1bf7b8900aee4f94a0ad8dad5affde67.ppt
- Количество слайдов: 51
 Financing Health Care and Economic Issues
Financing Health Care and Economic Issues
 Overview and Objectives • 7 weeks of GH 511 – Where are we now? • A message on health systems strengthening… • History of health policy, economic policies, and aid for health • Elements of health care reform • 3 health financing functions with specific focus on revenue collection • Share your perspectives and experiences
Overview and Objectives • 7 weeks of GH 511 – Where are we now? • A message on health systems strengthening… • History of health policy, economic policies, and aid for health • Elements of health care reform • 3 health financing functions with specific focus on revenue collection • Share your perspectives and experiences
 Your Experiences with Health Care Reform and Financing • What different types are used in the countries where you have been? • How have they worked? • Challenges with implementation? Need MONEY and PEOPLE who know how to LEAD and MANAAGE
Your Experiences with Health Care Reform and Financing • What different types are used in the countries where you have been? • How have they worked? • Challenges with implementation? Need MONEY and PEOPLE who know how to LEAD and MANAAGE
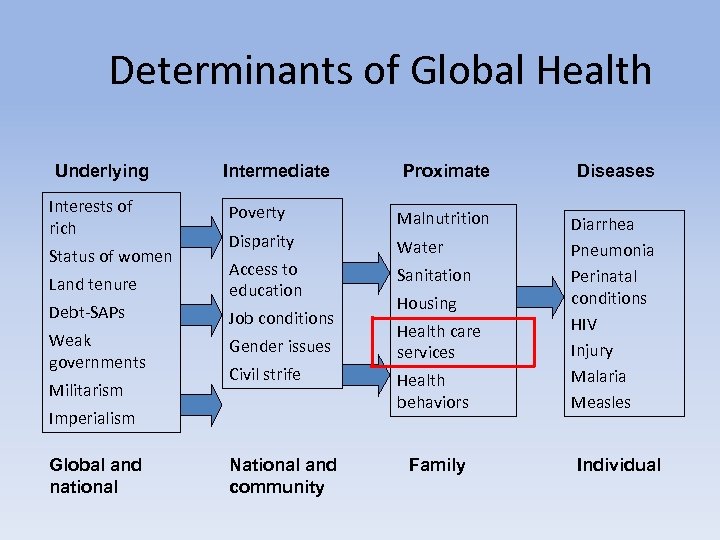 Determinants of Global Health Underlying Proximate Diseases Poverty Malnutrition Disparity Water Land tenure Access to education Sanitation Debt-SAPs Job conditions Weak governments Gender issues Diarrhea Pneumonia Perinatal conditions HIV Injury Malaria Measles Interests of rich Status of women Militarism Intermediate Civil strife Imperialism Global and national National and community Housing Health care services Health behaviors Family Individual
Determinants of Global Health Underlying Proximate Diseases Poverty Malnutrition Disparity Water Land tenure Access to education Sanitation Debt-SAPs Job conditions Weak governments Gender issues Diarrhea Pneumonia Perinatal conditions HIV Injury Malaria Measles Interests of rich Status of women Militarism Intermediate Civil strife Imperialism Global and national National and community Housing Health care services Health behaviors Family Individual
 Health Care Systems • Complex systems consisting of: – Health care consumers = people in need of health care services – Health care providers = people who deliver health care – Systematic arrangements for delivering health care = public and private agencies that organize, plan, regulate, finance, coordinate services Health care can be “catastrophically costly” and need can be unpredictable
Health Care Systems • Complex systems consisting of: – Health care consumers = people in need of health care services – Health care providers = people who deliver health care – Systematic arrangements for delivering health care = public and private agencies that organize, plan, regulate, finance, coordinate services Health care can be “catastrophically costly” and need can be unpredictable
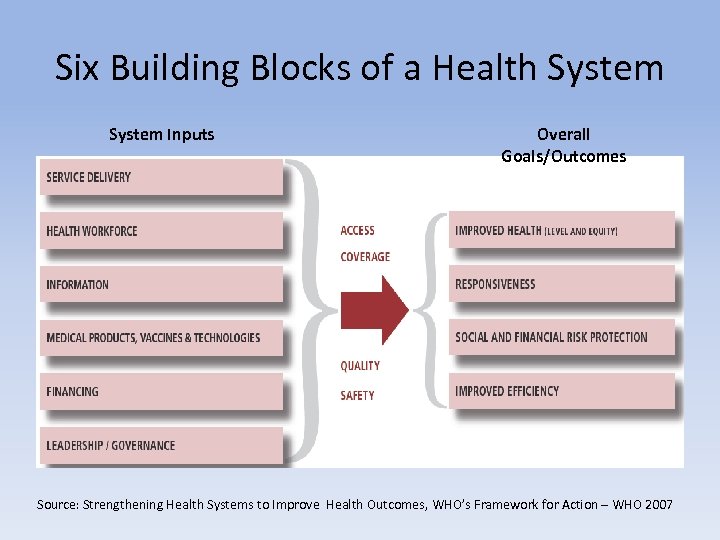 Six Building Blocks of a Health System Inputs Overall Goals/Outcomes Source: Strengthening Health Systems to Improve Health Outcomes, WHO’s Framework for Action – WHO 2007
Six Building Blocks of a Health System Inputs Overall Goals/Outcomes Source: Strengthening Health Systems to Improve Health Outcomes, WHO’s Framework for Action – WHO 2007
 5 Fundamental Questions 1. What are the boundaries of health systems? 2. What are health systems for? 3. How do we characterize the architecture of a health system? 4. How can we tell when a health system is performing well? 5. How do we relate architecture to health system performance?
5 Fundamental Questions 1. What are the boundaries of health systems? 2. What are health systems for? 3. How do we characterize the architecture of a health system? 4. How can we tell when a health system is performing well? 5. How do we relate architecture to health system performance?
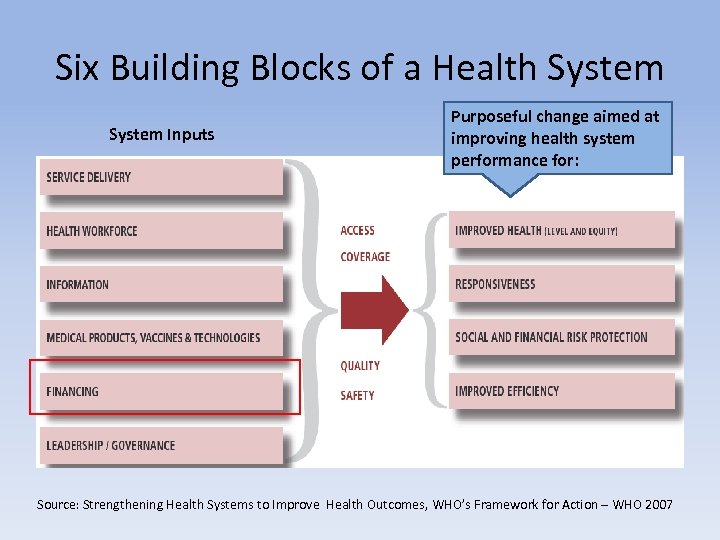 Six Building Blocks of a Health System Inputs Purposeful change aimed at improving health system performance for: Source: Strengthening Health Systems to Improve Health Outcomes, WHO’s Framework for Action – WHO 2007
Six Building Blocks of a Health System Inputs Purposeful change aimed at improving health system performance for: Source: Strengthening Health Systems to Improve Health Outcomes, WHO’s Framework for Action – WHO 2007
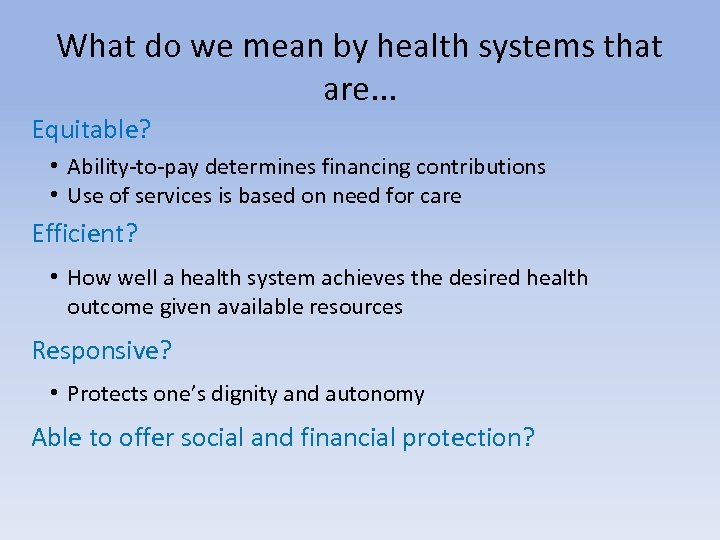 What do we mean by health systems that are. . . Equitable? • Ability-to-pay determines financing contributions • Use of services is based on need for care Efficient? • How well a health system achieves the desired health outcome given available resources Responsive? • Protects one’s dignity and autonomy Able to offer social and financial protection?
