022673c98f88dd002cef973b535578e4.ppt
- Количество слайдов: 70
 FRCR: Physics Lectures Diagnostic Radiology Lecture 8 Mammography and tomosynthesis Dr Tim Wood Clinical Scientist
FRCR: Physics Lectures Diagnostic Radiology Lecture 8 Mammography and tomosynthesis Dr Tim Wood Clinical Scientist
 Overview • Introduction to mammography • The mammography X-ray set • The physics of mammography – X-ray spectra for mammo • Film/screen vs digital mammography • The NHS Breast Screening programme • Tomosynthesis
Overview • Introduction to mammography • The mammography X-ray set • The physics of mammography – X-ray spectra for mammo • Film/screen vs digital mammography • The NHS Breast Screening programme • Tomosynthesis
 An introduction to mammography • The aims of mammography are: – Demonstrate microcalcifications – features with high inherent contrast, but 100 μm or less in diameter – Demonstrate low contrast masses within the breast tissue – these may be relatively large, but are often very low contrast as glandular and adipose tissue have very similar atomic number (7. 4 and 6. 5, respectively) • Hence, require good spatial and contrast resolution • Also used for screening so must be lowest dose possible (more on this later) • Presents a different technical challenge compared with everything discussed so far
An introduction to mammography • The aims of mammography are: – Demonstrate microcalcifications – features with high inherent contrast, but 100 μm or less in diameter – Demonstrate low contrast masses within the breast tissue – these may be relatively large, but are often very low contrast as glandular and adipose tissue have very similar atomic number (7. 4 and 6. 5, respectively) • Hence, require good spatial and contrast resolution • Also used for screening so must be lowest dose possible (more on this later) • Presents a different technical challenge compared with everything discussed so far
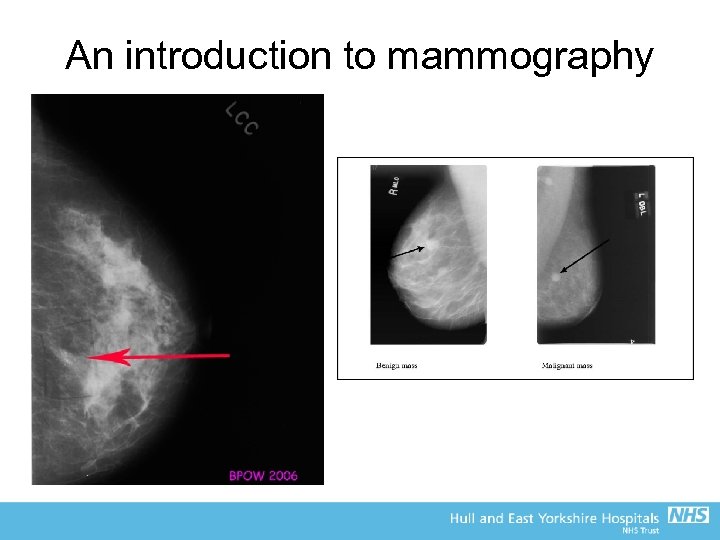 An introduction to mammography
An introduction to mammography
 The mammography X-ray set • Highly specialised X-ray systems required for mammography • Older sets based on a film-screen system • Modern sets utilise flat panels (typically direct conversion) • Sectra (now Philips) Micro. Dose uses a scanning fan beam geometry (see later)
The mammography X-ray set • Highly specialised X-ray systems required for mammography • Older sets based on a film-screen system • Modern sets utilise flat panels (typically direct conversion) • Sectra (now Philips) Micro. Dose uses a scanning fan beam geometry (see later)
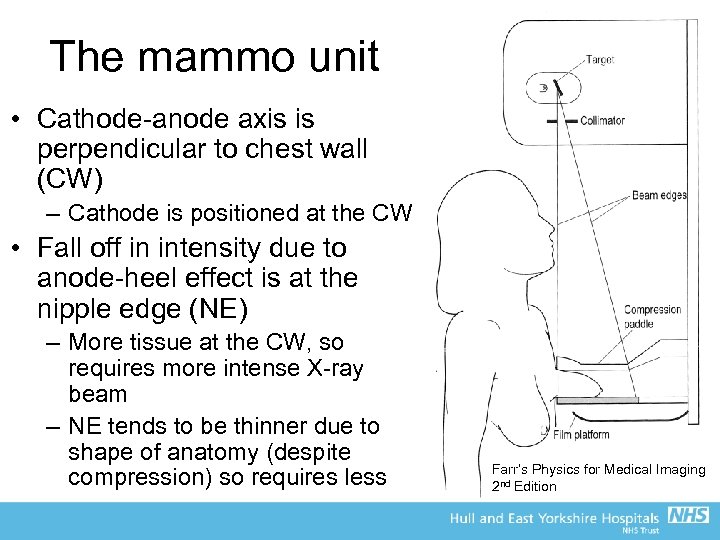 The mammo unit • Cathode-anode axis is perpendicular to chest wall (CW) – Cathode is positioned at the CW • Fall off in intensity due to anode-heel effect is at the nipple edge (NE) – More tissue at the CW, so requires more intense X-ray beam – NE tends to be thinner due to shape of anatomy (despite compression) so requires less Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • Cathode-anode axis is perpendicular to chest wall (CW) – Cathode is positioned at the CW • Fall off in intensity due to anode-heel effect is at the nipple edge (NE) – More tissue at the CW, so requires more intense X-ray beam – NE tends to be thinner due to shape of anatomy (despite compression) so requires less Farr’s Physics for Medical Imaging 2 nd Edition
