4673431157ef0d7f08dcda6c021137ce.ppt
- Количество слайдов: 48
Fertility transitions and induced abortion Dr Ernestina Coast e. coast@lse. ac. uk
Two objectives < Macro relationships < Abortion and fertility < Contraception-abortion paradox < Language and data < Micro perspectives < Pregnancy termination trajectories in Zambia
Global scale < 96 million unplanned pregnancies per year < Unplanned < 33 ≠ unwanted million estimated unintended pregnancies as a result of method failure or ineffective use
Abortion: end point of a set of events sex contraceptive use (non-use/ineffective use/failure) a pregnancy a decision to terminate access to abortion (safe/unsafe/legal/illegal) abortion morbidity / mortality
Abortion and fertility TFR = TF × Cm × Ci × Ca × Cc TF = total fecundity Cm = index of marriage Ci = postpartum infecundability Ca = induced abortion Cc = contraception
Abortion and fertility TFR = TF × Cm × Ci × Ca × Cc TF = total fecundity Cm = index of marriage Ci = postpartum infecundability Ca = induced abortion Cc = contraception
Induced abortion: data < Much Demographic & Health Survey data unusable: < “Did you have any miscarriages, abortions or stillbirths that ended before 2002? ” < Few reliable national estimates globally < Rare and non-representative < Few data of use to policymakers
< How, and to what extent, are rates of induced abortion and contraception related?
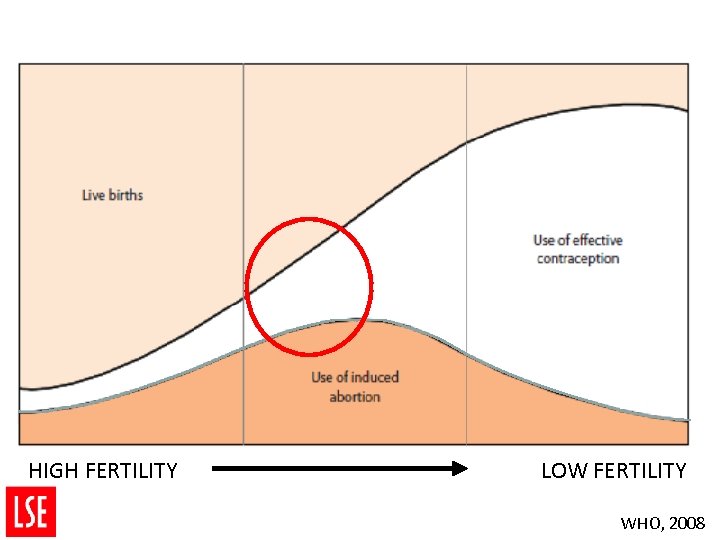
HIGH FERTILITY LOW FERTILITY WHO, 2008
Abortion & unmet need < Abortion as an outcome of unmet need for effective contraception? < People are motivated to regulate their fertility <using behavioural methods <supplied contraception <Inaccessible <and/or <Inconsistently or incorrectly used

Contraception-abortion “paradox” < Unmet need for contraception is high < Contraceptive prevalence is low < Less-effective contraceptive methods prevail
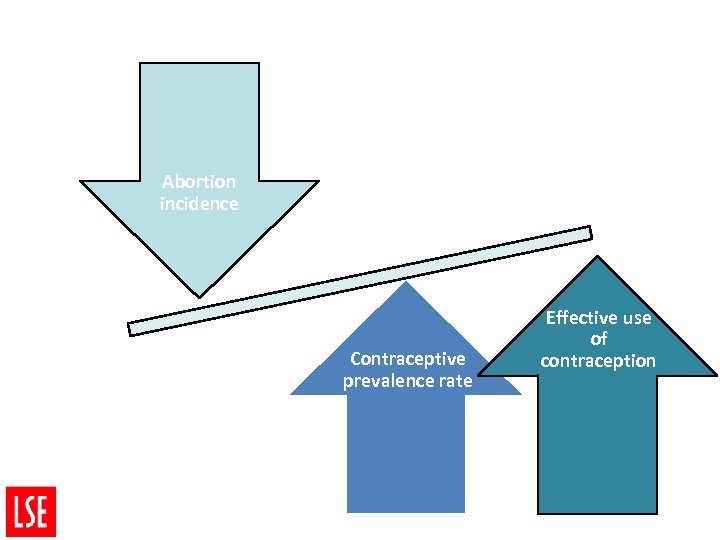
Abortion incidence Contraceptive prevalence rate Effective use of contraception
Intra-country variation < Urban-rural differentials in < Fertility < Unmet need < Effective contraceptive use (and access) < Likely to be echoed in < Urban-rural < Data (!) differentials in abortion rates
