Fluid-Management-and-Shock-Resuscitation.pptx
- Количество слайдов: 60
 Fluid Management and Shock Resuscitation Andrea Ika Hapsari
Fluid Management and Shock Resuscitation Andrea Ika Hapsari
 Outline n Normal Fluid Requirements n Definition of Shock n Types of Shock – – Hypovolemic Cardiogenic Distributive Obstructive n Resuscitation Fluids n Goals of Resuscitation
Outline n Normal Fluid Requirements n Definition of Shock n Types of Shock – – Hypovolemic Cardiogenic Distributive Obstructive n Resuscitation Fluids n Goals of Resuscitation
 Body Fluid Compartments n Total Body Water = 60% body weight – 70 Kg TBW = 42 L n 2/3 of TBW is intracellular (ICF) – 40% of body weight, 70 Kg = 28 L n 1/3 of TBW is extracellular (ECF) – 20% of body weight, 70 Kg = 14 L – Plasma volume is approx 4% of total body weight, but varies by age, gender, body habitus
Body Fluid Compartments n Total Body Water = 60% body weight – 70 Kg TBW = 42 L n 2/3 of TBW is intracellular (ICF) – 40% of body weight, 70 Kg = 28 L n 1/3 of TBW is extracellular (ECF) – 20% of body weight, 70 Kg = 14 L – Plasma volume is approx 4% of total body weight, but varies by age, gender, body habitus
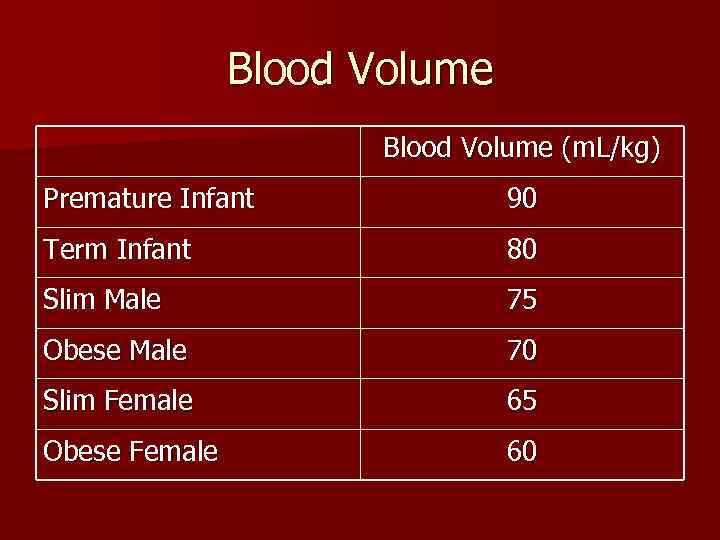 Blood Volume (m. L/kg) Premature Infant 90 Term Infant 80 Slim Male 75 Obese Male 70 Slim Female 65 Obese Female 60
Blood Volume (m. L/kg) Premature Infant 90 Term Infant 80 Slim Male 75 Obese Male 70 Slim Female 65 Obese Female 60
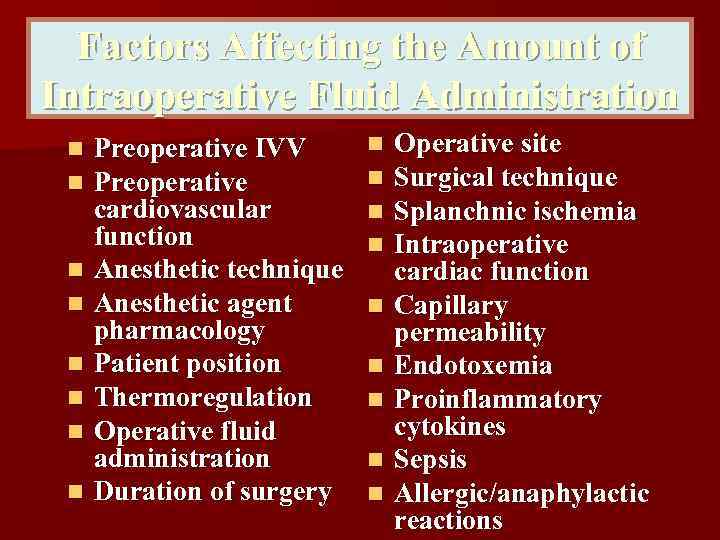 Factors Affecting the Amount of Intraoperative Fluid Administration n n n n Preoperative IVV Preoperative cardiovascular function Anesthetic technique Anesthetic agent pharmacology Patient position Thermoregulation Operative fluid administration Duration of surgery n n n n n Operative site Surgical technique Splanchnic ischemia Intraoperative cardiac function Capillary permeability Endotoxemia Proinflammatory cytokines Sepsis Allergic/anaphylactic reactions
Factors Affecting the Amount of Intraoperative Fluid Administration n n n n Preoperative IVV Preoperative cardiovascular function Anesthetic technique Anesthetic agent pharmacology Patient position Thermoregulation Operative fluid administration Duration of surgery n n n n n Operative site Surgical technique Splanchnic ischemia Intraoperative cardiac function Capillary permeability Endotoxemia Proinflammatory cytokines Sepsis Allergic/anaphylactic reactions
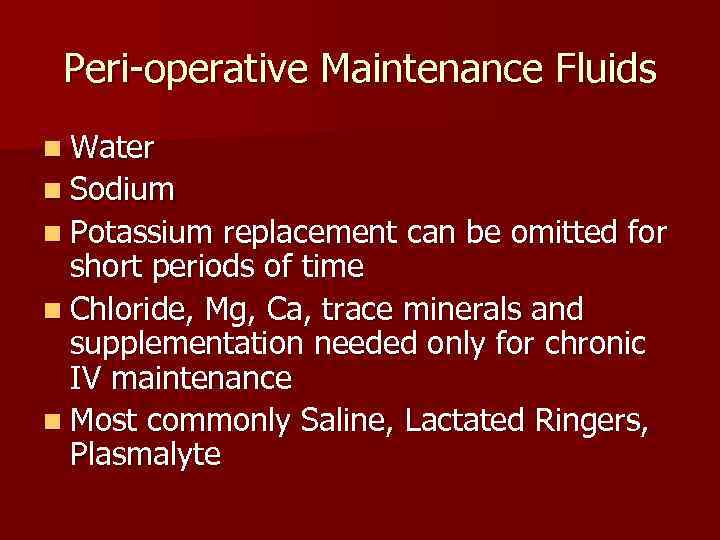 Peri-operative Maintenance Fluids n Water n Sodium n Potassium replacement can be omitted for short periods of time n Chloride, Mg, Ca, trace minerals and supplementation needed only for chronic IV maintenance n Most commonly Saline, Lactated Ringers, Plasmalyte
Peri-operative Maintenance Fluids n Water n Sodium n Potassium replacement can be omitted for short periods of time n Chloride, Mg, Ca, trace minerals and supplementation needed only for chronic IV maintenance n Most commonly Saline, Lactated Ringers, Plasmalyte
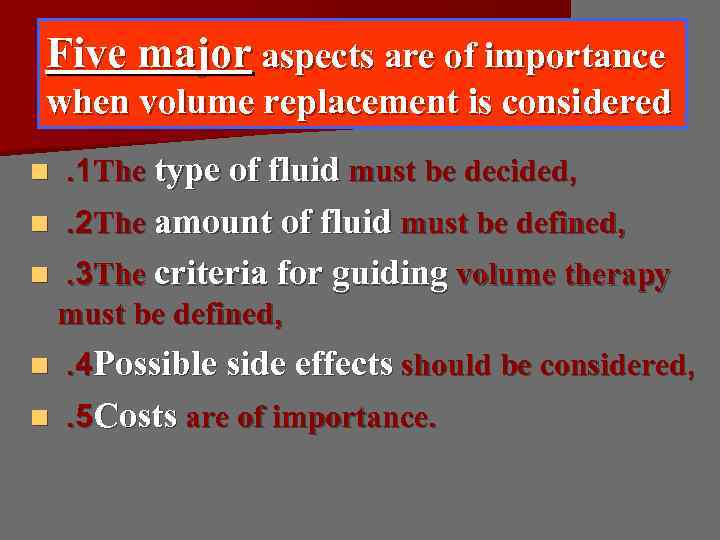 Five major aspects are of importance when volume replacement is considered n . 1 The type of fluid must be decided, n . 2 The amount of fluid must be defined, n . 3 The criteria for guiding volume therapy must be defined, n . 4 Possible side effects should be considered, n . 5 Costs are of importance.
Five major aspects are of importance when volume replacement is considered n . 1 The type of fluid must be decided, n . 2 The amount of fluid must be defined, n . 3 The criteria for guiding volume therapy must be defined, n . 4 Possible side effects should be considered, n . 5 Costs are of importance.
