First step into insulin therapy.ppt
- Количество слайдов: 98
 First step into insulin therapy (How to start insulin in a patient not controlled on OADs) By Dr. Muhammad Tahir Chaudhry B. Sc. M. B; B. S(Pb). C. diabetology(USA)
First step into insulin therapy (How to start insulin in a patient not controlled on OADs) By Dr. Muhammad Tahir Chaudhry B. Sc. M. B; B. S(Pb). C. diabetology(USA)
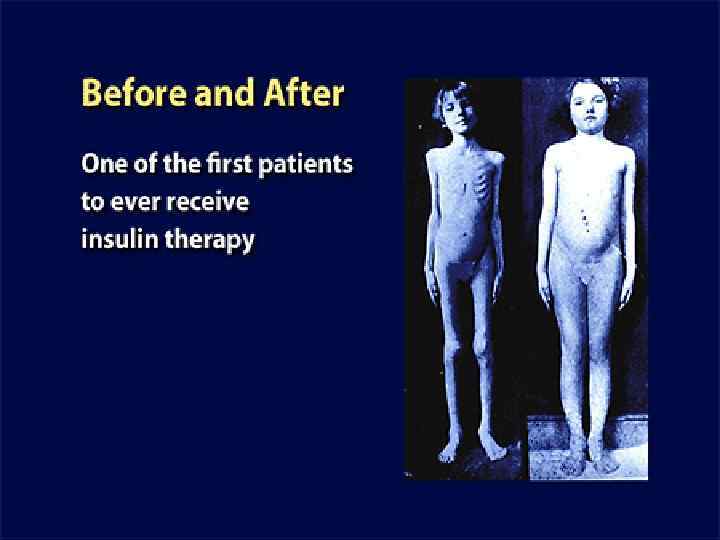
 The breakthrough: Toronto 1921 – Banting & Best
The breakthrough: Toronto 1921 – Banting & Best
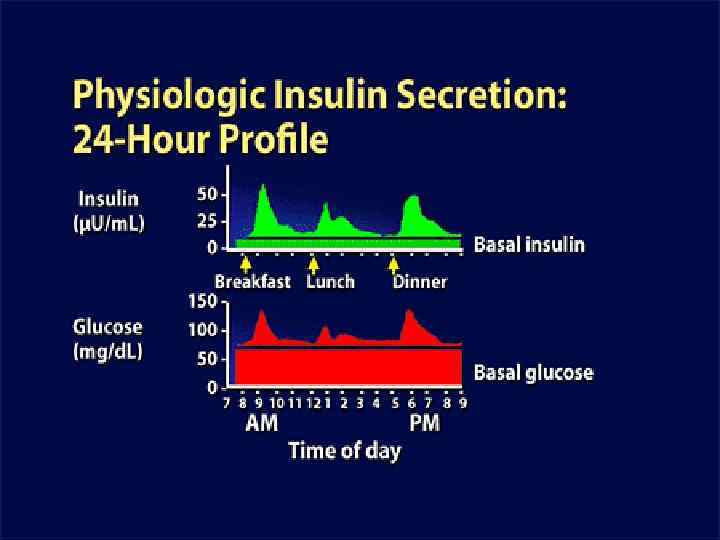
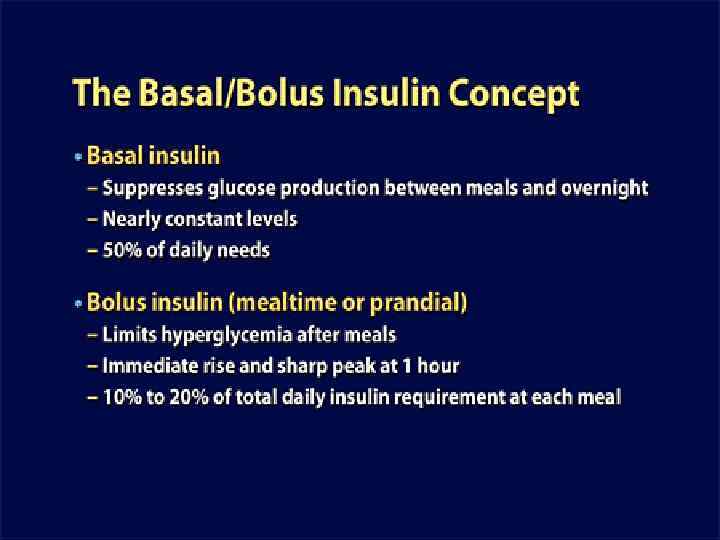
 Normal physiologic patterns of glucose and insulin secretion in our body
Normal physiologic patterns of glucose and insulin secretion in our body
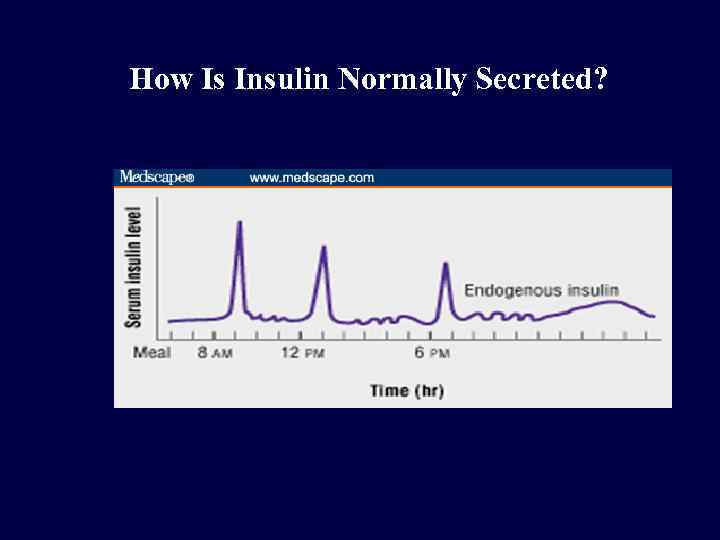 How Is Insulin Normally Secreted?
How Is Insulin Normally Secreted?
 The rapid early rise of insulin secretion in response to a meal is critical, because ü it ensures the prompt inhibition of endogenous glucose production by the liver üdisposal of the mealtime carbohydrate load, thus limiting postprandial glucose excursions.
The rapid early rise of insulin secretion in response to a meal is critical, because ü it ensures the prompt inhibition of endogenous glucose production by the liver üdisposal of the mealtime carbohydrate load, thus limiting postprandial glucose excursions.
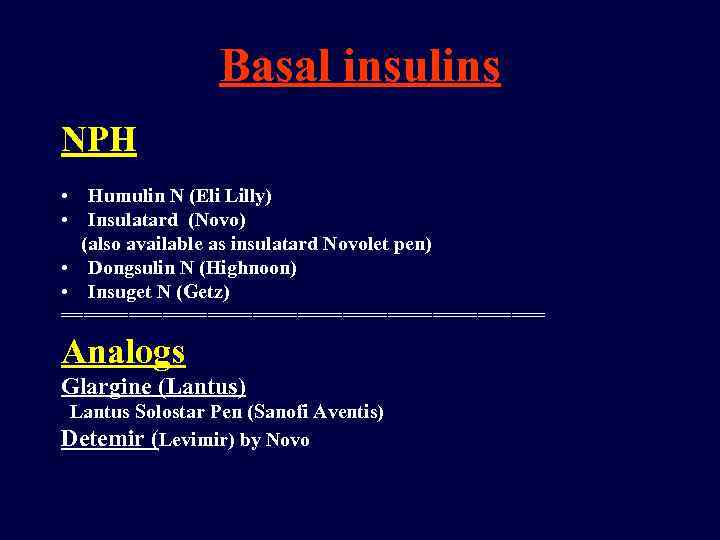 Basal insulins NPH • Humulin N (Eli Lilly) • Insulatard (Novo) (also available as insulatard Novolet pen) • Dongsulin N (Highnoon) • Insuget N (Getz) ====================== Analogs Glargine (Lantus) Lantus Solostar Pen (Sanofi Aventis) Detemir (Levimir) by Novo
Basal insulins NPH • Humulin N (Eli Lilly) • Insulatard (Novo) (also available as insulatard Novolet pen) • Dongsulin N (Highnoon) • Insuget N (Getz) ====================== Analogs Glargine (Lantus) Lantus Solostar Pen (Sanofi Aventis) Detemir (Levimir) by Novo
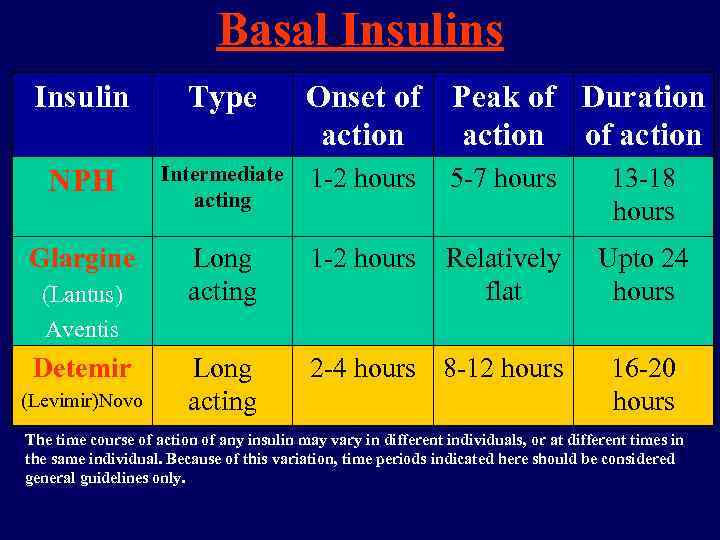 Basal Insulins Insulin Type Onset of action Peak of Duration action of action NPH Intermediate acting 1 -2 hours 5 -7 hours 13 -18 hours Glargine Long acting 1 -2 hours Relatively flat Upto 24 hours Long acting 2 -4 hours 8 -12 hours (Lantus) Aventis Detemir (Levimir)Novo 16 -20 hours The time course of action of any insulin may vary in different individuals, or at different times in the same individual. Because of this variation, time periods indicated here should be considered general guidelines only.
Basal Insulins Insulin Type Onset of action Peak of Duration action of action NPH Intermediate acting 1 -2 hours 5 -7 hours 13 -18 hours Glargine Long acting 1 -2 hours Relatively flat Upto 24 hours Long acting 2 -4 hours 8 -12 hours (Lantus) Aventis Detemir (Levimir)Novo 16 -20 hours The time course of action of any insulin may vary in different individuals, or at different times in the same individual. Because of this variation, time periods indicated here should be considered general guidelines only.
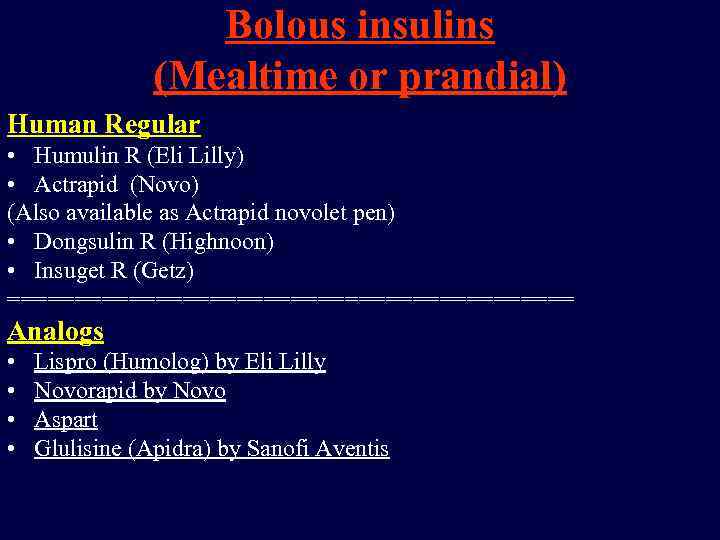 Bolous insulins (Mealtime or prandial) Human Regular • Humulin R (Eli Lilly) • Actrapid (Novo) (Also available as Actrapid novolet pen) • Dongsulin R (Highnoon) • Insuget R (Getz) ===================== Analogs • • Lispro (Humolog) by Eli Lilly Novorapid by Novo Aspart Glulisine (Apidra) by Sanofi Aventis
Bolous insulins (Mealtime or prandial) Human Regular • Humulin R (Eli Lilly) • Actrapid (Novo) (Also available as Actrapid novolet pen) • Dongsulin R (Highnoon) • Insuget R (Getz) ===================== Analogs • • Lispro (Humolog) by Eli Lilly Novorapid by Novo Aspart Glulisine (Apidra) by Sanofi Aventis
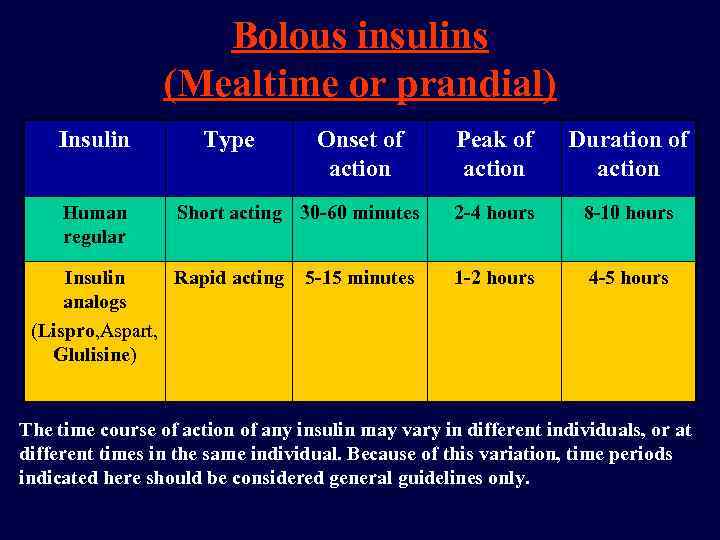 Bolous insulins (Mealtime or prandial) Insulin Human regular Type Onset of action Short acting 30 -60 minutes Insulin Rapid acting analogs (Lispro, Aspart, Glulisine) 5 -15 minutes Peak of action Duration of action 2 -4 hours 8 -10 hours 1 -2 hours 4 -5 hours The time course of action of any insulin may vary in different individuals, or at different times in the same individual. Because of this variation, time periods indicated here should be considered general guidelines only.