Language and data: pregnancy < Wanted vs. unwanted < Intended < Planned vs. unintended vs. unplanned


Data on (un)wanted / mistimed /(un)intended pregnancy < Survey data – posthoc rationalisation of “wantedness” (and then whether mistimed etc. ) < < retrospective Our Zambian data collected from women at the time of pregnancy termination < Unwanted at that point in time

Zambia: case study < Comparative study design - comparing the experiences of girls and women who seek <Safe abortion (SA) services <or <Post-abortion care (PAC) following an unsafe induced abortion
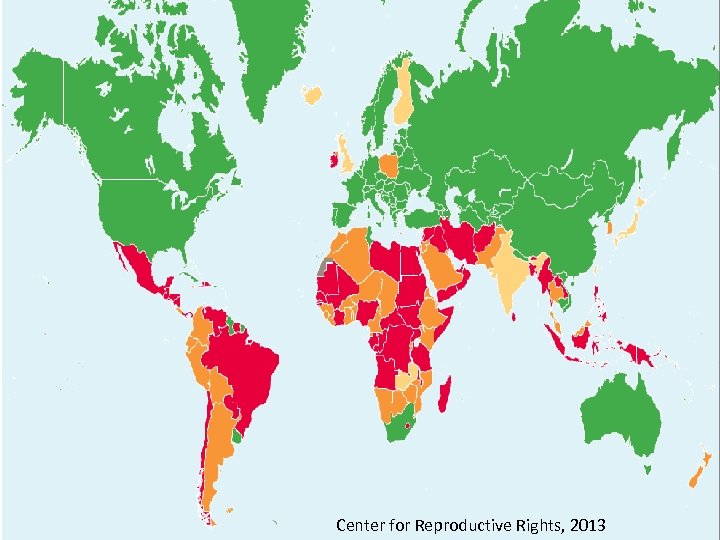
Center for Reproductive Rights, 2013
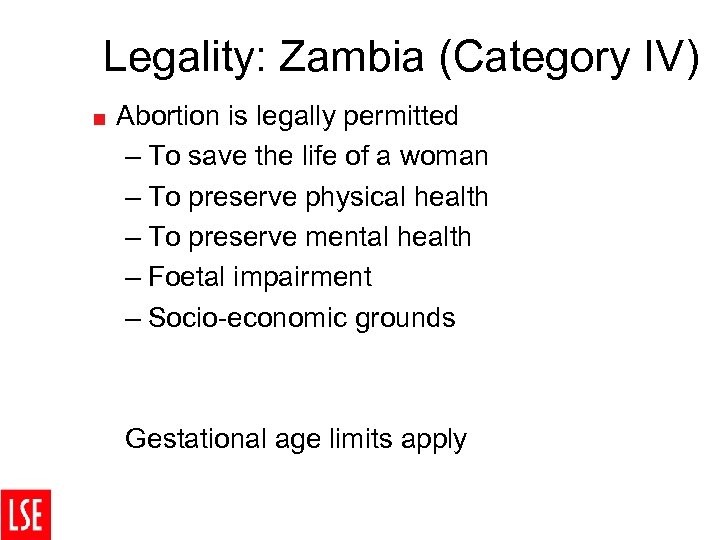
Legality: Zambia (Category IV) < Abortion is legally permitted – To save the life of a woman – To preserve physical health – To preserve mental health – Foetal impairment – Socio-economic grounds Gestational age limits apply
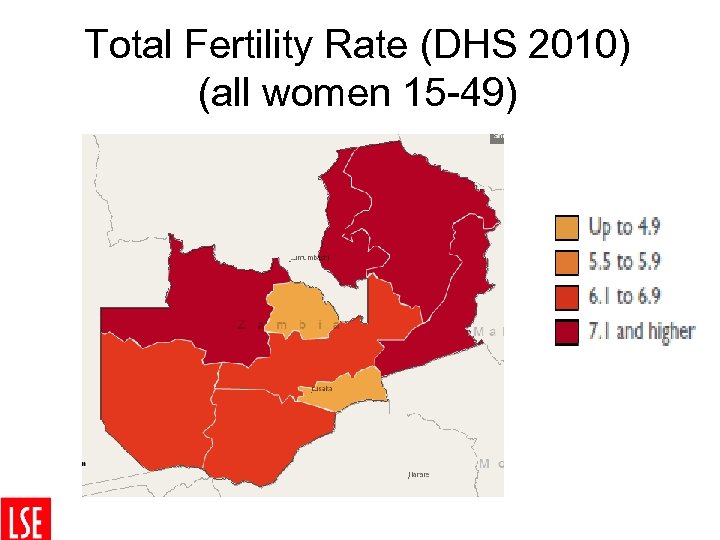
Zambia: Legality vs. services Legality of safe abortion Access to postabortion care Access to contraceptive services Adequate √ Medium Poor √ √ √
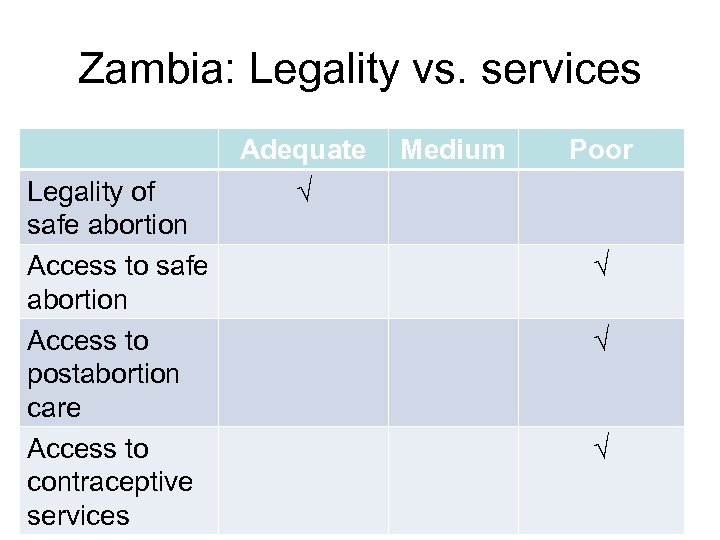
Total Fertility Rate (DHS 2010) (all women 15 -49)