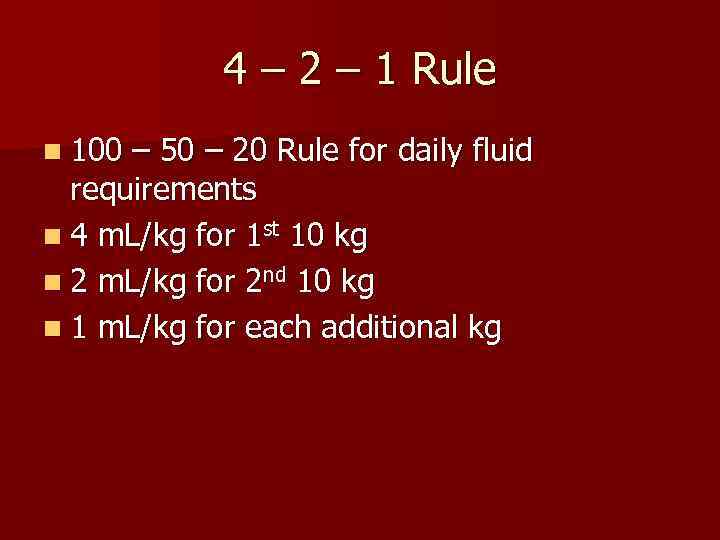 4 – 2 – 1 Rule n 100 – 50 – 20 Rule for daily fluid requirements n 4 m. L/kg for 1 st 10 kg n 2 m. L/kg for 2 nd 10 kg n 1 m. L/kg for each additional kg
4 – 2 – 1 Rule n 100 – 50 – 20 Rule for daily fluid requirements n 4 m. L/kg for 1 st 10 kg n 2 m. L/kg for 2 nd 10 kg n 1 m. L/kg for each additional kg
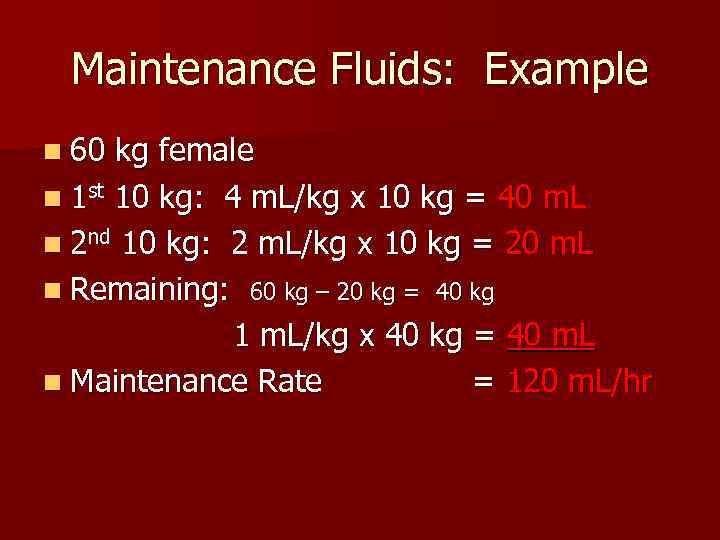 Maintenance Fluids: Example n 60 kg female n 1 st 10 kg: 4 m. L/kg x 10 kg = 40 m. L n 2 nd 10 kg: 2 m. L/kg x 10 kg = 20 m. L n Remaining: 60 kg – 20 kg = 40 kg 1 m. L/kg x 40 kg = 40 m. L n Maintenance Rate = 120 m. L/hr
Maintenance Fluids: Example n 60 kg female n 1 st 10 kg: 4 m. L/kg x 10 kg = 40 m. L n 2 nd 10 kg: 2 m. L/kg x 10 kg = 20 m. L n Remaining: 60 kg – 20 kg = 40 kg 1 m. L/kg x 40 kg = 40 m. L n Maintenance Rate = 120 m. L/hr
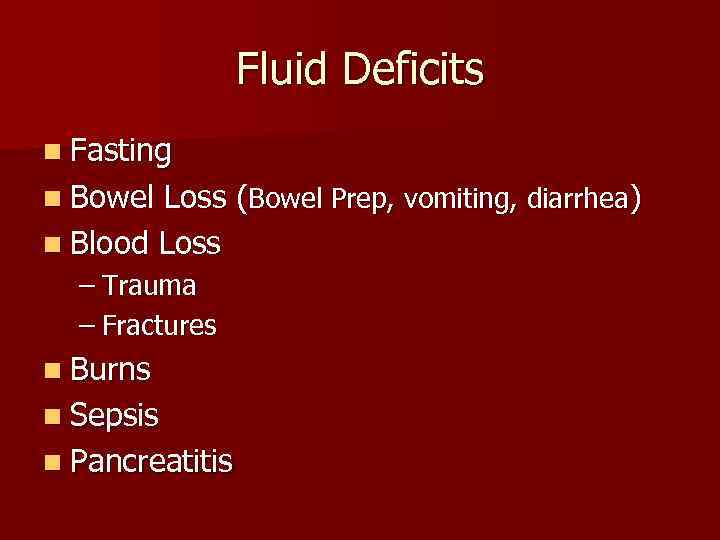 Fluid Deficits n Fasting n Bowel Loss (Bowel Prep, vomiting, diarrhea) n Blood Loss – Trauma – Fractures n Burns n Sepsis n Pancreatitis
Fluid Deficits n Fasting n Bowel Loss (Bowel Prep, vomiting, diarrhea) n Blood Loss – Trauma – Fractures n Burns n Sepsis n Pancreatitis
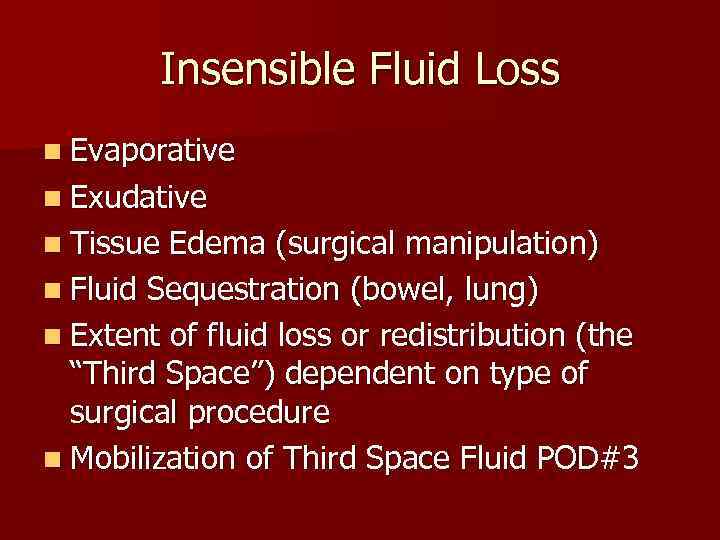 Insensible Fluid Loss n Evaporative n Exudative n Tissue Edema (surgical manipulation) n Fluid Sequestration (bowel, lung) n Extent of fluid loss or redistribution (the “Third Space”) dependent on type of surgical procedure n Mobilization of Third Space Fluid POD#3
Insensible Fluid Loss n Evaporative n Exudative n Tissue Edema (surgical manipulation) n Fluid Sequestration (bowel, lung) n Extent of fluid loss or redistribution (the “Third Space”) dependent on type of surgical procedure n Mobilization of Third Space Fluid POD#3
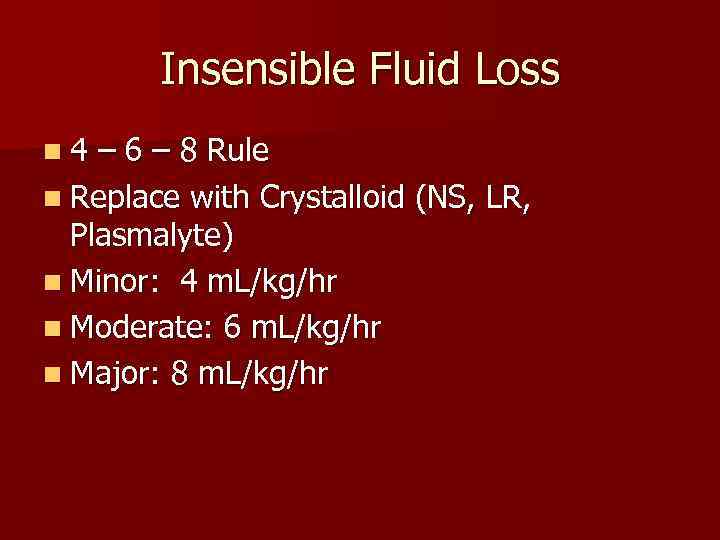 Insensible Fluid Loss n 4 – 6 – 8 Rule n Replace with Crystalloid (NS, LR, Plasmalyte) n Minor: 4 m. L/kg/hr n Moderate: 6 m. L/kg/hr n Major: 8 m. L/kg/hr
Insensible Fluid Loss n 4 – 6 – 8 Rule n Replace with Crystalloid (NS, LR, Plasmalyte) n Minor: 4 m. L/kg/hr n Moderate: 6 m. L/kg/hr n Major: 8 m. L/kg/hr
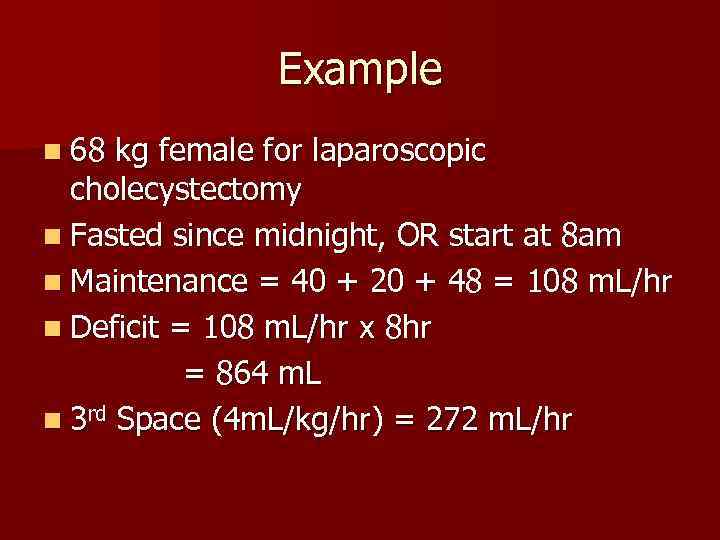 Example n 68 kg female for laparoscopic cholecystectomy n Fasted since midnight, OR start at 8 am n Maintenance = 40 + 20 + 48 = 108 m. L/hr n Deficit = 108 m. L/hr x 8 hr = 864 m. L n 3 rd Space (4 m. L/kg/hr) = 272 m. L/hr
Example n 68 kg female for laparoscopic cholecystectomy n Fasted since midnight, OR start at 8 am n Maintenance = 40 + 20 + 48 = 108 m. L/hr n Deficit = 108 m. L/hr x 8 hr = 864 m. L n 3 rd Space (4 m. L/kg/hr) = 272 m. L/hr
 Example n Intra-operative Fluid Replacement of: – Fluid Deficit 864 m. L – Maintenance Fluid 108 m. L/hr – 3 rd Space Loss 272 m. L/hr – Ongoing blood loss (crystalloid vs. colloid)
Example n Intra-operative Fluid Replacement of: – Fluid Deficit 864 m. L – Maintenance Fluid 108 m. L/hr – 3 rd Space Loss 272 m. L/hr – Ongoing blood loss (crystalloid vs. colloid)
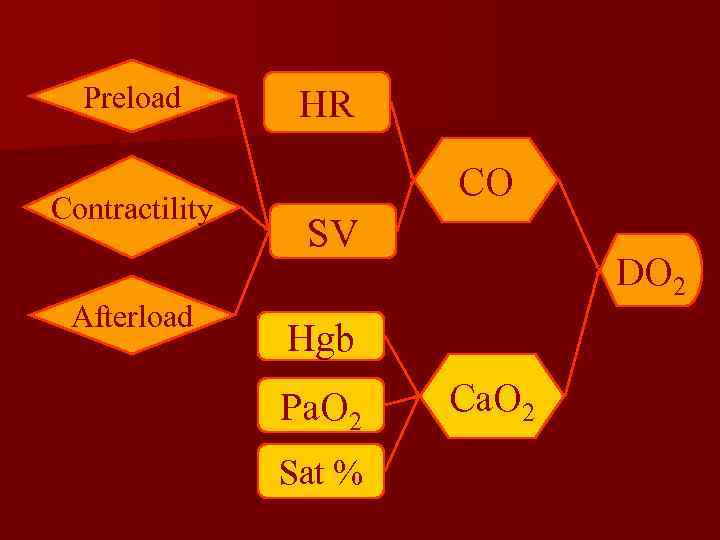
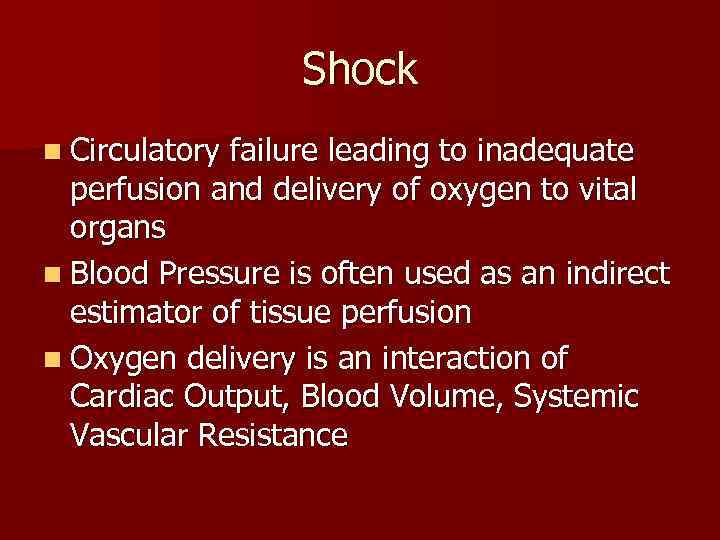 Shock n Circulatory failure leading to inadequate perfusion and delivery of oxygen to vital organs n Blood Pressure is often used as an indirect estimator of tissue perfusion n Oxygen delivery is an interaction of Cardiac Output, Blood Volume, Systemic Vascular Resistance
Shock n Circulatory failure leading to inadequate perfusion and delivery of oxygen to vital organs n Blood Pressure is often used as an indirect estimator of tissue perfusion n Oxygen delivery is an interaction of Cardiac Output, Blood Volume, Systemic Vascular Resistance
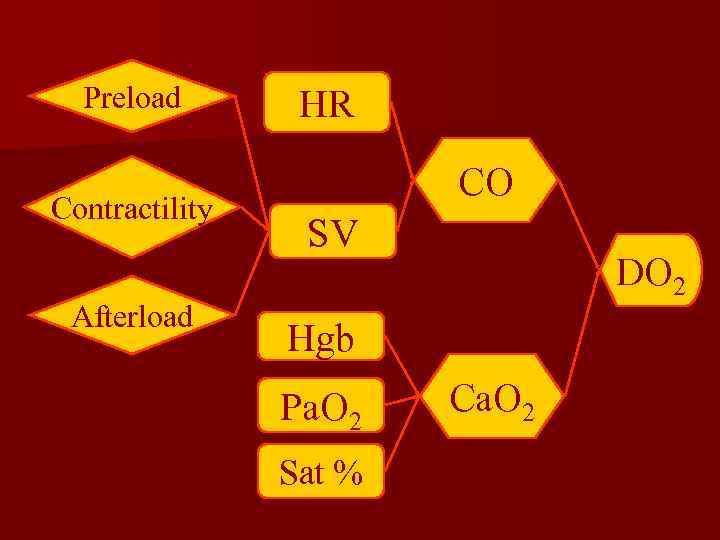 Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
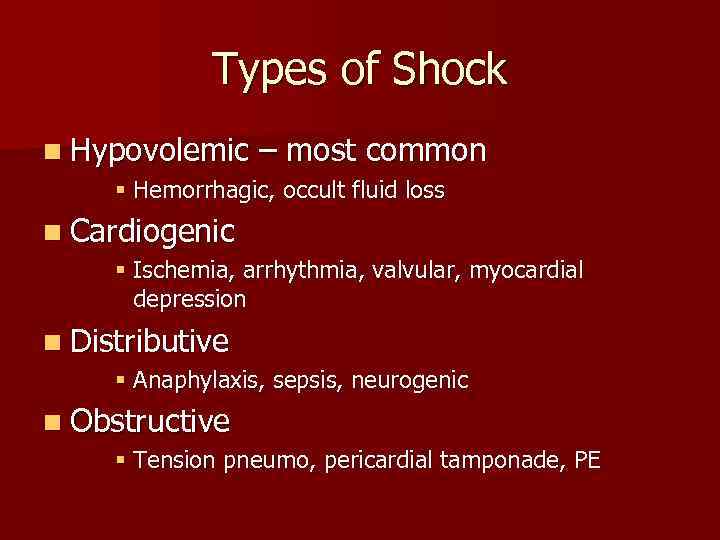 Types of Shock n Hypovolemic – most common § Hemorrhagic, occult fluid loss n Cardiogenic § Ischemia, arrhythmia, valvular, myocardial depression n Distributive § Anaphylaxis, sepsis, neurogenic n Obstructive § Tension pneumo, pericardial tamponade, PE
