c4faf54b1a6edd330b7f52909590fef9.ppt
- Количество слайдов: 186
 FOUR LECTURES 1 - Introduction in Pharmacology 2 - Introduction in Pharmacology 3 - Immunomodulators 4 - Cardiovascular concern in oral surgery
FOUR LECTURES 1 - Introduction in Pharmacology 2 - Introduction in Pharmacology 3 - Immunomodulators 4 - Cardiovascular concern in oral surgery
 REFERENCES 1 - Basic & Clinical Pharmacology Twelfth Edition Edited by Bertram G. Katzung, MD, Ph. D Associate Editors Susan B. Masters, Ph. D • 2 - Dental Management of the Medically Compromised Patient 8 TH EDITION 2013 • Copyright © 2013 by Mosby, an imprint of Elsevier Inc.
REFERENCES 1 - Basic & Clinical Pharmacology Twelfth Edition Edited by Bertram G. Katzung, MD, Ph. D Associate Editors Susan B. Masters, Ph. D • 2 - Dental Management of the Medically Compromised Patient 8 TH EDITION 2013 • Copyright © 2013 by Mosby, an imprint of Elsevier Inc.
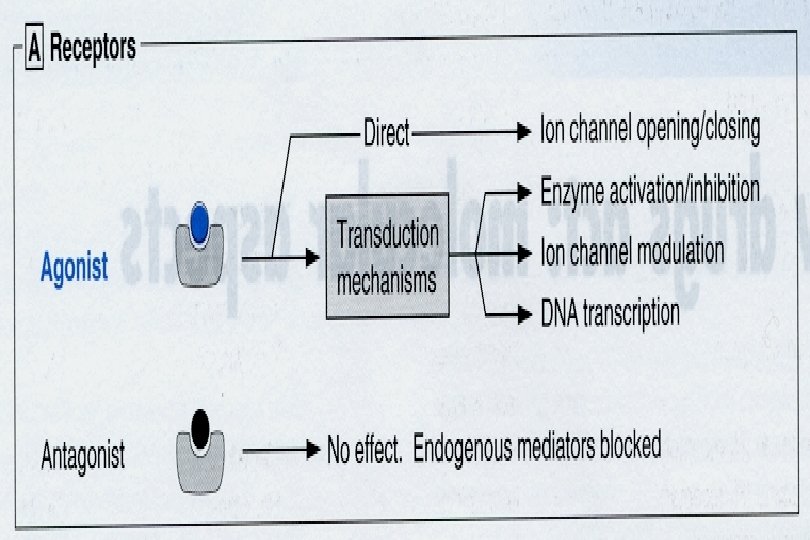
 General Principles of Pharmacology Targets for drug action * A drug is a chemical that affects physiological function in specific way * Most drugs are effective because they bind to particular target protein including receptors
General Principles of Pharmacology Targets for drug action * A drug is a chemical that affects physiological function in specific way * Most drugs are effective because they bind to particular target protein including receptors
 TEXT BOOK • PHARMACOLOGY BY • RANG & DALE (2009)
TEXT BOOK • PHARMACOLOGY BY • RANG & DALE (2009)
 TYPES OF RECEPTORS
TYPES OF RECEPTORS
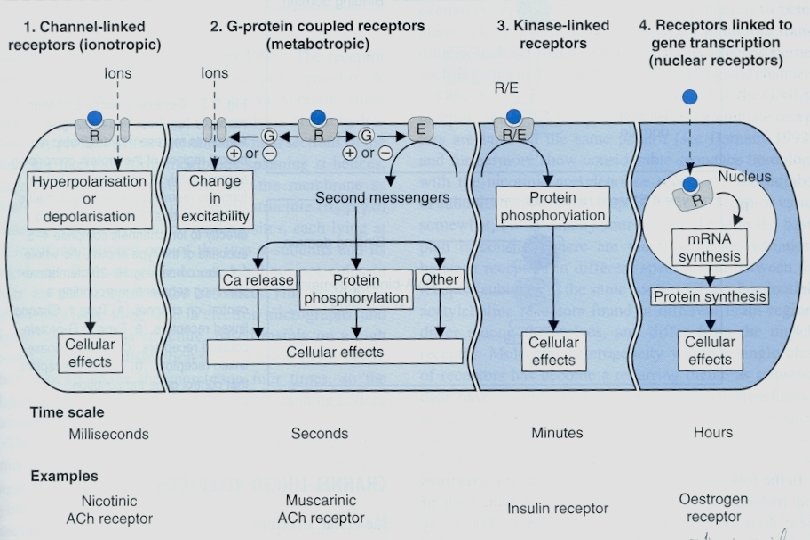
 TYPES OF RECEPTORS 1 - Channel-linked receptors - coupled directly to an ion channel such acetylcholine, GABA & Glutamate receptors 2 - G-protein-Coupled receptors - it produces second massenger as well as opening channel -stimulated by adrenergic drugs, muscarinic & hormones
TYPES OF RECEPTORS 1 - Channel-linked receptors - coupled directly to an ion channel such acetylcholine, GABA & Glutamate receptors 2 - G-protein-Coupled receptors - it produces second massenger as well as opening channel -stimulated by adrenergic drugs, muscarinic & hormones
 Continue TYPES OF RECEPTORS 3 - Kinase-linked receptors - insulin & growth hormone receptors - this type also linked to guanylate cyclase *** ALL PREVIOUS TYPES OF RECEPTORS ARE MEMBRANE BOUND 4 - Receptors that regulate gene transcription * They are soluble receptor usualy inside the cell (cytosol or intranuclear protein) * Steroid , thyroid, retinoic acid & vit D
Continue TYPES OF RECEPTORS 3 - Kinase-linked receptors - insulin & growth hormone receptors - this type also linked to guanylate cyclase *** ALL PREVIOUS TYPES OF RECEPTORS ARE MEMBRANE BOUND 4 - Receptors that regulate gene transcription * They are soluble receptor usualy inside the cell (cytosol or intranuclear protein) * Steroid , thyroid, retinoic acid & vit D
 Drug Specificity * Drug binds only to certain targets * Individual targets recognise only certain class of drug * There are no drugs completely specific in action * Increase the dose will affect other targets in cell
Drug Specificity * Drug binds only to certain targets * Individual targets recognise only certain class of drug * There are no drugs completely specific in action * Increase the dose will affect other targets in cell
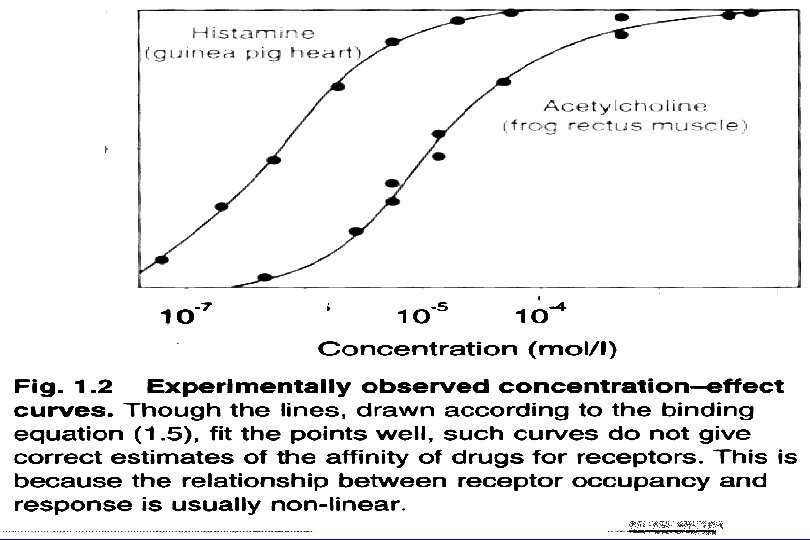
 Binding of Drugs to Receptors * Binding of drugs to receptors obeys the law of mass action (the rate of chemical reaction is proportional to the product concentrations of reactants) *At equilibrium, receptor occupancy is related to drug concentration * The higher the affinity of drug for receptor, the lower the concentration needed for occupancy
Binding of Drugs to Receptors * Binding of drugs to receptors obeys the law of mass action (the rate of chemical reaction is proportional to the product concentrations of reactants) *At equilibrium, receptor occupancy is related to drug concentration * The higher the affinity of drug for receptor, the lower the concentration needed for occupancy
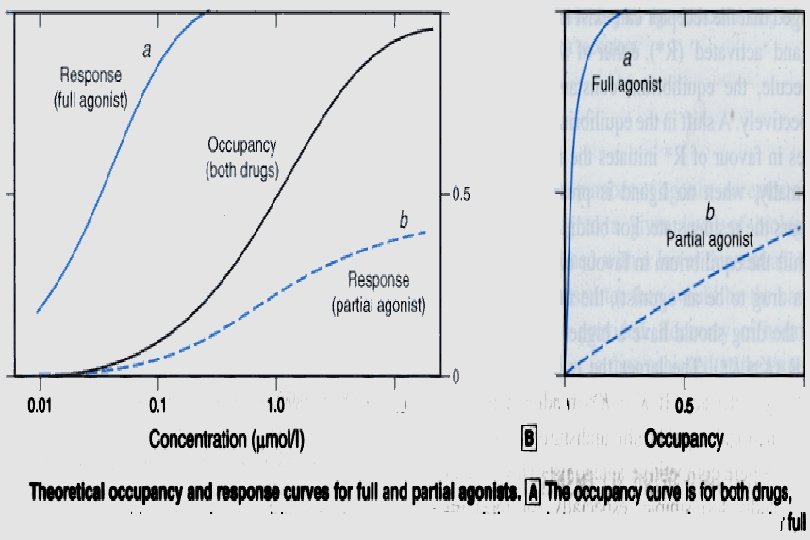
 Agonist & antagonist(blocker) * drug acting on receptor may be agonist or antagonist A- Agonist initiates changes in cell function * Full agonist: has high efficacy * Partial agonist - it produces submaximal effects - it has intermediate efficacy * Partial agonist: What is is the efficacy ? It is the ability of drug to initiate biochemical changes leads to the effect of drug
Agonist & antagonist(blocker) * drug acting on receptor may be agonist or antagonist A- Agonist initiates changes in cell function * Full agonist: has high efficacy * Partial agonist - it produces submaximal effects - it has intermediate efficacy * Partial agonist: What is is the efficacy ? It is the ability of drug to initiate biochemical changes leads to the effect of drug
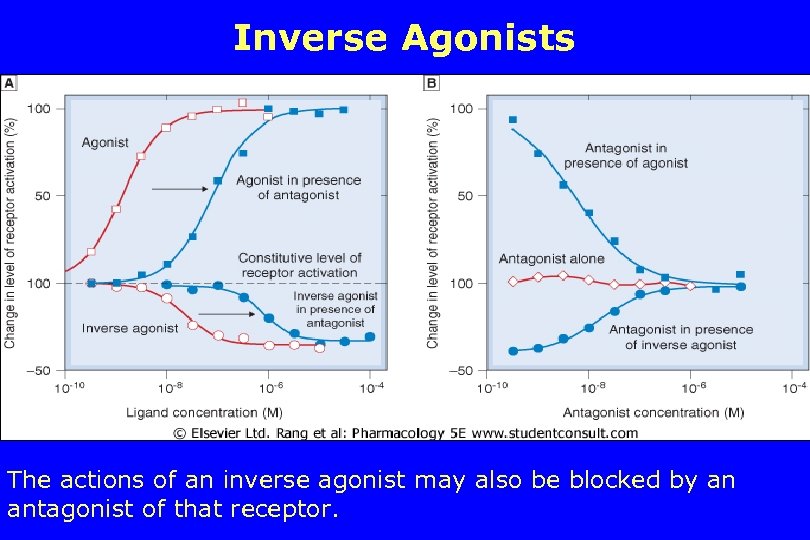 Inverse Agonists The actions of an inverse agonist may also be blocked by an antagonist of that receptor.
Inverse Agonists The actions of an inverse agonist may also be blocked by an antagonist of that receptor.
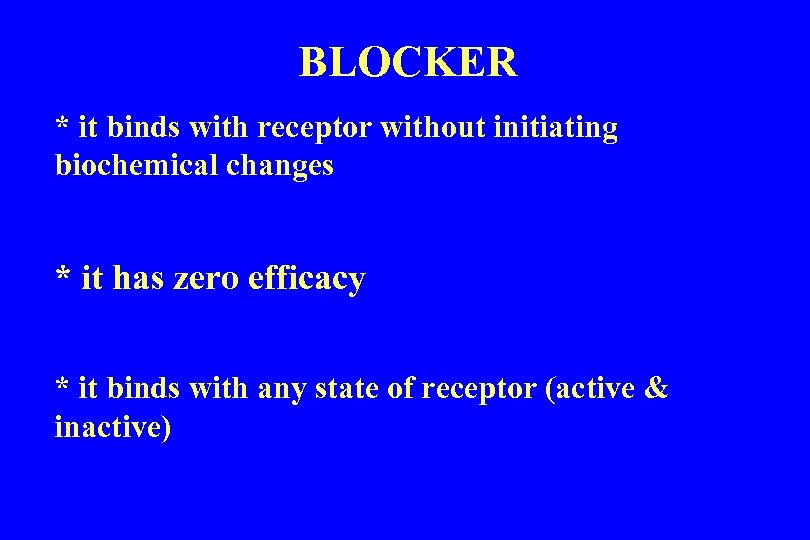 BLOCKER * it binds with receptor without initiating biochemical changes * it has zero efficacy * it binds with any state of receptor (active & inactive)
BLOCKER * it binds with receptor without initiating biochemical changes * it has zero efficacy * it binds with any state of receptor (active & inactive)
 Types Drug Antagonist A- Chemical antagonist B- Pharmacokinetic antagonist * one drug affecting other drug via: - Absorption - Metabolism - Excretion C- Competitive antagonism(BLOCKER) * Reversible & * Irreversible
Types Drug Antagonist A- Chemical antagonist B- Pharmacokinetic antagonist * one drug affecting other drug via: - Absorption - Metabolism - Excretion C- Competitive antagonism(BLOCKER) * Reversible & * Irreversible
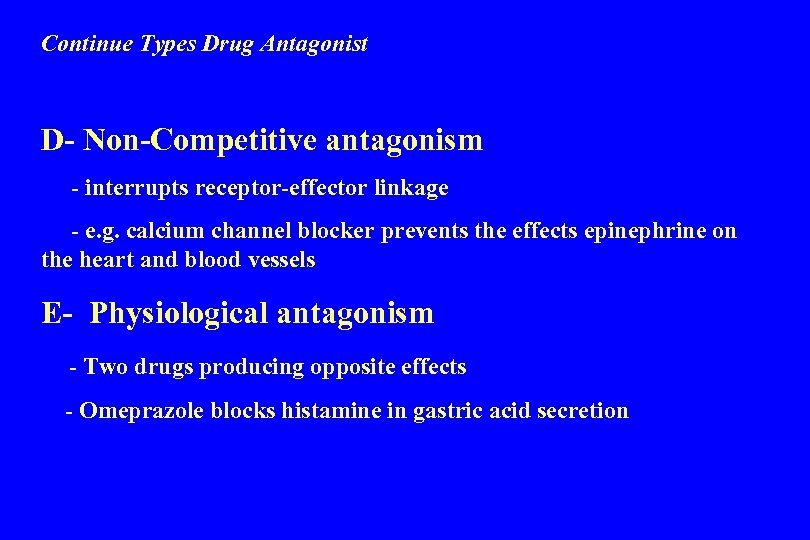 Continue Types Drug Antagonist D- Non-Competitive antagonism - interrupts receptor-effector linkage - e. g. calcium channel blocker prevents the effects epinephrine on the heart and blood vessels E- Physiological antagonism - Two drugs producing opposite effects - Omeprazole blocks histamine in gastric acid secretion
Continue Types Drug Antagonist D- Non-Competitive antagonism - interrupts receptor-effector linkage - e. g. calcium channel blocker prevents the effects epinephrine on the heart and blood vessels E- Physiological antagonism - Two drugs producing opposite effects - Omeprazole blocks histamine in gastric acid secretion
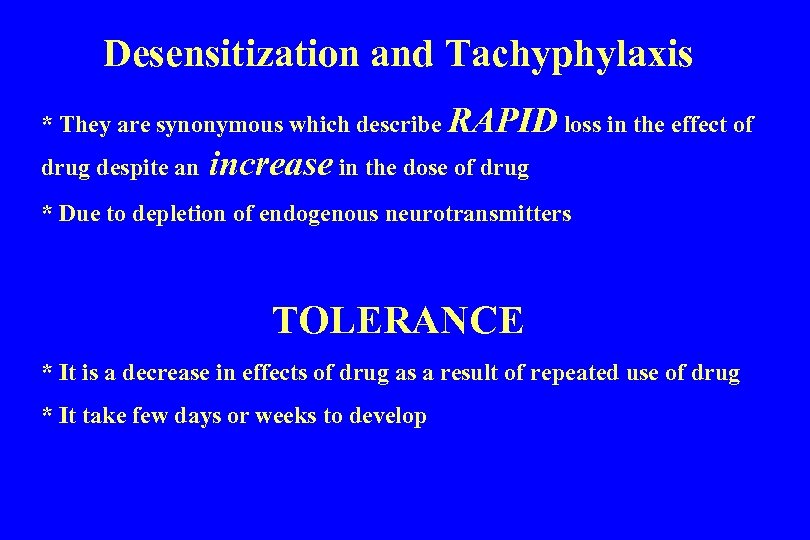 Desensitization and Tachyphylaxis * They are synonymous which describe RAPID loss in the effect of drug despite an increase in the dose of drug * Due to depletion of endogenous neurotransmitters TOLERANCE * It is a decrease in effects of drug as a result of repeated use of drug * It take few days or weeks to develop
Desensitization and Tachyphylaxis * They are synonymous which describe RAPID loss in the effect of drug despite an increase in the dose of drug * Due to depletion of endogenous neurotransmitters TOLERANCE * It is a decrease in effects of drug as a result of repeated use of drug * It take few days or weeks to develop
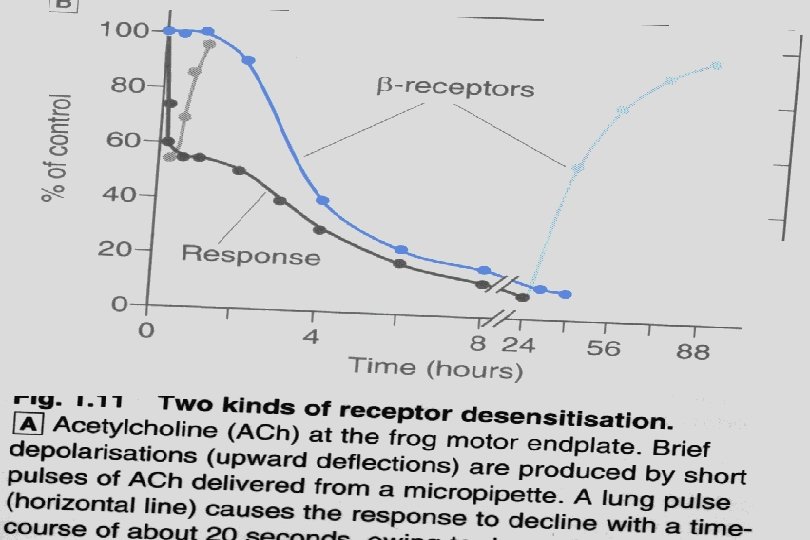
 Mechanism of Tolerance, Tachyphylaxis & desensitisation etc. . 1 - Change in Receptors - (agonist failure to induce biochemical changes) 2 - Loss of Receptors 3 - Exhaustion of mediators (depletion) 4 - increased metabolic degradation 5 - Physiological adaptation (kidney & antihypertensive) 6 - Active extrusion of drug from cells
Mechanism of Tolerance, Tachyphylaxis & desensitisation etc. . 1 - Change in Receptors - (agonist failure to induce biochemical changes) 2 - Loss of Receptors 3 - Exhaustion of mediators (depletion) 4 - increased metabolic degradation 5 - Physiological adaptation (kidney & antihypertensive) 6 - Active extrusion of drug from cells
 DOSE RESPONSE RELATIONSHIP It is a relationship between the drug amount (concentration) and pharmacological effects • Types of responses a- Graded response - response increases by increase the dose b- All or none response such as anti-convulsant.
DOSE RESPONSE RELATIONSHIP It is a relationship between the drug amount (concentration) and pharmacological effects • Types of responses a- Graded response - response increases by increase the dose b- All or none response such as anti-convulsant.