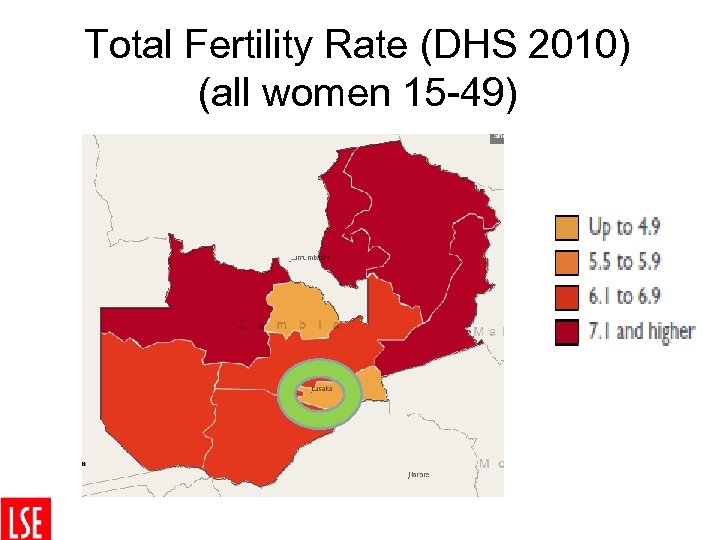
Total Fertility Rate (DHS 2010) (all women 15 -49)

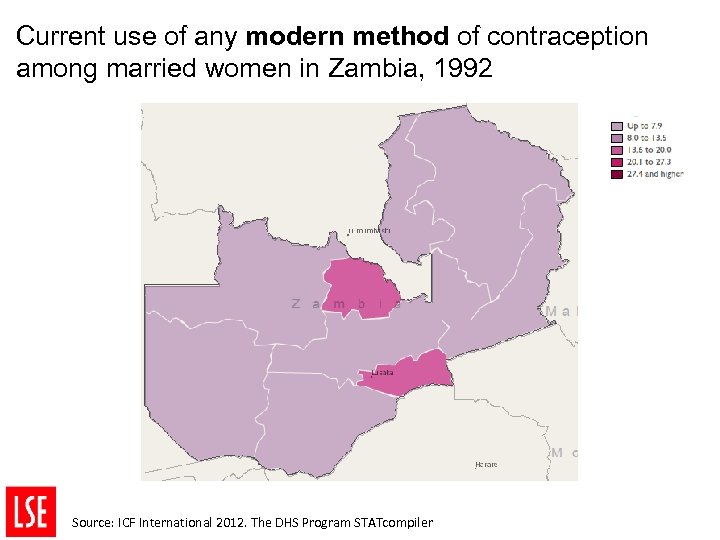
Current use of any modern method of contraception among married women in Zambia, 1992 Source: ICF International 2012. The DHS Program STATcompiler
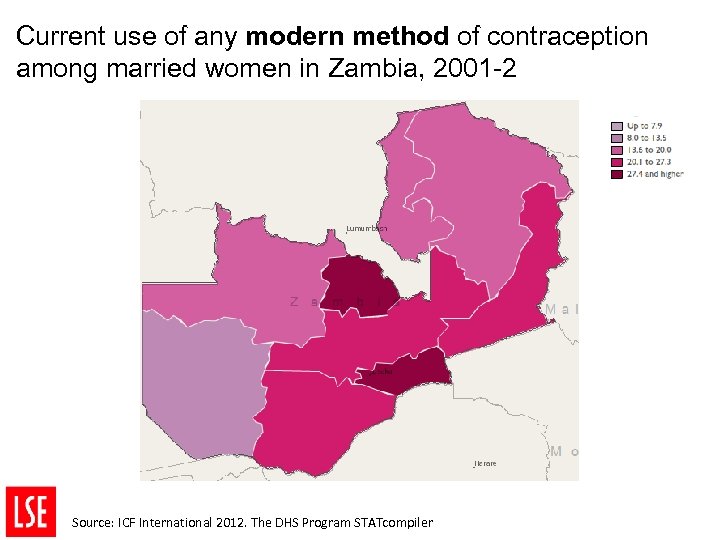
Current use of any modern method of contraception among married women in Zambia, 2001 -2 Source: ICF International 2012. The DHS Program STATcompiler
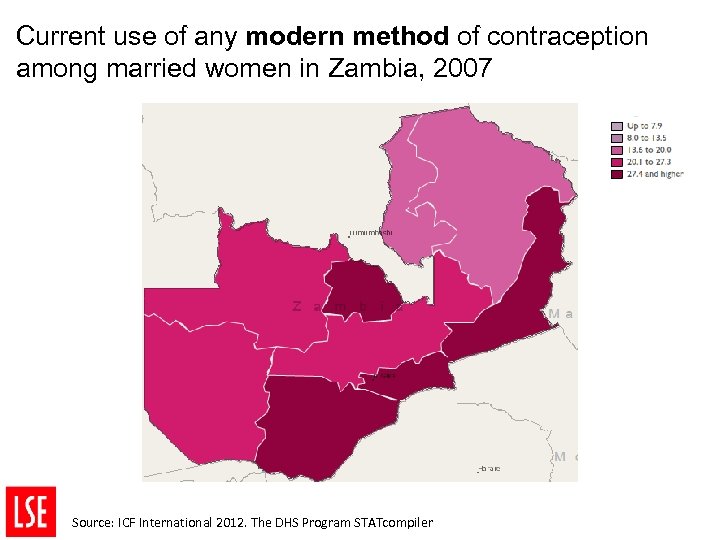
Current use of any modern method of contraception among married women in Zambia, 2007 Source: ICF International 2012. The DHS Program STATcompiler

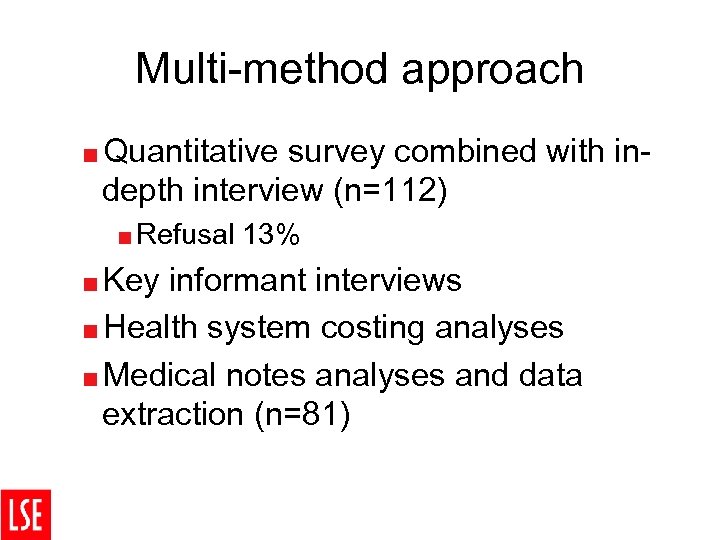
Multi-method approach <Quantitative survey combined with indepth interview (n=112) <Refusal <Key 13% informant interviews <Health system costing analyses <Medical notes analyses and data extraction (n=81)
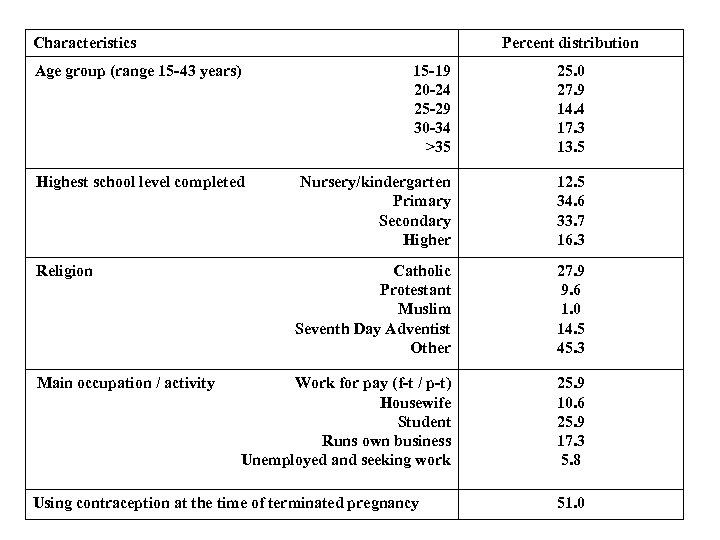