Types of Shock n Hypovolemic – most common § Hemorrhagic, occult fluid loss n Cardiogenic § Ischemia, arrhythmia, valvular, myocardial depression n Distributive § Anaphylaxis, sepsis, neurogenic n Obstructive § Tension pneumo, pericardial tamponade, PE
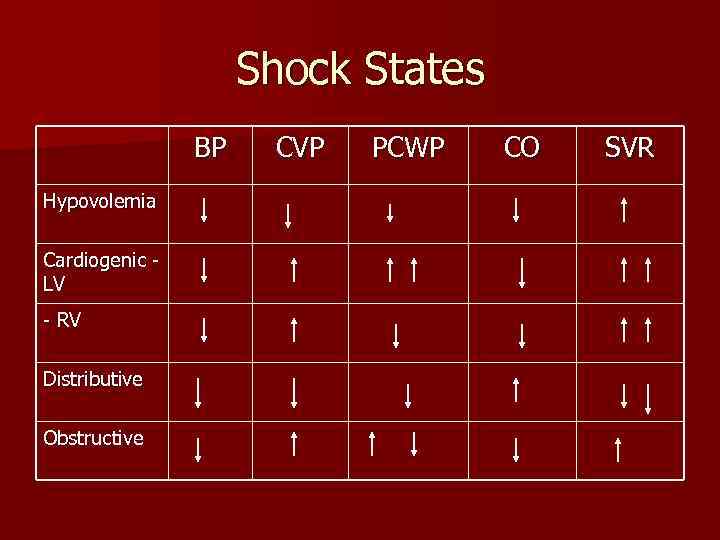 Shock States BP Hypovolemia Cardiogenic LV - RV Distributive Obstructive CVP PCWP CO SVR
Shock States BP Hypovolemia Cardiogenic LV - RV Distributive Obstructive CVP PCWP CO SVR
 Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
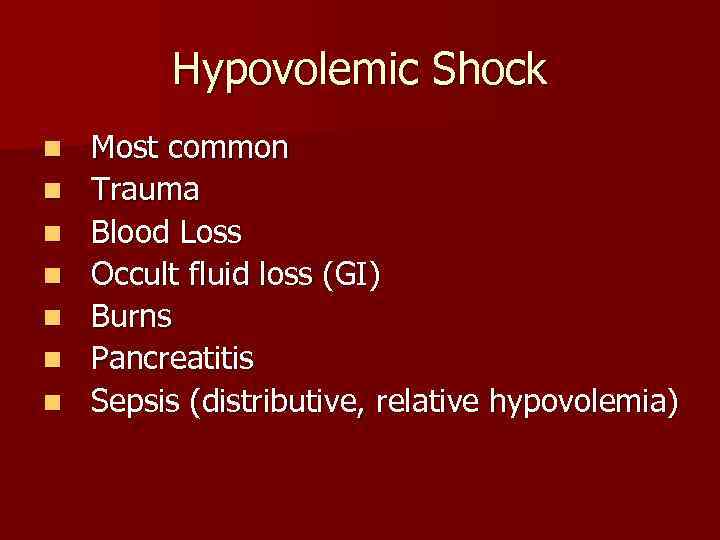 Hypovolemic Shock n n n n Most common Trauma Blood Loss Occult fluid loss (GI) Burns Pancreatitis Sepsis (distributive, relative hypovolemia)
Hypovolemic Shock n n n n Most common Trauma Blood Loss Occult fluid loss (GI) Burns Pancreatitis Sepsis (distributive, relative hypovolemia)
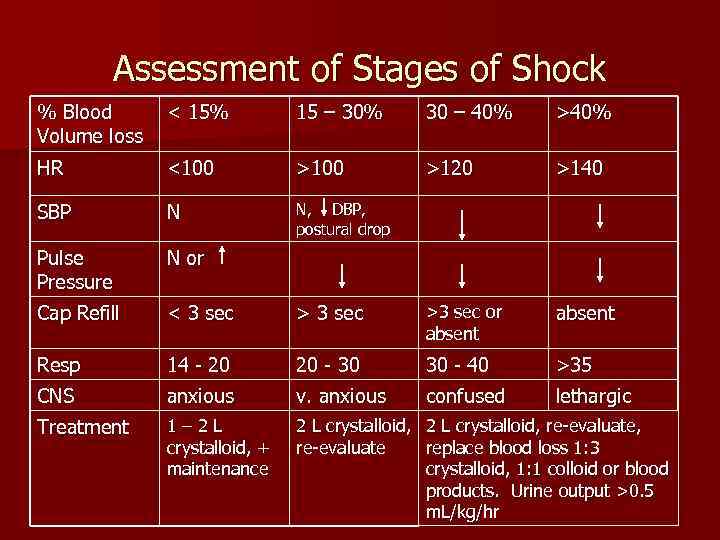 Assessment of Stages of Shock % Blood Volume loss < 15% 15 – 30% 30 – 40% >40% HR <100 >120 >140 SBP N N, DBP, postural drop Pulse Pressure N or Cap Refill < 3 sec >3 sec or absent Resp 14 - 20 20 - 30 30 - 40 >35 CNS anxious v. anxious confused lethargic Treatment 1– 2 L crystalloid, + maintenance 2 L crystalloid, re-evaluate, re-evaluate replace blood loss 1: 3 crystalloid, 1: 1 colloid or blood products. Urine output >0. 5 m. L/kg/hr
Assessment of Stages of Shock % Blood Volume loss < 15% 15 – 30% 30 – 40% >40% HR <100 >120 >140 SBP N N, DBP, postural drop Pulse Pressure N or Cap Refill < 3 sec >3 sec or absent Resp 14 - 20 20 - 30 30 - 40 >35 CNS anxious v. anxious confused lethargic Treatment 1– 2 L crystalloid, + maintenance 2 L crystalloid, re-evaluate, re-evaluate replace blood loss 1: 3 crystalloid, 1: 1 colloid or blood products. Urine output >0. 5 m. L/kg/hr
 Types of fluid must be decided,
Types of fluid must be decided,
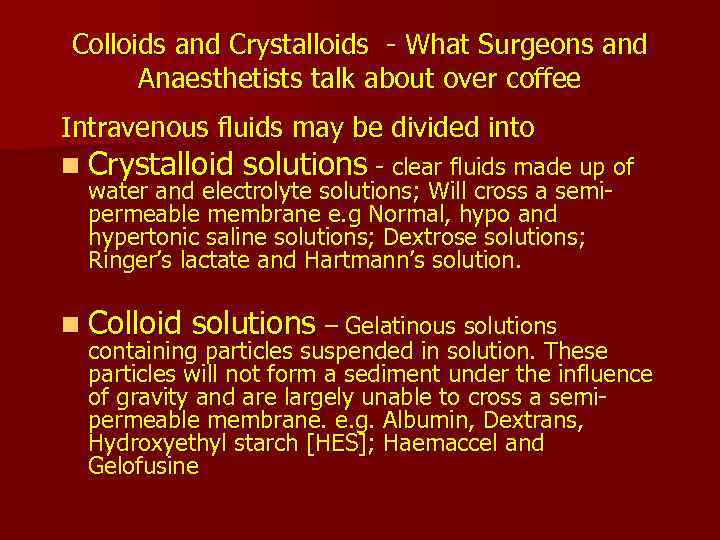 Colloids and Crystalloids - What Surgeons and Anaesthetists talk about over coffee Intravenous fluids may be divided into n Crystalloid solutions - clear fluids made up of water and electrolyte solutions; Will cross a semipermeable membrane e. g Normal, hypo and hypertonic saline solutions; Dextrose solutions; Ringer’s lactate and Hartmann’s solution. n Colloid solutions – Gelatinous solutions containing particles suspended in solution. These particles will not form a sediment under the influence of gravity and are largely unable to cross a semipermeable membrane. e. g. Albumin, Dextrans, Hydroxyethyl starch [HES]; Haemaccel and Gelofusine
Colloids and Crystalloids - What Surgeons and Anaesthetists talk about over coffee Intravenous fluids may be divided into n Crystalloid solutions - clear fluids made up of water and electrolyte solutions; Will cross a semipermeable membrane e. g Normal, hypo and hypertonic saline solutions; Dextrose solutions; Ringer’s lactate and Hartmann’s solution. n Colloid solutions – Gelatinous solutions containing particles suspended in solution. These particles will not form a sediment under the influence of gravity and are largely unable to cross a semipermeable membrane. e. g. Albumin, Dextrans, Hydroxyethyl starch [HES]; Haemaccel and Gelofusine
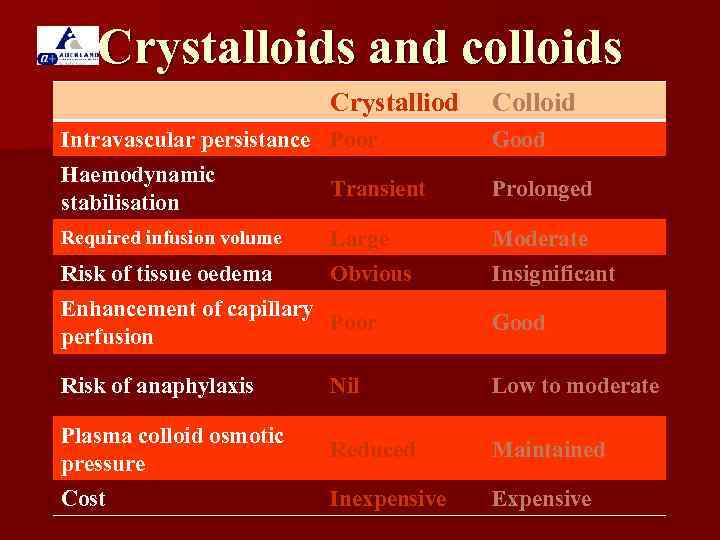 Crystalloids and colloids Crystalliod Colloid Intravascular persistance Poor Good Haemodynamic stabilisation Transient Prolonged Required infusion volume Large Moderate Risk of tissue oedema Obvious Insignificant Enhancement of capillary Poor perfusion Good Risk of anaphylaxis Nil Low to moderate Plasma colloid osmotic pressure Reduced Maintained Cost Inexpensive Expensive
Crystalloids and colloids Crystalliod Colloid Intravascular persistance Poor Good Haemodynamic stabilisation Transient Prolonged Required infusion volume Large Moderate Risk of tissue oedema Obvious Insignificant Enhancement of capillary Poor perfusion Good Risk of anaphylaxis Nil Low to moderate Plasma colloid osmotic pressure Reduced Maintained Cost Inexpensive Expensive