What do we mean by health systems that are. . . Equitable? • Ability-to-pay determines financing contributions • Use of services is based on need for care Efficient? • How well a health system achieves the desired health outcome given available resources Responsive? • Protects one’s dignity and autonomy Able to offer social and financial protection?
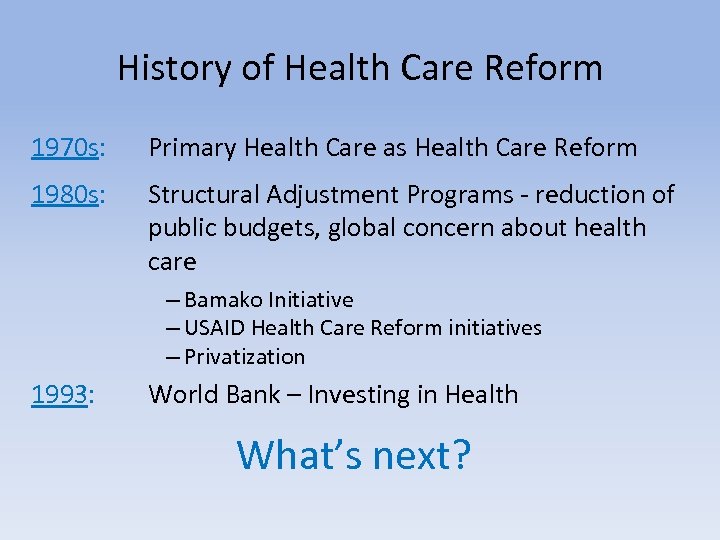 History of Health Care Reform 1970 s: Primary Health Care as Health Care Reform 1980 s: Structural Adjustment Programs - reduction of public budgets, global concern about health care – Bamako Initiative – USAID Health Care Reform initiatives – Privatization 1993: World Bank – Investing in Health What’s next?
History of Health Care Reform 1970 s: Primary Health Care as Health Care Reform 1980 s: Structural Adjustment Programs - reduction of public budgets, global concern about health care – Bamako Initiative – USAID Health Care Reform initiatives – Privatization 1993: World Bank – Investing in Health What’s next?
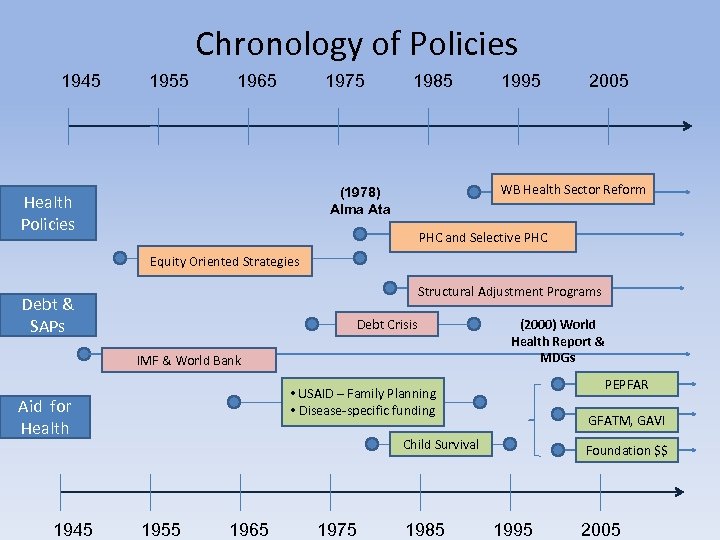 Chronology of Policies 1945 1955 1965 1975 1985 2005 WB Health Sector Reform (1978) Alma Ata Health Policies 1995 PHC and Selective PHC Equity Oriented Strategies Structural Adjustment Programs Debt & SAPs Debt Crisis IMF & World Bank PEPFAR • USAID – Family Planning • Disease-specific funding Aid for Health 1945 (2000) World Health Report & MDGs GFATM, GAVI Child Survival 1955 1965 1975 1985 Foundation $$ 1995 2005
Chronology of Policies 1945 1955 1965 1975 1985 2005 WB Health Sector Reform (1978) Alma Ata Health Policies 1995 PHC and Selective PHC Equity Oriented Strategies Structural Adjustment Programs Debt & SAPs Debt Crisis IMF & World Bank PEPFAR • USAID – Family Planning • Disease-specific funding Aid for Health 1945 (2000) World Health Report & MDGs GFATM, GAVI Child Survival 1955 1965 1975 1985 Foundation $$ 1995 2005
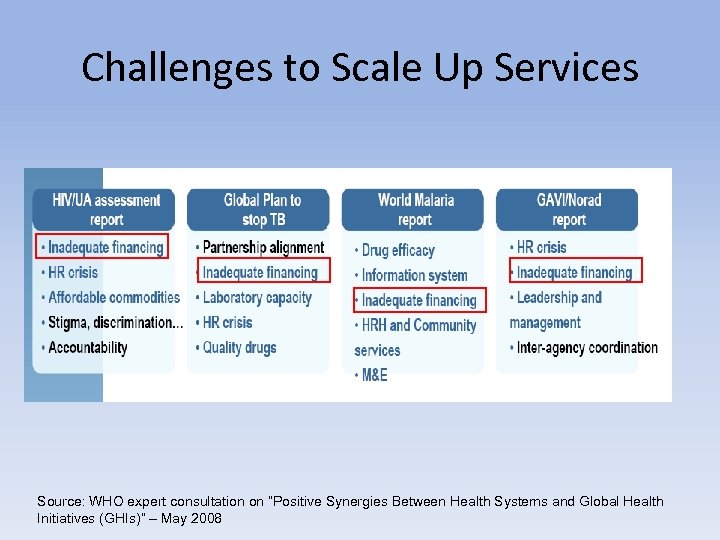 Challenges to Scale Up Services Source: WHO expert consultation on “Positive Synergies Between Health Systems and Global Health Initiatives (GHIs)” – May 2008
Challenges to Scale Up Services Source: WHO expert consultation on “Positive Synergies Between Health Systems and Global Health Initiatives (GHIs)” – May 2008
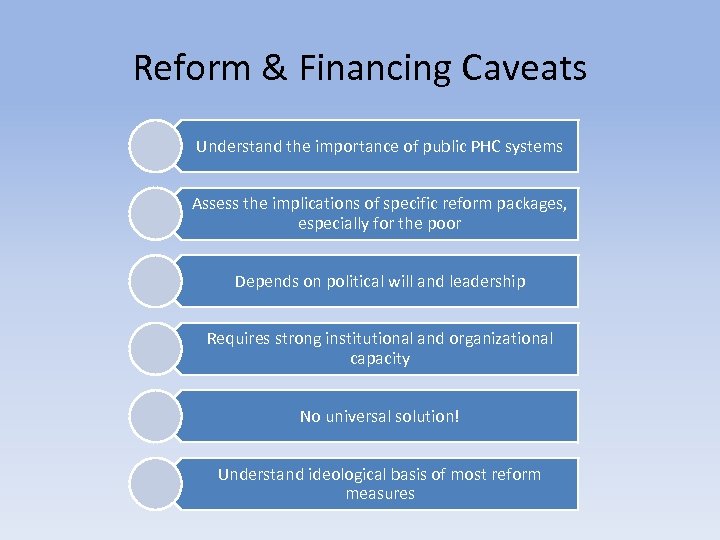 Reform & Financing Caveats Understand the importance of public PHC systems Assess the implications of specific reform packages, especially for the poor Depends on political will and leadership Requires strong institutional and organizational capacity No universal solution! Understand ideological basis of most reform measures
