7e4f7f66d0b60f67c72774b2f0446bcb.ppt
- Количество слайдов: 29
 Foundations for a Successful Patient-Centered ACO: First Steps Frank E. Belsito, DO, MMM and James J. Dearing, DO, FAAFP, FACOFP
Foundations for a Successful Patient-Centered ACO: First Steps Frank E. Belsito, DO, MMM and James J. Dearing, DO, FAAFP, FACOFP
 Evolving Healthcare Moving from a “Sick Care” system to a “Health Care” system
Evolving Healthcare Moving from a “Sick Care” system to a “Health Care” system
 A Time for Change • Health care is being delivered in a fragmented process • Lack of communication • Lack of coordination
A Time for Change • Health care is being delivered in a fragmented process • Lack of communication • Lack of coordination
 Payor Paradigm System paid by what we do, not the outcome of what we did
Payor Paradigm System paid by what we do, not the outcome of what we did
 Transformation from Fee-for-Service to Value-Based Payment: The Integrated Delivery System Perspective
Transformation from Fee-for-Service to Value-Based Payment: The Integrated Delivery System Perspective
 Value-Based Strategy Physician Alignment Delivering Value Demonstrating Value-Based Contracting
Value-Based Strategy Physician Alignment Delivering Value Demonstrating Value-Based Contracting
 Accountable Care Organization Anatomy refers to the Structure of the ACO is not itself an entity, but rather it is a contractual relationship dealing with delivery and financial strategies and tactics between an Organized Delivery System and CMS-Medicare. It is also used to expand the relationship to other payors such as BCBS, etc. We must first construct the ACO structure, creating the anatomy of the delivery system.
Accountable Care Organization Anatomy refers to the Structure of the ACO is not itself an entity, but rather it is a contractual relationship dealing with delivery and financial strategies and tactics between an Organized Delivery System and CMS-Medicare. It is also used to expand the relationship to other payors such as BCBS, etc. We must first construct the ACO structure, creating the anatomy of the delivery system.
 Creating an ACO and the payment systems to support them may well have the greatest potential for improving quality and controlling costs. There is no single formula for a successful ACO…. . so different approaches are encouraged
Creating an ACO and the payment systems to support them may well have the greatest potential for improving quality and controlling costs. There is no single formula for a successful ACO…. . so different approaches are encouraged
 Integrating Hospitals and Medical Groups Hospitals & PO + Operate in a manner of a multispecialty group practic
Integrating Hospitals and Medical Groups Hospitals & PO + Operate in a manner of a multispecialty group practic
 Governance Structure: All Parties at the Table Assure that all parties are at the table from the beginning: • Hospital Administration • Physicians engaged in the ACO development • Others?