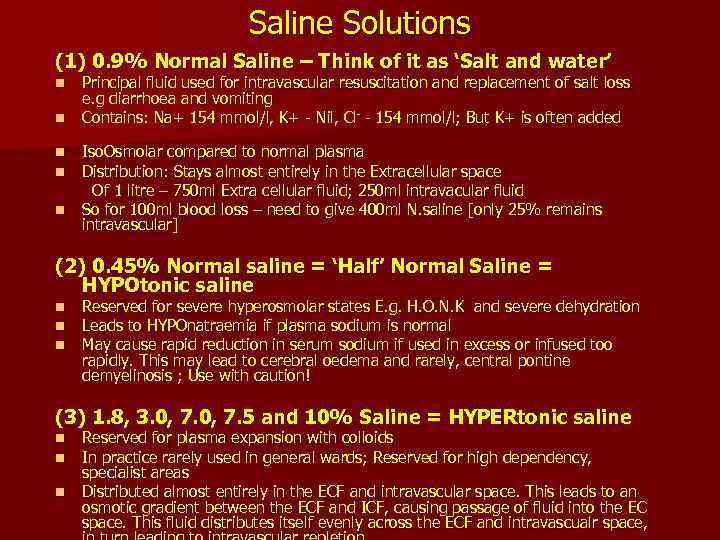 Saline Solutions (1) 0. 9% Normal Saline – Think of it as ‘Salt and water’ n n n Principal fluid used for intravascular resuscitation and replacement of salt loss e. g diarrhoea and vomiting Contains: Na+ 154 mmol/l, K+ - Nil, Cl- - 154 mmol/l; But K+ is often added Iso. Osmolar compared to normal plasma Distribution: Stays almost entirely in the Extracellular space Of 1 litre – 750 ml Extra cellular fluid; 250 ml intravacular fluid So for 100 ml blood loss – need to give 400 ml N. saline [only 25% remains intravascular] (2) 0. 45% Normal saline = ‘Half’ Normal Saline = HYPOtonic saline n n n Reserved for severe hyperosmolar states E. g. H. O. N. K and severe dehydration Leads to HYPOnatraemia if plasma sodium is normal May cause rapid reduction in serum sodium if used in excess or infused too rapidly. This may lead to cerebral oedema and rarely, central pontine demyelinosis ; Use with caution! (3) 1. 8, 3. 0, 7. 5 and 10% Saline = HYPERtonic saline n n n Reserved for plasma expansion with colloids In practice rarely used in general wards; Reserved for high dependency, specialist areas Distributed almost entirely in the ECF and intravascular space. This leads to an osmotic gradient between the ECF and ICF, causing passage of fluid into the EC space. This fluid distributes itself evenly across the ECF and intravascualr space,
Saline Solutions (1) 0. 9% Normal Saline – Think of it as ‘Salt and water’ n n n Principal fluid used for intravascular resuscitation and replacement of salt loss e. g diarrhoea and vomiting Contains: Na+ 154 mmol/l, K+ - Nil, Cl- - 154 mmol/l; But K+ is often added Iso. Osmolar compared to normal plasma Distribution: Stays almost entirely in the Extracellular space Of 1 litre – 750 ml Extra cellular fluid; 250 ml intravacular fluid So for 100 ml blood loss – need to give 400 ml N. saline [only 25% remains intravascular] (2) 0. 45% Normal saline = ‘Half’ Normal Saline = HYPOtonic saline n n n Reserved for severe hyperosmolar states E. g. H. O. N. K and severe dehydration Leads to HYPOnatraemia if plasma sodium is normal May cause rapid reduction in serum sodium if used in excess or infused too rapidly. This may lead to cerebral oedema and rarely, central pontine demyelinosis ; Use with caution! (3) 1. 8, 3. 0, 7. 5 and 10% Saline = HYPERtonic saline n n n Reserved for plasma expansion with colloids In practice rarely used in general wards; Reserved for high dependency, specialist areas Distributed almost entirely in the ECF and intravascular space. This leads to an osmotic gradient between the ECF and ICF, causing passage of fluid into the EC space. This fluid distributes itself evenly across the ECF and intravascualr space,
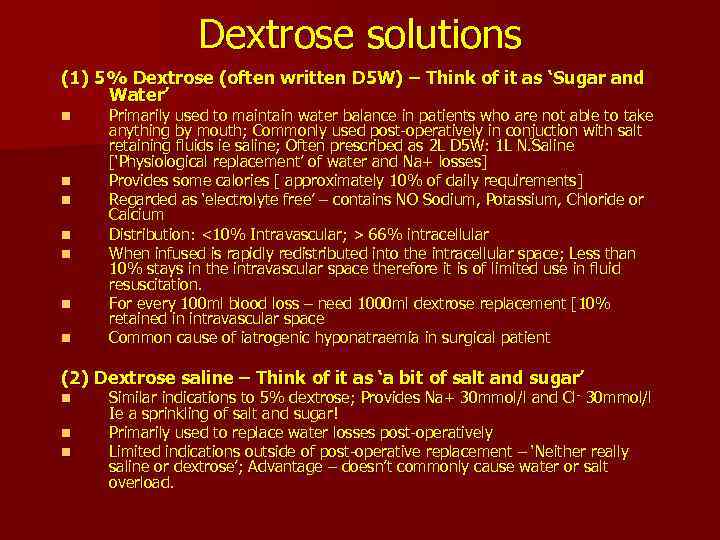 Dextrose solutions (1) 5% Dextrose (often written D 5 W) – Think of it as ‘Sugar and Water’ n n n n Primarily used to maintain water balance in patients who are not able to take anything by mouth; Commonly used post-operatively in conjuction with salt retaining fluids ie saline; Often prescribed as 2 L D 5 W: 1 L N. Saline [‘Physiological replacement’ of water and Na+ losses] Provides some calories [ approximately 10% of daily requirements] Regarded as ‘electrolyte free’ – contains NO Sodium, Potassium, Chloride or Calcium Distribution: <10% Intravascular; > 66% intracellular When infused is rapidly redistributed into the intracellular space; Less than 10% stays in the intravascular space therefore it is of limited use in fluid resuscitation. For every 100 ml blood loss – need 1000 ml dextrose replacement [10% retained in intravascular space Common cause of iatrogenic hyponatraemia in surgical patient (2) Dextrose saline – Think of it as ‘a bit of salt and sugar’ n n n Similar indications to 5% dextrose; Provides Na+ 30 mmol/l and Cl - 30 mmol/l Ie a sprinkling of salt and sugar! Primarily used to replace water losses post-operatively Limited indications outside of post-operative replacement – ‘Neither really saline or dextrose’; Advantage – doesn’t commonly cause water or salt overload.