 Therapeutic index * it is a measure of drug safety * How to calculate ? - LD 50/ED 50 Potency of drug * It is the minimum dose required to cause maximum response * Potency of drug is not important clinically
Therapeutic index * it is a measure of drug safety * How to calculate ? - LD 50/ED 50 Potency of drug * It is the minimum dose required to cause maximum response * Potency of drug is not important clinically
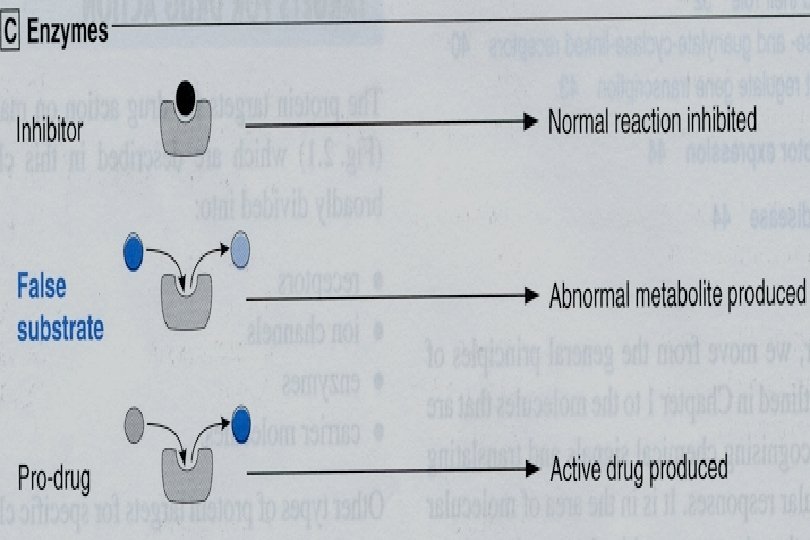
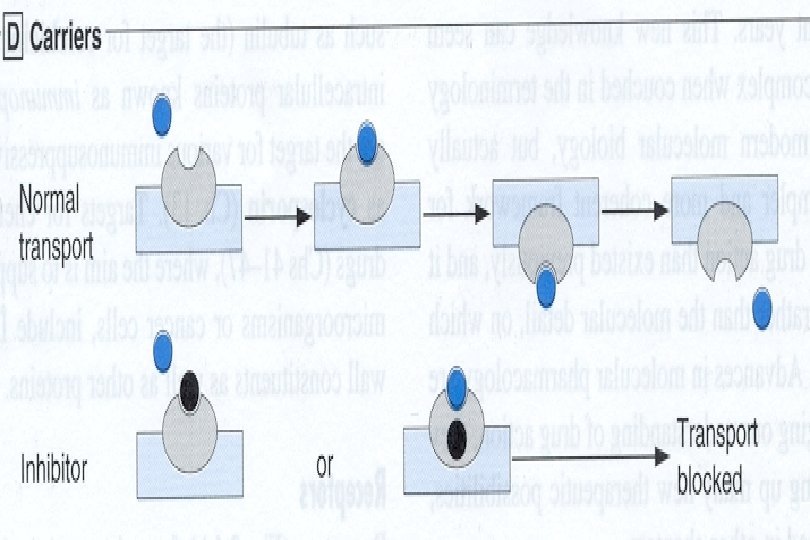
 HOW DRUGS MEDIATE THEIR ACTIONS ? * Via interacting with its target(s) leading to: 1 - activation or blocking of receptors 2 - block endogenous mediators (counterfeit) SUCH ALDOMET(ALPHA-METHYLDOPA} 3 -open or close ionic channels (Benzodiazepine &L. A. ) 4 - compete with uptake system (carrier) - imipramine, cocaine, proton pump inhibitor, digoxin, probenecid
HOW DRUGS MEDIATE THEIR ACTIONS ? * Via interacting with its target(s) leading to: 1 - activation or blocking of receptors 2 - block endogenous mediators (counterfeit) SUCH ALDOMET(ALPHA-METHYLDOPA} 3 -open or close ionic channels (Benzodiazepine &L. A. ) 4 - compete with uptake system (carrier) - imipramine, cocaine, proton pump inhibitor, digoxin, probenecid
 Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 5 - Enzymes (dihydrofolate reductase targeted by methotrexate & trimethoprim, cyclooxygenase, xanthine oxidase, MAO, Dopa decarboxylase, ACE etc…. . ) 6 - Other targets such as * Immunophilins in lymphocyte targeted by immunosuppresants such as Cyclosporin & Tacrolimus * Tubulin of phagocytes and other cells including cancerous cells - Targeted by Colchicine, Vincristine & Taxol
Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 5 - Enzymes (dihydrofolate reductase targeted by methotrexate & trimethoprim, cyclooxygenase, xanthine oxidase, MAO, Dopa decarboxylase, ACE etc…. . ) 6 - Other targets such as * Immunophilins in lymphocyte targeted by immunosuppresants such as Cyclosporin & Tacrolimus * Tubulin of phagocytes and other cells including cancerous cells - Targeted by Colchicine, Vincristine & Taxol
 Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 7 - Physical means - Osmotic diuretics - inhalational anesthesia 8 - Chelating agent * reacts with DNA or ions
Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 7 - Physical means - Osmotic diuretics - inhalational anesthesia 8 - Chelating agent * reacts with DNA or ions

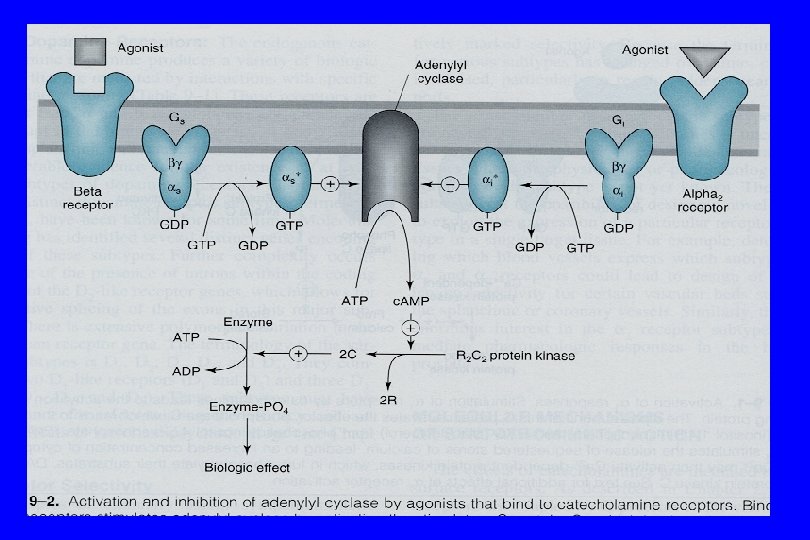
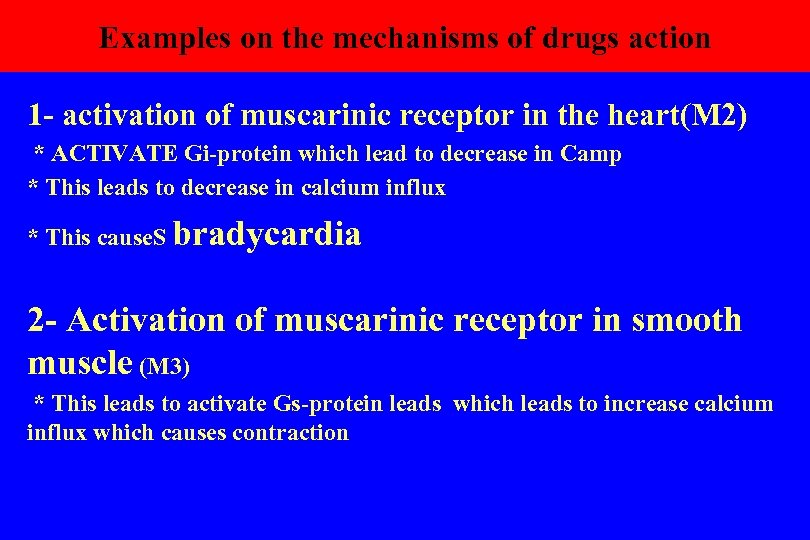 Examples on the mechanisms of drugs action 1 - activation of muscarinic receptor in the heart(M 2) * ACTIVATE Gi-protein which lead to decrease in Camp * This leads to decrease in calcium influx * This cause. S bradycardia 2 - Activation of muscarinic receptor in smooth muscle (M 3) * This leads to activate Gs-protein leads which leads to increase calcium influx which causes contraction
Examples on the mechanisms of drugs action 1 - activation of muscarinic receptor in the heart(M 2) * ACTIVATE Gi-protein which lead to decrease in Camp * This leads to decrease in calcium influx * This cause. S bradycardia 2 - Activation of muscarinic receptor in smooth muscle (M 3) * This leads to activate Gs-protein leads which leads to increase calcium influx which causes contraction
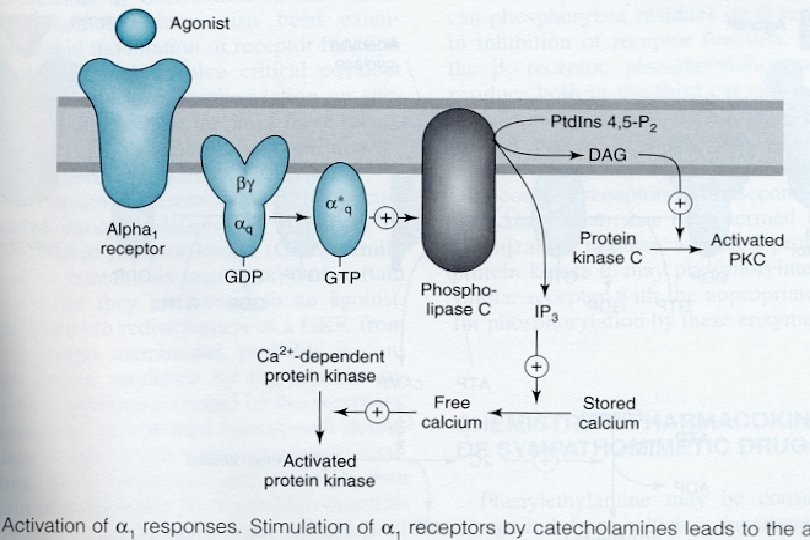
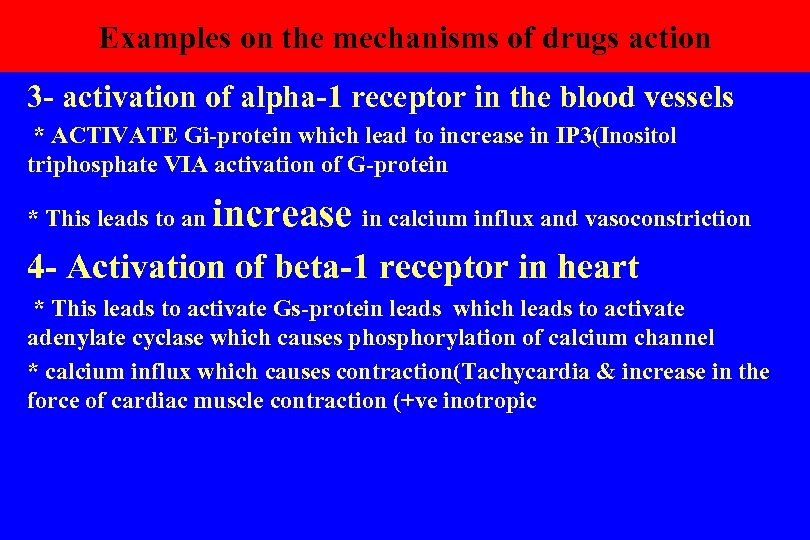 Examples on the mechanisms of drugs action 3 - activation of alpha-1 receptor in the blood vessels * ACTIVATE Gi-protein which lead to increase in IP 3(Inositol triphosphate VIA activation of G-protein * This leads to an increase in calcium influx and vasoconstriction 4 - Activation of beta-1 receptor in heart * This leads to activate Gs-protein leads which leads to activate adenylate cyclase which causes phosphorylation of calcium channel * calcium influx which causes contraction(Tachycardia & increase in the force of cardiac muscle contraction (+ve inotropic
Examples on the mechanisms of drugs action 3 - activation of alpha-1 receptor in the blood vessels * ACTIVATE Gi-protein which lead to increase in IP 3(Inositol triphosphate VIA activation of G-protein * This leads to an increase in calcium influx and vasoconstriction 4 - Activation of beta-1 receptor in heart * This leads to activate Gs-protein leads which leads to activate adenylate cyclase which causes phosphorylation of calcium channel * calcium influx which causes contraction(Tachycardia & increase in the force of cardiac muscle contraction (+ve inotropic
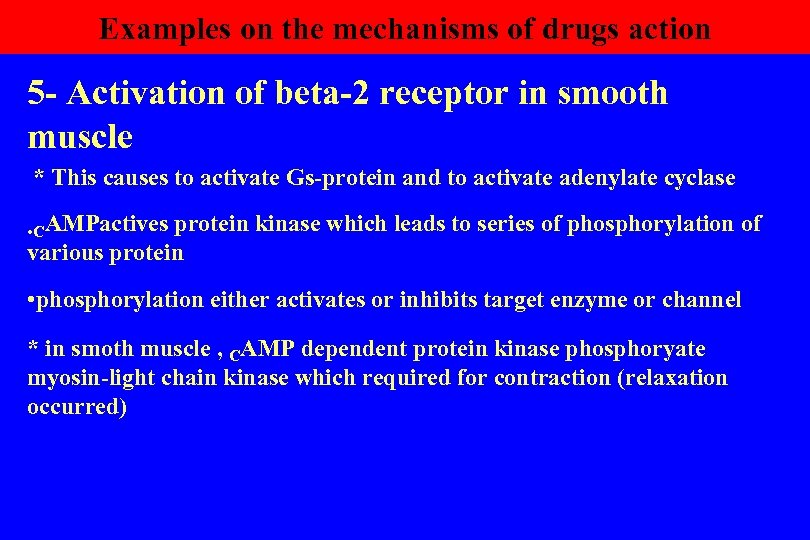 Examples on the mechanisms of drugs action 5 - Activation of beta-2 receptor in smooth muscle * This causes to activate Gs-protein and to activate adenylate cyclase • CAMPactives protein kinase which leads to series of phosphorylation of various protein • phosphorylation either activates or inhibits target enzyme or channel * in smoth muscle , CAMP dependent protein kinase phosphoryate myosin-light chain kinase which required for contraction (relaxation occurred)
Examples on the mechanisms of drugs action 5 - Activation of beta-2 receptor in smooth muscle * This causes to activate Gs-protein and to activate adenylate cyclase • CAMPactives protein kinase which leads to series of phosphorylation of various protein • phosphorylation either activates or inhibits target enzyme or channel * in smoth muscle , CAMP dependent protein kinase phosphoryate myosin-light chain kinase which required for contraction (relaxation occurred)
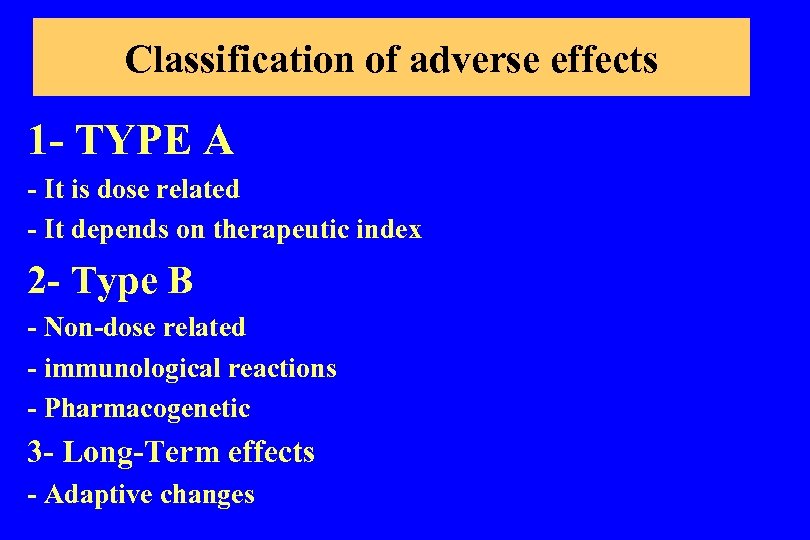 Classification of adverse effects 1 - TYPE A - It is dose related - It depends on therapeutic index 2 - Type B - Non-dose related - immunological reactions - Pharmacogenetic 3 - Long-Term effects - Adaptive changes
Classification of adverse effects 1 - TYPE A - It is dose related - It depends on therapeutic index 2 - Type B - Non-dose related - immunological reactions - Pharmacogenetic 3 - Long-Term effects - Adaptive changes
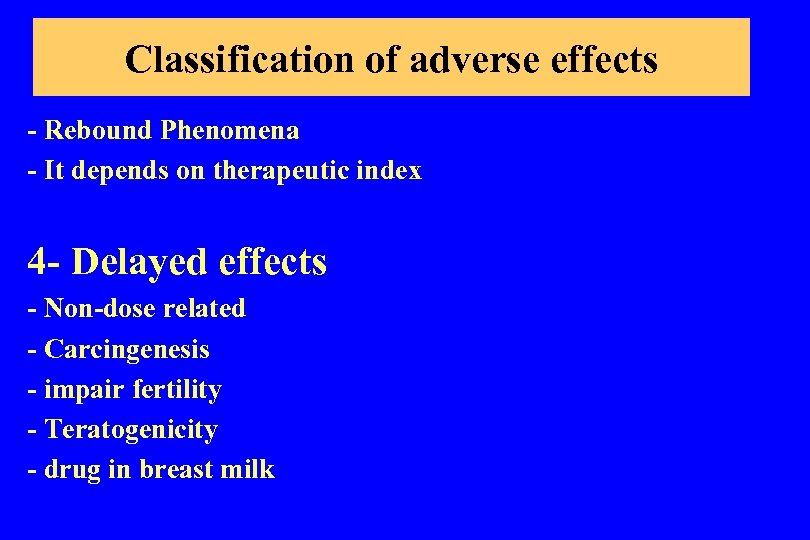 Classification of adverse effects - Rebound Phenomena - It depends on therapeutic index 4 - Delayed effects - Non-dose related - Carcingenesis - impair fertility - Teratogenicity - drug in breast milk
Classification of adverse effects - Rebound Phenomena - It depends on therapeutic index 4 - Delayed effects - Non-dose related - Carcingenesis - impair fertility - Teratogenicity - drug in breast milk
 Pharmacokinetic of drugs 1 - ABSORPTION OF DRUG - From the site of administration 2 - Distribution - To reach the site of action 3 - metabolism - to inactivate or activate 4 - Excretion
Pharmacokinetic of drugs 1 - ABSORPTION OF DRUG - From the site of administration 2 - Distribution - To reach the site of action 3 - metabolism - to inactivate or activate 4 - Excretion
 ROUTE OF DRUG ADMINISTRATION 1 - Oral administration (P. O. ) 2 - Subcutaneous (S. C. ) 3 - Intradermal 4 - Intramuscular (I. M. ) 5 - Intravenous (I. V. ) 6 - Sublingual 7 - Rectal
ROUTE OF DRUG ADMINISTRATION 1 - Oral administration (P. O. ) 2 - Subcutaneous (S. C. ) 3 - Intradermal 4 - Intramuscular (I. M. ) 5 - Intravenous (I. V. ) 6 - Sublingual 7 - Rectal
 ROUTE OF DRUG ADMINISTRATION 8 - Intrathecal & epidural 9 - Inhalation 10 - Topical * skin * eye * mucous membrane -nasal, vaginal, oropharynx
ROUTE OF DRUG ADMINISTRATION 8 - Intrathecal & epidural 9 - Inhalation 10 - Topical * skin * eye * mucous membrane -nasal, vaginal, oropharynx
 ORAL ADMINISTRATION 1 - PROS • Convenient • Safe ? • Economical (does not need sterilization) 2 - CONS • Requires patient compliance • Drugs irritant to stomach • Drugs not stable in GIT • Drugs extensively metabolize by the liver • Drugs NOT absorb from GIT • Leads to food drug interaction
ORAL ADMINISTRATION 1 - PROS • Convenient • Safe ? • Economical (does not need sterilization) 2 - CONS • Requires patient compliance • Drugs irritant to stomach • Drugs not stable in GIT • Drugs extensively metabolize by the liver • Drugs NOT absorb from GIT • Leads to food drug interaction
 INTRAVENOUS ADMINISTRATION 1 - PROS • Rapid action • Delivered the desired amount • irritant drug can be given only I. V. but NOT S. C. 2 - CONS • Increase the risk of adverse effects • Must inject slowly in order to minimize the effects of drug on the heart • It needs constant monitoring the reponse of patient
INTRAVENOUS ADMINISTRATION 1 - PROS • Rapid action • Delivered the desired amount • irritant drug can be given only I. V. but NOT S. C. 2 - CONS • Increase the risk of adverse effects • Must inject slowly in order to minimize the effects of drug on the heart • It needs constant monitoring the reponse of patient
 SUBCUTANEOUS ADMINISTRATION 1 - PROS • It provides sustain effects because of slow absorption • Addition of vasoconstrictor decreases further the rate of absorption from the site of injection • It is suitable for insoluble drugs such as pellets and suspension 2 - CONS • can not inject large volume • can not inject irritant drug • repeated injection leads to necrosis (atrophy of skin)
SUBCUTANEOUS ADMINISTRATION 1 - PROS • It provides sustain effects because of slow absorption • Addition of vasoconstrictor decreases further the rate of absorption from the site of injection • It is suitable for insoluble drugs such as pellets and suspension 2 - CONS • can not inject large volume • can not inject irritant drug • repeated injection leads to necrosis (atrophy of skin)
 INTRAMUSCULAR ADMINISTRATION 1 - PROS • Suitable for oily vehicle and irritant drug • The rate of absorption is very high because of high blood flow in the muscle 2 - CONS • It is not recommended in patient taking Anti-coagulant • Increase CPK
INTRAMUSCULAR ADMINISTRATION 1 - PROS • Suitable for oily vehicle and irritant drug • The rate of absorption is very high because of high blood flow in the muscle 2 - CONS • It is not recommended in patient taking Anti-coagulant • Increase CPK
 PULMONARY ADMINISTRATION 1 - PROS • Rapid absorption • Local administration into the lung is beneficial in bronchial asthma • Avoid hepatic effects • Can absorb fine droplets (aerosol), prticle size, gaseous and volatile drugs 2 - CONS • Difficult to regulate & administered the dose • some drugs cause lung irritation
PULMONARY ADMINISTRATION 1 - PROS • Rapid absorption • Local administration into the lung is beneficial in bronchial asthma • Avoid hepatic effects • Can absorb fine droplets (aerosol), prticle size, gaseous and volatile drugs 2 - CONS • Difficult to regulate & administered the dose • some drugs cause lung irritation
 TOPICAL ADMINISTRATION 1 - Mucous membrane • Rapid absorption such as local anesthetic & ADH 2 - Skin Lipophilic drugs absorb rapidly from skin such as nitroglycerin skin batch, scopolamine(MUSCARINIC BLOCKER) batch • Inflammed, burned, abraded skin absorb drug faster