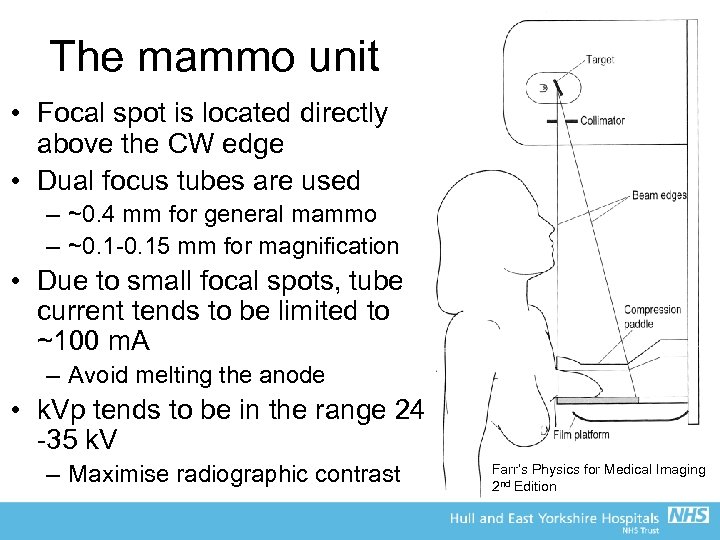 The mammo unit • Focal spot is located directly above the CW edge • Dual focus tubes are used – ~0. 4 mm for general mammo – ~0. 1 -0. 15 mm for magnification • Due to small focal spots, tube current tends to be limited to ~100 m. A – Avoid melting the anode • k. Vp tends to be in the range 24 -35 k. V – Maximise radiographic contrast Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • Focal spot is located directly above the CW edge • Dual focus tubes are used – ~0. 4 mm for general mammo – ~0. 1 -0. 15 mm for magnification • Due to small focal spots, tube current tends to be limited to ~100 m. A – Avoid melting the anode • k. Vp tends to be in the range 24 -35 k. V – Maximise radiographic contrast Farr’s Physics for Medical Imaging 2 nd Edition
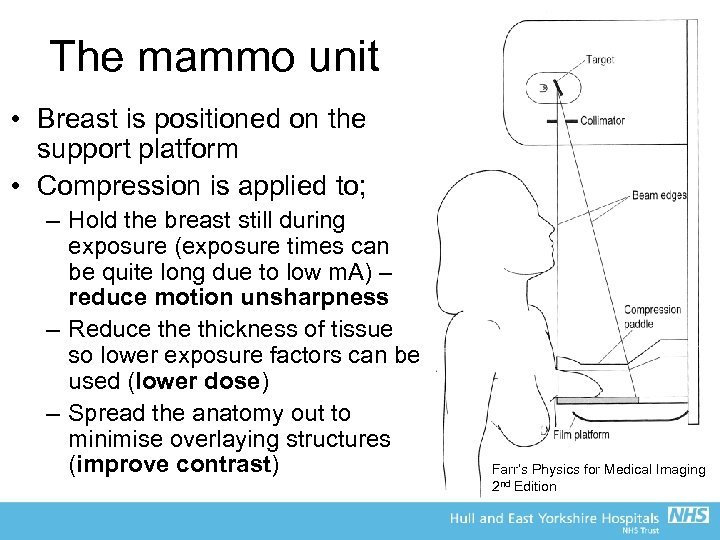 The mammo unit • Breast is positioned on the support platform • Compression is applied to; – Hold the breast still during exposure (exposure times can be quite long due to low m. A) – reduce motion unsharpness – Reduce thickness of tissue so lower exposure factors can be used (lower dose) – Spread the anatomy out to minimise overlaying structures (improve contrast) Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • Breast is positioned on the support platform • Compression is applied to; – Hold the breast still during exposure (exposure times can be quite long due to low m. A) – reduce motion unsharpness – Reduce thickness of tissue so lower exposure factors can be used (lower dose) – Spread the anatomy out to minimise overlaying structures (improve contrast) Farr’s Physics for Medical Imaging 2 nd Edition
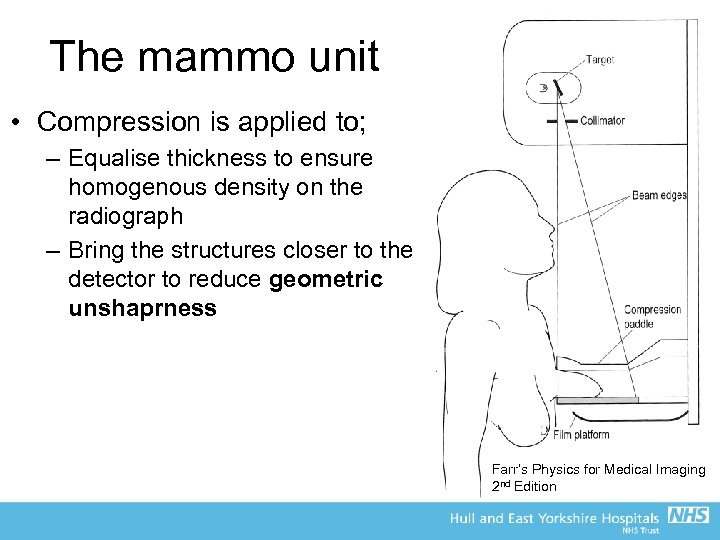 The mammo unit • Compression is applied to; – Equalise thickness to ensure homogenous density on the radiograph – Bring the structures closer to the detector to reduce geometric unshaprness Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • Compression is applied to; – Equalise thickness to ensure homogenous density on the radiograph – Bring the structures closer to the detector to reduce geometric unshaprness Farr’s Physics for Medical Imaging 2 nd Edition
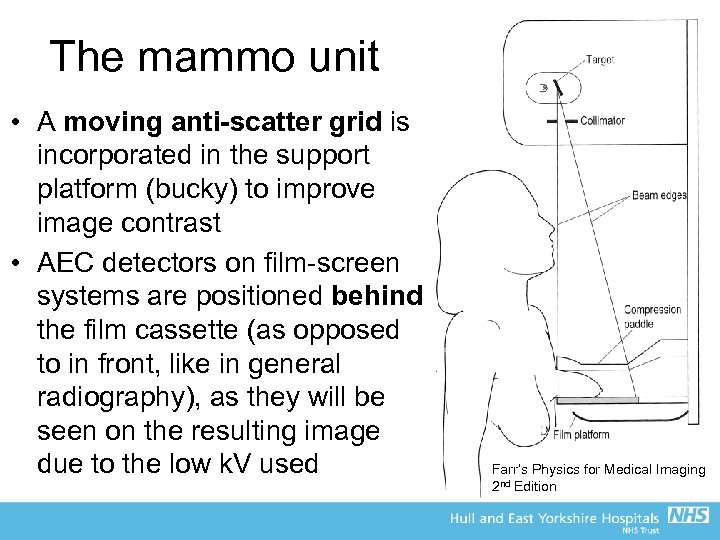 The mammo unit • A moving anti-scatter grid is incorporated in the support platform (bucky) to improve image contrast • AEC detectors on film-screen systems are positioned behind the film cassette (as opposed to in front, like in general radiography), as they will be seen on the resulting image due to the low k. V used Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • A moving anti-scatter grid is incorporated in the support platform (bucky) to improve image contrast • AEC detectors on film-screen systems are positioned behind the film cassette (as opposed to in front, like in general radiography), as they will be seen on the resulting image due to the low k. V used Farr’s Physics for Medical Imaging 2 nd Edition
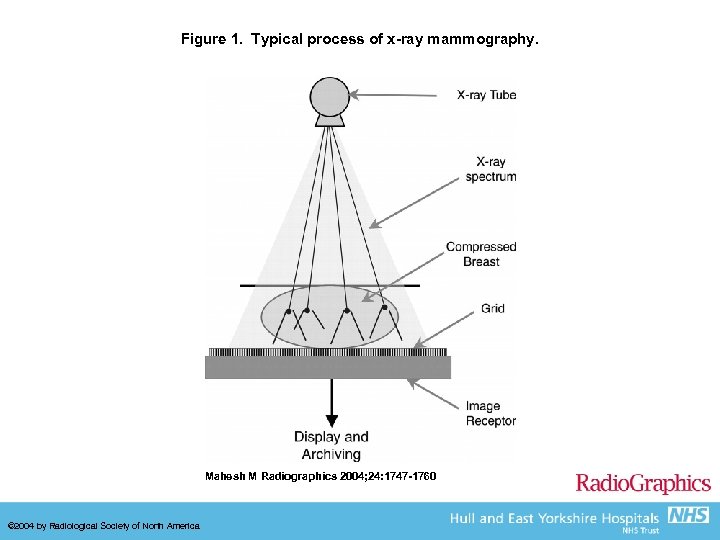 Figure 1. Typical process of x-ray mammography. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
Figure 1. Typical process of x-ray mammography. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
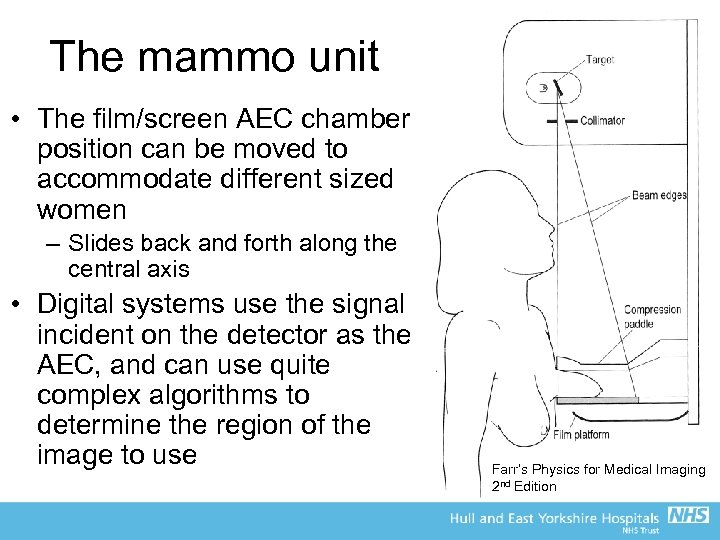 The mammo unit • The film/screen AEC chamber position can be moved to accommodate different sized women – Slides back and forth along the central axis • Digital systems use the signal incident on the detector as the AEC, and can use quite complex algorithms to determine the region of the image to use Farr’s Physics for Medical Imaging 2 nd Edition
The mammo unit • The film/screen AEC chamber position can be moved to accommodate different sized women – Slides back and forth along the central axis • Digital systems use the signal incident on the detector as the AEC, and can use quite complex algorithms to determine the region of the image to use Farr’s Physics for Medical Imaging 2 nd Edition