Dextrose solutions (1) 5% Dextrose (often written D 5 W) – Think of it as ‘Sugar and Water’ n n n n Primarily used to maintain water balance in patients who are not able to take anything by mouth; Commonly used post-operatively in conjuction with salt retaining fluids ie saline; Often prescribed as 2 L D 5 W: 1 L N. Saline [‘Physiological replacement’ of water and Na+ losses] Provides some calories [ approximately 10% of daily requirements] Regarded as ‘electrolyte free’ – contains NO Sodium, Potassium, Chloride or Calcium Distribution: <10% Intravascular; > 66% intracellular When infused is rapidly redistributed into the intracellular space; Less than 10% stays in the intravascular space therefore it is of limited use in fluid resuscitation. For every 100 ml blood loss – need 1000 ml dextrose replacement [10% retained in intravascular space Common cause of iatrogenic hyponatraemia in surgical patient (2) Dextrose saline – Think of it as ‘a bit of salt and sugar’ n n n Similar indications to 5% dextrose; Provides Na+ 30 mmol/l and Cl - 30 mmol/l Ie a sprinkling of salt and sugar! Primarily used to replace water losses post-operatively Limited indications outside of post-operative replacement – ‘Neither really saline or dextrose’; Advantage – doesn’t commonly cause water or salt overload.
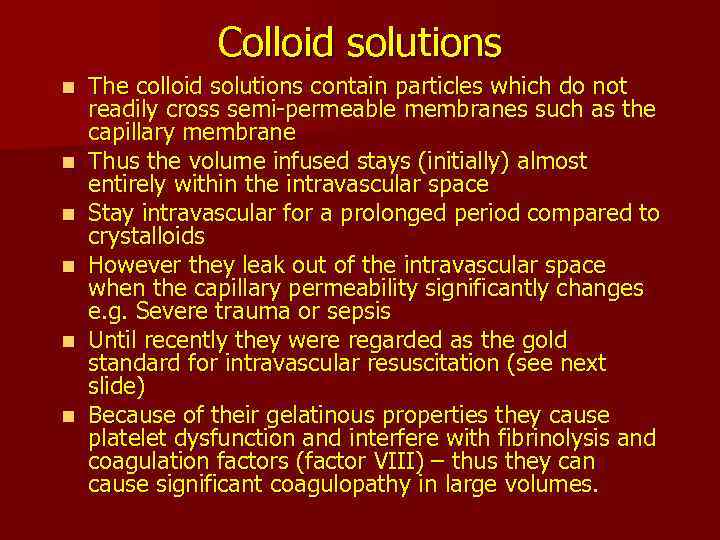 Colloid solutions n n n The colloid solutions contain particles which do not readily cross semi-permeable membranes such as the capillary membrane Thus the volume infused stays (initially) almost entirely within the intravascular space Stay intravascular for a prolonged period compared to crystalloids However they leak out of the intravascular space when the capillary permeability significantly changes e. g. Severe trauma or sepsis Until recently they were regarded as the gold standard for intravascular resuscitation (see next slide) Because of their gelatinous properties they cause platelet dysfunction and interfere with fibrinolysis and coagulation factors (factor VIII) – thus they can cause significant coagulopathy in large volumes.
Colloid solutions n n n The colloid solutions contain particles which do not readily cross semi-permeable membranes such as the capillary membrane Thus the volume infused stays (initially) almost entirely within the intravascular space Stay intravascular for a prolonged period compared to crystalloids However they leak out of the intravascular space when the capillary permeability significantly changes e. g. Severe trauma or sepsis Until recently they were regarded as the gold standard for intravascular resuscitation (see next slide) Because of their gelatinous properties they cause platelet dysfunction and interfere with fibrinolysis and coagulation factors (factor VIII) – thus they can cause significant coagulopathy in large volumes.
 Fluid Therapy n Quantitative Considerations are concern in fluid Management ( Volume ) n Qualitative Considerations oxygen-carrying capacity, coagulation, electrolyte and acid-base balance, and glucose metabolism are also of critical importance. ( Type )
Fluid Therapy n Quantitative Considerations are concern in fluid Management ( Volume ) n Qualitative Considerations oxygen-carrying capacity, coagulation, electrolyte and acid-base balance, and glucose metabolism are also of critical importance. ( Type )
 Fluid Resuscitation of Shock n Crystalloid Solutions – Normal saline – Ringers Lactate solution – Plasmalyte n Colloid Solutions – Pentastarch – Blood products (albumin, RBC, plasma)
Fluid Resuscitation of Shock n Crystalloid Solutions – Normal saline – Ringers Lactate solution – Plasmalyte n Colloid Solutions – Pentastarch – Blood products (albumin, RBC, plasma)
 Crystalloid Solutions n Normal Saline n Lactated Ringers Solution n Plasmalyte n Require 3: 1 replacement of volume loss n e. g. estimate 1 L blood loss, require 3 L of crystalloid to replace volume
Crystalloid Solutions n Normal Saline n Lactated Ringers Solution n Plasmalyte n Require 3: 1 replacement of volume loss n e. g. estimate 1 L blood loss, require 3 L of crystalloid to replace volume
 Colloid Solutions n HES n gelatin n Albumin 5% n Red Blood Cells n Fresh Frozen Plasma n Replacement of lost volume in 1: 1 ratio