TOPICAL ADMINISTRATION 1 - Mucous membrane • Rapid absorption such as local anesthetic & ADH 2 - Skin Lipophilic drugs absorb rapidly from skin such as nitroglycerin skin batch, scopolamine(MUSCARINIC BLOCKER) batch • Inflammed, burned, abraded skin absorb drug faster
 TOPICAL ADMINISTRATION 3 - Ophthalmic absorption • it is used for local effectss • systemic absorption occurs through NASOLACRIMAL CANAL such as β-adrenergic blockers eye drops • Ointment and suspension minimized systemic absorption • Ocular insert provides continous delivery of drug with minimum systemic absorption
TOPICAL ADMINISTRATION 3 - Ophthalmic absorption • it is used for local effectss • systemic absorption occurs through NASOLACRIMAL CANAL such as β-adrenergic blockers eye drops • Ointment and suspension minimized systemic absorption • Ocular insert provides continous delivery of drug with minimum systemic absorption
 SUBLINGUAL ADMINISTRATION • Excellent absorption for non-ionized drug Example Nitroglycerin, apomorphine (Uprima) • It has high absorption rate close to intravenous injection • Avoid hepatic first pass metabolism
SUBLINGUAL ADMINISTRATION • Excellent absorption for non-ionized drug Example Nitroglycerin, apomorphine (Uprima) • It has high absorption rate close to intravenous injection • Avoid hepatic first pass metabolism
 RECTAL ABSORPTION • It is used when oral route is warranted such as vomiting or coma • It has erratic, irregular and incomplete absorption (50%) • It goes in partial hepatic first pass metabolism • Some drugs may cause rectal irritation
RECTAL ABSORPTION • It is used when oral route is warranted such as vomiting or coma • It has erratic, irregular and incomplete absorption (50%) • It goes in partial hepatic first pass metabolism • Some drugs may cause rectal irritation
 DRUGS DISTRIBUTION Factors influence drug distribution 1 - Permeability of drug to biological membranes • Blood brain barrier • Testicular barrier • Placental barrier - LIPID SOLUBLE DRUGS -They have large Vd (volume of distribution) 2 - Extent of plasma protein - Highly protein bound stay in circulation & also have large Vd
DRUGS DISTRIBUTION Factors influence drug distribution 1 - Permeability of drug to biological membranes • Blood brain barrier • Testicular barrier • Placental barrier - LIPID SOLUBLE DRUGS -They have large Vd (volume of distribution) 2 - Extent of plasma protein - Highly protein bound stay in circulation & also have large Vd
 DRUGS DISTRIBUTION Factors influence drug distribution -Drugs with large Vd have the following properties • High protein binding • High lipid solubility • High affinity to other tissues such as bone & liver
DRUGS DISTRIBUTION Factors influence drug distribution -Drugs with large Vd have the following properties • High protein binding • High lipid solubility • High affinity to other tissues such as bone & liver
 DRUGS DISTRIBUTION Factors influence drug distribution 3 - Availability of transport mechanism - passive diffusion: The drug must be in unionized form - Active transport: require ATP - Facilitative diffusion: it requires carrier but without energy such vit B 12, glucose and amino acid - ion pair transport: the ionic compound combines reversibly with endogenous compound such as MUCIN in GIT 4 - Regional p. H - breast milk more acidic than blood: Weak base drugs accumulate in breast milk
DRUGS DISTRIBUTION Factors influence drug distribution 3 - Availability of transport mechanism - passive diffusion: The drug must be in unionized form - Active transport: require ATP - Facilitative diffusion: it requires carrier but without energy such vit B 12, glucose and amino acid - ion pair transport: the ionic compound combines reversibly with endogenous compound such as MUCIN in GIT 4 - Regional p. H - breast milk more acidic than blood: Weak base drugs accumulate in breast milk
 DRUGS DISTRIBUTION Factors influence drug distribution 4 - Rate of blood flow to tissues - Skeletal muscles have high blood flow 5 - Tissues mass
DRUGS DISTRIBUTION Factors influence drug distribution 4 - Rate of blood flow to tissues - Skeletal muscles have high blood flow 5 - Tissues mass
 DRUG METABOLISM OBJECTIVES OF METABOLISM 1 - To make the drug more water soluble in order to facilitate its excretion 2 - To activate or inactivate the drug * Some drugs become highly toxic or carcinogenic
DRUG METABOLISM OBJECTIVES OF METABOLISM 1 - To make the drug more water soluble in order to facilitate its excretion 2 - To activate or inactivate the drug * Some drugs become highly toxic or carcinogenic
 Factors influence Metabolism 1 - Drugs - inducer: rifampicin, dilantin, barbiturate - inhibitors: cimetidine, macrolide & antifungal drugs 2 - Liver diseases 3 - Diet - grape fruit, vitamins deficeincy such vit B 6 is cofactor for decarboxylation
Factors influence Metabolism 1 - Drugs - inducer: rifampicin, dilantin, barbiturate - inhibitors: cimetidine, macrolide & antifungal drugs 2 - Liver diseases 3 - Diet - grape fruit, vitamins deficeincy such vit B 6 is cofactor for decarboxylation
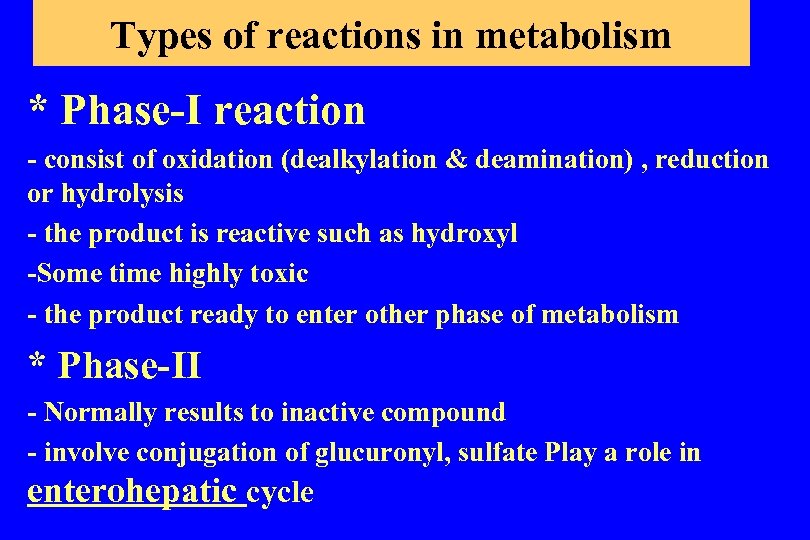 Types of reactions in metabolism * Phase-I reaction - consist of oxidation (dealkylation & deamination) , reduction or hydrolysis - the product is reactive such as hydroxyl -Some time highly toxic - the product ready to enter other phase of metabolism * Phase-II - Normally results to inactive compound - involve conjugation of glucuronyl, sulfate Play a role in enterohepatic cycle
Types of reactions in metabolism * Phase-I reaction - consist of oxidation (dealkylation & deamination) , reduction or hydrolysis - the product is reactive such as hydroxyl -Some time highly toxic - the product ready to enter other phase of metabolism * Phase-II - Normally results to inactive compound - involve conjugation of glucuronyl, sulfate Play a role in enterohepatic cycle
 EXCRETION OF DRUGS 1 - TYPES OF EXCRETION • Renal excretion • Biliary excretion • Pulmonary excretion • Excretion via other body fluids - Saliva -Breast milk
EXCRETION OF DRUGS 1 - TYPES OF EXCRETION • Renal excretion • Biliary excretion • Pulmonary excretion • Excretion via other body fluids - Saliva -Breast milk
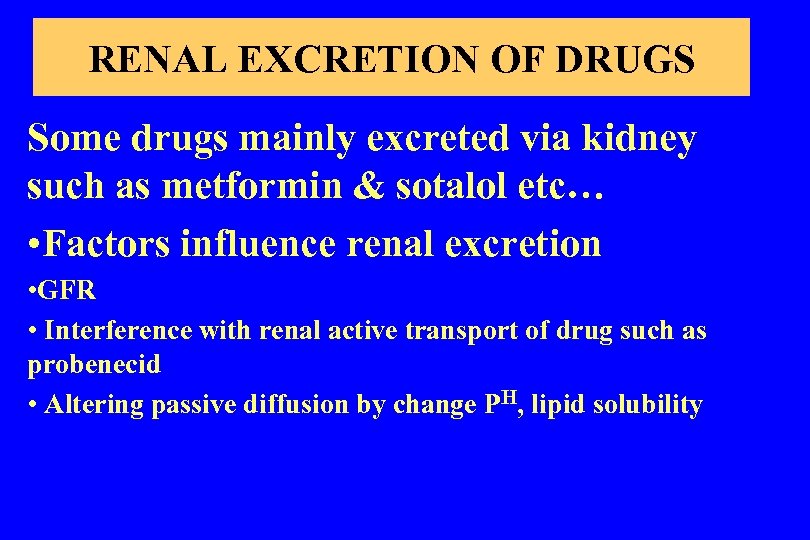 RENAL EXCRETION OF DRUGS Some drugs mainly excreted via kidney such as metformin & sotalol etc… • Factors influence renal excretion • GFR • Interference with renal active transport of drug such as probenecid • Altering passive diffusion by change PH, lipid solubility
RENAL EXCRETION OF DRUGS Some drugs mainly excreted via kidney such as metformin & sotalol etc… • Factors influence renal excretion • GFR • Interference with renal active transport of drug such as probenecid • Altering passive diffusion by change PH, lipid solubility
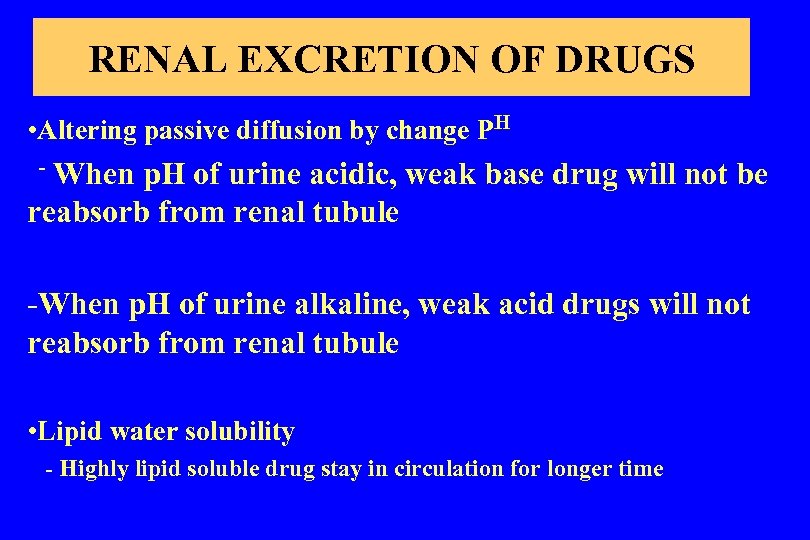 RENAL EXCRETION OF DRUGS • Altering passive diffusion by change PH - When p. H of urine acidic, weak base drug will not be reabsorb from renal tubule -When p. H of urine alkaline, weak acid drugs will not reabsorb from renal tubule • Lipid water solubility - Highly lipid soluble drug stay in circulation for longer time
RENAL EXCRETION OF DRUGS • Altering passive diffusion by change PH - When p. H of urine acidic, weak base drug will not be reabsorb from renal tubule -When p. H of urine alkaline, weak acid drugs will not reabsorb from renal tubule • Lipid water solubility - Highly lipid soluble drug stay in circulation for longer time
 BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS Liver cells transfer various drug from plasma to bile by • Transport system similar to renal tubule • conjugates drugs and concentrate these drugs in bile and the delivered into the intestine • Some conjugate drugs which is delivered into the intestine hydrolyzed to unconjugated drug (free drug) • The free drug reabsorb back into circulation • This called enterhepatic cycle.
BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS Liver cells transfer various drug from plasma to bile by • Transport system similar to renal tubule • conjugates drugs and concentrate these drugs in bile and the delivered into the intestine • Some conjugate drugs which is delivered into the intestine hydrolyzed to unconjugated drug (free drug) • The free drug reabsorb back into circulation • This called enterhepatic cycle.
 BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS • This creates a reservoir of recirculating drugs which represent around 20% of total drug in the body • This cycle maintains drug blood levels leading to prolongs the drug action • Examples of drugs go through enterohepatic cycle: - Digoxin - morphine - steroids including sex hormones
BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS • This creates a reservoir of recirculating drugs which represent around 20% of total drug in the body • This cycle maintains drug blood levels leading to prolongs the drug action • Examples of drugs go through enterohepatic cycle: - Digoxin - morphine - steroids including sex hormones
 PULMONARY EXCRETION OF DRUGS Pulmonary excretion does not require metabolism • Factors influence pulmonary excretion 1 - Rate of respiration 2 - Cardiac output 3 - solubility of gas in blood - High blood solubility decreases gases loss from lung - In contrast less blood soluble, leads to faster loss of gas via lung such nitrous oxide
PULMONARY EXCRETION OF DRUGS Pulmonary excretion does not require metabolism • Factors influence pulmonary excretion 1 - Rate of respiration 2 - Cardiac output 3 - solubility of gas in blood - High blood solubility decreases gases loss from lung - In contrast less blood soluble, leads to faster loss of gas via lung such nitrous oxide
 Excretion of drugs via other body fluids 1 - Sweat - Drugs or its metabolite may be responsible for induction of dermatitis or other skin reactions 2 - Saliva - change in taste or induction metallic taste 3 - Milk - The PH of milk is 6. 5, therefore the weak base drugs will concentrate in milk
Excretion of drugs via other body fluids 1 - Sweat - Drugs or its metabolite may be responsible for induction of dermatitis or other skin reactions 2 - Saliva - change in taste or induction metallic taste 3 - Milk - The PH of milk is 6. 5, therefore the weak base drugs will concentrate in milk
 3 rd lecture Immunosuppressors
3 rd lecture Immunosuppressors
 IMMUNOSUPPRESSANTS GOALS OF IMMUNOTHERAPY IN ORGAN TRANSPLANTS 1 - Prevention of the immune response example: acute rejection and vascular remodeling 2 - prevention of complications of immunodeficiency Such as infections and malignancy 3 -minimize drug induced and other non-immune toxicities