Reform & Financing Caveats Understand the importance of public PHC systems Assess the implications of specific reform packages, especially for the poor Depends on political will and leadership Requires strong institutional and organizational capacity No universal solution! Understand ideological basis of most reform measures
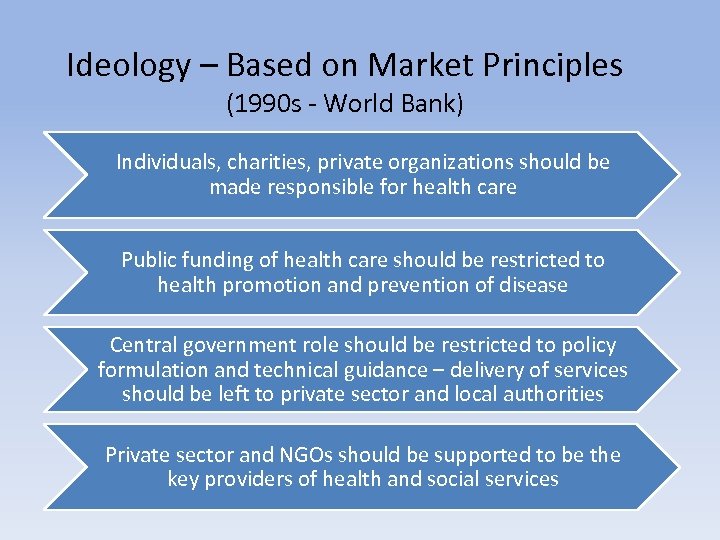 Ideology – Based on Market Principles (1990 s - World Bank) Individuals, charities, private organizations should be made responsible for health care Public funding of health care should be restricted to health promotion and prevention of disease Central government role should be restricted to policy formulation and technical guidance – delivery of services should be left to private sector and local authorities Private sector and NGOs should be supported to be the key providers of health and social services
Ideology – Based on Market Principles (1990 s - World Bank) Individuals, charities, private organizations should be made responsible for health care Public funding of health care should be restricted to health promotion and prevention of disease Central government role should be restricted to policy formulation and technical guidance – delivery of services should be left to private sector and local authorities Private sector and NGOs should be supported to be the key providers of health and social services
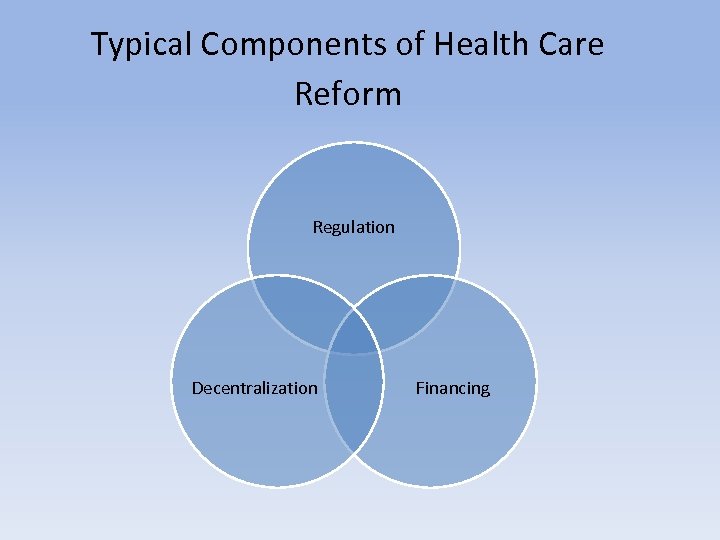 Typical Components of Health Care Reform Regulation Decentralization Financing
Typical Components of Health Care Reform Regulation Decentralization Financing
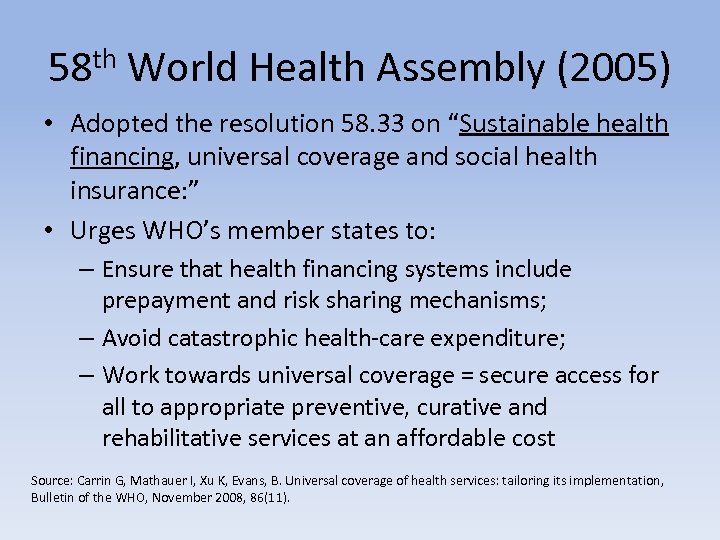 58 th World Health Assembly (2005) • Adopted the resolution 58. 33 on “Sustainable health financing, universal coverage and social health insurance: ” • Urges WHO’s member states to: – Ensure that health financing systems include prepayment and risk sharing mechanisms; – Avoid catastrophic health-care expenditure; – Work towards universal coverage = secure access for all to appropriate preventive, curative and rehabilitative services at an affordable cost Source: Carrin G, Mathauer I, Xu K, Evans, B. Universal coverage of health services: tailoring its implementation, Bulletin of the WHO, November 2008, 86(11).
58 th World Health Assembly (2005) • Adopted the resolution 58. 33 on “Sustainable health financing, universal coverage and social health insurance: ” • Urges WHO’s member states to: – Ensure that health financing systems include prepayment and risk sharing mechanisms; – Avoid catastrophic health-care expenditure; – Work towards universal coverage = secure access for all to appropriate preventive, curative and rehabilitative services at an affordable cost Source: Carrin G, Mathauer I, Xu K, Evans, B. Universal coverage of health services: tailoring its implementation, Bulletin of the WHO, November 2008, 86(11).