Bolous insulins (Mealtime or prandial) Insulin Human regular Type Onset of action Short acting 30 -60 minutes Insulin Rapid acting analogs (Lispro, Aspart, Glulisine) 5 -15 minutes Peak of action Duration of action 2 -4 hours 8 -10 hours 1 -2 hours 4 -5 hours The time course of action of any insulin may vary in different individuals, or at different times in the same individual. Because of this variation, time periods indicated here should be considered general guidelines only.
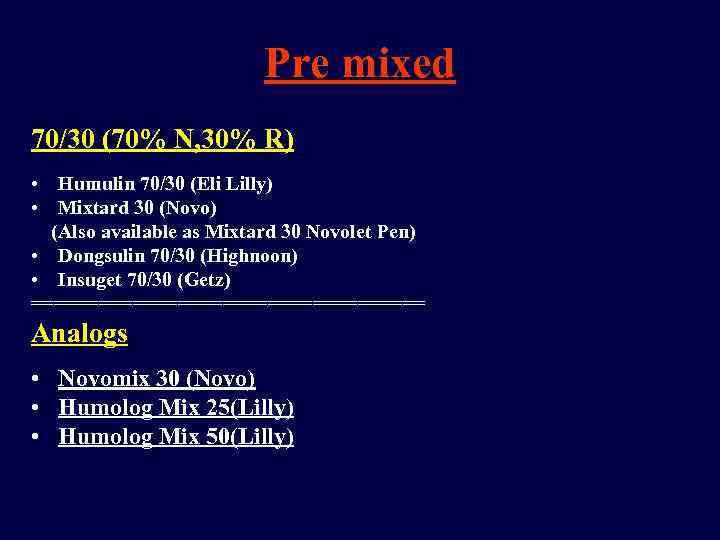 Pre mixed 70/30 (70% N, 30% R) • Humulin 70/30 (Eli Lilly) • Mixtard 30 (Novo) (Also available as Mixtard 30 Novolet Pen) • Dongsulin 70/30 (Highnoon) • Insuget 70/30 (Getz) ================== Analogs • Novomix 30 (Novo) • Humolog Mix 25(Lilly) • Humolog Mix 50(Lilly)
Pre mixed 70/30 (70% N, 30% R) • Humulin 70/30 (Eli Lilly) • Mixtard 30 (Novo) (Also available as Mixtard 30 Novolet Pen) • Dongsulin 70/30 (Highnoon) • Insuget 70/30 (Getz) ================== Analogs • Novomix 30 (Novo) • Humolog Mix 25(Lilly) • Humolog Mix 50(Lilly)
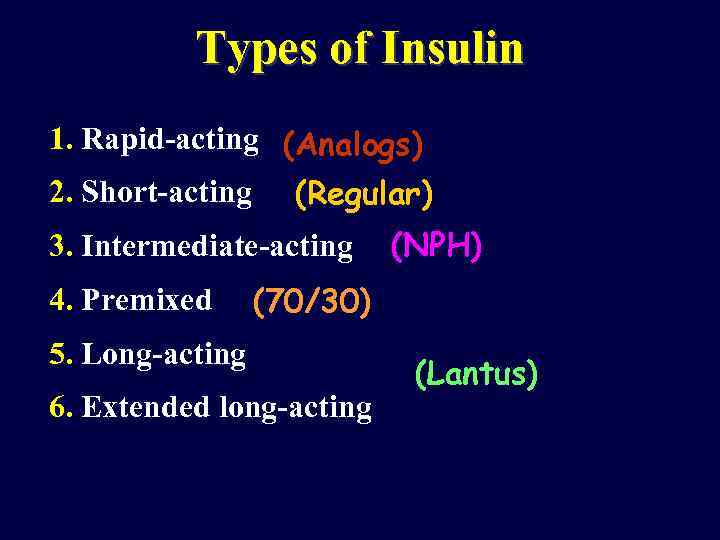 Types of Insulin 1. Rapid-acting (Analogs) 2. Short-acting (Regular) 3. Intermediate-acting 4. Premixed (NPH) (70/30) 5. Long-acting 6. Extended long-acting (Lantus)
Types of Insulin 1. Rapid-acting (Analogs) 2. Short-acting (Regular) 3. Intermediate-acting 4. Premixed (NPH) (70/30) 5. Long-acting 6. Extended long-acting (Lantus)
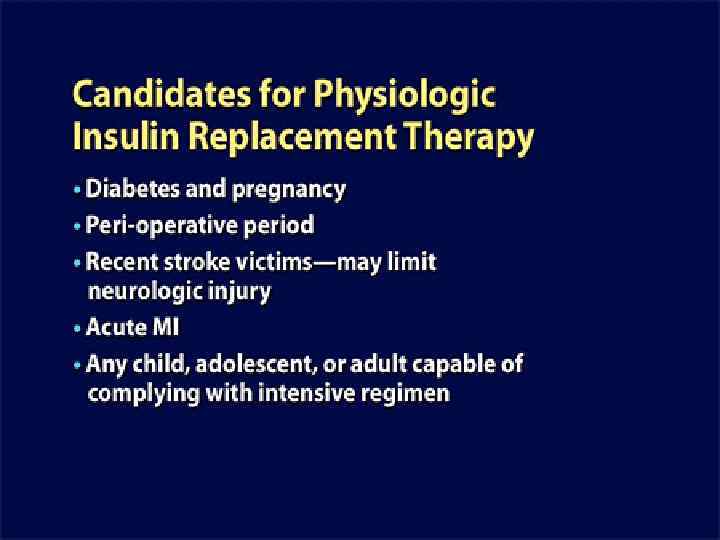
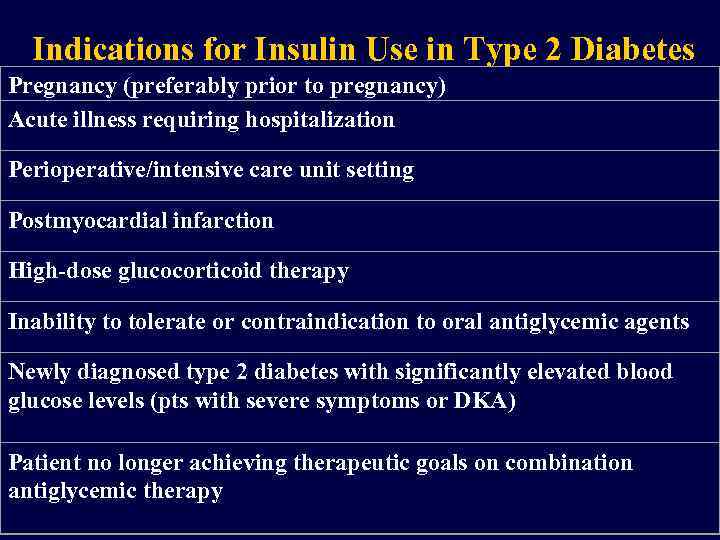 Indications for Insulin Use in Type 2 Diabetes Pregnancy (preferably prior to pregnancy) Acute illness requiring hospitalization Perioperative/intensive care unit setting Postmyocardial infarction High-dose glucocorticoid therapy Inability to tolerate or contraindication to oral antiglycemic agents Newly diagnosed type 2 diabetes with significantly elevated blood glucose levels (pts with severe symptoms or DKA) Patient no longer achieving therapeutic goals on combination antiglycemic therapy
Indications for Insulin Use in Type 2 Diabetes Pregnancy (preferably prior to pregnancy) Acute illness requiring hospitalization Perioperative/intensive care unit setting Postmyocardial infarction High-dose glucocorticoid therapy Inability to tolerate or contraindication to oral antiglycemic agents Newly diagnosed type 2 diabetes with significantly elevated blood glucose levels (pts with severe symptoms or DKA) Patient no longer achieving therapeutic goals on combination antiglycemic therapy
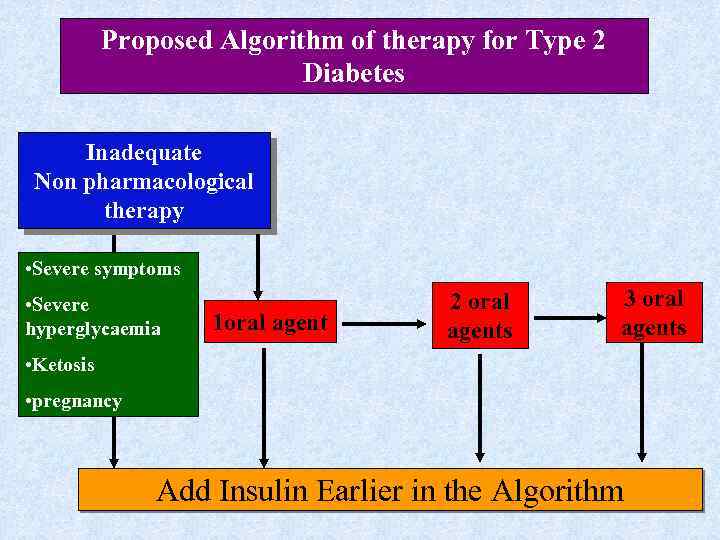 Proposed Algorithm of therapy for Type 2 Diabetes Inadequate Non pharmacological therapy • Severe symptoms • Severe hyperglycaemia 1 oral agent 2 oral agents 3 oral agents • Ketosis • pregnancy Add Insulin Earlier in the Algorithm
Proposed Algorithm of therapy for Type 2 Diabetes Inadequate Non pharmacological therapy • Severe symptoms • Severe hyperglycaemia 1 oral agent 2 oral agents 3 oral agents • Ketosis • pregnancy Add Insulin Earlier in the Algorithm
 First step into Insulin therapy
First step into Insulin therapy
 What we have in our pockets? • Basal Insulins (NPH, Lantus) • Bolus Insulins(Human Regular) • Premixed (Human 70/30)
What we have in our pockets? • Basal Insulins (NPH, Lantus) • Bolus Insulins(Human Regular) • Premixed (Human 70/30)
 The ADA Recommendations on the Use of Insulin in Type 2 Diabetes
The ADA Recommendations on the Use of Insulin in Type 2 Diabetes
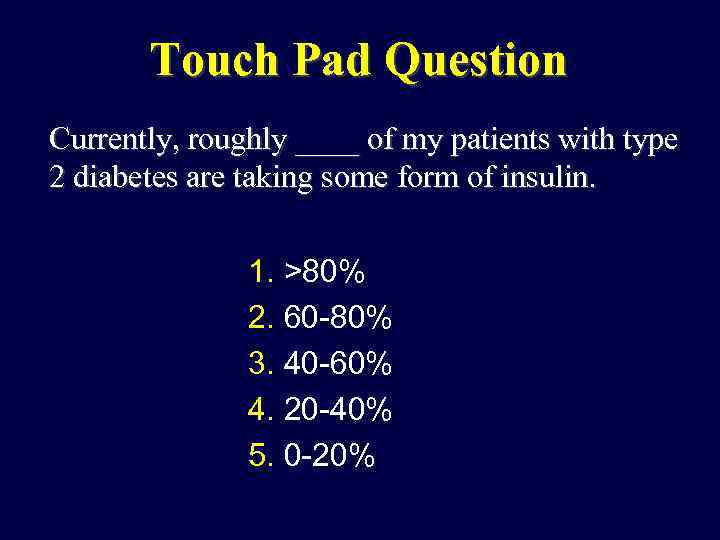 Touch Pad Question Currently, roughly ____ of my patients with type 2 diabetes are taking some form of insulin. 1. >80% 2. 60 -80% 3. 40 -60% 4. 20 -40% 5. 0 -20%
Touch Pad Question Currently, roughly ____ of my patients with type 2 diabetes are taking some form of insulin. 1. >80% 2. 60 -80% 3. 40 -60% 4. 20 -40% 5. 0 -20%
 Touch Pad Question When it comes to first-line insulin, I tend to prescribe: 1. An intermediate-acting insulin with fast-acting insulin as needed 2. A long-acting or extended long-acting insulin with fast-acting insulin as needed 3. A premixed insulin
Touch Pad Question When it comes to first-line insulin, I tend to prescribe: 1. An intermediate-acting insulin with fast-acting insulin as needed 2. A long-acting or extended long-acting insulin with fast-acting insulin as needed 3. A premixed insulin
 Advantages of Insulin Therapy • Oldest of the currently available medications, has the most clinical experience • Most effective of the diabetes medications in lowering glycemia – Can decrease any level of elevated Hb. A 1 c – No maximum dose of insulin beyond which a therapeutic effect will not occur • Beneficial effects on triglyceride and HDL cholesterol levels Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Advantages of Insulin Therapy • Oldest of the currently available medications, has the most clinical experience • Most effective of the diabetes medications in lowering glycemia – Can decrease any level of elevated Hb. A 1 c – No maximum dose of insulin beyond which a therapeutic effect will not occur • Beneficial effects on triglyceride and HDL cholesterol levels Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