Governance Structure: All Parties at the Table Assure that all parties are at the table from the beginning: • Hospital Administration • Physicians engaged in the ACO development • Others?
 Physician Buy In • Be sure that all physicians understand what you are trying to accomplish, primary care first and then specialists. • Primary Care Physicians (PCPs) will use the patient centered medical home model. (Physicians must understand identify with how the ACO will help their patients, accountability for care of the patient population. )
Physician Buy In • Be sure that all physicians understand what you are trying to accomplish, primary care first and then specialists. • Primary Care Physicians (PCPs) will use the patient centered medical home model. (Physicians must understand identify with how the ACO will help their patients, accountability for care of the patient population. )
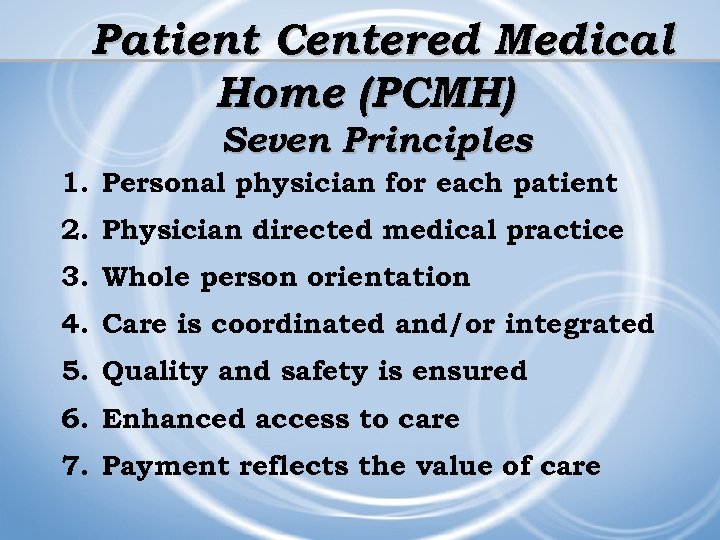 Patient Centered Medical Home (PCMH) Seven Principles 1. Personal physician for each patient 2. Physician directed medical practice 3. Whole person orientation 4. Care is coordinated and/or integrated 5. Quality and safety is ensured 6. Enhanced access to care 7. Payment reflects the value of care
Patient Centered Medical Home (PCMH) Seven Principles 1. Personal physician for each patient 2. Physician directed medical practice 3. Whole person orientation 4. Care is coordinated and/or integrated 5. Quality and safety is ensured 6. Enhanced access to care 7. Payment reflects the value of care
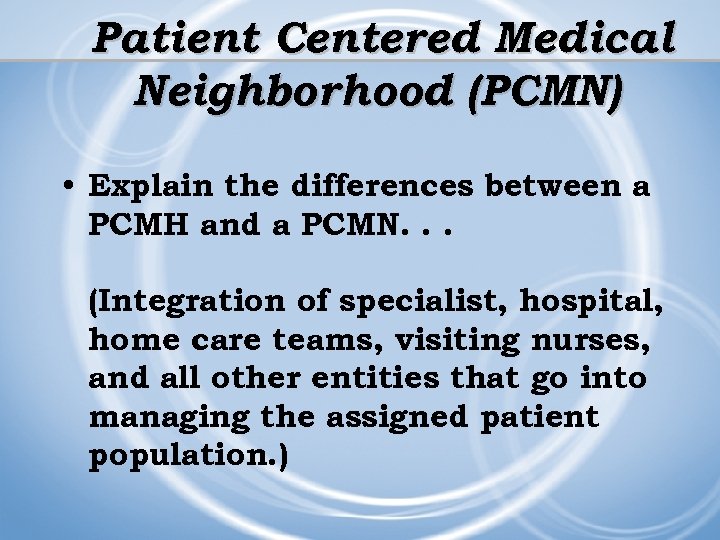 Patient Centered Medical Neighborhood (PCMN) • Explain the differences between a PCMH and a PCMN. . . (Integration of specialist, hospital, home care teams, visiting nurses, and all other entities that go into managing the assigned patient population. )
Patient Centered Medical Neighborhood (PCMN) • Explain the differences between a PCMH and a PCMN. . . (Integration of specialist, hospital, home care teams, visiting nurses, and all other entities that go into managing the assigned patient population. )
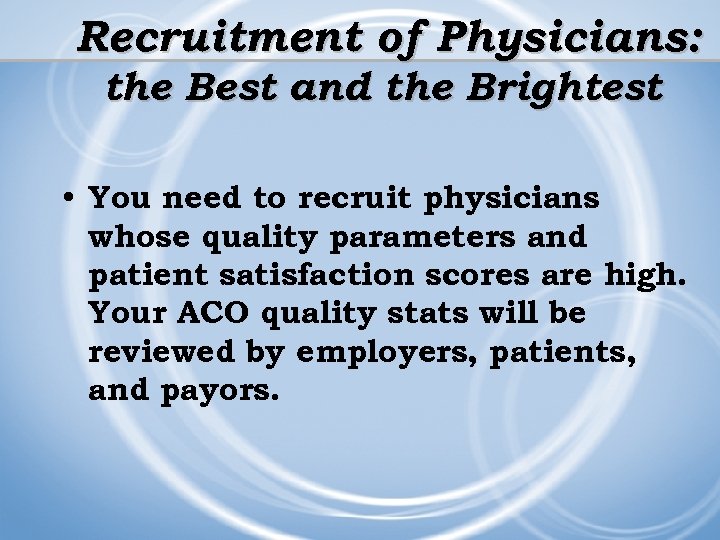 Recruitment of Physicians: the Best and the Brightest • You need to recruit physicians whose quality parameters and patient satisfaction scores are high. Your ACO quality stats will be reviewed by employers, patients, and payors.
Recruitment of Physicians: the Best and the Brightest • You need to recruit physicians whose quality parameters and patient satisfaction scores are high. Your ACO quality stats will be reviewed by employers, patients, and payors.
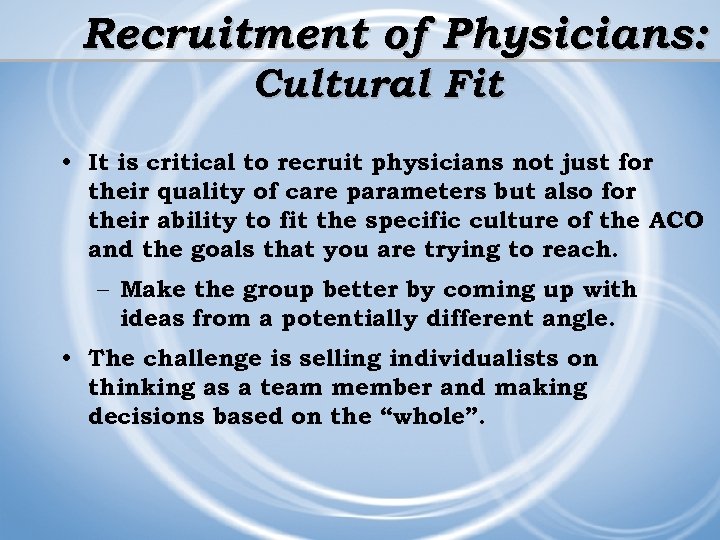 Recruitment of Physicians: Cultural Fit • It is critical to recruit physicians not just for their quality of care parameters but also for their ability to fit the specific culture of the ACO and the goals that you are trying to reach. – Make the group better by coming up with ideas from a potentially different angle. • The challenge is selling individualists on thinking as a team member and making decisions based on the “whole”.