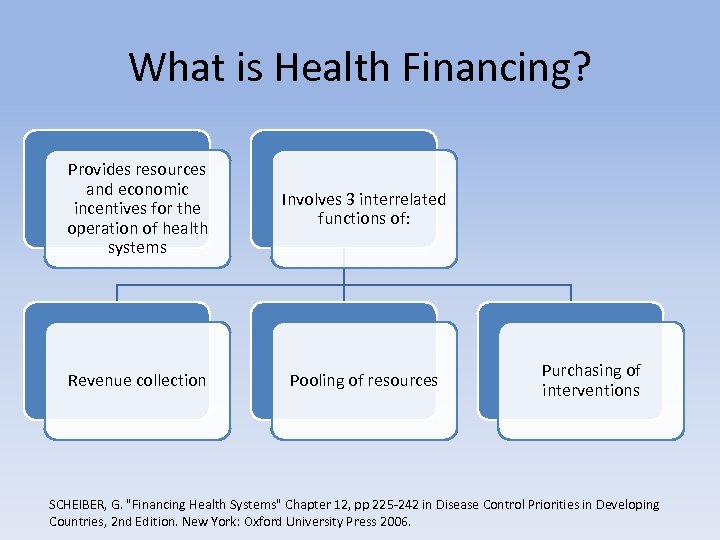 What is Health Financing? Provides resources and economic incentives for the operation of health systems Involves 3 interrelated functions of: Revenue collection Pooling of resources Purchasing of interventions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
What is Health Financing? Provides resources and economic incentives for the operation of health systems Involves 3 interrelated functions of: Revenue collection Pooling of resources Purchasing of interventions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
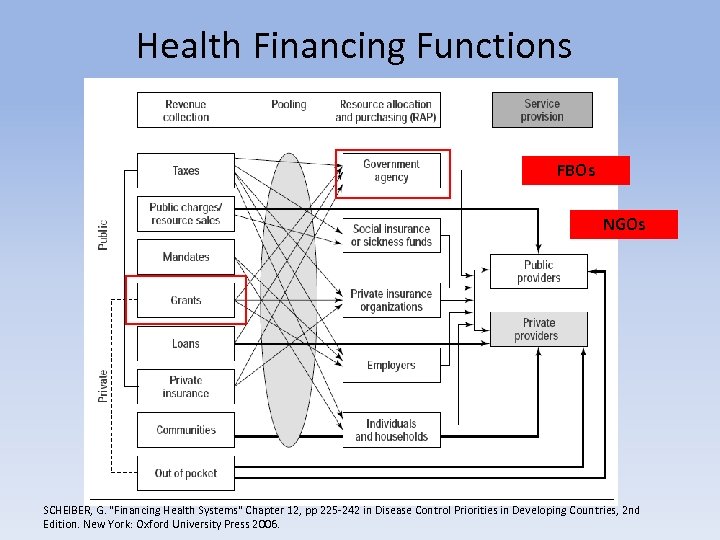 Health Financing Functions FBOs NGOs SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
Health Financing Functions FBOs NGOs SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
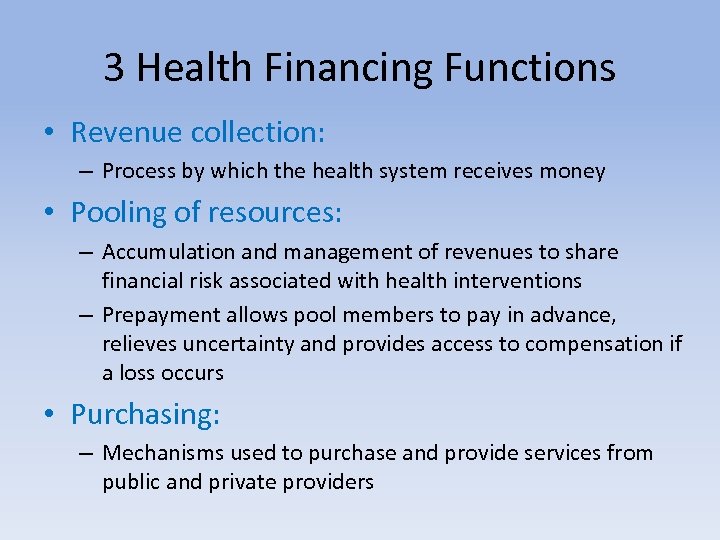 3 Health Financing Functions • Revenue collection: – Process by which the health system receives money • Pooling of resources: – Accumulation and management of revenues to share financial risk associated with health interventions – Prepayment allows pool members to pay in advance, relieves uncertainty and provides access to compensation if a loss occurs • Purchasing: – Mechanisms used to purchase and provide services from public and private providers
3 Health Financing Functions • Revenue collection: – Process by which the health system receives money • Pooling of resources: – Accumulation and management of revenues to share financial risk associated with health interventions – Prepayment allows pool members to pay in advance, relieves uncertainty and provides access to compensation if a loss occurs • Purchasing: – Mechanisms used to purchase and provide services from public and private providers
 3 Health Financing Functions • Raise sufficient and sustainable revenues in an efficient and equitable manner to provide: – Basic package of essential services – Financial protection against financial loss due to illness or injury • Managing revenues to equitably and efficiently pool health risks • Ensuring the purchase of health services in an allocatively and technically efficient manner SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
3 Health Financing Functions • Raise sufficient and sustainable revenues in an efficient and equitable manner to provide: – Basic package of essential services – Financial protection against financial loss due to illness or injury • Managing revenues to equitably and efficiently pool health risks • Ensuring the purchase of health services in an allocatively and technically efficient manner SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
 Fiscal Sustainability Generally been defined in terms of self-sufficiency: “Over a specific period, the managing entity will generate sufficient resources to fund the full costs of a particular program, sector, or economy, including the incremental service costs associated with new investments and the servicing and repayment of external debt. ” SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
Fiscal Sustainability Generally been defined in terms of self-sufficiency: “Over a specific period, the managing entity will generate sufficient resources to fund the full costs of a particular program, sector, or economy, including the incremental service costs associated with new investments and the servicing and repayment of external debt. ” SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
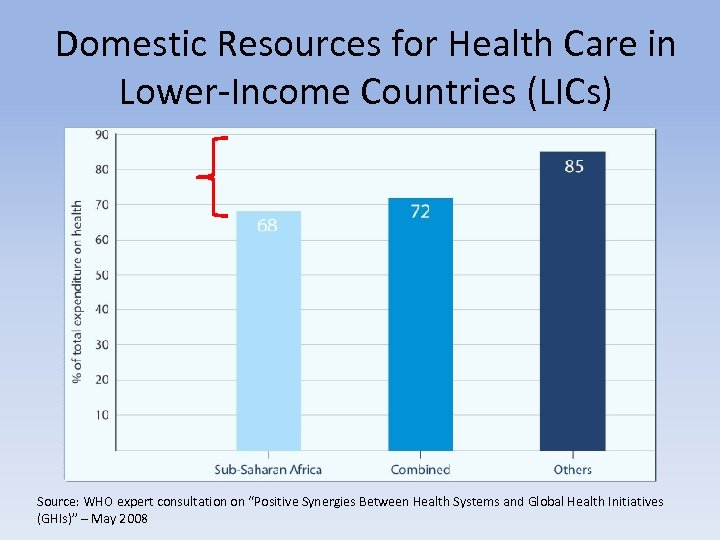 Domestic Resources for Health Care in Lower-Income Countries (LICs) Source: WHO expert consultation on “Positive Synergies Between Health Systems and Global Health Initiatives (GHIs)” – May 2008
Domestic Resources for Health Care in Lower-Income Countries (LICs) Source: WHO expert consultation on “Positive Synergies Between Health Systems and Global Health Initiatives (GHIs)” – May 2008
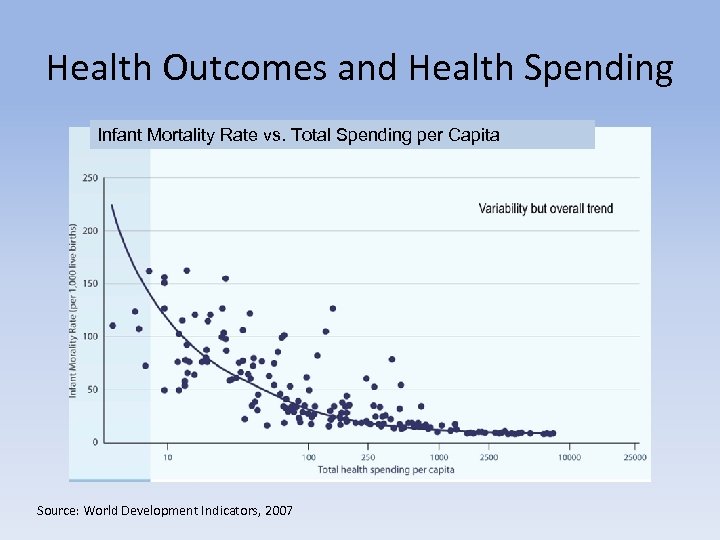 Health Outcomes and Health Spending Infant Mortality Rate vs. Total Spending per Capita Source: World Development Indicators, 2007
Health Outcomes and Health Spending Infant Mortality Rate vs. Total Spending per Capita Source: World Development Indicators, 2007