 Disadvantages of Insulin Therapy • Weight gain ~ 2 -4 kg – May adversely affect cardiovascular health • Hypoglycemia – However, rates of severe hypoglycemia in patients with type 2 diabetes are low… § Type 1 DM: 61 events per 100 patient-years § Type 2 DM: 1 -3 events per 100 patient-years Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Disadvantages of Insulin Therapy • Weight gain ~ 2 -4 kg – May adversely affect cardiovascular health • Hypoglycemia – However, rates of severe hypoglycemia in patients with type 2 diabetes are low… § Type 1 DM: 61 events per 100 patient-years § Type 2 DM: 1 -3 events per 100 patient-years Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
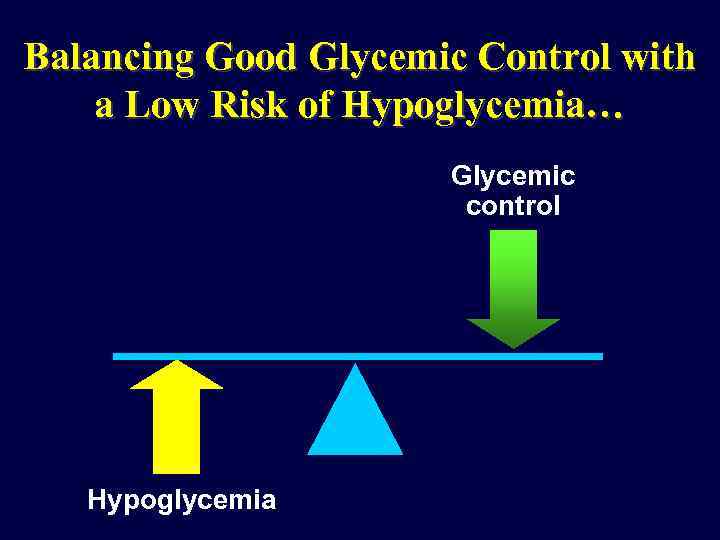 Balancing Good Glycemic Control with a Low Risk of Hypoglycemia… Glycemic control Hypoglycemia
Balancing Good Glycemic Control with a Low Risk of Hypoglycemia… Glycemic control Hypoglycemia
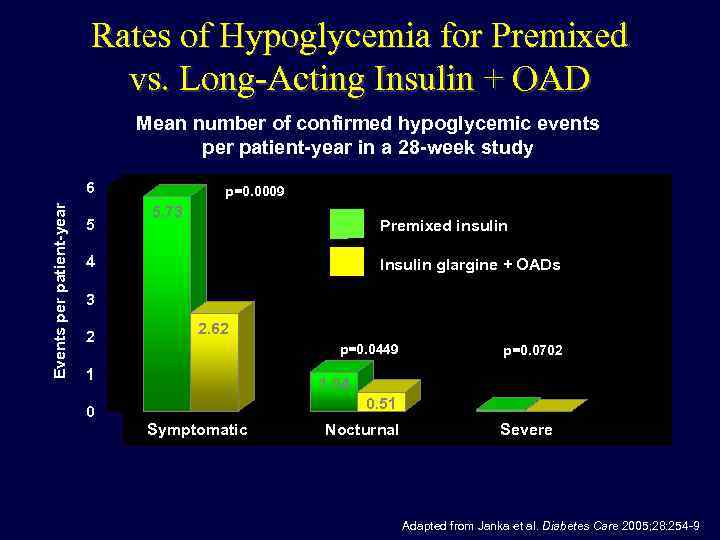 Rates of Hypoglycemia for Premixed vs. Long-Acting Insulin + OAD Mean number of confirmed hypoglycemic events per patient-year in a 28 -week study Events per patient-year 6 5 p=0. 0009 5. 73 Premixed insulin 4 Insulin glargine + OADs 3 2 2. 62 p=0. 0449 1 1. 04 0. 51 0 Symptomatic Nocturnal p=0. 0702 0. 05 0. 00 Severe Adapted from Janka et al. Diabetes Care 2005; 28: 254 -9.
Rates of Hypoglycemia for Premixed vs. Long-Acting Insulin + OAD Mean number of confirmed hypoglycemic events per patient-year in a 28 -week study Events per patient-year 6 5 p=0. 0009 5. 73 Premixed insulin 4 Insulin glargine + OADs 3 2 2. 62 p=0. 0449 1 1. 04 0. 51 0 Symptomatic Nocturnal p=0. 0702 0. 05 0. 00 Severe Adapted from Janka et al. Diabetes Care 2005; 28: 254 -9.
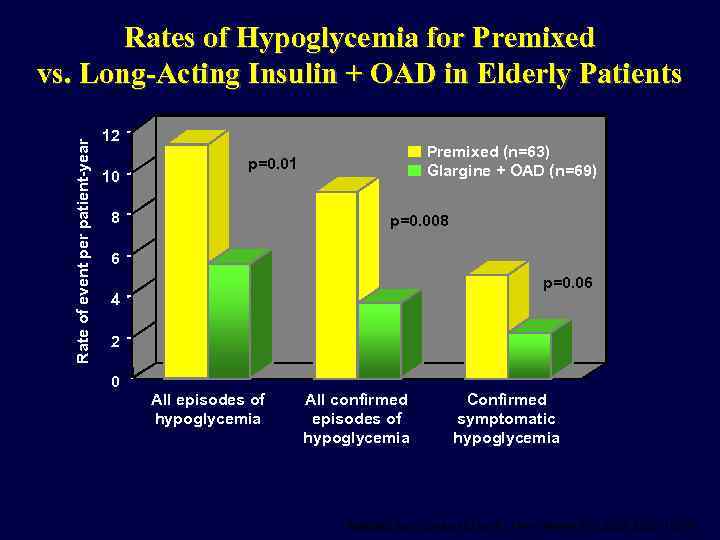 Rate of event per patient-year Rates of Hypoglycemia for Premixed vs. Long-Acting Insulin + OAD in Elderly Patients 12 10 Premixed (n=63) Glargine + OAD (n=69) p=0. 01 8 p=0. 008 6 p=0. 06 4 2 0 All episodes of hypoglycemia All confirmed episodes of hypoglycemia Confirmed symptomatic hypoglycemia Adapted from Janka HU et al. J Am Geriatr Soc 2007; 55(2): 182 -8.
Rate of event per patient-year Rates of Hypoglycemia for Premixed vs. Long-Acting Insulin + OAD in Elderly Patients 12 10 Premixed (n=63) Glargine + OAD (n=69) p=0. 01 8 p=0. 008 6 p=0. 06 4 2 0 All episodes of hypoglycemia All confirmed episodes of hypoglycemia Confirmed symptomatic hypoglycemia Adapted from Janka HU et al. J Am Geriatr Soc 2007; 55(2): 182 -8.
 The ADA Treatment Algorithm for the Initiation and Adjustment of Insulin
The ADA Treatment Algorithm for the Initiation and Adjustment of Insulin
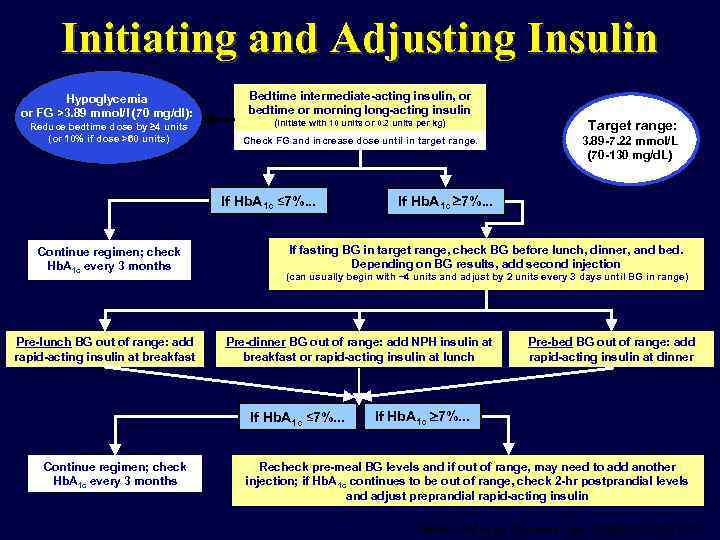 Initiating and Adjusting Insulin Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
Initiating and Adjusting Insulin Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
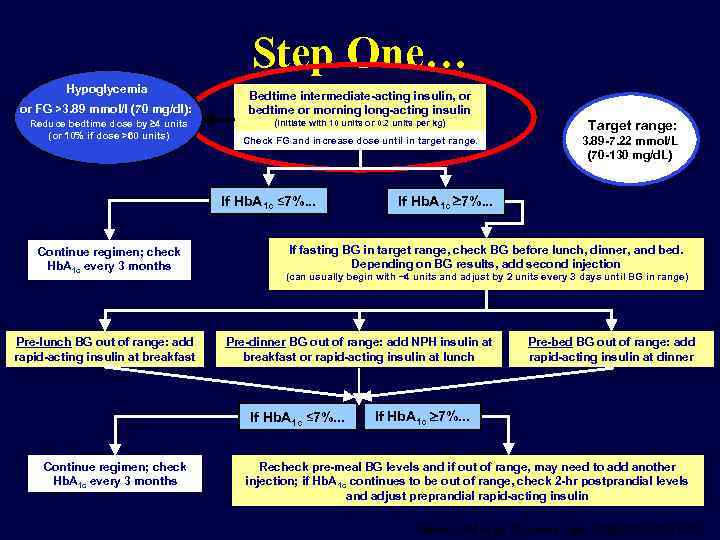 Step One… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin (initiate with 10 units or 0. 2 units per kg) Check FG and increase dose until in target range. If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
Step One… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin (initiate with 10 units or 0. 2 units per kg) Check FG and increase dose until in target range. If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
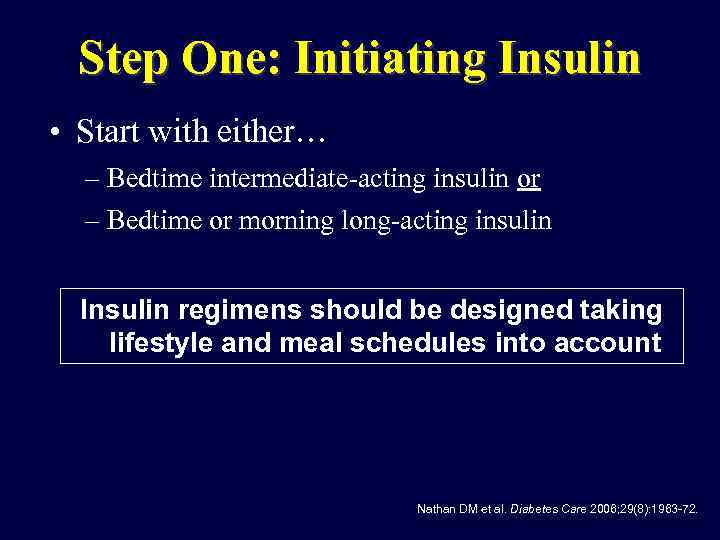 Step One: Initiating Insulin • Start with either… – Bedtime intermediate-acting insulin or – Bedtime or morning long-acting insulin Insulin regimens should be designed taking lifestyle and meal schedules into account Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Step One: Initiating Insulin • Start with either… – Bedtime intermediate-acting insulin or – Bedtime or morning long-acting insulin Insulin regimens should be designed taking lifestyle and meal schedules into account Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
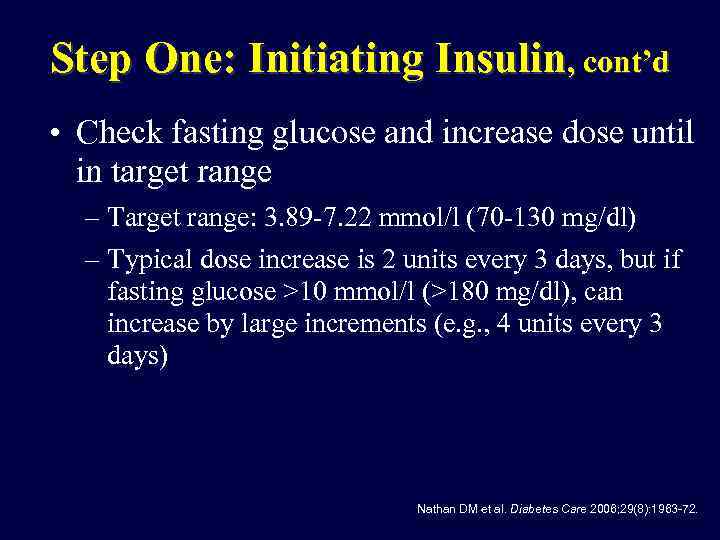 Step One: Initiating Insulin, cont’d • Check fasting glucose and increase dose until in target range – Target range: 3. 89 -7. 22 mmol/l (70 -130 mg/dl) – Typical dose increase is 2 units every 3 days, but if fasting glucose >10 mmol/l (>180 mg/dl), can increase by large increments (e. g. , 4 units every 3 days) Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Step One: Initiating Insulin, cont’d • Check fasting glucose and increase dose until in target range – Target range: 3. 89 -7. 22 mmol/l (70 -130 mg/dl) – Typical dose increase is 2 units every 3 days, but if fasting glucose >10 mmol/l (>180 mg/dl), can increase by large increments (e. g. , 4 units every 3 days) Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
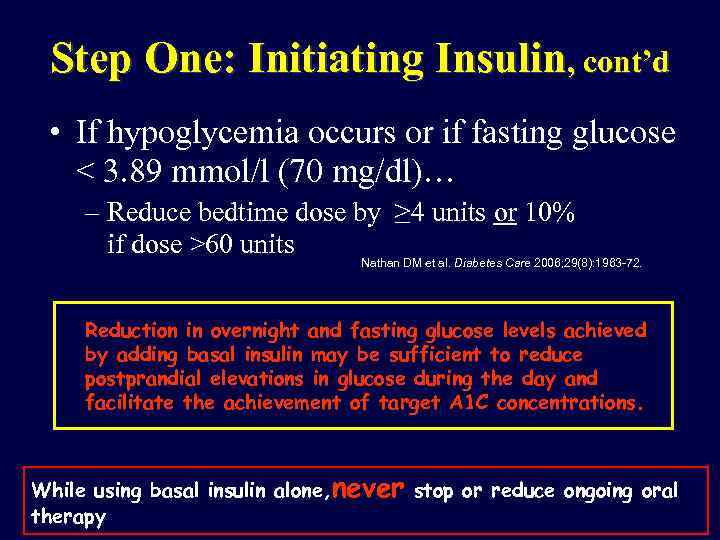 Step One: Initiating Insulin, cont’d • If hypoglycemia occurs or if fasting glucose < 3. 89 mmol/l (70 mg/dl)… – Reduce bedtime dose by ≥ 4 units or 10% if dose >60 units Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72. Reduction in overnight and fasting glucose levels achieved by adding basal insulin may be sufficient to reduce postprandial elevations in glucose during the day and facilitate the achievement of target A 1 C concentrations. While using basal insulin alone, never stop or reduce ongoing oral therapy
