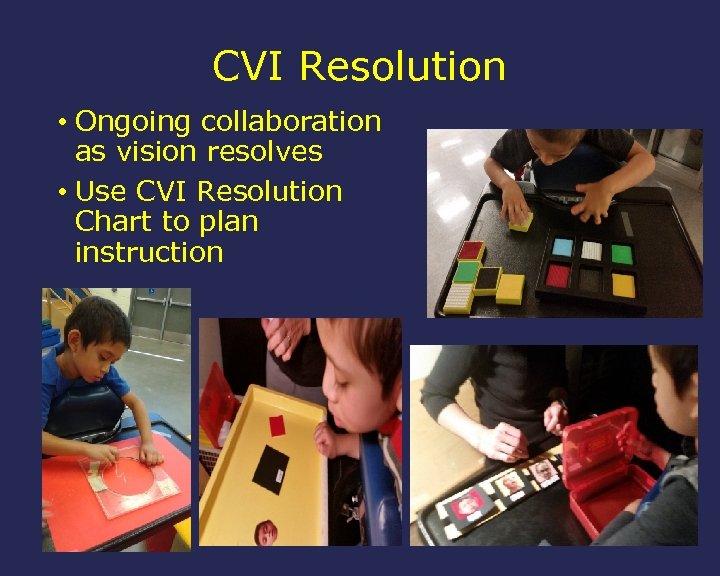
CVI Resolution • Ongoing collaboration as vision resolves • Use CVI Resolution Chart to plan instruction
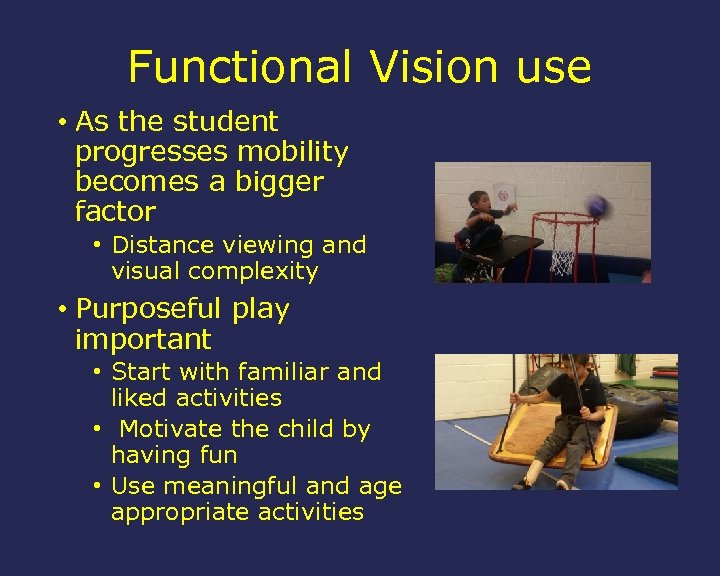
Functional Vision use • As the student progresses mobility becomes a bigger factor • Distance viewing and visual complexity • Purposeful play important • Start with familiar and liked activities • Motivate the child by having fun • Use meaningful and age appropriate activities
Start the Process! • Educate your Team • Teach others about FVAs, LMAs and eye reports • Often they don’t even know they exist • Teach them about the findings • Identify areas that the Team can be of assistance to you • Utilize the Multidisciplinary Team Interview Form to gather information • Walk your Team through the process the first few times, if necessary Distribute and review the final report to all Team members!
QUESTIONS?
References Barclay LA. Expanded core curriculum: Education. In: Goodman S and Wittenstein S, eds. Collaborative Assessment: Working with Students Who Are Blind or Visually Impaired, Including Those with Additional Disabilities. New York, NY: AFB Press; 2003: 94 -149. Dutton GN. Cognitive vision, its disorders and differential diagnosis in adults and children: Knowing where and what things are. Eye, 17(3), 289 -304. Erin JN, Topor I. Functional vision assessment of children with low vision, including those with multiple disabilities. In: Corn AL and Erin JN, eds. Foundations of Low Vision: Clinical and Functional Perspectives. 2 nd ed. New York, NY: AFB Press; 2010: 339 -389.
References Cont. Lueck AH, Dutton GN. Assessment of children with CVI: Introduction and Overview. In: Lueck A and Dutton G, eds. Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York, NY: AFB Press; 2015: 207 -260. Liefert FK. Expanded core curriculum: Orientation and mobility. In: Goodman S and Wittenstein S, eds. Collaborative Assessment: Working with Students Who Are Blind or Visually Impaired, Including Those with Additional Disabilities. New York, NY: AFB Press; 2003: 264 -297. Newcomb S. The reliability and validity of The CVI Range. Journal of Visual Impairment and Blindness. 2010; 104(10): 637 -647.
References Cont. Roman-Lantzy C. Cortical Visual Impairment: An Approach to Assessment and Intervention. New York, NY: AFB Press; 2007. Steendam M. Assessment linked to interventions: Observational assessment of young children and children with multiple disabilities. In: Lueck A and Dutton G, eds. Vision and the Brain: Understanding Cerebral Visual Impairment in Children. New York, NY: AFB Press; 2015: 391 -410. Smith M. Sensory learning kit. Louisville, KY: American Printing House for the Blind; 2009. Teplin SW. Visual impairment in infants and young children. Infants and Young Children. 1995; 8: 18 -51.

Thank You!! And… Good luck collaboratively meeting the challenges of students with multiple disabilities and CVI!
CONTACTS • Rajiv K. Panikkar- Low Vision Specialist • VM: 520 -770 -3730 • Email: rajiv. panikkar@asdb. az. gov • Joanne Szabo—Physical Therapist • VM: 520 -770 -3909 • Email: joanne. szabo@asdb. az. gov
2bccfa160c43aab26bcc8a7c5da0ead1.ppt