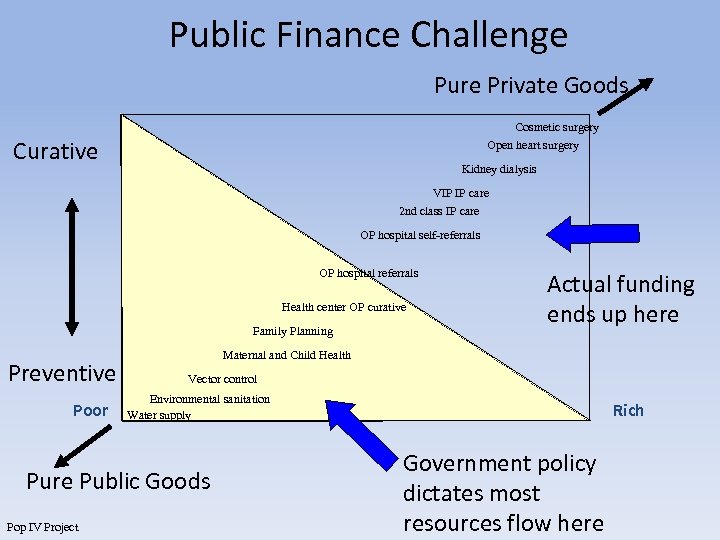 Public Finance Challenge Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis VIP IP care 2 nd class IP care OP hospital self-referrals OP hospital referrals Health center OP curative Family Planning Preventive Poor Maternal and Child Health Vector control Environmental sanitation Water supply Pure Public Goods Pop IV Project Actual funding ends up here Rich Government policy dictates most resources flow here
Public Finance Challenge Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis VIP IP care 2 nd class IP care OP hospital self-referrals OP hospital referrals Health center OP curative Family Planning Preventive Poor Maternal and Child Health Vector control Environmental sanitation Water supply Pure Public Goods Pop IV Project Actual funding ends up here Rich Government policy dictates most resources flow here
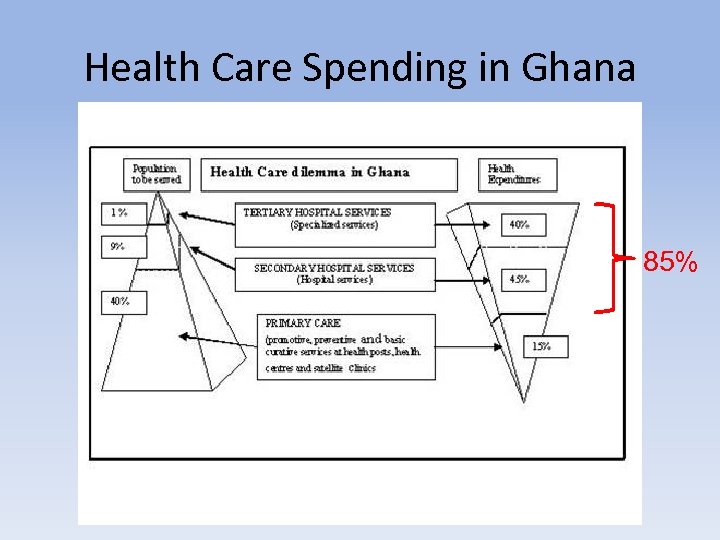 Health Care Spending in Ghana 85%
Health Care Spending in Ghana 85%
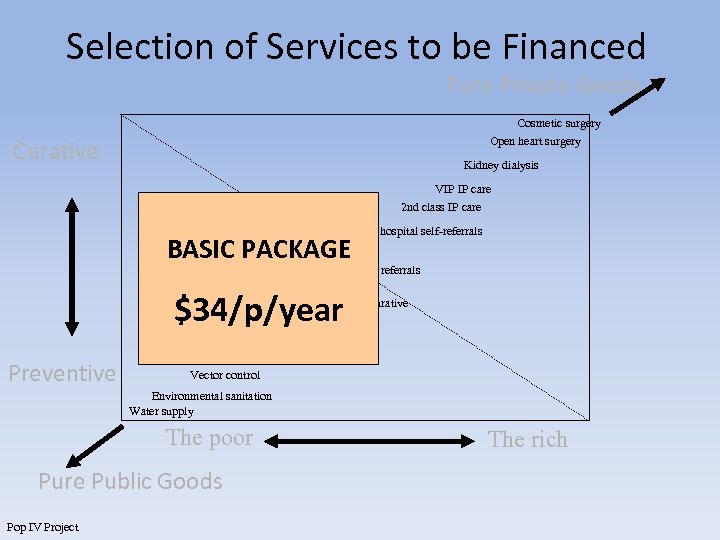 Selection of Services to be Financed Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis VIP IP care 2 nd class IP care BASIC PACKAGE OP hospital self-referrals OP hospital referrals $34/p/year Health center OP curative Family Planning Preventive Maternal and Child Health Vector control Environmental sanitation Water supply The poor Pure Public Goods Pop IV Project The rich
Selection of Services to be Financed Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis VIP IP care 2 nd class IP care BASIC PACKAGE OP hospital self-referrals OP hospital referrals $34/p/year Health center OP curative Family Planning Preventive Maternal and Child Health Vector control Environmental sanitation Water supply The poor Pure Public Goods Pop IV Project The rich
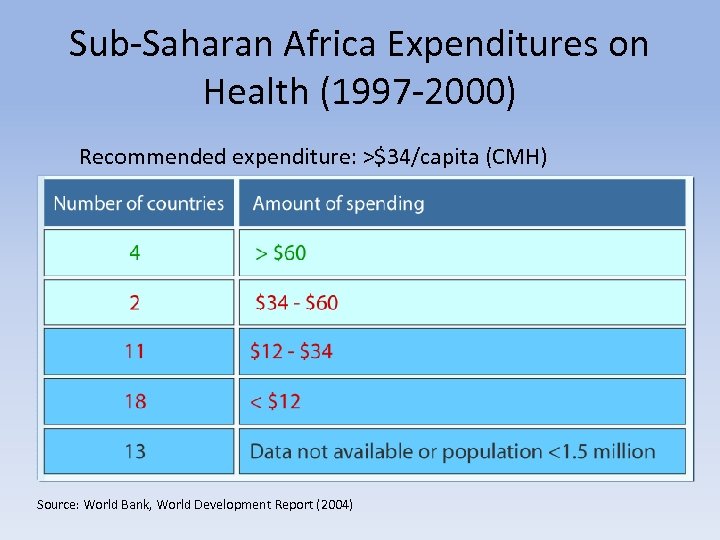 Sub-Saharan Africa Expenditures on Health (1997 -2000) Recommended expenditure: >$34/capita (CMH) Source: World Bank, World Development Report (2004)
Sub-Saharan Africa Expenditures on Health (1997 -2000) Recommended expenditure: >$34/capita (CMH) Source: World Bank, World Development Report (2004)
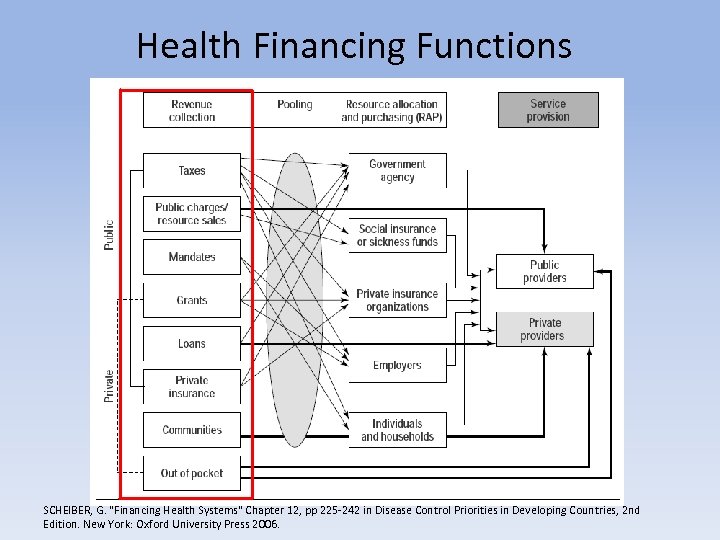 Health Financing Functions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
Health Financing Functions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
 Key Issues of Revenue Collection • Mobilize enough resources to finance expenditures for basic public and personal health services WITHOUT resorting to public sector borrowing (Tanzi and Zee 2000) • Raise revenues equitably and efficiently • Various types of organizations eventually receive funds • Conform with international standards SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
Key Issues of Revenue Collection • Mobilize enough resources to finance expenditures for basic public and personal health services WITHOUT resorting to public sector borrowing (Tanzi and Zee 2000) • Raise revenues equitably and efficiently • Various types of organizations eventually receive funds • Conform with international standards SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
 Types of Revenue Collection • • • Out-of-pocket payments (ex. user fees) Tax-based financing Types of Social Health Insurance (SHI) Prepayment Voluntary private insurance Community-based financing Prepayment makes risk sharing possible…
Types of Revenue Collection • • • Out-of-pocket payments (ex. user fees) Tax-based financing Types of Social Health Insurance (SHI) Prepayment Voluntary private insurance Community-based financing Prepayment makes risk sharing possible…
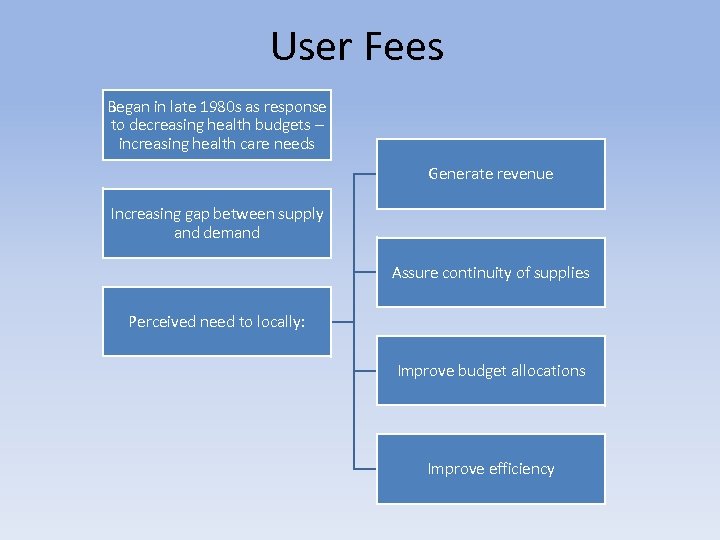 User Fees Began in late 1980 s as response to decreasing health budgets – increasing health care needs Generate revenue Increasing gap between supply and demand Assure continuity of supplies Perceived need to locally: Improve budget allocations Improve efficiency
User Fees Began in late 1980 s as response to decreasing health budgets – increasing health care needs Generate revenue Increasing gap between supply and demand Assure continuity of supplies Perceived need to locally: Improve budget allocations Improve efficiency