Step One: Initiating Insulin, cont’d • If hypoglycemia occurs or if fasting glucose < 3. 89 mmol/l (70 mg/dl)… – Reduce bedtime dose by ≥ 4 units or 10% if dose >60 units Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72. Reduction in overnight and fasting glucose levels achieved by adding basal insulin may be sufficient to reduce postprandial elevations in glucose during the day and facilitate the achievement of target A 1 C concentrations. While using basal insulin alone, never stop or reduce ongoing oral therapy
 After 2 -3 Months… • If Hb. A 1 c is <7%. . . – Continue regimen and check Hb. A 1 c every 3 months • If Hb. A 1 c is ≥ 7%. . . – Move to Step Two… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
After 2 -3 Months… • If Hb. A 1 c is <7%. . . – Continue regimen and check Hb. A 1 c every 3 months • If Hb. A 1 c is ≥ 7%. . . – Move to Step Two… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
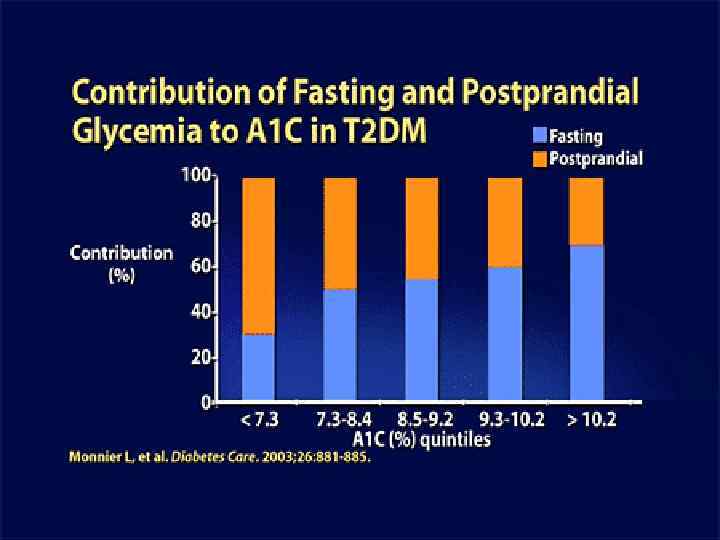
 With the addition of basal insulin and titration to target FBG levels, only about 60% of patients with type 2 diabetes are able to achieve A 1 C goals < 7%. [36] In the remaining patients with A 1 C levels above goal regardless of adequate fasting glucose levels, postprandial blood glucose levels are likely elevated.
With the addition of basal insulin and titration to target FBG levels, only about 60% of patients with type 2 diabetes are able to achieve A 1 C goals < 7%. [36] In the remaining patients with A 1 C levels above goal regardless of adequate fasting glucose levels, postprandial blood glucose levels are likely elevated.
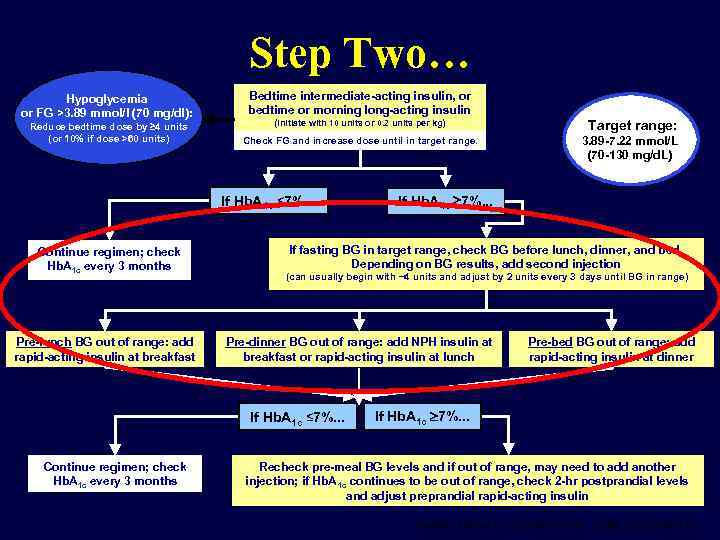 Step Two… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
Step Two… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
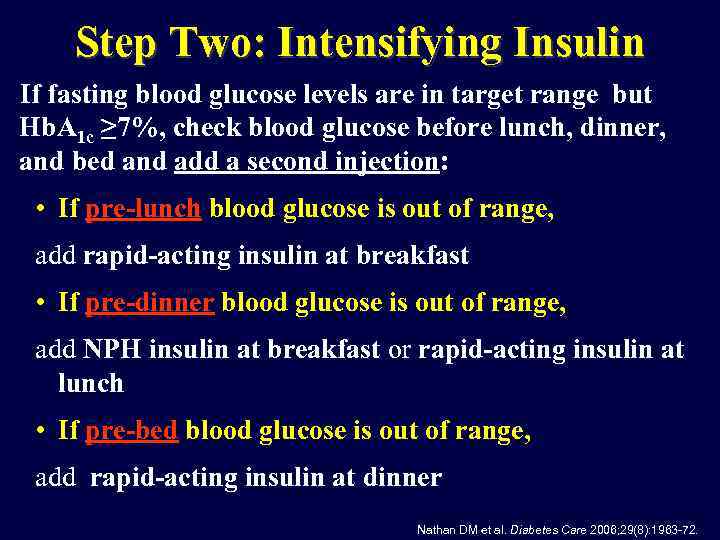 Step Two: Intensifying Insulin If fasting blood glucose levels are in target range but Hb. A 1 c ≥ 7%, check blood glucose before lunch, dinner, and bed and add a second injection: • If pre-lunch blood glucose is out of range, add rapid-acting insulin at breakfast • If pre-dinner blood glucose is out of range, add NPH insulin at breakfast or rapid-acting insulin at lunch • If pre-bed blood glucose is out of range, add rapid-acting insulin at dinner Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Step Two: Intensifying Insulin If fasting blood glucose levels are in target range but Hb. A 1 c ≥ 7%, check blood glucose before lunch, dinner, and bed and add a second injection: • If pre-lunch blood glucose is out of range, add rapid-acting insulin at breakfast • If pre-dinner blood glucose is out of range, add NPH insulin at breakfast or rapid-acting insulin at lunch • If pre-bed blood glucose is out of range, add rapid-acting insulin at dinner Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
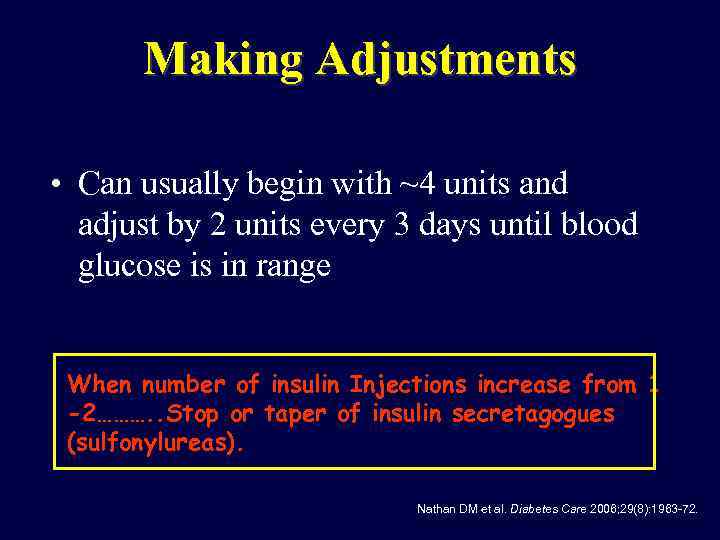 Making Adjustments • Can usually begin with ~4 units and adjust by 2 units every 3 days until blood glucose is in range When number of insulin Injections increase from 1 -2………. . Stop or taper of insulin secretagogues (sulfonylureas). Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Making Adjustments • Can usually begin with ~4 units and adjust by 2 units every 3 days until blood glucose is in range When number of insulin Injections increase from 1 -2………. . Stop or taper of insulin secretagogues (sulfonylureas). Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
 After 2 -3 Months… • If Hb. A 1 c is <7%. . . – Continue regimen and check Hb. A 1 c every 3 months • If Hb. A 1 c is ≥ 7%. . . – Move to Step Three… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
After 2 -3 Months… • If Hb. A 1 c is <7%. . . – Continue regimen and check Hb. A 1 c every 3 months • If Hb. A 1 c is ≥ 7%. . . – Move to Step Three… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
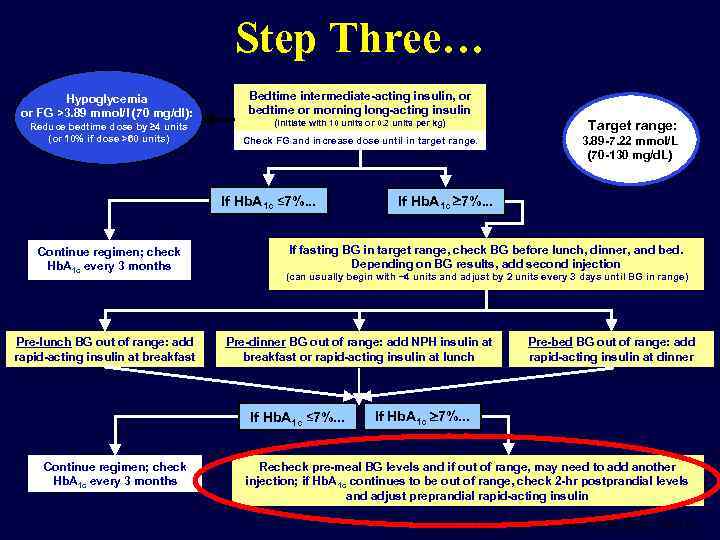 Step Three… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
Step Three… Hypoglycemia or FG >3. 89 mmol/l (70 mg/dl): Bedtime intermediate-acting insulin, or bedtime or morning long-acting insulin Reduce bedtime dose by ≥ 4 units (or 10% if dose >60 units) Check FG and increase dose until in target range. (initiate with 10 units or 0. 2 units per kg) If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Pre-lunch BG out of range: add rapid-acting insulin at breakfast 3. 89 -7. 22 mmol/L (70 -130 mg/d. L) If Hb. A 1 c 7%. . . If fasting BG in target range, check BG before lunch, dinner, and bed. Depending on BG results, add second injection (can usually begin with ~4 units and adjust by 2 units every 3 days until BG in range) Pre-dinner BG out of range: add NPH insulin at breakfast or rapid-acting insulin at lunch If Hb. A 1 c ≤ 7%. . . Continue regimen; check Hb. A 1 c every 3 months Target range: Pre-bed BG out of range: add rapid-acting insulin at dinner If Hb. A 1 c 7%. . . Recheck pre-meal BG levels and if out of range, may need to add another injection; if Hb. A 1 c continues to be out of range, check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care. 2006; 29(8): 1963 -72.