IMMUNOSUPPRESSANTS GOALS OF IMMUNOTHERAPY IN ORGAN TRANSPLANTS 1 - Prevention of the immune response example: acute rejection and vascular remodeling 2 - prevention of complications of immunodeficiency Such as infections and malignancy 3 -minimize drug induced and other non-immune toxicities
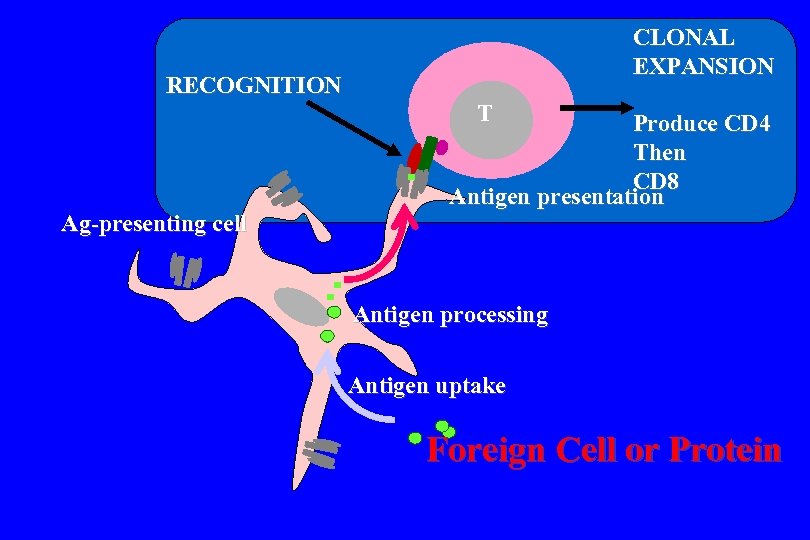 CLONAL EXPANSION RECOGNITION T Ag-presenting cell Produce CD 4 Then CD 8 Antigen presentation Antigen processing Antigen uptake Foreign Cell or Protein
CLONAL EXPANSION RECOGNITION T Ag-presenting cell Produce CD 4 Then CD 8 Antigen presentation Antigen processing Antigen uptake Foreign Cell or Protein
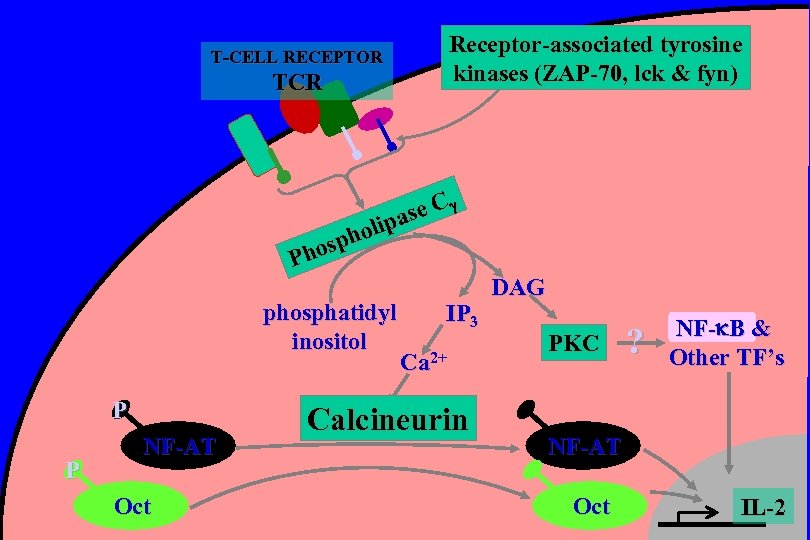 Receptor-associated tyrosine kinases (ZAP-70, lck & fyn) T-CELL RECEPTOR TCR se C a olip h osp Ph phosphatidyl inositol P P NF-AT Oct IP 3 Ca 2+ Calcineurin DAG PKC ? NF- B & Other TF’s NF-AT Oct IL-2
Receptor-associated tyrosine kinases (ZAP-70, lck & fyn) T-CELL RECEPTOR TCR se C a olip h osp Ph phosphatidyl inositol P P NF-AT Oct IP 3 Ca 2+ Calcineurin DAG PKC ? NF- B & Other TF’s NF-AT Oct IL-2
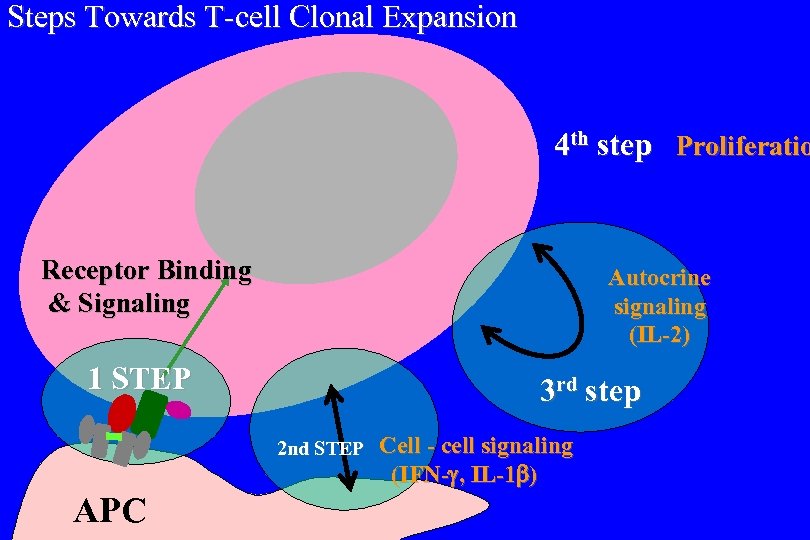 Steps Towards T-cell Clonal Expansion 4 th step Proliferatio Receptor Binding & Signaling Autocrine signaling (IL-2) 1 STEP 3 rd step 2 nd STEP Cell - cell signaling (IFN- , IL-1 ) APC
Steps Towards T-cell Clonal Expansion 4 th step Proliferatio Receptor Binding & Signaling Autocrine signaling (IL-2) 1 STEP 3 rd step 2 nd STEP Cell - cell signaling (IFN- , IL-1 ) APC
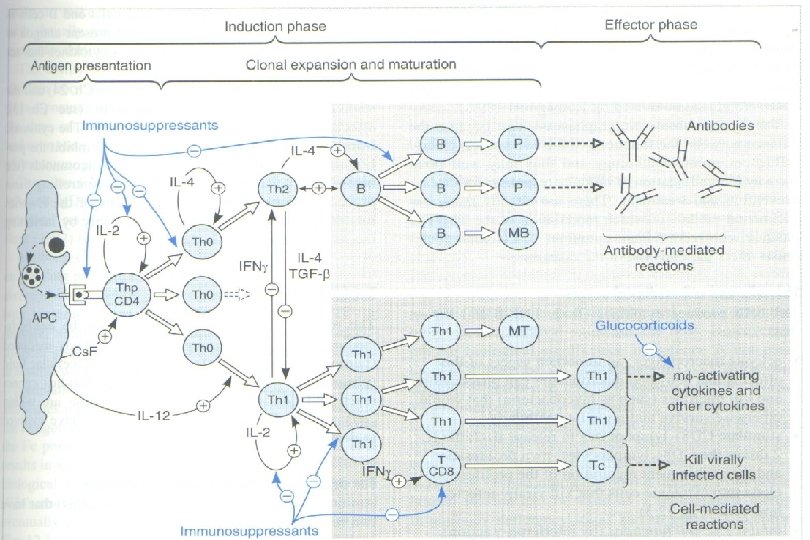
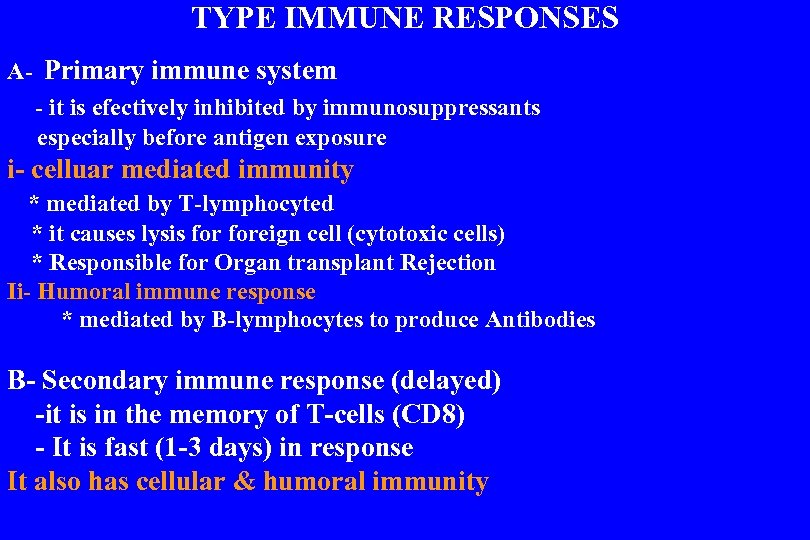 TYPE IMMUNE RESPONSES A- Primary immune system - it is efectively inhibited by immunosuppressants especially before antigen exposure i- celluar mediated immunity * mediated by T-lymphocyted * it causes lysis foreign cell (cytotoxic cells) * Responsible for Organ transplant Rejection Ii- Humoral immune response * mediated by B-lymphocytes to produce Antibodies B- Secondary immune response (delayed) -it is in the memory of T-cells (CD 8) - It is fast (1 -3 days) in response It also has cellular & humoral immunity
TYPE IMMUNE RESPONSES A- Primary immune system - it is efectively inhibited by immunosuppressants especially before antigen exposure i- celluar mediated immunity * mediated by T-lymphocyted * it causes lysis foreign cell (cytotoxic cells) * Responsible for Organ transplant Rejection Ii- Humoral immune response * mediated by B-lymphocytes to produce Antibodies B- Secondary immune response (delayed) -it is in the memory of T-cells (CD 8) - It is fast (1 -3 days) in response It also has cellular & humoral immunity
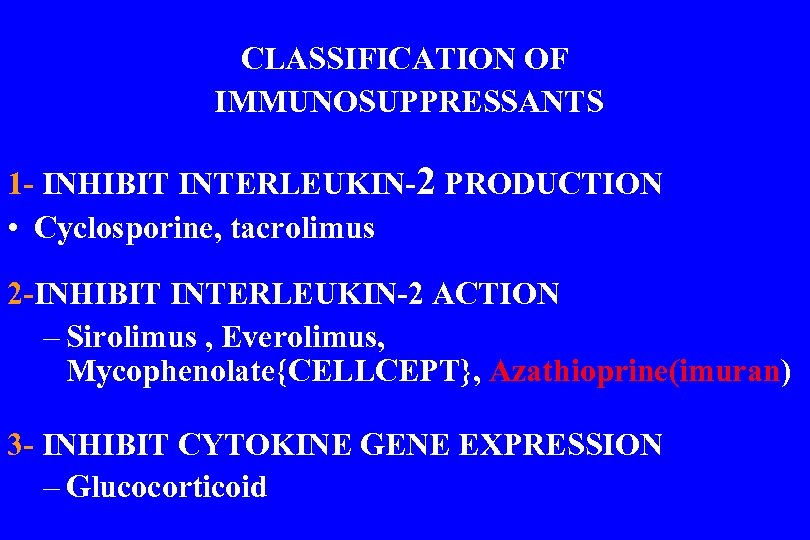 CLASSIFICATION OF IMMUNOSUPPRESSANTS 1 - INHIBIT INTERLEUKIN-2 PRODUCTION • Cyclosporine, tacrolimus 2 -INHIBIT INTERLEUKIN-2 ACTION – Sirolimus , Everolimus, Mycophenolate{CELLCEPT}, Azathioprine(imuran) 3 - INHIBIT CYTOKINE GENE EXPRESSION – Glucocorticoid
CLASSIFICATION OF IMMUNOSUPPRESSANTS 1 - INHIBIT INTERLEUKIN-2 PRODUCTION • Cyclosporine, tacrolimus 2 -INHIBIT INTERLEUKIN-2 ACTION – Sirolimus , Everolimus, Mycophenolate{CELLCEPT}, Azathioprine(imuran) 3 - INHIBIT CYTOKINE GENE EXPRESSION – Glucocorticoid
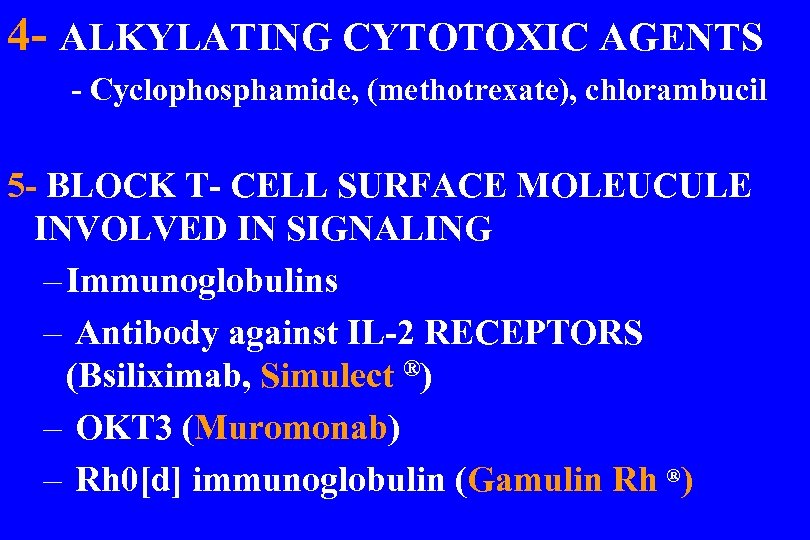 4 - ALKYLATING CYTOTOXIC AGENTS - Cyclophosphamide, (methotrexate), chlorambucil 5 - BLOCK T- CELL SURFACE MOLEUCULE INVOLVED IN SIGNALING – Immunoglobulins – Antibody against IL-2 RECEPTORS (Bsiliximab, Simulect ®) – OKT 3 (Muromonab) – Rh 0[d] immunoglobulin (Gamulin Rh ®)
4 - ALKYLATING CYTOTOXIC AGENTS - Cyclophosphamide, (methotrexate), chlorambucil 5 - BLOCK T- CELL SURFACE MOLEUCULE INVOLVED IN SIGNALING – Immunoglobulins – Antibody against IL-2 RECEPTORS (Bsiliximab, Simulect ®) – OKT 3 (Muromonab) – Rh 0[d] immunoglobulin (Gamulin Rh ®)
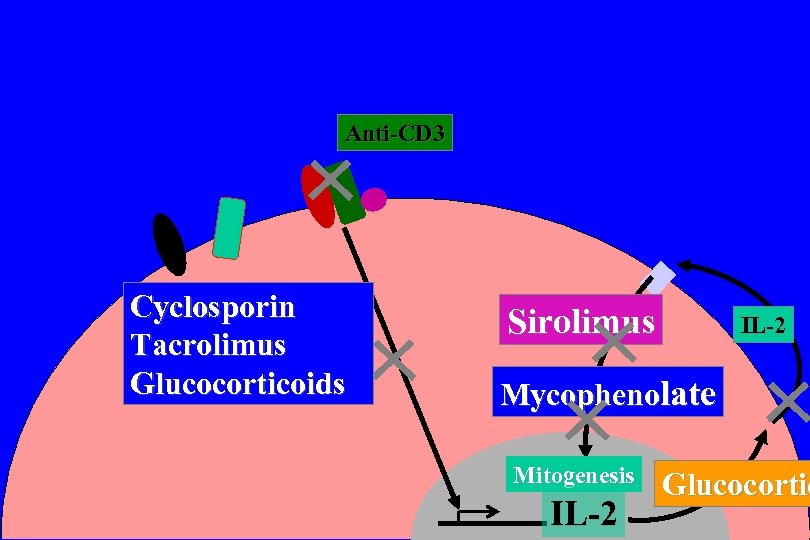 Anti-CD 3 Cyclosporin Tacrolimus Glucocorticoids Sirolimus IL-2 Mycophenolate Mitogenesis IL-2 Glucocortic
Anti-CD 3 Cyclosporin Tacrolimus Glucocorticoids Sirolimus IL-2 Mycophenolate Mitogenesis IL-2 Glucocortic
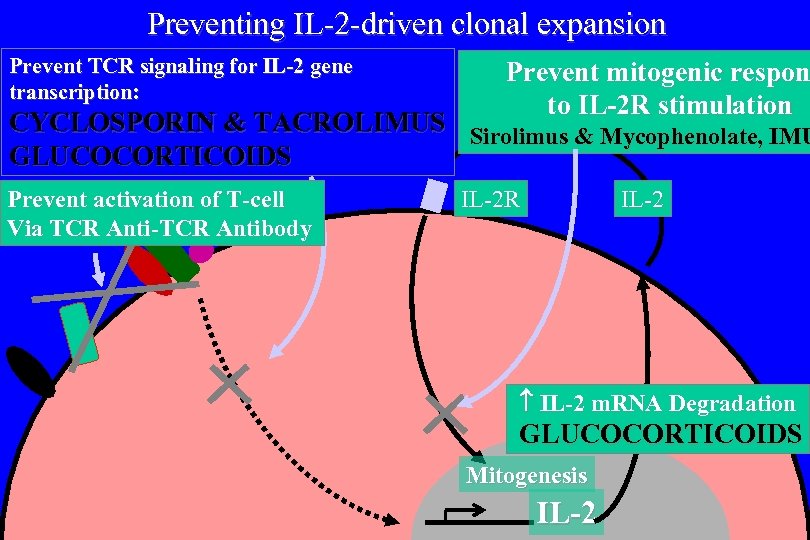 Preventing IL-2 -driven clonal expansion Prevent TCR signaling for IL-2 gene transcription: Prevent mitogenic respon to IL-2 R stimulation CYCLOSPORIN & TACROLIMUS Sirolimus & Mycophenolate, IMU GLUCOCORTICOIDS Prevent activation of T-cell Via TCR Anti-TCR Antibody IL-2 R IL-2 m. RNA Degradation GLUCOCORTICOIDS Mitogenesis IL-2
Preventing IL-2 -driven clonal expansion Prevent TCR signaling for IL-2 gene transcription: Prevent mitogenic respon to IL-2 R stimulation CYCLOSPORIN & TACROLIMUS Sirolimus & Mycophenolate, IMU GLUCOCORTICOIDS Prevent activation of T-cell Via TCR Anti-TCR Antibody IL-2 R IL-2 m. RNA Degradation GLUCOCORTICOIDS Mitogenesis IL-2
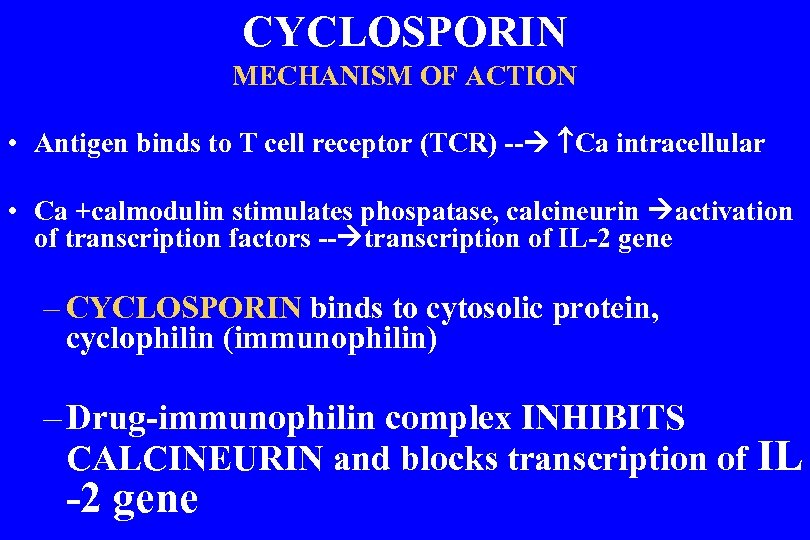 CYCLOSPORIN MECHANISM OF ACTION • Antigen binds to T cell receptor (TCR) -- Ca intracellular • Ca +calmodulin stimulates phospatase, calcineurin activation of transcription factors -- transcription of IL-2 gene – CYCLOSPORIN binds to cytosolic protein, cyclophilin (immunophilin) – Drug-immunophilin complex INHIBITS CALCINEURIN and blocks transcription of IL -2 gene
CYCLOSPORIN MECHANISM OF ACTION • Antigen binds to T cell receptor (TCR) -- Ca intracellular • Ca +calmodulin stimulates phospatase, calcineurin activation of transcription factors -- transcription of IL-2 gene – CYCLOSPORIN binds to cytosolic protein, cyclophilin (immunophilin) – Drug-immunophilin complex INHIBITS CALCINEURIN and blocks transcription of IL -2 gene
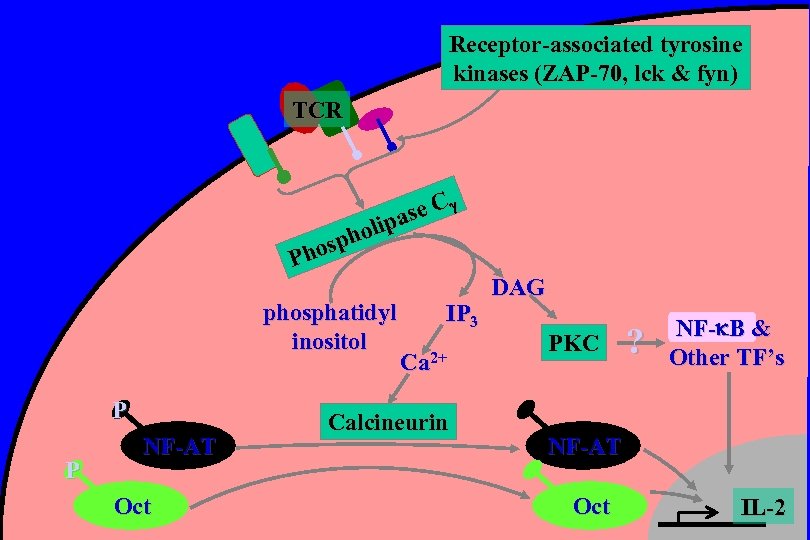 Receptor-associated tyrosine kinases (ZAP-70, lck & fyn) TCR se C a olip h osp Ph phosphatidyl inositol P P NF-AT Oct IP 3 Ca 2+ Calcineurin DAG PKC ? NF- B & Other TF’s NF-AT Oct IL-2
Receptor-associated tyrosine kinases (ZAP-70, lck & fyn) TCR se C a olip h osp Ph phosphatidyl inositol P P NF-AT Oct IP 3 Ca 2+ Calcineurin DAG PKC ? NF- B & Other TF’s NF-AT Oct IL-2
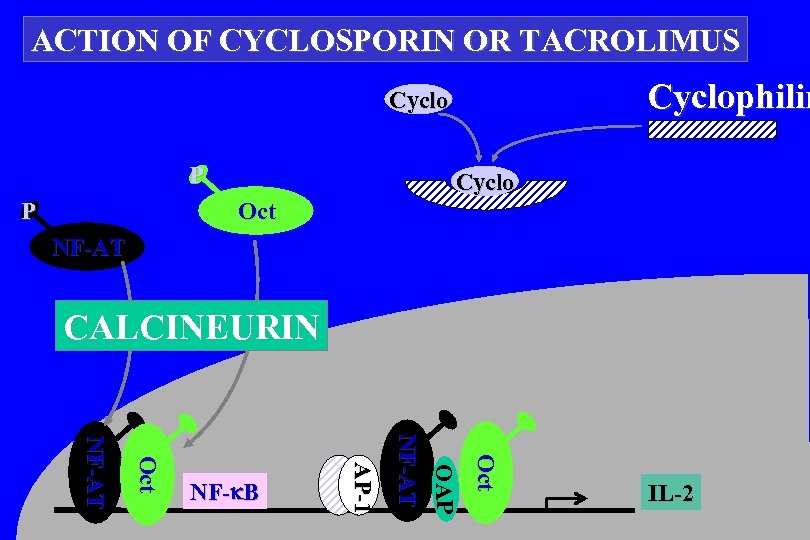 ACTION OF CYCLOSPORIN OR TACROLIMUS Cyclophilin Cyclo P P Cyclo Oct NF-AT CALCINEURIN Oct OAP NF-AT AP-1 Oct NF-AT NF- B IL-2
ACTION OF CYCLOSPORIN OR TACROLIMUS Cyclophilin Cyclo P P Cyclo Oct NF-AT CALCINEURIN Oct OAP NF-AT AP-1 Oct NF-AT NF- B IL-2
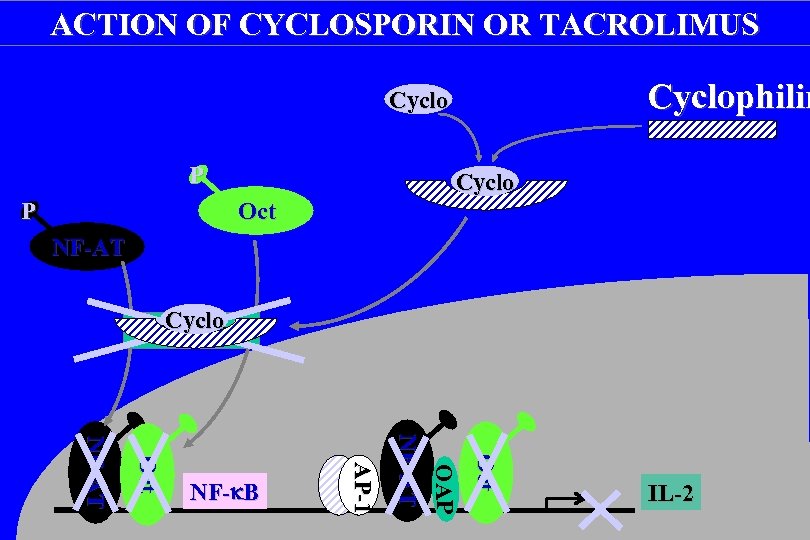 ACTION OF CYCLOSPORIN OR TACROLIMUS Cyclophilin Cyclo P P Cyclo Oct NF-AT Cyclo Calcineurin Oct OAP NF-AT AP-1 Oct NF-AT NF- B IL-2
ACTION OF CYCLOSPORIN OR TACROLIMUS Cyclophilin Cyclo P P Cyclo Oct NF-AT Cyclo Calcineurin Oct OAP NF-AT AP-1 Oct NF-AT NF- B IL-2
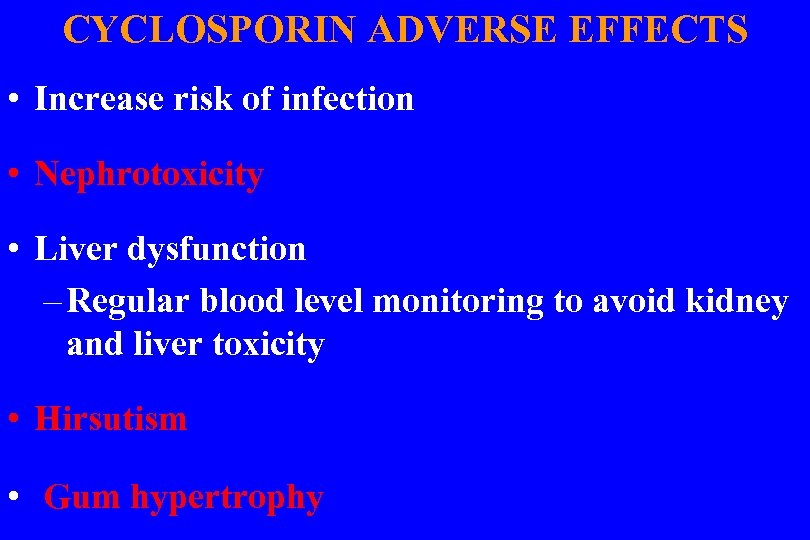 CYCLOSPORIN ADVERSE EFFECTS • Increase risk of infection • Nephrotoxicity • Liver dysfunction – Regular blood level monitoring to avoid kidney and liver toxicity • Hirsutism • Gum hypertrophy
CYCLOSPORIN ADVERSE EFFECTS • Increase risk of infection • Nephrotoxicity • Liver dysfunction – Regular blood level monitoring to avoid kidney and liver toxicity • Hirsutism • Gum hypertrophy
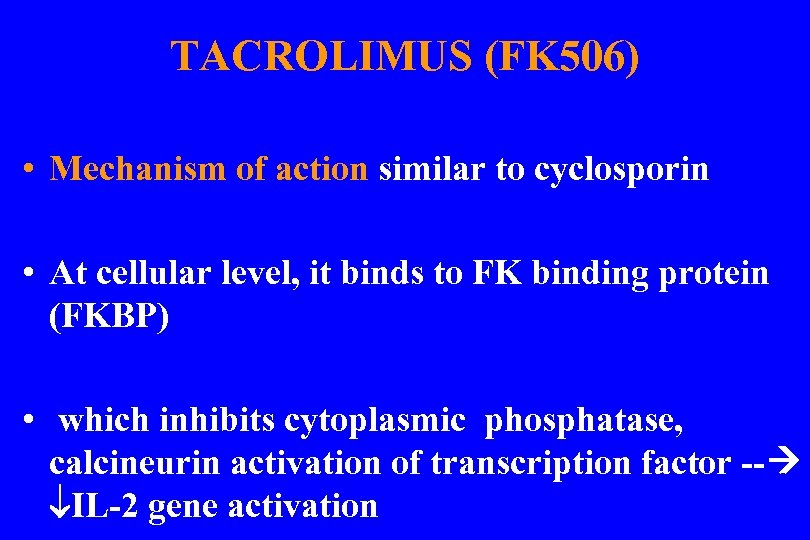 TACROLIMUS (FK 506) • Mechanism of action similar to cyclosporin • At cellular level, it binds to FK binding protein (FKBP) • which inhibits cytoplasmic phosphatase, calcineurin activation of transcription factor -- IL-2 gene activation
TACROLIMUS (FK 506) • Mechanism of action similar to cyclosporin • At cellular level, it binds to FK binding protein (FKBP) • which inhibits cytoplasmic phosphatase, calcineurin activation of transcription factor -- IL-2 gene activation
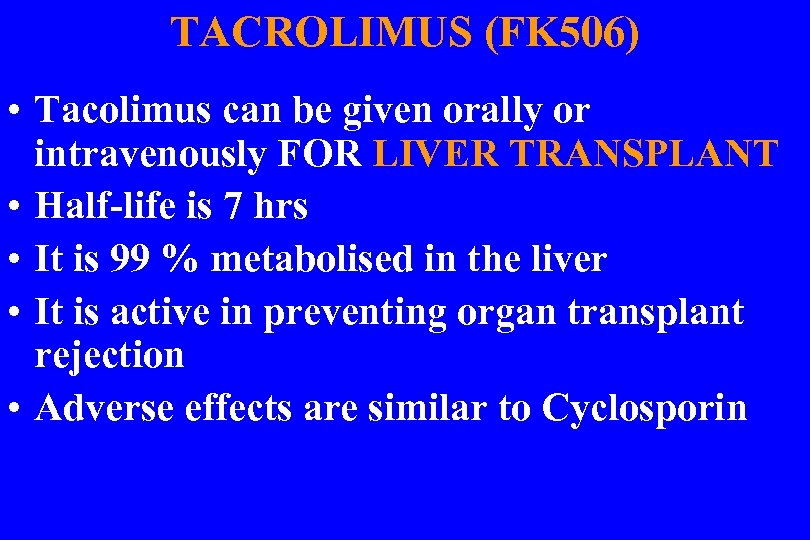 TACROLIMUS (FK 506) • Tacolimus can be given orally or intravenously FOR LIVER TRANSPLANT • Half-life is 7 hrs • It is 99 % metabolised in the liver • It is active in preventing organ transplant rejection • Adverse effects are similar to Cyclosporin
TACROLIMUS (FK 506) • Tacolimus can be given orally or intravenously FOR LIVER TRANSPLANT • Half-life is 7 hrs • It is 99 % metabolised in the liver • It is active in preventing organ transplant rejection • Adverse effects are similar to Cyclosporin
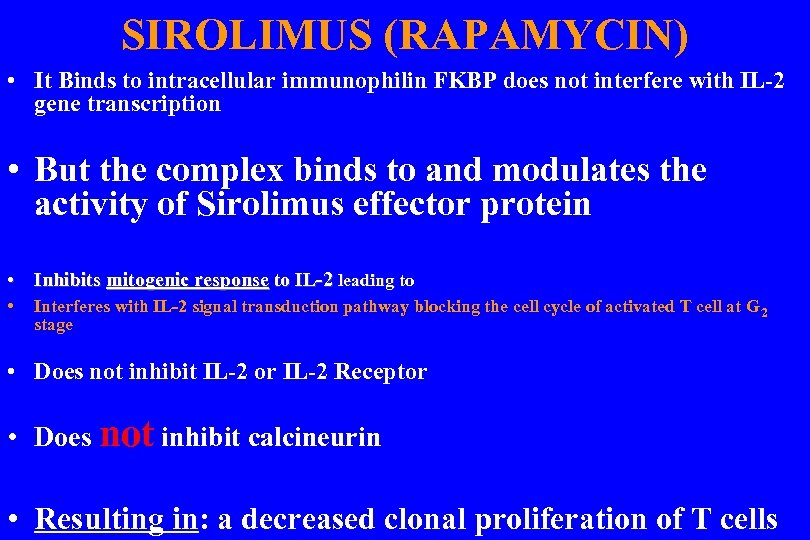 SIROLIMUS (RAPAMYCIN) • It Binds to intracellular immunophilin FKBP does not interfere with IL-2 gene transcription • But the complex binds to and modulates the activity of Sirolimus effector protein • Inhibits mitogenic response to IL-2 leading to • Interferes with IL-2 signal transduction pathway blocking the cell cycle of activated T cell at G 2 stage • Does not inhibit IL-2 or IL-2 Receptor • Does not inhibit calcineurin • Resulting in: a decreased clonal proliferation of T cells
SIROLIMUS (RAPAMYCIN) • It Binds to intracellular immunophilin FKBP does not interfere with IL-2 gene transcription • But the complex binds to and modulates the activity of Sirolimus effector protein • Inhibits mitogenic response to IL-2 leading to • Interferes with IL-2 signal transduction pathway blocking the cell cycle of activated T cell at G 2 stage • Does not inhibit IL-2 or IL-2 Receptor • Does not inhibit calcineurin • Resulting in: a decreased clonal proliferation of T cells
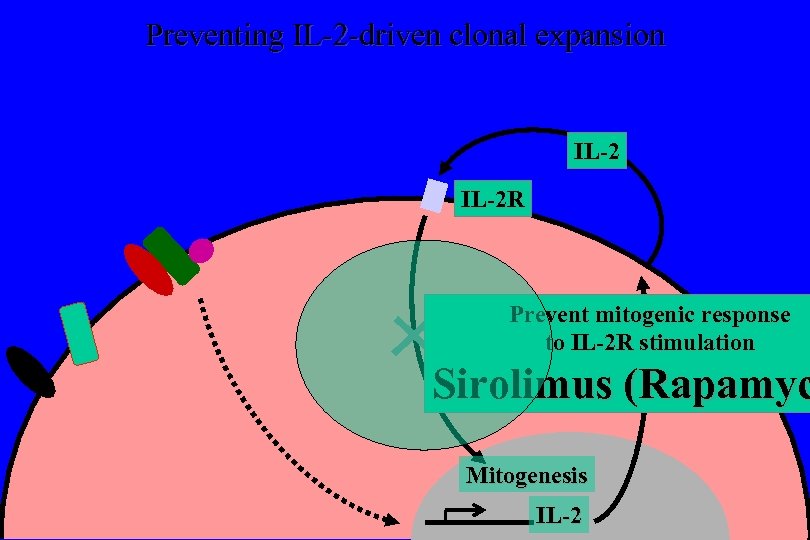 Preventing IL-2 -driven clonal expansion IL-2 R Prevent mitogenic response to IL-2 R stimulation Sirolimus (Rapamyc Mitogenesis IL-2
Preventing IL-2 -driven clonal expansion IL-2 R Prevent mitogenic response to IL-2 R stimulation Sirolimus (Rapamyc Mitogenesis IL-2
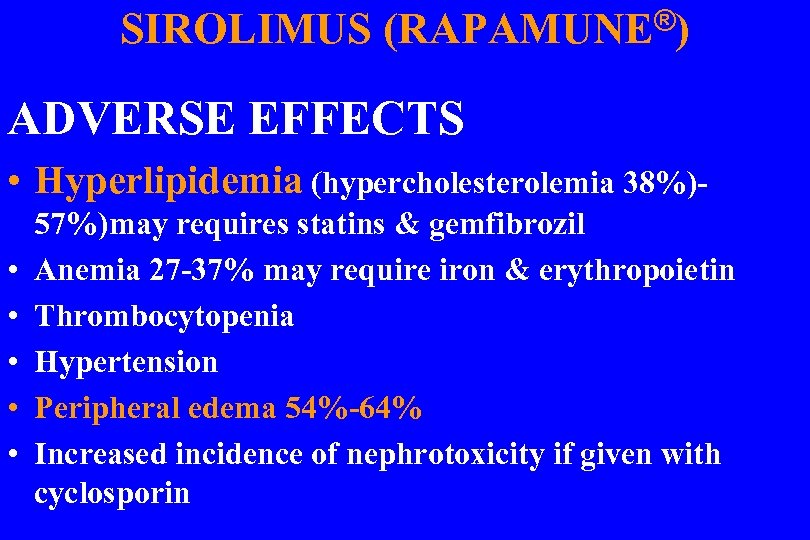 SIROLIMUS (RAPAMUNE®) ADVERSE EFFECTS • Hyperlipidemia (hypercholesterolemia 38%) • • • 57%)may requires statins & gemfibrozil Anemia 27 -37% may require iron & erythropoietin Thrombocytopenia Hypertension Peripheral edema 54%-64% Increased incidence of nephrotoxicity if given with cyclosporin
SIROLIMUS (RAPAMUNE®) ADVERSE EFFECTS • Hyperlipidemia (hypercholesterolemia 38%) • • • 57%)may requires statins & gemfibrozil Anemia 27 -37% may require iron & erythropoietin Thrombocytopenia Hypertension Peripheral edema 54%-64% Increased incidence of nephrotoxicity if given with cyclosporin
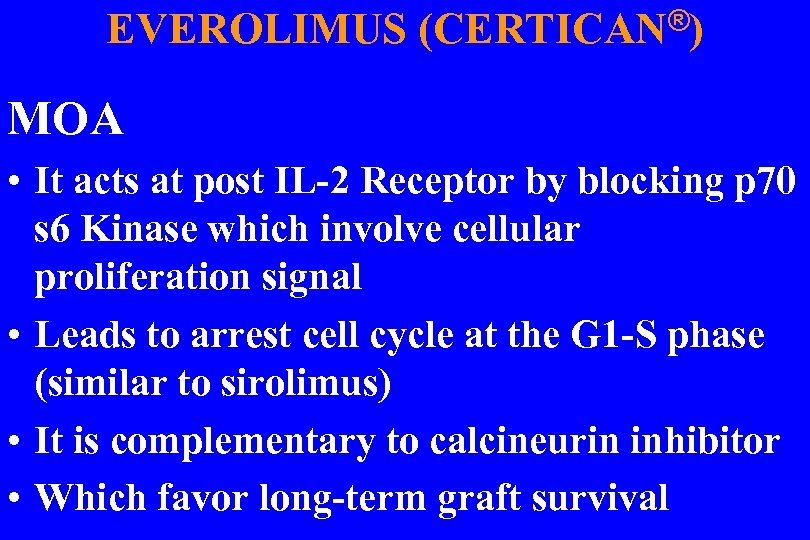 EVEROLIMUS (CERTICAN®) MOA • It acts at post IL-2 Receptor by blocking p 70 s 6 Kinase which involve cellular proliferation signal • Leads to arrest cell cycle at the G 1 -S phase (similar to sirolimus) • It is complementary to calcineurin inhibitor • Which favor long-term graft survival
EVEROLIMUS (CERTICAN®) MOA • It acts at post IL-2 Receptor by blocking p 70 s 6 Kinase which involve cellular proliferation signal • Leads to arrest cell cycle at the G 1 -S phase (similar to sirolimus) • It is complementary to calcineurin inhibitor • Which favor long-term graft survival