 The X-ray tube • In mammography, to maximise contrast use the lowest k. V possible • Typical compressed breast thickness is 40 -50 mm, and rarely greater than 80 mm • Ideal mono-energetic X-ray beam would be 1622 ke. V • Hence, the use of the full range of the Bremsstrahlung spectrum from a tungsten target with aluminium filters is not ideal for mammo • Use a range of different combinations of target and filter for different breast thicknesses and/or detectors
The X-ray tube • In mammography, to maximise contrast use the lowest k. V possible • Typical compressed breast thickness is 40 -50 mm, and rarely greater than 80 mm • Ideal mono-energetic X-ray beam would be 1622 ke. V • Hence, the use of the full range of the Bremsstrahlung spectrum from a tungsten target with aluminium filters is not ideal for mammo • Use a range of different combinations of target and filter for different breast thicknesses and/or detectors
 The mammography X-ray spectrum • Traditional film-screen mammography relies on the spectrum from a Molybdenum (Mo) target with a Mo filter for small to average sized breast (up to about 50 -60 mm) • Alternative filters such as Rhodium (Rh) can be used for thicker breasts, and some (but not many) systems use a Rh target as well • Tungsten targets are also used for thicker breasts, but in conjunction with the Rh filter (not Al like general radiography) • W/Rh is also primary target filter combination in digital systems (plus some other filters such as silver and very thin aluminium)
The mammography X-ray spectrum • Traditional film-screen mammography relies on the spectrum from a Molybdenum (Mo) target with a Mo filter for small to average sized breast (up to about 50 -60 mm) • Alternative filters such as Rhodium (Rh) can be used for thicker breasts, and some (but not many) systems use a Rh target as well • Tungsten targets are also used for thicker breasts, but in conjunction with the Rh filter (not Al like general radiography) • W/Rh is also primary target filter combination in digital systems (plus some other filters such as silver and very thin aluminium)
 The mammography X-ray spectrum • So why use these combinations for mammography? . . . • Mo – K-edge at 20 ke. V – Characteristic X-rays at 17. 4 and 19. 6 ke. V • Rh – K-edge at 23. 2 ke. V – Characteristic X-rays at 20. 2 and 22. 8 ke. V
The mammography X-ray spectrum • So why use these combinations for mammography? . . . • Mo – K-edge at 20 ke. V – Characteristic X-rays at 17. 4 and 19. 6 ke. V • Rh – K-edge at 23. 2 ke. V – Characteristic X-rays at 20. 2 and 22. 8 ke. V
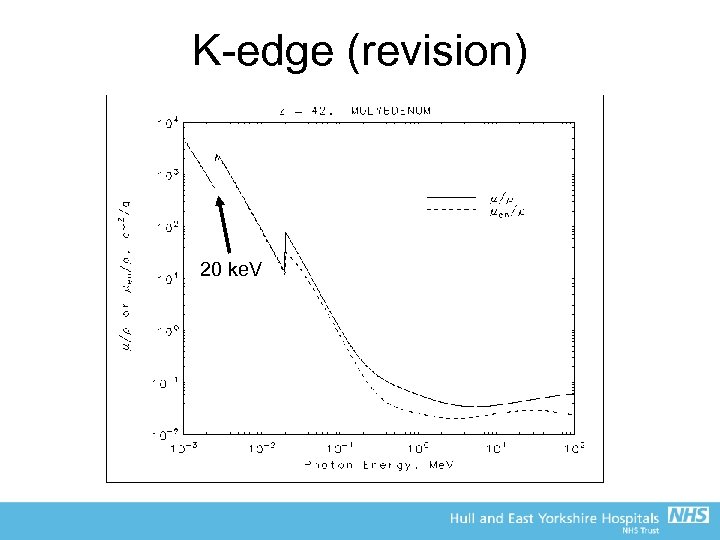 K-edge (revision) 20 ke. V
K-edge (revision) 20 ke. V
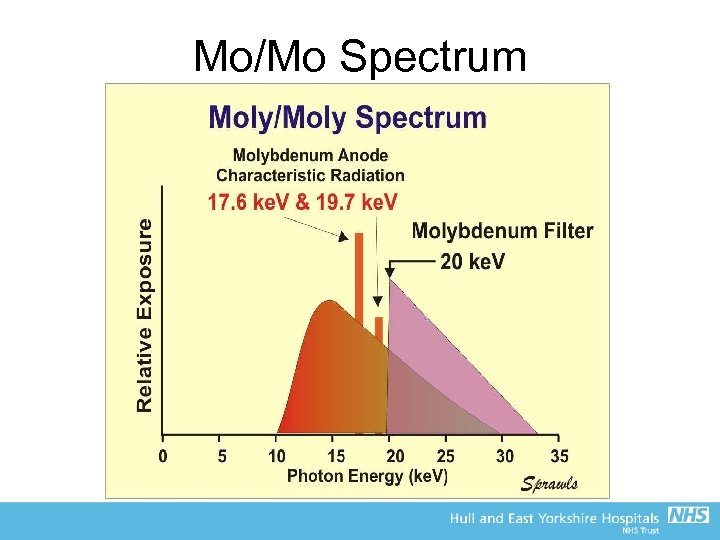 Mo/Mo Spectrum
Mo/Mo Spectrum
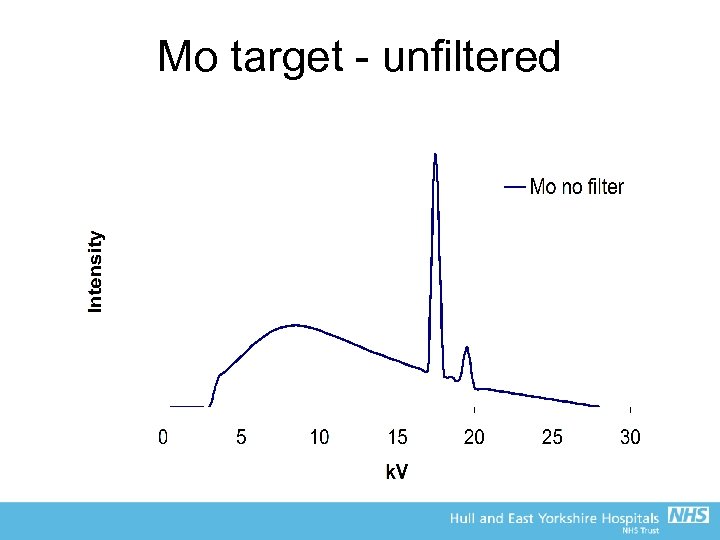
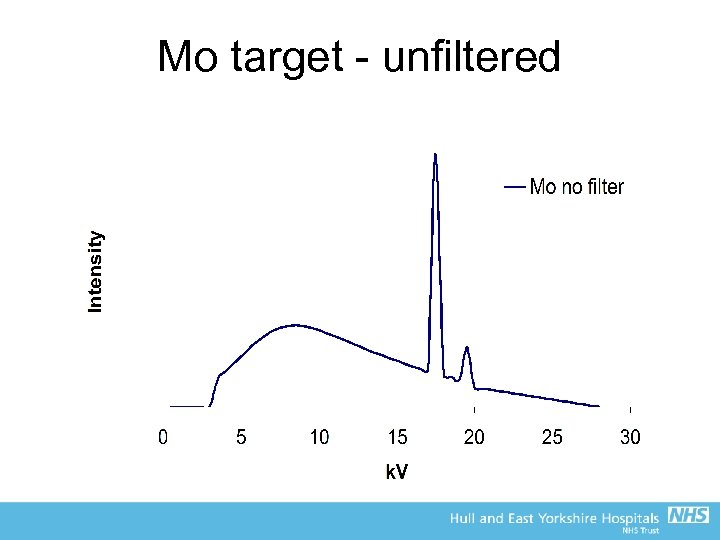 Mo target - unfiltered
Mo target - unfiltered
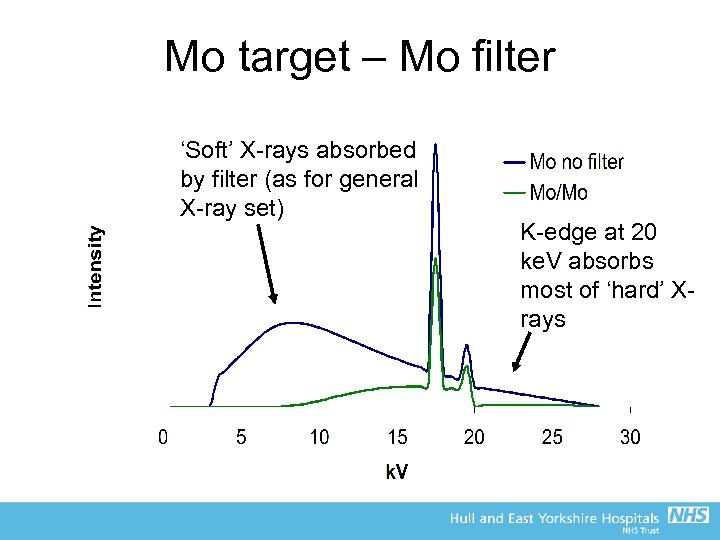 Mo target – Mo filter ‘Soft’ X-rays absorbed by filter (as for general X-ray set) K-edge at 20 ke. V absorbs most of ‘hard’ Xrays
Mo target – Mo filter ‘Soft’ X-rays absorbed by filter (as for general X-ray set) K-edge at 20 ke. V absorbs most of ‘hard’ Xrays
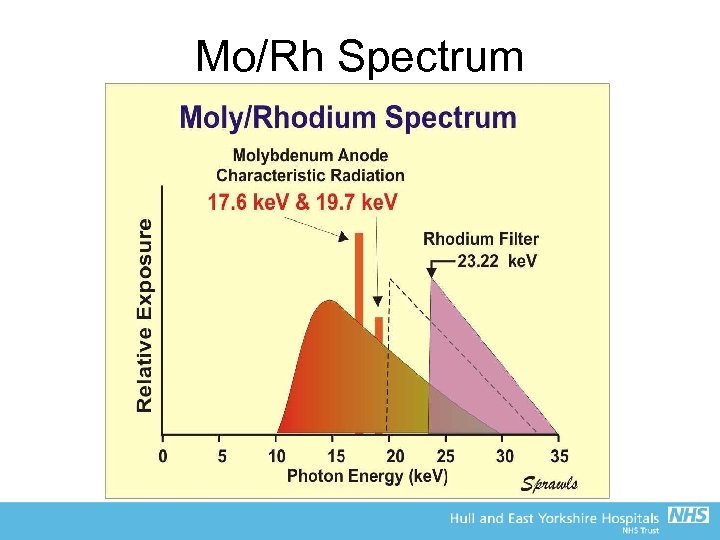 Mo/Rh Spectrum
Mo/Rh Spectrum
 Mo target - unfiltered
Mo target - unfiltered
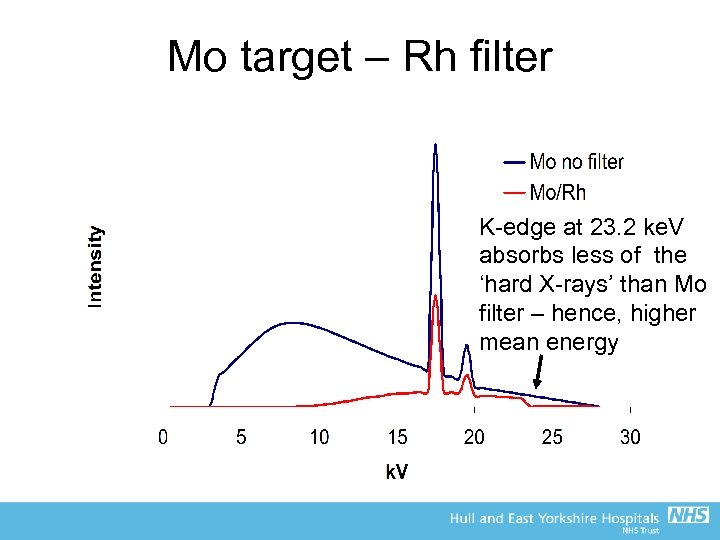 Mo target – Rh filter K-edge at 23. 2 ke. V absorbs less of the ‘hard X-rays’ than Mo filter – hence, higher mean energy