Colloid Solutions n HES n gelatin n Albumin 5% n Red Blood Cells n Fresh Frozen Plasma n Replacement of lost volume in 1: 1 ratio
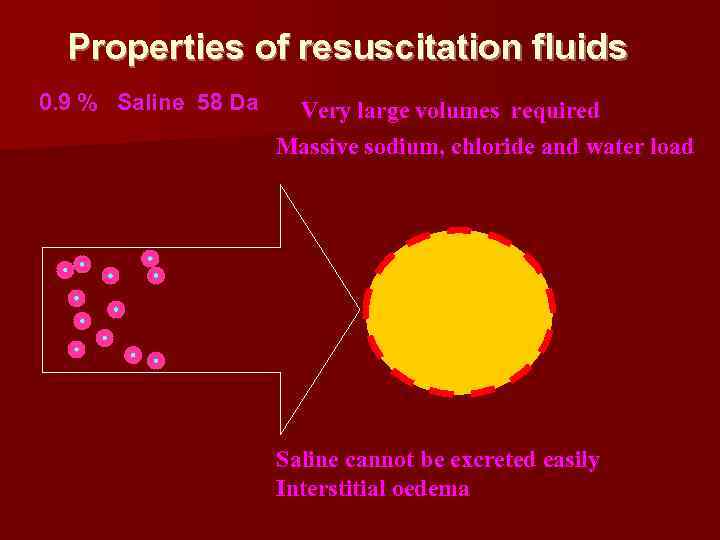 Properties of resuscitation fluids 0. 9 % Saline 58 Da Very large volumes required Massive sodium, chloride and water load Saline cannot be excreted easily Interstitial oedema
Properties of resuscitation fluids 0. 9 % Saline 58 Da Very large volumes required Massive sodium, chloride and water load Saline cannot be excreted easily Interstitial oedema
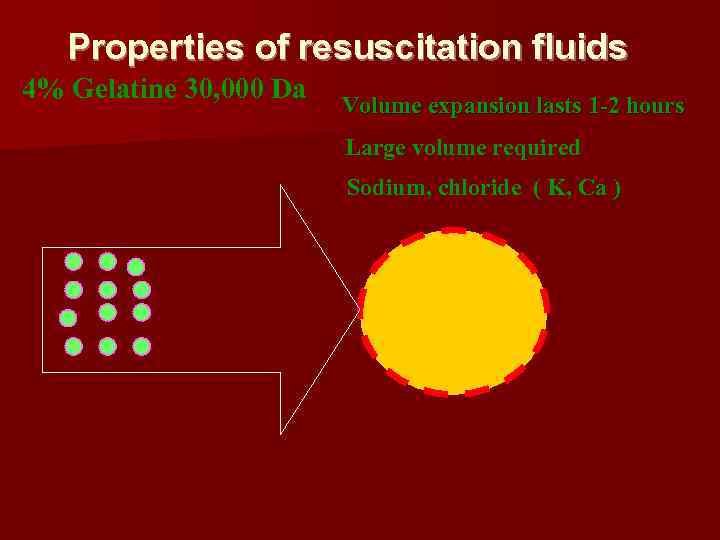 Properties of resuscitation fluids 4% Gelatine 30, 000 Da Volume expansion lasts 1 -2 hours Large volume required Sodium, chloride ( K, Ca )
Properties of resuscitation fluids 4% Gelatine 30, 000 Da Volume expansion lasts 1 -2 hours Large volume required Sodium, chloride ( K, Ca )
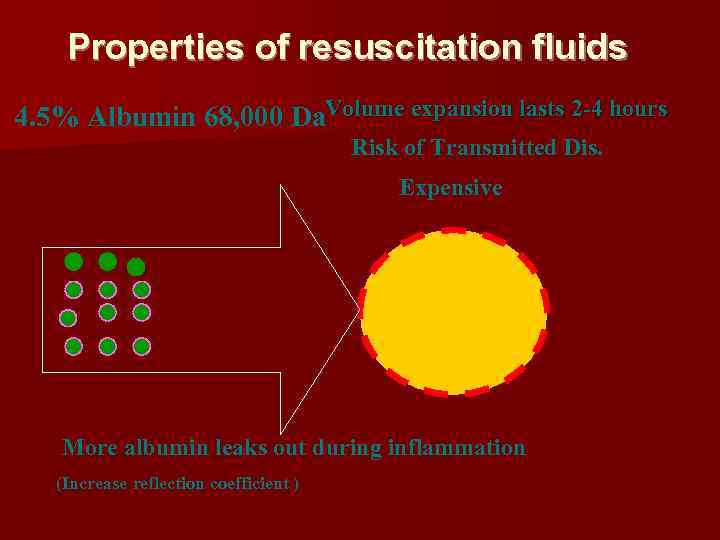 Properties of resuscitation fluids 4. 5% Albumin 68, 000 Da. Volume expansion lasts 2 -4 hours Risk of Transmitted Dis. Expensive More albumin leaks out during inflammation (Increase reflection coefficient )
Properties of resuscitation fluids 4. 5% Albumin 68, 000 Da. Volume expansion lasts 2 -4 hours Risk of Transmitted Dis. Expensive More albumin leaks out during inflammation (Increase reflection coefficient )
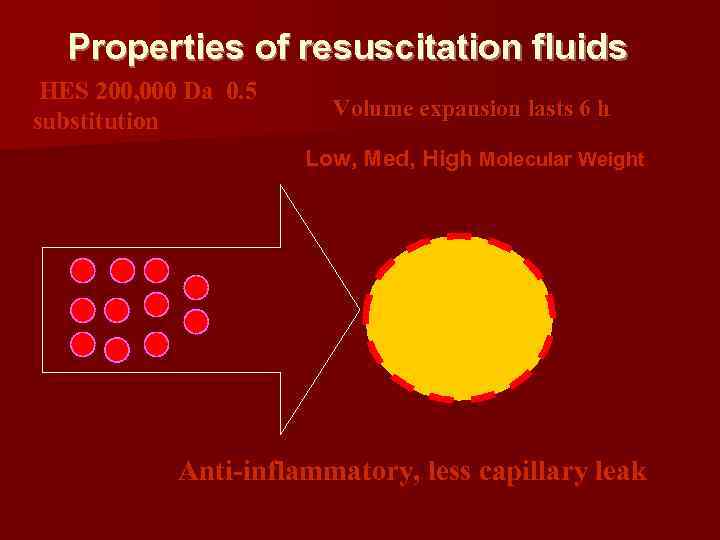 Properties of resuscitation fluids HES 200, 000 Da 0. 5 substitution Volume expansion lasts 6 h Low, Med, High Molecular Weight Anti-inflammatory, less capillary leak
Properties of resuscitation fluids HES 200, 000 Da 0. 5 substitution Volume expansion lasts 6 h Low, Med, High Molecular Weight Anti-inflammatory, less capillary leak
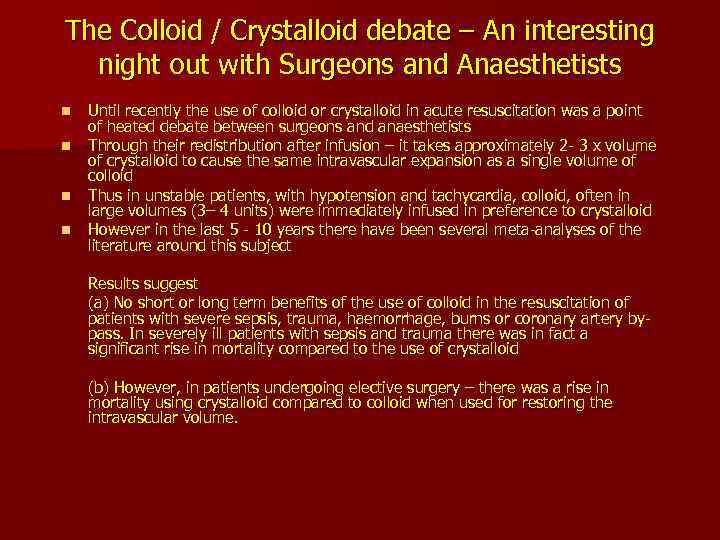 The Colloid / Crystalloid debate – An interesting night out with Surgeons and Anaesthetists n n Until recently the use of colloid or crystalloid in acute resuscitation was a point of heated debate between surgeons and anaesthetists Through their redistribution after infusion – it takes approximately 2 - 3 x volume of crystalloid to cause the same intravascular expansion as a single volume of colloid Thus in unstable patients, with hypotension and tachycardia, colloid, often in large volumes (3– 4 units) were immediately infused in preference to crystalloid However in the last 5 - 10 years there have been several meta-analyses of the literature around this subject Results suggest (a) No short or long term benefits of the use of colloid in the resuscitation of patients with severe sepsis, trauma, haemorrhage, burns or coronary artery bypass. In severely ill patients with sepsis and trauma there was in fact a significant rise in mortality compared to the use of crystalloid (b) However, in patients undergoing elective surgery – there was a rise in mortality using crystalloid compared to colloid when used for restoring the intravascular volume.
The Colloid / Crystalloid debate – An interesting night out with Surgeons and Anaesthetists n n Until recently the use of colloid or crystalloid in acute resuscitation was a point of heated debate between surgeons and anaesthetists Through their redistribution after infusion – it takes approximately 2 - 3 x volume of crystalloid to cause the same intravascular expansion as a single volume of colloid Thus in unstable patients, with hypotension and tachycardia, colloid, often in large volumes (3– 4 units) were immediately infused in preference to crystalloid However in the last 5 - 10 years there have been several meta-analyses of the literature around this subject Results suggest (a) No short or long term benefits of the use of colloid in the resuscitation of patients with severe sepsis, trauma, haemorrhage, burns or coronary artery bypass. In severely ill patients with sepsis and trauma there was in fact a significant rise in mortality compared to the use of crystalloid (b) However, in patients undergoing elective surgery – there was a rise in mortality using crystalloid compared to colloid when used for restoring the intravascular volume.