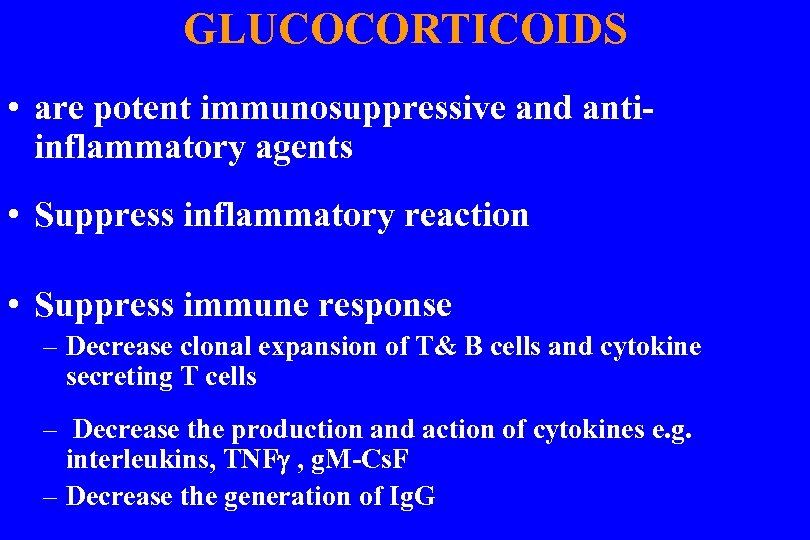 GLUCOCORTICOIDS • are potent immunosuppressive and antiinflammatory agents • Suppress inflammatory reaction • Suppress immune response – Decrease clonal expansion of T& B cells and cytokine secreting T cells – Decrease the production and action of cytokines e. g. interleukins, TNF , g. M-Cs. F – Decrease the generation of Ig. G
GLUCOCORTICOIDS • are potent immunosuppressive and antiinflammatory agents • Suppress inflammatory reaction • Suppress immune response – Decrease clonal expansion of T& B cells and cytokine secreting T cells – Decrease the production and action of cytokines e. g. interleukins, TNF , g. M-Cs. F – Decrease the generation of Ig. G
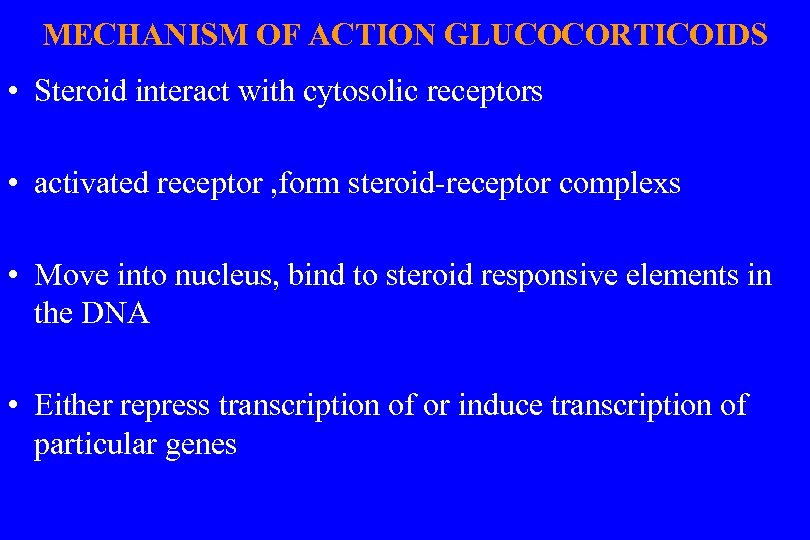 MECHANISM OF ACTION GLUCOCORTICOIDS • Steroid interact with cytosolic receptors • activated receptor , form steroid-receptor complexs • Move into nucleus, bind to steroid responsive elements in the DNA • Either repress transcription of or induce transcription of particular genes
MECHANISM OF ACTION GLUCOCORTICOIDS • Steroid interact with cytosolic receptors • activated receptor , form steroid-receptor complexs • Move into nucleus, bind to steroid responsive elements in the DNA • Either repress transcription of or induce transcription of particular genes
 Glucocorticoids • Suppression of transcription OF IL-2 • Reduced IL-2 m. RNA stability ( IL-2 m. RNA Degradation)
Glucocorticoids • Suppression of transcription OF IL-2 • Reduced IL-2 m. RNA stability ( IL-2 m. RNA Degradation)
 GLUCOCORTICOID CLINICAL USES • As anti-inflammatory & immuno- suppressive therapy – Asthma, allergic rhinitis, eczema, severe drug allergic reaction, rheumatoid arthritis , organ transplant • In neoplastic disease – Hodgkin’s disease, acute lymphocytic leukaemia • Replacement therapy • In adrenal insufficiency
GLUCOCORTICOID CLINICAL USES • As anti-inflammatory & immuno- suppressive therapy – Asthma, allergic rhinitis, eczema, severe drug allergic reaction, rheumatoid arthritis , organ transplant • In neoplastic disease – Hodgkin’s disease, acute lymphocytic leukaemia • Replacement therapy • In adrenal insufficiency
 ADVERSE EFFECTS • Suppress response to injury or infection • Suppress patients capacity to synthesize corticosteroids • Metabolic effect – Water and electrolyte imbalance – Osteoporosis – GI bleeding – hyperglycemia
ADVERSE EFFECTS • Suppress response to injury or infection • Suppress patients capacity to synthesize corticosteroids • Metabolic effect – Water and electrolyte imbalance – Osteoporosis – GI bleeding – hyperglycemia
 CYCLOPHOSPHAMIDE • is a nitrogen mustard, an alkylating agent • Is inactive until metabolised by the liver into its active phosphoamide mustard • Have alkyl groups which can cross link to two nucleophilic site of the DNA--- defective replication • Resulting in subsequent cell death
CYCLOPHOSPHAMIDE • is a nitrogen mustard, an alkylating agent • Is inactive until metabolised by the liver into its active phosphoamide mustard • Have alkyl groups which can cross link to two nucleophilic site of the DNA--- defective replication • Resulting in subsequent cell death

 CYCLOPHOSPHAMIDE • Has pronounced effect on the lymphocytes • Usually given orally for Autoimmune diseases • ADVERSE EFFECTS: – Depress bone marrow function – GI disturbance • Toxic metabolite acrolein – Haemorrhagic cystitis
CYCLOPHOSPHAMIDE • Has pronounced effect on the lymphocytes • Usually given orally for Autoimmune diseases • ADVERSE EFFECTS: – Depress bone marrow function – GI disturbance • Toxic metabolite acrolein – Haemorrhagic cystitis
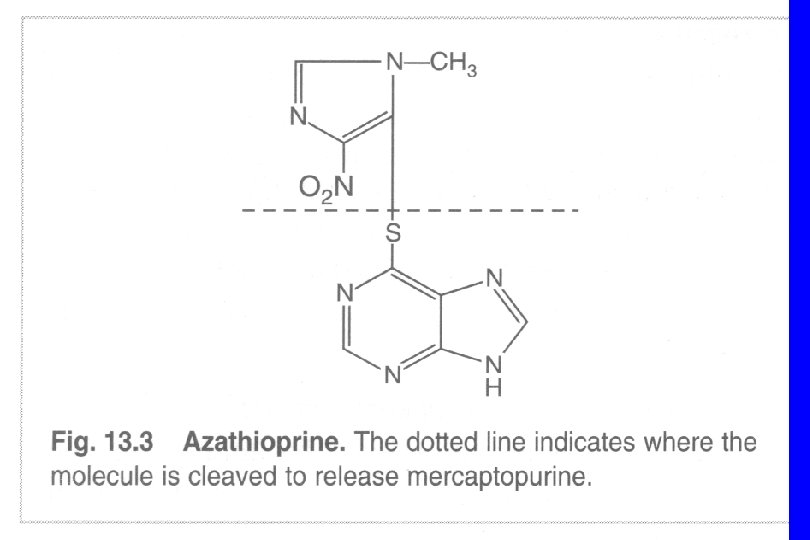
 AZATHIOPURINE (IMURAN®) • It is metabolised to give mercapturine which is a purine analog • interferes with purine synthesis and is cytotoxic on the dividing cell • Inhibit clonal prolifeation in the induction phase of the immune response • Inhibits both cell mediated antibody mediated immune reactions
AZATHIOPURINE (IMURAN®) • It is metabolised to give mercapturine which is a purine analog • interferes with purine synthesis and is cytotoxic on the dividing cell • Inhibit clonal prolifeation in the induction phase of the immune response • Inhibits both cell mediated antibody mediated immune reactions
 AZATHIOPURINE • USED - in organ transplant to prevent rejection - Autoimmune diseases with glucocorticoids • MAJOR SIDE EFFECT: - suppress bone marrow - Hepatotoxicity - Retinopathy
AZATHIOPURINE • USED - in organ transplant to prevent rejection - Autoimmune diseases with glucocorticoids • MAJOR SIDE EFFECT: - suppress bone marrow - Hepatotoxicity - Retinopathy
 MYCOPHENOLATE a- Mofetil salt CELLCEPT ® B- sodium salt (enteric coated) MYOFORTIC® Administered orally and is well absorbed • A semisynthetic derivative of fungal antibiotic • Converted to mycophenolic acid
MYCOPHENOLATE a- Mofetil salt CELLCEPT ® B- sodium salt (enteric coated) MYOFORTIC® Administered orally and is well absorbed • A semisynthetic derivative of fungal antibiotic • Converted to mycophenolic acid
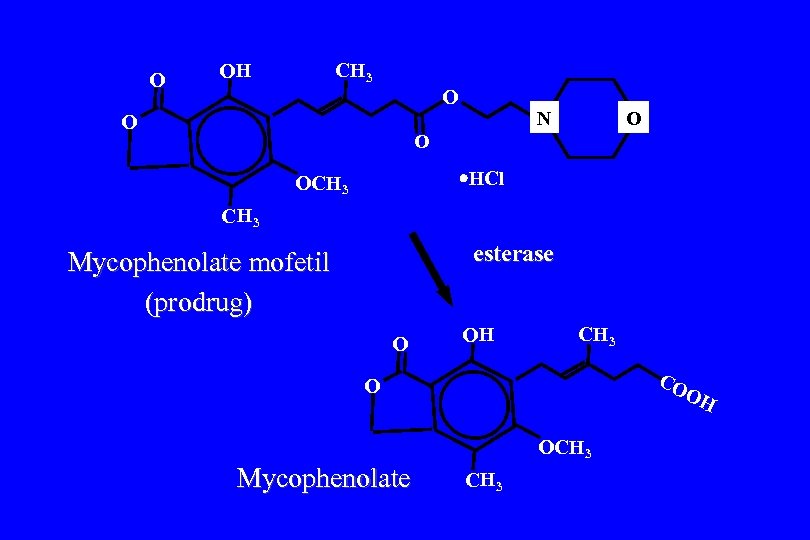 O OH CH 3 O O N O O HCl OCH 3 esterase Mycophenolate mofetil (prodrug) O OH CH 3 CO OH O OCH 3 Mycophenolate CH 3
O OH CH 3 O O N O O HCl OCH 3 esterase Mycophenolate mofetil (prodrug) O OH CH 3 CO OH O OCH 3 Mycophenolate CH 3
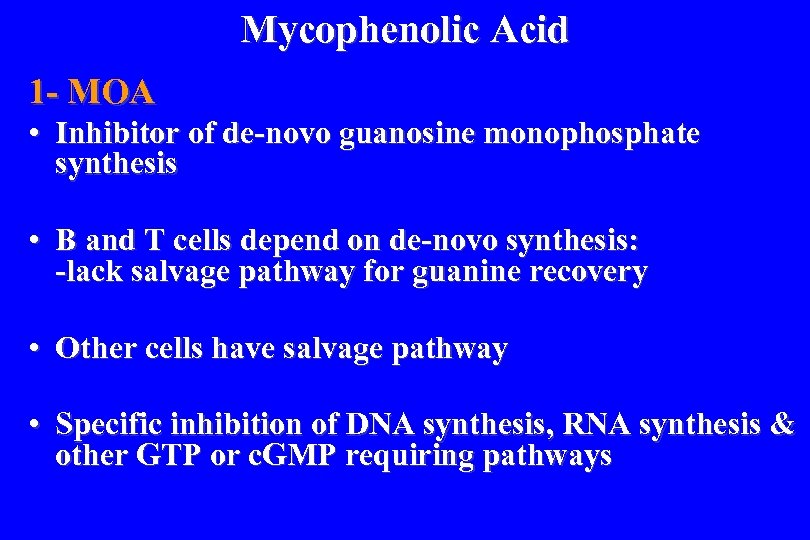 Mycophenolic Acid 1 - MOA • Inhibitor of de-novo guanosine monophosphate synthesis • B and T cells depend on de-novo synthesis: -lack salvage pathway for guanine recovery • Other cells have salvage pathway • Specific inhibition of DNA synthesis, RNA synthesis & other GTP or c. GMP requiring pathways
Mycophenolic Acid 1 - MOA • Inhibitor of de-novo guanosine monophosphate synthesis • B and T cells depend on de-novo synthesis: -lack salvage pathway for guanine recovery • Other cells have salvage pathway • Specific inhibition of DNA synthesis, RNA synthesis & other GTP or c. GMP requiring pathways
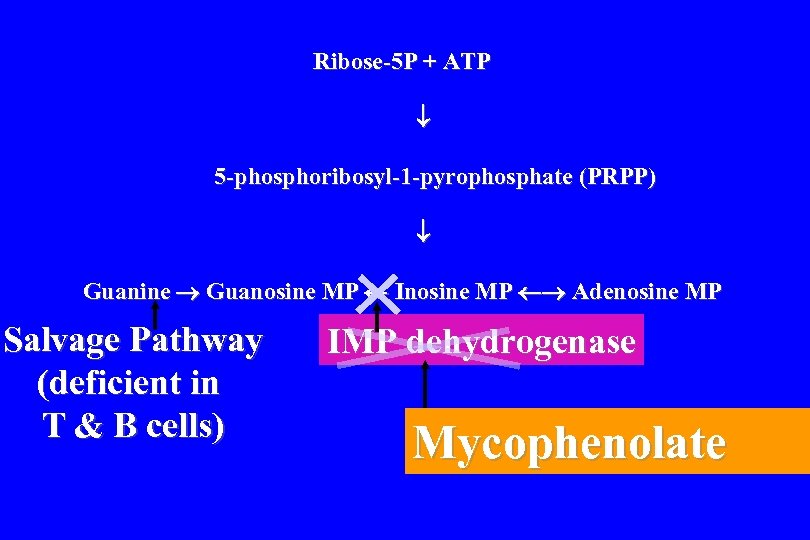 Ribose-5 P + ATP 5 -phosphoribosyl-1 -pyrophosphate (PRPP) Guanine Guanosine MP Inosine MP Adenosine MP Salvage Pathway (deficient in T & B cells) IMP dehydrogenase Mycophenolate
Ribose-5 P + ATP 5 -phosphoribosyl-1 -pyrophosphate (PRPP) Guanine Guanosine MP Inosine MP Adenosine MP Salvage Pathway (deficient in T & B cells) IMP dehydrogenase Mycophenolate
 2 - DRUG INTERACTION • Magnesium and aluminium impairs absorption 3 - USES - Trial used in kidney transplant with cyclosporine and steroids - Autoimmune diseases
2 - DRUG INTERACTION • Magnesium and aluminium impairs absorption 3 - USES - Trial used in kidney transplant with cyclosporine and steroids - Autoimmune diseases
 4 - ADVERSE EFFECTS • Peptic ulcer & esophagitis • Hypercholestrolemia • Diarrhea
4 - ADVERSE EFFECTS • Peptic ulcer & esophagitis • Hypercholestrolemia • Diarrhea
 IMMUNOSUPPRESSANT REGIMENS 1 - Basiliximab, cyclosporin, prednisolone 2 - Basiliximab, Azathioprine, cyclosporin, prednisolone 3 - Basiliximab, MMF, cyclosporin, prednisolone
IMMUNOSUPPRESSANT REGIMENS 1 - Basiliximab, cyclosporin, prednisolone 2 - Basiliximab, Azathioprine, cyclosporin, prednisolone 3 - Basiliximab, MMF, cyclosporin, prednisolone
 4 - Basiliximab, Everolimus, cyclosporin, prednisolone 5 - Basiliximab, Sirolimus, cyclosporin, prednisolone ******************** Basiliximab 20 mg divided into two doses: • First dose should be given on day 0 • and second dose given on day 4 if needed
4 - Basiliximab, Everolimus, cyclosporin, prednisolone 5 - Basiliximab, Sirolimus, cyclosporin, prednisolone ******************** Basiliximab 20 mg divided into two doses: • First dose should be given on day 0 • and second dose given on day 4 if needed
 IMMULOGLOBULINS • Antibodies against human lymphocytes • or their surface protein can have significant immunosupressant action
IMMULOGLOBULINS • Antibodies against human lymphocytes • or their surface protein can have significant immunosupressant action
 POLYCLONAL ANTIBODIES • Binds to protein on the surface of lymphocyte triggering the complement response - lysis of the lymphocyte • Indiscriminate action on all T cells EXAMPLE – ANTI-THYMPHOCYTE – Lymphocyte immune globulin ( killer cell) immunoglobulin (ATG, Atgam ®) • Immunizing horse with human Thymphocyte
POLYCLONAL ANTIBODIES • Binds to protein on the surface of lymphocyte triggering the complement response - lysis of the lymphocyte • Indiscriminate action on all T cells EXAMPLE – ANTI-THYMPHOCYTE – Lymphocyte immune globulin ( killer cell) immunoglobulin (ATG, Atgam ®) • Immunizing horse with human Thymphocyte
 ®) ATG (Atgam • MOA - Eliminate antigen –reactive T-lymphocytes (killer cells • CLINICAL USES 1 - Prevention & treatment of acute renal and other organ allograft rejection 2 - aplastic anemia who is not candidate for bone marrow transplant
®) ATG (Atgam • MOA - Eliminate antigen –reactive T-lymphocytes (killer cells • CLINICAL USES 1 - Prevention & treatment of acute renal and other organ allograft rejection 2 - aplastic anemia who is not candidate for bone marrow transplant
 ®) ATG (Atgam • ADVERSE EFFECTS - FEVER - Allergic reaction Therefore, it is premedicated by paracetamol & diphenhydramine & glucocorticoids
®) ATG (Atgam • ADVERSE EFFECTS - FEVER - Allergic reaction Therefore, it is premedicated by paracetamol & diphenhydramine & glucocorticoids
 MONOCLONAL ANTIBODIES • Direct against surface components of T cells – CD 3 proteins with antigen receptors Example : Muromonab-CD 3 ®) (Orthoclone
MONOCLONAL ANTIBODIES • Direct against surface components of T cells – CD 3 proteins with antigen receptors Example : Muromonab-CD 3 ®) (Orthoclone
 Muromonab-CD 3 (Orthoclone ®)OKT 3 1 - MOA • It binds with T-cell receptor-associated CD 3 glycoprotein 2 - CLINICAL USES • Acute allograft rejection resistant to conventional therapy
Muromonab-CD 3 (Orthoclone ®)OKT 3 1 - MOA • It binds with T-cell receptor-associated CD 3 glycoprotein 2 - CLINICAL USES • Acute allograft rejection resistant to conventional therapy
 Muromonab-CD 3 (Orthoclone ®)OKT 3 3 - ADVERSE EFFECTS • First dose effects flu-like symptoms (cytokine release syndrome) • Manifested by fever, respiratory dystress • Hypervolemic pulmonary edema
Muromonab-CD 3 (Orthoclone ®)OKT 3 3 - ADVERSE EFFECTS • First dose effects flu-like symptoms (cytokine release syndrome) • Manifested by fever, respiratory dystress • Hypervolemic pulmonary edema
![Rh[d] immunoglobulin (Gamulin®) • MOA: - Immunoglobulin against Rh antigen D Which prevents the Rh[d] immunoglobulin (Gamulin®) • MOA: - Immunoglobulin against Rh antigen D Which prevents the](https://present5.com/presentation/c4faf54b1a6edd330b7f52909590fef9/image-111.jpg) Rh[d] immunoglobulin (Gamulin®) • MOA: - Immunoglobulin against Rh antigen D Which prevents the interactions between the Rh antigen and maternal (mother) immune system • CLINICAL USES - Prophylaxis in Erythroblastosis fetalis - Idiopathic thrombocytopenia