Mo target – Rh filter K-edge at 23. 2 ke. V absorbs less of the ‘hard X-rays’ than Mo filter – hence, higher mean energy
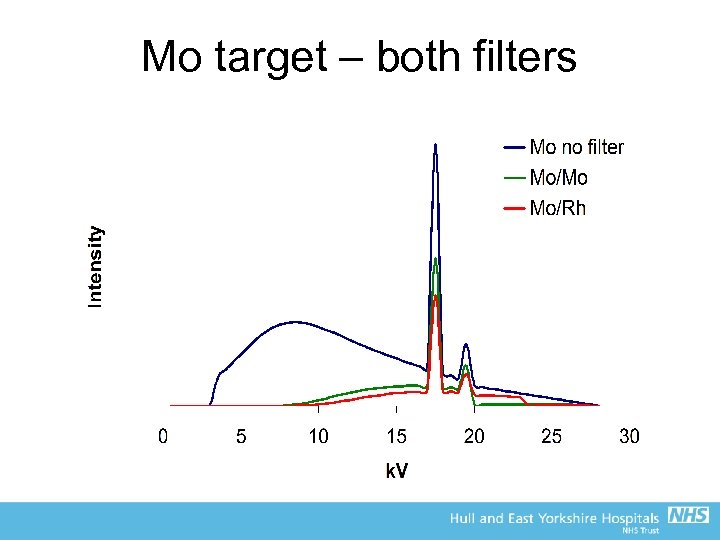 Mo target – both filters
Mo target – both filters
 Mammography X-ray spectra • Traditionally, mammography relies on the characteristic X-rays and K-edges of target/filter materials to produce a low energy spectrum around the ideal 16 -22 ke. V • Thicker breasts, however, require more penetrating beams, so W or Rh target may be used • Result in higher mean energy of X-ray beam • For thinner to thicker breasts, systems tend to use: – Mo/Mo then Mo/Rh then Rh/Rh or W/Rh
Mammography X-ray spectra • Traditionally, mammography relies on the characteristic X-rays and K-edges of target/filter materials to produce a low energy spectrum around the ideal 16 -22 ke. V • Thicker breasts, however, require more penetrating beams, so W or Rh target may be used • Result in higher mean energy of X-ray beam • For thinner to thicker breasts, systems tend to use: – Mo/Mo then Mo/Rh then Rh/Rh or W/Rh
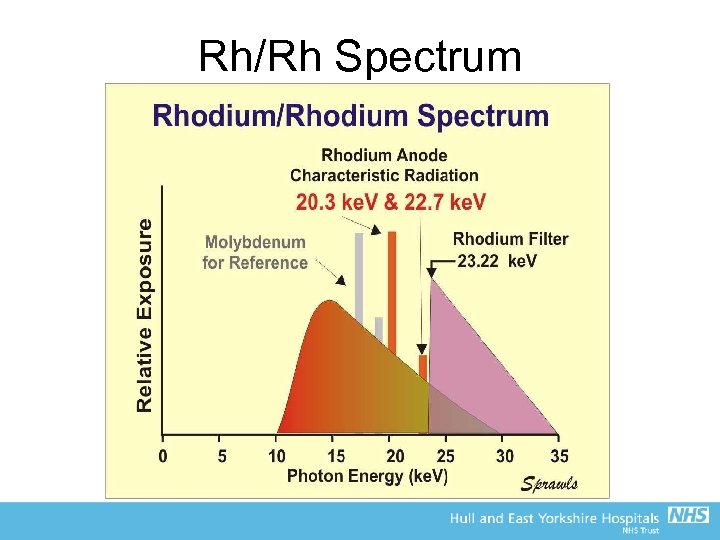 Rh/Rh Spectrum
Rh/Rh Spectrum
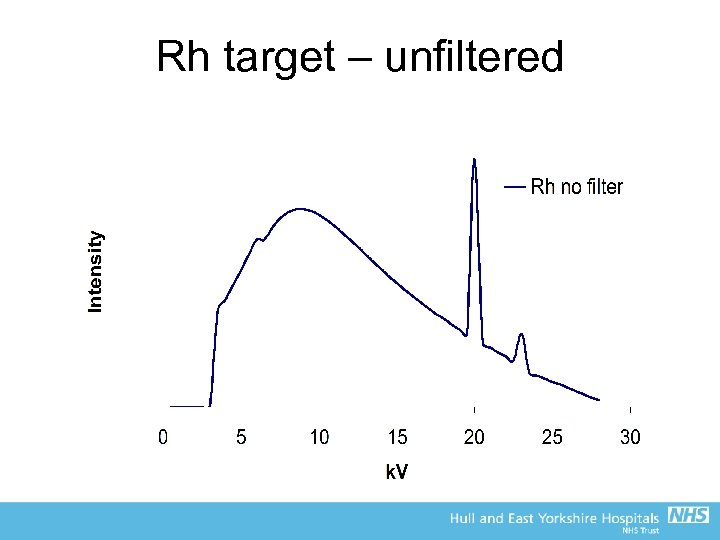 Rh target – unfiltered
Rh target – unfiltered
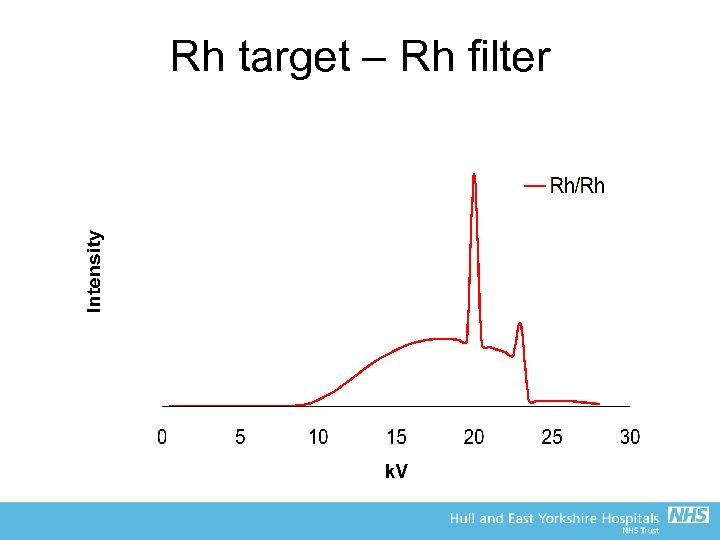 Rh target – Rh filter
Rh target – Rh filter
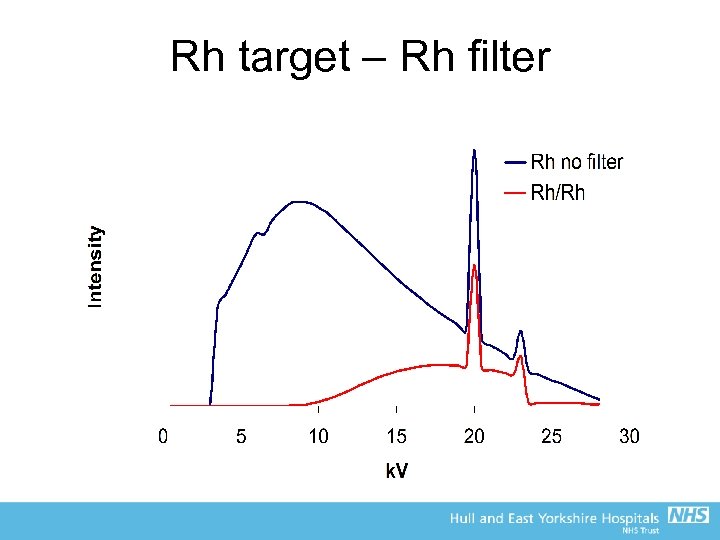 Rh target – Rh filter
Rh target – Rh filter
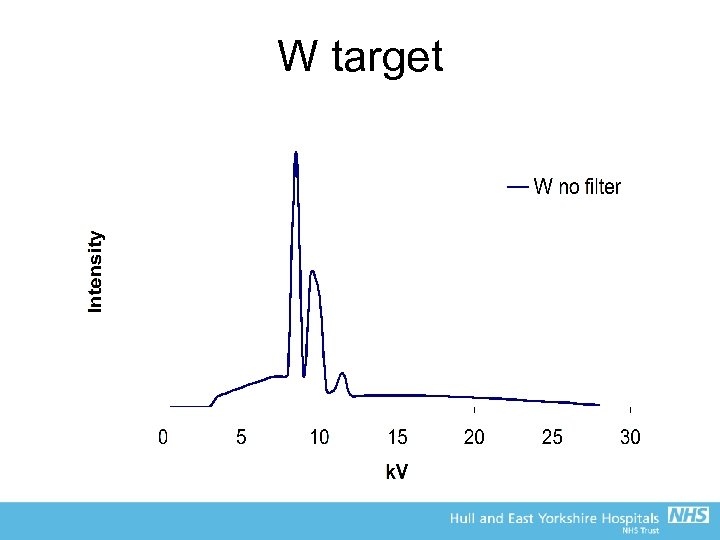 W target
W target
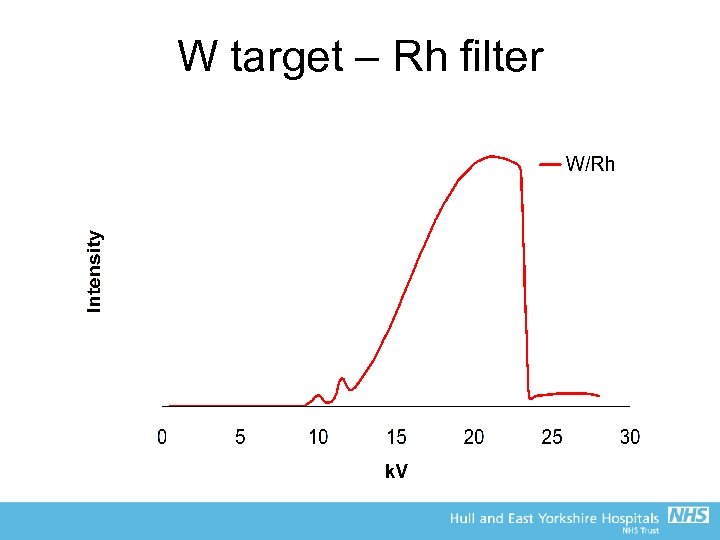 W target – Rh filter
W target – Rh filter
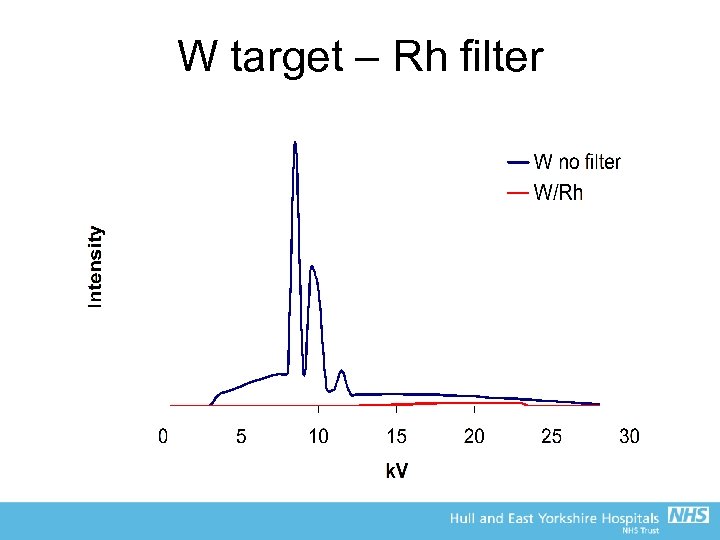 W target – Rh filter
W target – Rh filter
 Mammography X-ray spectra • Digital mammography tends to use W/Rh combination as digital gives much better contrast than the fixed dynamic range of film – Hence, the poorer contrast due to the harder X-ray beam is less significant than the gain due to the use of digital (window and level, image processing, etc) – Allows lower doses to be used for the same image quality – In practice, contrast resolution in digital is much better than film
Mammography X-ray spectra • Digital mammography tends to use W/Rh combination as digital gives much better contrast than the fixed dynamic range of film – Hence, the poorer contrast due to the harder X-ray beam is less significant than the gain due to the use of digital (window and level, image processing, etc) – Allows lower doses to be used for the same image quality – In practice, contrast resolution in digital is much better than film
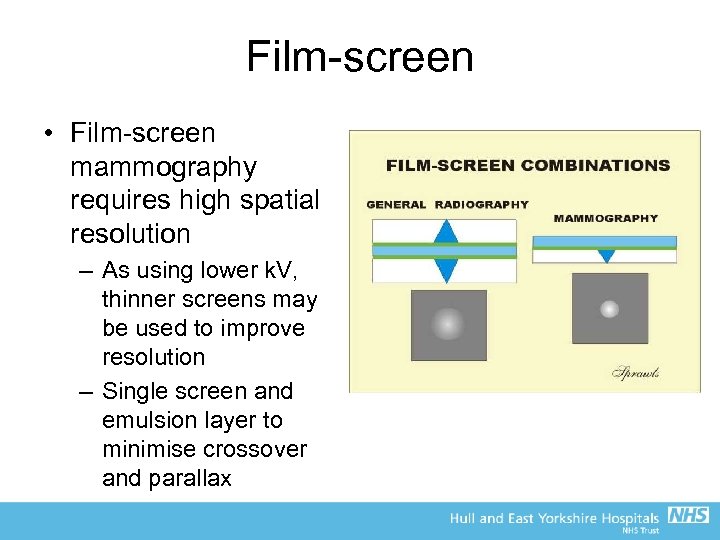 Film-screen • Film-screen mammography requires high spatial resolution – As using lower k. V, thinner screens may be used to improve resolution – Single screen and emulsion layer to minimise crossover and parallax
Film-screen • Film-screen mammography requires high spatial resolution – As using lower k. V, thinner screens may be used to improve resolution – Single screen and emulsion layer to minimise crossover and parallax
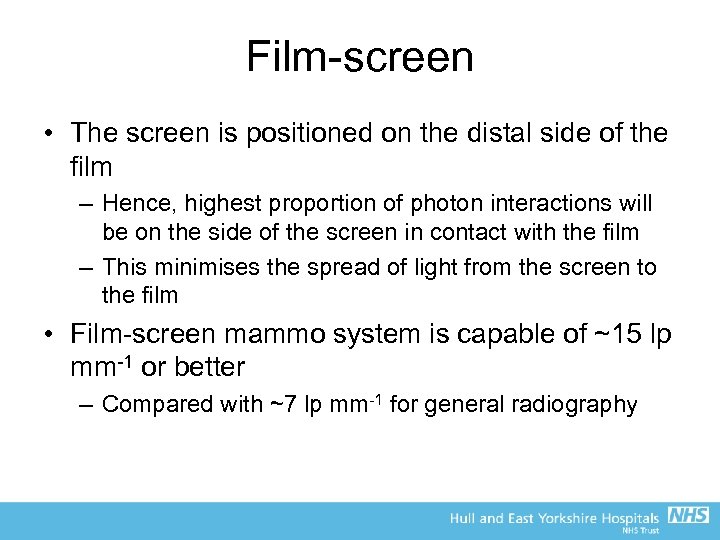 Film-screen • The screen is positioned on the distal side of the film – Hence, highest proportion of photon interactions will be on the side of the screen in contact with the film – This minimises the spread of light from the screen to the film • Film-screen mammo system is capable of ~15 lp mm-1 or better – Compared with ~7 lp mm-1 for general radiography