 User Fees • Characteristics: – Pay as you go - no risk pooling – Incentive effects – More resources directly for health • Evidence: – – Can raise significant revenue Frequent misuse of collected funds Frequent poor design and planning Highly political and controversial Source: Lagarde, M and Palmer, N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bulletin of the WHO, November 2008, 86(11).
User Fees • Characteristics: – Pay as you go - no risk pooling – Incentive effects – More resources directly for health • Evidence: – – Can raise significant revenue Frequent misuse of collected funds Frequent poor design and planning Highly political and controversial Source: Lagarde, M and Palmer, N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bulletin of the WHO, November 2008, 86(11).
 General Taxation • Characteristics: – Usually collected by the Ministry of Finance – as main source of revenue and serves the general population. – Mobilizes funds from everyone regardless of their health status, income, or occupation – Pools health risks across a large contributing population • Evidence: – Mildly regressive to progressive – Inequitable access for the poor – Reducing individual responsibility for one's own health? Source: Tax Based Financing for Health Systems: Options and Experiences, Discussion Paper #4, World Health Organization (2004).
General Taxation • Characteristics: – Usually collected by the Ministry of Finance – as main source of revenue and serves the general population. – Mobilizes funds from everyone regardless of their health status, income, or occupation – Pools health risks across a large contributing population • Evidence: – Mildly regressive to progressive – Inequitable access for the poor – Reducing individual responsibility for one's own health? Source: Tax Based Financing for Health Systems: Options and Experiences, Discussion Paper #4, World Health Organization (2004).
 Social Health Insurance (SHI) • Characteristics: – Mandatory participation – Large risk pools – Social solidarity • Evidence: – Covers people primarily in formal sector – May increase disparities between income groups
Social Health Insurance (SHI) • Characteristics: – Mandatory participation – Large risk pools – Social solidarity • Evidence: – Covers people primarily in formal sector – May increase disparities between income groups
 Voluntary Private Health Insurance • Characteristics: – Risk pooling – Payment based on ability and risk – Access based on payment • Evidence: – Generally not pro-poor – High-risk subscribers dropped or pay more – Rich capture more benefits
Voluntary Private Health Insurance • Characteristics: – Risk pooling – Payment based on ability and risk – Access based on payment • Evidence: – Generally not pro-poor – High-risk subscribers dropped or pay more – Rich capture more benefits
 Community-Based Financing • Bamako Initiative (1987) = “Women and children’s health through funding and management of essential drugs at the community level” • Characteristics: – Start up funds for basic equipment, provision of basic drugs, support costs – Drug charges to recover expenditures – as seed capital and for replenishment – Community health committees
Community-Based Financing • Bamako Initiative (1987) = “Women and children’s health through funding and management of essential drugs at the community level” • Characteristics: – Start up funds for basic equipment, provision of basic drugs, support costs – Drug charges to recover expenditures – as seed capital and for replenishment – Community health committees
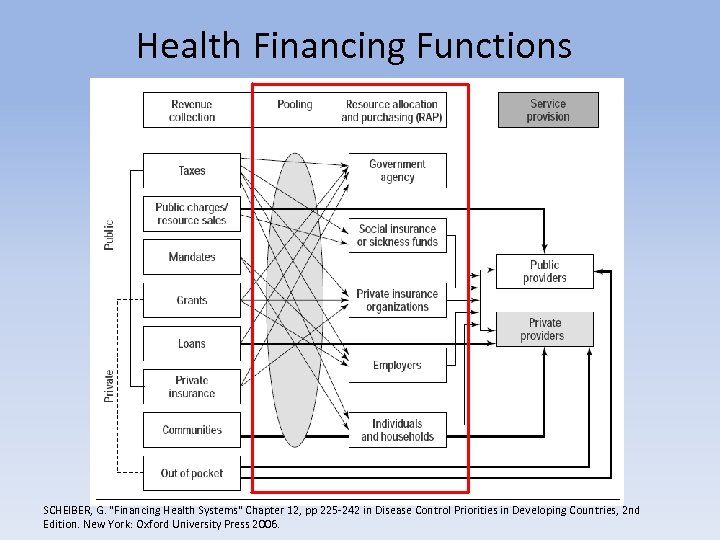 Health Financing Functions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
Health Financing Functions SCHEIBER, G. "Financing Health Systems" Chapter 12, pp 225 -242 in Disease Control Priorities in Developing Countries, 2 nd Edition. New York: Oxford University Press 2006.
 Pooling and Purchasing = Process to select interventions and pay for services and providers • Social Health Insurance • Community-Based Health Insurance • Other examples?
Pooling and Purchasing = Process to select interventions and pay for services and providers • Social Health Insurance • Community-Based Health Insurance • Other examples?