Rh[d] immunoglobulin (Gamulin®) • MOA: - Immunoglobulin against Rh antigen D Which prevents the interactions between the Rh antigen and maternal (mother) immune system • CLINICAL USES - Prophylaxis in Erythroblastosis fetalis - Idiopathic thrombocytopenia
![®] infliximab, Remicade MOA: Antibody against tumor necrosis factor alpha (TNF alpha) • USED: ®] infliximab, Remicade MOA: Antibody against tumor necrosis factor alpha (TNF alpha) • USED:](https://present5.com/presentation/c4faf54b1a6edd330b7f52909590fef9/image-112.jpg) ®] infliximab, Remicade MOA: Antibody against tumor necrosis factor alpha (TNF alpha) • USED: - for crohn’s disease - Rheumatoid arthritis with methotrexate who inadequate respond to methotrexate alone • CONTRAINDICATED: - CHF - & TUBERCULOSIS
®] infliximab, Remicade MOA: Antibody against tumor necrosis factor alpha (TNF alpha) • USED: - for crohn’s disease - Rheumatoid arthritis with methotrexate who inadequate respond to methotrexate alone • CONTRAINDICATED: - CHF - & TUBERCULOSIS
 ®) ETANERCEPT (Enbrel MOA: it binds with TNF and • blocks its interaction with cell surface receptor • CLINICAL USE - for rheumatoid arthritis & crohn. s disease
®) ETANERCEPT (Enbrel MOA: it binds with TNF and • blocks its interaction with cell surface receptor • CLINICAL USE - for rheumatoid arthritis & crohn. s disease
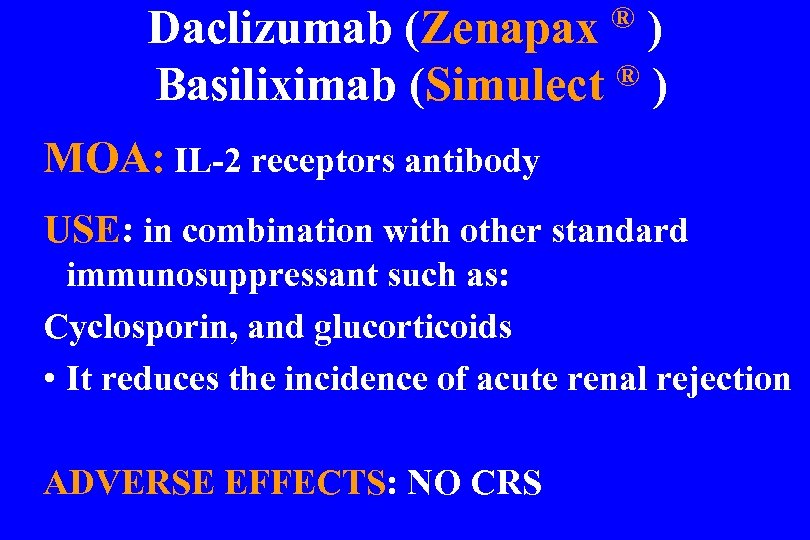 Daclizumab (Zenapax ® ) Basiliximab (Simulect MOA: IL-2 receptors antibody USE: in combination with other standard immunosuppressant such as: Cyclosporin, and glucorticoids • It reduces the incidence of acute renal rejection ADVERSE EFFECTS: NO CRS
Daclizumab (Zenapax ® ) Basiliximab (Simulect MOA: IL-2 receptors antibody USE: in combination with other standard immunosuppressant such as: Cyclosporin, and glucorticoids • It reduces the incidence of acute renal rejection ADVERSE EFFECTS: NO CRS
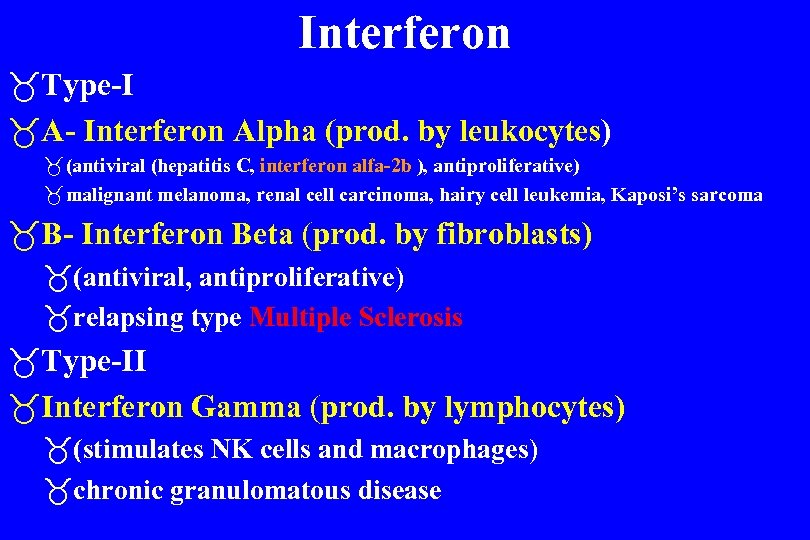 Interferon _Type-I _A- Interferon Alpha (prod. by leukocytes) _ (antiviral (hepatitis C, interferon alfa-2 b ), antiproliferative) _ malignant melanoma, renal cell carcinoma, hairy cell leukemia, Kaposi’s sarcoma _B- Interferon Beta (prod. by fibroblasts) _(antiviral, antiproliferative) _relapsing type Multiple Sclerosis _Type-II _Interferon Gamma (prod. by lymphocytes) _(stimulates NK cells and macrophages) _chronic granulomatous disease
Interferon _Type-I _A- Interferon Alpha (prod. by leukocytes) _ (antiviral (hepatitis C, interferon alfa-2 b ), antiproliferative) _ malignant melanoma, renal cell carcinoma, hairy cell leukemia, Kaposi’s sarcoma _B- Interferon Beta (prod. by fibroblasts) _(antiviral, antiproliferative) _relapsing type Multiple Sclerosis _Type-II _Interferon Gamma (prod. by lymphocytes) _(stimulates NK cells and macrophages) _chronic granulomatous disease
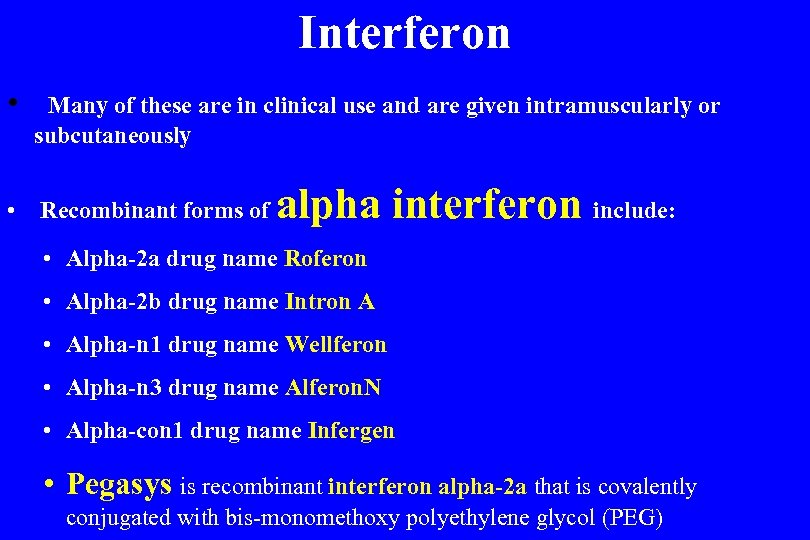 Interferon • Many of these are in clinical use and are given intramuscularly or subcutaneously • Recombinant forms of alpha interferon include: • Alpha-2 a drug name Roferon • Alpha-2 b drug name Intron A • Alpha-n 1 drug name Wellferon • Alpha-n 3 drug name Alferon. N • Alpha-con 1 drug name Infergen • Pegasys is recombinant interferon alpha-2 a that is covalently conjugated with bis-monomethoxy polyethylene glycol (PEG)
Interferon • Many of these are in clinical use and are given intramuscularly or subcutaneously • Recombinant forms of alpha interferon include: • Alpha-2 a drug name Roferon • Alpha-2 b drug name Intron A • Alpha-n 1 drug name Wellferon • Alpha-n 3 drug name Alferon. N • Alpha-con 1 drug name Infergen • Pegasys is recombinant interferon alpha-2 a that is covalently conjugated with bis-monomethoxy polyethylene glycol (PEG)
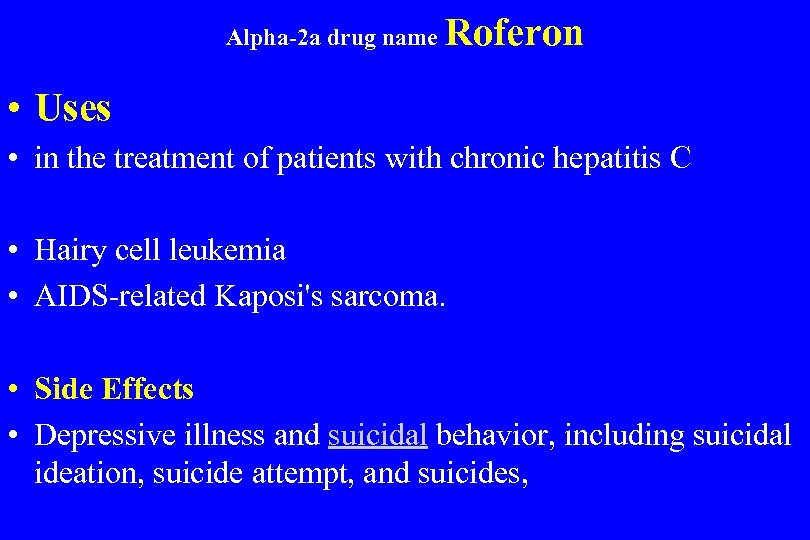 Alpha-2 a drug name Roferon • Uses • in the treatment of patients with chronic hepatitis C • Hairy cell leukemia • AIDS-related Kaposi's sarcoma. • Side Effects • Depressive illness and suicidal behavior, including suicidal ideation, suicide attempt, and suicides,
Alpha-2 a drug name Roferon • Uses • in the treatment of patients with chronic hepatitis C • Hairy cell leukemia • AIDS-related Kaposi's sarcoma. • Side Effects • Depressive illness and suicidal behavior, including suicidal ideation, suicide attempt, and suicides,
 Interferon • Recombinant forms of beta interferon include: • Beta-1 a drug name Avonex • Beta-1 b drug name Betaseron • Recombinant forms of gamma interferon include: • Interferon Gamma (Actimmunex®)
Interferon • Recombinant forms of beta interferon include: • Beta-1 a drug name Avonex • Beta-1 b drug name Betaseron • Recombinant forms of gamma interferon include: • Interferon Gamma (Actimmunex®)
 Interferon Beta Mechanism of Action Reduce the production of the TNFa , known to induce damage to myelin Reduce inflammation by: – Switching cytokine production from type 1 (pro-inflammatory) to type 2 (anti-inflammatory) cells – Decrease antigen presentation, to reduce the attack on myelin Reduce the ability of immune cells to cross the blood-brain barrier,
Interferon Beta Mechanism of Action Reduce the production of the TNFa , known to induce damage to myelin Reduce inflammation by: – Switching cytokine production from type 1 (pro-inflammatory) to type 2 (anti-inflammatory) cells – Decrease antigen presentation, to reduce the attack on myelin Reduce the ability of immune cells to cross the blood-brain barrier,
 Interferons : Avonex (Interferon -1 a) manufacture by biogen, usa Indication: relapsing forms of MS Dose: 30 mcg IM once weekly Reduces rate of clinical relapse Reduces the development of new lesions May delay progression of disability
Interferons : Avonex (Interferon -1 a) manufacture by biogen, usa Indication: relapsing forms of MS Dose: 30 mcg IM once weekly Reduces rate of clinical relapse Reduces the development of new lesions May delay progression of disability
 Interferons : Rebif (Interferon -1 a) Interferon -1 a Indication: relapsing/remitting forms of MS Dose: 22 or 44 mcg SC 3 times per week Decreases frequency of relapse Delays the increase in the volume of lesions May delay progression of disability
Interferons : Rebif (Interferon -1 a) Interferon -1 a Indication: relapsing/remitting forms of MS Dose: 22 or 44 mcg SC 3 times per week Decreases frequency of relapse Delays the increase in the volume of lesions May delay progression of disability
 Interferons : Betaseron (interferon beta-1 b Bayer Health. Care Pharmaceuticals Indication: Relapsing forms of MS Dose: 8 million IU SC every other day Reduces rate of clinical relapse Reduces the development of new lesions Delays the increase in the volume of lesions
Interferons : Betaseron (interferon beta-1 b Bayer Health. Care Pharmaceuticals Indication: Relapsing forms of MS Dose: 8 million IU SC every other day Reduces rate of clinical relapse Reduces the development of new lesions Delays the increase in the volume of lesions
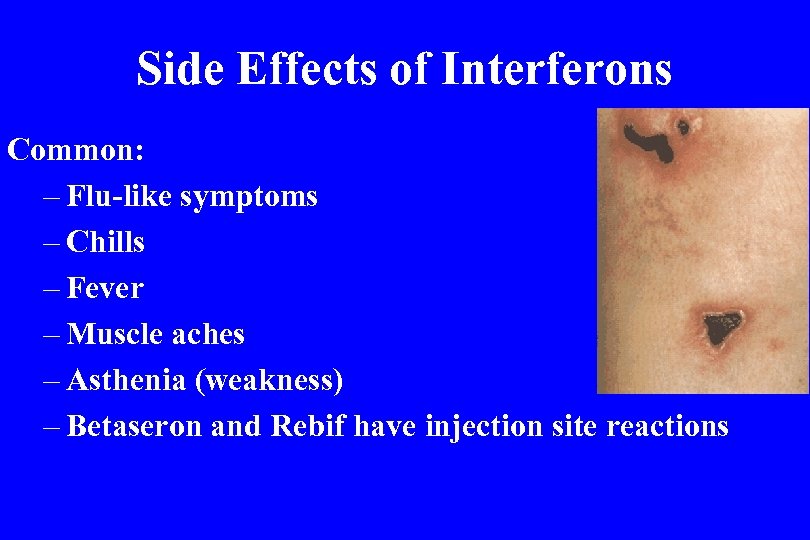 Side Effects of Interferons Common: – Flu-like symptoms – Chills – Fever – Muscle aches – Asthenia (weakness) – Betaseron and Rebif have injection site reactions
Side Effects of Interferons Common: – Flu-like symptoms – Chills – Fever – Muscle aches – Asthenia (weakness) – Betaseron and Rebif have injection site reactions
 Side Effects of Interferons Uncommon: – Severe depression – Suicide – Seizures – Cardiac effects – Anemia – Elevated liver enzymes – Severe hepatic injury, including cases of hepatic failure, has been reported in patients taking Avonex
Side Effects of Interferons Uncommon: – Severe depression – Suicide – Seizures – Cardiac effects – Anemia – Elevated liver enzymes – Severe hepatic injury, including cases of hepatic failure, has been reported in patients taking Avonex
 CARDIOVASCULAR CONCERN IN ORAL SURGERY • • • RISK ASSESSMENT One widely used method of expressing medical risk is the American Society of Anesthesiologists (ASA) This system originally was developed to classify patients according to perioperative risk with general anesthesia; • • it has been adapted for outpatient medical and dental use and for all types of surgical and nonsurgical procedures, regardless of the type of anesthesia used.
CARDIOVASCULAR CONCERN IN ORAL SURGERY • • • RISK ASSESSMENT One widely used method of expressing medical risk is the American Society of Anesthesiologists (ASA) This system originally was developed to classify patients according to perioperative risk with general anesthesia; • • it has been adapted for outpatient medical and dental use and for all types of surgical and nonsurgical procedures, regardless of the type of anesthesia used.
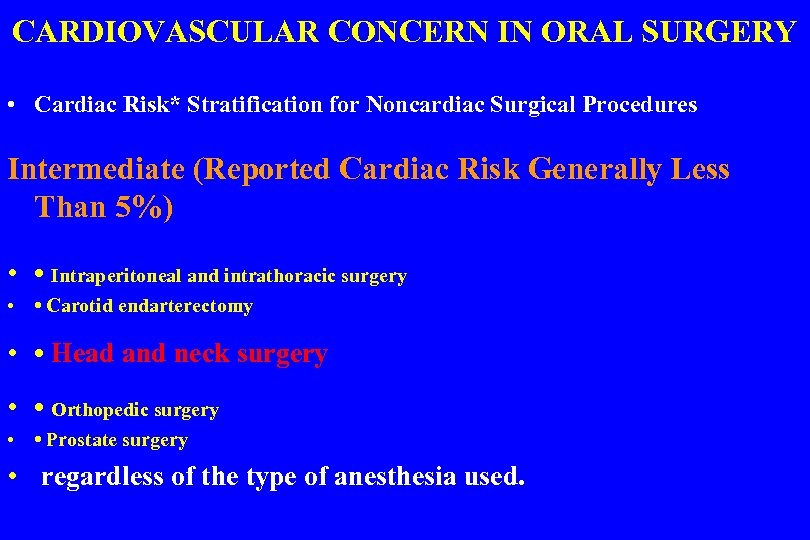 CARDIOVASCULAR CONCERN IN ORAL SURGERY • Cardiac Risk* Stratification for Noncardiac Surgical Procedures Intermediate (Reported Cardiac Risk Generally Less Than 5%) • • Intraperitoneal and intrathoracic surgery • • Carotid endarterectomy • • Head and neck surgery • • Orthopedic surgery • • Prostate surgery • regardless of the type of anesthesia used.
CARDIOVASCULAR CONCERN IN ORAL SURGERY • Cardiac Risk* Stratification for Noncardiac Surgical Procedures Intermediate (Reported Cardiac Risk Generally Less Than 5%) • • Intraperitoneal and intrathoracic surgery • • Carotid endarterectomy • • Head and neck surgery • • Orthopedic surgery • • Prostate surgery • regardless of the type of anesthesia used.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY The classification is as follows: • ASA III • ASA IV • ASA V
CARDIOVASCULAR CONCERN IN ORAL SURGERY The classification is as follows: • ASA III • ASA IV • ASA V
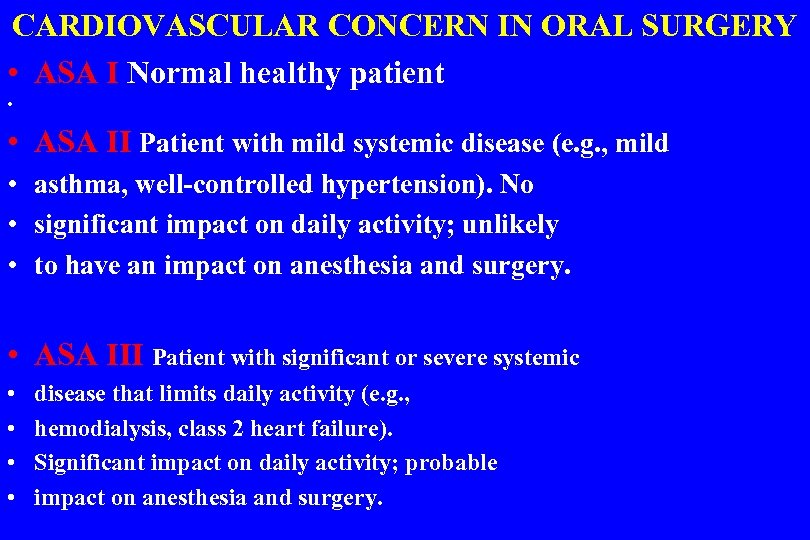 CARDIOVASCULAR CONCERN IN ORAL SURGERY • ASA I Normal healthy patient • • ASA II Patient with mild systemic disease (e. g. , mild • asthma, well-controlled hypertension). No • significant impact on daily activity; unlikely • to have an impact on anesthesia and surgery. • ASA III Patient with significant or severe systemic • • disease that limits daily activity (e. g. , hemodialysis, class 2 heart failure). Significant impact on daily activity; probable impact on anesthesia and surgery.
CARDIOVASCULAR CONCERN IN ORAL SURGERY • ASA I Normal healthy patient • • ASA II Patient with mild systemic disease (e. g. , mild • asthma, well-controlled hypertension). No • significant impact on daily activity; unlikely • to have an impact on anesthesia and surgery. • ASA III Patient with significant or severe systemic • • disease that limits daily activity (e. g. , hemodialysis, class 2 heart failure). Significant impact on daily activity; probable impact on anesthesia and surgery.