Film-screen • The screen is positioned on the distal side of the film – Hence, highest proportion of photon interactions will be on the side of the screen in contact with the film – This minimises the spread of light from the screen to the film • Film-screen mammo system is capable of ~15 lp mm-1 or better – Compared with ~7 lp mm-1 for general radiography
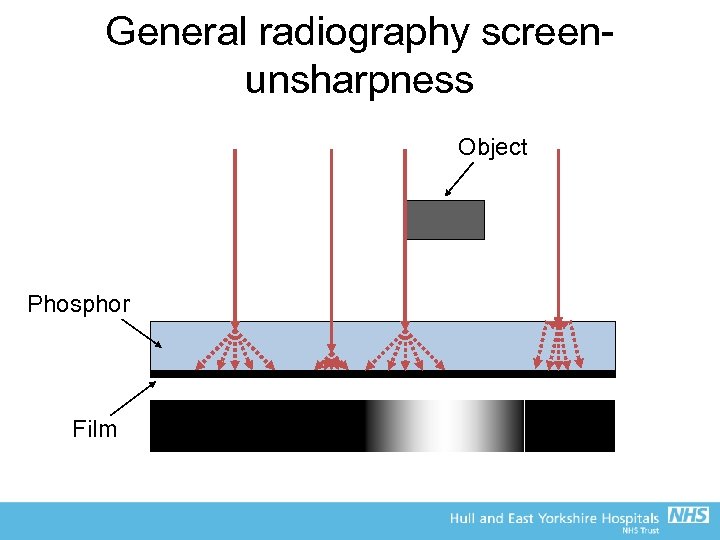 General radiography screenunsharpness Object Phosphor Film
General radiography screenunsharpness Object Phosphor Film
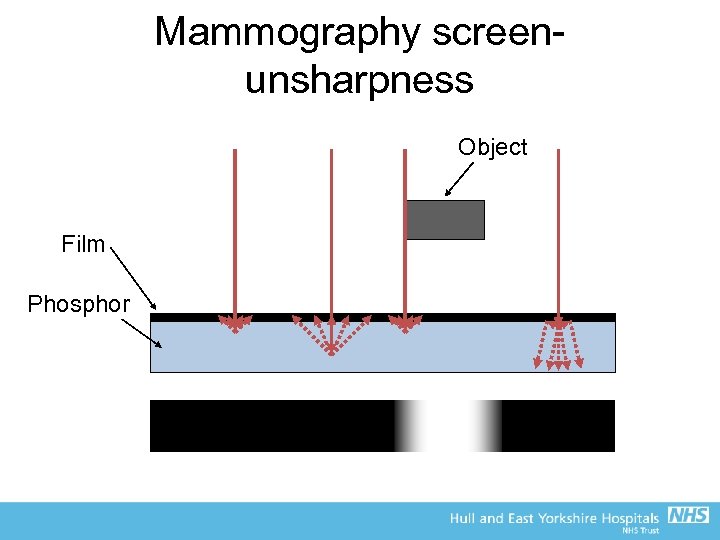 Mammography screenunsharpness Object Film Phosphor
Mammography screenunsharpness Object Film Phosphor
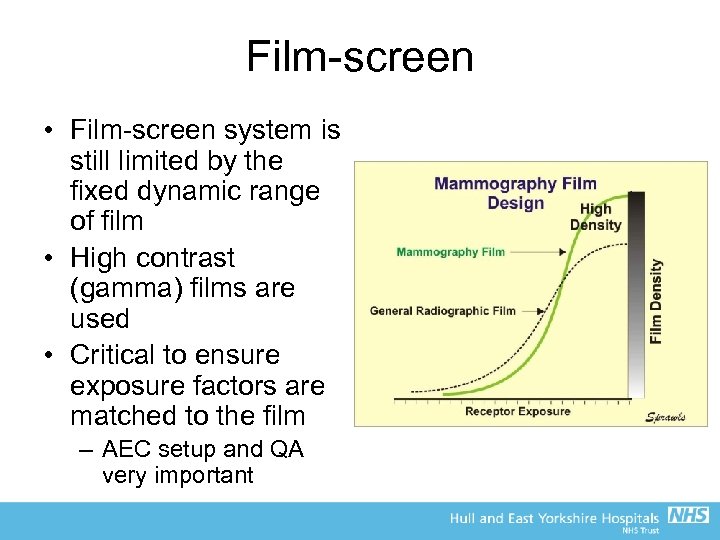 Film-screen • Film-screen system is still limited by the fixed dynamic range of film • High contrast (gamma) films are used • Critical to ensure exposure factors are matched to the film – AEC setup and QA very important
Film-screen • Film-screen system is still limited by the fixed dynamic range of film • High contrast (gamma) films are used • Critical to ensure exposure factors are matched to the film – AEC setup and QA very important
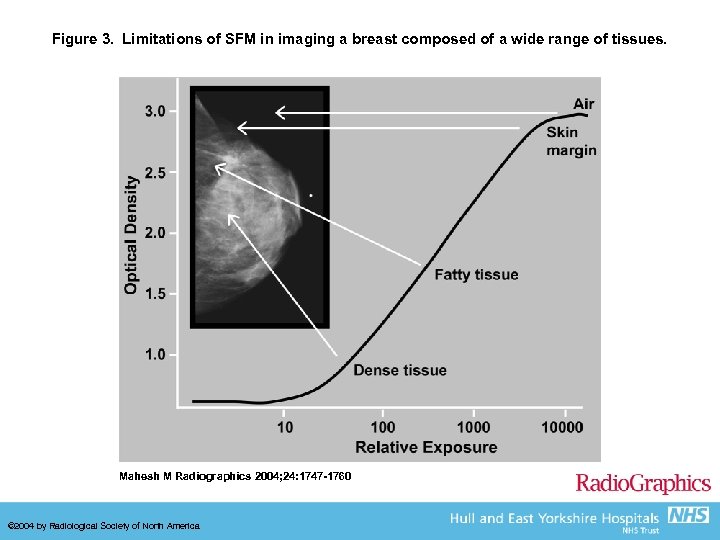 Figure 3. Limitations of SFM in imaging a breast composed of a wide range of tissues. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
Figure 3. Limitations of SFM in imaging a breast composed of a wide range of tissues. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
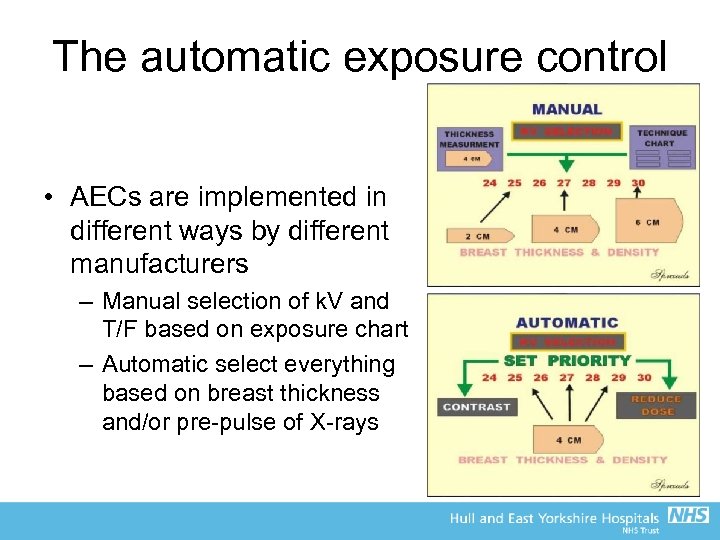 The automatic exposure control • AECs are implemented in different ways by different manufacturers – Manual selection of k. V and T/F based on exposure chart – Automatic select everything based on breast thickness and/or pre-pulse of X-rays
The automatic exposure control • AECs are implemented in different ways by different manufacturers – Manual selection of k. V and T/F based on exposure chart – Automatic select everything based on breast thickness and/or pre-pulse of X-rays
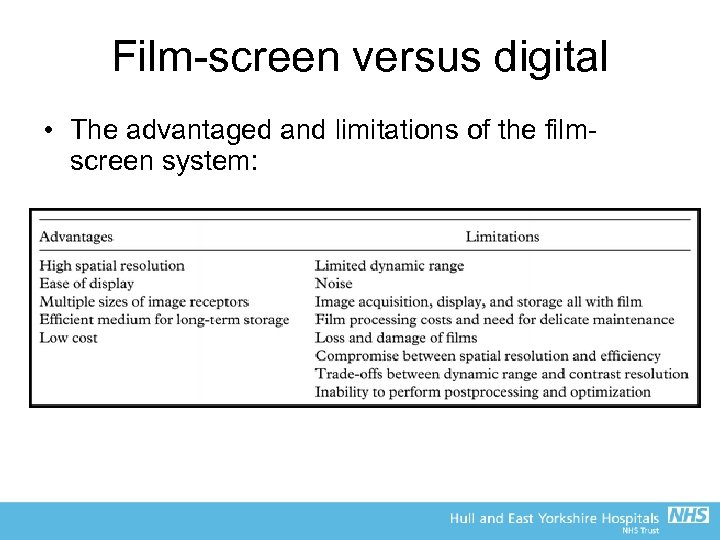 Film-screen versus digital • The advantaged and limitations of the filmscreen system:
Film-screen versus digital • The advantaged and limitations of the filmscreen system:
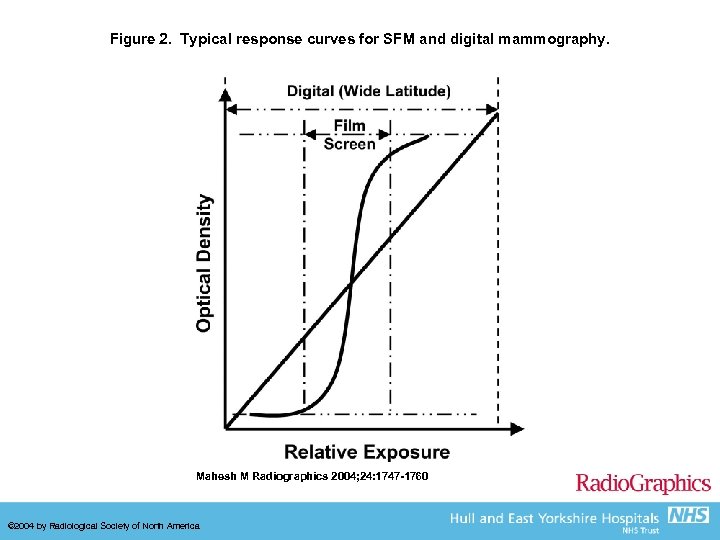 Figure 2. Typical response curves for SFM and digital mammography. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
Figure 2. Typical response curves for SFM and digital mammography. Mahesh M Radiographics 2004; 24: 1747 -1760 © 2004 by Radiological Society of North America
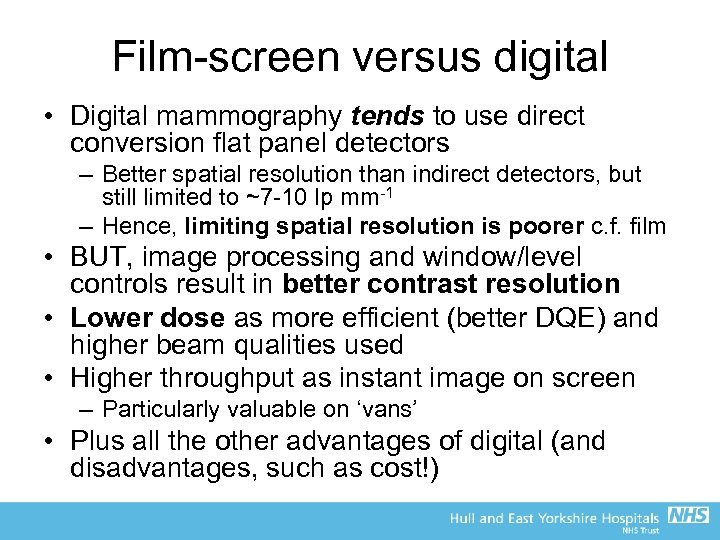 Film-screen versus digital • Digital mammography tends to use direct conversion flat panel detectors – Better spatial resolution than indirect detectors, but still limited to ~7 -10 lp mm-1 – Hence, limiting spatial resolution is poorer c. f. film • BUT, image processing and window/level controls result in better contrast resolution • Lower dose as more efficient (better DQE) and higher beam qualities used • Higher throughput as instant image on screen – Particularly valuable on ‘vans’ • Plus all the other advantages of digital (and disadvantages, such as cost!)
Film-screen versus digital • Digital mammography tends to use direct conversion flat panel detectors – Better spatial resolution than indirect detectors, but still limited to ~7 -10 lp mm-1 – Hence, limiting spatial resolution is poorer c. f. film • BUT, image processing and window/level controls result in better contrast resolution • Lower dose as more efficient (better DQE) and higher beam qualities used • Higher throughput as instant image on screen – Particularly valuable on ‘vans’ • Plus all the other advantages of digital (and disadvantages, such as cost!)