Recruitment of Physicians: Cultural Fit • It is critical to recruit physicians not just for their quality of care parameters but also for their ability to fit the specific culture of the ACO and the goals that you are trying to reach. – Make the group better by coming up with ideas from a potentially different angle. • The challenge is selling individualists on thinking as a team member and making decisions based on the “whole”.
 Success will depend on: 1) Complete and timely information about patients and the services they are receiving 2) Technology and skills for population management and coordination of care 3) Culture of teamwork among staff 4) Coordinated relationships with Specialists 5) Ability to measure and report on the quality of care
Success will depend on: 1) Complete and timely information about patients and the services they are receiving 2) Technology and skills for population management and coordination of care 3) Culture of teamwork among staff 4) Coordinated relationships with Specialists 5) Ability to measure and report on the quality of care
 Implementation of an Electronic Medical Record • All facilities need to be able to share patients’ medical records.
Implementation of an Electronic Medical Record • All facilities need to be able to share patients’ medical records.
 Develop Accountability of the Group and Assign a Leader The leader should have great quality parameters but will have to accept accountability for the team, not just his/her own stats.
Develop Accountability of the Group and Assign a Leader The leader should have great quality parameters but will have to accept accountability for the team, not just his/her own stats.
 Use Dashboards for Accountability • Every physician has a dashboard. Give them meaningful data: patient reports, productivity reports, and physician reports. • The brightest and the smartest will use that information to push your group in the right direction and make your ACO the most successful organization it can be. • There a number of vendors to provide data.
Use Dashboards for Accountability • Every physician has a dashboard. Give them meaningful data: patient reports, productivity reports, and physician reports. • The brightest and the smartest will use that information to push your group in the right direction and make your ACO the most successful organization it can be. • There a number of vendors to provide data.
 Care Coordination ü Case Management Coordinator ü Disease Registry ü PCMH ü Health Coaches ü Wellness Program ü Care Transition Coordinator
Care Coordination ü Case Management Coordinator ü Disease Registry ü PCMH ü Health Coaches ü Wellness Program ü Care Transition Coordinator
 Infrastructure Issues: Integrated Care • Coordination of both primary care and specialist doctors around the patient population (PCMH and Chronic Care Model) • List all patients in a registry by disease state and by all payors.
Infrastructure Issues: Integrated Care • Coordination of both primary care and specialist doctors around the patient population (PCMH and Chronic Care Model) • List all patients in a registry by disease state and by all payors.
 Infrastructure Issues (cont’d) (cont’d • Integrate patient registry with an electronic health record for both primary care and specialty facilities to enable exchange of info on patient real time. • Care managers embedded into practice sites to help manage chronic diseases/patients/issues in real time.
Infrastructure Issues (cont’d) (cont’d • Integrate patient registry with an electronic health record for both primary care and specialty facilities to enable exchange of info on patient real time. • Care managers embedded into practice sites to help manage chronic diseases/patients/issues in real time.
 Infrastructure Issues (Cont’d) (Cont’d • Discharged hospital patients are seen by within 24 -48 hours of discharge by their Primary Care Physician.
Infrastructure Issues (Cont’d) (Cont’d • Discharged hospital patients are seen by within 24 -48 hours of discharge by their Primary Care Physician.
 Payment Systems • In an ACO fee-for-service does not work. Under the Value-based strategy you have to deliver quality. There is a transition timeframe involved in switching. The question is how do you weather the transition?
Payment Systems • In an ACO fee-for-service does not work. Under the Value-based strategy you have to deliver quality. There is a transition timeframe involved in switching. The question is how do you weather the transition?
 Payment Systems (cont’d) • Create a payment system that incentivizes team activities. All players should work to the highest level of their degree. • Put the work at the least common denominator degree. • Provide daily dashboards with the most information possible.
Payment Systems (cont’d) • Create a payment system that incentivizes team activities. All players should work to the highest level of their degree. • Put the work at the least common denominator degree. • Provide daily dashboards with the most information possible.
 Clinical Integration is the Core Initiative Hospitals and Physician are turning to Clinical Integration to increase QUALITY and EFFICIENCY in care delivery.
Clinical Integration is the Core Initiative Hospitals and Physician are turning to Clinical Integration to increase QUALITY and EFFICIENCY in care delivery.
 Transforming care to significantly improve outcomes and resource utilization is MORE difficult than achieving “clinical integration”!
Transforming care to significantly improve outcomes and resource utilization is MORE difficult than achieving “clinical integration”!
 Negotiating with Payers • Don’t try to cut deals with payers until you have your act and data ready for the negotiation. • Don’t just accept the payer’s data unless you can compare to your real data.
Negotiating with Payers • Don’t try to cut deals with payers until you have your act and data ready for the negotiation. • Don’t just accept the payer’s data unless you can compare to your real data.
 • Questions/Comments?
• Questions/Comments?