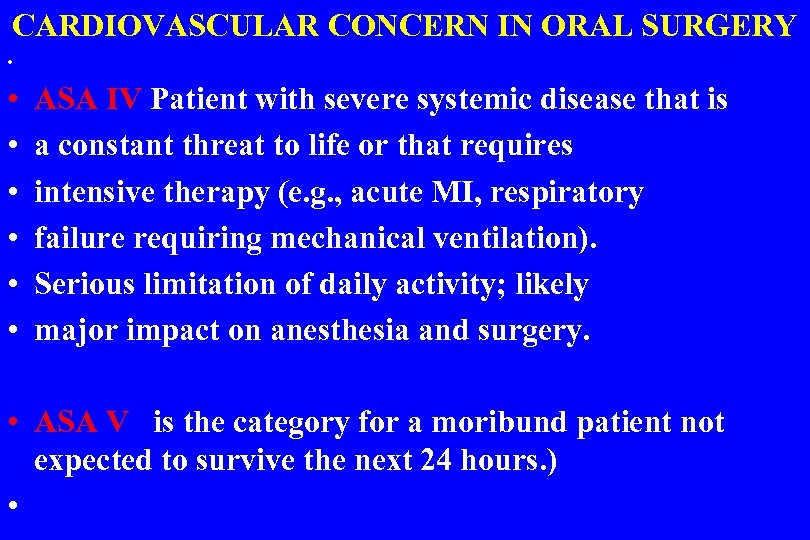 CARDIOVASCULAR CONCERN IN ORAL SURGERY • • ASA IV Patient with severe systemic disease that is a constant threat to life or that requires intensive therapy (e. g. , acute MI, respiratory failure requiring mechanical ventilation). Serious limitation of daily activity; likely major impact on anesthesia and surgery. • ASA V is the category for a moribund patient not expected to survive the next 24 hours. ) •
CARDIOVASCULAR CONCERN IN ORAL SURGERY • • ASA IV Patient with severe systemic disease that is a constant threat to life or that requires intensive therapy (e. g. , acute MI, respiratory failure requiring mechanical ventilation). Serious limitation of daily activity; likely major impact on anesthesia and surgery. • ASA V is the category for a moribund patient not expected to survive the next 24 hours. ) •
 CARDIOVASCULAR CONCERN IN ORAL SURGERY • Although it generally is helpful to classify patients using the ASA system, • the usefulness of this system is limited. Risk assessment more practically involves the evaluation of four components: 1 • The nature, severity, control, and stability of the patient’s medical condition as determined by the initial evaluation 2 • The functional capacity or ability of the patient to respond to a physical or an emotional demand
CARDIOVASCULAR CONCERN IN ORAL SURGERY • Although it generally is helpful to classify patients using the ASA system, • the usefulness of this system is limited. Risk assessment more practically involves the evaluation of four components: 1 • The nature, severity, control, and stability of the patient’s medical condition as determined by the initial evaluation 2 • The functional capacity or ability of the patient to respond to a physical or an emotional demand
 CARDIOVASCULAR CONCERN IN ORAL SURGERY Risk assessment more practically involves the evaluation of four components: 3 • The emotional status of the patient 4 • The type and magnitude of the planned procedure (invasive or noninvasive) All factors must be carefully weighed for each patient, to determine an accurate risk profile Risk assessment cannot be approached as a cookbook exercise.
CARDIOVASCULAR CONCERN IN ORAL SURGERY Risk assessment more practically involves the evaluation of four components: 3 • The emotional status of the patient 4 • The type and magnitude of the planned procedure (invasive or noninvasive) All factors must be carefully weighed for each patient, to determine an accurate risk profile Risk assessment cannot be approached as a cookbook exercise.
 • GENERAL TREATMENT MODIFICATIONS • Goal is to reduce that risk as much as possible. The dentist should always try to anticipate possible urgencies or emergencies and be prepared to manage them if they arise. • 1 • Giving prophylactic antibiotics before dental procedure in a patient at risk for infective endocarditis • 2 • Determining the international normalized ratio (INR) before surgery in a patient taking warfarin (Coumadin) • 3 • Ensuring food intake before dental treatment in in a diabetic patient on insulin
• GENERAL TREATMENT MODIFICATIONS • Goal is to reduce that risk as much as possible. The dentist should always try to anticipate possible urgencies or emergencies and be prepared to manage them if they arise. • 1 • Giving prophylactic antibiotics before dental procedure in a patient at risk for infective endocarditis • 2 • Determining the international normalized ratio (INR) before surgery in a patient taking warfarin (Coumadin) • 3 • Ensuring food intake before dental treatment in in a diabetic patient on insulin
 • TREATMENT MODIFICATIONS • 4 - Prescribing an anxiolytic drug for an anxious patient with stable angina • 5 - Limiting the amount of vasoconstrictor in a patient who takes a nonselective beta blocker • 6 - Administering nitrous oxide–oxygen to an anxious patient with poorly controlled hypertension • 7 - Using an upright chair position for a patient with heart failure • 8 - Avoiding the use of electrosurgery in a patient with a pacemaker
• TREATMENT MODIFICATIONS • 4 - Prescribing an anxiolytic drug for an anxious patient with stable angina • 5 - Limiting the amount of vasoconstrictor in a patient who takes a nonselective beta blocker • 6 - Administering nitrous oxide–oxygen to an anxious patient with poorly controlled hypertension • 7 - Using an upright chair position for a patient with heart failure • 8 - Avoiding the use of electrosurgery in a patient with a pacemaker
 • GENERAL TREATMENT MODIFICATIONS • 9 • Avoiding elective radiographs in a pregnant patient • 10 • Using additional local measures for hemostasis in a patient taking sodium warfarin (Coumadin) • 11 • Prescribing antibiotics for periodontal disease after extractions in a patient with poorly controlled diabetes
• GENERAL TREATMENT MODIFICATIONS • 9 • Avoiding elective radiographs in a pregnant patient • 10 • Using additional local measures for hemostasis in a patient taking sodium warfarin (Coumadin) • 11 • Prescribing antibiotics for periodontal disease after extractions in a patient with poorly controlled diabetes
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis 2 - Hypertension 3 - Ischemic Heart Disease Angina and Myocardial infarction 4 - Cardiac Arrhythmias 5 - Heart Failure (CHF)
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis 2 - Hypertension 3 - Ischemic Heart Disease Angina and Myocardial infarction 4 - Cardiac Arrhythmias 5 - Heart Failure (CHF)
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis • ETIOLOGY • About 90% of community-acquired cases of native valve • IE are due to streptococci, staphylococci, or enterococci, • with streptococci being the most common causative organisms.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis • ETIOLOGY • About 90% of community-acquired cases of native valve • IE are due to streptococci, staphylococci, or enterococci, • with streptococci being the most common causative organisms.
 CARDIOVASCULAR DISEASES 1 - Infective Endocarditis In IE associated with intravenous drug abuse • or secondary to health care contact • Streptococci continue to be the most common cause of IE • staphylococci have been gaining increasing importance. • Viridans streptococci (α-hemolytic streptococci), constituents of the normal oral flora and gastrointestinal • (GI) tract, remain the most common cause of community acquired native valve endocarditis they cause 30% to 65% of cases of IE
CARDIOVASCULAR DISEASES 1 - Infective Endocarditis In IE associated with intravenous drug abuse • or secondary to health care contact • Streptococci continue to be the most common cause of IE • staphylococci have been gaining increasing importance. • Viridans streptococci (α-hemolytic streptococci), constituents of the normal oral flora and gastrointestinal • (GI) tract, remain the most common cause of community acquired native valve endocarditis they cause 30% to 65% of cases of IE
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis • Underlying Condition Frequency of IE • Mitral valve prolapse 25 -30% • Aortic valve disease 12 -30% • Congenital heart disease 10 -20% • Prosthetic valve 10 -30% • Intravenous drug abuse 5 -20% •
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 1 - Infective Endocarditis • Underlying Condition Frequency of IE • Mitral valve prolapse 25 -30% • Aortic valve disease 12 -30% • Congenital heart disease 10 -20% • Prosthetic valve 10 -30% • Intravenous drug abuse 5 -20% •
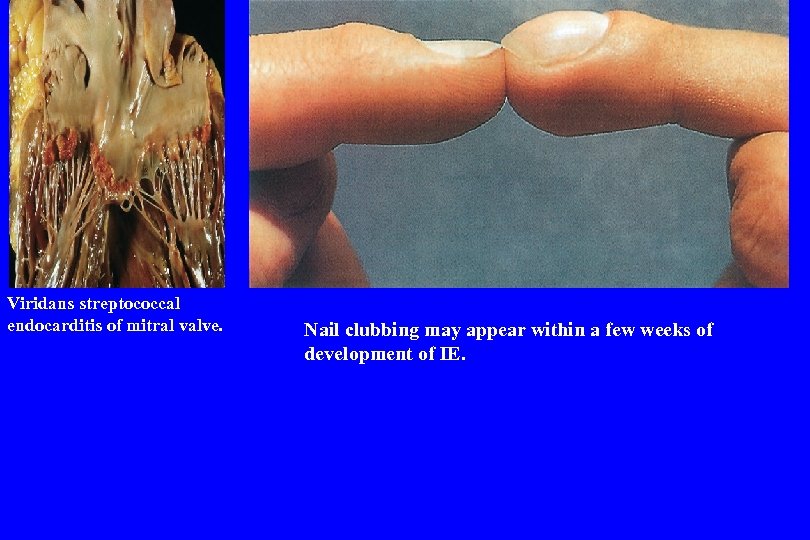 Viridans streptococcal endocarditis of mitral valve. Nail clubbing may appear within a few weeks of development of IE.
Viridans streptococcal endocarditis of mitral valve. Nail clubbing may appear within a few weeks of development of IE.
 • 1 - Infective Endocarditis • Definitive diagnosis of IE requires the presence of: • 1 - two major criteria • 2 - or one major and three minor criteria • 3 - or five minor criteria
• 1 - Infective Endocarditis • Definitive diagnosis of IE requires the presence of: • 1 - two major criteria • 2 - or one major and three minor criteria • 3 - or five minor criteria
 • 1 - Infective Endocarditis • Major criteria : 1 - Positive blood cultures 2 - Evidence of endocardial involvement such as: Positive findings on echocardiography presence of new valvular Regurgitation
• 1 - Infective Endocarditis • Major criteria : 1 - Positive blood cultures 2 - Evidence of endocardial involvement such as: Positive findings on echocardiography presence of new valvular Regurgitation
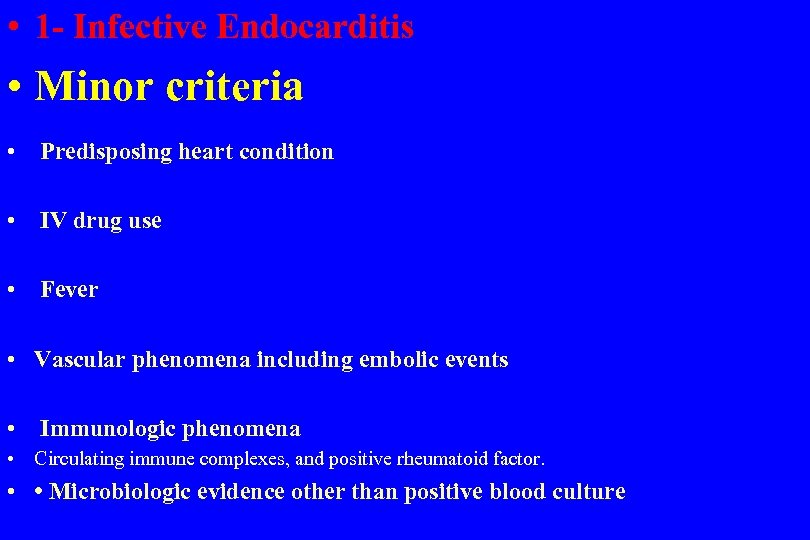 • 1 - Infective Endocarditis • Minor criteria • Predisposing heart condition • IV drug use • Fever • Vascular phenomena including embolic events • Immunologic phenomena • Circulating immune complexes, and positive rheumatoid factor. • • Microbiologic evidence other than positive blood culture
• 1 - Infective Endocarditis • Minor criteria • Predisposing heart condition • IV drug use • Fever • Vascular phenomena including embolic events • Immunologic phenomena • Circulating immune complexes, and positive rheumatoid factor. • • Microbiologic evidence other than positive blood culture
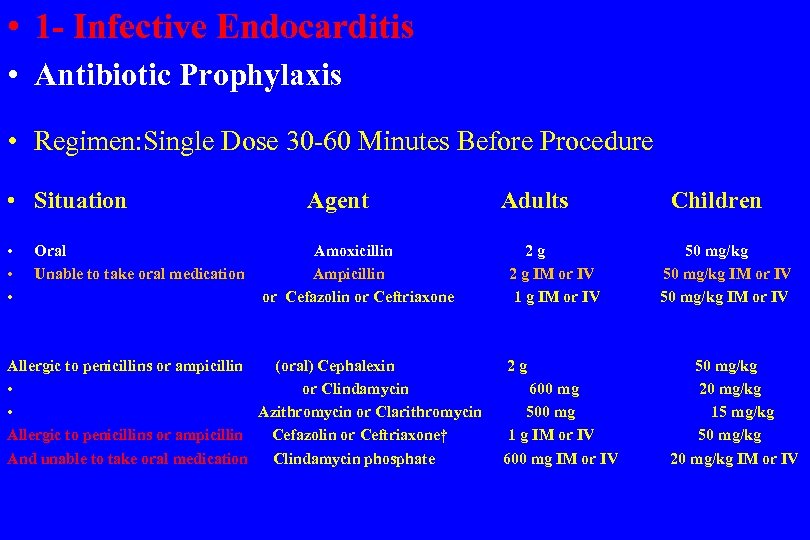 • 1 - Infective Endocarditis • Antibiotic Prophylaxis • Regimen: Single Dose 30 -60 Minutes Before Procedure • Situation Agent Adults Children • • • Oral Amoxicillin 2 g 50 mg/kg Unable to take oral medication Ampicillin 2 g IM or IV 50 mg/kg IM or IV or Cefazolin or Ceftriaxone 1 g IM or IV 50 mg/kg IM or IV Allergic to penicillins or ampicillin (oral) Cephalexin 2 g 50 mg/kg • or Clindamycin 600 mg 20 mg/kg • Azithromycin or Clarithromycin 500 mg 15 mg/kg Allergic to penicillins or ampicillin Cefazolin or Ceftriaxone† 1 g IM or IV 50 mg/kg And unable to take oral medication Clindamycin phosphate 600 mg IM or IV 20 mg/kg IM or IV
• 1 - Infective Endocarditis • Antibiotic Prophylaxis • Regimen: Single Dose 30 -60 Minutes Before Procedure • Situation Agent Adults Children • • • Oral Amoxicillin 2 g 50 mg/kg Unable to take oral medication Ampicillin 2 g IM or IV 50 mg/kg IM or IV or Cefazolin or Ceftriaxone 1 g IM or IV 50 mg/kg IM or IV Allergic to penicillins or ampicillin (oral) Cephalexin 2 g 50 mg/kg • or Clindamycin 600 mg 20 mg/kg • Azithromycin or Clarithromycin 500 mg 15 mg/kg Allergic to penicillins or ampicillin Cefazolin or Ceftriaxone† 1 g IM or IV 50 mg/kg And unable to take oral medication Clindamycin phosphate 600 mg IM or IV 20 mg/kg IM or IV
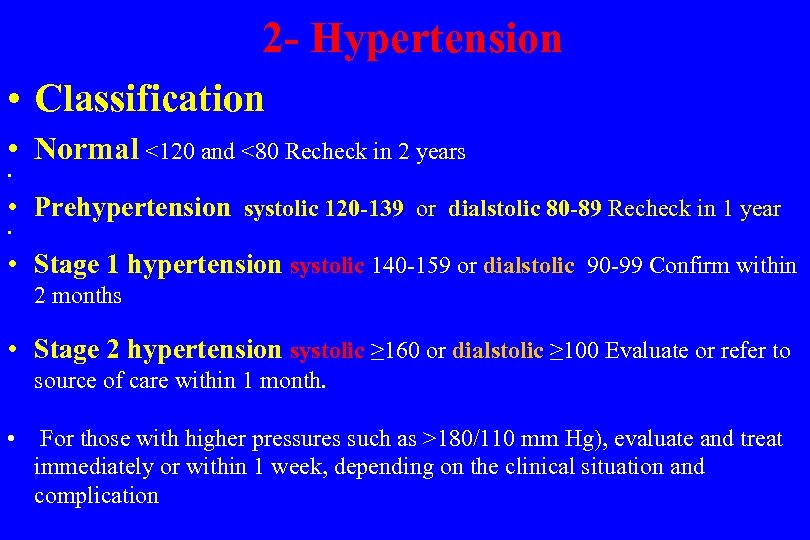 2 - Hypertension • Classification • Normal <120 and <80 Recheck in 2 years • • Prehypertension systolic 120 -139 or dialstolic 80 -89 Recheck in 1 year • • Stage 1 hypertension systolic 140 -159 or dialstolic 90 -99 Confirm within 2 months • Stage 2 hypertension systolic ≥ 160 or dialstolic ≥ 100 Evaluate or refer to source of care within 1 month. • For those with higher pressures such as >180/110 mm Hg), evaluate and treat immediately or within 1 week, depending on the clinical situation and complication
2 - Hypertension • Classification • Normal <120 and <80 Recheck in 2 years • • Prehypertension systolic 120 -139 or dialstolic 80 -89 Recheck in 1 year • • Stage 1 hypertension systolic 140 -159 or dialstolic 90 -99 Confirm within 2 months • Stage 2 hypertension systolic ≥ 160 or dialstolic ≥ 100 Evaluate or refer to source of care within 1 month. • For those with higher pressures such as >180/110 mm Hg), evaluate and treat immediately or within 1 week, depending on the clinical situation and complication
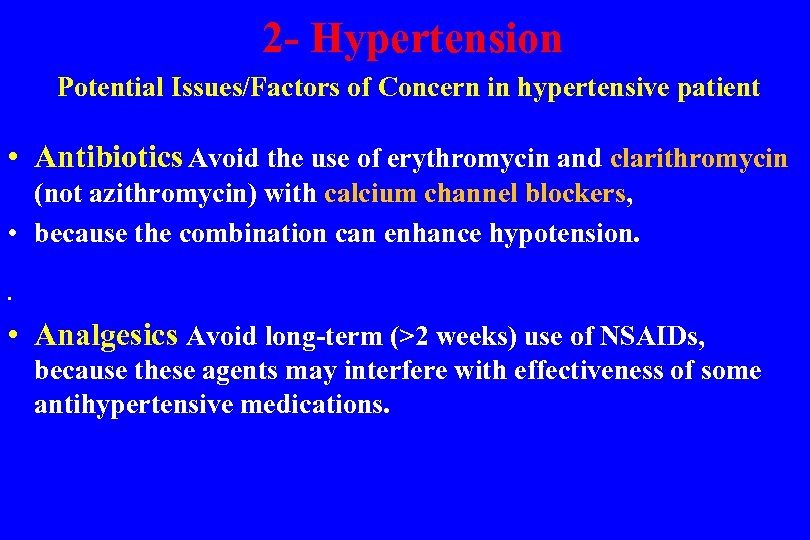 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Antibiotics Avoid the use of erythromycin and clarithromycin (not azithromycin) with calcium channel blockers, • because the combination can enhance hypotension. • • Analgesics Avoid long-term (>2 weeks) use of NSAIDs, because these agents may interfere with effectiveness of some antihypertensive medications.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Antibiotics Avoid the use of erythromycin and clarithromycin (not azithromycin) with calcium channel blockers, • because the combination can enhance hypotension. • • Analgesics Avoid long-term (>2 weeks) use of NSAIDs, because these agents may interfere with effectiveness of some antihypertensive medications.
 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Anesthesia Modest doses of local anesthetic with 1 : 100, 000 • or 1 : 200, 000 epinephrine (e. g. , 1 or 2 carpules) at a given time are of little clinical consequence in patients with blood pressure <180/110 mm Hg. • Greater quantities may be tolerated reasonably well, but with increased risk.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Anesthesia Modest doses of local anesthetic with 1 : 100, 000 • or 1 : 200, 000 epinephrine (e. g. , 1 or 2 carpules) at a given time are of little clinical consequence in patients with blood pressure <180/110 mm Hg. • Greater quantities may be tolerated reasonably well, but with increased risk.
 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Anesthesia • Levonordefrin should be avoided. In patients with uncontrolled hypertension (blood pressure >180/110 mm Hg), Levonordefrin is a sympathomimetic amine used as a vasoconstrictor in local anesthetic solutions. It has pharmacologic activity similar to that of epinephrine but is more stable. In equal concentrations, levonordefrin is less potent than epinephrine in raising blood pressure, and as a vasoconstrictor • the use of epinephrine may be tolerated but should be discussed with the physician.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Anesthesia • Levonordefrin should be avoided. In patients with uncontrolled hypertension (blood pressure >180/110 mm Hg), Levonordefrin is a sympathomimetic amine used as a vasoconstrictor in local anesthetic solutions. It has pharmacologic activity similar to that of epinephrine but is more stable. In equal concentrations, levonordefrin is less potent than epinephrine in raising blood pressure, and as a vasoconstrictor • the use of epinephrine may be tolerated but should be discussed with the physician.
 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Allergies No issues • Anxiety Patients with hypertension who are anxious or fearful are especially good candidates for preoperative oral and/or intraoperative inhalation sedation. • Apply good stress management protocols. • • Bleeding Excessive bleeding due to hypertension is possible BUT UNLIKELY.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Allergies No issues • Anxiety Patients with hypertension who are anxious or fearful are especially good candidates for preoperative oral and/or intraoperative inhalation sedation. • Apply good stress management protocols. • • Bleeding Excessive bleeding due to hypertension is possible BUT UNLIKELY.
 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Blood pressure • • Patients with a blood presure <180/110 mm Hg may receive any necessary dental treatment. • For patients with a pressure reading >180/110 mm Hg, • dental treatment should be deferred until blood pressure is brought under control. • If urgent or emergency dental treatment is required, it should be done in as limited and conservative a manner as possible.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Blood pressure • • Patients with a blood presure <180/110 mm Hg may receive any necessary dental treatment. • For patients with a pressure reading >180/110 mm Hg, • dental treatment should be deferred until blood pressure is brought under control. • If urgent or emergency dental treatment is required, it should be done in as limited and conservative a manner as possible.
 2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Chair position • Avoid rapid position changes owing to possibility • of antihypertensive drug-associated orthostatic hypotension • Drugs The nonselective β-adrenergic blockers can potentially interact with epinephrine, but such interaction is dose dependent • and very unlikely to occur at the usual doses. • Devices For patients with stage II hypertension (blood • pressure >160/100 mm Hg), periodic monitoring of • pressure during treatment may be advisable.
2 - Hypertension Potential Issues/Factors of Concern in hypertensive patient • Chair position • Avoid rapid position changes owing to possibility • of antihypertensive drug-associated orthostatic hypotension • Drugs The nonselective β-adrenergic blockers can potentially interact with epinephrine, but such interaction is dose dependent • and very unlikely to occur at the usual doses. • Devices For patients with stage II hypertension (blood • pressure >160/100 mm Hg), periodic monitoring of • pressure during treatment may be advisable.
 2 - Hypertension • Use of Vasoconstrictors. • • The effectiveness of local anesthesia is enhanced by the inclusion of a vasoconstrictor in the local anesthetic solution, which: 1 - delays systemic absorption 2 - increases the duration of anesthesia 3 - provides local hemostasis. 4 - Decrease systemic toxicity by minimizing systemic absorption.
2 - Hypertension • Use of Vasoconstrictors. • • The effectiveness of local anesthesia is enhanced by the inclusion of a vasoconstrictor in the local anesthetic solution, which: 1 - delays systemic absorption 2 - increases the duration of anesthesia 3 - provides local hemostasis. 4 - Decrease systemic toxicity by minimizing systemic absorption.
 2 - Hypertension • Use of Vasoconstrictors. • • the use of local anesthetic with a vasoconstrictor in a patient with hypertension could result in a potentially serious spike in blood pressure. • • The cardiovascular response to conventional doses of injected epinephrine, both in patients who are healthy and in those with hypertension, usually is of little clinical importance
2 - Hypertension • Use of Vasoconstrictors. • • the use of local anesthetic with a vasoconstrictor in a patient with hypertension could result in a potentially serious spike in blood pressure. • • The cardiovascular response to conventional doses of injected epinephrine, both in patients who are healthy and in those with hypertension, usually is of little clinical importance
 2 - Hypertension • Use of Vasoconstrictors. • • small doses such as those contained in one or • two cartridges of lidocaine with 1 : 100, 000 epinephrine • cause minimal physiologic changes. • This fact is due to a preponderance of action among β 2 receptor • and a decrease in diastolic pressure • Which leads to unchange in arterial pressure with only a • minimal increase in heart rate.