 New Health Care Reforms? • Changing role, size, spending in public sector • Transfer of responsibility to, promote expansion of and regulate NGO services • Addressing the nearly universal difference between policies and actual expenditure • Integration of services (IMCI, IMAI, IMPAC) • Operations (health systems) research
New Health Care Reforms? • Changing role, size, spending in public sector • Transfer of responsibility to, promote expansion of and regulate NGO services • Addressing the nearly universal difference between policies and actual expenditure • Integration of services (IMCI, IMAI, IMPAC) • Operations (health systems) research
 Community-Based Health Insurance (CBHI) • Principles: – Small risk pools – Social solidarity on small scale • Evidence: – – – Can enhance financial access to limited care Primarily curative oriented Geographic inequities (closer is better) Government’s re-distributive role important Generally failed to meet expectations
Community-Based Health Insurance (CBHI) • Principles: – Small risk pools – Social solidarity on small scale • Evidence: – – – Can enhance financial access to limited care Primarily curative oriented Geographic inequities (closer is better) Government’s re-distributive role important Generally failed to meet expectations
 CBHI Evidence Base General: • evidence base is limited in scope and questionable in quality • the effects are small and schemes serve only a limited section of the population Specifics: • strong evidence CBHI provides some financial protection by reducing out-of-pocket spending • moderate strength evidence that such schemes improve cost-recovery. • no evidence that schemes have an effect on the quality of care or the efficiency with which care is produced • these types of community financing arrangements are, at best, complementary to other more effective systems of health financing. • Regarding the costs and the benefits of various financing options, the current evidence base is mute on this point Ekman B. Health Policy Plan. 2004 Sep; 19(5): 249 -70.
CBHI Evidence Base General: • evidence base is limited in scope and questionable in quality • the effects are small and schemes serve only a limited section of the population Specifics: • strong evidence CBHI provides some financial protection by reducing out-of-pocket spending • moderate strength evidence that such schemes improve cost-recovery. • no evidence that schemes have an effect on the quality of care or the efficiency with which care is produced • these types of community financing arrangements are, at best, complementary to other more effective systems of health financing. • Regarding the costs and the benefits of various financing options, the current evidence base is mute on this point Ekman B. Health Policy Plan. 2004 Sep; 19(5): 249 -70.
 Decentralization • Transfer of fiscal, administrative, and/or political authority for planning, management and service delivery to lower levels of government. • Most often done for reasons beyond health • One pure model does not exist
Decentralization • Transfer of fiscal, administrative, and/or political authority for planning, management and service delivery to lower levels of government. • Most often done for reasons beyond health • One pure model does not exist
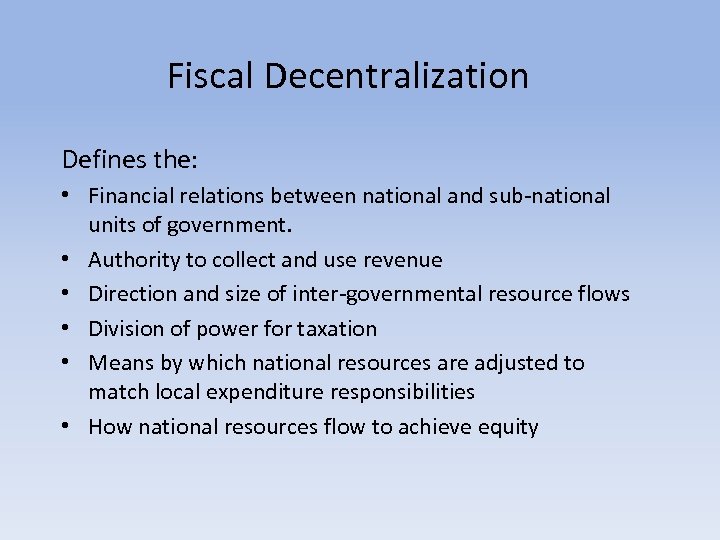 Fiscal Decentralization Defines the: • Financial relations between national and sub-national units of government. • Authority to collect and use revenue • Direction and size of inter-governmental resource flows • Division of power for taxation • Means by which national resources are adjusted to match local expenditure responsibilities • How national resources flow to achieve equity
Fiscal Decentralization Defines the: • Financial relations between national and sub-national units of government. • Authority to collect and use revenue • Direction and size of inter-governmental resource flows • Division of power for taxation • Means by which national resources are adjusted to match local expenditure responsibilities • How national resources flow to achieve equity
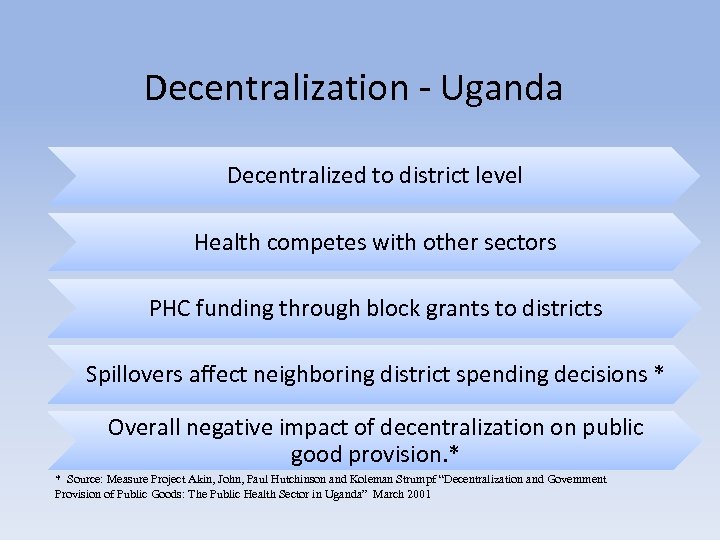 Decentralization - Uganda Decentralized to district level Health competes with other sectors PHC funding through block grants to districts Spillovers affect neighboring district spending decisions * Overall negative impact of decentralization on public good provision. * * Source: Measure Project Akin, John, Paul Hutchinson and Koleman Strumpf “Decentralization and Government Provision of Public Goods: The Public Health Sector in Uganda” March 2001
Decentralization - Uganda Decentralized to district level Health competes with other sectors PHC funding through block grants to districts Spillovers affect neighboring district spending decisions * Overall negative impact of decentralization on public good provision. * * Source: Measure Project Akin, John, Paul Hutchinson and Koleman Strumpf “Decentralization and Government Provision of Public Goods: The Public Health Sector in Uganda” March 2001
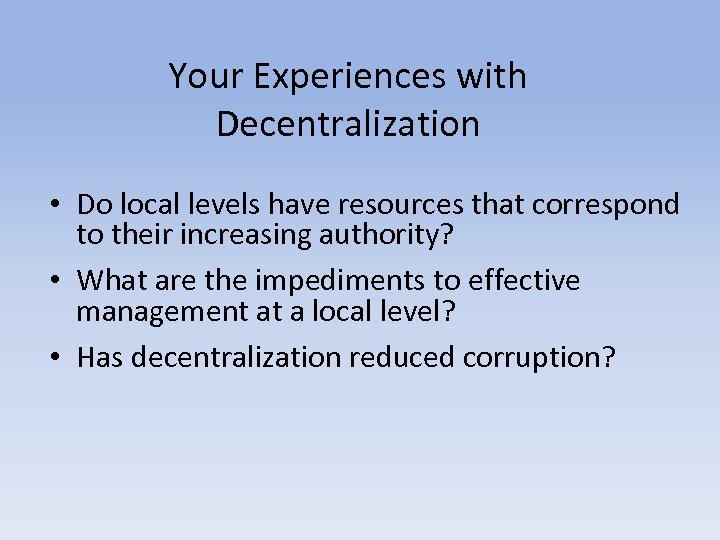 Your Experiences with Decentralization • Do local levels have resources that correspond to their increasing authority? • What are the impediments to effective management at a local level? • Has decentralization reduced corruption?
Your Experiences with Decentralization • Do local levels have resources that correspond to their increasing authority? • What are the impediments to effective management at a local level? • Has decentralization reduced corruption?