 Colloid or Crystalloid Resuscitation what should you do? Recommendations: n Colloid should NOT be used as the sole fluid replacement in resuscitation; Volumes infused should be limited because of side effects and lack of evidence for their continued use in the acutely ill. n In severely ill patients – principally use crystalloid and blood products; Colloid may be used in limited volume to reduce volume of fluids required or until blood products are available n In elective surgical patients – replace fluid loss with ‘physiological Hartmann’s and Ringer’s solutions; Blood products and colloid may be needed to replace intravascular volume acutely
Colloid or Crystalloid Resuscitation what should you do? Recommendations: n Colloid should NOT be used as the sole fluid replacement in resuscitation; Volumes infused should be limited because of side effects and lack of evidence for their continued use in the acutely ill. n In severely ill patients – principally use crystalloid and blood products; Colloid may be used in limited volume to reduce volume of fluids required or until blood products are available n In elective surgical patients – replace fluid loss with ‘physiological Hartmann’s and Ringer’s solutions; Blood products and colloid may be needed to replace intravascular volume acutely
 Oxygen Carrying Capacity n Only RBC contribute to oxygen carrying capacity (hemoglobin) n Replacement with all other solutions will – support volume – Improve end organ perfusion – Will NOT provide additional oxygen carrying capacity
Oxygen Carrying Capacity n Only RBC contribute to oxygen carrying capacity (hemoglobin) n Replacement with all other solutions will – support volume – Improve end organ perfusion – Will NOT provide additional oxygen carrying capacity
 RBC Transfusion n BC Red Cell Transfusion Guidelines recommend transfusion only to keep Hgb >70 g/d. L unless – Comorbid disease necessitating higher transfusion trigger (CAD, pulmonary disease, sepsis) – Hemodynamic instability despite adequate fluid resuscitation
RBC Transfusion n BC Red Cell Transfusion Guidelines recommend transfusion only to keep Hgb >70 g/d. L unless – Comorbid disease necessitating higher transfusion trigger (CAD, pulmonary disease, sepsis) – Hemodynamic instability despite adequate fluid resuscitation
 Goals of Fluid Resuscitation n Easily measured – Mentation – Blood Pressure – Heart Rate – Jugular Venous Pressure – Urine Output
Goals of Fluid Resuscitation n Easily measured – Mentation – Blood Pressure – Heart Rate – Jugular Venous Pressure – Urine Output
 Goals of Fluid Resuscitation n. A little less easily measured – Central Venous Pressure (CVP) – Left Atrial Pressure – Central Venous Oxygen Saturation SCVO 2
Goals of Fluid Resuscitation n. A little less easily measured – Central Venous Pressure (CVP) – Left Atrial Pressure – Central Venous Oxygen Saturation SCVO 2
 Goals of Fluid Resuscitation n. A bit more of a pain to measure – Pulmonary Capillary Wedge Pressure (PCWP) – Systemic Vascular Resistance (SVR) – Cardiac Output / Cardiac Index
Goals of Fluid Resuscitation n. A bit more of a pain to measure – Pulmonary Capillary Wedge Pressure (PCWP) – Systemic Vascular Resistance (SVR) – Cardiac Output / Cardiac Index
 Urine output A monitor of renal perfusion only, urine output is often used as a guide to adequacy of cardiac output as the kidney receives 25% of cardiac output. When renal perfusion is adequate urine output will > 0. 5 ml/kg/h. n n < 0. 5 ml/kg/h. Low Perfusion , inc Stress -> inc. ADH Positive P Vent -> dec. Atrial Natriuretic Peptide n Use of Diuretics such as Frusemide, Hyperglycemia and Dopamine abolishes its usefulness as a haemodynamic monitor.
Urine output A monitor of renal perfusion only, urine output is often used as a guide to adequacy of cardiac output as the kidney receives 25% of cardiac output. When renal perfusion is adequate urine output will > 0. 5 ml/kg/h. n n < 0. 5 ml/kg/h. Low Perfusion , inc Stress -> inc. ADH Positive P Vent -> dec. Atrial Natriuretic Peptide n Use of Diuretics such as Frusemide, Hyperglycemia and Dopamine abolishes its usefulness as a haemodynamic monitor.
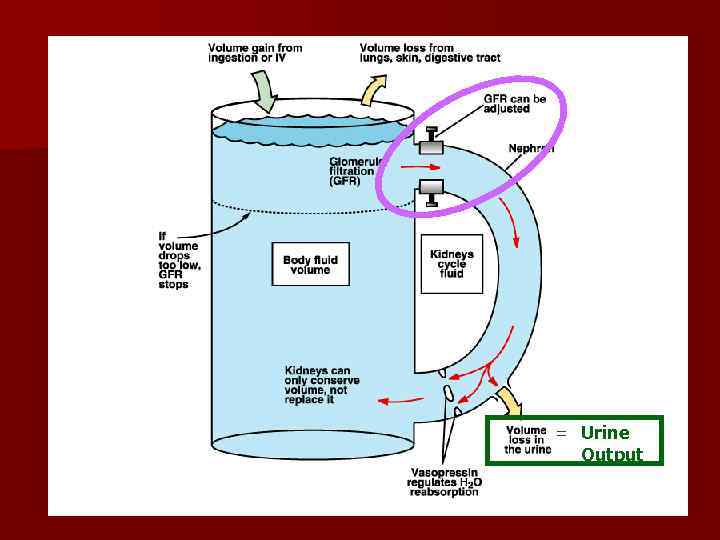 = Urine Output
= Urine Output
 Central Venous Pressure Catheter (CVP) n Principle : Measures of CVP but is useful to determine relative fluid balance n Utility Relative measurement of fluid status Allows large volume fluid administration Administration of potent vasoconstrictors epinephrine, norepinephrine
Central Venous Pressure Catheter (CVP) n Principle : Measures of CVP but is useful to determine relative fluid balance n Utility Relative measurement of fluid status Allows large volume fluid administration Administration of potent vasoconstrictors epinephrine, norepinephrine
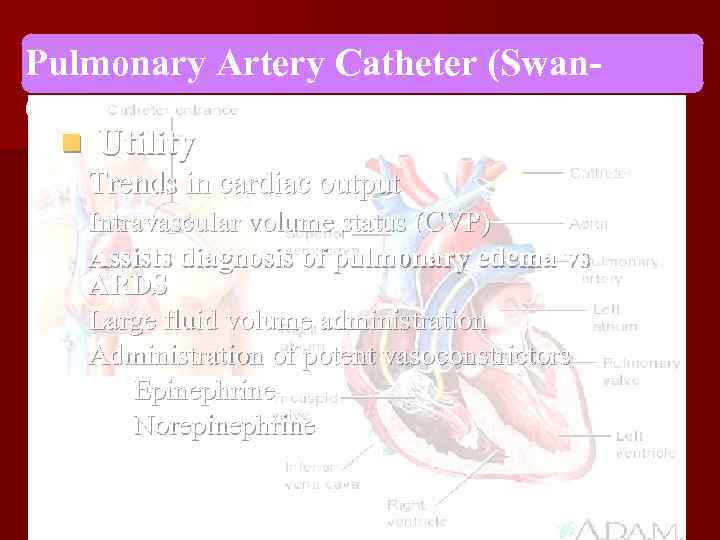 Pulmonary Artery Catheter (Swan. Ganz) n Utility Trends in cardiac output Intravascular volume status (CVP) Assists diagnosis of pulmonary edema vs ARDS Large fluid volume administration Administration of potent vasoconstrictors Epinephrine Norepinephrine
Pulmonary Artery Catheter (Swan. Ganz) n Utility Trends in cardiac output Intravascular volume status (CVP) Assists diagnosis of pulmonary edema vs ARDS Large fluid volume administration Administration of potent vasoconstrictors Epinephrine Norepinephrine
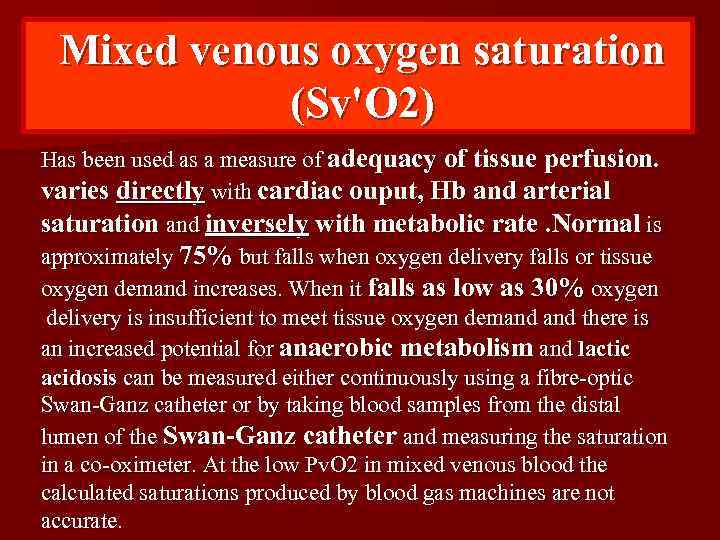 Mixed venous oxygen saturation (Sv'O 2) Has been used as a measure of adequacy of tissue perfusion. varies directly with cardiac ouput, Hb and arterial saturation and inversely with metabolic rate. Normal is approximately 75% but falls when oxygen delivery falls or tissue oxygen demand increases. When it falls as low as 30% oxygen delivery is insufficient to meet tissue oxygen demand there is an increased potential for anaerobic metabolism and lactic acidosis can be measured either continuously using a fibre-optic Swan-Ganz catheter or by taking blood samples from the distal lumen of the Swan-Ganz catheter and measuring the saturation in a co-oximeter. At the low Pv. O 2 in mixed venous blood the calculated saturations produced by blood gas machines are not accurate.
Mixed venous oxygen saturation (Sv'O 2) Has been used as a measure of adequacy of tissue perfusion. varies directly with cardiac ouput, Hb and arterial saturation and inversely with metabolic rate. Normal is approximately 75% but falls when oxygen delivery falls or tissue oxygen demand increases. When it falls as low as 30% oxygen delivery is insufficient to meet tissue oxygen demand there is an increased potential for anaerobic metabolism and lactic acidosis can be measured either continuously using a fibre-optic Swan-Ganz catheter or by taking blood samples from the distal lumen of the Swan-Ganz catheter and measuring the saturation in a co-oximeter. At the low Pv. O 2 in mixed venous blood the calculated saturations produced by blood gas machines are not accurate.