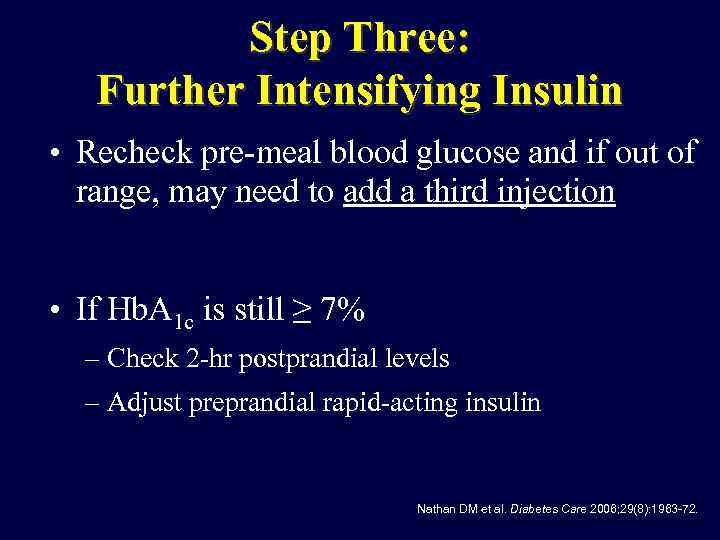 Step Three: Further Intensifying Insulin • Recheck pre-meal blood glucose and if out of range, may need to add a third injection • If Hb. A 1 c is still ≥ 7% – Check 2 -hr postprandial levels – Adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Step Three: Further Intensifying Insulin • Recheck pre-meal blood glucose and if out of range, may need to add a third injection • If Hb. A 1 c is still ≥ 7% – Check 2 -hr postprandial levels – Adjust preprandial rapid-acting insulin Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
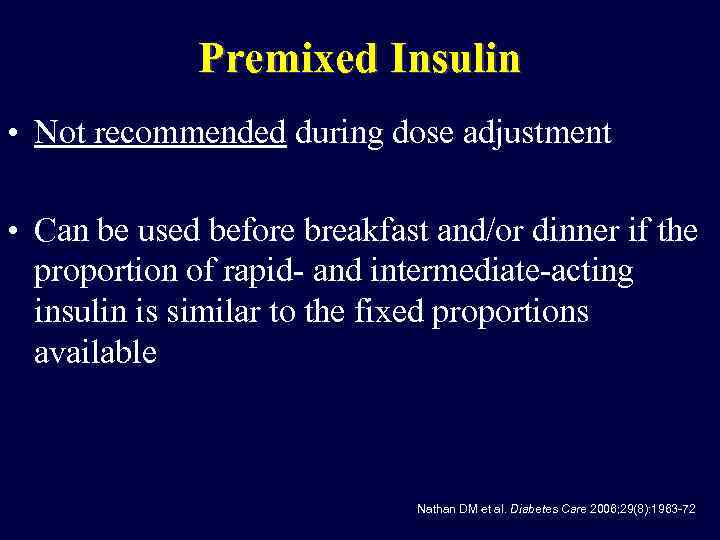 Premixed Insulin • Not recommended during dose adjustment • Can be used before breakfast and/or dinner if the proportion of rapid- and intermediate-acting insulin is similar to the fixed proportions available Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Premixed Insulin • Not recommended during dose adjustment • Can be used before breakfast and/or dinner if the proportion of rapid- and intermediate-acting insulin is similar to the fixed proportions available Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
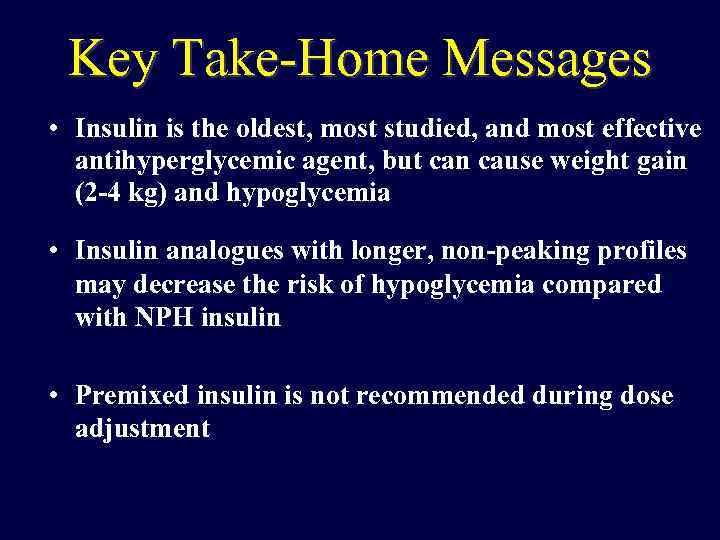 Key Take-Home Messages • Insulin is the oldest, most studied, and most effective antihyperglycemic agent, but can cause weight gain (2 -4 kg) and hypoglycemia • Insulin analogues with longer, non-peaking profiles may decrease the risk of hypoglycemia compared with NPH insulin • Premixed insulin is not recommended during dose adjustment
Key Take-Home Messages • Insulin is the oldest, most studied, and most effective antihyperglycemic agent, but can cause weight gain (2 -4 kg) and hypoglycemia • Insulin analogues with longer, non-peaking profiles may decrease the risk of hypoglycemia compared with NPH insulin • Premixed insulin is not recommended during dose adjustment
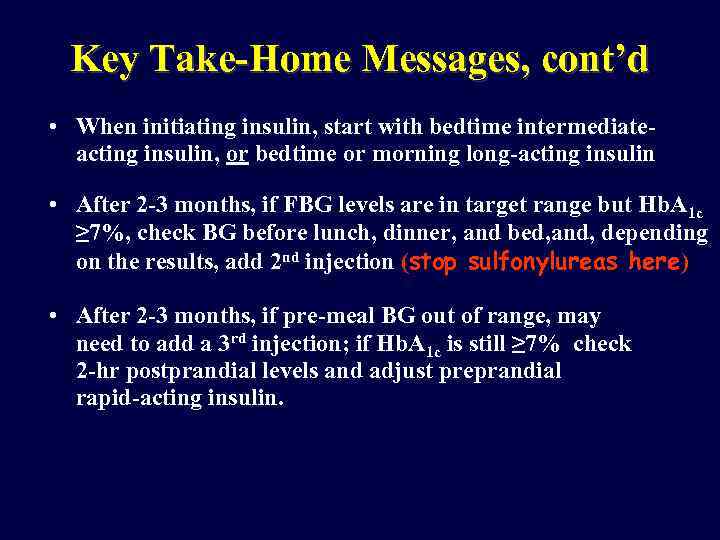 Key Take-Home Messages, cont’d • When initiating insulin, start with bedtime intermediateacting insulin, or bedtime or morning long-acting insulin • After 2 -3 months, if FBG levels are in target range but Hb. A 1 c ≥ 7%, check BG before lunch, dinner, and bed, and, depending on the results, add 2 nd injection (stop sulfonylureas here) • After 2 -3 months, if pre-meal BG out of range, may need to add a 3 rd injection; if Hb. A 1 c is still ≥ 7% check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin.
Key Take-Home Messages, cont’d • When initiating insulin, start with bedtime intermediateacting insulin, or bedtime or morning long-acting insulin • After 2 -3 months, if FBG levels are in target range but Hb. A 1 c ≥ 7%, check BG before lunch, dinner, and bed, and, depending on the results, add 2 nd injection (stop sulfonylureas here) • After 2 -3 months, if pre-meal BG out of range, may need to add a 3 rd injection; if Hb. A 1 c is still ≥ 7% check 2 -hr postprandial levels and adjust preprandial rapid-acting insulin.
 Regimen # 2
Regimen # 2
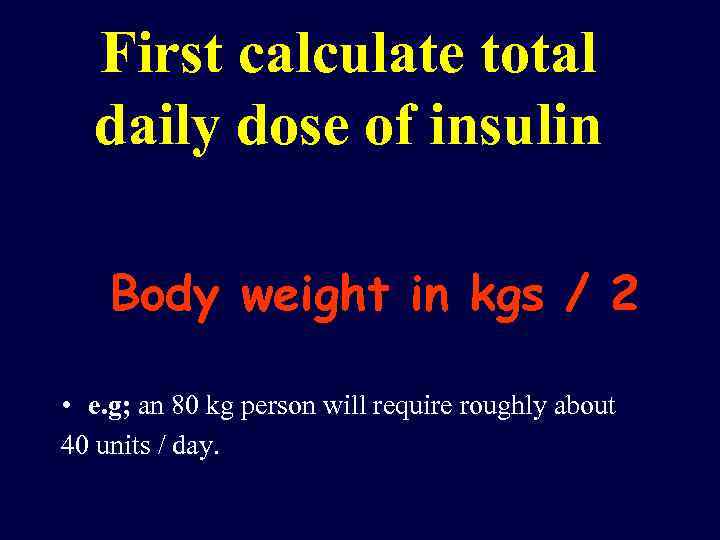 First calculate total daily dose of insulin Body weight in kgs / 2 • e. g; an 80 kg person will require roughly about 40 units / day.
First calculate total daily dose of insulin Body weight in kgs / 2 • e. g; an 80 kg person will require roughly about 40 units / day.
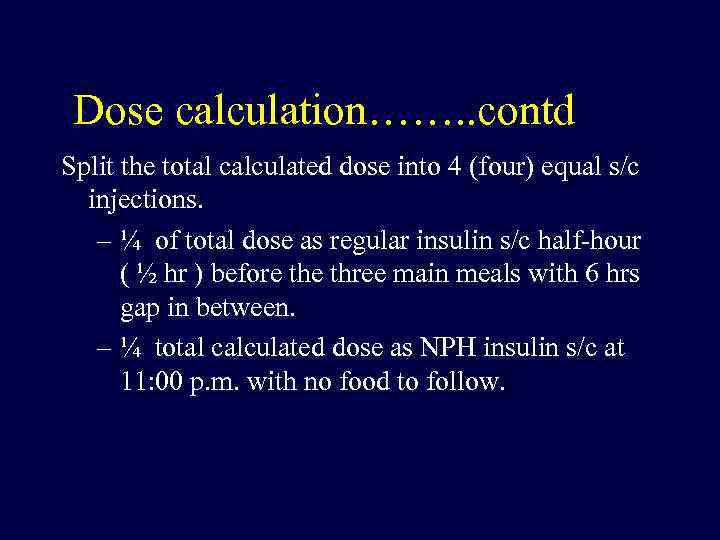 Dose calculation……. . contd Split the total calculated dose into 4 (four) equal s/c injections. – ¼ of total dose as regular insulin s/c half-hour ( ½ hr ) before three main meals with 6 hrs gap in between. – ¼ total calculated dose as NPH insulin s/c at 11: 00 p. m. with no food to follow.
Dose calculation……. . contd Split the total calculated dose into 4 (four) equal s/c injections. – ¼ of total dose as regular insulin s/c half-hour ( ½ hr ) before three main meals with 6 hrs gap in between. – ¼ total calculated dose as NPH insulin s/c at 11: 00 p. m. with no food to follow.
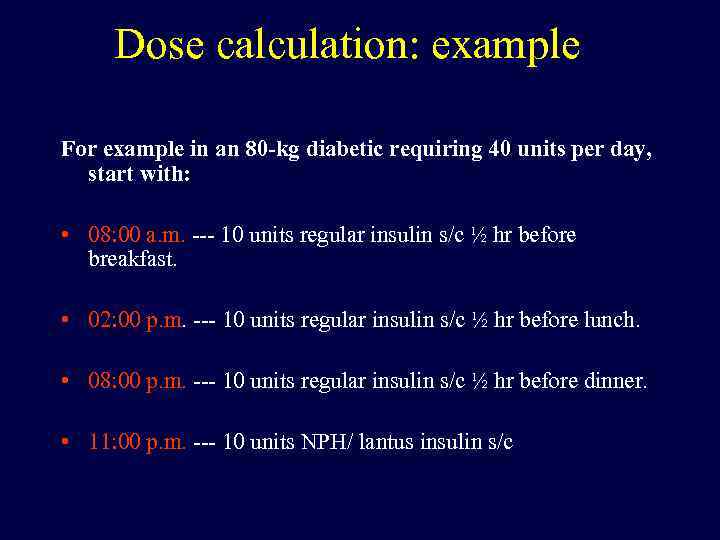 Dose calculation: example For example in an 80 -kg diabetic requiring 40 units per day, start with: • 08: 00 a. m. --- 10 units regular insulin s/c ½ hr before breakfast. • 02: 00 p. m. --- 10 units regular insulin s/c ½ hr before lunch. • 08: 00 p. m. --- 10 units regular insulin s/c ½ hr before dinner. • 11: 00 p. m. --- 10 units NPH/ lantus insulin s/c
Dose calculation: example For example in an 80 -kg diabetic requiring 40 units per day, start with: • 08: 00 a. m. --- 10 units regular insulin s/c ½ hr before breakfast. • 02: 00 p. m. --- 10 units regular insulin s/c ½ hr before lunch. • 08: 00 p. m. --- 10 units regular insulin s/c ½ hr before dinner. • 11: 00 p. m. --- 10 units NPH/ lantus insulin s/c
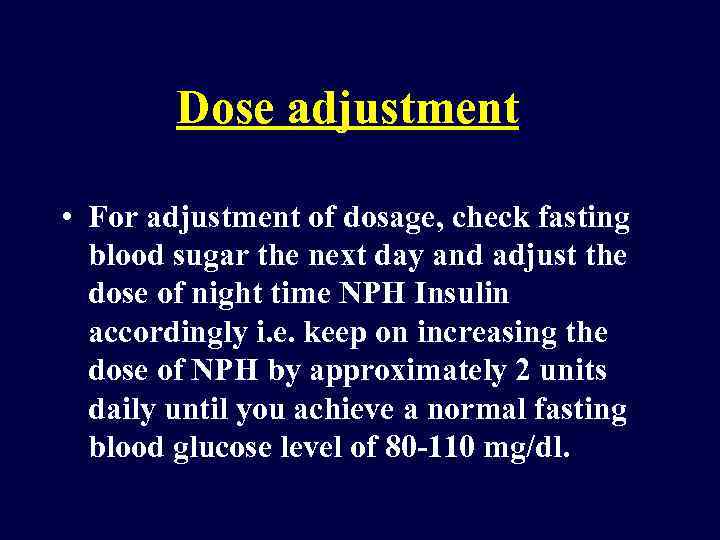 Dose adjustment • For adjustment of dosage, check fasting blood sugar the next day and adjust the dose of night time NPH Insulin accordingly i. e. keep on increasing the dose of NPH by approximately 2 units daily until you achieve a normal fasting blood glucose level of 80 -110 mg/dl.