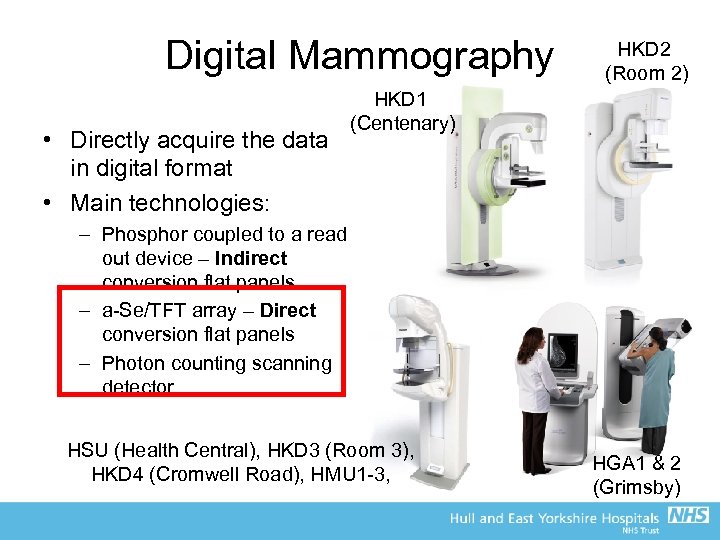 Digital Mammography • Directly acquire the data in digital format • Main technologies: HKD 2 (Room 2) HKD 1 (Centenary) – Phosphor coupled to a read out device – Indirect conversion flat panels – a-Se/TFT array – Direct conversion flat panels – Photon counting scanning detector HSU (Health Central), HKD 3 (Room 3), HKD 4 (Cromwell Road), HMU 1 -3, HGA 1 & 2 (Grimsby)
Digital Mammography • Directly acquire the data in digital format • Main technologies: HKD 2 (Room 2) HKD 1 (Centenary) – Phosphor coupled to a read out device – Indirect conversion flat panels – a-Se/TFT array – Direct conversion flat panels – Photon counting scanning detector HSU (Health Central), HKD 3 (Room 3), HKD 4 (Cromwell Road), HMU 1 -3, HGA 1 & 2 (Grimsby)
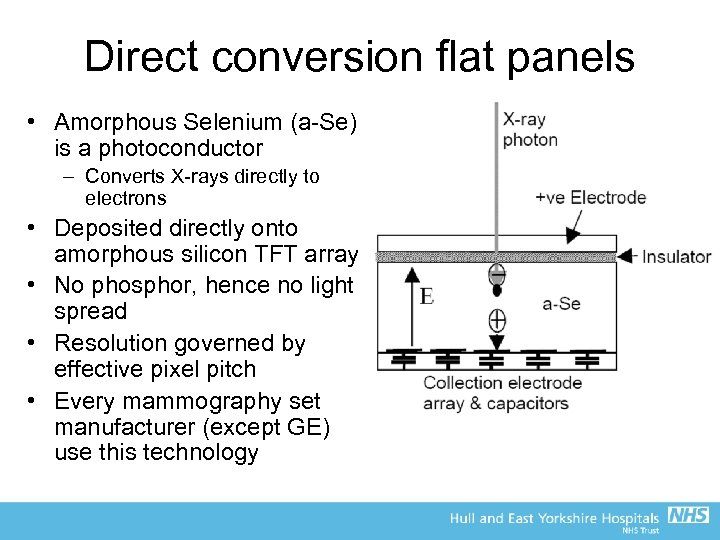 Direct conversion flat panels • Amorphous Selenium (a-Se) is a photoconductor – Converts X-rays directly to electrons • Deposited directly onto amorphous silicon TFT array • No phosphor, hence no light spread • Resolution governed by effective pixel pitch • Every mammography set manufacturer (except GE) use this technology
Direct conversion flat panels • Amorphous Selenium (a-Se) is a photoconductor – Converts X-rays directly to electrons • Deposited directly onto amorphous silicon TFT array • No phosphor, hence no light spread • Resolution governed by effective pixel pitch • Every mammography set manufacturer (except GE) use this technology
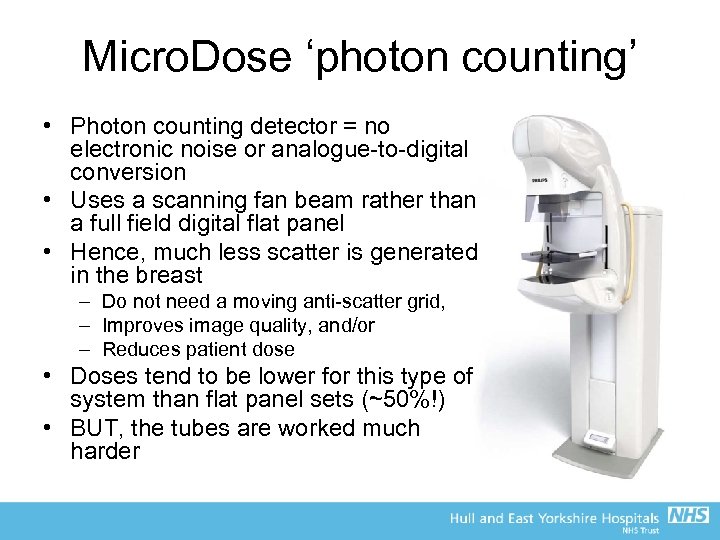 Micro. Dose ‘photon counting’ • Photon counting detector = no electronic noise or analogue-to-digital conversion • Uses a scanning fan beam rather than a full field digital flat panel • Hence, much less scatter is generated in the breast – Do not need a moving anti-scatter grid, – Improves image quality, and/or – Reduces patient dose • Doses tend to be lower for this type of system than flat panel sets (~50%!) • BUT, the tubes are worked much harder
Micro. Dose ‘photon counting’ • Photon counting detector = no electronic noise or analogue-to-digital conversion • Uses a scanning fan beam rather than a full field digital flat panel • Hence, much less scatter is generated in the breast – Do not need a moving anti-scatter grid, – Improves image quality, and/or – Reduces patient dose • Doses tend to be lower for this type of system than flat panel sets (~50%!) • BUT, the tubes are worked much harder
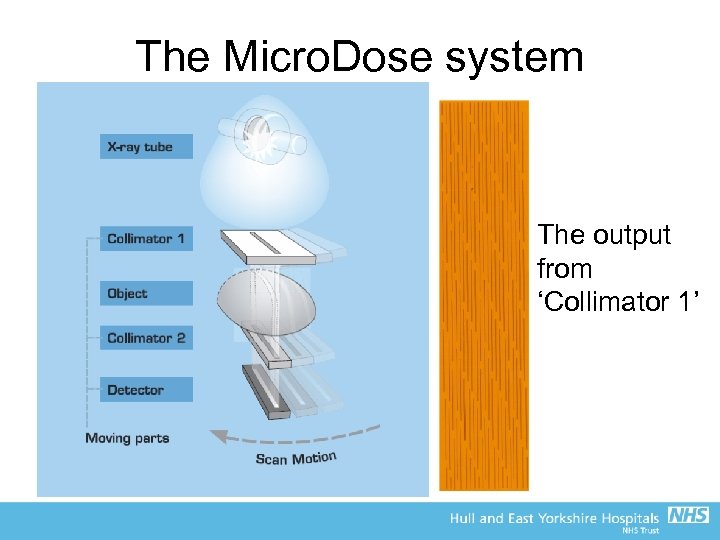 The Micro. Dose system The output from ‘Collimator 1’
The Micro. Dose system The output from ‘Collimator 1’
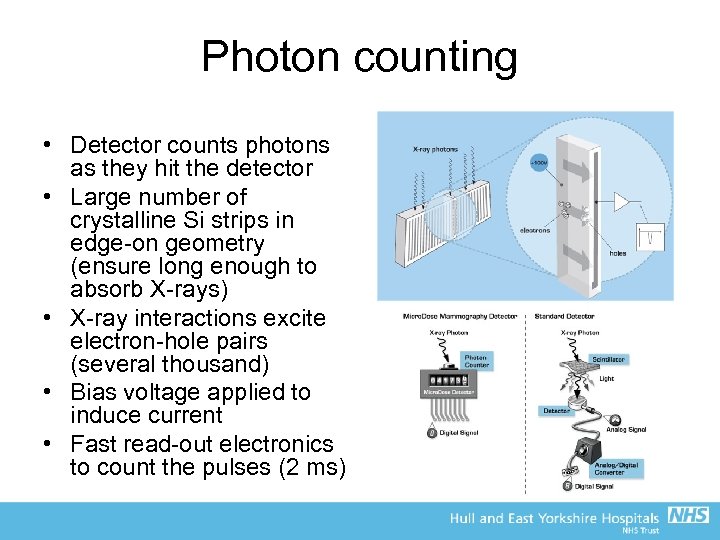 Photon counting • Detector counts photons as they hit the detector • Large number of crystalline Si strips in edge-on geometry (ensure long enough to absorb X-rays) • X-ray interactions excite electron-hole pairs (several thousand) • Bias voltage applied to induce current • Fast read-out electronics to count the pulses (2 ms)
Photon counting • Detector counts photons as they hit the detector • Large number of crystalline Si strips in edge-on geometry (ensure long enough to absorb X-rays) • X-ray interactions excite electron-hole pairs (several thousand) • Bias voltage applied to induce current • Fast read-out electronics to count the pulses (2 ms)
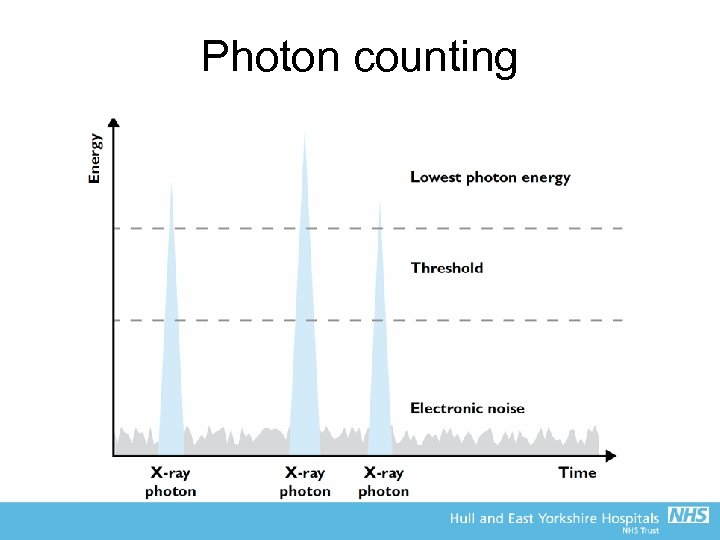 Photon counting
Photon counting
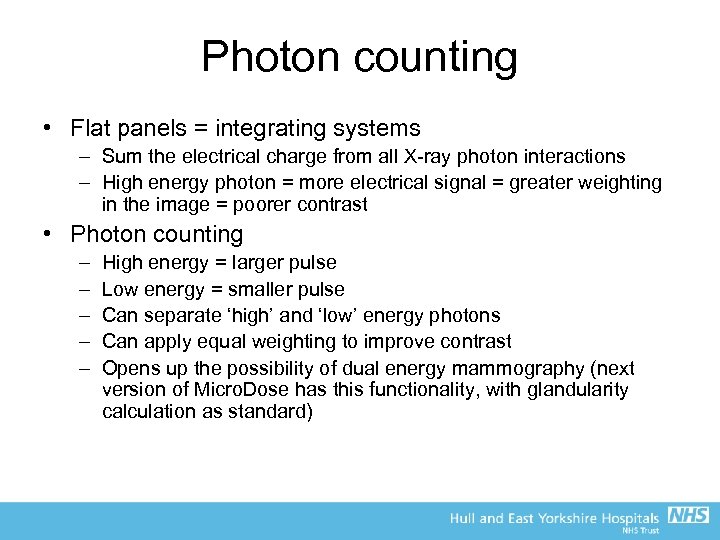 Photon counting • Flat panels = integrating systems – Sum the electrical charge from all X-ray photon interactions – High energy photon = more electrical signal = greater weighting in the image = poorer contrast • Photon counting – – – High energy = larger pulse Low energy = smaller pulse Can separate ‘high’ and ‘low’ energy photons Can apply equal weighting to improve contrast Opens up the possibility of dual energy mammography (next version of Micro. Dose has this functionality, with glandularity calculation as standard)
Photon counting • Flat panels = integrating systems – Sum the electrical charge from all X-ray photon interactions – High energy photon = more electrical signal = greater weighting in the image = poorer contrast • Photon counting – – – High energy = larger pulse Low energy = smaller pulse Can separate ‘high’ and ‘low’ energy photons Can apply equal weighting to improve contrast Opens up the possibility of dual energy mammography (next version of Micro. Dose has this functionality, with glandularity calculation as standard)
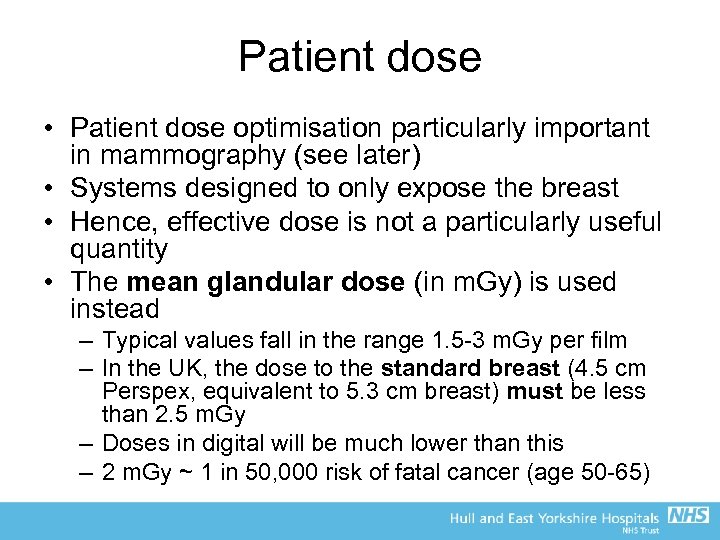 Patient dose • Patient dose optimisation particularly important in mammography (see later) • Systems designed to only expose the breast • Hence, effective dose is not a particularly useful quantity • The mean glandular dose (in m. Gy) is used instead – Typical values fall in the range 1. 5 -3 m. Gy per film – In the UK, the dose to the standard breast (4. 5 cm Perspex, equivalent to 5. 3 cm breast) must be less than 2. 5 m. Gy – Doses in digital will be much lower than this – 2 m. Gy ~ 1 in 50, 000 risk of fatal cancer (age 50 -65)
Patient dose • Patient dose optimisation particularly important in mammography (see later) • Systems designed to only expose the breast • Hence, effective dose is not a particularly useful quantity • The mean glandular dose (in m. Gy) is used instead – Typical values fall in the range 1. 5 -3 m. Gy per film – In the UK, the dose to the standard breast (4. 5 cm Perspex, equivalent to 5. 3 cm breast) must be less than 2. 5 m. Gy – Doses in digital will be much lower than this – 2 m. Gy ~ 1 in 50, 000 risk of fatal cancer (age 50 -65)