Characteristics Percent distribution Age group (range 15 -43 years) 15 -19 20 -24 25 -29 30 -34 >35 25. 0 27. 9 14. 4 17. 3 13. 5 Highest school level completed Nursery/kindergarten Primary Secondary Higher 12. 5 34. 6 33. 7 16. 3 Catholic Protestant Muslim Seventh Day Adventist Other 27. 9 9. 6 1. 0 14. 5 45. 3 Work for pay (f-t / p-t) Housewife Student Runs own business Unemployed and seeking work 25. 9 10. 6 25. 9 17. 3 5. 8 Religion Main occupation / activity Using contraception at the time of terminated pregnancy 51. 0


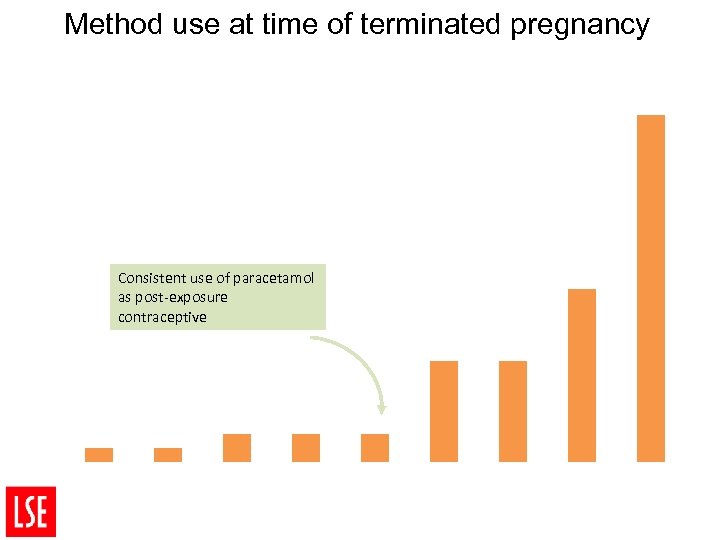
Method use at time of terminated pregnancy 45 % of women using contraceptives 40 35 30 25 20 Consistent use of paracetamol as post-exposure contraceptive 15 10 5 0 Female sterilisation IUD Implants Female condoms Other Injectables. Withdrawal Pill Male condom
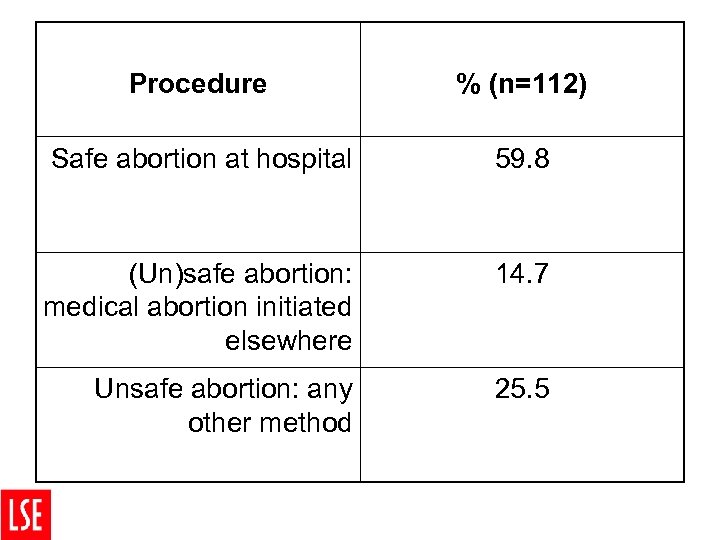
Procedure % (n=112) Safe abortion at hospital 59. 8 (Un)safe abortion: medical abortion initiated elsewhere 14. 7 Unsafe abortion: any other method 25. 5
Trajectories • Once the decision to terminate has occurred, the question is “How”? • Can be complex and iterative • Individuals navigate complex private and public health systems as well as unqualified “providers” in order to achieve their pregnancy termination. • Of those seeking PAC in our study, 15% had tried at least two different unsafe/unregulated methods before reaching the hospital for PAC.
Vignettes • Written by Research Assistants immediately after interview, and before translating and transcribing an interview. • NOT for analyses – Framework analyses of verbatim transcripts
Contraception: • A 32 year old woman who is married with four children. She is a very poor woman who is struggling with the up keep of her four children. The husband does not work and only depends on piece work to feed them. She does some piece work like washing of clothes just to earn some money for food. She was surprised to find out that she was pregnant because she was on a three months injectable contraceptive which was provided for free. The reason for attempting to terminate the pregnancy was because the cost of raising children is very expensive and already she was unable to send her four children to school. She had no money to even feed the family and so why would she have another child? The husband is not aware that she was pregnant and she intends to keep it that way.