2 - Hypertension • Use of Vasoconstrictors. • • small doses such as those contained in one or • two cartridges of lidocaine with 1 : 100, 000 epinephrine • cause minimal physiologic changes. • This fact is due to a preponderance of action among β 2 receptor • and a decrease in diastolic pressure • Which leads to unchange in arterial pressure with only a • minimal increase in heart rate.
 2 - Hypertension • Use of Vasoconstrictors. • • . After injection of 1. 8 m. L (one cartridge • 2% lidocaine with 1 : 100, 000 epinephrine • CAUSES no significant changes in heart rate or blood pressure. • Three cartridges injection causes significant increases in heart rate and systolic blood pressure • but with no adverse symptoms or sequelae.
2 - Hypertension • Use of Vasoconstrictors. • • . After injection of 1. 8 m. L (one cartridge • 2% lidocaine with 1 : 100, 000 epinephrine • CAUSES no significant changes in heart rate or blood pressure. • Three cartridges injection causes significant increases in heart rate and systolic blood pressure • but with no adverse symptoms or sequelae.
 2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, • however, because of its comparative excessive α 1 • stimulation. • The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in whom elective dental care should be deferred. • the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time
2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, • however, because of its comparative excessive α 1 • stimulation. • The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in whom elective dental care should be deferred. • the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time
 2 - Hypertension • Use of Vasoconstrictors. • care is taken to avoid inadvertent intravascular injection. • Consultation with the patient’s physician is advisable before a definitive decision is made. • An additional concern when patients with hypertension are treated is the potential for adverse drug interactions between vasoconstrictors and antihypertensive
2 - Hypertension • Use of Vasoconstrictors. • care is taken to avoid inadvertent intravascular injection. • Consultation with the patient’s physician is advisable before a definitive decision is made. • An additional concern when patients with hypertension are treated is the potential for adverse drug interactions between vasoconstrictors and antihypertensive
 2 - Hypertension • Use of Vasoconstrictors. • drugs—specifically, the nonselective β-adrenergic blocking agents. • The basis for concern with use of nonselective β-adrenergic blocking agents (e. g. , propranolol) is that the normal compensatory vasodilatation of skeletal muscle vasculature mediated by β 2 receptors is inhibited by these drugs • and injection of epinephrine, levonordefrin, or any other pressor agent may result in uncompensated peripheral vasoconstriction.
2 - Hypertension • Use of Vasoconstrictors. • drugs—specifically, the nonselective β-adrenergic blocking agents. • The basis for concern with use of nonselective β-adrenergic blocking agents (e. g. , propranolol) is that the normal compensatory vasodilatation of skeletal muscle vasculature mediated by β 2 receptors is inhibited by these drugs • and injection of epinephrine, levonordefrin, or any other pressor agent may result in uncompensated peripheral vasoconstriction.
 2 - Hypertension • Use of Vasoconstrictors. • because of unopposed stimulation of α 1 receptors. This vasoconstrictive effect could potentially cause a significant elevation in blood pressure and a compensatory bradycardia. • Adverse interactions are even less likely to occur in patients who take cardioselective beta blockers. • epinephrine in small doses of one to two cartridges containing • 1 : 100, 000 epinephrine can be used safely.
2 - Hypertension • Use of Vasoconstrictors. • because of unopposed stimulation of α 1 receptors. This vasoconstrictive effect could potentially cause a significant elevation in blood pressure and a compensatory bradycardia. • Adverse interactions are even less likely to occur in patients who take cardioselective beta blockers. • epinephrine in small doses of one to two cartridges containing • 1 : 100, 000 epinephrine can be used safely.
 2 - Hypertension • Use of Vasoconstrictors. • levonordefrin should be avoided with beta blockers • . Topical vasoconstrictors generally should not be used for local • hemostasis in patients with hypertension. • When performing crown and bridge procedures for patients • with hypertension
2 - Hypertension • Use of Vasoconstrictors. • levonordefrin should be avoided with beta blockers • . Topical vasoconstrictors generally should not be used for local • hemostasis in patients with hypertension. • When performing crown and bridge procedures for patients • with hypertension
 2 - Hypertension • Use of Vasoconstrictors. • the dentist should avoid using gingival retraction cord that contains epinephrine • because this material contains highly concentrated epinephrine, which can be quickly absorbed through abraided gingival • sulcus tissues, • resulting in tachycardia and elevated blood pressure.
2 - Hypertension • Use of Vasoconstrictors. • the dentist should avoid using gingival retraction cord that contains epinephrine • because this material contains highly concentrated epinephrine, which can be quickly absorbed through abraided gingival • sulcus tissues, • resulting in tachycardia and elevated blood pressure.
 2 - Hypertension • Use of Vasoconstrictors. • tetrahydrozoline (Visine) , oxymetazoline (Afrin); and phenylephrine (Neo-Synephrine • may be used to soak the cord, providing hemostatic effects similar to those obtained with epinephrine but with minimal cardiovascular • Several other effects are of concern with antihypertensive agents and dental management
2 - Hypertension • Use of Vasoconstrictors. • tetrahydrozoline (Visine) , oxymetazoline (Afrin); and phenylephrine (Neo-Synephrine • may be used to soak the cord, providing hemostatic effects similar to those obtained with epinephrine but with minimal cardiovascular • Several other effects are of concern with antihypertensive agents and dental management
 2 - Hypertension • Use of Vasoconstrictors. • Some antihypertensive agents, especially alpha blockers, alphabeta blockers, and diuretics, may predispose patients to development of orthostatic hypotension • and potentiate the actions of anxiolytic and sedative drugs. • Erythromycin and clarithromycin can exacerbate the hypotensive effect of calcium channel blockers.
2 - Hypertension • Use of Vasoconstrictors. • Some antihypertensive agents, especially alpha blockers, alphabeta blockers, and diuretics, may predispose patients to development of orthostatic hypotension • and potentiate the actions of anxiolytic and sedative drugs. • Erythromycin and clarithromycin can exacerbate the hypotensive effect of calcium channel blockers.
 2 - Hypertension • Use of Vasoconstrictors. • Anxiolytics and sedatives may be used for patients who take these antihypertensive medications • however, the usual dosage may need to be reduced. • The efficacy of antihypertensive drugs may be decreased by the prolonged use of nonsteroidal antiinflammatory drugs—an interaction that should be considered if these drugs are used for analgesia, • although the use of nonsteroidal antiinflammatory drugs for a few days is of little clinical importance.
2 - Hypertension • Use of Vasoconstrictors. • Anxiolytics and sedatives may be used for patients who take these antihypertensive medications • however, the usual dosage may need to be reduced. • The efficacy of antihypertensive drugs may be decreased by the prolonged use of nonsteroidal antiinflammatory drugs—an interaction that should be considered if these drugs are used for analgesia, • although the use of nonsteroidal antiinflammatory drugs for a few days is of little clinical importance.
 2 - Hypertension • Use of Vasoconstrictors. • • the use of local anesthetic with a vasoconstrictor in a patient with hypertension could result in a potentially serious spike in blood pressure. • • The cardiovascular response to conventional doses of injected epinephrine, both in patients who are healthy and in those with hypertension, usually is of little clinical importance.
2 - Hypertension • Use of Vasoconstrictors. • • the use of local anesthetic with a vasoconstrictor in a patient with hypertension could result in a potentially serious spike in blood pressure. • • The cardiovascular response to conventional doses of injected epinephrine, both in patients who are healthy and in those with hypertension, usually is of little clinical importance.
 2 - Hypertension • Use of Vasoconstrictors. • • small doses such as those contained in one or • two cartridges of lidocaine with 1 : 100, 000 epinephrine • cause minimal physiologic changes. • This fact is due to a preponderance of action among β 2 receptors and a decrease in diastolic pressure; thus, mean • arterial pressure is essentially unchanged, with only a • minimal increase in heart rate.
2 - Hypertension • Use of Vasoconstrictors. • • small doses such as those contained in one or • two cartridges of lidocaine with 1 : 100, 000 epinephrine • cause minimal physiologic changes. • This fact is due to a preponderance of action among β 2 receptors and a decrease in diastolic pressure; thus, mean • arterial pressure is essentially unchanged, with only a • minimal increase in heart rate.
 2 - Hypertension • Use of Vasoconstrictors. • Three cartridges were accompanied by significant increases in heart rate and systolic blood pressure, but with no adverse symptoms or sequelae • modest doses (one or two cartridges of 2% lidocaine with 1 : 100, 000 epinephrine) carries little clinical risk in
2 - Hypertension • Use of Vasoconstrictors. • Three cartridges were accompanied by significant increases in heart rate and systolic blood pressure, but with no adverse symptoms or sequelae • modest doses (one or two cartridges of 2% lidocaine with 1 : 100, 000 epinephrine) carries little clinical risk in
 2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, however, because of its comparative excessive α 1 stimulation. The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in • whom elective dental care should be deferred. • If urgent treatment becomes necessary, however, a decision must be made regarding the use of epinephrine, which will be dictated by the situation. • A reasonable conclusion from all of the available evidence is that the benefits of use of epinephrine outweigh the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time, and care is taken to avoid inadvertent intravascular injection.
2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, however, because of its comparative excessive α 1 stimulation. The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in • whom elective dental care should be deferred. • If urgent treatment becomes necessary, however, a decision must be made regarding the use of epinephrine, which will be dictated by the situation. • A reasonable conclusion from all of the available evidence is that the benefits of use of epinephrine outweigh the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time, and care is taken to avoid inadvertent intravascular injection.
 2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, however, because of its comparative excessive α 1 stimulation. The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in • whom elective dental care should be deferred. • A reasonable conclusion from all of the available evidence is that the benefits of use of epinephrine outweigh the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time, and care is taken to avoid inadvertent intravascular injection. • Consultation with the patient’s physician is advisable before a definitive decision is made. An additional concern when patients with hypertension are treated is the potential for adverse drug interactions between vasoconstrictors and antihypertensive drugs— specifically, the nonselective β-adrenergic blocking agents.
2 - Hypertension • Use of Vasoconstrictors. • Levonordefrin should be avoided in patients with hypertension, however, because of its comparative excessive α 1 stimulation. The use of epinephrine generally is not advised in patients with uncontrolled hypertension, in • whom elective dental care should be deferred. • A reasonable conclusion from all of the available evidence is that the benefits of use of epinephrine outweigh the increased risks, so long as modest doses (e. g. , one or two carpules) are used at one time, and care is taken to avoid inadvertent intravascular injection. • Consultation with the patient’s physician is advisable before a definitive decision is made. An additional concern when patients with hypertension are treated is the potential for adverse drug interactions between vasoconstrictors and antihypertensive drugs— specifically, the nonselective β-adrenergic blocking agents.
 2 - Hypertension • Use of Vasoconstrictors. • • The basis for concern with use of nonselective β-adrenergic blocking agents (e. g. , propranolol) is that the normal compensatory vasodilatation of skeletal muscle vasculature mediated by β 2 receptors is inhibited • by these drugs • • and injection of epinephrine, levonordefrin, or any other pressor agent may result in uncompensated peripheral vasoconstriction because of unopposed stimulation of α 1 receptors. • This vasoconstrictive effect could potentially cause a significant elevation in blood pressure and a compensatory bradycardia.
2 - Hypertension • Use of Vasoconstrictors. • • The basis for concern with use of nonselective β-adrenergic blocking agents (e. g. , propranolol) is that the normal compensatory vasodilatation of skeletal muscle vasculature mediated by β 2 receptors is inhibited • by these drugs • • and injection of epinephrine, levonordefrin, or any other pressor agent may result in uncompensated peripheral vasoconstriction because of unopposed stimulation of α 1 receptors. • This vasoconstrictive effect could potentially cause a significant elevation in blood pressure and a compensatory bradycardia.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Patient Evaluation/Risk Assessment Potential Issues/Concerns • • • Analgesics Ensure adequate postoperative pain control. • Anesthesia Avoid use of excessive amounts of epinephrine; • limit to two carpules of 1 : 100, 000 epinephrine • at a time (within 30 -45 minutes); greater • quantities may be tolerated well clinically but • with increasing risk.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Patient Evaluation/Risk Assessment Potential Issues/Concerns • • • Analgesics Ensure adequate postoperative pain control. • Anesthesia Avoid use of excessive amounts of epinephrine; • limit to two carpules of 1 : 100, 000 epinephrine • at a time (within 30 -45 minutes); greater • quantities may be tolerated well clinically but • with increasing risk.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Anxiety Use stress reduction protocol • Consider the use of preoperative oral sedation • (short-acting benzodiazepine) 1 hour before • procedure, as well as using N 2 O-O 2 inhalational • sedation intraoperatively
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Anxiety Use stress reduction protocol • Consider the use of preoperative oral sedation • (short-acting benzodiazepine) 1 hour before • procedure, as well as using N 2 O-O 2 inhalational • sedation intraoperatively
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Bleeding If patient is taking aspirin or other antiplatelet • medication, anticipate some excessive bleeding, • but modification of drug regimen is not required. • Chair position Ensure a comfortable chair position and avoid rapid position changes • • Drugs The use of excessive amounts of epinephrine with nonselective beta blockers can potentially cause a spike in blood pressure, but this is unlikely and appears to be dosedependent; avoid the use of epinephrine-impregnated retraction cord.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Bleeding If patient is taking aspirin or other antiplatelet • medication, anticipate some excessive bleeding, • but modification of drug regimen is not required. • Chair position Ensure a comfortable chair position and avoid rapid position changes • • Drugs The use of excessive amounts of epinephrine with nonselective beta blockers can potentially cause a spike in blood pressure, but this is unlikely and appears to be dosedependent; avoid the use of epinephrine-impregnated retraction cord.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Devices Patients who have coronary artery stents • do not require antibiotic prophylaxis; however, they are likely to be taking aspirin and/or clopidogrel (or other antiplatelet medication) to decrease the chance of stent-related thrombus. • Anticipate excessive bleeding, • but it generally is unnecessary to discontinue these medications. •
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Devices Patients who have coronary artery stents • do not require antibiotic prophylaxis; however, they are likely to be taking aspirin and/or clopidogrel (or other antiplatelet medication) to decrease the chance of stent-related thrombus. • Anticipate excessive bleeding, • but it generally is unnecessary to discontinue these medications. •
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Equipment Consider taking preoperative vital signs and the use of a pulse oximeter if oral sedation is used, or if the patient becomes symptomatic • • Emergencies Precipitation of an angina attack, MI, arrhythmia, or cardiac arrest is possible. • Have nitroglycerin readily available as well as oxygen. • • Be prepared to perform CPR and activate EMS. •
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 3 - Ischemic Heart Disease Angina and Myocardial infarction • Equipment Consider taking preoperative vital signs and the use of a pulse oximeter if oral sedation is used, or if the patient becomes symptomatic • • Emergencies Precipitation of an angina attack, MI, arrhythmia, or cardiac arrest is possible. • Have nitroglycerin readily available as well as oxygen. • • Be prepared to perform CPR and activate EMS. •
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Analgesics Provide good postoperative analgesia to minimize pain and associated stress. • Antibiotics For patients with pacemakers or ICDs, antibiotic prophylaxis to prevent bacterial endocarditis is not recommended. • • Some antibiotics (e. g. , metronidazole, extended-spectrum penicillins) are known to increase the INR in patients on warfarin (Coumadin); caution in their use is advised.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Analgesics Provide good postoperative analgesia to minimize pain and associated stress. • Antibiotics For patients with pacemakers or ICDs, antibiotic prophylaxis to prevent bacterial endocarditis is not recommended. • • Some antibiotics (e. g. , metronidazole, extended-spectrum penicillins) are known to increase the INR in patients on warfarin (Coumadin); caution in their use is advised.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Anesthesia Ensure profound local anesthesia. • Epinephrine containing local anesthetic can be used with minimal risk if the dose is limited to 0. 036 mg epinephrine (two capsules containing 1 : 100, 000 concentration). • Higher doses may be tolerated, but the risk of complications • increases with dose.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Anesthesia Ensure profound local anesthesia. • Epinephrine containing local anesthetic can be used with minimal risk if the dose is limited to 0. 036 mg epinephrine (two capsules containing 1 : 100, 000 concentration). • Higher doses may be tolerated, but the risk of complications • increases with dose.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Avoid the use of epinephrine in retraction cord. • Anxiety Establish good rapport, and schedule short morning appointments. • • Use anxiety reduction techniques: • • Provide preoperative sedation (short-acting benzodiazepine the night before and/or 1 hour before the appointment). • • Administer intraoperative sedation (nitrous oxide–oxygen).
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Avoid the use of epinephrine in retraction cord. • Anxiety Establish good rapport, and schedule short morning appointments. • • Use anxiety reduction techniques: • • Provide preoperative sedation (short-acting benzodiazepine the night before and/or 1 hour before the appointment). • • Administer intraoperative sedation (nitrous oxide–oxygen).
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • • • In patients taking warfarin: • Review current INR lab results (within 24 hours of surgical procedure). • • • If INR is within therapeutic range (2. 0 -3. 5), dental treatment, including minor oral surgery, can be performed without stopping or altering the warfarin regimen. • In patients taking dabigatran when major oral surgery is planned: • • Review current thrombin clotting time, activated partial thromboplastin time or ecarin clotting time lab results. • • Ensure patient has normal renal function.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • • • In patients taking warfarin: • Review current INR lab results (within 24 hours of surgical procedure). • • • If INR is within therapeutic range (2. 0 -3. 5), dental treatment, including minor oral surgery, can be performed without stopping or altering the warfarin regimen. • In patients taking dabigatran when major oral surgery is planned: • • Review current thrombin clotting time, activated partial thromboplastin time or ecarin clotting time lab results. • • Ensure patient has normal renal function.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • In patients taking warfarin, dabigatran or other anticoagulant/antiplatelet: • • Use local hemostatic measures and products including gelatin sponge, oxidized cellulose • or chitosan products in sockets, suturing, gauze pressure packs, and preoperative stents. • Tranexamic acid or ε-aminocaproic acid can be used as mouth rinse and/or to • soak gauze for placement at bleeding site.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • In patients taking warfarin, dabigatran or other anticoagulant/antiplatelet: • • Use local hemostatic measures and products including gelatin sponge, oxidized cellulose • or chitosan products in sockets, suturing, gauze pressure packs, and preoperative stents. • Tranexamic acid or ε-aminocaproic acid can be used as mouth rinse and/or to • soak gauze for placement at bleeding site.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Devices Pacemakers and ICDs may experience electromagnetic interference with dental • equipment such as ultrasonic scalers, ultrasonic bath cleaners, electrosurgery • devices, or battery-operated curing lights. • • Drugs In patients taking digoxin, watch for signs or symptoms of toxicity (e. g. , hypersalivation, visual changes); avoid epinephrine or levonordefrin.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Devices Pacemakers and ICDs may experience electromagnetic interference with dental • equipment such as ultrasonic scalers, ultrasonic bath cleaners, electrosurgery • devices, or battery-operated curing lights. • • Drugs In patients taking digoxin, watch for signs or symptoms of toxicity (e. g. , hypersalivation, visual changes); avoid epinephrine or levonordefrin.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Emergencies and urgent care • • For high-risk patient who requires urgent care, consider treating in special care clinic or hospital where a defibrillator can be used if needed. • • After consulting with physician, provide limited care only for pain control, treatment of acute infection, or control of bleeding, as appropriate. • • The following measures may be used as needed: • Placement of intravenous line • Sedation • Electrocardiogram (ECG) monitoring • Pulse oximetry • Blood pressure monitoring • Avoiding or limiting epinephrine
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 4 - Cardiac Arrhythmias • Emergencies and urgent care • • For high-risk patient who requires urgent care, consider treating in special care clinic or hospital where a defibrillator can be used if needed. • • After consulting with physician, provide limited care only for pain control, treatment of acute infection, or control of bleeding, as appropriate. • • The following measures may be used as needed: • Placement of intravenous line • Sedation • Electrocardiogram (ECG) monitoring • Pulse oximetry • Blood pressure monitoring • Avoiding or limiting epinephrine
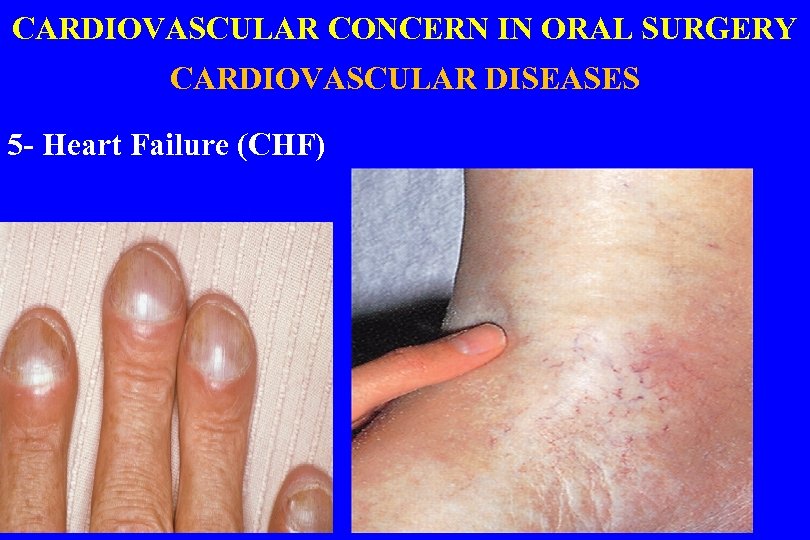 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF)
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF)
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Anesthesia It is very important to achieve and maintain excellent anesthesia in order to reduce stress and prevent cardiac crisis. • Use of epinephrine (1 : 100, 000) at a dose of no more than 2 carpules • in local anesthetics • generally causes no problems, but patients should be monitored closely. • Clinicians should provide good postoperative pain control. • General anesthesia should be Avoided.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Anesthesia It is very important to achieve and maintain excellent anesthesia in order to reduce stress and prevent cardiac crisis. • Use of epinephrine (1 : 100, 000) at a dose of no more than 2 carpules • in local anesthetics • generally causes no problems, but patients should be monitored closely. • Clinicians should provide good postoperative pain control. • General anesthesia should be Avoided.
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Anxiety Patients with untreated or poorly controlled HF • may appear very anxious and stressed and • are at risk for cardiac crisis. • Use of special anxiety/stress reduction techniques
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Anxiety Patients with untreated or poorly controlled HF • may appear very anxious and stressed and • are at risk for cardiac crisis. • Use of special anxiety/stress reduction techniques
 CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Drugs Patients with HF typically are on many medications. • The dentist should be aware of potential side effects and interactions such as NSAIDS LEADS TO DECREASE THE EFFICACY DIURETICS • The use of epinephrine or other pressor amines(either in gingival retraction cord or as agents to control bleeding) must be • avoided. • Digitalis toxicity may present a problem, so caution should be exercised in treating those patients.
CARDIOVASCULAR CONCERN IN ORAL SURGERY CARDIOVASCULAR DISEASES 5 - Heart Failure (CHF) • Drugs Patients with HF typically are on many medications. • The dentist should be aware of potential side effects and interactions such as NSAIDS LEADS TO DECREASE THE EFFICACY DIURETICS • The use of epinephrine or other pressor amines(either in gingival retraction cord or as agents to control bleeding) must be • avoided. • Digitalis toxicity may present a problem, so caution should be exercised in treating those patients.
 Thank you
Thank you