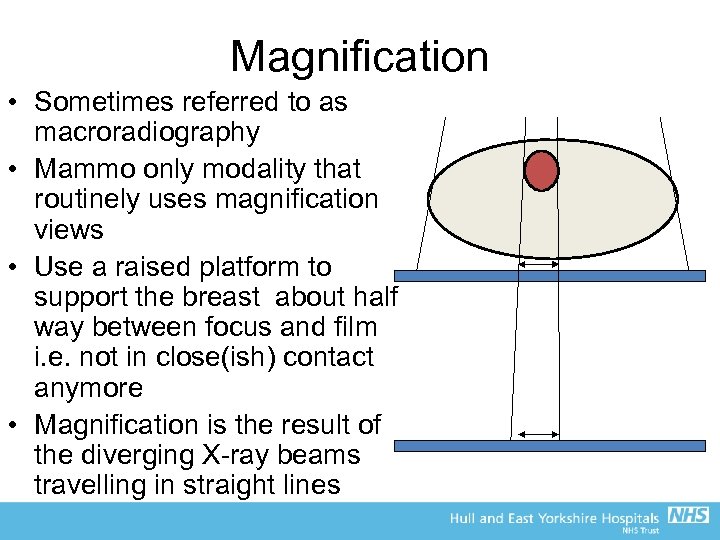 Magnification • Sometimes referred to as macroradiography • Mammo only modality that routinely uses magnification views • Use a raised platform to support the breast about half way between focus and film i. e. not in close(ish) contact anymore • Magnification is the result of the diverging X-ray beams travelling in straight lines
Magnification • Sometimes referred to as macroradiography • Mammo only modality that routinely uses magnification views • Use a raised platform to support the breast about half way between focus and film i. e. not in close(ish) contact anymore • Magnification is the result of the diverging X-ray beams travelling in straight lines
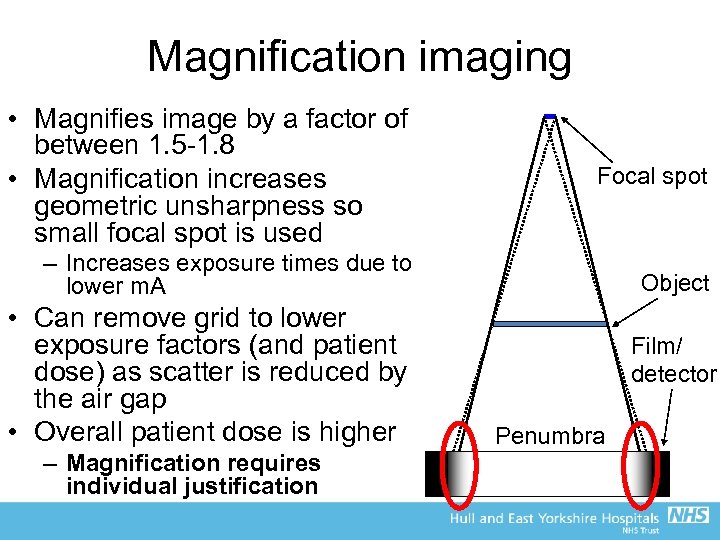 Magnification imaging • Magnifies image by a factor of between 1. 5 -1. 8 • Magnification increases geometric unsharpness so small focal spot is used Focal spot – Increases exposure times due to lower m. A Object • Can remove grid to lower exposure factors (and patient dose) as scatter is reduced by the air gap • Overall patient dose is higher – Magnification requires individual justification Film/ detector Penumbra
Magnification imaging • Magnifies image by a factor of between 1. 5 -1. 8 • Magnification increases geometric unsharpness so small focal spot is used Focal spot – Increases exposure times due to lower m. A Object • Can remove grid to lower exposure factors (and patient dose) as scatter is reduced by the air gap • Overall patient dose is higher – Magnification requires individual justification Film/ detector Penumbra
 The NHS Breast Screening Programme • Based on the Forrest Report (1986), the first breast screening programme in the world was setup in England in 1988 • All women in the age range 50 -70 invited every 3 years for mammogram – Two views of each breast – Age range recently extend to between late 40 s-73 • However, the fundamental principle of screening programme means that healthy women are exposed to radiation – What about justification?
The NHS Breast Screening Programme • Based on the Forrest Report (1986), the first breast screening programme in the world was setup in England in 1988 • All women in the age range 50 -70 invited every 3 years for mammogram – Two views of each breast – Age range recently extend to between late 40 s-73 • However, the fundamental principle of screening programme means that healthy women are exposed to radiation – What about justification?
 Justification of the NHSBSP • The vast majority of women X-rayed in the NHSBSP show no signs of cancer, and have no symptoms prior to attending – Women who display symptoms should go to their GP and be referred to the symptomatic unit at their local hospital (outside the scope of the NHSBSP, but in Hull these are the same) • On an individual basis, justification is difficult • Justification for the NHSBSP is based on the net benefit to the population, not the individual • However, this makes patient dose optmisation and quality assurance (QA) critical to effectiveness of the programme – QA also important due to the basic principles of mammography e. g. low k. V, high spatial resolution, etc
Justification of the NHSBSP • The vast majority of women X-rayed in the NHSBSP show no signs of cancer, and have no symptoms prior to attending – Women who display symptoms should go to their GP and be referred to the symptomatic unit at their local hospital (outside the scope of the NHSBSP, but in Hull these are the same) • On an individual basis, justification is difficult • Justification for the NHSBSP is based on the net benefit to the population, not the individual • However, this makes patient dose optmisation and quality assurance (QA) critical to effectiveness of the programme – QA also important due to the basic principles of mammography e. g. low k. V, high spatial resolution, etc
 QA and the NHSBSP • QA is a fundamental principle of the Breast Screening Programme • You are X-raying ‘healthy’ women, with no symptoms, so the JUSTIFICATION for the exposure (under IR(ME)R) is based on the net benefit to the population (rather than each individual), versus the risk of irradiating a large number of healthy women – This is a very current issue, given the recent publications about risk-benefit and overdiagnosis in the NHSBSP… • OPTIMISATION (under IR(ME)R) to ensure doses are ALARP is therefore incredibly important, so must make sure the X-ray equipment is fit for use!
QA and the NHSBSP • QA is a fundamental principle of the Breast Screening Programme • You are X-raying ‘healthy’ women, with no symptoms, so the JUSTIFICATION for the exposure (under IR(ME)R) is based on the net benefit to the population (rather than each individual), versus the risk of irradiating a large number of healthy women – This is a very current issue, given the recent publications about risk-benefit and overdiagnosis in the NHSBSP… • OPTIMISATION (under IR(ME)R) to ensure doses are ALARP is therefore incredibly important, so must make sure the X-ray equipment is fit for use!