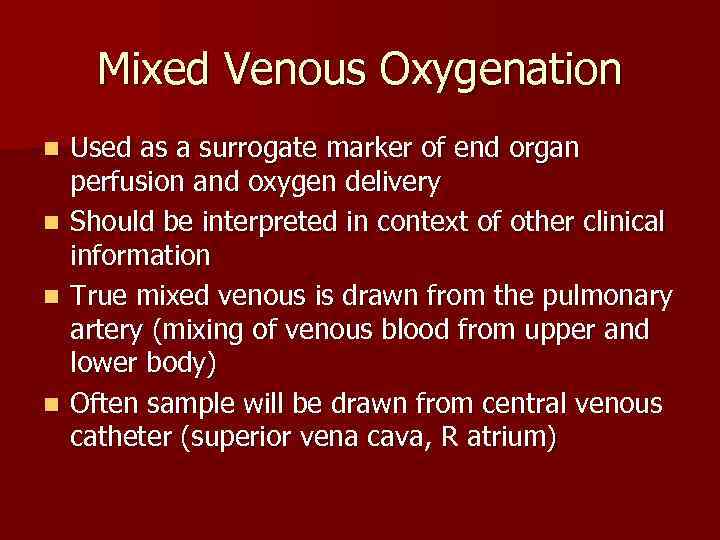 Mixed Venous Oxygenation n n Used as a surrogate marker of end organ perfusion and oxygen delivery Should be interpreted in context of other clinical information True mixed venous is drawn from the pulmonary artery (mixing of venous blood from upper and lower body) Often sample will be drawn from central venous catheter (superior vena cava, R atrium)
Mixed Venous Oxygenation n n Used as a surrogate marker of end organ perfusion and oxygen delivery Should be interpreted in context of other clinical information True mixed venous is drawn from the pulmonary artery (mixing of venous blood from upper and lower body) Often sample will be drawn from central venous catheter (superior vena cava, R atrium)
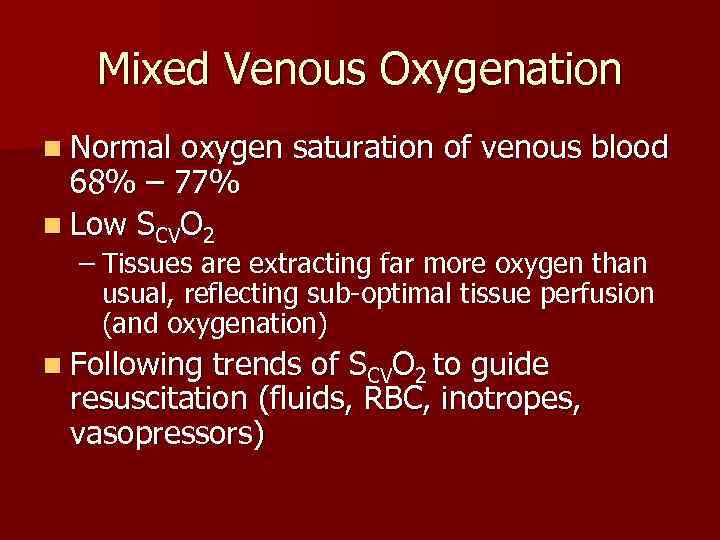 Mixed Venous Oxygenation n Normal oxygen saturation of venous blood 68% – 77% n Low SCVO 2 – Tissues are extracting far more oxygen than usual, reflecting sub-optimal tissue perfusion (and oxygenation) n Following trends of SCVO 2 to guide resuscitation (fluids, RBC, inotropes, vasopressors)
Mixed Venous Oxygenation n Normal oxygen saturation of venous blood 68% – 77% n Low SCVO 2 – Tissues are extracting far more oxygen than usual, reflecting sub-optimal tissue perfusion (and oxygenation) n Following trends of SCVO 2 to guide resuscitation (fluids, RBC, inotropes, vasopressors)
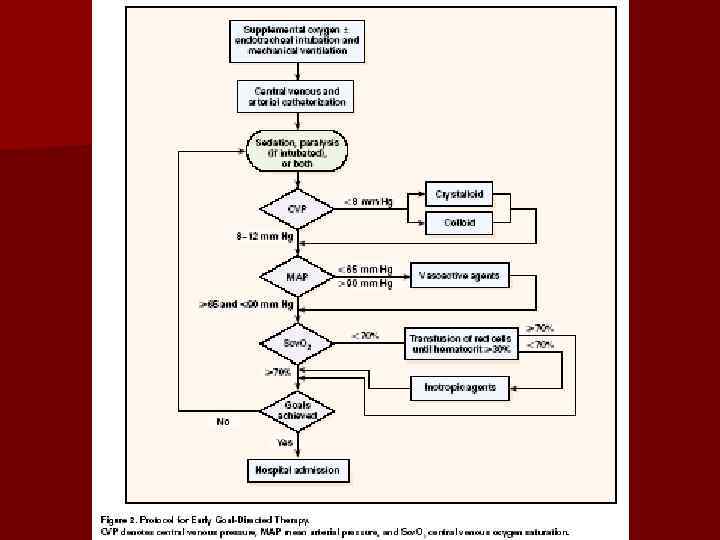
 Goals of Resuscitation n Rivers Study- Early Goal Directed Therapy in Sepsis and Septic Shock – Emergency department with severe sepsis or septic shock, randomized to goal directed protocol vs standard therapy prior to admission to ICU – Early goal directed therapy conferred lower APACHE scores, incidating less severe organ dysfunction
Goals of Resuscitation n Rivers Study- Early Goal Directed Therapy in Sepsis and Septic Shock – Emergency department with severe sepsis or septic shock, randomized to goal directed protocol vs standard therapy prior to admission to ICU – Early goal directed therapy conferred lower APACHE scores, incidating less severe organ dysfunction
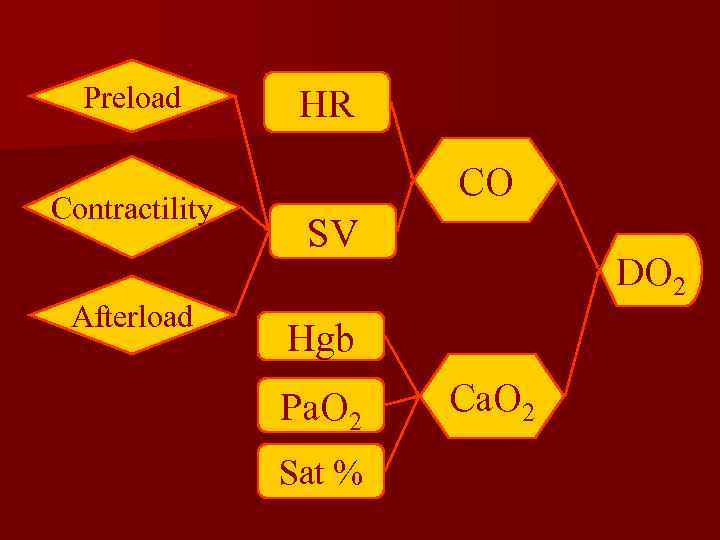 Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
Preload Contractility Afterload HR CO SV DO 2 Hgb Pa. O 2 Sat % Ca. O 2
 Bottom Line n n Resuscitation of Shock is all about getting oxygen to the tissues Initial assessment of volume deficit, replace that (with crystalloid), and reassess Continue volume resuscitation to target endpoints Can use mixed venous oxygen saturation to estimate tissue perfusion and oxygenation
Bottom Line n n Resuscitation of Shock is all about getting oxygen to the tissues Initial assessment of volume deficit, replace that (with crystalloid), and reassess Continue volume resuscitation to target endpoints Can use mixed venous oxygen saturation to estimate tissue perfusion and oxygenation
 Adverse outcomes Inadequate or Excessive fluid administration • Inadequate fluid administration can lead to a reduced effective circulating volume, diversion of blood toward vital organs (brain and heart) and away from nonvital organs (gut, skin, and kidneys), and inadequate tissue perfusion of the nonvital organs
Adverse outcomes Inadequate or Excessive fluid administration • Inadequate fluid administration can lead to a reduced effective circulating volume, diversion of blood toward vital organs (brain and heart) and away from nonvital organs (gut, skin, and kidneys), and inadequate tissue perfusion of the nonvital organs
 • Excess - Fluid increased pressure in venous circulation and results in loss of fluid from the intravascular space into interstitial (extracellular) space leads pulmonary and peripheral edema and consequent compromise of systemic and/or local tissue oxygenation Decrease wound healing - Intestinal edema is associated with impaired gastrointestinal function tolerance for enteral nutrition an increased the development of bacterial translocation, and the development of multiple organ dysfunction syndrome
• Excess - Fluid increased pressure in venous circulation and results in loss of fluid from the intravascular space into interstitial (extracellular) space leads pulmonary and peripheral edema and consequent compromise of systemic and/or local tissue oxygenation Decrease wound healing - Intestinal edema is associated with impaired gastrointestinal function tolerance for enteral nutrition an increased the development of bacterial translocation, and the development of multiple organ dysfunction syndrome
 Conclusion n Crystalloid and colloid n Balanced versus saline-based fluids n Correct dosage of fluid improves outcome Role of LV stroke volume Titration for Max CO - CVP - PAOP - Oesophageal Doppler. - Etc.
Conclusion n Crystalloid and colloid n Balanced versus saline-based fluids n Correct dosage of fluid improves outcome Role of LV stroke volume Titration for Max CO - CVP - PAOP - Oesophageal Doppler. - Etc.
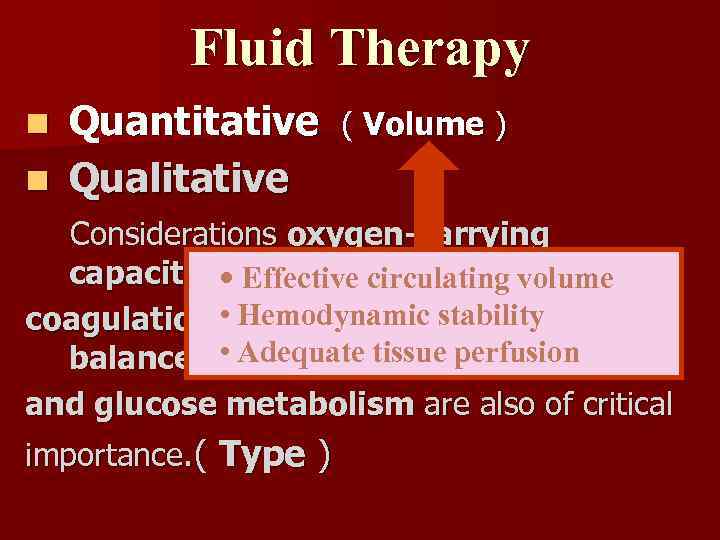 Fluid Therapy Quantitative n Qualitative n ( Volume ) Considerations oxygen-carrying capacity, • Effective circulating volume Hemodynamic stability coagulation, • electrolyte and acid-base balance, • Adequate tissue perfusion and glucose metabolism are also of critical importance. ( Type )
Fluid Therapy Quantitative n Qualitative n ( Volume ) Considerations oxygen-carrying capacity, • Effective circulating volume Hemodynamic stability coagulation, • electrolyte and acid-base balance, • Adequate tissue perfusion and glucose metabolism are also of critical importance. ( Type )
 Thank You
Thank You