Dose adjustment • For adjustment of dosage, check fasting blood sugar the next day and adjust the dose of night time NPH Insulin accordingly i. e. keep on increasing the dose of NPH by approximately 2 units daily until you achieve a normal fasting blood glucose level of 80 -110 mg/dl.
 Control BSF by adjusting the prior the dose of NPH
Control BSF by adjusting the prior the dose of NPH
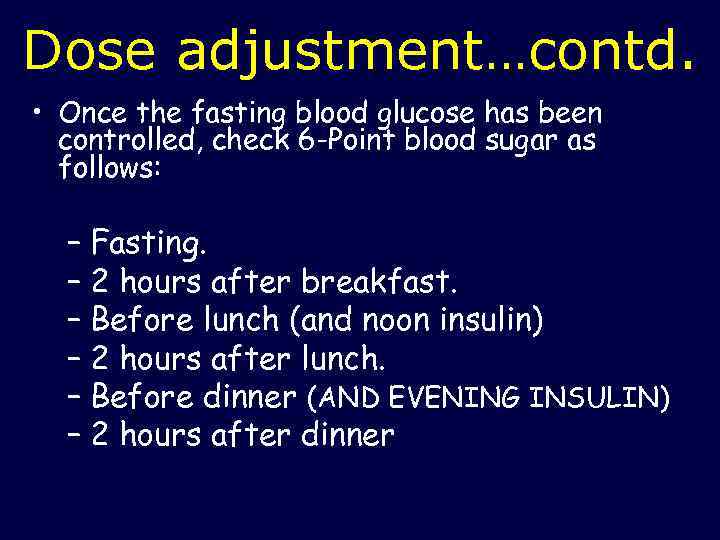 Dose adjustment…contd. • Once the fasting blood glucose has been controlled, check 6 -Point blood sugar as follows: – Fasting. – 2 hours after breakfast. – Before lunch (and noon insulin) – 2 hours after lunch. – Before dinner (AND EVENING INSULIN) – 2 hours after dinner
Dose adjustment…contd. • Once the fasting blood glucose has been controlled, check 6 -Point blood sugar as follows: – Fasting. – 2 hours after breakfast. – Before lunch (and noon insulin) – 2 hours after lunch. – Before dinner (AND EVENING INSULIN) – 2 hours after dinner
 Control random sugar level by adjusting the prior dose of regular insulin
Control random sugar level by adjusting the prior dose of regular insulin
 Dose adjustment…contd. • Now control any raised random reading by adjusting the dose of previously administered regular insulin. • For example: a high post lunch reading will NOT be controlled by increasing the dose of next insulin (as in sliding scale), rather adjustment of the pre-lunch regular insulin on the next day will bring down raised reading to the required levels.
Dose adjustment…contd. • Now control any raised random reading by adjusting the dose of previously administered regular insulin. • For example: a high post lunch reading will NOT be controlled by increasing the dose of next insulin (as in sliding scale), rather adjustment of the pre-lunch regular insulin on the next day will bring down raised reading to the required levels.
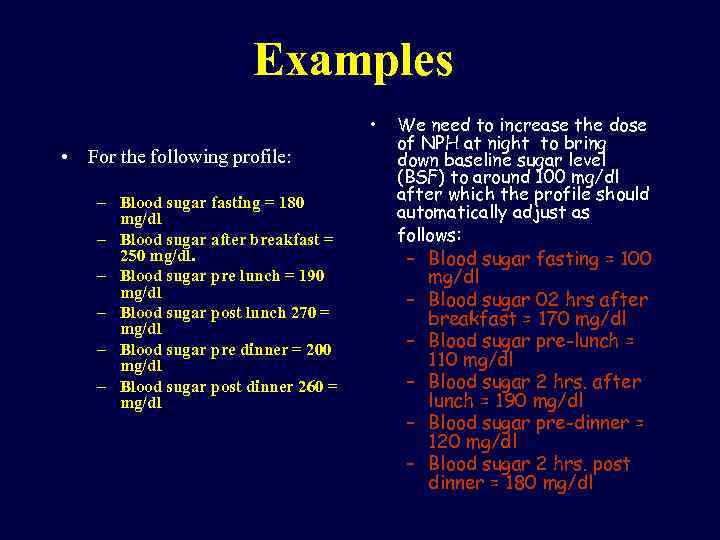 Examples • • For the following profile: – Blood sugar fasting = 180 mg/dl – Blood sugar after breakfast = 250 mg/dl. – Blood sugar pre lunch = 190 mg/dl – Blood sugar post lunch 270 = mg/dl – Blood sugar pre dinner = 200 mg/dl – Blood sugar post dinner 260 = mg/dl We need to increase the dose of NPH at night to bring down baseline sugar level (BSF) to around 100 mg/dl after which the profile should automatically adjust as follows: – Blood sugar fasting = 100 mg/dl – Blood sugar 02 hrs after breakfast = 170 mg/dl – Blood sugar pre-lunch = 110 mg/dl – Blood sugar 2 hrs. after lunch = 190 mg/dl – Blood sugar pre-dinner = 120 mg/dl – Blood sugar 2 hrs. post dinner = 180 mg/dl
Examples • • For the following profile: – Blood sugar fasting = 180 mg/dl – Blood sugar after breakfast = 250 mg/dl. – Blood sugar pre lunch = 190 mg/dl – Blood sugar post lunch 270 = mg/dl – Blood sugar pre dinner = 200 mg/dl – Blood sugar post dinner 260 = mg/dl We need to increase the dose of NPH at night to bring down baseline sugar level (BSF) to around 100 mg/dl after which the profile should automatically adjust as follows: – Blood sugar fasting = 100 mg/dl – Blood sugar 02 hrs after breakfast = 170 mg/dl – Blood sugar pre-lunch = 110 mg/dl – Blood sugar 2 hrs. after lunch = 190 mg/dl – Blood sugar pre-dinner = 120 mg/dl – Blood sugar 2 hrs. post dinner = 180 mg/dl
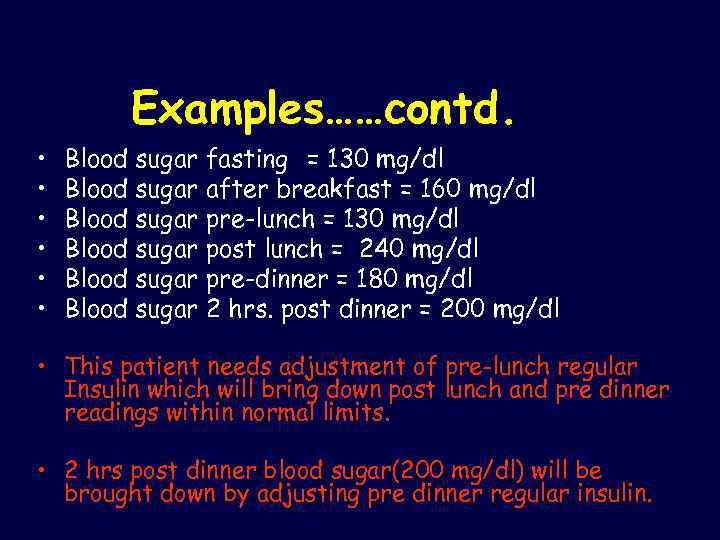 Examples……contd. • • • Blood sugar fasting = 130 mg/dl Blood sugar after breakfast = 160 mg/dl Blood sugar pre-lunch = 130 mg/dl Blood sugar post lunch = 240 mg/dl Blood sugar pre-dinner = 180 mg/dl Blood sugar 2 hrs. post dinner = 200 mg/dl • This patient needs adjustment of pre-lunch regular Insulin which will bring down post lunch and pre dinner readings within normal limits. • 2 hrs post dinner blood sugar(200 mg/dl) will be brought down by adjusting pre dinner regular insulin.
Examples……contd. • • • Blood sugar fasting = 130 mg/dl Blood sugar after breakfast = 160 mg/dl Blood sugar pre-lunch = 130 mg/dl Blood sugar post lunch = 240 mg/dl Blood sugar pre-dinner = 180 mg/dl Blood sugar 2 hrs. post dinner = 200 mg/dl • This patient needs adjustment of pre-lunch regular Insulin which will bring down post lunch and pre dinner readings within normal limits. • 2 hrs post dinner blood sugar(200 mg/dl) will be brought down by adjusting pre dinner regular insulin.
 Combinations • In types 2 subjects, once the blood sugar profile is normalized and the patient is not under any stress, the total daily dose (morning + noon + night + NPH at 11 p. m) may be divided into two 12 hourly injections of premixed Insulin
Combinations • In types 2 subjects, once the blood sugar profile is normalized and the patient is not under any stress, the total daily dose (morning + noon + night + NPH at 11 p. m) may be divided into two 12 hourly injections of premixed Insulin
 Examples…. contd. • e. g-1; If a patient is stabilized on • 10 U R + 12 U R + 10 U R + 12 U NPH; • then he may be shifted to • 44/2 = 22 units of 70/30 Insulin 12 hourly s/c ½ hr before meal. • e. g-2; If the adjusted Insulin is • 14 U R+16 U R+12 U R+8 U NPH, • then split the total dose: 30 U 70/30 before breakfast and 20 U 70/30 before dinner to compensate for the high morning and lunch Insulin.
Examples…. contd. • e. g-1; If a patient is stabilized on • 10 U R + 12 U R + 10 U R + 12 U NPH; • then he may be shifted to • 44/2 = 22 units of 70/30 Insulin 12 hourly s/c ½ hr before meal. • e. g-2; If the adjusted Insulin is • 14 U R+16 U R+12 U R+8 U NPH, • then split the total dose: 30 U 70/30 before breakfast and 20 U 70/30 before dinner to compensate for the high morning and lunch Insulin.
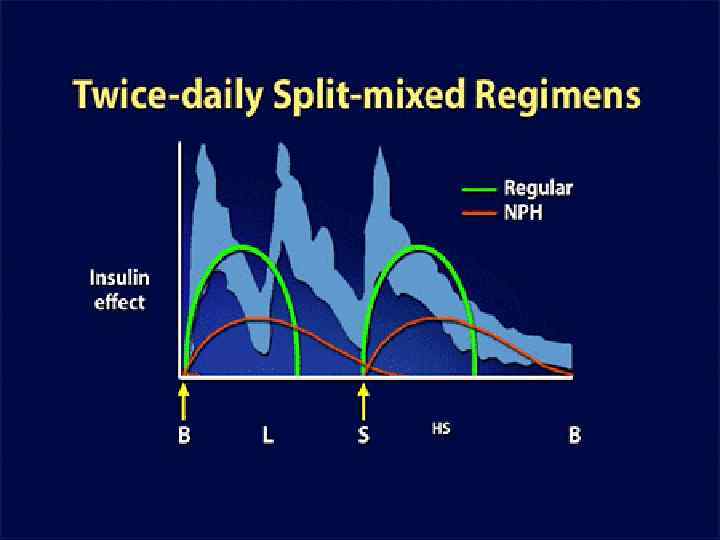
 Combinations………contd. • • • 1. 2. 3. Problem: Remember that BD dosing usually fails to cover lunch, especially if it is heavy. So: Always check for post lunch hyperglycemia when using this regimen. Solution: Patients can be advised to take their lunch (heavier meal) at breakfast; and breakfast (lighter meal) at lunch. Adding Glucobay with lunch some times provides a reasonable control. An alternate combination to overcome the problem is regular insulin for morning and noon, with premixed insulin at night.
Combinations………contd. • • • 1. 2. 3. Problem: Remember that BD dosing usually fails to cover lunch, especially if it is heavy. So: Always check for post lunch hyperglycemia when using this regimen. Solution: Patients can be advised to take their lunch (heavier meal) at breakfast; and breakfast (lighter meal) at lunch. Adding Glucobay with lunch some times provides a reasonable control. An alternate combination to overcome the problem is regular insulin for morning and noon, with premixed insulin at night.