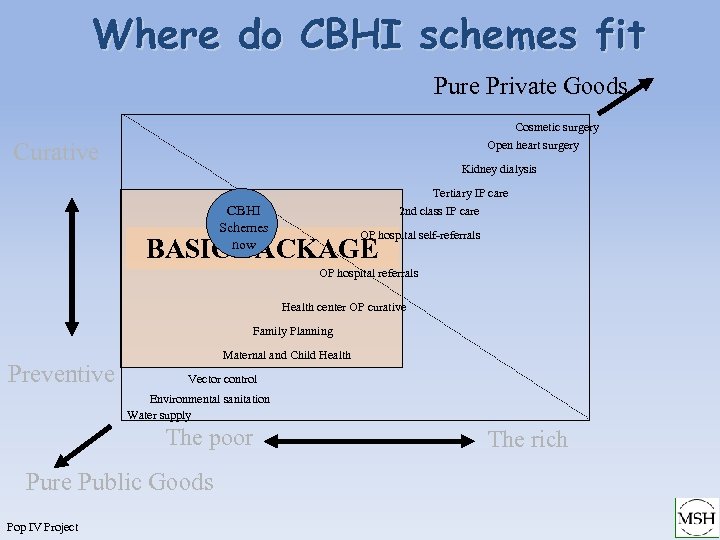 Where do CBHI schemes fit Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis Tertiary IP care 2 nd class IP care CBHI Schemes now OP hospital self-referrals BASIC PACKAGE OP hospital referrals Health center OP curative Family Planning Preventive Maternal and Child Health Vector control Environmental sanitation Water supply The poor Pure Public Goods Pop IV Project The rich
Where do CBHI schemes fit Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis Tertiary IP care 2 nd class IP care CBHI Schemes now OP hospital self-referrals BASIC PACKAGE OP hospital referrals Health center OP curative Family Planning Preventive Maternal and Child Health Vector control Environmental sanitation Water supply The poor Pure Public Goods Pop IV Project The rich
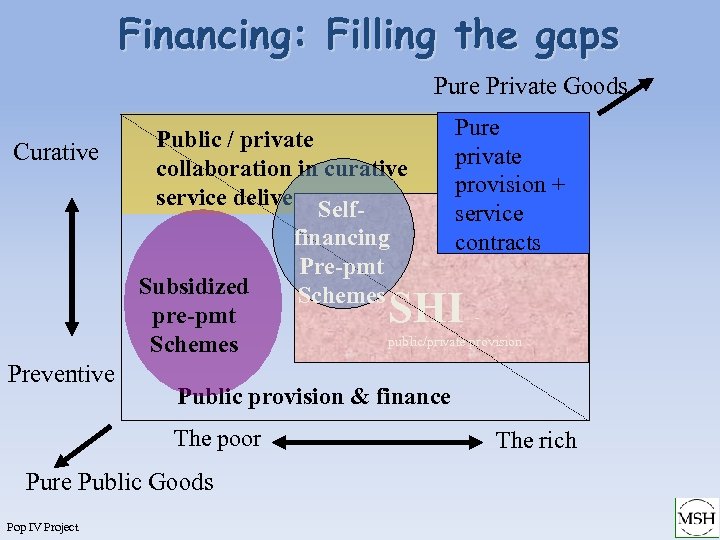 Financing: Filling the gaps Pure Private Goods Curative Public / private collaboration in curative service delivery Self. Subsidized pre-pmt Schemes Preventive SHI - public/private provision Public provision & finance The poor Pure Public Goods Pop IV Project financing Pre-pmt Schemes Pure private provision + service contracts The rich
Financing: Filling the gaps Pure Private Goods Curative Public / private collaboration in curative service delivery Self. Subsidized pre-pmt Schemes Preventive SHI - public/private provision Public provision & finance The poor Pure Public Goods Pop IV Project financing Pre-pmt Schemes Pure private provision + service contracts The rich
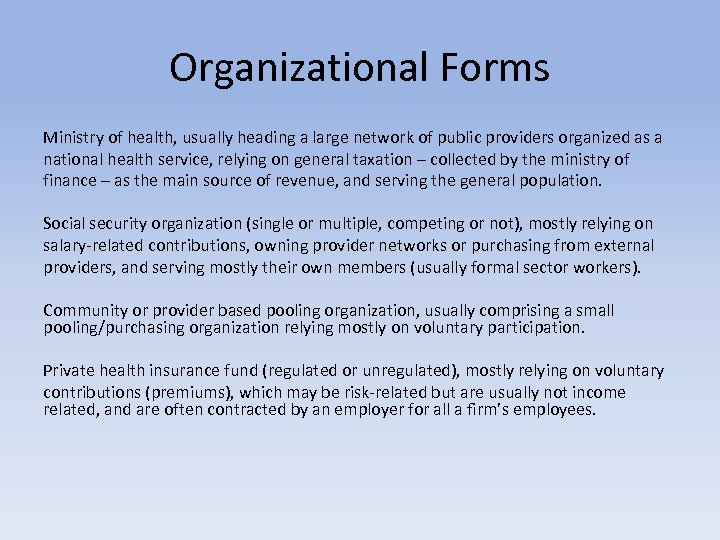 Organizational Forms Ministry of health, usually heading a large network of public providers organized as a national health service, relying on general taxation – collected by the ministry of finance – as the main source of revenue, and serving the general population. Social security organization (single or multiple, competing or not), mostly relying on salary-related contributions, owning provider networks or purchasing from external providers, and serving mostly their own members (usually formal sector workers). Community or provider based pooling organization, usually comprising a small pooling/purchasing organization relying mostly on voluntary participation. Private health insurance fund (regulated or unregulated), mostly relying on voluntary contributions (premiums), which may be risk-related but are usually not income related, and are often contracted by an employer for all a firm’s employees.
Organizational Forms Ministry of health, usually heading a large network of public providers organized as a national health service, relying on general taxation – collected by the ministry of finance – as the main source of revenue, and serving the general population. Social security organization (single or multiple, competing or not), mostly relying on salary-related contributions, owning provider networks or purchasing from external providers, and serving mostly their own members (usually formal sector workers). Community or provider based pooling organization, usually comprising a small pooling/purchasing organization relying mostly on voluntary participation. Private health insurance fund (regulated or unregulated), mostly relying on voluntary contributions (premiums), which may be risk-related but are usually not income related, and are often contracted by an employer for all a firm’s employees.
 Health Care Reform • Not enough funds for basic care • Misallocation - 80% of resources tend to go toward richest 10% of population, urban/rural inequities. For example, surgery for cancers rather than FP, treatment of TB, STI. • Inequity - poor lack basic access to HCare • Inefficiency – in allocation of health workers, purchase of drugs • Inadequate recurrent budgets - lack of maintenance; logistic problems; poor quality services; low productivity, poor access • Little control over local resources – peripheral health facilities often have disproportionately low resources for population served
Health Care Reform • Not enough funds for basic care • Misallocation - 80% of resources tend to go toward richest 10% of population, urban/rural inequities. For example, surgery for cancers rather than FP, treatment of TB, STI. • Inequity - poor lack basic access to HCare • Inefficiency – in allocation of health workers, purchase of drugs • Inadequate recurrent budgets - lack of maintenance; logistic problems; poor quality services; low productivity, poor access • Little control over local resources – peripheral health facilities often have disproportionately low resources for population served
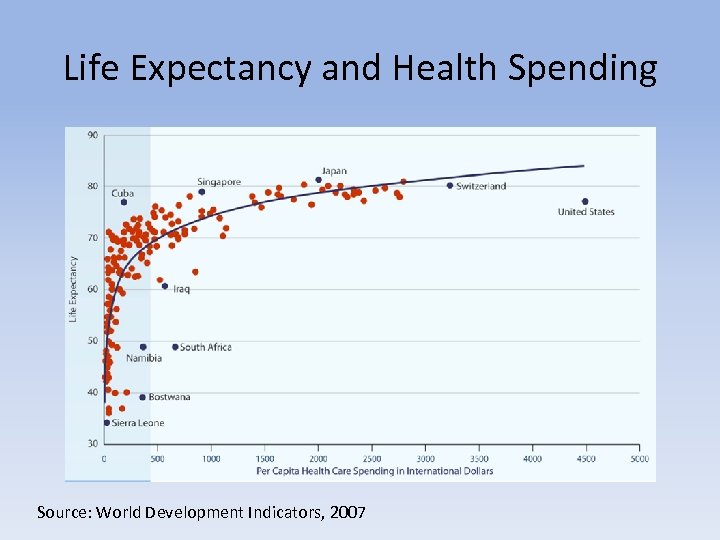 Life Expectancy and Health Spending Source: World Development Indicators, 2007
Life Expectancy and Health Spending Source: World Development Indicators, 2007