Poor post-partum FP She is a 26 year old married woman with three children, the youngest of which is 7 months old. She runs a small business, baking scones which she sells in her shop. She went to the clinic to start her family planning pill but she was told to come back when her periods start, and was not given any contraceptive supplies. Getting pregnant came as a surprise to her, and she self-induced an abortion using unspecified pills. She intends to have a normal life when she goes home and wants to start her family planning pills.
Diffusion of SA knowledge A 20 year old school leaver who lives with her “Aunty” in Lusaka in order to help out with childcare. She comes from a poor family and decided to have a To. P because her mother is a widow and can’t afford to raise a child. The boyfriend responsible doesn’t know anything about her being pregnant and he is no longer answering his phone. When she told her Aunty that she was pregnant, it was the Aunty who arranged with a Doctor for her to have a TOP and made a down payment of k 100 against the k 300 demanded by the doctor. The Doctor refused to complete treatment without full payment in advance, so the Aunty had to raise the balance and make a return visit, after which the respondent was treated and given a medical abortion.
Male involvement • After agreeing with the boyfriend to remove the pregnancy, they went together to a Clinic where they were seen by a friend of her boyfriend’s. She knew that her boyfriend had paid for this consultation, but did not know how much. She was given three tablets and told to insert them at home. After four days, the bleeding stopped. After two weeks she bled again and after another two weeks, clots started coming out. She went to visit her mother who noticed that she was pale and weak and that she had blood on her leg. She told her mother about what had happened and her mother took her to another clinic where they gave her injections and the bleeding stopped. After two weeks, she had stomach pains, came to a hospital, and was admitted for three nights. Scans revealed retained products in her uterus and severe infection.
Whose unwanted pregnancy? • She is a 20 year old school girl, who comes from a poor family and both her parents are dead. She lives with her widowed step-mother and some siblings. Her step-mother made her a herbal mix liquid and forced her to drink it in order to induce an abortion. The step-mother told her that if she did not terminate the pregnancy, she would be forced to leave the house. The respondent reported that the liquid gave her terrible stomach pains. It was a school friend who told her about the services available at the hospital, and she arrived at the hospital with no money. Once at the hospital she was provided with a medical abortion, and the standard registration fee for a medical card was waived because she was unable to pay for it. When she goes home, she thinks her step-mother will shout at her because she said she had gone to school, and she came to the hospital secretly. However, she said she will tell her stepmother about removing the pregnancy so that she stops forcing her to drink herbal drugs.
Pregnancy “wantedness” I: R: Feel free. You can tell me. Did you want to keep? How did you feel after finding out that you are pregnant? Yes, I wanted to keep it. You wanted to keep it. So what then happened next? I was told that there was no way that I would take care of this child. Who said that to you? My mother and my father. Okay I was asked “How I would care for that child? Where would I find clothes and how I would finish school? ”
Emergent policy issues
Safe vs unsafe • Is this dichotomy less useful given wife availability of medical abortion drugs? • Substantial proportions of girls and women procure a less-risky “unsafe” medical abortion • Lower risk unsafe abortion – Initiate termination using MA drugs
< Zambia Project Team: < < < Dr Ernestina Coast (P. I. ) Dr Tiziana Leone Dr Divya Parmar Dr Ellie Hukin Dr Emily Freeman Dr Susan Murray (KCL) Dr Bellington Vwalika (UTH/UNZA) Dr Bornwell Sikateyo (UTH/UNZA) Erica Chifumpu (RA) Victoria Saina (RA) Taza Mwense (RA) Doreen George (RA)
< ESRC Impact Maximisation Grant < http: //personal. lse. ac. uk/coast/Zambia. TOP. htm < e. coast@lse. ac. uk
4673431157ef0d7f08dcda6c021137ce.ppt