 Example • 10 U R before breakfast + 12 U R before lunch + 22 U 70/30 before dinner. • Insulin will be injected exactly 6 hrs apart as in the QID regimen.
Example • 10 U R before breakfast + 12 U R before lunch + 22 U 70/30 before dinner. • Insulin will be injected exactly 6 hrs apart as in the QID regimen.
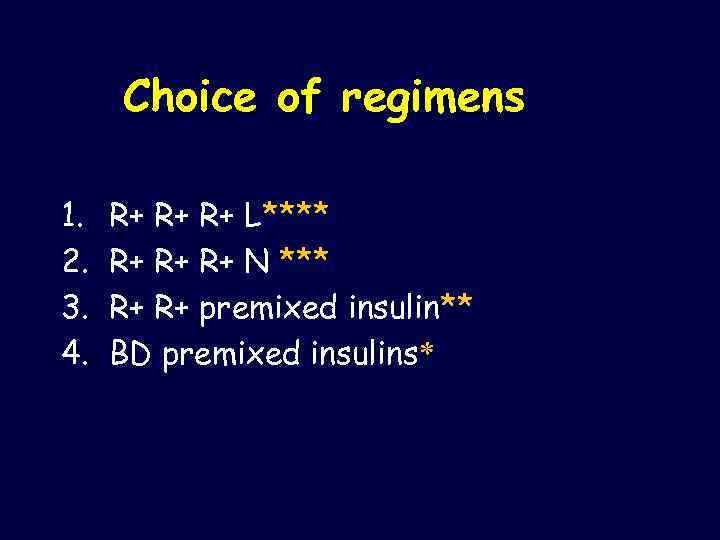 Choice of regimens 1. 2. 3. 4. R+ R+ R+ L**** R+ R+ R+ N *** R+ R+ premixed insulin** BD premixed insulins*
Choice of regimens 1. 2. 3. 4. R+ R+ R+ L**** R+ R+ R+ N *** R+ R+ premixed insulin** BD premixed insulins*
 Regimen # 3 (Pre mixed)
Regimen # 3 (Pre mixed)
 How to start pre mixed (70/30) Insulin
How to start pre mixed (70/30) Insulin
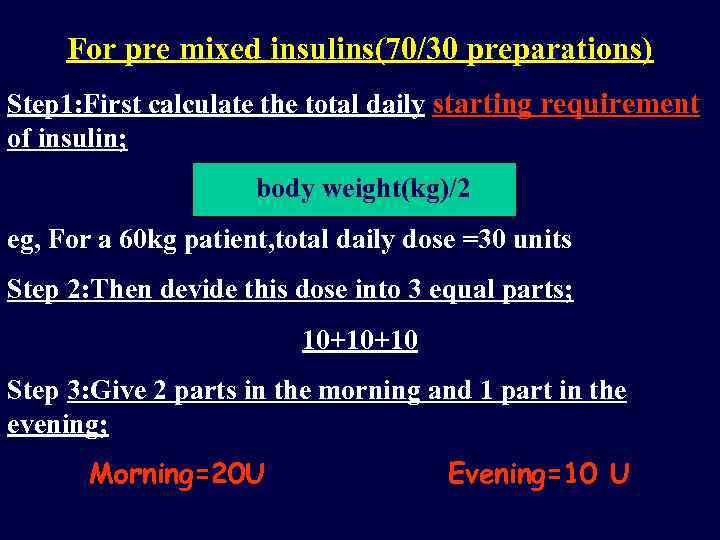 For pre mixed insulins(70/30 preparations) Step 1: First calculate the total daily starting requirement of insulin; body weight(kg)/2 eg, For a 60 kg patient, total daily dose =30 units Step 2: Then devide this dose into 3 equal parts; 10+10+10 Step 3: Give 2 parts in the morning and 1 part in the evening; Morning=20 U Evening=10 U
For pre mixed insulins(70/30 preparations) Step 1: First calculate the total daily starting requirement of insulin; body weight(kg)/2 eg, For a 60 kg patient, total daily dose =30 units Step 2: Then devide this dose into 3 equal parts; 10+10+10 Step 3: Give 2 parts in the morning and 1 part in the evening; Morning=20 U Evening=10 U
 Dose titration of Pre-mixed(70/30) preparations
Dose titration of Pre-mixed(70/30) preparations
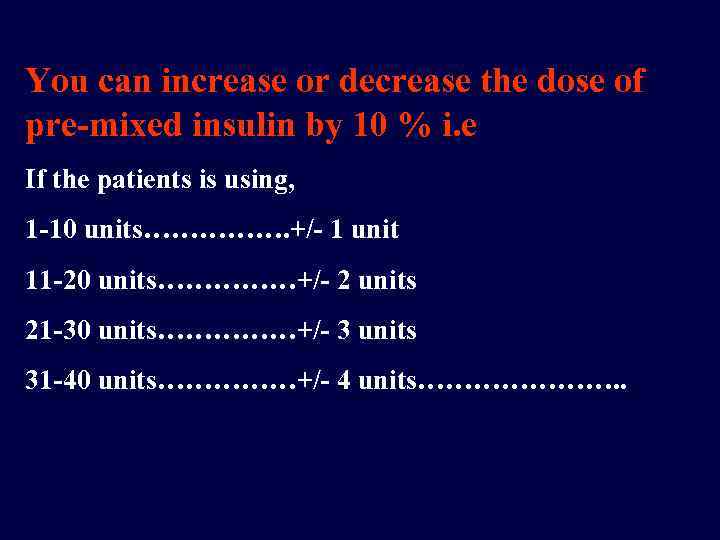 You can increase or decrease the dose of pre-mixed insulin by 10 % i. e If the patients is using, 1 -10 units……………. +/- 1 unit 11 -20 units……………+/- 2 units 21 -30 units……………+/- 3 units 31 -40 units……………+/- 4 units…………………. .
You can increase or decrease the dose of pre-mixed insulin by 10 % i. e If the patients is using, 1 -10 units……………. +/- 1 unit 11 -20 units……………+/- 2 units 21 -30 units……………+/- 3 units 31 -40 units……………+/- 4 units…………………. .
 Advantages and disadvantages of pre- mixed insulins
Advantages and disadvantages of pre- mixed insulins
 Advantages: Easy to administer for the physician. Easy to fill and inject by the patient. Provides both basal and bolus coverage with fewer number of injections.
Advantages: Easy to administer for the physician. Easy to fill and inject by the patient. Provides both basal and bolus coverage with fewer number of injections.
 Disadvantage: No dose flexability If u increase/decrease the dose of one component , the dose of other component is also changed un desirably
Disadvantage: No dose flexability If u increase/decrease the dose of one component , the dose of other component is also changed un desirably
 How to solve the problem of dosage flexibility
How to solve the problem of dosage flexibility
 Regimen # 4
Regimen # 4
 Disadvantage of split- mixed regimen Mid-night hypoglycemia
Disadvantage of split- mixed regimen Mid-night hypoglycemia
 How to solve the problem of nocturnal hypoglycemia
How to solve the problem of nocturnal hypoglycemia
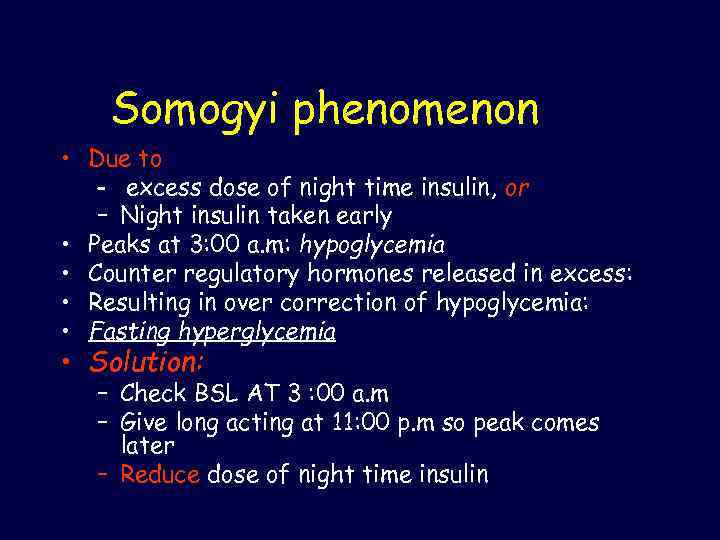 Somogyi phenomenon • Due to – excess dose of night time insulin, or – Night insulin taken early • Peaks at 3: 00 a. m: hypoglycemia • Counter regulatory hormones released in excess: • Resulting in over correction of hypoglycemia: • Fasting hyperglycemia • Solution: – Check BSL AT 3 : 00 a. m – Give long acting at 11: 00 p. m so peak comes later – Reduce dose of night time insulin
Somogyi phenomenon • Due to – excess dose of night time insulin, or – Night insulin taken early • Peaks at 3: 00 a. m: hypoglycemia • Counter regulatory hormones released in excess: • Resulting in over correction of hypoglycemia: • Fasting hyperglycemia • Solution: – Check BSL AT 3 : 00 a. m – Give long acting at 11: 00 p. m so peak comes later – Reduce dose of night time insulin
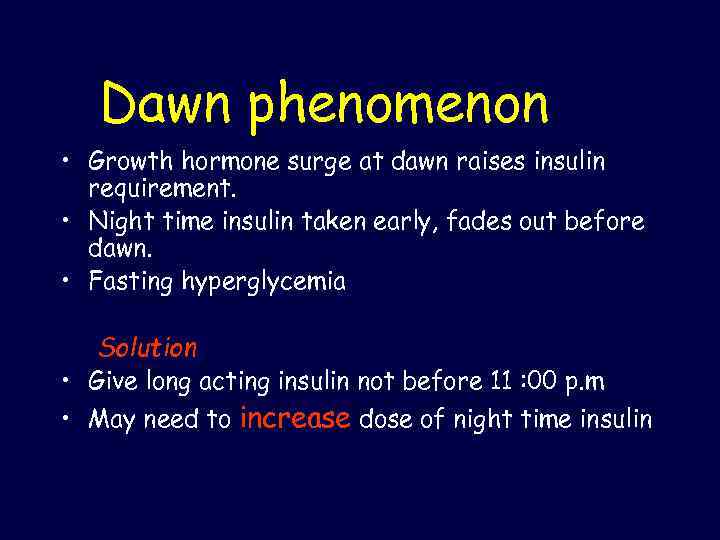 Dawn phenomenon • Growth hormone surge at dawn raises insulin requirement. • Night time insulin taken early, fades out before dawn. • Fasting hyperglycemia Solution • Give long acting insulin not before 11 : 00 p. m • May need to increase dose of night time insulin
Dawn phenomenon • Growth hormone surge at dawn raises insulin requirement. • Night time insulin taken early, fades out before dawn. • Fasting hyperglycemia Solution • Give long acting insulin not before 11 : 00 p. m • May need to increase dose of night time insulin
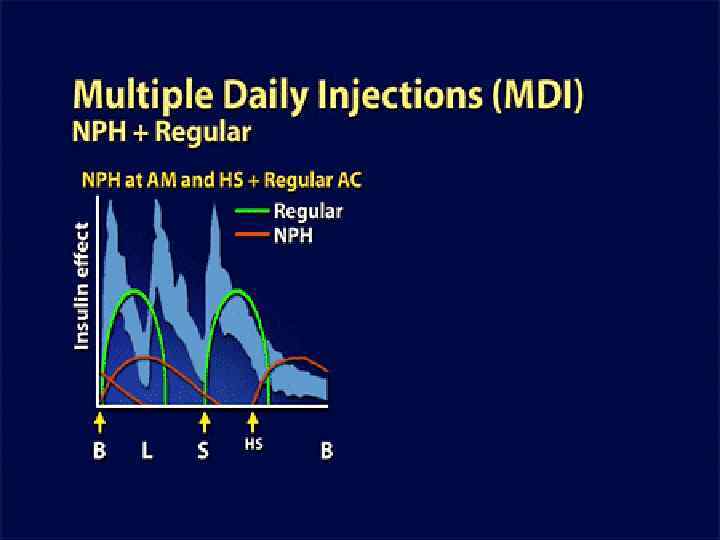
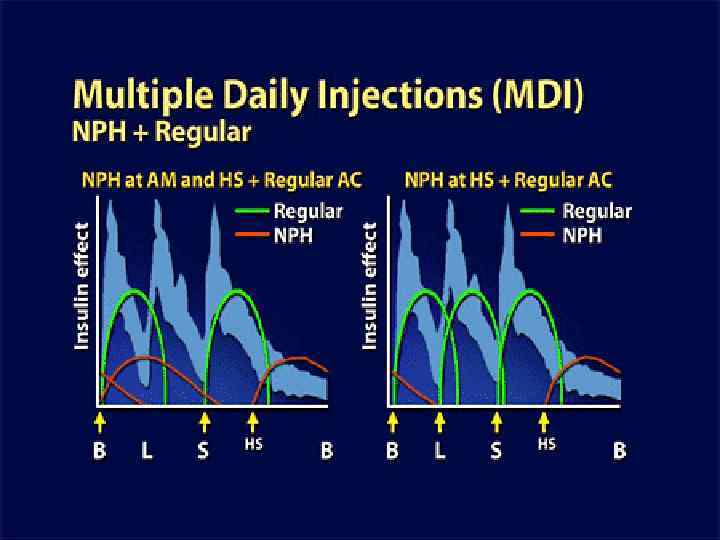
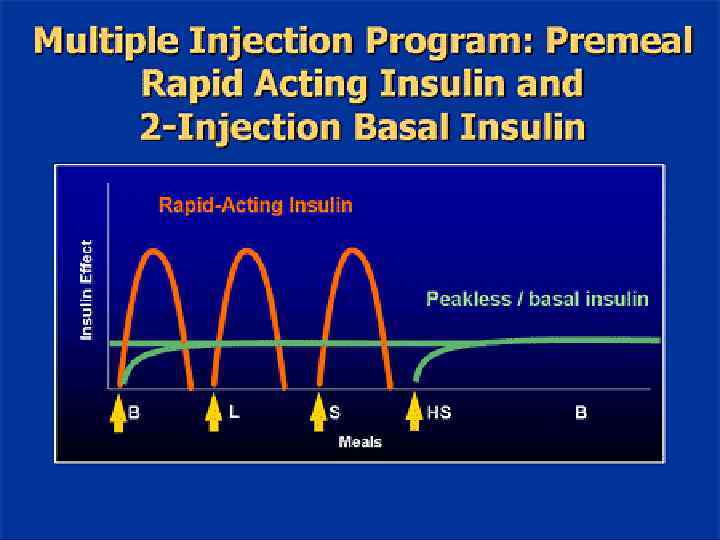
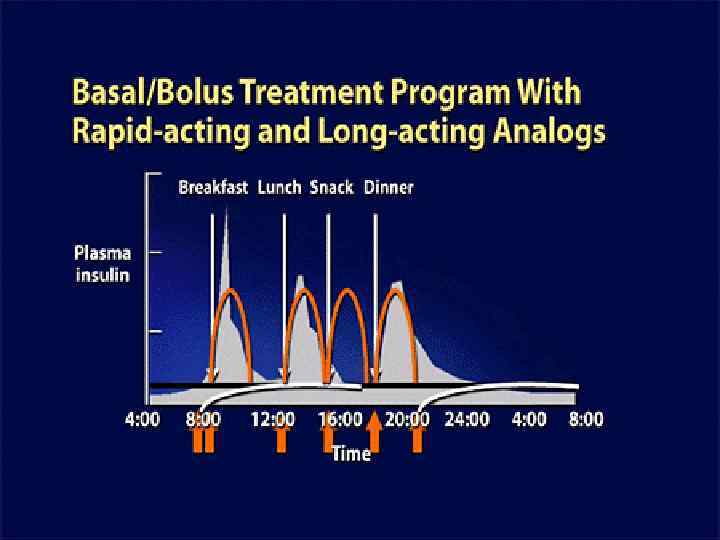