 The NHSBSP and QA • The national NHSBSP is split into localities (e. g. Humberside BSP) that then belong to regions (e. g. North East, Yorkshire and Humberside) • Quality Assurance Reference Centres (QARCs) are regional bodies that ensure the local BSP is fulfilling their obligations under national guidance for the NHSBSP • Inspect whole of local BSP (including surgery, etc) • For mammography, there are national guidance documents outlining the QA required, split into daily, weekly and monthly Radiographer tests and 6 monthly Physics QA
The NHSBSP and QA • The national NHSBSP is split into localities (e. g. Humberside BSP) that then belong to regions (e. g. North East, Yorkshire and Humberside) • Quality Assurance Reference Centres (QARCs) are regional bodies that ensure the local BSP is fulfilling their obligations under national guidance for the NHSBSP • Inspect whole of local BSP (including surgery, etc) • For mammography, there are national guidance documents outlining the QA required, split into daily, weekly and monthly Radiographer tests and 6 monthly Physics QA
 Physics QA • Test/measure (6 monthly): – – – k. V accuracy X-ray tube output for all T/F and range of k. V/m. As Half-value layers AEC performance Mean glandular dose to the standard breast Image quality with phantoms Beam alignments Uniformity Focal spot sizes Compression force Etc…
Physics QA • Test/measure (6 monthly): – – – k. V accuracy X-ray tube output for all T/F and range of k. V/m. As Half-value layers AEC performance Mean glandular dose to the standard breast Image quality with phantoms Beam alignments Uniformity Focal spot sizes Compression force Etc…
 Radiographer QA… • Daily – AEC consistency (B 1) – Visual check of acquisition and reporting monitors (B 2) – Inspection of breast support table and associated equipment (B 3) • Weekly – Contrast-to-noise ratio (CNR) (B 5) – Image quality (B 6) – Artefacts and uniformity (B 7) • Monthly – – Image quality (B 6) AEC consistency with varying thickness including CNR (B 10) Mechanical safety and beam function (B 11) Compression force (B 12) • Other (weekly/before use) – Stereo-tactic localising device (B 8)
Radiographer QA… • Daily – AEC consistency (B 1) – Visual check of acquisition and reporting monitors (B 2) – Inspection of breast support table and associated equipment (B 3) • Weekly – Contrast-to-noise ratio (CNR) (B 5) – Image quality (B 6) – Artefacts and uniformity (B 7) • Monthly – – Image quality (B 6) AEC consistency with varying thickness including CNR (B 10) Mechanical safety and beam function (B 11) Compression force (B 12) • Other (weekly/before use) – Stereo-tactic localising device (B 8)
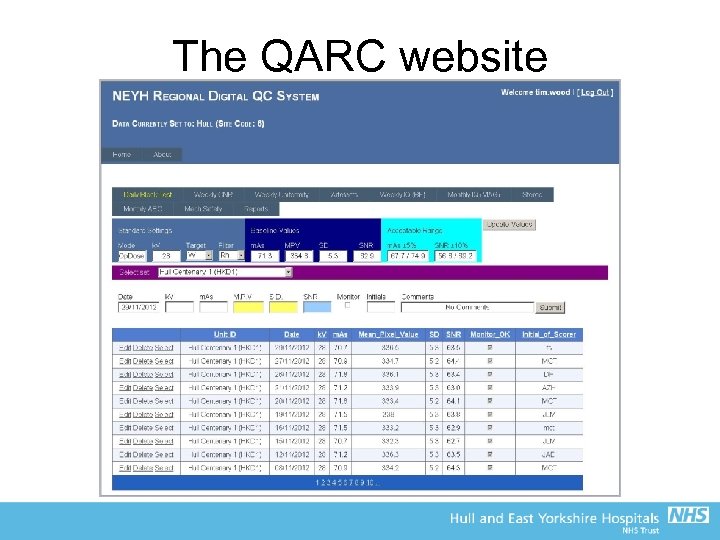 The QARC website
The QARC website
 Tomosynthesis • Digital tomosynthesis can be considered a halfway house between tomography and CT • There applications (and systems available) in general radiography, but most common implementation is in digital mammography • The basic principle is that a number of projections are acquired over a narrow range of angles, and the images are processed to give a series of ‘planes’ through the breast (strictly speaking they are not slices like in CT)
Tomosynthesis • Digital tomosynthesis can be considered a halfway house between tomography and CT • There applications (and systems available) in general radiography, but most common implementation is in digital mammography • The basic principle is that a number of projections are acquired over a narrow range of angles, and the images are processed to give a series of ‘planes’ through the breast (strictly speaking they are not slices like in CT)
 Tomosynthesis equipment
Tomosynthesis equipment
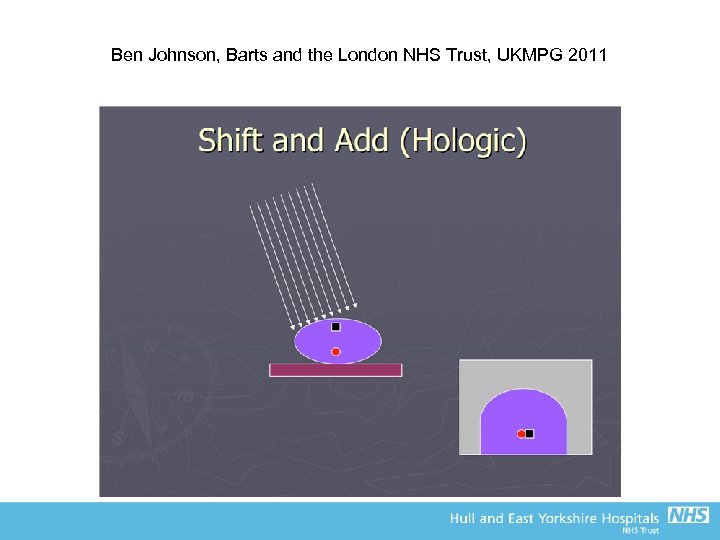
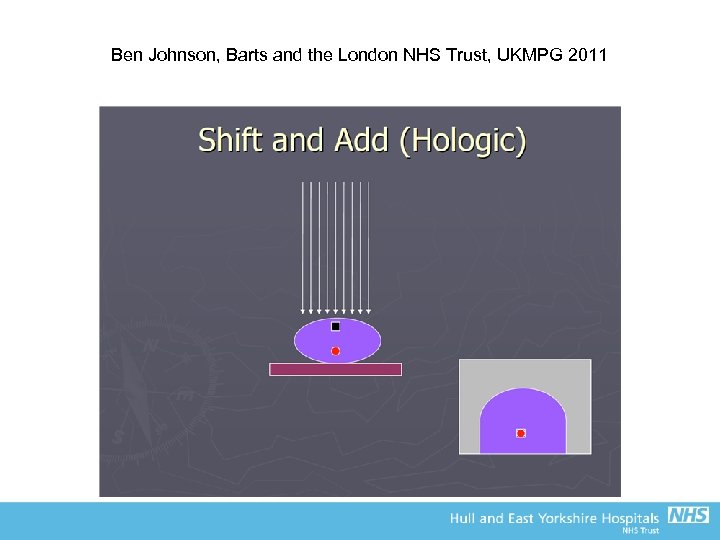
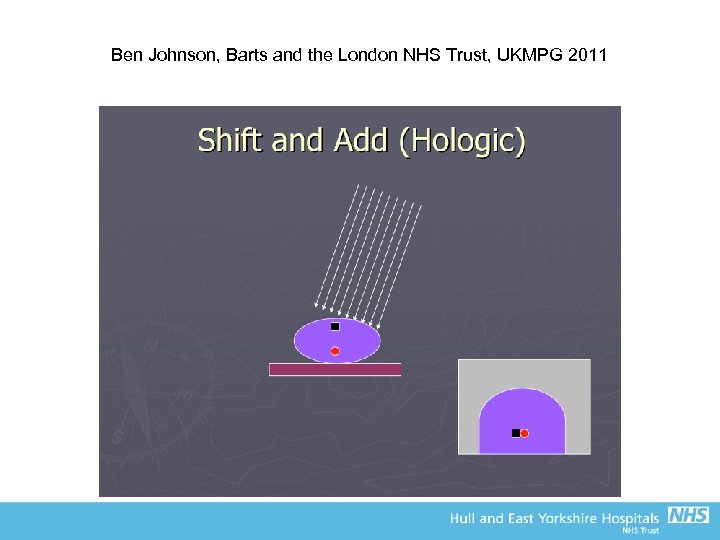
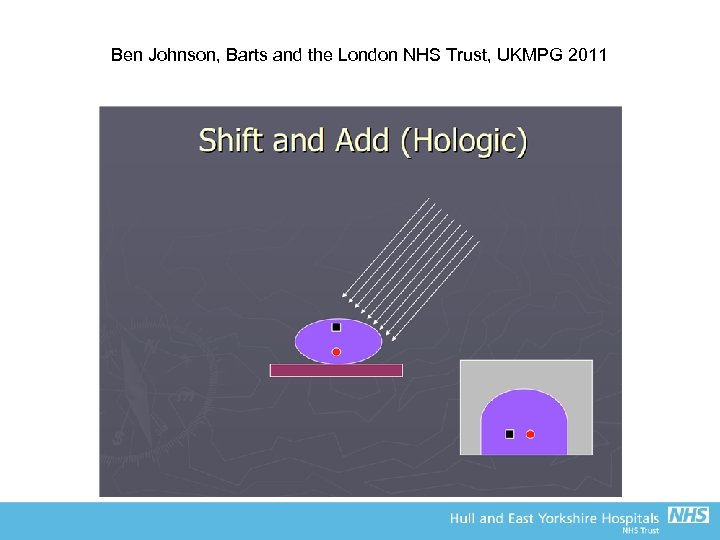
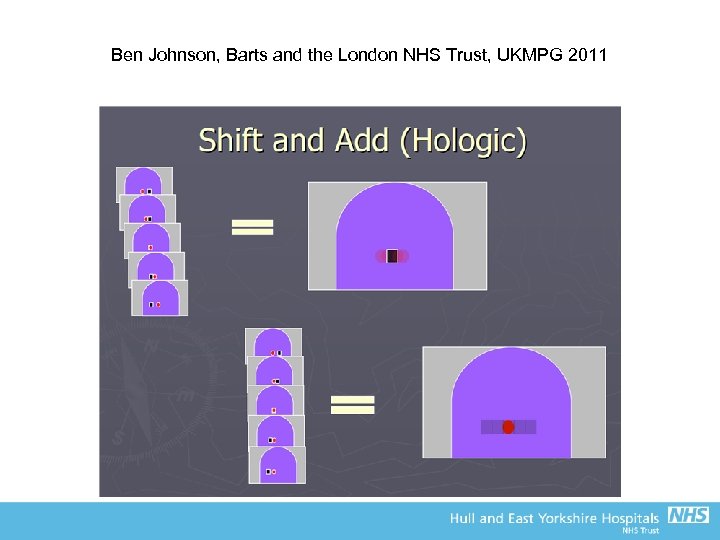
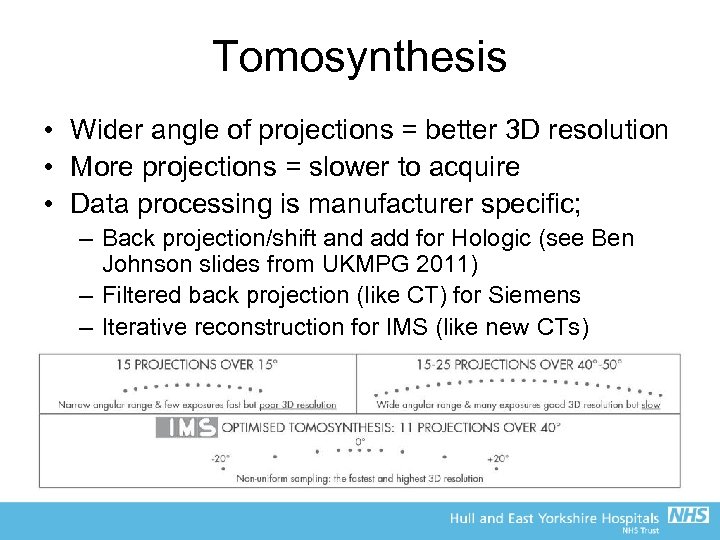 Tomosynthesis • Wider angle of projections = better 3 D resolution • More projections = slower to acquire • Data processing is manufacturer specific; – Back projection/shift and add for Hologic (see Ben Johnson slides from UKMPG 2011) – Filtered back projection (like CT) for Siemens – Iterative reconstruction for IMS (like new CTs)
Tomosynthesis • Wider angle of projections = better 3 D resolution • More projections = slower to acquire • Data processing is manufacturer specific; – Back projection/shift and add for Hologic (see Ben Johnson slides from UKMPG 2011) – Filtered back projection (like CT) for Siemens – Iterative reconstruction for IMS (like new CTs)
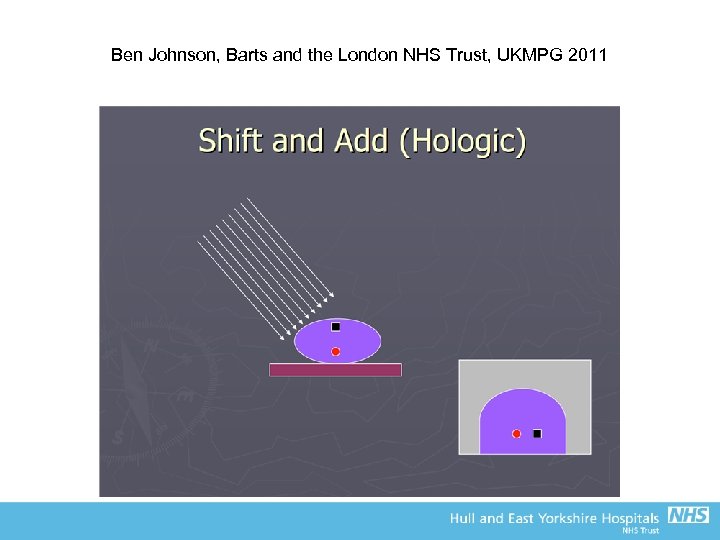 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
Ben Johnson, Barts and the London NHS Trust, UKMPG 2011
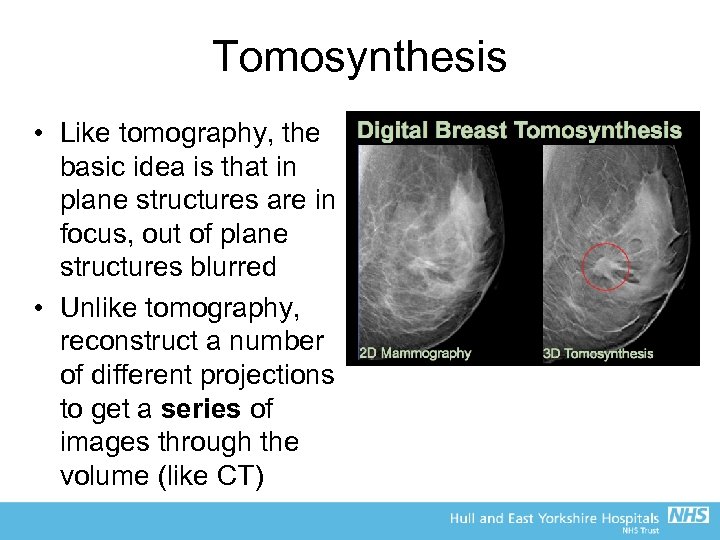 Tomosynthesis • Like tomography, the basic idea is that in plane structures are in focus, out of plane structures blurred • Unlike tomography, reconstruct a number of different projections to get a series of images through the volume (like CT)
Tomosynthesis • Like tomography, the basic idea is that in plane structures are in focus, out of plane structures blurred • Unlike tomography, reconstruct a number of different projections to get a series of images through the volume (like CT)


