fdab82a63c82d7cec9ed61162bbb8183.ppt
- Количество слайдов: 14
Florida Medicaid Update July 2015 Evelyn Leadbetter, MPA HTH Network Services Manager
Continuity of Care Requirements A key goal of the Statewide Medicaid Managed Care (SMMC) program is ensuring that recipients experience continuity of care, meaning that recipients experience no break in services or care coordination while transitioning from one service delivery system to another, one health plan to another, or from one service provider to another. The following is a reminder of the protections that apply for any Medicaid recipient who changes health plans: Health care providers should not cancel appointments with current patients. Health plans must honor any ongoing treatment that was authorized or scheduled prior to the recipient’s enrollment into the new health plan for up to 60 days after the recipient enrolls in the plan. Providers will be paid. Providers should continue providing any services that were previously authorized, regardless of whether the provider is participating in the plan’s network. Plans must pay providers for previously authorized services for up to 60 days, and must pay non-network providers at the rate previously received for up to 30 days. Prescriptions will be honored. Plans must allow recipients to continue to receive their prescriptions through their current provider, for up to 60 days, until their prescriptions can be transferred to a provider in the plan’s network.
Continuity of Care Requirements How does Sunshine, Staywell and Prestige ensure that these terms of the state contract are met? Example: On June 20 th patient is covered under Sunshine State when their doctor orders a test at the hospital and the hospital receives preauthorization from Sunshine State for test on July 3 rd. Patient elects to move his coverage to Staywell on June 21 st and goes into effect on July 1. Who is responsible for paying the claim? AHCA states: Health plans must honor any ongoing treatment that was authorized or scheduled prior to the recipient’s enrollment into the new health plan for up to 60 days after the recipient enrolls in the plan.
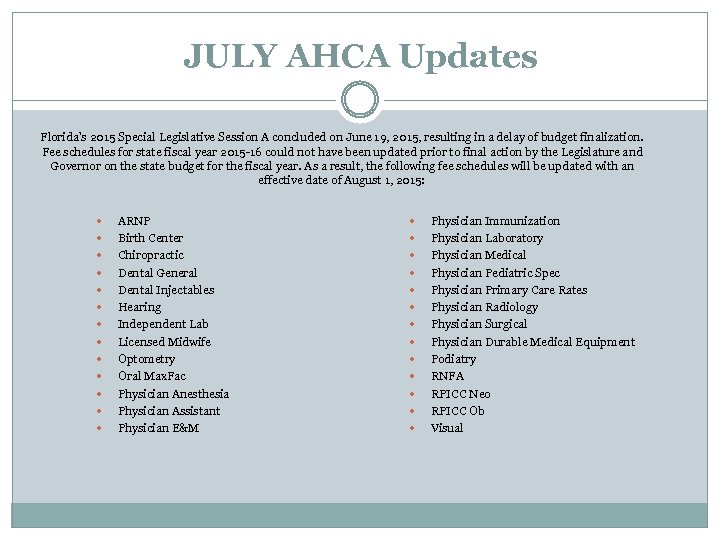
JULY AHCA Updates Florida’s 2015 Special Legislative Session A concluded on June 19, 2015, resulting in a delay of budget finalization. Fee schedules for state fiscal year 2015 -16 could not have been updated prior to final action by the Legislature and Governor on the state budget for the fiscal year. As a result, the following fee schedules will be updated with an effective date of August 1, 2015: ARNP Birth Center Chiropractic Dental General Dental Injectables Hearing Independent Lab Licensed Midwife Optometry Oral Max. Fac Physician Anesthesia Physician Assistant Physician E&M Physician Immunization Physician Laboratory Physician Medical Physician Pediatric Spec Physician Primary Care Rates Physician Radiology Physician Surgical Physician Durable Medical Equipment Podiatry RNFA RPICC Neo RPICC Ob Visual
JULY AHCA Updates Florida Medicaid July ICD-10 Newsletter Now Available In this issue: The Final Countdown Dual Coding Challenge Center for Medicare and Medicaid Services’ Second End-to-End Testing Save the Date: ICD-10 Managed Care Testing ICD-10 Workshops and Webinars
JULY AHCA Updates AHCA, along with its fiscal agent, HP Enterprise Services, will soon be coordinating ICD-10 provider testing to ensure readiness for the upcoming transition to ICD-10 Testing for all provider types will begin on August 3, 2015. To register for testing, please visit the ICD-10 Provider Testing Registration Site.
MLN Connects National Provider Call: Countdown to ICD-10 Thursday, August 27; 2: 30 -4 pm ET To Register: Visit MLN Connects Event Registration. Space may be limited, register early. Agenda National implementation update Coding guidance How to get answers to coding questions Claims that span the implementation date Results from acknowledgement and end-toend testing weeks Provider resources Target Audience: Medical coders, physicians, physician office staff, nurses and other non-physician practitioners, provider billing staff, health records staff, vendors, educators, system maintainers, laboratories, and all Medicare providers.
Patient Look Up (PLU) Webinar Provider organizations of all sizes – large hospital systems, small hospitals, rural hospitals, group practices, and sole practitioners – are invited to learn more about the service during our upcoming webinar. A brief Q&A will follow the presentation. Thursday, July 23, 2015 at 10: 00 am ET Register here – https: //attendee. gotowebinar. com/register/78015983166024 29698
Summer 2015 Florida Medicaid Provider Bulletin The bulletin contains articles related to: Non-Emergency Transportation Update Changes in Medicaid Summary of Services Medicaid Eligibility for Newborn Babies Facts about Medicare Part D Payment Error Rate Measure Project (2014) Update
Florida Medicaid Readiness and Training AHCA Registration for Area-Specific ICD-10 Training Staywell/Wellcare of Florida ICD-10 Compliance ICD-10 July Impact Assessment Survey • Sunshine Health ICD-10 Overview • Prestige July Provider Training: Access CMS Open Door Forum Information and sign up for July ODFs here. News Bytes – July/August 2015 Florida’s Health IT Initiatives Medicaid. gov ICD-10 Changes from ICD-9
Wellcare 2015 Provider Newsletters Provider Resources Well. Care will be compliant with the Centers for Medicare & Medicaid Services (CMS) rule for ICD-10 readiness beginning Oct. 1, 2015. Dual Processing of ICD-9 and ICD-10 Codes
Sunshine Health Important Provider Information: Univita ATA of Florida has a new Intake Form. This form must be used for all therapy requests effective immediately. Provider Resources
Prestige August is projected to include the updating of benefits, currently pending State approval. In regard to services currently deemed to need pre-certification The CPT codes will be lifted and the procedures won't require authorizations in advance. One service that is included in this change is the mammography, both diagnostic and routine screenings. Additional services will be announced following state approval. ICD-10 Implementation Connections provider newsletter
THANK YOU!
fdab82a63c82d7cec9ed61162bbb8183.ppt