 More physiologic regimens
More physiologic regimens
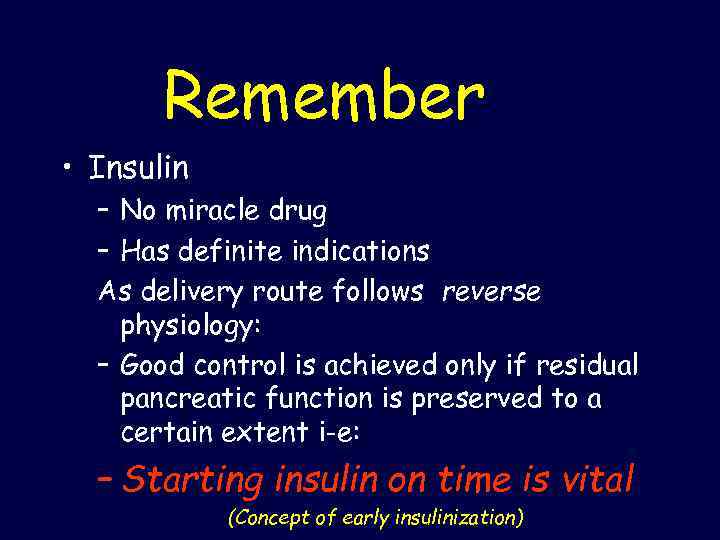 Remember • Insulin – No miracle drug – Has definite indications As delivery route follows reverse physiology: – Good control is achieved only if residual pancreatic function is preserved to a certain extent i-e: – Starting insulin on time is vital (Concept of early insulinization)
Remember • Insulin – No miracle drug – Has definite indications As delivery route follows reverse physiology: – Good control is achieved only if residual pancreatic function is preserved to a certain extent i-e: – Starting insulin on time is vital (Concept of early insulinization)
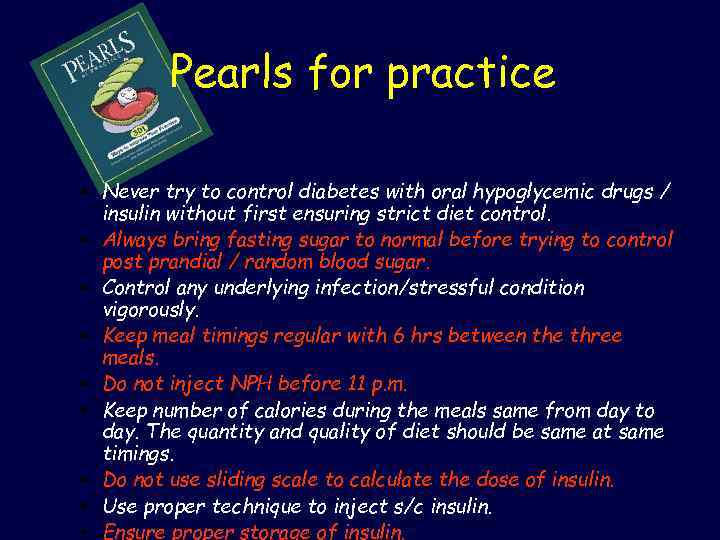 Pearls for practice § Never try to control diabetes with oral hypoglycemic drugs / insulin without first ensuring strict diet control. § Always bring fasting sugar to normal before trying to control post prandial / random blood sugar. § Control any underlying infection/stressful condition vigorously. § Keep meal timings regular with 6 hrs between the three meals. § Do not inject NPH before 11 p. m. § Keep number of calories during the meals same from day to day. The quantity and quality of diet should be same at same timings. § Do not use sliding scale to calculate the dose of insulin. § Use proper technique to inject s/c insulin. § Ensure proper storage of insulin.
Pearls for practice § Never try to control diabetes with oral hypoglycemic drugs / insulin without first ensuring strict diet control. § Always bring fasting sugar to normal before trying to control post prandial / random blood sugar. § Control any underlying infection/stressful condition vigorously. § Keep meal timings regular with 6 hrs between the three meals. § Do not inject NPH before 11 p. m. § Keep number of calories during the meals same from day to day. The quantity and quality of diet should be same at same timings. § Do not use sliding scale to calculate the dose of insulin. § Use proper technique to inject s/c insulin. § Ensure proper storage of insulin.
 Common Problems
Common Problems
 Problems can be avoided • Adherence to time table is all that is required to avoid problems: – Regular meals – Regular injections – Regular excercise
Problems can be avoided • Adherence to time table is all that is required to avoid problems: – Regular meals – Regular injections – Regular excercise
 Choosing an Insulin with a Lower Risk of Hypoglycemia • Insulin analogues with longer, non-peaking profiles may decrease the risk of hypoglycemia… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
Choosing an Insulin with a Lower Risk of Hypoglycemia • Insulin analogues with longer, non-peaking profiles may decrease the risk of hypoglycemia… Nathan DM et al. Diabetes Care 2006; 29(8): 1963 -72.
 Injection Techniques
Injection Techniques
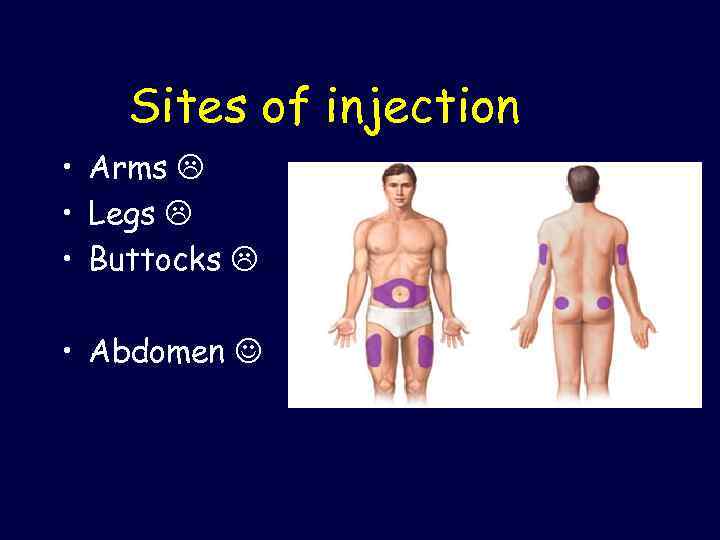 Sites of injection • Arms • Legs • Buttocks • Abdomen
Sites of injection • Arms • Legs • Buttocks • Abdomen
 Sites of injection……. contd. • Preferred site of injection is the abdominal wall due to • Easy access – Ample subcutaneous tissue • Absorption is not affected by exercise.
Sites of injection……. contd. • Preferred site of injection is the abdominal wall due to • Easy access – Ample subcutaneous tissue • Absorption is not affected by exercise.
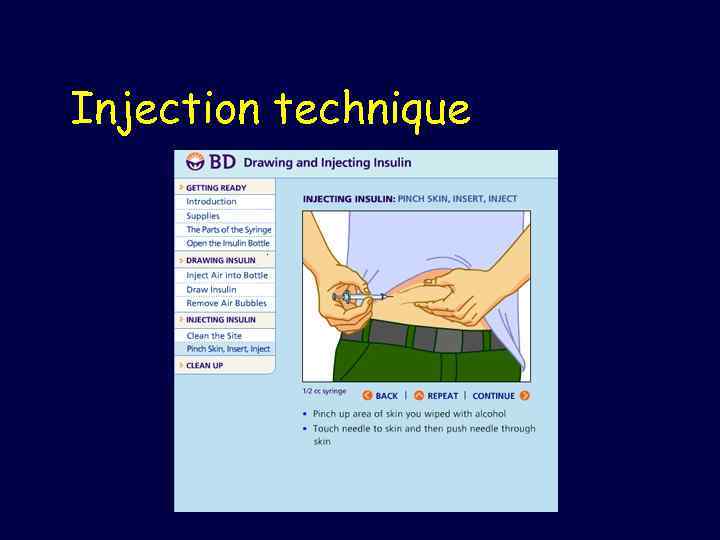 Injection technique
Injection technique
 Technique • • • Tight skin fold Spirit…. X Appropriate needle size 90 degree angle Change site to avoid lipodystrophy
Technique • • • Tight skin fold Spirit…. X Appropriate needle size 90 degree angle Change site to avoid lipodystrophy
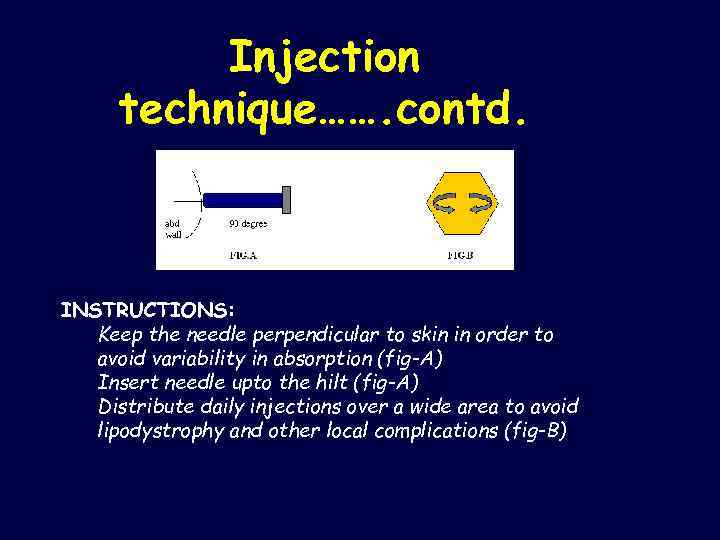 Injection technique……. contd. INSTRUCTIONS: Keep the needle perpendicular to skin in order to avoid variability in absorption (fig-A) Insert needle upto the hilt (fig-A) Distribute daily injections over a wide area to avoid lipodystrophy and other local complications (fig-B)
Injection technique……. contd. INSTRUCTIONS: Keep the needle perpendicular to skin in order to avoid variability in absorption (fig-A) Insert needle upto the hilt (fig-A) Distribute daily injections over a wide area to avoid lipodystrophy and other local complications (fig-B)
 Storage • Injections: refrigerate • Pens: do not refrigerate
Storage • Injections: refrigerate • Pens: do not refrigerate
 Shelf life • One month once opened
Shelf life • One month once opened
 Thank you all For Sparing your valuable time & Patient listening
Thank you all For Sparing your valuable time & Patient listening


